User login
FDA approves fidaxomicin for treatment of C. difficile–associated diarrhea
The Food and Drug Administration has approved fidaxomicin (Dificid) for the treatment of Clostridioides difficile–associated diarrhea in children aged 6 months and older.
Approval was based on results from SUNSHINE, a phase 3, multicenter, investigator-blind, randomized, parallel-group study in 142 pediatric patients aged between 6 months and 18 years with confirmed C. difficile infection who received either fidaxomicin or vancomycin for 10 days. Clinical response 2 days after the conclusion of treatment was similar in both groups (77.6% for fidaxomicin vs. 70.5% for vancomycin), and fidaxomicin had a superior sustained response 30 days after the conclusion of treatment (68.4% vs. 50.0%).
The safety of fidaxomicin was assessed in a pair of clinical trials involving 136 patients; the most common adverse events were pyrexia, abdominal pain, vomiting, diarrhea, constipation, increased aminotransferases, and rash. Four patients discontinued fidaxomicin treatment because of adverse events, and four patients died during the trials, though all deaths were in patients aged younger than 2 years and seemed to be related to other comorbidities.
“C. difficile is an important cause of health care– and community-associated diarrheal illness in children, and sustained cure is difficult to achieve in some patients. The fidaxomicin pediatric trial was the first randomized, controlled trial of C. difficile infection treatment in children,” Larry K. Kociolek, MD, associate medical director of infection prevention and control at Ann & Robert H. Lurie Children’s Hospital of Chicago, said in the press release from Merck, manufacturer of fidaxomicin.
*This story was updated on 1/27/2020.
The Food and Drug Administration has approved fidaxomicin (Dificid) for the treatment of Clostridioides difficile–associated diarrhea in children aged 6 months and older.
Approval was based on results from SUNSHINE, a phase 3, multicenter, investigator-blind, randomized, parallel-group study in 142 pediatric patients aged between 6 months and 18 years with confirmed C. difficile infection who received either fidaxomicin or vancomycin for 10 days. Clinical response 2 days after the conclusion of treatment was similar in both groups (77.6% for fidaxomicin vs. 70.5% for vancomycin), and fidaxomicin had a superior sustained response 30 days after the conclusion of treatment (68.4% vs. 50.0%).
The safety of fidaxomicin was assessed in a pair of clinical trials involving 136 patients; the most common adverse events were pyrexia, abdominal pain, vomiting, diarrhea, constipation, increased aminotransferases, and rash. Four patients discontinued fidaxomicin treatment because of adverse events, and four patients died during the trials, though all deaths were in patients aged younger than 2 years and seemed to be related to other comorbidities.
“C. difficile is an important cause of health care– and community-associated diarrheal illness in children, and sustained cure is difficult to achieve in some patients. The fidaxomicin pediatric trial was the first randomized, controlled trial of C. difficile infection treatment in children,” Larry K. Kociolek, MD, associate medical director of infection prevention and control at Ann & Robert H. Lurie Children’s Hospital of Chicago, said in the press release from Merck, manufacturer of fidaxomicin.
*This story was updated on 1/27/2020.
The Food and Drug Administration has approved fidaxomicin (Dificid) for the treatment of Clostridioides difficile–associated diarrhea in children aged 6 months and older.
Approval was based on results from SUNSHINE, a phase 3, multicenter, investigator-blind, randomized, parallel-group study in 142 pediatric patients aged between 6 months and 18 years with confirmed C. difficile infection who received either fidaxomicin or vancomycin for 10 days. Clinical response 2 days after the conclusion of treatment was similar in both groups (77.6% for fidaxomicin vs. 70.5% for vancomycin), and fidaxomicin had a superior sustained response 30 days after the conclusion of treatment (68.4% vs. 50.0%).
The safety of fidaxomicin was assessed in a pair of clinical trials involving 136 patients; the most common adverse events were pyrexia, abdominal pain, vomiting, diarrhea, constipation, increased aminotransferases, and rash. Four patients discontinued fidaxomicin treatment because of adverse events, and four patients died during the trials, though all deaths were in patients aged younger than 2 years and seemed to be related to other comorbidities.
“C. difficile is an important cause of health care– and community-associated diarrheal illness in children, and sustained cure is difficult to achieve in some patients. The fidaxomicin pediatric trial was the first randomized, controlled trial of C. difficile infection treatment in children,” Larry K. Kociolek, MD, associate medical director of infection prevention and control at Ann & Robert H. Lurie Children’s Hospital of Chicago, said in the press release from Merck, manufacturer of fidaxomicin.
*This story was updated on 1/27/2020.
Zika virus: Birth defects rose fourfold in U.S. hardest-hit areas
according to the Centers for Disease Control and Prevention.

That spike in the prevalence of brain abnormalities and/or microcephaly or eye abnormalities without brain abnormalities came during January through March 2017, about 6 months after the Zika outbreak’s reported peak in the jurisdictions with widespread local transmission, Puerto Rico and the U.S. Virgin Islands, wrote Ashley N. Smoots, MPH, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates in the Morbidity and Mortality Weekly Report.
In those two territories, the prevalence of birth defects potentially related to Zika virus infection was 5.6 per 1,000 live births during January through March 2017, compared with 1.3 per 1,000 in January through March 2016, they reported.
In the southern areas of Florida and Texas, where there was limited local Zika transmission, the highest prevalence of birth defects, 2.7 per 1,000, occurred during October through December 2016, and was only slightly greater than the baseline rate of 2.2 per 1,000 in January through March 2016, the investigators reported.
Among the other 19 jurisdictions (including Illinois, Louisiana, New Jersey, South Carolina, and Virginia) involved in the analysis, the rate of Zika virus–related birth defects never reached any higher than the 1.7 per 1,000 recorded at the start of the study period in January through March 2016, they said.
“Population-based birth defects surveillance is critical for identifying infants and fetuses with birth defects potentially related to Zika virus regardless of whether Zika virus testing was conducted, especially given the high prevalence of asymptomatic disease. These data can be used to inform follow-up care and services as well as strengthen surveillance,” the investigators wrote.
SOURCE: Smoots AN et al. MMWR. 2020 Jan 24;69(3):67-71.
according to the Centers for Disease Control and Prevention.

That spike in the prevalence of brain abnormalities and/or microcephaly or eye abnormalities without brain abnormalities came during January through March 2017, about 6 months after the Zika outbreak’s reported peak in the jurisdictions with widespread local transmission, Puerto Rico and the U.S. Virgin Islands, wrote Ashley N. Smoots, MPH, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates in the Morbidity and Mortality Weekly Report.
In those two territories, the prevalence of birth defects potentially related to Zika virus infection was 5.6 per 1,000 live births during January through March 2017, compared with 1.3 per 1,000 in January through March 2016, they reported.
In the southern areas of Florida and Texas, where there was limited local Zika transmission, the highest prevalence of birth defects, 2.7 per 1,000, occurred during October through December 2016, and was only slightly greater than the baseline rate of 2.2 per 1,000 in January through March 2016, the investigators reported.
Among the other 19 jurisdictions (including Illinois, Louisiana, New Jersey, South Carolina, and Virginia) involved in the analysis, the rate of Zika virus–related birth defects never reached any higher than the 1.7 per 1,000 recorded at the start of the study period in January through March 2016, they said.
“Population-based birth defects surveillance is critical for identifying infants and fetuses with birth defects potentially related to Zika virus regardless of whether Zika virus testing was conducted, especially given the high prevalence of asymptomatic disease. These data can be used to inform follow-up care and services as well as strengthen surveillance,” the investigators wrote.
SOURCE: Smoots AN et al. MMWR. 2020 Jan 24;69(3):67-71.
according to the Centers for Disease Control and Prevention.

That spike in the prevalence of brain abnormalities and/or microcephaly or eye abnormalities without brain abnormalities came during January through March 2017, about 6 months after the Zika outbreak’s reported peak in the jurisdictions with widespread local transmission, Puerto Rico and the U.S. Virgin Islands, wrote Ashley N. Smoots, MPH, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates in the Morbidity and Mortality Weekly Report.
In those two territories, the prevalence of birth defects potentially related to Zika virus infection was 5.6 per 1,000 live births during January through March 2017, compared with 1.3 per 1,000 in January through March 2016, they reported.
In the southern areas of Florida and Texas, where there was limited local Zika transmission, the highest prevalence of birth defects, 2.7 per 1,000, occurred during October through December 2016, and was only slightly greater than the baseline rate of 2.2 per 1,000 in January through March 2016, the investigators reported.
Among the other 19 jurisdictions (including Illinois, Louisiana, New Jersey, South Carolina, and Virginia) involved in the analysis, the rate of Zika virus–related birth defects never reached any higher than the 1.7 per 1,000 recorded at the start of the study period in January through March 2016, they said.
“Population-based birth defects surveillance is critical for identifying infants and fetuses with birth defects potentially related to Zika virus regardless of whether Zika virus testing was conducted, especially given the high prevalence of asymptomatic disease. These data can be used to inform follow-up care and services as well as strengthen surveillance,” the investigators wrote.
SOURCE: Smoots AN et al. MMWR. 2020 Jan 24;69(3):67-71.
FROM MMWR
Core behaviors enhance communication about neonatal death
Clinicians can improve communications with parents during neonatal end-of-life situations by adopting key behaviors such as sitting down to talk to parents and using the infant’s name, according to data from a simulation study.
“Empirical evidence regarding communication with parents during and after a child’s critical instability or death is scarce,” wrote Marie-Hélène Lizotte, MD, of Centre Hospitalier Universitaire Sainte-Justine, Montréal, and colleagues. Noting that realistic simulation has been shown to help clinicians improve their communication skills, the investigators recruited clinicians to participate in a simulated unsuccessful neonatal resuscitation to identify behaviors associated with optimal parent communication.
Behaviors associated with high scores for clinicians deemed “good communicators” included introducing themselves to parents, using the infant’s name (if known), sitting down to speak to parents, not leaving the infant alone on the bed after death, and allowing time for silence, the researchers reported in Pediatrics.
The investigators presented the video simulations to evaluators, including clinicians and bereaved parents. In the simulation, a term infant was born after an emergency cesarean delivery for fetal distress and died after an unsuccessful attempt at resuscitation. A manikin infant was programmed to remain pulseless, and two actors played the roles of the parents in the video.
Evaluators scored the videos for overall performance and for communication with the parent actors during and after the resuscitation.
Overall, parent evaluators and parent actors agreed with clinicians on what actions exemplified optimal communication in about 81% of evaluations. Discrepancies were mainly related to the language participants used related to death, as some parent evaluators said they had trouble understanding certain sentences or found them insensitive, such as “her heart never came back” and “allowing natural death.”
A total of 31 participants were recruited for the simulation, including 15 pediatric residents, 5 neonatal fellows, 3 neonatologists, 3 neonatal nurse practitioners, and 5 transport and resuscitation team providers. Videos of the simulations were examined by 21 evaluators, including bereaved parents, the parent actors, a neonatologist, a maternal-fetal medicine specialist, a psychologist, and a respiratory therapist. There were 651 evaluations.
The study findings were limited by several factors including the use of a single center, use of videos for evaluations, and the use of a single infant-resuscitation scenario, the researchers noted. The results were strengthened, however, by the large number of evaluations, and they support the core behaviors as “a skeleton on which to build additional skills with practice and training” with attention to cultural differences in their application, such as recognizing that infants are not named until after birth in some cultures, they said.
The existing literature on strategies for providing empathy and support to parents facing the death of a child is limited, but this simulation study provides a design model to help address this issue, Chris Feudtner, MD, of the Children’s Hospital of Philadelphia wrote in an accompanying editorial. “Overall, this study, in terms of design and methodologic rigor, is a great advance toward answering our key question: how to best support parents in such circumstances,” he said.
Dr. Feudtner said that he would divide the clinician behaviors into two groups. The first, “Calm kind politeness,” includes acknowledging the parents, introducing themselves, using the infant’s name, and remaining calm. The second set of behaviors, which he called “Skillful situational leadership,” includes preparing parents for the resuscitation activities and providing verbal milestones that prepared them for the fatal outcome.
“Picking up on a metaphor offered by the authors of the study, training and repetitive drills on these specific behaviors cannot be emphasized enough because they are not only the skeleton of excellent communication; they are likely also the muscles, the heart, and even the soul,” he concluded.
The study was supported by a grant from the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and Dr. Feudtner reported no financial conflicts.
SOURCE: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
Clinicians can improve communications with parents during neonatal end-of-life situations by adopting key behaviors such as sitting down to talk to parents and using the infant’s name, according to data from a simulation study.
“Empirical evidence regarding communication with parents during and after a child’s critical instability or death is scarce,” wrote Marie-Hélène Lizotte, MD, of Centre Hospitalier Universitaire Sainte-Justine, Montréal, and colleagues. Noting that realistic simulation has been shown to help clinicians improve their communication skills, the investigators recruited clinicians to participate in a simulated unsuccessful neonatal resuscitation to identify behaviors associated with optimal parent communication.
Behaviors associated with high scores for clinicians deemed “good communicators” included introducing themselves to parents, using the infant’s name (if known), sitting down to speak to parents, not leaving the infant alone on the bed after death, and allowing time for silence, the researchers reported in Pediatrics.
The investigators presented the video simulations to evaluators, including clinicians and bereaved parents. In the simulation, a term infant was born after an emergency cesarean delivery for fetal distress and died after an unsuccessful attempt at resuscitation. A manikin infant was programmed to remain pulseless, and two actors played the roles of the parents in the video.
Evaluators scored the videos for overall performance and for communication with the parent actors during and after the resuscitation.
Overall, parent evaluators and parent actors agreed with clinicians on what actions exemplified optimal communication in about 81% of evaluations. Discrepancies were mainly related to the language participants used related to death, as some parent evaluators said they had trouble understanding certain sentences or found them insensitive, such as “her heart never came back” and “allowing natural death.”
A total of 31 participants were recruited for the simulation, including 15 pediatric residents, 5 neonatal fellows, 3 neonatologists, 3 neonatal nurse practitioners, and 5 transport and resuscitation team providers. Videos of the simulations were examined by 21 evaluators, including bereaved parents, the parent actors, a neonatologist, a maternal-fetal medicine specialist, a psychologist, and a respiratory therapist. There were 651 evaluations.
The study findings were limited by several factors including the use of a single center, use of videos for evaluations, and the use of a single infant-resuscitation scenario, the researchers noted. The results were strengthened, however, by the large number of evaluations, and they support the core behaviors as “a skeleton on which to build additional skills with practice and training” with attention to cultural differences in their application, such as recognizing that infants are not named until after birth in some cultures, they said.
The existing literature on strategies for providing empathy and support to parents facing the death of a child is limited, but this simulation study provides a design model to help address this issue, Chris Feudtner, MD, of the Children’s Hospital of Philadelphia wrote in an accompanying editorial. “Overall, this study, in terms of design and methodologic rigor, is a great advance toward answering our key question: how to best support parents in such circumstances,” he said.
Dr. Feudtner said that he would divide the clinician behaviors into two groups. The first, “Calm kind politeness,” includes acknowledging the parents, introducing themselves, using the infant’s name, and remaining calm. The second set of behaviors, which he called “Skillful situational leadership,” includes preparing parents for the resuscitation activities and providing verbal milestones that prepared them for the fatal outcome.
“Picking up on a metaphor offered by the authors of the study, training and repetitive drills on these specific behaviors cannot be emphasized enough because they are not only the skeleton of excellent communication; they are likely also the muscles, the heart, and even the soul,” he concluded.
The study was supported by a grant from the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and Dr. Feudtner reported no financial conflicts.
SOURCE: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
Clinicians can improve communications with parents during neonatal end-of-life situations by adopting key behaviors such as sitting down to talk to parents and using the infant’s name, according to data from a simulation study.
“Empirical evidence regarding communication with parents during and after a child’s critical instability or death is scarce,” wrote Marie-Hélène Lizotte, MD, of Centre Hospitalier Universitaire Sainte-Justine, Montréal, and colleagues. Noting that realistic simulation has been shown to help clinicians improve their communication skills, the investigators recruited clinicians to participate in a simulated unsuccessful neonatal resuscitation to identify behaviors associated with optimal parent communication.
Behaviors associated with high scores for clinicians deemed “good communicators” included introducing themselves to parents, using the infant’s name (if known), sitting down to speak to parents, not leaving the infant alone on the bed after death, and allowing time for silence, the researchers reported in Pediatrics.
The investigators presented the video simulations to evaluators, including clinicians and bereaved parents. In the simulation, a term infant was born after an emergency cesarean delivery for fetal distress and died after an unsuccessful attempt at resuscitation. A manikin infant was programmed to remain pulseless, and two actors played the roles of the parents in the video.
Evaluators scored the videos for overall performance and for communication with the parent actors during and after the resuscitation.
Overall, parent evaluators and parent actors agreed with clinicians on what actions exemplified optimal communication in about 81% of evaluations. Discrepancies were mainly related to the language participants used related to death, as some parent evaluators said they had trouble understanding certain sentences or found them insensitive, such as “her heart never came back” and “allowing natural death.”
A total of 31 participants were recruited for the simulation, including 15 pediatric residents, 5 neonatal fellows, 3 neonatologists, 3 neonatal nurse practitioners, and 5 transport and resuscitation team providers. Videos of the simulations were examined by 21 evaluators, including bereaved parents, the parent actors, a neonatologist, a maternal-fetal medicine specialist, a psychologist, and a respiratory therapist. There were 651 evaluations.
The study findings were limited by several factors including the use of a single center, use of videos for evaluations, and the use of a single infant-resuscitation scenario, the researchers noted. The results were strengthened, however, by the large number of evaluations, and they support the core behaviors as “a skeleton on which to build additional skills with practice and training” with attention to cultural differences in their application, such as recognizing that infants are not named until after birth in some cultures, they said.
The existing literature on strategies for providing empathy and support to parents facing the death of a child is limited, but this simulation study provides a design model to help address this issue, Chris Feudtner, MD, of the Children’s Hospital of Philadelphia wrote in an accompanying editorial. “Overall, this study, in terms of design and methodologic rigor, is a great advance toward answering our key question: how to best support parents in such circumstances,” he said.
Dr. Feudtner said that he would divide the clinician behaviors into two groups. The first, “Calm kind politeness,” includes acknowledging the parents, introducing themselves, using the infant’s name, and remaining calm. The second set of behaviors, which he called “Skillful situational leadership,” includes preparing parents for the resuscitation activities and providing verbal milestones that prepared them for the fatal outcome.
“Picking up on a metaphor offered by the authors of the study, training and repetitive drills on these specific behaviors cannot be emphasized enough because they are not only the skeleton of excellent communication; they are likely also the muscles, the heart, and even the soul,” he concluded.
The study was supported by a grant from the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and Dr. Feudtner reported no financial conflicts.
SOURCE: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
FROM PEDIATRICS
Key clinical point: Clinicians who took steps such as sitting down and using the infant’s name were seen by parents as good communicators.
Major finding: Evaluators of a simulation agreed 81% of the time on defining optimal communication.
Study details: The data come from a simulation study of 31 participants and 21 evaluators and a total of 651 evaluations.
Disclosures: The study was supported in part by the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and editorialist said they had no financial conflicts.
Source: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
Bariatric surgery lacks impact on teens’ long-term mental health
Young people treated with bariatric surgery for severe obesity did not experience better mental health in the 5 years following their procedures, Swedish researchers said, and indeed fared worse than their nontreated peers on certain measures.
The results of this study do not necessarily argue “that metabolic and bariatric surgery during adolescence causes mental health problems,” the investigators wrote in the Lancet Child and Adolescent Health, but “it is reasonable to conclude that metabolic and bariatric surgery does not result in a substantial alleviation of mental health problems in adolescents with severe obesity,” and that “long-term mental health support should be required in programs providing adolescent metabolic and bariatric surgery.”
Kajsa Järvholm, PhD, of Skåne University Hospital, in Malmö, Sweden, and colleagues reported results from a prospective nonrandomized study that recruited 81 adolescents in Sweden aged 13-18 years (mean age, 16.5) who had a body mass index of 40 or higher, or BMI of 35 with obesity-related comorbidities and who underwent Roux-en-Y gastric bypass for weight loss. Subjects were matched by age, sex, and BMI to 80 controls (mean age, 15.8 years) who were assigned to conventional nonsurgical treatment. All patients were assessed at 1, 2, and 5 years.
Although mental health treatment, including use of psychiatric drugs, did not differ between the groups at baseline, during the follow-up period the subjects who underwent surgery saw 15% more impatient and outpatient mental health treatment, compared with controls, a significant difference. About a quarter of patients in the surgically treated group required specialized mental health treatment for the first time after their surgeries.
Though the surgical group lost much more weight – mean BMI was 32.3 at 5 years, compared with 41.7 for controls – none of the mental health changes from baseline were significantly associated with percentage change of BMI at 5 years.
The findings from the study are consistent with results from studies in adults in which bariatric surgery improves many health outcomes but does not alter the need for mental health treatment. Although 5 years is a longer follow-up than in previous studies in young patients – a key strength of the study – Dr. Järvholm and colleagues acknowledged some weaknesses, including a nonrandomized design, lack of a comparison group of nonobese youths for mental health measures, a small sample size, and a surgical procedure that is now out of favor in adolescents.
The study was funded by Swedish government and health foundations. Dr. Järvholm disclosed pharmaceutical industry funding not related to the study, and three coauthors also disclosed industry relationships.
SOURCE: Järvholm K et al. Lancet Child Adolesc Health. 2020. doi: 10.1016/s2352-4642(20)30024-9.
Young people treated with bariatric surgery for severe obesity did not experience better mental health in the 5 years following their procedures, Swedish researchers said, and indeed fared worse than their nontreated peers on certain measures.
The results of this study do not necessarily argue “that metabolic and bariatric surgery during adolescence causes mental health problems,” the investigators wrote in the Lancet Child and Adolescent Health, but “it is reasonable to conclude that metabolic and bariatric surgery does not result in a substantial alleviation of mental health problems in adolescents with severe obesity,” and that “long-term mental health support should be required in programs providing adolescent metabolic and bariatric surgery.”
Kajsa Järvholm, PhD, of Skåne University Hospital, in Malmö, Sweden, and colleagues reported results from a prospective nonrandomized study that recruited 81 adolescents in Sweden aged 13-18 years (mean age, 16.5) who had a body mass index of 40 or higher, or BMI of 35 with obesity-related comorbidities and who underwent Roux-en-Y gastric bypass for weight loss. Subjects were matched by age, sex, and BMI to 80 controls (mean age, 15.8 years) who were assigned to conventional nonsurgical treatment. All patients were assessed at 1, 2, and 5 years.
Although mental health treatment, including use of psychiatric drugs, did not differ between the groups at baseline, during the follow-up period the subjects who underwent surgery saw 15% more impatient and outpatient mental health treatment, compared with controls, a significant difference. About a quarter of patients in the surgically treated group required specialized mental health treatment for the first time after their surgeries.
Though the surgical group lost much more weight – mean BMI was 32.3 at 5 years, compared with 41.7 for controls – none of the mental health changes from baseline were significantly associated with percentage change of BMI at 5 years.
The findings from the study are consistent with results from studies in adults in which bariatric surgery improves many health outcomes but does not alter the need for mental health treatment. Although 5 years is a longer follow-up than in previous studies in young patients – a key strength of the study – Dr. Järvholm and colleagues acknowledged some weaknesses, including a nonrandomized design, lack of a comparison group of nonobese youths for mental health measures, a small sample size, and a surgical procedure that is now out of favor in adolescents.
The study was funded by Swedish government and health foundations. Dr. Järvholm disclosed pharmaceutical industry funding not related to the study, and three coauthors also disclosed industry relationships.
SOURCE: Järvholm K et al. Lancet Child Adolesc Health. 2020. doi: 10.1016/s2352-4642(20)30024-9.
Young people treated with bariatric surgery for severe obesity did not experience better mental health in the 5 years following their procedures, Swedish researchers said, and indeed fared worse than their nontreated peers on certain measures.
The results of this study do not necessarily argue “that metabolic and bariatric surgery during adolescence causes mental health problems,” the investigators wrote in the Lancet Child and Adolescent Health, but “it is reasonable to conclude that metabolic and bariatric surgery does not result in a substantial alleviation of mental health problems in adolescents with severe obesity,” and that “long-term mental health support should be required in programs providing adolescent metabolic and bariatric surgery.”
Kajsa Järvholm, PhD, of Skåne University Hospital, in Malmö, Sweden, and colleagues reported results from a prospective nonrandomized study that recruited 81 adolescents in Sweden aged 13-18 years (mean age, 16.5) who had a body mass index of 40 or higher, or BMI of 35 with obesity-related comorbidities and who underwent Roux-en-Y gastric bypass for weight loss. Subjects were matched by age, sex, and BMI to 80 controls (mean age, 15.8 years) who were assigned to conventional nonsurgical treatment. All patients were assessed at 1, 2, and 5 years.
Although mental health treatment, including use of psychiatric drugs, did not differ between the groups at baseline, during the follow-up period the subjects who underwent surgery saw 15% more impatient and outpatient mental health treatment, compared with controls, a significant difference. About a quarter of patients in the surgically treated group required specialized mental health treatment for the first time after their surgeries.
Though the surgical group lost much more weight – mean BMI was 32.3 at 5 years, compared with 41.7 for controls – none of the mental health changes from baseline were significantly associated with percentage change of BMI at 5 years.
The findings from the study are consistent with results from studies in adults in which bariatric surgery improves many health outcomes but does not alter the need for mental health treatment. Although 5 years is a longer follow-up than in previous studies in young patients – a key strength of the study – Dr. Järvholm and colleagues acknowledged some weaknesses, including a nonrandomized design, lack of a comparison group of nonobese youths for mental health measures, a small sample size, and a surgical procedure that is now out of favor in adolescents.
The study was funded by Swedish government and health foundations. Dr. Järvholm disclosed pharmaceutical industry funding not related to the study, and three coauthors also disclosed industry relationships.
SOURCE: Järvholm K et al. Lancet Child Adolesc Health. 2020. doi: 10.1016/s2352-4642(20)30024-9.
FROM THE LANCET CHILD & ADOLESCENT HEALTH
Key clinical point: Bariatric surgery was not associated with improvement in obese adolescents’ long-term mental health, despite significant weight loss.
Major finding: During 5 years of follow up, surgically treated patients experienced 15% more mental health care usage than controls.
Study details: A prospective, nonrandomized study involving 161 adolescents with a BMI of 40 or greater (or 35 with comorbidities).
Disclosures: The Swedish government and Swedish health research foundations sponsored the study.
Source: Järvholm K et al. Lancet Child Adolesc Health. 2020. doi: 10.1016/s2352-4642(20)30024-9.
Pubertal suppression reduces risk of later suicidal ideation in transgender people
Transgender adults who, as adolescents, desired and received pubertal suppression had reduced odds of suicidal ideation, compared with those who wanted but didn’t receive pubertal suppression during their teen years.
Raw frequency of lifetime suicidal ideation was 90% in transgender adults who wanted, but did not receive, pubertal suppression in adolescence, compared with 75% in those who did receive pubertal suppression in adolescence, according to a new analysis of a nationwide survey of transgender people reported in Pediatrics. After controlling for demographic variables, the lifetime adjusted odds ratio for suicidal ideation was 0.3 for those receiving pubertal suppression, compared with those who wanted but didn’t receive pubertal suppression.
The study was the first to examine this association, and findings were drawn from the 2015 U.S. Transgender Survey, the largest known dataset of transgender adults, wrote the study’s lead author Jack Turban, MD, and coinvestigators.
“Suicidality is of particular concern for this population because the estimated lifetime prevalence of suicide attempts among transgender people is as high as 40%,” noted Dr. Turban, a psychiatry resident at Harvard Medical School and Massachusetts General Hospital, Boston, and McLean Hospital, Belmont, Mass., and coauthors. Anxiety, depression, and suicidality all are more common among transgender youth, who make up almost 2% of the nation’s adolescent population, they said.
Among transgender youth, the researchers explained, a spectrum exists: “Some have minimal body dysphoria and do not desire pubertal suppression, whereas others report significant dysphoria around the physical changes related to puberty.” Accordingly, they said, “We examined only those youth who desired pubertal suppression,” because this is the population of youth about whom clinicians need to make treatment decisions.
For individuals who might experience distress from the irreversible bodily changes of endogenous puberty, suppression via gonadotropin releasing hormone analogues (GnRHas) “allows these adolescents more time to decide if they wish to either induce exogenous gender-congruent puberty or allow endogenous puberty to progress,” wrote Dr. Turban and his collaborators.
The U.S. Transgender Survey dataset includes response from over 27,000 transgender adults with nationwide representation. However, this study included only participants who were younger than 17 years in 1998, when GnRHas for pubertal suppression became available. Filtering this group further to just those respondents between the ages of 18 and 36 years whose survey responses indicated they had ever wanted pubertal suppression yielded 3,494 individuals. Of these individuals, just 2.5% (89 participants) had ever received pubertal suppression.
“Results from this study suggest that the majority of transgender adults in the United States who have wanted pubertal suppression did not receive it,” noted the authors. Even among the youngest respondents – who received care during puberty most recently – just 5% of the 18-year-olds in 2015 desiring pubertal suppression actually received the treatment.
Among other associations, individuals who were younger, those with feminine gender identity, those with male sex assigned at birth, and those reporting heterosexual sexual orientation were more likely to have received pubertal suppression.
Receiving GnRHas also was more likely for individuals with higher household income and more family support of their gender identity. Without insurance, studies have indicated that the annual cost of GnRHA treatment can be $4,000-$25,000. Another study noted that at the Boston Children’s Hospital Gender Management Service before 2012, fewer than 20% of patients were able to get insurance coverage for pubertal suppression, according to Dr. Turban and colleagues.
The study looked at suicidality over the past year and lifetime suicidality, as well as severe psychological distress and binge drinking over the past month. Investigators also asked about lifetime history of illicit drug use, hypothesizing that those who received pubertal suppression would have “superior mental health outcomes” when compared to those who desired – but didn’t receive – pubertal suppression, wrote Dr. Turban and coauthors.
Suicidality within the past 12 months and severe psychological distress were both significantly more common among those who did not receive pubertal suppression, but these associations lost significance after multivariable analysis. There was no difference in odds of suicide attempts, although the study may have been underpowered to detect some of these associations, said the investigators.
After statistical analysis to control for demographic variables, pubertal suppression still was associated with decreased odds of having suicidal ideation over the lifespan.
Dr. Turban and colleagues acknowledged that reverse causation may have been in play, because adolescents with better mental health might have been considered better candidates for GnRHa therapy. But the study’s large sample size and wide geographic reach are strengths, they said, concluding that overall, the findings lend support to existing recommendations from the Endocrine Society and the World Professional Association for Transgender Health that pubertal suppression therapy be available to those adolescents who desire it.
Investigators were supported by the U.S. Health Resources and Services Administration, the Patient-Centered Outcomes Research Institute, and the American Academy of Child & Adolescent Psychiatry. The authors reported that they had no financial conflicts of interest.
SOURCE: Turban JL et al. Pediatrics. 2020;145(2):e20191725.
Access to good medical care for transgender adolescents remains very limited. When it is available, puberty blockers are an excellent, conservative option for trans adolescents entering puberty so that they have time to consider longer-term treatment options with their providers and families. As demonstrated by the data in this study, good attention to transgender children can substantially improve their mental health.
The biggest barrier to health care for trans adolescents is access to knowledgeable providers – even more than affordability, which is improving with better coverage by payers. As noted in the study by Turban et al., the lack of access to care remains a huge problem.
It is not surprising that, when we neglect health care, we get bad outcomes. In that sense, the study by Turban et al. is quite intuitive. The few adolescents with access to the appropriate health care had better immediate outcomes. Still, as a scientist I take nothing for granted, and a study confirming what seems logical is important confirmation.
Joshua D. Safer, MD, who is the executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, both in New York, was asked to comment on the article by Turban et al. He said he had no relevant financial disclosures.
Access to good medical care for transgender adolescents remains very limited. When it is available, puberty blockers are an excellent, conservative option for trans adolescents entering puberty so that they have time to consider longer-term treatment options with their providers and families. As demonstrated by the data in this study, good attention to transgender children can substantially improve their mental health.
The biggest barrier to health care for trans adolescents is access to knowledgeable providers – even more than affordability, which is improving with better coverage by payers. As noted in the study by Turban et al., the lack of access to care remains a huge problem.
It is not surprising that, when we neglect health care, we get bad outcomes. In that sense, the study by Turban et al. is quite intuitive. The few adolescents with access to the appropriate health care had better immediate outcomes. Still, as a scientist I take nothing for granted, and a study confirming what seems logical is important confirmation.
Joshua D. Safer, MD, who is the executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, both in New York, was asked to comment on the article by Turban et al. He said he had no relevant financial disclosures.
Access to good medical care for transgender adolescents remains very limited. When it is available, puberty blockers are an excellent, conservative option for trans adolescents entering puberty so that they have time to consider longer-term treatment options with their providers and families. As demonstrated by the data in this study, good attention to transgender children can substantially improve their mental health.
The biggest barrier to health care for trans adolescents is access to knowledgeable providers – even more than affordability, which is improving with better coverage by payers. As noted in the study by Turban et al., the lack of access to care remains a huge problem.
It is not surprising that, when we neglect health care, we get bad outcomes. In that sense, the study by Turban et al. is quite intuitive. The few adolescents with access to the appropriate health care had better immediate outcomes. Still, as a scientist I take nothing for granted, and a study confirming what seems logical is important confirmation.
Joshua D. Safer, MD, who is the executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, both in New York, was asked to comment on the article by Turban et al. He said he had no relevant financial disclosures.
Transgender adults who, as adolescents, desired and received pubertal suppression had reduced odds of suicidal ideation, compared with those who wanted but didn’t receive pubertal suppression during their teen years.
Raw frequency of lifetime suicidal ideation was 90% in transgender adults who wanted, but did not receive, pubertal suppression in adolescence, compared with 75% in those who did receive pubertal suppression in adolescence, according to a new analysis of a nationwide survey of transgender people reported in Pediatrics. After controlling for demographic variables, the lifetime adjusted odds ratio for suicidal ideation was 0.3 for those receiving pubertal suppression, compared with those who wanted but didn’t receive pubertal suppression.
The study was the first to examine this association, and findings were drawn from the 2015 U.S. Transgender Survey, the largest known dataset of transgender adults, wrote the study’s lead author Jack Turban, MD, and coinvestigators.
“Suicidality is of particular concern for this population because the estimated lifetime prevalence of suicide attempts among transgender people is as high as 40%,” noted Dr. Turban, a psychiatry resident at Harvard Medical School and Massachusetts General Hospital, Boston, and McLean Hospital, Belmont, Mass., and coauthors. Anxiety, depression, and suicidality all are more common among transgender youth, who make up almost 2% of the nation’s adolescent population, they said.
Among transgender youth, the researchers explained, a spectrum exists: “Some have minimal body dysphoria and do not desire pubertal suppression, whereas others report significant dysphoria around the physical changes related to puberty.” Accordingly, they said, “We examined only those youth who desired pubertal suppression,” because this is the population of youth about whom clinicians need to make treatment decisions.
For individuals who might experience distress from the irreversible bodily changes of endogenous puberty, suppression via gonadotropin releasing hormone analogues (GnRHas) “allows these adolescents more time to decide if they wish to either induce exogenous gender-congruent puberty or allow endogenous puberty to progress,” wrote Dr. Turban and his collaborators.
The U.S. Transgender Survey dataset includes response from over 27,000 transgender adults with nationwide representation. However, this study included only participants who were younger than 17 years in 1998, when GnRHas for pubertal suppression became available. Filtering this group further to just those respondents between the ages of 18 and 36 years whose survey responses indicated they had ever wanted pubertal suppression yielded 3,494 individuals. Of these individuals, just 2.5% (89 participants) had ever received pubertal suppression.
“Results from this study suggest that the majority of transgender adults in the United States who have wanted pubertal suppression did not receive it,” noted the authors. Even among the youngest respondents – who received care during puberty most recently – just 5% of the 18-year-olds in 2015 desiring pubertal suppression actually received the treatment.
Among other associations, individuals who were younger, those with feminine gender identity, those with male sex assigned at birth, and those reporting heterosexual sexual orientation were more likely to have received pubertal suppression.
Receiving GnRHas also was more likely for individuals with higher household income and more family support of their gender identity. Without insurance, studies have indicated that the annual cost of GnRHA treatment can be $4,000-$25,000. Another study noted that at the Boston Children’s Hospital Gender Management Service before 2012, fewer than 20% of patients were able to get insurance coverage for pubertal suppression, according to Dr. Turban and colleagues.
The study looked at suicidality over the past year and lifetime suicidality, as well as severe psychological distress and binge drinking over the past month. Investigators also asked about lifetime history of illicit drug use, hypothesizing that those who received pubertal suppression would have “superior mental health outcomes” when compared to those who desired – but didn’t receive – pubertal suppression, wrote Dr. Turban and coauthors.
Suicidality within the past 12 months and severe psychological distress were both significantly more common among those who did not receive pubertal suppression, but these associations lost significance after multivariable analysis. There was no difference in odds of suicide attempts, although the study may have been underpowered to detect some of these associations, said the investigators.
After statistical analysis to control for demographic variables, pubertal suppression still was associated with decreased odds of having suicidal ideation over the lifespan.
Dr. Turban and colleagues acknowledged that reverse causation may have been in play, because adolescents with better mental health might have been considered better candidates for GnRHa therapy. But the study’s large sample size and wide geographic reach are strengths, they said, concluding that overall, the findings lend support to existing recommendations from the Endocrine Society and the World Professional Association for Transgender Health that pubertal suppression therapy be available to those adolescents who desire it.
Investigators were supported by the U.S. Health Resources and Services Administration, the Patient-Centered Outcomes Research Institute, and the American Academy of Child & Adolescent Psychiatry. The authors reported that they had no financial conflicts of interest.
SOURCE: Turban JL et al. Pediatrics. 2020;145(2):e20191725.
Transgender adults who, as adolescents, desired and received pubertal suppression had reduced odds of suicidal ideation, compared with those who wanted but didn’t receive pubertal suppression during their teen years.
Raw frequency of lifetime suicidal ideation was 90% in transgender adults who wanted, but did not receive, pubertal suppression in adolescence, compared with 75% in those who did receive pubertal suppression in adolescence, according to a new analysis of a nationwide survey of transgender people reported in Pediatrics. After controlling for demographic variables, the lifetime adjusted odds ratio for suicidal ideation was 0.3 for those receiving pubertal suppression, compared with those who wanted but didn’t receive pubertal suppression.
The study was the first to examine this association, and findings were drawn from the 2015 U.S. Transgender Survey, the largest known dataset of transgender adults, wrote the study’s lead author Jack Turban, MD, and coinvestigators.
“Suicidality is of particular concern for this population because the estimated lifetime prevalence of suicide attempts among transgender people is as high as 40%,” noted Dr. Turban, a psychiatry resident at Harvard Medical School and Massachusetts General Hospital, Boston, and McLean Hospital, Belmont, Mass., and coauthors. Anxiety, depression, and suicidality all are more common among transgender youth, who make up almost 2% of the nation’s adolescent population, they said.
Among transgender youth, the researchers explained, a spectrum exists: “Some have minimal body dysphoria and do not desire pubertal suppression, whereas others report significant dysphoria around the physical changes related to puberty.” Accordingly, they said, “We examined only those youth who desired pubertal suppression,” because this is the population of youth about whom clinicians need to make treatment decisions.
For individuals who might experience distress from the irreversible bodily changes of endogenous puberty, suppression via gonadotropin releasing hormone analogues (GnRHas) “allows these adolescents more time to decide if they wish to either induce exogenous gender-congruent puberty or allow endogenous puberty to progress,” wrote Dr. Turban and his collaborators.
The U.S. Transgender Survey dataset includes response from over 27,000 transgender adults with nationwide representation. However, this study included only participants who were younger than 17 years in 1998, when GnRHas for pubertal suppression became available. Filtering this group further to just those respondents between the ages of 18 and 36 years whose survey responses indicated they had ever wanted pubertal suppression yielded 3,494 individuals. Of these individuals, just 2.5% (89 participants) had ever received pubertal suppression.
“Results from this study suggest that the majority of transgender adults in the United States who have wanted pubertal suppression did not receive it,” noted the authors. Even among the youngest respondents – who received care during puberty most recently – just 5% of the 18-year-olds in 2015 desiring pubertal suppression actually received the treatment.
Among other associations, individuals who were younger, those with feminine gender identity, those with male sex assigned at birth, and those reporting heterosexual sexual orientation were more likely to have received pubertal suppression.
Receiving GnRHas also was more likely for individuals with higher household income and more family support of their gender identity. Without insurance, studies have indicated that the annual cost of GnRHA treatment can be $4,000-$25,000. Another study noted that at the Boston Children’s Hospital Gender Management Service before 2012, fewer than 20% of patients were able to get insurance coverage for pubertal suppression, according to Dr. Turban and colleagues.
The study looked at suicidality over the past year and lifetime suicidality, as well as severe psychological distress and binge drinking over the past month. Investigators also asked about lifetime history of illicit drug use, hypothesizing that those who received pubertal suppression would have “superior mental health outcomes” when compared to those who desired – but didn’t receive – pubertal suppression, wrote Dr. Turban and coauthors.
Suicidality within the past 12 months and severe psychological distress were both significantly more common among those who did not receive pubertal suppression, but these associations lost significance after multivariable analysis. There was no difference in odds of suicide attempts, although the study may have been underpowered to detect some of these associations, said the investigators.
After statistical analysis to control for demographic variables, pubertal suppression still was associated with decreased odds of having suicidal ideation over the lifespan.
Dr. Turban and colleagues acknowledged that reverse causation may have been in play, because adolescents with better mental health might have been considered better candidates for GnRHa therapy. But the study’s large sample size and wide geographic reach are strengths, they said, concluding that overall, the findings lend support to existing recommendations from the Endocrine Society and the World Professional Association for Transgender Health that pubertal suppression therapy be available to those adolescents who desire it.
Investigators were supported by the U.S. Health Resources and Services Administration, the Patient-Centered Outcomes Research Institute, and the American Academy of Child & Adolescent Psychiatry. The authors reported that they had no financial conflicts of interest.
SOURCE: Turban JL et al. Pediatrics. 2020;145(2):e20191725.
FROM PEDIATRICS
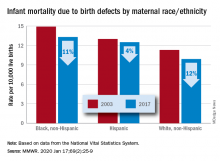
Infant deaths from birth defects decline, but some disparities widen
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
FROM MMWR
Family-focused therapy linked to longer remissions in youth at risk for bipolar disorder
A 4-month intensive program of family-focused therapy worked better than a less-intensive program in delaying new mood episodes among young people at risk of developing bipolar disorder, new research shows.
“This study extends the results of other randomized clinical trials indicating effects of family psychoeducation and skill training on the long-term trajectory of depressive symptoms in pediatric mood disorders,” wrote David J. Miklowitz, PhD, of the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, and colleagues. The study was published in JAMA Psychiatry.
For their research, the investigators recruited 127 subjects aged 9-17 years (mean age, 13 years) deemed at high risk for later bipolar I or II disorder for having depression or subthreshold mania along with active mood symptoms and a family history of bipolar disorder. Some 85% of subjects had depression symptoms at enrollment.
Subjects were randomized to 12 sessions over 4 months of family-focused therapy – a psychoeducation, communication, and problem-solving training program incorporating caretakers and also siblings if possible (n = 61) – or to 3 sessions of family-focused therapy and an additional 3 of individual therapy in the same 4-month time frame (n = 66). Medication was allowed for all subjects, and patients were followed for a median 2 years after the intervention. Baseline characteristics, medication use, and dropout rates were similar between the groups.
Both groups saw similarly high rates of new episodes of major depression, mania, or hypomania during follow-up; however, those in the intensive family-focused therapy group saw longer intervals of wellness, with a median 81 weeks (95% confidence interval, 56-123 weeks) from randomization until the first observed mood episode, compared with 63 weeks (95% CI, 44-78 weeks) to an episode for the less-intensive group (P = .03). Dr. Miklowitz and colleagues did not find differences in the severity of mood episodes following either treatment mode or in later conversion to bipolar I or II.
The researchers described as limitations of their study its inability to measure the “temporal relationship between changes in family communication and symptom changes in patients,” which would help answer whether improvements in communication patterns aid symptom regulation, or whether more stable patients are better able to manage difficult family interactions.
Family-focused therapy “may have uniquely enduring effects that extend into the maintenance phase of treatment,” Dr. Miklowitz and colleagues wrote.
The study was funded by the National Institute of Mental Health. Several coauthors, including the lead author, reported receiving research grants from NIMH and other foundations. Two additional coauthors reported receiving pharmaceutical industry funding, including advisory board and consulting fees.
SOURCE: Miklowitz DJ et al. JAMA Psychiatry. 2020 Jan 15. doi: 10.1001/jamapsychiatry.2019.4520.
A 4-month intensive program of family-focused therapy worked better than a less-intensive program in delaying new mood episodes among young people at risk of developing bipolar disorder, new research shows.
“This study extends the results of other randomized clinical trials indicating effects of family psychoeducation and skill training on the long-term trajectory of depressive symptoms in pediatric mood disorders,” wrote David J. Miklowitz, PhD, of the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, and colleagues. The study was published in JAMA Psychiatry.
For their research, the investigators recruited 127 subjects aged 9-17 years (mean age, 13 years) deemed at high risk for later bipolar I or II disorder for having depression or subthreshold mania along with active mood symptoms and a family history of bipolar disorder. Some 85% of subjects had depression symptoms at enrollment.
Subjects were randomized to 12 sessions over 4 months of family-focused therapy – a psychoeducation, communication, and problem-solving training program incorporating caretakers and also siblings if possible (n = 61) – or to 3 sessions of family-focused therapy and an additional 3 of individual therapy in the same 4-month time frame (n = 66). Medication was allowed for all subjects, and patients were followed for a median 2 years after the intervention. Baseline characteristics, medication use, and dropout rates were similar between the groups.
Both groups saw similarly high rates of new episodes of major depression, mania, or hypomania during follow-up; however, those in the intensive family-focused therapy group saw longer intervals of wellness, with a median 81 weeks (95% confidence interval, 56-123 weeks) from randomization until the first observed mood episode, compared with 63 weeks (95% CI, 44-78 weeks) to an episode for the less-intensive group (P = .03). Dr. Miklowitz and colleagues did not find differences in the severity of mood episodes following either treatment mode or in later conversion to bipolar I or II.
The researchers described as limitations of their study its inability to measure the “temporal relationship between changes in family communication and symptom changes in patients,” which would help answer whether improvements in communication patterns aid symptom regulation, or whether more stable patients are better able to manage difficult family interactions.
Family-focused therapy “may have uniquely enduring effects that extend into the maintenance phase of treatment,” Dr. Miklowitz and colleagues wrote.
The study was funded by the National Institute of Mental Health. Several coauthors, including the lead author, reported receiving research grants from NIMH and other foundations. Two additional coauthors reported receiving pharmaceutical industry funding, including advisory board and consulting fees.
SOURCE: Miklowitz DJ et al. JAMA Psychiatry. 2020 Jan 15. doi: 10.1001/jamapsychiatry.2019.4520.
A 4-month intensive program of family-focused therapy worked better than a less-intensive program in delaying new mood episodes among young people at risk of developing bipolar disorder, new research shows.
“This study extends the results of other randomized clinical trials indicating effects of family psychoeducation and skill training on the long-term trajectory of depressive symptoms in pediatric mood disorders,” wrote David J. Miklowitz, PhD, of the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, and colleagues. The study was published in JAMA Psychiatry.
For their research, the investigators recruited 127 subjects aged 9-17 years (mean age, 13 years) deemed at high risk for later bipolar I or II disorder for having depression or subthreshold mania along with active mood symptoms and a family history of bipolar disorder. Some 85% of subjects had depression symptoms at enrollment.
Subjects were randomized to 12 sessions over 4 months of family-focused therapy – a psychoeducation, communication, and problem-solving training program incorporating caretakers and also siblings if possible (n = 61) – or to 3 sessions of family-focused therapy and an additional 3 of individual therapy in the same 4-month time frame (n = 66). Medication was allowed for all subjects, and patients were followed for a median 2 years after the intervention. Baseline characteristics, medication use, and dropout rates were similar between the groups.
Both groups saw similarly high rates of new episodes of major depression, mania, or hypomania during follow-up; however, those in the intensive family-focused therapy group saw longer intervals of wellness, with a median 81 weeks (95% confidence interval, 56-123 weeks) from randomization until the first observed mood episode, compared with 63 weeks (95% CI, 44-78 weeks) to an episode for the less-intensive group (P = .03). Dr. Miklowitz and colleagues did not find differences in the severity of mood episodes following either treatment mode or in later conversion to bipolar I or II.
The researchers described as limitations of their study its inability to measure the “temporal relationship between changes in family communication and symptom changes in patients,” which would help answer whether improvements in communication patterns aid symptom regulation, or whether more stable patients are better able to manage difficult family interactions.
Family-focused therapy “may have uniquely enduring effects that extend into the maintenance phase of treatment,” Dr. Miklowitz and colleagues wrote.
The study was funded by the National Institute of Mental Health. Several coauthors, including the lead author, reported receiving research grants from NIMH and other foundations. Two additional coauthors reported receiving pharmaceutical industry funding, including advisory board and consulting fees.
SOURCE: Miklowitz DJ et al. JAMA Psychiatry. 2020 Jan 15. doi: 10.1001/jamapsychiatry.2019.4520.
FROM JAMA PSYCHIATRY
Anxiety may be a part of healthy development, sometimes
Anxiety is probably the most common behavioral health complaint that presents in the pediatrician’s office. The prevalence of anxiety is going up every year, and we do not have a good understanding why. Is it the pressure to perform at earlier and earlier ages? Is it the press of information or rapid communication of every disaster on Earth? Or are children not developing appropriate coping skills for the expectable challenges and stresses they will face through development? We do not know.
Anxiety disorders are most likely to present in the early school years – latency – between the ages of 6 and 12 years. Teenagers may present with new anxiety disorders or may disclose symptoms that they have been quietly managing since they were younger, when they were thought to be “shy.” These disorders include separation anxiety disorder, social phobia, selective mutism, specific phobia, and generalized anxiety disorder. This age period also is marked by high levels of normal anxiety because children’s cognitive development has advanced beyond their emotional development. They are capable of logic, can understand cause and effect, and can appreciate the passage of time and serious matters such as the permanence of death. Gone is the magical thinking of the preschool years! When an elementary student learns about global warming or a refugee crisis, they can fully appreciate the serious implications of the subject. What they lack is experience with tolerating uncertainty and worry and proceeding with life, focusing on what they might address or even bearing the fact that life is sometimes unfair. This mismatch of relative cognitive maturity with emotional immaturity can lead to anxiety and distress. This is particularly true as they face these challenges while they have new independence, spending longer days at school and less time with parents. Bearing this distress with caring adults, learning to focus on what they can do, and discovering that they and the world can go on even when something very unfair has happened is central to how they develop emotional maturity.
How a child learns to manage anxiety is very much determined by how their parents manage anxiety and how well their parents can tolerate their children’s distress. A parent who becomes overwhelmed when their child is upset about missing a goal in soccer will have a difficult time helping their child learn how to manage distress. And children who are facing chronic severe stress, such as poverty, domestic violence, or chronic illness in a parent, are facing the double challenge of managing persistent anxiety that may be impairing their parents’ ability to support them. When the child and their family are connected to a community that has not been able to effectively respond to larger problems, such as creating safe schools or neighborhoods, anxiety can become entrenched in despair.
It often is tempting to jump in with reassurance when your patient or their parents present with anxiety. But when you calmly show curiosity, you model tolerance of their distress. Are they fearful about very specific situations, such as being called on in class? Or do they become dysregulated when facing a separation from their parents, such as at bedtime or before school, seeking contact with their parents with endless questions? Find out how the parents are managing separations and whether they may be inadvertently rewarding by staying with them to negotiate or answer endless questions. Find out if parents may be accommodating anxiety by allowing their children to avoid normal situations that are stirring anxiety. Do they give in anytime their child shows resistance or have they learned to pick their battles and help their children face more-modest stress while avoiding only the most intensely anxious situations? Are the parents able to speak calmly and with good humor about these challenges or do they become very stressed and defensive? Is there a family history of anxiety? Managing a child’s anxiety every day can be exhausting, and parents might need a referral in addition to a discussion about how anxiety is developmentally normal.
For those parents that can manage this discussion, suggest that, like you, if they can remain calm during these times with their child (even if they don’t feel calm), it will help their child get better at managing anxiety, even if their child has an anxiety disorder. They also should be curious about their child’s worries, learning about the details and scenarios their children may be anticipating. They should express compassion about how uncomfortable anxiety is, coupled with their confident belief that the child will be able to tolerate and manage the situation even though it’s uncomfortable. This acknowledgment should not be a dismissal of the anxiety, instead it should be confidence that the child will learn to bear it.
When your patient is a teenager describing anxiety, unpack. Are they anxious about their performance on their five Advanced Placement exams? If their anxiety sounds more like appropriate stress, be compassionate and then curious about how they are learning to relax. Are they using drugs and alcohol? Or have they found healthy ways to unwind and recharge? Focusing on ways in which they are learning to care for themselves, making time for sleep and exercise, live time with friends, and senseless fun is therapeutic. Find out if their parents are supportive of their self-care. You might even give them a prescription!
Anxiety is often a private experience, and parents might not know about it until it presents with an explosion of distress or obstinacy when an anxious child is pushed into scary territory. Asking questions about specific worries (something happening to parents, germs, weather events) can illuminate the extent of anxiety. It also is worth exploring if there are rituals that help them manage their worries, whether they are common (finding a parent, hugging a pet, prayer) or more compulsive (repetitive undoing, hair pulling). Find out if there has recently been any serious stress or change for the family, such as the loss of a job or illness in a grandparent, that may be contributing to a child’s anxiety.
Anytime you see anxieties that are broad or extreme, disrupt their ability to function (go to school, participate in activities, build friendships), or if their parents are clearly struggling with managing their child’s distress, it is worthwhile to find a referral to a psychiatrist or psychologist for evaluation and further treatment. School avoidance constitutes an urgent need for evaluation, as every day of school missed makes it harder for the child to return to school. For all of your anxious patients, even when you make a referral to a psychiatrist for evaluation, teach your patients and parents about how critical adequate sleep and regular exercise are to managing anxiety. Remind them that an appropriate level of anxiety is normal and promotes performance and grit, despite the discomfort, and that learning how to manage anxiety is essential to growing up and building mental health.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at [email protected].
Anxiety is probably the most common behavioral health complaint that presents in the pediatrician’s office. The prevalence of anxiety is going up every year, and we do not have a good understanding why. Is it the pressure to perform at earlier and earlier ages? Is it the press of information or rapid communication of every disaster on Earth? Or are children not developing appropriate coping skills for the expectable challenges and stresses they will face through development? We do not know.
Anxiety disorders are most likely to present in the early school years – latency – between the ages of 6 and 12 years. Teenagers may present with new anxiety disorders or may disclose symptoms that they have been quietly managing since they were younger, when they were thought to be “shy.” These disorders include separation anxiety disorder, social phobia, selective mutism, specific phobia, and generalized anxiety disorder. This age period also is marked by high levels of normal anxiety because children’s cognitive development has advanced beyond their emotional development. They are capable of logic, can understand cause and effect, and can appreciate the passage of time and serious matters such as the permanence of death. Gone is the magical thinking of the preschool years! When an elementary student learns about global warming or a refugee crisis, they can fully appreciate the serious implications of the subject. What they lack is experience with tolerating uncertainty and worry and proceeding with life, focusing on what they might address or even bearing the fact that life is sometimes unfair. This mismatch of relative cognitive maturity with emotional immaturity can lead to anxiety and distress. This is particularly true as they face these challenges while they have new independence, spending longer days at school and less time with parents. Bearing this distress with caring adults, learning to focus on what they can do, and discovering that they and the world can go on even when something very unfair has happened is central to how they develop emotional maturity.
How a child learns to manage anxiety is very much determined by how their parents manage anxiety and how well their parents can tolerate their children’s distress. A parent who becomes overwhelmed when their child is upset about missing a goal in soccer will have a difficult time helping their child learn how to manage distress. And children who are facing chronic severe stress, such as poverty, domestic violence, or chronic illness in a parent, are facing the double challenge of managing persistent anxiety that may be impairing their parents’ ability to support them. When the child and their family are connected to a community that has not been able to effectively respond to larger problems, such as creating safe schools or neighborhoods, anxiety can become entrenched in despair.
It often is tempting to jump in with reassurance when your patient or their parents present with anxiety. But when you calmly show curiosity, you model tolerance of their distress. Are they fearful about very specific situations, such as being called on in class? Or do they become dysregulated when facing a separation from their parents, such as at bedtime or before school, seeking contact with their parents with endless questions? Find out how the parents are managing separations and whether they may be inadvertently rewarding by staying with them to negotiate or answer endless questions. Find out if parents may be accommodating anxiety by allowing their children to avoid normal situations that are stirring anxiety. Do they give in anytime their child shows resistance or have they learned to pick their battles and help their children face more-modest stress while avoiding only the most intensely anxious situations? Are the parents able to speak calmly and with good humor about these challenges or do they become very stressed and defensive? Is there a family history of anxiety? Managing a child’s anxiety every day can be exhausting, and parents might need a referral in addition to a discussion about how anxiety is developmentally normal.
For those parents that can manage this discussion, suggest that, like you, if they can remain calm during these times with their child (even if they don’t feel calm), it will help their child get better at managing anxiety, even if their child has an anxiety disorder. They also should be curious about their child’s worries, learning about the details and scenarios their children may be anticipating. They should express compassion about how uncomfortable anxiety is, coupled with their confident belief that the child will be able to tolerate and manage the situation even though it’s uncomfortable. This acknowledgment should not be a dismissal of the anxiety, instead it should be confidence that the child will learn to bear it.
When your patient is a teenager describing anxiety, unpack. Are they anxious about their performance on their five Advanced Placement exams? If their anxiety sounds more like appropriate stress, be compassionate and then curious about how they are learning to relax. Are they using drugs and alcohol? Or have they found healthy ways to unwind and recharge? Focusing on ways in which they are learning to care for themselves, making time for sleep and exercise, live time with friends, and senseless fun is therapeutic. Find out if their parents are supportive of their self-care. You might even give them a prescription!
Anxiety is often a private experience, and parents might not know about it until it presents with an explosion of distress or obstinacy when an anxious child is pushed into scary territory. Asking questions about specific worries (something happening to parents, germs, weather events) can illuminate the extent of anxiety. It also is worth exploring if there are rituals that help them manage their worries, whether they are common (finding a parent, hugging a pet, prayer) or more compulsive (repetitive undoing, hair pulling). Find out if there has recently been any serious stress or change for the family, such as the loss of a job or illness in a grandparent, that may be contributing to a child’s anxiety.
Anytime you see anxieties that are broad or extreme, disrupt their ability to function (go to school, participate in activities, build friendships), or if their parents are clearly struggling with managing their child’s distress, it is worthwhile to find a referral to a psychiatrist or psychologist for evaluation and further treatment. School avoidance constitutes an urgent need for evaluation, as every day of school missed makes it harder for the child to return to school. For all of your anxious patients, even when you make a referral to a psychiatrist for evaluation, teach your patients and parents about how critical adequate sleep and regular exercise are to managing anxiety. Remind them that an appropriate level of anxiety is normal and promotes performance and grit, despite the discomfort, and that learning how to manage anxiety is essential to growing up and building mental health.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at [email protected].
Anxiety is probably the most common behavioral health complaint that presents in the pediatrician’s office. The prevalence of anxiety is going up every year, and we do not have a good understanding why. Is it the pressure to perform at earlier and earlier ages? Is it the press of information or rapid communication of every disaster on Earth? Or are children not developing appropriate coping skills for the expectable challenges and stresses they will face through development? We do not know.
Anxiety disorders are most likely to present in the early school years – latency – between the ages of 6 and 12 years. Teenagers may present with new anxiety disorders or may disclose symptoms that they have been quietly managing since they were younger, when they were thought to be “shy.” These disorders include separation anxiety disorder, social phobia, selective mutism, specific phobia, and generalized anxiety disorder. This age period also is marked by high levels of normal anxiety because children’s cognitive development has advanced beyond their emotional development. They are capable of logic, can understand cause and effect, and can appreciate the passage of time and serious matters such as the permanence of death. Gone is the magical thinking of the preschool years! When an elementary student learns about global warming or a refugee crisis, they can fully appreciate the serious implications of the subject. What they lack is experience with tolerating uncertainty and worry and proceeding with life, focusing on what they might address or even bearing the fact that life is sometimes unfair. This mismatch of relative cognitive maturity with emotional immaturity can lead to anxiety and distress. This is particularly true as they face these challenges while they have new independence, spending longer days at school and less time with parents. Bearing this distress with caring adults, learning to focus on what they can do, and discovering that they and the world can go on even when something very unfair has happened is central to how they develop emotional maturity.
How a child learns to manage anxiety is very much determined by how their parents manage anxiety and how well their parents can tolerate their children’s distress. A parent who becomes overwhelmed when their child is upset about missing a goal in soccer will have a difficult time helping their child learn how to manage distress. And children who are facing chronic severe stress, such as poverty, domestic violence, or chronic illness in a parent, are facing the double challenge of managing persistent anxiety that may be impairing their parents’ ability to support them. When the child and their family are connected to a community that has not been able to effectively respond to larger problems, such as creating safe schools or neighborhoods, anxiety can become entrenched in despair.
It often is tempting to jump in with reassurance when your patient or their parents present with anxiety. But when you calmly show curiosity, you model tolerance of their distress. Are they fearful about very specific situations, such as being called on in class? Or do they become dysregulated when facing a separation from their parents, such as at bedtime or before school, seeking contact with their parents with endless questions? Find out how the parents are managing separations and whether they may be inadvertently rewarding by staying with them to negotiate or answer endless questions. Find out if parents may be accommodating anxiety by allowing their children to avoid normal situations that are stirring anxiety. Do they give in anytime their child shows resistance or have they learned to pick their battles and help their children face more-modest stress while avoiding only the most intensely anxious situations? Are the parents able to speak calmly and with good humor about these challenges or do they become very stressed and defensive? Is there a family history of anxiety? Managing a child’s anxiety every day can be exhausting, and parents might need a referral in addition to a discussion about how anxiety is developmentally normal.
For those parents that can manage this discussion, suggest that, like you, if they can remain calm during these times with their child (even if they don’t feel calm), it will help their child get better at managing anxiety, even if their child has an anxiety disorder. They also should be curious about their child’s worries, learning about the details and scenarios their children may be anticipating. They should express compassion about how uncomfortable anxiety is, coupled with their confident belief that the child will be able to tolerate and manage the situation even though it’s uncomfortable. This acknowledgment should not be a dismissal of the anxiety, instead it should be confidence that the child will learn to bear it.
When your patient is a teenager describing anxiety, unpack. Are they anxious about their performance on their five Advanced Placement exams? If their anxiety sounds more like appropriate stress, be compassionate and then curious about how they are learning to relax. Are they using drugs and alcohol? Or have they found healthy ways to unwind and recharge? Focusing on ways in which they are learning to care for themselves, making time for sleep and exercise, live time with friends, and senseless fun is therapeutic. Find out if their parents are supportive of their self-care. You might even give them a prescription!
Anxiety is often a private experience, and parents might not know about it until it presents with an explosion of distress or obstinacy when an anxious child is pushed into scary territory. Asking questions about specific worries (something happening to parents, germs, weather events) can illuminate the extent of anxiety. It also is worth exploring if there are rituals that help them manage their worries, whether they are common (finding a parent, hugging a pet, prayer) or more compulsive (repetitive undoing, hair pulling). Find out if there has recently been any serious stress or change for the family, such as the loss of a job or illness in a grandparent, that may be contributing to a child’s anxiety.
Anytime you see anxieties that are broad or extreme, disrupt their ability to function (go to school, participate in activities, build friendships), or if their parents are clearly struggling with managing their child’s distress, it is worthwhile to find a referral to a psychiatrist or psychologist for evaluation and further treatment. School avoidance constitutes an urgent need for evaluation, as every day of school missed makes it harder for the child to return to school. For all of your anxious patients, even when you make a referral to a psychiatrist for evaluation, teach your patients and parents about how critical adequate sleep and regular exercise are to managing anxiety. Remind them that an appropriate level of anxiety is normal and promotes performance and grit, despite the discomfort, and that learning how to manage anxiety is essential to growing up and building mental health.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at [email protected].
Runaway youth: Knowing the risk factors and care needs
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
FROM PEDIATRICS
Flu activity declines for second straight week
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
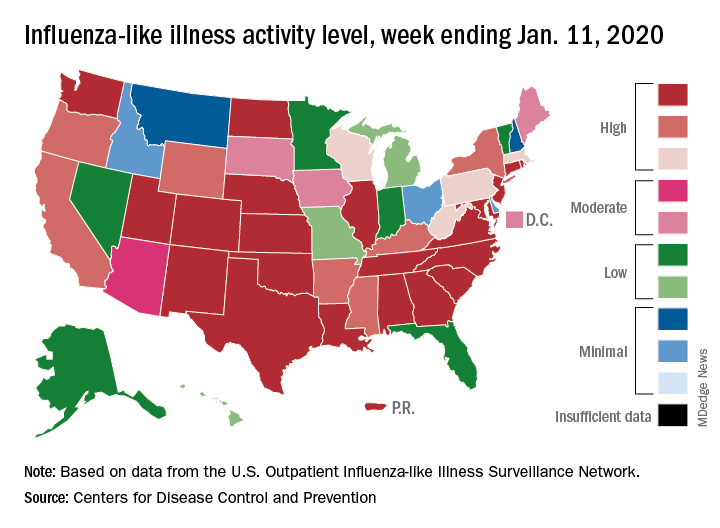
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
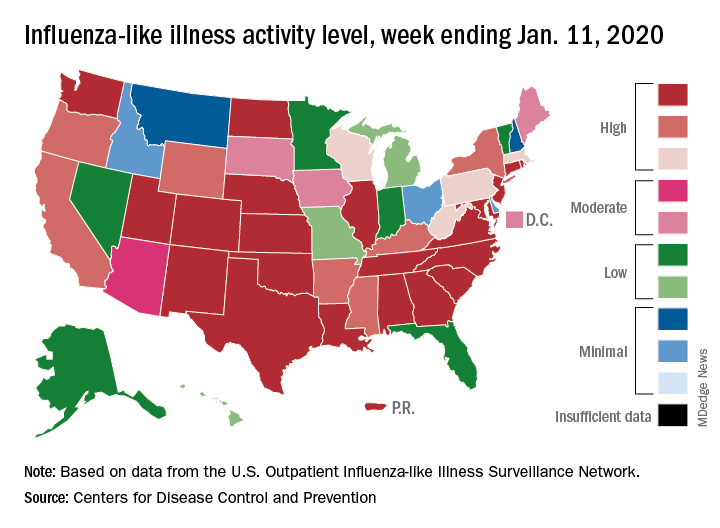
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
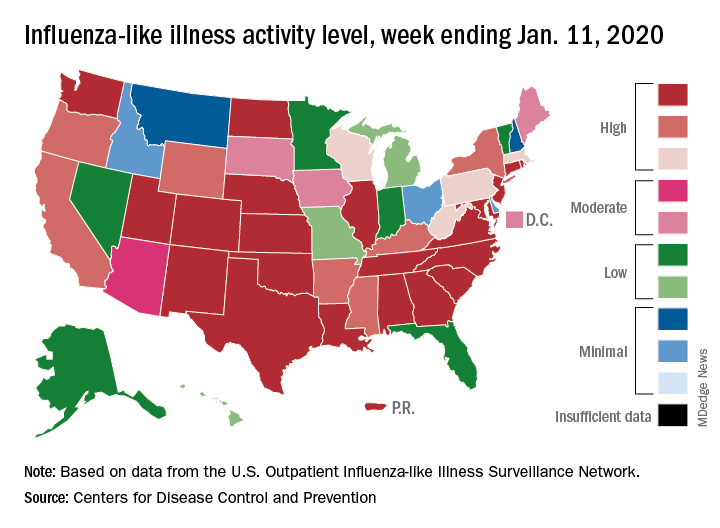
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.