User login
Fewer than half of preschool care programs meet activity guidelines
Only 43% of early child care programs in the United States met guidelines for both sufficient opportunities outdoors and 60-90 minutes of physical activity daily, according to researchers.
To date, no national study has examined these factors, according to Maria H. Boyle, MS, RD, with Abt Associates in Cambridge, Mass., and colleagues. They conducted the study published online in Pediatrics.
The results came “even employing a relatively lenient interpretation of the guidance,” the authors noted, and have particular significance because about 60% of preschool children in the United States are enrolled in center-based care.
Nearly three-fourths of the programs (74%) met the outdoor-opportunities guideline, but only 50% met the physical activity guideline.
Caring for Our Children (CFOC) guidance from the American Academy of Pediatrics recommends at least two outdoor physical activity opportunities (weather permitting) and at least 60-90 minutes allotted for moderate and vigorous physical activities each day during care for children aged 1-6 years.
Still, “children are frequently observed to be sedentary or inactive when in child care settings,” the authors wrote.
They found that some of the main barriers included weather and staff not joining outdoor play.
The researchers used the Study of Nutrition and Activity in Child Care Settings (SNACS), which assesses opportunities for physical activity opportunities and sedentary occasions for children aged 1-5 years at programs participating in the U.S. Department of Agriculture Child and Adult Care Food Program.
Their sample included 227 classrooms: 96 in child care centers and 131 in Head Start programs.
On 1 day (from February to July 2017) an observer in each sampled classroom recorded whether there were designated outdoor and indoor spaces for physical activity, whether that was a playground or other outdoor play space, such as a field, grassy area, or other open area, or parking lot used for play.
They looked for a separate indoor room or gym for active play and how many minutes the class spent in these spaces, and whether there were physical activity facilitators. They made note of barriers, including weather that was too hot or too cold or involved precipitation.
The data show that while almost all programs observed (97%) had dedicated outdoor play space, only 34% had a separate dedicated indoor play space – a gym, for example, or another room separate from main classrooms.
“Of those without a separate indoor play space, virtually all (99.8%) indicated a classroom was available for indoor play.”
Weather and staff not participating in play are barriers
After adjustment for program characteristics, weather barriers resulted in an average 74 fewer minutes daily allotted to physical activity (P < .001).
Another large barrier was staff not participating in play. That was associated with 31 fewer minutes per day allotted for physical activity (P < .001).
“Given the critical role of child care staff as gatekeepers in allowing and encouraging physical activity, it is as important to measure sedentary time when children are not permitted to be active as to measure time when they have opportunity to be active,” the authors wrote. “Best practice guidelines emphasize limiting time children are expected to stay seated during care.”
William Roberts, MD, professor in the department of family medicine and community health at the University of Minnesota in Minneapolis, said in an interview that the findings in this paper help quantify a public health concern as inactivity early sets a harmful precedent.
“Inactive kids too often become inactive adults subject to the long list of noncommunicable chronic diseases associated with lack of regular exercise,” he said.
Lack of movement in childhood, in a program setting or at home, contributes to the obesity epidemic, he pointed out.
“They also do not develop the motor and social skills associated with free play and physical activity,” he said.
He said the findings in this study can guide questions when choosing a child care program. He noted that parents should ask: “What are the opportunities for free play and physical activity?”
The authors and Dr. Roberts declared no relevant financial relationships.
Only 43% of early child care programs in the United States met guidelines for both sufficient opportunities outdoors and 60-90 minutes of physical activity daily, according to researchers.
To date, no national study has examined these factors, according to Maria H. Boyle, MS, RD, with Abt Associates in Cambridge, Mass., and colleagues. They conducted the study published online in Pediatrics.
The results came “even employing a relatively lenient interpretation of the guidance,” the authors noted, and have particular significance because about 60% of preschool children in the United States are enrolled in center-based care.
Nearly three-fourths of the programs (74%) met the outdoor-opportunities guideline, but only 50% met the physical activity guideline.
Caring for Our Children (CFOC) guidance from the American Academy of Pediatrics recommends at least two outdoor physical activity opportunities (weather permitting) and at least 60-90 minutes allotted for moderate and vigorous physical activities each day during care for children aged 1-6 years.
Still, “children are frequently observed to be sedentary or inactive when in child care settings,” the authors wrote.
They found that some of the main barriers included weather and staff not joining outdoor play.
The researchers used the Study of Nutrition and Activity in Child Care Settings (SNACS), which assesses opportunities for physical activity opportunities and sedentary occasions for children aged 1-5 years at programs participating in the U.S. Department of Agriculture Child and Adult Care Food Program.
Their sample included 227 classrooms: 96 in child care centers and 131 in Head Start programs.
On 1 day (from February to July 2017) an observer in each sampled classroom recorded whether there were designated outdoor and indoor spaces for physical activity, whether that was a playground or other outdoor play space, such as a field, grassy area, or other open area, or parking lot used for play.
They looked for a separate indoor room or gym for active play and how many minutes the class spent in these spaces, and whether there were physical activity facilitators. They made note of barriers, including weather that was too hot or too cold or involved precipitation.
The data show that while almost all programs observed (97%) had dedicated outdoor play space, only 34% had a separate dedicated indoor play space – a gym, for example, or another room separate from main classrooms.
“Of those without a separate indoor play space, virtually all (99.8%) indicated a classroom was available for indoor play.”
Weather and staff not participating in play are barriers
After adjustment for program characteristics, weather barriers resulted in an average 74 fewer minutes daily allotted to physical activity (P < .001).
Another large barrier was staff not participating in play. That was associated with 31 fewer minutes per day allotted for physical activity (P < .001).
“Given the critical role of child care staff as gatekeepers in allowing and encouraging physical activity, it is as important to measure sedentary time when children are not permitted to be active as to measure time when they have opportunity to be active,” the authors wrote. “Best practice guidelines emphasize limiting time children are expected to stay seated during care.”
William Roberts, MD, professor in the department of family medicine and community health at the University of Minnesota in Minneapolis, said in an interview that the findings in this paper help quantify a public health concern as inactivity early sets a harmful precedent.
“Inactive kids too often become inactive adults subject to the long list of noncommunicable chronic diseases associated with lack of regular exercise,” he said.
Lack of movement in childhood, in a program setting or at home, contributes to the obesity epidemic, he pointed out.
“They also do not develop the motor and social skills associated with free play and physical activity,” he said.
He said the findings in this study can guide questions when choosing a child care program. He noted that parents should ask: “What are the opportunities for free play and physical activity?”
The authors and Dr. Roberts declared no relevant financial relationships.
Only 43% of early child care programs in the United States met guidelines for both sufficient opportunities outdoors and 60-90 minutes of physical activity daily, according to researchers.
To date, no national study has examined these factors, according to Maria H. Boyle, MS, RD, with Abt Associates in Cambridge, Mass., and colleagues. They conducted the study published online in Pediatrics.
The results came “even employing a relatively lenient interpretation of the guidance,” the authors noted, and have particular significance because about 60% of preschool children in the United States are enrolled in center-based care.
Nearly three-fourths of the programs (74%) met the outdoor-opportunities guideline, but only 50% met the physical activity guideline.
Caring for Our Children (CFOC) guidance from the American Academy of Pediatrics recommends at least two outdoor physical activity opportunities (weather permitting) and at least 60-90 minutes allotted for moderate and vigorous physical activities each day during care for children aged 1-6 years.
Still, “children are frequently observed to be sedentary or inactive when in child care settings,” the authors wrote.
They found that some of the main barriers included weather and staff not joining outdoor play.
The researchers used the Study of Nutrition and Activity in Child Care Settings (SNACS), which assesses opportunities for physical activity opportunities and sedentary occasions for children aged 1-5 years at programs participating in the U.S. Department of Agriculture Child and Adult Care Food Program.
Their sample included 227 classrooms: 96 in child care centers and 131 in Head Start programs.
On 1 day (from February to July 2017) an observer in each sampled classroom recorded whether there were designated outdoor and indoor spaces for physical activity, whether that was a playground or other outdoor play space, such as a field, grassy area, or other open area, or parking lot used for play.
They looked for a separate indoor room or gym for active play and how many minutes the class spent in these spaces, and whether there were physical activity facilitators. They made note of barriers, including weather that was too hot or too cold or involved precipitation.
The data show that while almost all programs observed (97%) had dedicated outdoor play space, only 34% had a separate dedicated indoor play space – a gym, for example, or another room separate from main classrooms.
“Of those without a separate indoor play space, virtually all (99.8%) indicated a classroom was available for indoor play.”
Weather and staff not participating in play are barriers
After adjustment for program characteristics, weather barriers resulted in an average 74 fewer minutes daily allotted to physical activity (P < .001).
Another large barrier was staff not participating in play. That was associated with 31 fewer minutes per day allotted for physical activity (P < .001).
“Given the critical role of child care staff as gatekeepers in allowing and encouraging physical activity, it is as important to measure sedentary time when children are not permitted to be active as to measure time when they have opportunity to be active,” the authors wrote. “Best practice guidelines emphasize limiting time children are expected to stay seated during care.”
William Roberts, MD, professor in the department of family medicine and community health at the University of Minnesota in Minneapolis, said in an interview that the findings in this paper help quantify a public health concern as inactivity early sets a harmful precedent.
“Inactive kids too often become inactive adults subject to the long list of noncommunicable chronic diseases associated with lack of regular exercise,” he said.
Lack of movement in childhood, in a program setting or at home, contributes to the obesity epidemic, he pointed out.
“They also do not develop the motor and social skills associated with free play and physical activity,” he said.
He said the findings in this study can guide questions when choosing a child care program. He noted that parents should ask: “What are the opportunities for free play and physical activity?”
The authors and Dr. Roberts declared no relevant financial relationships.
FROM PEDIATRICS
Children and COVID: New cases up by 50%
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
New law bans infant sleep products linked to 200 deaths
A new law will ban certain infant sleep products blamed for the deaths of more than 200 babies in the United States.
On May 16, President Joe Biden signed legislation that prohibits the manufacture and sale of crib bumpers or inclined sleepers for infants, due to the risk of suffocation, according to CBS News.
H.R. 3182, or the Safe Sleep for Babies Act of 2021, notes that sleepers and bumpers will be considered “banned hazardous products” under the Consumer Product Safety Act. It gives manufacturers and retailers 180 days to comply with the new rule.
“The dangers posed to babies have been apparent for years,” Teresa Murray, who directs the consumer watchdog office for the U.S. PIRG Education Fund, said in a statement.
“It’s unfortunate that this law could take months to take effect,” she said. “Parents and caregivers need to recognize the dangers of these products and get them out of their homes now.”
H.R. 3182 defines inclined sleepers as products that have a sleep surface slanted greater than 10 degrees and are intended for babies up to 1 year old. Crib bumpers include any material that is designed to cover the sides of a crib, which includes padding or vinyl bumper guards but not non-padded mesh crib liners.
The U.S. Consumer Product Safety Commission has received reports of more than 113 deaths involving crib bumpers between 1990 and 2019, as well as 113 nonfatal incidents between 2008 and 2019, according to a report from the commission.
More than 100 babies have died from infant-inclined sleep products, according to the commission, which has recalled numerous versions in recent years. But older models are still in circulation, CBS News reported.
Last year, the commission approved a federal safety rule that bans several types of sleep products for babies under 5 months old. Set to take effect next month, the rule requires products marketed for infants to meet the same federal safety standards as required for cribs and similar products.
Parents and advocates have called for a ban on these products for decades, according to CBS, since they can lead to suffocation when an infant’s nose and mouth are covered by a bumper or become stuck between a bumper and crib mattress.
Sudden unexpected infant death, or SUID – which includes sudden infant death syndrome, or SIDS – is the leading cause of injury death in infancy, according to the American Academy of Pediatrics. The group’s recommendations for safe sleep advise that infants should sleep on their back on a firm, flat surface without any extra padding, pillows, blankets, stuffed toys, bumpers, or other soft items in the sleep space.
A version of this article first appeared on WebMD.com.
A new law will ban certain infant sleep products blamed for the deaths of more than 200 babies in the United States.
On May 16, President Joe Biden signed legislation that prohibits the manufacture and sale of crib bumpers or inclined sleepers for infants, due to the risk of suffocation, according to CBS News.
H.R. 3182, or the Safe Sleep for Babies Act of 2021, notes that sleepers and bumpers will be considered “banned hazardous products” under the Consumer Product Safety Act. It gives manufacturers and retailers 180 days to comply with the new rule.
“The dangers posed to babies have been apparent for years,” Teresa Murray, who directs the consumer watchdog office for the U.S. PIRG Education Fund, said in a statement.
“It’s unfortunate that this law could take months to take effect,” she said. “Parents and caregivers need to recognize the dangers of these products and get them out of their homes now.”
H.R. 3182 defines inclined sleepers as products that have a sleep surface slanted greater than 10 degrees and are intended for babies up to 1 year old. Crib bumpers include any material that is designed to cover the sides of a crib, which includes padding or vinyl bumper guards but not non-padded mesh crib liners.
The U.S. Consumer Product Safety Commission has received reports of more than 113 deaths involving crib bumpers between 1990 and 2019, as well as 113 nonfatal incidents between 2008 and 2019, according to a report from the commission.
More than 100 babies have died from infant-inclined sleep products, according to the commission, which has recalled numerous versions in recent years. But older models are still in circulation, CBS News reported.
Last year, the commission approved a federal safety rule that bans several types of sleep products for babies under 5 months old. Set to take effect next month, the rule requires products marketed for infants to meet the same federal safety standards as required for cribs and similar products.
Parents and advocates have called for a ban on these products for decades, according to CBS, since they can lead to suffocation when an infant’s nose and mouth are covered by a bumper or become stuck between a bumper and crib mattress.
Sudden unexpected infant death, or SUID – which includes sudden infant death syndrome, or SIDS – is the leading cause of injury death in infancy, according to the American Academy of Pediatrics. The group’s recommendations for safe sleep advise that infants should sleep on their back on a firm, flat surface without any extra padding, pillows, blankets, stuffed toys, bumpers, or other soft items in the sleep space.
A version of this article first appeared on WebMD.com.
A new law will ban certain infant sleep products blamed for the deaths of more than 200 babies in the United States.
On May 16, President Joe Biden signed legislation that prohibits the manufacture and sale of crib bumpers or inclined sleepers for infants, due to the risk of suffocation, according to CBS News.
H.R. 3182, or the Safe Sleep for Babies Act of 2021, notes that sleepers and bumpers will be considered “banned hazardous products” under the Consumer Product Safety Act. It gives manufacturers and retailers 180 days to comply with the new rule.
“The dangers posed to babies have been apparent for years,” Teresa Murray, who directs the consumer watchdog office for the U.S. PIRG Education Fund, said in a statement.
“It’s unfortunate that this law could take months to take effect,” she said. “Parents and caregivers need to recognize the dangers of these products and get them out of their homes now.”
H.R. 3182 defines inclined sleepers as products that have a sleep surface slanted greater than 10 degrees and are intended for babies up to 1 year old. Crib bumpers include any material that is designed to cover the sides of a crib, which includes padding or vinyl bumper guards but not non-padded mesh crib liners.
The U.S. Consumer Product Safety Commission has received reports of more than 113 deaths involving crib bumpers between 1990 and 2019, as well as 113 nonfatal incidents between 2008 and 2019, according to a report from the commission.
More than 100 babies have died from infant-inclined sleep products, according to the commission, which has recalled numerous versions in recent years. But older models are still in circulation, CBS News reported.
Last year, the commission approved a federal safety rule that bans several types of sleep products for babies under 5 months old. Set to take effect next month, the rule requires products marketed for infants to meet the same federal safety standards as required for cribs and similar products.
Parents and advocates have called for a ban on these products for decades, according to CBS, since they can lead to suffocation when an infant’s nose and mouth are covered by a bumper or become stuck between a bumper and crib mattress.
Sudden unexpected infant death, or SUID – which includes sudden infant death syndrome, or SIDS – is the leading cause of injury death in infancy, according to the American Academy of Pediatrics. The group’s recommendations for safe sleep advise that infants should sleep on their back on a firm, flat surface without any extra padding, pillows, blankets, stuffed toys, bumpers, or other soft items in the sleep space.
A version of this article first appeared on WebMD.com.
Pfizer COVID vaccine performs well in youth with rheumatic diseases
The Pfizer-BioNTech mRNA vaccine (Comirnaty) showed a good safety profile with minimal short-term side effects and no negative impact on disease activity in a cohort of adolescents and young adults with rheumatic diseases, according to research presented at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance, held virtually this year.
Only 3% of patients experience a severe transient adverse event, according to Merav Heshin-Bekenstein, MD, of Dana-Dwek Children’s Hospital at the Tel Aviv Sourasky Medical Center in Israel. The findings were published in Rheumatology.
“We found that the mRNA Pfizer vaccine was immunogenic and induced an adequate humoral immune response in adolescent patients,” Dr. Heshin-Bekenstein told CARRA attendees. “It was definitely comparable to healthy controls and practically all patients were seropositive following the second vaccine, except for one patient with long-standing systemic sclerosis.”
The findings were not necessarily surprising but were encouraging to Melissa S. Oliver, MD, assistant professor of clinical pediatrics in the division of pediatric rheumatology at Indiana University, Indianapolis. Dr. Oliver wasn’t part of the study team.
“We know that the COVID vaccines in healthy adolescents have shown good efficacy with minimal side effects, and it’s good to see that this study showed that in those with rheumatic diseases on immunosuppressive therapy,” Dr. Oliver told this news organization.
Until now, the data on COVID-19 vaccines in teens with rheumatic illnesses has been limited, she said, so “many pediatric rheumatologists only have the data from adult studies to go on or personal experience with their own cohort of patients.”
But the high immunogenicity seen in the study was a pleasant surprise to Beth H. Rutstein, MD, assistant professor of clinical pediatrics in the division of rheumatology at Children’s Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania.
“I was both surprised and thrilled with Dr. Heshin-Bekenstein’s findings suggesting near-universal seroconversion for patients with rheumatic disease regardless of underlying diagnosis or immunomodulatory therapy regimen, as much of the adult data has suggested a poorer seroconversion rate” and lower antibody titers in adults with similar illnesses, Dr. Rutstein said in an interview.
The study “provides essential reassurance that vaccination against COVID-19 does not increase the risk of disease flare or worsen disease severity scores,” said Dr. Rutstein, who was not associated with the research. “Rather than speaking purely anecdotally with our patients and their families, we can refer to the science – which is always more reassuring for both our patients and ourselves.”
Study included diverse conditions and therapies
Risk factors for poor outcomes with COVID-19 in children include obesity, cardiovascular disease, chronic lung disease, diabetes, and asthma, Dr. Heshin-Bekenstein told CARRA attendees. Multisystem inflammatory syndrome in children (MIS-C) and long COVID are also potential complications of COVID-19 with less understood risk factors.
Although COVID-19 is most often mild in children, certain severe, systemic rheumatic diseases increase hospitalization risk, including systemic lupus erythematosus (SLE) and vasculitis. Evidence has also shown that COVID-19 infection increases the risk of disease flare in teens with juvenile-onset rheumatic diseases, so it’s “crucial to prevent COVID-19 disease in this population,” Dr. Heshin-Bekenstein said.
Her study therefore aimed to assess the safety and immunogenicity of the Pfizer mRNA vaccine for teens with juvenile-onset rheumatic diseases and those taking immunomodulatory medications. The international prospective multicenter study ran from April to November 2021 at three pediatric rheumatology clinics in Israel and one in Slovenia. Endpoints included short-term side effects, vaccination impact on clinical disease activity, immunogenicity at 2-9 weeks after the second dose, and, secondarily, efficacy against COVID-19 infection.
The 91 participants included adolescents aged 12-18 and young adults aged 18-21. Nearly half of the participants (46%) had juvenile idiopathic arthritis (JIA), and 14% had SLE. Other participants’ conditions included systemic vasculitis, idiopathic uveitis, inflammatory bowel disease–related arthritis, systemic or localized scleroderma, juvenile dermatomyositis, or an autoinflammatory disease. Participants’ mean disease duration was 4.8 years.
The researchers compared the patients with a control group of 40 individuals with similar demographics but without rheumatic disease. The researchers used the LIAISON quantitative assay to assess serum IgG antibody levels against the SARS-CoV-2 spike protein in both groups.
Eight in 10 participants with rheumatic disease were taking an immunomodulatory medication, including a conventional synthetic disease-modifying antirheumatic drug (csDMARD) in 40%, a biologic DMARD in 37%, tumor necrosis factor (TNF) inhibitors in 32%, hydroxychloroquine (HCQ) in 19%, glucocorticoids in 14%, and mycophenolate in 11%. A smaller proportion were on other biologics: JAK inhibitors in 6.6%, anti-CD20 drugs in 4.4%, and an IL-6 inhibitor in 1%.
Side effects similar in both groups
None of the side effects reported by participants were statistically different between those with rheumatic disease and the control group. Localized pain was the most common side effect, reported by 73%-79% of participants after each dose. About twice as many participants with rheumatic disease experienced muscle aches and joint pains, compared with the control group, but the differences were not significant. Fever occurred more often in those with rheumatic disease (6%, five cases) than without (3%, one case). One-third of those with rheumatic disease felt tiredness, compared with 20% of the control group.
None of the healthy controls were hospitalized after vaccination, but three rheumatic patients were, including two after the first dose. Both were 17 years old, had systemic vasculitis with granulomatosis with polyangiitis (GPA), and were taking rituximab (Rituxan). One patient experienced acute onset of chronic renal failure, fever, dehydration, and high C-reactive protein within hours of vaccination. The other experienced new onset of pulmonary hemorrhage a week after vaccination.
In addition, a 14-year-old female with lupus, taking only HCQ, went to the emergency department with fever, headache, vomiting, and joint pain 1 day after the second vaccine dose. She had normal inflammatory markers and no change in disease activity score, and she was discharged with low-dose steroids tapered after 2 weeks.
Immune response high in patients with rheumatic disease
Immunogenicity was similar in both groups, with 97% seropositivity in the rheumatic disease group and 100% in the control group. Average IgG titers were 242 in the rheumatic group and 388 in the control group (P < .0001). Seropositivity was 88% in those taking mycophenolate with another drug (100% with mycophenolate monotherapy), 90% with HCQ, 94% with any csDMARDs and another drug (100% with csDMARD monotherapy), and 100% for all other drugs. During 3 months’ follow-up after vaccination, there were no COVID-19 cases among the participants.
Dr. Heshin-Bekenstein noted that their results showed better immunogenicity in teens, compared with adults, for two specific drugs. Seropositivity in teens taking methotrexate (Rheumatrex, Trexall) or rituximab was 100% in this study, compared with 84% in adults taking methotrexate and 39% in adults taking rituximab in a previous study. However, only three patients in this study were taking rituximab, and only seven were taking methotrexate.
The study’s heterogenous population was both a strength and a weakness of the study. “Due to the diversity of rheumatic diseases and medications included in this cohort, it was not possible to draw significant conclusions regarding the impact of the immunomodulatory medications and type of disease” on titers, Dr. Heshin-Bekenstein told attendees.
Still, “I think as pediatric rheumatologists, we can feel reassured in recommending the COVID-19 vaccine to our patients,” Dr. Oliver said. “I will add that every patient is different, and everyone should have a conversation with their physician about receiving the COVID-19 vaccine.” Dr. Oliver said she discusses vaccination, including COVID vaccination, with every patient, and it’s been challenging to address concerns in the midst of so much misinformation circulating about the vaccine.
These findings do raise questions about whether it’s still necessary to hold immunomodulatory medications to get the vaccine,” Dr. Rutstein said.
“Many families are nervous to pause their medications before and after the vaccine as is currently recommended for many therapies by the American College of Rheumatology, and I do share that concern for some of my patients with more clinically unstable disease, so I try to work with each family to decide on best timing and have delayed or deferred the series until some patients are on a steady dose of a new immunomodulatory medication if it has been recently started,” Dr. Rutstein said. “This is one of the reasons why Dr. Heshin-Bekenstein’s study is so important – we may be holding medications that can be safely continued and even further decrease the risk of disease flare.”
None of the physicians have disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Pfizer-BioNTech mRNA vaccine (Comirnaty) showed a good safety profile with minimal short-term side effects and no negative impact on disease activity in a cohort of adolescents and young adults with rheumatic diseases, according to research presented at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance, held virtually this year.
Only 3% of patients experience a severe transient adverse event, according to Merav Heshin-Bekenstein, MD, of Dana-Dwek Children’s Hospital at the Tel Aviv Sourasky Medical Center in Israel. The findings were published in Rheumatology.
“We found that the mRNA Pfizer vaccine was immunogenic and induced an adequate humoral immune response in adolescent patients,” Dr. Heshin-Bekenstein told CARRA attendees. “It was definitely comparable to healthy controls and practically all patients were seropositive following the second vaccine, except for one patient with long-standing systemic sclerosis.”
The findings were not necessarily surprising but were encouraging to Melissa S. Oliver, MD, assistant professor of clinical pediatrics in the division of pediatric rheumatology at Indiana University, Indianapolis. Dr. Oliver wasn’t part of the study team.
“We know that the COVID vaccines in healthy adolescents have shown good efficacy with minimal side effects, and it’s good to see that this study showed that in those with rheumatic diseases on immunosuppressive therapy,” Dr. Oliver told this news organization.
Until now, the data on COVID-19 vaccines in teens with rheumatic illnesses has been limited, she said, so “many pediatric rheumatologists only have the data from adult studies to go on or personal experience with their own cohort of patients.”
But the high immunogenicity seen in the study was a pleasant surprise to Beth H. Rutstein, MD, assistant professor of clinical pediatrics in the division of rheumatology at Children’s Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania.
“I was both surprised and thrilled with Dr. Heshin-Bekenstein’s findings suggesting near-universal seroconversion for patients with rheumatic disease regardless of underlying diagnosis or immunomodulatory therapy regimen, as much of the adult data has suggested a poorer seroconversion rate” and lower antibody titers in adults with similar illnesses, Dr. Rutstein said in an interview.
The study “provides essential reassurance that vaccination against COVID-19 does not increase the risk of disease flare or worsen disease severity scores,” said Dr. Rutstein, who was not associated with the research. “Rather than speaking purely anecdotally with our patients and their families, we can refer to the science – which is always more reassuring for both our patients and ourselves.”
Study included diverse conditions and therapies
Risk factors for poor outcomes with COVID-19 in children include obesity, cardiovascular disease, chronic lung disease, diabetes, and asthma, Dr. Heshin-Bekenstein told CARRA attendees. Multisystem inflammatory syndrome in children (MIS-C) and long COVID are also potential complications of COVID-19 with less understood risk factors.
Although COVID-19 is most often mild in children, certain severe, systemic rheumatic diseases increase hospitalization risk, including systemic lupus erythematosus (SLE) and vasculitis. Evidence has also shown that COVID-19 infection increases the risk of disease flare in teens with juvenile-onset rheumatic diseases, so it’s “crucial to prevent COVID-19 disease in this population,” Dr. Heshin-Bekenstein said.
Her study therefore aimed to assess the safety and immunogenicity of the Pfizer mRNA vaccine for teens with juvenile-onset rheumatic diseases and those taking immunomodulatory medications. The international prospective multicenter study ran from April to November 2021 at three pediatric rheumatology clinics in Israel and one in Slovenia. Endpoints included short-term side effects, vaccination impact on clinical disease activity, immunogenicity at 2-9 weeks after the second dose, and, secondarily, efficacy against COVID-19 infection.
The 91 participants included adolescents aged 12-18 and young adults aged 18-21. Nearly half of the participants (46%) had juvenile idiopathic arthritis (JIA), and 14% had SLE. Other participants’ conditions included systemic vasculitis, idiopathic uveitis, inflammatory bowel disease–related arthritis, systemic or localized scleroderma, juvenile dermatomyositis, or an autoinflammatory disease. Participants’ mean disease duration was 4.8 years.
The researchers compared the patients with a control group of 40 individuals with similar demographics but without rheumatic disease. The researchers used the LIAISON quantitative assay to assess serum IgG antibody levels against the SARS-CoV-2 spike protein in both groups.
Eight in 10 participants with rheumatic disease were taking an immunomodulatory medication, including a conventional synthetic disease-modifying antirheumatic drug (csDMARD) in 40%, a biologic DMARD in 37%, tumor necrosis factor (TNF) inhibitors in 32%, hydroxychloroquine (HCQ) in 19%, glucocorticoids in 14%, and mycophenolate in 11%. A smaller proportion were on other biologics: JAK inhibitors in 6.6%, anti-CD20 drugs in 4.4%, and an IL-6 inhibitor in 1%.
Side effects similar in both groups
None of the side effects reported by participants were statistically different between those with rheumatic disease and the control group. Localized pain was the most common side effect, reported by 73%-79% of participants after each dose. About twice as many participants with rheumatic disease experienced muscle aches and joint pains, compared with the control group, but the differences were not significant. Fever occurred more often in those with rheumatic disease (6%, five cases) than without (3%, one case). One-third of those with rheumatic disease felt tiredness, compared with 20% of the control group.
None of the healthy controls were hospitalized after vaccination, but three rheumatic patients were, including two after the first dose. Both were 17 years old, had systemic vasculitis with granulomatosis with polyangiitis (GPA), and were taking rituximab (Rituxan). One patient experienced acute onset of chronic renal failure, fever, dehydration, and high C-reactive protein within hours of vaccination. The other experienced new onset of pulmonary hemorrhage a week after vaccination.
In addition, a 14-year-old female with lupus, taking only HCQ, went to the emergency department with fever, headache, vomiting, and joint pain 1 day after the second vaccine dose. She had normal inflammatory markers and no change in disease activity score, and she was discharged with low-dose steroids tapered after 2 weeks.
Immune response high in patients with rheumatic disease
Immunogenicity was similar in both groups, with 97% seropositivity in the rheumatic disease group and 100% in the control group. Average IgG titers were 242 in the rheumatic group and 388 in the control group (P < .0001). Seropositivity was 88% in those taking mycophenolate with another drug (100% with mycophenolate monotherapy), 90% with HCQ, 94% with any csDMARDs and another drug (100% with csDMARD monotherapy), and 100% for all other drugs. During 3 months’ follow-up after vaccination, there were no COVID-19 cases among the participants.
Dr. Heshin-Bekenstein noted that their results showed better immunogenicity in teens, compared with adults, for two specific drugs. Seropositivity in teens taking methotrexate (Rheumatrex, Trexall) or rituximab was 100% in this study, compared with 84% in adults taking methotrexate and 39% in adults taking rituximab in a previous study. However, only three patients in this study were taking rituximab, and only seven were taking methotrexate.
The study’s heterogenous population was both a strength and a weakness of the study. “Due to the diversity of rheumatic diseases and medications included in this cohort, it was not possible to draw significant conclusions regarding the impact of the immunomodulatory medications and type of disease” on titers, Dr. Heshin-Bekenstein told attendees.
Still, “I think as pediatric rheumatologists, we can feel reassured in recommending the COVID-19 vaccine to our patients,” Dr. Oliver said. “I will add that every patient is different, and everyone should have a conversation with their physician about receiving the COVID-19 vaccine.” Dr. Oliver said she discusses vaccination, including COVID vaccination, with every patient, and it’s been challenging to address concerns in the midst of so much misinformation circulating about the vaccine.
These findings do raise questions about whether it’s still necessary to hold immunomodulatory medications to get the vaccine,” Dr. Rutstein said.
“Many families are nervous to pause their medications before and after the vaccine as is currently recommended for many therapies by the American College of Rheumatology, and I do share that concern for some of my patients with more clinically unstable disease, so I try to work with each family to decide on best timing and have delayed or deferred the series until some patients are on a steady dose of a new immunomodulatory medication if it has been recently started,” Dr. Rutstein said. “This is one of the reasons why Dr. Heshin-Bekenstein’s study is so important – we may be holding medications that can be safely continued and even further decrease the risk of disease flare.”
None of the physicians have disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Pfizer-BioNTech mRNA vaccine (Comirnaty) showed a good safety profile with minimal short-term side effects and no negative impact on disease activity in a cohort of adolescents and young adults with rheumatic diseases, according to research presented at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance, held virtually this year.
Only 3% of patients experience a severe transient adverse event, according to Merav Heshin-Bekenstein, MD, of Dana-Dwek Children’s Hospital at the Tel Aviv Sourasky Medical Center in Israel. The findings were published in Rheumatology.
“We found that the mRNA Pfizer vaccine was immunogenic and induced an adequate humoral immune response in adolescent patients,” Dr. Heshin-Bekenstein told CARRA attendees. “It was definitely comparable to healthy controls and practically all patients were seropositive following the second vaccine, except for one patient with long-standing systemic sclerosis.”
The findings were not necessarily surprising but were encouraging to Melissa S. Oliver, MD, assistant professor of clinical pediatrics in the division of pediatric rheumatology at Indiana University, Indianapolis. Dr. Oliver wasn’t part of the study team.
“We know that the COVID vaccines in healthy adolescents have shown good efficacy with minimal side effects, and it’s good to see that this study showed that in those with rheumatic diseases on immunosuppressive therapy,” Dr. Oliver told this news organization.
Until now, the data on COVID-19 vaccines in teens with rheumatic illnesses has been limited, she said, so “many pediatric rheumatologists only have the data from adult studies to go on or personal experience with their own cohort of patients.”
But the high immunogenicity seen in the study was a pleasant surprise to Beth H. Rutstein, MD, assistant professor of clinical pediatrics in the division of rheumatology at Children’s Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania.
“I was both surprised and thrilled with Dr. Heshin-Bekenstein’s findings suggesting near-universal seroconversion for patients with rheumatic disease regardless of underlying diagnosis or immunomodulatory therapy regimen, as much of the adult data has suggested a poorer seroconversion rate” and lower antibody titers in adults with similar illnesses, Dr. Rutstein said in an interview.
The study “provides essential reassurance that vaccination against COVID-19 does not increase the risk of disease flare or worsen disease severity scores,” said Dr. Rutstein, who was not associated with the research. “Rather than speaking purely anecdotally with our patients and their families, we can refer to the science – which is always more reassuring for both our patients and ourselves.”
Study included diverse conditions and therapies
Risk factors for poor outcomes with COVID-19 in children include obesity, cardiovascular disease, chronic lung disease, diabetes, and asthma, Dr. Heshin-Bekenstein told CARRA attendees. Multisystem inflammatory syndrome in children (MIS-C) and long COVID are also potential complications of COVID-19 with less understood risk factors.
Although COVID-19 is most often mild in children, certain severe, systemic rheumatic diseases increase hospitalization risk, including systemic lupus erythematosus (SLE) and vasculitis. Evidence has also shown that COVID-19 infection increases the risk of disease flare in teens with juvenile-onset rheumatic diseases, so it’s “crucial to prevent COVID-19 disease in this population,” Dr. Heshin-Bekenstein said.
Her study therefore aimed to assess the safety and immunogenicity of the Pfizer mRNA vaccine for teens with juvenile-onset rheumatic diseases and those taking immunomodulatory medications. The international prospective multicenter study ran from April to November 2021 at three pediatric rheumatology clinics in Israel and one in Slovenia. Endpoints included short-term side effects, vaccination impact on clinical disease activity, immunogenicity at 2-9 weeks after the second dose, and, secondarily, efficacy against COVID-19 infection.
The 91 participants included adolescents aged 12-18 and young adults aged 18-21. Nearly half of the participants (46%) had juvenile idiopathic arthritis (JIA), and 14% had SLE. Other participants’ conditions included systemic vasculitis, idiopathic uveitis, inflammatory bowel disease–related arthritis, systemic or localized scleroderma, juvenile dermatomyositis, or an autoinflammatory disease. Participants’ mean disease duration was 4.8 years.
The researchers compared the patients with a control group of 40 individuals with similar demographics but without rheumatic disease. The researchers used the LIAISON quantitative assay to assess serum IgG antibody levels against the SARS-CoV-2 spike protein in both groups.
Eight in 10 participants with rheumatic disease were taking an immunomodulatory medication, including a conventional synthetic disease-modifying antirheumatic drug (csDMARD) in 40%, a biologic DMARD in 37%, tumor necrosis factor (TNF) inhibitors in 32%, hydroxychloroquine (HCQ) in 19%, glucocorticoids in 14%, and mycophenolate in 11%. A smaller proportion were on other biologics: JAK inhibitors in 6.6%, anti-CD20 drugs in 4.4%, and an IL-6 inhibitor in 1%.
Side effects similar in both groups
None of the side effects reported by participants were statistically different between those with rheumatic disease and the control group. Localized pain was the most common side effect, reported by 73%-79% of participants after each dose. About twice as many participants with rheumatic disease experienced muscle aches and joint pains, compared with the control group, but the differences were not significant. Fever occurred more often in those with rheumatic disease (6%, five cases) than without (3%, one case). One-third of those with rheumatic disease felt tiredness, compared with 20% of the control group.
None of the healthy controls were hospitalized after vaccination, but three rheumatic patients were, including two after the first dose. Both were 17 years old, had systemic vasculitis with granulomatosis with polyangiitis (GPA), and were taking rituximab (Rituxan). One patient experienced acute onset of chronic renal failure, fever, dehydration, and high C-reactive protein within hours of vaccination. The other experienced new onset of pulmonary hemorrhage a week after vaccination.
In addition, a 14-year-old female with lupus, taking only HCQ, went to the emergency department with fever, headache, vomiting, and joint pain 1 day after the second vaccine dose. She had normal inflammatory markers and no change in disease activity score, and she was discharged with low-dose steroids tapered after 2 weeks.
Immune response high in patients with rheumatic disease
Immunogenicity was similar in both groups, with 97% seropositivity in the rheumatic disease group and 100% in the control group. Average IgG titers were 242 in the rheumatic group and 388 in the control group (P < .0001). Seropositivity was 88% in those taking mycophenolate with another drug (100% with mycophenolate monotherapy), 90% with HCQ, 94% with any csDMARDs and another drug (100% with csDMARD monotherapy), and 100% for all other drugs. During 3 months’ follow-up after vaccination, there were no COVID-19 cases among the participants.
Dr. Heshin-Bekenstein noted that their results showed better immunogenicity in teens, compared with adults, for two specific drugs. Seropositivity in teens taking methotrexate (Rheumatrex, Trexall) or rituximab was 100% in this study, compared with 84% in adults taking methotrexate and 39% in adults taking rituximab in a previous study. However, only three patients in this study were taking rituximab, and only seven were taking methotrexate.
The study’s heterogenous population was both a strength and a weakness of the study. “Due to the diversity of rheumatic diseases and medications included in this cohort, it was not possible to draw significant conclusions regarding the impact of the immunomodulatory medications and type of disease” on titers, Dr. Heshin-Bekenstein told attendees.
Still, “I think as pediatric rheumatologists, we can feel reassured in recommending the COVID-19 vaccine to our patients,” Dr. Oliver said. “I will add that every patient is different, and everyone should have a conversation with their physician about receiving the COVID-19 vaccine.” Dr. Oliver said she discusses vaccination, including COVID vaccination, with every patient, and it’s been challenging to address concerns in the midst of so much misinformation circulating about the vaccine.
These findings do raise questions about whether it’s still necessary to hold immunomodulatory medications to get the vaccine,” Dr. Rutstein said.
“Many families are nervous to pause their medications before and after the vaccine as is currently recommended for many therapies by the American College of Rheumatology, and I do share that concern for some of my patients with more clinically unstable disease, so I try to work with each family to decide on best timing and have delayed or deferred the series until some patients are on a steady dose of a new immunomodulatory medication if it has been recently started,” Dr. Rutstein said. “This is one of the reasons why Dr. Heshin-Bekenstein’s study is so important – we may be holding medications that can be safely continued and even further decrease the risk of disease flare.”
None of the physicians have disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CARRA 2022
Ondansetron use for acute gastroenteritis in children accelerates
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
FROM JAMA NETWORK OPEN
CDC updates guidelines for hepatitis outbreak among children
The Centers for Disease Control and Prevention updated its recommendations for doctors and public health officials regarding the unusual outbreak of acute hepatitis among children.
As of May 5, the CDC and state health departments are investigating 109 children with hepatitis of unknown origin across 25 states and territories.
More than half have tested positive for adenovirus, the CDC said. More than 90% have been hospitalized, and 14% have had liver transplants. Five deaths are under investigation.
This week’s CDC alert provides updated recommendations for testing, given the potential association between adenovirus infection and pediatric hepatitis, or liver inflammation.
“Clinicians are recommended to consider adenovirus testing for patients with hepatitis of unknown etiology and to report such cases to their state or jurisdictional public health authorities,” the CDC said.
Doctors should also consider collecting a blood sample, respiratory sample, and stool sample. They may also collect liver tissue if a biopsy occurred or an autopsy is available.
In November 2021, clinicians at a large children’s hospital in Alabama notified the CDC about five pediatric patients with significant liver injury, including three with acute liver failure, who also tested positive for adenovirus. All children were previously healthy, and none had COVID-19, according to a CDC alert in April.
Four additional pediatric patients with hepatitis and adenovirus infection were identified. After lab testing found adenovirus infection in all nine patients in the initial cluster, public health officials began investigating a possible association between pediatric hepatitis and adenovirus. Among the five specimens that could be sequenced, they were all adenovirus type 41.
Unexplained hepatitis cases have been reported in children worldwide, reaching 450 cases and 11 deaths, according to the latest update from the European Centre for Disease Prevention and Control.
The cases have been reported in more than two dozen countries around the world, with 14 countries reporting more than five cases. The United Kingdom and the United States have reported the largest case counts so far.
In the United Kingdom, officials have identified 163 cases in children under age 16 years, including 11 that required liver transplants.
In the European Union, 14 countries have reported 106 cases collectively, with Italy reporting 35 cases and Spain reporting 22 cases. Outside of the European Union, Brazil has reported 16, Indonesia has reported 15, and Israel has reported 12.
Among the 11 deaths reported globally, the Uniyed States has reported five, Indonesia has reported five, and Palestine has reported one.
The cause of severe hepatitis remains a mystery, according to Ars Technica. Some cases have been identified retrospectively, dating back to the beginning of October 2021.
About 70% of the cases that have been tested for an adenovirus have tested positive, and subtype testing continues to show adenovirus type 41. The cases don’t appear to be linked to common causes, such as hepatitis viruses A, B, C, D, or E, which can cause liver inflammation and injury.
Adenoviruses aren’t known to cause hepatitis in healthy children, though the viruses have been linked to liver damage in children with compromised immune systems, according to Ars Technica. Adenoviruses typically cause respiratory infections in children, although type 41 tends to cause gastrointestinal illness.
“At present, the leading hypotheses remain those which involve adenovirus,” Philippa Easterbrook, a senior scientist at the WHO, said May 10 during a press briefing.
“I think [there’s] also still an important consideration about the role of COVID as well, either as a co-infection or as a past infection,” she said.
WHO officials expect data within a week from U.K. cases, Ms. Easterbrook said, which may indicate whether the adenovirus is an incidental infection or a more direct cause.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention updated its recommendations for doctors and public health officials regarding the unusual outbreak of acute hepatitis among children.
As of May 5, the CDC and state health departments are investigating 109 children with hepatitis of unknown origin across 25 states and territories.
More than half have tested positive for adenovirus, the CDC said. More than 90% have been hospitalized, and 14% have had liver transplants. Five deaths are under investigation.
This week’s CDC alert provides updated recommendations for testing, given the potential association between adenovirus infection and pediatric hepatitis, or liver inflammation.
“Clinicians are recommended to consider adenovirus testing for patients with hepatitis of unknown etiology and to report such cases to their state or jurisdictional public health authorities,” the CDC said.
Doctors should also consider collecting a blood sample, respiratory sample, and stool sample. They may also collect liver tissue if a biopsy occurred or an autopsy is available.
In November 2021, clinicians at a large children’s hospital in Alabama notified the CDC about five pediatric patients with significant liver injury, including three with acute liver failure, who also tested positive for adenovirus. All children were previously healthy, and none had COVID-19, according to a CDC alert in April.
Four additional pediatric patients with hepatitis and adenovirus infection were identified. After lab testing found adenovirus infection in all nine patients in the initial cluster, public health officials began investigating a possible association between pediatric hepatitis and adenovirus. Among the five specimens that could be sequenced, they were all adenovirus type 41.
Unexplained hepatitis cases have been reported in children worldwide, reaching 450 cases and 11 deaths, according to the latest update from the European Centre for Disease Prevention and Control.
The cases have been reported in more than two dozen countries around the world, with 14 countries reporting more than five cases. The United Kingdom and the United States have reported the largest case counts so far.
In the United Kingdom, officials have identified 163 cases in children under age 16 years, including 11 that required liver transplants.
In the European Union, 14 countries have reported 106 cases collectively, with Italy reporting 35 cases and Spain reporting 22 cases. Outside of the European Union, Brazil has reported 16, Indonesia has reported 15, and Israel has reported 12.
Among the 11 deaths reported globally, the Uniyed States has reported five, Indonesia has reported five, and Palestine has reported one.
The cause of severe hepatitis remains a mystery, according to Ars Technica. Some cases have been identified retrospectively, dating back to the beginning of October 2021.
About 70% of the cases that have been tested for an adenovirus have tested positive, and subtype testing continues to show adenovirus type 41. The cases don’t appear to be linked to common causes, such as hepatitis viruses A, B, C, D, or E, which can cause liver inflammation and injury.
Adenoviruses aren’t known to cause hepatitis in healthy children, though the viruses have been linked to liver damage in children with compromised immune systems, according to Ars Technica. Adenoviruses typically cause respiratory infections in children, although type 41 tends to cause gastrointestinal illness.
“At present, the leading hypotheses remain those which involve adenovirus,” Philippa Easterbrook, a senior scientist at the WHO, said May 10 during a press briefing.
“I think [there’s] also still an important consideration about the role of COVID as well, either as a co-infection or as a past infection,” she said.
WHO officials expect data within a week from U.K. cases, Ms. Easterbrook said, which may indicate whether the adenovirus is an incidental infection or a more direct cause.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention updated its recommendations for doctors and public health officials regarding the unusual outbreak of acute hepatitis among children.
As of May 5, the CDC and state health departments are investigating 109 children with hepatitis of unknown origin across 25 states and territories.
More than half have tested positive for adenovirus, the CDC said. More than 90% have been hospitalized, and 14% have had liver transplants. Five deaths are under investigation.
This week’s CDC alert provides updated recommendations for testing, given the potential association between adenovirus infection and pediatric hepatitis, or liver inflammation.
“Clinicians are recommended to consider adenovirus testing for patients with hepatitis of unknown etiology and to report such cases to their state or jurisdictional public health authorities,” the CDC said.
Doctors should also consider collecting a blood sample, respiratory sample, and stool sample. They may also collect liver tissue if a biopsy occurred or an autopsy is available.
In November 2021, clinicians at a large children’s hospital in Alabama notified the CDC about five pediatric patients with significant liver injury, including three with acute liver failure, who also tested positive for adenovirus. All children were previously healthy, and none had COVID-19, according to a CDC alert in April.
Four additional pediatric patients with hepatitis and adenovirus infection were identified. After lab testing found adenovirus infection in all nine patients in the initial cluster, public health officials began investigating a possible association between pediatric hepatitis and adenovirus. Among the five specimens that could be sequenced, they were all adenovirus type 41.
Unexplained hepatitis cases have been reported in children worldwide, reaching 450 cases and 11 deaths, according to the latest update from the European Centre for Disease Prevention and Control.
The cases have been reported in more than two dozen countries around the world, with 14 countries reporting more than five cases. The United Kingdom and the United States have reported the largest case counts so far.
In the United Kingdom, officials have identified 163 cases in children under age 16 years, including 11 that required liver transplants.
In the European Union, 14 countries have reported 106 cases collectively, with Italy reporting 35 cases and Spain reporting 22 cases. Outside of the European Union, Brazil has reported 16, Indonesia has reported 15, and Israel has reported 12.
Among the 11 deaths reported globally, the Uniyed States has reported five, Indonesia has reported five, and Palestine has reported one.
The cause of severe hepatitis remains a mystery, according to Ars Technica. Some cases have been identified retrospectively, dating back to the beginning of October 2021.
About 70% of the cases that have been tested for an adenovirus have tested positive, and subtype testing continues to show adenovirus type 41. The cases don’t appear to be linked to common causes, such as hepatitis viruses A, B, C, D, or E, which can cause liver inflammation and injury.
Adenoviruses aren’t known to cause hepatitis in healthy children, though the viruses have been linked to liver damage in children with compromised immune systems, according to Ars Technica. Adenoviruses typically cause respiratory infections in children, although type 41 tends to cause gastrointestinal illness.
“At present, the leading hypotheses remain those which involve adenovirus,” Philippa Easterbrook, a senior scientist at the WHO, said May 10 during a press briefing.
“I think [there’s] also still an important consideration about the role of COVID as well, either as a co-infection or as a past infection,” she said.
WHO officials expect data within a week from U.K. cases, Ms. Easterbrook said, which may indicate whether the adenovirus is an incidental infection or a more direct cause.
A version of this article first appeared on Medscape.com.
Four mental health trajectories in youth: Predicting persistent psychopathology
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
FROM JAMA NETWORK OPEN
Measles outbreaks: Protecting your patients during international travel
The U.S. immunization program is one of the best public health success stories. Physicians who provide care for children are familiar with the routine childhood immunization schedule and administer a measles-containing vaccine at age-appropriate times. Thanks to its rigorous implementation and acceptance, endemic measles (absence of continuous virus transmission for > 1 year) was eliminated in the U.S. in 2000. Loss of this status was in jeopardy in 2019 when 22 measles outbreaks occurred in 17 states (7 were multistate outbreaks). That year, 1,163 cases were reported.1 Most cases occurred in unvaccinated persons (89%) and 81 cases were imported of which 54 were in U.S. citizens returning from international travel. All outbreaks were linked to travel. Fortunately, the outbreaks were controlled prior to the elimination deadline, or the United States would have lost its measles elimination status. Restrictions on travel because of COVID-19 have relaxed significantly since the introduction of COVID-19 vaccines, resulting in increased regional and international travel. Multiple countries, including the United States noted a decline in routine immunizations rates during the last 2 years. Recent U.S. data for the 2020-2021 school year indicates that MMR immunizations rates (two doses) for kindergarteners declined to 93.9% (range 78.9% to > 98.9%), while the overall percentage of those students with an exemption remained low at 2.2%. Vaccine coverage greater than 95% was reported in only 16 states. Coverage of less than 90% was reported in seven states and the District of Columbia (Georgia, Idaho, Kentucky, Maryland, Minnesota, Ohio, and Wisconsin).2 Vaccine coverage should be 95% or higher to maintain herd immunity and control outbreaks.
Why is measles prevention so important? Many physicians practicing in the United States today have never seen a case or know its potential complications. I saw my first case as a resident in an immigrant child. It took our training director to point out the subtle signs and symptoms. It was the first time I saw Kolpik spots. Measles is transmitted person to person via large respiratory droplets and less often by airborne spread. It is highly contagious for susceptible individuals with an attack rate of 90%. In this case, a medical student on the team developed symptoms about 10 days later. Six years would pass before I diagnosed my next case of measles. An HIV patient acquired it after close contact with someone who was in the prodromal stage. He presented with the 3 C’s: Cough, coryza, and conjunctivitis, in addition to fever and an erythematous rash. He did not recover from complications of the disease.
Prior to the routine administration of a measles vaccine, 3-4 million cases with almost 500 deaths occurred annually in the United States. Worldwide, 35 million cases and more than 6 million deaths occurred each year. Here, most patients recover completely; however, complications including otitis media, pneumonia, croup, and encephalitis can develop. Complications commonly occur in immunocompromised individuals and young children. Groups with the highest fatality rates include children aged less than 5 years, immunocompromised persons, and pregnant women. Worldwide, fatality rates are dependent on the patients underlying nutritional and health status in addition to the quality of health care available.3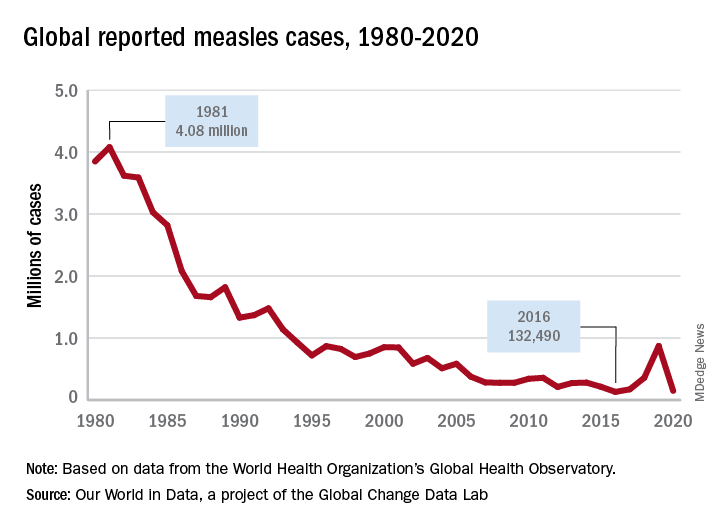
Measles vaccine was licensed in 1963 and cases began to decline (Figure 1). There was a resurgence in 1989 but it was not limited to the United States. The cause of the U.S. resurgence was multifactorial: Widespread viral transmission among unvaccinated preschool-age children residing in inner cities, outbreaks in vaccinated school-age children, outbreaks in students and personnel on college campuses, and primary vaccine failure (2%-5% of recipients failed to have an adequate response). In 1989, to help prevent future outbreaks, the United States recommended a two-dose schedule for measles and in 1993, the Vaccines for Children Program, a federally funded program, was established to improve access to vaccines for all children.
What is going on internationally?
Figure 2 lists the top 10 countries with current measles outbreaks.

Most countries on the list may not be typical travel destinations for tourists; however, they are common destinations for individuals visiting friends and relatives after immigrating to the United States. In contrast to the United States, most countries with limited resources and infrastructure have mass-vaccination campaigns to ensure vaccine administration to large segments of the population. They too have been affected by the COVID-19 pandemic. By report, at least 41 countries delayed implementation of their measles campaign in 2020 and 2021, thus, leading to the potential for even larger outbreaks.4
Progress toward the global elimination of measles is evidenced by the following: All 194 countries now include one dose of measles in their routine schedules; between 2000 and 2019 coverage of one dose of measles increased from 72% to 85% and countries with more than 90% coverage increased from 45% to 63%. Finally, the number of countries offering two doses of measles increased from 50% to 91% and vaccine coverage increased from 18% to 71% over the same time period.3
What can you do for your patients and their parents before they travel abroad?
- Inform all staff that the MMR vaccine can be administered to children as young as 6 months and at times other than those listed on the routine immunization schedule. This will help avoid parents seeking vaccine being denied an appointment.
- Children 6-11 months need 1 dose of MMR. Two additional doses will still need to be administered at the routine time.
- Children 12 months or older need 2 doses of MMR at least 4 weeks apart.
- If yellow fever vaccine is needed, coordinate administration with a travel medicine clinic since both are live vaccines and must be given on the same day.
- Any person born after 1956 should have 2 doses of MMR at least 4 weeks apart if they have no evidence of immunity.
- Encourage parents to always inform you and your staff of any international travel plans.
Moving forward, remember this increased global activity and the presence of inadequately vaccinated individuals/communities keeps the United States at continued risk for measles outbreaks. The source of the next outbreak may only be one plane ride away.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
This article was updated 6/29/22.
References
1. Patel M et al. MMWR. 2019 Oct 11; 68(40):893-6.
2. Seither R et al. MMWR. 2022 Apr 22;71(16):561-8.
3. Gastañaduy PA et al. J Infect Dis. 2021 Sep 30;224(12 Suppl 2):S420-8. doi: 10.1093/infdis/jiaa793.
4. Centers for Disease Control and Prevention. Measles (Rubeola). http://www.CDC.gov/Measles.
The U.S. immunization program is one of the best public health success stories. Physicians who provide care for children are familiar with the routine childhood immunization schedule and administer a measles-containing vaccine at age-appropriate times. Thanks to its rigorous implementation and acceptance, endemic measles (absence of continuous virus transmission for > 1 year) was eliminated in the U.S. in 2000. Loss of this status was in jeopardy in 2019 when 22 measles outbreaks occurred in 17 states (7 were multistate outbreaks). That year, 1,163 cases were reported.1 Most cases occurred in unvaccinated persons (89%) and 81 cases were imported of which 54 were in U.S. citizens returning from international travel. All outbreaks were linked to travel. Fortunately, the outbreaks were controlled prior to the elimination deadline, or the United States would have lost its measles elimination status. Restrictions on travel because of COVID-19 have relaxed significantly since the introduction of COVID-19 vaccines, resulting in increased regional and international travel. Multiple countries, including the United States noted a decline in routine immunizations rates during the last 2 years. Recent U.S. data for the 2020-2021 school year indicates that MMR immunizations rates (two doses) for kindergarteners declined to 93.9% (range 78.9% to > 98.9%), while the overall percentage of those students with an exemption remained low at 2.2%. Vaccine coverage greater than 95% was reported in only 16 states. Coverage of less than 90% was reported in seven states and the District of Columbia (Georgia, Idaho, Kentucky, Maryland, Minnesota, Ohio, and Wisconsin).2 Vaccine coverage should be 95% or higher to maintain herd immunity and control outbreaks.
Why is measles prevention so important? Many physicians practicing in the United States today have never seen a case or know its potential complications. I saw my first case as a resident in an immigrant child. It took our training director to point out the subtle signs and symptoms. It was the first time I saw Kolpik spots. Measles is transmitted person to person via large respiratory droplets and less often by airborne spread. It is highly contagious for susceptible individuals with an attack rate of 90%. In this case, a medical student on the team developed symptoms about 10 days later. Six years would pass before I diagnosed my next case of measles. An HIV patient acquired it after close contact with someone who was in the prodromal stage. He presented with the 3 C’s: Cough, coryza, and conjunctivitis, in addition to fever and an erythematous rash. He did not recover from complications of the disease.
Prior to the routine administration of a measles vaccine, 3-4 million cases with almost 500 deaths occurred annually in the United States. Worldwide, 35 million cases and more than 6 million deaths occurred each year. Here, most patients recover completely; however, complications including otitis media, pneumonia, croup, and encephalitis can develop. Complications commonly occur in immunocompromised individuals and young children. Groups with the highest fatality rates include children aged less than 5 years, immunocompromised persons, and pregnant women. Worldwide, fatality rates are dependent on the patients underlying nutritional and health status in addition to the quality of health care available.3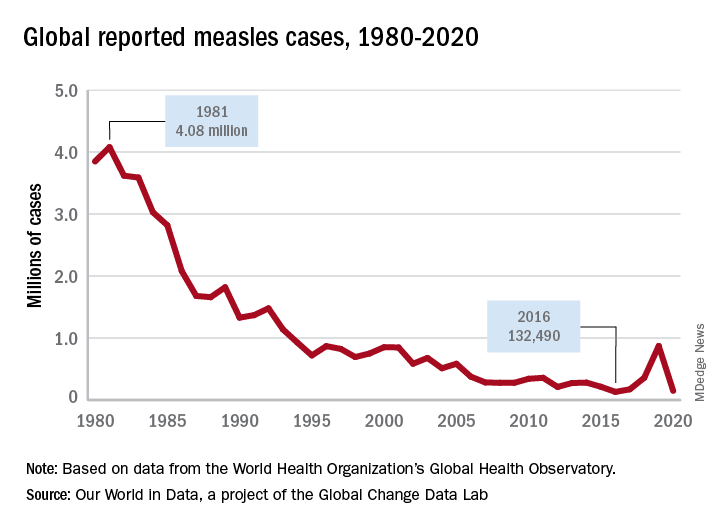
Measles vaccine was licensed in 1963 and cases began to decline (Figure 1). There was a resurgence in 1989 but it was not limited to the United States. The cause of the U.S. resurgence was multifactorial: Widespread viral transmission among unvaccinated preschool-age children residing in inner cities, outbreaks in vaccinated school-age children, outbreaks in students and personnel on college campuses, and primary vaccine failure (2%-5% of recipients failed to have an adequate response). In 1989, to help prevent future outbreaks, the United States recommended a two-dose schedule for measles and in 1993, the Vaccines for Children Program, a federally funded program, was established to improve access to vaccines for all children.
What is going on internationally?
Figure 2 lists the top 10 countries with current measles outbreaks.

Most countries on the list may not be typical travel destinations for tourists; however, they are common destinations for individuals visiting friends and relatives after immigrating to the United States. In contrast to the United States, most countries with limited resources and infrastructure have mass-vaccination campaigns to ensure vaccine administration to large segments of the population. They too have been affected by the COVID-19 pandemic. By report, at least 41 countries delayed implementation of their measles campaign in 2020 and 2021, thus, leading to the potential for even larger outbreaks.4
Progress toward the global elimination of measles is evidenced by the following: All 194 countries now include one dose of measles in their routine schedules; between 2000 and 2019 coverage of one dose of measles increased from 72% to 85% and countries with more than 90% coverage increased from 45% to 63%. Finally, the number of countries offering two doses of measles increased from 50% to 91% and vaccine coverage increased from 18% to 71% over the same time period.3
What can you do for your patients and their parents before they travel abroad?
- Inform all staff that the MMR vaccine can be administered to children as young as 6 months and at times other than those listed on the routine immunization schedule. This will help avoid parents seeking vaccine being denied an appointment.
- Children 6-11 months need 1 dose of MMR. Two additional doses will still need to be administered at the routine time.
- Children 12 months or older need 2 doses of MMR at least 4 weeks apart.
- If yellow fever vaccine is needed, coordinate administration with a travel medicine clinic since both are live vaccines and must be given on the same day.
- Any person born after 1956 should have 2 doses of MMR at least 4 weeks apart if they have no evidence of immunity.
- Encourage parents to always inform you and your staff of any international travel plans.
Moving forward, remember this increased global activity and the presence of inadequately vaccinated individuals/communities keeps the United States at continued risk for measles outbreaks. The source of the next outbreak may only be one plane ride away.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
This article was updated 6/29/22.
References
1. Patel M et al. MMWR. 2019 Oct 11; 68(40):893-6.
2. Seither R et al. MMWR. 2022 Apr 22;71(16):561-8.
3. Gastañaduy PA et al. J Infect Dis. 2021 Sep 30;224(12 Suppl 2):S420-8. doi: 10.1093/infdis/jiaa793.
4. Centers for Disease Control and Prevention. Measles (Rubeola). http://www.CDC.gov/Measles.
The U.S. immunization program is one of the best public health success stories. Physicians who provide care for children are familiar with the routine childhood immunization schedule and administer a measles-containing vaccine at age-appropriate times. Thanks to its rigorous implementation and acceptance, endemic measles (absence of continuous virus transmission for > 1 year) was eliminated in the U.S. in 2000. Loss of this status was in jeopardy in 2019 when 22 measles outbreaks occurred in 17 states (7 were multistate outbreaks). That year, 1,163 cases were reported.1 Most cases occurred in unvaccinated persons (89%) and 81 cases were imported of which 54 were in U.S. citizens returning from international travel. All outbreaks were linked to travel. Fortunately, the outbreaks were controlled prior to the elimination deadline, or the United States would have lost its measles elimination status. Restrictions on travel because of COVID-19 have relaxed significantly since the introduction of COVID-19 vaccines, resulting in increased regional and international travel. Multiple countries, including the United States noted a decline in routine immunizations rates during the last 2 years. Recent U.S. data for the 2020-2021 school year indicates that MMR immunizations rates (two doses) for kindergarteners declined to 93.9% (range 78.9% to > 98.9%), while the overall percentage of those students with an exemption remained low at 2.2%. Vaccine coverage greater than 95% was reported in only 16 states. Coverage of less than 90% was reported in seven states and the District of Columbia (Georgia, Idaho, Kentucky, Maryland, Minnesota, Ohio, and Wisconsin).2 Vaccine coverage should be 95% or higher to maintain herd immunity and control outbreaks.
Why is measles prevention so important? Many physicians practicing in the United States today have never seen a case or know its potential complications. I saw my first case as a resident in an immigrant child. It took our training director to point out the subtle signs and symptoms. It was the first time I saw Kolpik spots. Measles is transmitted person to person via large respiratory droplets and less often by airborne spread. It is highly contagious for susceptible individuals with an attack rate of 90%. In this case, a medical student on the team developed symptoms about 10 days later. Six years would pass before I diagnosed my next case of measles. An HIV patient acquired it after close contact with someone who was in the prodromal stage. He presented with the 3 C’s: Cough, coryza, and conjunctivitis, in addition to fever and an erythematous rash. He did not recover from complications of the disease.
Prior to the routine administration of a measles vaccine, 3-4 million cases with almost 500 deaths occurred annually in the United States. Worldwide, 35 million cases and more than 6 million deaths occurred each year. Here, most patients recover completely; however, complications including otitis media, pneumonia, croup, and encephalitis can develop. Complications commonly occur in immunocompromised individuals and young children. Groups with the highest fatality rates include children aged less than 5 years, immunocompromised persons, and pregnant women. Worldwide, fatality rates are dependent on the patients underlying nutritional and health status in addition to the quality of health care available.3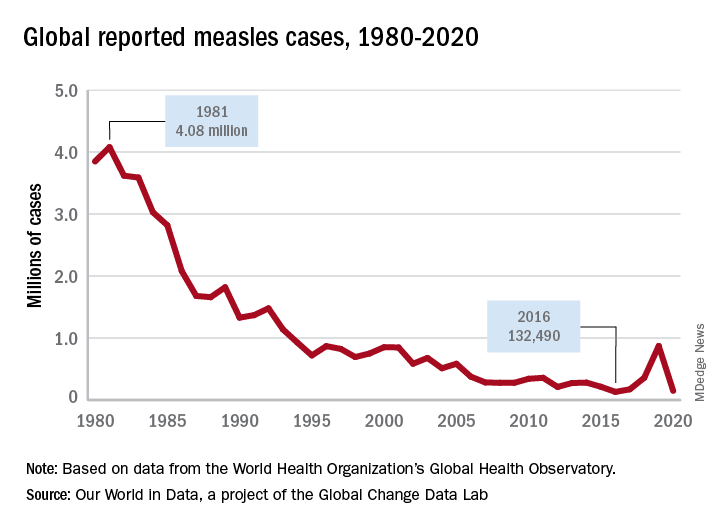
Measles vaccine was licensed in 1963 and cases began to decline (Figure 1). There was a resurgence in 1989 but it was not limited to the United States. The cause of the U.S. resurgence was multifactorial: Widespread viral transmission among unvaccinated preschool-age children residing in inner cities, outbreaks in vaccinated school-age children, outbreaks in students and personnel on college campuses, and primary vaccine failure (2%-5% of recipients failed to have an adequate response). In 1989, to help prevent future outbreaks, the United States recommended a two-dose schedule for measles and in 1993, the Vaccines for Children Program, a federally funded program, was established to improve access to vaccines for all children.
What is going on internationally?
Figure 2 lists the top 10 countries with current measles outbreaks.

Most countries on the list may not be typical travel destinations for tourists; however, they are common destinations for individuals visiting friends and relatives after immigrating to the United States. In contrast to the United States, most countries with limited resources and infrastructure have mass-vaccination campaigns to ensure vaccine administration to large segments of the population. They too have been affected by the COVID-19 pandemic. By report, at least 41 countries delayed implementation of their measles campaign in 2020 and 2021, thus, leading to the potential for even larger outbreaks.4
Progress toward the global elimination of measles is evidenced by the following: All 194 countries now include one dose of measles in their routine schedules; between 2000 and 2019 coverage of one dose of measles increased from 72% to 85% and countries with more than 90% coverage increased from 45% to 63%. Finally, the number of countries offering two doses of measles increased from 50% to 91% and vaccine coverage increased from 18% to 71% over the same time period.3
What can you do for your patients and their parents before they travel abroad?
- Inform all staff that the MMR vaccine can be administered to children as young as 6 months and at times other than those listed on the routine immunization schedule. This will help avoid parents seeking vaccine being denied an appointment.
- Children 6-11 months need 1 dose of MMR. Two additional doses will still need to be administered at the routine time.
- Children 12 months or older need 2 doses of MMR at least 4 weeks apart.
- If yellow fever vaccine is needed, coordinate administration with a travel medicine clinic since both are live vaccines and must be given on the same day.
- Any person born after 1956 should have 2 doses of MMR at least 4 weeks apart if they have no evidence of immunity.
- Encourage parents to always inform you and your staff of any international travel plans.
Moving forward, remember this increased global activity and the presence of inadequately vaccinated individuals/communities keeps the United States at continued risk for measles outbreaks. The source of the next outbreak may only be one plane ride away.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
This article was updated 6/29/22.
References
1. Patel M et al. MMWR. 2019 Oct 11; 68(40):893-6.
2. Seither R et al. MMWR. 2022 Apr 22;71(16):561-8.
3. Gastañaduy PA et al. J Infect Dis. 2021 Sep 30;224(12 Suppl 2):S420-8. doi: 10.1093/infdis/jiaa793.
4. Centers for Disease Control and Prevention. Measles (Rubeola). http://www.CDC.gov/Measles.
Low butyrylcholinesterase: A possible biomarker of SIDS risk?
Reduced levels of the cholinergic-system enzyme butyrylcholinesterase (BChE) may provide another piece of the puzzle for sudden infant death syndrome (SIDS), preliminary data from Australian researchers suggested.
A small case-control study led by Carmel T. Harrington, PhD,* a sleep medicine expert and honorary research fellow at the Children’s Hospital at Westmead (Australia), found that measurements in 722 dried blood spots taken during neonatal screening 2 or 3 days after birth were lower in babies who subsequently died of SIDS, compared with those of matched surviving controls and other babies who died of non-SIDS causes.
In groups in which cases were reported as SIDS death (n = 26) there was strong evidence that lower BChE-specific activity was associated with death (odds ratio, 0.73 per U/mg; 95% confidence interval, 0.60-0.89, P = .0014). In groups with a non-SIDS death (n = 41), there was no evidence of a linear association between BChE activity and death (OR, 1.001 per U/mg; 95% CI, 0.89-1.13, P = .99). A cohort of 655 age- and sex-matched controls served as a reference group.
Writing online in eBioMedicine, the researchers concluded that a previously unidentified cholinergic deficit, identifiable by abnormal BChE-specific activity, is present at birth in SIDS babies and represents a measurable, specific vulnerability prior to their death. “The finding presents the possibility of identifying infants at future risk for SIDS and it provides a specific avenue for future research into interventions prior to death.”
They hypothesized that the association is evidence of an altered cholinergic homeostasis and claim theirs is the first study to identify a measurable biochemical marker in babies who succumbed to SIDS. The marker “could plausibly produce functional alterations to an infant’s autonomic and arousal responses to an exogenous stressor leaving them vulnerable to sudden death.”
Commenting in a press release, Dr. Harrington said that “babies have a very powerful mechanism to let us know when they are not happy. Usually, if a baby is confronted with a life-threatening situation, such as difficulty breathing during sleep because they are on their tummies, they will arouse and cry out. What this research shows is that some babies don’t have this same robust arousal response.” Despite the sparse data, she believes that BChE is likely involved.
Providing a U.S. perspective on the study but not involved in it, Fern R. Hauck, MD, MS, a professor of family medicine and public health at the University of Virginia, Charlottesville, said that “the media coverage presenting this as the ‘cause of SIDS,’ for which we may find a cure within 5 years, is very disturbing and very misleading. The data are very preliminary and results are based on only 26 SIDS cases.” In addition, the blood samples were more than 2 years old.
This research needs to be repeated in other labs in larger and diverse SIDS populations, she added. “Furthermore, we are not provided any racial-ethnic information about the SIDS cases in this study. In the U.S., the infants who are at greatest risk of dying from SIDS are most commonly African American and Native American/Alaska Native, and thus, these studies would need to be repeated in U.S. populations.”
Dr. Hauck added that, while the differences in blood levels of this enzyme were statistically different, even if this is confirmed by larger studies, there was enough overlap in the blood levels between cases and controls that it could not be used as a blood test at this point with any reasonable predictive value.
As the authors pointed out, she said, the leading theory of SIDS causation is that multiple factors interact. “While everyone would be happy to find one single explanation, it is not so simple. This research does, however, bring into focus the issues of arousal in SIDS and work on biomarkers. The arousal issue is one researchers have been working on for a long time.”
The SIDS research community has long been interested in biomarkers, Dr. Hauck continued. “Dr. Hannah Kinney’s first autoradiography study reported decreased muscarinic cholinergic receptor binding in the arcuate nucleus in SIDS, which the butyrylcholinesterase work further elaborates. More recently, Dr. Kinney reported abnormal cholinergic binding in the mesopontine reticular formation that is related to arousal and REM.”
Moreover, Robin Haynes and colleagues reported in 2017 that differences in serotonin can similarly be found in newborns on a newborn blood test, she said. “Like the butyrylcholinesterase research, there is a lot of work to do before understanding how specifically it can identify risk. The problem with using it prematurely is that it will unnecessarily alarm parents that their baby will die, and, to make it worse, be inaccurate in our warning.”
She also expressed concern that with the focus on a biomarker, parents will forget that SIDS and other sleep-related infant deaths have come down considerably in the United States thanks to greater emphasis on promoting safe infant sleep behaviors.
The research was supported by a crowdfunding campaign and by NSW Health Pathology. The authors disclosed no conflicts of interest. Dr. Hauck disclosed no conflicts of interest.
* This story was corrected on 5/20/2022.
Reduced levels of the cholinergic-system enzyme butyrylcholinesterase (BChE) may provide another piece of the puzzle for sudden infant death syndrome (SIDS), preliminary data from Australian researchers suggested.
A small case-control study led by Carmel T. Harrington, PhD,* a sleep medicine expert and honorary research fellow at the Children’s Hospital at Westmead (Australia), found that measurements in 722 dried blood spots taken during neonatal screening 2 or 3 days after birth were lower in babies who subsequently died of SIDS, compared with those of matched surviving controls and other babies who died of non-SIDS causes.
In groups in which cases were reported as SIDS death (n = 26) there was strong evidence that lower BChE-specific activity was associated with death (odds ratio, 0.73 per U/mg; 95% confidence interval, 0.60-0.89, P = .0014). In groups with a non-SIDS death (n = 41), there was no evidence of a linear association between BChE activity and death (OR, 1.001 per U/mg; 95% CI, 0.89-1.13, P = .99). A cohort of 655 age- and sex-matched controls served as a reference group.
Writing online in eBioMedicine, the researchers concluded that a previously unidentified cholinergic deficit, identifiable by abnormal BChE-specific activity, is present at birth in SIDS babies and represents a measurable, specific vulnerability prior to their death. “The finding presents the possibility of identifying infants at future risk for SIDS and it provides a specific avenue for future research into interventions prior to death.”
They hypothesized that the association is evidence of an altered cholinergic homeostasis and claim theirs is the first study to identify a measurable biochemical marker in babies who succumbed to SIDS. The marker “could plausibly produce functional alterations to an infant’s autonomic and arousal responses to an exogenous stressor leaving them vulnerable to sudden death.”
Commenting in a press release, Dr. Harrington said that “babies have a very powerful mechanism to let us know when they are not happy. Usually, if a baby is confronted with a life-threatening situation, such as difficulty breathing during sleep because they are on their tummies, they will arouse and cry out. What this research shows is that some babies don’t have this same robust arousal response.” Despite the sparse data, she believes that BChE is likely involved.
Providing a U.S. perspective on the study but not involved in it, Fern R. Hauck, MD, MS, a professor of family medicine and public health at the University of Virginia, Charlottesville, said that “the media coverage presenting this as the ‘cause of SIDS,’ for which we may find a cure within 5 years, is very disturbing and very misleading. The data are very preliminary and results are based on only 26 SIDS cases.” In addition, the blood samples were more than 2 years old.
This research needs to be repeated in other labs in larger and diverse SIDS populations, she added. “Furthermore, we are not provided any racial-ethnic information about the SIDS cases in this study. In the U.S., the infants who are at greatest risk of dying from SIDS are most commonly African American and Native American/Alaska Native, and thus, these studies would need to be repeated in U.S. populations.”
Dr. Hauck added that, while the differences in blood levels of this enzyme were statistically different, even if this is confirmed by larger studies, there was enough overlap in the blood levels between cases and controls that it could not be used as a blood test at this point with any reasonable predictive value.
As the authors pointed out, she said, the leading theory of SIDS causation is that multiple factors interact. “While everyone would be happy to find one single explanation, it is not so simple. This research does, however, bring into focus the issues of arousal in SIDS and work on biomarkers. The arousal issue is one researchers have been working on for a long time.”
The SIDS research community has long been interested in biomarkers, Dr. Hauck continued. “Dr. Hannah Kinney’s first autoradiography study reported decreased muscarinic cholinergic receptor binding in the arcuate nucleus in SIDS, which the butyrylcholinesterase work further elaborates. More recently, Dr. Kinney reported abnormal cholinergic binding in the mesopontine reticular formation that is related to arousal and REM.”
Moreover, Robin Haynes and colleagues reported in 2017 that differences in serotonin can similarly be found in newborns on a newborn blood test, she said. “Like the butyrylcholinesterase research, there is a lot of work to do before understanding how specifically it can identify risk. The problem with using it prematurely is that it will unnecessarily alarm parents that their baby will die, and, to make it worse, be inaccurate in our warning.”
She also expressed concern that with the focus on a biomarker, parents will forget that SIDS and other sleep-related infant deaths have come down considerably in the United States thanks to greater emphasis on promoting safe infant sleep behaviors.
The research was supported by a crowdfunding campaign and by NSW Health Pathology. The authors disclosed no conflicts of interest. Dr. Hauck disclosed no conflicts of interest.
* This story was corrected on 5/20/2022.
Reduced levels of the cholinergic-system enzyme butyrylcholinesterase (BChE) may provide another piece of the puzzle for sudden infant death syndrome (SIDS), preliminary data from Australian researchers suggested.
A small case-control study led by Carmel T. Harrington, PhD,* a sleep medicine expert and honorary research fellow at the Children’s Hospital at Westmead (Australia), found that measurements in 722 dried blood spots taken during neonatal screening 2 or 3 days after birth were lower in babies who subsequently died of SIDS, compared with those of matched surviving controls and other babies who died of non-SIDS causes.
In groups in which cases were reported as SIDS death (n = 26) there was strong evidence that lower BChE-specific activity was associated with death (odds ratio, 0.73 per U/mg; 95% confidence interval, 0.60-0.89, P = .0014). In groups with a non-SIDS death (n = 41), there was no evidence of a linear association between BChE activity and death (OR, 1.001 per U/mg; 95% CI, 0.89-1.13, P = .99). A cohort of 655 age- and sex-matched controls served as a reference group.
Writing online in eBioMedicine, the researchers concluded that a previously unidentified cholinergic deficit, identifiable by abnormal BChE-specific activity, is present at birth in SIDS babies and represents a measurable, specific vulnerability prior to their death. “The finding presents the possibility of identifying infants at future risk for SIDS and it provides a specific avenue for future research into interventions prior to death.”
They hypothesized that the association is evidence of an altered cholinergic homeostasis and claim theirs is the first study to identify a measurable biochemical marker in babies who succumbed to SIDS. The marker “could plausibly produce functional alterations to an infant’s autonomic and arousal responses to an exogenous stressor leaving them vulnerable to sudden death.”
Commenting in a press release, Dr. Harrington said that “babies have a very powerful mechanism to let us know when they are not happy. Usually, if a baby is confronted with a life-threatening situation, such as difficulty breathing during sleep because they are on their tummies, they will arouse and cry out. What this research shows is that some babies don’t have this same robust arousal response.” Despite the sparse data, she believes that BChE is likely involved.
Providing a U.S. perspective on the study but not involved in it, Fern R. Hauck, MD, MS, a professor of family medicine and public health at the University of Virginia, Charlottesville, said that “the media coverage presenting this as the ‘cause of SIDS,’ for which we may find a cure within 5 years, is very disturbing and very misleading. The data are very preliminary and results are based on only 26 SIDS cases.” In addition, the blood samples were more than 2 years old.
This research needs to be repeated in other labs in larger and diverse SIDS populations, she added. “Furthermore, we are not provided any racial-ethnic information about the SIDS cases in this study. In the U.S., the infants who are at greatest risk of dying from SIDS are most commonly African American and Native American/Alaska Native, and thus, these studies would need to be repeated in U.S. populations.”
Dr. Hauck added that, while the differences in blood levels of this enzyme were statistically different, even if this is confirmed by larger studies, there was enough overlap in the blood levels between cases and controls that it could not be used as a blood test at this point with any reasonable predictive value.
As the authors pointed out, she said, the leading theory of SIDS causation is that multiple factors interact. “While everyone would be happy to find one single explanation, it is not so simple. This research does, however, bring into focus the issues of arousal in SIDS and work on biomarkers. The arousal issue is one researchers have been working on for a long time.”
The SIDS research community has long been interested in biomarkers, Dr. Hauck continued. “Dr. Hannah Kinney’s first autoradiography study reported decreased muscarinic cholinergic receptor binding in the arcuate nucleus in SIDS, which the butyrylcholinesterase work further elaborates. More recently, Dr. Kinney reported abnormal cholinergic binding in the mesopontine reticular formation that is related to arousal and REM.”
Moreover, Robin Haynes and colleagues reported in 2017 that differences in serotonin can similarly be found in newborns on a newborn blood test, she said. “Like the butyrylcholinesterase research, there is a lot of work to do before understanding how specifically it can identify risk. The problem with using it prematurely is that it will unnecessarily alarm parents that their baby will die, and, to make it worse, be inaccurate in our warning.”
She also expressed concern that with the focus on a biomarker, parents will forget that SIDS and other sleep-related infant deaths have come down considerably in the United States thanks to greater emphasis on promoting safe infant sleep behaviors.
The research was supported by a crowdfunding campaign and by NSW Health Pathology. The authors disclosed no conflicts of interest. Dr. Hauck disclosed no conflicts of interest.
* This story was corrected on 5/20/2022.
FROM EBIOMEDICINE
Myositis guidelines aim to standardize adult and pediatric care
All patients with idiopathic inflammatory myopathies (IIM) should be screened for swallowing difficulties, according to the first evidence-based guideline to be produced.
The guideline, which has been developed by a working group of the British Society for Rheumatology (BSR), also advises that all diagnosed patients should have their myositis antibody levels checked and have their overall well-being assessed. Other recommendations for all patients include the use of glucocorticoids to reduce muscle inflammation and conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) for long-term treatment.
“Finally, now, we’re able to standardize the way we treat adults and children with IIM,” senior guideline author Hector Chinoy, PhD, said at the society’s annual meeting.
It has been a long labor of love, however, taking 4 years to get the guideline published, said Dr. Chinoy, professor of rheumatology and neuromuscular disease at the University of Manchester (England), and a consultant at Salford (England) Royal Hospital.
“We’re not covering diagnosis, classification, or the investigation of suspected IIM,” said Dr. Chinoy. Inclusion body myositis also is not included.
Altogether, there are 13 recommendations that have been developed using a PICO (patient or population, intervention, comparison, outcome) format, graded based on the quality of the available evidence, and then voted on by the working group members to give a score of the strength of agreement. Dr. Chinoy noted that there was a checklist included in the Supplementary Data section of the guideline to help follow the recommendations.
“The target audience for the guideline reflects the variety of clinicians caring for patients with IIM,” Dr. Chinoy said. So that is not just pediatric and adult rheumatologists, but also neurologists, dermatologists, respiratory physicians, oncologists, gastroenterologists, cardiologists, and of course other health care professionals. This includes rheumatology and neurology nurses, psychologists, speech and language therapists, and podiatrists, as well as rheumatology specialist pharmacists, physiotherapists, and occupational therapists.
With reference to the latter, Liza McCann, MBBS, who co-led the development of the guideline, said in a statement released by the BSR that the guideline “highlights the importance of exercise, led and monitored by specialist physiotherapists and occupational therapists.”
Dr. McCann, a consultant pediatric rheumatologist at Alder Hey Hospital, Liverpool, England, and Honorary Clinical Lecturer at the University of Liverpool, added that the guidelines also cover “the need to address psychological wellbeing as an integral part of treatment, in parallel with pharmacological therapies.”
Recommendation highlights
Some of the highlights of the recommendations include the use of high-dose glucocorticoids to manage skeletal muscle inflammation at the time of treatment induction, with specific guidance on the different doses to use in adults and in children. There also is guidance on the use of csDMARDs in both populations and what to use if there is refractory disease – with the strongest evidence supporting the use of intravenous immunoglobulin (IVIG) or cyclophosphamide, and possibly rituximab and abatacept.
“There is insufficient evidence to recommend JAK inhibition,” Dr. Chinoy said. The data search used to develop the guideline had a cutoff of October 2020, but even now there is only anecdotal evidence from case studies, he added.
Importantly, the guidelines recognize that childhood IIM differs from adult disease and call for children to be managed by pediatric specialists.
“Routine assessment of dysphagia should be considered in all patients,” Dr. Chinoy said, “so ask the question.” The recommendation is that a swallowing assessment should involve a speech and language therapist or gastroenterologist, and that IVIG be considered for active disease and dysphagia that is resistant to other treatments.
There also are recommendations to screen adult patients for interstitial lung disease, consider fracture risk, and screen adult patients for cancer if they have specific risk factors that include older age at onset, male gender, dysphagia, and rapid disease onset, among others.
Separate cancer screening guidelines on cards
“Around one in four patients with myositis will develop cancer within the 3 years either before or after myositis onset,” Alexander Oldroyd, MBChB, PhD, said in a separate presentation at the BSR annual meeting.
“It’s a hugely increased risk compared to the general population, and a great worry for patients,” he added. Exactly why there is an increased risk is not known, but “there’s a big link between the biological onset of cancer and myositis.”
Dr. Oldroyd, who is an NIHR Academic Clinical Lecturer at the University of Manchester in England and a coauthor of the BSR myositis guideline, is part of a special interest group set up by the International Myositis Assessment and Clinical Studies Group (IMACS) that is in the process of developing separate guidelines for cancer screening in people newly diagnosed with IIM.
The aim was to produce evidence-based recommendations that were both “pragmatic and practical,” that could help clinicians answer patient’s questions on their risk and how best and how often to screen them, Dr. Oldroyd explained. Importantly, IMACS has endeavored to create recommendations that should be applicable across different countries and health care systems.
“We had to acknowledge that there’s not a lot of evidence base there,” Dr. Oldroyd said, noting that he and colleagues conducted a systematic literature review and meta-analysis and used a Delphi process to draft 20 recommendations. These cover identifying risk factors for cancer in people with myositis and categorizing people into low, medium, and high-risk categories. The recommendations also cover what should constitute basic and enhanced screening, and how often someone should be screened.
Moreover, the authors make recommendations on the use of imaging modalities such as PET and CT scans, as well as upper and lower gastrointestinal endoscopy and naso-endoscopy.
“As rheumatologists, we don’t talk about cancer a lot,” Dr. Oldroyd said. “We pick up a lot of incidental cancers, but we don’t usually talk about cancer screening with patients.” That’s something that needs to change, he said.
“It’s important – just get it out in the open, talk to people about it,” Dr. Oldroyd said.
“Tell them what you’re wanting to do, how you’re wanting to investigate for it, clearly communicate their risk,” he said. “But also acknowledge the limited evidence as well, and clearly communicate the results.”
Dr. Chinoy acknowledged he had received fees for presentations (UCB, Biogen), consultancy (Alexion, Novartis, Eli Lilly, Orphazyme, AstraZeneca), or grant support (Eli Lilly, UCB) that had been paid via his institution for the purpose of furthering myositis research. Dr. Oldroyd had no conflicts of interest to disclose.
All patients with idiopathic inflammatory myopathies (IIM) should be screened for swallowing difficulties, according to the first evidence-based guideline to be produced.
The guideline, which has been developed by a working group of the British Society for Rheumatology (BSR), also advises that all diagnosed patients should have their myositis antibody levels checked and have their overall well-being assessed. Other recommendations for all patients include the use of glucocorticoids to reduce muscle inflammation and conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) for long-term treatment.
“Finally, now, we’re able to standardize the way we treat adults and children with IIM,” senior guideline author Hector Chinoy, PhD, said at the society’s annual meeting.
It has been a long labor of love, however, taking 4 years to get the guideline published, said Dr. Chinoy, professor of rheumatology and neuromuscular disease at the University of Manchester (England), and a consultant at Salford (England) Royal Hospital.
“We’re not covering diagnosis, classification, or the investigation of suspected IIM,” said Dr. Chinoy. Inclusion body myositis also is not included.
Altogether, there are 13 recommendations that have been developed using a PICO (patient or population, intervention, comparison, outcome) format, graded based on the quality of the available evidence, and then voted on by the working group members to give a score of the strength of agreement. Dr. Chinoy noted that there was a checklist included in the Supplementary Data section of the guideline to help follow the recommendations.
“The target audience for the guideline reflects the variety of clinicians caring for patients with IIM,” Dr. Chinoy said. So that is not just pediatric and adult rheumatologists, but also neurologists, dermatologists, respiratory physicians, oncologists, gastroenterologists, cardiologists, and of course other health care professionals. This includes rheumatology and neurology nurses, psychologists, speech and language therapists, and podiatrists, as well as rheumatology specialist pharmacists, physiotherapists, and occupational therapists.
With reference to the latter, Liza McCann, MBBS, who co-led the development of the guideline, said in a statement released by the BSR that the guideline “highlights the importance of exercise, led and monitored by specialist physiotherapists and occupational therapists.”
Dr. McCann, a consultant pediatric rheumatologist at Alder Hey Hospital, Liverpool, England, and Honorary Clinical Lecturer at the University of Liverpool, added that the guidelines also cover “the need to address psychological wellbeing as an integral part of treatment, in parallel with pharmacological therapies.”
Recommendation highlights
Some of the highlights of the recommendations include the use of high-dose glucocorticoids to manage skeletal muscle inflammation at the time of treatment induction, with specific guidance on the different doses to use in adults and in children. There also is guidance on the use of csDMARDs in both populations and what to use if there is refractory disease – with the strongest evidence supporting the use of intravenous immunoglobulin (IVIG) or cyclophosphamide, and possibly rituximab and abatacept.
“There is insufficient evidence to recommend JAK inhibition,” Dr. Chinoy said. The data search used to develop the guideline had a cutoff of October 2020, but even now there is only anecdotal evidence from case studies, he added.
Importantly, the guidelines recognize that childhood IIM differs from adult disease and call for children to be managed by pediatric specialists.
“Routine assessment of dysphagia should be considered in all patients,” Dr. Chinoy said, “so ask the question.” The recommendation is that a swallowing assessment should involve a speech and language therapist or gastroenterologist, and that IVIG be considered for active disease and dysphagia that is resistant to other treatments.
There also are recommendations to screen adult patients for interstitial lung disease, consider fracture risk, and screen adult patients for cancer if they have specific risk factors that include older age at onset, male gender, dysphagia, and rapid disease onset, among others.
Separate cancer screening guidelines on cards
“Around one in four patients with myositis will develop cancer within the 3 years either before or after myositis onset,” Alexander Oldroyd, MBChB, PhD, said in a separate presentation at the BSR annual meeting.
“It’s a hugely increased risk compared to the general population, and a great worry for patients,” he added. Exactly why there is an increased risk is not known, but “there’s a big link between the biological onset of cancer and myositis.”
Dr. Oldroyd, who is an NIHR Academic Clinical Lecturer at the University of Manchester in England and a coauthor of the BSR myositis guideline, is part of a special interest group set up by the International Myositis Assessment and Clinical Studies Group (IMACS) that is in the process of developing separate guidelines for cancer screening in people newly diagnosed with IIM.
The aim was to produce evidence-based recommendations that were both “pragmatic and practical,” that could help clinicians answer patient’s questions on their risk and how best and how often to screen them, Dr. Oldroyd explained. Importantly, IMACS has endeavored to create recommendations that should be applicable across different countries and health care systems.
“We had to acknowledge that there’s not a lot of evidence base there,” Dr. Oldroyd said, noting that he and colleagues conducted a systematic literature review and meta-analysis and used a Delphi process to draft 20 recommendations. These cover identifying risk factors for cancer in people with myositis and categorizing people into low, medium, and high-risk categories. The recommendations also cover what should constitute basic and enhanced screening, and how often someone should be screened.
Moreover, the authors make recommendations on the use of imaging modalities such as PET and CT scans, as well as upper and lower gastrointestinal endoscopy and naso-endoscopy.
“As rheumatologists, we don’t talk about cancer a lot,” Dr. Oldroyd said. “We pick up a lot of incidental cancers, but we don’t usually talk about cancer screening with patients.” That’s something that needs to change, he said.
“It’s important – just get it out in the open, talk to people about it,” Dr. Oldroyd said.
“Tell them what you’re wanting to do, how you’re wanting to investigate for it, clearly communicate their risk,” he said. “But also acknowledge the limited evidence as well, and clearly communicate the results.”
Dr. Chinoy acknowledged he had received fees for presentations (UCB, Biogen), consultancy (Alexion, Novartis, Eli Lilly, Orphazyme, AstraZeneca), or grant support (Eli Lilly, UCB) that had been paid via his institution for the purpose of furthering myositis research. Dr. Oldroyd had no conflicts of interest to disclose.
All patients with idiopathic inflammatory myopathies (IIM) should be screened for swallowing difficulties, according to the first evidence-based guideline to be produced.
The guideline, which has been developed by a working group of the British Society for Rheumatology (BSR), also advises that all diagnosed patients should have their myositis antibody levels checked and have their overall well-being assessed. Other recommendations for all patients include the use of glucocorticoids to reduce muscle inflammation and conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) for long-term treatment.
“Finally, now, we’re able to standardize the way we treat adults and children with IIM,” senior guideline author Hector Chinoy, PhD, said at the society’s annual meeting.
It has been a long labor of love, however, taking 4 years to get the guideline published, said Dr. Chinoy, professor of rheumatology and neuromuscular disease at the University of Manchester (England), and a consultant at Salford (England) Royal Hospital.
“We’re not covering diagnosis, classification, or the investigation of suspected IIM,” said Dr. Chinoy. Inclusion body myositis also is not included.
Altogether, there are 13 recommendations that have been developed using a PICO (patient or population, intervention, comparison, outcome) format, graded based on the quality of the available evidence, and then voted on by the working group members to give a score of the strength of agreement. Dr. Chinoy noted that there was a checklist included in the Supplementary Data section of the guideline to help follow the recommendations.
“The target audience for the guideline reflects the variety of clinicians caring for patients with IIM,” Dr. Chinoy said. So that is not just pediatric and adult rheumatologists, but also neurologists, dermatologists, respiratory physicians, oncologists, gastroenterologists, cardiologists, and of course other health care professionals. This includes rheumatology and neurology nurses, psychologists, speech and language therapists, and podiatrists, as well as rheumatology specialist pharmacists, physiotherapists, and occupational therapists.
With reference to the latter, Liza McCann, MBBS, who co-led the development of the guideline, said in a statement released by the BSR that the guideline “highlights the importance of exercise, led and monitored by specialist physiotherapists and occupational therapists.”
Dr. McCann, a consultant pediatric rheumatologist at Alder Hey Hospital, Liverpool, England, and Honorary Clinical Lecturer at the University of Liverpool, added that the guidelines also cover “the need to address psychological wellbeing as an integral part of treatment, in parallel with pharmacological therapies.”
Recommendation highlights
Some of the highlights of the recommendations include the use of high-dose glucocorticoids to manage skeletal muscle inflammation at the time of treatment induction, with specific guidance on the different doses to use in adults and in children. There also is guidance on the use of csDMARDs in both populations and what to use if there is refractory disease – with the strongest evidence supporting the use of intravenous immunoglobulin (IVIG) or cyclophosphamide, and possibly rituximab and abatacept.
“There is insufficient evidence to recommend JAK inhibition,” Dr. Chinoy said. The data search used to develop the guideline had a cutoff of October 2020, but even now there is only anecdotal evidence from case studies, he added.
Importantly, the guidelines recognize that childhood IIM differs from adult disease and call for children to be managed by pediatric specialists.
“Routine assessment of dysphagia should be considered in all patients,” Dr. Chinoy said, “so ask the question.” The recommendation is that a swallowing assessment should involve a speech and language therapist or gastroenterologist, and that IVIG be considered for active disease and dysphagia that is resistant to other treatments.
There also are recommendations to screen adult patients for interstitial lung disease, consider fracture risk, and screen adult patients for cancer if they have specific risk factors that include older age at onset, male gender, dysphagia, and rapid disease onset, among others.
Separate cancer screening guidelines on cards
“Around one in four patients with myositis will develop cancer within the 3 years either before or after myositis onset,” Alexander Oldroyd, MBChB, PhD, said in a separate presentation at the BSR annual meeting.
“It’s a hugely increased risk compared to the general population, and a great worry for patients,” he added. Exactly why there is an increased risk is not known, but “there’s a big link between the biological onset of cancer and myositis.”
Dr. Oldroyd, who is an NIHR Academic Clinical Lecturer at the University of Manchester in England and a coauthor of the BSR myositis guideline, is part of a special interest group set up by the International Myositis Assessment and Clinical Studies Group (IMACS) that is in the process of developing separate guidelines for cancer screening in people newly diagnosed with IIM.
The aim was to produce evidence-based recommendations that were both “pragmatic and practical,” that could help clinicians answer patient’s questions on their risk and how best and how often to screen them, Dr. Oldroyd explained. Importantly, IMACS has endeavored to create recommendations that should be applicable across different countries and health care systems.
“We had to acknowledge that there’s not a lot of evidence base there,” Dr. Oldroyd said, noting that he and colleagues conducted a systematic literature review and meta-analysis and used a Delphi process to draft 20 recommendations. These cover identifying risk factors for cancer in people with myositis and categorizing people into low, medium, and high-risk categories. The recommendations also cover what should constitute basic and enhanced screening, and how often someone should be screened.
Moreover, the authors make recommendations on the use of imaging modalities such as PET and CT scans, as well as upper and lower gastrointestinal endoscopy and naso-endoscopy.
“As rheumatologists, we don’t talk about cancer a lot,” Dr. Oldroyd said. “We pick up a lot of incidental cancers, but we don’t usually talk about cancer screening with patients.” That’s something that needs to change, he said.
“It’s important – just get it out in the open, talk to people about it,” Dr. Oldroyd said.
“Tell them what you’re wanting to do, how you’re wanting to investigate for it, clearly communicate their risk,” he said. “But also acknowledge the limited evidence as well, and clearly communicate the results.”
Dr. Chinoy acknowledged he had received fees for presentations (UCB, Biogen), consultancy (Alexion, Novartis, Eli Lilly, Orphazyme, AstraZeneca), or grant support (Eli Lilly, UCB) that had been paid via his institution for the purpose of furthering myositis research. Dr. Oldroyd had no conflicts of interest to disclose.
FROM BSR 2022







