User login
Prodrug infusion beats oral Parkinson’s disease therapy for motor symptoms
, according to a new study. The beneficial effects of these phosphate prodrugs of levodopa and carbidopa were most noticeable in the early morning, results of the phase 1B study showed.
As Parkinson’s disease progresses and dosing of oral levodopa/carbidopa (LD/CD) increases, its therapeutic window narrows, resulting in troublesome dyskinesia at peak drug levels and tremors and rigidity when levels fall.
“Foslevodopa/foscarbidopa shows lower ‘off’ time than oral levodopa/carbidopa, and this was statistically significant. Also, foslevodopa/foscarbidopa (fosL/fosC) showed more ‘on’ time without dyskinesia, compared with oral levodopa/carbidopa. This was also statistically significant,” lead author Sven Stodtmann, PhD, of AbbVie GmbH, Ludwigshafen, Germany, reported in his recorded presentation at the Movement Disorders Society’s 23rd International Congress of Parkinson’s Disease and Movement Disorder (Virtual) 2020.
Continuous infusion versus oral therapy
The analysis included 20 patients, and all data from these individuals were collected between 4:30 a.m. and 9:30 p.m.
Participants were 12 men and 8 women, aged 30-80 years, with advanced, idiopathic Parkinson’s disease responsive to levodopa but inadequately controlled on their current stable therapy, having a minimum of 2.5 off hours/day. Mean age was 61.3 plus or minus 10.5 years (range 35-77 years).
In this single-arm, open-label study, they received subcutaneous infusions of personalized therapeutic doses of fosL/fosC 24 hours/day for 28 days after a 10- to 30-day screening period during which they recorded LD/CD doses in a diary and had motor symptoms monitored using a wearable device.
Following the screening period, fosL/fosC doses were titrated over up to 5 days, with subsequent weekly study visits, for a total time on fosL/fosC of 28 days. Drug titration was aimed at maximizing functional on time and minimizing the number of off episodes while minimizing troublesome dyskinesia.
Continuous infusion of fosL/fosC performed better than oral LD/CD on all counts.
“The off time is much lower in the morning for people on foslevodopa/foscarbidopa [compared with oral LD/CD] because this is a 24-hour infusion product,” Dr. Stodtmann explained.
The effect was maintained over the course of the day with little fluctuation with fosL/fosC, off periods never exceeding about 25% between 4:30 a.m. and 9 p.m. For LD/CD, off periods were highest in the early morning and peaked at about 50% on a 3- to 4-hour cycle during the course of the day.
Increased on time without dyskinesia varied between about 60% and 80% during the day with fosL/fosC, showing the greatest difference between fosL/fosC and oral LD/CD in the early morning hours.
“On time with nontroublesome dyskinesia was lower for foscarbidopa/foslevodopa, compared to oral levodopa/carbidopa, but this was not statistically significant,” Dr. Stodtmann said. On time with troublesome dyskinesia followed the same pattern, again, not statistically significant.
Looking at the data another way, the investigators calculated the odds ratios of motor symptoms using fosL/fosC, compared with oral LD/CD. Use of fosL/fosC was associated with a 59% lower risk of being in the off state during the day, compared with oral LD/CD (odds ratio, 0.4; 95% confidence interval, 0.2-0.7; P < .01). Similarly, the probability of being in the on state without dyskinesia was much greater with fosL/fosC (OR, 2.75; 95% CI, 1.08-6.99; P < .05).
Encouraging, but more data needed
Indu Subramanian, MD, of the department of neurology at the University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education, and Clinical Center at the West Los Angeles Veterans Affairs Hospital, commented that the field has been waiting to see data on fosL/fosC.
“It seems like it’s pretty reasonable in terms of what the goals were, which is to improve stability of Parkinson’s symptoms, to improve off time and give on time without troublesome dyskinesia,” she said. “So I think those [goals] have been met.”
Dr. Subramanian, who was not involved with the research, said she would have liked to have seen results concerning safety of this drug formulation, which the presentation lacked, “because historically, there have been issues with nodule formation and skin breakdown, things like that, due to the stability of the product in the subcutaneous form. … So, always to my understanding, there has been this search for things that are tolerated in the subcutaneous delivery.”
If this formulation proves safe and tolerable, Dr. Subramanian sees a potential place for it for some patients with advanced Parkinson’s disease.
“Certainly a subcutaneous formulation will be better than something that requires … deep brain surgery or even a pump insertion like Duopa [carbidopa/levodopa enteral suspension, AbbVie] or something like that,” she said. “I think [it] would be beneficial over something with the gut because the gut historically has been a problem to rely on in advanced Parkinson’s patients due to slower transit times, and the gut itself is affected with Parkinson’s disease.”
Dr. Stodtmann and all coauthors are employees of AbbVie, which was the sponsor of the study and was responsible for all aspects of it. Dr. Subramanian has given talks for Acadia Pharmaceuticals and Acorda Therapeutics in the past.
A version of this article originally appeared on Medscape.com.
, according to a new study. The beneficial effects of these phosphate prodrugs of levodopa and carbidopa were most noticeable in the early morning, results of the phase 1B study showed.
As Parkinson’s disease progresses and dosing of oral levodopa/carbidopa (LD/CD) increases, its therapeutic window narrows, resulting in troublesome dyskinesia at peak drug levels and tremors and rigidity when levels fall.
“Foslevodopa/foscarbidopa shows lower ‘off’ time than oral levodopa/carbidopa, and this was statistically significant. Also, foslevodopa/foscarbidopa (fosL/fosC) showed more ‘on’ time without dyskinesia, compared with oral levodopa/carbidopa. This was also statistically significant,” lead author Sven Stodtmann, PhD, of AbbVie GmbH, Ludwigshafen, Germany, reported in his recorded presentation at the Movement Disorders Society’s 23rd International Congress of Parkinson’s Disease and Movement Disorder (Virtual) 2020.
Continuous infusion versus oral therapy
The analysis included 20 patients, and all data from these individuals were collected between 4:30 a.m. and 9:30 p.m.
Participants were 12 men and 8 women, aged 30-80 years, with advanced, idiopathic Parkinson’s disease responsive to levodopa but inadequately controlled on their current stable therapy, having a minimum of 2.5 off hours/day. Mean age was 61.3 plus or minus 10.5 years (range 35-77 years).
In this single-arm, open-label study, they received subcutaneous infusions of personalized therapeutic doses of fosL/fosC 24 hours/day for 28 days after a 10- to 30-day screening period during which they recorded LD/CD doses in a diary and had motor symptoms monitored using a wearable device.
Following the screening period, fosL/fosC doses were titrated over up to 5 days, with subsequent weekly study visits, for a total time on fosL/fosC of 28 days. Drug titration was aimed at maximizing functional on time and minimizing the number of off episodes while minimizing troublesome dyskinesia.
Continuous infusion of fosL/fosC performed better than oral LD/CD on all counts.
“The off time is much lower in the morning for people on foslevodopa/foscarbidopa [compared with oral LD/CD] because this is a 24-hour infusion product,” Dr. Stodtmann explained.
The effect was maintained over the course of the day with little fluctuation with fosL/fosC, off periods never exceeding about 25% between 4:30 a.m. and 9 p.m. For LD/CD, off periods were highest in the early morning and peaked at about 50% on a 3- to 4-hour cycle during the course of the day.
Increased on time without dyskinesia varied between about 60% and 80% during the day with fosL/fosC, showing the greatest difference between fosL/fosC and oral LD/CD in the early morning hours.
“On time with nontroublesome dyskinesia was lower for foscarbidopa/foslevodopa, compared to oral levodopa/carbidopa, but this was not statistically significant,” Dr. Stodtmann said. On time with troublesome dyskinesia followed the same pattern, again, not statistically significant.
Looking at the data another way, the investigators calculated the odds ratios of motor symptoms using fosL/fosC, compared with oral LD/CD. Use of fosL/fosC was associated with a 59% lower risk of being in the off state during the day, compared with oral LD/CD (odds ratio, 0.4; 95% confidence interval, 0.2-0.7; P < .01). Similarly, the probability of being in the on state without dyskinesia was much greater with fosL/fosC (OR, 2.75; 95% CI, 1.08-6.99; P < .05).
Encouraging, but more data needed
Indu Subramanian, MD, of the department of neurology at the University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education, and Clinical Center at the West Los Angeles Veterans Affairs Hospital, commented that the field has been waiting to see data on fosL/fosC.
“It seems like it’s pretty reasonable in terms of what the goals were, which is to improve stability of Parkinson’s symptoms, to improve off time and give on time without troublesome dyskinesia,” she said. “So I think those [goals] have been met.”
Dr. Subramanian, who was not involved with the research, said she would have liked to have seen results concerning safety of this drug formulation, which the presentation lacked, “because historically, there have been issues with nodule formation and skin breakdown, things like that, due to the stability of the product in the subcutaneous form. … So, always to my understanding, there has been this search for things that are tolerated in the subcutaneous delivery.”
If this formulation proves safe and tolerable, Dr. Subramanian sees a potential place for it for some patients with advanced Parkinson’s disease.
“Certainly a subcutaneous formulation will be better than something that requires … deep brain surgery or even a pump insertion like Duopa [carbidopa/levodopa enteral suspension, AbbVie] or something like that,” she said. “I think [it] would be beneficial over something with the gut because the gut historically has been a problem to rely on in advanced Parkinson’s patients due to slower transit times, and the gut itself is affected with Parkinson’s disease.”
Dr. Stodtmann and all coauthors are employees of AbbVie, which was the sponsor of the study and was responsible for all aspects of it. Dr. Subramanian has given talks for Acadia Pharmaceuticals and Acorda Therapeutics in the past.
A version of this article originally appeared on Medscape.com.
, according to a new study. The beneficial effects of these phosphate prodrugs of levodopa and carbidopa were most noticeable in the early morning, results of the phase 1B study showed.
As Parkinson’s disease progresses and dosing of oral levodopa/carbidopa (LD/CD) increases, its therapeutic window narrows, resulting in troublesome dyskinesia at peak drug levels and tremors and rigidity when levels fall.
“Foslevodopa/foscarbidopa shows lower ‘off’ time than oral levodopa/carbidopa, and this was statistically significant. Also, foslevodopa/foscarbidopa (fosL/fosC) showed more ‘on’ time without dyskinesia, compared with oral levodopa/carbidopa. This was also statistically significant,” lead author Sven Stodtmann, PhD, of AbbVie GmbH, Ludwigshafen, Germany, reported in his recorded presentation at the Movement Disorders Society’s 23rd International Congress of Parkinson’s Disease and Movement Disorder (Virtual) 2020.
Continuous infusion versus oral therapy
The analysis included 20 patients, and all data from these individuals were collected between 4:30 a.m. and 9:30 p.m.
Participants were 12 men and 8 women, aged 30-80 years, with advanced, idiopathic Parkinson’s disease responsive to levodopa but inadequately controlled on their current stable therapy, having a minimum of 2.5 off hours/day. Mean age was 61.3 plus or minus 10.5 years (range 35-77 years).
In this single-arm, open-label study, they received subcutaneous infusions of personalized therapeutic doses of fosL/fosC 24 hours/day for 28 days after a 10- to 30-day screening period during which they recorded LD/CD doses in a diary and had motor symptoms monitored using a wearable device.
Following the screening period, fosL/fosC doses were titrated over up to 5 days, with subsequent weekly study visits, for a total time on fosL/fosC of 28 days. Drug titration was aimed at maximizing functional on time and minimizing the number of off episodes while minimizing troublesome dyskinesia.
Continuous infusion of fosL/fosC performed better than oral LD/CD on all counts.
“The off time is much lower in the morning for people on foslevodopa/foscarbidopa [compared with oral LD/CD] because this is a 24-hour infusion product,” Dr. Stodtmann explained.
The effect was maintained over the course of the day with little fluctuation with fosL/fosC, off periods never exceeding about 25% between 4:30 a.m. and 9 p.m. For LD/CD, off periods were highest in the early morning and peaked at about 50% on a 3- to 4-hour cycle during the course of the day.
Increased on time without dyskinesia varied between about 60% and 80% during the day with fosL/fosC, showing the greatest difference between fosL/fosC and oral LD/CD in the early morning hours.
“On time with nontroublesome dyskinesia was lower for foscarbidopa/foslevodopa, compared to oral levodopa/carbidopa, but this was not statistically significant,” Dr. Stodtmann said. On time with troublesome dyskinesia followed the same pattern, again, not statistically significant.
Looking at the data another way, the investigators calculated the odds ratios of motor symptoms using fosL/fosC, compared with oral LD/CD. Use of fosL/fosC was associated with a 59% lower risk of being in the off state during the day, compared with oral LD/CD (odds ratio, 0.4; 95% confidence interval, 0.2-0.7; P < .01). Similarly, the probability of being in the on state without dyskinesia was much greater with fosL/fosC (OR, 2.75; 95% CI, 1.08-6.99; P < .05).
Encouraging, but more data needed
Indu Subramanian, MD, of the department of neurology at the University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education, and Clinical Center at the West Los Angeles Veterans Affairs Hospital, commented that the field has been waiting to see data on fosL/fosC.
“It seems like it’s pretty reasonable in terms of what the goals were, which is to improve stability of Parkinson’s symptoms, to improve off time and give on time without troublesome dyskinesia,” she said. “So I think those [goals] have been met.”
Dr. Subramanian, who was not involved with the research, said she would have liked to have seen results concerning safety of this drug formulation, which the presentation lacked, “because historically, there have been issues with nodule formation and skin breakdown, things like that, due to the stability of the product in the subcutaneous form. … So, always to my understanding, there has been this search for things that are tolerated in the subcutaneous delivery.”
If this formulation proves safe and tolerable, Dr. Subramanian sees a potential place for it for some patients with advanced Parkinson’s disease.
“Certainly a subcutaneous formulation will be better than something that requires … deep brain surgery or even a pump insertion like Duopa [carbidopa/levodopa enteral suspension, AbbVie] or something like that,” she said. “I think [it] would be beneficial over something with the gut because the gut historically has been a problem to rely on in advanced Parkinson’s patients due to slower transit times, and the gut itself is affected with Parkinson’s disease.”
Dr. Stodtmann and all coauthors are employees of AbbVie, which was the sponsor of the study and was responsible for all aspects of it. Dr. Subramanian has given talks for Acadia Pharmaceuticals and Acorda Therapeutics in the past.
A version of this article originally appeared on Medscape.com.
Telemedicine feasible and reliable in Parkinson’s trial
, a 1-year, phase 3 clinical trial has shown. The trial was an add-on study involving a subset of subjects from the STEADY-PD III trial of isradipine in early Parkinson’s disease.
Although the trial was conducted before SARS-CoV-2 arrived on the scene, the findings have particular relevance for being able to conduct a variety of clinical trials in the face of COVID-19 and the need to limit in-person interactions.
The 40 participants used tablets to complete three remote, video-based assessments during 1 year, with each remote visit planned to be completed within 4 weeks of an in-person visit. It was easy to enroll patients, and they completed about 95% of planned visits, said neurologist Christopher Tarolli, MD, of the University of Rochester (N.Y.).
He presented the study findings at the Movement Disorder Society’s 23rd International Congress of Parkinson’s Disease and Movement Disorders (Virtual) 2020.
“The visits were clearly feasible, and we were able to do them [84%] within that 4-week time frame around the in-person visit,” he said. “The visits were also reasonably reliable, particularly so for what we call the nonmotor outcomes and the patient-reported outcomes.”
In-person versus remote assessment
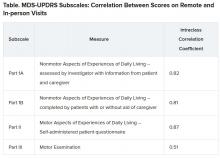
For the remote visits, participants completed primarily the same battery of tests as the in-person visits. Responses on the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) subscales demonstrated “that there was excellent correlation between patient-reported and nonmotor outcome measures and moderate correlation between in-person and remote-performed motor assessments,” Dr. Tarolli said.
He explained that the study used modified motor assessments (MDS-UPDRS Part III) that excluded testing of rigidity and postural instability, which require hands-on testing by a trained examiner and thus are impossible to do remotely.
Additionally, the somewhat lower correlation on this subscale was probably the result of different investigators conducting in-person versus remote assessments, with a subset of in-person investigators who tended to rate participants more severely driving down the correlation. “I think if these methods were applied in future trials, the in-person and remote investigators would optimally be the same person,” Dr. Tarolli suggested.
Room for error?
Indu Subramanian, MD, of the department of neurology at the University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education, and Clinical Center at the West Los Angeles Veterans Affairs Hospital, commented that “the reliability of UPDRS [part] III is where I would want to have, for sure, a little bit more of a deep dive. … possibly the same patient be rated by the same person.”
She also noted that doing remote and in-person assessments within 4 weeks of each other leaves a lot of room for variability. “You could see the same patient in the morning and then do UPDRS in the afternoon, and it can be totally different depending on when you meet the person,” she said.
Only so much testing can be done remotely. Nonetheless, she questioned whether it is really a valid UPDRS if rigidity and postural stability measures are eliminated. “[Is] this now a new modified UPDRS that we’re going to use that is as good as the old UPDRS moving forward, a home version of UPDRS or whatever we’re going to call it?”
Dr. Subramanian mentioned that patients have told her that UPDRS part III does not really measure what is most important to them, such as making pastries for their grandchildren rather than rapidly tapping their fingers.
“That speaks a little bit to the fact that we should have more patient-centered outcomes and things that patients can report. … things that are not going to require necessarily an in-person exam as maybe measures that really can be used moving forward in studies,” she suggested.
Patient satisfaction with remote visits
Greater than 90% of the patients were satisfied or very satisfied overall with the remote visits, including the convenience, comfort, and connection (using the devices and Internet connection), with “patients describing enjoying being able to do these visits from the comfort of their own home, not having to travel,” Dr. Tarolli said. Not having to drive in an ‘off’ state “was actually something that some participants identified as a safety benefit from this as well.”
There was also a time benefit to the patients and investigators. The average length of the remote visits was 54.3 minutes each versus 74 minutes of interaction for in-person visits, mainly a result of more efficient hand-offs between the neurologist and the study coordinator during the remote visits, plus being able to pause the remote visit to give a medication dose time to take effect.
For the patient, there was a large amount of time saved when travel time was considered – a total of 190.2 minutes on average for travel and testing for the in-person visits.
About three-quarters (76%) of the study patients said that remote visits would increase their likelihood of participating in future trials. However, that result may be skewed by the fact that these were already people willing to participate in a remote trial, so the generalizability of the result may be affected. Nonetheless, Dr. Tarolli said he thinks that, as technology gets better and older people become more comfortable with it, remote visits within Parkinson’s research studies may become more common.
One caveat he mentioned is that, with remote visits, the neurologist misses a chance to observe a patient’s whole body and construct a global impression of how he or she is moving. On the other hand, remote video gives the investigator the chance to see the living environment of the patient and suggest changes for safety, such as to reduce the risk of falling for a person with unsteadiness of gait living in a crowded house.
“It really allows us to make a more holistic assessment of how our patient is functioning outside the clinic, which I think we’ve traditionally had really no way of doing,” Dr. Tarolli said.
His final suggestion for anyone contemplating conducting studies with remote visits is to develop a team that is comfortable troubleshooting the technological aspects of those visits.
UCLA’s Dr. Subramanian lauded the University of Rochester team for their efforts in moving remote visits forward. “They’re at the cutting edge of these sorts of things,” she said. “So I’m assuming that they’ll come out with more things [for visits] to become better that are going to move this forward, which is exciting.”
Dr. Tarolli has disclosed no relevant financial relationships. Dr. Subramanian has given talks for Acorda Pharmaceuticals and Acadia Pharmaceuticals in the past. The study had only university, government, foundation, and other nonprofit support.
A version of this article originally appeared on Medscape.com.
, a 1-year, phase 3 clinical trial has shown. The trial was an add-on study involving a subset of subjects from the STEADY-PD III trial of isradipine in early Parkinson’s disease.
Although the trial was conducted before SARS-CoV-2 arrived on the scene, the findings have particular relevance for being able to conduct a variety of clinical trials in the face of COVID-19 and the need to limit in-person interactions.
The 40 participants used tablets to complete three remote, video-based assessments during 1 year, with each remote visit planned to be completed within 4 weeks of an in-person visit. It was easy to enroll patients, and they completed about 95% of planned visits, said neurologist Christopher Tarolli, MD, of the University of Rochester (N.Y.).
He presented the study findings at the Movement Disorder Society’s 23rd International Congress of Parkinson’s Disease and Movement Disorders (Virtual) 2020.
“The visits were clearly feasible, and we were able to do them [84%] within that 4-week time frame around the in-person visit,” he said. “The visits were also reasonably reliable, particularly so for what we call the nonmotor outcomes and the patient-reported outcomes.”
In-person versus remote assessment
For the remote visits, participants completed primarily the same battery of tests as the in-person visits. Responses on the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) subscales demonstrated “that there was excellent correlation between patient-reported and nonmotor outcome measures and moderate correlation between in-person and remote-performed motor assessments,” Dr. Tarolli said.
He explained that the study used modified motor assessments (MDS-UPDRS Part III) that excluded testing of rigidity and postural instability, which require hands-on testing by a trained examiner and thus are impossible to do remotely.
Additionally, the somewhat lower correlation on this subscale was probably the result of different investigators conducting in-person versus remote assessments, with a subset of in-person investigators who tended to rate participants more severely driving down the correlation. “I think if these methods were applied in future trials, the in-person and remote investigators would optimally be the same person,” Dr. Tarolli suggested.
Room for error?
Indu Subramanian, MD, of the department of neurology at the University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education, and Clinical Center at the West Los Angeles Veterans Affairs Hospital, commented that “the reliability of UPDRS [part] III is where I would want to have, for sure, a little bit more of a deep dive. … possibly the same patient be rated by the same person.”
She also noted that doing remote and in-person assessments within 4 weeks of each other leaves a lot of room for variability. “You could see the same patient in the morning and then do UPDRS in the afternoon, and it can be totally different depending on when you meet the person,” she said.
Only so much testing can be done remotely. Nonetheless, she questioned whether it is really a valid UPDRS if rigidity and postural stability measures are eliminated. “[Is] this now a new modified UPDRS that we’re going to use that is as good as the old UPDRS moving forward, a home version of UPDRS or whatever we’re going to call it?”
Dr. Subramanian mentioned that patients have told her that UPDRS part III does not really measure what is most important to them, such as making pastries for their grandchildren rather than rapidly tapping their fingers.
“That speaks a little bit to the fact that we should have more patient-centered outcomes and things that patients can report. … things that are not going to require necessarily an in-person exam as maybe measures that really can be used moving forward in studies,” she suggested.
Patient satisfaction with remote visits
Greater than 90% of the patients were satisfied or very satisfied overall with the remote visits, including the convenience, comfort, and connection (using the devices and Internet connection), with “patients describing enjoying being able to do these visits from the comfort of their own home, not having to travel,” Dr. Tarolli said. Not having to drive in an ‘off’ state “was actually something that some participants identified as a safety benefit from this as well.”
There was also a time benefit to the patients and investigators. The average length of the remote visits was 54.3 minutes each versus 74 minutes of interaction for in-person visits, mainly a result of more efficient hand-offs between the neurologist and the study coordinator during the remote visits, plus being able to pause the remote visit to give a medication dose time to take effect.
For the patient, there was a large amount of time saved when travel time was considered – a total of 190.2 minutes on average for travel and testing for the in-person visits.
About three-quarters (76%) of the study patients said that remote visits would increase their likelihood of participating in future trials. However, that result may be skewed by the fact that these were already people willing to participate in a remote trial, so the generalizability of the result may be affected. Nonetheless, Dr. Tarolli said he thinks that, as technology gets better and older people become more comfortable with it, remote visits within Parkinson’s research studies may become more common.
One caveat he mentioned is that, with remote visits, the neurologist misses a chance to observe a patient’s whole body and construct a global impression of how he or she is moving. On the other hand, remote video gives the investigator the chance to see the living environment of the patient and suggest changes for safety, such as to reduce the risk of falling for a person with unsteadiness of gait living in a crowded house.
“It really allows us to make a more holistic assessment of how our patient is functioning outside the clinic, which I think we’ve traditionally had really no way of doing,” Dr. Tarolli said.
His final suggestion for anyone contemplating conducting studies with remote visits is to develop a team that is comfortable troubleshooting the technological aspects of those visits.
UCLA’s Dr. Subramanian lauded the University of Rochester team for their efforts in moving remote visits forward. “They’re at the cutting edge of these sorts of things,” she said. “So I’m assuming that they’ll come out with more things [for visits] to become better that are going to move this forward, which is exciting.”
Dr. Tarolli has disclosed no relevant financial relationships. Dr. Subramanian has given talks for Acorda Pharmaceuticals and Acadia Pharmaceuticals in the past. The study had only university, government, foundation, and other nonprofit support.
A version of this article originally appeared on Medscape.com.
, a 1-year, phase 3 clinical trial has shown. The trial was an add-on study involving a subset of subjects from the STEADY-PD III trial of isradipine in early Parkinson’s disease.
Although the trial was conducted before SARS-CoV-2 arrived on the scene, the findings have particular relevance for being able to conduct a variety of clinical trials in the face of COVID-19 and the need to limit in-person interactions.
The 40 participants used tablets to complete three remote, video-based assessments during 1 year, with each remote visit planned to be completed within 4 weeks of an in-person visit. It was easy to enroll patients, and they completed about 95% of planned visits, said neurologist Christopher Tarolli, MD, of the University of Rochester (N.Y.).
He presented the study findings at the Movement Disorder Society’s 23rd International Congress of Parkinson’s Disease and Movement Disorders (Virtual) 2020.
“The visits were clearly feasible, and we were able to do them [84%] within that 4-week time frame around the in-person visit,” he said. “The visits were also reasonably reliable, particularly so for what we call the nonmotor outcomes and the patient-reported outcomes.”
In-person versus remote assessment
For the remote visits, participants completed primarily the same battery of tests as the in-person visits. Responses on the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) subscales demonstrated “that there was excellent correlation between patient-reported and nonmotor outcome measures and moderate correlation between in-person and remote-performed motor assessments,” Dr. Tarolli said.
He explained that the study used modified motor assessments (MDS-UPDRS Part III) that excluded testing of rigidity and postural instability, which require hands-on testing by a trained examiner and thus are impossible to do remotely.
Additionally, the somewhat lower correlation on this subscale was probably the result of different investigators conducting in-person versus remote assessments, with a subset of in-person investigators who tended to rate participants more severely driving down the correlation. “I think if these methods were applied in future trials, the in-person and remote investigators would optimally be the same person,” Dr. Tarolli suggested.
Room for error?
Indu Subramanian, MD, of the department of neurology at the University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education, and Clinical Center at the West Los Angeles Veterans Affairs Hospital, commented that “the reliability of UPDRS [part] III is where I would want to have, for sure, a little bit more of a deep dive. … possibly the same patient be rated by the same person.”
She also noted that doing remote and in-person assessments within 4 weeks of each other leaves a lot of room for variability. “You could see the same patient in the morning and then do UPDRS in the afternoon, and it can be totally different depending on when you meet the person,” she said.
Only so much testing can be done remotely. Nonetheless, she questioned whether it is really a valid UPDRS if rigidity and postural stability measures are eliminated. “[Is] this now a new modified UPDRS that we’re going to use that is as good as the old UPDRS moving forward, a home version of UPDRS or whatever we’re going to call it?”
Dr. Subramanian mentioned that patients have told her that UPDRS part III does not really measure what is most important to them, such as making pastries for their grandchildren rather than rapidly tapping their fingers.
“That speaks a little bit to the fact that we should have more patient-centered outcomes and things that patients can report. … things that are not going to require necessarily an in-person exam as maybe measures that really can be used moving forward in studies,” she suggested.
Patient satisfaction with remote visits
Greater than 90% of the patients were satisfied or very satisfied overall with the remote visits, including the convenience, comfort, and connection (using the devices and Internet connection), with “patients describing enjoying being able to do these visits from the comfort of their own home, not having to travel,” Dr. Tarolli said. Not having to drive in an ‘off’ state “was actually something that some participants identified as a safety benefit from this as well.”
There was also a time benefit to the patients and investigators. The average length of the remote visits was 54.3 minutes each versus 74 minutes of interaction for in-person visits, mainly a result of more efficient hand-offs between the neurologist and the study coordinator during the remote visits, plus being able to pause the remote visit to give a medication dose time to take effect.
For the patient, there was a large amount of time saved when travel time was considered – a total of 190.2 minutes on average for travel and testing for the in-person visits.
About three-quarters (76%) of the study patients said that remote visits would increase their likelihood of participating in future trials. However, that result may be skewed by the fact that these were already people willing to participate in a remote trial, so the generalizability of the result may be affected. Nonetheless, Dr. Tarolli said he thinks that, as technology gets better and older people become more comfortable with it, remote visits within Parkinson’s research studies may become more common.
One caveat he mentioned is that, with remote visits, the neurologist misses a chance to observe a patient’s whole body and construct a global impression of how he or she is moving. On the other hand, remote video gives the investigator the chance to see the living environment of the patient and suggest changes for safety, such as to reduce the risk of falling for a person with unsteadiness of gait living in a crowded house.
“It really allows us to make a more holistic assessment of how our patient is functioning outside the clinic, which I think we’ve traditionally had really no way of doing,” Dr. Tarolli said.
His final suggestion for anyone contemplating conducting studies with remote visits is to develop a team that is comfortable troubleshooting the technological aspects of those visits.
UCLA’s Dr. Subramanian lauded the University of Rochester team for their efforts in moving remote visits forward. “They’re at the cutting edge of these sorts of things,” she said. “So I’m assuming that they’ll come out with more things [for visits] to become better that are going to move this forward, which is exciting.”
Dr. Tarolli has disclosed no relevant financial relationships. Dr. Subramanian has given talks for Acorda Pharmaceuticals and Acadia Pharmaceuticals in the past. The study had only university, government, foundation, and other nonprofit support.
A version of this article originally appeared on Medscape.com.
Blood biomarker may predict Parkinson’s disease progression
Although the biomarker, neurofilament light chain (NfL), is not especially specific, it is the first blood-based biomarker for Parkinson’s disease.
Neurofilaments are components of the neural cytoskeleton, where they maintain structure along with other functions. Following axonal damage, NfL gets released into extracellular fluids. Previously, NfL has been detected in cerebrospinal fluid (CSF) in patients with multiple sclerosis and neurodegenerative dementias. NfL in the CSF can distinguish Parkinson’s disease (PD) from multiple system atrophy and progressive supranuclear palsy.
That’s useful, but a serum marker would open new doors. “An easily accessible biomarker that will serve as an indicator of diagnosis, disease state, and progression, as well as a marker of response to therapeutic intervention is needed. A biomarker will strengthen the ability to select patients for inclusion or stratification within clinical trials,” commented Okeanis Vaou, MD, director of the movement disorders program at St. Elizabeth’s Medical Center in Brighton, Mass. Dr. Vaou was not involved in the study, which was published Aug. 15 in Movement Disorders.
A potential biomarker?
To determine if serum NfL levels would correlate with CSF values and had potential as a biomarker, a large, multi-institutional team of researchers led by Brit Mollenhauer, MD, of the University Medical Center Goettingen (Germany), and Danielle Graham, MD, of Biogen, drew data from a prospective, longitudinal, single-center project called the De Novo Parkinson’s disease (DeNoPa) cohort.
The researchers analyzed data from 176 subjects, including drug-naive patients with newly diagnosed PD; age, sex, and education matched healthy controls; and patients who were initially diagnosed with Parkinson’s disease but had their diagnoses changed to a cognate or neurodegenerative disorder (OND). The researchers also drew 514 serum samples from the prospective longitudinal, observational, international multicenter study Parkinson’s Progression Marker Initiative (PPMI) cohort.
In the DeNoPa cohort, OND patients had the highest median CSF NfL levels at baseline (839 pg/mL) followed by PD patients (562 pg/mL) and healthy controls (494 pg/mL; P = .01). There was a strong correlation between CSF and serum NfL levels in a cross-sectional exploratory study with the PPMI cohort.
Age and sex covariates in the PPMI cohort explained 51% of NfL variability. After adjustment for age and sex, baseline median blood NfL levels were highest in the OND group (16.23 pg/mL), followed by the genetic PD group (13.36 pg/mL), prodromal participants (12.20 pg/mL), PD patients (11.73 pg/mL), unaffected mutation carriers (11.63 pg/mL), and healthy controls (11.05 pg/mL; F test P < .0001). Median serum NfL increased by 3.35% per year of age (P < .0001), and median serum NfL was 6.79% higher in women (P = .0002).
Doubling of adjusted serum NfL levels were associated with a median increase in the Movement Disorder Society Unified Parkinson’s Disease Rating Scale total score of 3.45 points (false-discovery rate–adjusted P = .0115), a median decrease in Symbol Digit Modality Test total score of 1.39 (FDR P = .026), a median decrease in Hopkins Verbal Learning Tests with discrimination recognition score of 0.3 (FDR P = .03), and a median decrease in Hopkins Verbal Learning Tests with retention score of 0.029 (FDR P = .04).
More specific markers needed
The findings are intriguing, said Dr Vaou, but “we need to acknowledge that increased NfL levels are not specific enough to Parkinson’s disease and reflect neuronal and axonal damage. Therefore, there is a need for more specific markers to support diagnostic accuracy, rate of progression, and ultimate prognosis. A serum NfL assay may be useful to clinicians evaluating patients with PD or OND diagnosis and mitigate the misdiagnosis of atypical PD. NfL may be particularly useful in differentiating PD from cognate disorders such as multiple system atrophy, progressive supranuclear palsy, and dementia with Lewy bodies.”
The current success is the result of large patient databases containing phenotypic data, imaging, and tests of tissue, blood, and cerebrospinal fluid, along with collaborations between advocacy groups, academia, and industry, according to Dr. Vaou. As that work continues, it could uncover more specific biomarkers “that will allow us not only to help with diagnosis and treatment but with disease progression, inclusion, recruitment and stratification in clinical studies, as well as (be an) indicator of response to therapeutic intervention of an investigational drug.”
The study was funded by the Michael J. Fox Foundation for Parkinson’s Research. Dr. Vaou had no relevant financial disclosures.
SOURCE: Mollenhauer B et al. Mov Disord. 2020 Aug 15. doi: 10.1002/mds.28206.
Although the biomarker, neurofilament light chain (NfL), is not especially specific, it is the first blood-based biomarker for Parkinson’s disease.
Neurofilaments are components of the neural cytoskeleton, where they maintain structure along with other functions. Following axonal damage, NfL gets released into extracellular fluids. Previously, NfL has been detected in cerebrospinal fluid (CSF) in patients with multiple sclerosis and neurodegenerative dementias. NfL in the CSF can distinguish Parkinson’s disease (PD) from multiple system atrophy and progressive supranuclear palsy.
That’s useful, but a serum marker would open new doors. “An easily accessible biomarker that will serve as an indicator of diagnosis, disease state, and progression, as well as a marker of response to therapeutic intervention is needed. A biomarker will strengthen the ability to select patients for inclusion or stratification within clinical trials,” commented Okeanis Vaou, MD, director of the movement disorders program at St. Elizabeth’s Medical Center in Brighton, Mass. Dr. Vaou was not involved in the study, which was published Aug. 15 in Movement Disorders.
A potential biomarker?
To determine if serum NfL levels would correlate with CSF values and had potential as a biomarker, a large, multi-institutional team of researchers led by Brit Mollenhauer, MD, of the University Medical Center Goettingen (Germany), and Danielle Graham, MD, of Biogen, drew data from a prospective, longitudinal, single-center project called the De Novo Parkinson’s disease (DeNoPa) cohort.
The researchers analyzed data from 176 subjects, including drug-naive patients with newly diagnosed PD; age, sex, and education matched healthy controls; and patients who were initially diagnosed with Parkinson’s disease but had their diagnoses changed to a cognate or neurodegenerative disorder (OND). The researchers also drew 514 serum samples from the prospective longitudinal, observational, international multicenter study Parkinson’s Progression Marker Initiative (PPMI) cohort.
In the DeNoPa cohort, OND patients had the highest median CSF NfL levels at baseline (839 pg/mL) followed by PD patients (562 pg/mL) and healthy controls (494 pg/mL; P = .01). There was a strong correlation between CSF and serum NfL levels in a cross-sectional exploratory study with the PPMI cohort.
Age and sex covariates in the PPMI cohort explained 51% of NfL variability. After adjustment for age and sex, baseline median blood NfL levels were highest in the OND group (16.23 pg/mL), followed by the genetic PD group (13.36 pg/mL), prodromal participants (12.20 pg/mL), PD patients (11.73 pg/mL), unaffected mutation carriers (11.63 pg/mL), and healthy controls (11.05 pg/mL; F test P < .0001). Median serum NfL increased by 3.35% per year of age (P < .0001), and median serum NfL was 6.79% higher in women (P = .0002).
Doubling of adjusted serum NfL levels were associated with a median increase in the Movement Disorder Society Unified Parkinson’s Disease Rating Scale total score of 3.45 points (false-discovery rate–adjusted P = .0115), a median decrease in Symbol Digit Modality Test total score of 1.39 (FDR P = .026), a median decrease in Hopkins Verbal Learning Tests with discrimination recognition score of 0.3 (FDR P = .03), and a median decrease in Hopkins Verbal Learning Tests with retention score of 0.029 (FDR P = .04).
More specific markers needed
The findings are intriguing, said Dr Vaou, but “we need to acknowledge that increased NfL levels are not specific enough to Parkinson’s disease and reflect neuronal and axonal damage. Therefore, there is a need for more specific markers to support diagnostic accuracy, rate of progression, and ultimate prognosis. A serum NfL assay may be useful to clinicians evaluating patients with PD or OND diagnosis and mitigate the misdiagnosis of atypical PD. NfL may be particularly useful in differentiating PD from cognate disorders such as multiple system atrophy, progressive supranuclear palsy, and dementia with Lewy bodies.”
The current success is the result of large patient databases containing phenotypic data, imaging, and tests of tissue, blood, and cerebrospinal fluid, along with collaborations between advocacy groups, academia, and industry, according to Dr. Vaou. As that work continues, it could uncover more specific biomarkers “that will allow us not only to help with diagnosis and treatment but with disease progression, inclusion, recruitment and stratification in clinical studies, as well as (be an) indicator of response to therapeutic intervention of an investigational drug.”
The study was funded by the Michael J. Fox Foundation for Parkinson’s Research. Dr. Vaou had no relevant financial disclosures.
SOURCE: Mollenhauer B et al. Mov Disord. 2020 Aug 15. doi: 10.1002/mds.28206.
Although the biomarker, neurofilament light chain (NfL), is not especially specific, it is the first blood-based biomarker for Parkinson’s disease.
Neurofilaments are components of the neural cytoskeleton, where they maintain structure along with other functions. Following axonal damage, NfL gets released into extracellular fluids. Previously, NfL has been detected in cerebrospinal fluid (CSF) in patients with multiple sclerosis and neurodegenerative dementias. NfL in the CSF can distinguish Parkinson’s disease (PD) from multiple system atrophy and progressive supranuclear palsy.
That’s useful, but a serum marker would open new doors. “An easily accessible biomarker that will serve as an indicator of diagnosis, disease state, and progression, as well as a marker of response to therapeutic intervention is needed. A biomarker will strengthen the ability to select patients for inclusion or stratification within clinical trials,” commented Okeanis Vaou, MD, director of the movement disorders program at St. Elizabeth’s Medical Center in Brighton, Mass. Dr. Vaou was not involved in the study, which was published Aug. 15 in Movement Disorders.
A potential biomarker?
To determine if serum NfL levels would correlate with CSF values and had potential as a biomarker, a large, multi-institutional team of researchers led by Brit Mollenhauer, MD, of the University Medical Center Goettingen (Germany), and Danielle Graham, MD, of Biogen, drew data from a prospective, longitudinal, single-center project called the De Novo Parkinson’s disease (DeNoPa) cohort.
The researchers analyzed data from 176 subjects, including drug-naive patients with newly diagnosed PD; age, sex, and education matched healthy controls; and patients who were initially diagnosed with Parkinson’s disease but had their diagnoses changed to a cognate or neurodegenerative disorder (OND). The researchers also drew 514 serum samples from the prospective longitudinal, observational, international multicenter study Parkinson’s Progression Marker Initiative (PPMI) cohort.
In the DeNoPa cohort, OND patients had the highest median CSF NfL levels at baseline (839 pg/mL) followed by PD patients (562 pg/mL) and healthy controls (494 pg/mL; P = .01). There was a strong correlation between CSF and serum NfL levels in a cross-sectional exploratory study with the PPMI cohort.
Age and sex covariates in the PPMI cohort explained 51% of NfL variability. After adjustment for age and sex, baseline median blood NfL levels were highest in the OND group (16.23 pg/mL), followed by the genetic PD group (13.36 pg/mL), prodromal participants (12.20 pg/mL), PD patients (11.73 pg/mL), unaffected mutation carriers (11.63 pg/mL), and healthy controls (11.05 pg/mL; F test P < .0001). Median serum NfL increased by 3.35% per year of age (P < .0001), and median serum NfL was 6.79% higher in women (P = .0002).
Doubling of adjusted serum NfL levels were associated with a median increase in the Movement Disorder Society Unified Parkinson’s Disease Rating Scale total score of 3.45 points (false-discovery rate–adjusted P = .0115), a median decrease in Symbol Digit Modality Test total score of 1.39 (FDR P = .026), a median decrease in Hopkins Verbal Learning Tests with discrimination recognition score of 0.3 (FDR P = .03), and a median decrease in Hopkins Verbal Learning Tests with retention score of 0.029 (FDR P = .04).
More specific markers needed
The findings are intriguing, said Dr Vaou, but “we need to acknowledge that increased NfL levels are not specific enough to Parkinson’s disease and reflect neuronal and axonal damage. Therefore, there is a need for more specific markers to support diagnostic accuracy, rate of progression, and ultimate prognosis. A serum NfL assay may be useful to clinicians evaluating patients with PD or OND diagnosis and mitigate the misdiagnosis of atypical PD. NfL may be particularly useful in differentiating PD from cognate disorders such as multiple system atrophy, progressive supranuclear palsy, and dementia with Lewy bodies.”
The current success is the result of large patient databases containing phenotypic data, imaging, and tests of tissue, blood, and cerebrospinal fluid, along with collaborations between advocacy groups, academia, and industry, according to Dr. Vaou. As that work continues, it could uncover more specific biomarkers “that will allow us not only to help with diagnosis and treatment but with disease progression, inclusion, recruitment and stratification in clinical studies, as well as (be an) indicator of response to therapeutic intervention of an investigational drug.”
The study was funded by the Michael J. Fox Foundation for Parkinson’s Research. Dr. Vaou had no relevant financial disclosures.
SOURCE: Mollenhauer B et al. Mov Disord. 2020 Aug 15. doi: 10.1002/mds.28206.
FROM MOVEMENT DISORDERS
Are aging physicians a burden?
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
The evaluation of physicians with alleged cognitive decline
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
Concussion linked to risk for dementia, Parkinson’s disease, and ADHD
new research suggests. Results from a retrospective, population-based cohort study showed that controlling for socioeconomic status and overall health did not significantly affect this association.
The link between concussion and risk for ADHD and for mood and anxiety disorder was stronger in the women than in the men. In addition, having a history of multiple concussions strengthened the association between concussion and subsequent mood and anxiety disorder, dementia, and Parkinson’s disease compared with experiencing just one concussion.
The findings are similar to those of previous studies, noted lead author Marc P. Morissette, PhD, research assistant at the Pan Am Clinic Foundation in Winnipeg, Manitoba, Canada. “The main methodological differences separating our study from previous studies in this area is a focus on concussion-specific injuries identified from medical records and the potential for study participants to have up to 25 years of follow-up data,” said Dr. Morissette.
The findings were published online July 27 in Family Medicine and Community Health, a BMJ journal.
Almost 190,000 participants
Several studies have shown associations between head injury and increased risk for ADHD, depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. However, many of these studies relied on self-reported medical history, included all forms of traumatic brain injury, and failed to adjust for preexisting health conditions.
An improved understanding of concussion and the risks associated with it could help physicians manage their patients’ long-term needs, the investigators noted.
In the current study, the researchers examined anonymized administrative health data collected between the periods of 1990–1991 and 2014–2015 in the Manitoba Population Research Data Repository at the Manitoba Center for Health Policy.
Eligible patients had been diagnosed with concussion in accordance with standard criteria. Participants were excluded if they had been diagnosed with dementia or Parkinson’s disease before the incident concussion during the study period. The investigators matched three control participants to each included patient on the basis of age, sex, and location.
Study outcome was time from index date (date of first concussion) to diagnosis of ADHD, mood and anxiety disorder, dementia, or Parkinson’s disease. The researchers controlled for socioeconomic status using the Socioeconomic Factor Index, version 2 (SEFI2), and for preexisting medical conditions using the Charlson Comorbidity Index (CCI).
The study included 28,021 men (mean age, 25 years) and 19,462 women (mean age, 30 years) in the concussion group and 81,871 men (mean age, 25 years) and 57,159 women (mean age, 30 years) in the control group. Mean SEFI2 score was approximately −0.05, and mean CCI score was approximately 0.2.
Dose effect?
Results showed that concussion was associated with an increased risk for ADHD (hazard ratio [HR], 1.39), mood and anxiety disorder (HR, 1.72), dementia (HR, 1.72), and Parkinson’s disease (HR, 1.57).
After a concussion, the risk of developing ADHD was 28% higher and the risk of developing mood and anxiety disorder was 7% higher among women than among men. Gender was not associated with risk for dementia or Parkinson’s disease after concussion.
Sustaining a second concussion increased the strength of the association with risk for dementia compared with sustaining a single concussion (HR, 1.62). Similarly, sustaining more than three concussions increased the strength of the association with the risk for mood and anxiety disorders (HR for more than three vs one concussion, 1.22) and Parkinson›s disease (HR, 3.27).
A sensitivity analysis found similar associations between concussion and risk for mood and anxiety disorder among all age groups. Younger participants were at greater risk for ADHD, however, and older participants were at greater risk for dementia and Parkinson’s disease.
Increased awareness of concussion and the outcomes of interest, along with improved diagnostic tools, may have influenced the study’s findings, Dr. Morissette noted. “The sex-based differences may be due to either pathophysiological differences in response to concussive injuries or potentially a difference in willingness to seek medical care or share symptoms, concussion-related or otherwise, with a medical professional,” he said.
“We are hopeful that our findings will encourage practitioners to be cognizant of various conditions that may present in individuals who have previously experienced a concussion,” Dr. Morissette added. “If physicians are aware of the various associations identified following a concussion, it may lead to more thorough clinical examination at initial presentation, along with more dedicated care throughout the patient’s life.”
Association versus causation
Commenting on the research, Steven Erickson, MD, sports medicine specialist at Banner–University Medicine Neuroscience Institute, Phoenix, Ariz., noted that although the study showed an association between concussion and subsequent diagnosis of ADHD, anxiety, and Parkinson’s disease, “this association should not be misconstrued as causation.” He added that the study’s conclusions “are just as likely to be due to labeling theory” or a self-fulfilling prophecy.
“Patients diagnosed with ADHD, anxiety, or Parkinson’s disease may recall concussion and associate the two diagnoses; but patients who have not previously been diagnosed with a concussion cannot draw that conclusion,” said Dr. Erickson, who was not involved with the research.
Citing the apparent gender difference in the strength of the association between concussion and the outcomes of interest, Dr. Erickson noted that women are more likely to report symptoms in general “and therefore are more likely to be diagnosed with ADHD and anxiety disorders” because of differences in reporting rather than incidence of disease.
“Further research needs to be done to definitively determine a causal relationship between concussion and any psychiatric or neurologic diagnosis,” Dr. Erickson concluded.
The study was funded by the Pan Am Clinic Foundation. Dr. Morissette and Dr. Erickson have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. Results from a retrospective, population-based cohort study showed that controlling for socioeconomic status and overall health did not significantly affect this association.
The link between concussion and risk for ADHD and for mood and anxiety disorder was stronger in the women than in the men. In addition, having a history of multiple concussions strengthened the association between concussion and subsequent mood and anxiety disorder, dementia, and Parkinson’s disease compared with experiencing just one concussion.
The findings are similar to those of previous studies, noted lead author Marc P. Morissette, PhD, research assistant at the Pan Am Clinic Foundation in Winnipeg, Manitoba, Canada. “The main methodological differences separating our study from previous studies in this area is a focus on concussion-specific injuries identified from medical records and the potential for study participants to have up to 25 years of follow-up data,” said Dr. Morissette.
The findings were published online July 27 in Family Medicine and Community Health, a BMJ journal.
Almost 190,000 participants
Several studies have shown associations between head injury and increased risk for ADHD, depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. However, many of these studies relied on self-reported medical history, included all forms of traumatic brain injury, and failed to adjust for preexisting health conditions.
An improved understanding of concussion and the risks associated with it could help physicians manage their patients’ long-term needs, the investigators noted.
In the current study, the researchers examined anonymized administrative health data collected between the periods of 1990–1991 and 2014–2015 in the Manitoba Population Research Data Repository at the Manitoba Center for Health Policy.
Eligible patients had been diagnosed with concussion in accordance with standard criteria. Participants were excluded if they had been diagnosed with dementia or Parkinson’s disease before the incident concussion during the study period. The investigators matched three control participants to each included patient on the basis of age, sex, and location.
Study outcome was time from index date (date of first concussion) to diagnosis of ADHD, mood and anxiety disorder, dementia, or Parkinson’s disease. The researchers controlled for socioeconomic status using the Socioeconomic Factor Index, version 2 (SEFI2), and for preexisting medical conditions using the Charlson Comorbidity Index (CCI).
The study included 28,021 men (mean age, 25 years) and 19,462 women (mean age, 30 years) in the concussion group and 81,871 men (mean age, 25 years) and 57,159 women (mean age, 30 years) in the control group. Mean SEFI2 score was approximately −0.05, and mean CCI score was approximately 0.2.
Dose effect?
Results showed that concussion was associated with an increased risk for ADHD (hazard ratio [HR], 1.39), mood and anxiety disorder (HR, 1.72), dementia (HR, 1.72), and Parkinson’s disease (HR, 1.57).
After a concussion, the risk of developing ADHD was 28% higher and the risk of developing mood and anxiety disorder was 7% higher among women than among men. Gender was not associated with risk for dementia or Parkinson’s disease after concussion.
Sustaining a second concussion increased the strength of the association with risk for dementia compared with sustaining a single concussion (HR, 1.62). Similarly, sustaining more than three concussions increased the strength of the association with the risk for mood and anxiety disorders (HR for more than three vs one concussion, 1.22) and Parkinson›s disease (HR, 3.27).
A sensitivity analysis found similar associations between concussion and risk for mood and anxiety disorder among all age groups. Younger participants were at greater risk for ADHD, however, and older participants were at greater risk for dementia and Parkinson’s disease.
Increased awareness of concussion and the outcomes of interest, along with improved diagnostic tools, may have influenced the study’s findings, Dr. Morissette noted. “The sex-based differences may be due to either pathophysiological differences in response to concussive injuries or potentially a difference in willingness to seek medical care or share symptoms, concussion-related or otherwise, with a medical professional,” he said.
“We are hopeful that our findings will encourage practitioners to be cognizant of various conditions that may present in individuals who have previously experienced a concussion,” Dr. Morissette added. “If physicians are aware of the various associations identified following a concussion, it may lead to more thorough clinical examination at initial presentation, along with more dedicated care throughout the patient’s life.”
Association versus causation
Commenting on the research, Steven Erickson, MD, sports medicine specialist at Banner–University Medicine Neuroscience Institute, Phoenix, Ariz., noted that although the study showed an association between concussion and subsequent diagnosis of ADHD, anxiety, and Parkinson’s disease, “this association should not be misconstrued as causation.” He added that the study’s conclusions “are just as likely to be due to labeling theory” or a self-fulfilling prophecy.
“Patients diagnosed with ADHD, anxiety, or Parkinson’s disease may recall concussion and associate the two diagnoses; but patients who have not previously been diagnosed with a concussion cannot draw that conclusion,” said Dr. Erickson, who was not involved with the research.
Citing the apparent gender difference in the strength of the association between concussion and the outcomes of interest, Dr. Erickson noted that women are more likely to report symptoms in general “and therefore are more likely to be diagnosed with ADHD and anxiety disorders” because of differences in reporting rather than incidence of disease.
“Further research needs to be done to definitively determine a causal relationship between concussion and any psychiatric or neurologic diagnosis,” Dr. Erickson concluded.
The study was funded by the Pan Am Clinic Foundation. Dr. Morissette and Dr. Erickson have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. Results from a retrospective, population-based cohort study showed that controlling for socioeconomic status and overall health did not significantly affect this association.
The link between concussion and risk for ADHD and for mood and anxiety disorder was stronger in the women than in the men. In addition, having a history of multiple concussions strengthened the association between concussion and subsequent mood and anxiety disorder, dementia, and Parkinson’s disease compared with experiencing just one concussion.
The findings are similar to those of previous studies, noted lead author Marc P. Morissette, PhD, research assistant at the Pan Am Clinic Foundation in Winnipeg, Manitoba, Canada. “The main methodological differences separating our study from previous studies in this area is a focus on concussion-specific injuries identified from medical records and the potential for study participants to have up to 25 years of follow-up data,” said Dr. Morissette.
The findings were published online July 27 in Family Medicine and Community Health, a BMJ journal.
Almost 190,000 participants
Several studies have shown associations between head injury and increased risk for ADHD, depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. However, many of these studies relied on self-reported medical history, included all forms of traumatic brain injury, and failed to adjust for preexisting health conditions.
An improved understanding of concussion and the risks associated with it could help physicians manage their patients’ long-term needs, the investigators noted.
In the current study, the researchers examined anonymized administrative health data collected between the periods of 1990–1991 and 2014–2015 in the Manitoba Population Research Data Repository at the Manitoba Center for Health Policy.
Eligible patients had been diagnosed with concussion in accordance with standard criteria. Participants were excluded if they had been diagnosed with dementia or Parkinson’s disease before the incident concussion during the study period. The investigators matched three control participants to each included patient on the basis of age, sex, and location.
Study outcome was time from index date (date of first concussion) to diagnosis of ADHD, mood and anxiety disorder, dementia, or Parkinson’s disease. The researchers controlled for socioeconomic status using the Socioeconomic Factor Index, version 2 (SEFI2), and for preexisting medical conditions using the Charlson Comorbidity Index (CCI).
The study included 28,021 men (mean age, 25 years) and 19,462 women (mean age, 30 years) in the concussion group and 81,871 men (mean age, 25 years) and 57,159 women (mean age, 30 years) in the control group. Mean SEFI2 score was approximately −0.05, and mean CCI score was approximately 0.2.
Dose effect?
Results showed that concussion was associated with an increased risk for ADHD (hazard ratio [HR], 1.39), mood and anxiety disorder (HR, 1.72), dementia (HR, 1.72), and Parkinson’s disease (HR, 1.57).
After a concussion, the risk of developing ADHD was 28% higher and the risk of developing mood and anxiety disorder was 7% higher among women than among men. Gender was not associated with risk for dementia or Parkinson’s disease after concussion.
Sustaining a second concussion increased the strength of the association with risk for dementia compared with sustaining a single concussion (HR, 1.62). Similarly, sustaining more than three concussions increased the strength of the association with the risk for mood and anxiety disorders (HR for more than three vs one concussion, 1.22) and Parkinson›s disease (HR, 3.27).
A sensitivity analysis found similar associations between concussion and risk for mood and anxiety disorder among all age groups. Younger participants were at greater risk for ADHD, however, and older participants were at greater risk for dementia and Parkinson’s disease.
Increased awareness of concussion and the outcomes of interest, along with improved diagnostic tools, may have influenced the study’s findings, Dr. Morissette noted. “The sex-based differences may be due to either pathophysiological differences in response to concussive injuries or potentially a difference in willingness to seek medical care or share symptoms, concussion-related or otherwise, with a medical professional,” he said.
“We are hopeful that our findings will encourage practitioners to be cognizant of various conditions that may present in individuals who have previously experienced a concussion,” Dr. Morissette added. “If physicians are aware of the various associations identified following a concussion, it may lead to more thorough clinical examination at initial presentation, along with more dedicated care throughout the patient’s life.”
Association versus causation
Commenting on the research, Steven Erickson, MD, sports medicine specialist at Banner–University Medicine Neuroscience Institute, Phoenix, Ariz., noted that although the study showed an association between concussion and subsequent diagnosis of ADHD, anxiety, and Parkinson’s disease, “this association should not be misconstrued as causation.” He added that the study’s conclusions “are just as likely to be due to labeling theory” or a self-fulfilling prophecy.
“Patients diagnosed with ADHD, anxiety, or Parkinson’s disease may recall concussion and associate the two diagnoses; but patients who have not previously been diagnosed with a concussion cannot draw that conclusion,” said Dr. Erickson, who was not involved with the research.
Citing the apparent gender difference in the strength of the association between concussion and the outcomes of interest, Dr. Erickson noted that women are more likely to report symptoms in general “and therefore are more likely to be diagnosed with ADHD and anxiety disorders” because of differences in reporting rather than incidence of disease.
“Further research needs to be done to definitively determine a causal relationship between concussion and any psychiatric or neurologic diagnosis,” Dr. Erickson concluded.
The study was funded by the Pan Am Clinic Foundation. Dr. Morissette and Dr. Erickson have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
From Family Medicine and Community Health
Can DBS in early Parkinson’s disease reduce disease progression?
According to the investigators, a larger trial is needed to confirm these findings, which were published online ahead of print June 29 in Neurology.
Adverse events were similar between patients who underwent DBS and drug therapy and those who underwent drug therapy alone. This result is a preliminary indication of the safety of long-term DBS therapy, according to the researchers. Furthermore, patients who received DBS required a significantly lower levodopa equivalent daily dose (LEDD) and were less likely to need polypharmacy than were patients who received medical treatment alone.
“While we can be really excited about these findings, we can’t change our practice, what we recommend to patients, based on this [study],” said David Charles, MD, professor and vice chair of neurology at Vanderbilt University, Nashville, Tenn. “We have to do the next trial to get that class of evidence.”
An extension of a pilot trial
Previous research has indicated that treatment with DBS and optimal medical therapy provides benefits beyond those of medical therapy alone in patients with mid-stage or advanced Parkinson’s disease. Dr. Charles and colleagues conducted a randomized, single-blind pilot study to examine the safety and tolerability of STN DBS in 30 patients with early Parkinson’s disease. Eligible participants had Hoehn and Yahr stage II off medication, were between 50 and 75 years of age, had taken medication for 6 months to 4 years, and had no dyskinesia or other motor fluctuations.
Patients were randomly assigned in equal groups to optimal drug therapy plus STN DBS or to drug therapy alone. Investigators evaluated patients every 6 months for 2 years. The results suggested that STN DBS was safe and slowed the progression of rest tremor in this population.
Apart from research that included patients with advanced Parkinson’s disease, data relating to long-term follow-up of patients undergoing DBS for Parkinson’s disease have been limited. Prospective studies have found that DBS provides motor benefits in patients with advanced Parkinson’s disease after 5-10 years, but they have not included control groups of patients randomly assigned to medication alone. Understanding the durability of effect of DBS is particularly important in patients with early Parkinson’s disease, because they could be exposed to stimulation for a longer time than other patients.
DBS may slow progression of rest tremor
Dr. Charles and colleagues invited patients who completed their pilot study to participate in an observational follow-up study. All 29 patients who completed the pilot study consented to participate in the follow-up. The investigators conducted annual outpatient examinations at 3, 4, and 5 years after baseline. These examinations were similar to those conducted at baseline in the pilot trial. Patients’ scores on the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III were obtained through blinded video assessment. Rigidity was not assessed. The investigators calculated patients’ levodopa equivalent daily dose (LEDD) and total electrical energy delivered (TEED). Adverse events were classified as mild, moderate, or severe.
Because of a problem with study funding, the investigators examined only eight patients in the optimal therapy group and nine patients in the DBS group at 3 years. The final analysis included 28 patients, because one patient was found not to have met inclusion criteria after the trial was completed.
At 5 years, participants’ mean age was 66.1 years. Participants had been taking medications for Parkinson’s disease for a mean duration of 7.2 years. No deaths occurred during the study. Four participants who had been assigned randomly to optimal drug therapy chose to receive STN DBS during the study. The investigators evaluated these participants in the treatment group to which they had been assigned at randomization using an intention-to-treat analysis that compared early STN DBS plus drug therapy with drug therapy alone.
Among patients with early DBS, the odds ratio (OR) of worse UPDRS III scores during 5 years was 0.42, compared with the medical therapy group. The difference in mean UPDRS III score between groups due to randomization was 3.70, which was a clinically important difference, according to the investigators.
In the early DBS group, the OR of worse rest tremor was 0.21, compared with the drug therapy group. The between-group difference in mean rest tremor score favored the DBS group. Excluding rest tremor from participants’ UPDRS III scores eliminated between-group differences in the odds of having worse motor symptoms and in the magnitude of difference of motor symptom score.
In the early DBS group, the OR of requiring a greater LEDD was 0.26, compared with the drug therapy group. The between group difference in mean LEDD significantly favored the DBS group. In addition, at 5 years, the proportion of patients requiring polypharmacy was 93% in the drug therapy group and 43% in the DBS group.
The investigators found no difference between groups in the prevalence of dyskinesia at baseline. At 5 years, the prevalence of dyskinesia was 50% in the drug therapy group and 21% in the DBS group. The difference was not statistically significant, however.
The study groups had similar adverse event profiles. Five adverse events during follow-up were related to surgery or the DBS device. The most common of the 13 study-related adverse events was nausea.
The study’s most significant finding is that “DBS implanted in early Parkinson’s disease decreases the risk of disease progression,” said Dr. Charles. No therapy, including DBS, has been proven to decrease this risk. “This is class II evidence. We have to get class I evidence before we change practice.”
Dr. Charles and colleagues have received Food and Drug Administration approval for a multicenter phase 3 trial to obtain this evidence. The new trial may extend findings regarding DBS in mid-stage and advanced Parkinson’s disease to early-stage Parkinson’s disease. That is, it may show that DBS plus drug therapy in early stage Parkinson’s disease is safe, efficacious, and superior to standard medical therapy alone. “But the reason to do the trial is to determine if it changes or slows the progression of the disease,” said Dr. Charles.
Effect on dyskinesia is unclear
“If a patient does go on to develop problems that need DBS management, and only a small fraction of patients with Parkinson’s disease evolve to this need, then this procedure can be performed at that time,” said Peter A. LeWitt, MD, Sastry Foundation Endowed Chair in Neurology at Wayne State University in Detroit.
“One confound of the study is that DBS provides symptomatic relief of dyskinesias if a patient has developed this problem after a few years of levodopa treatment,” Dr. LeWitt added. “To demonstrate that early use of DBS prevented the development of dyskinesias, the study design should have included a period of turning off the stimulators to determine whether the generation of dyskinesias was prevented, rather than merely suppressed by DBS, as any patient would experience.
“Finally, the goal of reducing use of levodopa dose medications or polypharmacy doesn’t justify subjecting a patient to a brain operation that is not without risks and great expense,” Dr. LeWitt continued. “The results of this underpowered study add to my opinion that the ‘premature’ use of DBS is not a good idea for the management of Parkinson’s disease.”
Medtronic, which manufactures the DBS device that the investigators used, provided part of the study’s funding. Vanderbilt University receives income for research or educational programs that Dr. Charles leads. Dr. LeWitt had no pertinent disclosures.
SOURCE: Hacker ML et al. Neurology. 2020 Jun 29. doi: 10.1212/WNL.0000000000009946.
According to the investigators, a larger trial is needed to confirm these findings, which were published online ahead of print June 29 in Neurology.
Adverse events were similar between patients who underwent DBS and drug therapy and those who underwent drug therapy alone. This result is a preliminary indication of the safety of long-term DBS therapy, according to the researchers. Furthermore, patients who received DBS required a significantly lower levodopa equivalent daily dose (LEDD) and were less likely to need polypharmacy than were patients who received medical treatment alone.
“While we can be really excited about these findings, we can’t change our practice, what we recommend to patients, based on this [study],” said David Charles, MD, professor and vice chair of neurology at Vanderbilt University, Nashville, Tenn. “We have to do the next trial to get that class of evidence.”
An extension of a pilot trial
Previous research has indicated that treatment with DBS and optimal medical therapy provides benefits beyond those of medical therapy alone in patients with mid-stage or advanced Parkinson’s disease. Dr. Charles and colleagues conducted a randomized, single-blind pilot study to examine the safety and tolerability of STN DBS in 30 patients with early Parkinson’s disease. Eligible participants had Hoehn and Yahr stage II off medication, were between 50 and 75 years of age, had taken medication for 6 months to 4 years, and had no dyskinesia or other motor fluctuations.
Patients were randomly assigned in equal groups to optimal drug therapy plus STN DBS or to drug therapy alone. Investigators evaluated patients every 6 months for 2 years. The results suggested that STN DBS was safe and slowed the progression of rest tremor in this population.
Apart from research that included patients with advanced Parkinson’s disease, data relating to long-term follow-up of patients undergoing DBS for Parkinson’s disease have been limited. Prospective studies have found that DBS provides motor benefits in patients with advanced Parkinson’s disease after 5-10 years, but they have not included control groups of patients randomly assigned to medication alone. Understanding the durability of effect of DBS is particularly important in patients with early Parkinson’s disease, because they could be exposed to stimulation for a longer time than other patients.
DBS may slow progression of rest tremor
Dr. Charles and colleagues invited patients who completed their pilot study to participate in an observational follow-up study. All 29 patients who completed the pilot study consented to participate in the follow-up. The investigators conducted annual outpatient examinations at 3, 4, and 5 years after baseline. These examinations were similar to those conducted at baseline in the pilot trial. Patients’ scores on the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III were obtained through blinded video assessment. Rigidity was not assessed. The investigators calculated patients’ levodopa equivalent daily dose (LEDD) and total electrical energy delivered (TEED). Adverse events were classified as mild, moderate, or severe.
Because of a problem with study funding, the investigators examined only eight patients in the optimal therapy group and nine patients in the DBS group at 3 years. The final analysis included 28 patients, because one patient was found not to have met inclusion criteria after the trial was completed.
At 5 years, participants’ mean age was 66.1 years. Participants had been taking medications for Parkinson’s disease for a mean duration of 7.2 years. No deaths occurred during the study. Four participants who had been assigned randomly to optimal drug therapy chose to receive STN DBS during the study. The investigators evaluated these participants in the treatment group to which they had been assigned at randomization using an intention-to-treat analysis that compared early STN DBS plus drug therapy with drug therapy alone.
Among patients with early DBS, the odds ratio (OR) of worse UPDRS III scores during 5 years was 0.42, compared with the medical therapy group. The difference in mean UPDRS III score between groups due to randomization was 3.70, which was a clinically important difference, according to the investigators.
In the early DBS group, the OR of worse rest tremor was 0.21, compared with the drug therapy group. The between-group difference in mean rest tremor score favored the DBS group. Excluding rest tremor from participants’ UPDRS III scores eliminated between-group differences in the odds of having worse motor symptoms and in the magnitude of difference of motor symptom score.
In the early DBS group, the OR of requiring a greater LEDD was 0.26, compared with the drug therapy group. The between group difference in mean LEDD significantly favored the DBS group. In addition, at 5 years, the proportion of patients requiring polypharmacy was 93% in the drug therapy group and 43% in the DBS group.
The investigators found no difference between groups in the prevalence of dyskinesia at baseline. At 5 years, the prevalence of dyskinesia was 50% in the drug therapy group and 21% in the DBS group. The difference was not statistically significant, however.
The study groups had similar adverse event profiles. Five adverse events during follow-up were related to surgery or the DBS device. The most common of the 13 study-related adverse events was nausea.
The study’s most significant finding is that “DBS implanted in early Parkinson’s disease decreases the risk of disease progression,” said Dr. Charles. No therapy, including DBS, has been proven to decrease this risk. “This is class II evidence. We have to get class I evidence before we change practice.”
Dr. Charles and colleagues have received Food and Drug Administration approval for a multicenter phase 3 trial to obtain this evidence. The new trial may extend findings regarding DBS in mid-stage and advanced Parkinson’s disease to early-stage Parkinson’s disease. That is, it may show that DBS plus drug therapy in early stage Parkinson’s disease is safe, efficacious, and superior to standard medical therapy alone. “But the reason to do the trial is to determine if it changes or slows the progression of the disease,” said Dr. Charles.
Effect on dyskinesia is unclear
“If a patient does go on to develop problems that need DBS management, and only a small fraction of patients with Parkinson’s disease evolve to this need, then this procedure can be performed at that time,” said Peter A. LeWitt, MD, Sastry Foundation Endowed Chair in Neurology at Wayne State University in Detroit.
“One confound of the study is that DBS provides symptomatic relief of dyskinesias if a patient has developed this problem after a few years of levodopa treatment,” Dr. LeWitt added. “To demonstrate that early use of DBS prevented the development of dyskinesias, the study design should have included a period of turning off the stimulators to determine whether the generation of dyskinesias was prevented, rather than merely suppressed by DBS, as any patient would experience.
“Finally, the goal of reducing use of levodopa dose medications or polypharmacy doesn’t justify subjecting a patient to a brain operation that is not without risks and great expense,” Dr. LeWitt continued. “The results of this underpowered study add to my opinion that the ‘premature’ use of DBS is not a good idea for the management of Parkinson’s disease.”
Medtronic, which manufactures the DBS device that the investigators used, provided part of the study’s funding. Vanderbilt University receives income for research or educational programs that Dr. Charles leads. Dr. LeWitt had no pertinent disclosures.
SOURCE: Hacker ML et al. Neurology. 2020 Jun 29. doi: 10.1212/WNL.0000000000009946.
According to the investigators, a larger trial is needed to confirm these findings, which were published online ahead of print June 29 in Neurology.
Adverse events were similar between patients who underwent DBS and drug therapy and those who underwent drug therapy alone. This result is a preliminary indication of the safety of long-term DBS therapy, according to the researchers. Furthermore, patients who received DBS required a significantly lower levodopa equivalent daily dose (LEDD) and were less likely to need polypharmacy than were patients who received medical treatment alone.
“While we can be really excited about these findings, we can’t change our practice, what we recommend to patients, based on this [study],” said David Charles, MD, professor and vice chair of neurology at Vanderbilt University, Nashville, Tenn. “We have to do the next trial to get that class of evidence.”
An extension of a pilot trial
Previous research has indicated that treatment with DBS and optimal medical therapy provides benefits beyond those of medical therapy alone in patients with mid-stage or advanced Parkinson’s disease. Dr. Charles and colleagues conducted a randomized, single-blind pilot study to examine the safety and tolerability of STN DBS in 30 patients with early Parkinson’s disease. Eligible participants had Hoehn and Yahr stage II off medication, were between 50 and 75 years of age, had taken medication for 6 months to 4 years, and had no dyskinesia or other motor fluctuations.
Patients were randomly assigned in equal groups to optimal drug therapy plus STN DBS or to drug therapy alone. Investigators evaluated patients every 6 months for 2 years. The results suggested that STN DBS was safe and slowed the progression of rest tremor in this population.
Apart from research that included patients with advanced Parkinson’s disease, data relating to long-term follow-up of patients undergoing DBS for Parkinson’s disease have been limited. Prospective studies have found that DBS provides motor benefits in patients with advanced Parkinson’s disease after 5-10 years, but they have not included control groups of patients randomly assigned to medication alone. Understanding the durability of effect of DBS is particularly important in patients with early Parkinson’s disease, because they could be exposed to stimulation for a longer time than other patients.
DBS may slow progression of rest tremor
Dr. Charles and colleagues invited patients who completed their pilot study to participate in an observational follow-up study. All 29 patients who completed the pilot study consented to participate in the follow-up. The investigators conducted annual outpatient examinations at 3, 4, and 5 years after baseline. These examinations were similar to those conducted at baseline in the pilot trial. Patients’ scores on the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III were obtained through blinded video assessment. Rigidity was not assessed. The investigators calculated patients’ levodopa equivalent daily dose (LEDD) and total electrical energy delivered (TEED). Adverse events were classified as mild, moderate, or severe.
Because of a problem with study funding, the investigators examined only eight patients in the optimal therapy group and nine patients in the DBS group at 3 years. The final analysis included 28 patients, because one patient was found not to have met inclusion criteria after the trial was completed.
At 5 years, participants’ mean age was 66.1 years. Participants had been taking medications for Parkinson’s disease for a mean duration of 7.2 years. No deaths occurred during the study. Four participants who had been assigned randomly to optimal drug therapy chose to receive STN DBS during the study. The investigators evaluated these participants in the treatment group to which they had been assigned at randomization using an intention-to-treat analysis that compared early STN DBS plus drug therapy with drug therapy alone.
Among patients with early DBS, the odds ratio (OR) of worse UPDRS III scores during 5 years was 0.42, compared with the medical therapy group. The difference in mean UPDRS III score between groups due to randomization was 3.70, which was a clinically important difference, according to the investigators.
In the early DBS group, the OR of worse rest tremor was 0.21, compared with the drug therapy group. The between-group difference in mean rest tremor score favored the DBS group. Excluding rest tremor from participants’ UPDRS III scores eliminated between-group differences in the odds of having worse motor symptoms and in the magnitude of difference of motor symptom score.
In the early DBS group, the OR of requiring a greater LEDD was 0.26, compared with the drug therapy group. The between group difference in mean LEDD significantly favored the DBS group. In addition, at 5 years, the proportion of patients requiring polypharmacy was 93% in the drug therapy group and 43% in the DBS group.
The investigators found no difference between groups in the prevalence of dyskinesia at baseline. At 5 years, the prevalence of dyskinesia was 50% in the drug therapy group and 21% in the DBS group. The difference was not statistically significant, however.
The study groups had similar adverse event profiles. Five adverse events during follow-up were related to surgery or the DBS device. The most common of the 13 study-related adverse events was nausea.
The study’s most significant finding is that “DBS implanted in early Parkinson’s disease decreases the risk of disease progression,” said Dr. Charles. No therapy, including DBS, has been proven to decrease this risk. “This is class II evidence. We have to get class I evidence before we change practice.”
Dr. Charles and colleagues have received Food and Drug Administration approval for a multicenter phase 3 trial to obtain this evidence. The new trial may extend findings regarding DBS in mid-stage and advanced Parkinson’s disease to early-stage Parkinson’s disease. That is, it may show that DBS plus drug therapy in early stage Parkinson’s disease is safe, efficacious, and superior to standard medical therapy alone. “But the reason to do the trial is to determine if it changes or slows the progression of the disease,” said Dr. Charles.
Effect on dyskinesia is unclear
“If a patient does go on to develop problems that need DBS management, and only a small fraction of patients with Parkinson’s disease evolve to this need, then this procedure can be performed at that time,” said Peter A. LeWitt, MD, Sastry Foundation Endowed Chair in Neurology at Wayne State University in Detroit.
“One confound of the study is that DBS provides symptomatic relief of dyskinesias if a patient has developed this problem after a few years of levodopa treatment,” Dr. LeWitt added. “To demonstrate that early use of DBS prevented the development of dyskinesias, the study design should have included a period of turning off the stimulators to determine whether the generation of dyskinesias was prevented, rather than merely suppressed by DBS, as any patient would experience.
“Finally, the goal of reducing use of levodopa dose medications or polypharmacy doesn’t justify subjecting a patient to a brain operation that is not without risks and great expense,” Dr. LeWitt continued. “The results of this underpowered study add to my opinion that the ‘premature’ use of DBS is not a good idea for the management of Parkinson’s disease.”
Medtronic, which manufactures the DBS device that the investigators used, provided part of the study’s funding. Vanderbilt University receives income for research or educational programs that Dr. Charles leads. Dr. LeWitt had no pertinent disclosures.
SOURCE: Hacker ML et al. Neurology. 2020 Jun 29. doi: 10.1212/WNL.0000000000009946.
FROM NEUROLOGY
Circadian rhythm changes linked to future Parkinson’s disease risk
a new study suggests. “We found that men with abnormal circadian rhythms had three times the risk of developing Parkinson’s disease over an 11-year follow-up period,” lead author, Yue Leng, MD, University of California, San Francisco, said in an interview.
“If confirmed to be a risk factor for Parkinson’s disease, then circadian rhythmicity could be a promising intervention target and will open new opportunities for the prevention and management of Parkinson’s disease,” the researchers concluded.
The study was published online in JAMA Neurology on June 15.
Circadian disruption is very common in neurodegenerative diseases such as Parkinson’s disease, but there isn’t much information on how it may predict the disease, Dr. Leng explained. “We wanted to see whether circadian abnormalities may predict Parkinson’s disease,” she said. “Parkinson’s disease has a long prodromal phase where brain changes have started to occur but no clinical symptoms have become evident. It would be useful to be able to identify these patients, and maybe changes in circadian rhythms may help us to do that,” she added.
For the study, the researchers analyzed data from 2,930 community-dwelling men aged 65 years or older (mean age, 76 years) who participated in the Osteoporotic Fractures in Men Study, in which they underwent comprehensive sleep and rest-activity rhythms assessment. “Patterns of rest and activity were measured with an actigraph device, which is worn on the wrist like a watch and captures movements which are translated into a rest-activity rhythm model – one of the most commonly used and evidence-based measures of circadian rhythm,” Dr. Leng said. Men were asked to wear the actigraphs continuously for a minimum of three 24-hour periods.
Results showed that 78 men (2.7%) developed Parkinson’s disease during the 11-year follow-up. After accounting for all covariates, the risk of Parkinson’s disease increased with decreasing circadian amplitude (strength of the rhythm) with an odds ratio of 1.77 per each decrease by one standard deviation; mesor (mean level of activity) with an odds ratio of 1.64; or robustness (how closely activity follows a 24-hour pattern) with an odds ratio of 1.54.
Those in the lowest quartile of amplitude, mesor, or robustness had approximately three times the risk of developing Parkinson’s disease compared with those in the highest quartile of amplitude. The association remained after further adjustment for nighttime sleep disturbances.
“It has previously been shown that daytime napping has been linked to risk of developing Parkinson’s disease. Now we have shown that abnormalities in the overall 24-hour circadian rest activity rhythm are also present in the prodromal phase of Parkinson’s disease, and this association was independent of several confounders, including nighttime sleep disturbances,” Dr. Leng said.
“This raises awareness of the importance of circadian rhythm in older individuals and changes in their 24-hour pattern of behavior could be an early signal of Parkinson’s disease,” she said.
“This study does not tell us whether these circadian changes are causal for Parkinson’s or not,” Dr. Leng noted.
Future studies are needed to explore underlying mechanisms and to determine whether circadian disruption itself might contribute to the development of Parkinson’s disease, the researchers said.
“If there is a causal link, then using techniques to improve circadian rhythm could help to prevent or slow the onset of Parkinson’s disease,” Dr. Leng suggested. There are many established therapies that act on circadian rhythm including bright light therapy, melatonin, and chronotherapy, she added.
Support for this study was provided by the National Institute on Aging (NIA); the National Institute of Arthritis and Musculoskeletal and Skin Diseases; the National Center for Advancing Translational Sciences; the National Heart, Lung, and Blood Institute; and the Weill Pilot Award. Dr. Leng reported grants from the NIA and the University of California, San Francisco, Weill Institute for Neurosciences during the conduct of the study; and grants from Global Brain Health Institute, the Alzheimer’s Association, and the Alzheimer’s Society outside the submitted work.
A version of this article originally appeared on Medscape.com.
a new study suggests. “We found that men with abnormal circadian rhythms had three times the risk of developing Parkinson’s disease over an 11-year follow-up period,” lead author, Yue Leng, MD, University of California, San Francisco, said in an interview.
“If confirmed to be a risk factor for Parkinson’s disease, then circadian rhythmicity could be a promising intervention target and will open new opportunities for the prevention and management of Parkinson’s disease,” the researchers concluded.
The study was published online in JAMA Neurology on June 15.
Circadian disruption is very common in neurodegenerative diseases such as Parkinson’s disease, but there isn’t much information on how it may predict the disease, Dr. Leng explained. “We wanted to see whether circadian abnormalities may predict Parkinson’s disease,” she said. “Parkinson’s disease has a long prodromal phase where brain changes have started to occur but no clinical symptoms have become evident. It would be useful to be able to identify these patients, and maybe changes in circadian rhythms may help us to do that,” she added.
For the study, the researchers analyzed data from 2,930 community-dwelling men aged 65 years or older (mean age, 76 years) who participated in the Osteoporotic Fractures in Men Study, in which they underwent comprehensive sleep and rest-activity rhythms assessment. “Patterns of rest and activity were measured with an actigraph device, which is worn on the wrist like a watch and captures movements which are translated into a rest-activity rhythm model – one of the most commonly used and evidence-based measures of circadian rhythm,” Dr. Leng said. Men were asked to wear the actigraphs continuously for a minimum of three 24-hour periods.
Results showed that 78 men (2.7%) developed Parkinson’s disease during the 11-year follow-up. After accounting for all covariates, the risk of Parkinson’s disease increased with decreasing circadian amplitude (strength of the rhythm) with an odds ratio of 1.77 per each decrease by one standard deviation; mesor (mean level of activity) with an odds ratio of 1.64; or robustness (how closely activity follows a 24-hour pattern) with an odds ratio of 1.54.
Those in the lowest quartile of amplitude, mesor, or robustness had approximately three times the risk of developing Parkinson’s disease compared with those in the highest quartile of amplitude. The association remained after further adjustment for nighttime sleep disturbances.
“It has previously been shown that daytime napping has been linked to risk of developing Parkinson’s disease. Now we have shown that abnormalities in the overall 24-hour circadian rest activity rhythm are also present in the prodromal phase of Parkinson’s disease, and this association was independent of several confounders, including nighttime sleep disturbances,” Dr. Leng said.
“This raises awareness of the importance of circadian rhythm in older individuals and changes in their 24-hour pattern of behavior could be an early signal of Parkinson’s disease,” she said.
“This study does not tell us whether these circadian changes are causal for Parkinson’s or not,” Dr. Leng noted.
Future studies are needed to explore underlying mechanisms and to determine whether circadian disruption itself might contribute to the development of Parkinson’s disease, the researchers said.
“If there is a causal link, then using techniques to improve circadian rhythm could help to prevent or slow the onset of Parkinson’s disease,” Dr. Leng suggested. There are many established therapies that act on circadian rhythm including bright light therapy, melatonin, and chronotherapy, she added.
Support for this study was provided by the National Institute on Aging (NIA); the National Institute of Arthritis and Musculoskeletal and Skin Diseases; the National Center for Advancing Translational Sciences; the National Heart, Lung, and Blood Institute; and the Weill Pilot Award. Dr. Leng reported grants from the NIA and the University of California, San Francisco, Weill Institute for Neurosciences during the conduct of the study; and grants from Global Brain Health Institute, the Alzheimer’s Association, and the Alzheimer’s Society outside the submitted work.
A version of this article originally appeared on Medscape.com.
a new study suggests. “We found that men with abnormal circadian rhythms had three times the risk of developing Parkinson’s disease over an 11-year follow-up period,” lead author, Yue Leng, MD, University of California, San Francisco, said in an interview.
“If confirmed to be a risk factor for Parkinson’s disease, then circadian rhythmicity could be a promising intervention target and will open new opportunities for the prevention and management of Parkinson’s disease,” the researchers concluded.
The study was published online in JAMA Neurology on June 15.
Circadian disruption is very common in neurodegenerative diseases such as Parkinson’s disease, but there isn’t much information on how it may predict the disease, Dr. Leng explained. “We wanted to see whether circadian abnormalities may predict Parkinson’s disease,” she said. “Parkinson’s disease has a long prodromal phase where brain changes have started to occur but no clinical symptoms have become evident. It would be useful to be able to identify these patients, and maybe changes in circadian rhythms may help us to do that,” she added.
For the study, the researchers analyzed data from 2,930 community-dwelling men aged 65 years or older (mean age, 76 years) who participated in the Osteoporotic Fractures in Men Study, in which they underwent comprehensive sleep and rest-activity rhythms assessment. “Patterns of rest and activity were measured with an actigraph device, which is worn on the wrist like a watch and captures movements which are translated into a rest-activity rhythm model – one of the most commonly used and evidence-based measures of circadian rhythm,” Dr. Leng said. Men were asked to wear the actigraphs continuously for a minimum of three 24-hour periods.
Results showed that 78 men (2.7%) developed Parkinson’s disease during the 11-year follow-up. After accounting for all covariates, the risk of Parkinson’s disease increased with decreasing circadian amplitude (strength of the rhythm) with an odds ratio of 1.77 per each decrease by one standard deviation; mesor (mean level of activity) with an odds ratio of 1.64; or robustness (how closely activity follows a 24-hour pattern) with an odds ratio of 1.54.
Those in the lowest quartile of amplitude, mesor, or robustness had approximately three times the risk of developing Parkinson’s disease compared with those in the highest quartile of amplitude. The association remained after further adjustment for nighttime sleep disturbances.
“It has previously been shown that daytime napping has been linked to risk of developing Parkinson’s disease. Now we have shown that abnormalities in the overall 24-hour circadian rest activity rhythm are also present in the prodromal phase of Parkinson’s disease, and this association was independent of several confounders, including nighttime sleep disturbances,” Dr. Leng said.
“This raises awareness of the importance of circadian rhythm in older individuals and changes in their 24-hour pattern of behavior could be an early signal of Parkinson’s disease,” she said.
“This study does not tell us whether these circadian changes are causal for Parkinson’s or not,” Dr. Leng noted.
Future studies are needed to explore underlying mechanisms and to determine whether circadian disruption itself might contribute to the development of Parkinson’s disease, the researchers said.
“If there is a causal link, then using techniques to improve circadian rhythm could help to prevent or slow the onset of Parkinson’s disease,” Dr. Leng suggested. There are many established therapies that act on circadian rhythm including bright light therapy, melatonin, and chronotherapy, she added.
Support for this study was provided by the National Institute on Aging (NIA); the National Institute of Arthritis and Musculoskeletal and Skin Diseases; the National Center for Advancing Translational Sciences; the National Heart, Lung, and Blood Institute; and the Weill Pilot Award. Dr. Leng reported grants from the NIA and the University of California, San Francisco, Weill Institute for Neurosciences during the conduct of the study; and grants from Global Brain Health Institute, the Alzheimer’s Association, and the Alzheimer’s Society outside the submitted work.
A version of this article originally appeared on Medscape.com.
FROM JAMA NEUROLOGY
Nilotinib is safe in moderate and advanced Parkinson’s disease
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
FROM AAN 2020
FDA approves apomorphine sublingual film for ‘off’ episodes in Parkinson’s disease
, the manufacturer has announced. This marks the first approval for a sublingual therapy for this indication, which is defined as the re-emergence or worsening of Parkinson’s disease symptoms that have otherwise been controlled with standard care of levodopa/carbidopa, Sunovion reports. Almost 60% of patients with Parkinson’s disease experience off episodes.
The approval “affords healthcare providers with a needed option that can be added to their patients’ medication regimen to adequately address off episodes as their Parkinson’s disease progresses,” Stewart Factor, DO, professor of neurology and director of the Movement Disorders Program at Emory University School of Medicine, Atlanta, Georgia, said in a press release from the manufacturer.
“We know from our research and discussion with the Parkinson’s community that off episodes can significantly disrupt a patient’s daily life,” Todd Sherer, PhD, CEO of the Michael J. Fox Foundation for Parkinson’s Research, said in the same release. He added that the Fox Foundation “supported early clinical development of sublingual apomorphine.”
The treatment is expected to be available in US pharmacies in September.
Disruptive symptoms
Off episodes can include periods of tremor, slowed movement, and stiffness and occur during daytime hours.
“Several years after a person is diagnosed with [Parkinson’s disease] they may notice problems such as having trouble getting out of bed in the morning or having difficulty getting out of a chair, or that they feel frozen while trying to walk as the effect of their maintenance medication diminishes,” Dr. Factor noted.
Subcutaneous infusion of the dopamine agonist apomorphine previously has shown benefit in treating persistent motor fluctuations in patients with Parkinson’s disease.
Apomorphine hydrochloride sublingual film is a novel formulation of apomorphine. It dissolves under the tongue to help improve off episode symptoms as needed up to five times per day.
A phase 3 study of 109 patients that was published in December in Lancet Neurology showed that those who received the sublingual film therapy had a mean reduction of 11.1 points on the Movement Disorder Society Unified Parkinson’s Disease Rating Scale Part III 30 minutes after dosing at the 12-week assessment. This was a significant improvement in motor symptoms versus those who received placebo (mean difference, -7.6 points; P = .0002).
In addition, initial clinical improvement was found 15 minutes after dosing.
The most frequently reported treatment-emergent adverse events in the study population were oropharyngeal reactions, followed by nausea, somnolence, and dizziness.
Long-term safety?
“The availability of this new apomorphine sublingual formulation, along with an inhaled formulation under development, will broaden the treatment options for off periods,” Angelo Antonini, MD, PhD, from University of Padua, Italy, wrote in an accompanying editorial in The Lancet Neurology.
Although the results were encouraging, he noted some caution should be heeded.
Because of “the high rate of oropharyngeal adverse events, long-term safety needs to be monitored once the product is registered and available for chronic use in patients with Parkinson’s disease,” Dr. Antonini wrote.
Other safety information issued by the manufacturer includes a warning that patients who take the 5HT3 antagonists ondansetron, dolasetron, palonosetron, granisetron, or alosetron for nausea should not also use apomorphine hydrochloride sublingual film.
“People taking ondansetron together with apomorphine, the active ingredient in Kynmobi, have had very low blood pressure and lost consciousness or ‘blacked out,’ “ the warning notes.
It also should not be taken by individuals who are allergic to the ingredients in the medication, including sodium metabisulfite.
This article first appeared on Medscape.com.
, the manufacturer has announced. This marks the first approval for a sublingual therapy for this indication, which is defined as the re-emergence or worsening of Parkinson’s disease symptoms that have otherwise been controlled with standard care of levodopa/carbidopa, Sunovion reports. Almost 60% of patients with Parkinson’s disease experience off episodes.
The approval “affords healthcare providers with a needed option that can be added to their patients’ medication regimen to adequately address off episodes as their Parkinson’s disease progresses,” Stewart Factor, DO, professor of neurology and director of the Movement Disorders Program at Emory University School of Medicine, Atlanta, Georgia, said in a press release from the manufacturer.
“We know from our research and discussion with the Parkinson’s community that off episodes can significantly disrupt a patient’s daily life,” Todd Sherer, PhD, CEO of the Michael J. Fox Foundation for Parkinson’s Research, said in the same release. He added that the Fox Foundation “supported early clinical development of sublingual apomorphine.”
The treatment is expected to be available in US pharmacies in September.
Disruptive symptoms
Off episodes can include periods of tremor, slowed movement, and stiffness and occur during daytime hours.
“Several years after a person is diagnosed with [Parkinson’s disease] they may notice problems such as having trouble getting out of bed in the morning or having difficulty getting out of a chair, or that they feel frozen while trying to walk as the effect of their maintenance medication diminishes,” Dr. Factor noted.
Subcutaneous infusion of the dopamine agonist apomorphine previously has shown benefit in treating persistent motor fluctuations in patients with Parkinson’s disease.
Apomorphine hydrochloride sublingual film is a novel formulation of apomorphine. It dissolves under the tongue to help improve off episode symptoms as needed up to five times per day.
A phase 3 study of 109 patients that was published in December in Lancet Neurology showed that those who received the sublingual film therapy had a mean reduction of 11.1 points on the Movement Disorder Society Unified Parkinson’s Disease Rating Scale Part III 30 minutes after dosing at the 12-week assessment. This was a significant improvement in motor symptoms versus those who received placebo (mean difference, -7.6 points; P = .0002).
In addition, initial clinical improvement was found 15 minutes after dosing.
The most frequently reported treatment-emergent adverse events in the study population were oropharyngeal reactions, followed by nausea, somnolence, and dizziness.
Long-term safety?
“The availability of this new apomorphine sublingual formulation, along with an inhaled formulation under development, will broaden the treatment options for off periods,” Angelo Antonini, MD, PhD, from University of Padua, Italy, wrote in an accompanying editorial in The Lancet Neurology.
Although the results were encouraging, he noted some caution should be heeded.
Because of “the high rate of oropharyngeal adverse events, long-term safety needs to be monitored once the product is registered and available for chronic use in patients with Parkinson’s disease,” Dr. Antonini wrote.
Other safety information issued by the manufacturer includes a warning that patients who take the 5HT3 antagonists ondansetron, dolasetron, palonosetron, granisetron, or alosetron for nausea should not also use apomorphine hydrochloride sublingual film.
“People taking ondansetron together with apomorphine, the active ingredient in Kynmobi, have had very low blood pressure and lost consciousness or ‘blacked out,’ “ the warning notes.
It also should not be taken by individuals who are allergic to the ingredients in the medication, including sodium metabisulfite.
This article first appeared on Medscape.com.
, the manufacturer has announced. This marks the first approval for a sublingual therapy for this indication, which is defined as the re-emergence or worsening of Parkinson’s disease symptoms that have otherwise been controlled with standard care of levodopa/carbidopa, Sunovion reports. Almost 60% of patients with Parkinson’s disease experience off episodes.
The approval “affords healthcare providers with a needed option that can be added to their patients’ medication regimen to adequately address off episodes as their Parkinson’s disease progresses,” Stewart Factor, DO, professor of neurology and director of the Movement Disorders Program at Emory University School of Medicine, Atlanta, Georgia, said in a press release from the manufacturer.
“We know from our research and discussion with the Parkinson’s community that off episodes can significantly disrupt a patient’s daily life,” Todd Sherer, PhD, CEO of the Michael J. Fox Foundation for Parkinson’s Research, said in the same release. He added that the Fox Foundation “supported early clinical development of sublingual apomorphine.”
The treatment is expected to be available in US pharmacies in September.
Disruptive symptoms
Off episodes can include periods of tremor, slowed movement, and stiffness and occur during daytime hours.
“Several years after a person is diagnosed with [Parkinson’s disease] they may notice problems such as having trouble getting out of bed in the morning or having difficulty getting out of a chair, or that they feel frozen while trying to walk as the effect of their maintenance medication diminishes,” Dr. Factor noted.
Subcutaneous infusion of the dopamine agonist apomorphine previously has shown benefit in treating persistent motor fluctuations in patients with Parkinson’s disease.
Apomorphine hydrochloride sublingual film is a novel formulation of apomorphine. It dissolves under the tongue to help improve off episode symptoms as needed up to five times per day.
A phase 3 study of 109 patients that was published in December in Lancet Neurology showed that those who received the sublingual film therapy had a mean reduction of 11.1 points on the Movement Disorder Society Unified Parkinson’s Disease Rating Scale Part III 30 minutes after dosing at the 12-week assessment. This was a significant improvement in motor symptoms versus those who received placebo (mean difference, -7.6 points; P = .0002).
In addition, initial clinical improvement was found 15 minutes after dosing.
The most frequently reported treatment-emergent adverse events in the study population were oropharyngeal reactions, followed by nausea, somnolence, and dizziness.
Long-term safety?
“The availability of this new apomorphine sublingual formulation, along with an inhaled formulation under development, will broaden the treatment options for off periods,” Angelo Antonini, MD, PhD, from University of Padua, Italy, wrote in an accompanying editorial in The Lancet Neurology.
Although the results were encouraging, he noted some caution should be heeded.
Because of “the high rate of oropharyngeal adverse events, long-term safety needs to be monitored once the product is registered and available for chronic use in patients with Parkinson’s disease,” Dr. Antonini wrote.
Other safety information issued by the manufacturer includes a warning that patients who take the 5HT3 antagonists ondansetron, dolasetron, palonosetron, granisetron, or alosetron for nausea should not also use apomorphine hydrochloride sublingual film.
“People taking ondansetron together with apomorphine, the active ingredient in Kynmobi, have had very low blood pressure and lost consciousness or ‘blacked out,’ “ the warning notes.
It also should not be taken by individuals who are allergic to the ingredients in the medication, including sodium metabisulfite.
This article first appeared on Medscape.com.
GI symptoms in Parkinson’s disease correlate with less microbial diversity
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Jade E. Kenna, a PhD candidate and research assistant at the Perron Institute of Neurological and Translational Science in Perth, Australia, described findings from a multicenter assessment of 167 patients with Parkinson’s disease and 100 controls from movement disorders clinics in Australia. Participants completed the self-report Gastrointestinal Symptom Rating Scale (GSRS), which rates the frequency and severity of 15 GI symptoms. In addition, stool samples were analyzed using targeted sequencing to characterize gut microbiome composition.
Although Parkinson’s disease is recognized primarily as a motor disorder, GI dysfunction may be one of the first symptoms. “This is hypothesized to result from a change in microbiota towards an inflammatory, dysbiotic composition,” Ms. Kenna said. A limited number of studies have reported an association between altered microbiota composition, GI symptoms, and Parkinson’s disease, but not in Australian cohorts.
Total GSRS score was significantly higher in patients with Parkinson’s disease, compared with controls. Eight of the symptoms – heartburn, acid reflux, nausea or vomiting, borborygmus, increased flatus, decreased passage of stools, feeling of incomplete evacuation, and passing hard stools – were significantly increased in patients with Parkinson’s disease. GSRS symptoms can be categorized as upper, lower, general, hypoactive, or hyperactive, and patients with Parkinson’s disease had significantly increased ratings in the upper, lower, and hypoactive GI symptom domains.
“This is quite a novel finding as not only has this not been assessed in an Australian cohort of individuals before, but the majority of existing literature focuses on the presence of constipation only,” Ms. Kenna said. “The treatment and understanding of nonmotor symptoms of Parkinson’s disease, in particular GI symptoms, remain as one of the top unmet needs reported by patients with Parkinson’s disease themselves. Therefore, a better, more thorough understanding of these symptoms is clearly needed, and research into this area has such value in terms of improving current therapeutic approaches, management strategies, and patient education.”
Microbial analyses found that Firmicutes and Proteobacteria were significantly increased and Verrucomicrobia trended toward an increase in patients with Parkinson’s disease. Fusobacteria was increased in controls. “Proteobacteria and Verrucomicrobia are known to promote inflammation, which can lead to GI symptoms. Furthermore, Faecalibacterium and Ruminococcus, which are reduced in [Parkinson’s disease], can metabolize various substrates to produce [short-chain fatty acids] like butyrate, which are known to aid against intestinal barrier dysfunction and inflammation,” she said.
Individuals with Parkinson’s disease had significantly less microbial diversity. As Parkinson’s disease severity and GI symptom severity increased, microbiome diversity decreased, Ms. Kenna said. “As reduced diversity is associated with increased intestinal inflammation, this indicates that the altered microbiome we saw in [individuals with Parkinson’s disease] may be instigating the increase in incidence and severity of GI symptoms.”
Ms. Kenna reported that she had no disclosures.
SOURCE: Kenna JE. AAN 2020, Abstract S17.006.
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Jade E. Kenna, a PhD candidate and research assistant at the Perron Institute of Neurological and Translational Science in Perth, Australia, described findings from a multicenter assessment of 167 patients with Parkinson’s disease and 100 controls from movement disorders clinics in Australia. Participants completed the self-report Gastrointestinal Symptom Rating Scale (GSRS), which rates the frequency and severity of 15 GI symptoms. In addition, stool samples were analyzed using targeted sequencing to characterize gut microbiome composition.
Although Parkinson’s disease is recognized primarily as a motor disorder, GI dysfunction may be one of the first symptoms. “This is hypothesized to result from a change in microbiota towards an inflammatory, dysbiotic composition,” Ms. Kenna said. A limited number of studies have reported an association between altered microbiota composition, GI symptoms, and Parkinson’s disease, but not in Australian cohorts.
Total GSRS score was significantly higher in patients with Parkinson’s disease, compared with controls. Eight of the symptoms – heartburn, acid reflux, nausea or vomiting, borborygmus, increased flatus, decreased passage of stools, feeling of incomplete evacuation, and passing hard stools – were significantly increased in patients with Parkinson’s disease. GSRS symptoms can be categorized as upper, lower, general, hypoactive, or hyperactive, and patients with Parkinson’s disease had significantly increased ratings in the upper, lower, and hypoactive GI symptom domains.
“This is quite a novel finding as not only has this not been assessed in an Australian cohort of individuals before, but the majority of existing literature focuses on the presence of constipation only,” Ms. Kenna said. “The treatment and understanding of nonmotor symptoms of Parkinson’s disease, in particular GI symptoms, remain as one of the top unmet needs reported by patients with Parkinson’s disease themselves. Therefore, a better, more thorough understanding of these symptoms is clearly needed, and research into this area has such value in terms of improving current therapeutic approaches, management strategies, and patient education.”
Microbial analyses found that Firmicutes and Proteobacteria were significantly increased and Verrucomicrobia trended toward an increase in patients with Parkinson’s disease. Fusobacteria was increased in controls. “Proteobacteria and Verrucomicrobia are known to promote inflammation, which can lead to GI symptoms. Furthermore, Faecalibacterium and Ruminococcus, which are reduced in [Parkinson’s disease], can metabolize various substrates to produce [short-chain fatty acids] like butyrate, which are known to aid against intestinal barrier dysfunction and inflammation,” she said.
Individuals with Parkinson’s disease had significantly less microbial diversity. As Parkinson’s disease severity and GI symptom severity increased, microbiome diversity decreased, Ms. Kenna said. “As reduced diversity is associated with increased intestinal inflammation, this indicates that the altered microbiome we saw in [individuals with Parkinson’s disease] may be instigating the increase in incidence and severity of GI symptoms.”
Ms. Kenna reported that she had no disclosures.
SOURCE: Kenna JE. AAN 2020, Abstract S17.006.
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Jade E. Kenna, a PhD candidate and research assistant at the Perron Institute of Neurological and Translational Science in Perth, Australia, described findings from a multicenter assessment of 167 patients with Parkinson’s disease and 100 controls from movement disorders clinics in Australia. Participants completed the self-report Gastrointestinal Symptom Rating Scale (GSRS), which rates the frequency and severity of 15 GI symptoms. In addition, stool samples were analyzed using targeted sequencing to characterize gut microbiome composition.
Although Parkinson’s disease is recognized primarily as a motor disorder, GI dysfunction may be one of the first symptoms. “This is hypothesized to result from a change in microbiota towards an inflammatory, dysbiotic composition,” Ms. Kenna said. A limited number of studies have reported an association between altered microbiota composition, GI symptoms, and Parkinson’s disease, but not in Australian cohorts.
Total GSRS score was significantly higher in patients with Parkinson’s disease, compared with controls. Eight of the symptoms – heartburn, acid reflux, nausea or vomiting, borborygmus, increased flatus, decreased passage of stools, feeling of incomplete evacuation, and passing hard stools – were significantly increased in patients with Parkinson’s disease. GSRS symptoms can be categorized as upper, lower, general, hypoactive, or hyperactive, and patients with Parkinson’s disease had significantly increased ratings in the upper, lower, and hypoactive GI symptom domains.
“This is quite a novel finding as not only has this not been assessed in an Australian cohort of individuals before, but the majority of existing literature focuses on the presence of constipation only,” Ms. Kenna said. “The treatment and understanding of nonmotor symptoms of Parkinson’s disease, in particular GI symptoms, remain as one of the top unmet needs reported by patients with Parkinson’s disease themselves. Therefore, a better, more thorough understanding of these symptoms is clearly needed, and research into this area has such value in terms of improving current therapeutic approaches, management strategies, and patient education.”
Microbial analyses found that Firmicutes and Proteobacteria were significantly increased and Verrucomicrobia trended toward an increase in patients with Parkinson’s disease. Fusobacteria was increased in controls. “Proteobacteria and Verrucomicrobia are known to promote inflammation, which can lead to GI symptoms. Furthermore, Faecalibacterium and Ruminococcus, which are reduced in [Parkinson’s disease], can metabolize various substrates to produce [short-chain fatty acids] like butyrate, which are known to aid against intestinal barrier dysfunction and inflammation,” she said.
Individuals with Parkinson’s disease had significantly less microbial diversity. As Parkinson’s disease severity and GI symptom severity increased, microbiome diversity decreased, Ms. Kenna said. “As reduced diversity is associated with increased intestinal inflammation, this indicates that the altered microbiome we saw in [individuals with Parkinson’s disease] may be instigating the increase in incidence and severity of GI symptoms.”
Ms. Kenna reported that she had no disclosures.
SOURCE: Kenna JE. AAN 2020, Abstract S17.006.
FROM AAN 2020