User login
ESC: Ticagrelor linked to less bypass-related bleeding
LONDON – Ticagrelor was associated with fewer major bleeding complications compared with clopidogrel when stopped before revascularization surgery, in a large observational study that included all patients on dual antiplatelet therapy who underwent bypass surgery over a 2-year period in Sweden.
The overall incidence of major bleeding was 12.9% and 17.6%, respectively, when these antiplatelet agents were stopped before coronary artery bypass grafting (CABG). The adjusted odds ratio (OR) was 0.72, representing a 28% lower incidence with ticagrelor than with clopidogrel (P = .012).The study findings indicated that it might be safe to stop ticagrelor but not clopidogrel slightly closer to the procedure than is currently recommended by European (Eur Heart J. 2014;35:2541-2619) and American (J Am Coll Cardiol. 2013;61:e179-e347) guidelines.
“The overall incidence of major CABG-related bleeding complications was lower with ticagrelor than with clopidogrel,” Dr. Anders Jeppsson said at the annual meeting of the European Society of Cardiology.
“The difference was mainly driven by a lower incidence when clopidogrel and ticagrelor were discontinued 72 to 120 hours before surgery,” he added.
Dr. Jeppsson of Sahlgrenska (Sweden) University Hospital and the University of Gothenburg noted that the incidence of CABG-related major bleeding was highest for both antiplatelet agents when they were stopped less than 24 hours before surgery but that there was no significant difference between the two antiplatelet agents.
“Discontinuation of ticagrelor 3 days before CABG, as opposed to 5 days, did not increase the incidence of major bleeding complications,” he reported. The OR for discontinuing ticagrelor at 72-120 hours versus more than 120 hours before surgery was 0.93 (P = .08). However, the situation was not the same for discontinuing clopidogrel, with a higher rate of bleeding when the drug was discontinued closer to surgery (OR = 1.17, P = .033).
The findings, which were published online Sept. 1 in the European Heart Journal (doi:10.1093/eurheartj/ehv381), come from an analysis of data prospectively obtained from the SWEDEHEART registry and other local Swedish registries, databases, and patient records. Dr. Jeppsson explained that the aims were to compare the incidence of CABG-related bleeding complications among patients with acute coronary syndromes (ACS) who were taking dual antiplatelet therapy with aspirin and either clopidogrel or ticagrelor in a real-world setting and to see if shorter discontinuation periods before surgery might be feasible.
“A short discontinuation time would reduce the risk for thrombotic events while waiting [for surgery] and save hospital resources,” Dr. Jeppsson said. “But on the other hand it may increase the risk for bleeding complications.”
Data from January 2012 to December 2013 were obtained on all patients in Sweden who were taking dual antiplatelet therapy before CABG. This time period was chosen as it was when ticagrelor was first introduced for the first-line treatment of ACS in the country. Of 2,418 patients identified, 10 were taking prasugrel and were excluded from the analysis. A further 164 patients were excluded as they had discontinued dual antiplatelet therapy more than 2 weeks before having surgery, leaving 1,266 patients who had received ticagrelor and 978 who had been taking clopidogrel.The Bleeding Academic Research Consortium (BARC) Type 4 definition (Circulation. 2011;123:2736-47) was primarily used to identify CABG-related bleeding, with three other published definitions also used, including those used in the BART (N Engl J Med. 2008;358:2319-31) and PLATO (N Engl J Med. 2009;361:1045-57) antiplatelet trials.The overall incidence of major bleeding complications was significantly lower with ticagrelor versus clopidogrel using all four of the bleeding definitions.
However, discontinuing ticagrelor 24 hours or less before CABG showed that while there was a similar amount of BARC major bleeding (P = .052) compared with stopping clopidogrel, the median amount of blood loss (P less than .001), need for red blood cell (P = .028) or platelet (P less than .001) transfusion was greater.To illustrate the dangers of major bleeding on patient outcome, Dr. Jeppsson noted that patients who experienced major bleeding were almost 15 times more likely to die 30 days after the procedure than were those who had no major bleeding. The 30-day mortality rate was higher in clopidogrel than ticagrelor-treated patients (2.7% vs 1.7%) and incidence of thrombotic events was 2.8% and 2.3% These are unadjusted findings and the study was not statistically powered to look at these as end points, Dr. Jeppsson emphasized. These factors were registered for safety reasons, he said.
The study was supported by an investigator-sponsored study program of AstraZeneca and the Swedish Heart and Lung Foundation. Dr. Jeppsson has received research grants, consulting fees or speaker’s honorarium from AstraZeneca in addition to several other pharmaceutical companies.
LONDON – Ticagrelor was associated with fewer major bleeding complications compared with clopidogrel when stopped before revascularization surgery, in a large observational study that included all patients on dual antiplatelet therapy who underwent bypass surgery over a 2-year period in Sweden.
The overall incidence of major bleeding was 12.9% and 17.6%, respectively, when these antiplatelet agents were stopped before coronary artery bypass grafting (CABG). The adjusted odds ratio (OR) was 0.72, representing a 28% lower incidence with ticagrelor than with clopidogrel (P = .012).The study findings indicated that it might be safe to stop ticagrelor but not clopidogrel slightly closer to the procedure than is currently recommended by European (Eur Heart J. 2014;35:2541-2619) and American (J Am Coll Cardiol. 2013;61:e179-e347) guidelines.
“The overall incidence of major CABG-related bleeding complications was lower with ticagrelor than with clopidogrel,” Dr. Anders Jeppsson said at the annual meeting of the European Society of Cardiology.
“The difference was mainly driven by a lower incidence when clopidogrel and ticagrelor were discontinued 72 to 120 hours before surgery,” he added.
Dr. Jeppsson of Sahlgrenska (Sweden) University Hospital and the University of Gothenburg noted that the incidence of CABG-related major bleeding was highest for both antiplatelet agents when they were stopped less than 24 hours before surgery but that there was no significant difference between the two antiplatelet agents.
“Discontinuation of ticagrelor 3 days before CABG, as opposed to 5 days, did not increase the incidence of major bleeding complications,” he reported. The OR for discontinuing ticagrelor at 72-120 hours versus more than 120 hours before surgery was 0.93 (P = .08). However, the situation was not the same for discontinuing clopidogrel, with a higher rate of bleeding when the drug was discontinued closer to surgery (OR = 1.17, P = .033).
The findings, which were published online Sept. 1 in the European Heart Journal (doi:10.1093/eurheartj/ehv381), come from an analysis of data prospectively obtained from the SWEDEHEART registry and other local Swedish registries, databases, and patient records. Dr. Jeppsson explained that the aims were to compare the incidence of CABG-related bleeding complications among patients with acute coronary syndromes (ACS) who were taking dual antiplatelet therapy with aspirin and either clopidogrel or ticagrelor in a real-world setting and to see if shorter discontinuation periods before surgery might be feasible.
“A short discontinuation time would reduce the risk for thrombotic events while waiting [for surgery] and save hospital resources,” Dr. Jeppsson said. “But on the other hand it may increase the risk for bleeding complications.”
Data from January 2012 to December 2013 were obtained on all patients in Sweden who were taking dual antiplatelet therapy before CABG. This time period was chosen as it was when ticagrelor was first introduced for the first-line treatment of ACS in the country. Of 2,418 patients identified, 10 were taking prasugrel and were excluded from the analysis. A further 164 patients were excluded as they had discontinued dual antiplatelet therapy more than 2 weeks before having surgery, leaving 1,266 patients who had received ticagrelor and 978 who had been taking clopidogrel.The Bleeding Academic Research Consortium (BARC) Type 4 definition (Circulation. 2011;123:2736-47) was primarily used to identify CABG-related bleeding, with three other published definitions also used, including those used in the BART (N Engl J Med. 2008;358:2319-31) and PLATO (N Engl J Med. 2009;361:1045-57) antiplatelet trials.The overall incidence of major bleeding complications was significantly lower with ticagrelor versus clopidogrel using all four of the bleeding definitions.
However, discontinuing ticagrelor 24 hours or less before CABG showed that while there was a similar amount of BARC major bleeding (P = .052) compared with stopping clopidogrel, the median amount of blood loss (P less than .001), need for red blood cell (P = .028) or platelet (P less than .001) transfusion was greater.To illustrate the dangers of major bleeding on patient outcome, Dr. Jeppsson noted that patients who experienced major bleeding were almost 15 times more likely to die 30 days after the procedure than were those who had no major bleeding. The 30-day mortality rate was higher in clopidogrel than ticagrelor-treated patients (2.7% vs 1.7%) and incidence of thrombotic events was 2.8% and 2.3% These are unadjusted findings and the study was not statistically powered to look at these as end points, Dr. Jeppsson emphasized. These factors were registered for safety reasons, he said.
The study was supported by an investigator-sponsored study program of AstraZeneca and the Swedish Heart and Lung Foundation. Dr. Jeppsson has received research grants, consulting fees or speaker’s honorarium from AstraZeneca in addition to several other pharmaceutical companies.
LONDON – Ticagrelor was associated with fewer major bleeding complications compared with clopidogrel when stopped before revascularization surgery, in a large observational study that included all patients on dual antiplatelet therapy who underwent bypass surgery over a 2-year period in Sweden.
The overall incidence of major bleeding was 12.9% and 17.6%, respectively, when these antiplatelet agents were stopped before coronary artery bypass grafting (CABG). The adjusted odds ratio (OR) was 0.72, representing a 28% lower incidence with ticagrelor than with clopidogrel (P = .012).The study findings indicated that it might be safe to stop ticagrelor but not clopidogrel slightly closer to the procedure than is currently recommended by European (Eur Heart J. 2014;35:2541-2619) and American (J Am Coll Cardiol. 2013;61:e179-e347) guidelines.
“The overall incidence of major CABG-related bleeding complications was lower with ticagrelor than with clopidogrel,” Dr. Anders Jeppsson said at the annual meeting of the European Society of Cardiology.
“The difference was mainly driven by a lower incidence when clopidogrel and ticagrelor were discontinued 72 to 120 hours before surgery,” he added.
Dr. Jeppsson of Sahlgrenska (Sweden) University Hospital and the University of Gothenburg noted that the incidence of CABG-related major bleeding was highest for both antiplatelet agents when they were stopped less than 24 hours before surgery but that there was no significant difference between the two antiplatelet agents.
“Discontinuation of ticagrelor 3 days before CABG, as opposed to 5 days, did not increase the incidence of major bleeding complications,” he reported. The OR for discontinuing ticagrelor at 72-120 hours versus more than 120 hours before surgery was 0.93 (P = .08). However, the situation was not the same for discontinuing clopidogrel, with a higher rate of bleeding when the drug was discontinued closer to surgery (OR = 1.17, P = .033).
The findings, which were published online Sept. 1 in the European Heart Journal (doi:10.1093/eurheartj/ehv381), come from an analysis of data prospectively obtained from the SWEDEHEART registry and other local Swedish registries, databases, and patient records. Dr. Jeppsson explained that the aims were to compare the incidence of CABG-related bleeding complications among patients with acute coronary syndromes (ACS) who were taking dual antiplatelet therapy with aspirin and either clopidogrel or ticagrelor in a real-world setting and to see if shorter discontinuation periods before surgery might be feasible.
“A short discontinuation time would reduce the risk for thrombotic events while waiting [for surgery] and save hospital resources,” Dr. Jeppsson said. “But on the other hand it may increase the risk for bleeding complications.”
Data from January 2012 to December 2013 were obtained on all patients in Sweden who were taking dual antiplatelet therapy before CABG. This time period was chosen as it was when ticagrelor was first introduced for the first-line treatment of ACS in the country. Of 2,418 patients identified, 10 were taking prasugrel and were excluded from the analysis. A further 164 patients were excluded as they had discontinued dual antiplatelet therapy more than 2 weeks before having surgery, leaving 1,266 patients who had received ticagrelor and 978 who had been taking clopidogrel.The Bleeding Academic Research Consortium (BARC) Type 4 definition (Circulation. 2011;123:2736-47) was primarily used to identify CABG-related bleeding, with three other published definitions also used, including those used in the BART (N Engl J Med. 2008;358:2319-31) and PLATO (N Engl J Med. 2009;361:1045-57) antiplatelet trials.The overall incidence of major bleeding complications was significantly lower with ticagrelor versus clopidogrel using all four of the bleeding definitions.
However, discontinuing ticagrelor 24 hours or less before CABG showed that while there was a similar amount of BARC major bleeding (P = .052) compared with stopping clopidogrel, the median amount of blood loss (P less than .001), need for red blood cell (P = .028) or platelet (P less than .001) transfusion was greater.To illustrate the dangers of major bleeding on patient outcome, Dr. Jeppsson noted that patients who experienced major bleeding were almost 15 times more likely to die 30 days after the procedure than were those who had no major bleeding. The 30-day mortality rate was higher in clopidogrel than ticagrelor-treated patients (2.7% vs 1.7%) and incidence of thrombotic events was 2.8% and 2.3% These are unadjusted findings and the study was not statistically powered to look at these as end points, Dr. Jeppsson emphasized. These factors were registered for safety reasons, he said.
The study was supported by an investigator-sponsored study program of AstraZeneca and the Swedish Heart and Lung Foundation. Dr. Jeppsson has received research grants, consulting fees or speaker’s honorarium from AstraZeneca in addition to several other pharmaceutical companies.
AT THE ESC CONGRESS 2015
Key clinical point: Ticagrelor was associated with fewer bleeding complications compared with clopidogrel even when stopped closer to coronary artery bypass surgery (CABG).
Major finding: The overall incidence of major bleeding with aspirin/ticagrelor versus aspirin/clopidogrel was 12.9% vs. 17.6% (adjusted hazard ratio 0.72, P = .012).
Data source: Retrospective, observational registry study of all acute coronary syndrome patients in Sweden on dual antiplatelet therapy who underwent CABG between 2012 and 2013.
Disclosures: The study was supported by an investigator-sponsored study program of AstraZeneca and the Swedish Heart and Lung Foundation. Dr. Jeppsson has received research grants, consulting fees or speaker’s honorarium from AstraZeneca in addition to several other pharmaceutical companies.
Heart attack risk rises in first month after knee, hip arthroplasty
Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery, but not at 6 months after surgery, a cohort study showed.
The finding challenges other studies suggesting that total knee or hip arthroplasty surgery reduces the risk of serious cardiovascular events among individuals with osteoarthritis.
Analysis of data from 13,849 British patients who underwent a total knee arthroplasty, 6,063 patients who received total hip arthroplasty, and an equal number of matched controls showed a greater than eightfold increase in the risk of myocardial infarction in the first postoperative month in the knee arthroplasty group (hazard ratio, 8.75), and a fourfold increase in risk in the hip arthroplasty group (HR, 4.33), compared with controls.
However, the hazard ratio declined to insignificance after 6 months, in contrast to the risk of venous thromboembolism – a known complication of arthroplasty – according to a paper published online in the Aug. 31 edition of Arthritis & Rheumatology.
“The major difference between the previous study and ours is that cardiovascular events occurring shortly after total joint arthroplasty were excluded from the previous study,” wrote Na Lu and his colleagues from Boston University.
The study observed 306 cases of myocardial infarction among individuals who underwent total knee arthroplasty and 128 cases in those who underwent total hip arthroplasty (Arthritis Rheumatol. 2015; August 31 [doi:10.1002/art.39246]).
The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no other conflicts of interest declared.
Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery, but not at 6 months after surgery, a cohort study showed.
The finding challenges other studies suggesting that total knee or hip arthroplasty surgery reduces the risk of serious cardiovascular events among individuals with osteoarthritis.
Analysis of data from 13,849 British patients who underwent a total knee arthroplasty, 6,063 patients who received total hip arthroplasty, and an equal number of matched controls showed a greater than eightfold increase in the risk of myocardial infarction in the first postoperative month in the knee arthroplasty group (hazard ratio, 8.75), and a fourfold increase in risk in the hip arthroplasty group (HR, 4.33), compared with controls.
However, the hazard ratio declined to insignificance after 6 months, in contrast to the risk of venous thromboembolism – a known complication of arthroplasty – according to a paper published online in the Aug. 31 edition of Arthritis & Rheumatology.
“The major difference between the previous study and ours is that cardiovascular events occurring shortly after total joint arthroplasty were excluded from the previous study,” wrote Na Lu and his colleagues from Boston University.
The study observed 306 cases of myocardial infarction among individuals who underwent total knee arthroplasty and 128 cases in those who underwent total hip arthroplasty (Arthritis Rheumatol. 2015; August 31 [doi:10.1002/art.39246]).
The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no other conflicts of interest declared.
Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery, but not at 6 months after surgery, a cohort study showed.
The finding challenges other studies suggesting that total knee or hip arthroplasty surgery reduces the risk of serious cardiovascular events among individuals with osteoarthritis.
Analysis of data from 13,849 British patients who underwent a total knee arthroplasty, 6,063 patients who received total hip arthroplasty, and an equal number of matched controls showed a greater than eightfold increase in the risk of myocardial infarction in the first postoperative month in the knee arthroplasty group (hazard ratio, 8.75), and a fourfold increase in risk in the hip arthroplasty group (HR, 4.33), compared with controls.
However, the hazard ratio declined to insignificance after 6 months, in contrast to the risk of venous thromboembolism – a known complication of arthroplasty – according to a paper published online in the Aug. 31 edition of Arthritis & Rheumatology.
“The major difference between the previous study and ours is that cardiovascular events occurring shortly after total joint arthroplasty were excluded from the previous study,” wrote Na Lu and his colleagues from Boston University.
The study observed 306 cases of myocardial infarction among individuals who underwent total knee arthroplasty and 128 cases in those who underwent total hip arthroplasty (Arthritis Rheumatol. 2015; August 31 [doi:10.1002/art.39246]).
The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no other conflicts of interest declared.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery.
Major finding: Patients undergoing total knee arthroplasty have an eightfold increase in the risk of myocardial infarction in the month after surgery.
Data source: Cohort study of 13,849 total knee arthroplasty patients and 6,063 total hip arthroplasty patients and an equal number of matched controls.
Disclosures: The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no conflicts of interest declared.
Less posttransplant primary biliary cirrhosis with preventive UDCA
Only 21% of liver transplantation patients who received ursodeoxycholic acid (UDCA) after surgery developed recurrent primary biliary cirrhosis, compared with 62% of patients who did not receive the bile acid, researchers reported in the Journal of Hepatology.
The results provide strong evidence that routinely giving liver transplant patients UDCA can prevent or delay recurrent primary biliary cirrhosis, said Alexie Bosch at Hôpital Edouard Herriot in Lyon, France, and his associates.
Primary biliary cirrhosis can recur after liver transplantation and increases the chances of graft dysfunction, the researchers noted. UDCA is the only approved medical treatment for primary biliary cirrhosis in the United States or Europe, but no research team has studied its potential to prevent recurrent primary biliary cirrhosis after liver transplantation, they added. Therefore, they retrospectively studied 90 patients with primary biliary cirrhosis who underwent liver transplantation at five centers in France and Switzerland between 1988 and 2010. In all, 21% of patients received oral UDCA (10-15 mg/kg per day in two divided doses) within 2 weeks after their operation, while the rest received it only if they developed biopsy-confirmed recurrent primary biliary cirrhosis. Biopsies were taken at posttransplant year 1 and every 5 years after that, or when clinically indicated, the investigators noted (J Hepatol. 2015 Aug. 14. doi: 10.1016/j.jhep.2015.07.038).
Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of postsurgical follow-up (P = .014), the researchers reported. The chances of recurrent primary biliary cirrhosis at 5, 10, and 15 years after transplantation were 11%, 21%, and 40% in the UDCA group, compared with 32%, 53%, and 70% for patients who did not receive prophylactic UDCA, they added. A multivariable analysis showed that recurrent primary biliary cirrhosis was associated with not receiving prophylactic UDCA (hazard ratio, 0.32; 95% confidence interval, 0.11, 0.91), but was not linked to donor age, Model For End-Stage Liver Disease (MELD) score, or sex mismatch between donor and recipient, the investigators said. Preventive UDCA also was tied to a 1.6-year longer median time to recurrence, although the trend did not reach statistical significance.
Although the study was retrospective and most patients who received UDCA were treated at one transplant center, all centers had similar histologic findings for recurrent primary biliary cirrhosis, said the researchers. Biopsies also were histologically similar regardless of whether they were event driven or obtained based on the study protocol, and time to recurrence did not vary based on biopsy type, they added. “In our multivariate analysis, we took care to account for all risk factors and confounders, as well as to test multilevel models in order to exclude potential misleading results and center effects,” they emphasized. “Given the extremely limited feasibility of prospective studies and the good tolerance and acceptability of long-term UDCA therapy, these results support the extended use of UDCA as prophylaxis for primary biliary cirrhosis recurrence after liver transplantation.”
The researchers declared no funding sources and reported having no conflicts of interest.
Only 21% of liver transplantation patients who received ursodeoxycholic acid (UDCA) after surgery developed recurrent primary biliary cirrhosis, compared with 62% of patients who did not receive the bile acid, researchers reported in the Journal of Hepatology.
The results provide strong evidence that routinely giving liver transplant patients UDCA can prevent or delay recurrent primary biliary cirrhosis, said Alexie Bosch at Hôpital Edouard Herriot in Lyon, France, and his associates.
Primary biliary cirrhosis can recur after liver transplantation and increases the chances of graft dysfunction, the researchers noted. UDCA is the only approved medical treatment for primary biliary cirrhosis in the United States or Europe, but no research team has studied its potential to prevent recurrent primary biliary cirrhosis after liver transplantation, they added. Therefore, they retrospectively studied 90 patients with primary biliary cirrhosis who underwent liver transplantation at five centers in France and Switzerland between 1988 and 2010. In all, 21% of patients received oral UDCA (10-15 mg/kg per day in two divided doses) within 2 weeks after their operation, while the rest received it only if they developed biopsy-confirmed recurrent primary biliary cirrhosis. Biopsies were taken at posttransplant year 1 and every 5 years after that, or when clinically indicated, the investigators noted (J Hepatol. 2015 Aug. 14. doi: 10.1016/j.jhep.2015.07.038).
Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of postsurgical follow-up (P = .014), the researchers reported. The chances of recurrent primary biliary cirrhosis at 5, 10, and 15 years after transplantation were 11%, 21%, and 40% in the UDCA group, compared with 32%, 53%, and 70% for patients who did not receive prophylactic UDCA, they added. A multivariable analysis showed that recurrent primary biliary cirrhosis was associated with not receiving prophylactic UDCA (hazard ratio, 0.32; 95% confidence interval, 0.11, 0.91), but was not linked to donor age, Model For End-Stage Liver Disease (MELD) score, or sex mismatch between donor and recipient, the investigators said. Preventive UDCA also was tied to a 1.6-year longer median time to recurrence, although the trend did not reach statistical significance.
Although the study was retrospective and most patients who received UDCA were treated at one transplant center, all centers had similar histologic findings for recurrent primary biliary cirrhosis, said the researchers. Biopsies also were histologically similar regardless of whether they were event driven or obtained based on the study protocol, and time to recurrence did not vary based on biopsy type, they added. “In our multivariate analysis, we took care to account for all risk factors and confounders, as well as to test multilevel models in order to exclude potential misleading results and center effects,” they emphasized. “Given the extremely limited feasibility of prospective studies and the good tolerance and acceptability of long-term UDCA therapy, these results support the extended use of UDCA as prophylaxis for primary biliary cirrhosis recurrence after liver transplantation.”
The researchers declared no funding sources and reported having no conflicts of interest.
Only 21% of liver transplantation patients who received ursodeoxycholic acid (UDCA) after surgery developed recurrent primary biliary cirrhosis, compared with 62% of patients who did not receive the bile acid, researchers reported in the Journal of Hepatology.
The results provide strong evidence that routinely giving liver transplant patients UDCA can prevent or delay recurrent primary biliary cirrhosis, said Alexie Bosch at Hôpital Edouard Herriot in Lyon, France, and his associates.
Primary biliary cirrhosis can recur after liver transplantation and increases the chances of graft dysfunction, the researchers noted. UDCA is the only approved medical treatment for primary biliary cirrhosis in the United States or Europe, but no research team has studied its potential to prevent recurrent primary biliary cirrhosis after liver transplantation, they added. Therefore, they retrospectively studied 90 patients with primary biliary cirrhosis who underwent liver transplantation at five centers in France and Switzerland between 1988 and 2010. In all, 21% of patients received oral UDCA (10-15 mg/kg per day in two divided doses) within 2 weeks after their operation, while the rest received it only if they developed biopsy-confirmed recurrent primary biliary cirrhosis. Biopsies were taken at posttransplant year 1 and every 5 years after that, or when clinically indicated, the investigators noted (J Hepatol. 2015 Aug. 14. doi: 10.1016/j.jhep.2015.07.038).
Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of postsurgical follow-up (P = .014), the researchers reported. The chances of recurrent primary biliary cirrhosis at 5, 10, and 15 years after transplantation were 11%, 21%, and 40% in the UDCA group, compared with 32%, 53%, and 70% for patients who did not receive prophylactic UDCA, they added. A multivariable analysis showed that recurrent primary biliary cirrhosis was associated with not receiving prophylactic UDCA (hazard ratio, 0.32; 95% confidence interval, 0.11, 0.91), but was not linked to donor age, Model For End-Stage Liver Disease (MELD) score, or sex mismatch between donor and recipient, the investigators said. Preventive UDCA also was tied to a 1.6-year longer median time to recurrence, although the trend did not reach statistical significance.
Although the study was retrospective and most patients who received UDCA were treated at one transplant center, all centers had similar histologic findings for recurrent primary biliary cirrhosis, said the researchers. Biopsies also were histologically similar regardless of whether they were event driven or obtained based on the study protocol, and time to recurrence did not vary based on biopsy type, they added. “In our multivariate analysis, we took care to account for all risk factors and confounders, as well as to test multilevel models in order to exclude potential misleading results and center effects,” they emphasized. “Given the extremely limited feasibility of prospective studies and the good tolerance and acceptability of long-term UDCA therapy, these results support the extended use of UDCA as prophylaxis for primary biliary cirrhosis recurrence after liver transplantation.”
The researchers declared no funding sources and reported having no conflicts of interest.
FROM THE JOURNAL OF HEPATOLOGY
Key clinical point: Treatment with prophylactic ursodeoxycholic acid might help prevent recurrent primary biliary cirrhosis after liver transplantation.
Major finding: Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of follow-up (P = .014).
Data source: Multicenter retrospective study of 90 patients who underwent liver transplantation for primary biliary cirrhosis.
Disclosures: The researchers declared no funding sources and reported having no conflicts of interest.
Burning the midnight oil does not impact surgical outcomes
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The risks of adverse outcomes of elective daytime surgical procedures were similar whether or not the attending physician had provided medical care the previous night.
Major finding: The primary composite endpoint was similar between the postmidnight and control groups (22.2% vs. 22.4%; P = .66).
Data source: Population-based, retrospective, matched cohort study in 38,978 patients.
Disclosures: Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
Scoring tool points to postop ventilator dependence
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A preoperative risk score can help identify patients at highest risk for postoperative ventilator dependence.
Major finding: A risk score greater than 3 identified the top 20%-30% of patients experiencing 60%-70% of postop ventilator dependence events.
Data source: Retrospective analysis of 7,473 elective general and vascular surgical patients.
Disclosures: The authors reported having no financial disclosures.
OR-focused effort cuts catheter use, surgical UTIs
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: An OR-focused multidisciplinary effort decreased catheter use in the operating room and catheter-associated UTIs.
Major finding: Catheter utilization in short cases declined 9% and surgical CAUTI by 89%.
Data source: Observational analysis of 2,809 surgical catheters placed.
Disclosures: The authors reported having no financial disclosures.
Longer hospitalization after bariatric surgery ups readmission risk
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
FROM SURGERY
Key clinical point: Short length of hospital stay after bariatric surgery was not a risk factor for readmission.
Major finding: Patients who were hospitalized for 3 days and longer were two to four times as likely to be readmitted than were patients with 1-day stays (P less than .001 for both).
Data source: Multicenter database analysis of postoperative outcomes for 95,294 bariatric surgery patients.
Disclosures: The Medical College of Wisconsin and the National Institutes of Health supported the research. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Modifiable risk factors foretell colonic anastomotic leak
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
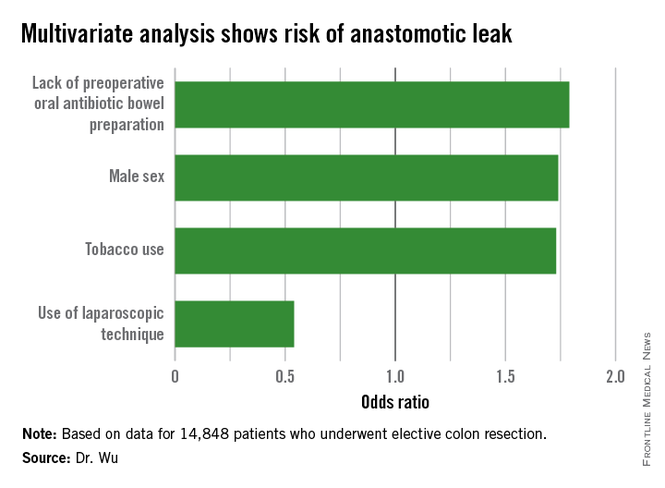
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
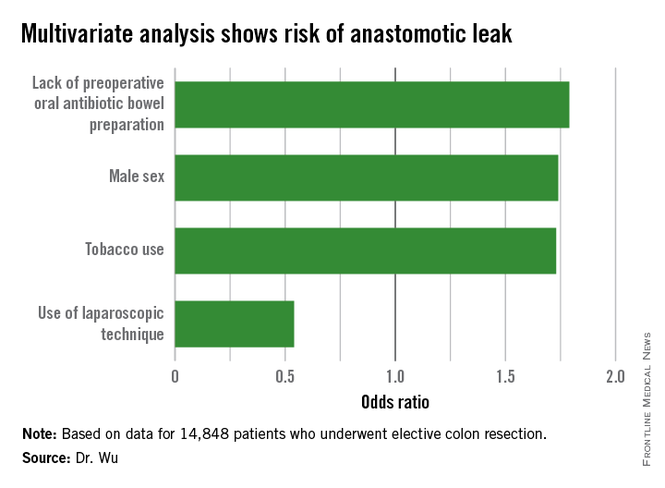
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
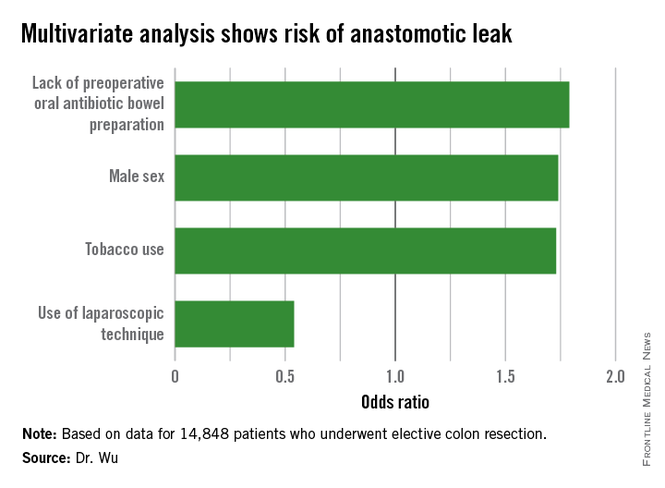
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Altering specific patient and operative factors can modify the risk of anastomotic leakage after colectomy.
Major finding: Male sex (OR, 1.74), tobacco use (OR, 1.73), and lack of an oral antibiotic bowel preparation (OR, 1.79) predicted anastomotic leak.
Data source: A retrospective study of 14,848 elective colectomies.
Disclosures: The authors reported having no relevant financial disclosures.
Intestinal obstruction risk increased in some childhood cancer survivors
Childhood cancer survivors are at an increased risk for developing an intestinal obstruction requiring surgery (IOS) 5 or more years after the initial cancer diagnosis, according to a study based on data from the Childhood Cancer Survivor Study.
The risk was greater among those who had a pelvic or abdominal tumor and had been exposed to pelvic or abdominal radiotherapy, reported the authors, who pointed out that no study has “rigorously” investigated the incidence of intestinal obstruction in childhood cancer survivors. The study appeared online in the Journal of Clinical Oncology (2015 Aug 10 doi: 10.1200/JCO.2015.61.5070).
The subjects in the study had been diagnosed with cancer before age 21 years between 1970 and 1986 and were followed longitudinally in the CCSS. The sample included 12,316 childhood cancer survivors who had survived at least 5 years from the time they were diagnosed with cancer and 4,023 of their siblings.
The cumulative incidence of “late” IOS (occurring at least 5 years after the cancer diagnosis) was 5.8% among those who had an abdominopelvic tumor and 1% among those who had other types of cancer, compared with 0.3% among siblings, who served as controls in the study. After adjusting for year of diagnosis, age at diagnosis, cancer type, radiotherapy, surgery, and other confounding factors, the risk of late IOS was significantly increased among those who had an abdominopelvic tumor (3.6 times greater) and those who had received abdominal/pelvic radiotherapy (2.4 times greater). Mortality was also almost twofold higher among those who developed late IOS when adjusted for the same factors, but there was no association with chemotherapy, cyclophosphamide equivalent dose, or platinum agent score and late IOS.
“The risk of IOS extends for decades beyond cancer diagnosis, implying the need for long-term vigilance, especially among survivors with abdominal or pelvic tumors and survivors who have undergone treatment with abdominal or pelvic surgery or radiotherapy,” concluded lead author Dr. Arin Madenci of Boston Children’s Hospital and his coauthors.
“Widespread awareness of the signs and symptoms of IOS will facilitate timely presentation and effective management of this complication. Although prevention of IOS is not currently possible, education of survivors of cancer, their families, and their health care providers is critical,” they added.
The study was supported by grants from the National Cancer Institute and Cancer Center Support (Centers of Research Excellence) and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
Childhood cancer survivors are at an increased risk for developing an intestinal obstruction requiring surgery (IOS) 5 or more years after the initial cancer diagnosis, according to a study based on data from the Childhood Cancer Survivor Study.
The risk was greater among those who had a pelvic or abdominal tumor and had been exposed to pelvic or abdominal radiotherapy, reported the authors, who pointed out that no study has “rigorously” investigated the incidence of intestinal obstruction in childhood cancer survivors. The study appeared online in the Journal of Clinical Oncology (2015 Aug 10 doi: 10.1200/JCO.2015.61.5070).
The subjects in the study had been diagnosed with cancer before age 21 years between 1970 and 1986 and were followed longitudinally in the CCSS. The sample included 12,316 childhood cancer survivors who had survived at least 5 years from the time they were diagnosed with cancer and 4,023 of their siblings.
The cumulative incidence of “late” IOS (occurring at least 5 years after the cancer diagnosis) was 5.8% among those who had an abdominopelvic tumor and 1% among those who had other types of cancer, compared with 0.3% among siblings, who served as controls in the study. After adjusting for year of diagnosis, age at diagnosis, cancer type, radiotherapy, surgery, and other confounding factors, the risk of late IOS was significantly increased among those who had an abdominopelvic tumor (3.6 times greater) and those who had received abdominal/pelvic radiotherapy (2.4 times greater). Mortality was also almost twofold higher among those who developed late IOS when adjusted for the same factors, but there was no association with chemotherapy, cyclophosphamide equivalent dose, or platinum agent score and late IOS.
“The risk of IOS extends for decades beyond cancer diagnosis, implying the need for long-term vigilance, especially among survivors with abdominal or pelvic tumors and survivors who have undergone treatment with abdominal or pelvic surgery or radiotherapy,” concluded lead author Dr. Arin Madenci of Boston Children’s Hospital and his coauthors.
“Widespread awareness of the signs and symptoms of IOS will facilitate timely presentation and effective management of this complication. Although prevention of IOS is not currently possible, education of survivors of cancer, their families, and their health care providers is critical,” they added.
The study was supported by grants from the National Cancer Institute and Cancer Center Support (Centers of Research Excellence) and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
Childhood cancer survivors are at an increased risk for developing an intestinal obstruction requiring surgery (IOS) 5 or more years after the initial cancer diagnosis, according to a study based on data from the Childhood Cancer Survivor Study.
The risk was greater among those who had a pelvic or abdominal tumor and had been exposed to pelvic or abdominal radiotherapy, reported the authors, who pointed out that no study has “rigorously” investigated the incidence of intestinal obstruction in childhood cancer survivors. The study appeared online in the Journal of Clinical Oncology (2015 Aug 10 doi: 10.1200/JCO.2015.61.5070).
The subjects in the study had been diagnosed with cancer before age 21 years between 1970 and 1986 and were followed longitudinally in the CCSS. The sample included 12,316 childhood cancer survivors who had survived at least 5 years from the time they were diagnosed with cancer and 4,023 of their siblings.
The cumulative incidence of “late” IOS (occurring at least 5 years after the cancer diagnosis) was 5.8% among those who had an abdominopelvic tumor and 1% among those who had other types of cancer, compared with 0.3% among siblings, who served as controls in the study. After adjusting for year of diagnosis, age at diagnosis, cancer type, radiotherapy, surgery, and other confounding factors, the risk of late IOS was significantly increased among those who had an abdominopelvic tumor (3.6 times greater) and those who had received abdominal/pelvic radiotherapy (2.4 times greater). Mortality was also almost twofold higher among those who developed late IOS when adjusted for the same factors, but there was no association with chemotherapy, cyclophosphamide equivalent dose, or platinum agent score and late IOS.
“The risk of IOS extends for decades beyond cancer diagnosis, implying the need for long-term vigilance, especially among survivors with abdominal or pelvic tumors and survivors who have undergone treatment with abdominal or pelvic surgery or radiotherapy,” concluded lead author Dr. Arin Madenci of Boston Children’s Hospital and his coauthors.
“Widespread awareness of the signs and symptoms of IOS will facilitate timely presentation and effective management of this complication. Although prevention of IOS is not currently possible, education of survivors of cancer, their families, and their health care providers is critical,” they added.
The study was supported by grants from the National Cancer Institute and Cancer Center Support (Centers of Research Excellence) and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Some childhood cancer survivors are at a significantly increased risk of developing an intestinal obstruction requiring surgery (IOS), which should be considered in their long-term follow-up.
Major finding: The cumulative incidence of IOS occurring at least 5 years after the cancer diagnosis was 5.8% among those who had an abdominopelvic tumor and 1% among those who did not have an abdominopelvic tumor, compared with 0.3% among sibling controls in the study, and late IOS was associated with increased mortality.
Data source: A retrospective cohort study involving 12,316 childhood cancer survivors who had survived at least 5 years and 4,023 of their siblings, who served as controls, from the Childhood Cancer Survivor Study.
Disclosures: The study was supported by National Cancer Institute and Cancer Center Support (Centers of Research Excellence) grants, and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
Are oral antibiotics enough to reduce colorectal surgery infections?
CHICAGO – Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection in a large national patient sample.
Oral antibiotics (OA) alone significantly reduced the rate of any surgical site infection (SSI) by 44% (odds ratio, 0.56; 95% confidence interval, 0.36-0.87) and wound SSI by 59% (OR, 0.41; 95% CI, 0.23-0.72), compared with no bowel preparation in propensity-adjusted multivariate analysis.
OA combined with mechanical bowel preparation (MBP) was independently associated with significant reductions of 54%, 58%, and 41%, respectively, for any SSI (OR, 0.46; 95% CI, 0.38-0.55), wound SSI (OR, 0.42; 95% CI, 0.33-0.53), and organ space SSI (OR, 0.59; 95% CI, 0.44-0.78).
In contrast, MBP, which was used in 40.8% of cases, was not independently associated with reduced rates of any SSI (OR, 0.95; 95% CI, 0.82-1.10), wound SSI (OR, 0.91; 95% CI, 0.76-1.09), or organ space SSI (OR, 1.0; 95% CI, 0.79-1.27), according to Dr. Sarah Koller of Temple University Hospital in Philadelphia and her associates.
A limitation of the study was the lack of information on type of OA or MBP used, patient compliance, and use of parenteral antibiotic prophylaxis.
“Randomized clinical trials are needed to determine the true benefits of oral antibiotics alone versus combined oral antibiotics and mechanical bowel prep prior to elective colorectal resection,” Dr. Koller said at the American College of Surgeons/National Surgery Quality Improvement Program National Conference.
Session comoderator Dr. E. Patchen Dellinger, of the University of Washington in Seattle, commented, “Logically, it’s hard for me to believe that oral antibiotics would affect a couple of kilograms of stool in the colon and yet here are these tantalizing data. So we do need the prospective trial you mention.
“But, the other thing that blows my mind every time I see these data is 49% of people getting a mechanical bowel prep without oral antibiotics, which has conclusively been shown to be useless for anything but torture of the patient.”
Significant variability in the use of bowel preparation exists within the surgical community, with a recent survey of colorectal surgeons revealing that 76% routinely used MBP and only 36% routinely used oral antibiotics, Dr. Koller observed.
In the current analysis, just 3.3% of patients received OA, 30.4% OA plus MBP, 40.8% MBP, and 25.5% no bowel preparation.
Physicians have been slow to abandon MBP, despite multiple studies showing that MBP alone does not reduce SSIs in elective colon and rectal surgery. There also have been reports of higher rates of anastomotic leak, increased cardiac or metabolic complications, and a slower return of bowel function with MBP.
Several studies, including a recent Cochrane Database Review, have shown that oral or intravenous antibiotic prophylaxis reduces surgical wound infection after colorectal surgery. The comparison groups are not uniform across the studies, however, and the controversy persists as to which type of bowel prep best reduces SSI after colorectal surgery, she said.
To explore this issue, the investigators identified all patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013. The cohort included 19,372 patients with complete preoperative bowel preparation data. Patients who were ventilator dependent or had infections or open wounds at the time of surgery were excluded.
The overall rates of any SSI, wound SSI (superficial and/or deep), and organ space SSI were 9.5%, 6.4%, and 3.5%, respectively.
With regard to adverse outcomes cited in previous studies, only OA plus MBP was shown to independently reduce anastomotic leak (OR, 0.57; 95% CI, 0.42-0.78) and postoperative ileus (OR, 0.79; 95% CI, 0.68-0.92), compared with no bowel prep, Dr. Koller reported.
Both OA and OA plus MBP, however, decreased length of stay by 0.83 days.
None of the bowel preparations were independently associated with increased rates of cardiac or renal complications, she said.
The investigators were not able to track rates of Clostridium difficile colitis after administration of the oral antibiotics. Dr. Koller acknowledged this is a concern when using oral antibiotics and may contribute to why they aren’t used frequently.
Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
CHICAGO – Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection in a large national patient sample.
Oral antibiotics (OA) alone significantly reduced the rate of any surgical site infection (SSI) by 44% (odds ratio, 0.56; 95% confidence interval, 0.36-0.87) and wound SSI by 59% (OR, 0.41; 95% CI, 0.23-0.72), compared with no bowel preparation in propensity-adjusted multivariate analysis.
OA combined with mechanical bowel preparation (MBP) was independently associated with significant reductions of 54%, 58%, and 41%, respectively, for any SSI (OR, 0.46; 95% CI, 0.38-0.55), wound SSI (OR, 0.42; 95% CI, 0.33-0.53), and organ space SSI (OR, 0.59; 95% CI, 0.44-0.78).
In contrast, MBP, which was used in 40.8% of cases, was not independently associated with reduced rates of any SSI (OR, 0.95; 95% CI, 0.82-1.10), wound SSI (OR, 0.91; 95% CI, 0.76-1.09), or organ space SSI (OR, 1.0; 95% CI, 0.79-1.27), according to Dr. Sarah Koller of Temple University Hospital in Philadelphia and her associates.
A limitation of the study was the lack of information on type of OA or MBP used, patient compliance, and use of parenteral antibiotic prophylaxis.
“Randomized clinical trials are needed to determine the true benefits of oral antibiotics alone versus combined oral antibiotics and mechanical bowel prep prior to elective colorectal resection,” Dr. Koller said at the American College of Surgeons/National Surgery Quality Improvement Program National Conference.
Session comoderator Dr. E. Patchen Dellinger, of the University of Washington in Seattle, commented, “Logically, it’s hard for me to believe that oral antibiotics would affect a couple of kilograms of stool in the colon and yet here are these tantalizing data. So we do need the prospective trial you mention.
“But, the other thing that blows my mind every time I see these data is 49% of people getting a mechanical bowel prep without oral antibiotics, which has conclusively been shown to be useless for anything but torture of the patient.”
Significant variability in the use of bowel preparation exists within the surgical community, with a recent survey of colorectal surgeons revealing that 76% routinely used MBP and only 36% routinely used oral antibiotics, Dr. Koller observed.
In the current analysis, just 3.3% of patients received OA, 30.4% OA plus MBP, 40.8% MBP, and 25.5% no bowel preparation.
Physicians have been slow to abandon MBP, despite multiple studies showing that MBP alone does not reduce SSIs in elective colon and rectal surgery. There also have been reports of higher rates of anastomotic leak, increased cardiac or metabolic complications, and a slower return of bowel function with MBP.
Several studies, including a recent Cochrane Database Review, have shown that oral or intravenous antibiotic prophylaxis reduces surgical wound infection after colorectal surgery. The comparison groups are not uniform across the studies, however, and the controversy persists as to which type of bowel prep best reduces SSI after colorectal surgery, she said.
To explore this issue, the investigators identified all patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013. The cohort included 19,372 patients with complete preoperative bowel preparation data. Patients who were ventilator dependent or had infections or open wounds at the time of surgery were excluded.
The overall rates of any SSI, wound SSI (superficial and/or deep), and organ space SSI were 9.5%, 6.4%, and 3.5%, respectively.
With regard to adverse outcomes cited in previous studies, only OA plus MBP was shown to independently reduce anastomotic leak (OR, 0.57; 95% CI, 0.42-0.78) and postoperative ileus (OR, 0.79; 95% CI, 0.68-0.92), compared with no bowel prep, Dr. Koller reported.
Both OA and OA plus MBP, however, decreased length of stay by 0.83 days.
None of the bowel preparations were independently associated with increased rates of cardiac or renal complications, she said.
The investigators were not able to track rates of Clostridium difficile colitis after administration of the oral antibiotics. Dr. Koller acknowledged this is a concern when using oral antibiotics and may contribute to why they aren’t used frequently.
Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
CHICAGO – Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection in a large national patient sample.
Oral antibiotics (OA) alone significantly reduced the rate of any surgical site infection (SSI) by 44% (odds ratio, 0.56; 95% confidence interval, 0.36-0.87) and wound SSI by 59% (OR, 0.41; 95% CI, 0.23-0.72), compared with no bowel preparation in propensity-adjusted multivariate analysis.
OA combined with mechanical bowel preparation (MBP) was independently associated with significant reductions of 54%, 58%, and 41%, respectively, for any SSI (OR, 0.46; 95% CI, 0.38-0.55), wound SSI (OR, 0.42; 95% CI, 0.33-0.53), and organ space SSI (OR, 0.59; 95% CI, 0.44-0.78).
In contrast, MBP, which was used in 40.8% of cases, was not independently associated with reduced rates of any SSI (OR, 0.95; 95% CI, 0.82-1.10), wound SSI (OR, 0.91; 95% CI, 0.76-1.09), or organ space SSI (OR, 1.0; 95% CI, 0.79-1.27), according to Dr. Sarah Koller of Temple University Hospital in Philadelphia and her associates.
A limitation of the study was the lack of information on type of OA or MBP used, patient compliance, and use of parenteral antibiotic prophylaxis.
“Randomized clinical trials are needed to determine the true benefits of oral antibiotics alone versus combined oral antibiotics and mechanical bowel prep prior to elective colorectal resection,” Dr. Koller said at the American College of Surgeons/National Surgery Quality Improvement Program National Conference.
Session comoderator Dr. E. Patchen Dellinger, of the University of Washington in Seattle, commented, “Logically, it’s hard for me to believe that oral antibiotics would affect a couple of kilograms of stool in the colon and yet here are these tantalizing data. So we do need the prospective trial you mention.
“But, the other thing that blows my mind every time I see these data is 49% of people getting a mechanical bowel prep without oral antibiotics, which has conclusively been shown to be useless for anything but torture of the patient.”
Significant variability in the use of bowel preparation exists within the surgical community, with a recent survey of colorectal surgeons revealing that 76% routinely used MBP and only 36% routinely used oral antibiotics, Dr. Koller observed.
In the current analysis, just 3.3% of patients received OA, 30.4% OA plus MBP, 40.8% MBP, and 25.5% no bowel preparation.
Physicians have been slow to abandon MBP, despite multiple studies showing that MBP alone does not reduce SSIs in elective colon and rectal surgery. There also have been reports of higher rates of anastomotic leak, increased cardiac or metabolic complications, and a slower return of bowel function with MBP.
Several studies, including a recent Cochrane Database Review, have shown that oral or intravenous antibiotic prophylaxis reduces surgical wound infection after colorectal surgery. The comparison groups are not uniform across the studies, however, and the controversy persists as to which type of bowel prep best reduces SSI after colorectal surgery, she said.
To explore this issue, the investigators identified all patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013. The cohort included 19,372 patients with complete preoperative bowel preparation data. Patients who were ventilator dependent or had infections or open wounds at the time of surgery were excluded.
The overall rates of any SSI, wound SSI (superficial and/or deep), and organ space SSI were 9.5%, 6.4%, and 3.5%, respectively.
With regard to adverse outcomes cited in previous studies, only OA plus MBP was shown to independently reduce anastomotic leak (OR, 0.57; 95% CI, 0.42-0.78) and postoperative ileus (OR, 0.79; 95% CI, 0.68-0.92), compared with no bowel prep, Dr. Koller reported.
Both OA and OA plus MBP, however, decreased length of stay by 0.83 days.
None of the bowel preparations were independently associated with increased rates of cardiac or renal complications, she said.
The investigators were not able to track rates of Clostridium difficile colitis after administration of the oral antibiotics. Dr. Koller acknowledged this is a concern when using oral antibiotics and may contribute to why they aren’t used frequently.
Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection.
Major finding: Oral antibiotics alone significantly reduced the rate of any surgical site infection by 44% and wound SSI by 59%.
Data source: Data from 19,372 patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013.
Disclosures: Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.