User login
Study: More DVTs than expected in patients who had varicose vein surgeries
A retrospective study of patients who underwent varicose vein surgeries with a tourniquet found a greater incidence of deep vein thromboses (DVTs) than previous studies.
Within the first 3 postoperative days, 113 (7.7%) of the 1,461 patients had DVTs. The researchers also found that DVTs occurred significantly more often in patients with gastrocnemius vein dilation (GVD). A total of 410 (28%) of the study’s participants had GVTs, and the incidence of DVTs was significantly greater in individuals with GVD compared to those without such a symptom. GVD had a higher predictive power for postoperative DVT than did all of the other risk factors examined in univariate and multivariate analyses.
The vast majority of the DVTs diagnosed were isolated distal. While 94 patients suffered from this kind of DVT, the remaining 19 DVTs were proximal. According to Dr. Chen Kai of Wenzhou (China) Medical University, and colleagues, proximal DVTs were nearly always asymptomatic and a larger percentage of them took more time to disappear than did the distal DVTs. Within 6 months following anticoagulant therapy, 94.3% of the distal DVTs exhibited thrombus resolution and 55.6% of the proximal DVTs were thrombus free. None of the study’s participants had died because of DVT or pulmonary embolus during the 6 months following their surgeries.
This study’s “present data reflect a higher incidence of postoperative DVT than previous studies, and we also identify GVD as a significant risk factor. Larger prospective studies will be needed to evaluate this issue precisely and to understand the clinical relevance of these results,” wrote the researchers.Find the full study in Thombosis Research (doi: 10.1016/j.thromres.2015.03.008).
A retrospective study of patients who underwent varicose vein surgeries with a tourniquet found a greater incidence of deep vein thromboses (DVTs) than previous studies.
Within the first 3 postoperative days, 113 (7.7%) of the 1,461 patients had DVTs. The researchers also found that DVTs occurred significantly more often in patients with gastrocnemius vein dilation (GVD). A total of 410 (28%) of the study’s participants had GVTs, and the incidence of DVTs was significantly greater in individuals with GVD compared to those without such a symptom. GVD had a higher predictive power for postoperative DVT than did all of the other risk factors examined in univariate and multivariate analyses.
The vast majority of the DVTs diagnosed were isolated distal. While 94 patients suffered from this kind of DVT, the remaining 19 DVTs were proximal. According to Dr. Chen Kai of Wenzhou (China) Medical University, and colleagues, proximal DVTs were nearly always asymptomatic and a larger percentage of them took more time to disappear than did the distal DVTs. Within 6 months following anticoagulant therapy, 94.3% of the distal DVTs exhibited thrombus resolution and 55.6% of the proximal DVTs were thrombus free. None of the study’s participants had died because of DVT or pulmonary embolus during the 6 months following their surgeries.
This study’s “present data reflect a higher incidence of postoperative DVT than previous studies, and we also identify GVD as a significant risk factor. Larger prospective studies will be needed to evaluate this issue precisely and to understand the clinical relevance of these results,” wrote the researchers.Find the full study in Thombosis Research (doi: 10.1016/j.thromres.2015.03.008).
A retrospective study of patients who underwent varicose vein surgeries with a tourniquet found a greater incidence of deep vein thromboses (DVTs) than previous studies.
Within the first 3 postoperative days, 113 (7.7%) of the 1,461 patients had DVTs. The researchers also found that DVTs occurred significantly more often in patients with gastrocnemius vein dilation (GVD). A total of 410 (28%) of the study’s participants had GVTs, and the incidence of DVTs was significantly greater in individuals with GVD compared to those without such a symptom. GVD had a higher predictive power for postoperative DVT than did all of the other risk factors examined in univariate and multivariate analyses.
The vast majority of the DVTs diagnosed were isolated distal. While 94 patients suffered from this kind of DVT, the remaining 19 DVTs were proximal. According to Dr. Chen Kai of Wenzhou (China) Medical University, and colleagues, proximal DVTs were nearly always asymptomatic and a larger percentage of them took more time to disappear than did the distal DVTs. Within 6 months following anticoagulant therapy, 94.3% of the distal DVTs exhibited thrombus resolution and 55.6% of the proximal DVTs were thrombus free. None of the study’s participants had died because of DVT or pulmonary embolus during the 6 months following their surgeries.
This study’s “present data reflect a higher incidence of postoperative DVT than previous studies, and we also identify GVD as a significant risk factor. Larger prospective studies will be needed to evaluate this issue precisely and to understand the clinical relevance of these results,” wrote the researchers.Find the full study in Thombosis Research (doi: 10.1016/j.thromres.2015.03.008).
Risk scale predicts mortality after gastric cancer surgery
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
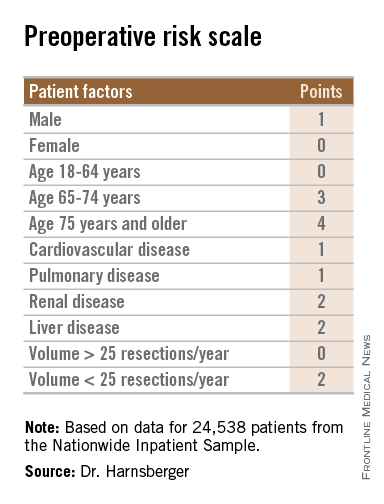
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
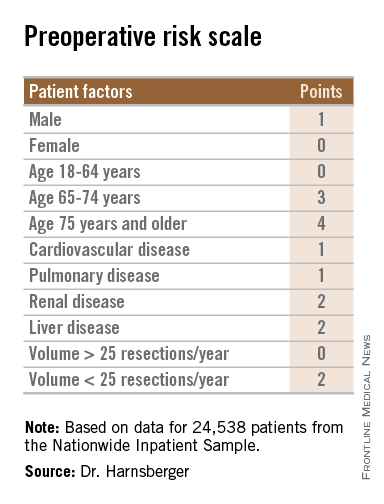
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
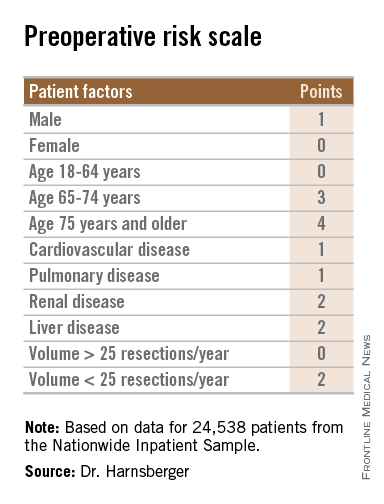
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
AT SSO 2015
Key clinical point: The bedside risk scale can be used in patient counseling prior to surgery for gastric malignancies.
Major finding: Patients with scores of 0-5 had perioperative death rates of 1.3%-4.5%. Patients with higher scores had death rates ranging from 6.0% to 23.1%.
Data source: Review of retrospective data on 24,538 adults who underwent partial or total gastric resection for malignancies.
Disclosures: The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
Four-port laparoscopic cholecystectomy linked to less fatigue
Single-port and four-port laparoscopic cholecystectomy were associated with similar self-reported pain scores and physiologic measures of recovery, according to a double-blinded, randomized trial published online in the Journal of the American College of Surgery.
But patients in the four-port arm reported significantly less fatigue (P = .009), and 40% needed postoperative narcotics, compared with 60% of patients who underwent single-port laparoscopy (P = .056), reported Dr. Juliane Bingener and her associates at Mayo Clinic, Rochester, N.Y.
“The data from this study may assist patients and surgeons in the discussion on how to choose a procedure,” said the researchers. “If fast postoperative recovery is the most important goal, four-port cholecystectomy may be more advantageous than single-port laparoscopic cholecystectomy. If cosmesis is the most important factor, single-port entry may be chosen” (J. Am. Coll. Surg. 2015 March 2 [doi:10.1016/j.jamcollsurg.2015.02.022]).
The study comprised 110 patients, of whom half underwent single-port and half underwent four-port laparoscopic cholecystectomy, all performed by the same surgeon. The primary outcome was patient-reported pain 7 days after the procedure, as measured by the visual analog scale (VAS). In all, 81% of patients were female, and median age was 47.5 years, the researchers reported.
Postoperative VAS pain scores rose significantly for both groups, compared with baseline, but did not significantly differ between the groups, said the investigators (single-port: 4.2 ± 2.4; four-port: 4.2 ± 2.2; P = .83). Cytokine levels and variations in heart rate also were similar between the groups.
However, measures of fatigue on the linear analog self-assessment were better with four-port entry, compared with the single-port approach (3.1 ± 2.1, versus 4.2 ± 2.2, respectively; P = .009), the investigators reported. And 49% of patients in the single-port group reported severe fatigue (a score greater than 5), compared with only 22% of the four-port group (P = .005).
“While this could be due to alpha-error, the fact that the group with the higher fatigue levels (single port) also seemed to be taking more oral narcotic pain medication before discharge … while maintaining similar pain scores in the postoperative period and otherwise having a similar distribution of factors affecting postoperative pain … suggests that the narcotic pain medication may have indeed had an influence on the fatigue scores,” the investigators said.
The National Institutes of Health and the National Center for Advancing Translational Sciences funded the research. The authors declared no conflicts of interest.
Single-port and four-port laparoscopic cholecystectomy were associated with similar self-reported pain scores and physiologic measures of recovery, according to a double-blinded, randomized trial published online in the Journal of the American College of Surgery.
But patients in the four-port arm reported significantly less fatigue (P = .009), and 40% needed postoperative narcotics, compared with 60% of patients who underwent single-port laparoscopy (P = .056), reported Dr. Juliane Bingener and her associates at Mayo Clinic, Rochester, N.Y.
“The data from this study may assist patients and surgeons in the discussion on how to choose a procedure,” said the researchers. “If fast postoperative recovery is the most important goal, four-port cholecystectomy may be more advantageous than single-port laparoscopic cholecystectomy. If cosmesis is the most important factor, single-port entry may be chosen” (J. Am. Coll. Surg. 2015 March 2 [doi:10.1016/j.jamcollsurg.2015.02.022]).
The study comprised 110 patients, of whom half underwent single-port and half underwent four-port laparoscopic cholecystectomy, all performed by the same surgeon. The primary outcome was patient-reported pain 7 days after the procedure, as measured by the visual analog scale (VAS). In all, 81% of patients were female, and median age was 47.5 years, the researchers reported.
Postoperative VAS pain scores rose significantly for both groups, compared with baseline, but did not significantly differ between the groups, said the investigators (single-port: 4.2 ± 2.4; four-port: 4.2 ± 2.2; P = .83). Cytokine levels and variations in heart rate also were similar between the groups.
However, measures of fatigue on the linear analog self-assessment were better with four-port entry, compared with the single-port approach (3.1 ± 2.1, versus 4.2 ± 2.2, respectively; P = .009), the investigators reported. And 49% of patients in the single-port group reported severe fatigue (a score greater than 5), compared with only 22% of the four-port group (P = .005).
“While this could be due to alpha-error, the fact that the group with the higher fatigue levels (single port) also seemed to be taking more oral narcotic pain medication before discharge … while maintaining similar pain scores in the postoperative period and otherwise having a similar distribution of factors affecting postoperative pain … suggests that the narcotic pain medication may have indeed had an influence on the fatigue scores,” the investigators said.
The National Institutes of Health and the National Center for Advancing Translational Sciences funded the research. The authors declared no conflicts of interest.
Single-port and four-port laparoscopic cholecystectomy were associated with similar self-reported pain scores and physiologic measures of recovery, according to a double-blinded, randomized trial published online in the Journal of the American College of Surgery.
But patients in the four-port arm reported significantly less fatigue (P = .009), and 40% needed postoperative narcotics, compared with 60% of patients who underwent single-port laparoscopy (P = .056), reported Dr. Juliane Bingener and her associates at Mayo Clinic, Rochester, N.Y.
“The data from this study may assist patients and surgeons in the discussion on how to choose a procedure,” said the researchers. “If fast postoperative recovery is the most important goal, four-port cholecystectomy may be more advantageous than single-port laparoscopic cholecystectomy. If cosmesis is the most important factor, single-port entry may be chosen” (J. Am. Coll. Surg. 2015 March 2 [doi:10.1016/j.jamcollsurg.2015.02.022]).
The study comprised 110 patients, of whom half underwent single-port and half underwent four-port laparoscopic cholecystectomy, all performed by the same surgeon. The primary outcome was patient-reported pain 7 days after the procedure, as measured by the visual analog scale (VAS). In all, 81% of patients were female, and median age was 47.5 years, the researchers reported.
Postoperative VAS pain scores rose significantly for both groups, compared with baseline, but did not significantly differ between the groups, said the investigators (single-port: 4.2 ± 2.4; four-port: 4.2 ± 2.2; P = .83). Cytokine levels and variations in heart rate also were similar between the groups.
However, measures of fatigue on the linear analog self-assessment were better with four-port entry, compared with the single-port approach (3.1 ± 2.1, versus 4.2 ± 2.2, respectively; P = .009), the investigators reported. And 49% of patients in the single-port group reported severe fatigue (a score greater than 5), compared with only 22% of the four-port group (P = .005).
“While this could be due to alpha-error, the fact that the group with the higher fatigue levels (single port) also seemed to be taking more oral narcotic pain medication before discharge … while maintaining similar pain scores in the postoperative period and otherwise having a similar distribution of factors affecting postoperative pain … suggests that the narcotic pain medication may have indeed had an influence on the fatigue scores,” the investigators said.
The National Institutes of Health and the National Center for Advancing Translational Sciences funded the research. The authors declared no conflicts of interest.
FROM JOURNAL OF THE AMERICAN COLLEGE OF SURGERY
Key clinical point: Four-port laparoscopic cholecystectomy was associated with less fatigue than was single-port laparoscopic cholecystectomy.
Major finding: Seven days after surgery, self-reported fatigue was lower for the four-port entry group compared with the single-port group (P = .009).
Data source: Double-blinded, randomized controlled trial of 110 patients who underwent single-port or four-port laparoscopic cholecystectomy.
Disclosures: The National Institutes of Health and the National Center for Advancing Translational Sciences funded the research. The authors declared no conflicts of interest.
Noisy OR linked to communication gaps, surgical site infections
Noise in the OR has been on the rise for decades, prompting researchers to look into the links between sound levels, health impacts on surgeons, and patient outcomes.
A recent literature review found that noise levels in operating rooms frequently exceed OSHA guidelines for safe work environments. The OSHA recommendation for hospitals in general is 45 time-weighted average decibels (dbA) with a maximum peak of 140 dbA for “impulsive noise” events (Anesthesiology 2014;121:894-8). The sources of noise are many: moving of equipment, clashing metal instruments, pumps, suction apparatus, air warming units, monitors, alarms, nonclinical conversation, and background music. The review found evidence of the impact of noise on communication among staff, concentration of the surgeon, performance of complex tasks by surgeons and anesthesiologists and, potentially, patient outcomes. Noise was found to be greater at the beginning and closing of procedures, and routine peak levels reported were in excess of 100 dBA for various procedures and as high as 131 dBA in some instances.
Another study linked communication gaps in the OR to high noise levels (J. Am. Coll. Surg. 2013:216:933-8). The amount of noise from equipment, staff conversation, and background music was found to have a negative impact on surgeon performance, especially when complex tasks were in process.
Noise pollution during surgery is now being studied in terms of patient outcomes, postop complications, and surgical-site infections (SSIs) in particular.
A pilot study in the United Kingdom looked at noise in the OR as a possible surrogate marker for intraoperative behavior and a potential predictor of SSIs. With a small sample of 35 elective open abdominal procedures, a significant correlation was detected between noise levels and the 30-day postop SSI rate in these patients (Br. J. Surg. 2011;98:1021-5).
Another study has found that high noise levels in the operating room were linked to surgical site infections after outpatient hernia repair (Surgery 2015 Feb. 28 [doi: 10.1016/j.surg.2014.12.026]). “Noise levels were substantially greater in patients with surgical site infections from time point of 50 minutes onwards, which correlated to when wound closure was occurring,” wrote Dr. Shamik Dholakia and his associates at the Milton Keynes General Hospital in Buckinghamshire, England.
The researchers found that music and conversation were the two main contributors to increased noise levels in the OR. “Both of these factors may have distracting influences on the operator and contribute to lower levels of concentration, and so need to be considered as potential issues that could be improved to reduce error,” they said.
Past studies have linked surgical site infections (SSI) with lapses in aseptic technique, which can occur if the OR team is distracted. To assess the role of OR noise in SSI risk, the investigators prospectively studied 64 male, otherwise healthy outpatients who underwent left-side inguinal hernia repair at a single hospital. All patients received a prophylactic dose of 1.2 grams of co-amoxiclav antibiotic, and the same kind of mesh and suture were used for all cases, the investigators said.
The researchers used a decibel meter to measure sound levels in the OR during surgeries, and interviewed patients weekly for the next 30 days to detect SSI.
Five patients (7.8%) developed SSI, all of which were superficial. Swabs from these patients grew mixed skin flora that were sensitive to penicillin, said the researchers.
The mean level for background noise was 47.6 dB before the procedure started. On average, noise levels during procedures for which patients developed SSI were 11.337 dB higher than during other procedures. “Although the actual formula is complex, the accepted rule is that an increase of 10 decibels is perceived to be approximately twice as loud,” the investigators said. “Hence, we believe that this increase in loudness is significant enough to effect the operation. On the basis of our results, we hypothesize that poor concentration caused by high levels of noise may affect one’s ability to perform adequate aseptic closure and increase the probability of developing SSI.”
Surgical assistants usually closed the surgical wounds, which was notable because music’s effects on concentration vary with experience, the researchers noted. “Music may have a soothing, calming, and positive effect on senior experienced operators, whereas it may be distracting and reduce ability to concentrate on junior operators who are not experienced and still learning how to perform the procedure,” they said. “This finding is an important one that the lead surgeon needs to be aware of.”The investigators reported no funding sources or conflicts of interest.
Hospitals are noisy. Noise intensities in operating rooms frequently exceed those found in the hospital’s boiler room.
As pointed out in the accompanying news article, noise in the operating room can be harmful both to the patient and to the health care provider. Evidence is growing of the negative impact on performance and health of nurses, anesthesiologists, and surgeons caused by exposure to the levels of noise commonly experienced in modern operating rooms.
Much of the noise is staff generated. Music and conversations unrelated to clinical care can add close to 90 dBA to the substantial ambient noises produced by air-conditioning systems and monitors. Any attempt at clinically relevant discussion must exceed this background cacophony to be heard.
One big step toward a remedy is simple and inexpensive. All staff should be aware of the harmful effects of excessive noise. Sources of unnecessary noise should be identified and minimized. It has been suggested that a “sterile cockpit” environment (as routinely employed in commercial airplanes) be imposed during critical moments of a surgical procedure. Short of this, educational efforts, such as this brief news report, will go a long way toward cleaning up the noise pollution commonly encountered in our operating rooms.
Dr. Jonathan Katz is clinical professor of anesthesiology, Yale University Medical Center, New Haven, Conn., and attending anesthiologist at St. Vincent Medical Center, Bridgeport, Conn.
Hospitals are noisy. Noise intensities in operating rooms frequently exceed those found in the hospital’s boiler room.
As pointed out in the accompanying news article, noise in the operating room can be harmful both to the patient and to the health care provider. Evidence is growing of the negative impact on performance and health of nurses, anesthesiologists, and surgeons caused by exposure to the levels of noise commonly experienced in modern operating rooms.
Much of the noise is staff generated. Music and conversations unrelated to clinical care can add close to 90 dBA to the substantial ambient noises produced by air-conditioning systems and monitors. Any attempt at clinically relevant discussion must exceed this background cacophony to be heard.
One big step toward a remedy is simple and inexpensive. All staff should be aware of the harmful effects of excessive noise. Sources of unnecessary noise should be identified and minimized. It has been suggested that a “sterile cockpit” environment (as routinely employed in commercial airplanes) be imposed during critical moments of a surgical procedure. Short of this, educational efforts, such as this brief news report, will go a long way toward cleaning up the noise pollution commonly encountered in our operating rooms.
Dr. Jonathan Katz is clinical professor of anesthesiology, Yale University Medical Center, New Haven, Conn., and attending anesthiologist at St. Vincent Medical Center, Bridgeport, Conn.
Hospitals are noisy. Noise intensities in operating rooms frequently exceed those found in the hospital’s boiler room.
As pointed out in the accompanying news article, noise in the operating room can be harmful both to the patient and to the health care provider. Evidence is growing of the negative impact on performance and health of nurses, anesthesiologists, and surgeons caused by exposure to the levels of noise commonly experienced in modern operating rooms.
Much of the noise is staff generated. Music and conversations unrelated to clinical care can add close to 90 dBA to the substantial ambient noises produced by air-conditioning systems and monitors. Any attempt at clinically relevant discussion must exceed this background cacophony to be heard.
One big step toward a remedy is simple and inexpensive. All staff should be aware of the harmful effects of excessive noise. Sources of unnecessary noise should be identified and minimized. It has been suggested that a “sterile cockpit” environment (as routinely employed in commercial airplanes) be imposed during critical moments of a surgical procedure. Short of this, educational efforts, such as this brief news report, will go a long way toward cleaning up the noise pollution commonly encountered in our operating rooms.
Dr. Jonathan Katz is clinical professor of anesthesiology, Yale University Medical Center, New Haven, Conn., and attending anesthiologist at St. Vincent Medical Center, Bridgeport, Conn.
Noise in the OR has been on the rise for decades, prompting researchers to look into the links between sound levels, health impacts on surgeons, and patient outcomes.
A recent literature review found that noise levels in operating rooms frequently exceed OSHA guidelines for safe work environments. The OSHA recommendation for hospitals in general is 45 time-weighted average decibels (dbA) with a maximum peak of 140 dbA for “impulsive noise” events (Anesthesiology 2014;121:894-8). The sources of noise are many: moving of equipment, clashing metal instruments, pumps, suction apparatus, air warming units, monitors, alarms, nonclinical conversation, and background music. The review found evidence of the impact of noise on communication among staff, concentration of the surgeon, performance of complex tasks by surgeons and anesthesiologists and, potentially, patient outcomes. Noise was found to be greater at the beginning and closing of procedures, and routine peak levels reported were in excess of 100 dBA for various procedures and as high as 131 dBA in some instances.
Another study linked communication gaps in the OR to high noise levels (J. Am. Coll. Surg. 2013:216:933-8). The amount of noise from equipment, staff conversation, and background music was found to have a negative impact on surgeon performance, especially when complex tasks were in process.
Noise pollution during surgery is now being studied in terms of patient outcomes, postop complications, and surgical-site infections (SSIs) in particular.
A pilot study in the United Kingdom looked at noise in the OR as a possible surrogate marker for intraoperative behavior and a potential predictor of SSIs. With a small sample of 35 elective open abdominal procedures, a significant correlation was detected between noise levels and the 30-day postop SSI rate in these patients (Br. J. Surg. 2011;98:1021-5).
Another study has found that high noise levels in the operating room were linked to surgical site infections after outpatient hernia repair (Surgery 2015 Feb. 28 [doi: 10.1016/j.surg.2014.12.026]). “Noise levels were substantially greater in patients with surgical site infections from time point of 50 minutes onwards, which correlated to when wound closure was occurring,” wrote Dr. Shamik Dholakia and his associates at the Milton Keynes General Hospital in Buckinghamshire, England.
The researchers found that music and conversation were the two main contributors to increased noise levels in the OR. “Both of these factors may have distracting influences on the operator and contribute to lower levels of concentration, and so need to be considered as potential issues that could be improved to reduce error,” they said.
Past studies have linked surgical site infections (SSI) with lapses in aseptic technique, which can occur if the OR team is distracted. To assess the role of OR noise in SSI risk, the investigators prospectively studied 64 male, otherwise healthy outpatients who underwent left-side inguinal hernia repair at a single hospital. All patients received a prophylactic dose of 1.2 grams of co-amoxiclav antibiotic, and the same kind of mesh and suture were used for all cases, the investigators said.
The researchers used a decibel meter to measure sound levels in the OR during surgeries, and interviewed patients weekly for the next 30 days to detect SSI.
Five patients (7.8%) developed SSI, all of which were superficial. Swabs from these patients grew mixed skin flora that were sensitive to penicillin, said the researchers.
The mean level for background noise was 47.6 dB before the procedure started. On average, noise levels during procedures for which patients developed SSI were 11.337 dB higher than during other procedures. “Although the actual formula is complex, the accepted rule is that an increase of 10 decibels is perceived to be approximately twice as loud,” the investigators said. “Hence, we believe that this increase in loudness is significant enough to effect the operation. On the basis of our results, we hypothesize that poor concentration caused by high levels of noise may affect one’s ability to perform adequate aseptic closure and increase the probability of developing SSI.”
Surgical assistants usually closed the surgical wounds, which was notable because music’s effects on concentration vary with experience, the researchers noted. “Music may have a soothing, calming, and positive effect on senior experienced operators, whereas it may be distracting and reduce ability to concentrate on junior operators who are not experienced and still learning how to perform the procedure,” they said. “This finding is an important one that the lead surgeon needs to be aware of.”The investigators reported no funding sources or conflicts of interest.
Noise in the OR has been on the rise for decades, prompting researchers to look into the links between sound levels, health impacts on surgeons, and patient outcomes.
A recent literature review found that noise levels in operating rooms frequently exceed OSHA guidelines for safe work environments. The OSHA recommendation for hospitals in general is 45 time-weighted average decibels (dbA) with a maximum peak of 140 dbA for “impulsive noise” events (Anesthesiology 2014;121:894-8). The sources of noise are many: moving of equipment, clashing metal instruments, pumps, suction apparatus, air warming units, monitors, alarms, nonclinical conversation, and background music. The review found evidence of the impact of noise on communication among staff, concentration of the surgeon, performance of complex tasks by surgeons and anesthesiologists and, potentially, patient outcomes. Noise was found to be greater at the beginning and closing of procedures, and routine peak levels reported were in excess of 100 dBA for various procedures and as high as 131 dBA in some instances.
Another study linked communication gaps in the OR to high noise levels (J. Am. Coll. Surg. 2013:216:933-8). The amount of noise from equipment, staff conversation, and background music was found to have a negative impact on surgeon performance, especially when complex tasks were in process.
Noise pollution during surgery is now being studied in terms of patient outcomes, postop complications, and surgical-site infections (SSIs) in particular.
A pilot study in the United Kingdom looked at noise in the OR as a possible surrogate marker for intraoperative behavior and a potential predictor of SSIs. With a small sample of 35 elective open abdominal procedures, a significant correlation was detected between noise levels and the 30-day postop SSI rate in these patients (Br. J. Surg. 2011;98:1021-5).
Another study has found that high noise levels in the operating room were linked to surgical site infections after outpatient hernia repair (Surgery 2015 Feb. 28 [doi: 10.1016/j.surg.2014.12.026]). “Noise levels were substantially greater in patients with surgical site infections from time point of 50 minutes onwards, which correlated to when wound closure was occurring,” wrote Dr. Shamik Dholakia and his associates at the Milton Keynes General Hospital in Buckinghamshire, England.
The researchers found that music and conversation were the two main contributors to increased noise levels in the OR. “Both of these factors may have distracting influences on the operator and contribute to lower levels of concentration, and so need to be considered as potential issues that could be improved to reduce error,” they said.
Past studies have linked surgical site infections (SSI) with lapses in aseptic technique, which can occur if the OR team is distracted. To assess the role of OR noise in SSI risk, the investigators prospectively studied 64 male, otherwise healthy outpatients who underwent left-side inguinal hernia repair at a single hospital. All patients received a prophylactic dose of 1.2 grams of co-amoxiclav antibiotic, and the same kind of mesh and suture were used for all cases, the investigators said.
The researchers used a decibel meter to measure sound levels in the OR during surgeries, and interviewed patients weekly for the next 30 days to detect SSI.
Five patients (7.8%) developed SSI, all of which were superficial. Swabs from these patients grew mixed skin flora that were sensitive to penicillin, said the researchers.
The mean level for background noise was 47.6 dB before the procedure started. On average, noise levels during procedures for which patients developed SSI were 11.337 dB higher than during other procedures. “Although the actual formula is complex, the accepted rule is that an increase of 10 decibels is perceived to be approximately twice as loud,” the investigators said. “Hence, we believe that this increase in loudness is significant enough to effect the operation. On the basis of our results, we hypothesize that poor concentration caused by high levels of noise may affect one’s ability to perform adequate aseptic closure and increase the probability of developing SSI.”
Surgical assistants usually closed the surgical wounds, which was notable because music’s effects on concentration vary with experience, the researchers noted. “Music may have a soothing, calming, and positive effect on senior experienced operators, whereas it may be distracting and reduce ability to concentrate on junior operators who are not experienced and still learning how to perform the procedure,” they said. “This finding is an important one that the lead surgeon needs to be aware of.”The investigators reported no funding sources or conflicts of interest.
FROM SURGERY
Key clinical point: Higher noise levels in the operating room correlated with surgical site infections (SSI) after outpatient hernia repair.
Major finding: On average, noise levels during procedures for which patients developed SSI were 11.337 decibels higher than during other procedures.
Data source: Prospective study of 64 young, healthy males who underwent outpatient left-sided hernia repair.
Disclosures: The investigators reported no funding sources or conflicts of interest.
Several factors predict postbariatric surgery readmission
Bariatric surgery is generally safe and readmissions are rare, but prolonged operative time, operation complexity, and major postoperative complications are among several risk factors for readmission identified in a large retrospective cohort.
Of 18,186 patients from the 2012 American College of Surgeons National Surgical Quality Improvement program (ACS NSQIP) database who had bariatric surgery as a primary procedure, 5% were readmitted. Of 815 patients with any major complication, 31% were readmitted. Factors found on multivariate analysis to significantly predict readmission within 30 days were age, sex, body mass index, American Society of Anesthesiology (ASA) risk class, diabetes status, hypertension, and steroid use, Dr. Christa R. Abraham of Albany (N.Y.) Medical College and her colleagues reported online in the Journal of the American College of Surgeons.
Further, all major postoperative complications were significant predictors of readmission, including bleeding requiring transfusion, urinary tract infections, and superficial surgical site infection (SSI). Other significant predictors were deep SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, mechanical ventilation for more than 48 hours, pulmonary embolism, deep vein thrombosis, and sepsis, the investigators said (J. Am. Coll. Surg. 2015 [doi:10.1016/j.jamcollsurg.2015.02.018]).
Of the patients included in the study, 1,819 had a laparoscopic gastric band, 9,613 had laparoscopic Roux-en-Y gastric bypass, 6,439 had gastroplasties, and 315 had open Roux-en-Y gastric bypass. All had a BMI of at least 30 kg/m2, and had a postsurgery length of stay of 14 days or fewer. Most were ASA risk class 3 or lower, and most were functionally independent.
Complications were more common with laparoscopic and open Roux-en-y gastric bypass (5.5% and 11.8%, respectively) rather than with gastroplasty and sleeve (3.4%) and laparoscopic banding (1.4%).
The findings are of value, because while bariatric surgery is a low-risk procedure, and it is extremely common; in 2013 there were 179,000 such surgeries performed in the United States.

“Bariatric surgery is one of the fastest-growing surgical interest areas, making analysis of patient outcomes and reasons for readmission important,” the investigators explained.
The ability to identify high-risk patients could allow for targeted interventions to prevent readmission, they said.
For example, steroid use, which was identified as a risk factor in the current study, is modifiable.
“In our practice, steroids are discontinued for 6 weeks prior to bariatric surgery and patients who are steroid dependent are unlikely to undergo bariatric surgery,” they said.
Additionally, they “try to minimize readmission for patients with infections by treating with antibiotics following operation and continuing antibiotics at discharge.”
The investigators noted that the ACS NSQIP MORBPROB (estimated probability of morbidity) tool is a good tool for predicting readmission among prospective bariatric patients, although it may not fully capture the effect of preexisting conditions.
“These data led us to change our own practice by risk-stratifying patients with higher ASA and BMI to consider surgical options, and to begin early surveillance soon after discharge,” they said.
The authors reported having no disclosures.
Bariatric surgery is generally safe and readmissions are rare, but prolonged operative time, operation complexity, and major postoperative complications are among several risk factors for readmission identified in a large retrospective cohort.
Of 18,186 patients from the 2012 American College of Surgeons National Surgical Quality Improvement program (ACS NSQIP) database who had bariatric surgery as a primary procedure, 5% were readmitted. Of 815 patients with any major complication, 31% were readmitted. Factors found on multivariate analysis to significantly predict readmission within 30 days were age, sex, body mass index, American Society of Anesthesiology (ASA) risk class, diabetes status, hypertension, and steroid use, Dr. Christa R. Abraham of Albany (N.Y.) Medical College and her colleagues reported online in the Journal of the American College of Surgeons.
Further, all major postoperative complications were significant predictors of readmission, including bleeding requiring transfusion, urinary tract infections, and superficial surgical site infection (SSI). Other significant predictors were deep SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, mechanical ventilation for more than 48 hours, pulmonary embolism, deep vein thrombosis, and sepsis, the investigators said (J. Am. Coll. Surg. 2015 [doi:10.1016/j.jamcollsurg.2015.02.018]).
Of the patients included in the study, 1,819 had a laparoscopic gastric band, 9,613 had laparoscopic Roux-en-Y gastric bypass, 6,439 had gastroplasties, and 315 had open Roux-en-Y gastric bypass. All had a BMI of at least 30 kg/m2, and had a postsurgery length of stay of 14 days or fewer. Most were ASA risk class 3 or lower, and most were functionally independent.
Complications were more common with laparoscopic and open Roux-en-y gastric bypass (5.5% and 11.8%, respectively) rather than with gastroplasty and sleeve (3.4%) and laparoscopic banding (1.4%).
The findings are of value, because while bariatric surgery is a low-risk procedure, and it is extremely common; in 2013 there were 179,000 such surgeries performed in the United States.

“Bariatric surgery is one of the fastest-growing surgical interest areas, making analysis of patient outcomes and reasons for readmission important,” the investigators explained.
The ability to identify high-risk patients could allow for targeted interventions to prevent readmission, they said.
For example, steroid use, which was identified as a risk factor in the current study, is modifiable.
“In our practice, steroids are discontinued for 6 weeks prior to bariatric surgery and patients who are steroid dependent are unlikely to undergo bariatric surgery,” they said.
Additionally, they “try to minimize readmission for patients with infections by treating with antibiotics following operation and continuing antibiotics at discharge.”
The investigators noted that the ACS NSQIP MORBPROB (estimated probability of morbidity) tool is a good tool for predicting readmission among prospective bariatric patients, although it may not fully capture the effect of preexisting conditions.
“These data led us to change our own practice by risk-stratifying patients with higher ASA and BMI to consider surgical options, and to begin early surveillance soon after discharge,” they said.
The authors reported having no disclosures.
Bariatric surgery is generally safe and readmissions are rare, but prolonged operative time, operation complexity, and major postoperative complications are among several risk factors for readmission identified in a large retrospective cohort.
Of 18,186 patients from the 2012 American College of Surgeons National Surgical Quality Improvement program (ACS NSQIP) database who had bariatric surgery as a primary procedure, 5% were readmitted. Of 815 patients with any major complication, 31% were readmitted. Factors found on multivariate analysis to significantly predict readmission within 30 days were age, sex, body mass index, American Society of Anesthesiology (ASA) risk class, diabetes status, hypertension, and steroid use, Dr. Christa R. Abraham of Albany (N.Y.) Medical College and her colleagues reported online in the Journal of the American College of Surgeons.
Further, all major postoperative complications were significant predictors of readmission, including bleeding requiring transfusion, urinary tract infections, and superficial surgical site infection (SSI). Other significant predictors were deep SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, mechanical ventilation for more than 48 hours, pulmonary embolism, deep vein thrombosis, and sepsis, the investigators said (J. Am. Coll. Surg. 2015 [doi:10.1016/j.jamcollsurg.2015.02.018]).
Of the patients included in the study, 1,819 had a laparoscopic gastric band, 9,613 had laparoscopic Roux-en-Y gastric bypass, 6,439 had gastroplasties, and 315 had open Roux-en-Y gastric bypass. All had a BMI of at least 30 kg/m2, and had a postsurgery length of stay of 14 days or fewer. Most were ASA risk class 3 or lower, and most were functionally independent.
Complications were more common with laparoscopic and open Roux-en-y gastric bypass (5.5% and 11.8%, respectively) rather than with gastroplasty and sleeve (3.4%) and laparoscopic banding (1.4%).
The findings are of value, because while bariatric surgery is a low-risk procedure, and it is extremely common; in 2013 there were 179,000 such surgeries performed in the United States.

“Bariatric surgery is one of the fastest-growing surgical interest areas, making analysis of patient outcomes and reasons for readmission important,” the investigators explained.
The ability to identify high-risk patients could allow for targeted interventions to prevent readmission, they said.
For example, steroid use, which was identified as a risk factor in the current study, is modifiable.
“In our practice, steroids are discontinued for 6 weeks prior to bariatric surgery and patients who are steroid dependent are unlikely to undergo bariatric surgery,” they said.
Additionally, they “try to minimize readmission for patients with infections by treating with antibiotics following operation and continuing antibiotics at discharge.”
The investigators noted that the ACS NSQIP MORBPROB (estimated probability of morbidity) tool is a good tool for predicting readmission among prospective bariatric patients, although it may not fully capture the effect of preexisting conditions.
“These data led us to change our own practice by risk-stratifying patients with higher ASA and BMI to consider surgical options, and to begin early surveillance soon after discharge,” they said.
The authors reported having no disclosures.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Knowing risk factors for readmission after bariatric surgery can allow for targeted interventions.
Major finding: Steroid use is among several risk factors for readmission following bariatric surgery (incidence rate ratio, 2.07)
Data source: A retrospective cohort study involving 18,186 patients.
Disclosures: The authors reported having no disclosures.
Cost comparison favors minimally invasive over conventional AVR
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Mortality, stroke, renal failure, and other complications were not significantly different between mini-aortic valve replacement and conventional replacement.
Major finding: Total hospital costs were significantly lower with mini-AVR, compared with conventional replacement ($36,348 vs. $38,239).
Data source: A retrospective data analysis of patient records for isolated AVR repair, extracted from a regional, multi-institutional Society of Thoracic Surgeons database.
Disclosures: The authors reported that they had no relevant conflicts of interest.
Halting biologics before surgery tied to flares in psoriasis, psoriatic arthritis
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis.
Major finding: Discontinuing biologic therapy before surgery was associated with a significant risk of flare (40% with stoppage vs. 8.7% with continuation; P = .003).
Data source: A retrospective cohort study of 42 patients with psoriasis and/or psoriatic arthritis who underwent 77 surgical procedures.
Disclosures: The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Heparin, warfarin tied to similar VTE rates after radical cystectomy
Venous thromboembolisms affected 6.4% of patients who underwent radical cystectomy, even though all patients received heparin in the hospital as recommended by the American Urological Association, researchers reported.
“Using an in-house, heparin-based anticoagulation protocol consistent with current AUA guidelines has not decreased the rate of venous thromboembolism compared to historical warfarin use,” wrote Dr. Andrew Sun and his colleagues at the University of Southern California Institute of Urology in Los Angeles. Most episodes of VTE occurred after patients were discharged home, and “future studies are needed to establish the benefits of extended-duration [VTE] prophylaxis regimens that cover the critical posthospitalization period,” the researchers added (J. UroL 2015;193:565-9).
Previous studies have reported venous thromboembolism rates of 3%-6% in cystectomy patients, a rate that is more than double that reported for nephrectomy or prostatectomy patients. For their study, the investigators retrospectively assessed 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection for urothelial bladder cancer between 1971 and 2012. Symptomatic VTE developed among 109 patients overall (4.7%), compared with 6.4% of those who received the modern, heparin-based protocol implemented in 2009 (P = .089).
Furthermore, 58% of all cases occurred after patients stopped anticoagulation therapy and were discharged home. The median time of onset was 20 days after surgery (range, 2-91 days), and VTE was significantly more common among patients with a higher body mass index, prolonged hospital stays, positive surgical margins and orthotopic diversion procedures, compared with other patients. Surgical techniques remained consistent throughout the study.
The study was retrospective, and thus “could not prove any cause and effect relationships. This underscores the need for additional prospective data in this area of research,” said the investigators. “We focused only on open radical cystectomy, and thus, findings may not be generalizable to minimally invasive modalities, on which there is even a greater paucity of data.”
Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
Venous thromboembolisms affected 6.4% of patients who underwent radical cystectomy, even though all patients received heparin in the hospital as recommended by the American Urological Association, researchers reported.
“Using an in-house, heparin-based anticoagulation protocol consistent with current AUA guidelines has not decreased the rate of venous thromboembolism compared to historical warfarin use,” wrote Dr. Andrew Sun and his colleagues at the University of Southern California Institute of Urology in Los Angeles. Most episodes of VTE occurred after patients were discharged home, and “future studies are needed to establish the benefits of extended-duration [VTE] prophylaxis regimens that cover the critical posthospitalization period,” the researchers added (J. UroL 2015;193:565-9).
Previous studies have reported venous thromboembolism rates of 3%-6% in cystectomy patients, a rate that is more than double that reported for nephrectomy or prostatectomy patients. For their study, the investigators retrospectively assessed 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection for urothelial bladder cancer between 1971 and 2012. Symptomatic VTE developed among 109 patients overall (4.7%), compared with 6.4% of those who received the modern, heparin-based protocol implemented in 2009 (P = .089).
Furthermore, 58% of all cases occurred after patients stopped anticoagulation therapy and were discharged home. The median time of onset was 20 days after surgery (range, 2-91 days), and VTE was significantly more common among patients with a higher body mass index, prolonged hospital stays, positive surgical margins and orthotopic diversion procedures, compared with other patients. Surgical techniques remained consistent throughout the study.
The study was retrospective, and thus “could not prove any cause and effect relationships. This underscores the need for additional prospective data in this area of research,” said the investigators. “We focused only on open radical cystectomy, and thus, findings may not be generalizable to minimally invasive modalities, on which there is even a greater paucity of data.”
Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
Venous thromboembolisms affected 6.4% of patients who underwent radical cystectomy, even though all patients received heparin in the hospital as recommended by the American Urological Association, researchers reported.
“Using an in-house, heparin-based anticoagulation protocol consistent with current AUA guidelines has not decreased the rate of venous thromboembolism compared to historical warfarin use,” wrote Dr. Andrew Sun and his colleagues at the University of Southern California Institute of Urology in Los Angeles. Most episodes of VTE occurred after patients were discharged home, and “future studies are needed to establish the benefits of extended-duration [VTE] prophylaxis regimens that cover the critical posthospitalization period,” the researchers added (J. UroL 2015;193:565-9).
Previous studies have reported venous thromboembolism rates of 3%-6% in cystectomy patients, a rate that is more than double that reported for nephrectomy or prostatectomy patients. For their study, the investigators retrospectively assessed 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection for urothelial bladder cancer between 1971 and 2012. Symptomatic VTE developed among 109 patients overall (4.7%), compared with 6.4% of those who received the modern, heparin-based protocol implemented in 2009 (P = .089).
Furthermore, 58% of all cases occurred after patients stopped anticoagulation therapy and were discharged home. The median time of onset was 20 days after surgery (range, 2-91 days), and VTE was significantly more common among patients with a higher body mass index, prolonged hospital stays, positive surgical margins and orthotopic diversion procedures, compared with other patients. Surgical techniques remained consistent throughout the study.
The study was retrospective, and thus “could not prove any cause and effect relationships. This underscores the need for additional prospective data in this area of research,” said the investigators. “We focused only on open radical cystectomy, and thus, findings may not be generalizable to minimally invasive modalities, on which there is even a greater paucity of data.”
Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
FROM THE JOURNAL OF UROLOGY
Key clinical point: Heparin and warfarin were linked to similar rates of postcystectomy venous thromboembolism.
Major finding: Symptomatic VTE affected 4.7% of patients in the overall cohort, compared with 6.4% of those treated with the modern, heparin-based protocol (P = .089).
Data source: A single-center retrospective cohort study of 2,316 patients who underwent open radical cystectomy and extended pelvic lymph node dissection.
Disclosures: Senior author Dr. Siamak Daneshmand reported financial or other relationships with Endo and Cubist. The authors reported no funding sources or other relevant conflicts of interest.
Fast-track protocol cuts lung resection complications, LOS
CHICAGO – An enhanced recovery pathway reduces short-term complications and hospital stays following cancer-related lung resection without raising readmissions or emergency visits after discharge, a study showed.
“A multimodal pathway for open, elective lobectomy seems to improve efficiency and quality of care,” Dr. Amin Madani, from McGill University in Montreal, said at the annual meeting of the Central Surgical Association (CSA).
Prior research suggests that an enhanced recovery pathway (ERP), also known as fast-track protocols, can improve surgical outcomes, but there is little evidence to support its use and effectiveness in lung resection.
Surgeons at McGill established an integrated, multimodal approach to perioperative care of these patients after creating a written, evidence-based, step-by-step pathway. Key elements are standardized preoperative patient education; removal of urine drains on postoperative day 1; removal of the last chest tube by postop (POD) day 3, if there is <300 cc of drainage in 24 hours and no air leak; ambulation goals of more than 75 m thrice-daily by POD 3; introduction of solid food on POD 1; and a target discharge of POD 4; Dr. Madani explained.
To examine the effectiveness of the pathway, the authors retrospectively analyzed outcomes in 127 patients undergoing elective lung resection for primary or secondary lung cancer receiving traditional care and 107 patients treated after the ERP was implemented in September 2012. At baseline, the two groups were similar with respect to age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) scores, pulmonary function, and smoking history.
Hospital length of stay was significantly reduced after the ERP from a median of 7 days with traditional care to 6 days (P < .01), driven largely by patients with an uncomplicated hospital course who were discharged after a median of 5 days after the pathway was implemented, Dr. Madani said.
It was not the case that patients went home too early, as readmissions (5% vs. 6%) and ED visits (3% vs. 5%) were similar between both groups, he added.
After the pathway was implemented, patients had earlier Foley catheter removal (POD 2 vs. 1), IV discontinuation (POD 3 vs. 2), ambulation (POD 2 vs. 1), last chest tube removal (POD 5 vs. 4), and epidural removal (POD 5 vs. 4).
The enhanced recovery pathway group had fewer overall complications than did the traditional care group (37% vs. 50%; P = .03), a threefold decrease in urinary tract infections (3% vs. 12%; P < .01), and a trend toward fewer pulmonary complications (25% vs. 31%; P = .38) and surgical site infections (1% vs. 6%; P = .07), he said.
Despite significantly earlier removal of chest tubes after the pathway, there was no difference in the incidence of pneumothorax or pleural effusion requiring tube re-insertion, affirming that “Chest tubes were not being removed too early, causing harm to patients,” Dr. Madani said.
In multivariate regression analysis adjusted for age, sex, BMI, and ASA score, there was a significant negative association between implementation of an enhanced recovery pathway and length of stay (beta, –0.18; P < .01) and complications (odds ratio, 0.46; P < .01), but not readmissions (OR, 1.59; P = .44).
Early removal of chest tubes and urinary catheter were independent predictors of decreased length of stay.
Dr. L. Michael Brunt, a discussant from Washington University in St. Louis, said the development of care pathways to enhance recovery after surgery is gaining a lot of interest in the surgical community, but went on to ask how much it cost to implement.
The overall cost of the surgeon-driven initiative, involving multiple pathways for various surgical procedures, is about $120,000 annually, or $100/patient for the 1,200 patients undergoing surgery using an ERP program at the McGill University Health Centre each year, Dr. Madani said. This cost also includes a full-time nurse practitioner now serving as the pathway coordinator and roughly $13,000 for patient education booklets, but no additional staff.
An audience member questioned whether the authors have identified factors predicting which patients would fail to meet pathway goals, observing that in the colorectal field, there are patients such as the 80-year-old, narcotic-naive woman with diabetes, who simply won’t progress.
“That’s a very good point, and I agree there are some patients whom you can’t fast track,” Dr. Madani replied. “Part of the deal here is that, yes, we have this protocolized pathway; however, the surgeon still has the right to change that if they feel it is important. We didn’t look at the specifics of which patient [factors] achieved adherence, but we could at some point in the future.”
CSA president and session moderator Christopher McHenry, from MetroHealth Medical Center in Cleveland, said he was impressed with the study and called the findings very believable.
“I think all of these recovery pathways can be very beneficial,” Dr. McHenry said in an interview. “It helps us re-look at how we’re managing our patients and see if there are ways that we can improve on their postoperative management that may lead to earlier discharge.”
The study was funded by an investigator-initiated research grant from Ethicon Canada. Dr. Madani, his coauthors, Dr. Brunt, and Dr. McHenry reported having no financial conflicts.
CHICAGO – An enhanced recovery pathway reduces short-term complications and hospital stays following cancer-related lung resection without raising readmissions or emergency visits after discharge, a study showed.
“A multimodal pathway for open, elective lobectomy seems to improve efficiency and quality of care,” Dr. Amin Madani, from McGill University in Montreal, said at the annual meeting of the Central Surgical Association (CSA).
Prior research suggests that an enhanced recovery pathway (ERP), also known as fast-track protocols, can improve surgical outcomes, but there is little evidence to support its use and effectiveness in lung resection.
Surgeons at McGill established an integrated, multimodal approach to perioperative care of these patients after creating a written, evidence-based, step-by-step pathway. Key elements are standardized preoperative patient education; removal of urine drains on postoperative day 1; removal of the last chest tube by postop (POD) day 3, if there is <300 cc of drainage in 24 hours and no air leak; ambulation goals of more than 75 m thrice-daily by POD 3; introduction of solid food on POD 1; and a target discharge of POD 4; Dr. Madani explained.
To examine the effectiveness of the pathway, the authors retrospectively analyzed outcomes in 127 patients undergoing elective lung resection for primary or secondary lung cancer receiving traditional care and 107 patients treated after the ERP was implemented in September 2012. At baseline, the two groups were similar with respect to age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) scores, pulmonary function, and smoking history.
Hospital length of stay was significantly reduced after the ERP from a median of 7 days with traditional care to 6 days (P < .01), driven largely by patients with an uncomplicated hospital course who were discharged after a median of 5 days after the pathway was implemented, Dr. Madani said.
It was not the case that patients went home too early, as readmissions (5% vs. 6%) and ED visits (3% vs. 5%) were similar between both groups, he added.
After the pathway was implemented, patients had earlier Foley catheter removal (POD 2 vs. 1), IV discontinuation (POD 3 vs. 2), ambulation (POD 2 vs. 1), last chest tube removal (POD 5 vs. 4), and epidural removal (POD 5 vs. 4).
The enhanced recovery pathway group had fewer overall complications than did the traditional care group (37% vs. 50%; P = .03), a threefold decrease in urinary tract infections (3% vs. 12%; P < .01), and a trend toward fewer pulmonary complications (25% vs. 31%; P = .38) and surgical site infections (1% vs. 6%; P = .07), he said.
Despite significantly earlier removal of chest tubes after the pathway, there was no difference in the incidence of pneumothorax or pleural effusion requiring tube re-insertion, affirming that “Chest tubes were not being removed too early, causing harm to patients,” Dr. Madani said.
In multivariate regression analysis adjusted for age, sex, BMI, and ASA score, there was a significant negative association between implementation of an enhanced recovery pathway and length of stay (beta, –0.18; P < .01) and complications (odds ratio, 0.46; P < .01), but not readmissions (OR, 1.59; P = .44).
Early removal of chest tubes and urinary catheter were independent predictors of decreased length of stay.
Dr. L. Michael Brunt, a discussant from Washington University in St. Louis, said the development of care pathways to enhance recovery after surgery is gaining a lot of interest in the surgical community, but went on to ask how much it cost to implement.
The overall cost of the surgeon-driven initiative, involving multiple pathways for various surgical procedures, is about $120,000 annually, or $100/patient for the 1,200 patients undergoing surgery using an ERP program at the McGill University Health Centre each year, Dr. Madani said. This cost also includes a full-time nurse practitioner now serving as the pathway coordinator and roughly $13,000 for patient education booklets, but no additional staff.
An audience member questioned whether the authors have identified factors predicting which patients would fail to meet pathway goals, observing that in the colorectal field, there are patients such as the 80-year-old, narcotic-naive woman with diabetes, who simply won’t progress.
“That’s a very good point, and I agree there are some patients whom you can’t fast track,” Dr. Madani replied. “Part of the deal here is that, yes, we have this protocolized pathway; however, the surgeon still has the right to change that if they feel it is important. We didn’t look at the specifics of which patient [factors] achieved adherence, but we could at some point in the future.”
CSA president and session moderator Christopher McHenry, from MetroHealth Medical Center in Cleveland, said he was impressed with the study and called the findings very believable.
“I think all of these recovery pathways can be very beneficial,” Dr. McHenry said in an interview. “It helps us re-look at how we’re managing our patients and see if there are ways that we can improve on their postoperative management that may lead to earlier discharge.”
The study was funded by an investigator-initiated research grant from Ethicon Canada. Dr. Madani, his coauthors, Dr. Brunt, and Dr. McHenry reported having no financial conflicts.
CHICAGO – An enhanced recovery pathway reduces short-term complications and hospital stays following cancer-related lung resection without raising readmissions or emergency visits after discharge, a study showed.
“A multimodal pathway for open, elective lobectomy seems to improve efficiency and quality of care,” Dr. Amin Madani, from McGill University in Montreal, said at the annual meeting of the Central Surgical Association (CSA).
Prior research suggests that an enhanced recovery pathway (ERP), also known as fast-track protocols, can improve surgical outcomes, but there is little evidence to support its use and effectiveness in lung resection.
Surgeons at McGill established an integrated, multimodal approach to perioperative care of these patients after creating a written, evidence-based, step-by-step pathway. Key elements are standardized preoperative patient education; removal of urine drains on postoperative day 1; removal of the last chest tube by postop (POD) day 3, if there is <300 cc of drainage in 24 hours and no air leak; ambulation goals of more than 75 m thrice-daily by POD 3; introduction of solid food on POD 1; and a target discharge of POD 4; Dr. Madani explained.
To examine the effectiveness of the pathway, the authors retrospectively analyzed outcomes in 127 patients undergoing elective lung resection for primary or secondary lung cancer receiving traditional care and 107 patients treated after the ERP was implemented in September 2012. At baseline, the two groups were similar with respect to age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) scores, pulmonary function, and smoking history.
Hospital length of stay was significantly reduced after the ERP from a median of 7 days with traditional care to 6 days (P < .01), driven largely by patients with an uncomplicated hospital course who were discharged after a median of 5 days after the pathway was implemented, Dr. Madani said.
It was not the case that patients went home too early, as readmissions (5% vs. 6%) and ED visits (3% vs. 5%) were similar between both groups, he added.
After the pathway was implemented, patients had earlier Foley catheter removal (POD 2 vs. 1), IV discontinuation (POD 3 vs. 2), ambulation (POD 2 vs. 1), last chest tube removal (POD 5 vs. 4), and epidural removal (POD 5 vs. 4).
The enhanced recovery pathway group had fewer overall complications than did the traditional care group (37% vs. 50%; P = .03), a threefold decrease in urinary tract infections (3% vs. 12%; P < .01), and a trend toward fewer pulmonary complications (25% vs. 31%; P = .38) and surgical site infections (1% vs. 6%; P = .07), he said.
Despite significantly earlier removal of chest tubes after the pathway, there was no difference in the incidence of pneumothorax or pleural effusion requiring tube re-insertion, affirming that “Chest tubes were not being removed too early, causing harm to patients,” Dr. Madani said.
In multivariate regression analysis adjusted for age, sex, BMI, and ASA score, there was a significant negative association between implementation of an enhanced recovery pathway and length of stay (beta, –0.18; P < .01) and complications (odds ratio, 0.46; P < .01), but not readmissions (OR, 1.59; P = .44).
Early removal of chest tubes and urinary catheter were independent predictors of decreased length of stay.
Dr. L. Michael Brunt, a discussant from Washington University in St. Louis, said the development of care pathways to enhance recovery after surgery is gaining a lot of interest in the surgical community, but went on to ask how much it cost to implement.
The overall cost of the surgeon-driven initiative, involving multiple pathways for various surgical procedures, is about $120,000 annually, or $100/patient for the 1,200 patients undergoing surgery using an ERP program at the McGill University Health Centre each year, Dr. Madani said. This cost also includes a full-time nurse practitioner now serving as the pathway coordinator and roughly $13,000 for patient education booklets, but no additional staff.
An audience member questioned whether the authors have identified factors predicting which patients would fail to meet pathway goals, observing that in the colorectal field, there are patients such as the 80-year-old, narcotic-naive woman with diabetes, who simply won’t progress.
“That’s a very good point, and I agree there are some patients whom you can’t fast track,” Dr. Madani replied. “Part of the deal here is that, yes, we have this protocolized pathway; however, the surgeon still has the right to change that if they feel it is important. We didn’t look at the specifics of which patient [factors] achieved adherence, but we could at some point in the future.”
CSA president and session moderator Christopher McHenry, from MetroHealth Medical Center in Cleveland, said he was impressed with the study and called the findings very believable.
“I think all of these recovery pathways can be very beneficial,” Dr. McHenry said in an interview. “It helps us re-look at how we’re managing our patients and see if there are ways that we can improve on their postoperative management that may lead to earlier discharge.”
The study was funded by an investigator-initiated research grant from Ethicon Canada. Dr. Madani, his coauthors, Dr. Brunt, and Dr. McHenry reported having no financial conflicts.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: An enhanced recovery pathway reduces complications and hospital stay following lung cancer resection without raising readmissions or ED visits.
Major finding: Patients in the enhanced recovery pathway vs. traditional care had fewer overall complications (37% vs. 50%; P = .03) and threefold fewer UTIs (3% vs. 12%; P < .01).
Data source: Observational study of 234 patients undergoing lung resection.
Disclosures: The study was funded by an investigator-initiated research grant from Ethicon Canada. Dr. Madani, his coauthors, Dr. Brunt, and Dr. McHenry reported having no financial conflicts.
Ranolazine plus beta-blockers might prevent postop AF
PHOENIX – Twice-daily ranolazine following adult cardiac surgery seemed to protect against atrial fibrillation, based on a retrospective cohort study at the University of Florida Jacksonville Medical Center.
Ranolazine (Ranexa) was dosed orally at 1,000 mg the morning of surgery, and then resumed after extubation, generally the night of surgery. The goal was 1,000 mg orally twice a day, for a maximum of 7 hospital days; patients usually went home before then, so they received an average of nine doses. The drug was discontinued at discharge.
Six (10.5%) of 57 patients in the ranolazine group developed postoperative atrial fibrillation (POAF) versus 26 (45.6%) of 57 matched controls (P < .0001). The first case came at postop day 3 in the ranolazine group, but within 24 hours in the control group. One person in the ranolazine group and one in the control group had a history of AF.
There was no statistical difference in ICU length of stay, 30-day readmission for cardiac causes, or 30-day cardiovascular mortality; the one cardiovascular death was in the control group.
Two-thirds of the patients had coronary artery bypass grafts, and the rest had either valve surgery or a combination of both surgeries. Patients were 60 years old on average, and two-thirds were men, Drayton Hammond, Pharm.D., said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Ranolazine is indicated for chronic angina, not POAF prevention, but some previous investigations have suggested a possible benefit. A randomized, controlled clinical trial is currently looking into the matter.
At least retrospectively, the drug was “beneficial, definitely. There is about a 35% absolute-risk reduction,” said Dr. Hammond, who conducted the study while at the Jacksonville hospital.
Doctors there continue to use ranolazine for postop AF prophylaxis, as they see fit, said Dr. Hammond, now an assistant professor of pharmacy practice at the University of Arkansas for Medical Sciences, in Little Rock.
Gilead, the maker of the Ranexa, is also working on a ranolazine-dronedarone combination for paroxysmal AF.
More than half of the ranolazine patients in the study developed symptomatic hypotension within 72 hours of surgery, versus about a third in the control group (P = .0004). The drug was discontinued in one ranolazine patient because of hypotension. The problem resolved after 72 hours.
“We don’t have a good explanation” for the side effect. Perhaps there were differences in myocardial stunning or vasopressor use between the groups, but “we had the same three surgeons” for all the cases, Dr. Hammond said.
Ranolazine labeling notes the risk of hypotension and orthostatic hypotension. Labeling also warns of QT interval prolongation and renal failure in susceptible patients. The investigators found no between-group differences in bradycardia, new renal failure, or neurological events.
Overall, 53 (93%) patients in the ranolazine group were on postoperative beta-blockers, and 54 (94.7%) on postop statins; 48 (84.2%) in the control group were on beta-blockers postop and 47 (82.5%) on statins. Beta-blockers are first-line treatment to prevent postop AF; patients on any other antiarrhythmic were excluded from the trial, as were those who died during surgery.
PHOENIX – Twice-daily ranolazine following adult cardiac surgery seemed to protect against atrial fibrillation, based on a retrospective cohort study at the University of Florida Jacksonville Medical Center.
Ranolazine (Ranexa) was dosed orally at 1,000 mg the morning of surgery, and then resumed after extubation, generally the night of surgery. The goal was 1,000 mg orally twice a day, for a maximum of 7 hospital days; patients usually went home before then, so they received an average of nine doses. The drug was discontinued at discharge.
Six (10.5%) of 57 patients in the ranolazine group developed postoperative atrial fibrillation (POAF) versus 26 (45.6%) of 57 matched controls (P < .0001). The first case came at postop day 3 in the ranolazine group, but within 24 hours in the control group. One person in the ranolazine group and one in the control group had a history of AF.
There was no statistical difference in ICU length of stay, 30-day readmission for cardiac causes, or 30-day cardiovascular mortality; the one cardiovascular death was in the control group.
Two-thirds of the patients had coronary artery bypass grafts, and the rest had either valve surgery or a combination of both surgeries. Patients were 60 years old on average, and two-thirds were men, Drayton Hammond, Pharm.D., said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Ranolazine is indicated for chronic angina, not POAF prevention, but some previous investigations have suggested a possible benefit. A randomized, controlled clinical trial is currently looking into the matter.
At least retrospectively, the drug was “beneficial, definitely. There is about a 35% absolute-risk reduction,” said Dr. Hammond, who conducted the study while at the Jacksonville hospital.
Doctors there continue to use ranolazine for postop AF prophylaxis, as they see fit, said Dr. Hammond, now an assistant professor of pharmacy practice at the University of Arkansas for Medical Sciences, in Little Rock.
Gilead, the maker of the Ranexa, is also working on a ranolazine-dronedarone combination for paroxysmal AF.
More than half of the ranolazine patients in the study developed symptomatic hypotension within 72 hours of surgery, versus about a third in the control group (P = .0004). The drug was discontinued in one ranolazine patient because of hypotension. The problem resolved after 72 hours.
“We don’t have a good explanation” for the side effect. Perhaps there were differences in myocardial stunning or vasopressor use between the groups, but “we had the same three surgeons” for all the cases, Dr. Hammond said.
Ranolazine labeling notes the risk of hypotension and orthostatic hypotension. Labeling also warns of QT interval prolongation and renal failure in susceptible patients. The investigators found no between-group differences in bradycardia, new renal failure, or neurological events.
Overall, 53 (93%) patients in the ranolazine group were on postoperative beta-blockers, and 54 (94.7%) on postop statins; 48 (84.2%) in the control group were on beta-blockers postop and 47 (82.5%) on statins. Beta-blockers are first-line treatment to prevent postop AF; patients on any other antiarrhythmic were excluded from the trial, as were those who died during surgery.
PHOENIX – Twice-daily ranolazine following adult cardiac surgery seemed to protect against atrial fibrillation, based on a retrospective cohort study at the University of Florida Jacksonville Medical Center.
Ranolazine (Ranexa) was dosed orally at 1,000 mg the morning of surgery, and then resumed after extubation, generally the night of surgery. The goal was 1,000 mg orally twice a day, for a maximum of 7 hospital days; patients usually went home before then, so they received an average of nine doses. The drug was discontinued at discharge.
Six (10.5%) of 57 patients in the ranolazine group developed postoperative atrial fibrillation (POAF) versus 26 (45.6%) of 57 matched controls (P < .0001). The first case came at postop day 3 in the ranolazine group, but within 24 hours in the control group. One person in the ranolazine group and one in the control group had a history of AF.
There was no statistical difference in ICU length of stay, 30-day readmission for cardiac causes, or 30-day cardiovascular mortality; the one cardiovascular death was in the control group.
Two-thirds of the patients had coronary artery bypass grafts, and the rest had either valve surgery or a combination of both surgeries. Patients were 60 years old on average, and two-thirds were men, Drayton Hammond, Pharm.D., said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Ranolazine is indicated for chronic angina, not POAF prevention, but some previous investigations have suggested a possible benefit. A randomized, controlled clinical trial is currently looking into the matter.
At least retrospectively, the drug was “beneficial, definitely. There is about a 35% absolute-risk reduction,” said Dr. Hammond, who conducted the study while at the Jacksonville hospital.
Doctors there continue to use ranolazine for postop AF prophylaxis, as they see fit, said Dr. Hammond, now an assistant professor of pharmacy practice at the University of Arkansas for Medical Sciences, in Little Rock.
Gilead, the maker of the Ranexa, is also working on a ranolazine-dronedarone combination for paroxysmal AF.
More than half of the ranolazine patients in the study developed symptomatic hypotension within 72 hours of surgery, versus about a third in the control group (P = .0004). The drug was discontinued in one ranolazine patient because of hypotension. The problem resolved after 72 hours.
“We don’t have a good explanation” for the side effect. Perhaps there were differences in myocardial stunning or vasopressor use between the groups, but “we had the same three surgeons” for all the cases, Dr. Hammond said.
Ranolazine labeling notes the risk of hypotension and orthostatic hypotension. Labeling also warns of QT interval prolongation and renal failure in susceptible patients. The investigators found no between-group differences in bradycardia, new renal failure, or neurological events.
Overall, 53 (93%) patients in the ranolazine group were on postoperative beta-blockers, and 54 (94.7%) on postop statins; 48 (84.2%) in the control group were on beta-blockers postop and 47 (82.5%) on statins. Beta-blockers are first-line treatment to prevent postop AF; patients on any other antiarrhythmic were excluded from the trial, as were those who died during surgery.
AT THE CRITICAL CARE CONGRESS
Key clinical point: Ranolazine’s protective effect seems to come at the cost of symptomatic hypotension in the first 3 days after surgery.
Major finding: Postop atrial fibrillation occurred in 6 (10.5%) of 57 patients in the ranolazine group and 26 (45.6%) of 57 matched controls (P < .0001).
Data source: Retrospective cohort study of postop follow-up in 114 adults who had cardiac surgery.
Disclosures: There was no outside funding for the work. The investigators said they have no financial relationship with Gilead, maker of ranolazine (Ranexa).