User login
Your grandmother, the metabolic influencer
“Grandma’s workouts may have made you healthier.” The title and accompanying photo of a pair of well-worn women’s running shoes caught my eye immediately. For whatever reason, we are a family of exercisers. My wife has competed in several triathlons and won two of them. With her I have cycled across the United States. It has not surprised us that all three of our children have run at least one marathon. I have always viewed their continued devotion to an active lifestyle and their healthy bodies as a tribute to the benefits of our attempts at parenting by example. We certainly didn’t coach them, lecture them, or run family boot camps on weekends and school vacations.
I had never really given much thought as to whether their grandparents also may have played any role in their affinity for physical activity until I read that article. Apparently, my mother was a gifted athlete as a young woman. I have seen photos of her playing tennis, skiing, and diving and heard stories, but I never saw her do any of these activities except a single perfect swan dive when I must have been 8 or 9 years old.
Similarly, scrapbooks reveal that my mother-in-law had an active sports life in high school. But we never saw any evidence of her athletic activity save a devotion to a gentle backstroke in the cold Maine waters during the summer. My wife and I and our children never saw these grandmothers do anything more sporting or physically taxing than single-handedly preparing a full Thanksgiving dinner. How could their exercise habits have influenced the health of their grandchildren?
A team of researchers at the Joslin Diabetes Center in Boston found that female mice who were given the opportunity to exercise produced offspring that had lower fat mass, higher bone mineral density, and insulin levels usually associated with a lower risk of type 2 diabetes. And, in a bit of a surprise, the next generation of offspring accrued a similar benefit even though its mothers were not exercising. The role of exercise in the fathers was eliminated by experimental design.
So it appears that the first-generation offspring’s gametes and hence the third generation was being exposed in utero to something generated by the grandmothers’ exercise. It does not appear to be a behavior pattern that is passed on. It may have to do with epigenetics. Searching for this unknown factor is ongoing and broad based.
Obviously, similar studies in humans are not on the drawing board. Our reproductive cycle is significantly longer than the 2 years of the mouse. However, looking at their current data, the researchers feel comfortable encouraging a mother to exercise during pregnancy as long as it is compatible with the particulars of her obstetrical course. It would be unkind and without basis in fact to blame your mother’s or your mother-in-law’s sedentary behavior for your child’s poor metabolic health. However, it is reasonable to point out to women considering pregnancy that, in addition to avoiding alcohol and smoking, a good dose of exercise during pregnancy will benefit their children. You can point out that it may even benefit their grandchildren. And of course, once the baby is born and a mother feels comfortable returning to her exercise regime, she should go for it. Remind her also that parenting by example is still the best way to do it.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
“Grandma’s workouts may have made you healthier.” The title and accompanying photo of a pair of well-worn women’s running shoes caught my eye immediately. For whatever reason, we are a family of exercisers. My wife has competed in several triathlons and won two of them. With her I have cycled across the United States. It has not surprised us that all three of our children have run at least one marathon. I have always viewed their continued devotion to an active lifestyle and their healthy bodies as a tribute to the benefits of our attempts at parenting by example. We certainly didn’t coach them, lecture them, or run family boot camps on weekends and school vacations.
I had never really given much thought as to whether their grandparents also may have played any role in their affinity for physical activity until I read that article. Apparently, my mother was a gifted athlete as a young woman. I have seen photos of her playing tennis, skiing, and diving and heard stories, but I never saw her do any of these activities except a single perfect swan dive when I must have been 8 or 9 years old.
Similarly, scrapbooks reveal that my mother-in-law had an active sports life in high school. But we never saw any evidence of her athletic activity save a devotion to a gentle backstroke in the cold Maine waters during the summer. My wife and I and our children never saw these grandmothers do anything more sporting or physically taxing than single-handedly preparing a full Thanksgiving dinner. How could their exercise habits have influenced the health of their grandchildren?
A team of researchers at the Joslin Diabetes Center in Boston found that female mice who were given the opportunity to exercise produced offspring that had lower fat mass, higher bone mineral density, and insulin levels usually associated with a lower risk of type 2 diabetes. And, in a bit of a surprise, the next generation of offspring accrued a similar benefit even though its mothers were not exercising. The role of exercise in the fathers was eliminated by experimental design.
So it appears that the first-generation offspring’s gametes and hence the third generation was being exposed in utero to something generated by the grandmothers’ exercise. It does not appear to be a behavior pattern that is passed on. It may have to do with epigenetics. Searching for this unknown factor is ongoing and broad based.
Obviously, similar studies in humans are not on the drawing board. Our reproductive cycle is significantly longer than the 2 years of the mouse. However, looking at their current data, the researchers feel comfortable encouraging a mother to exercise during pregnancy as long as it is compatible with the particulars of her obstetrical course. It would be unkind and without basis in fact to blame your mother’s or your mother-in-law’s sedentary behavior for your child’s poor metabolic health. However, it is reasonable to point out to women considering pregnancy that, in addition to avoiding alcohol and smoking, a good dose of exercise during pregnancy will benefit their children. You can point out that it may even benefit their grandchildren. And of course, once the baby is born and a mother feels comfortable returning to her exercise regime, she should go for it. Remind her also that parenting by example is still the best way to do it.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
“Grandma’s workouts may have made you healthier.” The title and accompanying photo of a pair of well-worn women’s running shoes caught my eye immediately. For whatever reason, we are a family of exercisers. My wife has competed in several triathlons and won two of them. With her I have cycled across the United States. It has not surprised us that all three of our children have run at least one marathon. I have always viewed their continued devotion to an active lifestyle and their healthy bodies as a tribute to the benefits of our attempts at parenting by example. We certainly didn’t coach them, lecture them, or run family boot camps on weekends and school vacations.
I had never really given much thought as to whether their grandparents also may have played any role in their affinity for physical activity until I read that article. Apparently, my mother was a gifted athlete as a young woman. I have seen photos of her playing tennis, skiing, and diving and heard stories, but I never saw her do any of these activities except a single perfect swan dive when I must have been 8 or 9 years old.
Similarly, scrapbooks reveal that my mother-in-law had an active sports life in high school. But we never saw any evidence of her athletic activity save a devotion to a gentle backstroke in the cold Maine waters during the summer. My wife and I and our children never saw these grandmothers do anything more sporting or physically taxing than single-handedly preparing a full Thanksgiving dinner. How could their exercise habits have influenced the health of their grandchildren?
A team of researchers at the Joslin Diabetes Center in Boston found that female mice who were given the opportunity to exercise produced offspring that had lower fat mass, higher bone mineral density, and insulin levels usually associated with a lower risk of type 2 diabetes. And, in a bit of a surprise, the next generation of offspring accrued a similar benefit even though its mothers were not exercising. The role of exercise in the fathers was eliminated by experimental design.
So it appears that the first-generation offspring’s gametes and hence the third generation was being exposed in utero to something generated by the grandmothers’ exercise. It does not appear to be a behavior pattern that is passed on. It may have to do with epigenetics. Searching for this unknown factor is ongoing and broad based.
Obviously, similar studies in humans are not on the drawing board. Our reproductive cycle is significantly longer than the 2 years of the mouse. However, looking at their current data, the researchers feel comfortable encouraging a mother to exercise during pregnancy as long as it is compatible with the particulars of her obstetrical course. It would be unkind and without basis in fact to blame your mother’s or your mother-in-law’s sedentary behavior for your child’s poor metabolic health. However, it is reasonable to point out to women considering pregnancy that, in addition to avoiding alcohol and smoking, a good dose of exercise during pregnancy will benefit their children. You can point out that it may even benefit their grandchildren. And of course, once the baby is born and a mother feels comfortable returning to her exercise regime, she should go for it. Remind her also that parenting by example is still the best way to do it.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Children and COVID: Weekly cases keep rising past 100,000
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.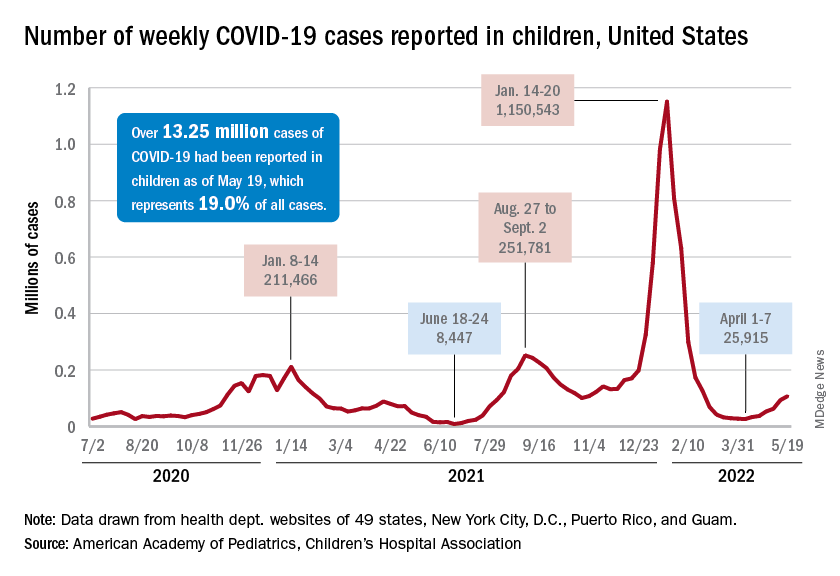
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”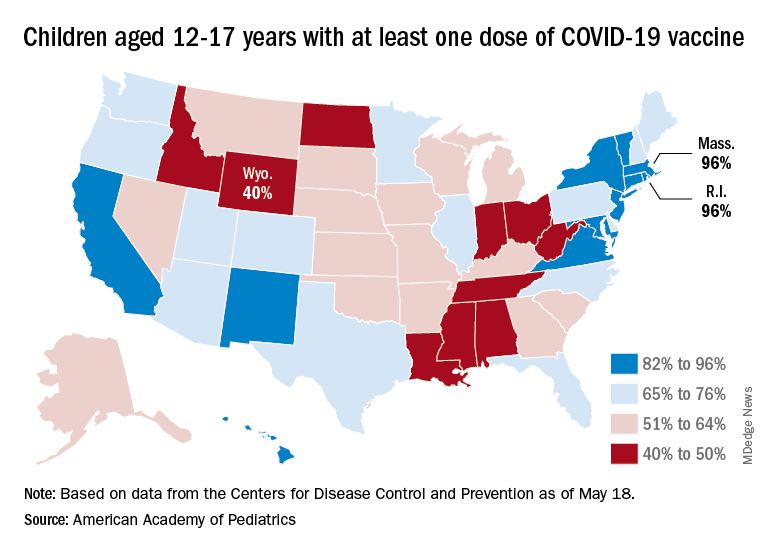
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.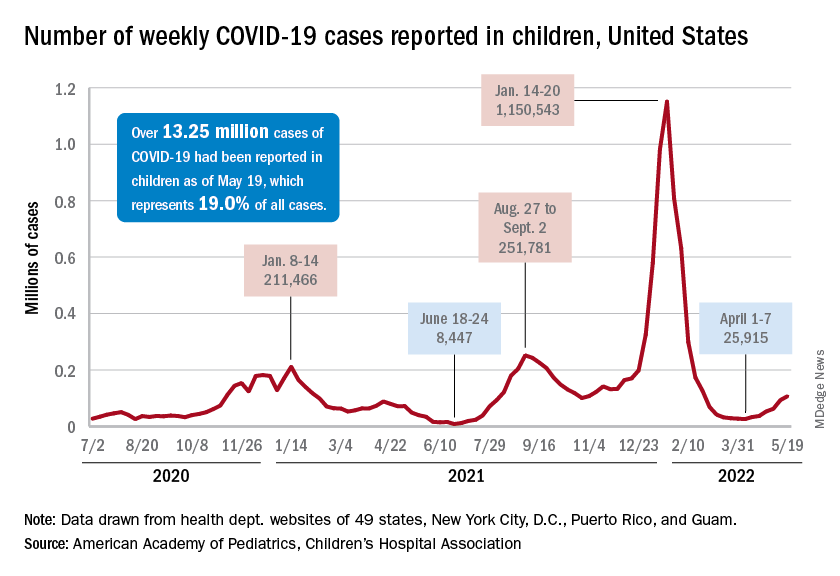
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”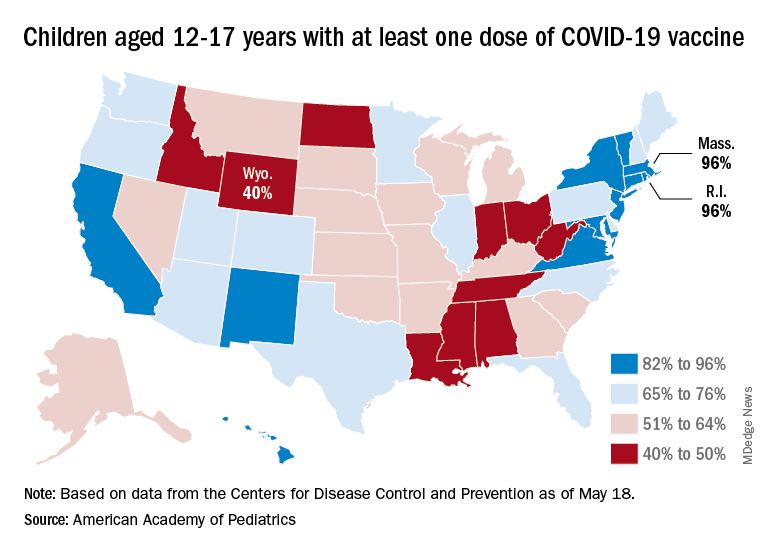
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.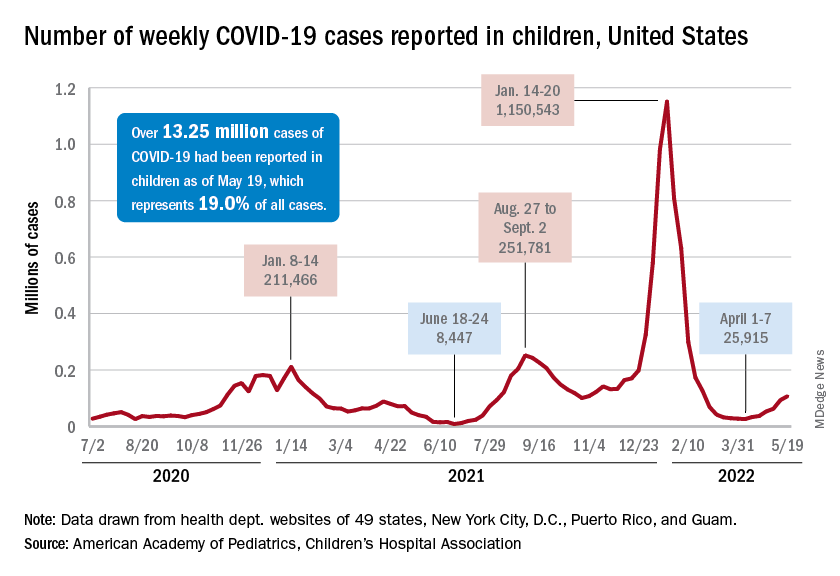
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”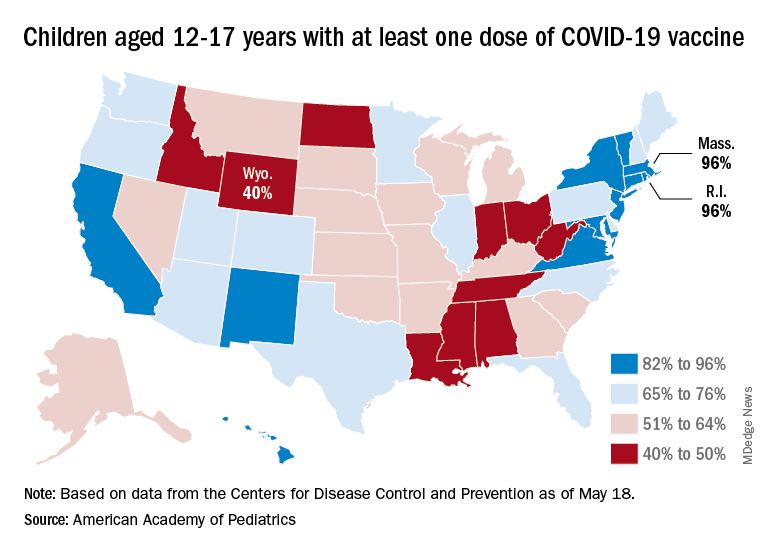
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
FDA, AMA prepare for potential COVID-19 shots for children younger than 6
Regulators and the nation’s largest physician organization took separate steps in recent days to prepare for expected authorization of use of COVID-19 vaccines in children younger than age 6.
The Food and Drug Administration on May 23 announced its Vaccines and Related Biological Products Advisory Committee will meet June 15 to discuss expanding the use of COVID vaccines from Pfizer and Moderna.
The panel will examine a request from Pfizer and its partner BioNTech for an emergency use authorization (EUA) of its vaccine to cover children ages 6 months through 4 years. The EUA expansion for the Moderna shot would cover children ages 6 months through 5 years, the FDA said.
Many parents and physicians have been urging regulators to clear COVID shots for young children, among whom rates of infection are high.
The American Medical Association in February announced an update of its Current Procedural Terminology (CPT) to prepare for an eventual FDA clearance of the Pfizer-BioNTech shot for children aged 6 months to younger than 5 years. On May 19, the association announced a new CPT update to prepare for FDA clearance for use of the Moderna COVID-19 vaccine for children 6 months through 5 years.
“Extending COVID-19 vaccination protection to approximately 18 million young children will significantly reduce their risk of COVID-19 infection, hospitalization, and death, and give their parents incredible peace of mind,” Gerald Harmon, MD, AMA’s president, said in a statement. “We strongly urge all parents to get their infants and toddlers vaccinated as soon as they are eligible for a COVID-19 vaccine.”
Both the Moderna and the Pfizer-BioNTech COVID vaccines would be given to these young children in low doses.
On May 23, Pfizer announced results from a phase 2/3 trial evaluating a series of three shots of its vaccine in children ages 6 months to younger than 5 years.
Vaccine efficacy, which was a secondary endpoint in this study, was 80.3% in this age group, Pfizer said. The analysis was based on 10 symptomatic cases of COVID-19. The trial’s protocol specifies a formal analysis will be performed when at least 21 cases have accrued from 7 days after the third dose. The company said it would share final data on the effectiveness of the vaccine once the results are available.
Moderna on April 28 issued a statement with details about testing of its vaccine in young children. Vaccine efficacy was estimated at about 51% for children aged 6 months to younger than 2 years and 37% for the children aged 2 years to younger than 6. Paul Burton, MD, Moderna’s chief medical officer, spoke about this rate during a May 1 appearance on CBS’ Face the Nation.
“What it means for parents, for caregivers, is that if they give the Moderna vaccine to these little kids, they would basically cut in half the risk of that child getting symptomatic COVID,” Dr. Burton said in the interview. “Now, the number, 50%, I know is often lower than we are used to seeing with our vaccine, but it’s because this study was conducted during a time of Omicron.”
The FDA’s vaccine advisory committee also will meet on June 14 discuss potential use under an EUA of Moderna’s COVID vaccine for children and teenagers aged 6-17 years. The Pfizer-BioNTech vaccine already is authorized under an EUA for people aged 5 years and older.
The FDA has to date granted both conditional clearances, or EUAs, and regular approvals for COVID vaccines.
EUAs are meant to be temporary, allowing for rapid introduction of medicines in response to public health crises such as the pandemic. The FDA also uses EUAs to provide initial clearances of additional indications for products, as would be the case with the authorizations Moderna and Pfizer-BioNTech are seeking for their COVID vaccines.
Companies that want to continue to sell EUA-cleared products or promote EUA-cleared indications beyond the time of the public health crisis must seek regular approvals.
The FDA cleared the Pfizer-BioNTech and Moderna COVID vaccines under EUAs in December 2020. The agency then granted a regular approval for the Pfizer-BioNTech vaccine for people ages 16 and older in August 2021 based on more robust data. Regular approval for the Moderna vaccine for people ages 18 and older followed in January 2022.
Varied reactions among parents
Attitudes in the United States about pediatric COVID vaccines are far from uniform.
The initial uptake has disappointed physicians and researchers, who have been urging wider use of the COVID vaccination among children and teens for whom the FDA already has granted a clearance. Many parents are hesitating to bring their children for the COVID vaccines, according to the Centers for Disease Control and Prevention. Only 35.4% of children ages 5-11 had received at least one dose of a COVID vaccine, CDC staff said during a meeting.
Yet many other parents are demanding this medicine for their young children, urging the FDA to move quickly to clear COVID shots.
A private Facebook group called “Protect Their Future: A Call to Action for COVID Vaccines in Kids <5” boasts about 6,200 members. Many parents and physicians have used Twitter in recent months to press for a speedy review of COVID vaccines for the youngest children, often using the hashtag #immunizeunder5s. A group called Protect Their Future, which uses @ImmunizeUnder5s as its Twitter handle, had 5,288 followers as of the afternoon of May 23.
A special panel of the House of Representatives, the Select Subcommittee on the Coronavirus Crisis, on May 23 joined those tweeting about the need to soon authorize COVID vaccines for very young children.
“Parents have been waiting many months for vaccines for their young children,” the subcommittee tweeted. “They deserve to hear from @US_FDA why this lengthy process has been in children’s best interests.”
A version of this article first appeared on Medscape.com.
Regulators and the nation’s largest physician organization took separate steps in recent days to prepare for expected authorization of use of COVID-19 vaccines in children younger than age 6.
The Food and Drug Administration on May 23 announced its Vaccines and Related Biological Products Advisory Committee will meet June 15 to discuss expanding the use of COVID vaccines from Pfizer and Moderna.
The panel will examine a request from Pfizer and its partner BioNTech for an emergency use authorization (EUA) of its vaccine to cover children ages 6 months through 4 years. The EUA expansion for the Moderna shot would cover children ages 6 months through 5 years, the FDA said.
Many parents and physicians have been urging regulators to clear COVID shots for young children, among whom rates of infection are high.
The American Medical Association in February announced an update of its Current Procedural Terminology (CPT) to prepare for an eventual FDA clearance of the Pfizer-BioNTech shot for children aged 6 months to younger than 5 years. On May 19, the association announced a new CPT update to prepare for FDA clearance for use of the Moderna COVID-19 vaccine for children 6 months through 5 years.
“Extending COVID-19 vaccination protection to approximately 18 million young children will significantly reduce their risk of COVID-19 infection, hospitalization, and death, and give their parents incredible peace of mind,” Gerald Harmon, MD, AMA’s president, said in a statement. “We strongly urge all parents to get their infants and toddlers vaccinated as soon as they are eligible for a COVID-19 vaccine.”
Both the Moderna and the Pfizer-BioNTech COVID vaccines would be given to these young children in low doses.
On May 23, Pfizer announced results from a phase 2/3 trial evaluating a series of three shots of its vaccine in children ages 6 months to younger than 5 years.
Vaccine efficacy, which was a secondary endpoint in this study, was 80.3% in this age group, Pfizer said. The analysis was based on 10 symptomatic cases of COVID-19. The trial’s protocol specifies a formal analysis will be performed when at least 21 cases have accrued from 7 days after the third dose. The company said it would share final data on the effectiveness of the vaccine once the results are available.
Moderna on April 28 issued a statement with details about testing of its vaccine in young children. Vaccine efficacy was estimated at about 51% for children aged 6 months to younger than 2 years and 37% for the children aged 2 years to younger than 6. Paul Burton, MD, Moderna’s chief medical officer, spoke about this rate during a May 1 appearance on CBS’ Face the Nation.
“What it means for parents, for caregivers, is that if they give the Moderna vaccine to these little kids, they would basically cut in half the risk of that child getting symptomatic COVID,” Dr. Burton said in the interview. “Now, the number, 50%, I know is often lower than we are used to seeing with our vaccine, but it’s because this study was conducted during a time of Omicron.”
The FDA’s vaccine advisory committee also will meet on June 14 discuss potential use under an EUA of Moderna’s COVID vaccine for children and teenagers aged 6-17 years. The Pfizer-BioNTech vaccine already is authorized under an EUA for people aged 5 years and older.
The FDA has to date granted both conditional clearances, or EUAs, and regular approvals for COVID vaccines.
EUAs are meant to be temporary, allowing for rapid introduction of medicines in response to public health crises such as the pandemic. The FDA also uses EUAs to provide initial clearances of additional indications for products, as would be the case with the authorizations Moderna and Pfizer-BioNTech are seeking for their COVID vaccines.
Companies that want to continue to sell EUA-cleared products or promote EUA-cleared indications beyond the time of the public health crisis must seek regular approvals.
The FDA cleared the Pfizer-BioNTech and Moderna COVID vaccines under EUAs in December 2020. The agency then granted a regular approval for the Pfizer-BioNTech vaccine for people ages 16 and older in August 2021 based on more robust data. Regular approval for the Moderna vaccine for people ages 18 and older followed in January 2022.
Varied reactions among parents
Attitudes in the United States about pediatric COVID vaccines are far from uniform.
The initial uptake has disappointed physicians and researchers, who have been urging wider use of the COVID vaccination among children and teens for whom the FDA already has granted a clearance. Many parents are hesitating to bring their children for the COVID vaccines, according to the Centers for Disease Control and Prevention. Only 35.4% of children ages 5-11 had received at least one dose of a COVID vaccine, CDC staff said during a meeting.
Yet many other parents are demanding this medicine for their young children, urging the FDA to move quickly to clear COVID shots.
A private Facebook group called “Protect Their Future: A Call to Action for COVID Vaccines in Kids <5” boasts about 6,200 members. Many parents and physicians have used Twitter in recent months to press for a speedy review of COVID vaccines for the youngest children, often using the hashtag #immunizeunder5s. A group called Protect Their Future, which uses @ImmunizeUnder5s as its Twitter handle, had 5,288 followers as of the afternoon of May 23.
A special panel of the House of Representatives, the Select Subcommittee on the Coronavirus Crisis, on May 23 joined those tweeting about the need to soon authorize COVID vaccines for very young children.
“Parents have been waiting many months for vaccines for their young children,” the subcommittee tweeted. “They deserve to hear from @US_FDA why this lengthy process has been in children’s best interests.”
A version of this article first appeared on Medscape.com.
Regulators and the nation’s largest physician organization took separate steps in recent days to prepare for expected authorization of use of COVID-19 vaccines in children younger than age 6.
The Food and Drug Administration on May 23 announced its Vaccines and Related Biological Products Advisory Committee will meet June 15 to discuss expanding the use of COVID vaccines from Pfizer and Moderna.
The panel will examine a request from Pfizer and its partner BioNTech for an emergency use authorization (EUA) of its vaccine to cover children ages 6 months through 4 years. The EUA expansion for the Moderna shot would cover children ages 6 months through 5 years, the FDA said.
Many parents and physicians have been urging regulators to clear COVID shots for young children, among whom rates of infection are high.
The American Medical Association in February announced an update of its Current Procedural Terminology (CPT) to prepare for an eventual FDA clearance of the Pfizer-BioNTech shot for children aged 6 months to younger than 5 years. On May 19, the association announced a new CPT update to prepare for FDA clearance for use of the Moderna COVID-19 vaccine for children 6 months through 5 years.
“Extending COVID-19 vaccination protection to approximately 18 million young children will significantly reduce their risk of COVID-19 infection, hospitalization, and death, and give their parents incredible peace of mind,” Gerald Harmon, MD, AMA’s president, said in a statement. “We strongly urge all parents to get their infants and toddlers vaccinated as soon as they are eligible for a COVID-19 vaccine.”
Both the Moderna and the Pfizer-BioNTech COVID vaccines would be given to these young children in low doses.
On May 23, Pfizer announced results from a phase 2/3 trial evaluating a series of three shots of its vaccine in children ages 6 months to younger than 5 years.
Vaccine efficacy, which was a secondary endpoint in this study, was 80.3% in this age group, Pfizer said. The analysis was based on 10 symptomatic cases of COVID-19. The trial’s protocol specifies a formal analysis will be performed when at least 21 cases have accrued from 7 days after the third dose. The company said it would share final data on the effectiveness of the vaccine once the results are available.
Moderna on April 28 issued a statement with details about testing of its vaccine in young children. Vaccine efficacy was estimated at about 51% for children aged 6 months to younger than 2 years and 37% for the children aged 2 years to younger than 6. Paul Burton, MD, Moderna’s chief medical officer, spoke about this rate during a May 1 appearance on CBS’ Face the Nation.
“What it means for parents, for caregivers, is that if they give the Moderna vaccine to these little kids, they would basically cut in half the risk of that child getting symptomatic COVID,” Dr. Burton said in the interview. “Now, the number, 50%, I know is often lower than we are used to seeing with our vaccine, but it’s because this study was conducted during a time of Omicron.”
The FDA’s vaccine advisory committee also will meet on June 14 discuss potential use under an EUA of Moderna’s COVID vaccine for children and teenagers aged 6-17 years. The Pfizer-BioNTech vaccine already is authorized under an EUA for people aged 5 years and older.
The FDA has to date granted both conditional clearances, or EUAs, and regular approvals for COVID vaccines.
EUAs are meant to be temporary, allowing for rapid introduction of medicines in response to public health crises such as the pandemic. The FDA also uses EUAs to provide initial clearances of additional indications for products, as would be the case with the authorizations Moderna and Pfizer-BioNTech are seeking for their COVID vaccines.
Companies that want to continue to sell EUA-cleared products or promote EUA-cleared indications beyond the time of the public health crisis must seek regular approvals.
The FDA cleared the Pfizer-BioNTech and Moderna COVID vaccines under EUAs in December 2020. The agency then granted a regular approval for the Pfizer-BioNTech vaccine for people ages 16 and older in August 2021 based on more robust data. Regular approval for the Moderna vaccine for people ages 18 and older followed in January 2022.
Varied reactions among parents
Attitudes in the United States about pediatric COVID vaccines are far from uniform.
The initial uptake has disappointed physicians and researchers, who have been urging wider use of the COVID vaccination among children and teens for whom the FDA already has granted a clearance. Many parents are hesitating to bring their children for the COVID vaccines, according to the Centers for Disease Control and Prevention. Only 35.4% of children ages 5-11 had received at least one dose of a COVID vaccine, CDC staff said during a meeting.
Yet many other parents are demanding this medicine for their young children, urging the FDA to move quickly to clear COVID shots.
A private Facebook group called “Protect Their Future: A Call to Action for COVID Vaccines in Kids <5” boasts about 6,200 members. Many parents and physicians have used Twitter in recent months to press for a speedy review of COVID vaccines for the youngest children, often using the hashtag #immunizeunder5s. A group called Protect Their Future, which uses @ImmunizeUnder5s as its Twitter handle, had 5,288 followers as of the afternoon of May 23.
A special panel of the House of Representatives, the Select Subcommittee on the Coronavirus Crisis, on May 23 joined those tweeting about the need to soon authorize COVID vaccines for very young children.
“Parents have been waiting many months for vaccines for their young children,” the subcommittee tweeted. “They deserve to hear from @US_FDA why this lengthy process has been in children’s best interests.”
A version of this article first appeared on Medscape.com.
Fewer teens giving birth, but cases are more complex
Debra Katz, CNM, has noticed a shift in the number of teenagers coming to the teen obstetrics program at St. Joseph’s Medical Center in Paterson, N.J. A decade ago, about 30 adolescents gave birth in a given month; now, that figure is closer to 20, said Ms. Katz, chief of the nurse midwifery service at the center.
Ms. Katz’s observations mirror a national trend: The rate of teen births is falling in the United States, according to a study published in Obstetrics and Gynecology.
But, there’s a catch. The adolescents who are giving birth are more likely to have obesity, mental health problems, asthma, and other conditions that can complicate their pregnancies, the research shows. Rates of delivery complications have also increased in this age group.
Ms. Katz said that, compared with adult patients, teens tend to require longer medical visits. Most patients have limited knowledge of what prenatal care entails.
“Most of these patients have never even had a female [gynecologic] exam before,” Ms. Katz said. “They come in and they’re not used to the equipment. They’re not used to the terminology.”
Also consistent with the national trends, St. Joseph’s younger patients often have mental health problems or obesity. Many also lack stable housing and adequate food.
“Unfortunately, we are seeing a greater number of patients with morbid obesity; there’s a lot of bipolar disease; here’s a lot of depression; there’s a lot of anxiety,” Ms. Katz said. “And we also have a bit of PTSD [post traumatic stress disorder] as well.”
These factors make clinical practice more complex, according to the authors of the new study. “To optimize adolescent pregnancy outcomes, prenatal care will likely need to provide increasingly complex clinical management in addition to addressing outreach challenges of this population,” the authors of the new study write.
At St. Joseph’s, teens receive prenatal care in a group setting with other patients who are due to deliver in the same month. This model, called CenteringPregnancy, can increase self-esteem, build community, and may improve patient outcomes, Ms. Katz said. The program uses a team approach that includes a dietitian and social worker to address social support needs.
Shifting health status
To characterize delivery hospitalization trends for patients aged 11-19 years, Anna P. Staniczenko, MD, with Columbia University Irving Medical Center, New York, and her colleagues conducted a cross-sectional analysis of data from the 2000-2018 National Inpatient Sample.
Of more than 73 million estimated delivery hospitalizations during that period, 88,363 occurred in patients aged 11-14 years, and 6,359,331 were among patients aged 15-19 years.
Deliveries among patients aged 11-14 years decreased from 2.1 per 1,000 to 0.4 per 1,000 during the time frame. Deliveries among patients aged 15-19 years decreased from 11.5% of all deliveries to 4.8% over the study period.
Among patients aged 11-19 years, rates of comorbidities significantly increased from 2000 to 2018, the researchers found. The prevalence of obesity increased from 0.2% to 7.2%, asthma increased from 1.6% to 7%, while mental health conditions increased from 0.5% to 7.1%.
Severe maternal morbidity, defined as a patient having at least one of 20 conditions, including stroke, heart failure, and sepsis, increased from 0.5% to 0.7%. The rate of postpartum hemorrhage increased from 2.9% to 4.7%, the rate of cesarean delivery increased from 15.2% to 19.5%, and that of hypertensive disorders of pregnancy increased from 7.5% to 13.7%.
An often overlooked group
Adolescent pregnancies are more common in the United States than in other wealthy nations, and about 80% are unintended. In addition to the growth in comorbid conditions, adolescent mothers are at an increased risk of living under the poverty line, and children born to teen moms may be at increased risk for adverse pediatric outcomes.
Still, these pregnancies “may be planned and desired. ... It is unclear that there is an ‘ideal’ rate of pregnancy for this age group,” the study authors write.
Prior research has shown an increase in rates of chronic conditions among adults giving birth, but, “from what I could tell, this is really the first data” on chronic conditions in the pediatric obstetric population, said Lindsay K. Admon, MD, an ob.gyn. at the University of Michigan, Ann Arbor, who wrote an editorial accompanying the journal article.
Behind the decline
That there are fewer teen deliveries may be because the adolescent population is savvier about contraceptive methods. In addition, the Affordable Care Act expanded insurance coverage of contraception, said Stephanie Teal, MD, MPH, chair of obstetrics and gynecology and reproductive biology at University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine, Cleveland.
Dr. Teal was involved in the Colorado Family Planning Initiative, a state effort that showed that long-acting reversible contraception was effective and acceptable to young people.
“We are definitely seeing more adolescents who use birth control the first time they have sex,” Dr. Teal told this news organization. “When I started in practice, it was fairly uncommon that I would see a teenager who was sexually active who was consistently using a birth control method. And now they just look at me, roll their eyes, and are, like, ‘Duh, of course. He uses condoms, and I have an IUD.’ ”
To the extent that these deliveries include unintended pregnancies, the data may point to a need for clinicians to provide contraceptive education to adolescents with chronic conditions, according to Dr. Admon.
Abortion shifts
If U.S. Supreme Court rulings and state laws further limit access to contraception or abortion, the result could lead to more teen deliveries, Dr. Admon said.
While the adolescent birth rate has plummeted, the teen abortion rate has not increased, Dr. Teal said.
“Pregnancy is a time of health risk for women, and it’s getting riskier,” she said. “Our concern is that if people are having to go through a pregnancy that they don’t feel physically or financially or emotionally prepared to go through, that we will see an increase in these kinds of adverse health outcomes with birth.”
One study author has a leadership role on an American College of Obstetricians and Gynecologists safe motherhood initiative that has received unrestricted funding from Merck for Mothers. Another author has ties to Delfina Care, and one is on the board of directors of Planned Parenthood of Greater New York. Dr. Admon receives funding from the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Teal has received grants from Merck, Bayer Healthcare, Sebela, and Medicines360 and personal fees from Merck and from Bayer Healthcare. Ms. Katz has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Debra Katz, CNM, has noticed a shift in the number of teenagers coming to the teen obstetrics program at St. Joseph’s Medical Center in Paterson, N.J. A decade ago, about 30 adolescents gave birth in a given month; now, that figure is closer to 20, said Ms. Katz, chief of the nurse midwifery service at the center.
Ms. Katz’s observations mirror a national trend: The rate of teen births is falling in the United States, according to a study published in Obstetrics and Gynecology.
But, there’s a catch. The adolescents who are giving birth are more likely to have obesity, mental health problems, asthma, and other conditions that can complicate their pregnancies, the research shows. Rates of delivery complications have also increased in this age group.
Ms. Katz said that, compared with adult patients, teens tend to require longer medical visits. Most patients have limited knowledge of what prenatal care entails.
“Most of these patients have never even had a female [gynecologic] exam before,” Ms. Katz said. “They come in and they’re not used to the equipment. They’re not used to the terminology.”
Also consistent with the national trends, St. Joseph’s younger patients often have mental health problems or obesity. Many also lack stable housing and adequate food.
“Unfortunately, we are seeing a greater number of patients with morbid obesity; there’s a lot of bipolar disease; here’s a lot of depression; there’s a lot of anxiety,” Ms. Katz said. “And we also have a bit of PTSD [post traumatic stress disorder] as well.”
These factors make clinical practice more complex, according to the authors of the new study. “To optimize adolescent pregnancy outcomes, prenatal care will likely need to provide increasingly complex clinical management in addition to addressing outreach challenges of this population,” the authors of the new study write.
At St. Joseph’s, teens receive prenatal care in a group setting with other patients who are due to deliver in the same month. This model, called CenteringPregnancy, can increase self-esteem, build community, and may improve patient outcomes, Ms. Katz said. The program uses a team approach that includes a dietitian and social worker to address social support needs.
Shifting health status
To characterize delivery hospitalization trends for patients aged 11-19 years, Anna P. Staniczenko, MD, with Columbia University Irving Medical Center, New York, and her colleagues conducted a cross-sectional analysis of data from the 2000-2018 National Inpatient Sample.
Of more than 73 million estimated delivery hospitalizations during that period, 88,363 occurred in patients aged 11-14 years, and 6,359,331 were among patients aged 15-19 years.
Deliveries among patients aged 11-14 years decreased from 2.1 per 1,000 to 0.4 per 1,000 during the time frame. Deliveries among patients aged 15-19 years decreased from 11.5% of all deliveries to 4.8% over the study period.
Among patients aged 11-19 years, rates of comorbidities significantly increased from 2000 to 2018, the researchers found. The prevalence of obesity increased from 0.2% to 7.2%, asthma increased from 1.6% to 7%, while mental health conditions increased from 0.5% to 7.1%.
Severe maternal morbidity, defined as a patient having at least one of 20 conditions, including stroke, heart failure, and sepsis, increased from 0.5% to 0.7%. The rate of postpartum hemorrhage increased from 2.9% to 4.7%, the rate of cesarean delivery increased from 15.2% to 19.5%, and that of hypertensive disorders of pregnancy increased from 7.5% to 13.7%.
An often overlooked group
Adolescent pregnancies are more common in the United States than in other wealthy nations, and about 80% are unintended. In addition to the growth in comorbid conditions, adolescent mothers are at an increased risk of living under the poverty line, and children born to teen moms may be at increased risk for adverse pediatric outcomes.
Still, these pregnancies “may be planned and desired. ... It is unclear that there is an ‘ideal’ rate of pregnancy for this age group,” the study authors write.
Prior research has shown an increase in rates of chronic conditions among adults giving birth, but, “from what I could tell, this is really the first data” on chronic conditions in the pediatric obstetric population, said Lindsay K. Admon, MD, an ob.gyn. at the University of Michigan, Ann Arbor, who wrote an editorial accompanying the journal article.
Behind the decline
That there are fewer teen deliveries may be because the adolescent population is savvier about contraceptive methods. In addition, the Affordable Care Act expanded insurance coverage of contraception, said Stephanie Teal, MD, MPH, chair of obstetrics and gynecology and reproductive biology at University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine, Cleveland.
Dr. Teal was involved in the Colorado Family Planning Initiative, a state effort that showed that long-acting reversible contraception was effective and acceptable to young people.
“We are definitely seeing more adolescents who use birth control the first time they have sex,” Dr. Teal told this news organization. “When I started in practice, it was fairly uncommon that I would see a teenager who was sexually active who was consistently using a birth control method. And now they just look at me, roll their eyes, and are, like, ‘Duh, of course. He uses condoms, and I have an IUD.’ ”
To the extent that these deliveries include unintended pregnancies, the data may point to a need for clinicians to provide contraceptive education to adolescents with chronic conditions, according to Dr. Admon.
Abortion shifts
If U.S. Supreme Court rulings and state laws further limit access to contraception or abortion, the result could lead to more teen deliveries, Dr. Admon said.
While the adolescent birth rate has plummeted, the teen abortion rate has not increased, Dr. Teal said.
“Pregnancy is a time of health risk for women, and it’s getting riskier,” she said. “Our concern is that if people are having to go through a pregnancy that they don’t feel physically or financially or emotionally prepared to go through, that we will see an increase in these kinds of adverse health outcomes with birth.”
One study author has a leadership role on an American College of Obstetricians and Gynecologists safe motherhood initiative that has received unrestricted funding from Merck for Mothers. Another author has ties to Delfina Care, and one is on the board of directors of Planned Parenthood of Greater New York. Dr. Admon receives funding from the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Teal has received grants from Merck, Bayer Healthcare, Sebela, and Medicines360 and personal fees from Merck and from Bayer Healthcare. Ms. Katz has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Debra Katz, CNM, has noticed a shift in the number of teenagers coming to the teen obstetrics program at St. Joseph’s Medical Center in Paterson, N.J. A decade ago, about 30 adolescents gave birth in a given month; now, that figure is closer to 20, said Ms. Katz, chief of the nurse midwifery service at the center.
Ms. Katz’s observations mirror a national trend: The rate of teen births is falling in the United States, according to a study published in Obstetrics and Gynecology.
But, there’s a catch. The adolescents who are giving birth are more likely to have obesity, mental health problems, asthma, and other conditions that can complicate their pregnancies, the research shows. Rates of delivery complications have also increased in this age group.
Ms. Katz said that, compared with adult patients, teens tend to require longer medical visits. Most patients have limited knowledge of what prenatal care entails.
“Most of these patients have never even had a female [gynecologic] exam before,” Ms. Katz said. “They come in and they’re not used to the equipment. They’re not used to the terminology.”
Also consistent with the national trends, St. Joseph’s younger patients often have mental health problems or obesity. Many also lack stable housing and adequate food.
“Unfortunately, we are seeing a greater number of patients with morbid obesity; there’s a lot of bipolar disease; here’s a lot of depression; there’s a lot of anxiety,” Ms. Katz said. “And we also have a bit of PTSD [post traumatic stress disorder] as well.”
These factors make clinical practice more complex, according to the authors of the new study. “To optimize adolescent pregnancy outcomes, prenatal care will likely need to provide increasingly complex clinical management in addition to addressing outreach challenges of this population,” the authors of the new study write.
At St. Joseph’s, teens receive prenatal care in a group setting with other patients who are due to deliver in the same month. This model, called CenteringPregnancy, can increase self-esteem, build community, and may improve patient outcomes, Ms. Katz said. The program uses a team approach that includes a dietitian and social worker to address social support needs.
Shifting health status
To characterize delivery hospitalization trends for patients aged 11-19 years, Anna P. Staniczenko, MD, with Columbia University Irving Medical Center, New York, and her colleagues conducted a cross-sectional analysis of data from the 2000-2018 National Inpatient Sample.
Of more than 73 million estimated delivery hospitalizations during that period, 88,363 occurred in patients aged 11-14 years, and 6,359,331 were among patients aged 15-19 years.
Deliveries among patients aged 11-14 years decreased from 2.1 per 1,000 to 0.4 per 1,000 during the time frame. Deliveries among patients aged 15-19 years decreased from 11.5% of all deliveries to 4.8% over the study period.
Among patients aged 11-19 years, rates of comorbidities significantly increased from 2000 to 2018, the researchers found. The prevalence of obesity increased from 0.2% to 7.2%, asthma increased from 1.6% to 7%, while mental health conditions increased from 0.5% to 7.1%.
Severe maternal morbidity, defined as a patient having at least one of 20 conditions, including stroke, heart failure, and sepsis, increased from 0.5% to 0.7%. The rate of postpartum hemorrhage increased from 2.9% to 4.7%, the rate of cesarean delivery increased from 15.2% to 19.5%, and that of hypertensive disorders of pregnancy increased from 7.5% to 13.7%.
An often overlooked group
Adolescent pregnancies are more common in the United States than in other wealthy nations, and about 80% are unintended. In addition to the growth in comorbid conditions, adolescent mothers are at an increased risk of living under the poverty line, and children born to teen moms may be at increased risk for adverse pediatric outcomes.
Still, these pregnancies “may be planned and desired. ... It is unclear that there is an ‘ideal’ rate of pregnancy for this age group,” the study authors write.
Prior research has shown an increase in rates of chronic conditions among adults giving birth, but, “from what I could tell, this is really the first data” on chronic conditions in the pediatric obstetric population, said Lindsay K. Admon, MD, an ob.gyn. at the University of Michigan, Ann Arbor, who wrote an editorial accompanying the journal article.
Behind the decline
That there are fewer teen deliveries may be because the adolescent population is savvier about contraceptive methods. In addition, the Affordable Care Act expanded insurance coverage of contraception, said Stephanie Teal, MD, MPH, chair of obstetrics and gynecology and reproductive biology at University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine, Cleveland.
Dr. Teal was involved in the Colorado Family Planning Initiative, a state effort that showed that long-acting reversible contraception was effective and acceptable to young people.
“We are definitely seeing more adolescents who use birth control the first time they have sex,” Dr. Teal told this news organization. “When I started in practice, it was fairly uncommon that I would see a teenager who was sexually active who was consistently using a birth control method. And now they just look at me, roll their eyes, and are, like, ‘Duh, of course. He uses condoms, and I have an IUD.’ ”
To the extent that these deliveries include unintended pregnancies, the data may point to a need for clinicians to provide contraceptive education to adolescents with chronic conditions, according to Dr. Admon.
Abortion shifts
If U.S. Supreme Court rulings and state laws further limit access to contraception or abortion, the result could lead to more teen deliveries, Dr. Admon said.
While the adolescent birth rate has plummeted, the teen abortion rate has not increased, Dr. Teal said.
“Pregnancy is a time of health risk for women, and it’s getting riskier,” she said. “Our concern is that if people are having to go through a pregnancy that they don’t feel physically or financially or emotionally prepared to go through, that we will see an increase in these kinds of adverse health outcomes with birth.”
One study author has a leadership role on an American College of Obstetricians and Gynecologists safe motherhood initiative that has received unrestricted funding from Merck for Mothers. Another author has ties to Delfina Care, and one is on the board of directors of Planned Parenthood of Greater New York. Dr. Admon receives funding from the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Teal has received grants from Merck, Bayer Healthcare, Sebela, and Medicines360 and personal fees from Merck and from Bayer Healthcare. Ms. Katz has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Food allergy risk not greater in C-section infants
Cesarean births are not likely linked to an elevated risk of food allergy during the first year of life, an Australian study found.
Published online in the Journal of Allergy and Clinical Immunology, the findings may help assess the risks and benefits of cesarean delivery and reassure women who require it that their babies are not more likely to develop food allergy, according to Rachel L. Peters, PhD, an epidemiologist at the Murdoch Child Research Institute (MCRI) in Melbourne, and colleagues.
Dr. Peters’ group undertook the analysis to clarify a possible association between mode of delivery and food allergy risk, which has remained unclear owing to the absence of studies with both challenge-proven food allergy outcomes and detailed information on the type and timing of cesarean delivery.
“The infant immune system undergoes rapid development during the neonatal period,” Dr. Peters said in an MCRI press release, and the mode of delivery may interfere with the normal development of the immune system. “Babies born by cesarean have less exposure to the bacteria from the mother’s gut and vagina, which influence the composition of the baby’s microbiome and immune system development. However, this doesn’t appear to play a major role in the development of food allergy,” she said.
The HealthNuts study
In the period 2007-2011, the longitudinal population-based HealthNuts cohort study enrolled 5,276 12-month-olds who underwent skin prick testing and oral food challenge for sensitization to egg, peanut, sesame, and either shellfish or cow’s milk. It linked the resulting data to additional birth statistics from the Victorian Perinatal Data Collection when children turned 6.
Birth data were obtained on 2,045 babies, and in this subgroup with linked data, 30% were born by cesarean – similar to the 31.7% of U.S. cesarean births in 2019 – and 12.7% of these had food allergy versus 13.2% of those delivered vaginally.
Compared with vaginal birth, C-section was not associated with the risk of food allergy (adjusted odds ratio [aOR] 0.95, 95% confidence interval [CI], 0.70-0.30).
Nor did the timing of the C-section have an effect. Cesarean delivery either before labor or after onset of labor was not associated with the risk of food allergy (aOR, 0.83, 95% CI, 0.55-1.23) and aOR, 1.13, 95% CI, 0.75-1.72), respectively.
Compared with vaginal delivery, elective or emergency cesarean was not associated with food allergy risk (aOR, 1.05, 95% CI, 0.71-1.55, and aOR, 0.86, 95% CI, 0.56-1.31).
Similarly, no evidence emerged of an effect modification by breastfeeding, older siblings, pet dog ownership, or maternal allergy.
“This study is helpful because in addition to blood and skin tests, it also used food challenge, which is the gold standard,” Terri Brown-Whitehorn, MD, an attending physician in the division of allergy and immunology at Children’s Hospital of Philadelphia, said in an interview. “If no actual food is given, the other tests could lead to false positives.”
Dr. Brown-Whitehorn, who was not involved in the MCRI research, said the findings are not likely to affect most decisions about C-sections because most are not voluntary. “But if a mother had a first baby by emergency cesarean section, she might be given the option of having the next one by the same method.”
She said the current advice is to introduce even high-risk foods to a child’s diet early on to ward off the development of food allergies.
According to the microbial exposure hypothesis, it was previously thought that a potential link between cesarean birth and allergy might reflect differences in early exposure to maternal flora beneficial to the immune system in the vagina during delivery. A C-section might bypass the opportunity for neonatal gut colonization with maternal gut and vaginal flora, thereby raising allergy risk. A 2018 meta-analysis, for example, suggested cesarean birth could raise the risk for food allergies by 21%.
In other research from HealthNuts, 30% of child peanut allergy and 90% of egg allergy appear to resolve naturally by age 6. These numbers are somewhat higher than what Dr. Brown-Whitehorn sees. “We find that about 20% of peanut allergies and about 70% or 80% – maybe a bit less – of egg allergies resolve by age 6.”
This research was supported by the National Health & Medical Research Council of Australia, the Ilhan Food Allergy Foundation, AnaphylaxiStop, the Charles and Sylvia Viertel Medical Research Foundation, the Victorian Government’s Operational Infrastructure Support Program, and the Melbourne Children’s Clinician-Scientist Fellowship.
Dr. Peters disclosed no competing interests. Several coauthors reported research support or employment with private companies and one is the inventor of an MCRI-held patent. Dr. Brown-Whitehorn had no competing interests to disclose.
Cesarean births are not likely linked to an elevated risk of food allergy during the first year of life, an Australian study found.
Published online in the Journal of Allergy and Clinical Immunology, the findings may help assess the risks and benefits of cesarean delivery and reassure women who require it that their babies are not more likely to develop food allergy, according to Rachel L. Peters, PhD, an epidemiologist at the Murdoch Child Research Institute (MCRI) in Melbourne, and colleagues.
Dr. Peters’ group undertook the analysis to clarify a possible association between mode of delivery and food allergy risk, which has remained unclear owing to the absence of studies with both challenge-proven food allergy outcomes and detailed information on the type and timing of cesarean delivery.
“The infant immune system undergoes rapid development during the neonatal period,” Dr. Peters said in an MCRI press release, and the mode of delivery may interfere with the normal development of the immune system. “Babies born by cesarean have less exposure to the bacteria from the mother’s gut and vagina, which influence the composition of the baby’s microbiome and immune system development. However, this doesn’t appear to play a major role in the development of food allergy,” she said.
The HealthNuts study
In the period 2007-2011, the longitudinal population-based HealthNuts cohort study enrolled 5,276 12-month-olds who underwent skin prick testing and oral food challenge for sensitization to egg, peanut, sesame, and either shellfish or cow’s milk. It linked the resulting data to additional birth statistics from the Victorian Perinatal Data Collection when children turned 6.
Birth data were obtained on 2,045 babies, and in this subgroup with linked data, 30% were born by cesarean – similar to the 31.7% of U.S. cesarean births in 2019 – and 12.7% of these had food allergy versus 13.2% of those delivered vaginally.
Compared with vaginal birth, C-section was not associated with the risk of food allergy (adjusted odds ratio [aOR] 0.95, 95% confidence interval [CI], 0.70-0.30).
Nor did the timing of the C-section have an effect. Cesarean delivery either before labor or after onset of labor was not associated with the risk of food allergy (aOR, 0.83, 95% CI, 0.55-1.23) and aOR, 1.13, 95% CI, 0.75-1.72), respectively.
Compared with vaginal delivery, elective or emergency cesarean was not associated with food allergy risk (aOR, 1.05, 95% CI, 0.71-1.55, and aOR, 0.86, 95% CI, 0.56-1.31).
Similarly, no evidence emerged of an effect modification by breastfeeding, older siblings, pet dog ownership, or maternal allergy.
“This study is helpful because in addition to blood and skin tests, it also used food challenge, which is the gold standard,” Terri Brown-Whitehorn, MD, an attending physician in the division of allergy and immunology at Children’s Hospital of Philadelphia, said in an interview. “If no actual food is given, the other tests could lead to false positives.”
Dr. Brown-Whitehorn, who was not involved in the MCRI research, said the findings are not likely to affect most decisions about C-sections because most are not voluntary. “But if a mother had a first baby by emergency cesarean section, she might be given the option of having the next one by the same method.”
She said the current advice is to introduce even high-risk foods to a child’s diet early on to ward off the development of food allergies.
According to the microbial exposure hypothesis, it was previously thought that a potential link between cesarean birth and allergy might reflect differences in early exposure to maternal flora beneficial to the immune system in the vagina during delivery. A C-section might bypass the opportunity for neonatal gut colonization with maternal gut and vaginal flora, thereby raising allergy risk. A 2018 meta-analysis, for example, suggested cesarean birth could raise the risk for food allergies by 21%.
In other research from HealthNuts, 30% of child peanut allergy and 90% of egg allergy appear to resolve naturally by age 6. These numbers are somewhat higher than what Dr. Brown-Whitehorn sees. “We find that about 20% of peanut allergies and about 70% or 80% – maybe a bit less – of egg allergies resolve by age 6.”
This research was supported by the National Health & Medical Research Council of Australia, the Ilhan Food Allergy Foundation, AnaphylaxiStop, the Charles and Sylvia Viertel Medical Research Foundation, the Victorian Government’s Operational Infrastructure Support Program, and the Melbourne Children’s Clinician-Scientist Fellowship.
Dr. Peters disclosed no competing interests. Several coauthors reported research support or employment with private companies and one is the inventor of an MCRI-held patent. Dr. Brown-Whitehorn had no competing interests to disclose.
Cesarean births are not likely linked to an elevated risk of food allergy during the first year of life, an Australian study found.
Published online in the Journal of Allergy and Clinical Immunology, the findings may help assess the risks and benefits of cesarean delivery and reassure women who require it that their babies are not more likely to develop food allergy, according to Rachel L. Peters, PhD, an epidemiologist at the Murdoch Child Research Institute (MCRI) in Melbourne, and colleagues.
Dr. Peters’ group undertook the analysis to clarify a possible association between mode of delivery and food allergy risk, which has remained unclear owing to the absence of studies with both challenge-proven food allergy outcomes and detailed information on the type and timing of cesarean delivery.
“The infant immune system undergoes rapid development during the neonatal period,” Dr. Peters said in an MCRI press release, and the mode of delivery may interfere with the normal development of the immune system. “Babies born by cesarean have less exposure to the bacteria from the mother’s gut and vagina, which influence the composition of the baby’s microbiome and immune system development. However, this doesn’t appear to play a major role in the development of food allergy,” she said.
The HealthNuts study
In the period 2007-2011, the longitudinal population-based HealthNuts cohort study enrolled 5,276 12-month-olds who underwent skin prick testing and oral food challenge for sensitization to egg, peanut, sesame, and either shellfish or cow’s milk. It linked the resulting data to additional birth statistics from the Victorian Perinatal Data Collection when children turned 6.
Birth data were obtained on 2,045 babies, and in this subgroup with linked data, 30% were born by cesarean – similar to the 31.7% of U.S. cesarean births in 2019 – and 12.7% of these had food allergy versus 13.2% of those delivered vaginally.
Compared with vaginal birth, C-section was not associated with the risk of food allergy (adjusted odds ratio [aOR] 0.95, 95% confidence interval [CI], 0.70-0.30).
Nor did the timing of the C-section have an effect. Cesarean delivery either before labor or after onset of labor was not associated with the risk of food allergy (aOR, 0.83, 95% CI, 0.55-1.23) and aOR, 1.13, 95% CI, 0.75-1.72), respectively.
Compared with vaginal delivery, elective or emergency cesarean was not associated with food allergy risk (aOR, 1.05, 95% CI, 0.71-1.55, and aOR, 0.86, 95% CI, 0.56-1.31).
Similarly, no evidence emerged of an effect modification by breastfeeding, older siblings, pet dog ownership, or maternal allergy.
“This study is helpful because in addition to blood and skin tests, it also used food challenge, which is the gold standard,” Terri Brown-Whitehorn, MD, an attending physician in the division of allergy and immunology at Children’s Hospital of Philadelphia, said in an interview. “If no actual food is given, the other tests could lead to false positives.”
Dr. Brown-Whitehorn, who was not involved in the MCRI research, said the findings are not likely to affect most decisions about C-sections because most are not voluntary. “But if a mother had a first baby by emergency cesarean section, she might be given the option of having the next one by the same method.”
She said the current advice is to introduce even high-risk foods to a child’s diet early on to ward off the development of food allergies.
According to the microbial exposure hypothesis, it was previously thought that a potential link between cesarean birth and allergy might reflect differences in early exposure to maternal flora beneficial to the immune system in the vagina during delivery. A C-section might bypass the opportunity for neonatal gut colonization with maternal gut and vaginal flora, thereby raising allergy risk. A 2018 meta-analysis, for example, suggested cesarean birth could raise the risk for food allergies by 21%.
In other research from HealthNuts, 30% of child peanut allergy and 90% of egg allergy appear to resolve naturally by age 6. These numbers are somewhat higher than what Dr. Brown-Whitehorn sees. “We find that about 20% of peanut allergies and about 70% or 80% – maybe a bit less – of egg allergies resolve by age 6.”
This research was supported by the National Health & Medical Research Council of Australia, the Ilhan Food Allergy Foundation, AnaphylaxiStop, the Charles and Sylvia Viertel Medical Research Foundation, the Victorian Government’s Operational Infrastructure Support Program, and the Melbourne Children’s Clinician-Scientist Fellowship.
Dr. Peters disclosed no competing interests. Several coauthors reported research support or employment with private companies and one is the inventor of an MCRI-held patent. Dr. Brown-Whitehorn had no competing interests to disclose.
FROM JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY
Exploding e-cigarettes cause traumatic injuries in teens
A study shows that, over a 4-year period, 15 teenagers were injured from exploding e-cigarettes, according to surgeons who have treated young people at nine hospitals in the United States.
“It definitely was an injury we were seeing frequently,” Shannon Acker, MD, an assistant professor of pediatric surgery at the University of Colorado at Denver, Aurora, and a pediatric surgeon at Children’s Hospital Colorado, said in a statement.
Reporting in the Journal of Surgical Research, doctors detail injuries from e-cigarette explosions from January 2016 through December 2019. Ten teens were hospitalized, including three who were admitted to ICUs.
“When we think about e-cigarettes, vaping, and the problems of marketing cigarettes to teenagers, it usually has to do with addiction and lung injury,” said Dr. Acker, a coauthor of the new study. “Whereas we, as trauma surgeons, were seeing these other traumatic injuries.”
Six of the teens had facial burns, five of them lost multiple teeth, five had burns around the thighs and groin, four burned their hands, and four burned their eyes. One teen injured their radial nerve, which runs through the arm. Another cut their face, and one fractured their jaw.
Overall, six teens needed surgery, including one who needed multiple operations for a severe hand injury.
Three of the teenagers had never used e-cigarettes before the day they were hurt.
Vaping has become far more common than smoking traditional cigarettes among U.S. teens in recent years. More than 2 million of them currently use e-cigarettes, according to the Food and Drug Administration, including more than 11% of high school students and almost 3% of middle schoolers.
Most e-cigarettes contain nicotine, which is highly addictive and can impair healthy brain development in adolescents, according to the CDC. Other chemicals and flavorings in the liquids that are heated during vaping can also damage the lungs. Fires and explosions, while rare, are also a risk that’s been previously documented by the FDA, the Centers for Disease Control and Prevention, and the Federal Emergency Management Agency.
Nationwide, there were 195 reported explosions and fires involving e-cigarettes in all ages between 2009 and 2016, according to a FEMA report. While no deaths were reported, 29% of these cases involved severe injuries.
“The shape and construction of electronic cigarettes” can make them behave like “flaming rockets when a battery fails,” according to FEMA.
Vaping devices typically use a rechargeable lithium-ion battery that vaporizes the liquid nicotine solution, Dr. Acker said. “They are not highly regulated, and the batteries may be of inferior quality and prone to explosion.”
A version of this article first appeared on WebMD.com.
A study shows that, over a 4-year period, 15 teenagers were injured from exploding e-cigarettes, according to surgeons who have treated young people at nine hospitals in the United States.
“It definitely was an injury we were seeing frequently,” Shannon Acker, MD, an assistant professor of pediatric surgery at the University of Colorado at Denver, Aurora, and a pediatric surgeon at Children’s Hospital Colorado, said in a statement.
Reporting in the Journal of Surgical Research, doctors detail injuries from e-cigarette explosions from January 2016 through December 2019. Ten teens were hospitalized, including three who were admitted to ICUs.
“When we think about e-cigarettes, vaping, and the problems of marketing cigarettes to teenagers, it usually has to do with addiction and lung injury,” said Dr. Acker, a coauthor of the new study. “Whereas we, as trauma surgeons, were seeing these other traumatic injuries.”
Six of the teens had facial burns, five of them lost multiple teeth, five had burns around the thighs and groin, four burned their hands, and four burned their eyes. One teen injured their radial nerve, which runs through the arm. Another cut their face, and one fractured their jaw.
Overall, six teens needed surgery, including one who needed multiple operations for a severe hand injury.
Three of the teenagers had never used e-cigarettes before the day they were hurt.
Vaping has become far more common than smoking traditional cigarettes among U.S. teens in recent years. More than 2 million of them currently use e-cigarettes, according to the Food and Drug Administration, including more than 11% of high school students and almost 3% of middle schoolers.
Most e-cigarettes contain nicotine, which is highly addictive and can impair healthy brain development in adolescents, according to the CDC. Other chemicals and flavorings in the liquids that are heated during vaping can also damage the lungs. Fires and explosions, while rare, are also a risk that’s been previously documented by the FDA, the Centers for Disease Control and Prevention, and the Federal Emergency Management Agency.
Nationwide, there were 195 reported explosions and fires involving e-cigarettes in all ages between 2009 and 2016, according to a FEMA report. While no deaths were reported, 29% of these cases involved severe injuries.
“The shape and construction of electronic cigarettes” can make them behave like “flaming rockets when a battery fails,” according to FEMA.
Vaping devices typically use a rechargeable lithium-ion battery that vaporizes the liquid nicotine solution, Dr. Acker said. “They are not highly regulated, and the batteries may be of inferior quality and prone to explosion.”
A version of this article first appeared on WebMD.com.
A study shows that, over a 4-year period, 15 teenagers were injured from exploding e-cigarettes, according to surgeons who have treated young people at nine hospitals in the United States.
“It definitely was an injury we were seeing frequently,” Shannon Acker, MD, an assistant professor of pediatric surgery at the University of Colorado at Denver, Aurora, and a pediatric surgeon at Children’s Hospital Colorado, said in a statement.
Reporting in the Journal of Surgical Research, doctors detail injuries from e-cigarette explosions from January 2016 through December 2019. Ten teens were hospitalized, including three who were admitted to ICUs.
“When we think about e-cigarettes, vaping, and the problems of marketing cigarettes to teenagers, it usually has to do with addiction and lung injury,” said Dr. Acker, a coauthor of the new study. “Whereas we, as trauma surgeons, were seeing these other traumatic injuries.”
Six of the teens had facial burns, five of them lost multiple teeth, five had burns around the thighs and groin, four burned their hands, and four burned their eyes. One teen injured their radial nerve, which runs through the arm. Another cut their face, and one fractured their jaw.
Overall, six teens needed surgery, including one who needed multiple operations for a severe hand injury.
Three of the teenagers had never used e-cigarettes before the day they were hurt.
Vaping has become far more common than smoking traditional cigarettes among U.S. teens in recent years. More than 2 million of them currently use e-cigarettes, according to the Food and Drug Administration, including more than 11% of high school students and almost 3% of middle schoolers.
Most e-cigarettes contain nicotine, which is highly addictive and can impair healthy brain development in adolescents, according to the CDC. Other chemicals and flavorings in the liquids that are heated during vaping can also damage the lungs. Fires and explosions, while rare, are also a risk that’s been previously documented by the FDA, the Centers for Disease Control and Prevention, and the Federal Emergency Management Agency.
Nationwide, there were 195 reported explosions and fires involving e-cigarettes in all ages between 2009 and 2016, according to a FEMA report. While no deaths were reported, 29% of these cases involved severe injuries.
“The shape and construction of electronic cigarettes” can make them behave like “flaming rockets when a battery fails,” according to FEMA.
Vaping devices typically use a rechargeable lithium-ion battery that vaporizes the liquid nicotine solution, Dr. Acker said. “They are not highly regulated, and the batteries may be of inferior quality and prone to explosion.”
A version of this article first appeared on WebMD.com.
FROM THE JOURNAL OF SURGICAL RESEARCH
RSV kills 100,000 kids under age 5 a year worldwide
Respiratory syncytial virus (RSV) caused more than 100,000 deaths in children under age 5 years globally in 2019, according to an analysis published online in The Lancet.
Researchers, led by You Li, PhD, of Nanjing (China) Medical University, found that nearly half of those (more than 45,000) occurred in children younger than 6 months old.
They estimated that RSV causes 1 in 50 deaths among children under 5 years old, and 1 in 28 deaths in children under 6 months old.
Additionally, RSV is responsible for an estimated 3.6 million hospital admissions globally each year, according to the report.
This analysis is the first to sift RSV disease burden into narrow age brackets, the authors said.
The numbers highlight that almost all of the deaths (97%) were in low- and middle-income countries.
Messages for prevention
Tina Hartert, MD, MPH, a professor in the division of allergy, pulmonary, and critical care medicine at Vanderbilt University, Nashville, Tenn., who was not part of the study, wrote in an invited commentary that these findings will be important in RSV prevention.
Among the most notable findings, she wrote, is the heavy mortality in the 0- to 6-month age group, which she notes is “the age group targeted by vaccination during pregnancy and birth-dose immunoprophylaxis.”
Dr. Hartert, who coauthored the commentary with Justin R. Ortiz, MD, MS, with the Center for Vaccine Development and Global Health, University of Maryland, Baltimore, told this news organization, “RSV is a respiratory virus that infects nearly every child by the time they are 2-3 years of age, with severe infection and death most common in the youngest infants. Vaccines that prevent the most severe infections in these young infants will likely be one of the best ways to prevent these severe infections and death.”
Though the authors found most deaths occur in low- and middle-income countries, RSV is one of the most common reasons for infant hospitalization in the US and affects 1% to 3% of infants, half of whom are full-term and otherwise healthy, Dr. Hartert said.
It is also one of the most common causes of infant lower respiratory tract infection in young children in the United States, she said, and it causes the most severe disease at the age extremes, with older adults experiencing significant morbidity with RSV.
Dr. Li said in an interview that although the team did not focus on reporting country-specific estimates in this work, their previous work, resulted in estimates of 98,000-155,000 RSV-related hospitalizations in children under 5 years old in the United States in 2019. Between 65,000 and 86,000 were in infants less than 1 year old.
Currently, he said, the only available RSV prophylaxis is palivizumab (Synagis), which is expensive and given only to high-risk infants in high-income countries, including the United States.
“There have been a number of promising RSV prophylactic products including maternal vaccine and monoclonal antibodies that have the potential for targeting the general infant population – not just high-risk infants – in late-phase clinical trials,” he said. “Our estimates of RSV-related disease burden will help anticipate the impact of future RSV immunization programs.”
Pandemic changed patterns
This research was completed before the COVID-19 pandemic, and it is not yet known how that could affect RSV disease burden long term.
However, Dr. Hartert said, RSV circulation has been significantly changed during the pandemic, both in intensity and timing, likely because of a combination of COVID and the public health preventive measures.
“As people return to normal activities and the public health measures put in place to stop the spread of COVID are eased, we are likely to see increases in circulation of RSV and return to its circulation during the winter months – typically similar to circulation of flu – from November through March in temperate climates in the northern hemisphere,” she said.
A coauthor of the paper, Harish Nair, PhD, with the Centre for Global Health, Usher Institute, University of Edinburgh, said in a press release that their findings have particular significance as COVID restrictions ease around the globe.
“The majority of the young children born in the last 2 years have never been exposed to RSV (and therefore have no immunity against this virus),” Nair wrote.
Most deaths occurring outside hospitals
A challenge in reducing the deaths in those 5 years old and younger is that most (76%) of deaths are happening in the community outside hospitals.
The authors wrote: “For every RSV-associated acute lower respiratory infection in-hospital death, we estimate approximately three more deaths attributable to RSV in the community.”
The percentage dying outside hospitals is even larger (81%) in low- to middle-income countries.
This work built on a previous review by the team that analyzed 317 studies. They updated their search with 113 new eligible studies and unpublished data from 51 papers published between Jan. 1, 2017, and Dec. 31, 2020.
The authors acknowledged some limitations, including variations in study settings and in definitions for acute lower respiratory infection, healthcare access, and eligibility for RSV testing.
The study was funded by EU Innovative Medicines Initiative Respiratory Syncytial Virus Consortium in Europe. Dr. Li reported grants from Wellcome Trust and the World Health Organization outside the submitted work. Dr. Hartert, Dr. Ortiz, and Dr. Nair disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Respiratory syncytial virus (RSV) caused more than 100,000 deaths in children under age 5 years globally in 2019, according to an analysis published online in The Lancet.
Researchers, led by You Li, PhD, of Nanjing (China) Medical University, found that nearly half of those (more than 45,000) occurred in children younger than 6 months old.
They estimated that RSV causes 1 in 50 deaths among children under 5 years old, and 1 in 28 deaths in children under 6 months old.
Additionally, RSV is responsible for an estimated 3.6 million hospital admissions globally each year, according to the report.
This analysis is the first to sift RSV disease burden into narrow age brackets, the authors said.
The numbers highlight that almost all of the deaths (97%) were in low- and middle-income countries.
Messages for prevention
Tina Hartert, MD, MPH, a professor in the division of allergy, pulmonary, and critical care medicine at Vanderbilt University, Nashville, Tenn., who was not part of the study, wrote in an invited commentary that these findings will be important in RSV prevention.
Among the most notable findings, she wrote, is the heavy mortality in the 0- to 6-month age group, which she notes is “the age group targeted by vaccination during pregnancy and birth-dose immunoprophylaxis.”
Dr. Hartert, who coauthored the commentary with Justin R. Ortiz, MD, MS, with the Center for Vaccine Development and Global Health, University of Maryland, Baltimore, told this news organization, “RSV is a respiratory virus that infects nearly every child by the time they are 2-3 years of age, with severe infection and death most common in the youngest infants. Vaccines that prevent the most severe infections in these young infants will likely be one of the best ways to prevent these severe infections and death.”
Though the authors found most deaths occur in low- and middle-income countries, RSV is one of the most common reasons for infant hospitalization in the US and affects 1% to 3% of infants, half of whom are full-term and otherwise healthy, Dr. Hartert said.
It is also one of the most common causes of infant lower respiratory tract infection in young children in the United States, she said, and it causes the most severe disease at the age extremes, with older adults experiencing significant morbidity with RSV.
Dr. Li said in an interview that although the team did not focus on reporting country-specific estimates in this work, their previous work, resulted in estimates of 98,000-155,000 RSV-related hospitalizations in children under 5 years old in the United States in 2019. Between 65,000 and 86,000 were in infants less than 1 year old.
Currently, he said, the only available RSV prophylaxis is palivizumab (Synagis), which is expensive and given only to high-risk infants in high-income countries, including the United States.
“There have been a number of promising RSV prophylactic products including maternal vaccine and monoclonal antibodies that have the potential for targeting the general infant population – not just high-risk infants – in late-phase clinical trials,” he said. “Our estimates of RSV-related disease burden will help anticipate the impact of future RSV immunization programs.”
Pandemic changed patterns
This research was completed before the COVID-19 pandemic, and it is not yet known how that could affect RSV disease burden long term.
However, Dr. Hartert said, RSV circulation has been significantly changed during the pandemic, both in intensity and timing, likely because of a combination of COVID and the public health preventive measures.
“As people return to normal activities and the public health measures put in place to stop the spread of COVID are eased, we are likely to see increases in circulation of RSV and return to its circulation during the winter months – typically similar to circulation of flu – from November through March in temperate climates in the northern hemisphere,” she said.
A coauthor of the paper, Harish Nair, PhD, with the Centre for Global Health, Usher Institute, University of Edinburgh, said in a press release that their findings have particular significance as COVID restrictions ease around the globe.
“The majority of the young children born in the last 2 years have never been exposed to RSV (and therefore have no immunity against this virus),” Nair wrote.
Most deaths occurring outside hospitals
A challenge in reducing the deaths in those 5 years old and younger is that most (76%) of deaths are happening in the community outside hospitals.
The authors wrote: “For every RSV-associated acute lower respiratory infection in-hospital death, we estimate approximately three more deaths attributable to RSV in the community.”
The percentage dying outside hospitals is even larger (81%) in low- to middle-income countries.
This work built on a previous review by the team that analyzed 317 studies. They updated their search with 113 new eligible studies and unpublished data from 51 papers published between Jan. 1, 2017, and Dec. 31, 2020.
The authors acknowledged some limitations, including variations in study settings and in definitions for acute lower respiratory infection, healthcare access, and eligibility for RSV testing.
The study was funded by EU Innovative Medicines Initiative Respiratory Syncytial Virus Consortium in Europe. Dr. Li reported grants from Wellcome Trust and the World Health Organization outside the submitted work. Dr. Hartert, Dr. Ortiz, and Dr. Nair disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Respiratory syncytial virus (RSV) caused more than 100,000 deaths in children under age 5 years globally in 2019, according to an analysis published online in The Lancet.
Researchers, led by You Li, PhD, of Nanjing (China) Medical University, found that nearly half of those (more than 45,000) occurred in children younger than 6 months old.
They estimated that RSV causes 1 in 50 deaths among children under 5 years old, and 1 in 28 deaths in children under 6 months old.
Additionally, RSV is responsible for an estimated 3.6 million hospital admissions globally each year, according to the report.
This analysis is the first to sift RSV disease burden into narrow age brackets, the authors said.
The numbers highlight that almost all of the deaths (97%) were in low- and middle-income countries.
Messages for prevention
Tina Hartert, MD, MPH, a professor in the division of allergy, pulmonary, and critical care medicine at Vanderbilt University, Nashville, Tenn., who was not part of the study, wrote in an invited commentary that these findings will be important in RSV prevention.
Among the most notable findings, she wrote, is the heavy mortality in the 0- to 6-month age group, which she notes is “the age group targeted by vaccination during pregnancy and birth-dose immunoprophylaxis.”
Dr. Hartert, who coauthored the commentary with Justin R. Ortiz, MD, MS, with the Center for Vaccine Development and Global Health, University of Maryland, Baltimore, told this news organization, “RSV is a respiratory virus that infects nearly every child by the time they are 2-3 years of age, with severe infection and death most common in the youngest infants. Vaccines that prevent the most severe infections in these young infants will likely be one of the best ways to prevent these severe infections and death.”
Though the authors found most deaths occur in low- and middle-income countries, RSV is one of the most common reasons for infant hospitalization in the US and affects 1% to 3% of infants, half of whom are full-term and otherwise healthy, Dr. Hartert said.
It is also one of the most common causes of infant lower respiratory tract infection in young children in the United States, she said, and it causes the most severe disease at the age extremes, with older adults experiencing significant morbidity with RSV.
Dr. Li said in an interview that although the team did not focus on reporting country-specific estimates in this work, their previous work, resulted in estimates of 98,000-155,000 RSV-related hospitalizations in children under 5 years old in the United States in 2019. Between 65,000 and 86,000 were in infants less than 1 year old.
Currently, he said, the only available RSV prophylaxis is palivizumab (Synagis), which is expensive and given only to high-risk infants in high-income countries, including the United States.
“There have been a number of promising RSV prophylactic products including maternal vaccine and monoclonal antibodies that have the potential for targeting the general infant population – not just high-risk infants – in late-phase clinical trials,” he said. “Our estimates of RSV-related disease burden will help anticipate the impact of future RSV immunization programs.”
Pandemic changed patterns
This research was completed before the COVID-19 pandemic, and it is not yet known how that could affect RSV disease burden long term.
However, Dr. Hartert said, RSV circulation has been significantly changed during the pandemic, both in intensity and timing, likely because of a combination of COVID and the public health preventive measures.
“As people return to normal activities and the public health measures put in place to stop the spread of COVID are eased, we are likely to see increases in circulation of RSV and return to its circulation during the winter months – typically similar to circulation of flu – from November through March in temperate climates in the northern hemisphere,” she said.
A coauthor of the paper, Harish Nair, PhD, with the Centre for Global Health, Usher Institute, University of Edinburgh, said in a press release that their findings have particular significance as COVID restrictions ease around the globe.
“The majority of the young children born in the last 2 years have never been exposed to RSV (and therefore have no immunity against this virus),” Nair wrote.
Most deaths occurring outside hospitals
A challenge in reducing the deaths in those 5 years old and younger is that most (76%) of deaths are happening in the community outside hospitals.
The authors wrote: “For every RSV-associated acute lower respiratory infection in-hospital death, we estimate approximately three more deaths attributable to RSV in the community.”
The percentage dying outside hospitals is even larger (81%) in low- to middle-income countries.
This work built on a previous review by the team that analyzed 317 studies. They updated their search with 113 new eligible studies and unpublished data from 51 papers published between Jan. 1, 2017, and Dec. 31, 2020.
The authors acknowledged some limitations, including variations in study settings and in definitions for acute lower respiratory infection, healthcare access, and eligibility for RSV testing.
The study was funded by EU Innovative Medicines Initiative Respiratory Syncytial Virus Consortium in Europe. Dr. Li reported grants from Wellcome Trust and the World Health Organization outside the submitted work. Dr. Hartert, Dr. Ortiz, and Dr. Nair disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Cannabis vaping continues its rise in teens
More teenagers in the United States reported cannabis use with vaping in 2019, compared with 2017, while cannabis use without vaping declined, based on annual survey data from more than 50,000 teens.
“With vaping prevalence rising so quickly among teens, getting a clearer picture of how cannabis use is shifting helps inform prevention and cessation efforts,” corresponding author Noah T. Kreski, MPH, of Columbia University, New York, said in an interview.
“In just 2 years, the most common cannabis use pattern changed from ‘occasional use without vaping’ to ‘frequent use with vaping,’ said Mx. Kreski, who uses the honorific Mx. and the pronouns they/them. “Knowing that, as well as the high overlap of cannabis vaping with nicotine use and binge drinking, adds to the urgency of reducing adolescent vaping.”
To quantify the trends in cannabis vaping, the researchers reviewed data from Monitoring the Future, an annual survey of high school students across the United States. The study population included 51,052 individuals; approximately 49% were male and 49% were non-Hispanic White. The researchers examined frequency of cannabis use, trends across demographic groups, and concurrent use of cannabis and other substances such as alcohol and tobacco. The findings were published in the journal Addiction.
Frequent cannabis use was defined as six or more times in the past 30 days; occasional use was defined as one to five times in the past 30 days.
Frequent cannabis use with vaping increased from 2.1% in 2017 to 5.4% in 2019. Occasional cannabis use with vaping also increased, though less dramatically, from less than 2% in 2017 to approximately 3.5% in 2019.
By contrast, both frequent and occasional cannabis use without vaping declined from 2017 to 2019 (from 3.8% to 2.1% and from 6.9% to 4.4%, respectively).
Overall, the prevalence of any level of cannabis use increased from 13.9% in 2017 to 15.4% in 2019. Both males and females showed a similar increase in reported frequent cannabis use with vaping of approximately 3%.
The results document that vaping cannabis has become more common than smoking alone among U.S. teens across almost all demographic groups, and across sex, race, urbanicity, and level of parent education; however, the increased was especially marked among Hispanic/Latinx teens and those of lower socioeconomic status, the researchers wrote.
The researchers also examined the associations between cannabis use with and without vaping and concurrent nicotine and alcohol use. Overall, the strongest association was between smoking or vaping nicotine and vaping cannabis; teens who smoked or vaped nicotine were 42 times more likely than nonnicotine users to report vaping cannabis in the past 30 days (adjusted odds ratio, 42.28). In addition, more occasions of binge drinking were more strongly associated with cannabis use with vaping (up to 10 times more likely), compared with cannabis use without vaping, (aORs, 4.48-10.09).
The study findings were limited by several factors, including the lack of questions on tetrahydrocannabinol (THC) or cannabidiol content of the cannabis products used, although evidence suggests that the potency of cannabis products in the United States is increasing, the researchers noted. Other limitations included the cross-sectional design, which prevents making associations about causality, and lack of data on the quantity of cannabis used; only data on frequency of use were recorded.
However, the results reflect a rise in cannabis use with vaping among teens in the United States, along with an increased risk of tobacco use, e-cigarette use, and binge drinking, the researchers said.
As cannabis legalization expands across the United States, policies are needed to deter use among adolescents, the researchers wrote. “These policies should be crafted to reduce an emphasis on criminalization in preference for public health promotion given the history of unequal application of punitive consequences of drug use for racialized minorities in the United States. As products, delivery systems, potency, and marketing proliferate within a for-profit industry, increased attention to youth trends, including investment in sustained and evidence-based prevention and intervention, is increasingly necessary.”
The take-home message for clinicians is to ask whether your patients are vaping, because the prevalence is not only up, but fairly universal, Mx. Kreski said. “Have a discussion that covers a broad range of substance use topics and informs teens of the potential risks of vaping, while avoiding stigma.”
The message for parents is “to talk to your kids about the risks of vaping,” said Mx. Kreski. “Prioritize open communication rather than punishment, and work together with your teens to prevent or reduce vaping.” The message for teens: “Understand that vaping has risks. You should feel empowered to talk to your parents or doctor about those risks. While it may seem like everyone’s vaping, the majority don’t. Keeping communication open between parents/caregivers, teens, and health care providers is one of the best ways to address these trends in vaping.”
Beware more powerful cannabis products
“While drug use in general is declining in adolescents, marijuana use remains very common,” Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“There is growing evidence that marijuana is now the first drug used by adolescents – replacing alcohol and nicotine – and frequent use can lead to substance abuse,” said Dr. Curran, who specializes in adolescent medicine but was involved in the study. “Cannabis use patterns have evolved over time. As I frequently tell my patients and their families, new strains and hybrids of marijuana have higher potencies of THC. Many adolescents are eschewing smoking and in its place using marijuana concentrates (wax, oil, shatter) via vape, dab pen, or rig. Use of these methods puts adolescents at high risk of social and health complications such as [e-cigarette or vaping use-associated lung injury], cannabis hyperemesis syndrome, and psychosis – and understanding these patterns and associated drug use helps health care professionals and parents keep adolescents safe.”
The take-home message for clinicians is that marijuana use via vaping continues to rise and to become more common than “traditional” marijuana smoking, Dr. Curran said. “This increase is across genders, in nearly all race/ethnicities (especially in Latinx youth), and in youth from lower socioeconomic status.” Vaping marijuana is associated with other substance abuse, so health care professionals should include questions about different forms of marijuana use, such as vape, dab pen, or rig, when working with patients, and counsel patients and families about the risks associated with use of any of these products.
The study was supported by the National Center for Injury Prevention and Control and by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More teenagers in the United States reported cannabis use with vaping in 2019, compared with 2017, while cannabis use without vaping declined, based on annual survey data from more than 50,000 teens.
“With vaping prevalence rising so quickly among teens, getting a clearer picture of how cannabis use is shifting helps inform prevention and cessation efforts,” corresponding author Noah T. Kreski, MPH, of Columbia University, New York, said in an interview.
“In just 2 years, the most common cannabis use pattern changed from ‘occasional use without vaping’ to ‘frequent use with vaping,’ said Mx. Kreski, who uses the honorific Mx. and the pronouns they/them. “Knowing that, as well as the high overlap of cannabis vaping with nicotine use and binge drinking, adds to the urgency of reducing adolescent vaping.”
To quantify the trends in cannabis vaping, the researchers reviewed data from Monitoring the Future, an annual survey of high school students across the United States. The study population included 51,052 individuals; approximately 49% were male and 49% were non-Hispanic White. The researchers examined frequency of cannabis use, trends across demographic groups, and concurrent use of cannabis and other substances such as alcohol and tobacco. The findings were published in the journal Addiction.
Frequent cannabis use was defined as six or more times in the past 30 days; occasional use was defined as one to five times in the past 30 days.
Frequent cannabis use with vaping increased from 2.1% in 2017 to 5.4% in 2019. Occasional cannabis use with vaping also increased, though less dramatically, from less than 2% in 2017 to approximately 3.5% in 2019.
By contrast, both frequent and occasional cannabis use without vaping declined from 2017 to 2019 (from 3.8% to 2.1% and from 6.9% to 4.4%, respectively).
Overall, the prevalence of any level of cannabis use increased from 13.9% in 2017 to 15.4% in 2019. Both males and females showed a similar increase in reported frequent cannabis use with vaping of approximately 3%.
The results document that vaping cannabis has become more common than smoking alone among U.S. teens across almost all demographic groups, and across sex, race, urbanicity, and level of parent education; however, the increased was especially marked among Hispanic/Latinx teens and those of lower socioeconomic status, the researchers wrote.
The researchers also examined the associations between cannabis use with and without vaping and concurrent nicotine and alcohol use. Overall, the strongest association was between smoking or vaping nicotine and vaping cannabis; teens who smoked or vaped nicotine were 42 times more likely than nonnicotine users to report vaping cannabis in the past 30 days (adjusted odds ratio, 42.28). In addition, more occasions of binge drinking were more strongly associated with cannabis use with vaping (up to 10 times more likely), compared with cannabis use without vaping, (aORs, 4.48-10.09).
The study findings were limited by several factors, including the lack of questions on tetrahydrocannabinol (THC) or cannabidiol content of the cannabis products used, although evidence suggests that the potency of cannabis products in the United States is increasing, the researchers noted. Other limitations included the cross-sectional design, which prevents making associations about causality, and lack of data on the quantity of cannabis used; only data on frequency of use were recorded.
However, the results reflect a rise in cannabis use with vaping among teens in the United States, along with an increased risk of tobacco use, e-cigarette use, and binge drinking, the researchers said.
As cannabis legalization expands across the United States, policies are needed to deter use among adolescents, the researchers wrote. “These policies should be crafted to reduce an emphasis on criminalization in preference for public health promotion given the history of unequal application of punitive consequences of drug use for racialized minorities in the United States. As products, delivery systems, potency, and marketing proliferate within a for-profit industry, increased attention to youth trends, including investment in sustained and evidence-based prevention and intervention, is increasingly necessary.”
The take-home message for clinicians is to ask whether your patients are vaping, because the prevalence is not only up, but fairly universal, Mx. Kreski said. “Have a discussion that covers a broad range of substance use topics and informs teens of the potential risks of vaping, while avoiding stigma.”
The message for parents is “to talk to your kids about the risks of vaping,” said Mx. Kreski. “Prioritize open communication rather than punishment, and work together with your teens to prevent or reduce vaping.” The message for teens: “Understand that vaping has risks. You should feel empowered to talk to your parents or doctor about those risks. While it may seem like everyone’s vaping, the majority don’t. Keeping communication open between parents/caregivers, teens, and health care providers is one of the best ways to address these trends in vaping.”
Beware more powerful cannabis products
“While drug use in general is declining in adolescents, marijuana use remains very common,” Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“There is growing evidence that marijuana is now the first drug used by adolescents – replacing alcohol and nicotine – and frequent use can lead to substance abuse,” said Dr. Curran, who specializes in adolescent medicine but was involved in the study. “Cannabis use patterns have evolved over time. As I frequently tell my patients and their families, new strains and hybrids of marijuana have higher potencies of THC. Many adolescents are eschewing smoking and in its place using marijuana concentrates (wax, oil, shatter) via vape, dab pen, or rig. Use of these methods puts adolescents at high risk of social and health complications such as [e-cigarette or vaping use-associated lung injury], cannabis hyperemesis syndrome, and psychosis – and understanding these patterns and associated drug use helps health care professionals and parents keep adolescents safe.”
The take-home message for clinicians is that marijuana use via vaping continues to rise and to become more common than “traditional” marijuana smoking, Dr. Curran said. “This increase is across genders, in nearly all race/ethnicities (especially in Latinx youth), and in youth from lower socioeconomic status.” Vaping marijuana is associated with other substance abuse, so health care professionals should include questions about different forms of marijuana use, such as vape, dab pen, or rig, when working with patients, and counsel patients and families about the risks associated with use of any of these products.
The study was supported by the National Center for Injury Prevention and Control and by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More teenagers in the United States reported cannabis use with vaping in 2019, compared with 2017, while cannabis use without vaping declined, based on annual survey data from more than 50,000 teens.
“With vaping prevalence rising so quickly among teens, getting a clearer picture of how cannabis use is shifting helps inform prevention and cessation efforts,” corresponding author Noah T. Kreski, MPH, of Columbia University, New York, said in an interview.
“In just 2 years, the most common cannabis use pattern changed from ‘occasional use without vaping’ to ‘frequent use with vaping,’ said Mx. Kreski, who uses the honorific Mx. and the pronouns they/them. “Knowing that, as well as the high overlap of cannabis vaping with nicotine use and binge drinking, adds to the urgency of reducing adolescent vaping.”
To quantify the trends in cannabis vaping, the researchers reviewed data from Monitoring the Future, an annual survey of high school students across the United States. The study population included 51,052 individuals; approximately 49% were male and 49% were non-Hispanic White. The researchers examined frequency of cannabis use, trends across demographic groups, and concurrent use of cannabis and other substances such as alcohol and tobacco. The findings were published in the journal Addiction.
Frequent cannabis use was defined as six or more times in the past 30 days; occasional use was defined as one to five times in the past 30 days.
Frequent cannabis use with vaping increased from 2.1% in 2017 to 5.4% in 2019. Occasional cannabis use with vaping also increased, though less dramatically, from less than 2% in 2017 to approximately 3.5% in 2019.
By contrast, both frequent and occasional cannabis use without vaping declined from 2017 to 2019 (from 3.8% to 2.1% and from 6.9% to 4.4%, respectively).
Overall, the prevalence of any level of cannabis use increased from 13.9% in 2017 to 15.4% in 2019. Both males and females showed a similar increase in reported frequent cannabis use with vaping of approximately 3%.
The results document that vaping cannabis has become more common than smoking alone among U.S. teens across almost all demographic groups, and across sex, race, urbanicity, and level of parent education; however, the increased was especially marked among Hispanic/Latinx teens and those of lower socioeconomic status, the researchers wrote.
The researchers also examined the associations between cannabis use with and without vaping and concurrent nicotine and alcohol use. Overall, the strongest association was between smoking or vaping nicotine and vaping cannabis; teens who smoked or vaped nicotine were 42 times more likely than nonnicotine users to report vaping cannabis in the past 30 days (adjusted odds ratio, 42.28). In addition, more occasions of binge drinking were more strongly associated with cannabis use with vaping (up to 10 times more likely), compared with cannabis use without vaping, (aORs, 4.48-10.09).
The study findings were limited by several factors, including the lack of questions on tetrahydrocannabinol (THC) or cannabidiol content of the cannabis products used, although evidence suggests that the potency of cannabis products in the United States is increasing, the researchers noted. Other limitations included the cross-sectional design, which prevents making associations about causality, and lack of data on the quantity of cannabis used; only data on frequency of use were recorded.
However, the results reflect a rise in cannabis use with vaping among teens in the United States, along with an increased risk of tobacco use, e-cigarette use, and binge drinking, the researchers said.
As cannabis legalization expands across the United States, policies are needed to deter use among adolescents, the researchers wrote. “These policies should be crafted to reduce an emphasis on criminalization in preference for public health promotion given the history of unequal application of punitive consequences of drug use for racialized minorities in the United States. As products, delivery systems, potency, and marketing proliferate within a for-profit industry, increased attention to youth trends, including investment in sustained and evidence-based prevention and intervention, is increasingly necessary.”
The take-home message for clinicians is to ask whether your patients are vaping, because the prevalence is not only up, but fairly universal, Mx. Kreski said. “Have a discussion that covers a broad range of substance use topics and informs teens of the potential risks of vaping, while avoiding stigma.”
The message for parents is “to talk to your kids about the risks of vaping,” said Mx. Kreski. “Prioritize open communication rather than punishment, and work together with your teens to prevent or reduce vaping.” The message for teens: “Understand that vaping has risks. You should feel empowered to talk to your parents or doctor about those risks. While it may seem like everyone’s vaping, the majority don’t. Keeping communication open between parents/caregivers, teens, and health care providers is one of the best ways to address these trends in vaping.”
Beware more powerful cannabis products
“While drug use in general is declining in adolescents, marijuana use remains very common,” Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“There is growing evidence that marijuana is now the first drug used by adolescents – replacing alcohol and nicotine – and frequent use can lead to substance abuse,” said Dr. Curran, who specializes in adolescent medicine but was involved in the study. “Cannabis use patterns have evolved over time. As I frequently tell my patients and their families, new strains and hybrids of marijuana have higher potencies of THC. Many adolescents are eschewing smoking and in its place using marijuana concentrates (wax, oil, shatter) via vape, dab pen, or rig. Use of these methods puts adolescents at high risk of social and health complications such as [e-cigarette or vaping use-associated lung injury], cannabis hyperemesis syndrome, and psychosis – and understanding these patterns and associated drug use helps health care professionals and parents keep adolescents safe.”
The take-home message for clinicians is that marijuana use via vaping continues to rise and to become more common than “traditional” marijuana smoking, Dr. Curran said. “This increase is across genders, in nearly all race/ethnicities (especially in Latinx youth), and in youth from lower socioeconomic status.” Vaping marijuana is associated with other substance abuse, so health care professionals should include questions about different forms of marijuana use, such as vape, dab pen, or rig, when working with patients, and counsel patients and families about the risks associated with use of any of these products.
The study was supported by the National Center for Injury Prevention and Control and by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM ADDICTION
The baby formula shortage continues
Meghan Block of Weymouth, Mass., starts her search at 5 a.m. every morning – combing local retailer websites for baby formula.
Her own children have been off it for years. But her cousin in New Hampshire has a 2-month-old son who needs hypoallergenic formula, and the nationwide shortage has left the new mom scrambling to find what her baby needs.
“I’d equate this to how we were all frantically looking for vaccine appointments when they first rolled out,” Ms. Block said. “Parents are all mobilizing for each other.”
She added, “What people aren’t talking about is the stress on new mothers this is causing. If you’re on the edge of the baby blues and postpartum depression, and you can’t find food for your babies – these parents could be in crisis.”
For weeks, a pandemic-induced supply chain shortage – along with a massive recall from top formula manufacturer Abbott Nutrition – has left shelves empty and parents panicked, fearing their dwindling formula supplies will disappear entirely.
Abbott announced that its previously shuttered Michigan factory would reopen, but it remains unclear how soon that will make a noticeable difference.
The Food and Drug Administration announced Monday, May 16, that it would ease restrictions for selling foreign-made baby formula in the U.S. to broaden supply.
President Joe Biden invoked the the Defense Production Act on May 18, which requires suppliers to send resources to formula plants before giving them to other customers. The president is also authorizing the Defense Department to use commercial aircraft to pick up infant formula overseas that meets federal standards and fly it to the U.S. – a measure dubbed “Operation Fly Formula.”
But in the meantime, hospital staff and pediatricians are fielding questions from parents that they can’t always answer.
“People want to know if the shortage is ending soon, and that’s hard to predict. Even with the factory back online, the end could still be 1-3 months away,” Joshua Wechsler, MD, pediatric gastroenterologist at Ann & Robert H. Lurie Children’s Hospital of Chicago, said in an interview.
Most formulas on the market have comparable alternatives, Dr. Wechsler said, but there are fewer options for parents of special-needs babies – those with allergies and specific dietary requirements.
This has required around-the-clock work from dietitians and pediatricians to find sufficient options for these babies and monitor their ability to tolerate new kinds of formula.
“We’re advising parents not to dilute formula, not to buy it from sources you’re unfamiliar with, and no homemade formulas,” Dr. Wechsler said.
He said in some instances he has seen weight loss among babies whose supplies were stretching thin, and in very rare cases, hospitalizations.
According to recent reports, two children were hospitalized in mid-May at Le Bonheur Children’s Hospital, Memphis, Tenn., as a result of the formula shortage.
Those most affected by the crisis, doctors say, are lower-income families. Half of the infant formula purchased in the United States is through Women, Infants, and Children (WIC) benefits, a federal assistance program, which provides formula for free but only limited types and brands.
But in most cases, hospitals and pediatricians have the means to provide caregivers with supplementary formula, said Amy Hair, MD, program director of neonatal nutrition at Texas Children’s Hospital.
“Here in the hospital, we’re OK, because we’re able to switch through different options for patients and we’re sending families home with a short supply to bridge them over,” Dr. Hair said. “We encourage patients to talk to their pediatricians, who usually have in-office supplies.”
She also advises parents to look in smaller pharmacies and stores rather than bigger retailers, along with ordering it straight from the formula manufacturers online.
“We’re reassuring families we think this is temporary,” Dr. Hair said. “Providers have been dealing with this for a while, so we have some strategies in place to help caregivers through the shortage.”
In the meantime, parents continue to lean on each other for help and resources. Ms. Block’s cousin in New Hampshire, Jamie Boudreau, said she has friends and family on the lookout across the country for hypoallergenic formula for her son.
She currently has about a 1-month supply, but she worries constantly that will be depleted before the shortage ends.
“It’s definitely been very stressful,” Ms. Boudreau said. “I, as an adult, can go days without eating, but my tiny 2-month-old little boy – he can’t go more than 3 hours. What am I going to do if in 4 weeks I don’t have any more?”
Meghan Block of Weymouth, Mass., starts her search at 5 a.m. every morning – combing local retailer websites for baby formula.
Her own children have been off it for years. But her cousin in New Hampshire has a 2-month-old son who needs hypoallergenic formula, and the nationwide shortage has left the new mom scrambling to find what her baby needs.
“I’d equate this to how we were all frantically looking for vaccine appointments when they first rolled out,” Ms. Block said. “Parents are all mobilizing for each other.”
She added, “What people aren’t talking about is the stress on new mothers this is causing. If you’re on the edge of the baby blues and postpartum depression, and you can’t find food for your babies – these parents could be in crisis.”
For weeks, a pandemic-induced supply chain shortage – along with a massive recall from top formula manufacturer Abbott Nutrition – has left shelves empty and parents panicked, fearing their dwindling formula supplies will disappear entirely.
Abbott announced that its previously shuttered Michigan factory would reopen, but it remains unclear how soon that will make a noticeable difference.
The Food and Drug Administration announced Monday, May 16, that it would ease restrictions for selling foreign-made baby formula in the U.S. to broaden supply.
President Joe Biden invoked the the Defense Production Act on May 18, which requires suppliers to send resources to formula plants before giving them to other customers. The president is also authorizing the Defense Department to use commercial aircraft to pick up infant formula overseas that meets federal standards and fly it to the U.S. – a measure dubbed “Operation Fly Formula.”
But in the meantime, hospital staff and pediatricians are fielding questions from parents that they can’t always answer.
“People want to know if the shortage is ending soon, and that’s hard to predict. Even with the factory back online, the end could still be 1-3 months away,” Joshua Wechsler, MD, pediatric gastroenterologist at Ann & Robert H. Lurie Children’s Hospital of Chicago, said in an interview.
Most formulas on the market have comparable alternatives, Dr. Wechsler said, but there are fewer options for parents of special-needs babies – those with allergies and specific dietary requirements.
This has required around-the-clock work from dietitians and pediatricians to find sufficient options for these babies and monitor their ability to tolerate new kinds of formula.
“We’re advising parents not to dilute formula, not to buy it from sources you’re unfamiliar with, and no homemade formulas,” Dr. Wechsler said.
He said in some instances he has seen weight loss among babies whose supplies were stretching thin, and in very rare cases, hospitalizations.
According to recent reports, two children were hospitalized in mid-May at Le Bonheur Children’s Hospital, Memphis, Tenn., as a result of the formula shortage.
Those most affected by the crisis, doctors say, are lower-income families. Half of the infant formula purchased in the United States is through Women, Infants, and Children (WIC) benefits, a federal assistance program, which provides formula for free but only limited types and brands.
But in most cases, hospitals and pediatricians have the means to provide caregivers with supplementary formula, said Amy Hair, MD, program director of neonatal nutrition at Texas Children’s Hospital.
“Here in the hospital, we’re OK, because we’re able to switch through different options for patients and we’re sending families home with a short supply to bridge them over,” Dr. Hair said. “We encourage patients to talk to their pediatricians, who usually have in-office supplies.”
She also advises parents to look in smaller pharmacies and stores rather than bigger retailers, along with ordering it straight from the formula manufacturers online.
“We’re reassuring families we think this is temporary,” Dr. Hair said. “Providers have been dealing with this for a while, so we have some strategies in place to help caregivers through the shortage.”
In the meantime, parents continue to lean on each other for help and resources. Ms. Block’s cousin in New Hampshire, Jamie Boudreau, said she has friends and family on the lookout across the country for hypoallergenic formula for her son.
She currently has about a 1-month supply, but she worries constantly that will be depleted before the shortage ends.
“It’s definitely been very stressful,” Ms. Boudreau said. “I, as an adult, can go days without eating, but my tiny 2-month-old little boy – he can’t go more than 3 hours. What am I going to do if in 4 weeks I don’t have any more?”
Meghan Block of Weymouth, Mass., starts her search at 5 a.m. every morning – combing local retailer websites for baby formula.
Her own children have been off it for years. But her cousin in New Hampshire has a 2-month-old son who needs hypoallergenic formula, and the nationwide shortage has left the new mom scrambling to find what her baby needs.
“I’d equate this to how we were all frantically looking for vaccine appointments when they first rolled out,” Ms. Block said. “Parents are all mobilizing for each other.”
She added, “What people aren’t talking about is the stress on new mothers this is causing. If you’re on the edge of the baby blues and postpartum depression, and you can’t find food for your babies – these parents could be in crisis.”
For weeks, a pandemic-induced supply chain shortage – along with a massive recall from top formula manufacturer Abbott Nutrition – has left shelves empty and parents panicked, fearing their dwindling formula supplies will disappear entirely.
Abbott announced that its previously shuttered Michigan factory would reopen, but it remains unclear how soon that will make a noticeable difference.
The Food and Drug Administration announced Monday, May 16, that it would ease restrictions for selling foreign-made baby formula in the U.S. to broaden supply.
President Joe Biden invoked the the Defense Production Act on May 18, which requires suppliers to send resources to formula plants before giving them to other customers. The president is also authorizing the Defense Department to use commercial aircraft to pick up infant formula overseas that meets federal standards and fly it to the U.S. – a measure dubbed “Operation Fly Formula.”
But in the meantime, hospital staff and pediatricians are fielding questions from parents that they can’t always answer.
“People want to know if the shortage is ending soon, and that’s hard to predict. Even with the factory back online, the end could still be 1-3 months away,” Joshua Wechsler, MD, pediatric gastroenterologist at Ann & Robert H. Lurie Children’s Hospital of Chicago, said in an interview.
Most formulas on the market have comparable alternatives, Dr. Wechsler said, but there are fewer options for parents of special-needs babies – those with allergies and specific dietary requirements.
This has required around-the-clock work from dietitians and pediatricians to find sufficient options for these babies and monitor their ability to tolerate new kinds of formula.
“We’re advising parents not to dilute formula, not to buy it from sources you’re unfamiliar with, and no homemade formulas,” Dr. Wechsler said.
He said in some instances he has seen weight loss among babies whose supplies were stretching thin, and in very rare cases, hospitalizations.
According to recent reports, two children were hospitalized in mid-May at Le Bonheur Children’s Hospital, Memphis, Tenn., as a result of the formula shortage.
Those most affected by the crisis, doctors say, are lower-income families. Half of the infant formula purchased in the United States is through Women, Infants, and Children (WIC) benefits, a federal assistance program, which provides formula for free but only limited types and brands.
But in most cases, hospitals and pediatricians have the means to provide caregivers with supplementary formula, said Amy Hair, MD, program director of neonatal nutrition at Texas Children’s Hospital.
“Here in the hospital, we’re OK, because we’re able to switch through different options for patients and we’re sending families home with a short supply to bridge them over,” Dr. Hair said. “We encourage patients to talk to their pediatricians, who usually have in-office supplies.”
She also advises parents to look in smaller pharmacies and stores rather than bigger retailers, along with ordering it straight from the formula manufacturers online.
“We’re reassuring families we think this is temporary,” Dr. Hair said. “Providers have been dealing with this for a while, so we have some strategies in place to help caregivers through the shortage.”
In the meantime, parents continue to lean on each other for help and resources. Ms. Block’s cousin in New Hampshire, Jamie Boudreau, said she has friends and family on the lookout across the country for hypoallergenic formula for her son.
She currently has about a 1-month supply, but she worries constantly that will be depleted before the shortage ends.
“It’s definitely been very stressful,” Ms. Boudreau said. “I, as an adult, can go days without eating, but my tiny 2-month-old little boy – he can’t go more than 3 hours. What am I going to do if in 4 weeks I don’t have any more?”
Poorest children at higher risk for PICU admissions, death
SAN FRANCISCO – Children who live in neighborhoods that are at the bottom of the socioeconomic ladder are at significantly greater risk for being admitted to a pediatric intensive care unit (PICU) and of dying there, a study of Medicaid data showed.
Among more than 4 million children and adolescents in 12 U.S. states, those in the most socioeconomically deprived quartile had a significantly higher risk for PICU admission and in-hospital death, compared with patients from the least-deprived areas.
Black children were also at significantly higher risk for death than children of other races, reported Hannah K. Mitchell, BMBS, MSc, from Evelina Children’s Hospital, London.“I think we need to do better work for trying to understand the mechanisms behind these disparities, ... whether they can be intervened over in a hospital setting, and to try to identify targeted interventions,” she said during a presentation at the American Thoracic Society International Conference 2022.
Medicaid data
During her residency in pediatrics at Children’s Hospital of Philadelphia, Ms. Mitchell and colleagues conducted a study to determine whether there were disparities in PICU admissions and mortality according to socioeconomic deprivation in specific neighborhoods.
They created a retrospective cohort study of Medicaid patients from birth to age 20 who were covered from 2007 through 2014 in 12 U.S. states, using ZIP codes to identify areas of social deprivation.
They restricted the analysis to children from households with annual incomes below 150% of the federal poverty line and divided the cohort into socioeconomic quartiles.
A total of nearly 4.1 million children and adolescents were included in the sample. Of this group, 274,782 were admitted to a PICU during the study period.
The median age of children admitted to a PICU was 4 years (interquartile range 0-15), and slightly more than two-thirds (68.5%) had a chronic complex condition.
In all, 43.5% were identified as White, and 32.1% were identified as Black. Ms. Mitchell noted that one of the limitations of the study was missing data on patients of Hispanic/Latinx origin.
The mortality rate among all patients admitted to a PICU was 2.5%.
In univariate logistic regression analysis, the odds ratio for PICU admission among children living in the most impoverished circumstances was 1.21 (P < .0001).
Among all patients admitted to a PICU, the OR for death for children in the most deprived quartile, compared with the least deprived was 1.12 (P = .0047).
In addition, Black children were significantly more likely than White children to be admitted to a PICU (OR, 1.14; P < .0001) and to die in hospital (OR, 1.18, P < .0001).
Ms. Mitchell said that clinicians need to move beyond describing disparities and should instead begin to focus on interventions to eliminate or reduce them.
She noted that children in poor neighborhoods may be more likely to receive care in lower-quality hospitals or may be treated differently from other children when hospitalized because of their socioeconomic status.
Poor housing, environmental injustice
A pediatric pulmonary specialist who works in a safety net hospital told this news organization that there are multiple factors that contribute to increased risk for PICU admissions and mortality in disadvantaged neighborhoods.
“The overwhelming majority of our patients are not only of low socioeconomic status on an individual level but also live in areas of great socioeconomic deprivation, and all of those social determinants of health are resulting in increased admissions to the PICU,” said Robyn T. Cohen, MD, associate professor of pediatrics at Boston University Medical Center.
“They’re living in poor housing conditions with environmental pollution and experiencing competing priorities that prevent early access to care or the ability to obtain medications. We should be doing better to prevent that from happening” said Dr. Cohen, who co-moderated the session but was not involved with the study.
The study was supported by a grant from the National Institutes of Health. Ms. Mitchell and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – Children who live in neighborhoods that are at the bottom of the socioeconomic ladder are at significantly greater risk for being admitted to a pediatric intensive care unit (PICU) and of dying there, a study of Medicaid data showed.
Among more than 4 million children and adolescents in 12 U.S. states, those in the most socioeconomically deprived quartile had a significantly higher risk for PICU admission and in-hospital death, compared with patients from the least-deprived areas.
Black children were also at significantly higher risk for death than children of other races, reported Hannah K. Mitchell, BMBS, MSc, from Evelina Children’s Hospital, London.“I think we need to do better work for trying to understand the mechanisms behind these disparities, ... whether they can be intervened over in a hospital setting, and to try to identify targeted interventions,” she said during a presentation at the American Thoracic Society International Conference 2022.
Medicaid data
During her residency in pediatrics at Children’s Hospital of Philadelphia, Ms. Mitchell and colleagues conducted a study to determine whether there were disparities in PICU admissions and mortality according to socioeconomic deprivation in specific neighborhoods.
They created a retrospective cohort study of Medicaid patients from birth to age 20 who were covered from 2007 through 2014 in 12 U.S. states, using ZIP codes to identify areas of social deprivation.
They restricted the analysis to children from households with annual incomes below 150% of the federal poverty line and divided the cohort into socioeconomic quartiles.
A total of nearly 4.1 million children and adolescents were included in the sample. Of this group, 274,782 were admitted to a PICU during the study period.
The median age of children admitted to a PICU was 4 years (interquartile range 0-15), and slightly more than two-thirds (68.5%) had a chronic complex condition.
In all, 43.5% were identified as White, and 32.1% were identified as Black. Ms. Mitchell noted that one of the limitations of the study was missing data on patients of Hispanic/Latinx origin.
The mortality rate among all patients admitted to a PICU was 2.5%.
In univariate logistic regression analysis, the odds ratio for PICU admission among children living in the most impoverished circumstances was 1.21 (P < .0001).
Among all patients admitted to a PICU, the OR for death for children in the most deprived quartile, compared with the least deprived was 1.12 (P = .0047).
In addition, Black children were significantly more likely than White children to be admitted to a PICU (OR, 1.14; P < .0001) and to die in hospital (OR, 1.18, P < .0001).
Ms. Mitchell said that clinicians need to move beyond describing disparities and should instead begin to focus on interventions to eliminate or reduce them.
She noted that children in poor neighborhoods may be more likely to receive care in lower-quality hospitals or may be treated differently from other children when hospitalized because of their socioeconomic status.
Poor housing, environmental injustice
A pediatric pulmonary specialist who works in a safety net hospital told this news organization that there are multiple factors that contribute to increased risk for PICU admissions and mortality in disadvantaged neighborhoods.
“The overwhelming majority of our patients are not only of low socioeconomic status on an individual level but also live in areas of great socioeconomic deprivation, and all of those social determinants of health are resulting in increased admissions to the PICU,” said Robyn T. Cohen, MD, associate professor of pediatrics at Boston University Medical Center.
“They’re living in poor housing conditions with environmental pollution and experiencing competing priorities that prevent early access to care or the ability to obtain medications. We should be doing better to prevent that from happening” said Dr. Cohen, who co-moderated the session but was not involved with the study.
The study was supported by a grant from the National Institutes of Health. Ms. Mitchell and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – Children who live in neighborhoods that are at the bottom of the socioeconomic ladder are at significantly greater risk for being admitted to a pediatric intensive care unit (PICU) and of dying there, a study of Medicaid data showed.
Among more than 4 million children and adolescents in 12 U.S. states, those in the most socioeconomically deprived quartile had a significantly higher risk for PICU admission and in-hospital death, compared with patients from the least-deprived areas.
Black children were also at significantly higher risk for death than children of other races, reported Hannah K. Mitchell, BMBS, MSc, from Evelina Children’s Hospital, London.“I think we need to do better work for trying to understand the mechanisms behind these disparities, ... whether they can be intervened over in a hospital setting, and to try to identify targeted interventions,” she said during a presentation at the American Thoracic Society International Conference 2022.
Medicaid data
During her residency in pediatrics at Children’s Hospital of Philadelphia, Ms. Mitchell and colleagues conducted a study to determine whether there were disparities in PICU admissions and mortality according to socioeconomic deprivation in specific neighborhoods.
They created a retrospective cohort study of Medicaid patients from birth to age 20 who were covered from 2007 through 2014 in 12 U.S. states, using ZIP codes to identify areas of social deprivation.
They restricted the analysis to children from households with annual incomes below 150% of the federal poverty line and divided the cohort into socioeconomic quartiles.
A total of nearly 4.1 million children and adolescents were included in the sample. Of this group, 274,782 were admitted to a PICU during the study period.
The median age of children admitted to a PICU was 4 years (interquartile range 0-15), and slightly more than two-thirds (68.5%) had a chronic complex condition.
In all, 43.5% were identified as White, and 32.1% were identified as Black. Ms. Mitchell noted that one of the limitations of the study was missing data on patients of Hispanic/Latinx origin.
The mortality rate among all patients admitted to a PICU was 2.5%.
In univariate logistic regression analysis, the odds ratio for PICU admission among children living in the most impoverished circumstances was 1.21 (P < .0001).
Among all patients admitted to a PICU, the OR for death for children in the most deprived quartile, compared with the least deprived was 1.12 (P = .0047).
In addition, Black children were significantly more likely than White children to be admitted to a PICU (OR, 1.14; P < .0001) and to die in hospital (OR, 1.18, P < .0001).
Ms. Mitchell said that clinicians need to move beyond describing disparities and should instead begin to focus on interventions to eliminate or reduce them.
She noted that children in poor neighborhoods may be more likely to receive care in lower-quality hospitals or may be treated differently from other children when hospitalized because of their socioeconomic status.
Poor housing, environmental injustice
A pediatric pulmonary specialist who works in a safety net hospital told this news organization that there are multiple factors that contribute to increased risk for PICU admissions and mortality in disadvantaged neighborhoods.
“The overwhelming majority of our patients are not only of low socioeconomic status on an individual level but also live in areas of great socioeconomic deprivation, and all of those social determinants of health are resulting in increased admissions to the PICU,” said Robyn T. Cohen, MD, associate professor of pediatrics at Boston University Medical Center.
“They’re living in poor housing conditions with environmental pollution and experiencing competing priorities that prevent early access to care or the ability to obtain medications. We should be doing better to prevent that from happening” said Dr. Cohen, who co-moderated the session but was not involved with the study.
The study was supported by a grant from the National Institutes of Health. Ms. Mitchell and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.




