User login
Study identifies SSI risk factors after open LEB
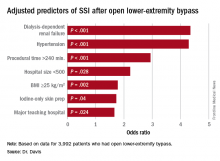
COLUMBUS, OHIO – A study of vascular procedures at 35 Michigan hospitals has identified three risk factors for surgical site infection after lower-extremity bypass that hospitals and vascular surgery teams may be able to modify.
“Patients who had iodine-only skin antiseptic preparation, a high-peak intraoperative glucose, or long operative times were more likely to have substantially increased risk for surgical site infection (SSI),” Frank Davis, MD, of the University of Michigan said in reporting the study results at the annual meeting of the Midwestern Vascular Surgical Society. Those risk factors are modifiable, Dr. Davis said.
“Specific attention needs to be served moving forward in attempts to decrease the risk of SSI for lower-extremity bypass,” Dr. Davis said. “The incidence of SSI in our cohort across the state of Michigan was approximately 9.2%, and for those who did develop a SSI, there was a substantial increase in 30-day morbidity.”
Patients who had an SSI were more than three times more likely to have a major amputation (9% vs. 2.3%) than those without, and more than five times more likely to have a reoperation (3.9% vs. 0.7%), Dr. Davis said.
“With regard to preoperative symptomatology, those with lower peripheral artery questionnaire scores, resting pain, or acute ischemia were more likely to develop SSI postoperatively,” Dr. Davis said. “Patients who underwent an interim coronal bypass had a significant increase of SSI in comparison to all other bypass configurations.”
He also noted that major teaching hospitals or hospitals with 500 or fewer beds had higher rates of SSI.
“Targeted improvements in preoperative care may decrease complications and improve vascular patient outcomes,” Dr. Davis said.
Dr. Davis had no relationships to disclose.
COLUMBUS, OHIO – A study of vascular procedures at 35 Michigan hospitals has identified three risk factors for surgical site infection after lower-extremity bypass that hospitals and vascular surgery teams may be able to modify.
“Patients who had iodine-only skin antiseptic preparation, a high-peak intraoperative glucose, or long operative times were more likely to have substantially increased risk for surgical site infection (SSI),” Frank Davis, MD, of the University of Michigan said in reporting the study results at the annual meeting of the Midwestern Vascular Surgical Society. Those risk factors are modifiable, Dr. Davis said.
“Specific attention needs to be served moving forward in attempts to decrease the risk of SSI for lower-extremity bypass,” Dr. Davis said. “The incidence of SSI in our cohort across the state of Michigan was approximately 9.2%, and for those who did develop a SSI, there was a substantial increase in 30-day morbidity.”
Patients who had an SSI were more than three times more likely to have a major amputation (9% vs. 2.3%) than those without, and more than five times more likely to have a reoperation (3.9% vs. 0.7%), Dr. Davis said.
“With regard to preoperative symptomatology, those with lower peripheral artery questionnaire scores, resting pain, or acute ischemia were more likely to develop SSI postoperatively,” Dr. Davis said. “Patients who underwent an interim coronal bypass had a significant increase of SSI in comparison to all other bypass configurations.”
He also noted that major teaching hospitals or hospitals with 500 or fewer beds had higher rates of SSI.
“Targeted improvements in preoperative care may decrease complications and improve vascular patient outcomes,” Dr. Davis said.
Dr. Davis had no relationships to disclose.
COLUMBUS, OHIO – A study of vascular procedures at 35 Michigan hospitals has identified three risk factors for surgical site infection after lower-extremity bypass that hospitals and vascular surgery teams may be able to modify.
“Patients who had iodine-only skin antiseptic preparation, a high-peak intraoperative glucose, or long operative times were more likely to have substantially increased risk for surgical site infection (SSI),” Frank Davis, MD, of the University of Michigan said in reporting the study results at the annual meeting of the Midwestern Vascular Surgical Society. Those risk factors are modifiable, Dr. Davis said.
“Specific attention needs to be served moving forward in attempts to decrease the risk of SSI for lower-extremity bypass,” Dr. Davis said. “The incidence of SSI in our cohort across the state of Michigan was approximately 9.2%, and for those who did develop a SSI, there was a substantial increase in 30-day morbidity.”
Patients who had an SSI were more than three times more likely to have a major amputation (9% vs. 2.3%) than those without, and more than five times more likely to have a reoperation (3.9% vs. 0.7%), Dr. Davis said.
“With regard to preoperative symptomatology, those with lower peripheral artery questionnaire scores, resting pain, or acute ischemia were more likely to develop SSI postoperatively,” Dr. Davis said. “Patients who underwent an interim coronal bypass had a significant increase of SSI in comparison to all other bypass configurations.”
He also noted that major teaching hospitals or hospitals with 500 or fewer beds had higher rates of SSI.
“Targeted improvements in preoperative care may decrease complications and improve vascular patient outcomes,” Dr. Davis said.
Dr. Davis had no relationships to disclose.
AT MIDWESTERN VASCULAR 2016
Key clinical point: Study identified three key modifiable risk factors in surgical site infection (SSI) open after lower-extremity bypass (LEB).
Major finding: Incidence of SSI was 9.2% in the study cohort.
Data source: Blue Cross Blue Shield Michigan Vascular Intervention Collaborative database of 3,992 open LEB operations at 35 centers from January 2012 to June 2015.
Disclosures: Dr. Davis reported having no financial disclosures.
Results puzzling for embolic protection during TAVR
The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during transcatheter aortic valve replacement yielded puzzling and somewhat contradictory results, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
Virtually every device in this industry-sponsored study involving 363 elderly patients (mean age, 83.4 years) with severe aortic stenosis trapped particulate debris as intended, the mean volume of new lesions in the protected areas of the brain was reduced by 42%, and the number and volume of new lesions correlated with neurocognitive outcomes at 30 days.
However, the reduction in lesion volume did not achieve statistical significance, and the improvement in neurocognitive function also did not reach statistical significance.
In addition, “the sample size was clearly too low to assess clinical outcomes, and in retrospect, was also too low to evaluate follow-up MRI findings or neurocognitive outcomes.” Nevertheless, the trial “provides reassuring evidence of device safety,” said Samir R. Kapadia, MD, of the Cleveland Clinic (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.023).
In this prospective study, the investigators assessed patients at 17 medical centers in the United States and 2 in Germany. In addition to being elderly, the study patients were at high risk because of frequent comorbidities, including atrial fibrillation (31.7%) and prior stroke (5.8%).
The remaining 123 patients underwent TAVR but not MRI in a safety arm of the trial.
The protection devices were placed “without safety concerns” in most patients. The rate of major adverse events with the device was 7.3%, markedly less than the 18.3% prespecified performance goal for this outcome. Total procedure time was lengthened by only 13 minutes when the device was used, and total fluoroscopy time was increased by only 3 minutes. These findings demonstrate the overall safety of using the device, Dr. Kapadia said.
Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the filters in 99% of patients.
The mean volume of new cerebral lesions in areas of the brain protected by the device was reduced by 42%, compared with that in patients who underwent TAVR without the protection device. However, this reduction was not statistically significant, so the primary efficacy endpoint of the study was not met.
Similarly, neurocognitive testing at 30 days showed that the volume of new lesions correlated with poorer outcomes. However, the difference in neurocognitive function between the intervention group and the control group did not reach statistical significance.
Several limitations likely contributed to this lack of statistical significance, Dr. Kapadia said.
First, the 5-day “window” for MRI assessment was too long. Both the number and the volume of new lesions rapidly changed over time, which led to marked variance in MRI findings depending on when the images were taken.
In addition, only one TAVR device was available at the time the trial was designed, so the study wasn’t stratified by type of valve device. But several new devices became available during the study, and the study investigators were permitted to use any of them. Both pre- and postimplantation techniques differ among these TAVR devices, but these differences could not be accounted for, given the study design.
Also, certain risk factors for stroke, especially certain findings on baseline MRI, were not understood when the trial was designed, and those factors also were not accounted for, Dr. Kapadia said.
Claret Medical funded the study. Dr. Kapadia reported having no relevant financial disclosures; his associates reported numerous ties to industry sources. The meeting was sponsored by the Cardiovascular Research Foundation.
From a logical standpoint, a device that collects cerebral embolic material in 99% of cases should prevent ischemic brain injury, yet the findings from this randomized trial don’t appear to support the routine use of such devices. But it would be inappropriate and unfair to close the book on cerebral protection after this chapter.
The authors acknowledge that an MRI “window” of 5 days creates too much heterogeneity in the data, that multiple TAVR devices requiring different implantation techniques further muddy the picture, and that in retrospect the sample size was inadequate and the study was underpowered. In addition, rigorous neurocognitive assessment can be challenging in elderly, recovering patients, and results can depend on the time of day and the patient’s alertness.
Despite the negative findings regarding both primary and secondary endpoints, the data do show the overall safety of embolic protection devices. We are dealing with a potential benefit that cannot be ignored as TAVR shifts to younger and lower-risk patients.
Azeem Latib, MD, is in the interventional cardiology unit at San Raffaele Scientific Institute in Milan. Matteo Pagnesi, MD, is in the interventional cardiology unit at EMO-GVM Centro Cuore Columbus in Milan. San Raffaele Scientific Institute has been involved in clinical studies of embolic protection devices made by Claret Medical, Innovative Cardiovascular Solutions, and Keystone Heart. Dr. Latib and Dr. Pagnesi reported having no other relevant financial disclosures. They made these remarks in an editorial accompanying Dr. Kapadia’s report (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.036).
From a logical standpoint, a device that collects cerebral embolic material in 99% of cases should prevent ischemic brain injury, yet the findings from this randomized trial don’t appear to support the routine use of such devices. But it would be inappropriate and unfair to close the book on cerebral protection after this chapter.
The authors acknowledge that an MRI “window” of 5 days creates too much heterogeneity in the data, that multiple TAVR devices requiring different implantation techniques further muddy the picture, and that in retrospect the sample size was inadequate and the study was underpowered. In addition, rigorous neurocognitive assessment can be challenging in elderly, recovering patients, and results can depend on the time of day and the patient’s alertness.
Despite the negative findings regarding both primary and secondary endpoints, the data do show the overall safety of embolic protection devices. We are dealing with a potential benefit that cannot be ignored as TAVR shifts to younger and lower-risk patients.
Azeem Latib, MD, is in the interventional cardiology unit at San Raffaele Scientific Institute in Milan. Matteo Pagnesi, MD, is in the interventional cardiology unit at EMO-GVM Centro Cuore Columbus in Milan. San Raffaele Scientific Institute has been involved in clinical studies of embolic protection devices made by Claret Medical, Innovative Cardiovascular Solutions, and Keystone Heart. Dr. Latib and Dr. Pagnesi reported having no other relevant financial disclosures. They made these remarks in an editorial accompanying Dr. Kapadia’s report (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.036).
From a logical standpoint, a device that collects cerebral embolic material in 99% of cases should prevent ischemic brain injury, yet the findings from this randomized trial don’t appear to support the routine use of such devices. But it would be inappropriate and unfair to close the book on cerebral protection after this chapter.
The authors acknowledge that an MRI “window” of 5 days creates too much heterogeneity in the data, that multiple TAVR devices requiring different implantation techniques further muddy the picture, and that in retrospect the sample size was inadequate and the study was underpowered. In addition, rigorous neurocognitive assessment can be challenging in elderly, recovering patients, and results can depend on the time of day and the patient’s alertness.
Despite the negative findings regarding both primary and secondary endpoints, the data do show the overall safety of embolic protection devices. We are dealing with a potential benefit that cannot be ignored as TAVR shifts to younger and lower-risk patients.
Azeem Latib, MD, is in the interventional cardiology unit at San Raffaele Scientific Institute in Milan. Matteo Pagnesi, MD, is in the interventional cardiology unit at EMO-GVM Centro Cuore Columbus in Milan. San Raffaele Scientific Institute has been involved in clinical studies of embolic protection devices made by Claret Medical, Innovative Cardiovascular Solutions, and Keystone Heart. Dr. Latib and Dr. Pagnesi reported having no other relevant financial disclosures. They made these remarks in an editorial accompanying Dr. Kapadia’s report (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.036).
The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during transcatheter aortic valve replacement yielded puzzling and somewhat contradictory results, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
Virtually every device in this industry-sponsored study involving 363 elderly patients (mean age, 83.4 years) with severe aortic stenosis trapped particulate debris as intended, the mean volume of new lesions in the protected areas of the brain was reduced by 42%, and the number and volume of new lesions correlated with neurocognitive outcomes at 30 days.
However, the reduction in lesion volume did not achieve statistical significance, and the improvement in neurocognitive function also did not reach statistical significance.
In addition, “the sample size was clearly too low to assess clinical outcomes, and in retrospect, was also too low to evaluate follow-up MRI findings or neurocognitive outcomes.” Nevertheless, the trial “provides reassuring evidence of device safety,” said Samir R. Kapadia, MD, of the Cleveland Clinic (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.023).
In this prospective study, the investigators assessed patients at 17 medical centers in the United States and 2 in Germany. In addition to being elderly, the study patients were at high risk because of frequent comorbidities, including atrial fibrillation (31.7%) and prior stroke (5.8%).
The remaining 123 patients underwent TAVR but not MRI in a safety arm of the trial.
The protection devices were placed “without safety concerns” in most patients. The rate of major adverse events with the device was 7.3%, markedly less than the 18.3% prespecified performance goal for this outcome. Total procedure time was lengthened by only 13 minutes when the device was used, and total fluoroscopy time was increased by only 3 minutes. These findings demonstrate the overall safety of using the device, Dr. Kapadia said.
Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the filters in 99% of patients.
The mean volume of new cerebral lesions in areas of the brain protected by the device was reduced by 42%, compared with that in patients who underwent TAVR without the protection device. However, this reduction was not statistically significant, so the primary efficacy endpoint of the study was not met.
Similarly, neurocognitive testing at 30 days showed that the volume of new lesions correlated with poorer outcomes. However, the difference in neurocognitive function between the intervention group and the control group did not reach statistical significance.
Several limitations likely contributed to this lack of statistical significance, Dr. Kapadia said.
First, the 5-day “window” for MRI assessment was too long. Both the number and the volume of new lesions rapidly changed over time, which led to marked variance in MRI findings depending on when the images were taken.
In addition, only one TAVR device was available at the time the trial was designed, so the study wasn’t stratified by type of valve device. But several new devices became available during the study, and the study investigators were permitted to use any of them. Both pre- and postimplantation techniques differ among these TAVR devices, but these differences could not be accounted for, given the study design.
Also, certain risk factors for stroke, especially certain findings on baseline MRI, were not understood when the trial was designed, and those factors also were not accounted for, Dr. Kapadia said.
Claret Medical funded the study. Dr. Kapadia reported having no relevant financial disclosures; his associates reported numerous ties to industry sources. The meeting was sponsored by the Cardiovascular Research Foundation.
The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during transcatheter aortic valve replacement yielded puzzling and somewhat contradictory results, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
Virtually every device in this industry-sponsored study involving 363 elderly patients (mean age, 83.4 years) with severe aortic stenosis trapped particulate debris as intended, the mean volume of new lesions in the protected areas of the brain was reduced by 42%, and the number and volume of new lesions correlated with neurocognitive outcomes at 30 days.
However, the reduction in lesion volume did not achieve statistical significance, and the improvement in neurocognitive function also did not reach statistical significance.
In addition, “the sample size was clearly too low to assess clinical outcomes, and in retrospect, was also too low to evaluate follow-up MRI findings or neurocognitive outcomes.” Nevertheless, the trial “provides reassuring evidence of device safety,” said Samir R. Kapadia, MD, of the Cleveland Clinic (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.023).
In this prospective study, the investigators assessed patients at 17 medical centers in the United States and 2 in Germany. In addition to being elderly, the study patients were at high risk because of frequent comorbidities, including atrial fibrillation (31.7%) and prior stroke (5.8%).
The remaining 123 patients underwent TAVR but not MRI in a safety arm of the trial.
The protection devices were placed “without safety concerns” in most patients. The rate of major adverse events with the device was 7.3%, markedly less than the 18.3% prespecified performance goal for this outcome. Total procedure time was lengthened by only 13 minutes when the device was used, and total fluoroscopy time was increased by only 3 minutes. These findings demonstrate the overall safety of using the device, Dr. Kapadia said.
Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the filters in 99% of patients.
The mean volume of new cerebral lesions in areas of the brain protected by the device was reduced by 42%, compared with that in patients who underwent TAVR without the protection device. However, this reduction was not statistically significant, so the primary efficacy endpoint of the study was not met.
Similarly, neurocognitive testing at 30 days showed that the volume of new lesions correlated with poorer outcomes. However, the difference in neurocognitive function between the intervention group and the control group did not reach statistical significance.
Several limitations likely contributed to this lack of statistical significance, Dr. Kapadia said.
First, the 5-day “window” for MRI assessment was too long. Both the number and the volume of new lesions rapidly changed over time, which led to marked variance in MRI findings depending on when the images were taken.
In addition, only one TAVR device was available at the time the trial was designed, so the study wasn’t stratified by type of valve device. But several new devices became available during the study, and the study investigators were permitted to use any of them. Both pre- and postimplantation techniques differ among these TAVR devices, but these differences could not be accounted for, given the study design.
Also, certain risk factors for stroke, especially certain findings on baseline MRI, were not understood when the trial was designed, and those factors also were not accounted for, Dr. Kapadia said.
Claret Medical funded the study. Dr. Kapadia reported having no relevant financial disclosures; his associates reported numerous ties to industry sources. The meeting was sponsored by the Cardiovascular Research Foundation.
Key clinical point: The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during TAVR yielded puzzling and contradictory results.
Major finding: Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the cerebral protection filters in 99% of patients.
Data source: A prospective, international, randomized trial involving 363 elderly patients undergoing TAVR for severe aortic stenosis.
Disclosures: Claret Medical funded the study. Dr. Kapadia reported having no relevant financial disclosures; his associates reported numerous ties to industry sources.
Ezetimibe’s ACS benefit centers on high-risk, post-CABG patients
ROME – Patients who have undergone coronary artery bypass surgery and who later have an acute coronary syndrome event gain the most from an aggressive lipid-lowering regimen, according to an exploratory analysis of data from more than 18,000 patients enrolled in the IMPROVE-IT trial that tested the incremental benefit from ezetimibe treatment when added to a statin.
Additional exploratory analyses further showed that high-risk acute coronary syndrome (ACS) patients without a history of coronary artery bypass grafting (CABG) also benefited from adding ezetimibe to a background regimen of simvastatin, but the benefit from adding ezetimibe completely disappeared in low-risk ACS patients, Alon Eisen, MD, said at the annual congress of the European Society of Cardiology.
‘The benefit of adding ezetimibe to a statin was enhanced in patients with prior CABG and in other high-risk patients with no prior CABG, supporting the use of more intensive lipid-lowering therapy in these high-risk patients,” said Dr. Eisen, a cardiologist at Brigham and Women’s Hospital in Boston. He also highlighted that ezetimibe is “a safe drug that is coming off patent.” Adding ezetimibe had a moderate effect on LDL cholesterol levels, cutting them from a median of 70 mg/dL in patients in the placebo arm to a median of 54 mg/dL in the group who received ezetimibe.
These results “show that if we pick the right patients, a very benign drug can have a great benefit,” said Eugene Braunwald, MD, a coinvestigator on the IMPROVE-IT trial and a collaborator with Dr. Eisen on the new analysis. The new findings “emphasize that the higher a patient’s risk, the more effect they get from cholesterol-lowering treatment,” said Dr. Braunwald, professor of medicine at Harvard University and a cardiologist at Brigham and Women’s Hospital, both in Boston.
The second exploratory analysis reported by Dr. Eisen looked at the more than 16,000 patients in IMPROVE-IT without history of CABG. The analysis applied a newly developed, nine-item formula for stratifying atherothrombotic risk (Circulation. 2016 July 26;134[4];304-13) to divide these patients into low-, intermediate- and high-risk subgroups. Patients in the high-risk subgroup (20% of the IMPROVE-IT subgroup) had a 6–percentage point reduction in their primary endpoint event rate with added ezetimibe treatment, while those at intermediate risk (31%) got a 2–percentage point decrease in endpoint events, and low-risk patients (49%) actually showed a small, less than 1–percentage point increase in endpoint events with added ezetimibe, Dr. Eisen reported.
IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
[email protected]
On Twitter @mitchelzoler
I suspect that the patients in IMPROVE-IT with a history of coronary artery bypass graft surgery were more likely than the other enrolled acute coronary syndrome patients to have more extensive and systemic atherosclerotic disease. Although coronary artery bypass addresses the most acute obstructions to coronary flow that exist at the time of surgery, the procedure does not cure the patient’s underlying vascular disease. We know that a substantial majority of coronary events occur in arteries that are not heavily stenosed.
Another important limitation to keep in mind about the IMPROVE-IT trial was that the background statin treatment all patients received was modest – 40 mg of simvastatin daily. In real-world practice, high-risk patients should go on the most potent statin regimen they can tolerate – ideally, 40 mg daily of rosuvastatin. The need for additional lipid-lowering interventions, with ezetimibe or other drugs, can then be considered as an add-on to aggressive statin therapy.
Richard A. Chazal, MD, is an invasive cardiologist and medical director of the Heart and Vascular Institute of Lee Memorial Health System in Fort Myers, Fla. He is also the current president of the American College of Cardiology. He had no disclosures. He made these comments in an interview.
I suspect that the patients in IMPROVE-IT with a history of coronary artery bypass graft surgery were more likely than the other enrolled acute coronary syndrome patients to have more extensive and systemic atherosclerotic disease. Although coronary artery bypass addresses the most acute obstructions to coronary flow that exist at the time of surgery, the procedure does not cure the patient’s underlying vascular disease. We know that a substantial majority of coronary events occur in arteries that are not heavily stenosed.
Another important limitation to keep in mind about the IMPROVE-IT trial was that the background statin treatment all patients received was modest – 40 mg of simvastatin daily. In real-world practice, high-risk patients should go on the most potent statin regimen they can tolerate – ideally, 40 mg daily of rosuvastatin. The need for additional lipid-lowering interventions, with ezetimibe or other drugs, can then be considered as an add-on to aggressive statin therapy.
Richard A. Chazal, MD, is an invasive cardiologist and medical director of the Heart and Vascular Institute of Lee Memorial Health System in Fort Myers, Fla. He is also the current president of the American College of Cardiology. He had no disclosures. He made these comments in an interview.
I suspect that the patients in IMPROVE-IT with a history of coronary artery bypass graft surgery were more likely than the other enrolled acute coronary syndrome patients to have more extensive and systemic atherosclerotic disease. Although coronary artery bypass addresses the most acute obstructions to coronary flow that exist at the time of surgery, the procedure does not cure the patient’s underlying vascular disease. We know that a substantial majority of coronary events occur in arteries that are not heavily stenosed.
Another important limitation to keep in mind about the IMPROVE-IT trial was that the background statin treatment all patients received was modest – 40 mg of simvastatin daily. In real-world practice, high-risk patients should go on the most potent statin regimen they can tolerate – ideally, 40 mg daily of rosuvastatin. The need for additional lipid-lowering interventions, with ezetimibe or other drugs, can then be considered as an add-on to aggressive statin therapy.
Richard A. Chazal, MD, is an invasive cardiologist and medical director of the Heart and Vascular Institute of Lee Memorial Health System in Fort Myers, Fla. He is also the current president of the American College of Cardiology. He had no disclosures. He made these comments in an interview.
ROME – Patients who have undergone coronary artery bypass surgery and who later have an acute coronary syndrome event gain the most from an aggressive lipid-lowering regimen, according to an exploratory analysis of data from more than 18,000 patients enrolled in the IMPROVE-IT trial that tested the incremental benefit from ezetimibe treatment when added to a statin.
Additional exploratory analyses further showed that high-risk acute coronary syndrome (ACS) patients without a history of coronary artery bypass grafting (CABG) also benefited from adding ezetimibe to a background regimen of simvastatin, but the benefit from adding ezetimibe completely disappeared in low-risk ACS patients, Alon Eisen, MD, said at the annual congress of the European Society of Cardiology.
‘The benefit of adding ezetimibe to a statin was enhanced in patients with prior CABG and in other high-risk patients with no prior CABG, supporting the use of more intensive lipid-lowering therapy in these high-risk patients,” said Dr. Eisen, a cardiologist at Brigham and Women’s Hospital in Boston. He also highlighted that ezetimibe is “a safe drug that is coming off patent.” Adding ezetimibe had a moderate effect on LDL cholesterol levels, cutting them from a median of 70 mg/dL in patients in the placebo arm to a median of 54 mg/dL in the group who received ezetimibe.
These results “show that if we pick the right patients, a very benign drug can have a great benefit,” said Eugene Braunwald, MD, a coinvestigator on the IMPROVE-IT trial and a collaborator with Dr. Eisen on the new analysis. The new findings “emphasize that the higher a patient’s risk, the more effect they get from cholesterol-lowering treatment,” said Dr. Braunwald, professor of medicine at Harvard University and a cardiologist at Brigham and Women’s Hospital, both in Boston.
The second exploratory analysis reported by Dr. Eisen looked at the more than 16,000 patients in IMPROVE-IT without history of CABG. The analysis applied a newly developed, nine-item formula for stratifying atherothrombotic risk (Circulation. 2016 July 26;134[4];304-13) to divide these patients into low-, intermediate- and high-risk subgroups. Patients in the high-risk subgroup (20% of the IMPROVE-IT subgroup) had a 6–percentage point reduction in their primary endpoint event rate with added ezetimibe treatment, while those at intermediate risk (31%) got a 2–percentage point decrease in endpoint events, and low-risk patients (49%) actually showed a small, less than 1–percentage point increase in endpoint events with added ezetimibe, Dr. Eisen reported.
IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
[email protected]
On Twitter @mitchelzoler
ROME – Patients who have undergone coronary artery bypass surgery and who later have an acute coronary syndrome event gain the most from an aggressive lipid-lowering regimen, according to an exploratory analysis of data from more than 18,000 patients enrolled in the IMPROVE-IT trial that tested the incremental benefit from ezetimibe treatment when added to a statin.
Additional exploratory analyses further showed that high-risk acute coronary syndrome (ACS) patients without a history of coronary artery bypass grafting (CABG) also benefited from adding ezetimibe to a background regimen of simvastatin, but the benefit from adding ezetimibe completely disappeared in low-risk ACS patients, Alon Eisen, MD, said at the annual congress of the European Society of Cardiology.
‘The benefit of adding ezetimibe to a statin was enhanced in patients with prior CABG and in other high-risk patients with no prior CABG, supporting the use of more intensive lipid-lowering therapy in these high-risk patients,” said Dr. Eisen, a cardiologist at Brigham and Women’s Hospital in Boston. He also highlighted that ezetimibe is “a safe drug that is coming off patent.” Adding ezetimibe had a moderate effect on LDL cholesterol levels, cutting them from a median of 70 mg/dL in patients in the placebo arm to a median of 54 mg/dL in the group who received ezetimibe.
These results “show that if we pick the right patients, a very benign drug can have a great benefit,” said Eugene Braunwald, MD, a coinvestigator on the IMPROVE-IT trial and a collaborator with Dr. Eisen on the new analysis. The new findings “emphasize that the higher a patient’s risk, the more effect they get from cholesterol-lowering treatment,” said Dr. Braunwald, professor of medicine at Harvard University and a cardiologist at Brigham and Women’s Hospital, both in Boston.
The second exploratory analysis reported by Dr. Eisen looked at the more than 16,000 patients in IMPROVE-IT without history of CABG. The analysis applied a newly developed, nine-item formula for stratifying atherothrombotic risk (Circulation. 2016 July 26;134[4];304-13) to divide these patients into low-, intermediate- and high-risk subgroups. Patients in the high-risk subgroup (20% of the IMPROVE-IT subgroup) had a 6–percentage point reduction in their primary endpoint event rate with added ezetimibe treatment, while those at intermediate risk (31%) got a 2–percentage point decrease in endpoint events, and low-risk patients (49%) actually showed a small, less than 1–percentage point increase in endpoint events with added ezetimibe, Dr. Eisen reported.
IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
[email protected]
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2016
Key clinical point:
Major finding: The absolute primary-event risk reduction was 9% in post-CABG patients and 1% in all other patients.
Data source: An exploratory, post-hoc analysis of data collected in IMPROVE-IT, a multicenter trial with 18,144 patients.
Disclosures: IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
VIDEO: Pre–gastric bypass antibiotics alter gut microbiome
WASHINGTON – Antibiotics given in advance of gastric bypass surgery preferentially alter the microbiome, nudging it toward a more “lean” physiologic profile.
Given before a sleeve gastrectomy, vancomycin, which has little gut penetration, barely shifted the high ratio of Firmicutes to Bacteroidetes, a profile typically associated with obesity and insulin resistance. But cefazolin, which has much higher gut penetration, suppressed the presence of Firmicutes, which metabolize fat, and allowed the expansion of carbohydrate-loving Bacteroidetes – a profile generally seen in lean people.
Cyrus Jahansouz, MD, of the University of Minnesota, Minneapolis, and his colleagues wanted to examine whether a shift in preoperative antibiotics might affect the way the microbiome re-establishes itself in the wake of vertical sleeve gastrectomy. They enrolled 32 patients who were candidates for the procedure. None had undergone prior gastrointestinal surgery, and none had been exposed to antibiotics in the 3 months prior to bariatric surgery. They were similar in age, weight, body mass index, and fasting glucose. The mean HbA1c was about 6%.
Patients were randomized to three groups: maximal diet therapy (800 calories per day) without surgery; vertical sleeve gastrectomy with the usual preoperative antibiotic cefazolin and the postsurgical diet; and vertical sleeve gastrectomy with preoperative vancomycin and the postsurgical diet. All patients gave a fecal sample immediately before surgery and another one 6 days after surgery.
Preoperative cluster analysis of bacterial DNA showed that all of the samples had a similar composition, predominated by Firmicutes species (60%-70%). Bacteroidetes species made up about 20%-30%, with Proteobacteriae, Actinobacteriae, Verrucomicrobia, and other phyla comprising the remainder of the microbiome.
At the second sampling, the diet-only group showed no microbiome changes at all. The vancomycin group showed a very small but not significant expansion of Bacteroidetes and reduction of Firmicutes.
Patients in the cefazolin group showed a significant shift in the ratio – and it was quite striking, Dr. Jahansouz said. Among these patients, Firmicutes had decreased from 70% to 40% of the community. Bacteroidetes showed a corresponding shift, increasing from 20% of the community to 45%. The findings are quite surprising, he noted, considering that only one dose of antibiotic was associated with the changes and that they were evident within just a few days.
Although “a little hard to interpret” because of its small size and short follow-up, the study suggests that antibiotic choice might contribute to the success of weight-loss surgery, Dr. Jahansouz said at the annual clinical congress of the American College of Surgeons.
“There are still several factors in the perioperative period that we have to study to be able to identify what other things might have also influenced the shift,” he said in an interview. “But I do think that, in the future, these changes can be manipulated to benefit metabolic outcomes.”
Two phyla – Bacteroidetes and Firmicutes – dominate the human gut microbiome in a dynamic ratio that is highly associated with the way energy is extracted from food. Bacteroidetes species specialize in carbohydrate digestion and Firmicutes in fat digestion. “In a lean, insulin-sensitive state, Bacteroidetes dominates the human gut microbiome,” Dr. Jahansouz said. “With the progression of obesity and insulin resistance, there is a subsequent shift in the microbiome phenotype, favoring the growth of Firmicutes at the expense and reduction of Bacteroidetes. This is a significant change, because this obesity-associated phenotype has an increased capacity to harvest energy. It’s not the same for a lean person to consume 1,000 calories as it is for an obese person to consume them.”
Bariatric surgery has been shown to alter the gut microbiome, shifting it toward this more “lean” profile (Cell Metab. 2015 Aug 4;22[2]:228-38). This shift may be an important component of the still not fully elucidated mechanisms by which bariatric surgery causes weight loss and normalizes insulin signaling, Dr. Jahansouz said.
Dr. Jahansouz is following this group of patients to explore whether there are differences in weight loss and insulin signaling. He also will track whether the microbiome stabilizes at its early postsurgical profile, or continues to shift, either toward an even higher Bacteroidetes to Firmicutes ratio, or back to a more “obese” profile.
He and his colleagues are also investigating the effect of antibiotics and gastric bypass surgery in mouse models. “I can say that antibiotics seem to have a remarkable impact on the effect of mouse sleeve gastrectomy. We’re not quite there yet with humans,” but the data are compelling.
Dr. Jahansouz said that he had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @Alz_Gal
WASHINGTON – Antibiotics given in advance of gastric bypass surgery preferentially alter the microbiome, nudging it toward a more “lean” physiologic profile.
Given before a sleeve gastrectomy, vancomycin, which has little gut penetration, barely shifted the high ratio of Firmicutes to Bacteroidetes, a profile typically associated with obesity and insulin resistance. But cefazolin, which has much higher gut penetration, suppressed the presence of Firmicutes, which metabolize fat, and allowed the expansion of carbohydrate-loving Bacteroidetes – a profile generally seen in lean people.
Cyrus Jahansouz, MD, of the University of Minnesota, Minneapolis, and his colleagues wanted to examine whether a shift in preoperative antibiotics might affect the way the microbiome re-establishes itself in the wake of vertical sleeve gastrectomy. They enrolled 32 patients who were candidates for the procedure. None had undergone prior gastrointestinal surgery, and none had been exposed to antibiotics in the 3 months prior to bariatric surgery. They were similar in age, weight, body mass index, and fasting glucose. The mean HbA1c was about 6%.
Patients were randomized to three groups: maximal diet therapy (800 calories per day) without surgery; vertical sleeve gastrectomy with the usual preoperative antibiotic cefazolin and the postsurgical diet; and vertical sleeve gastrectomy with preoperative vancomycin and the postsurgical diet. All patients gave a fecal sample immediately before surgery and another one 6 days after surgery.
Preoperative cluster analysis of bacterial DNA showed that all of the samples had a similar composition, predominated by Firmicutes species (60%-70%). Bacteroidetes species made up about 20%-30%, with Proteobacteriae, Actinobacteriae, Verrucomicrobia, and other phyla comprising the remainder of the microbiome.
At the second sampling, the diet-only group showed no microbiome changes at all. The vancomycin group showed a very small but not significant expansion of Bacteroidetes and reduction of Firmicutes.
Patients in the cefazolin group showed a significant shift in the ratio – and it was quite striking, Dr. Jahansouz said. Among these patients, Firmicutes had decreased from 70% to 40% of the community. Bacteroidetes showed a corresponding shift, increasing from 20% of the community to 45%. The findings are quite surprising, he noted, considering that only one dose of antibiotic was associated with the changes and that they were evident within just a few days.
Although “a little hard to interpret” because of its small size and short follow-up, the study suggests that antibiotic choice might contribute to the success of weight-loss surgery, Dr. Jahansouz said at the annual clinical congress of the American College of Surgeons.
“There are still several factors in the perioperative period that we have to study to be able to identify what other things might have also influenced the shift,” he said in an interview. “But I do think that, in the future, these changes can be manipulated to benefit metabolic outcomes.”
Two phyla – Bacteroidetes and Firmicutes – dominate the human gut microbiome in a dynamic ratio that is highly associated with the way energy is extracted from food. Bacteroidetes species specialize in carbohydrate digestion and Firmicutes in fat digestion. “In a lean, insulin-sensitive state, Bacteroidetes dominates the human gut microbiome,” Dr. Jahansouz said. “With the progression of obesity and insulin resistance, there is a subsequent shift in the microbiome phenotype, favoring the growth of Firmicutes at the expense and reduction of Bacteroidetes. This is a significant change, because this obesity-associated phenotype has an increased capacity to harvest energy. It’s not the same for a lean person to consume 1,000 calories as it is for an obese person to consume them.”
Bariatric surgery has been shown to alter the gut microbiome, shifting it toward this more “lean” profile (Cell Metab. 2015 Aug 4;22[2]:228-38). This shift may be an important component of the still not fully elucidated mechanisms by which bariatric surgery causes weight loss and normalizes insulin signaling, Dr. Jahansouz said.
Dr. Jahansouz is following this group of patients to explore whether there are differences in weight loss and insulin signaling. He also will track whether the microbiome stabilizes at its early postsurgical profile, or continues to shift, either toward an even higher Bacteroidetes to Firmicutes ratio, or back to a more “obese” profile.
He and his colleagues are also investigating the effect of antibiotics and gastric bypass surgery in mouse models. “I can say that antibiotics seem to have a remarkable impact on the effect of mouse sleeve gastrectomy. We’re not quite there yet with humans,” but the data are compelling.
Dr. Jahansouz said that he had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @Alz_Gal
WASHINGTON – Antibiotics given in advance of gastric bypass surgery preferentially alter the microbiome, nudging it toward a more “lean” physiologic profile.
Given before a sleeve gastrectomy, vancomycin, which has little gut penetration, barely shifted the high ratio of Firmicutes to Bacteroidetes, a profile typically associated with obesity and insulin resistance. But cefazolin, which has much higher gut penetration, suppressed the presence of Firmicutes, which metabolize fat, and allowed the expansion of carbohydrate-loving Bacteroidetes – a profile generally seen in lean people.
Cyrus Jahansouz, MD, of the University of Minnesota, Minneapolis, and his colleagues wanted to examine whether a shift in preoperative antibiotics might affect the way the microbiome re-establishes itself in the wake of vertical sleeve gastrectomy. They enrolled 32 patients who were candidates for the procedure. None had undergone prior gastrointestinal surgery, and none had been exposed to antibiotics in the 3 months prior to bariatric surgery. They were similar in age, weight, body mass index, and fasting glucose. The mean HbA1c was about 6%.
Patients were randomized to three groups: maximal diet therapy (800 calories per day) without surgery; vertical sleeve gastrectomy with the usual preoperative antibiotic cefazolin and the postsurgical diet; and vertical sleeve gastrectomy with preoperative vancomycin and the postsurgical diet. All patients gave a fecal sample immediately before surgery and another one 6 days after surgery.
Preoperative cluster analysis of bacterial DNA showed that all of the samples had a similar composition, predominated by Firmicutes species (60%-70%). Bacteroidetes species made up about 20%-30%, with Proteobacteriae, Actinobacteriae, Verrucomicrobia, and other phyla comprising the remainder of the microbiome.
At the second sampling, the diet-only group showed no microbiome changes at all. The vancomycin group showed a very small but not significant expansion of Bacteroidetes and reduction of Firmicutes.
Patients in the cefazolin group showed a significant shift in the ratio – and it was quite striking, Dr. Jahansouz said. Among these patients, Firmicutes had decreased from 70% to 40% of the community. Bacteroidetes showed a corresponding shift, increasing from 20% of the community to 45%. The findings are quite surprising, he noted, considering that only one dose of antibiotic was associated with the changes and that they were evident within just a few days.
Although “a little hard to interpret” because of its small size and short follow-up, the study suggests that antibiotic choice might contribute to the success of weight-loss surgery, Dr. Jahansouz said at the annual clinical congress of the American College of Surgeons.
“There are still several factors in the perioperative period that we have to study to be able to identify what other things might have also influenced the shift,” he said in an interview. “But I do think that, in the future, these changes can be manipulated to benefit metabolic outcomes.”
Two phyla – Bacteroidetes and Firmicutes – dominate the human gut microbiome in a dynamic ratio that is highly associated with the way energy is extracted from food. Bacteroidetes species specialize in carbohydrate digestion and Firmicutes in fat digestion. “In a lean, insulin-sensitive state, Bacteroidetes dominates the human gut microbiome,” Dr. Jahansouz said. “With the progression of obesity and insulin resistance, there is a subsequent shift in the microbiome phenotype, favoring the growth of Firmicutes at the expense and reduction of Bacteroidetes. This is a significant change, because this obesity-associated phenotype has an increased capacity to harvest energy. It’s not the same for a lean person to consume 1,000 calories as it is for an obese person to consume them.”
Bariatric surgery has been shown to alter the gut microbiome, shifting it toward this more “lean” profile (Cell Metab. 2015 Aug 4;22[2]:228-38). This shift may be an important component of the still not fully elucidated mechanisms by which bariatric surgery causes weight loss and normalizes insulin signaling, Dr. Jahansouz said.
Dr. Jahansouz is following this group of patients to explore whether there are differences in weight loss and insulin signaling. He also will track whether the microbiome stabilizes at its early postsurgical profile, or continues to shift, either toward an even higher Bacteroidetes to Firmicutes ratio, or back to a more “obese” profile.
He and his colleagues are also investigating the effect of antibiotics and gastric bypass surgery in mouse models. “I can say that antibiotics seem to have a remarkable impact on the effect of mouse sleeve gastrectomy. We’re not quite there yet with humans,” but the data are compelling.
Dr. Jahansouz said that he had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @Alz_Gal
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
Adjunctive azithromycin cuts postcesarean infection
Adding a single intravenous dose of azithromycin to standard antibiotic prophylaxis further reduces maternal infections without increasing neonatal adverse outcomes after nonelective cesarean delivery, according to a report published in the New England Journal of Medicine.
The adjunctive azithromycin also significantly decreased rates of postpartum fever and of readmission or unscheduled office visits, wrote Alan T.N. Tita, MD, PhD, of the University of Alabama at Birmingham, and his colleagues.
Recent studies have suggested that extended-spectrum prophylaxis using azithromycin, when added to standard cephalosporin prophylaxis, would further reduce the incidence of post-cesarean infection, chiefly because of azithromycin’s coverage of ureaplasma species that are frequently associated with these infections. The C/SOAP (Cesarean Section Optimal Antibiotic Prophylaxis) trial tested this hypothesis in 2,013 women who underwent nonelective cesarean delivery of singleton neonates at 14 U.S. hospitals during a 3.5-year period.
All the women received standard antibiotic prophylaxis (usually with cefazolin) and were randomly assigned to receive either a 500-mg dose of azithromycin (1,019 participants) or a matching placebo (994 participants) before surgical incision.
The primary outcome measure – a composite of endometritis; wound infection; or other infections such as abdominopelvic abscess, maternal sepsis, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, or meningitis occurring up to 6 weeks after surgery – developed in half as many women in the azithromycin group (6.1%) as in the placebo group (12.0%). The relative risk (RR) was 0.51 (P less than .001).
Azithromycin, in particular, was associated with significantly lower rates of endometritis (3.8% vs. 6.1%; RR, 0.62; P = .02) and wound infection (2.4% vs. 6.6%; RR, 0.35; P less than .001). This benefit extended across all subgroups of patients regardless of study site, maternal obesity status, the presence or absence of membrane rupture at randomization, preterm or term delivery, or maternal diabetes status.
The number of patients who would need to be treated to prevent one study outcome was 17 for the primary outcome, 43 for endometritis, and 24 for wound infections, the researchers reported (N Engl J Med. 2016 Sep 29;375:1231-41).
Serious maternal adverse events also were less common with azithromycin (1.5%) than with placebo (2.9%). Neonatal outcomes did not differ between the study groups. The rate of combined neonatal death or complications was 14.3% with azithromycin and 13.6% with placebo, a nonsignificant difference.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Pfizer donated the azithromycin used in the trial. Dr. Tita reported having no relevant financial disclosures; his colleagues reported ties to numerous industry sources.
This well-designed, pragmatic, multicenter trial shows that a single adjunctive dose of azithromycin likely would reduce the number of infectious complications for women undergoing nonelective cesarean section.
The addition of azithromycin may have been particularly effective for the 73% of this study population who had a body mass index of 30 kg/m2 or more. Obesity is known to double the risk of infectious complications, and previous studies have suggested that cefazolin may be underdosed in women with increased BMI values. It appears that azithromycin improved outcomes on the basis of the additive effects of the two drugs against common surgical pathogens, such as staphylococcus species. Information provided in the Supplementary Appendix accompanying the article indicates that routine bacterial cultures, when done, were much-less-frequently positive in the azithromycin group.
Robert A. Weinstein, MD, and Kenneth M. Boyer, MD, are at Rush University Medical Center and Cook County Health and Hospital System, both in Chicago. Dr. Weinstein reported receiving support from Merck outside of this work, and Dr. Boyer reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Sept 29. doi: 10.1056/NEJMe1610010).
This well-designed, pragmatic, multicenter trial shows that a single adjunctive dose of azithromycin likely would reduce the number of infectious complications for women undergoing nonelective cesarean section.
The addition of azithromycin may have been particularly effective for the 73% of this study population who had a body mass index of 30 kg/m2 or more. Obesity is known to double the risk of infectious complications, and previous studies have suggested that cefazolin may be underdosed in women with increased BMI values. It appears that azithromycin improved outcomes on the basis of the additive effects of the two drugs against common surgical pathogens, such as staphylococcus species. Information provided in the Supplementary Appendix accompanying the article indicates that routine bacterial cultures, when done, were much-less-frequently positive in the azithromycin group.
Robert A. Weinstein, MD, and Kenneth M. Boyer, MD, are at Rush University Medical Center and Cook County Health and Hospital System, both in Chicago. Dr. Weinstein reported receiving support from Merck outside of this work, and Dr. Boyer reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Sept 29. doi: 10.1056/NEJMe1610010).
This well-designed, pragmatic, multicenter trial shows that a single adjunctive dose of azithromycin likely would reduce the number of infectious complications for women undergoing nonelective cesarean section.
The addition of azithromycin may have been particularly effective for the 73% of this study population who had a body mass index of 30 kg/m2 or more. Obesity is known to double the risk of infectious complications, and previous studies have suggested that cefazolin may be underdosed in women with increased BMI values. It appears that azithromycin improved outcomes on the basis of the additive effects of the two drugs against common surgical pathogens, such as staphylococcus species. Information provided in the Supplementary Appendix accompanying the article indicates that routine bacterial cultures, when done, were much-less-frequently positive in the azithromycin group.
Robert A. Weinstein, MD, and Kenneth M. Boyer, MD, are at Rush University Medical Center and Cook County Health and Hospital System, both in Chicago. Dr. Weinstein reported receiving support from Merck outside of this work, and Dr. Boyer reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Sept 29. doi: 10.1056/NEJMe1610010).
Adding a single intravenous dose of azithromycin to standard antibiotic prophylaxis further reduces maternal infections without increasing neonatal adverse outcomes after nonelective cesarean delivery, according to a report published in the New England Journal of Medicine.
The adjunctive azithromycin also significantly decreased rates of postpartum fever and of readmission or unscheduled office visits, wrote Alan T.N. Tita, MD, PhD, of the University of Alabama at Birmingham, and his colleagues.
Recent studies have suggested that extended-spectrum prophylaxis using azithromycin, when added to standard cephalosporin prophylaxis, would further reduce the incidence of post-cesarean infection, chiefly because of azithromycin’s coverage of ureaplasma species that are frequently associated with these infections. The C/SOAP (Cesarean Section Optimal Antibiotic Prophylaxis) trial tested this hypothesis in 2,013 women who underwent nonelective cesarean delivery of singleton neonates at 14 U.S. hospitals during a 3.5-year period.
All the women received standard antibiotic prophylaxis (usually with cefazolin) and were randomly assigned to receive either a 500-mg dose of azithromycin (1,019 participants) or a matching placebo (994 participants) before surgical incision.
The primary outcome measure – a composite of endometritis; wound infection; or other infections such as abdominopelvic abscess, maternal sepsis, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, or meningitis occurring up to 6 weeks after surgery – developed in half as many women in the azithromycin group (6.1%) as in the placebo group (12.0%). The relative risk (RR) was 0.51 (P less than .001).
Azithromycin, in particular, was associated with significantly lower rates of endometritis (3.8% vs. 6.1%; RR, 0.62; P = .02) and wound infection (2.4% vs. 6.6%; RR, 0.35; P less than .001). This benefit extended across all subgroups of patients regardless of study site, maternal obesity status, the presence or absence of membrane rupture at randomization, preterm or term delivery, or maternal diabetes status.
The number of patients who would need to be treated to prevent one study outcome was 17 for the primary outcome, 43 for endometritis, and 24 for wound infections, the researchers reported (N Engl J Med. 2016 Sep 29;375:1231-41).
Serious maternal adverse events also were less common with azithromycin (1.5%) than with placebo (2.9%). Neonatal outcomes did not differ between the study groups. The rate of combined neonatal death or complications was 14.3% with azithromycin and 13.6% with placebo, a nonsignificant difference.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Pfizer donated the azithromycin used in the trial. Dr. Tita reported having no relevant financial disclosures; his colleagues reported ties to numerous industry sources.
Adding a single intravenous dose of azithromycin to standard antibiotic prophylaxis further reduces maternal infections without increasing neonatal adverse outcomes after nonelective cesarean delivery, according to a report published in the New England Journal of Medicine.
The adjunctive azithromycin also significantly decreased rates of postpartum fever and of readmission or unscheduled office visits, wrote Alan T.N. Tita, MD, PhD, of the University of Alabama at Birmingham, and his colleagues.
Recent studies have suggested that extended-spectrum prophylaxis using azithromycin, when added to standard cephalosporin prophylaxis, would further reduce the incidence of post-cesarean infection, chiefly because of azithromycin’s coverage of ureaplasma species that are frequently associated with these infections. The C/SOAP (Cesarean Section Optimal Antibiotic Prophylaxis) trial tested this hypothesis in 2,013 women who underwent nonelective cesarean delivery of singleton neonates at 14 U.S. hospitals during a 3.5-year period.
All the women received standard antibiotic prophylaxis (usually with cefazolin) and were randomly assigned to receive either a 500-mg dose of azithromycin (1,019 participants) or a matching placebo (994 participants) before surgical incision.
The primary outcome measure – a composite of endometritis; wound infection; or other infections such as abdominopelvic abscess, maternal sepsis, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, or meningitis occurring up to 6 weeks after surgery – developed in half as many women in the azithromycin group (6.1%) as in the placebo group (12.0%). The relative risk (RR) was 0.51 (P less than .001).
Azithromycin, in particular, was associated with significantly lower rates of endometritis (3.8% vs. 6.1%; RR, 0.62; P = .02) and wound infection (2.4% vs. 6.6%; RR, 0.35; P less than .001). This benefit extended across all subgroups of patients regardless of study site, maternal obesity status, the presence or absence of membrane rupture at randomization, preterm or term delivery, or maternal diabetes status.
The number of patients who would need to be treated to prevent one study outcome was 17 for the primary outcome, 43 for endometritis, and 24 for wound infections, the researchers reported (N Engl J Med. 2016 Sep 29;375:1231-41).
Serious maternal adverse events also were less common with azithromycin (1.5%) than with placebo (2.9%). Neonatal outcomes did not differ between the study groups. The rate of combined neonatal death or complications was 14.3% with azithromycin and 13.6% with placebo, a nonsignificant difference.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Pfizer donated the azithromycin used in the trial. Dr. Tita reported having no relevant financial disclosures; his colleagues reported ties to numerous industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Nearly half of patients readmitted after liver transplant
Nearly half of patients were readmitted to the hospital within 90 days of liver transplantation, according to a single-center retrospective study.
“As readmission portends decreased survival, an emphasis should be placed on identifying and optimizing those at increased risk. If readmission does occur, however, it presents an opportunity to intervene, as virtually no patients died during initial readmission,” Madhukar S. Patel, MD, and his associates at Massachusetts General Hospital, Boston, wrote online in HPB.
Long wait times for liver transplantation in this part of the country lead to “high patient acuity,” the researchers noted. To better understand the correlates and consequences of posttransplant readmissions, they reviewed the records for 325 adults who underwent liver transplantation at their hospital between 2005 and 2015. Patients averaged 56 years old and had awaited transplant for a mean of 1 year (standard deviation, 506 days). Their average MELD (Model for End-Stage Liver Disease) scores were 30.3 at transplant (SD, 5.8), and 16.9 (SD, 9.4) on postoperative day 5. Their average hospital length of stay was 12 days, the investigators reported (HPB. 2016 Sep 15. doi: 10.1016/j.hpb.2016.08.003). A total of 149 patients (46%) were readmitted within 90 days of discharge, most often for infections (28% of readmissions), followed by medication issues (19%) and biliary complications (11%). The strongest predictor of posttransplant readmission was hepatitis C virus (HCV) infection, which more than doubled the odds of readmission, compared with alcoholic liver disease (odds ratio, 2.37; 95% confidence interval, 1.44-3.91; P = .001). Transplantees with HCV might benefit from closer outpatient follow-up to detect worsening liver function, diagnostic algorithms to help prevent unnecessary readmissions, and associated nosocomial infections, and pre- and posttransplant direct-acting antiviral therapy, “although the impact [of direct-acting antiviral] therapy on readmissions] is unknown at this time,” the investigators said.
The multivariable analysis also linked readmissions to longer hospital stays (OR, 1.03; P = .04), while age and male sex were protective factors, the investigators said. “Although speculative, it is possible that these factors may be protective due to differences in social support structures upon discharge,” they wrote, noting that women are more likely than men to outlive their partners and thus to live alone in later life.
Readmission within 90 days was associated with a significantly lower rate of survival at 5 years (75% vs. 88% for patients who were not readmitted; P = .008). But only one patient died during the initial readmission, “suggesting that when readmission does occur, it may be an opportunity to intervene,” the researchers said. Strategies include earlier extubation and removal of indwelling catheters, decreasing levels of immunosuppression, lowering treatment thresholds, and shifting patients with laboratory abnormalities to the outpatient setting, they noted. “At our center a process has been initiated in which the inpatient transplant attending surgeon directly passes off discharged patients to the outpatient team,” the investigators wrote. “Additionally, for patients discharged to an acute rehabilitation facility, a specific transplant physician point of contact is provided to the team at the rehab center in case any questions or issues arise [after] discharge. Although these strategies are a reasonable starting point, follow-up studies remain necessary in order to evaluate the impact of these interventions in this patient cohort.”
The researchers reported no funding sources and had no relevant financial disclosures.
Nearly half of patients were readmitted to the hospital within 90 days of liver transplantation, according to a single-center retrospective study.
“As readmission portends decreased survival, an emphasis should be placed on identifying and optimizing those at increased risk. If readmission does occur, however, it presents an opportunity to intervene, as virtually no patients died during initial readmission,” Madhukar S. Patel, MD, and his associates at Massachusetts General Hospital, Boston, wrote online in HPB.
Long wait times for liver transplantation in this part of the country lead to “high patient acuity,” the researchers noted. To better understand the correlates and consequences of posttransplant readmissions, they reviewed the records for 325 adults who underwent liver transplantation at their hospital between 2005 and 2015. Patients averaged 56 years old and had awaited transplant for a mean of 1 year (standard deviation, 506 days). Their average MELD (Model for End-Stage Liver Disease) scores were 30.3 at transplant (SD, 5.8), and 16.9 (SD, 9.4) on postoperative day 5. Their average hospital length of stay was 12 days, the investigators reported (HPB. 2016 Sep 15. doi: 10.1016/j.hpb.2016.08.003). A total of 149 patients (46%) were readmitted within 90 days of discharge, most often for infections (28% of readmissions), followed by medication issues (19%) and biliary complications (11%). The strongest predictor of posttransplant readmission was hepatitis C virus (HCV) infection, which more than doubled the odds of readmission, compared with alcoholic liver disease (odds ratio, 2.37; 95% confidence interval, 1.44-3.91; P = .001). Transplantees with HCV might benefit from closer outpatient follow-up to detect worsening liver function, diagnostic algorithms to help prevent unnecessary readmissions, and associated nosocomial infections, and pre- and posttransplant direct-acting antiviral therapy, “although the impact [of direct-acting antiviral] therapy on readmissions] is unknown at this time,” the investigators said.
The multivariable analysis also linked readmissions to longer hospital stays (OR, 1.03; P = .04), while age and male sex were protective factors, the investigators said. “Although speculative, it is possible that these factors may be protective due to differences in social support structures upon discharge,” they wrote, noting that women are more likely than men to outlive their partners and thus to live alone in later life.
Readmission within 90 days was associated with a significantly lower rate of survival at 5 years (75% vs. 88% for patients who were not readmitted; P = .008). But only one patient died during the initial readmission, “suggesting that when readmission does occur, it may be an opportunity to intervene,” the researchers said. Strategies include earlier extubation and removal of indwelling catheters, decreasing levels of immunosuppression, lowering treatment thresholds, and shifting patients with laboratory abnormalities to the outpatient setting, they noted. “At our center a process has been initiated in which the inpatient transplant attending surgeon directly passes off discharged patients to the outpatient team,” the investigators wrote. “Additionally, for patients discharged to an acute rehabilitation facility, a specific transplant physician point of contact is provided to the team at the rehab center in case any questions or issues arise [after] discharge. Although these strategies are a reasonable starting point, follow-up studies remain necessary in order to evaluate the impact of these interventions in this patient cohort.”
The researchers reported no funding sources and had no relevant financial disclosures.
Nearly half of patients were readmitted to the hospital within 90 days of liver transplantation, according to a single-center retrospective study.
“As readmission portends decreased survival, an emphasis should be placed on identifying and optimizing those at increased risk. If readmission does occur, however, it presents an opportunity to intervene, as virtually no patients died during initial readmission,” Madhukar S. Patel, MD, and his associates at Massachusetts General Hospital, Boston, wrote online in HPB.
Long wait times for liver transplantation in this part of the country lead to “high patient acuity,” the researchers noted. To better understand the correlates and consequences of posttransplant readmissions, they reviewed the records for 325 adults who underwent liver transplantation at their hospital between 2005 and 2015. Patients averaged 56 years old and had awaited transplant for a mean of 1 year (standard deviation, 506 days). Their average MELD (Model for End-Stage Liver Disease) scores were 30.3 at transplant (SD, 5.8), and 16.9 (SD, 9.4) on postoperative day 5. Their average hospital length of stay was 12 days, the investigators reported (HPB. 2016 Sep 15. doi: 10.1016/j.hpb.2016.08.003). A total of 149 patients (46%) were readmitted within 90 days of discharge, most often for infections (28% of readmissions), followed by medication issues (19%) and biliary complications (11%). The strongest predictor of posttransplant readmission was hepatitis C virus (HCV) infection, which more than doubled the odds of readmission, compared with alcoholic liver disease (odds ratio, 2.37; 95% confidence interval, 1.44-3.91; P = .001). Transplantees with HCV might benefit from closer outpatient follow-up to detect worsening liver function, diagnostic algorithms to help prevent unnecessary readmissions, and associated nosocomial infections, and pre- and posttransplant direct-acting antiviral therapy, “although the impact [of direct-acting antiviral] therapy on readmissions] is unknown at this time,” the investigators said.
The multivariable analysis also linked readmissions to longer hospital stays (OR, 1.03; P = .04), while age and male sex were protective factors, the investigators said. “Although speculative, it is possible that these factors may be protective due to differences in social support structures upon discharge,” they wrote, noting that women are more likely than men to outlive their partners and thus to live alone in later life.
Readmission within 90 days was associated with a significantly lower rate of survival at 5 years (75% vs. 88% for patients who were not readmitted; P = .008). But only one patient died during the initial readmission, “suggesting that when readmission does occur, it may be an opportunity to intervene,” the researchers said. Strategies include earlier extubation and removal of indwelling catheters, decreasing levels of immunosuppression, lowering treatment thresholds, and shifting patients with laboratory abnormalities to the outpatient setting, they noted. “At our center a process has been initiated in which the inpatient transplant attending surgeon directly passes off discharged patients to the outpatient team,” the investigators wrote. “Additionally, for patients discharged to an acute rehabilitation facility, a specific transplant physician point of contact is provided to the team at the rehab center in case any questions or issues arise [after] discharge. Although these strategies are a reasonable starting point, follow-up studies remain necessary in order to evaluate the impact of these interventions in this patient cohort.”
The researchers reported no funding sources and had no relevant financial disclosures.
FROM HPB
Key clinical point: Nearly half of liver recipients at Massachusetts General Hospital were readmitted within 90 days.
Major finding: A total of 46% of patients were readmitted, with hepatitis C virus infection being the strongest predictor of readmission (odds ratio, 2.37, compared with alcoholic liver disease).
Data source: A single-center retrospective study of 325 liver transplant patients between 2005 and 2015.
Disclosures: The researchers reported no funding sources and had no relevant financial disclosures.
Benefits of early endovascular thrombectomy outlined in five trials
For patients with large-vessel ischemic stroke, endovascular thrombectomy produces better functional outcomes at 90 days than does optimal medical therapy, as long as the procedure is started within 7.3 hours of symptom onset, according to a report published online Sept. 27 in JAMA.
The benefit of thrombectomy was greatest when the procedure was begun under 2 hours from symptom onset, and it became nonsignificant after 7 hours and 18 minutes elapsed. This emphasizes “the importance of programs to enhance patient awareness, out-of-hospital care, and in-hospital management to shorten symptom onset-to-treatment times,” wrote Jeffrey L. Saver, MD, of the University of California, Los Angeles, and his associates.
Five major randomized trials have demonstrated the benefit of second-generation endovascular recanalization therapies over medical therapy in this patient population, but uncertainties persist regarding the timing of the intervention. For example, practice guidelines in the United States recommend thrombectomy until 6 hours after symptom onset, but the Food and Drug Administration allows thrombectomy devices to be used up to 8 hours after symptom onset and Canadian guidelines recommend the procedure for selected patients up to 12 hours after symptom onset.
The investigators for the five trials formed the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration to pool their individual patient data and perform a meta-analysis to clarify the issue of timing. They assessed patients’ functional independence at 90 days using the modified Rankin Score (mRS). The study participants included 634 patients who had been randomly assigned to endovascular thrombectomy and 653 randomly assigned to medical therapy.
The intervention correlated with a substantially lower degree of patient disability at 90 days than did medical therapy: the mean mRS was 2.9 in the thrombectomy group and 3.6 in the medical therapy group. In addition, increasing delays in treatment were associated with higher levels of residual disability in the thrombectomy group but not in the medical therapy group, the investigators reported.
“Based on the current study, and assuming the findings are generalizable to the population of patients with acute ischemic stroke due to large-vessel occlusion, among every 1,000 patients achieving substantial endovascular reperfusion, for every 15-minute faster ED door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence (mRS 0-2),” Dr. Saver and his associates wrote (JAMA. 2016;316[12]:1279-88).
These findings reinforce current recommendations to attempt endovascular thrombectomy when the procedure can be initiated within 6 hours of symptom onset, and they also “provide evidence that potentially supports strengthening of the recommendation for treatment from 6 through 7.3 hours after symptom onset,” they added.
No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
Earlier thrombectomy has such a profound effect on stroke patients’ outcomes that substantial changes in the current medical system are warranted to shorten these times even further. In this study, median time from symptom onset to randomization was approximately 3 hours, median time to arterial puncture was approximately 4 hours, and median time to reperfusion was nearly 5 hours.
Reducing the number of patients who are transferred from community hospitals to facilities with stroke centers would shorten door-to-reperfusion time a great deal. It is estimated that direct transport to stroke centers would allow endovascular thrombectomy for an additional 13% of stroke patients. Telemedicine, mobile stroke units, and out-of-hospital administration of tissue plasminogen activator are other possibilities that should be investigated.
Steven Warach, MD, PhD, and S. Claiborne Johnston, MD, PhD, are with the University of Texas at Austin. They reported having no relevant financial disclosures. Dr. Warach and Dr. Johnston made these remarks in an editorial (JAMA. 2016;316[12]:1265-6) accompanying Dr. Saver’s report.
Earlier thrombectomy has such a profound effect on stroke patients’ outcomes that substantial changes in the current medical system are warranted to shorten these times even further. In this study, median time from symptom onset to randomization was approximately 3 hours, median time to arterial puncture was approximately 4 hours, and median time to reperfusion was nearly 5 hours.
Reducing the number of patients who are transferred from community hospitals to facilities with stroke centers would shorten door-to-reperfusion time a great deal. It is estimated that direct transport to stroke centers would allow endovascular thrombectomy for an additional 13% of stroke patients. Telemedicine, mobile stroke units, and out-of-hospital administration of tissue plasminogen activator are other possibilities that should be investigated.
Steven Warach, MD, PhD, and S. Claiborne Johnston, MD, PhD, are with the University of Texas at Austin. They reported having no relevant financial disclosures. Dr. Warach and Dr. Johnston made these remarks in an editorial (JAMA. 2016;316[12]:1265-6) accompanying Dr. Saver’s report.
Earlier thrombectomy has such a profound effect on stroke patients’ outcomes that substantial changes in the current medical system are warranted to shorten these times even further. In this study, median time from symptom onset to randomization was approximately 3 hours, median time to arterial puncture was approximately 4 hours, and median time to reperfusion was nearly 5 hours.
Reducing the number of patients who are transferred from community hospitals to facilities with stroke centers would shorten door-to-reperfusion time a great deal. It is estimated that direct transport to stroke centers would allow endovascular thrombectomy for an additional 13% of stroke patients. Telemedicine, mobile stroke units, and out-of-hospital administration of tissue plasminogen activator are other possibilities that should be investigated.
Steven Warach, MD, PhD, and S. Claiborne Johnston, MD, PhD, are with the University of Texas at Austin. They reported having no relevant financial disclosures. Dr. Warach and Dr. Johnston made these remarks in an editorial (JAMA. 2016;316[12]:1265-6) accompanying Dr. Saver’s report.
For patients with large-vessel ischemic stroke, endovascular thrombectomy produces better functional outcomes at 90 days than does optimal medical therapy, as long as the procedure is started within 7.3 hours of symptom onset, according to a report published online Sept. 27 in JAMA.
The benefit of thrombectomy was greatest when the procedure was begun under 2 hours from symptom onset, and it became nonsignificant after 7 hours and 18 minutes elapsed. This emphasizes “the importance of programs to enhance patient awareness, out-of-hospital care, and in-hospital management to shorten symptom onset-to-treatment times,” wrote Jeffrey L. Saver, MD, of the University of California, Los Angeles, and his associates.
Five major randomized trials have demonstrated the benefit of second-generation endovascular recanalization therapies over medical therapy in this patient population, but uncertainties persist regarding the timing of the intervention. For example, practice guidelines in the United States recommend thrombectomy until 6 hours after symptom onset, but the Food and Drug Administration allows thrombectomy devices to be used up to 8 hours after symptom onset and Canadian guidelines recommend the procedure for selected patients up to 12 hours after symptom onset.
The investigators for the five trials formed the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration to pool their individual patient data and perform a meta-analysis to clarify the issue of timing. They assessed patients’ functional independence at 90 days using the modified Rankin Score (mRS). The study participants included 634 patients who had been randomly assigned to endovascular thrombectomy and 653 randomly assigned to medical therapy.
The intervention correlated with a substantially lower degree of patient disability at 90 days than did medical therapy: the mean mRS was 2.9 in the thrombectomy group and 3.6 in the medical therapy group. In addition, increasing delays in treatment were associated with higher levels of residual disability in the thrombectomy group but not in the medical therapy group, the investigators reported.
“Based on the current study, and assuming the findings are generalizable to the population of patients with acute ischemic stroke due to large-vessel occlusion, among every 1,000 patients achieving substantial endovascular reperfusion, for every 15-minute faster ED door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence (mRS 0-2),” Dr. Saver and his associates wrote (JAMA. 2016;316[12]:1279-88).
These findings reinforce current recommendations to attempt endovascular thrombectomy when the procedure can be initiated within 6 hours of symptom onset, and they also “provide evidence that potentially supports strengthening of the recommendation for treatment from 6 through 7.3 hours after symptom onset,” they added.
No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
For patients with large-vessel ischemic stroke, endovascular thrombectomy produces better functional outcomes at 90 days than does optimal medical therapy, as long as the procedure is started within 7.3 hours of symptom onset, according to a report published online Sept. 27 in JAMA.
The benefit of thrombectomy was greatest when the procedure was begun under 2 hours from symptom onset, and it became nonsignificant after 7 hours and 18 minutes elapsed. This emphasizes “the importance of programs to enhance patient awareness, out-of-hospital care, and in-hospital management to shorten symptom onset-to-treatment times,” wrote Jeffrey L. Saver, MD, of the University of California, Los Angeles, and his associates.
Five major randomized trials have demonstrated the benefit of second-generation endovascular recanalization therapies over medical therapy in this patient population, but uncertainties persist regarding the timing of the intervention. For example, practice guidelines in the United States recommend thrombectomy until 6 hours after symptom onset, but the Food and Drug Administration allows thrombectomy devices to be used up to 8 hours after symptom onset and Canadian guidelines recommend the procedure for selected patients up to 12 hours after symptom onset.
The investigators for the five trials formed the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration to pool their individual patient data and perform a meta-analysis to clarify the issue of timing. They assessed patients’ functional independence at 90 days using the modified Rankin Score (mRS). The study participants included 634 patients who had been randomly assigned to endovascular thrombectomy and 653 randomly assigned to medical therapy.
The intervention correlated with a substantially lower degree of patient disability at 90 days than did medical therapy: the mean mRS was 2.9 in the thrombectomy group and 3.6 in the medical therapy group. In addition, increasing delays in treatment were associated with higher levels of residual disability in the thrombectomy group but not in the medical therapy group, the investigators reported.
“Based on the current study, and assuming the findings are generalizable to the population of patients with acute ischemic stroke due to large-vessel occlusion, among every 1,000 patients achieving substantial endovascular reperfusion, for every 15-minute faster ED door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence (mRS 0-2),” Dr. Saver and his associates wrote (JAMA. 2016;316[12]:1279-88).
These findings reinforce current recommendations to attempt endovascular thrombectomy when the procedure can be initiated within 6 hours of symptom onset, and they also “provide evidence that potentially supports strengthening of the recommendation for treatment from 6 through 7.3 hours after symptom onset,” they added.
No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
FROM JAMA
Key clinical point: Endovascular thrombectomy started within 7.3 hours of symptom onset for large-vessel ischemic stroke produces better outcomes than does optimal medical therapy.
Major finding: For every 15-minute shorter door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence.
Data source: A meta-analysis of pooled data from five randomized clinical trials involving 1,287 patients.
Disclosures: No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
Less pain, quicker discharge with post-TORS dexamethasone
SEATTLE – A longer course of dexamethasone was a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery in a randomized trial from the Oregon Health and Science University, Portland.
Thirty-five subjects were randomized to the standard 10-mg intraoperative dexamethasone dose plus 8 mg every 8 hours for up to 4 days; 33 others were randomized to the intraoperative dose plus placebo. All the subjects had transoral robotic surgery (TORS) resection for T1 or T2 oropharyngeal squamous cell carcinoma, either partial pharyngectomy/radical tonsillectomy, base of tongue resection, or both.
The dexamethasone group had significantly less pain on postop day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up. “They were much more likely to be on a full-soft diet, while the placebo group was mostly still on purees, and just starting into soft foods,” said lead investigator Daniel Clayburgh, MD, a head and neck cancer specialist at the university.
Otherwise, however, the extra dexamethasone wasn’t much help; pain scores were the same in both groups for the first couple days after surgery and at follow-up, and both groups used the same amount of post-op opioids. Other than food tolerance, dysphagia metrics were pretty much the same.
“I was actually anticipating a little bit more of a benefit, but there are potentially some benefits to extended corticosteroid courses after TORS. It’s safe, and well tolerated so long as you screen out diabetes and other problems with hyperglycemia,” as was done in the study, he said. “It does decrease post-op length of stay and may provide a modest decrease in post-op pain, and may slightly accelerate advancement of dietary consistency,” Dr. Clayburgh said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
Although he and his colleagues are mulling over what to do with the findings in light of other initiatives to reduce post-TORS pain, they are now likely to extend dexamethasone courses when significant post-op pain seems likely, and doing so is not otherwise contraindicated, he said.
Intraoperative corticosteroids are now routine for TORS, based on the strength of benefit in the tonsillectomy literature. The team decided to try an extended course because “being rather simple minded surgeons, we thought that if one dose is good, more should be better,” Dr. Clayburgh said.
The dexamethasone group was slightly younger than the placebo group (56 vs. 61 years) but otherwise similar; most were men. In addition to patients with hyperglycemia issues, those with confounders for post-op speech and swallowing recovery were among those excluded from the trial. Subjects required nasogastric feeding tubes for a median of 6.5 days postoperatively, lost a mean of 10 pounds in the first 2 post-op weeks, and were hospitalized for a mean of about 5 days. Dexamethasone was delivered orally or by nasogastric tube.
There was no external funding for the study, and Dr. Clayburgh had no relevant financial disclosures.
SEATTLE – A longer course of dexamethasone was a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery in a randomized trial from the Oregon Health and Science University, Portland.
Thirty-five subjects were randomized to the standard 10-mg intraoperative dexamethasone dose plus 8 mg every 8 hours for up to 4 days; 33 others were randomized to the intraoperative dose plus placebo. All the subjects had transoral robotic surgery (TORS) resection for T1 or T2 oropharyngeal squamous cell carcinoma, either partial pharyngectomy/radical tonsillectomy, base of tongue resection, or both.
The dexamethasone group had significantly less pain on postop day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up. “They were much more likely to be on a full-soft diet, while the placebo group was mostly still on purees, and just starting into soft foods,” said lead investigator Daniel Clayburgh, MD, a head and neck cancer specialist at the university.
Otherwise, however, the extra dexamethasone wasn’t much help; pain scores were the same in both groups for the first couple days after surgery and at follow-up, and both groups used the same amount of post-op opioids. Other than food tolerance, dysphagia metrics were pretty much the same.
“I was actually anticipating a little bit more of a benefit, but there are potentially some benefits to extended corticosteroid courses after TORS. It’s safe, and well tolerated so long as you screen out diabetes and other problems with hyperglycemia,” as was done in the study, he said. “It does decrease post-op length of stay and may provide a modest decrease in post-op pain, and may slightly accelerate advancement of dietary consistency,” Dr. Clayburgh said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
Although he and his colleagues are mulling over what to do with the findings in light of other initiatives to reduce post-TORS pain, they are now likely to extend dexamethasone courses when significant post-op pain seems likely, and doing so is not otherwise contraindicated, he said.
Intraoperative corticosteroids are now routine for TORS, based on the strength of benefit in the tonsillectomy literature. The team decided to try an extended course because “being rather simple minded surgeons, we thought that if one dose is good, more should be better,” Dr. Clayburgh said.
The dexamethasone group was slightly younger than the placebo group (56 vs. 61 years) but otherwise similar; most were men. In addition to patients with hyperglycemia issues, those with confounders for post-op speech and swallowing recovery were among those excluded from the trial. Subjects required nasogastric feeding tubes for a median of 6.5 days postoperatively, lost a mean of 10 pounds in the first 2 post-op weeks, and were hospitalized for a mean of about 5 days. Dexamethasone was delivered orally or by nasogastric tube.
There was no external funding for the study, and Dr. Clayburgh had no relevant financial disclosures.
SEATTLE – A longer course of dexamethasone was a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery in a randomized trial from the Oregon Health and Science University, Portland.
Thirty-five subjects were randomized to the standard 10-mg intraoperative dexamethasone dose plus 8 mg every 8 hours for up to 4 days; 33 others were randomized to the intraoperative dose plus placebo. All the subjects had transoral robotic surgery (TORS) resection for T1 or T2 oropharyngeal squamous cell carcinoma, either partial pharyngectomy/radical tonsillectomy, base of tongue resection, or both.
The dexamethasone group had significantly less pain on postop day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up. “They were much more likely to be on a full-soft diet, while the placebo group was mostly still on purees, and just starting into soft foods,” said lead investigator Daniel Clayburgh, MD, a head and neck cancer specialist at the university.
Otherwise, however, the extra dexamethasone wasn’t much help; pain scores were the same in both groups for the first couple days after surgery and at follow-up, and both groups used the same amount of post-op opioids. Other than food tolerance, dysphagia metrics were pretty much the same.
“I was actually anticipating a little bit more of a benefit, but there are potentially some benefits to extended corticosteroid courses after TORS. It’s safe, and well tolerated so long as you screen out diabetes and other problems with hyperglycemia,” as was done in the study, he said. “It does decrease post-op length of stay and may provide a modest decrease in post-op pain, and may slightly accelerate advancement of dietary consistency,” Dr. Clayburgh said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
Although he and his colleagues are mulling over what to do with the findings in light of other initiatives to reduce post-TORS pain, they are now likely to extend dexamethasone courses when significant post-op pain seems likely, and doing so is not otherwise contraindicated, he said.
Intraoperative corticosteroids are now routine for TORS, based on the strength of benefit in the tonsillectomy literature. The team decided to try an extended course because “being rather simple minded surgeons, we thought that if one dose is good, more should be better,” Dr. Clayburgh said.
The dexamethasone group was slightly younger than the placebo group (56 vs. 61 years) but otherwise similar; most were men. In addition to patients with hyperglycemia issues, those with confounders for post-op speech and swallowing recovery were among those excluded from the trial. Subjects required nasogastric feeding tubes for a median of 6.5 days postoperatively, lost a mean of 10 pounds in the first 2 post-op weeks, and were hospitalized for a mean of about 5 days. Dexamethasone was delivered orally or by nasogastric tube.
There was no external funding for the study, and Dr. Clayburgh had no relevant financial disclosures.
AT AHNS 2016
Key clinical point: A longer course of dexamethasone is a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery.
Major finding: The dexamethasone group had significantly less pain on post-op day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up.
Data source: A randomized trial of 68 TORS patients.
Disclosures: There was no external funding for the study, and the lead investigator had no relevant financial disclosures.
Guideline recommends optimal periop management of geriatric patients
SAN DIEGO – As the number of surgery patients over the age of 65 continues to burgeon, clinicians have a resource to help them provide optimal perioperative care to this patient population.
At the American College of Surgeons/National Surgical Quality Improvement Program National Conference, Ronnie A. Rosenthal, MD, discussed highlights from “Optimal Perioperative Management of the Geriatric Patient: A Best Practice Guideline from the ACS NSQIP/American Geriatrics Society,” which was published in January 2016.
Work on the guideline began in 2013, when a 28-member multidisciplinary panel began to conduct a structured search of Medline to identify systematic reviews, meta-analyses, practice guidelines, and clinical trials on the topic. The panel included experts from ACS, the ACS Geriatric Surgery Task Force, the American Society of Anesthesiologists, the American Geriatrics Society, and the AGS’ Geriatrics for Specialists Initiative. The 61-page document is divided into four categories: immediate preoperative period, intraoperative management, postoperative care, and care transitions.
Working with patients on goals
As noted in the guideline, a primary goal of the immediate preoperative period is to discuss with the patient his or her goals and expectations. Patient expectations are influenced by their treatment preferences. In fact, researchers have found that older patients are less likely to want a treatment – even if it results in cure – that may result in severe functional or cognitive impairment. For patients with existing advanced directives, organizations representing nurses, anesthesiologists, and surgeons all agree that there must be a “reconsideration” of these directives prior to surgery. A discussion that includes the new risks of the procedure must be conducted to ensure that the approach to potential life-threatening problems is consistent with the patient’s values.
Preoperative management of medications
Another recommendation for the preoperative period is to ensure that older patients have shorter fasts, have appropriate prophylactic antibiotics, continue medications with withdrawal potential, and discontinue medications that are not essential. The latter point is based on the Beers Criteria, a list of medications that are inappropriate or potentially inappropriate to use in older adults (J Am Geriatr Soc. 2015 Nov;63[11]:2227-46). “You want to discontinue as many inappropriate medications as possible, because one of the main side effects of their use is delirium, and you want to avoid that,” said Dr. Rosenthal, professor of surgery at the Yale University, New Haven, Conn., and one of the guideline authors.
Anesthesia and pain management
Intraoperative management strategies contained in the guideline include establishing an anesthetic approach and a perioperative analgesia pain plan, preventing postoperative nausea and vomiting, assessing patient safety in the OR, preventing predictable complications, and optimizing fluid management. Physiologic effects of anesthesia medications include changes in systemic vascular resistance, cardiac preload, baroreceptor responses, lung mechanics, oxygen diffusion, neurotransmitter function, and end-organ blood flow, among others. “These physiologic changes of aging have significant clinical implications,” Dr. Rosenthal noted. “These are variable among individuals and variable among organ systems, and it’s important that we pay attention to that. Because of this variability, there is insufficient evidence to recommend a single ‘best’ anesthetic plan for all older adults.”
The guideline recommends that each patient have an individualized pain plan that consists of a directed pain history and physical exam and is appropriately titrated for increased sensitivity. “It should include a prophylactic bowel regimen for anybody who’s on an opioid in particular,” she said. “We should avoid inappropriate medications like benzodiazepines, and we should use a multimodal therapy with opioid-sparing and regional techniques.”
Pulmonary considerations for anesthesia include susceptibility to hypocarbia and hypoxemia, and susceptibility to residual anesthetic effects. “Because of physiologic changes, the anesthesia medications aren’t metabolized in the same way,” she said. “Older people may have lower drug requirements and may not recover as quickly from the effects of these drugs. This can lead to respiratory compromise and also can increase the risk of aspiration.” Strategies to prevent pulmonary complications include using regional anesthesia when possible and avoiding the use of intermediate- and long-acting neuromuscular blocking agents. Dr. Rosenthal said that there is insufficient evidence in the current medical literature to recommend a single “best” intraoperative fluid management plan for all older adults. “Part of the reason it’s so difficult is because of the cardiac physiologic changes [with aging],” she explained. “Older people are susceptible to volume overload. On the other hand, they also may have an exaggerated decline in cardiac function if you give them too little fluid and they have insufficient preload. It’s a very fine line and that’s why it’s hard to recommend a single best strategy.”
Be alert to postoperative delirium
Postoperatively, the guideline recommends that care plans include controlling perioperative acute pain; addressing delirium/cognitive issues; preventing functional decline, falls, pressure ulcers, and urinary track infections; maintaining adequate nutrition; and avoiding pulmonary complications. Dr. Rosenthal underscored the importance of using the four-question Short Confusion Assessment Method (Short CAM) to assess for delirium. “For it to be delirium, there has to be evidence of acute change in mental status from baseline; it has to be acute and fluctuating, and characterized by inattention,” she said. “The patient also has to have either disorganized thinking or an altered level of consciousness.”
Many of the precipitating factors of delirium can be prevented by treating pain, watching medications, preventing dehydration and undernutrition, removing catheters and other devices when possible, preventing constipation, and using minimally invasive techniques to reduce the physiologic stress of surgery. “Sometimes symptoms of delirium are a warning sign that something else is going on, such as an infection, hypoxemia, electrolyte imbalance, neurological events, and major organ dysfunction,” she said. The first-line therapy for treating delirium as recommended in the guideline is a multicomponent intervention that focuses on frequent reorientation with voice, calendars, and clocks; eliminating use of restraints; having familiar objects in the room; and ensuring the use of assistive devices. The second-line therapy is antipsychotic medications at the lowest effective dose. “The mantra is start low and go slow,” she said.
Preventing postoperative functional decline
Another postoperative strategy in the guideline involves targeted fall prevention, such as having an assistive device at the bedside if used as an outpatient and prescribing early physical therapy focused on maintaining mobility as the primary event. “Every day an older patient is immobilized it takes at least 3 days to regain the lost function,” Dr. Rosenthal said. “And for older surgical patients, one in four experiences a significant decline in function by hospital discharge and 60% experience some loss of independence.” (The latter statistic comes from a study published online July 13, 2016, in JAMA Surgery: doi:10.1001/jamasurg.2016.1689.) Interventions for preventing functional decline include promotion of family participation in care, early mobilization, early physical/occupational therapy referral, geriatric consultation, comprehensive discharge planning, and nutritional support. She pointed out that an estimated 40% of community-dwelling elders and two-thirds of nursing home residents are either malnourished or “at risk” of malnutrition.
Transition of care
The final category in the guideline, transition of care, recommends an assessment of social support/home health needs, complete medication review, predischarge geriatric assessment, formal written discharge instructions, and communication with the patient’s primary care physician. “Common models of transitional care involve good coordination with the primary care physician,” she said. “There’s good data to show that people who see their primary care physician within 2 weeks of discharge do better in terms of readmission.”
Dr. Rosenthal reported having no financial disclosures.
SAN DIEGO – As the number of surgery patients over the age of 65 continues to burgeon, clinicians have a resource to help them provide optimal perioperative care to this patient population.
At the American College of Surgeons/National Surgical Quality Improvement Program National Conference, Ronnie A. Rosenthal, MD, discussed highlights from “Optimal Perioperative Management of the Geriatric Patient: A Best Practice Guideline from the ACS NSQIP/American Geriatrics Society,” which was published in January 2016.
Work on the guideline began in 2013, when a 28-member multidisciplinary panel began to conduct a structured search of Medline to identify systematic reviews, meta-analyses, practice guidelines, and clinical trials on the topic. The panel included experts from ACS, the ACS Geriatric Surgery Task Force, the American Society of Anesthesiologists, the American Geriatrics Society, and the AGS’ Geriatrics for Specialists Initiative. The 61-page document is divided into four categories: immediate preoperative period, intraoperative management, postoperative care, and care transitions.
Working with patients on goals
As noted in the guideline, a primary goal of the immediate preoperative period is to discuss with the patient his or her goals and expectations. Patient expectations are influenced by their treatment preferences. In fact, researchers have found that older patients are less likely to want a treatment – even if it results in cure – that may result in severe functional or cognitive impairment. For patients with existing advanced directives, organizations representing nurses, anesthesiologists, and surgeons all agree that there must be a “reconsideration” of these directives prior to surgery. A discussion that includes the new risks of the procedure must be conducted to ensure that the approach to potential life-threatening problems is consistent with the patient’s values.
Preoperative management of medications
Another recommendation for the preoperative period is to ensure that older patients have shorter fasts, have appropriate prophylactic antibiotics, continue medications with withdrawal potential, and discontinue medications that are not essential. The latter point is based on the Beers Criteria, a list of medications that are inappropriate or potentially inappropriate to use in older adults (J Am Geriatr Soc. 2015 Nov;63[11]:2227-46). “You want to discontinue as many inappropriate medications as possible, because one of the main side effects of their use is delirium, and you want to avoid that,” said Dr. Rosenthal, professor of surgery at the Yale University, New Haven, Conn., and one of the guideline authors.
Anesthesia and pain management
Intraoperative management strategies contained in the guideline include establishing an anesthetic approach and a perioperative analgesia pain plan, preventing postoperative nausea and vomiting, assessing patient safety in the OR, preventing predictable complications, and optimizing fluid management. Physiologic effects of anesthesia medications include changes in systemic vascular resistance, cardiac preload, baroreceptor responses, lung mechanics, oxygen diffusion, neurotransmitter function, and end-organ blood flow, among others. “These physiologic changes of aging have significant clinical implications,” Dr. Rosenthal noted. “These are variable among individuals and variable among organ systems, and it’s important that we pay attention to that. Because of this variability, there is insufficient evidence to recommend a single ‘best’ anesthetic plan for all older adults.”
The guideline recommends that each patient have an individualized pain plan that consists of a directed pain history and physical exam and is appropriately titrated for increased sensitivity. “It should include a prophylactic bowel regimen for anybody who’s on an opioid in particular,” she said. “We should avoid inappropriate medications like benzodiazepines, and we should use a multimodal therapy with opioid-sparing and regional techniques.”
Pulmonary considerations for anesthesia include susceptibility to hypocarbia and hypoxemia, and susceptibility to residual anesthetic effects. “Because of physiologic changes, the anesthesia medications aren’t metabolized in the same way,” she said. “Older people may have lower drug requirements and may not recover as quickly from the effects of these drugs. This can lead to respiratory compromise and also can increase the risk of aspiration.” Strategies to prevent pulmonary complications include using regional anesthesia when possible and avoiding the use of intermediate- and long-acting neuromuscular blocking agents. Dr. Rosenthal said that there is insufficient evidence in the current medical literature to recommend a single “best” intraoperative fluid management plan for all older adults. “Part of the reason it’s so difficult is because of the cardiac physiologic changes [with aging],” she explained. “Older people are susceptible to volume overload. On the other hand, they also may have an exaggerated decline in cardiac function if you give them too little fluid and they have insufficient preload. It’s a very fine line and that’s why it’s hard to recommend a single best strategy.”
Be alert to postoperative delirium
Postoperatively, the guideline recommends that care plans include controlling perioperative acute pain; addressing delirium/cognitive issues; preventing functional decline, falls, pressure ulcers, and urinary track infections; maintaining adequate nutrition; and avoiding pulmonary complications. Dr. Rosenthal underscored the importance of using the four-question Short Confusion Assessment Method (Short CAM) to assess for delirium. “For it to be delirium, there has to be evidence of acute change in mental status from baseline; it has to be acute and fluctuating, and characterized by inattention,” she said. “The patient also has to have either disorganized thinking or an altered level of consciousness.”
Many of the precipitating factors of delirium can be prevented by treating pain, watching medications, preventing dehydration and undernutrition, removing catheters and other devices when possible, preventing constipation, and using minimally invasive techniques to reduce the physiologic stress of surgery. “Sometimes symptoms of delirium are a warning sign that something else is going on, such as an infection, hypoxemia, electrolyte imbalance, neurological events, and major organ dysfunction,” she said. The first-line therapy for treating delirium as recommended in the guideline is a multicomponent intervention that focuses on frequent reorientation with voice, calendars, and clocks; eliminating use of restraints; having familiar objects in the room; and ensuring the use of assistive devices. The second-line therapy is antipsychotic medications at the lowest effective dose. “The mantra is start low and go slow,” she said.
Preventing postoperative functional decline
Another postoperative strategy in the guideline involves targeted fall prevention, such as having an assistive device at the bedside if used as an outpatient and prescribing early physical therapy focused on maintaining mobility as the primary event. “Every day an older patient is immobilized it takes at least 3 days to regain the lost function,” Dr. Rosenthal said. “And for older surgical patients, one in four experiences a significant decline in function by hospital discharge and 60% experience some loss of independence.” (The latter statistic comes from a study published online July 13, 2016, in JAMA Surgery: doi:10.1001/jamasurg.2016.1689.) Interventions for preventing functional decline include promotion of family participation in care, early mobilization, early physical/occupational therapy referral, geriatric consultation, comprehensive discharge planning, and nutritional support. She pointed out that an estimated 40% of community-dwelling elders and two-thirds of nursing home residents are either malnourished or “at risk” of malnutrition.
Transition of care
The final category in the guideline, transition of care, recommends an assessment of social support/home health needs, complete medication review, predischarge geriatric assessment, formal written discharge instructions, and communication with the patient’s primary care physician. “Common models of transitional care involve good coordination with the primary care physician,” she said. “There’s good data to show that people who see their primary care physician within 2 weeks of discharge do better in terms of readmission.”
Dr. Rosenthal reported having no financial disclosures.
SAN DIEGO – As the number of surgery patients over the age of 65 continues to burgeon, clinicians have a resource to help them provide optimal perioperative care to this patient population.
At the American College of Surgeons/National Surgical Quality Improvement Program National Conference, Ronnie A. Rosenthal, MD, discussed highlights from “Optimal Perioperative Management of the Geriatric Patient: A Best Practice Guideline from the ACS NSQIP/American Geriatrics Society,” which was published in January 2016.
Work on the guideline began in 2013, when a 28-member multidisciplinary panel began to conduct a structured search of Medline to identify systematic reviews, meta-analyses, practice guidelines, and clinical trials on the topic. The panel included experts from ACS, the ACS Geriatric Surgery Task Force, the American Society of Anesthesiologists, the American Geriatrics Society, and the AGS’ Geriatrics for Specialists Initiative. The 61-page document is divided into four categories: immediate preoperative period, intraoperative management, postoperative care, and care transitions.
Working with patients on goals
As noted in the guideline, a primary goal of the immediate preoperative period is to discuss with the patient his or her goals and expectations. Patient expectations are influenced by their treatment preferences. In fact, researchers have found that older patients are less likely to want a treatment – even if it results in cure – that may result in severe functional or cognitive impairment. For patients with existing advanced directives, organizations representing nurses, anesthesiologists, and surgeons all agree that there must be a “reconsideration” of these directives prior to surgery. A discussion that includes the new risks of the procedure must be conducted to ensure that the approach to potential life-threatening problems is consistent with the patient’s values.
Preoperative management of medications
Another recommendation for the preoperative period is to ensure that older patients have shorter fasts, have appropriate prophylactic antibiotics, continue medications with withdrawal potential, and discontinue medications that are not essential. The latter point is based on the Beers Criteria, a list of medications that are inappropriate or potentially inappropriate to use in older adults (J Am Geriatr Soc. 2015 Nov;63[11]:2227-46). “You want to discontinue as many inappropriate medications as possible, because one of the main side effects of their use is delirium, and you want to avoid that,” said Dr. Rosenthal, professor of surgery at the Yale University, New Haven, Conn., and one of the guideline authors.
Anesthesia and pain management
Intraoperative management strategies contained in the guideline include establishing an anesthetic approach and a perioperative analgesia pain plan, preventing postoperative nausea and vomiting, assessing patient safety in the OR, preventing predictable complications, and optimizing fluid management. Physiologic effects of anesthesia medications include changes in systemic vascular resistance, cardiac preload, baroreceptor responses, lung mechanics, oxygen diffusion, neurotransmitter function, and end-organ blood flow, among others. “These physiologic changes of aging have significant clinical implications,” Dr. Rosenthal noted. “These are variable among individuals and variable among organ systems, and it’s important that we pay attention to that. Because of this variability, there is insufficient evidence to recommend a single ‘best’ anesthetic plan for all older adults.”
The guideline recommends that each patient have an individualized pain plan that consists of a directed pain history and physical exam and is appropriately titrated for increased sensitivity. “It should include a prophylactic bowel regimen for anybody who’s on an opioid in particular,” she said. “We should avoid inappropriate medications like benzodiazepines, and we should use a multimodal therapy with opioid-sparing and regional techniques.”
Pulmonary considerations for anesthesia include susceptibility to hypocarbia and hypoxemia, and susceptibility to residual anesthetic effects. “Because of physiologic changes, the anesthesia medications aren’t metabolized in the same way,” she said. “Older people may have lower drug requirements and may not recover as quickly from the effects of these drugs. This can lead to respiratory compromise and also can increase the risk of aspiration.” Strategies to prevent pulmonary complications include using regional anesthesia when possible and avoiding the use of intermediate- and long-acting neuromuscular blocking agents. Dr. Rosenthal said that there is insufficient evidence in the current medical literature to recommend a single “best” intraoperative fluid management plan for all older adults. “Part of the reason it’s so difficult is because of the cardiac physiologic changes [with aging],” she explained. “Older people are susceptible to volume overload. On the other hand, they also may have an exaggerated decline in cardiac function if you give them too little fluid and they have insufficient preload. It’s a very fine line and that’s why it’s hard to recommend a single best strategy.”
Be alert to postoperative delirium
Postoperatively, the guideline recommends that care plans include controlling perioperative acute pain; addressing delirium/cognitive issues; preventing functional decline, falls, pressure ulcers, and urinary track infections; maintaining adequate nutrition; and avoiding pulmonary complications. Dr. Rosenthal underscored the importance of using the four-question Short Confusion Assessment Method (Short CAM) to assess for delirium. “For it to be delirium, there has to be evidence of acute change in mental status from baseline; it has to be acute and fluctuating, and characterized by inattention,” she said. “The patient also has to have either disorganized thinking or an altered level of consciousness.”
Many of the precipitating factors of delirium can be prevented by treating pain, watching medications, preventing dehydration and undernutrition, removing catheters and other devices when possible, preventing constipation, and using minimally invasive techniques to reduce the physiologic stress of surgery. “Sometimes symptoms of delirium are a warning sign that something else is going on, such as an infection, hypoxemia, electrolyte imbalance, neurological events, and major organ dysfunction,” she said. The first-line therapy for treating delirium as recommended in the guideline is a multicomponent intervention that focuses on frequent reorientation with voice, calendars, and clocks; eliminating use of restraints; having familiar objects in the room; and ensuring the use of assistive devices. The second-line therapy is antipsychotic medications at the lowest effective dose. “The mantra is start low and go slow,” she said.
Preventing postoperative functional decline
Another postoperative strategy in the guideline involves targeted fall prevention, such as having an assistive device at the bedside if used as an outpatient and prescribing early physical therapy focused on maintaining mobility as the primary event. “Every day an older patient is immobilized it takes at least 3 days to regain the lost function,” Dr. Rosenthal said. “And for older surgical patients, one in four experiences a significant decline in function by hospital discharge and 60% experience some loss of independence.” (The latter statistic comes from a study published online July 13, 2016, in JAMA Surgery: doi:10.1001/jamasurg.2016.1689.) Interventions for preventing functional decline include promotion of family participation in care, early mobilization, early physical/occupational therapy referral, geriatric consultation, comprehensive discharge planning, and nutritional support. She pointed out that an estimated 40% of community-dwelling elders and two-thirds of nursing home residents are either malnourished or “at risk” of malnutrition.
Transition of care
The final category in the guideline, transition of care, recommends an assessment of social support/home health needs, complete medication review, predischarge geriatric assessment, formal written discharge instructions, and communication with the patient’s primary care physician. “Common models of transitional care involve good coordination with the primary care physician,” she said. “There’s good data to show that people who see their primary care physician within 2 weeks of discharge do better in terms of readmission.”
Dr. Rosenthal reported having no financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
CSF lactate concentration identifies postneurosurgical bacterial meningitis
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
FROM BMC INFECTIOUS DISEASES
Key clinical point: CSF lactate concentration accurately identifies bacterial meningitis that develops after neurosurgery.
Major finding: CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%.
Data source: A meta-analysis of five published studies involving 404 patients during a 15-year period.
Disclosures: This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.