User login
Remote ischemic preconditioning does no good
Remote ischemic preconditioning failed to improve outcomes among higher-risk patients undergoing elective cardiac surgery in two separate large clinical trials reported online Oct. 5 in the New England Journal of Medicine.
Both studies clearly showed that the technique did not provide greater protection of the heart, brain, or kidneys than did a sham technique, failing to improve any of the numerous primary or secondary endpoints or to produce a benefit in any of several subgroups of patients.
Remote ischemic preconditioning involves protecting the heart and other organs against surgery-related acute ischemia/reperfusion injury by first applying brief cycles of ischemia and reperfusion to a remote organ or tissue. It is thought that this stimulus produces a blood-borne response that conveys a protective effect from the remote area to the target organs. This remote preconditioning can be accomplished noninvasively by inflating and deflating a standard blood pressure cuff on the upper arm or thigh for brief periods.
Some early studies indicated that using this technique during cardiovascular surgery improved serum cardiac and renal biomarkers, which implied protection of these organs against ischemia/reperfusion injury. But more recent prospective clinical trials have shown no such benefit. None of these studies were adequately powered to assess the effect on hard clinical endpoints, and most were single center, unblinded, and had no standardized anesthesia regimen.
RIPHeart study
To address these study limitations, the RIPHeart Study investigators performed a prospective double-blind controlled trial among 1,385 adults undergoing elective cardiovascular surgery requiring cardiopulmonary bypass at 14 university hospitals in Germany during a 3-year period. The participants had a mean EuroSCORE (European System for Cardiac Operative Risk Evaluation) of 6 or higher, indicating that most of them were at higher than average risk, and all received the same anesthetic, intravenous propofol. A total of 692 patients were randomly assigned to undergo four 5-minute cycles of upper-arm ischemia/reperfusion after being anesthetized and 693 to undergo sham ischemia/reperfusion on a dummy arm hidden by surgical drapes, said Dr. Patrick Meybohm of the department of anesthesiology, intensive care medicine, and pain therapy at University Hospital Frankfurt and his associates.
The primary endpoint – a composite of death from any cause, nonfatal MI, stroke, or acute renal failure before hospital discharge – occurred in 14.3% of the intervention group and 14.6% of the control group, a nonsignificant difference. Furthermore, no significant differences between the two study groups were seen in any of the individual components of this composite measure, or in any secondary endpoints such as duration of mechanical ventilation, ICU length of stay, hospital length of stay, troponin levels, creatinine levels, onset of atrial fibrillation, or incidence of postoperative delirium. All outcome measures remained similar between the two study groups at 30-day, 90-day, and 1-year follow-ups (N Engl J Med 2015 Oct 5. doi: 10.1056/NEJMoa1413579).
In addition, estimated event-free survival at 30 days was 85.2% with the true intervention and 85.0% with the sham intervention, another nonsignificant difference. These estimates remained similar between the two study groups at 90 days and 1 year. The findings of the primary analysis were confirmed in the “completely concordant” per-protocol analysis, Dr. Meybohm and his associates noted.
ERICCA trial
In the Effect of Remote Ischemic Preconditioning on Clinical Outcomes in Patients Undergoing CABG (ERICCA) study, investigators assessed 1,612 adults undergoing on-pump CABG (with or without valve surgery) using blood cardioplegia at 30 cardiac surgery centers in the United Kingdom during a 3-year period. These patients were randomly assigned to undergo remote ischemic preconditioning with a standard blood pressure cuff on the upper arm for four 5-minute cycles (801 participants) or a sham procedure using a deactivated blood pressure cuff (811 participants) before surgery but while anesthetized, said Dr. Derek J. Hausenloy of the Hatter Cardiovascular Institute, University College London, and his associates.
The primary endpoint – a composite of death from cardiovascular causes, nonfatal MI, coronary revascularization, or stroke within 1 year – was 26.5% with true preconditioning and 27.7% with the sham procedure, a nonsignificant difference. There were no significant differences between the two study groups in any of the individual components of this composite or according to type of anesthesia or the interval between preconditioning and surgical incision.
These findings remained strongly consistent across all subgroups of patients evaluated, regardless of troponin levels, inotrope score, presence or absence of kidney injury, degree of kidney injury, length of ICU stay, length of hospital stay, or performance on 6-minute walk test, Dr. Hausenloy and his associates said (N Engl J Med. 2015 Oct 5. doi: 10.1056/NEJMoa1413534).
In both trials, the rate of adverse effects from remote ischemic preconditioning was the same between the true and the sham procedures, and the only adverse effect considered to be related to preconditioning was an increased incidence of skin petechiae (4.4% vs. 0.2%) in the ERICCA study.
The investigators’ financial disclosures are available at NEJM.org.
The conclusions from the RIPHeart study and the ERRICA study are definitive: Remote ischemic preconditioning is ineffective in adults undergoing on-pump cardiac surgery.
We do not yet understand why. Cardiopulmonary bypass itself, as well as hypothermia and cardioplegia, are known to be cardioprotective, so it may be that further cardioprotection is simply not possible. It also might be that concomitant medications, particularly propofol and opioids, diminish or even block the cardioprotective effects of remote ischemic preconditioning.
The most obvious explanation for the negative results of these two large trials is that other cardioprotective measures may have masked the effect of remote ischemic preconditioning or rendered it redundant.
Dr. Michael Zaugg and Eliana Lucchinetti, Ph.D., of the departments of anesthesiology and pain medicine and in the Cardiovascular Research Centre at the University of Alberta, Edmonton, made these remarks in an editorial accompanying the two reports on remote ischemic preconditioning (N Engl J Med. 2015 Oct 5. doi: 10.1056/MEJMe1510338). Their financial disclosures are available at NEJM.org.
The conclusions from the RIPHeart study and the ERRICA study are definitive: Remote ischemic preconditioning is ineffective in adults undergoing on-pump cardiac surgery.
We do not yet understand why. Cardiopulmonary bypass itself, as well as hypothermia and cardioplegia, are known to be cardioprotective, so it may be that further cardioprotection is simply not possible. It also might be that concomitant medications, particularly propofol and opioids, diminish or even block the cardioprotective effects of remote ischemic preconditioning.
The most obvious explanation for the negative results of these two large trials is that other cardioprotective measures may have masked the effect of remote ischemic preconditioning or rendered it redundant.
Dr. Michael Zaugg and Eliana Lucchinetti, Ph.D., of the departments of anesthesiology and pain medicine and in the Cardiovascular Research Centre at the University of Alberta, Edmonton, made these remarks in an editorial accompanying the two reports on remote ischemic preconditioning (N Engl J Med. 2015 Oct 5. doi: 10.1056/MEJMe1510338). Their financial disclosures are available at NEJM.org.
The conclusions from the RIPHeart study and the ERRICA study are definitive: Remote ischemic preconditioning is ineffective in adults undergoing on-pump cardiac surgery.
We do not yet understand why. Cardiopulmonary bypass itself, as well as hypothermia and cardioplegia, are known to be cardioprotective, so it may be that further cardioprotection is simply not possible. It also might be that concomitant medications, particularly propofol and opioids, diminish or even block the cardioprotective effects of remote ischemic preconditioning.
The most obvious explanation for the negative results of these two large trials is that other cardioprotective measures may have masked the effect of remote ischemic preconditioning or rendered it redundant.
Dr. Michael Zaugg and Eliana Lucchinetti, Ph.D., of the departments of anesthesiology and pain medicine and in the Cardiovascular Research Centre at the University of Alberta, Edmonton, made these remarks in an editorial accompanying the two reports on remote ischemic preconditioning (N Engl J Med. 2015 Oct 5. doi: 10.1056/MEJMe1510338). Their financial disclosures are available at NEJM.org.
Remote ischemic preconditioning failed to improve outcomes among higher-risk patients undergoing elective cardiac surgery in two separate large clinical trials reported online Oct. 5 in the New England Journal of Medicine.
Both studies clearly showed that the technique did not provide greater protection of the heart, brain, or kidneys than did a sham technique, failing to improve any of the numerous primary or secondary endpoints or to produce a benefit in any of several subgroups of patients.
Remote ischemic preconditioning involves protecting the heart and other organs against surgery-related acute ischemia/reperfusion injury by first applying brief cycles of ischemia and reperfusion to a remote organ or tissue. It is thought that this stimulus produces a blood-borne response that conveys a protective effect from the remote area to the target organs. This remote preconditioning can be accomplished noninvasively by inflating and deflating a standard blood pressure cuff on the upper arm or thigh for brief periods.
Some early studies indicated that using this technique during cardiovascular surgery improved serum cardiac and renal biomarkers, which implied protection of these organs against ischemia/reperfusion injury. But more recent prospective clinical trials have shown no such benefit. None of these studies were adequately powered to assess the effect on hard clinical endpoints, and most were single center, unblinded, and had no standardized anesthesia regimen.
RIPHeart study
To address these study limitations, the RIPHeart Study investigators performed a prospective double-blind controlled trial among 1,385 adults undergoing elective cardiovascular surgery requiring cardiopulmonary bypass at 14 university hospitals in Germany during a 3-year period. The participants had a mean EuroSCORE (European System for Cardiac Operative Risk Evaluation) of 6 or higher, indicating that most of them were at higher than average risk, and all received the same anesthetic, intravenous propofol. A total of 692 patients were randomly assigned to undergo four 5-minute cycles of upper-arm ischemia/reperfusion after being anesthetized and 693 to undergo sham ischemia/reperfusion on a dummy arm hidden by surgical drapes, said Dr. Patrick Meybohm of the department of anesthesiology, intensive care medicine, and pain therapy at University Hospital Frankfurt and his associates.
The primary endpoint – a composite of death from any cause, nonfatal MI, stroke, or acute renal failure before hospital discharge – occurred in 14.3% of the intervention group and 14.6% of the control group, a nonsignificant difference. Furthermore, no significant differences between the two study groups were seen in any of the individual components of this composite measure, or in any secondary endpoints such as duration of mechanical ventilation, ICU length of stay, hospital length of stay, troponin levels, creatinine levels, onset of atrial fibrillation, or incidence of postoperative delirium. All outcome measures remained similar between the two study groups at 30-day, 90-day, and 1-year follow-ups (N Engl J Med 2015 Oct 5. doi: 10.1056/NEJMoa1413579).
In addition, estimated event-free survival at 30 days was 85.2% with the true intervention and 85.0% with the sham intervention, another nonsignificant difference. These estimates remained similar between the two study groups at 90 days and 1 year. The findings of the primary analysis were confirmed in the “completely concordant” per-protocol analysis, Dr. Meybohm and his associates noted.
ERICCA trial
In the Effect of Remote Ischemic Preconditioning on Clinical Outcomes in Patients Undergoing CABG (ERICCA) study, investigators assessed 1,612 adults undergoing on-pump CABG (with or without valve surgery) using blood cardioplegia at 30 cardiac surgery centers in the United Kingdom during a 3-year period. These patients were randomly assigned to undergo remote ischemic preconditioning with a standard blood pressure cuff on the upper arm for four 5-minute cycles (801 participants) or a sham procedure using a deactivated blood pressure cuff (811 participants) before surgery but while anesthetized, said Dr. Derek J. Hausenloy of the Hatter Cardiovascular Institute, University College London, and his associates.
The primary endpoint – a composite of death from cardiovascular causes, nonfatal MI, coronary revascularization, or stroke within 1 year – was 26.5% with true preconditioning and 27.7% with the sham procedure, a nonsignificant difference. There were no significant differences between the two study groups in any of the individual components of this composite or according to type of anesthesia or the interval between preconditioning and surgical incision.
These findings remained strongly consistent across all subgroups of patients evaluated, regardless of troponin levels, inotrope score, presence or absence of kidney injury, degree of kidney injury, length of ICU stay, length of hospital stay, or performance on 6-minute walk test, Dr. Hausenloy and his associates said (N Engl J Med. 2015 Oct 5. doi: 10.1056/NEJMoa1413534).
In both trials, the rate of adverse effects from remote ischemic preconditioning was the same between the true and the sham procedures, and the only adverse effect considered to be related to preconditioning was an increased incidence of skin petechiae (4.4% vs. 0.2%) in the ERICCA study.
The investigators’ financial disclosures are available at NEJM.org.
Remote ischemic preconditioning failed to improve outcomes among higher-risk patients undergoing elective cardiac surgery in two separate large clinical trials reported online Oct. 5 in the New England Journal of Medicine.
Both studies clearly showed that the technique did not provide greater protection of the heart, brain, or kidneys than did a sham technique, failing to improve any of the numerous primary or secondary endpoints or to produce a benefit in any of several subgroups of patients.
Remote ischemic preconditioning involves protecting the heart and other organs against surgery-related acute ischemia/reperfusion injury by first applying brief cycles of ischemia and reperfusion to a remote organ or tissue. It is thought that this stimulus produces a blood-borne response that conveys a protective effect from the remote area to the target organs. This remote preconditioning can be accomplished noninvasively by inflating and deflating a standard blood pressure cuff on the upper arm or thigh for brief periods.
Some early studies indicated that using this technique during cardiovascular surgery improved serum cardiac and renal biomarkers, which implied protection of these organs against ischemia/reperfusion injury. But more recent prospective clinical trials have shown no such benefit. None of these studies were adequately powered to assess the effect on hard clinical endpoints, and most were single center, unblinded, and had no standardized anesthesia regimen.
RIPHeart study
To address these study limitations, the RIPHeart Study investigators performed a prospective double-blind controlled trial among 1,385 adults undergoing elective cardiovascular surgery requiring cardiopulmonary bypass at 14 university hospitals in Germany during a 3-year period. The participants had a mean EuroSCORE (European System for Cardiac Operative Risk Evaluation) of 6 or higher, indicating that most of them were at higher than average risk, and all received the same anesthetic, intravenous propofol. A total of 692 patients were randomly assigned to undergo four 5-minute cycles of upper-arm ischemia/reperfusion after being anesthetized and 693 to undergo sham ischemia/reperfusion on a dummy arm hidden by surgical drapes, said Dr. Patrick Meybohm of the department of anesthesiology, intensive care medicine, and pain therapy at University Hospital Frankfurt and his associates.
The primary endpoint – a composite of death from any cause, nonfatal MI, stroke, or acute renal failure before hospital discharge – occurred in 14.3% of the intervention group and 14.6% of the control group, a nonsignificant difference. Furthermore, no significant differences between the two study groups were seen in any of the individual components of this composite measure, or in any secondary endpoints such as duration of mechanical ventilation, ICU length of stay, hospital length of stay, troponin levels, creatinine levels, onset of atrial fibrillation, or incidence of postoperative delirium. All outcome measures remained similar between the two study groups at 30-day, 90-day, and 1-year follow-ups (N Engl J Med 2015 Oct 5. doi: 10.1056/NEJMoa1413579).
In addition, estimated event-free survival at 30 days was 85.2% with the true intervention and 85.0% with the sham intervention, another nonsignificant difference. These estimates remained similar between the two study groups at 90 days and 1 year. The findings of the primary analysis were confirmed in the “completely concordant” per-protocol analysis, Dr. Meybohm and his associates noted.
ERICCA trial
In the Effect of Remote Ischemic Preconditioning on Clinical Outcomes in Patients Undergoing CABG (ERICCA) study, investigators assessed 1,612 adults undergoing on-pump CABG (with or without valve surgery) using blood cardioplegia at 30 cardiac surgery centers in the United Kingdom during a 3-year period. These patients were randomly assigned to undergo remote ischemic preconditioning with a standard blood pressure cuff on the upper arm for four 5-minute cycles (801 participants) or a sham procedure using a deactivated blood pressure cuff (811 participants) before surgery but while anesthetized, said Dr. Derek J. Hausenloy of the Hatter Cardiovascular Institute, University College London, and his associates.
The primary endpoint – a composite of death from cardiovascular causes, nonfatal MI, coronary revascularization, or stroke within 1 year – was 26.5% with true preconditioning and 27.7% with the sham procedure, a nonsignificant difference. There were no significant differences between the two study groups in any of the individual components of this composite or according to type of anesthesia or the interval between preconditioning and surgical incision.
These findings remained strongly consistent across all subgroups of patients evaluated, regardless of troponin levels, inotrope score, presence or absence of kidney injury, degree of kidney injury, length of ICU stay, length of hospital stay, or performance on 6-minute walk test, Dr. Hausenloy and his associates said (N Engl J Med. 2015 Oct 5. doi: 10.1056/NEJMoa1413534).
In both trials, the rate of adverse effects from remote ischemic preconditioning was the same between the true and the sham procedures, and the only adverse effect considered to be related to preconditioning was an increased incidence of skin petechiae (4.4% vs. 0.2%) in the ERICCA study.
The investigators’ financial disclosures are available at NEJM.org.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Readmissions for C. difficile infections high among elderly
LAS VEGAS – More than one in 10 patients with Clostridium difficile infection at the time of hospital discharge are readmitted for C. difficile infection within 90 days, according to findings from a review of Medicare data from 2009 to 2011.
Of a random sample of nearly 900,000 Part A inpatients and Part D prescription drug claimants during the study period, about 8,500 were hospitalized with a primary or secondary diagnosis of C. difficile infection, and of 7,042 of those who were discharged alive and who were eligible for the study, 945 (13.4%) were readmitted within 90 days, Dr. Charles M. Psoinos reported at the annual meeting of the American Association for the Surgery of Trauma.
Compared with 1,900 patients not readmitted for any reason, those who were readmitted had more baseline comorbidities (average Elixhauser index, 5.9 vs. 4.7), and a significantly shorter length of stay during the index hospitalization (9.2 vs. 11.8 days), and those older than 95 years were twice as likely as those aged 65-70 years to be readmitted, as were those with an emergent vs. nonemergent index hospitalization, said Dr. Psoinos of the University of Massachusetts, Worcester.
Further, the readmission rate was lower in the 39% of patients discharged on oral metronidazole (19%), and in the 12% discharged on oral vancomycin (28%), than among the 38% discharged with no ongoing treatment (48%), while those discharged on both oral metronidazole and vancomycin were at increased risk for readmission (odds ratio, 1.29), he said.
The 90-day all cause mortality rate was nearly doubled in those who were readmitted, compared with those who were not (17.8% vs. 8.9%; OR, 1.77), he said.
Patients who were and were not readmitted did not differ significantly with respect to age (mean of about 80 years) and race distribution, and the outcomes were adjusted for the differences in baseline comorbidities and other confounding factors.
The findings could have important implications for reducing readmissions among Medicare beneficiaries, Dr. Psoinos said.
The incidence of C. difficile infections has increased nearly eightfold in the elderly population over the last several decades, and the elderly now account for more than 70% of hospitalized patients with such infections. Recurrence rates range from 5% to 31% after cessation of therapy, and readmission rates are similar, he explained, noting that treatment recommendations for C. difficile infections are commonly based on symptoms and their severity, with oral metronidazole recommended for mild and moderate disease, vancomycin only for severe disease, and dual therapy for complicated severe disease.
Though limited by the retrospective design of the study, the findings suggest that C. difficile patients discharged from the hospital may benefit from ongoing monotherapy treatment to reduce subclinical infections and induce long-term eradication, and that elderly patients on dual therapy may benefit from continued hospitalization until they are appropriate for discharge on monotherapy.
These strategies could reduce the rate of readmissions, Dr. Psoinos concluded.
Dr. Psoinos reported having no relevant financial conflicts.
LAS VEGAS – More than one in 10 patients with Clostridium difficile infection at the time of hospital discharge are readmitted for C. difficile infection within 90 days, according to findings from a review of Medicare data from 2009 to 2011.
Of a random sample of nearly 900,000 Part A inpatients and Part D prescription drug claimants during the study period, about 8,500 were hospitalized with a primary or secondary diagnosis of C. difficile infection, and of 7,042 of those who were discharged alive and who were eligible for the study, 945 (13.4%) were readmitted within 90 days, Dr. Charles M. Psoinos reported at the annual meeting of the American Association for the Surgery of Trauma.
Compared with 1,900 patients not readmitted for any reason, those who were readmitted had more baseline comorbidities (average Elixhauser index, 5.9 vs. 4.7), and a significantly shorter length of stay during the index hospitalization (9.2 vs. 11.8 days), and those older than 95 years were twice as likely as those aged 65-70 years to be readmitted, as were those with an emergent vs. nonemergent index hospitalization, said Dr. Psoinos of the University of Massachusetts, Worcester.
Further, the readmission rate was lower in the 39% of patients discharged on oral metronidazole (19%), and in the 12% discharged on oral vancomycin (28%), than among the 38% discharged with no ongoing treatment (48%), while those discharged on both oral metronidazole and vancomycin were at increased risk for readmission (odds ratio, 1.29), he said.
The 90-day all cause mortality rate was nearly doubled in those who were readmitted, compared with those who were not (17.8% vs. 8.9%; OR, 1.77), he said.
Patients who were and were not readmitted did not differ significantly with respect to age (mean of about 80 years) and race distribution, and the outcomes were adjusted for the differences in baseline comorbidities and other confounding factors.
The findings could have important implications for reducing readmissions among Medicare beneficiaries, Dr. Psoinos said.
The incidence of C. difficile infections has increased nearly eightfold in the elderly population over the last several decades, and the elderly now account for more than 70% of hospitalized patients with such infections. Recurrence rates range from 5% to 31% after cessation of therapy, and readmission rates are similar, he explained, noting that treatment recommendations for C. difficile infections are commonly based on symptoms and their severity, with oral metronidazole recommended for mild and moderate disease, vancomycin only for severe disease, and dual therapy for complicated severe disease.
Though limited by the retrospective design of the study, the findings suggest that C. difficile patients discharged from the hospital may benefit from ongoing monotherapy treatment to reduce subclinical infections and induce long-term eradication, and that elderly patients on dual therapy may benefit from continued hospitalization until they are appropriate for discharge on monotherapy.
These strategies could reduce the rate of readmissions, Dr. Psoinos concluded.
Dr. Psoinos reported having no relevant financial conflicts.
LAS VEGAS – More than one in 10 patients with Clostridium difficile infection at the time of hospital discharge are readmitted for C. difficile infection within 90 days, according to findings from a review of Medicare data from 2009 to 2011.
Of a random sample of nearly 900,000 Part A inpatients and Part D prescription drug claimants during the study period, about 8,500 were hospitalized with a primary or secondary diagnosis of C. difficile infection, and of 7,042 of those who were discharged alive and who were eligible for the study, 945 (13.4%) were readmitted within 90 days, Dr. Charles M. Psoinos reported at the annual meeting of the American Association for the Surgery of Trauma.
Compared with 1,900 patients not readmitted for any reason, those who were readmitted had more baseline comorbidities (average Elixhauser index, 5.9 vs. 4.7), and a significantly shorter length of stay during the index hospitalization (9.2 vs. 11.8 days), and those older than 95 years were twice as likely as those aged 65-70 years to be readmitted, as were those with an emergent vs. nonemergent index hospitalization, said Dr. Psoinos of the University of Massachusetts, Worcester.
Further, the readmission rate was lower in the 39% of patients discharged on oral metronidazole (19%), and in the 12% discharged on oral vancomycin (28%), than among the 38% discharged with no ongoing treatment (48%), while those discharged on both oral metronidazole and vancomycin were at increased risk for readmission (odds ratio, 1.29), he said.
The 90-day all cause mortality rate was nearly doubled in those who were readmitted, compared with those who were not (17.8% vs. 8.9%; OR, 1.77), he said.
Patients who were and were not readmitted did not differ significantly with respect to age (mean of about 80 years) and race distribution, and the outcomes were adjusted for the differences in baseline comorbidities and other confounding factors.
The findings could have important implications for reducing readmissions among Medicare beneficiaries, Dr. Psoinos said.
The incidence of C. difficile infections has increased nearly eightfold in the elderly population over the last several decades, and the elderly now account for more than 70% of hospitalized patients with such infections. Recurrence rates range from 5% to 31% after cessation of therapy, and readmission rates are similar, he explained, noting that treatment recommendations for C. difficile infections are commonly based on symptoms and their severity, with oral metronidazole recommended for mild and moderate disease, vancomycin only for severe disease, and dual therapy for complicated severe disease.
Though limited by the retrospective design of the study, the findings suggest that C. difficile patients discharged from the hospital may benefit from ongoing monotherapy treatment to reduce subclinical infections and induce long-term eradication, and that elderly patients on dual therapy may benefit from continued hospitalization until they are appropriate for discharge on monotherapy.
These strategies could reduce the rate of readmissions, Dr. Psoinos concluded.
Dr. Psoinos reported having no relevant financial conflicts.
AT THE AAST ANNUAL MEETING
Key clinical point: More than 1 in 10 patients with Clostridium difficile infection at the time of hospital discharge are readmitted for C. difficile infection within 90 days, according to findings from a review of Medicare data from 2009 to 2011.
Major finding: Of 7,042 discharged patients, 945 (13.4%) were readmitted within 90 days.
Data source: A retrospective cohort study of about 900,000 Medicare beneficiaries.
Disclosures: Dr. Psoinos reported having no relevant financial disclosures.
IPC maintains first-line status in preventing DVT in most surgical patients
Intermittent pneumatic compression remains the consensus choice as the sole prophylactic agent for deep vein thrombosis in low- or moderate-risk surgical patients, according to a literature analysis published online ahead of print in September in the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
Dr. Nirvana Sadaghianloo of the University of Nice (France) Sophia Antipolis and Dr. Alan Dardik of Yale University in New Haven, Conn., used the MEDLINE and Cochrane libraries to find individual studies and meta-analyses published in English since 2011 assessing the efficacy of intermittent pneumatic compression (IPC) in preventing deep vein thrombosis (DVT), which included the American College of Chest Physicians ninth edition guidelines (2012). They stated that, although the overall quality of studies regarding the use of IPC was low, IPC showed efficacy in prevention of DVT for more than 30 years (J Vasc Surg Venous Lymphat Disord. 2015 doi: 10.1016/j.jvsv.2015.07.006).
“IPC represents a good alternative to pharmacologic agents when the risk of thrombosis is moderate or low or when the risk of bleeding is high or may have serious consequences for the patient,” they stated.
However, they also found that most recommendations suggested that, in high-risk patients, IPC plays a role primarily as an additional modality to provide additional benefit in preventing DVT when is used in combination with pharmacologic therapy. They highlighted how the choice of any thromboprophylactic agent required a systematic risk assessment as a critical prerequisite.
Overall, risk stratification was most frequently assessed by the Caprini or Rogers score for most general, abdominal-pelvic, bariatric, vascular, plastic, and gynecologic surgery patients and by the Padua Prediction Score for hospitalized medical patients. In addition, major orthopedic surgery patients and stroke patients with restricted mobility were usually considered high risk, Dr. Sadaghianloo and Dr. Dardik said.
From their assessment of the literature, they determined that “further studies are needed to assess practical clinical questions that remain unanswered, including optimal cuff length and location, sequence and duration of pressure, and whether use of IPC in an outpatient setting can be effective and achieve good compliance.”
The authors reported that they had no conflicts of interest.
Intermittent pneumatic compression remains the consensus choice as the sole prophylactic agent for deep vein thrombosis in low- or moderate-risk surgical patients, according to a literature analysis published online ahead of print in September in the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
Dr. Nirvana Sadaghianloo of the University of Nice (France) Sophia Antipolis and Dr. Alan Dardik of Yale University in New Haven, Conn., used the MEDLINE and Cochrane libraries to find individual studies and meta-analyses published in English since 2011 assessing the efficacy of intermittent pneumatic compression (IPC) in preventing deep vein thrombosis (DVT), which included the American College of Chest Physicians ninth edition guidelines (2012). They stated that, although the overall quality of studies regarding the use of IPC was low, IPC showed efficacy in prevention of DVT for more than 30 years (J Vasc Surg Venous Lymphat Disord. 2015 doi: 10.1016/j.jvsv.2015.07.006).
“IPC represents a good alternative to pharmacologic agents when the risk of thrombosis is moderate or low or when the risk of bleeding is high or may have serious consequences for the patient,” they stated.
However, they also found that most recommendations suggested that, in high-risk patients, IPC plays a role primarily as an additional modality to provide additional benefit in preventing DVT when is used in combination with pharmacologic therapy. They highlighted how the choice of any thromboprophylactic agent required a systematic risk assessment as a critical prerequisite.
Overall, risk stratification was most frequently assessed by the Caprini or Rogers score for most general, abdominal-pelvic, bariatric, vascular, plastic, and gynecologic surgery patients and by the Padua Prediction Score for hospitalized medical patients. In addition, major orthopedic surgery patients and stroke patients with restricted mobility were usually considered high risk, Dr. Sadaghianloo and Dr. Dardik said.
From their assessment of the literature, they determined that “further studies are needed to assess practical clinical questions that remain unanswered, including optimal cuff length and location, sequence and duration of pressure, and whether use of IPC in an outpatient setting can be effective and achieve good compliance.”
The authors reported that they had no conflicts of interest.
Intermittent pneumatic compression remains the consensus choice as the sole prophylactic agent for deep vein thrombosis in low- or moderate-risk surgical patients, according to a literature analysis published online ahead of print in September in the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
Dr. Nirvana Sadaghianloo of the University of Nice (France) Sophia Antipolis and Dr. Alan Dardik of Yale University in New Haven, Conn., used the MEDLINE and Cochrane libraries to find individual studies and meta-analyses published in English since 2011 assessing the efficacy of intermittent pneumatic compression (IPC) in preventing deep vein thrombosis (DVT), which included the American College of Chest Physicians ninth edition guidelines (2012). They stated that, although the overall quality of studies regarding the use of IPC was low, IPC showed efficacy in prevention of DVT for more than 30 years (J Vasc Surg Venous Lymphat Disord. 2015 doi: 10.1016/j.jvsv.2015.07.006).
“IPC represents a good alternative to pharmacologic agents when the risk of thrombosis is moderate or low or when the risk of bleeding is high or may have serious consequences for the patient,” they stated.
However, they also found that most recommendations suggested that, in high-risk patients, IPC plays a role primarily as an additional modality to provide additional benefit in preventing DVT when is used in combination with pharmacologic therapy. They highlighted how the choice of any thromboprophylactic agent required a systematic risk assessment as a critical prerequisite.
Overall, risk stratification was most frequently assessed by the Caprini or Rogers score for most general, abdominal-pelvic, bariatric, vascular, plastic, and gynecologic surgery patients and by the Padua Prediction Score for hospitalized medical patients. In addition, major orthopedic surgery patients and stroke patients with restricted mobility were usually considered high risk, Dr. Sadaghianloo and Dr. Dardik said.
From their assessment of the literature, they determined that “further studies are needed to assess practical clinical questions that remain unanswered, including optimal cuff length and location, sequence and duration of pressure, and whether use of IPC in an outpatient setting can be effective and achieve good compliance.”
The authors reported that they had no conflicts of interest.
FROM JOURNAL OF VASCULAR SURGERY: VENOUS AND LYMPHATIC DISORDERS
Key clinical point: IPC is efficacious as the sole prophylactic agent in low- or moderate-risk surgical patients and in patients with high risk of bleeding with drug therapy.
Major finding: In high-risk patients, IPC is an added modality for preventing DVT in combination with pharmacologic prophylaxis.
Data source: Researchers performed an assessment of the literature in English since 2011 in MEDLINE and the Cochrane libraries.
Disclosures: The authors reported that they had no conflicts of interest.
Hospitalization driving bariatric surgery cost differences
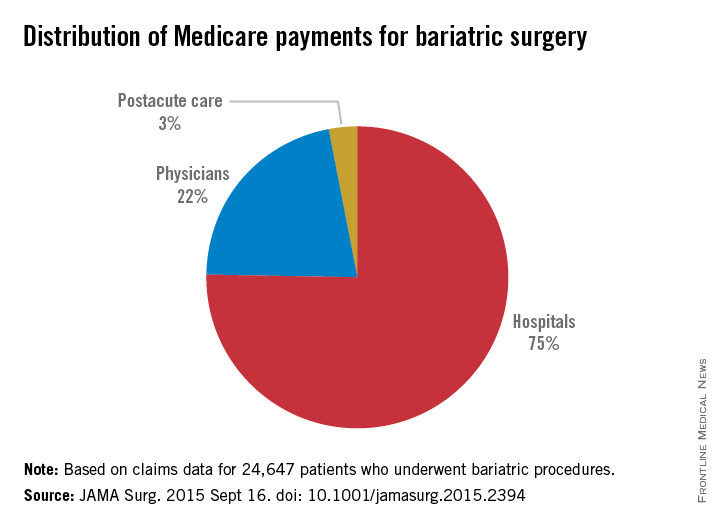
Medicare payments to hospitals for bariatric operations varied by nearly $2,000 per episode of care, mostly because of differences in costs incurred in the initial – or index – hospitalization.
The findings, published online Sept. 16 in JAMA Surgery, offer hospitals a guide to where cost variation is highest (doi:10.1001/jamasurg.2015.2394) for these procedures.
Knowing where costs vary the most is particularly important if hospitals opt to accept bundled Medicare payments for bariatric procedures, which are a proposed addition to 48 other episodes of care that can currently be reimbursed in this way. Under bundled care payment programs, hospitals receive a single payment for all services related to a surgery or other episode of care, thereby accepting more risk when inefficiencies occur.
For their research, Dr. Tyler R. Grenda and his colleagues at University of Michigan, Ann Arbor, Center for Healthcare Outcomes and Policy, looked at claims data for 24,647 patients receiving bariatric procedures at 463 hospitals during 2011-2012.
Operations included laparoscopic gastric banding, laparoscopic Roux-en-Y gastric bypass, and open Roux-en-Y gastric bypass, with fewer than 5% of patients receiving other interventions. Mean total payments varied from $11,086 to $13,073 per episode of care, defined as index hospitalization through 30 days postdischarge, for a 16.5% difference between the lowest and highest hospital quartiles.
The index hospitalization was responsible for the largest portion of total payments (75%), seen in the study, followed by physician services (21%) and postacute care services (2.8%).
The large share of costs incurred during the index hospitalization was “likely owing to inpatient complications that drive [diagnosis-related group] up-coding,” the authors wrote, noting that DRG with complications result in higher Medicare payments.
Dr. Grenda and his colleagues concluded that bariatric surgery “appears to have a distinct pattern of hospital cost variation” unlike that seen in other procedures that have been studied to identify drivers of cost differences. “This difference in the pattern of variation emphasizes the importance of understanding cost variation specific to each procedure,” they wrote.
For example, a study that looked at hip fracture repair found that postacute care accounted for a large portion of variation in payments, while less variation was seen for the index hospitalization (Health Serv Res. 2010;45[6, pt 1]:1783-95).
In the current policy environment, in which bundled payments are seen as a way to shift cost accountability to hospitals, “a detailed understanding of variation in the costs for bariatric surgery will be essential for hospitals to identify areas of risk and opportunities for improvement,” the researchers wrote in their analysis.
Dr. Grenda and his colleagues’ research was funded by Agency for Healthcare Research and Quality. One coauthor and the supervisor of the study, Dr. Justin Dimnick, disclosed a financial relationship with ArborMetrix, a health care analytics firm not involved with the study; he is also an editor of JAMA Surgery, which published the study.
Medicare payments to hospitals for bariatric operations varied by nearly $2,000 per episode of care, mostly because of differences in costs incurred in the initial – or index – hospitalization.
The findings, published online Sept. 16 in JAMA Surgery, offer hospitals a guide to where cost variation is highest (doi:10.1001/jamasurg.2015.2394) for these procedures.
Knowing where costs vary the most is particularly important if hospitals opt to accept bundled Medicare payments for bariatric procedures, which are a proposed addition to 48 other episodes of care that can currently be reimbursed in this way. Under bundled care payment programs, hospitals receive a single payment for all services related to a surgery or other episode of care, thereby accepting more risk when inefficiencies occur.
For their research, Dr. Tyler R. Grenda and his colleagues at University of Michigan, Ann Arbor, Center for Healthcare Outcomes and Policy, looked at claims data for 24,647 patients receiving bariatric procedures at 463 hospitals during 2011-2012.
Operations included laparoscopic gastric banding, laparoscopic Roux-en-Y gastric bypass, and open Roux-en-Y gastric bypass, with fewer than 5% of patients receiving other interventions. Mean total payments varied from $11,086 to $13,073 per episode of care, defined as index hospitalization through 30 days postdischarge, for a 16.5% difference between the lowest and highest hospital quartiles.
The index hospitalization was responsible for the largest portion of total payments (75%), seen in the study, followed by physician services (21%) and postacute care services (2.8%).
The large share of costs incurred during the index hospitalization was “likely owing to inpatient complications that drive [diagnosis-related group] up-coding,” the authors wrote, noting that DRG with complications result in higher Medicare payments.
Dr. Grenda and his colleagues concluded that bariatric surgery “appears to have a distinct pattern of hospital cost variation” unlike that seen in other procedures that have been studied to identify drivers of cost differences. “This difference in the pattern of variation emphasizes the importance of understanding cost variation specific to each procedure,” they wrote.
For example, a study that looked at hip fracture repair found that postacute care accounted for a large portion of variation in payments, while less variation was seen for the index hospitalization (Health Serv Res. 2010;45[6, pt 1]:1783-95).
In the current policy environment, in which bundled payments are seen as a way to shift cost accountability to hospitals, “a detailed understanding of variation in the costs for bariatric surgery will be essential for hospitals to identify areas of risk and opportunities for improvement,” the researchers wrote in their analysis.
Dr. Grenda and his colleagues’ research was funded by Agency for Healthcare Research and Quality. One coauthor and the supervisor of the study, Dr. Justin Dimnick, disclosed a financial relationship with ArborMetrix, a health care analytics firm not involved with the study; he is also an editor of JAMA Surgery, which published the study.
Medicare payments to hospitals for bariatric operations varied by nearly $2,000 per episode of care, mostly because of differences in costs incurred in the initial – or index – hospitalization.
The findings, published online Sept. 16 in JAMA Surgery, offer hospitals a guide to where cost variation is highest (doi:10.1001/jamasurg.2015.2394) for these procedures.
Knowing where costs vary the most is particularly important if hospitals opt to accept bundled Medicare payments for bariatric procedures, which are a proposed addition to 48 other episodes of care that can currently be reimbursed in this way. Under bundled care payment programs, hospitals receive a single payment for all services related to a surgery or other episode of care, thereby accepting more risk when inefficiencies occur.
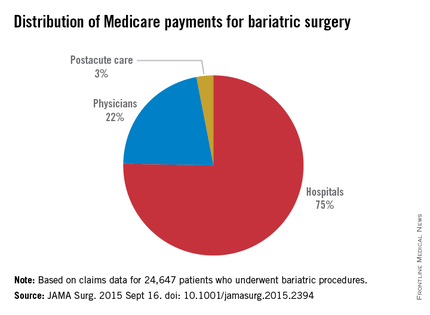
For their research, Dr. Tyler R. Grenda and his colleagues at University of Michigan, Ann Arbor, Center for Healthcare Outcomes and Policy, looked at claims data for 24,647 patients receiving bariatric procedures at 463 hospitals during 2011-2012.
Operations included laparoscopic gastric banding, laparoscopic Roux-en-Y gastric bypass, and open Roux-en-Y gastric bypass, with fewer than 5% of patients receiving other interventions. Mean total payments varied from $11,086 to $13,073 per episode of care, defined as index hospitalization through 30 days postdischarge, for a 16.5% difference between the lowest and highest hospital quartiles.
The index hospitalization was responsible for the largest portion of total payments (75%), seen in the study, followed by physician services (21%) and postacute care services (2.8%).
The large share of costs incurred during the index hospitalization was “likely owing to inpatient complications that drive [diagnosis-related group] up-coding,” the authors wrote, noting that DRG with complications result in higher Medicare payments.
Dr. Grenda and his colleagues concluded that bariatric surgery “appears to have a distinct pattern of hospital cost variation” unlike that seen in other procedures that have been studied to identify drivers of cost differences. “This difference in the pattern of variation emphasizes the importance of understanding cost variation specific to each procedure,” they wrote.
For example, a study that looked at hip fracture repair found that postacute care accounted for a large portion of variation in payments, while less variation was seen for the index hospitalization (Health Serv Res. 2010;45[6, pt 1]:1783-95).
In the current policy environment, in which bundled payments are seen as a way to shift cost accountability to hospitals, “a detailed understanding of variation in the costs for bariatric surgery will be essential for hospitals to identify areas of risk and opportunities for improvement,” the researchers wrote in their analysis.
Dr. Grenda and his colleagues’ research was funded by Agency for Healthcare Research and Quality. One coauthor and the supervisor of the study, Dr. Justin Dimnick, disclosed a financial relationship with ArborMetrix, a health care analytics firm not involved with the study; he is also an editor of JAMA Surgery, which published the study.
FROM JAMA SURGERY
Key clinical point: Initial hospitalization costs account for the lion’s share of cost variation for bariatric operations covered under Medicare.
Major finding: Mean total costs varied from $11,086 to about $13,073 per care episode, a 16.5% difference between the lowest- and highest-quartile hospitals; index hospitalizations accounted for 75% of payments, with less spent on physician fees and aftercare.
Data source: Medicare claims data for nearly 25,000 bariatric procedures performed at U.S. hospitals during 2011-2012.
Disclosures: Study was sponsored by the Agency for Healthcare Research and Quality; one coauthor disclosed financial relationship with a health analytics firm and journal editorship.
Respiratory problems make adenotonsillectomy recovery worse for kids
Respiratory compromise and secondary hemorrhage were the most common early side effects in children who had adenotonsillectomies; children with obstructive sleep apnea (OSA) have nearly five times more respiratory complications after surgery than children without OSA, a multistudy review concluded.
Graziela De Luca Canto, Ph.D., of the Federal University of Santa Catarina, Brazil, and her associates performed a data review by identifying 1,254 different citations found via electronic database searches; after eliminations, only 23 studies were included in the final analysis. Although children with OSA have nearly five times more respiratory complications after adenotonsillectomy than their peers, (odds ratio, 4.90), they are less likely to have postoperative bleeding, compared with children without OSA (OR, 0.41). Among both groups, the most frequent complication was respiratory compromise (9.4%), followed by secondary hemorrhage (2.6%).
Because children with OSA are more likely to require supplemental oxygen, oral or nasal airway insertion, or assisted ventilation in the immediate postoperative period than their peers, the authors suggested that anesthesiologists would be wise to screen patients for snoring, airway dysfunction, and other airway anatomic disorders before performing surgery.
“Children with OSA are clearly at higher anesthetic risk than are patients with normal upper airway function. … Despite the pressure to reduce costs, both surgeons and anesthesiologists should improve screening procedures, perhaps develop alternate surgical approaches, to decrease the risks,” the investigators wrote.
Read the full article in Pediatrics 2015 (doi: 10.1542/peds.2015-1283).
Respiratory compromise and secondary hemorrhage were the most common early side effects in children who had adenotonsillectomies; children with obstructive sleep apnea (OSA) have nearly five times more respiratory complications after surgery than children without OSA, a multistudy review concluded.
Graziela De Luca Canto, Ph.D., of the Federal University of Santa Catarina, Brazil, and her associates performed a data review by identifying 1,254 different citations found via electronic database searches; after eliminations, only 23 studies were included in the final analysis. Although children with OSA have nearly five times more respiratory complications after adenotonsillectomy than their peers, (odds ratio, 4.90), they are less likely to have postoperative bleeding, compared with children without OSA (OR, 0.41). Among both groups, the most frequent complication was respiratory compromise (9.4%), followed by secondary hemorrhage (2.6%).
Because children with OSA are more likely to require supplemental oxygen, oral or nasal airway insertion, or assisted ventilation in the immediate postoperative period than their peers, the authors suggested that anesthesiologists would be wise to screen patients for snoring, airway dysfunction, and other airway anatomic disorders before performing surgery.
“Children with OSA are clearly at higher anesthetic risk than are patients with normal upper airway function. … Despite the pressure to reduce costs, both surgeons and anesthesiologists should improve screening procedures, perhaps develop alternate surgical approaches, to decrease the risks,” the investigators wrote.
Read the full article in Pediatrics 2015 (doi: 10.1542/peds.2015-1283).
Respiratory compromise and secondary hemorrhage were the most common early side effects in children who had adenotonsillectomies; children with obstructive sleep apnea (OSA) have nearly five times more respiratory complications after surgery than children without OSA, a multistudy review concluded.
Graziela De Luca Canto, Ph.D., of the Federal University of Santa Catarina, Brazil, and her associates performed a data review by identifying 1,254 different citations found via electronic database searches; after eliminations, only 23 studies were included in the final analysis. Although children with OSA have nearly five times more respiratory complications after adenotonsillectomy than their peers, (odds ratio, 4.90), they are less likely to have postoperative bleeding, compared with children without OSA (OR, 0.41). Among both groups, the most frequent complication was respiratory compromise (9.4%), followed by secondary hemorrhage (2.6%).
Because children with OSA are more likely to require supplemental oxygen, oral or nasal airway insertion, or assisted ventilation in the immediate postoperative period than their peers, the authors suggested that anesthesiologists would be wise to screen patients for snoring, airway dysfunction, and other airway anatomic disorders before performing surgery.
“Children with OSA are clearly at higher anesthetic risk than are patients with normal upper airway function. … Despite the pressure to reduce costs, both surgeons and anesthesiologists should improve screening procedures, perhaps develop alternate surgical approaches, to decrease the risks,” the investigators wrote.
Read the full article in Pediatrics 2015 (doi: 10.1542/peds.2015-1283).
FROM PEDIATRICS
Intraperitoneal bupivacaine disappoints in postop pain relief
NEW YORK – While some evidence in the surgical literature suggests that intraperitoneal bupivacaine reduces postoperative pain scores and narcotic use, a new randomized controlled trial shows no significant improvement in patients undergoing robot-assisted total laparoscopic hysterectomy.
“Despite evidence of benefit in laparoscopic surgery, there does not appear to be a benefit for using intraperitoneal bupivacaine. We need a larger sample size to study this,” Dr. Allan Klapper said at the annual Minimally Invasive Surgery Week.
The uptake of robot-assisted total laparoscopic hysterectomy increased by 9.5% in the United States, and hospitals with robotic capabilities perform 22.4% of hysterectomies with this technique, according to Dr. Klapper, an ob.gyn. at West Pennsylvania Allegheny Health System in Pittsburgh. Minimally invasive surgery, however, does not completely eliminate postoperative pain, and between one-third and two-thirds of patients report pain following such surgery.
Intraperitoneal bupivacaine (IB) was selected for the study because of positive reports in small studies of patients undergoing laparoscopic cholecystectomy and gynecologic procedures, Dr. Klapper explained. He noted that the positive studies were of poor quality, but other studies – also of poor quality – had negative results.
To investigate the role of IB in reducing postoperative pain and narcotic requirements in patients undergoing robot-assisted total laparoscopic hysterectomy, Dr. Klapper and his colleagues launched a prospective, double-blind, randomized, placebo-controlled trial comparing IB to normal saline in 41 patients managed with a standardized postoperative analgesic regimen.
Baseline characteristics showed no differences between the two groups in surgical indications, body mass index, operating room time, number of previous surgeries, and the percentage of patients undergoing lymph node dissection. Patients were excluded from the analysis if they converted to laparotomy, were allergic to IB, or were currently on treatment for chronic pain.
Complete data on pain response, as assessed by the visual analog scale, was available for 29 of the 41 patients. No significant differences in postoperative pain scores were observed between the two groups at 1, 16, 18, and 24 hours. Further, there was no significant difference in morphine dose between the IB and normal saline groups.
“One finding was the opposite of what I would have expected. Patients who underwent lymph node dissection used significantly less narcotic analgesic [P = .03],” Dr. Klapper told the audience.
Study strengths were the prospective, randomized design, and its being adequately powered to detect a significant difference between the two groups. But the study was conducted at a single institution and did not include data beyond 24 hours. Also, Dr. Klapper said that perhaps results should have been stratified according to indications for surgery.
“There is more and more pressure on us to achieve higher patient satisfaction scores. Soon down the line, patient satisfaction will become a metric for compensation. We need to focus on what we can do to improve patient satisfaction scores and experience,” Dr. Klapper said. “A larger sample of gynecologic oncology patients is needed to further support these conclusions, and we need to fine tune to avoid the problems in this study.”
The meeting was presented by the Society of Laparoendoscopic Surgeons and affiliated societies. Dr. Klapper reported that he is on the speakers bureau for Astellas.
NEW YORK – While some evidence in the surgical literature suggests that intraperitoneal bupivacaine reduces postoperative pain scores and narcotic use, a new randomized controlled trial shows no significant improvement in patients undergoing robot-assisted total laparoscopic hysterectomy.
“Despite evidence of benefit in laparoscopic surgery, there does not appear to be a benefit for using intraperitoneal bupivacaine. We need a larger sample size to study this,” Dr. Allan Klapper said at the annual Minimally Invasive Surgery Week.
The uptake of robot-assisted total laparoscopic hysterectomy increased by 9.5% in the United States, and hospitals with robotic capabilities perform 22.4% of hysterectomies with this technique, according to Dr. Klapper, an ob.gyn. at West Pennsylvania Allegheny Health System in Pittsburgh. Minimally invasive surgery, however, does not completely eliminate postoperative pain, and between one-third and two-thirds of patients report pain following such surgery.
Intraperitoneal bupivacaine (IB) was selected for the study because of positive reports in small studies of patients undergoing laparoscopic cholecystectomy and gynecologic procedures, Dr. Klapper explained. He noted that the positive studies were of poor quality, but other studies – also of poor quality – had negative results.
To investigate the role of IB in reducing postoperative pain and narcotic requirements in patients undergoing robot-assisted total laparoscopic hysterectomy, Dr. Klapper and his colleagues launched a prospective, double-blind, randomized, placebo-controlled trial comparing IB to normal saline in 41 patients managed with a standardized postoperative analgesic regimen.
Baseline characteristics showed no differences between the two groups in surgical indications, body mass index, operating room time, number of previous surgeries, and the percentage of patients undergoing lymph node dissection. Patients were excluded from the analysis if they converted to laparotomy, were allergic to IB, or were currently on treatment for chronic pain.
Complete data on pain response, as assessed by the visual analog scale, was available for 29 of the 41 patients. No significant differences in postoperative pain scores were observed between the two groups at 1, 16, 18, and 24 hours. Further, there was no significant difference in morphine dose between the IB and normal saline groups.
“One finding was the opposite of what I would have expected. Patients who underwent lymph node dissection used significantly less narcotic analgesic [P = .03],” Dr. Klapper told the audience.
Study strengths were the prospective, randomized design, and its being adequately powered to detect a significant difference between the two groups. But the study was conducted at a single institution and did not include data beyond 24 hours. Also, Dr. Klapper said that perhaps results should have been stratified according to indications for surgery.
“There is more and more pressure on us to achieve higher patient satisfaction scores. Soon down the line, patient satisfaction will become a metric for compensation. We need to focus on what we can do to improve patient satisfaction scores and experience,” Dr. Klapper said. “A larger sample of gynecologic oncology patients is needed to further support these conclusions, and we need to fine tune to avoid the problems in this study.”
The meeting was presented by the Society of Laparoendoscopic Surgeons and affiliated societies. Dr. Klapper reported that he is on the speakers bureau for Astellas.
NEW YORK – While some evidence in the surgical literature suggests that intraperitoneal bupivacaine reduces postoperative pain scores and narcotic use, a new randomized controlled trial shows no significant improvement in patients undergoing robot-assisted total laparoscopic hysterectomy.
“Despite evidence of benefit in laparoscopic surgery, there does not appear to be a benefit for using intraperitoneal bupivacaine. We need a larger sample size to study this,” Dr. Allan Klapper said at the annual Minimally Invasive Surgery Week.
The uptake of robot-assisted total laparoscopic hysterectomy increased by 9.5% in the United States, and hospitals with robotic capabilities perform 22.4% of hysterectomies with this technique, according to Dr. Klapper, an ob.gyn. at West Pennsylvania Allegheny Health System in Pittsburgh. Minimally invasive surgery, however, does not completely eliminate postoperative pain, and between one-third and two-thirds of patients report pain following such surgery.
Intraperitoneal bupivacaine (IB) was selected for the study because of positive reports in small studies of patients undergoing laparoscopic cholecystectomy and gynecologic procedures, Dr. Klapper explained. He noted that the positive studies were of poor quality, but other studies – also of poor quality – had negative results.
To investigate the role of IB in reducing postoperative pain and narcotic requirements in patients undergoing robot-assisted total laparoscopic hysterectomy, Dr. Klapper and his colleagues launched a prospective, double-blind, randomized, placebo-controlled trial comparing IB to normal saline in 41 patients managed with a standardized postoperative analgesic regimen.
Baseline characteristics showed no differences between the two groups in surgical indications, body mass index, operating room time, number of previous surgeries, and the percentage of patients undergoing lymph node dissection. Patients were excluded from the analysis if they converted to laparotomy, were allergic to IB, or were currently on treatment for chronic pain.
Complete data on pain response, as assessed by the visual analog scale, was available for 29 of the 41 patients. No significant differences in postoperative pain scores were observed between the two groups at 1, 16, 18, and 24 hours. Further, there was no significant difference in morphine dose between the IB and normal saline groups.
“One finding was the opposite of what I would have expected. Patients who underwent lymph node dissection used significantly less narcotic analgesic [P = .03],” Dr. Klapper told the audience.
Study strengths were the prospective, randomized design, and its being adequately powered to detect a significant difference between the two groups. But the study was conducted at a single institution and did not include data beyond 24 hours. Also, Dr. Klapper said that perhaps results should have been stratified according to indications for surgery.
“There is more and more pressure on us to achieve higher patient satisfaction scores. Soon down the line, patient satisfaction will become a metric for compensation. We need to focus on what we can do to improve patient satisfaction scores and experience,” Dr. Klapper said. “A larger sample of gynecologic oncology patients is needed to further support these conclusions, and we need to fine tune to avoid the problems in this study.”
The meeting was presented by the Society of Laparoendoscopic Surgeons and affiliated societies. Dr. Klapper reported that he is on the speakers bureau for Astellas.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Intraperitoneal bupivacaine does not appear to achieve meaningful postoperative pain relief in total laparoscopic hysterectomy.
Major finding: No significant difference was observed between placebo and active treatment in pain scores or need for narcotics.
Data source: A prospective, randomized, placebo-controlled study of 41 patients.
Disclosures: Dr. Klapper reported that he is on the speakers bureau for Astellas.
ESC: Noncardiac surgery in HCM patients warrants special attention
LONDON – Hypertrophic cardiomyopathy patients undergoing noncardiac surgery posted significantly worse 30-day composite outcomes than did closely matched controls undergoing the same sorts of surgical procedures.
“Our recommendation is that when hypertrophic cardiomyopathy patients need noncardiac surgery they should be evaluated and treated at an experienced center,” Dr. Milind Y. Desai concluded at the annual congress of the European Society of Cardiology.
There is a dearth of data on outcomes of noncardiac surgery in patients with hypertrophic cardiomyopathy (HCM). This was the impetus for Dr. Desai and his coinvestigators at the Cleveland Clinic to conduct a case-control study involving 92 consecutive adults with HCM undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 controls matched for age, gender, and type of surgery. Enrollment was restricted to HCM patients who hadn’t previously undergone septal myectomy or alcohol ablation.
The primary outcome was the 30-day composite of postoperative death, MI, stroke, or heart failure. The incidence was 10% in the HCM group, significantly greater than the 3% rate in controls. Moreover, 4% of HCM patients developed postoperative atrial fibrillation, compared with none of the controls. Three deaths occurred among the 92 HCM patients, an incidence twice that in the control group.
The special challenge of noncardiac surgery in HCM patients is that their heart condition is characterized by systolic anterior motion of the mitral valve, dynamic left ventricular outflow tract obstruction, diastolic dysfunction, and mitral regurgitation. The rapid blood pressure and fluid shifts that occur during noncardiac surgery require special attention in such patients, Dr. Desai observed.
The HCM patients in this series received such attention, he added. They were more likely than controls to be on beta-blocker therapy at surgery, they received lower doses of ephedrine intraoperatively so as to avoid aggravating outflow tract obstruction, and they spent half as much time as controls with a systolic blood pressure below 90 mm Hg or a heart rate greater than 100 bpm.
“Care was taken to make sure these patients did not decompensate,” he noted.
Dr. Desai reported no financial conflicts regarding this study, conducted free of commercial support.
LONDON – Hypertrophic cardiomyopathy patients undergoing noncardiac surgery posted significantly worse 30-day composite outcomes than did closely matched controls undergoing the same sorts of surgical procedures.
“Our recommendation is that when hypertrophic cardiomyopathy patients need noncardiac surgery they should be evaluated and treated at an experienced center,” Dr. Milind Y. Desai concluded at the annual congress of the European Society of Cardiology.
There is a dearth of data on outcomes of noncardiac surgery in patients with hypertrophic cardiomyopathy (HCM). This was the impetus for Dr. Desai and his coinvestigators at the Cleveland Clinic to conduct a case-control study involving 92 consecutive adults with HCM undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 controls matched for age, gender, and type of surgery. Enrollment was restricted to HCM patients who hadn’t previously undergone septal myectomy or alcohol ablation.
The primary outcome was the 30-day composite of postoperative death, MI, stroke, or heart failure. The incidence was 10% in the HCM group, significantly greater than the 3% rate in controls. Moreover, 4% of HCM patients developed postoperative atrial fibrillation, compared with none of the controls. Three deaths occurred among the 92 HCM patients, an incidence twice that in the control group.
The special challenge of noncardiac surgery in HCM patients is that their heart condition is characterized by systolic anterior motion of the mitral valve, dynamic left ventricular outflow tract obstruction, diastolic dysfunction, and mitral regurgitation. The rapid blood pressure and fluid shifts that occur during noncardiac surgery require special attention in such patients, Dr. Desai observed.
The HCM patients in this series received such attention, he added. They were more likely than controls to be on beta-blocker therapy at surgery, they received lower doses of ephedrine intraoperatively so as to avoid aggravating outflow tract obstruction, and they spent half as much time as controls with a systolic blood pressure below 90 mm Hg or a heart rate greater than 100 bpm.
“Care was taken to make sure these patients did not decompensate,” he noted.
Dr. Desai reported no financial conflicts regarding this study, conducted free of commercial support.
LONDON – Hypertrophic cardiomyopathy patients undergoing noncardiac surgery posted significantly worse 30-day composite outcomes than did closely matched controls undergoing the same sorts of surgical procedures.
“Our recommendation is that when hypertrophic cardiomyopathy patients need noncardiac surgery they should be evaluated and treated at an experienced center,” Dr. Milind Y. Desai concluded at the annual congress of the European Society of Cardiology.
There is a dearth of data on outcomes of noncardiac surgery in patients with hypertrophic cardiomyopathy (HCM). This was the impetus for Dr. Desai and his coinvestigators at the Cleveland Clinic to conduct a case-control study involving 92 consecutive adults with HCM undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 controls matched for age, gender, and type of surgery. Enrollment was restricted to HCM patients who hadn’t previously undergone septal myectomy or alcohol ablation.
The primary outcome was the 30-day composite of postoperative death, MI, stroke, or heart failure. The incidence was 10% in the HCM group, significantly greater than the 3% rate in controls. Moreover, 4% of HCM patients developed postoperative atrial fibrillation, compared with none of the controls. Three deaths occurred among the 92 HCM patients, an incidence twice that in the control group.
The special challenge of noncardiac surgery in HCM patients is that their heart condition is characterized by systolic anterior motion of the mitral valve, dynamic left ventricular outflow tract obstruction, diastolic dysfunction, and mitral regurgitation. The rapid blood pressure and fluid shifts that occur during noncardiac surgery require special attention in such patients, Dr. Desai observed.
The HCM patients in this series received such attention, he added. They were more likely than controls to be on beta-blocker therapy at surgery, they received lower doses of ephedrine intraoperatively so as to avoid aggravating outflow tract obstruction, and they spent half as much time as controls with a systolic blood pressure below 90 mm Hg or a heart rate greater than 100 bpm.
“Care was taken to make sure these patients did not decompensate,” he noted.
Dr. Desai reported no financial conflicts regarding this study, conducted free of commercial support.
AT THE ESC CONGRESS 2015
Key clinical point: Hypertrophic cardiomyopathy patients undergoing noncardiac surgery have significantly worse outcomes than do matched controls undergoing similar operations.
Major finding: The 30-day composite endpoint of death, MI, stroke, or heart failure occurred in 10% of hypertrophic cardiomyopathy patients who underwent noncardiac surgery, compared with 3% of matched controls.
Data source: A case-control study comparing 30-day outcomes in 92 consecutive hypertrophic cardiomyopathy patients undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 matched controls.
Disclosures: This study was conducted free of commercial support, and the presenter reported having no financial conflicts.
Low-volume surgeons have most complications with mesh slings
The 10-year incidence of serious complications after mesh-sling surgery for stress urinary incontinence is a relatively low 3.29, but patients treated by surgeons who perform a low volume of the procedures have a 37% higher relative risk of requiring further surgery for complications, compared with patients of experienced surgeons, according to a report published online Sept. 9 in JAMA Surgery.
“These findings support the regulatory statements that suggest that patients should be counseled regarding serious complications that can occur with mesh-based procedures for SUI and that surgeons should achieve expertise in their chosen procedure,” wrote Dr. Blayne Welk of the department of surgery and the department of epidemiology and biostatistics at Western University and St. Joseph’s Health Care, London (Ont.) and his associates.
The investigators performed a population-based retrospective cohort study to determine the incidence of surgical removal or revision after a mesh-sling procedure for SUI and to examine whether there are specific risk factors for mesh-related complications. They analyzed data for 59,887 women who underwent the procedure across Ontario during a 10-year period. Median follow-up was 4.4 years.
The procedures were performed by 1,068 surgeons: 293 urologists, 625 gynecologists, and 150 unspecified clinicians. Cases were classified according to whether the surgeon performed a high or low volume of mesh-sling procedures specifically for SUI. High volume was defined as a number at or above the 75th percentile for yearly volume in the province, or more than 16 procedures per year.
Overall, 1,307 women (2.2%) required mesh removal or revision a median of 1 year after the initial surgery. The cumulative incidence of the composite outcome of removal/revision of vaginal or urethral mesh, removal of a foreign body, endoscopic treatment of a urethral foreign body or mesh encrustation, uretrolysis, or repair of a urethrovaginal fistula was 3.29 at 10 years, Dr. Welk and his associates reported. Surgical specialty had no significant effect on complication risk.
This incidence is consistent with previous report from HMOs in the United States and a meta-analysis of clinical trial results, the investigators noted (JAMA Surg. 2015 Sept. 9. doi: 10.1001/jamasurg.2015.2590). Patients of low-volume surgeons had a 37% higher relative risk of complications requiring reoperation than did patients of high-volume surgeons. In a further analysis of the data, patients of low-volume surgeons were significantly more likely to experience the composite outcome than were patients of high-volume surgeons (hazard ratio, 1.37), and, again, the difference between surgical specialties was nonsignificant.
Urologists and gynecologists have very different surgical training and day-to-day practices, the researchers noted, and as a result they hypothesized that complication rates might differ between the two groups of clinicians. But that was not proven in the findings.
“This suggests that procedure-specific knowledge and experience is important for surgery to treat SUI, rather than general operative training,” Dr. Welk and his associates wrote.
Women who underwent multiple mesh-based procedures for SUI were at highest risk for the composite endpoint. Their absolute risk for later mesh removal or revision was 4.87%.
“This novel finding should temper the enthusiasm of case series that suggest that the use of multiple synthetic slings is safe and efficacious,” the researchers wrote.
This finding is also important in light of the fact that 1,307 of the study participants underwent more than one mesh implant procedure, presumably for recurrent SUI.
This study was supported by the Ontario Ministry of Health and Long-term Care and the Academic Medical Organization of Southwestern Ontario. Dr. Welk reported receiving grant funding from Astellas Canada.
The call to centralize complex, high-risk surgical procedures at expert centers is well known, but what about commonly performed, same-day procedures with low risks of complications, such as mesh-sling surgery for stress urinary incontinence? Must patients be referred only to high-volume surgeons?
This likely would be impractical if not impossible for a procedure that is performed so frequently. A more reasonable approach would be for low-volume surgeons to use structured proctoring and/or coaching models to develop expertise and mandatory outcomes reporting to assure high-quality care. Even though clinicians will not welcome this approach, it probably will become required in the near future and tied to reimbursements. Ultimately, surgeons should be the drivers for change and should not wait for payers or regulators to impose punitive measures.
Dr. Christian P. Meyer and Dr. Quoc-Dien Trinh are with the Center for Surgery and Public Health and the division of urologic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston. They reported having no relevant financial disclosures. These remarks are adapted from an invited commentary (JAMA Surg. 2015 Sept. 9. doi: 10.1001/jamasurg.2015.2596) accompanying Dr. Welk’s report.
The call to centralize complex, high-risk surgical procedures at expert centers is well known, but what about commonly performed, same-day procedures with low risks of complications, such as mesh-sling surgery for stress urinary incontinence? Must patients be referred only to high-volume surgeons?
This likely would be impractical if not impossible for a procedure that is performed so frequently. A more reasonable approach would be for low-volume surgeons to use structured proctoring and/or coaching models to develop expertise and mandatory outcomes reporting to assure high-quality care. Even though clinicians will not welcome this approach, it probably will become required in the near future and tied to reimbursements. Ultimately, surgeons should be the drivers for change and should not wait for payers or regulators to impose punitive measures.
Dr. Christian P. Meyer and Dr. Quoc-Dien Trinh are with the Center for Surgery and Public Health and the division of urologic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston. They reported having no relevant financial disclosures. These remarks are adapted from an invited commentary (JAMA Surg. 2015 Sept. 9. doi: 10.1001/jamasurg.2015.2596) accompanying Dr. Welk’s report.
The call to centralize complex, high-risk surgical procedures at expert centers is well known, but what about commonly performed, same-day procedures with low risks of complications, such as mesh-sling surgery for stress urinary incontinence? Must patients be referred only to high-volume surgeons?
This likely would be impractical if not impossible for a procedure that is performed so frequently. A more reasonable approach would be for low-volume surgeons to use structured proctoring and/or coaching models to develop expertise and mandatory outcomes reporting to assure high-quality care. Even though clinicians will not welcome this approach, it probably will become required in the near future and tied to reimbursements. Ultimately, surgeons should be the drivers for change and should not wait for payers or regulators to impose punitive measures.
Dr. Christian P. Meyer and Dr. Quoc-Dien Trinh are with the Center for Surgery and Public Health and the division of urologic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston. They reported having no relevant financial disclosures. These remarks are adapted from an invited commentary (JAMA Surg. 2015 Sept. 9. doi: 10.1001/jamasurg.2015.2596) accompanying Dr. Welk’s report.
The 10-year incidence of serious complications after mesh-sling surgery for stress urinary incontinence is a relatively low 3.29, but patients treated by surgeons who perform a low volume of the procedures have a 37% higher relative risk of requiring further surgery for complications, compared with patients of experienced surgeons, according to a report published online Sept. 9 in JAMA Surgery.
“These findings support the regulatory statements that suggest that patients should be counseled regarding serious complications that can occur with mesh-based procedures for SUI and that surgeons should achieve expertise in their chosen procedure,” wrote Dr. Blayne Welk of the department of surgery and the department of epidemiology and biostatistics at Western University and St. Joseph’s Health Care, London (Ont.) and his associates.
The investigators performed a population-based retrospective cohort study to determine the incidence of surgical removal or revision after a mesh-sling procedure for SUI and to examine whether there are specific risk factors for mesh-related complications. They analyzed data for 59,887 women who underwent the procedure across Ontario during a 10-year period. Median follow-up was 4.4 years.
The procedures were performed by 1,068 surgeons: 293 urologists, 625 gynecologists, and 150 unspecified clinicians. Cases were classified according to whether the surgeon performed a high or low volume of mesh-sling procedures specifically for SUI. High volume was defined as a number at or above the 75th percentile for yearly volume in the province, or more than 16 procedures per year.
Overall, 1,307 women (2.2%) required mesh removal or revision a median of 1 year after the initial surgery. The cumulative incidence of the composite outcome of removal/revision of vaginal or urethral mesh, removal of a foreign body, endoscopic treatment of a urethral foreign body or mesh encrustation, uretrolysis, or repair of a urethrovaginal fistula was 3.29 at 10 years, Dr. Welk and his associates reported. Surgical specialty had no significant effect on complication risk.
This incidence is consistent with previous report from HMOs in the United States and a meta-analysis of clinical trial results, the investigators noted (JAMA Surg. 2015 Sept. 9. doi: 10.1001/jamasurg.2015.2590). Patients of low-volume surgeons had a 37% higher relative risk of complications requiring reoperation than did patients of high-volume surgeons. In a further analysis of the data, patients of low-volume surgeons were significantly more likely to experience the composite outcome than were patients of high-volume surgeons (hazard ratio, 1.37), and, again, the difference between surgical specialties was nonsignificant.
Urologists and gynecologists have very different surgical training and day-to-day practices, the researchers noted, and as a result they hypothesized that complication rates might differ between the two groups of clinicians. But that was not proven in the findings.
“This suggests that procedure-specific knowledge and experience is important for surgery to treat SUI, rather than general operative training,” Dr. Welk and his associates wrote.
Women who underwent multiple mesh-based procedures for SUI were at highest risk for the composite endpoint. Their absolute risk for later mesh removal or revision was 4.87%.
“This novel finding should temper the enthusiasm of case series that suggest that the use of multiple synthetic slings is safe and efficacious,” the researchers wrote.
This finding is also important in light of the fact that 1,307 of the study participants underwent more than one mesh implant procedure, presumably for recurrent SUI.
This study was supported by the Ontario Ministry of Health and Long-term Care and the Academic Medical Organization of Southwestern Ontario. Dr. Welk reported receiving grant funding from Astellas Canada.
The 10-year incidence of serious complications after mesh-sling surgery for stress urinary incontinence is a relatively low 3.29, but patients treated by surgeons who perform a low volume of the procedures have a 37% higher relative risk of requiring further surgery for complications, compared with patients of experienced surgeons, according to a report published online Sept. 9 in JAMA Surgery.
“These findings support the regulatory statements that suggest that patients should be counseled regarding serious complications that can occur with mesh-based procedures for SUI and that surgeons should achieve expertise in their chosen procedure,” wrote Dr. Blayne Welk of the department of surgery and the department of epidemiology and biostatistics at Western University and St. Joseph’s Health Care, London (Ont.) and his associates.
The investigators performed a population-based retrospective cohort study to determine the incidence of surgical removal or revision after a mesh-sling procedure for SUI and to examine whether there are specific risk factors for mesh-related complications. They analyzed data for 59,887 women who underwent the procedure across Ontario during a 10-year period. Median follow-up was 4.4 years.
The procedures were performed by 1,068 surgeons: 293 urologists, 625 gynecologists, and 150 unspecified clinicians. Cases were classified according to whether the surgeon performed a high or low volume of mesh-sling procedures specifically for SUI. High volume was defined as a number at or above the 75th percentile for yearly volume in the province, or more than 16 procedures per year.
Overall, 1,307 women (2.2%) required mesh removal or revision a median of 1 year after the initial surgery. The cumulative incidence of the composite outcome of removal/revision of vaginal or urethral mesh, removal of a foreign body, endoscopic treatment of a urethral foreign body or mesh encrustation, uretrolysis, or repair of a urethrovaginal fistula was 3.29 at 10 years, Dr. Welk and his associates reported. Surgical specialty had no significant effect on complication risk.
This incidence is consistent with previous report from HMOs in the United States and a meta-analysis of clinical trial results, the investigators noted (JAMA Surg. 2015 Sept. 9. doi: 10.1001/jamasurg.2015.2590). Patients of low-volume surgeons had a 37% higher relative risk of complications requiring reoperation than did patients of high-volume surgeons. In a further analysis of the data, patients of low-volume surgeons were significantly more likely to experience the composite outcome than were patients of high-volume surgeons (hazard ratio, 1.37), and, again, the difference between surgical specialties was nonsignificant.
Urologists and gynecologists have very different surgical training and day-to-day practices, the researchers noted, and as a result they hypothesized that complication rates might differ between the two groups of clinicians. But that was not proven in the findings.
“This suggests that procedure-specific knowledge and experience is important for surgery to treat SUI, rather than general operative training,” Dr. Welk and his associates wrote.
Women who underwent multiple mesh-based procedures for SUI were at highest risk for the composite endpoint. Their absolute risk for later mesh removal or revision was 4.87%.
“This novel finding should temper the enthusiasm of case series that suggest that the use of multiple synthetic slings is safe and efficacious,” the researchers wrote.
This finding is also important in light of the fact that 1,307 of the study participants underwent more than one mesh implant procedure, presumably for recurrent SUI.
This study was supported by the Ontario Ministry of Health and Long-term Care and the Academic Medical Organization of Southwestern Ontario. Dr. Welk reported receiving grant funding from Astellas Canada.
FROM JAMA SURGERY
Key clinical point: The complication rate after mesh sling surgery for SUI is relatively low and highly correlated with the surgeon’s experience with the procedure.
Major finding: Patients of low-volume surgeons had a 37% higher relative risk of complications requiring reoperation than did patients of high-volume surgeons.
Data source: A population-based retrospective cohort study of 59,887 women who had SUI mesh surgery across Ontario during a 10-year period.
Disclosures: This study was supported by the Ontario Ministry of Health and Long-term Care and the Academic Medical Organization of Southwestern Ontario. Dr. Welk reported receiving grant funding from Astellas Canada.
Postop delirium heightens risk of other dangerous complications
Delirium is not only the most common major complication of elective surgery in older adults, it also markedly raises the risk of all adverse outcomes, including prolonged length of stay, discharge to an institution rather than home, and readmission within 30 days, according to a report published online Sept. 9 in JAMA Surgery.
“Given its high prevalence and negative effect, delirium should be considered as the leading postoperative complication contributing to adverse outcomes” in this patient population, wrote Dr. Lauren J. Gleason of the department of medicine at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her associates.
Delirium is typically considered a less serious event than other major postoperative complications, even though its association with higher in-hospital mortality, 6-month mortality, functional decline, and higher health care costs has been well documented. To assess whether delirium should be considered equivalent to other major life-altering or life-threatening complications, the investigators studied 566 patients aged 70 years and older who underwent elective orthopedic, general, or vascular procedures at Beth Israel Deaconess or Brigham and Women’s Hospital in a 3-year period. The data were collected for the Successful Aging after Elective Surgery (SAGES) study.
Operations included total hip or knee replacement, lumbar or cervical laminectomy, lower-extremity bypass, open abdominal aortic aneurysm repair, open colectomyt, and laparoscopic colectomy. In general, these patients were highly functional and highly educated. The mean age was 76.7 years, and 93% of the study participants were white.
Delirium developed in 135 patients (24%) – much more frequently than all other major complications combined (47 patients, or 8%). This is comparable with rates of delirium reported in other studies of elective noncardiac surgeries, Dr. Gleason and her associates noted. Other major complications included unstable arrhythmias, respiratory failure, abscess requiring incision and drainage, abdominal compartment syndrome, anastomotic leak, deep surgical site infection, and hernia repair.
Compared with patients who didn’t develop delirium, those who did had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission, the investigators reported (JAMA Surg. 2015 Sept 9. doi: 10.1001/jamasurg.2015.2606).
Since delirium is often preventable, clinicians should try harder to implement preventive strategies before surgery and continue them afterward. The Hospital Elder Life Program, proactive geriatric consultation, and comanagement services all have proved effective in this regard, they added.
This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation. The authors reported no relevant disclosures.
Delirium is not only the most common major complication of elective surgery in older adults, it also markedly raises the risk of all adverse outcomes, including prolonged length of stay, discharge to an institution rather than home, and readmission within 30 days, according to a report published online Sept. 9 in JAMA Surgery.
“Given its high prevalence and negative effect, delirium should be considered as the leading postoperative complication contributing to adverse outcomes” in this patient population, wrote Dr. Lauren J. Gleason of the department of medicine at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her associates.
Delirium is typically considered a less serious event than other major postoperative complications, even though its association with higher in-hospital mortality, 6-month mortality, functional decline, and higher health care costs has been well documented. To assess whether delirium should be considered equivalent to other major life-altering or life-threatening complications, the investigators studied 566 patients aged 70 years and older who underwent elective orthopedic, general, or vascular procedures at Beth Israel Deaconess or Brigham and Women’s Hospital in a 3-year period. The data were collected for the Successful Aging after Elective Surgery (SAGES) study.
Operations included total hip or knee replacement, lumbar or cervical laminectomy, lower-extremity bypass, open abdominal aortic aneurysm repair, open colectomyt, and laparoscopic colectomy. In general, these patients were highly functional and highly educated. The mean age was 76.7 years, and 93% of the study participants were white.
Delirium developed in 135 patients (24%) – much more frequently than all other major complications combined (47 patients, or 8%). This is comparable with rates of delirium reported in other studies of elective noncardiac surgeries, Dr. Gleason and her associates noted. Other major complications included unstable arrhythmias, respiratory failure, abscess requiring incision and drainage, abdominal compartment syndrome, anastomotic leak, deep surgical site infection, and hernia repair.
Compared with patients who didn’t develop delirium, those who did had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission, the investigators reported (JAMA Surg. 2015 Sept 9. doi: 10.1001/jamasurg.2015.2606).
Since delirium is often preventable, clinicians should try harder to implement preventive strategies before surgery and continue them afterward. The Hospital Elder Life Program, proactive geriatric consultation, and comanagement services all have proved effective in this regard, they added.
This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation. The authors reported no relevant disclosures.
Delirium is not only the most common major complication of elective surgery in older adults, it also markedly raises the risk of all adverse outcomes, including prolonged length of stay, discharge to an institution rather than home, and readmission within 30 days, according to a report published online Sept. 9 in JAMA Surgery.
“Given its high prevalence and negative effect, delirium should be considered as the leading postoperative complication contributing to adverse outcomes” in this patient population, wrote Dr. Lauren J. Gleason of the department of medicine at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her associates.
Delirium is typically considered a less serious event than other major postoperative complications, even though its association with higher in-hospital mortality, 6-month mortality, functional decline, and higher health care costs has been well documented. To assess whether delirium should be considered equivalent to other major life-altering or life-threatening complications, the investigators studied 566 patients aged 70 years and older who underwent elective orthopedic, general, or vascular procedures at Beth Israel Deaconess or Brigham and Women’s Hospital in a 3-year period. The data were collected for the Successful Aging after Elective Surgery (SAGES) study.
Operations included total hip or knee replacement, lumbar or cervical laminectomy, lower-extremity bypass, open abdominal aortic aneurysm repair, open colectomyt, and laparoscopic colectomy. In general, these patients were highly functional and highly educated. The mean age was 76.7 years, and 93% of the study participants were white.
Delirium developed in 135 patients (24%) – much more frequently than all other major complications combined (47 patients, or 8%). This is comparable with rates of delirium reported in other studies of elective noncardiac surgeries, Dr. Gleason and her associates noted. Other major complications included unstable arrhythmias, respiratory failure, abscess requiring incision and drainage, abdominal compartment syndrome, anastomotic leak, deep surgical site infection, and hernia repair.
Compared with patients who didn’t develop delirium, those who did had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission, the investigators reported (JAMA Surg. 2015 Sept 9. doi: 10.1001/jamasurg.2015.2606).
Since delirium is often preventable, clinicians should try harder to implement preventive strategies before surgery and continue them afterward. The Hospital Elder Life Program, proactive geriatric consultation, and comanagement services all have proved effective in this regard, they added.
This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation. The authors reported no relevant disclosures.
FROM JAMA SURGERY
Key clinical point: Delirium is the most common and among the most harmful of complications of elective surgery in older adults.
Major finding: Elderly patients who developed delirium had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission.
Data source: A prospective cohort study involving 566 older adults undergoing elective surgery at two hospitals in a 3-year period.
Disclosures: This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation.
ESC: Statins reduce postoperative noncardiac surgery event rates
LONDON – Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days by 17% when compared with no statin use in a large, international observational study.
Results of the prospective VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation) study showed that the primary composite endpoint of all-cause mortality, myocardial injury after noncardiac surgery (MINS), or stroke at 30 days was 11.8% in a propensity-matched cohort of patients, 2,845 of whom were treated with a statin and 4,492 who were not. The relative risk (RR) for this composite endpoint was 0.83 favoring the use of preoperative statins, with a 95% confidence interval (CI) of 0.73-0.95 and a P value of .007.
Perioperative statin vs. no statin use also cut all-cause mortality by 42% (RR, 0.58; 95% CI, 0.40-0.83; P = .003), cardiovascular mortality by 58% (RR, 0.42; 95% CI, 0.23-0.76; P = .004), and MINS by 14% (RR, 0.86; 95% CI, 0.73-0.98; P = .002).
“These study results are hypothesis generating at most,” emphasized Dr. Otavio Berwanger, who presented the findings at the annual congress of the European Society of Cardiology while they were simultaneously published online (Eur Heart J. 2015 Sept. 1. doi: 10.1093/eurheartj/ehv456).
“It is true that, in this large representative cohort of contemporary patients, statins were associated with lower event rates,” added Dr. Berwanger of Hospital do Coração in São Paulo, Brazil, and “together with the previous body of evidence, statins appear to be an interesting and attractive intervention to reduce postoperative events.” A large-scale, randomized trial is needed, however, to answer the question of whether statins should be used preoperatively to prevent postoperative events in noncardiac surgery patients.
Over a 4-year period that started in August 2007, more than 15,000 individuals aged 45 years or older who were undergoing a variety of noncardiac surgical procedures that required regional or a general anesthetic and at least an overnight stay in the hospital were recruited at 12 centers in eight countries in North and South America, Africa, Asia, Australia, and Europe.
One of the objectives of the study was to examine the use of perioperative statins on cardiovascular events at 30 days, and to do this, the VISION investigators identified the patients who had received a statin in the 7 days prior to surgery and then used propensity matching to form a control group of patients that had not received a statin in the week before surgery.
Just under half of the propensity-matched population was male, with an average age of nearly 69 years. Around 70% of the population had hypertension, 9%-10% had a prior stroke, and 13% had active cancer. Surgeries were urgent in about 2% and emergent in 8%. Around a quarter had undergone orthopedic procedures, and 4% were vascular surgeries. Overall, 36% of surgeries were classified as low risk and 39% as other.
One of the limitations of the study, however, is that, despite the propensity matching, there were some variables that remained different between the two groups, with higher rates of coronary artery disease (20% vs. 14%), peripheral vascular disease (8% vs. 5%), diabetes (30% vs. 25%), and preoperative use of aspirin (25% vs. 19%) and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (53% vs. 48%) in the statin- versus nonstatin-treated patients.
Other limitations are that these data are observational and the use of statins could be just a surrogate for unmeasured confounders that relate to prognosis. Information on the type and dosing of statins also was not obtained, and there was no information collected on potential liver or muscle function side effects.
Nevertheless, the VISION investigators noted in the published paper that the results are consistent with those from other observational studies and prior small-scale, randomized trials and so do add important information. They noted that these data were collected prospectively in a broader range of patients and types of surgeries than has been reported previously. In addition, patients were recruited from several countries and were actively monitored for outcomes and events were centrally adjudicated. VISION is also the only study to report on the effects of statins on MINS.
“Another message from our results is that the use of long-term statins is sub-optimal in high cardiovascular risk patients, who should be on long-term lipid-lowering therapy independently of surgery,” the VISION investigators wrote in their report.
The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
LONDON – Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days by 17% when compared with no statin use in a large, international observational study.
Results of the prospective VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation) study showed that the primary composite endpoint of all-cause mortality, myocardial injury after noncardiac surgery (MINS), or stroke at 30 days was 11.8% in a propensity-matched cohort of patients, 2,845 of whom were treated with a statin and 4,492 who were not. The relative risk (RR) for this composite endpoint was 0.83 favoring the use of preoperative statins, with a 95% confidence interval (CI) of 0.73-0.95 and a P value of .007.
Perioperative statin vs. no statin use also cut all-cause mortality by 42% (RR, 0.58; 95% CI, 0.40-0.83; P = .003), cardiovascular mortality by 58% (RR, 0.42; 95% CI, 0.23-0.76; P = .004), and MINS by 14% (RR, 0.86; 95% CI, 0.73-0.98; P = .002).
“These study results are hypothesis generating at most,” emphasized Dr. Otavio Berwanger, who presented the findings at the annual congress of the European Society of Cardiology while they were simultaneously published online (Eur Heart J. 2015 Sept. 1. doi: 10.1093/eurheartj/ehv456).
“It is true that, in this large representative cohort of contemporary patients, statins were associated with lower event rates,” added Dr. Berwanger of Hospital do Coração in São Paulo, Brazil, and “together with the previous body of evidence, statins appear to be an interesting and attractive intervention to reduce postoperative events.” A large-scale, randomized trial is needed, however, to answer the question of whether statins should be used preoperatively to prevent postoperative events in noncardiac surgery patients.
Over a 4-year period that started in August 2007, more than 15,000 individuals aged 45 years or older who were undergoing a variety of noncardiac surgical procedures that required regional or a general anesthetic and at least an overnight stay in the hospital were recruited at 12 centers in eight countries in North and South America, Africa, Asia, Australia, and Europe.
One of the objectives of the study was to examine the use of perioperative statins on cardiovascular events at 30 days, and to do this, the VISION investigators identified the patients who had received a statin in the 7 days prior to surgery and then used propensity matching to form a control group of patients that had not received a statin in the week before surgery.
Just under half of the propensity-matched population was male, with an average age of nearly 69 years. Around 70% of the population had hypertension, 9%-10% had a prior stroke, and 13% had active cancer. Surgeries were urgent in about 2% and emergent in 8%. Around a quarter had undergone orthopedic procedures, and 4% were vascular surgeries. Overall, 36% of surgeries were classified as low risk and 39% as other.
One of the limitations of the study, however, is that, despite the propensity matching, there were some variables that remained different between the two groups, with higher rates of coronary artery disease (20% vs. 14%), peripheral vascular disease (8% vs. 5%), diabetes (30% vs. 25%), and preoperative use of aspirin (25% vs. 19%) and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (53% vs. 48%) in the statin- versus nonstatin-treated patients.
Other limitations are that these data are observational and the use of statins could be just a surrogate for unmeasured confounders that relate to prognosis. Information on the type and dosing of statins also was not obtained, and there was no information collected on potential liver or muscle function side effects.
Nevertheless, the VISION investigators noted in the published paper that the results are consistent with those from other observational studies and prior small-scale, randomized trials and so do add important information. They noted that these data were collected prospectively in a broader range of patients and types of surgeries than has been reported previously. In addition, patients were recruited from several countries and were actively monitored for outcomes and events were centrally adjudicated. VISION is also the only study to report on the effects of statins on MINS.
“Another message from our results is that the use of long-term statins is sub-optimal in high cardiovascular risk patients, who should be on long-term lipid-lowering therapy independently of surgery,” the VISION investigators wrote in their report.
The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
LONDON – Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days by 17% when compared with no statin use in a large, international observational study.
Results of the prospective VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation) study showed that the primary composite endpoint of all-cause mortality, myocardial injury after noncardiac surgery (MINS), or stroke at 30 days was 11.8% in a propensity-matched cohort of patients, 2,845 of whom were treated with a statin and 4,492 who were not. The relative risk (RR) for this composite endpoint was 0.83 favoring the use of preoperative statins, with a 95% confidence interval (CI) of 0.73-0.95 and a P value of .007.
Perioperative statin vs. no statin use also cut all-cause mortality by 42% (RR, 0.58; 95% CI, 0.40-0.83; P = .003), cardiovascular mortality by 58% (RR, 0.42; 95% CI, 0.23-0.76; P = .004), and MINS by 14% (RR, 0.86; 95% CI, 0.73-0.98; P = .002).
“These study results are hypothesis generating at most,” emphasized Dr. Otavio Berwanger, who presented the findings at the annual congress of the European Society of Cardiology while they were simultaneously published online (Eur Heart J. 2015 Sept. 1. doi: 10.1093/eurheartj/ehv456).
“It is true that, in this large representative cohort of contemporary patients, statins were associated with lower event rates,” added Dr. Berwanger of Hospital do Coração in São Paulo, Brazil, and “together with the previous body of evidence, statins appear to be an interesting and attractive intervention to reduce postoperative events.” A large-scale, randomized trial is needed, however, to answer the question of whether statins should be used preoperatively to prevent postoperative events in noncardiac surgery patients.
Over a 4-year period that started in August 2007, more than 15,000 individuals aged 45 years or older who were undergoing a variety of noncardiac surgical procedures that required regional or a general anesthetic and at least an overnight stay in the hospital were recruited at 12 centers in eight countries in North and South America, Africa, Asia, Australia, and Europe.
One of the objectives of the study was to examine the use of perioperative statins on cardiovascular events at 30 days, and to do this, the VISION investigators identified the patients who had received a statin in the 7 days prior to surgery and then used propensity matching to form a control group of patients that had not received a statin in the week before surgery.
Just under half of the propensity-matched population was male, with an average age of nearly 69 years. Around 70% of the population had hypertension, 9%-10% had a prior stroke, and 13% had active cancer. Surgeries were urgent in about 2% and emergent in 8%. Around a quarter had undergone orthopedic procedures, and 4% were vascular surgeries. Overall, 36% of surgeries were classified as low risk and 39% as other.
One of the limitations of the study, however, is that, despite the propensity matching, there were some variables that remained different between the two groups, with higher rates of coronary artery disease (20% vs. 14%), peripheral vascular disease (8% vs. 5%), diabetes (30% vs. 25%), and preoperative use of aspirin (25% vs. 19%) and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (53% vs. 48%) in the statin- versus nonstatin-treated patients.
Other limitations are that these data are observational and the use of statins could be just a surrogate for unmeasured confounders that relate to prognosis. Information on the type and dosing of statins also was not obtained, and there was no information collected on potential liver or muscle function side effects.
Nevertheless, the VISION investigators noted in the published paper that the results are consistent with those from other observational studies and prior small-scale, randomized trials and so do add important information. They noted that these data were collected prospectively in a broader range of patients and types of surgeries than has been reported previously. In addition, patients were recruited from several countries and were actively monitored for outcomes and events were centrally adjudicated. VISION is also the only study to report on the effects of statins on MINS.
“Another message from our results is that the use of long-term statins is sub-optimal in high cardiovascular risk patients, who should be on long-term lipid-lowering therapy independently of surgery,” the VISION investigators wrote in their report.
The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
AT THE ESC CONGRESS 2015
Key clinical point: Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days, but the findings are hypothesis generating and need validation in a randomized controlled clinical trial.
Major finding: The primary composite outcome (all-cause mortality, myocardial injury after noncardiac surgery, or stroke at 30 days) was 11.8% overall in the propensity-matched cohort, with a 17% relative risk reduction favoring the use of statin versus no statin (P = .007).
Data source: The VISION study is an international, prospective, observational study of more than 15,000 patients who underwent noncardiac surgery between 2007 and 2011.
Disclosures: The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.