User login
Improving Epistaxis Knowledge and Management Among Nursing Staff
From the University of Chicago Medical Center, Chicago, IL.
Abstract
Background: Epistaxis is a common chief complaint addressed by otolaryngologists. A review of the literature showed that there is a deficit in epistaxis education within the nursing community. Conversations with our nursing colleagues confirmed this unmet demand.
Objective: This quality improvement project aimed to increase general epistaxis knowledge, perceived comfort level managing nosebleeds, and perceived ability to stop nosebleeds among our nursing staff.
Methods: Data were collected through a survey administered before and after our intervention. The survey tested general epistaxis knowledge and assessed comfort and confidence in stopping epistaxis. Our intervention was an educational session covering pertinent epistaxis etiology and management. Quality improvement principles were used to optimize delivery of the intervention.
Results: A total of 51 nurses participated in the project. After participating in the in-service educational session, nurses answered significantly more epistaxis general knowledge questions correctly (mean [SD] difference, 2.07 [1.10] questions; 95% CI, 1.74-2.39; P < .001). There was no statistically significant difference in additional correct questions when stratified by clinical experience or clinical setting (P = .128 and P = 0.446, respectively). Nurses also reported feeling significantly more comfortable and significantly more confident in managing nosebleeds after the in-service (P = .007 and P < 0.001, respectively); 74.46% of nurses had an improvement in comfort level in managing epistaxis and 43.90% of nurses had an improvement in confidence in stopping epistaxis. After we moved the educational session from mid-shift to shift change, the nursing staff reported more satisfaction while maintaining similar improvements in knowledge and confidence.
Conclusion: We were able to significantly increase epistaxis knowledge, improve comfort levels managing epistaxis, and improve confidence in successful epistaxis management. Nurses of varying clinical experience and different clinical settings benefitted equally from our intervention.
Keywords: nosebleed; in-service; quality improvement.
Epistaxis, or nosebleed, is estimated to be the chief complaint in 1 in 200 emergency department visits in the United States.1 Additionally, it represents up to one-third of otolaryngology-related emergency room admissions.2 There is no existing literature, to our best knowledge, specifically investigating the incidence of epistaxis after a patient is admitted. Anecdotally, inpatients who develop epistaxis account for an appreciable number of consults to otolaryngology (ENT). Epistaxis is a cross-disciplinary issue, occurring in a range of clinical settings. For example, patients with epistaxis can present to the emergency department or to an outpatient primary care clinic before being referred to ENT. Additionally, inpatients on many different services can develop spontaneous epistaxis due to a variety of environmental and iatrogenic factors, such as dry air, use of nasal cannula, and initiation of anticoagulation. Based on the experience of our ENT providers and discussions with our nursing colleagues, we concluded that there was an interest in epistaxis management training among our nursing workforce.
The presence of unmet demand for epistaxis education among our nursing colleagues was supported by our literature review. A study performed in England surveyed emergency department nurses on first aid measures for management of epistaxis, including ideal head positioning, location of pressure application, and duration of pressure application.3 Overall, only 12% to 14% of the nursing staff answered all 3 questions correctly.3 Additionally, 73% to 78% of the nursing staff felt that their training in epistaxis management was inadequate, and 88% desired further training in epistaxis management.3 If generalized, this study confirms the demand for further epistaxis education among nurses.
In-services have previously been shown to be effective educational tools within the nursing community. A study in Ethiopia that evaluated pain management knowledge and attitudes before and after an in-service found a significant improvement in mean rank score of nurses’ knowledge and attitudes regarding pain management after they participated in the in-service.4 Scores on the knowledge survey improved from 41.4% before the intervention to 63.0% post intervention.4 A study in Connecticut evaluated nurses’ confidence in discussing suicidal ideation with patients and knowledge surrounding suicide precautions.5 After participating in an in-service, nurses were significantly more confident in discussing suicidal ideation with patients; application of appropriate suicide precautions also increased after the in-service.5
Our aim was for nurses to have an improvement in overall epistaxis knowledge, perceived comfort level managing nosebleeds, and perceived ability to stop nosebleeds after attending our in-service. Additionally, an overarching priority was to provide high-quality epistaxis education based on the literature and best practice guidelines.
Methods
Setting
This study was carried out at an 811-bed quaternary care center located in Chicago, Illinois. In fiscal year 2021, there were 91 643 emergency department visits and 33 805 hospital admissions. At our flagship hospital, 2658 patients were diagnosed with epistaxis during fiscal year 2021. The emergency department saw 533 patients with epistaxis, with 342 requiring admission and 191 being discharged. Separately, 566 inpatients received a diagnosis of epistaxis during their admission. The remainder of the patients with epistaxis were seen on an outpatient basis.
Data Collection
Data were collected from nurses on 5 different inpatient units. An email with information about the in-service was sent to the nurse managers of the inpatient units. These 5 units were included because the nurse managers responded to the email and facilitated delivery of the in-service. Data collection took place from August to December 2020.
Intervention
A quality improvement team composed of a resident physician champion, nurse educators, and nurse managers was formed. The physician champion was a senior otolaryngology resident who was responsible for designing and administering the pre-test, in-service, and post test. The nurse educators and nurse managers helped coordinate times for the in-service and promoted the in-service for their staff.
Our intervention was an educational in-service, a technique that is commonly used at our institution for nurse education. In-services typically involve delivering a lecture on a clinically relevant topic to a group of nurses on a unit. In developing the in-service, a top priority was to present high-quality evidence-based material. There is an abundance of information in the literature surrounding epistaxis management. The clinical practice guideline published by the American Academy of Otolaryngology lists nasal compression, application of vasoconstrictors, nasal packing, and nasal cautery as first-line treatments for the management of epistaxis.6 Nasal packing and nasal cautery tend to be perceived as interventions that require a certain level of expertise and specialized supplies. As such, these interventions are not often performed by floor nurses. In contrast, nasal compression and application of vasoconstrictors require only a few easily accessible supplies, and the risks are relatively minimal. When performing nasal compression, the clinical practice guidelines recommend firm, sustained compression to the lower third of the nose for 5 minutes or longer.6 Topical vasoconstrictors are generally underutilized in epistaxis management. In a study looking at a random sample of all US emergency department visits from 1992 to 2001, only 18% of visits used an epistaxis-related medication.2 Oxymetazoline hydrochloride is a topical vasoconstrictor that is commonly used as a nasal decongestant. However, its vasoconstrictor properties also make it a useful tool for controlling epistaxis. In a study looking at emergency department visits at the University of Texas Health Science Center, 65% of patients had resolution of nosebleed with application of oxymetazoline hydrochloride as the only intervention, with another 18% experiencing resolution of nosebleed with a combination of oxymetazoline hydrochloride and silver nitrate cautery.7 Based on review of the literature, nasal compression and application of vasoconstrictors seemed to be low-resource interventions with minimal morbidity. Therefore, management centered around nasal compression and use of topical vasoconstrictors seemed appropriate for our nursing staff.
The in-service included information about the etiology and management of epistaxis. Particular emphasis was placed on addressing and debunking common misconceptions about nosebleed management. With regards to management, our presentation focused on the use of topical vasoconstrictors and firm pressure to the lower third of the nose for at least 5 minutes. Nasal packing and nasal cautery were presented as procedures that ENT would perform. After the in-service, questions from the nurses were answered as time permitted.
Testing and Outcomes
A pre-test was administered before each in-service. The pre-test components comprised a knowledge survey and a descriptive survey. The general epistaxis knowledge questions on the pre-test included the location of blood vessels most commonly responsible for nosebleeds, the ideal positioning of a patient during a nosebleed, the appropriate location to hold pressure during a nosebleed, and the appropriate duration to hold pressure during a nosebleed. The descriptive survey portion asked nurses to rate whether they felt “very comfortable,” “comfortable,” “uncomfortable,” or “very uncomfortable” managing nosebleeds. It also asked whether nurses thought they would be able to “always,” “usually,” “rarely,” or “never” stop nosebleeds on the floor. We collected demographic information, including gender identity, years of clinical experience, and primary clinical environment.
The post test asked the same questions as the pre-test and was administered immediately after the in-service in order to assess its impact. We also established an ongoing dialogue with our nursing colleagues to obtain feedback on the sessions.
Primary outcomes of interest were the difference in general epistaxis knowledge questions answered correctly between the pre-test and the post test; the difference in comfort level in managing epistaxis before and after the in-service; and the difference in confidence to stop nosebleeds before and after the in-service. A secondary outcome was determining the audience for the in-service. Specifically, we wanted to determine whether there were different outcomes based on clinical setting or years of clinical experience. If nurses in a certain clinical environment or beyond a certain experience level did not show significant improvement from pre-test to post test, we would not target them for the in-service. Another secondary outcome was determining optimal timing for delivery of the in-service. We wanted to determine if there was a nursing preference for delivering the in-service at mid-shift vs shift change.
Analysis
Statistical calculations were performed using Stata 15 (StataCorp LLC). A P value < .05 was considered to be statistically significant. Where applicable, 95% confidence intervals (CI) were calculated. T-test was used to determine whether there was a statistically significant difference between pre-test and post-test epistaxis knowledge question scores. T-test was also used to determine whether there was a statistically significant difference in test scores between nurses receiving the in-service at mid-shift vs shift change. Pearson chi-squared tests were used to determine if there was a statistically significant difference between pre-test and post-test perceptions of epistaxis management, and to investigate outcomes between different subsets of nurses.
SQUIRE 2.0 guidelines were utilized to provide a framework for this project and to structure the manuscript.8 This study met criteria for exemption from institutional review board approval.
Results
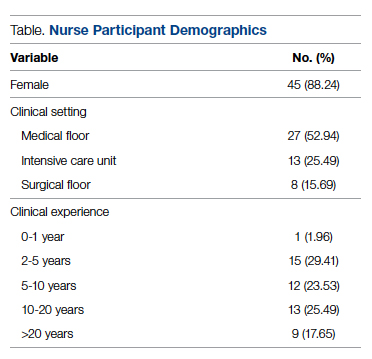
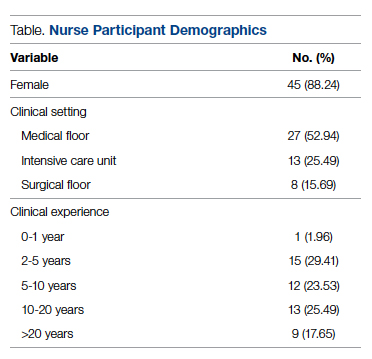
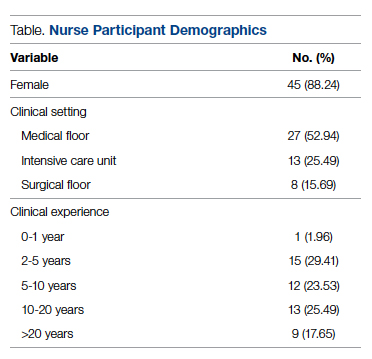
Fifty-one nurses took part in this project (Table). The majority of participants identified as female (88.24%), and just over half worked on medical floors (52.94%), with most of the remainder working in intensive care (25.49%) and surgical (15.69%) settings. There was a wide range of clinical experience, with 1.96% reporting 0 to 1 years of experience, 29.41% reporting 2 to 5 years, 23.53% reporting 5 to 10 years, 25.49% reporting 10 to 20 years, and 17.65% reporting more than 20 years.
There were unanswered questions on both the pre-test and post test. There was no consistently unanswered question. Omitted answers on the epistaxis knowledge questions were recorded as an “incorrect” answer. Omitted answers on the perception questions were considered null values and not considered in final analysis.
Primary Measures
General epistaxis knowledge (Figure, part A) improved from the pre-test, where out of 4 questions, the mean (SD) score was 1.74 (1.02) correct questions, to the post-test, where out of 4 questions, the mean score was 3.80 (0.40) correct questions. After participating in the in-service, nurses answered significantly more questions about epistaxis general knowledge correctly (mean difference, 2.07 [1.10]; 95% CI, 1.74-2.39; P < .001), and 80.43% of them got a perfect score on the epistaxis knowledge questions.
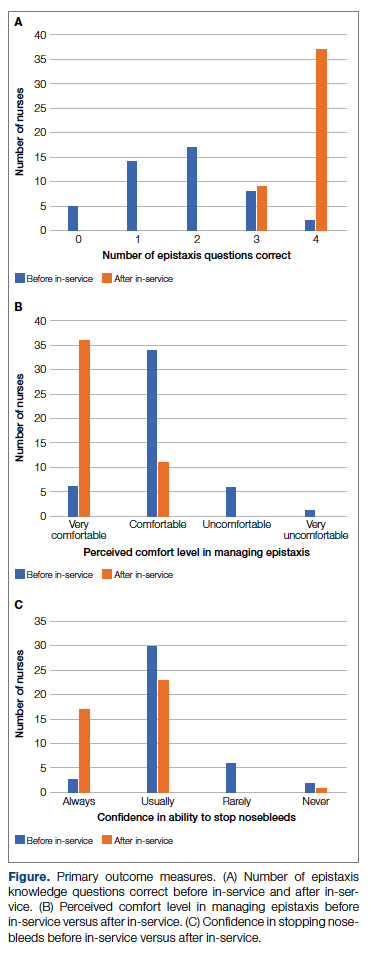
The second primary measure was the difference in comfort level in managing nosebleed. After participating in the in-service, nurses felt significantly more comfortable in managing nosebleeds (Figure, part B; P = .007), with 74.46% of nurses having an improved comfort level managing nosebleeds. Before the in-service, 12.76% of nurses felt “very comfortable” in managing nosebleeds vs more than three-quarters (76.59%) after the in-service. Of those who answered that they felt “comfortable” managing nosebleeds on the pre-test, 82.35% improved to feeling “very comfortable” in managing nosebleeds. Before the in-service, 14.89% of nurses felt “uncomfortable” or “very uncomfortable” in managing nosebleeds, and this decreased to 0 post intervention. After the in-service, 100.00% of nurses felt “comfortable” or “very comfortable” in managing nosebleeds.
After receiving the in-service, nurses felt significantly more confident in stopping nosebleeds (Figure, part C; P < .001), with 43.90% of them having an improvement in confidence in stopping epistaxis. Before the in-service, 7.31% of nurses felt that they would “always” be able to stop a nose-bleed, and this increased to 41.46% after the in-service. Of those who answered that they felt that they would “usually” be able to stop a nosebleed on the pre-test, 36.67% changed their answer to state that they would “always” be able to stop a nosebleed on the post test. Before the in-service, 19.51% of nurses felt that they would “rarely” or “never” be able to stop a nosebleed, and this decreased to 2.44% after the in-service.
Secondary Measures
All of the nurses who participated either “strongly agreed” or “agreed” that they learned something new from the in-service. However, to determine whether there was a population who would benefit most from the in-service, we stratified the data by years of clinical experience. There was no statistically significant difference in whether nurses with varying clinical experience learned something new (P = .148): 100% of nurses with 0-1 years of experience, 80.00% of nurses with 2-5 years of experience, 100% of nurses with 5-10 years of experience, 69.23% of nurses with 10-20 years of experience, and 100% of nurses with >20 years of experience “strongly agreed” that they learned something new from this in-service. There was no statistically significant difference on the post test compared to the pre-test in additional correct questions when stratified by clinical experience (P = .128). Second, when we stratified by clinical setting, we did not find a statistically significant difference in whether nurses in different clinical settings learned something new (P = .929): 88.89% of nurses in the medical setting, 87.50% of nurses in the surgical setting, and 84.62% of nurses in the intensive care setting “strongly agreed” that they learned something new from this presentation. On investigating additional questions correct on the post test compared to the pre-test, there was no statistically significant difference in additional correct questions when stratified by clinical setting (P = .446).
Optimal timing of the in-service was another important outcome. Initially, the in-service was administered at mid-shift, with 9 nurses participating at mid-shift, but our nursing colleagues gave unanimous feedback that this was a suboptimal time for delivery of an in-service. We changed the timing of the in-service to shift change; 42 nurses received the in-service at shift-change. There was no statistically significant difference in scores on the epistaxis knowledge questions between these two groups (P = .123). This indicated to us that changing the timing of the delivery resulted in similarly improved outcomes while having the added benefit of being preferred by our nursing colleagues.
Discussion
In undertaking this project, our primary aims were to improve epistaxis knowledge and perceived management in our nursing staff. Among our nursing staff, we were able to significantly increase epistaxis knowledge, improve comfort levels managing epistaxis, and improve confidence in successful epistaxis management. We also found that nurses of varying clinical experience and different clinical settings benefited equally from our intervention. Using quality improvement principles, we optimized our delivery. Our in-service focused on educating nurses to use epistaxis management techniques that were resource-efficient and low risk.
After participating in the in-service, nurses answered significantly more questions about epistaxis general knowledge correctly (Figure, part A; mean difference, 2.07 questions [1.10]; 95% CI, 1.74-2.39; P < .001), felt significantly more comfortable in managing nosebleeds (Figure, part B; P = .007), and felt significantly more confident in stopping nosebleeds (Figure, part C; P < .001). Based on these results, we successfully achieved our primary aims.
Our secondary aim was to determine the audience that would benefit the most from the in-service. All of the nurses who participated either “strongly agreed” or “agreed” that they learned something new from the in-service. There was no statistically significant difference in whether nurses of varying clinical experience learned something new (P = .148) or in additional correct questions when stratified by clinical experience (P =.128). Also, there was no statistically significant difference in whether nurses in different clinical settings learned something new (P = .929) or in additional correct questions when stratified by clinical setting (P = .446). These results indicated to us that all participants learned something new and that there was no specific target audience, but rather that all participants benefitted from our session.
Our nursing colleagues gave us feedback that the timing of the in-service during mid-shift was not ideal. It was difficult to gather nurses mid-shift due to pressing patient-care duties. Nurses also found it difficult to give their full attention at this time. Nurses, nurse educators, and nurse managers suggested that we conduct the in-service at shift change in order to capture a larger population and take advantage of time relatively free of clinical duties. Giving the in-service at a time with relatively fewer clinical responsibilities allowed for a more robust question-and-answer session. It also allowed our nursing colleagues to pay full attention to the in-service. There was no statistically significant difference in epistaxis general knowledge questions answered correctly; this indicates that the quality of the education session did not vary greatly. However, our nursing colleagues strongly preferred the in-service at shift change. By making this modification to our intervention, we were able to optimize our intervention.
The previously mentioned study in England reported that only 12% to 14% of their nursing staff got a perfect score on epistaxis knowledge questions. Prior to our study, there was no literature investigating the impact of an in-service on epistaxis knowledge. After our intervention, 80.43% of our nurses got a perfect score on the epistaxis knowledge questions. We believe that this is a fair comparison because our post-test questions were identical to the survey questions used in the previously mentioned study in England, with the addition of one question.3 Further, the findings of our study are consistent with other studies regarding the positive effect of in-service education on knowledge and attitudes surrounding clinical topics. Similar to the study in Ethiopia investigating nurses’ knowledge surrounding pain management, our study noted a significant improvement in nurses’ knowledge after participating in the in-service.4 Also, when comparing our study to the study performed in Connecticut investigating nurses’ confidence surrounding suicide precautions, we found a similar significant improvement in confidence in management after participating in the in-service.5
Given our reliance on a survey as a tool to collect information, our study was subject to nonresponse bias. For each main outcome question, there was a handful of nonresponders. While this likely indicated either overlooking a question or deferring to answer due to clinical inexperience or nonapplicable clinical role, it is possible that this may have represented a respondent who did not benefit from the in-service. Another source of possible bias is sampling bias. Attempts were made to capture a wide range of nurses at the in-service. However, if a nurse was not interested in the topic material, whether due to abundant clinical experience or disinterest, it is possible that they may not have attended. Additionally, the cohort was selected purely based on responses from nursing managers to the initial email. It is possible that nonresponding units may have benefitted differently from this in-service.
There were several limitations within our analysis. We did not collect data assessing the long-term retention of epistaxis knowledge and management techniques. It is possible that epistaxis knowledge, comfort in managing nosebleeds, and perceived confidence in stopping nosebleeds decreased back to baseline several months after the in-service. Ideally, we would have been able to collect this data to assess retention of the in-service information. Unfortunately, a significant number of nurses who initially participated in the project became lost to follow-up, making such data collection impossible. Additionally, there was no assessment of actual ability to stop nosebleeds before vs after this in-service. Perceived management of epistaxis vs actual management of epistaxis are 2 vastly different things. However, this data would have been difficult to collect, and it likely would not have been in the best interest of patients, especially before the in-service was administered. As an improvement to this project, we could have assessed how many nosebleeds nurses had seen and successfully stopped after the in-service. As previously mentioned, this was not possible due to losing a significant number of nurses to follow-up. Finally, we did not collect objective data on preference for administration of in-service at mid-shift vs shift change. We relied on subjective data from conversations with our colleagues. By collecting objective data, we could have supported this change to our intervention with data.
The primary challenge to sustainability for this intervention is nursing turnover. With each wave of departing nurses and new nursing hires, the difficulty of ensuring a consistent knowledge base and management standards within our nursing workforce became clearer. After optimizing our intervention, our solution was to provide a hospital-wide in-service, which was recorded and uploaded to an institution-wide in-service library. In this way, a nurse with the desire to learn about epistaxis management could access the material at any point in time. Another solution would have been to appoint champions for epistaxis management within each major department to deliver the epistaxis in-service to new hires and new rotators within the department. However, given the turnover witnessed in our study cohort, this may not be sustainable long term.
Conclusion
Epistaxis is a chief complaint that can present in many different clinical settings and situations. Therefore, the ability to stop epistaxis in a timely and effective fashion is valuable. Our study demonstrated that in-services can improve epistaxis knowledge and improve perceived epistaxis management. Ideally, this intervention will lead to improved patient care. Given that epistaxis is a ubiquitous issue, this study may benefit other institutions who want to improve care for patients with epistaxis.
Next steps for this intervention include utilizing in-services for epistaxis education at other institutions and collecting long-term data within our own institution. Collecting long-term data would allow us to assess the retention of epistaxis knowledge from our in-service.
Acknowledgments: The author thanks the nurse managers, nurse educators, and staff nurses involved in this project, as well as Dr. Louis Portugal for providing mentorship throughout this process and Dr. Dara Adams for assisting with statistical analysis.
Corresponding author: Avery Nelson, MD, University of Chicago Medical Center, 5841 S Maryland Ave, MC 1035, Chicago, IL 60637; [email protected]
Disclosures: None reported.
1. Pallin DJ, Chng Y-M, McKay MP, et al. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46(1):77-81. doi:10.1016/j.annemergmed.2004.12.014
2. Walker TWM, Macfarlane TV, McGarry GW. The epidemiology and chronobiology of epistaxis: An investigation of Scottish hospital admissions 1995-2004. Clin Otolaryngol. 2007;32(5):361-365. doi:10.1111/j.1749-4486.2007.01530.x
3. Hakim N, Mummadi SM, Jolly K, et al. Nurse-led epistaxis management within the emergency department. Br J Nurs. 2018;27(1):41-46. doi:10.12968/bjon.2018.27.1.41
4. Germossa GN, Sjetne IS, Hellesø R. The impact of an in-service educational program on nurses’ knowledge and attitudes regarding pain management in an Ethiopian University Hospital. Front Public Health. 2018;6:229. doi:10.3389/fpubh.2018.00229
5. Manister NN, Murray S, Burke JM, Finegan M, McKiernan ME. Effectiveness of nursing education to prevent inpatient suicide. J Contin Educ Nurs. 2017;48(9):413-419. doi:10.3928/00220124-20170816-07
6. Tunkel DE, Anne S, Payne SC, et al. Clinical practice guideline: nosebleed (epistaxis) executive summary. Otolaryngol Head Neck Surg. 2020;162(1):S1-S38. doi:10.1177/0194599819890327
7. Krempl GA, Noorily AD. Use of oxymetazoline in the management of epistaxis. Ann Otol Rhinol Laryngol. 1995;104(9 Part 1):704-706. doi:10.1177/000348949510400906
8. Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0—standards for quality improvement reporting excellence—revised publication guidelines from a detailed consensus process. J Am Coll Surg. 2016;222(3):317-323. doi:10.1016/j.jamcollsurg.2015.07.456
From the University of Chicago Medical Center, Chicago, IL.
Abstract
Background: Epistaxis is a common chief complaint addressed by otolaryngologists. A review of the literature showed that there is a deficit in epistaxis education within the nursing community. Conversations with our nursing colleagues confirmed this unmet demand.
Objective: This quality improvement project aimed to increase general epistaxis knowledge, perceived comfort level managing nosebleeds, and perceived ability to stop nosebleeds among our nursing staff.
Methods: Data were collected through a survey administered before and after our intervention. The survey tested general epistaxis knowledge and assessed comfort and confidence in stopping epistaxis. Our intervention was an educational session covering pertinent epistaxis etiology and management. Quality improvement principles were used to optimize delivery of the intervention.
Results: A total of 51 nurses participated in the project. After participating in the in-service educational session, nurses answered significantly more epistaxis general knowledge questions correctly (mean [SD] difference, 2.07 [1.10] questions; 95% CI, 1.74-2.39; P < .001). There was no statistically significant difference in additional correct questions when stratified by clinical experience or clinical setting (P = .128 and P = 0.446, respectively). Nurses also reported feeling significantly more comfortable and significantly more confident in managing nosebleeds after the in-service (P = .007 and P < 0.001, respectively); 74.46% of nurses had an improvement in comfort level in managing epistaxis and 43.90% of nurses had an improvement in confidence in stopping epistaxis. After we moved the educational session from mid-shift to shift change, the nursing staff reported more satisfaction while maintaining similar improvements in knowledge and confidence.
Conclusion: We were able to significantly increase epistaxis knowledge, improve comfort levels managing epistaxis, and improve confidence in successful epistaxis management. Nurses of varying clinical experience and different clinical settings benefitted equally from our intervention.
Keywords: nosebleed; in-service; quality improvement.
Epistaxis, or nosebleed, is estimated to be the chief complaint in 1 in 200 emergency department visits in the United States.1 Additionally, it represents up to one-third of otolaryngology-related emergency room admissions.2 There is no existing literature, to our best knowledge, specifically investigating the incidence of epistaxis after a patient is admitted. Anecdotally, inpatients who develop epistaxis account for an appreciable number of consults to otolaryngology (ENT). Epistaxis is a cross-disciplinary issue, occurring in a range of clinical settings. For example, patients with epistaxis can present to the emergency department or to an outpatient primary care clinic before being referred to ENT. Additionally, inpatients on many different services can develop spontaneous epistaxis due to a variety of environmental and iatrogenic factors, such as dry air, use of nasal cannula, and initiation of anticoagulation. Based on the experience of our ENT providers and discussions with our nursing colleagues, we concluded that there was an interest in epistaxis management training among our nursing workforce.
The presence of unmet demand for epistaxis education among our nursing colleagues was supported by our literature review. A study performed in England surveyed emergency department nurses on first aid measures for management of epistaxis, including ideal head positioning, location of pressure application, and duration of pressure application.3 Overall, only 12% to 14% of the nursing staff answered all 3 questions correctly.3 Additionally, 73% to 78% of the nursing staff felt that their training in epistaxis management was inadequate, and 88% desired further training in epistaxis management.3 If generalized, this study confirms the demand for further epistaxis education among nurses.
In-services have previously been shown to be effective educational tools within the nursing community. A study in Ethiopia that evaluated pain management knowledge and attitudes before and after an in-service found a significant improvement in mean rank score of nurses’ knowledge and attitudes regarding pain management after they participated in the in-service.4 Scores on the knowledge survey improved from 41.4% before the intervention to 63.0% post intervention.4 A study in Connecticut evaluated nurses’ confidence in discussing suicidal ideation with patients and knowledge surrounding suicide precautions.5 After participating in an in-service, nurses were significantly more confident in discussing suicidal ideation with patients; application of appropriate suicide precautions also increased after the in-service.5
Our aim was for nurses to have an improvement in overall epistaxis knowledge, perceived comfort level managing nosebleeds, and perceived ability to stop nosebleeds after attending our in-service. Additionally, an overarching priority was to provide high-quality epistaxis education based on the literature and best practice guidelines.
Methods
Setting
This study was carried out at an 811-bed quaternary care center located in Chicago, Illinois. In fiscal year 2021, there were 91 643 emergency department visits and 33 805 hospital admissions. At our flagship hospital, 2658 patients were diagnosed with epistaxis during fiscal year 2021. The emergency department saw 533 patients with epistaxis, with 342 requiring admission and 191 being discharged. Separately, 566 inpatients received a diagnosis of epistaxis during their admission. The remainder of the patients with epistaxis were seen on an outpatient basis.
Data Collection
Data were collected from nurses on 5 different inpatient units. An email with information about the in-service was sent to the nurse managers of the inpatient units. These 5 units were included because the nurse managers responded to the email and facilitated delivery of the in-service. Data collection took place from August to December 2020.
Intervention
A quality improvement team composed of a resident physician champion, nurse educators, and nurse managers was formed. The physician champion was a senior otolaryngology resident who was responsible for designing and administering the pre-test, in-service, and post test. The nurse educators and nurse managers helped coordinate times for the in-service and promoted the in-service for their staff.
Our intervention was an educational in-service, a technique that is commonly used at our institution for nurse education. In-services typically involve delivering a lecture on a clinically relevant topic to a group of nurses on a unit. In developing the in-service, a top priority was to present high-quality evidence-based material. There is an abundance of information in the literature surrounding epistaxis management. The clinical practice guideline published by the American Academy of Otolaryngology lists nasal compression, application of vasoconstrictors, nasal packing, and nasal cautery as first-line treatments for the management of epistaxis.6 Nasal packing and nasal cautery tend to be perceived as interventions that require a certain level of expertise and specialized supplies. As such, these interventions are not often performed by floor nurses. In contrast, nasal compression and application of vasoconstrictors require only a few easily accessible supplies, and the risks are relatively minimal. When performing nasal compression, the clinical practice guidelines recommend firm, sustained compression to the lower third of the nose for 5 minutes or longer.6 Topical vasoconstrictors are generally underutilized in epistaxis management. In a study looking at a random sample of all US emergency department visits from 1992 to 2001, only 18% of visits used an epistaxis-related medication.2 Oxymetazoline hydrochloride is a topical vasoconstrictor that is commonly used as a nasal decongestant. However, its vasoconstrictor properties also make it a useful tool for controlling epistaxis. In a study looking at emergency department visits at the University of Texas Health Science Center, 65% of patients had resolution of nosebleed with application of oxymetazoline hydrochloride as the only intervention, with another 18% experiencing resolution of nosebleed with a combination of oxymetazoline hydrochloride and silver nitrate cautery.7 Based on review of the literature, nasal compression and application of vasoconstrictors seemed to be low-resource interventions with minimal morbidity. Therefore, management centered around nasal compression and use of topical vasoconstrictors seemed appropriate for our nursing staff.
The in-service included information about the etiology and management of epistaxis. Particular emphasis was placed on addressing and debunking common misconceptions about nosebleed management. With regards to management, our presentation focused on the use of topical vasoconstrictors and firm pressure to the lower third of the nose for at least 5 minutes. Nasal packing and nasal cautery were presented as procedures that ENT would perform. After the in-service, questions from the nurses were answered as time permitted.
Testing and Outcomes
A pre-test was administered before each in-service. The pre-test components comprised a knowledge survey and a descriptive survey. The general epistaxis knowledge questions on the pre-test included the location of blood vessels most commonly responsible for nosebleeds, the ideal positioning of a patient during a nosebleed, the appropriate location to hold pressure during a nosebleed, and the appropriate duration to hold pressure during a nosebleed. The descriptive survey portion asked nurses to rate whether they felt “very comfortable,” “comfortable,” “uncomfortable,” or “very uncomfortable” managing nosebleeds. It also asked whether nurses thought they would be able to “always,” “usually,” “rarely,” or “never” stop nosebleeds on the floor. We collected demographic information, including gender identity, years of clinical experience, and primary clinical environment.
The post test asked the same questions as the pre-test and was administered immediately after the in-service in order to assess its impact. We also established an ongoing dialogue with our nursing colleagues to obtain feedback on the sessions.
Primary outcomes of interest were the difference in general epistaxis knowledge questions answered correctly between the pre-test and the post test; the difference in comfort level in managing epistaxis before and after the in-service; and the difference in confidence to stop nosebleeds before and after the in-service. A secondary outcome was determining the audience for the in-service. Specifically, we wanted to determine whether there were different outcomes based on clinical setting or years of clinical experience. If nurses in a certain clinical environment or beyond a certain experience level did not show significant improvement from pre-test to post test, we would not target them for the in-service. Another secondary outcome was determining optimal timing for delivery of the in-service. We wanted to determine if there was a nursing preference for delivering the in-service at mid-shift vs shift change.
Analysis
Statistical calculations were performed using Stata 15 (StataCorp LLC). A P value < .05 was considered to be statistically significant. Where applicable, 95% confidence intervals (CI) were calculated. T-test was used to determine whether there was a statistically significant difference between pre-test and post-test epistaxis knowledge question scores. T-test was also used to determine whether there was a statistically significant difference in test scores between nurses receiving the in-service at mid-shift vs shift change. Pearson chi-squared tests were used to determine if there was a statistically significant difference between pre-test and post-test perceptions of epistaxis management, and to investigate outcomes between different subsets of nurses.
SQUIRE 2.0 guidelines were utilized to provide a framework for this project and to structure the manuscript.8 This study met criteria for exemption from institutional review board approval.
Results
Fifty-one nurses took part in this project (Table). The majority of participants identified as female (88.24%), and just over half worked on medical floors (52.94%), with most of the remainder working in intensive care (25.49%) and surgical (15.69%) settings. There was a wide range of clinical experience, with 1.96% reporting 0 to 1 years of experience, 29.41% reporting 2 to 5 years, 23.53% reporting 5 to 10 years, 25.49% reporting 10 to 20 years, and 17.65% reporting more than 20 years.
There were unanswered questions on both the pre-test and post test. There was no consistently unanswered question. Omitted answers on the epistaxis knowledge questions were recorded as an “incorrect” answer. Omitted answers on the perception questions were considered null values and not considered in final analysis.
Primary Measures
General epistaxis knowledge (Figure, part A) improved from the pre-test, where out of 4 questions, the mean (SD) score was 1.74 (1.02) correct questions, to the post-test, where out of 4 questions, the mean score was 3.80 (0.40) correct questions. After participating in the in-service, nurses answered significantly more questions about epistaxis general knowledge correctly (mean difference, 2.07 [1.10]; 95% CI, 1.74-2.39; P < .001), and 80.43% of them got a perfect score on the epistaxis knowledge questions.
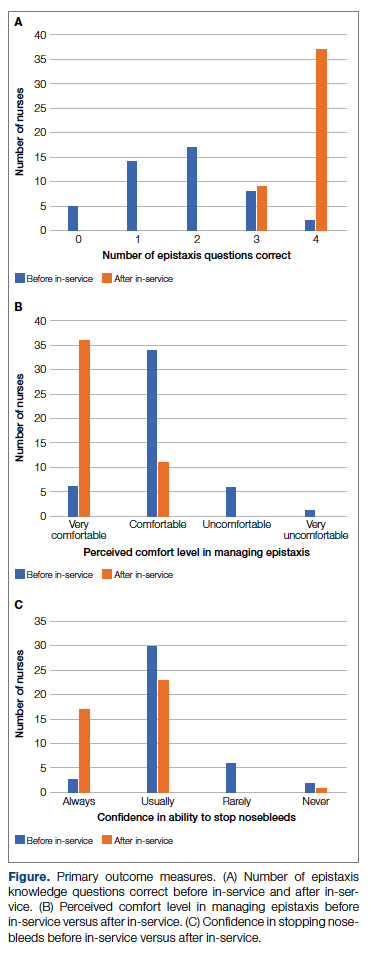
The second primary measure was the difference in comfort level in managing nosebleed. After participating in the in-service, nurses felt significantly more comfortable in managing nosebleeds (Figure, part B; P = .007), with 74.46% of nurses having an improved comfort level managing nosebleeds. Before the in-service, 12.76% of nurses felt “very comfortable” in managing nosebleeds vs more than three-quarters (76.59%) after the in-service. Of those who answered that they felt “comfortable” managing nosebleeds on the pre-test, 82.35% improved to feeling “very comfortable” in managing nosebleeds. Before the in-service, 14.89% of nurses felt “uncomfortable” or “very uncomfortable” in managing nosebleeds, and this decreased to 0 post intervention. After the in-service, 100.00% of nurses felt “comfortable” or “very comfortable” in managing nosebleeds.
After receiving the in-service, nurses felt significantly more confident in stopping nosebleeds (Figure, part C; P < .001), with 43.90% of them having an improvement in confidence in stopping epistaxis. Before the in-service, 7.31% of nurses felt that they would “always” be able to stop a nose-bleed, and this increased to 41.46% after the in-service. Of those who answered that they felt that they would “usually” be able to stop a nosebleed on the pre-test, 36.67% changed their answer to state that they would “always” be able to stop a nosebleed on the post test. Before the in-service, 19.51% of nurses felt that they would “rarely” or “never” be able to stop a nosebleed, and this decreased to 2.44% after the in-service.
Secondary Measures
All of the nurses who participated either “strongly agreed” or “agreed” that they learned something new from the in-service. However, to determine whether there was a population who would benefit most from the in-service, we stratified the data by years of clinical experience. There was no statistically significant difference in whether nurses with varying clinical experience learned something new (P = .148): 100% of nurses with 0-1 years of experience, 80.00% of nurses with 2-5 years of experience, 100% of nurses with 5-10 years of experience, 69.23% of nurses with 10-20 years of experience, and 100% of nurses with >20 years of experience “strongly agreed” that they learned something new from this in-service. There was no statistically significant difference on the post test compared to the pre-test in additional correct questions when stratified by clinical experience (P = .128). Second, when we stratified by clinical setting, we did not find a statistically significant difference in whether nurses in different clinical settings learned something new (P = .929): 88.89% of nurses in the medical setting, 87.50% of nurses in the surgical setting, and 84.62% of nurses in the intensive care setting “strongly agreed” that they learned something new from this presentation. On investigating additional questions correct on the post test compared to the pre-test, there was no statistically significant difference in additional correct questions when stratified by clinical setting (P = .446).
Optimal timing of the in-service was another important outcome. Initially, the in-service was administered at mid-shift, with 9 nurses participating at mid-shift, but our nursing colleagues gave unanimous feedback that this was a suboptimal time for delivery of an in-service. We changed the timing of the in-service to shift change; 42 nurses received the in-service at shift-change. There was no statistically significant difference in scores on the epistaxis knowledge questions between these two groups (P = .123). This indicated to us that changing the timing of the delivery resulted in similarly improved outcomes while having the added benefit of being preferred by our nursing colleagues.
Discussion
In undertaking this project, our primary aims were to improve epistaxis knowledge and perceived management in our nursing staff. Among our nursing staff, we were able to significantly increase epistaxis knowledge, improve comfort levels managing epistaxis, and improve confidence in successful epistaxis management. We also found that nurses of varying clinical experience and different clinical settings benefited equally from our intervention. Using quality improvement principles, we optimized our delivery. Our in-service focused on educating nurses to use epistaxis management techniques that were resource-efficient and low risk.
After participating in the in-service, nurses answered significantly more questions about epistaxis general knowledge correctly (Figure, part A; mean difference, 2.07 questions [1.10]; 95% CI, 1.74-2.39; P < .001), felt significantly more comfortable in managing nosebleeds (Figure, part B; P = .007), and felt significantly more confident in stopping nosebleeds (Figure, part C; P < .001). Based on these results, we successfully achieved our primary aims.
Our secondary aim was to determine the audience that would benefit the most from the in-service. All of the nurses who participated either “strongly agreed” or “agreed” that they learned something new from the in-service. There was no statistically significant difference in whether nurses of varying clinical experience learned something new (P = .148) or in additional correct questions when stratified by clinical experience (P =.128). Also, there was no statistically significant difference in whether nurses in different clinical settings learned something new (P = .929) or in additional correct questions when stratified by clinical setting (P = .446). These results indicated to us that all participants learned something new and that there was no specific target audience, but rather that all participants benefitted from our session.
Our nursing colleagues gave us feedback that the timing of the in-service during mid-shift was not ideal. It was difficult to gather nurses mid-shift due to pressing patient-care duties. Nurses also found it difficult to give their full attention at this time. Nurses, nurse educators, and nurse managers suggested that we conduct the in-service at shift change in order to capture a larger population and take advantage of time relatively free of clinical duties. Giving the in-service at a time with relatively fewer clinical responsibilities allowed for a more robust question-and-answer session. It also allowed our nursing colleagues to pay full attention to the in-service. There was no statistically significant difference in epistaxis general knowledge questions answered correctly; this indicates that the quality of the education session did not vary greatly. However, our nursing colleagues strongly preferred the in-service at shift change. By making this modification to our intervention, we were able to optimize our intervention.
The previously mentioned study in England reported that only 12% to 14% of their nursing staff got a perfect score on epistaxis knowledge questions. Prior to our study, there was no literature investigating the impact of an in-service on epistaxis knowledge. After our intervention, 80.43% of our nurses got a perfect score on the epistaxis knowledge questions. We believe that this is a fair comparison because our post-test questions were identical to the survey questions used in the previously mentioned study in England, with the addition of one question.3 Further, the findings of our study are consistent with other studies regarding the positive effect of in-service education on knowledge and attitudes surrounding clinical topics. Similar to the study in Ethiopia investigating nurses’ knowledge surrounding pain management, our study noted a significant improvement in nurses’ knowledge after participating in the in-service.4 Also, when comparing our study to the study performed in Connecticut investigating nurses’ confidence surrounding suicide precautions, we found a similar significant improvement in confidence in management after participating in the in-service.5
Given our reliance on a survey as a tool to collect information, our study was subject to nonresponse bias. For each main outcome question, there was a handful of nonresponders. While this likely indicated either overlooking a question or deferring to answer due to clinical inexperience or nonapplicable clinical role, it is possible that this may have represented a respondent who did not benefit from the in-service. Another source of possible bias is sampling bias. Attempts were made to capture a wide range of nurses at the in-service. However, if a nurse was not interested in the topic material, whether due to abundant clinical experience or disinterest, it is possible that they may not have attended. Additionally, the cohort was selected purely based on responses from nursing managers to the initial email. It is possible that nonresponding units may have benefitted differently from this in-service.
There were several limitations within our analysis. We did not collect data assessing the long-term retention of epistaxis knowledge and management techniques. It is possible that epistaxis knowledge, comfort in managing nosebleeds, and perceived confidence in stopping nosebleeds decreased back to baseline several months after the in-service. Ideally, we would have been able to collect this data to assess retention of the in-service information. Unfortunately, a significant number of nurses who initially participated in the project became lost to follow-up, making such data collection impossible. Additionally, there was no assessment of actual ability to stop nosebleeds before vs after this in-service. Perceived management of epistaxis vs actual management of epistaxis are 2 vastly different things. However, this data would have been difficult to collect, and it likely would not have been in the best interest of patients, especially before the in-service was administered. As an improvement to this project, we could have assessed how many nosebleeds nurses had seen and successfully stopped after the in-service. As previously mentioned, this was not possible due to losing a significant number of nurses to follow-up. Finally, we did not collect objective data on preference for administration of in-service at mid-shift vs shift change. We relied on subjective data from conversations with our colleagues. By collecting objective data, we could have supported this change to our intervention with data.
The primary challenge to sustainability for this intervention is nursing turnover. With each wave of departing nurses and new nursing hires, the difficulty of ensuring a consistent knowledge base and management standards within our nursing workforce became clearer. After optimizing our intervention, our solution was to provide a hospital-wide in-service, which was recorded and uploaded to an institution-wide in-service library. In this way, a nurse with the desire to learn about epistaxis management could access the material at any point in time. Another solution would have been to appoint champions for epistaxis management within each major department to deliver the epistaxis in-service to new hires and new rotators within the department. However, given the turnover witnessed in our study cohort, this may not be sustainable long term.
Conclusion
Epistaxis is a chief complaint that can present in many different clinical settings and situations. Therefore, the ability to stop epistaxis in a timely and effective fashion is valuable. Our study demonstrated that in-services can improve epistaxis knowledge and improve perceived epistaxis management. Ideally, this intervention will lead to improved patient care. Given that epistaxis is a ubiquitous issue, this study may benefit other institutions who want to improve care for patients with epistaxis.
Next steps for this intervention include utilizing in-services for epistaxis education at other institutions and collecting long-term data within our own institution. Collecting long-term data would allow us to assess the retention of epistaxis knowledge from our in-service.
Acknowledgments: The author thanks the nurse managers, nurse educators, and staff nurses involved in this project, as well as Dr. Louis Portugal for providing mentorship throughout this process and Dr. Dara Adams for assisting with statistical analysis.
Corresponding author: Avery Nelson, MD, University of Chicago Medical Center, 5841 S Maryland Ave, MC 1035, Chicago, IL 60637; [email protected]
Disclosures: None reported.
From the University of Chicago Medical Center, Chicago, IL.
Abstract
Background: Epistaxis is a common chief complaint addressed by otolaryngologists. A review of the literature showed that there is a deficit in epistaxis education within the nursing community. Conversations with our nursing colleagues confirmed this unmet demand.
Objective: This quality improvement project aimed to increase general epistaxis knowledge, perceived comfort level managing nosebleeds, and perceived ability to stop nosebleeds among our nursing staff.
Methods: Data were collected through a survey administered before and after our intervention. The survey tested general epistaxis knowledge and assessed comfort and confidence in stopping epistaxis. Our intervention was an educational session covering pertinent epistaxis etiology and management. Quality improvement principles were used to optimize delivery of the intervention.
Results: A total of 51 nurses participated in the project. After participating in the in-service educational session, nurses answered significantly more epistaxis general knowledge questions correctly (mean [SD] difference, 2.07 [1.10] questions; 95% CI, 1.74-2.39; P < .001). There was no statistically significant difference in additional correct questions when stratified by clinical experience or clinical setting (P = .128 and P = 0.446, respectively). Nurses also reported feeling significantly more comfortable and significantly more confident in managing nosebleeds after the in-service (P = .007 and P < 0.001, respectively); 74.46% of nurses had an improvement in comfort level in managing epistaxis and 43.90% of nurses had an improvement in confidence in stopping epistaxis. After we moved the educational session from mid-shift to shift change, the nursing staff reported more satisfaction while maintaining similar improvements in knowledge and confidence.
Conclusion: We were able to significantly increase epistaxis knowledge, improve comfort levels managing epistaxis, and improve confidence in successful epistaxis management. Nurses of varying clinical experience and different clinical settings benefitted equally from our intervention.
Keywords: nosebleed; in-service; quality improvement.
Epistaxis, or nosebleed, is estimated to be the chief complaint in 1 in 200 emergency department visits in the United States.1 Additionally, it represents up to one-third of otolaryngology-related emergency room admissions.2 There is no existing literature, to our best knowledge, specifically investigating the incidence of epistaxis after a patient is admitted. Anecdotally, inpatients who develop epistaxis account for an appreciable number of consults to otolaryngology (ENT). Epistaxis is a cross-disciplinary issue, occurring in a range of clinical settings. For example, patients with epistaxis can present to the emergency department or to an outpatient primary care clinic before being referred to ENT. Additionally, inpatients on many different services can develop spontaneous epistaxis due to a variety of environmental and iatrogenic factors, such as dry air, use of nasal cannula, and initiation of anticoagulation. Based on the experience of our ENT providers and discussions with our nursing colleagues, we concluded that there was an interest in epistaxis management training among our nursing workforce.
The presence of unmet demand for epistaxis education among our nursing colleagues was supported by our literature review. A study performed in England surveyed emergency department nurses on first aid measures for management of epistaxis, including ideal head positioning, location of pressure application, and duration of pressure application.3 Overall, only 12% to 14% of the nursing staff answered all 3 questions correctly.3 Additionally, 73% to 78% of the nursing staff felt that their training in epistaxis management was inadequate, and 88% desired further training in epistaxis management.3 If generalized, this study confirms the demand for further epistaxis education among nurses.
In-services have previously been shown to be effective educational tools within the nursing community. A study in Ethiopia that evaluated pain management knowledge and attitudes before and after an in-service found a significant improvement in mean rank score of nurses’ knowledge and attitudes regarding pain management after they participated in the in-service.4 Scores on the knowledge survey improved from 41.4% before the intervention to 63.0% post intervention.4 A study in Connecticut evaluated nurses’ confidence in discussing suicidal ideation with patients and knowledge surrounding suicide precautions.5 After participating in an in-service, nurses were significantly more confident in discussing suicidal ideation with patients; application of appropriate suicide precautions also increased after the in-service.5
Our aim was for nurses to have an improvement in overall epistaxis knowledge, perceived comfort level managing nosebleeds, and perceived ability to stop nosebleeds after attending our in-service. Additionally, an overarching priority was to provide high-quality epistaxis education based on the literature and best practice guidelines.
Methods
Setting
This study was carried out at an 811-bed quaternary care center located in Chicago, Illinois. In fiscal year 2021, there were 91 643 emergency department visits and 33 805 hospital admissions. At our flagship hospital, 2658 patients were diagnosed with epistaxis during fiscal year 2021. The emergency department saw 533 patients with epistaxis, with 342 requiring admission and 191 being discharged. Separately, 566 inpatients received a diagnosis of epistaxis during their admission. The remainder of the patients with epistaxis were seen on an outpatient basis.
Data Collection
Data were collected from nurses on 5 different inpatient units. An email with information about the in-service was sent to the nurse managers of the inpatient units. These 5 units were included because the nurse managers responded to the email and facilitated delivery of the in-service. Data collection took place from August to December 2020.
Intervention
A quality improvement team composed of a resident physician champion, nurse educators, and nurse managers was formed. The physician champion was a senior otolaryngology resident who was responsible for designing and administering the pre-test, in-service, and post test. The nurse educators and nurse managers helped coordinate times for the in-service and promoted the in-service for their staff.
Our intervention was an educational in-service, a technique that is commonly used at our institution for nurse education. In-services typically involve delivering a lecture on a clinically relevant topic to a group of nurses on a unit. In developing the in-service, a top priority was to present high-quality evidence-based material. There is an abundance of information in the literature surrounding epistaxis management. The clinical practice guideline published by the American Academy of Otolaryngology lists nasal compression, application of vasoconstrictors, nasal packing, and nasal cautery as first-line treatments for the management of epistaxis.6 Nasal packing and nasal cautery tend to be perceived as interventions that require a certain level of expertise and specialized supplies. As such, these interventions are not often performed by floor nurses. In contrast, nasal compression and application of vasoconstrictors require only a few easily accessible supplies, and the risks are relatively minimal. When performing nasal compression, the clinical practice guidelines recommend firm, sustained compression to the lower third of the nose for 5 minutes or longer.6 Topical vasoconstrictors are generally underutilized in epistaxis management. In a study looking at a random sample of all US emergency department visits from 1992 to 2001, only 18% of visits used an epistaxis-related medication.2 Oxymetazoline hydrochloride is a topical vasoconstrictor that is commonly used as a nasal decongestant. However, its vasoconstrictor properties also make it a useful tool for controlling epistaxis. In a study looking at emergency department visits at the University of Texas Health Science Center, 65% of patients had resolution of nosebleed with application of oxymetazoline hydrochloride as the only intervention, with another 18% experiencing resolution of nosebleed with a combination of oxymetazoline hydrochloride and silver nitrate cautery.7 Based on review of the literature, nasal compression and application of vasoconstrictors seemed to be low-resource interventions with minimal morbidity. Therefore, management centered around nasal compression and use of topical vasoconstrictors seemed appropriate for our nursing staff.
The in-service included information about the etiology and management of epistaxis. Particular emphasis was placed on addressing and debunking common misconceptions about nosebleed management. With regards to management, our presentation focused on the use of topical vasoconstrictors and firm pressure to the lower third of the nose for at least 5 minutes. Nasal packing and nasal cautery were presented as procedures that ENT would perform. After the in-service, questions from the nurses were answered as time permitted.
Testing and Outcomes
A pre-test was administered before each in-service. The pre-test components comprised a knowledge survey and a descriptive survey. The general epistaxis knowledge questions on the pre-test included the location of blood vessels most commonly responsible for nosebleeds, the ideal positioning of a patient during a nosebleed, the appropriate location to hold pressure during a nosebleed, and the appropriate duration to hold pressure during a nosebleed. The descriptive survey portion asked nurses to rate whether they felt “very comfortable,” “comfortable,” “uncomfortable,” or “very uncomfortable” managing nosebleeds. It also asked whether nurses thought they would be able to “always,” “usually,” “rarely,” or “never” stop nosebleeds on the floor. We collected demographic information, including gender identity, years of clinical experience, and primary clinical environment.
The post test asked the same questions as the pre-test and was administered immediately after the in-service in order to assess its impact. We also established an ongoing dialogue with our nursing colleagues to obtain feedback on the sessions.
Primary outcomes of interest were the difference in general epistaxis knowledge questions answered correctly between the pre-test and the post test; the difference in comfort level in managing epistaxis before and after the in-service; and the difference in confidence to stop nosebleeds before and after the in-service. A secondary outcome was determining the audience for the in-service. Specifically, we wanted to determine whether there were different outcomes based on clinical setting or years of clinical experience. If nurses in a certain clinical environment or beyond a certain experience level did not show significant improvement from pre-test to post test, we would not target them for the in-service. Another secondary outcome was determining optimal timing for delivery of the in-service. We wanted to determine if there was a nursing preference for delivering the in-service at mid-shift vs shift change.
Analysis
Statistical calculations were performed using Stata 15 (StataCorp LLC). A P value < .05 was considered to be statistically significant. Where applicable, 95% confidence intervals (CI) were calculated. T-test was used to determine whether there was a statistically significant difference between pre-test and post-test epistaxis knowledge question scores. T-test was also used to determine whether there was a statistically significant difference in test scores between nurses receiving the in-service at mid-shift vs shift change. Pearson chi-squared tests were used to determine if there was a statistically significant difference between pre-test and post-test perceptions of epistaxis management, and to investigate outcomes between different subsets of nurses.
SQUIRE 2.0 guidelines were utilized to provide a framework for this project and to structure the manuscript.8 This study met criteria for exemption from institutional review board approval.
Results
Fifty-one nurses took part in this project (Table). The majority of participants identified as female (88.24%), and just over half worked on medical floors (52.94%), with most of the remainder working in intensive care (25.49%) and surgical (15.69%) settings. There was a wide range of clinical experience, with 1.96% reporting 0 to 1 years of experience, 29.41% reporting 2 to 5 years, 23.53% reporting 5 to 10 years, 25.49% reporting 10 to 20 years, and 17.65% reporting more than 20 years.
There were unanswered questions on both the pre-test and post test. There was no consistently unanswered question. Omitted answers on the epistaxis knowledge questions were recorded as an “incorrect” answer. Omitted answers on the perception questions were considered null values and not considered in final analysis.
Primary Measures
General epistaxis knowledge (Figure, part A) improved from the pre-test, where out of 4 questions, the mean (SD) score was 1.74 (1.02) correct questions, to the post-test, where out of 4 questions, the mean score was 3.80 (0.40) correct questions. After participating in the in-service, nurses answered significantly more questions about epistaxis general knowledge correctly (mean difference, 2.07 [1.10]; 95% CI, 1.74-2.39; P < .001), and 80.43% of them got a perfect score on the epistaxis knowledge questions.
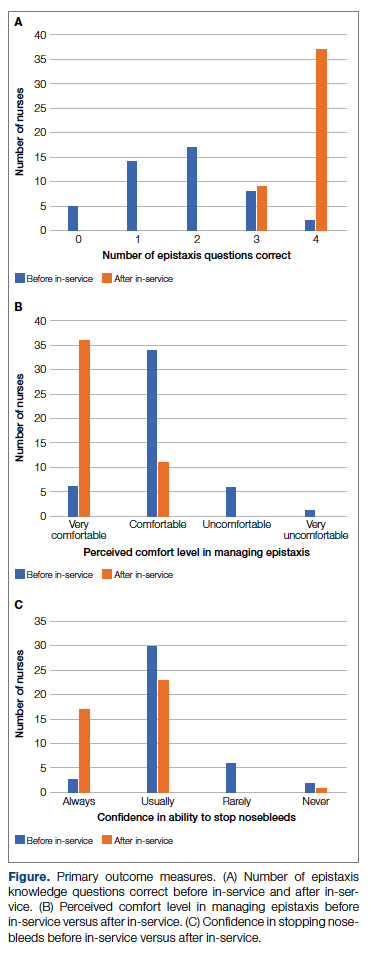
The second primary measure was the difference in comfort level in managing nosebleed. After participating in the in-service, nurses felt significantly more comfortable in managing nosebleeds (Figure, part B; P = .007), with 74.46% of nurses having an improved comfort level managing nosebleeds. Before the in-service, 12.76% of nurses felt “very comfortable” in managing nosebleeds vs more than three-quarters (76.59%) after the in-service. Of those who answered that they felt “comfortable” managing nosebleeds on the pre-test, 82.35% improved to feeling “very comfortable” in managing nosebleeds. Before the in-service, 14.89% of nurses felt “uncomfortable” or “very uncomfortable” in managing nosebleeds, and this decreased to 0 post intervention. After the in-service, 100.00% of nurses felt “comfortable” or “very comfortable” in managing nosebleeds.
After receiving the in-service, nurses felt significantly more confident in stopping nosebleeds (Figure, part C; P < .001), with 43.90% of them having an improvement in confidence in stopping epistaxis. Before the in-service, 7.31% of nurses felt that they would “always” be able to stop a nose-bleed, and this increased to 41.46% after the in-service. Of those who answered that they felt that they would “usually” be able to stop a nosebleed on the pre-test, 36.67% changed their answer to state that they would “always” be able to stop a nosebleed on the post test. Before the in-service, 19.51% of nurses felt that they would “rarely” or “never” be able to stop a nosebleed, and this decreased to 2.44% after the in-service.
Secondary Measures
All of the nurses who participated either “strongly agreed” or “agreed” that they learned something new from the in-service. However, to determine whether there was a population who would benefit most from the in-service, we stratified the data by years of clinical experience. There was no statistically significant difference in whether nurses with varying clinical experience learned something new (P = .148): 100% of nurses with 0-1 years of experience, 80.00% of nurses with 2-5 years of experience, 100% of nurses with 5-10 years of experience, 69.23% of nurses with 10-20 years of experience, and 100% of nurses with >20 years of experience “strongly agreed” that they learned something new from this in-service. There was no statistically significant difference on the post test compared to the pre-test in additional correct questions when stratified by clinical experience (P = .128). Second, when we stratified by clinical setting, we did not find a statistically significant difference in whether nurses in different clinical settings learned something new (P = .929): 88.89% of nurses in the medical setting, 87.50% of nurses in the surgical setting, and 84.62% of nurses in the intensive care setting “strongly agreed” that they learned something new from this presentation. On investigating additional questions correct on the post test compared to the pre-test, there was no statistically significant difference in additional correct questions when stratified by clinical setting (P = .446).
Optimal timing of the in-service was another important outcome. Initially, the in-service was administered at mid-shift, with 9 nurses participating at mid-shift, but our nursing colleagues gave unanimous feedback that this was a suboptimal time for delivery of an in-service. We changed the timing of the in-service to shift change; 42 nurses received the in-service at shift-change. There was no statistically significant difference in scores on the epistaxis knowledge questions between these two groups (P = .123). This indicated to us that changing the timing of the delivery resulted in similarly improved outcomes while having the added benefit of being preferred by our nursing colleagues.
Discussion
In undertaking this project, our primary aims were to improve epistaxis knowledge and perceived management in our nursing staff. Among our nursing staff, we were able to significantly increase epistaxis knowledge, improve comfort levels managing epistaxis, and improve confidence in successful epistaxis management. We also found that nurses of varying clinical experience and different clinical settings benefited equally from our intervention. Using quality improvement principles, we optimized our delivery. Our in-service focused on educating nurses to use epistaxis management techniques that were resource-efficient and low risk.
After participating in the in-service, nurses answered significantly more questions about epistaxis general knowledge correctly (Figure, part A; mean difference, 2.07 questions [1.10]; 95% CI, 1.74-2.39; P < .001), felt significantly more comfortable in managing nosebleeds (Figure, part B; P = .007), and felt significantly more confident in stopping nosebleeds (Figure, part C; P < .001). Based on these results, we successfully achieved our primary aims.
Our secondary aim was to determine the audience that would benefit the most from the in-service. All of the nurses who participated either “strongly agreed” or “agreed” that they learned something new from the in-service. There was no statistically significant difference in whether nurses of varying clinical experience learned something new (P = .148) or in additional correct questions when stratified by clinical experience (P =.128). Also, there was no statistically significant difference in whether nurses in different clinical settings learned something new (P = .929) or in additional correct questions when stratified by clinical setting (P = .446). These results indicated to us that all participants learned something new and that there was no specific target audience, but rather that all participants benefitted from our session.
Our nursing colleagues gave us feedback that the timing of the in-service during mid-shift was not ideal. It was difficult to gather nurses mid-shift due to pressing patient-care duties. Nurses also found it difficult to give their full attention at this time. Nurses, nurse educators, and nurse managers suggested that we conduct the in-service at shift change in order to capture a larger population and take advantage of time relatively free of clinical duties. Giving the in-service at a time with relatively fewer clinical responsibilities allowed for a more robust question-and-answer session. It also allowed our nursing colleagues to pay full attention to the in-service. There was no statistically significant difference in epistaxis general knowledge questions answered correctly; this indicates that the quality of the education session did not vary greatly. However, our nursing colleagues strongly preferred the in-service at shift change. By making this modification to our intervention, we were able to optimize our intervention.
The previously mentioned study in England reported that only 12% to 14% of their nursing staff got a perfect score on epistaxis knowledge questions. Prior to our study, there was no literature investigating the impact of an in-service on epistaxis knowledge. After our intervention, 80.43% of our nurses got a perfect score on the epistaxis knowledge questions. We believe that this is a fair comparison because our post-test questions were identical to the survey questions used in the previously mentioned study in England, with the addition of one question.3 Further, the findings of our study are consistent with other studies regarding the positive effect of in-service education on knowledge and attitudes surrounding clinical topics. Similar to the study in Ethiopia investigating nurses’ knowledge surrounding pain management, our study noted a significant improvement in nurses’ knowledge after participating in the in-service.4 Also, when comparing our study to the study performed in Connecticut investigating nurses’ confidence surrounding suicide precautions, we found a similar significant improvement in confidence in management after participating in the in-service.5
Given our reliance on a survey as a tool to collect information, our study was subject to nonresponse bias. For each main outcome question, there was a handful of nonresponders. While this likely indicated either overlooking a question or deferring to answer due to clinical inexperience or nonapplicable clinical role, it is possible that this may have represented a respondent who did not benefit from the in-service. Another source of possible bias is sampling bias. Attempts were made to capture a wide range of nurses at the in-service. However, if a nurse was not interested in the topic material, whether due to abundant clinical experience or disinterest, it is possible that they may not have attended. Additionally, the cohort was selected purely based on responses from nursing managers to the initial email. It is possible that nonresponding units may have benefitted differently from this in-service.
There were several limitations within our analysis. We did not collect data assessing the long-term retention of epistaxis knowledge and management techniques. It is possible that epistaxis knowledge, comfort in managing nosebleeds, and perceived confidence in stopping nosebleeds decreased back to baseline several months after the in-service. Ideally, we would have been able to collect this data to assess retention of the in-service information. Unfortunately, a significant number of nurses who initially participated in the project became lost to follow-up, making such data collection impossible. Additionally, there was no assessment of actual ability to stop nosebleeds before vs after this in-service. Perceived management of epistaxis vs actual management of epistaxis are 2 vastly different things. However, this data would have been difficult to collect, and it likely would not have been in the best interest of patients, especially before the in-service was administered. As an improvement to this project, we could have assessed how many nosebleeds nurses had seen and successfully stopped after the in-service. As previously mentioned, this was not possible due to losing a significant number of nurses to follow-up. Finally, we did not collect objective data on preference for administration of in-service at mid-shift vs shift change. We relied on subjective data from conversations with our colleagues. By collecting objective data, we could have supported this change to our intervention with data.
The primary challenge to sustainability for this intervention is nursing turnover. With each wave of departing nurses and new nursing hires, the difficulty of ensuring a consistent knowledge base and management standards within our nursing workforce became clearer. After optimizing our intervention, our solution was to provide a hospital-wide in-service, which was recorded and uploaded to an institution-wide in-service library. In this way, a nurse with the desire to learn about epistaxis management could access the material at any point in time. Another solution would have been to appoint champions for epistaxis management within each major department to deliver the epistaxis in-service to new hires and new rotators within the department. However, given the turnover witnessed in our study cohort, this may not be sustainable long term.
Conclusion
Epistaxis is a chief complaint that can present in many different clinical settings and situations. Therefore, the ability to stop epistaxis in a timely and effective fashion is valuable. Our study demonstrated that in-services can improve epistaxis knowledge and improve perceived epistaxis management. Ideally, this intervention will lead to improved patient care. Given that epistaxis is a ubiquitous issue, this study may benefit other institutions who want to improve care for patients with epistaxis.
Next steps for this intervention include utilizing in-services for epistaxis education at other institutions and collecting long-term data within our own institution. Collecting long-term data would allow us to assess the retention of epistaxis knowledge from our in-service.
Acknowledgments: The author thanks the nurse managers, nurse educators, and staff nurses involved in this project, as well as Dr. Louis Portugal for providing mentorship throughout this process and Dr. Dara Adams for assisting with statistical analysis.
Corresponding author: Avery Nelson, MD, University of Chicago Medical Center, 5841 S Maryland Ave, MC 1035, Chicago, IL 60637; [email protected]
Disclosures: None reported.
1. Pallin DJ, Chng Y-M, McKay MP, et al. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46(1):77-81. doi:10.1016/j.annemergmed.2004.12.014
2. Walker TWM, Macfarlane TV, McGarry GW. The epidemiology and chronobiology of epistaxis: An investigation of Scottish hospital admissions 1995-2004. Clin Otolaryngol. 2007;32(5):361-365. doi:10.1111/j.1749-4486.2007.01530.x
3. Hakim N, Mummadi SM, Jolly K, et al. Nurse-led epistaxis management within the emergency department. Br J Nurs. 2018;27(1):41-46. doi:10.12968/bjon.2018.27.1.41
4. Germossa GN, Sjetne IS, Hellesø R. The impact of an in-service educational program on nurses’ knowledge and attitudes regarding pain management in an Ethiopian University Hospital. Front Public Health. 2018;6:229. doi:10.3389/fpubh.2018.00229
5. Manister NN, Murray S, Burke JM, Finegan M, McKiernan ME. Effectiveness of nursing education to prevent inpatient suicide. J Contin Educ Nurs. 2017;48(9):413-419. doi:10.3928/00220124-20170816-07
6. Tunkel DE, Anne S, Payne SC, et al. Clinical practice guideline: nosebleed (epistaxis) executive summary. Otolaryngol Head Neck Surg. 2020;162(1):S1-S38. doi:10.1177/0194599819890327
7. Krempl GA, Noorily AD. Use of oxymetazoline in the management of epistaxis. Ann Otol Rhinol Laryngol. 1995;104(9 Part 1):704-706. doi:10.1177/000348949510400906
8. Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0—standards for quality improvement reporting excellence—revised publication guidelines from a detailed consensus process. J Am Coll Surg. 2016;222(3):317-323. doi:10.1016/j.jamcollsurg.2015.07.456
1. Pallin DJ, Chng Y-M, McKay MP, et al. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46(1):77-81. doi:10.1016/j.annemergmed.2004.12.014
2. Walker TWM, Macfarlane TV, McGarry GW. The epidemiology and chronobiology of epistaxis: An investigation of Scottish hospital admissions 1995-2004. Clin Otolaryngol. 2007;32(5):361-365. doi:10.1111/j.1749-4486.2007.01530.x
3. Hakim N, Mummadi SM, Jolly K, et al. Nurse-led epistaxis management within the emergency department. Br J Nurs. 2018;27(1):41-46. doi:10.12968/bjon.2018.27.1.41
4. Germossa GN, Sjetne IS, Hellesø R. The impact of an in-service educational program on nurses’ knowledge and attitudes regarding pain management in an Ethiopian University Hospital. Front Public Health. 2018;6:229. doi:10.3389/fpubh.2018.00229
5. Manister NN, Murray S, Burke JM, Finegan M, McKiernan ME. Effectiveness of nursing education to prevent inpatient suicide. J Contin Educ Nurs. 2017;48(9):413-419. doi:10.3928/00220124-20170816-07
6. Tunkel DE, Anne S, Payne SC, et al. Clinical practice guideline: nosebleed (epistaxis) executive summary. Otolaryngol Head Neck Surg. 2020;162(1):S1-S38. doi:10.1177/0194599819890327
7. Krempl GA, Noorily AD. Use of oxymetazoline in the management of epistaxis. Ann Otol Rhinol Laryngol. 1995;104(9 Part 1):704-706. doi:10.1177/000348949510400906
8. Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0—standards for quality improvement reporting excellence—revised publication guidelines from a detailed consensus process. J Am Coll Surg. 2016;222(3):317-323. doi:10.1016/j.jamcollsurg.2015.07.456
Comorbidity Coding and Its Impact on Hospital Complexity: Reply
Authors' Response
We agree with the valid comments made by Dr. Kerguelen and will respond to each set of questions in order.
Regarding the first set of questions on how we knew that our CMI was low and our patient acuity was under- represented, the University of Miami Health System is a designated cancer center with a Prospective Payment System exempt model (PPS exempt), and is one of 11 hospitals in the United States excluded for payment under the Inpatient Prospective Payment System. We know, therefore, that we care for a very complex patient population. Additionally, we benchmark ourselves against other academic medical centers (AMCs) with similarly complex patients and had noted that our patients appeared “less complex.” Specifically, our baseline CMI was 1.77 in early 2018 compared with an overall higher CMI for the AMC cohort; also, the total number of diagnoses we captured was lower than that in other AMCs. These 2 facts together alerted us that we likely had coding and clinical documentation improvement (CDI) opportunities. We recognized that our complexity was not being captured both because the clinical information was not documented in a manner readily translatable to ICD-10 codes and codes were missed when the documentation did exist. To remedy these problems, we implemented multiple immediate “fixes,” which included revamping our CDI efforts, re-education, and enhancements to our electronic health record for providers, CDIs, and coders. Since publication of our article, our CMI has continued to increase month over month, up to 2.57 most recently in May 2022, as we have continued to focus on several additional initiatives to impact both better documentation and coding.
The second set of questions asked whether the perceived low CMI was causing problems with payers and about the risk of artificially increasing the CMI through overdiagnosis as well as audit mechanisms to avoid this, and changes in expected mortality and observed mortality. To our knowledge, the lower CMI did not cause any problems with payers, but this is something we are currently tracking. Coding and documentation are constantly audited both internally (by our quality department) and externally (using Inter-Rater Reliability audits and validation), with no noted trend or targeted opportunities. We only include comorbidities that are current, actively monitored/managed, and pertinent to the care of our patients. We have not noted a change in denials, which gives us confidence we are not now overdiagnosing.
Our observed mortality has also increased. We, like all institutions, experienced the confounding factor of the COVID-19 pandemic, which coincided with the higher observed mortality over the course of the past 2 years. While the observed mortality (indicating sicker patients assuming no worsening of care processes) may partly explain our increased coding complexity, our decreasing mortality index (observed:expected mortality) suggests that our efforts to improve documentation and coding likely reflect improved capture of missed complexity (Figure).
We understand the concerns raised by Dr. Kerguelen about potential mis(over)coding. As part of this quality initiative, therefore, we plan long-term evaluations of our processes and metrics to better determine and guide our understanding of the impact of what we have already implemented and future interventions. In fact, we are in the process of analyzing additional interventions and hope to share results from these evaluations soon.
Marie Anne Sosa, MD
Tanira Ferreira, MD
Hayley Gershengorn, MD
Melissa Soto
Estin Kelly
Ameena Shrestha
Julianne Burgos
Sandeep Devabhaktuni
Dipen Parekh, MD
Maritza Suarez, MD
University of Miami Hospital and Clinics, Miami, FL
[email protected]
Disclosures: None reported.
Authors' Response
We agree with the valid comments made by Dr. Kerguelen and will respond to each set of questions in order.
Regarding the first set of questions on how we knew that our CMI was low and our patient acuity was under- represented, the University of Miami Health System is a designated cancer center with a Prospective Payment System exempt model (PPS exempt), and is one of 11 hospitals in the United States excluded for payment under the Inpatient Prospective Payment System. We know, therefore, that we care for a very complex patient population. Additionally, we benchmark ourselves against other academic medical centers (AMCs) with similarly complex patients and had noted that our patients appeared “less complex.” Specifically, our baseline CMI was 1.77 in early 2018 compared with an overall higher CMI for the AMC cohort; also, the total number of diagnoses we captured was lower than that in other AMCs. These 2 facts together alerted us that we likely had coding and clinical documentation improvement (CDI) opportunities. We recognized that our complexity was not being captured both because the clinical information was not documented in a manner readily translatable to ICD-10 codes and codes were missed when the documentation did exist. To remedy these problems, we implemented multiple immediate “fixes,” which included revamping our CDI efforts, re-education, and enhancements to our electronic health record for providers, CDIs, and coders. Since publication of our article, our CMI has continued to increase month over month, up to 2.57 most recently in May 2022, as we have continued to focus on several additional initiatives to impact both better documentation and coding.
The second set of questions asked whether the perceived low CMI was causing problems with payers and about the risk of artificially increasing the CMI through overdiagnosis as well as audit mechanisms to avoid this, and changes in expected mortality and observed mortality. To our knowledge, the lower CMI did not cause any problems with payers, but this is something we are currently tracking. Coding and documentation are constantly audited both internally (by our quality department) and externally (using Inter-Rater Reliability audits and validation), with no noted trend or targeted opportunities. We only include comorbidities that are current, actively monitored/managed, and pertinent to the care of our patients. We have not noted a change in denials, which gives us confidence we are not now overdiagnosing.
Our observed mortality has also increased. We, like all institutions, experienced the confounding factor of the COVID-19 pandemic, which coincided with the higher observed mortality over the course of the past 2 years. While the observed mortality (indicating sicker patients assuming no worsening of care processes) may partly explain our increased coding complexity, our decreasing mortality index (observed:expected mortality) suggests that our efforts to improve documentation and coding likely reflect improved capture of missed complexity (Figure).
We understand the concerns raised by Dr. Kerguelen about potential mis(over)coding. As part of this quality initiative, therefore, we plan long-term evaluations of our processes and metrics to better determine and guide our understanding of the impact of what we have already implemented and future interventions. In fact, we are in the process of analyzing additional interventions and hope to share results from these evaluations soon.
Marie Anne Sosa, MD
Tanira Ferreira, MD
Hayley Gershengorn, MD
Melissa Soto
Estin Kelly
Ameena Shrestha
Julianne Burgos
Sandeep Devabhaktuni
Dipen Parekh, MD
Maritza Suarez, MD
University of Miami Hospital and Clinics, Miami, FL
[email protected]
Disclosures: None reported.
Authors' Response
We agree with the valid comments made by Dr. Kerguelen and will respond to each set of questions in order.
Regarding the first set of questions on how we knew that our CMI was low and our patient acuity was under- represented, the University of Miami Health System is a designated cancer center with a Prospective Payment System exempt model (PPS exempt), and is one of 11 hospitals in the United States excluded for payment under the Inpatient Prospective Payment System. We know, therefore, that we care for a very complex patient population. Additionally, we benchmark ourselves against other academic medical centers (AMCs) with similarly complex patients and had noted that our patients appeared “less complex.” Specifically, our baseline CMI was 1.77 in early 2018 compared with an overall higher CMI for the AMC cohort; also, the total number of diagnoses we captured was lower than that in other AMCs. These 2 facts together alerted us that we likely had coding and clinical documentation improvement (CDI) opportunities. We recognized that our complexity was not being captured both because the clinical information was not documented in a manner readily translatable to ICD-10 codes and codes were missed when the documentation did exist. To remedy these problems, we implemented multiple immediate “fixes,” which included revamping our CDI efforts, re-education, and enhancements to our electronic health record for providers, CDIs, and coders. Since publication of our article, our CMI has continued to increase month over month, up to 2.57 most recently in May 2022, as we have continued to focus on several additional initiatives to impact both better documentation and coding.
The second set of questions asked whether the perceived low CMI was causing problems with payers and about the risk of artificially increasing the CMI through overdiagnosis as well as audit mechanisms to avoid this, and changes in expected mortality and observed mortality. To our knowledge, the lower CMI did not cause any problems with payers, but this is something we are currently tracking. Coding and documentation are constantly audited both internally (by our quality department) and externally (using Inter-Rater Reliability audits and validation), with no noted trend or targeted opportunities. We only include comorbidities that are current, actively monitored/managed, and pertinent to the care of our patients. We have not noted a change in denials, which gives us confidence we are not now overdiagnosing.
Our observed mortality has also increased. We, like all institutions, experienced the confounding factor of the COVID-19 pandemic, which coincided with the higher observed mortality over the course of the past 2 years. While the observed mortality (indicating sicker patients assuming no worsening of care processes) may partly explain our increased coding complexity, our decreasing mortality index (observed:expected mortality) suggests that our efforts to improve documentation and coding likely reflect improved capture of missed complexity (Figure).
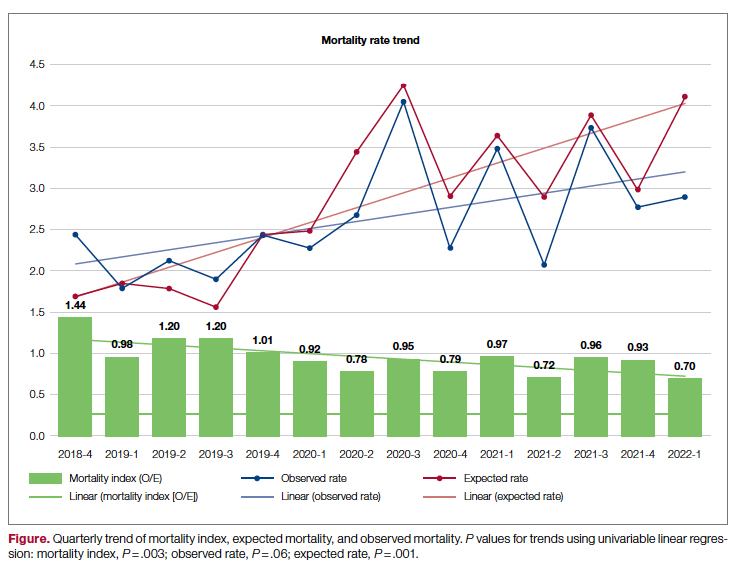
We understand the concerns raised by Dr. Kerguelen about potential mis(over)coding. As part of this quality initiative, therefore, we plan long-term evaluations of our processes and metrics to better determine and guide our understanding of the impact of what we have already implemented and future interventions. In fact, we are in the process of analyzing additional interventions and hope to share results from these evaluations soon.
Marie Anne Sosa, MD
Tanira Ferreira, MD
Hayley Gershengorn, MD
Melissa Soto
Estin Kelly
Ameena Shrestha
Julianne Burgos
Sandeep Devabhaktuni
Dipen Parekh, MD
Maritza Suarez, MD
University of Miami Hospital and Clinics, Miami, FL
[email protected]
Disclosures: None reported.
Comorbidity Coding and Its Impact on Hospital Complexity
To the Editor:
I read with interest the article by Sosa and colleagues1 in which they present some stimulating analyses pertaining to a topic that we have been discussing at my institution for several years. Part of this discussion deals with the complexity of our hospital and how complexity is affected by comorbidity coding.
In 2013, we implemented the International Refined-DRGs (IR-DRGs) system to measure complexity at our hospital in Bogotá, Colombia. Our perception at that time was that the case mix index (CMI) was very low (0.7566), even for a general hospital with a high volume of pathologies with low relative weight (RW). Two medical auditors were assigned to review the medical records in order to improve the quality, quantity, and order of diagnoses. Emphasis was placed on patients with stays longer than 5 days and with only 1 diagnosis coded at admission. Additionally, International Classification of Diseases 10th Revision (World Health Organization version) diagnoses from chapters R (Symptoms and Signs Not Elsewhere Classified) and V through Y (External Causes) were blocked in the electronic health record. With these measures, our CMI increased 74%, reaching 1.3151 by the end of 2021, with a maximum peak of 1.6743 in May 2021, which coincided with the third peak of COVID-19 in Colombia.
However, the article by Sosa and colleagues draws my attention to the following: why do the authors state that their CMI is low and the patient acuity was under-represented? Is this due to a comparison with similar hospitals, or to a recommendation from a regulatory agency? We have found our CMI remains low because of a high volume of nonsurgical care (60%), deliveries, and digestive, respiratory, and urinary pathologies of low RW.
Also, was the perceived low CMI causing problems with payers? And further, how did the authors avoid the risk of artificially increasing the CMI through overdiagnosis of patients, and were there audit mechanisms to avoid this? While there was a clear change in expected mortality, did the observed mortality also change with the strategies implemented? This last question is relevant because, if the observed mortality were maintained, this would provide evidence that a coding problem was the cause of their hospital’s low CMI.
I reiterate my congratulations to the authors for presenting analyses that are very useful to other providers and researchers worldwide interested in addressing management issues related to the correct identification and classification of patients.
Carlos Kerguelen, MD, MA
Fundacion Santa Fe de Bogotá, Bogotá, Colombia
[email protected]
Disclosures: None reported.
1. Sosa M, Ferreira T, Gershengorn H, et al. Improving hospital metrics through the implementation of a comorbidity capture tool and other quality initiatives. J Clin Outcomes Manage. 2022;29(2):80-87. doi:10.12788/jcom.0088
To the Editor:
I read with interest the article by Sosa and colleagues1 in which they present some stimulating analyses pertaining to a topic that we have been discussing at my institution for several years. Part of this discussion deals with the complexity of our hospital and how complexity is affected by comorbidity coding.
In 2013, we implemented the International Refined-DRGs (IR-DRGs) system to measure complexity at our hospital in Bogotá, Colombia. Our perception at that time was that the case mix index (CMI) was very low (0.7566), even for a general hospital with a high volume of pathologies with low relative weight (RW). Two medical auditors were assigned to review the medical records in order to improve the quality, quantity, and order of diagnoses. Emphasis was placed on patients with stays longer than 5 days and with only 1 diagnosis coded at admission. Additionally, International Classification of Diseases 10th Revision (World Health Organization version) diagnoses from chapters R (Symptoms and Signs Not Elsewhere Classified) and V through Y (External Causes) were blocked in the electronic health record. With these measures, our CMI increased 74%, reaching 1.3151 by the end of 2021, with a maximum peak of 1.6743 in May 2021, which coincided with the third peak of COVID-19 in Colombia.
However, the article by Sosa and colleagues draws my attention to the following: why do the authors state that their CMI is low and the patient acuity was under-represented? Is this due to a comparison with similar hospitals, or to a recommendation from a regulatory agency? We have found our CMI remains low because of a high volume of nonsurgical care (60%), deliveries, and digestive, respiratory, and urinary pathologies of low RW.
Also, was the perceived low CMI causing problems with payers? And further, how did the authors avoid the risk of artificially increasing the CMI through overdiagnosis of patients, and were there audit mechanisms to avoid this? While there was a clear change in expected mortality, did the observed mortality also change with the strategies implemented? This last question is relevant because, if the observed mortality were maintained, this would provide evidence that a coding problem was the cause of their hospital’s low CMI.
I reiterate my congratulations to the authors for presenting analyses that are very useful to other providers and researchers worldwide interested in addressing management issues related to the correct identification and classification of patients.
Carlos Kerguelen, MD, MA
Fundacion Santa Fe de Bogotá, Bogotá, Colombia
[email protected]
Disclosures: None reported.
To the Editor:
I read with interest the article by Sosa and colleagues1 in which they present some stimulating analyses pertaining to a topic that we have been discussing at my institution for several years. Part of this discussion deals with the complexity of our hospital and how complexity is affected by comorbidity coding.
In 2013, we implemented the International Refined-DRGs (IR-DRGs) system to measure complexity at our hospital in Bogotá, Colombia. Our perception at that time was that the case mix index (CMI) was very low (0.7566), even for a general hospital with a high volume of pathologies with low relative weight (RW). Two medical auditors were assigned to review the medical records in order to improve the quality, quantity, and order of diagnoses. Emphasis was placed on patients with stays longer than 5 days and with only 1 diagnosis coded at admission. Additionally, International Classification of Diseases 10th Revision (World Health Organization version) diagnoses from chapters R (Symptoms and Signs Not Elsewhere Classified) and V through Y (External Causes) were blocked in the electronic health record. With these measures, our CMI increased 74%, reaching 1.3151 by the end of 2021, with a maximum peak of 1.6743 in May 2021, which coincided with the third peak of COVID-19 in Colombia.
However, the article by Sosa and colleagues draws my attention to the following: why do the authors state that their CMI is low and the patient acuity was under-represented? Is this due to a comparison with similar hospitals, or to a recommendation from a regulatory agency? We have found our CMI remains low because of a high volume of nonsurgical care (60%), deliveries, and digestive, respiratory, and urinary pathologies of low RW.
Also, was the perceived low CMI causing problems with payers? And further, how did the authors avoid the risk of artificially increasing the CMI through overdiagnosis of patients, and were there audit mechanisms to avoid this? While there was a clear change in expected mortality, did the observed mortality also change with the strategies implemented? This last question is relevant because, if the observed mortality were maintained, this would provide evidence that a coding problem was the cause of their hospital’s low CMI.
I reiterate my congratulations to the authors for presenting analyses that are very useful to other providers and researchers worldwide interested in addressing management issues related to the correct identification and classification of patients.
Carlos Kerguelen, MD, MA
Fundacion Santa Fe de Bogotá, Bogotá, Colombia
[email protected]
Disclosures: None reported.
1. Sosa M, Ferreira T, Gershengorn H, et al. Improving hospital metrics through the implementation of a comorbidity capture tool and other quality initiatives. J Clin Outcomes Manage. 2022;29(2):80-87. doi:10.12788/jcom.0088
1. Sosa M, Ferreira T, Gershengorn H, et al. Improving hospital metrics through the implementation of a comorbidity capture tool and other quality initiatives. J Clin Outcomes Manage. 2022;29(2):80-87. doi:10.12788/jcom.0088
Supporting Patients on Complex Care Journeys: How Technology Can Bridge the Gaps
From Memora Health (Dr. Flyckt and Dr. Colbert), San Francisco, CA; and Harvard Medical School (Dr. Colbert), Boston, MA.
A close relative was recently diagnosed with follicular lymphoma. He was cared for at a high-ranked cancer center by physicians with demonstrated expertise, and even had the support of a care navigator. Still, he was often left feeling overwhelmed and confused, holding an inch-thick stack of papers, instructions, and pamphlets. As he left his treatment planning visit, reeling from the emotional burden of his diagnosis and all the unfamiliar terminology, he didn’t know what to do or what to expect. Later, when he experienced early signs of tumor lysis syndrome, he struggled to reach his care team for triage and guidance. When he went to the emergency room, his oncologist was never informed.
This scenario is unfortunately common, and versions of this scenario play out thousands of times each day across the US health system. Within the clinic and hospital setting, patients receive excellent care from their providers, but a disconnect emerges once the patient leaves these medical settings: patients at home struggle to find guidance and support, while care teams lack the tools to engage patients between visits or monitor their health across care settings, providers, or episodes of care.
Leveraging Technology to Move From Episodes of Care to Complex Care Journeys
The use of automated messaging, artificial intelligence and natural language processing–driven chat experiences, and text-based support is becoming more common. However, health care lags behind other industries in the adoption of these technologies.1,2 The slow pace can be warranted, given that health care is more complicated and higher risk than inquiring about a lost package, ordering groceries, or applying for a mortgage. At the same time, many of the consumer engagement tools used to guide an applicant through the multiple steps and complexities of their home loan process or to prompt viewers to select new shows to binge have applications in health care.
Over the past few years, technologies have emerged that guide patients through complex care journeys and allow care teams to monitor and engage patients between visits. These solutions come in different formats, but generally patients can receive messages on their phones that contain disease-specific educational content, prompts to fill prescriptions and take medications, and reminders and guidance on how to prepare for appointments and procedures. These programs also collect relevant data from patients through survey and electronic patient-reported outcomes instruments, as well as connected patient monitoring devices, that help track patient progress and identify issues as they arise. Many programs also incorporate symptom triage pathways and use natural language processing to respond automatically to patient questions and concerns.3,4
These technology solutions can automate many tasks that in the past required a care team member to spend hours on the phone. Newly freed from such repetitive tasks, care teams can now focus on more in-depth interactions with those patients who are most in need—the types of interactions that are more satisfying and rewarding. Such assistance is particularly needed today with the staffing shortages faced by most health systems.5
In addition, technology allows teams to see the panel of patients they are caring for and to quickly identify and take action on any specific needs or issues. Care teams can focus on any patient and see where they are in their journey. When appropriate, some solutions also allow care teams to engage directly with patients through text-messaging, creating a seamless experience and unified communication channel. Ideally, these solutions should be linked or embedded within the electronic health record or other primary system of record, so that teams can easily access these tools through their existing workflows and avoid creating yet another interface to navigate.
The Impact of Low-Tech Solutions to Deliver High-Touch Support
There is evidence showing that digital patient navigation tools impact patient care. In the oncology setting, patients with a digital navigator have achieved over 95% adherence rates with complex oral chemotherapy regimens (Memora Health Unpublished Data. 2022.). In the postpartum setting, a text message–based program improved screening rates for postpartum depression and did so with very high patient satisfaction ratings.6 Particularly notable is the fact that this depression screening program achieved these results in a population that was predominantly low income, with more than half belonging to underrepresented minority populations.6
We believe these digital patient navigation technologies, specifically low-tech solutions that don’t require app downloads, portal log-ins, or high-speed internet, will transform care delivery over the next 5 to 10 years. Successful management of complex conditions like diabetes or cancer requires more than 3 hours of care each day,7 yet most patients spend only 1 or 2 hours per month directly interacting with their health care providers. However, most patients carry their phones with them at all times, and artificial intelligence–enabled text support is “always on” to provide support, monitoring, and guidance, wherever a patient happens to be when assistance is needed.
Shifting the Model to Support a Lifetime of Care
While still in the early stages of development, these tools have the potential to radically alter the practice of medicine, shifting the focus from episodic interactions to continuous journey-based care delivery. Outside of an acute event bringing a patient into the clinic or emergency room, many patients go a year or more without seeing their primary care providers.8 During that time, an immense amount of information is underreported or completely lost. Capturing this information in real-time and more holistically over a person’s lifetime of care could provide physicians better insight to both better manage and more fully evaluate the success of treatment plans by tracking patient symptoms, pain, and functional status over time. With this more longitudinal view of the patient, we see a pathway towards achieving the Quadruple Aim: patients who are more supported will achieve better outcomes at lower cost, they will have a better experience, and care teams will be empowered to focus their time on more satisfying activities rather than repetitive administrative tasks.
Corresponding author: James A. Colbert, MD, MBA; [email protected]
Disclosures: Dr. Flyckt and Dr. Colbert are employed by Memora Health, an organization that helps health care systems digitize and automate care journeys.
1. Hermes S, Riasanow T, Clemons EK, et al. The digital transformation of the healthcare industry: exploring the rise of emerging platform ecosystems and their influence on the role of patients. Bus Res. 2020;13:1033-1069. doi:10.1007/s40685-020-00125-x
2. Van Velthoven MH, Cordon C. Sustainable adoption of digital health innovations: perspectives from a stakeholder workshop. J Med Internet Res. 2019;21(3):e11922. doi:10.2196/11922
3. Campbell K, Louie P, Levine B, Gililland J. Using patient engagement platforms in the postoperative management of patients. Curr Rev Musculoskelet Med. 2020;13(4):479-484. doi:10.1007/s12178-020-09638-8
4. Xu L, Sanders L, Li K, Chow JCL. Chatbot for health care and oncology applications using artificial intelligence and machine learning: systematic review. JMIR Cancer. 2021;7(4):e27850. doi:10.2196/27850
5. Data brief: health care workforce challenges threaten hospitals’ ability to care for patients. American Hospital Association. Accessed July 24, 2022. www.aha.org/fact-sheets/2021-11-01-data-brief-health-care-workforce-challenges-threaten-hospitals-ability-care
6. Gaulton JS, Leitner K, Hahn L, et al. Healing at home: applying innovation principles to redesign and optimise postpartum care. BMJ Innovations. 2022;8:37-41.
7. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209-214. doi:10.1370/afm.310
8. Ganguli I, Shi Z, E. Orav J, et al. Declining use of primary care among commercially insured adults in the united states, 2008–2016. Ann Intern Med. 2020;172:240-247. doi:10.7326/M19-1834
From Memora Health (Dr. Flyckt and Dr. Colbert), San Francisco, CA; and Harvard Medical School (Dr. Colbert), Boston, MA.
A close relative was recently diagnosed with follicular lymphoma. He was cared for at a high-ranked cancer center by physicians with demonstrated expertise, and even had the support of a care navigator. Still, he was often left feeling overwhelmed and confused, holding an inch-thick stack of papers, instructions, and pamphlets. As he left his treatment planning visit, reeling from the emotional burden of his diagnosis and all the unfamiliar terminology, he didn’t know what to do or what to expect. Later, when he experienced early signs of tumor lysis syndrome, he struggled to reach his care team for triage and guidance. When he went to the emergency room, his oncologist was never informed.
This scenario is unfortunately common, and versions of this scenario play out thousands of times each day across the US health system. Within the clinic and hospital setting, patients receive excellent care from their providers, but a disconnect emerges once the patient leaves these medical settings: patients at home struggle to find guidance and support, while care teams lack the tools to engage patients between visits or monitor their health across care settings, providers, or episodes of care.
Leveraging Technology to Move From Episodes of Care to Complex Care Journeys
The use of automated messaging, artificial intelligence and natural language processing–driven chat experiences, and text-based support is becoming more common. However, health care lags behind other industries in the adoption of these technologies.1,2 The slow pace can be warranted, given that health care is more complicated and higher risk than inquiring about a lost package, ordering groceries, or applying for a mortgage. At the same time, many of the consumer engagement tools used to guide an applicant through the multiple steps and complexities of their home loan process or to prompt viewers to select new shows to binge have applications in health care.
Over the past few years, technologies have emerged that guide patients through complex care journeys and allow care teams to monitor and engage patients between visits. These solutions come in different formats, but generally patients can receive messages on their phones that contain disease-specific educational content, prompts to fill prescriptions and take medications, and reminders and guidance on how to prepare for appointments and procedures. These programs also collect relevant data from patients through survey and electronic patient-reported outcomes instruments, as well as connected patient monitoring devices, that help track patient progress and identify issues as they arise. Many programs also incorporate symptom triage pathways and use natural language processing to respond automatically to patient questions and concerns.3,4
These technology solutions can automate many tasks that in the past required a care team member to spend hours on the phone. Newly freed from such repetitive tasks, care teams can now focus on more in-depth interactions with those patients who are most in need—the types of interactions that are more satisfying and rewarding. Such assistance is particularly needed today with the staffing shortages faced by most health systems.5
In addition, technology allows teams to see the panel of patients they are caring for and to quickly identify and take action on any specific needs or issues. Care teams can focus on any patient and see where they are in their journey. When appropriate, some solutions also allow care teams to engage directly with patients through text-messaging, creating a seamless experience and unified communication channel. Ideally, these solutions should be linked or embedded within the electronic health record or other primary system of record, so that teams can easily access these tools through their existing workflows and avoid creating yet another interface to navigate.
The Impact of Low-Tech Solutions to Deliver High-Touch Support
There is evidence showing that digital patient navigation tools impact patient care. In the oncology setting, patients with a digital navigator have achieved over 95% adherence rates with complex oral chemotherapy regimens (Memora Health Unpublished Data. 2022.). In the postpartum setting, a text message–based program improved screening rates for postpartum depression and did so with very high patient satisfaction ratings.6 Particularly notable is the fact that this depression screening program achieved these results in a population that was predominantly low income, with more than half belonging to underrepresented minority populations.6
We believe these digital patient navigation technologies, specifically low-tech solutions that don’t require app downloads, portal log-ins, or high-speed internet, will transform care delivery over the next 5 to 10 years. Successful management of complex conditions like diabetes or cancer requires more than 3 hours of care each day,7 yet most patients spend only 1 or 2 hours per month directly interacting with their health care providers. However, most patients carry their phones with them at all times, and artificial intelligence–enabled text support is “always on” to provide support, monitoring, and guidance, wherever a patient happens to be when assistance is needed.
Shifting the Model to Support a Lifetime of Care
While still in the early stages of development, these tools have the potential to radically alter the practice of medicine, shifting the focus from episodic interactions to continuous journey-based care delivery. Outside of an acute event bringing a patient into the clinic or emergency room, many patients go a year or more without seeing their primary care providers.8 During that time, an immense amount of information is underreported or completely lost. Capturing this information in real-time and more holistically over a person’s lifetime of care could provide physicians better insight to both better manage and more fully evaluate the success of treatment plans by tracking patient symptoms, pain, and functional status over time. With this more longitudinal view of the patient, we see a pathway towards achieving the Quadruple Aim: patients who are more supported will achieve better outcomes at lower cost, they will have a better experience, and care teams will be empowered to focus their time on more satisfying activities rather than repetitive administrative tasks.
Corresponding author: James A. Colbert, MD, MBA; [email protected]
Disclosures: Dr. Flyckt and Dr. Colbert are employed by Memora Health, an organization that helps health care systems digitize and automate care journeys.
From Memora Health (Dr. Flyckt and Dr. Colbert), San Francisco, CA; and Harvard Medical School (Dr. Colbert), Boston, MA.
A close relative was recently diagnosed with follicular lymphoma. He was cared for at a high-ranked cancer center by physicians with demonstrated expertise, and even had the support of a care navigator. Still, he was often left feeling overwhelmed and confused, holding an inch-thick stack of papers, instructions, and pamphlets. As he left his treatment planning visit, reeling from the emotional burden of his diagnosis and all the unfamiliar terminology, he didn’t know what to do or what to expect. Later, when he experienced early signs of tumor lysis syndrome, he struggled to reach his care team for triage and guidance. When he went to the emergency room, his oncologist was never informed.
This scenario is unfortunately common, and versions of this scenario play out thousands of times each day across the US health system. Within the clinic and hospital setting, patients receive excellent care from their providers, but a disconnect emerges once the patient leaves these medical settings: patients at home struggle to find guidance and support, while care teams lack the tools to engage patients between visits or monitor their health across care settings, providers, or episodes of care.
Leveraging Technology to Move From Episodes of Care to Complex Care Journeys
The use of automated messaging, artificial intelligence and natural language processing–driven chat experiences, and text-based support is becoming more common. However, health care lags behind other industries in the adoption of these technologies.1,2 The slow pace can be warranted, given that health care is more complicated and higher risk than inquiring about a lost package, ordering groceries, or applying for a mortgage. At the same time, many of the consumer engagement tools used to guide an applicant through the multiple steps and complexities of their home loan process or to prompt viewers to select new shows to binge have applications in health care.
Over the past few years, technologies have emerged that guide patients through complex care journeys and allow care teams to monitor and engage patients between visits. These solutions come in different formats, but generally patients can receive messages on their phones that contain disease-specific educational content, prompts to fill prescriptions and take medications, and reminders and guidance on how to prepare for appointments and procedures. These programs also collect relevant data from patients through survey and electronic patient-reported outcomes instruments, as well as connected patient monitoring devices, that help track patient progress and identify issues as they arise. Many programs also incorporate symptom triage pathways and use natural language processing to respond automatically to patient questions and concerns.3,4
These technology solutions can automate many tasks that in the past required a care team member to spend hours on the phone. Newly freed from such repetitive tasks, care teams can now focus on more in-depth interactions with those patients who are most in need—the types of interactions that are more satisfying and rewarding. Such assistance is particularly needed today with the staffing shortages faced by most health systems.5
In addition, technology allows teams to see the panel of patients they are caring for and to quickly identify and take action on any specific needs or issues. Care teams can focus on any patient and see where they are in their journey. When appropriate, some solutions also allow care teams to engage directly with patients through text-messaging, creating a seamless experience and unified communication channel. Ideally, these solutions should be linked or embedded within the electronic health record or other primary system of record, so that teams can easily access these tools through their existing workflows and avoid creating yet another interface to navigate.
The Impact of Low-Tech Solutions to Deliver High-Touch Support
There is evidence showing that digital patient navigation tools impact patient care. In the oncology setting, patients with a digital navigator have achieved over 95% adherence rates with complex oral chemotherapy regimens (Memora Health Unpublished Data. 2022.). In the postpartum setting, a text message–based program improved screening rates for postpartum depression and did so with very high patient satisfaction ratings.6 Particularly notable is the fact that this depression screening program achieved these results in a population that was predominantly low income, with more than half belonging to underrepresented minority populations.6
We believe these digital patient navigation technologies, specifically low-tech solutions that don’t require app downloads, portal log-ins, or high-speed internet, will transform care delivery over the next 5 to 10 years. Successful management of complex conditions like diabetes or cancer requires more than 3 hours of care each day,7 yet most patients spend only 1 or 2 hours per month directly interacting with their health care providers. However, most patients carry their phones with them at all times, and artificial intelligence–enabled text support is “always on” to provide support, monitoring, and guidance, wherever a patient happens to be when assistance is needed.
Shifting the Model to Support a Lifetime of Care
While still in the early stages of development, these tools have the potential to radically alter the practice of medicine, shifting the focus from episodic interactions to continuous journey-based care delivery. Outside of an acute event bringing a patient into the clinic or emergency room, many patients go a year or more without seeing their primary care providers.8 During that time, an immense amount of information is underreported or completely lost. Capturing this information in real-time and more holistically over a person’s lifetime of care could provide physicians better insight to both better manage and more fully evaluate the success of treatment plans by tracking patient symptoms, pain, and functional status over time. With this more longitudinal view of the patient, we see a pathway towards achieving the Quadruple Aim: patients who are more supported will achieve better outcomes at lower cost, they will have a better experience, and care teams will be empowered to focus their time on more satisfying activities rather than repetitive administrative tasks.
Corresponding author: James A. Colbert, MD, MBA; [email protected]
Disclosures: Dr. Flyckt and Dr. Colbert are employed by Memora Health, an organization that helps health care systems digitize and automate care journeys.
1. Hermes S, Riasanow T, Clemons EK, et al. The digital transformation of the healthcare industry: exploring the rise of emerging platform ecosystems and their influence on the role of patients. Bus Res. 2020;13:1033-1069. doi:10.1007/s40685-020-00125-x
2. Van Velthoven MH, Cordon C. Sustainable adoption of digital health innovations: perspectives from a stakeholder workshop. J Med Internet Res. 2019;21(3):e11922. doi:10.2196/11922
3. Campbell K, Louie P, Levine B, Gililland J. Using patient engagement platforms in the postoperative management of patients. Curr Rev Musculoskelet Med. 2020;13(4):479-484. doi:10.1007/s12178-020-09638-8
4. Xu L, Sanders L, Li K, Chow JCL. Chatbot for health care and oncology applications using artificial intelligence and machine learning: systematic review. JMIR Cancer. 2021;7(4):e27850. doi:10.2196/27850
5. Data brief: health care workforce challenges threaten hospitals’ ability to care for patients. American Hospital Association. Accessed July 24, 2022. www.aha.org/fact-sheets/2021-11-01-data-brief-health-care-workforce-challenges-threaten-hospitals-ability-care
6. Gaulton JS, Leitner K, Hahn L, et al. Healing at home: applying innovation principles to redesign and optimise postpartum care. BMJ Innovations. 2022;8:37-41.
7. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209-214. doi:10.1370/afm.310
8. Ganguli I, Shi Z, E. Orav J, et al. Declining use of primary care among commercially insured adults in the united states, 2008–2016. Ann Intern Med. 2020;172:240-247. doi:10.7326/M19-1834
1. Hermes S, Riasanow T, Clemons EK, et al. The digital transformation of the healthcare industry: exploring the rise of emerging platform ecosystems and their influence on the role of patients. Bus Res. 2020;13:1033-1069. doi:10.1007/s40685-020-00125-x
2. Van Velthoven MH, Cordon C. Sustainable adoption of digital health innovations: perspectives from a stakeholder workshop. J Med Internet Res. 2019;21(3):e11922. doi:10.2196/11922
3. Campbell K, Louie P, Levine B, Gililland J. Using patient engagement platforms in the postoperative management of patients. Curr Rev Musculoskelet Med. 2020;13(4):479-484. doi:10.1007/s12178-020-09638-8
4. Xu L, Sanders L, Li K, Chow JCL. Chatbot for health care and oncology applications using artificial intelligence and machine learning: systematic review. JMIR Cancer. 2021;7(4):e27850. doi:10.2196/27850
5. Data brief: health care workforce challenges threaten hospitals’ ability to care for patients. American Hospital Association. Accessed July 24, 2022. www.aha.org/fact-sheets/2021-11-01-data-brief-health-care-workforce-challenges-threaten-hospitals-ability-care
6. Gaulton JS, Leitner K, Hahn L, et al. Healing at home: applying innovation principles to redesign and optimise postpartum care. BMJ Innovations. 2022;8:37-41.
7. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209-214. doi:10.1370/afm.310
8. Ganguli I, Shi Z, E. Orav J, et al. Declining use of primary care among commercially insured adults in the united states, 2008–2016. Ann Intern Med. 2020;172:240-247. doi:10.7326/M19-1834
The Mission of Continuous Improvement in Health Care: A New Era for Clinical Outcomes Management
This issue of the Journal of Clinical Outcomes (JCOM) debuts a new cover design that brings forward the articles and features in each issue. Although the Journal’s cover has a new look, JCOM’s goals remain the same—improving care by disseminating evidence of quality improvement in health care and sharing access to the medical literature with our readers. We continue our mission to promote the best medical practice by providing clinicians with updates and communicating advances that lead to measurable improvement in health care delivery, quality, and outcomes.
As we continue the work of improving health care quality, knowledge gaps and unmet needs in the literature remain. These unmet needs are evident throughout all phases of health care delivery. Moreover, the Institutes of Medicine report that centered on efforts to build a safer health care environment by redesigning health care processes remains salient.1 The journey to continuous improvement in health care, where we achieve threshold change in the quality of each process and across the entire health care system, requires collective effort. Such efforts include establishing clear metrics and measurements for improvement goals throughout the patient’s journey through diagnosis, treatment, transitions of care, and disease management.2,3 To address evidence and knowledge gaps in the literature, JCOM publishes reports of original studies and quality improvement projects as well as reviews, providing its 30,000 readers with new evidence to implement in daily practice. We welcome submissions of original research reports, reports of quality improvement projects that follow the SQUIRE 2.0 standards,4 and perspectives on developments and innovations in health care delivery.
The next chapter in health care delivery improvement will encompass value-based care.5 This new era of clinical outcomes management will dictate the metrics and outcomes reporting6 and how to plan future investments. The value-based phase will increase innovation and shape policies that advance population health, transforming every step in the care delivery journey.7 The next phase in health care delivery will also create a viable financial structure while implementing effective performance measures for optimal outcomes through patient-centered care and optimization of cost and care strategies. In light of health care’s evolution toward a value-based model, JCOM welcomes submissions of manuscripts that explore themes central to this model, including patient-centered care, implementation of best practices, system design, safety, cost-effectiveness, and the balance between cost optimization and quality. For JCOM’s authors and readers, our editorial team remains commited to the highest standards in timely publishing to support our community through our collective expertise and dedication to quality improvement.
Corresponding author: Ebrahim Barkoudah, MD, MPH, Department of Medicine, Brigham and Women’s Hospital, Boston, MA; [email protected]
1. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000.
2. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-10. doi:10.1136/bmjqs-2014-003675
3. Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm. 2007;64(14 Suppl 9):S3-9. doi:10.2146/ajhp070190
4. Revised Standards for Quality Improvement Reporting Excellence. SQUIRE 2.0. Accessed July 25, 2022. http://squire-statement.org
5. Gray M. Value based healthcare. BMJ. 2017;356:j437. doi:10.1136/bmj.j437
6. What is value-based healthcare? NEJM Catalyst. January 1, 2017. Accessed July 25, 2022. catalyst.nejm.org/doi/full/10.1056/CAT.17.0558
7. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business Press; 2006.
This issue of the Journal of Clinical Outcomes (JCOM) debuts a new cover design that brings forward the articles and features in each issue. Although the Journal’s cover has a new look, JCOM’s goals remain the same—improving care by disseminating evidence of quality improvement in health care and sharing access to the medical literature with our readers. We continue our mission to promote the best medical practice by providing clinicians with updates and communicating advances that lead to measurable improvement in health care delivery, quality, and outcomes.
As we continue the work of improving health care quality, knowledge gaps and unmet needs in the literature remain. These unmet needs are evident throughout all phases of health care delivery. Moreover, the Institutes of Medicine report that centered on efforts to build a safer health care environment by redesigning health care processes remains salient.1 The journey to continuous improvement in health care, where we achieve threshold change in the quality of each process and across the entire health care system, requires collective effort. Such efforts include establishing clear metrics and measurements for improvement goals throughout the patient’s journey through diagnosis, treatment, transitions of care, and disease management.2,3 To address evidence and knowledge gaps in the literature, JCOM publishes reports of original studies and quality improvement projects as well as reviews, providing its 30,000 readers with new evidence to implement in daily practice. We welcome submissions of original research reports, reports of quality improvement projects that follow the SQUIRE 2.0 standards,4 and perspectives on developments and innovations in health care delivery.
The next chapter in health care delivery improvement will encompass value-based care.5 This new era of clinical outcomes management will dictate the metrics and outcomes reporting6 and how to plan future investments. The value-based phase will increase innovation and shape policies that advance population health, transforming every step in the care delivery journey.7 The next phase in health care delivery will also create a viable financial structure while implementing effective performance measures for optimal outcomes through patient-centered care and optimization of cost and care strategies. In light of health care’s evolution toward a value-based model, JCOM welcomes submissions of manuscripts that explore themes central to this model, including patient-centered care, implementation of best practices, system design, safety, cost-effectiveness, and the balance between cost optimization and quality. For JCOM’s authors and readers, our editorial team remains commited to the highest standards in timely publishing to support our community through our collective expertise and dedication to quality improvement.
Corresponding author: Ebrahim Barkoudah, MD, MPH, Department of Medicine, Brigham and Women’s Hospital, Boston, MA; [email protected]
This issue of the Journal of Clinical Outcomes (JCOM) debuts a new cover design that brings forward the articles and features in each issue. Although the Journal’s cover has a new look, JCOM’s goals remain the same—improving care by disseminating evidence of quality improvement in health care and sharing access to the medical literature with our readers. We continue our mission to promote the best medical practice by providing clinicians with updates and communicating advances that lead to measurable improvement in health care delivery, quality, and outcomes.
As we continue the work of improving health care quality, knowledge gaps and unmet needs in the literature remain. These unmet needs are evident throughout all phases of health care delivery. Moreover, the Institutes of Medicine report that centered on efforts to build a safer health care environment by redesigning health care processes remains salient.1 The journey to continuous improvement in health care, where we achieve threshold change in the quality of each process and across the entire health care system, requires collective effort. Such efforts include establishing clear metrics and measurements for improvement goals throughout the patient’s journey through diagnosis, treatment, transitions of care, and disease management.2,3 To address evidence and knowledge gaps in the literature, JCOM publishes reports of original studies and quality improvement projects as well as reviews, providing its 30,000 readers with new evidence to implement in daily practice. We welcome submissions of original research reports, reports of quality improvement projects that follow the SQUIRE 2.0 standards,4 and perspectives on developments and innovations in health care delivery.
The next chapter in health care delivery improvement will encompass value-based care.5 This new era of clinical outcomes management will dictate the metrics and outcomes reporting6 and how to plan future investments. The value-based phase will increase innovation and shape policies that advance population health, transforming every step in the care delivery journey.7 The next phase in health care delivery will also create a viable financial structure while implementing effective performance measures for optimal outcomes through patient-centered care and optimization of cost and care strategies. In light of health care’s evolution toward a value-based model, JCOM welcomes submissions of manuscripts that explore themes central to this model, including patient-centered care, implementation of best practices, system design, safety, cost-effectiveness, and the balance between cost optimization and quality. For JCOM’s authors and readers, our editorial team remains commited to the highest standards in timely publishing to support our community through our collective expertise and dedication to quality improvement.
Corresponding author: Ebrahim Barkoudah, MD, MPH, Department of Medicine, Brigham and Women’s Hospital, Boston, MA; [email protected]
1. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000.
2. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-10. doi:10.1136/bmjqs-2014-003675
3. Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm. 2007;64(14 Suppl 9):S3-9. doi:10.2146/ajhp070190
4. Revised Standards for Quality Improvement Reporting Excellence. SQUIRE 2.0. Accessed July 25, 2022. http://squire-statement.org
5. Gray M. Value based healthcare. BMJ. 2017;356:j437. doi:10.1136/bmj.j437
6. What is value-based healthcare? NEJM Catalyst. January 1, 2017. Accessed July 25, 2022. catalyst.nejm.org/doi/full/10.1056/CAT.17.0558
7. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business Press; 2006.
1. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000.
2. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-10. doi:10.1136/bmjqs-2014-003675
3. Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm. 2007;64(14 Suppl 9):S3-9. doi:10.2146/ajhp070190
4. Revised Standards for Quality Improvement Reporting Excellence. SQUIRE 2.0. Accessed July 25, 2022. http://squire-statement.org
5. Gray M. Value based healthcare. BMJ. 2017;356:j437. doi:10.1136/bmj.j437
6. What is value-based healthcare? NEJM Catalyst. January 1, 2017. Accessed July 25, 2022. catalyst.nejm.org/doi/full/10.1056/CAT.17.0558
7. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business Press; 2006.
Geriatric-Centered Interdisciplinary Care Pathway Reduces Delirium in Hospitalized Older Adults With Traumatic Injury
Study 1 Overview (Park et al)
Objective: To examine whether implementation of a geriatric trauma clinical pathway is associated with reduced rates of delirium in older adults with traumatic injury.
Design: Retrospective case-control study of electronic health records.
Setting and participants: Eligible patients were persons aged 65 years or older who were admitted to the trauma service and did not undergo an operation. A Geriatric Trauma Care Pathway was developed by a multidisciplinary Stanford Quality Pathways team and formally launched on November 1, 2018. The clinical pathway was designed to incorporate geriatric best practices, which included order sets (eg, age-appropriate nonpharmacological interventions and pharmacological dosages), guidelines (eg, Institute for Healthcare Improvement Age-Friendly Health systems 4M framework), automated consultations (comprehensive geriatric assessment), and escalation pathways executed by a multidisciplinary team (eg, pain, bowel, and sleep regulation). The clinical pathway began with admission to the emergency department (ED) (ie, automatic trigger of geriatric trauma care admission order set), daily multidisciplinary team meetings during acute hospitalization, and a transitional care team consultation for postdischarge follow-up or home visit.
Main outcome measures: The primary outcome was delirium as determined by a positive Confusion Assessment Method (CAM) score or a diagnosis of delirium by the clinical team. The secondary outcome was hospital length of stay (LOS). Process measures for pathway compliance (eg, achieving adequate pain control, early mobilization, advance care planning) were assessed. Outcome measures were compared between patients who underwent the Geriatric Trauma Care Pathway intervention (postimplementation group) vs patients who were treated prior to pathway implementation (baseline pre-implementation group).
Main results: Of the 859 eligible patients, 712 were included in the analysis (442 [62.1%] in the baseline pre-implementation group and 270 [37.9%] in the postimplementation group); mean (SD) age was 81.4 (9.1) years, and 394 (55.3%) were women. The injury mechanism was similar between groups, with falls being the most common cause of injury (247 [55.9%] in the baseline group vs 162 [60.0%] in the postimplementation group; P = .43). Injuries as measured by Injury Severity Score (ISS) were minor or moderate in both groups (261 [59.0%] in baseline group vs 168 [62.2%] in postimplementation group; P = .87). The adjusted odds ratio (OR) for delirium in the postimplementation group was lower compared to the baseline pre-implementation group (OR, 0.54; 95% CI, 0.37-0.80; P < .001). Measures of advance care planning in the postimplementation group improved, including more frequent goals-of-care documentation (53.7% in postimplementation group vs 16.7% in baseline group; P < .001) and a shortened time to first goals-of-care discussion upon presenting to the ED (36 hours in postimplementation group vs 50 hours in baseline group; P = .03).
Conclusion: Implementation of a multidisciplinary geriatric trauma clinical pathway for older adults with traumatic injury at a single level I trauma center was associated with reduced rates of delirium.
Study 2 Overview (Bryant et al)
Objective: To determine whether an interdisciplinary care pathway for frail trauma patients can improve in-hospital mortality, complications, and 30-day readmissions.
Design: Retrospective cohort study of frail patients.
Setting and participants: Eligible patients were persons aged 65 years or older who were admitted to the trauma service and survived more than 24 hours; admitted to and discharged from the trauma unit; and determined to be pre-frail or frail by a geriatrician’s assessment. A Frailty Identification and Care Pathway designed to reduce delirium and complications in frail older trauma patients was developed by a multidisciplinary team and implemented in 2016. The standardized evidence-based interdisciplinary care pathway included utilization of order sets and interventions for delirium prevention, early ambulation, bowel and pain regimens, nutrition and physical therapy consults, medication management, care-goal setting, and geriatric assessments.
Main outcome measures: The main outcomes were delirium as determined by a positive CAM score, major complications as defined by the Trauma Quality Improvement Project, in-hospital mortality, and 30-day hospital readmission. Outcome measures were compared between patients who underwent Frailty Identification and Care Pathway intervention (postintervention group) vs patients who were treated prior to pathway implementation (pre-intervention group).
Main results: A total of 269 frail patients were included in the analysis (125 in pre-intervention group vs 144 in postintervention group). Patient demographic and admission characteristics were similar between the 2 groups: mean age was 83.5 (7.1) years, 60.6% were women, and median ISS was 10 (interquartile range [IQR], 9-14). The injury mechanism was similar between groups, with falls accounting for 92.8% and 86.1% of injuries in the pre-intervention and postintervention groups, respectively (P = .07). In univariate analysis, the Frailty Identification and Care Pathway intervention was associated with a significant reduction in delirium (12.5% vs 21.6%, P = .04) and 30-day hospital readmission (2.7% vs 9.6%, P = .01) compared to patients in the pre-intervention group. However, rates of major complications (28.5% vs 28.0%, P = 0.93) and in-hospital mortality (4.2% vs 7.2%, P = .28) were similar between the pre-intervention and postintervention groups. In multivariate logistic regression models adjusted for patient characteristics (age, sex, race, ISS), patients in the postintervention group had lower delirium (OR, 0.44; 95% CI, 0.22-0.88; P = .02) and 30-day hospital readmission (OR, 0.25; 95% CI, 0.07-0.84; P = .02) rates compared to those in the pre-intervention group.
Conclusion: Implementation of an interdisciplinary care protocol for frail geriatric trauma patients significantly decreased their risks for in-hospital delirium and 30-day hospital readmission.
Commentary
Traumatic injuries in older adults are associated with higher morbidity and mortality compared to younger patients, with falls and motor vehicle accidents accounting for a majority of these injuries. Astoundingly, up to one-third of this vulnerable population presenting to hospitals with an ISS greater than 15 may die during hospitalization.1 As a result, a large number of studies and clinical trials have focused on interventions that are designed to reduce fall risks, and hence reduce adverse consequences of traumatic injuries that may arise after falls.2 However, this emphasis on falls prevention has overshadowed a need to develop effective geriatric-centered clinical interventions that aim to improve outcomes in older adults who present to hospitals with traumatic injuries. Furthermore, frailty—a geriatric syndrome indicative of an increased state of vulnerability and predictive of adverse outcomes such as delirium—is highly prevalent in older patients with traumatic injury.3 Thus, there is an urgent need to develop novel, hospital-based, traumatic injury–targeting strategies that incorporate a thoughtful redesign of the care framework that includes evidence-based interventions for geriatric syndromes such as delirium and frailty.
The study reported by Park et al (Study 1) represents the latest effort to evaluate inpatient management strategies designed to improve outcomes in hospitalized older adults who have sustained traumatic injury. Through the implementation of a novel multidisciplinary Geriatric Trauma Care Pathway that incorporates geriatric best practices, this intervention was found to be associated with a 46% lower risk of in-hospital delirium. Because of the inclusion of all age-eligible patients across all strata of traumatic injuries, rather than preselecting for those at the highest risk for poor clinical outcomes, the benefits of this intervention extend to those with minor or moderate injury severity. Furthermore, the improvement in delirium (ie, the primary outcome) is particularly meaningful given that delirium is one of the most common hospital-associated complications that increase hospital LOS, discharge to an institution, and mortality in older adults. Finally, the study’s observed reduced time to a first goals-of-care discussion and increased frequency of goals-of-care documentation after intervention should not be overlooked. The improvements in these 2 process measures are highly significant given that advanced care planning, an intervention that helps to align patients’ values, goals, and treatments, is completed at substantially lower rates in older adults in the acute hospital setting.4
Similarly, in an earlier published study, Bryant and colleagues (Study 2) also show that a geriatric-focused interdisciplinary trauma care pathway is associated with delirium risk reduction in hospitalized older trauma patients. Much like Study 1, the Frailty Identification and Care Pathway utilized in Study 2 is an evidence-based interdisciplinary care pathway that includes the use of geriatric assessments, order sets, and geriatric best practices. Moreover, its exclusive inclusion of pre-frail and frail older patients (ie, those at higher risk for poor outcomes) with moderate injury severity (median ISS of 10 [IQR, 9-14]) suggests that this type of care pathway benefits hospitalized older trauma patients, who are particularly vulnerable to adverse complications such as delirium. Moreover, the successful utilization of the FRAIL questionnaire, a validated frailty screening tool, by surgical residents in the ED to initiate this care pathway demonstrates the feasibility of its use in expediting frailty screening in older patients in trauma care.
Application for Clinical Practice and System Implementation
Findings from the 2 studies discussed in this review indicate that implementation of interdisciplinary clinical care pathways predicated on evidence-based geriatric principles and best practices is a promising approach to reduce delirium in hospitalized older trauma patients. These studies have helped to lay the groundwork in outlining the roadmaps (eg, processes and infrastructures) needed to create such clinical pathways. These key elements include: (1) integration of a multidisciplinary committee (eg, representation from trauma, emergency, and geriatric medicine, nursing, physical and occupational therapy, pharmacy, social work) in pathway design and implementation; (2) adaption of evidence-based geriatric best practices (eg, the Institute for Healthcare Improvement Age-Friendly Health System 4M framework [medication, mentation, mobility, what matters]) to prioritize interventions and to design a pathway that incorporates these features; (3) incorporation of comprehensive geriatric assessment by interdisciplinary providers; (4) utilization of validated clinical instruments to assess physical and cognitive functions, frailty, delirium, and social determinants of health; (5) modification of electronic health record systems to encompass order sets that incorporate evidence-based, nonpharmacological and pharmacological interventions to manage symptoms (eg, delirium, pain, bowel movement, sleep, immobility, polypharmacy) essential to quality geriatric care; and (6) integration of patient and caregiver preferences via goals-of-care discussions and corresponding documentation and communication of these goals.
Additionally, these 2 studies imparted some strategies that may facilitate the implementation of interdisciplinary clinical care pathways in trauma care. Examples of such facilitators include: (1) collaboration with champions within each specialty to reinforce education and buy-in; (2) creation of automatically triggered order sets upon patient presentation to the ED that unites distinct features of clinical pathways; (3) adaption and reorganization of existing hospital infrastructures and resources to meet the needs of clinical pathways implementation (eg, utilizing information technology resources to develop electronic health record order sets; using quality department to develop clinical pathway guidelines and electronic outcome dashboards); and (4) development of individualized patient and caregiver education materials based on care needs (eg, principles of delirium prevention and preservation of mobility during hospitalization) to prepare and engage these stakeholders in patient care and recovery.
Practice Points
- A geriatric interdisciplinary care model can be effectively applied to the management of acute trauma in older patients.
- Interdisciplinary clinical pathways should incorporate geriatric best practices and guidelines and age-appropriate order sets to prioritize and integrate care.
—Fred Ko, MD, MS
1. Hashmi A, Ibrahim-Zada I, Rhee P, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76(3):894-901. doi:10.1097/TA.0b013e3182ab0763
2. Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7(7):CD012221. doi:10.1002/14651858.CD012221.pub2
3. Joseph B, Pandit V, Zangbar B, et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg. 2014;149(8):766-772. doi:10.1001/jamasurg.2014.296
4. Hopkins SA, Bentley A, Phillips V, Barclay S. Advance care plans and hospitalized frail older adults: a systematic review. BMJ Support Palliat Care. 2020;10(2):164-174. doi:10.1136/bmjspcare-2019-002093
Study 1 Overview (Park et al)
Objective: To examine whether implementation of a geriatric trauma clinical pathway is associated with reduced rates of delirium in older adults with traumatic injury.
Design: Retrospective case-control study of electronic health records.
Setting and participants: Eligible patients were persons aged 65 years or older who were admitted to the trauma service and did not undergo an operation. A Geriatric Trauma Care Pathway was developed by a multidisciplinary Stanford Quality Pathways team and formally launched on November 1, 2018. The clinical pathway was designed to incorporate geriatric best practices, which included order sets (eg, age-appropriate nonpharmacological interventions and pharmacological dosages), guidelines (eg, Institute for Healthcare Improvement Age-Friendly Health systems 4M framework), automated consultations (comprehensive geriatric assessment), and escalation pathways executed by a multidisciplinary team (eg, pain, bowel, and sleep regulation). The clinical pathway began with admission to the emergency department (ED) (ie, automatic trigger of geriatric trauma care admission order set), daily multidisciplinary team meetings during acute hospitalization, and a transitional care team consultation for postdischarge follow-up or home visit.
Main outcome measures: The primary outcome was delirium as determined by a positive Confusion Assessment Method (CAM) score or a diagnosis of delirium by the clinical team. The secondary outcome was hospital length of stay (LOS). Process measures for pathway compliance (eg, achieving adequate pain control, early mobilization, advance care planning) were assessed. Outcome measures were compared between patients who underwent the Geriatric Trauma Care Pathway intervention (postimplementation group) vs patients who were treated prior to pathway implementation (baseline pre-implementation group).
Main results: Of the 859 eligible patients, 712 were included in the analysis (442 [62.1%] in the baseline pre-implementation group and 270 [37.9%] in the postimplementation group); mean (SD) age was 81.4 (9.1) years, and 394 (55.3%) were women. The injury mechanism was similar between groups, with falls being the most common cause of injury (247 [55.9%] in the baseline group vs 162 [60.0%] in the postimplementation group; P = .43). Injuries as measured by Injury Severity Score (ISS) were minor or moderate in both groups (261 [59.0%] in baseline group vs 168 [62.2%] in postimplementation group; P = .87). The adjusted odds ratio (OR) for delirium in the postimplementation group was lower compared to the baseline pre-implementation group (OR, 0.54; 95% CI, 0.37-0.80; P < .001). Measures of advance care planning in the postimplementation group improved, including more frequent goals-of-care documentation (53.7% in postimplementation group vs 16.7% in baseline group; P < .001) and a shortened time to first goals-of-care discussion upon presenting to the ED (36 hours in postimplementation group vs 50 hours in baseline group; P = .03).
Conclusion: Implementation of a multidisciplinary geriatric trauma clinical pathway for older adults with traumatic injury at a single level I trauma center was associated with reduced rates of delirium.
Study 2 Overview (Bryant et al)
Objective: To determine whether an interdisciplinary care pathway for frail trauma patients can improve in-hospital mortality, complications, and 30-day readmissions.
Design: Retrospective cohort study of frail patients.
Setting and participants: Eligible patients were persons aged 65 years or older who were admitted to the trauma service and survived more than 24 hours; admitted to and discharged from the trauma unit; and determined to be pre-frail or frail by a geriatrician’s assessment. A Frailty Identification and Care Pathway designed to reduce delirium and complications in frail older trauma patients was developed by a multidisciplinary team and implemented in 2016. The standardized evidence-based interdisciplinary care pathway included utilization of order sets and interventions for delirium prevention, early ambulation, bowel and pain regimens, nutrition and physical therapy consults, medication management, care-goal setting, and geriatric assessments.
Main outcome measures: The main outcomes were delirium as determined by a positive CAM score, major complications as defined by the Trauma Quality Improvement Project, in-hospital mortality, and 30-day hospital readmission. Outcome measures were compared between patients who underwent Frailty Identification and Care Pathway intervention (postintervention group) vs patients who were treated prior to pathway implementation (pre-intervention group).
Main results: A total of 269 frail patients were included in the analysis (125 in pre-intervention group vs 144 in postintervention group). Patient demographic and admission characteristics were similar between the 2 groups: mean age was 83.5 (7.1) years, 60.6% were women, and median ISS was 10 (interquartile range [IQR], 9-14). The injury mechanism was similar between groups, with falls accounting for 92.8% and 86.1% of injuries in the pre-intervention and postintervention groups, respectively (P = .07). In univariate analysis, the Frailty Identification and Care Pathway intervention was associated with a significant reduction in delirium (12.5% vs 21.6%, P = .04) and 30-day hospital readmission (2.7% vs 9.6%, P = .01) compared to patients in the pre-intervention group. However, rates of major complications (28.5% vs 28.0%, P = 0.93) and in-hospital mortality (4.2% vs 7.2%, P = .28) were similar between the pre-intervention and postintervention groups. In multivariate logistic regression models adjusted for patient characteristics (age, sex, race, ISS), patients in the postintervention group had lower delirium (OR, 0.44; 95% CI, 0.22-0.88; P = .02) and 30-day hospital readmission (OR, 0.25; 95% CI, 0.07-0.84; P = .02) rates compared to those in the pre-intervention group.
Conclusion: Implementation of an interdisciplinary care protocol for frail geriatric trauma patients significantly decreased their risks for in-hospital delirium and 30-day hospital readmission.
Commentary
Traumatic injuries in older adults are associated with higher morbidity and mortality compared to younger patients, with falls and motor vehicle accidents accounting for a majority of these injuries. Astoundingly, up to one-third of this vulnerable population presenting to hospitals with an ISS greater than 15 may die during hospitalization.1 As a result, a large number of studies and clinical trials have focused on interventions that are designed to reduce fall risks, and hence reduce adverse consequences of traumatic injuries that may arise after falls.2 However, this emphasis on falls prevention has overshadowed a need to develop effective geriatric-centered clinical interventions that aim to improve outcomes in older adults who present to hospitals with traumatic injuries. Furthermore, frailty—a geriatric syndrome indicative of an increased state of vulnerability and predictive of adverse outcomes such as delirium—is highly prevalent in older patients with traumatic injury.3 Thus, there is an urgent need to develop novel, hospital-based, traumatic injury–targeting strategies that incorporate a thoughtful redesign of the care framework that includes evidence-based interventions for geriatric syndromes such as delirium and frailty.
The study reported by Park et al (Study 1) represents the latest effort to evaluate inpatient management strategies designed to improve outcomes in hospitalized older adults who have sustained traumatic injury. Through the implementation of a novel multidisciplinary Geriatric Trauma Care Pathway that incorporates geriatric best practices, this intervention was found to be associated with a 46% lower risk of in-hospital delirium. Because of the inclusion of all age-eligible patients across all strata of traumatic injuries, rather than preselecting for those at the highest risk for poor clinical outcomes, the benefits of this intervention extend to those with minor or moderate injury severity. Furthermore, the improvement in delirium (ie, the primary outcome) is particularly meaningful given that delirium is one of the most common hospital-associated complications that increase hospital LOS, discharge to an institution, and mortality in older adults. Finally, the study’s observed reduced time to a first goals-of-care discussion and increased frequency of goals-of-care documentation after intervention should not be overlooked. The improvements in these 2 process measures are highly significant given that advanced care planning, an intervention that helps to align patients’ values, goals, and treatments, is completed at substantially lower rates in older adults in the acute hospital setting.4
Similarly, in an earlier published study, Bryant and colleagues (Study 2) also show that a geriatric-focused interdisciplinary trauma care pathway is associated with delirium risk reduction in hospitalized older trauma patients. Much like Study 1, the Frailty Identification and Care Pathway utilized in Study 2 is an evidence-based interdisciplinary care pathway that includes the use of geriatric assessments, order sets, and geriatric best practices. Moreover, its exclusive inclusion of pre-frail and frail older patients (ie, those at higher risk for poor outcomes) with moderate injury severity (median ISS of 10 [IQR, 9-14]) suggests that this type of care pathway benefits hospitalized older trauma patients, who are particularly vulnerable to adverse complications such as delirium. Moreover, the successful utilization of the FRAIL questionnaire, a validated frailty screening tool, by surgical residents in the ED to initiate this care pathway demonstrates the feasibility of its use in expediting frailty screening in older patients in trauma care.
Application for Clinical Practice and System Implementation
Findings from the 2 studies discussed in this review indicate that implementation of interdisciplinary clinical care pathways predicated on evidence-based geriatric principles and best practices is a promising approach to reduce delirium in hospitalized older trauma patients. These studies have helped to lay the groundwork in outlining the roadmaps (eg, processes and infrastructures) needed to create such clinical pathways. These key elements include: (1) integration of a multidisciplinary committee (eg, representation from trauma, emergency, and geriatric medicine, nursing, physical and occupational therapy, pharmacy, social work) in pathway design and implementation; (2) adaption of evidence-based geriatric best practices (eg, the Institute for Healthcare Improvement Age-Friendly Health System 4M framework [medication, mentation, mobility, what matters]) to prioritize interventions and to design a pathway that incorporates these features; (3) incorporation of comprehensive geriatric assessment by interdisciplinary providers; (4) utilization of validated clinical instruments to assess physical and cognitive functions, frailty, delirium, and social determinants of health; (5) modification of electronic health record systems to encompass order sets that incorporate evidence-based, nonpharmacological and pharmacological interventions to manage symptoms (eg, delirium, pain, bowel movement, sleep, immobility, polypharmacy) essential to quality geriatric care; and (6) integration of patient and caregiver preferences via goals-of-care discussions and corresponding documentation and communication of these goals.
Additionally, these 2 studies imparted some strategies that may facilitate the implementation of interdisciplinary clinical care pathways in trauma care. Examples of such facilitators include: (1) collaboration with champions within each specialty to reinforce education and buy-in; (2) creation of automatically triggered order sets upon patient presentation to the ED that unites distinct features of clinical pathways; (3) adaption and reorganization of existing hospital infrastructures and resources to meet the needs of clinical pathways implementation (eg, utilizing information technology resources to develop electronic health record order sets; using quality department to develop clinical pathway guidelines and electronic outcome dashboards); and (4) development of individualized patient and caregiver education materials based on care needs (eg, principles of delirium prevention and preservation of mobility during hospitalization) to prepare and engage these stakeholders in patient care and recovery.
Practice Points
- A geriatric interdisciplinary care model can be effectively applied to the management of acute trauma in older patients.
- Interdisciplinary clinical pathways should incorporate geriatric best practices and guidelines and age-appropriate order sets to prioritize and integrate care.
—Fred Ko, MD, MS
Study 1 Overview (Park et al)
Objective: To examine whether implementation of a geriatric trauma clinical pathway is associated with reduced rates of delirium in older adults with traumatic injury.
Design: Retrospective case-control study of electronic health records.
Setting and participants: Eligible patients were persons aged 65 years or older who were admitted to the trauma service and did not undergo an operation. A Geriatric Trauma Care Pathway was developed by a multidisciplinary Stanford Quality Pathways team and formally launched on November 1, 2018. The clinical pathway was designed to incorporate geriatric best practices, which included order sets (eg, age-appropriate nonpharmacological interventions and pharmacological dosages), guidelines (eg, Institute for Healthcare Improvement Age-Friendly Health systems 4M framework), automated consultations (comprehensive geriatric assessment), and escalation pathways executed by a multidisciplinary team (eg, pain, bowel, and sleep regulation). The clinical pathway began with admission to the emergency department (ED) (ie, automatic trigger of geriatric trauma care admission order set), daily multidisciplinary team meetings during acute hospitalization, and a transitional care team consultation for postdischarge follow-up or home visit.
Main outcome measures: The primary outcome was delirium as determined by a positive Confusion Assessment Method (CAM) score or a diagnosis of delirium by the clinical team. The secondary outcome was hospital length of stay (LOS). Process measures for pathway compliance (eg, achieving adequate pain control, early mobilization, advance care planning) were assessed. Outcome measures were compared between patients who underwent the Geriatric Trauma Care Pathway intervention (postimplementation group) vs patients who were treated prior to pathway implementation (baseline pre-implementation group).
Main results: Of the 859 eligible patients, 712 were included in the analysis (442 [62.1%] in the baseline pre-implementation group and 270 [37.9%] in the postimplementation group); mean (SD) age was 81.4 (9.1) years, and 394 (55.3%) were women. The injury mechanism was similar between groups, with falls being the most common cause of injury (247 [55.9%] in the baseline group vs 162 [60.0%] in the postimplementation group; P = .43). Injuries as measured by Injury Severity Score (ISS) were minor or moderate in both groups (261 [59.0%] in baseline group vs 168 [62.2%] in postimplementation group; P = .87). The adjusted odds ratio (OR) for delirium in the postimplementation group was lower compared to the baseline pre-implementation group (OR, 0.54; 95% CI, 0.37-0.80; P < .001). Measures of advance care planning in the postimplementation group improved, including more frequent goals-of-care documentation (53.7% in postimplementation group vs 16.7% in baseline group; P < .001) and a shortened time to first goals-of-care discussion upon presenting to the ED (36 hours in postimplementation group vs 50 hours in baseline group; P = .03).
Conclusion: Implementation of a multidisciplinary geriatric trauma clinical pathway for older adults with traumatic injury at a single level I trauma center was associated with reduced rates of delirium.
Study 2 Overview (Bryant et al)
Objective: To determine whether an interdisciplinary care pathway for frail trauma patients can improve in-hospital mortality, complications, and 30-day readmissions.
Design: Retrospective cohort study of frail patients.
Setting and participants: Eligible patients were persons aged 65 years or older who were admitted to the trauma service and survived more than 24 hours; admitted to and discharged from the trauma unit; and determined to be pre-frail or frail by a geriatrician’s assessment. A Frailty Identification and Care Pathway designed to reduce delirium and complications in frail older trauma patients was developed by a multidisciplinary team and implemented in 2016. The standardized evidence-based interdisciplinary care pathway included utilization of order sets and interventions for delirium prevention, early ambulation, bowel and pain regimens, nutrition and physical therapy consults, medication management, care-goal setting, and geriatric assessments.
Main outcome measures: The main outcomes were delirium as determined by a positive CAM score, major complications as defined by the Trauma Quality Improvement Project, in-hospital mortality, and 30-day hospital readmission. Outcome measures were compared between patients who underwent Frailty Identification and Care Pathway intervention (postintervention group) vs patients who were treated prior to pathway implementation (pre-intervention group).
Main results: A total of 269 frail patients were included in the analysis (125 in pre-intervention group vs 144 in postintervention group). Patient demographic and admission characteristics were similar between the 2 groups: mean age was 83.5 (7.1) years, 60.6% were women, and median ISS was 10 (interquartile range [IQR], 9-14). The injury mechanism was similar between groups, with falls accounting for 92.8% and 86.1% of injuries in the pre-intervention and postintervention groups, respectively (P = .07). In univariate analysis, the Frailty Identification and Care Pathway intervention was associated with a significant reduction in delirium (12.5% vs 21.6%, P = .04) and 30-day hospital readmission (2.7% vs 9.6%, P = .01) compared to patients in the pre-intervention group. However, rates of major complications (28.5% vs 28.0%, P = 0.93) and in-hospital mortality (4.2% vs 7.2%, P = .28) were similar between the pre-intervention and postintervention groups. In multivariate logistic regression models adjusted for patient characteristics (age, sex, race, ISS), patients in the postintervention group had lower delirium (OR, 0.44; 95% CI, 0.22-0.88; P = .02) and 30-day hospital readmission (OR, 0.25; 95% CI, 0.07-0.84; P = .02) rates compared to those in the pre-intervention group.
Conclusion: Implementation of an interdisciplinary care protocol for frail geriatric trauma patients significantly decreased their risks for in-hospital delirium and 30-day hospital readmission.
Commentary
Traumatic injuries in older adults are associated with higher morbidity and mortality compared to younger patients, with falls and motor vehicle accidents accounting for a majority of these injuries. Astoundingly, up to one-third of this vulnerable population presenting to hospitals with an ISS greater than 15 may die during hospitalization.1 As a result, a large number of studies and clinical trials have focused on interventions that are designed to reduce fall risks, and hence reduce adverse consequences of traumatic injuries that may arise after falls.2 However, this emphasis on falls prevention has overshadowed a need to develop effective geriatric-centered clinical interventions that aim to improve outcomes in older adults who present to hospitals with traumatic injuries. Furthermore, frailty—a geriatric syndrome indicative of an increased state of vulnerability and predictive of adverse outcomes such as delirium—is highly prevalent in older patients with traumatic injury.3 Thus, there is an urgent need to develop novel, hospital-based, traumatic injury–targeting strategies that incorporate a thoughtful redesign of the care framework that includes evidence-based interventions for geriatric syndromes such as delirium and frailty.
The study reported by Park et al (Study 1) represents the latest effort to evaluate inpatient management strategies designed to improve outcomes in hospitalized older adults who have sustained traumatic injury. Through the implementation of a novel multidisciplinary Geriatric Trauma Care Pathway that incorporates geriatric best practices, this intervention was found to be associated with a 46% lower risk of in-hospital delirium. Because of the inclusion of all age-eligible patients across all strata of traumatic injuries, rather than preselecting for those at the highest risk for poor clinical outcomes, the benefits of this intervention extend to those with minor or moderate injury severity. Furthermore, the improvement in delirium (ie, the primary outcome) is particularly meaningful given that delirium is one of the most common hospital-associated complications that increase hospital LOS, discharge to an institution, and mortality in older adults. Finally, the study’s observed reduced time to a first goals-of-care discussion and increased frequency of goals-of-care documentation after intervention should not be overlooked. The improvements in these 2 process measures are highly significant given that advanced care planning, an intervention that helps to align patients’ values, goals, and treatments, is completed at substantially lower rates in older adults in the acute hospital setting.4
Similarly, in an earlier published study, Bryant and colleagues (Study 2) also show that a geriatric-focused interdisciplinary trauma care pathway is associated with delirium risk reduction in hospitalized older trauma patients. Much like Study 1, the Frailty Identification and Care Pathway utilized in Study 2 is an evidence-based interdisciplinary care pathway that includes the use of geriatric assessments, order sets, and geriatric best practices. Moreover, its exclusive inclusion of pre-frail and frail older patients (ie, those at higher risk for poor outcomes) with moderate injury severity (median ISS of 10 [IQR, 9-14]) suggests that this type of care pathway benefits hospitalized older trauma patients, who are particularly vulnerable to adverse complications such as delirium. Moreover, the successful utilization of the FRAIL questionnaire, a validated frailty screening tool, by surgical residents in the ED to initiate this care pathway demonstrates the feasibility of its use in expediting frailty screening in older patients in trauma care.
Application for Clinical Practice and System Implementation
Findings from the 2 studies discussed in this review indicate that implementation of interdisciplinary clinical care pathways predicated on evidence-based geriatric principles and best practices is a promising approach to reduce delirium in hospitalized older trauma patients. These studies have helped to lay the groundwork in outlining the roadmaps (eg, processes and infrastructures) needed to create such clinical pathways. These key elements include: (1) integration of a multidisciplinary committee (eg, representation from trauma, emergency, and geriatric medicine, nursing, physical and occupational therapy, pharmacy, social work) in pathway design and implementation; (2) adaption of evidence-based geriatric best practices (eg, the Institute for Healthcare Improvement Age-Friendly Health System 4M framework [medication, mentation, mobility, what matters]) to prioritize interventions and to design a pathway that incorporates these features; (3) incorporation of comprehensive geriatric assessment by interdisciplinary providers; (4) utilization of validated clinical instruments to assess physical and cognitive functions, frailty, delirium, and social determinants of health; (5) modification of electronic health record systems to encompass order sets that incorporate evidence-based, nonpharmacological and pharmacological interventions to manage symptoms (eg, delirium, pain, bowel movement, sleep, immobility, polypharmacy) essential to quality geriatric care; and (6) integration of patient and caregiver preferences via goals-of-care discussions and corresponding documentation and communication of these goals.
Additionally, these 2 studies imparted some strategies that may facilitate the implementation of interdisciplinary clinical care pathways in trauma care. Examples of such facilitators include: (1) collaboration with champions within each specialty to reinforce education and buy-in; (2) creation of automatically triggered order sets upon patient presentation to the ED that unites distinct features of clinical pathways; (3) adaption and reorganization of existing hospital infrastructures and resources to meet the needs of clinical pathways implementation (eg, utilizing information technology resources to develop electronic health record order sets; using quality department to develop clinical pathway guidelines and electronic outcome dashboards); and (4) development of individualized patient and caregiver education materials based on care needs (eg, principles of delirium prevention and preservation of mobility during hospitalization) to prepare and engage these stakeholders in patient care and recovery.
Practice Points
- A geriatric interdisciplinary care model can be effectively applied to the management of acute trauma in older patients.
- Interdisciplinary clinical pathways should incorporate geriatric best practices and guidelines and age-appropriate order sets to prioritize and integrate care.
—Fred Ko, MD, MS
1. Hashmi A, Ibrahim-Zada I, Rhee P, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76(3):894-901. doi:10.1097/TA.0b013e3182ab0763
2. Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7(7):CD012221. doi:10.1002/14651858.CD012221.pub2
3. Joseph B, Pandit V, Zangbar B, et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg. 2014;149(8):766-772. doi:10.1001/jamasurg.2014.296
4. Hopkins SA, Bentley A, Phillips V, Barclay S. Advance care plans and hospitalized frail older adults: a systematic review. BMJ Support Palliat Care. 2020;10(2):164-174. doi:10.1136/bmjspcare-2019-002093
1. Hashmi A, Ibrahim-Zada I, Rhee P, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76(3):894-901. doi:10.1097/TA.0b013e3182ab0763
2. Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7(7):CD012221. doi:10.1002/14651858.CD012221.pub2
3. Joseph B, Pandit V, Zangbar B, et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg. 2014;149(8):766-772. doi:10.1001/jamasurg.2014.296
4. Hopkins SA, Bentley A, Phillips V, Barclay S. Advance care plans and hospitalized frail older adults: a systematic review. BMJ Support Palliat Care. 2020;10(2):164-174. doi:10.1136/bmjspcare-2019-002093
CRC screening coverage continuum is complete
In a huge win for patients, Medicare will begin covering colonoscopies after a positive noninvasive stool test starting in 2023. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at HHS and legislative pressure by members across the country.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening program and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test,” said David Lieberman, MD, AGAF, who met with Centers for Medicare & Medicaid Services officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” said AGA president John Carethers, MD, AGAF, who met with CMS in early July to advocate for this change.
Thank you to everyone in the GI community who advocated for this important change!
CMS announced the coverage change as part of the 2023 Medicare proposed rule, which was released July 7, 2022. The rule must be finalized this fall before taking effect Jan. 2, 2023.
In a huge win for patients, Medicare will begin covering colonoscopies after a positive noninvasive stool test starting in 2023. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at HHS and legislative pressure by members across the country.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening program and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test,” said David Lieberman, MD, AGAF, who met with Centers for Medicare & Medicaid Services officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” said AGA president John Carethers, MD, AGAF, who met with CMS in early July to advocate for this change.
Thank you to everyone in the GI community who advocated for this important change!
CMS announced the coverage change as part of the 2023 Medicare proposed rule, which was released July 7, 2022. The rule must be finalized this fall before taking effect Jan. 2, 2023.
In a huge win for patients, Medicare will begin covering colonoscopies after a positive noninvasive stool test starting in 2023. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at HHS and legislative pressure by members across the country.
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening program and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive noninvasive screening test,” said David Lieberman, MD, AGAF, who met with Centers for Medicare & Medicaid Services officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
“This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” said AGA president John Carethers, MD, AGAF, who met with CMS in early July to advocate for this change.
Thank you to everyone in the GI community who advocated for this important change!
CMS announced the coverage change as part of the 2023 Medicare proposed rule, which was released July 7, 2022. The rule must be finalized this fall before taking effect Jan. 2, 2023.
Don’t let insurance policies burden GI practices
Join us at AGA Advocacy Day on Thursday, Sept. 22, 2022, to virtually meet with your members of Congress to urge them to rein in insurance policies like prior authorization and step therapy.
If GI providers don’t have a seat at the table and engage with lawmakers, these decisions will be influenced by payers and other parties that do not have your or your patients’ best interests at heart.
AGA Advocacy Day is held shortly before the end of the fiscal year – prime time to educate policymakers and their staff about your everyday challenges and the reality of GI patient care in your state. We will also discuss the need for robust federal funding for GI research and the devastating impact that Medicare cuts could have on your practice.
Register today and AGA will take care of the rest, including scheduling your meetings and providing comprehensive advocacy training. Now more than ever, your voice needs to be heard on Capitol Hill.
Join us at AGA Advocacy Day on Thursday, Sept. 22, 2022, to virtually meet with your members of Congress to urge them to rein in insurance policies like prior authorization and step therapy.
If GI providers don’t have a seat at the table and engage with lawmakers, these decisions will be influenced by payers and other parties that do not have your or your patients’ best interests at heart.
AGA Advocacy Day is held shortly before the end of the fiscal year – prime time to educate policymakers and their staff about your everyday challenges and the reality of GI patient care in your state. We will also discuss the need for robust federal funding for GI research and the devastating impact that Medicare cuts could have on your practice.
Register today and AGA will take care of the rest, including scheduling your meetings and providing comprehensive advocacy training. Now more than ever, your voice needs to be heard on Capitol Hill.
Join us at AGA Advocacy Day on Thursday, Sept. 22, 2022, to virtually meet with your members of Congress to urge them to rein in insurance policies like prior authorization and step therapy.
If GI providers don’t have a seat at the table and engage with lawmakers, these decisions will be influenced by payers and other parties that do not have your or your patients’ best interests at heart.
AGA Advocacy Day is held shortly before the end of the fiscal year – prime time to educate policymakers and their staff about your everyday challenges and the reality of GI patient care in your state. We will also discuss the need for robust federal funding for GI research and the devastating impact that Medicare cuts could have on your practice.
Register today and AGA will take care of the rest, including scheduling your meetings and providing comprehensive advocacy training. Now more than ever, your voice needs to be heard on Capitol Hill.
Understanding proposed changes to Medicare payment policies
On July 7, the Centers for Medicare & Medicaid Services released the calendar year (CY) 2023 Medicare Physician Fee Schedule Proposed Rule and can now be found in the Federal Register.
Good news!
In a win for patients, and thanks to collective advocacy efforts from AGA and partner societies, CMS is proposing to expand the regulatory definition of “colorectal cancer screening tests” and waive cost sharing for a necessary follow-up colonoscopy after a positive stool-based screening test.
Looming cuts
The rule proposes 4% cuts to Medicare physician reimbursement through required decreases in the conversion factor and expiration of temporary fixes passed by Congress. AGA will continue to work with a coalition of national and state medical societies in urging Congress to prevent these cuts before Jan. 1, 2023.
What to know
- CMS expands colorectal cancer screening in a proposal to waive cost sharing for a follow-up colonoscopy to a positive stool-based colorectal cancer screening test and to cover the service for individuals 45 years of age and above.
- Medicare payment cuts are looming with cuts to the proposed CY 2023 conversion factor.
- Split/shared visits policy delayed until CY 2024.
- Payment rates for new bariatric device codes proposed.
On July 7, the Centers for Medicare & Medicaid Services released the calendar year (CY) 2023 Medicare Physician Fee Schedule Proposed Rule and can now be found in the Federal Register.
Good news!
In a win for patients, and thanks to collective advocacy efforts from AGA and partner societies, CMS is proposing to expand the regulatory definition of “colorectal cancer screening tests” and waive cost sharing for a necessary follow-up colonoscopy after a positive stool-based screening test.
Looming cuts
The rule proposes 4% cuts to Medicare physician reimbursement through required decreases in the conversion factor and expiration of temporary fixes passed by Congress. AGA will continue to work with a coalition of national and state medical societies in urging Congress to prevent these cuts before Jan. 1, 2023.
What to know
- CMS expands colorectal cancer screening in a proposal to waive cost sharing for a follow-up colonoscopy to a positive stool-based colorectal cancer screening test and to cover the service for individuals 45 years of age and above.
- Medicare payment cuts are looming with cuts to the proposed CY 2023 conversion factor.
- Split/shared visits policy delayed until CY 2024.
- Payment rates for new bariatric device codes proposed.
On July 7, the Centers for Medicare & Medicaid Services released the calendar year (CY) 2023 Medicare Physician Fee Schedule Proposed Rule and can now be found in the Federal Register.
Good news!
In a win for patients, and thanks to collective advocacy efforts from AGA and partner societies, CMS is proposing to expand the regulatory definition of “colorectal cancer screening tests” and waive cost sharing for a necessary follow-up colonoscopy after a positive stool-based screening test.
Looming cuts
The rule proposes 4% cuts to Medicare physician reimbursement through required decreases in the conversion factor and expiration of temporary fixes passed by Congress. AGA will continue to work with a coalition of national and state medical societies in urging Congress to prevent these cuts before Jan. 1, 2023.
What to know
- CMS expands colorectal cancer screening in a proposal to waive cost sharing for a follow-up colonoscopy to a positive stool-based colorectal cancer screening test and to cover the service for individuals 45 years of age and above.
- Medicare payment cuts are looming with cuts to the proposed CY 2023 conversion factor.
- Split/shared visits policy delayed until CY 2024.
- Payment rates for new bariatric device codes proposed.
Job market for physicians, advanced practitioners rebounds after COVID-19 slump: Report
After a year of uncertainty and decline because of the COVID-19 pandemic, according to a recently released report from Merritt Hawkins, the physician search division of AMN Healthcare.
The study is based on an analysis of job search and consulting assignments that the firm conducted on behalf of its health care organization clients from April 1, 2021, to March 31, 2022.
“Search engagements were down a little over 30% in 2020, but by the end of 2021, everything started spiking dramatically to the point of where we were at a 34-year high,” Michael Belkin, divisional vice president with Merritt Hawkins, told this news organization. “The pendulum has gone all the way back. People are more interested in going out and seeing their physicians.”
Demand for physicians was suppressed during the peak of the pandemic, as many hospitals curtailed elective procedures and many patients refrained from entering a medical facility. A large backlog of patients needing care subsequently developed.
This, combined with an aging population and widespread chronic medical conditions, has caused a strong surge in demand for physicians and advanced practitioners, according to the report.
In addition to the volume of searches increasing, physician starting salaries have rebounded from the COVID-19 downturn.
Average starting salaries of 14 physician specialties tracked in 2021/2022 increased, while only 3 decreased. Orthopedic surgeons were offered an average of $565,000 to start, exclusive of signing bonuses and other incentives, up from $546,000 the previous year. Urologists were offered an average of $510,000 to start, up from $497,000; gastroenterologists were offered $474,000, up from $453,000; while radiologists were offered $455,000, up from $401,000.
Similarly, a recent Medscape study based on responses from more than 13,000 U.S. physicians across 29 specialties found that income for all physician specialists increased, with otolaryngologists, gastroenterologists, and dermatologists experiencing the greatest gains.
A new reality
While the job market for physicians and advanced practitioners has seemingly recovered, there are many differences between today’s working environment for clinicians and what existed during the pandemic.
First, specialists are now stepping into the spotlight, a position that primary care clinicians previously held. The majority of Merritt Hawkins’ search engagements (64%) in 2021/2022 were for physician specialists, including cardiologists, gastroenterologists, orthopedic surgeons, neurologists, oncologists, and others. Only 17% of the search engagements were for primary care physicians, down from 18% in 2020/2021 and 20% in 2019/2020.
“We’ve seen specialties bounce back faster. Of course, you’ve got the aging population; you’ve got people that want that specialized care,” Mr. Belkin said.
Advanced practitioners also are playing a more significant role in the postpandemic word. In fact, 19% of Merritt Hawkins’ search engagements were for advanced practitioners, including nurse practitioners (NPs), physician assistants, and certified registered nurse anesthetists, up from 18% the previous year and just 13% the year prior to that, indicating growing demand for nonphysician providers.
NPs, in fact, topped the list of most requested search engagements, underscoring a shift from traditional physician office-based primary care delivery settings toward “convenient care” settings such as urgent care centers and retail clinics that are largely staffed by NPs and other advanced practitioners.
Advanced practitioners are taking on more responsibility for primary care simply because there is a large number of these professionals ready to take on the challenge.
The health care industry was “not able to produce enough primary care physicians over the last decade. So advanced practitioners, I believe, have slowly started to work alongside those primary care physicians. In a lot of areas such as your retail space, your CVS, your Walmart, your Walgreens, your standalone urgent cares, they’ve stepped up,” Mr. Belkin said.
Advanced practitioners also are providing the convenience that consumers are increasingly demanding.
“We are a society that wants things immediately ... but it’s still a challenge to schedule an appointment with a physician. However, it’s less of a challenge to get into a retail clinic or an urgent care center or to schedule something through telehealth,” Mr. Belkin noted.
More than just money
With the job market strong, the challenge for health care organizations is to create competitive recruiting packages. Sure enough, 92% of candidates were offered signing bonuses in 2021/2022 compared with just 61% in 2020/2021.
The financial incentives, however, might not be enough. In this environment, health care organizations need to go beyond simply offering competitive salaries to new recruits. For example, clinicians are seeking flexibility, as many potential hires are seeking remote positions. In fact, 18% of radiology search engagements were for teleradiologists, while 15% of its search engagements for psychiatrists were for telepsychiatrists in 2021/2022.
“Right now, quality of life is a very important factor. It’s work-life balance. It’s sensitivity to the stresses that we just experienced over the last 2.5 years,” Mr. Belkin concluded. “There’s more sensitivity around the culture of the organizations. What’s the leadership like? How did the organization handle the pandemic? How do they respond?”
A version of this article first appeared on Medscape.com.
After a year of uncertainty and decline because of the COVID-19 pandemic, according to a recently released report from Merritt Hawkins, the physician search division of AMN Healthcare.
The study is based on an analysis of job search and consulting assignments that the firm conducted on behalf of its health care organization clients from April 1, 2021, to March 31, 2022.
“Search engagements were down a little over 30% in 2020, but by the end of 2021, everything started spiking dramatically to the point of where we were at a 34-year high,” Michael Belkin, divisional vice president with Merritt Hawkins, told this news organization. “The pendulum has gone all the way back. People are more interested in going out and seeing their physicians.”
Demand for physicians was suppressed during the peak of the pandemic, as many hospitals curtailed elective procedures and many patients refrained from entering a medical facility. A large backlog of patients needing care subsequently developed.
This, combined with an aging population and widespread chronic medical conditions, has caused a strong surge in demand for physicians and advanced practitioners, according to the report.
In addition to the volume of searches increasing, physician starting salaries have rebounded from the COVID-19 downturn.
Average starting salaries of 14 physician specialties tracked in 2021/2022 increased, while only 3 decreased. Orthopedic surgeons were offered an average of $565,000 to start, exclusive of signing bonuses and other incentives, up from $546,000 the previous year. Urologists were offered an average of $510,000 to start, up from $497,000; gastroenterologists were offered $474,000, up from $453,000; while radiologists were offered $455,000, up from $401,000.
Similarly, a recent Medscape study based on responses from more than 13,000 U.S. physicians across 29 specialties found that income for all physician specialists increased, with otolaryngologists, gastroenterologists, and dermatologists experiencing the greatest gains.
A new reality
While the job market for physicians and advanced practitioners has seemingly recovered, there are many differences between today’s working environment for clinicians and what existed during the pandemic.
First, specialists are now stepping into the spotlight, a position that primary care clinicians previously held. The majority of Merritt Hawkins’ search engagements (64%) in 2021/2022 were for physician specialists, including cardiologists, gastroenterologists, orthopedic surgeons, neurologists, oncologists, and others. Only 17% of the search engagements were for primary care physicians, down from 18% in 2020/2021 and 20% in 2019/2020.
“We’ve seen specialties bounce back faster. Of course, you’ve got the aging population; you’ve got people that want that specialized care,” Mr. Belkin said.
Advanced practitioners also are playing a more significant role in the postpandemic word. In fact, 19% of Merritt Hawkins’ search engagements were for advanced practitioners, including nurse practitioners (NPs), physician assistants, and certified registered nurse anesthetists, up from 18% the previous year and just 13% the year prior to that, indicating growing demand for nonphysician providers.
NPs, in fact, topped the list of most requested search engagements, underscoring a shift from traditional physician office-based primary care delivery settings toward “convenient care” settings such as urgent care centers and retail clinics that are largely staffed by NPs and other advanced practitioners.
Advanced practitioners are taking on more responsibility for primary care simply because there is a large number of these professionals ready to take on the challenge.
The health care industry was “not able to produce enough primary care physicians over the last decade. So advanced practitioners, I believe, have slowly started to work alongside those primary care physicians. In a lot of areas such as your retail space, your CVS, your Walmart, your Walgreens, your standalone urgent cares, they’ve stepped up,” Mr. Belkin said.
Advanced practitioners also are providing the convenience that consumers are increasingly demanding.
“We are a society that wants things immediately ... but it’s still a challenge to schedule an appointment with a physician. However, it’s less of a challenge to get into a retail clinic or an urgent care center or to schedule something through telehealth,” Mr. Belkin noted.
More than just money
With the job market strong, the challenge for health care organizations is to create competitive recruiting packages. Sure enough, 92% of candidates were offered signing bonuses in 2021/2022 compared with just 61% in 2020/2021.
The financial incentives, however, might not be enough. In this environment, health care organizations need to go beyond simply offering competitive salaries to new recruits. For example, clinicians are seeking flexibility, as many potential hires are seeking remote positions. In fact, 18% of radiology search engagements were for teleradiologists, while 15% of its search engagements for psychiatrists were for telepsychiatrists in 2021/2022.
“Right now, quality of life is a very important factor. It’s work-life balance. It’s sensitivity to the stresses that we just experienced over the last 2.5 years,” Mr. Belkin concluded. “There’s more sensitivity around the culture of the organizations. What’s the leadership like? How did the organization handle the pandemic? How do they respond?”
A version of this article first appeared on Medscape.com.
After a year of uncertainty and decline because of the COVID-19 pandemic, according to a recently released report from Merritt Hawkins, the physician search division of AMN Healthcare.
The study is based on an analysis of job search and consulting assignments that the firm conducted on behalf of its health care organization clients from April 1, 2021, to March 31, 2022.
“Search engagements were down a little over 30% in 2020, but by the end of 2021, everything started spiking dramatically to the point of where we were at a 34-year high,” Michael Belkin, divisional vice president with Merritt Hawkins, told this news organization. “The pendulum has gone all the way back. People are more interested in going out and seeing their physicians.”
Demand for physicians was suppressed during the peak of the pandemic, as many hospitals curtailed elective procedures and many patients refrained from entering a medical facility. A large backlog of patients needing care subsequently developed.
This, combined with an aging population and widespread chronic medical conditions, has caused a strong surge in demand for physicians and advanced practitioners, according to the report.
In addition to the volume of searches increasing, physician starting salaries have rebounded from the COVID-19 downturn.
Average starting salaries of 14 physician specialties tracked in 2021/2022 increased, while only 3 decreased. Orthopedic surgeons were offered an average of $565,000 to start, exclusive of signing bonuses and other incentives, up from $546,000 the previous year. Urologists were offered an average of $510,000 to start, up from $497,000; gastroenterologists were offered $474,000, up from $453,000; while radiologists were offered $455,000, up from $401,000.
Similarly, a recent Medscape study based on responses from more than 13,000 U.S. physicians across 29 specialties found that income for all physician specialists increased, with otolaryngologists, gastroenterologists, and dermatologists experiencing the greatest gains.
A new reality
While the job market for physicians and advanced practitioners has seemingly recovered, there are many differences between today’s working environment for clinicians and what existed during the pandemic.
First, specialists are now stepping into the spotlight, a position that primary care clinicians previously held. The majority of Merritt Hawkins’ search engagements (64%) in 2021/2022 were for physician specialists, including cardiologists, gastroenterologists, orthopedic surgeons, neurologists, oncologists, and others. Only 17% of the search engagements were for primary care physicians, down from 18% in 2020/2021 and 20% in 2019/2020.
“We’ve seen specialties bounce back faster. Of course, you’ve got the aging population; you’ve got people that want that specialized care,” Mr. Belkin said.
Advanced practitioners also are playing a more significant role in the postpandemic word. In fact, 19% of Merritt Hawkins’ search engagements were for advanced practitioners, including nurse practitioners (NPs), physician assistants, and certified registered nurse anesthetists, up from 18% the previous year and just 13% the year prior to that, indicating growing demand for nonphysician providers.
NPs, in fact, topped the list of most requested search engagements, underscoring a shift from traditional physician office-based primary care delivery settings toward “convenient care” settings such as urgent care centers and retail clinics that are largely staffed by NPs and other advanced practitioners.
Advanced practitioners are taking on more responsibility for primary care simply because there is a large number of these professionals ready to take on the challenge.
The health care industry was “not able to produce enough primary care physicians over the last decade. So advanced practitioners, I believe, have slowly started to work alongside those primary care physicians. In a lot of areas such as your retail space, your CVS, your Walmart, your Walgreens, your standalone urgent cares, they’ve stepped up,” Mr. Belkin said.
Advanced practitioners also are providing the convenience that consumers are increasingly demanding.
“We are a society that wants things immediately ... but it’s still a challenge to schedule an appointment with a physician. However, it’s less of a challenge to get into a retail clinic or an urgent care center or to schedule something through telehealth,” Mr. Belkin noted.
More than just money
With the job market strong, the challenge for health care organizations is to create competitive recruiting packages. Sure enough, 92% of candidates were offered signing bonuses in 2021/2022 compared with just 61% in 2020/2021.
The financial incentives, however, might not be enough. In this environment, health care organizations need to go beyond simply offering competitive salaries to new recruits. For example, clinicians are seeking flexibility, as many potential hires are seeking remote positions. In fact, 18% of radiology search engagements were for teleradiologists, while 15% of its search engagements for psychiatrists were for telepsychiatrists in 2021/2022.
“Right now, quality of life is a very important factor. It’s work-life balance. It’s sensitivity to the stresses that we just experienced over the last 2.5 years,” Mr. Belkin concluded. “There’s more sensitivity around the culture of the organizations. What’s the leadership like? How did the organization handle the pandemic? How do they respond?”
A version of this article first appeared on Medscape.com.