User login
What are your weaknesses?
In a video posted to TikTok by the comedian Will Flanary, MD, better known to his followers as Dr. Glaucomflecken, he imitates a neurosurgical residency interview. With glasses perched on the bridge of his nose, Dr. Glaucomflecken poses as the attending, asking: “What are your weaknesses?”
The residency applicant answers without hesitation: “My physiological need for sleep.” “What are your strengths?” The resident replies with the hard, steely stare of the determined and uninitiated: “My desire to eliminate my physiological need for sleep.”
If you follow Dr. Glaucomflecken on Twitter, you might know the skit I’m referencing. For many physicians and physicians-in-training, what makes the satire successful is its reflection of reality.
Many things have changed in medicine since his time, but the tired trope of the sleepless surgeon hangs on. Undaunted, I spent my second and third year of medical school accumulating accolades, conducting research, and connecting with mentors with the singular goal of joining the surgical ranks.
Midway through my third year, I completed a month-long surgical subinternship designed to give students a taste of what life would look like as an intern. I loved the operating room; it felt like the difference between being on dry land and being underwater. There were fewer distractions – your patient in the spotlight while everything else receded to the shadows.
However, as the month wore on, something stronger took hold. I couldn’t keep my eyes open in the darkened operating rooms and had to decline stools, fearing that I would fall asleep if I sat down.
On early morning prerounds, it’s 4:50 a.m. when I glance at the clock and pull back the curtain, already apologizing. My patient rolls over, flashing a wry smile. “Do you ever go home?” I’ve seen residents respond to this exact question in various ways. I live here. Yes. No. Soon. Not enough. My partner doesn’t think so.
There are days and, yes, years when we are led to believe this is what we live for: to be constantly available to our patients. It feels like a hollow victory when the patient, 2 days out from a total colectomy, begins to worry about your personal life. I ask her how she slept (not enough), any fevers (no), vomiting (no), urinating (I pause – she has a catheter).
My favorite part of these early morning rounds is the pause in my scripted litany of questions to listen to heart and lungs. It never fails to feel sacred: Patients become so quiet and still that I can’t help but think they have faith in me. Without prompting, she slides the back of her hospital gown forward like a curtain, already taking deep breaths so I can hear her lungs.
I look outside. The streetlights are still on, and from the seventh-floor window, I can watch staff making their way through the sliding double-doors, just beyond the yellowed pools of streetlight. I smile. I love medicine. I’m so tired.
For many in medicine, we are treated, and thus behave, as though our ability to manipulate physiology should also apply within the borders of our bodies: commanding less sleep, food, or bathroom breaks.
It places health care workers solidly in the realm of superhuman, living beyond one’s corporeal needs. The pandemic only heightened this misappropriation – adding hero and setting out a pedestal for health care workers to make their ungainly ascent. This kind of unsolicited admiration implicitly implies inhumanness, an otherness.
What would it look like if we started treating ourselves less like physicians and more like patients? I wish I was offering a solution, but really this is just a story.
To students rising through the ranks of medical training, identify what it is you need early and often. I can count on one hand how many physicians I’ve seen take a lunch break – even 10 minutes. Embrace hard work and self-preservation equally. My hope is that if enough of us take this path, it just might become a matter of course.
Dr. Meffert is a resident in the department of emergency medicine, MedStar Georgetown University Hospital, Washington Hospital Center, Washington. Dr. Meffert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a video posted to TikTok by the comedian Will Flanary, MD, better known to his followers as Dr. Glaucomflecken, he imitates a neurosurgical residency interview. With glasses perched on the bridge of his nose, Dr. Glaucomflecken poses as the attending, asking: “What are your weaknesses?”
The residency applicant answers without hesitation: “My physiological need for sleep.” “What are your strengths?” The resident replies with the hard, steely stare of the determined and uninitiated: “My desire to eliminate my physiological need for sleep.”
If you follow Dr. Glaucomflecken on Twitter, you might know the skit I’m referencing. For many physicians and physicians-in-training, what makes the satire successful is its reflection of reality.
Many things have changed in medicine since his time, but the tired trope of the sleepless surgeon hangs on. Undaunted, I spent my second and third year of medical school accumulating accolades, conducting research, and connecting with mentors with the singular goal of joining the surgical ranks.
Midway through my third year, I completed a month-long surgical subinternship designed to give students a taste of what life would look like as an intern. I loved the operating room; it felt like the difference between being on dry land and being underwater. There were fewer distractions – your patient in the spotlight while everything else receded to the shadows.
However, as the month wore on, something stronger took hold. I couldn’t keep my eyes open in the darkened operating rooms and had to decline stools, fearing that I would fall asleep if I sat down.
On early morning prerounds, it’s 4:50 a.m. when I glance at the clock and pull back the curtain, already apologizing. My patient rolls over, flashing a wry smile. “Do you ever go home?” I’ve seen residents respond to this exact question in various ways. I live here. Yes. No. Soon. Not enough. My partner doesn’t think so.
There are days and, yes, years when we are led to believe this is what we live for: to be constantly available to our patients. It feels like a hollow victory when the patient, 2 days out from a total colectomy, begins to worry about your personal life. I ask her how she slept (not enough), any fevers (no), vomiting (no), urinating (I pause – she has a catheter).
My favorite part of these early morning rounds is the pause in my scripted litany of questions to listen to heart and lungs. It never fails to feel sacred: Patients become so quiet and still that I can’t help but think they have faith in me. Without prompting, she slides the back of her hospital gown forward like a curtain, already taking deep breaths so I can hear her lungs.
I look outside. The streetlights are still on, and from the seventh-floor window, I can watch staff making their way through the sliding double-doors, just beyond the yellowed pools of streetlight. I smile. I love medicine. I’m so tired.
For many in medicine, we are treated, and thus behave, as though our ability to manipulate physiology should also apply within the borders of our bodies: commanding less sleep, food, or bathroom breaks.
It places health care workers solidly in the realm of superhuman, living beyond one’s corporeal needs. The pandemic only heightened this misappropriation – adding hero and setting out a pedestal for health care workers to make their ungainly ascent. This kind of unsolicited admiration implicitly implies inhumanness, an otherness.
What would it look like if we started treating ourselves less like physicians and more like patients? I wish I was offering a solution, but really this is just a story.
To students rising through the ranks of medical training, identify what it is you need early and often. I can count on one hand how many physicians I’ve seen take a lunch break – even 10 minutes. Embrace hard work and self-preservation equally. My hope is that if enough of us take this path, it just might become a matter of course.
Dr. Meffert is a resident in the department of emergency medicine, MedStar Georgetown University Hospital, Washington Hospital Center, Washington. Dr. Meffert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a video posted to TikTok by the comedian Will Flanary, MD, better known to his followers as Dr. Glaucomflecken, he imitates a neurosurgical residency interview. With glasses perched on the bridge of his nose, Dr. Glaucomflecken poses as the attending, asking: “What are your weaknesses?”
The residency applicant answers without hesitation: “My physiological need for sleep.” “What are your strengths?” The resident replies with the hard, steely stare of the determined and uninitiated: “My desire to eliminate my physiological need for sleep.”
If you follow Dr. Glaucomflecken on Twitter, you might know the skit I’m referencing. For many physicians and physicians-in-training, what makes the satire successful is its reflection of reality.
Many things have changed in medicine since his time, but the tired trope of the sleepless surgeon hangs on. Undaunted, I spent my second and third year of medical school accumulating accolades, conducting research, and connecting with mentors with the singular goal of joining the surgical ranks.
Midway through my third year, I completed a month-long surgical subinternship designed to give students a taste of what life would look like as an intern. I loved the operating room; it felt like the difference between being on dry land and being underwater. There were fewer distractions – your patient in the spotlight while everything else receded to the shadows.
However, as the month wore on, something stronger took hold. I couldn’t keep my eyes open in the darkened operating rooms and had to decline stools, fearing that I would fall asleep if I sat down.
On early morning prerounds, it’s 4:50 a.m. when I glance at the clock and pull back the curtain, already apologizing. My patient rolls over, flashing a wry smile. “Do you ever go home?” I’ve seen residents respond to this exact question in various ways. I live here. Yes. No. Soon. Not enough. My partner doesn’t think so.
There are days and, yes, years when we are led to believe this is what we live for: to be constantly available to our patients. It feels like a hollow victory when the patient, 2 days out from a total colectomy, begins to worry about your personal life. I ask her how she slept (not enough), any fevers (no), vomiting (no), urinating (I pause – she has a catheter).
My favorite part of these early morning rounds is the pause in my scripted litany of questions to listen to heart and lungs. It never fails to feel sacred: Patients become so quiet and still that I can’t help but think they have faith in me. Without prompting, she slides the back of her hospital gown forward like a curtain, already taking deep breaths so I can hear her lungs.
I look outside. The streetlights are still on, and from the seventh-floor window, I can watch staff making their way through the sliding double-doors, just beyond the yellowed pools of streetlight. I smile. I love medicine. I’m so tired.
For many in medicine, we are treated, and thus behave, as though our ability to manipulate physiology should also apply within the borders of our bodies: commanding less sleep, food, or bathroom breaks.
It places health care workers solidly in the realm of superhuman, living beyond one’s corporeal needs. The pandemic only heightened this misappropriation – adding hero and setting out a pedestal for health care workers to make their ungainly ascent. This kind of unsolicited admiration implicitly implies inhumanness, an otherness.
What would it look like if we started treating ourselves less like physicians and more like patients? I wish I was offering a solution, but really this is just a story.
To students rising through the ranks of medical training, identify what it is you need early and often. I can count on one hand how many physicians I’ve seen take a lunch break – even 10 minutes. Embrace hard work and self-preservation equally. My hope is that if enough of us take this path, it just might become a matter of course.
Dr. Meffert is a resident in the department of emergency medicine, MedStar Georgetown University Hospital, Washington Hospital Center, Washington. Dr. Meffert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The testing we order should help, not hurt
Ordering and interpreting tests is at the heart of what we do as family physicians. Ordering tests judiciously and interpreting them accurately is not easy. The Choosing Wisely campaign1 has focused our attention on the need to think carefully before ordering tests, whether they be laboratory tests or imaging. Before ordering any test, one should always ask: Is the result of this test going to help me make better decisions about managing this patient?
I would like to highlight and expand on 2 problematic issues Kaminski and Venkat raise in their excellent article on testing in this issue of JFP.2
First, they advise us to know the pretest probability of a disease before we order a test. If we order a test on a patient for whom the probability of disease is very low, a positive result is likely to be a false-positive and mislead us into thinking the patient has the disease when he does not. If we order a test for a patient with a high probability of disease and the result is negative, there is great danger of a false-negative. We might think the patient does not have the disease, but she does.
There is a deeper problem here, however. Primary care physicians are notorious for overestimating disease probability. In a recent study, primary care clinicians overestimated the pretest probability of disease 2- to 10-fold in scenarios involving 4 common diagnoses: breast cancer, coronary artery disease (CAD), pneumonia, and urinary tract infection.3 Even after receiving a negative test result, clinicians still overestimated the chance of disease in all the scenarios. For example, when presented with a 43-year-old premenopausal woman with atypical chest pain and a normal electrocardiogram, clinicians’ average estimate of the probability of CAD was 10%—considerably higher than true estimates of 1% to 4.4%.3
To improve your accuracy in judging pretest probabilities, see the diagnostic test calculators in Essential Evidence Plus (www.essentialevidenceplus.com/).
Secondly, Kaminski and Venkat advise us to try to avoid the testing cascade.2 The associated dangers to patients are considerable. For a cautionary tale, I recommend you read the essay by Michael B. Rothberg, MD, MPH, called “The $50,000 Physical”.4 Dr. Rothberg describes the testing cascade his 85-year-old father experienced, which led to a liver biopsy that nearly killed him from post-biopsy bleeding. Always remember: Testing is a double-edged sword. It can help—or harm—your patients.
1. American Board of Internal Medicine Foundation. Choosing Wisely. Accessed June 30, 2022. www.choosingwisely.org/
2. Kaminski M, Venkat N. A judicious approach to ordering lab tests. J Fam Pract. 2022;71:245-250. doi: 10.12788/jfp.0444
3. Morgan DJ, Pineles L, Owczarzak J, et al. Accuracy of practitioner estimates of probability of diagnosis before and after testing. JAMA Intern Med. 2021;181:747-755. doi: 10.1001/jamainternmed.2021.0269
4. Rothberg MB. The $50 000 physical. JAMA. 2020;323:1682-1683. doi: 10.1001/jama.2020.2866
Ordering and interpreting tests is at the heart of what we do as family physicians. Ordering tests judiciously and interpreting them accurately is not easy. The Choosing Wisely campaign1 has focused our attention on the need to think carefully before ordering tests, whether they be laboratory tests or imaging. Before ordering any test, one should always ask: Is the result of this test going to help me make better decisions about managing this patient?
I would like to highlight and expand on 2 problematic issues Kaminski and Venkat raise in their excellent article on testing in this issue of JFP.2
First, they advise us to know the pretest probability of a disease before we order a test. If we order a test on a patient for whom the probability of disease is very low, a positive result is likely to be a false-positive and mislead us into thinking the patient has the disease when he does not. If we order a test for a patient with a high probability of disease and the result is negative, there is great danger of a false-negative. We might think the patient does not have the disease, but she does.
There is a deeper problem here, however. Primary care physicians are notorious for overestimating disease probability. In a recent study, primary care clinicians overestimated the pretest probability of disease 2- to 10-fold in scenarios involving 4 common diagnoses: breast cancer, coronary artery disease (CAD), pneumonia, and urinary tract infection.3 Even after receiving a negative test result, clinicians still overestimated the chance of disease in all the scenarios. For example, when presented with a 43-year-old premenopausal woman with atypical chest pain and a normal electrocardiogram, clinicians’ average estimate of the probability of CAD was 10%—considerably higher than true estimates of 1% to 4.4%.3
To improve your accuracy in judging pretest probabilities, see the diagnostic test calculators in Essential Evidence Plus (www.essentialevidenceplus.com/).
Secondly, Kaminski and Venkat advise us to try to avoid the testing cascade.2 The associated dangers to patients are considerable. For a cautionary tale, I recommend you read the essay by Michael B. Rothberg, MD, MPH, called “The $50,000 Physical”.4 Dr. Rothberg describes the testing cascade his 85-year-old father experienced, which led to a liver biopsy that nearly killed him from post-biopsy bleeding. Always remember: Testing is a double-edged sword. It can help—or harm—your patients.
Ordering and interpreting tests is at the heart of what we do as family physicians. Ordering tests judiciously and interpreting them accurately is not easy. The Choosing Wisely campaign1 has focused our attention on the need to think carefully before ordering tests, whether they be laboratory tests or imaging. Before ordering any test, one should always ask: Is the result of this test going to help me make better decisions about managing this patient?
I would like to highlight and expand on 2 problematic issues Kaminski and Venkat raise in their excellent article on testing in this issue of JFP.2
First, they advise us to know the pretest probability of a disease before we order a test. If we order a test on a patient for whom the probability of disease is very low, a positive result is likely to be a false-positive and mislead us into thinking the patient has the disease when he does not. If we order a test for a patient with a high probability of disease and the result is negative, there is great danger of a false-negative. We might think the patient does not have the disease, but she does.
There is a deeper problem here, however. Primary care physicians are notorious for overestimating disease probability. In a recent study, primary care clinicians overestimated the pretest probability of disease 2- to 10-fold in scenarios involving 4 common diagnoses: breast cancer, coronary artery disease (CAD), pneumonia, and urinary tract infection.3 Even after receiving a negative test result, clinicians still overestimated the chance of disease in all the scenarios. For example, when presented with a 43-year-old premenopausal woman with atypical chest pain and a normal electrocardiogram, clinicians’ average estimate of the probability of CAD was 10%—considerably higher than true estimates of 1% to 4.4%.3
To improve your accuracy in judging pretest probabilities, see the diagnostic test calculators in Essential Evidence Plus (www.essentialevidenceplus.com/).
Secondly, Kaminski and Venkat advise us to try to avoid the testing cascade.2 The associated dangers to patients are considerable. For a cautionary tale, I recommend you read the essay by Michael B. Rothberg, MD, MPH, called “The $50,000 Physical”.4 Dr. Rothberg describes the testing cascade his 85-year-old father experienced, which led to a liver biopsy that nearly killed him from post-biopsy bleeding. Always remember: Testing is a double-edged sword. It can help—or harm—your patients.
1. American Board of Internal Medicine Foundation. Choosing Wisely. Accessed June 30, 2022. www.choosingwisely.org/
2. Kaminski M, Venkat N. A judicious approach to ordering lab tests. J Fam Pract. 2022;71:245-250. doi: 10.12788/jfp.0444
3. Morgan DJ, Pineles L, Owczarzak J, et al. Accuracy of practitioner estimates of probability of diagnosis before and after testing. JAMA Intern Med. 2021;181:747-755. doi: 10.1001/jamainternmed.2021.0269
4. Rothberg MB. The $50 000 physical. JAMA. 2020;323:1682-1683. doi: 10.1001/jama.2020.2866
1. American Board of Internal Medicine Foundation. Choosing Wisely. Accessed June 30, 2022. www.choosingwisely.org/
2. Kaminski M, Venkat N. A judicious approach to ordering lab tests. J Fam Pract. 2022;71:245-250. doi: 10.12788/jfp.0444
3. Morgan DJ, Pineles L, Owczarzak J, et al. Accuracy of practitioner estimates of probability of diagnosis before and after testing. JAMA Intern Med. 2021;181:747-755. doi: 10.1001/jamainternmed.2021.0269
4. Rothberg MB. The $50 000 physical. JAMA. 2020;323:1682-1683. doi: 10.1001/jama.2020.2866
A judicious approach to ordering lab tests
CASE
A 35-year-old man arrives for an annual wellness visit with no specific complaints and no significant personal or family history. His normal exam includes a blood pressure of 110/74 mm Hg and a body mass index (BMI) of 23.6. You order “routine labs” for prevention, which include a comprehensive metabolic panel (CMP), fasting lipid profile, and thyroid-stimulating hormone (TSH) and 25(OH) vitamin D tests. Are you practicing value-based laboratory testing?
The answer to this question appears in the Case discussion at the end of the article.
Value-based care, including care provided through laboratory testing, can achieve the Institute for Healthcare Improvement’s Triple Aim of improving population health, improving the patient experience of care (including quality and satisfaction), and reducing cost: Value = (Quality x Patient experience) / Cost.1
As quality and patient experience rise and cost falls, the value of care increases. Unnecessary lab testing, however, can negatively impact this equation:
- Error introduced by unnecessary testing can adversely affect quality.
- Patients experience inconvenience and sometimes cascades of testing, in addition to financial responsibility, from unnecessary testing.
- Low-value testing also contributes to work burden and provider burnout by requiring additional review and follow-up.
Rising health care costs are approaching 18% of the US gross domestic product, driven in large part by a wasteful and inefficient care delivery system.2 One review of “waste domains” identified by the Institute of Medicine estimates that approximately one-quarter of health care costs represent waste, including overtreatment, breakdowns of care coordination, and pricing that fails to correlate to the level of care received.3 High-volume, low-cost testing contributes more to total cost than low-volume, high-cost tests.4
Provider and system factors that contribute to ongoing waste
A lack of awareness of waste and how to reduce it contribute to the problem, as does an underappreciation of the harmful effects caused by incidental abnormal results.
Provider intolerance of diagnostic uncertainty often leads to ordering even more tests.
Continue to: Also, a hope of avoiding...
Also, a hope of avoiding missed diagnoses and potential lawsuits leads to defensive practice and more testing. In addition, patients and family members can exert pressure based on a belief that more testing represents better care. Of course, financial revenues from testing may come into play, with few disincentives to forgo testing. Something that also comes into play is that evidence-based guidance on cost-effective laboratory testing may be lacking, or there may be a lack of knowledge on how to access existing evidence.
Automated systems can facilitate wasteful laboratory testing, and the heavy testing practices of hospitals and specialists may be inappropriately applied to outpatient primary care.
Factors affecting the cost of laboratory testing
Laboratory test results drive 70% of today’s medical decisions.5 Negotiated insurance payment for tests is usually much less than the direct out-of-pocket costs charged to the patient. Without insurance, lab tests can cost patients between $100 and $1000.6 If multiple tests are ordered, the costs could likely be many thousands of dollars.
Actual costs typically vary by the testing facility, the patient’s health plan, and location in the United States; hospital-based testing tends to be the most expensive. Insurers will pay for lab tests with appropriate indications that are covered in the contract with the provider.6
Choosing Wisely initiative weighs in on lab testing
Choosing Wisely, a prominent initiative of the American Board of Internal Medicine Foundation, promotes appropriate resource utilization through educational campaigns that detail how to avoid unnecessary medical tests, treatments, and procedures.7 Recommendations are based largely on specialty society consensus and disease-oriented evidence. Choosing Wisely recommendations advise against the following7:
- performing laboratory blood testing unless clinically indicated or necessary for diagnosis or management, in order to avoid iatrogenic anemia. (American Academy of Family Physicians; Society for the Advancement of Patient Blood Management)
- requesting just a serum creatinine to test adult patients with diabetes and/or hypertension for chronic kidney disease. Use the kidney profile: serum creatinine with estimated glomerular filtration rate and urinary albumin-creatinine ratio. (American Society for Clinical Pathology)
- routinely screening for prostate cancer using a prostate-specific antigen test. It should be performed only after engaging in shared decision-making with the patient. (American Academy of Family Physicians; American Urological Association)
- screening for genital herpes simplex virus infectionFrutiger LT Std in asymptomatic adults, including pregnant women. (American Academy of Family Physicians)
- performing preoperative medical tests for eye surgery unless there are specific medical indications. (American Academy of Ophthalmology)
Sequential steps to takefor value-based lab ordering
Ask the question: “How will ordering this specific test change the management of my patient?” From there, take sequential steps using sound, evidence-based pathways. Morgan and colleagues8 outline the following practical approaches to rational test ordering:
- Perform a thorough clinical assessment.
- Consider the probability and implications of a positive test result.
- Practice patient-centered communication: address the patient’s concerns and discuss the risks and benefits of tests and how they will influence management.
- Follow clinical guidelines when available.
- Avoid ordering tests to reassure the patient; unnecessary tests with insignificant results do little to reduce patient anxieties.
- Avoid letting uncertainty drive unnecessary testing. Watchful waiting can allow time for the illness to resolve or declare itself.
Let’s consider this approach in the context of 4 areas: preventive care, diagnostic evaluation, ongoing management of chronic conditions, and preoperative testing.
Continue to: Preventive guidance from the USPSTF
Preventive guidance from the USPSTF
An independent volunteer panel of 16 national experts in prevention and evidence-based medicine develop recommendations for the US Preventive Services Task Force (USPSTF).9 These guidelines are based on evidence and are updated as new evidence surfaces. Thirteen recommendations, some of which advise avoiding preventive procedures that could cause harm to patients, cover laboratory tests used in screening for conditions such as hyperlipidemia10 and prostate cancer.11 We review the ones pertinent to our patient later at the end of the Case.
While the target audience for USPSTF recommendations is clinicians who provide preventive care, the recommendations are widely followed by policymakers, managed care organizations, public and private payers, quality improvement organizations, research institutions, and patients.
Take a critical look at how you approach the diagnostic evaluation
To reduce unnecessary testing in the diagnostic evaluation of patients, first consider pretest probability, test sensitivity and specificity, narrowly out-of-range tests, habitually paired tests, and repetitive laboratory testing.
Pretest probability, and test sensitivity and specificity. Pretest probability is the estimated chance that the patient has the disease before the test result is known. In a patient with low pretest probability of a disease, the ability to conclusively arrive at the diagnosis with one positive result is limited. Similarly, for tests in patients with high pretest probability of disease, a negative test cannot be used to firmly rule out a diagnosis.12
Reliability also depends on test sensitivity (the proportion of true positive results) and specificity (the proportion of true negative results). A test with high sensitivity but low specificity will generate more false-positive results, with potential harm to patients who do not have a disease.
The pretest probability along with test sensitivity and specificity help a clinician to interpret a test result, and even decide whether to order the test at all. For example, the anti-nuclear antibody (ANA) test for systemic lupus erythematosus (SLE) has a sensitivity of 100% and a specificity of 86%13; it will always be positive in a patient with SLE. But when applied to individuals with low likelihood of SLE, false-positives are more common; the ANA is falsely positive in up to 14% of healthy individuals, depending on the population studied.13
Ordering a test may be unnecessary if the results will not change the treatment plan. For example, in a female patient with classic symptoms of an uncomplicated urinary tract infection, a urine culture and even a urinalysis may not change treatment.
Continue to: Narrowly out-of-range tests
Narrowly out-of-range tests. Test results that fall just outside the “normal” range may be of questionable significance. When an asymptomatic patient has mildly elevated liver enzymes, should additional tests be ordered to avoid missing a treatable disorder? In these scenarios, a history, including possible contributing factors such as alcohol or substance misuse, must be paired with the clinical presentation to assess pre-test probability of a particular condition.14 Repeating a narrowly out-of-range test is an option in patients when follow-up is possible. Alternatively, you could pursue watchful waiting and monitor a minor abnormality over time while being vigilant for clinical changes. This whole-patient approach will guide the decision of whether to order additional testing.
Habitually paired tests. Reflexively ordering tests together often contributes to unnecessary testing. Examples of commonly paired tests are serum lipase with amylase, C-reactive protein (CRP) with erythrocyte sedimentation rate (ESR), and TSH with free T4 to monitor patients with treated hypothyroidism. These tests add minimal value together and can be decoupled.15-17 Evidence supports ordering serum lipase alone, CRP instead of ESR, and TSH alone for monitoring thyroid status.
Some commonly paired tests may not even be necessary for diagnosis. The well-established Rotterdam Criteria for diagnosing polycystic ovary syndrome specify clinical features and ovarian ultrasound for diagnosis.18 They do not require measurement of commonly ordered follicle-stimulating hormone and luteinizing hormone for diagnosis.
Serial rather than parallel testing, a “2-step approach,” is a strategy made easier with the advent of the electronic medical record (EMR) and computerized lab systems.8 These records and lab systems allow providers to order reflex tests, and to add on additional tests, if necessary, to an existing blood specimen.
Repetitive laboratory testing. Repetitive inpatient laboratory testing in patients who are clinically stable is wasteful and potentially harmful. Interventions involving physician education alone show mixed results, but combining education with clinician audit and feedback, along with EMR-enabled restrictive ordering, have resulted in significant and sustained reductions in repetitive laboratory testing.19
Continue to: Ongoing management of chronic conditions
Ongoing management of chronic conditions
Evidence-based guidelines support choices of tests and testing intervals for ongoing management of chronic conditions such as diabetes, hyperlipidemia, and hypertension.
Diabetes. Guidelines also define quality standards that are applied to value-based contracts. For example, the American Diabetes Association recommends assessing A1C every 6 months in patients whose type 2 diabetes is under stable control.20
Hyperlipidemia. For patients diagnosed with hyperlipidemia, 2018 clinical practice guidelines published by multiple specialty societies recommend assessing adherence and response to lifestyle changes and LDL-C–lowering medications with repeat lipid measurement 4 to 12 weeks after statin initiation or dose adjustment, repeated every 3 to 12 months as needed.21
Hypertension. With a new diagnosis of hypertension, guidelines advise an initial assessment for comorbidities and end-organ damage with an electrocardiogram, urinalysis, glucose level, blood count, electrolytes, creatinine, calcium, lipids, and urinary albumin/creatinine ratio. For ongoing monitoring, guidelines recommend assessment for end-organ damage through regular measurements of creatinine, glomerular filtration rate, and urinary microalbumin/creatinine ratio. Initiation and alteration of medications should prompt appropriate additional lab follow-up—eg, a measurement of serum potassium after starting a diuretic.22
Preoperative testing
Preoperative testing is overused in low-risk, ambulatory surgery. And testing, even with abnormal results, does not affect postoperative outcomes.23
Continue to: The American Society of Anesthesiologists (ASA) Physical Status Classification System
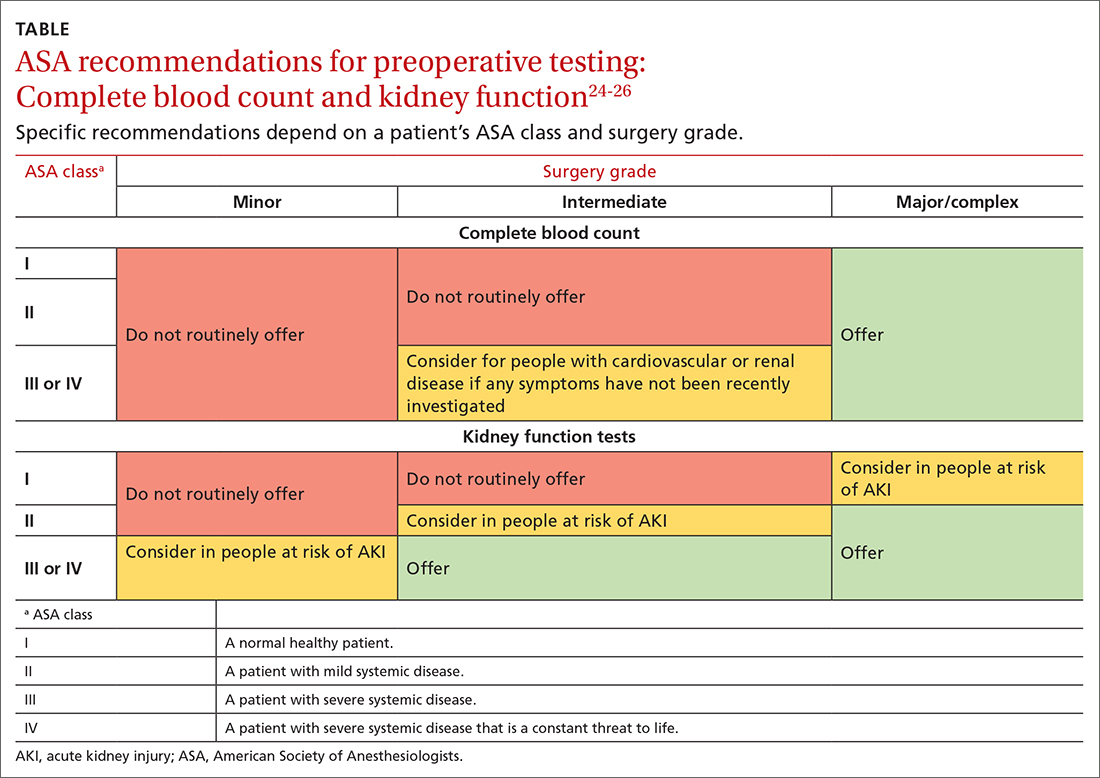
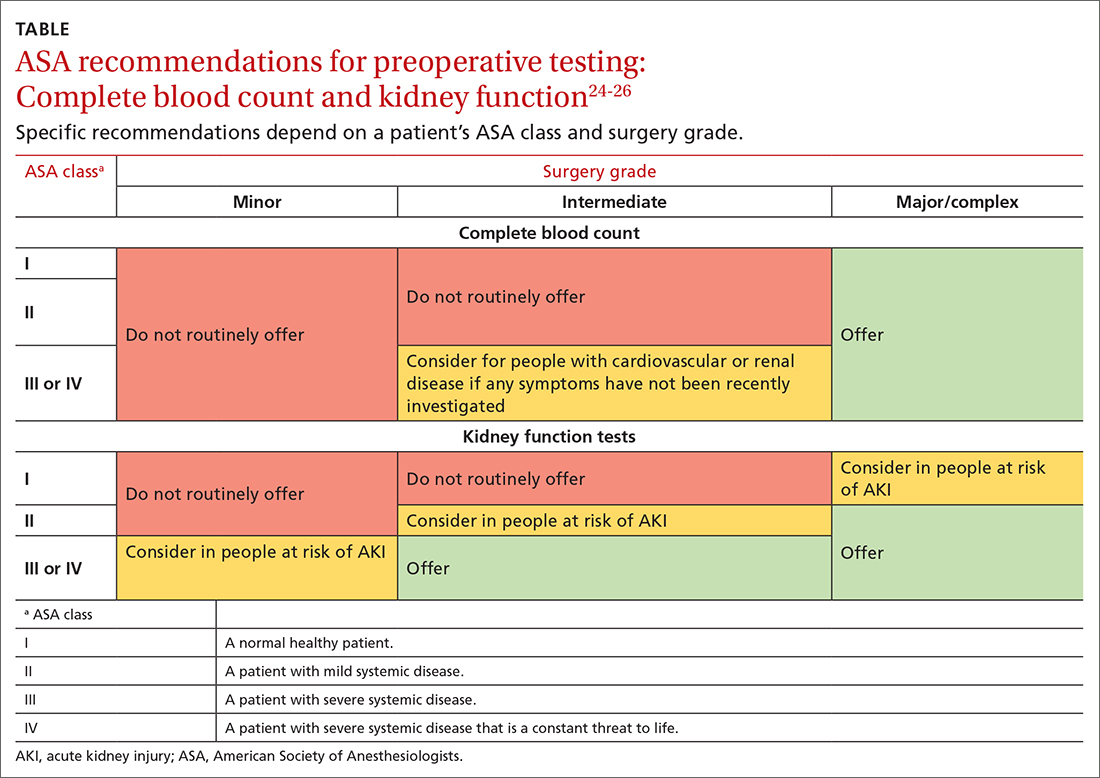
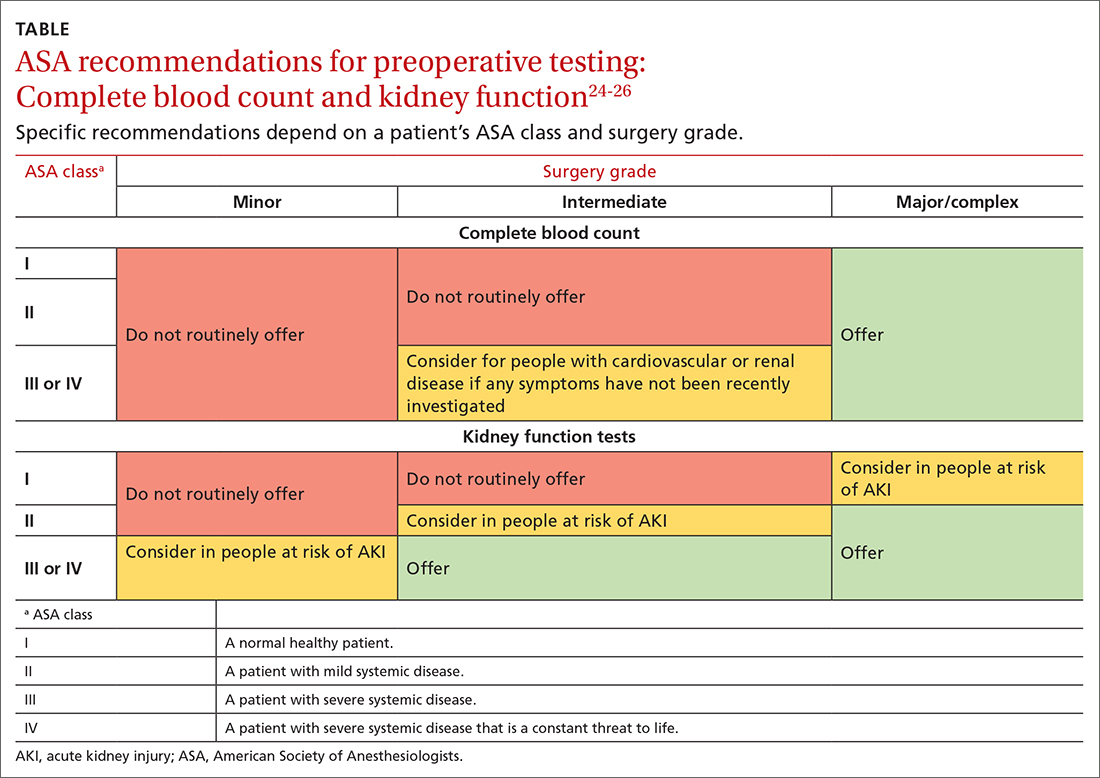
The American Society of Anesthesiologists (ASA) Physical Status Classification System, which has been in use for more than 60 years, considers the patient’s physical status (ASA grades I-VI),24 and when paired with surgery grades of minor, intermediate, and major/complex, can help assess preoperative risk and guide preoperative testing (TABLE).24-26
Preoperative medical testing did not reduce the risk of medical adverse events during or after cataract surgery when compared with selective or no testing.27 Unnecessary preoperative testing can lead to a nonproductive cascade of additional investigations. In a 2018 study of Medicare beneficiaries, unnecessary routine preoperative testing and testing sequelae for cataract surgery was calculated to cost Medicare up to $45.4 million annually.28
CASE
You would not be practicing value-based laboratory testing, according to the USPSTF, if you ordered a CMP, fasting lipid profile, and TSH and 25(OH) vitamin D tests for this healthy 35-year-old man whose family history, blood pressure, and BMI do not put him at elevated risk. Universal lipid screening (Grade Ba) is recommended for all adults ages 40 to 75. Thyroid screening tests and measurement of 25(OH) vitamin D level (I statementsa) are not recommended. The USPSTF has not evaluated chemistry panels for screening.
The USPSTF would recommend the following actions for this patient:
- Screen for HIV (ages 15 to 65 years; and younger or older if patient is at risk). (A recommendationa,29)
- Screen for hepatitis C virus (in those ages 18 to 79). (B recommendation30)
The following USPSTF recommendations might have come into play if this patient had certain risk factors, or if the patient had been a woman:
- Screen for diabetes if the patient is overweight or obese (B recommendation).
- Screen for hepatitis B in adults at risk (B recommendation).
- Screen for gonorrhea and chlamydia in women at risk (B recommendation). Such screening has an “I”statement for screening men at risk.
Continue to: As noted, costs of laboratory...
As noted, costs of laboratory testing vary widely, depending upon what tests are ordered, what type of insurance the patient has, and which tests the patient’s insurance covers. Who performs the testing also factors into the cost. Payers negotiate reduced fees for commercial lab testing, but potential out-of-pocket costs to patients are much higher.
For our healthy 35-year-old man, the cost of the initially proposed testing (CMP, lipid panel, TSH, and 25[OH] vitamin D level) ranges from a negotiated payer cost of $85 to potential patient out-of-pocket cost of more than $400.6
Insurance would cover the USPSTF-recommended testing (HIV and hepatitis C screening tests), which might incur only a patient co-pay, and cost the system about $65.
The USPSTF home page, found at www.uspreventiveservicestaskforce.org/uspstf/ includes recommendations that can be sorted for your patients. A web and mobile device application is also available through the website.
a USPSTF grade definitions:
A: There is high certainty that the net benefit is substantial. Offer service.
B: There is high certainty that the net benefit is moderate, or there is moderate certainty that the net benefit is moderate to substantial. Offer service.
C: There is at least moderate certainty that the net benefit is small. Offer service selectively.
D: There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. Don’t offer service.
I: Current evidence is insufficient to assess the balance of benefits and harms of the service.
CORRESPONDENCE
Mitchell Kaminski, MD, MBA, 901 Walnut Street, 10th Floor, Jefferson College of Population Health, Philadelphia, PA 19107; [email protected]
1. IHI. What is the Triple Aim? Accessed June 20, 2022. http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx#:~:text=It%20is%20IHI’s%20belief%20that,capita%20cost%20of%20health%20care
2. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024-1039. doi: 10.1001/jama.2018.1150
3. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system estimated costs and potential for savings. JAMA. 2019;322:1501-1509. doi:10.1001/jama.2019.13978
4. Mafi JN, Russell K, Bortz BA, et al. Low-cost, high-volume health services contribute the most to unnecessary health spending. Health Aff. 2017;36:1701-1704. doi: 10.1377/hlthaff.2017.0385
5. CDC. Strengthening clinical laboratories. 2018. Accessed June 2020, 2022. www.cdc.gov/csels/dls/strengthening-clinical-labs.html
6. Vuong KT. How much do lab tests cost without insurance in 2022? Accessed May 11, 2022. www.talktomira.com/post/how-much-do-lab-test-cost-without-insurance
7. Choosing Wisely: Promoting conversations between providers and patients. Accessed June 20, 2022. www.choosingwisely.org
8. Morgan S, van Driel M, Coleman J, et al. Rational test ordering in family medicine. Can Fam Physician. 2015;61:535-537.
9. US Preventive Services Taskforce. Screening for glaucoma and impaired vision. Accessed June 20, 2022. www.uspreventiveservicestaskforce.org/uspstf
10. Arnold MJ, O’Malley PG, Downs JR. Key recommendations on managing dyslipidemia for cardiovascular risk reduction: stopping where the evidence does. Am Fam Physician. 2021;103:455-458.
11. Welch HG, Albertsen PC. Reconsidering prostate cancer mortality—the future of PSA screening. N Engl J Med. 2020;382:1557-1563. doi: 10.1056/NEJMms1914228
12. American Society for Microbiology. Why pretest and posttest probability matter in the time of COVID-19. Accessed June 20, 2022. https://asm.org/Articles/2020/June/Why-Pretest-and-Posttest-Probability-Matter-in-the
13. Slater CA, Davis RB, Shmerling RH. Antinuclear antibody testing. A study of clinical utility. Arch Intern Med. 1996;156:1421-1425.
14. Aragon G, Younossi ZM. When and how to evaluate mildly elevated liver enzymes in apparently healthy patients. Cleve Clin J Med. 2010;77:195-204. doi: 10.3949/ccjm.77a.09064
15. Ismail OZ, Bhayana V. Lipase or amylase for the diagnosis of acute pancreatitis? Clin Biochem. 2017;50:1275-1280. doi: 10.1016/j.clinbiochem.2017.07.003.
16. Gottheil S, Khemani E, Copley K, et al. Reducing inappropriate ESR testing with computerized clinical decision support. BMJ Quality Improvement Reports, 2016;5:u211376.w4582. doi: 10.1136/bmjquality.u211376.w4582
17. Schneider C, Feller M, Bauer DC, et al. Initial evaluation of thyroid dysfunction - are simultaneous TSH and fT4 tests necessary? PloS One. 2018;13:e0196631–e0196631. doi: 10.1371/journal.pone.0196631
18. Williams T, Mortada R, Porter S. Diagnosis and treatment of polycystic ovary syndrome. Am Fam Physician. 2016;94:106-113.
19. Eaton KP, Levy K, Soong C et.al. Evidence-Based Guidelines to Eliminate Repetitive Laboratory Testing. JAMA Intern Med. 2017;177:1833-1839. doi: 10.1001/jamainternmed.2017.5152
20. ADA. Glycemic targets: standards of medical care in diabetes—2021. Diabetes Care. 2021;44:S73-S84. doi: 10.2337/dc21-S006
21. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/ AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2019;139:e1082-e1143. doi: 10.1161/CIR.0000000000000625
22. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026.
23. Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518-528. doi: 10.1097/SLA.0b013e318265bcdb
24. ASA. ASA physical status classification system. Accessed June 22,2022. www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system
25. NLM. Preoperative tests (update): routine preoperative tests for elective surgery. Accessed June 22, 2022. www.ncbi.nlm.nih.gov/books/NBK367919/
26. ASA. American Society of Anesthesiologists releases list of commonly used tests and treatments to question-AS PART OF CHOOSING WISELY® CAMPAIGN. Accessed June 22, 2022. www.asahq.org/about-asa/newsroom/news-releases/2013/10/choosing-wisely
27. Keay L, Lindsley K, Tielsch J, et al. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev. 2019;1:CD007293. doi: 10.1002/14651858.CD007293.pub4
28. Chen CL, Clay TH, McLeod S, et al. A revised estimate of costs associated with routine preoperative testing in Medicare cataract patients with a procedure-specific indicator. JAMA Ophthalmol. 2018;136:231-238. doi:10.1001/jamaophthalmol.2017.6372
29. USPSTF. Human immunodeficiency virus (HIV) infection: screening. Accessed May 16, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/human-immunodeficiency-virus-hiv-infection-screening
30. USPSTF. Hepatitis C virus infection in adolescents and adults: screening. Accessed June 20, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening
CASE
A 35-year-old man arrives for an annual wellness visit with no specific complaints and no significant personal or family history. His normal exam includes a blood pressure of 110/74 mm Hg and a body mass index (BMI) of 23.6. You order “routine labs” for prevention, which include a comprehensive metabolic panel (CMP), fasting lipid profile, and thyroid-stimulating hormone (TSH) and 25(OH) vitamin D tests. Are you practicing value-based laboratory testing?
The answer to this question appears in the Case discussion at the end of the article.
Value-based care, including care provided through laboratory testing, can achieve the Institute for Healthcare Improvement’s Triple Aim of improving population health, improving the patient experience of care (including quality and satisfaction), and reducing cost: Value = (Quality x Patient experience) / Cost.1
As quality and patient experience rise and cost falls, the value of care increases. Unnecessary lab testing, however, can negatively impact this equation:
- Error introduced by unnecessary testing can adversely affect quality.
- Patients experience inconvenience and sometimes cascades of testing, in addition to financial responsibility, from unnecessary testing.
- Low-value testing also contributes to work burden and provider burnout by requiring additional review and follow-up.
Rising health care costs are approaching 18% of the US gross domestic product, driven in large part by a wasteful and inefficient care delivery system.2 One review of “waste domains” identified by the Institute of Medicine estimates that approximately one-quarter of health care costs represent waste, including overtreatment, breakdowns of care coordination, and pricing that fails to correlate to the level of care received.3 High-volume, low-cost testing contributes more to total cost than low-volume, high-cost tests.4
Provider and system factors that contribute to ongoing waste
A lack of awareness of waste and how to reduce it contribute to the problem, as does an underappreciation of the harmful effects caused by incidental abnormal results.
Provider intolerance of diagnostic uncertainty often leads to ordering even more tests.
Continue to: Also, a hope of avoiding...
Also, a hope of avoiding missed diagnoses and potential lawsuits leads to defensive practice and more testing. In addition, patients and family members can exert pressure based on a belief that more testing represents better care. Of course, financial revenues from testing may come into play, with few disincentives to forgo testing. Something that also comes into play is that evidence-based guidance on cost-effective laboratory testing may be lacking, or there may be a lack of knowledge on how to access existing evidence.
Automated systems can facilitate wasteful laboratory testing, and the heavy testing practices of hospitals and specialists may be inappropriately applied to outpatient primary care.
Factors affecting the cost of laboratory testing
Laboratory test results drive 70% of today’s medical decisions.5 Negotiated insurance payment for tests is usually much less than the direct out-of-pocket costs charged to the patient. Without insurance, lab tests can cost patients between $100 and $1000.6 If multiple tests are ordered, the costs could likely be many thousands of dollars.
Actual costs typically vary by the testing facility, the patient’s health plan, and location in the United States; hospital-based testing tends to be the most expensive. Insurers will pay for lab tests with appropriate indications that are covered in the contract with the provider.6
Choosing Wisely initiative weighs in on lab testing
Choosing Wisely, a prominent initiative of the American Board of Internal Medicine Foundation, promotes appropriate resource utilization through educational campaigns that detail how to avoid unnecessary medical tests, treatments, and procedures.7 Recommendations are based largely on specialty society consensus and disease-oriented evidence. Choosing Wisely recommendations advise against the following7:
- performing laboratory blood testing unless clinically indicated or necessary for diagnosis or management, in order to avoid iatrogenic anemia. (American Academy of Family Physicians; Society for the Advancement of Patient Blood Management)
- requesting just a serum creatinine to test adult patients with diabetes and/or hypertension for chronic kidney disease. Use the kidney profile: serum creatinine with estimated glomerular filtration rate and urinary albumin-creatinine ratio. (American Society for Clinical Pathology)
- routinely screening for prostate cancer using a prostate-specific antigen test. It should be performed only after engaging in shared decision-making with the patient. (American Academy of Family Physicians; American Urological Association)
- screening for genital herpes simplex virus infectionFrutiger LT Std in asymptomatic adults, including pregnant women. (American Academy of Family Physicians)
- performing preoperative medical tests for eye surgery unless there are specific medical indications. (American Academy of Ophthalmology)
Sequential steps to takefor value-based lab ordering
Ask the question: “How will ordering this specific test change the management of my patient?” From there, take sequential steps using sound, evidence-based pathways. Morgan and colleagues8 outline the following practical approaches to rational test ordering:
- Perform a thorough clinical assessment.
- Consider the probability and implications of a positive test result.
- Practice patient-centered communication: address the patient’s concerns and discuss the risks and benefits of tests and how they will influence management.
- Follow clinical guidelines when available.
- Avoid ordering tests to reassure the patient; unnecessary tests with insignificant results do little to reduce patient anxieties.
- Avoid letting uncertainty drive unnecessary testing. Watchful waiting can allow time for the illness to resolve or declare itself.
Let’s consider this approach in the context of 4 areas: preventive care, diagnostic evaluation, ongoing management of chronic conditions, and preoperative testing.
Continue to: Preventive guidance from the USPSTF
Preventive guidance from the USPSTF
An independent volunteer panel of 16 national experts in prevention and evidence-based medicine develop recommendations for the US Preventive Services Task Force (USPSTF).9 These guidelines are based on evidence and are updated as new evidence surfaces. Thirteen recommendations, some of which advise avoiding preventive procedures that could cause harm to patients, cover laboratory tests used in screening for conditions such as hyperlipidemia10 and prostate cancer.11 We review the ones pertinent to our patient later at the end of the Case.
While the target audience for USPSTF recommendations is clinicians who provide preventive care, the recommendations are widely followed by policymakers, managed care organizations, public and private payers, quality improvement organizations, research institutions, and patients.
Take a critical look at how you approach the diagnostic evaluation
To reduce unnecessary testing in the diagnostic evaluation of patients, first consider pretest probability, test sensitivity and specificity, narrowly out-of-range tests, habitually paired tests, and repetitive laboratory testing.
Pretest probability, and test sensitivity and specificity. Pretest probability is the estimated chance that the patient has the disease before the test result is known. In a patient with low pretest probability of a disease, the ability to conclusively arrive at the diagnosis with one positive result is limited. Similarly, for tests in patients with high pretest probability of disease, a negative test cannot be used to firmly rule out a diagnosis.12
Reliability also depends on test sensitivity (the proportion of true positive results) and specificity (the proportion of true negative results). A test with high sensitivity but low specificity will generate more false-positive results, with potential harm to patients who do not have a disease.
The pretest probability along with test sensitivity and specificity help a clinician to interpret a test result, and even decide whether to order the test at all. For example, the anti-nuclear antibody (ANA) test for systemic lupus erythematosus (SLE) has a sensitivity of 100% and a specificity of 86%13; it will always be positive in a patient with SLE. But when applied to individuals with low likelihood of SLE, false-positives are more common; the ANA is falsely positive in up to 14% of healthy individuals, depending on the population studied.13
Ordering a test may be unnecessary if the results will not change the treatment plan. For example, in a female patient with classic symptoms of an uncomplicated urinary tract infection, a urine culture and even a urinalysis may not change treatment.
Continue to: Narrowly out-of-range tests
Narrowly out-of-range tests. Test results that fall just outside the “normal” range may be of questionable significance. When an asymptomatic patient has mildly elevated liver enzymes, should additional tests be ordered to avoid missing a treatable disorder? In these scenarios, a history, including possible contributing factors such as alcohol or substance misuse, must be paired with the clinical presentation to assess pre-test probability of a particular condition.14 Repeating a narrowly out-of-range test is an option in patients when follow-up is possible. Alternatively, you could pursue watchful waiting and monitor a minor abnormality over time while being vigilant for clinical changes. This whole-patient approach will guide the decision of whether to order additional testing.
Habitually paired tests. Reflexively ordering tests together often contributes to unnecessary testing. Examples of commonly paired tests are serum lipase with amylase, C-reactive protein (CRP) with erythrocyte sedimentation rate (ESR), and TSH with free T4 to monitor patients with treated hypothyroidism. These tests add minimal value together and can be decoupled.15-17 Evidence supports ordering serum lipase alone, CRP instead of ESR, and TSH alone for monitoring thyroid status.
Some commonly paired tests may not even be necessary for diagnosis. The well-established Rotterdam Criteria for diagnosing polycystic ovary syndrome specify clinical features and ovarian ultrasound for diagnosis.18 They do not require measurement of commonly ordered follicle-stimulating hormone and luteinizing hormone for diagnosis.
Serial rather than parallel testing, a “2-step approach,” is a strategy made easier with the advent of the electronic medical record (EMR) and computerized lab systems.8 These records and lab systems allow providers to order reflex tests, and to add on additional tests, if necessary, to an existing blood specimen.
Repetitive laboratory testing. Repetitive inpatient laboratory testing in patients who are clinically stable is wasteful and potentially harmful. Interventions involving physician education alone show mixed results, but combining education with clinician audit and feedback, along with EMR-enabled restrictive ordering, have resulted in significant and sustained reductions in repetitive laboratory testing.19
Continue to: Ongoing management of chronic conditions
Ongoing management of chronic conditions
Evidence-based guidelines support choices of tests and testing intervals for ongoing management of chronic conditions such as diabetes, hyperlipidemia, and hypertension.
Diabetes. Guidelines also define quality standards that are applied to value-based contracts. For example, the American Diabetes Association recommends assessing A1C every 6 months in patients whose type 2 diabetes is under stable control.20
Hyperlipidemia. For patients diagnosed with hyperlipidemia, 2018 clinical practice guidelines published by multiple specialty societies recommend assessing adherence and response to lifestyle changes and LDL-C–lowering medications with repeat lipid measurement 4 to 12 weeks after statin initiation or dose adjustment, repeated every 3 to 12 months as needed.21
Hypertension. With a new diagnosis of hypertension, guidelines advise an initial assessment for comorbidities and end-organ damage with an electrocardiogram, urinalysis, glucose level, blood count, electrolytes, creatinine, calcium, lipids, and urinary albumin/creatinine ratio. For ongoing monitoring, guidelines recommend assessment for end-organ damage through regular measurements of creatinine, glomerular filtration rate, and urinary microalbumin/creatinine ratio. Initiation and alteration of medications should prompt appropriate additional lab follow-up—eg, a measurement of serum potassium after starting a diuretic.22
Preoperative testing
Preoperative testing is overused in low-risk, ambulatory surgery. And testing, even with abnormal results, does not affect postoperative outcomes.23
Continue to: The American Society of Anesthesiologists (ASA) Physical Status Classification System
The American Society of Anesthesiologists (ASA) Physical Status Classification System, which has been in use for more than 60 years, considers the patient’s physical status (ASA grades I-VI),24 and when paired with surgery grades of minor, intermediate, and major/complex, can help assess preoperative risk and guide preoperative testing (TABLE).24-26
Preoperative medical testing did not reduce the risk of medical adverse events during or after cataract surgery when compared with selective or no testing.27 Unnecessary preoperative testing can lead to a nonproductive cascade of additional investigations. In a 2018 study of Medicare beneficiaries, unnecessary routine preoperative testing and testing sequelae for cataract surgery was calculated to cost Medicare up to $45.4 million annually.28
CASE
You would not be practicing value-based laboratory testing, according to the USPSTF, if you ordered a CMP, fasting lipid profile, and TSH and 25(OH) vitamin D tests for this healthy 35-year-old man whose family history, blood pressure, and BMI do not put him at elevated risk. Universal lipid screening (Grade Ba) is recommended for all adults ages 40 to 75. Thyroid screening tests and measurement of 25(OH) vitamin D level (I statementsa) are not recommended. The USPSTF has not evaluated chemistry panels for screening.
The USPSTF would recommend the following actions for this patient:
- Screen for HIV (ages 15 to 65 years; and younger or older if patient is at risk). (A recommendationa,29)
- Screen for hepatitis C virus (in those ages 18 to 79). (B recommendation30)
The following USPSTF recommendations might have come into play if this patient had certain risk factors, or if the patient had been a woman:
- Screen for diabetes if the patient is overweight or obese (B recommendation).
- Screen for hepatitis B in adults at risk (B recommendation).
- Screen for gonorrhea and chlamydia in women at risk (B recommendation). Such screening has an “I”statement for screening men at risk.
Continue to: As noted, costs of laboratory...
As noted, costs of laboratory testing vary widely, depending upon what tests are ordered, what type of insurance the patient has, and which tests the patient’s insurance covers. Who performs the testing also factors into the cost. Payers negotiate reduced fees for commercial lab testing, but potential out-of-pocket costs to patients are much higher.
For our healthy 35-year-old man, the cost of the initially proposed testing (CMP, lipid panel, TSH, and 25[OH] vitamin D level) ranges from a negotiated payer cost of $85 to potential patient out-of-pocket cost of more than $400.6
Insurance would cover the USPSTF-recommended testing (HIV and hepatitis C screening tests), which might incur only a patient co-pay, and cost the system about $65.
The USPSTF home page, found at www.uspreventiveservicestaskforce.org/uspstf/ includes recommendations that can be sorted for your patients. A web and mobile device application is also available through the website.
a USPSTF grade definitions:
A: There is high certainty that the net benefit is substantial. Offer service.
B: There is high certainty that the net benefit is moderate, or there is moderate certainty that the net benefit is moderate to substantial. Offer service.
C: There is at least moderate certainty that the net benefit is small. Offer service selectively.
D: There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. Don’t offer service.
I: Current evidence is insufficient to assess the balance of benefits and harms of the service.
CORRESPONDENCE
Mitchell Kaminski, MD, MBA, 901 Walnut Street, 10th Floor, Jefferson College of Population Health, Philadelphia, PA 19107; [email protected]
CASE
A 35-year-old man arrives for an annual wellness visit with no specific complaints and no significant personal or family history. His normal exam includes a blood pressure of 110/74 mm Hg and a body mass index (BMI) of 23.6. You order “routine labs” for prevention, which include a comprehensive metabolic panel (CMP), fasting lipid profile, and thyroid-stimulating hormone (TSH) and 25(OH) vitamin D tests. Are you practicing value-based laboratory testing?
The answer to this question appears in the Case discussion at the end of the article.
Value-based care, including care provided through laboratory testing, can achieve the Institute for Healthcare Improvement’s Triple Aim of improving population health, improving the patient experience of care (including quality and satisfaction), and reducing cost: Value = (Quality x Patient experience) / Cost.1
As quality and patient experience rise and cost falls, the value of care increases. Unnecessary lab testing, however, can negatively impact this equation:
- Error introduced by unnecessary testing can adversely affect quality.
- Patients experience inconvenience and sometimes cascades of testing, in addition to financial responsibility, from unnecessary testing.
- Low-value testing also contributes to work burden and provider burnout by requiring additional review and follow-up.
Rising health care costs are approaching 18% of the US gross domestic product, driven in large part by a wasteful and inefficient care delivery system.2 One review of “waste domains” identified by the Institute of Medicine estimates that approximately one-quarter of health care costs represent waste, including overtreatment, breakdowns of care coordination, and pricing that fails to correlate to the level of care received.3 High-volume, low-cost testing contributes more to total cost than low-volume, high-cost tests.4
Provider and system factors that contribute to ongoing waste
A lack of awareness of waste and how to reduce it contribute to the problem, as does an underappreciation of the harmful effects caused by incidental abnormal results.
Provider intolerance of diagnostic uncertainty often leads to ordering even more tests.
Continue to: Also, a hope of avoiding...
Also, a hope of avoiding missed diagnoses and potential lawsuits leads to defensive practice and more testing. In addition, patients and family members can exert pressure based on a belief that more testing represents better care. Of course, financial revenues from testing may come into play, with few disincentives to forgo testing. Something that also comes into play is that evidence-based guidance on cost-effective laboratory testing may be lacking, or there may be a lack of knowledge on how to access existing evidence.
Automated systems can facilitate wasteful laboratory testing, and the heavy testing practices of hospitals and specialists may be inappropriately applied to outpatient primary care.
Factors affecting the cost of laboratory testing
Laboratory test results drive 70% of today’s medical decisions.5 Negotiated insurance payment for tests is usually much less than the direct out-of-pocket costs charged to the patient. Without insurance, lab tests can cost patients between $100 and $1000.6 If multiple tests are ordered, the costs could likely be many thousands of dollars.
Actual costs typically vary by the testing facility, the patient’s health plan, and location in the United States; hospital-based testing tends to be the most expensive. Insurers will pay for lab tests with appropriate indications that are covered in the contract with the provider.6
Choosing Wisely initiative weighs in on lab testing
Choosing Wisely, a prominent initiative of the American Board of Internal Medicine Foundation, promotes appropriate resource utilization through educational campaigns that detail how to avoid unnecessary medical tests, treatments, and procedures.7 Recommendations are based largely on specialty society consensus and disease-oriented evidence. Choosing Wisely recommendations advise against the following7:
- performing laboratory blood testing unless clinically indicated or necessary for diagnosis or management, in order to avoid iatrogenic anemia. (American Academy of Family Physicians; Society for the Advancement of Patient Blood Management)
- requesting just a serum creatinine to test adult patients with diabetes and/or hypertension for chronic kidney disease. Use the kidney profile: serum creatinine with estimated glomerular filtration rate and urinary albumin-creatinine ratio. (American Society for Clinical Pathology)
- routinely screening for prostate cancer using a prostate-specific antigen test. It should be performed only after engaging in shared decision-making with the patient. (American Academy of Family Physicians; American Urological Association)
- screening for genital herpes simplex virus infectionFrutiger LT Std in asymptomatic adults, including pregnant women. (American Academy of Family Physicians)
- performing preoperative medical tests for eye surgery unless there are specific medical indications. (American Academy of Ophthalmology)
Sequential steps to takefor value-based lab ordering
Ask the question: “How will ordering this specific test change the management of my patient?” From there, take sequential steps using sound, evidence-based pathways. Morgan and colleagues8 outline the following practical approaches to rational test ordering:
- Perform a thorough clinical assessment.
- Consider the probability and implications of a positive test result.
- Practice patient-centered communication: address the patient’s concerns and discuss the risks and benefits of tests and how they will influence management.
- Follow clinical guidelines when available.
- Avoid ordering tests to reassure the patient; unnecessary tests with insignificant results do little to reduce patient anxieties.
- Avoid letting uncertainty drive unnecessary testing. Watchful waiting can allow time for the illness to resolve or declare itself.
Let’s consider this approach in the context of 4 areas: preventive care, diagnostic evaluation, ongoing management of chronic conditions, and preoperative testing.
Continue to: Preventive guidance from the USPSTF
Preventive guidance from the USPSTF
An independent volunteer panel of 16 national experts in prevention and evidence-based medicine develop recommendations for the US Preventive Services Task Force (USPSTF).9 These guidelines are based on evidence and are updated as new evidence surfaces. Thirteen recommendations, some of which advise avoiding preventive procedures that could cause harm to patients, cover laboratory tests used in screening for conditions such as hyperlipidemia10 and prostate cancer.11 We review the ones pertinent to our patient later at the end of the Case.
While the target audience for USPSTF recommendations is clinicians who provide preventive care, the recommendations are widely followed by policymakers, managed care organizations, public and private payers, quality improvement organizations, research institutions, and patients.
Take a critical look at how you approach the diagnostic evaluation
To reduce unnecessary testing in the diagnostic evaluation of patients, first consider pretest probability, test sensitivity and specificity, narrowly out-of-range tests, habitually paired tests, and repetitive laboratory testing.
Pretest probability, and test sensitivity and specificity. Pretest probability is the estimated chance that the patient has the disease before the test result is known. In a patient with low pretest probability of a disease, the ability to conclusively arrive at the diagnosis with one positive result is limited. Similarly, for tests in patients with high pretest probability of disease, a negative test cannot be used to firmly rule out a diagnosis.12
Reliability also depends on test sensitivity (the proportion of true positive results) and specificity (the proportion of true negative results). A test with high sensitivity but low specificity will generate more false-positive results, with potential harm to patients who do not have a disease.
The pretest probability along with test sensitivity and specificity help a clinician to interpret a test result, and even decide whether to order the test at all. For example, the anti-nuclear antibody (ANA) test for systemic lupus erythematosus (SLE) has a sensitivity of 100% and a specificity of 86%13; it will always be positive in a patient with SLE. But when applied to individuals with low likelihood of SLE, false-positives are more common; the ANA is falsely positive in up to 14% of healthy individuals, depending on the population studied.13
Ordering a test may be unnecessary if the results will not change the treatment plan. For example, in a female patient with classic symptoms of an uncomplicated urinary tract infection, a urine culture and even a urinalysis may not change treatment.
Continue to: Narrowly out-of-range tests
Narrowly out-of-range tests. Test results that fall just outside the “normal” range may be of questionable significance. When an asymptomatic patient has mildly elevated liver enzymes, should additional tests be ordered to avoid missing a treatable disorder? In these scenarios, a history, including possible contributing factors such as alcohol or substance misuse, must be paired with the clinical presentation to assess pre-test probability of a particular condition.14 Repeating a narrowly out-of-range test is an option in patients when follow-up is possible. Alternatively, you could pursue watchful waiting and monitor a minor abnormality over time while being vigilant for clinical changes. This whole-patient approach will guide the decision of whether to order additional testing.
Habitually paired tests. Reflexively ordering tests together often contributes to unnecessary testing. Examples of commonly paired tests are serum lipase with amylase, C-reactive protein (CRP) with erythrocyte sedimentation rate (ESR), and TSH with free T4 to monitor patients with treated hypothyroidism. These tests add minimal value together and can be decoupled.15-17 Evidence supports ordering serum lipase alone, CRP instead of ESR, and TSH alone for monitoring thyroid status.
Some commonly paired tests may not even be necessary for diagnosis. The well-established Rotterdam Criteria for diagnosing polycystic ovary syndrome specify clinical features and ovarian ultrasound for diagnosis.18 They do not require measurement of commonly ordered follicle-stimulating hormone and luteinizing hormone for diagnosis.
Serial rather than parallel testing, a “2-step approach,” is a strategy made easier with the advent of the electronic medical record (EMR) and computerized lab systems.8 These records and lab systems allow providers to order reflex tests, and to add on additional tests, if necessary, to an existing blood specimen.
Repetitive laboratory testing. Repetitive inpatient laboratory testing in patients who are clinically stable is wasteful and potentially harmful. Interventions involving physician education alone show mixed results, but combining education with clinician audit and feedback, along with EMR-enabled restrictive ordering, have resulted in significant and sustained reductions in repetitive laboratory testing.19
Continue to: Ongoing management of chronic conditions
Ongoing management of chronic conditions
Evidence-based guidelines support choices of tests and testing intervals for ongoing management of chronic conditions such as diabetes, hyperlipidemia, and hypertension.
Diabetes. Guidelines also define quality standards that are applied to value-based contracts. For example, the American Diabetes Association recommends assessing A1C every 6 months in patients whose type 2 diabetes is under stable control.20
Hyperlipidemia. For patients diagnosed with hyperlipidemia, 2018 clinical practice guidelines published by multiple specialty societies recommend assessing adherence and response to lifestyle changes and LDL-C–lowering medications with repeat lipid measurement 4 to 12 weeks after statin initiation or dose adjustment, repeated every 3 to 12 months as needed.21
Hypertension. With a new diagnosis of hypertension, guidelines advise an initial assessment for comorbidities and end-organ damage with an electrocardiogram, urinalysis, glucose level, blood count, electrolytes, creatinine, calcium, lipids, and urinary albumin/creatinine ratio. For ongoing monitoring, guidelines recommend assessment for end-organ damage through regular measurements of creatinine, glomerular filtration rate, and urinary microalbumin/creatinine ratio. Initiation and alteration of medications should prompt appropriate additional lab follow-up—eg, a measurement of serum potassium after starting a diuretic.22
Preoperative testing
Preoperative testing is overused in low-risk, ambulatory surgery. And testing, even with abnormal results, does not affect postoperative outcomes.23
Continue to: The American Society of Anesthesiologists (ASA) Physical Status Classification System
The American Society of Anesthesiologists (ASA) Physical Status Classification System, which has been in use for more than 60 years, considers the patient’s physical status (ASA grades I-VI),24 and when paired with surgery grades of minor, intermediate, and major/complex, can help assess preoperative risk and guide preoperative testing (TABLE).24-26
Preoperative medical testing did not reduce the risk of medical adverse events during or after cataract surgery when compared with selective or no testing.27 Unnecessary preoperative testing can lead to a nonproductive cascade of additional investigations. In a 2018 study of Medicare beneficiaries, unnecessary routine preoperative testing and testing sequelae for cataract surgery was calculated to cost Medicare up to $45.4 million annually.28
CASE
You would not be practicing value-based laboratory testing, according to the USPSTF, if you ordered a CMP, fasting lipid profile, and TSH and 25(OH) vitamin D tests for this healthy 35-year-old man whose family history, blood pressure, and BMI do not put him at elevated risk. Universal lipid screening (Grade Ba) is recommended for all adults ages 40 to 75. Thyroid screening tests and measurement of 25(OH) vitamin D level (I statementsa) are not recommended. The USPSTF has not evaluated chemistry panels for screening.
The USPSTF would recommend the following actions for this patient:
- Screen for HIV (ages 15 to 65 years; and younger or older if patient is at risk). (A recommendationa,29)
- Screen for hepatitis C virus (in those ages 18 to 79). (B recommendation30)
The following USPSTF recommendations might have come into play if this patient had certain risk factors, or if the patient had been a woman:
- Screen for diabetes if the patient is overweight or obese (B recommendation).
- Screen for hepatitis B in adults at risk (B recommendation).
- Screen for gonorrhea and chlamydia in women at risk (B recommendation). Such screening has an “I”statement for screening men at risk.
Continue to: As noted, costs of laboratory...
As noted, costs of laboratory testing vary widely, depending upon what tests are ordered, what type of insurance the patient has, and which tests the patient’s insurance covers. Who performs the testing also factors into the cost. Payers negotiate reduced fees for commercial lab testing, but potential out-of-pocket costs to patients are much higher.
For our healthy 35-year-old man, the cost of the initially proposed testing (CMP, lipid panel, TSH, and 25[OH] vitamin D level) ranges from a negotiated payer cost of $85 to potential patient out-of-pocket cost of more than $400.6
Insurance would cover the USPSTF-recommended testing (HIV and hepatitis C screening tests), which might incur only a patient co-pay, and cost the system about $65.
The USPSTF home page, found at www.uspreventiveservicestaskforce.org/uspstf/ includes recommendations that can be sorted for your patients. A web and mobile device application is also available through the website.
a USPSTF grade definitions:
A: There is high certainty that the net benefit is substantial. Offer service.
B: There is high certainty that the net benefit is moderate, or there is moderate certainty that the net benefit is moderate to substantial. Offer service.
C: There is at least moderate certainty that the net benefit is small. Offer service selectively.
D: There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. Don’t offer service.
I: Current evidence is insufficient to assess the balance of benefits and harms of the service.
CORRESPONDENCE
Mitchell Kaminski, MD, MBA, 901 Walnut Street, 10th Floor, Jefferson College of Population Health, Philadelphia, PA 19107; [email protected]
1. IHI. What is the Triple Aim? Accessed June 20, 2022. http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx#:~:text=It%20is%20IHI’s%20belief%20that,capita%20cost%20of%20health%20care
2. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024-1039. doi: 10.1001/jama.2018.1150
3. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system estimated costs and potential for savings. JAMA. 2019;322:1501-1509. doi:10.1001/jama.2019.13978
4. Mafi JN, Russell K, Bortz BA, et al. Low-cost, high-volume health services contribute the most to unnecessary health spending. Health Aff. 2017;36:1701-1704. doi: 10.1377/hlthaff.2017.0385
5. CDC. Strengthening clinical laboratories. 2018. Accessed June 2020, 2022. www.cdc.gov/csels/dls/strengthening-clinical-labs.html
6. Vuong KT. How much do lab tests cost without insurance in 2022? Accessed May 11, 2022. www.talktomira.com/post/how-much-do-lab-test-cost-without-insurance
7. Choosing Wisely: Promoting conversations between providers and patients. Accessed June 20, 2022. www.choosingwisely.org
8. Morgan S, van Driel M, Coleman J, et al. Rational test ordering in family medicine. Can Fam Physician. 2015;61:535-537.
9. US Preventive Services Taskforce. Screening for glaucoma and impaired vision. Accessed June 20, 2022. www.uspreventiveservicestaskforce.org/uspstf
10. Arnold MJ, O’Malley PG, Downs JR. Key recommendations on managing dyslipidemia for cardiovascular risk reduction: stopping where the evidence does. Am Fam Physician. 2021;103:455-458.
11. Welch HG, Albertsen PC. Reconsidering prostate cancer mortality—the future of PSA screening. N Engl J Med. 2020;382:1557-1563. doi: 10.1056/NEJMms1914228
12. American Society for Microbiology. Why pretest and posttest probability matter in the time of COVID-19. Accessed June 20, 2022. https://asm.org/Articles/2020/June/Why-Pretest-and-Posttest-Probability-Matter-in-the
13. Slater CA, Davis RB, Shmerling RH. Antinuclear antibody testing. A study of clinical utility. Arch Intern Med. 1996;156:1421-1425.
14. Aragon G, Younossi ZM. When and how to evaluate mildly elevated liver enzymes in apparently healthy patients. Cleve Clin J Med. 2010;77:195-204. doi: 10.3949/ccjm.77a.09064
15. Ismail OZ, Bhayana V. Lipase or amylase for the diagnosis of acute pancreatitis? Clin Biochem. 2017;50:1275-1280. doi: 10.1016/j.clinbiochem.2017.07.003.
16. Gottheil S, Khemani E, Copley K, et al. Reducing inappropriate ESR testing with computerized clinical decision support. BMJ Quality Improvement Reports, 2016;5:u211376.w4582. doi: 10.1136/bmjquality.u211376.w4582
17. Schneider C, Feller M, Bauer DC, et al. Initial evaluation of thyroid dysfunction - are simultaneous TSH and fT4 tests necessary? PloS One. 2018;13:e0196631–e0196631. doi: 10.1371/journal.pone.0196631
18. Williams T, Mortada R, Porter S. Diagnosis and treatment of polycystic ovary syndrome. Am Fam Physician. 2016;94:106-113.
19. Eaton KP, Levy K, Soong C et.al. Evidence-Based Guidelines to Eliminate Repetitive Laboratory Testing. JAMA Intern Med. 2017;177:1833-1839. doi: 10.1001/jamainternmed.2017.5152
20. ADA. Glycemic targets: standards of medical care in diabetes—2021. Diabetes Care. 2021;44:S73-S84. doi: 10.2337/dc21-S006
21. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/ AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2019;139:e1082-e1143. doi: 10.1161/CIR.0000000000000625
22. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026.
23. Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518-528. doi: 10.1097/SLA.0b013e318265bcdb
24. ASA. ASA physical status classification system. Accessed June 22,2022. www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system
25. NLM. Preoperative tests (update): routine preoperative tests for elective surgery. Accessed June 22, 2022. www.ncbi.nlm.nih.gov/books/NBK367919/
26. ASA. American Society of Anesthesiologists releases list of commonly used tests and treatments to question-AS PART OF CHOOSING WISELY® CAMPAIGN. Accessed June 22, 2022. www.asahq.org/about-asa/newsroom/news-releases/2013/10/choosing-wisely
27. Keay L, Lindsley K, Tielsch J, et al. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev. 2019;1:CD007293. doi: 10.1002/14651858.CD007293.pub4
28. Chen CL, Clay TH, McLeod S, et al. A revised estimate of costs associated with routine preoperative testing in Medicare cataract patients with a procedure-specific indicator. JAMA Ophthalmol. 2018;136:231-238. doi:10.1001/jamaophthalmol.2017.6372
29. USPSTF. Human immunodeficiency virus (HIV) infection: screening. Accessed May 16, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/human-immunodeficiency-virus-hiv-infection-screening
30. USPSTF. Hepatitis C virus infection in adolescents and adults: screening. Accessed June 20, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening
1. IHI. What is the Triple Aim? Accessed June 20, 2022. http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx#:~:text=It%20is%20IHI’s%20belief%20that,capita%20cost%20of%20health%20care
2. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024-1039. doi: 10.1001/jama.2018.1150
3. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system estimated costs and potential for savings. JAMA. 2019;322:1501-1509. doi:10.1001/jama.2019.13978
4. Mafi JN, Russell K, Bortz BA, et al. Low-cost, high-volume health services contribute the most to unnecessary health spending. Health Aff. 2017;36:1701-1704. doi: 10.1377/hlthaff.2017.0385
5. CDC. Strengthening clinical laboratories. 2018. Accessed June 2020, 2022. www.cdc.gov/csels/dls/strengthening-clinical-labs.html
6. Vuong KT. How much do lab tests cost without insurance in 2022? Accessed May 11, 2022. www.talktomira.com/post/how-much-do-lab-test-cost-without-insurance
7. Choosing Wisely: Promoting conversations between providers and patients. Accessed June 20, 2022. www.choosingwisely.org
8. Morgan S, van Driel M, Coleman J, et al. Rational test ordering in family medicine. Can Fam Physician. 2015;61:535-537.
9. US Preventive Services Taskforce. Screening for glaucoma and impaired vision. Accessed June 20, 2022. www.uspreventiveservicestaskforce.org/uspstf
10. Arnold MJ, O’Malley PG, Downs JR. Key recommendations on managing dyslipidemia for cardiovascular risk reduction: stopping where the evidence does. Am Fam Physician. 2021;103:455-458.
11. Welch HG, Albertsen PC. Reconsidering prostate cancer mortality—the future of PSA screening. N Engl J Med. 2020;382:1557-1563. doi: 10.1056/NEJMms1914228
12. American Society for Microbiology. Why pretest and posttest probability matter in the time of COVID-19. Accessed June 20, 2022. https://asm.org/Articles/2020/June/Why-Pretest-and-Posttest-Probability-Matter-in-the
13. Slater CA, Davis RB, Shmerling RH. Antinuclear antibody testing. A study of clinical utility. Arch Intern Med. 1996;156:1421-1425.
14. Aragon G, Younossi ZM. When and how to evaluate mildly elevated liver enzymes in apparently healthy patients. Cleve Clin J Med. 2010;77:195-204. doi: 10.3949/ccjm.77a.09064
15. Ismail OZ, Bhayana V. Lipase or amylase for the diagnosis of acute pancreatitis? Clin Biochem. 2017;50:1275-1280. doi: 10.1016/j.clinbiochem.2017.07.003.
16. Gottheil S, Khemani E, Copley K, et al. Reducing inappropriate ESR testing with computerized clinical decision support. BMJ Quality Improvement Reports, 2016;5:u211376.w4582. doi: 10.1136/bmjquality.u211376.w4582
17. Schneider C, Feller M, Bauer DC, et al. Initial evaluation of thyroid dysfunction - are simultaneous TSH and fT4 tests necessary? PloS One. 2018;13:e0196631–e0196631. doi: 10.1371/journal.pone.0196631
18. Williams T, Mortada R, Porter S. Diagnosis and treatment of polycystic ovary syndrome. Am Fam Physician. 2016;94:106-113.
19. Eaton KP, Levy K, Soong C et.al. Evidence-Based Guidelines to Eliminate Repetitive Laboratory Testing. JAMA Intern Med. 2017;177:1833-1839. doi: 10.1001/jamainternmed.2017.5152
20. ADA. Glycemic targets: standards of medical care in diabetes—2021. Diabetes Care. 2021;44:S73-S84. doi: 10.2337/dc21-S006
21. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/ AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2019;139:e1082-e1143. doi: 10.1161/CIR.0000000000000625
22. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026.
23. Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518-528. doi: 10.1097/SLA.0b013e318265bcdb
24. ASA. ASA physical status classification system. Accessed June 22,2022. www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system
25. NLM. Preoperative tests (update): routine preoperative tests for elective surgery. Accessed June 22, 2022. www.ncbi.nlm.nih.gov/books/NBK367919/
26. ASA. American Society of Anesthesiologists releases list of commonly used tests and treatments to question-AS PART OF CHOOSING WISELY® CAMPAIGN. Accessed June 22, 2022. www.asahq.org/about-asa/newsroom/news-releases/2013/10/choosing-wisely
27. Keay L, Lindsley K, Tielsch J, et al. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev. 2019;1:CD007293. doi: 10.1002/14651858.CD007293.pub4
28. Chen CL, Clay TH, McLeod S, et al. A revised estimate of costs associated with routine preoperative testing in Medicare cataract patients with a procedure-specific indicator. JAMA Ophthalmol. 2018;136:231-238. doi:10.1001/jamaophthalmol.2017.6372
29. USPSTF. Human immunodeficiency virus (HIV) infection: screening. Accessed May 16, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/human-immunodeficiency-virus-hiv-infection-screening
30. USPSTF. Hepatitis C virus infection in adolescents and adults: screening. Accessed June 20, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening
PRACTICE RECOMMENDATIONS
› Follow US Preventive Services Task Force and professional society recommendations for laboratory testing, including choice and frequency of tests. A
› Consider the pretest probability of your patient having a disease, and order the most sensitive and specific test to diagnose a new condition. Employ a 2-step approach with a second laboratory test when the first is outside the reference range. B
› Refrain from ordering routine preoperative testing for patients undergoing low-risk surgeries; these data do not improve postoperative outcomes, can lead to costly testing cascades, and may delay necessary surgical care for patients. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Mark Cuban’s discounted pharmacy offers imatinib at a fraction of the cost
, including several drugs used in oncology.
One of the drugs offering the biggest savings is generic imatinib (originator product Gleevec), which is used for chronic myelogenous leukemia (CML), certain acute lymphocytic leukemia (ALL) and certain types of gastrointestinal stromal tumors (GIST).
Imatinib has a list retail price of $2,502.
At the Mark Cuban pharmacy, it is available for $14.40, which offers a saving of $2,488.
The online pharmacy, known as the Mark Cuban Cost Plus Drug Company (MCCPDC), began operating in January. It is selling more than 100 generic prescription drugs at the cost of ingredients and manufacturing plus 15% margin, $3 pharmacy dispensing fee, and $5 shipping fee.
“We will do whatever it takes to get affordable pharmaceuticals to patients,” said Alex Oshmyansky, MD, PhD, founder and CEO of MCCPDC, in a company statement. “The markup on potentially lifesaving drugs that people depend on is a problem that can’t be ignored. It is imperative that we take action and help expand access to these medications for those who need them most.”
The company is a registered pharmaceutical wholesaler, and as such, can “bypass middlemen and outrageous markups,” the company notes in a press release. They have partnered with the digital health care company Truepill, which built and powers the pharmacy’s website.
At its launch, the pharmacy offered 109 generic medications. So far, the generics offered for oncology include generic anastrozole, letrozole, raloxifene, and tamoxifen for use in breast cancer, as well as the chemotherapy methotrexate and generic imatinib, as mentioned above. All of the drugs sold through the MCCPDC have prices much lower than in the standard marketplace. Becker’s Hospital Review recently published a list of the 50 drugs with the biggest savings at Cuban’s pharmacy.
At the top of the list was albendazole, an anthelmintic that retails for $6,565. In contrast, the MCCPDC price is $453, which translates to a savings of more than $6,000 for a 30-count supply.
The second-largest savings was for imatinib.
For the other cancer drugs, the savings were less substantial, reflecting their much lower retail price, but savings still ranged between $66 and $200 per product.
Overall, 14 of the top 50 discounted drugs are slated to save consumers more than $500 for a 30-count supply when purchased from MCCPDC.
Medicare could save billions
Medicare would save billions if it used this online pharmacy, say researchers from Harvard University, who recently published a study in Annals of Internal Medicine giving some estimates.
The team analyzed 89 generic drugs listed at MCCPDC and found that Medicare Part D could have saved more than $3 billion in 2020 if they had purchased them at these prices. For example, aripiprazole, a commonly used psychiatric medication, was purchased for more than $2 per pill, while the same generic formulation of the drug is sold by Cuban’s company for $0.24 per pill. Overall, just with this one drug, Medicare could have saved $233 million in 2020.
“We found that Medicare spent $9.6 billion on 89 generic drugs in 2020,” commented lead author Hussain S. Lalani, MD, MPH in a tweet. “It could have saved up to $3.6 billion on 77 of the 89 drugs if it purchased them at the largest quantity sold by Mark Cuban’s Cost Plus Drug Company. The other 12 drugs ($1.5B) did not offer savings.”
Dr. Lalani pointed out that the price transparency provided by MCCPDC is “helping us to understand the cost of many generic drugs and highlights inefficiencies in the supply chain for generic drugs.”
In standard practice, there are “multiple actors” involved in distributing the drug from the pharmaceutical manufacturer to the patient, he explained. “Mark Cuban’s company does not accept health insurance, buys from the manufacturer, and sells it directly to consumers online!”
He added that innovation and policy reform are needed. “We know that many drug prices are outrageous, and the supply chain is also expensive & NOT working right,” he tweeted. “We need a system that delivers innovative, affordable, and accessible medicines for all Americans.”
Commenting on Dr. Lalani’s Twitter thread, Eric Topol, MD, Medscape’s editor-in-chief, said that “the many billions the U.S. could save each year by MCCPDC is remarkable.”
Dr. Topol also noted that the savings estimated in the Annals of Internal Medicine paper were based on fewer than 100 generic drugs that are currently available, but he said that “there will be >1,000 more offered in the next year.”
No insurance, no PBMs
Prior to launching the online pharmacy, Mr. Cuban established a pharmacy benefit manager (PBM) operation to serve companies providing prescription coverage in their employee benefit plans. According to a press release, MCCPDC has pledged to be “radically transparent” in its own negotiations as a PBM, revealing the true costs it pays for drugs and eliminating spread pricing and misaligned rebate incentives. MCCPDC anticipates that its PBM could save companies millions of dollars with no changes to its benefits, as it will eliminate the traditional PBM model.
However, the online pharmacy is a cash-only venture, because MCCPDC refuses to pay third-party PBMs in order to be allowed to process insurance claims. But the model allows patients to immediately purchase medications at a cost that is often less than what they might pay when having to deal with deductible and copay requirements.
In the future, MCCPDC plans to start manufacturing medications. The company is currently building a state-of-the-art pharmaceutical facility in Dallas, at which it plans to produce its own high-quality medicines at the lowest possible prices.
A version of this article first appeared on Medscape.com.
, including several drugs used in oncology.
One of the drugs offering the biggest savings is generic imatinib (originator product Gleevec), which is used for chronic myelogenous leukemia (CML), certain acute lymphocytic leukemia (ALL) and certain types of gastrointestinal stromal tumors (GIST).
Imatinib has a list retail price of $2,502.
At the Mark Cuban pharmacy, it is available for $14.40, which offers a saving of $2,488.
The online pharmacy, known as the Mark Cuban Cost Plus Drug Company (MCCPDC), began operating in January. It is selling more than 100 generic prescription drugs at the cost of ingredients and manufacturing plus 15% margin, $3 pharmacy dispensing fee, and $5 shipping fee.
“We will do whatever it takes to get affordable pharmaceuticals to patients,” said Alex Oshmyansky, MD, PhD, founder and CEO of MCCPDC, in a company statement. “The markup on potentially lifesaving drugs that people depend on is a problem that can’t be ignored. It is imperative that we take action and help expand access to these medications for those who need them most.”
The company is a registered pharmaceutical wholesaler, and as such, can “bypass middlemen and outrageous markups,” the company notes in a press release. They have partnered with the digital health care company Truepill, which built and powers the pharmacy’s website.
At its launch, the pharmacy offered 109 generic medications. So far, the generics offered for oncology include generic anastrozole, letrozole, raloxifene, and tamoxifen for use in breast cancer, as well as the chemotherapy methotrexate and generic imatinib, as mentioned above. All of the drugs sold through the MCCPDC have prices much lower than in the standard marketplace. Becker’s Hospital Review recently published a list of the 50 drugs with the biggest savings at Cuban’s pharmacy.
At the top of the list was albendazole, an anthelmintic that retails for $6,565. In contrast, the MCCPDC price is $453, which translates to a savings of more than $6,000 for a 30-count supply.
The second-largest savings was for imatinib.
For the other cancer drugs, the savings were less substantial, reflecting their much lower retail price, but savings still ranged between $66 and $200 per product.
Overall, 14 of the top 50 discounted drugs are slated to save consumers more than $500 for a 30-count supply when purchased from MCCPDC.
Medicare could save billions
Medicare would save billions if it used this online pharmacy, say researchers from Harvard University, who recently published a study in Annals of Internal Medicine giving some estimates.
The team analyzed 89 generic drugs listed at MCCPDC and found that Medicare Part D could have saved more than $3 billion in 2020 if they had purchased them at these prices. For example, aripiprazole, a commonly used psychiatric medication, was purchased for more than $2 per pill, while the same generic formulation of the drug is sold by Cuban’s company for $0.24 per pill. Overall, just with this one drug, Medicare could have saved $233 million in 2020.
“We found that Medicare spent $9.6 billion on 89 generic drugs in 2020,” commented lead author Hussain S. Lalani, MD, MPH in a tweet. “It could have saved up to $3.6 billion on 77 of the 89 drugs if it purchased them at the largest quantity sold by Mark Cuban’s Cost Plus Drug Company. The other 12 drugs ($1.5B) did not offer savings.”
Dr. Lalani pointed out that the price transparency provided by MCCPDC is “helping us to understand the cost of many generic drugs and highlights inefficiencies in the supply chain for generic drugs.”
In standard practice, there are “multiple actors” involved in distributing the drug from the pharmaceutical manufacturer to the patient, he explained. “Mark Cuban’s company does not accept health insurance, buys from the manufacturer, and sells it directly to consumers online!”
He added that innovation and policy reform are needed. “We know that many drug prices are outrageous, and the supply chain is also expensive & NOT working right,” he tweeted. “We need a system that delivers innovative, affordable, and accessible medicines for all Americans.”
Commenting on Dr. Lalani’s Twitter thread, Eric Topol, MD, Medscape’s editor-in-chief, said that “the many billions the U.S. could save each year by MCCPDC is remarkable.”
Dr. Topol also noted that the savings estimated in the Annals of Internal Medicine paper were based on fewer than 100 generic drugs that are currently available, but he said that “there will be >1,000 more offered in the next year.”
No insurance, no PBMs
Prior to launching the online pharmacy, Mr. Cuban established a pharmacy benefit manager (PBM) operation to serve companies providing prescription coverage in their employee benefit plans. According to a press release, MCCPDC has pledged to be “radically transparent” in its own negotiations as a PBM, revealing the true costs it pays for drugs and eliminating spread pricing and misaligned rebate incentives. MCCPDC anticipates that its PBM could save companies millions of dollars with no changes to its benefits, as it will eliminate the traditional PBM model.
However, the online pharmacy is a cash-only venture, because MCCPDC refuses to pay third-party PBMs in order to be allowed to process insurance claims. But the model allows patients to immediately purchase medications at a cost that is often less than what they might pay when having to deal with deductible and copay requirements.
In the future, MCCPDC plans to start manufacturing medications. The company is currently building a state-of-the-art pharmaceutical facility in Dallas, at which it plans to produce its own high-quality medicines at the lowest possible prices.
A version of this article first appeared on Medscape.com.
, including several drugs used in oncology.
One of the drugs offering the biggest savings is generic imatinib (originator product Gleevec), which is used for chronic myelogenous leukemia (CML), certain acute lymphocytic leukemia (ALL) and certain types of gastrointestinal stromal tumors (GIST).
Imatinib has a list retail price of $2,502.
At the Mark Cuban pharmacy, it is available for $14.40, which offers a saving of $2,488.
The online pharmacy, known as the Mark Cuban Cost Plus Drug Company (MCCPDC), began operating in January. It is selling more than 100 generic prescription drugs at the cost of ingredients and manufacturing plus 15% margin, $3 pharmacy dispensing fee, and $5 shipping fee.
“We will do whatever it takes to get affordable pharmaceuticals to patients,” said Alex Oshmyansky, MD, PhD, founder and CEO of MCCPDC, in a company statement. “The markup on potentially lifesaving drugs that people depend on is a problem that can’t be ignored. It is imperative that we take action and help expand access to these medications for those who need them most.”
The company is a registered pharmaceutical wholesaler, and as such, can “bypass middlemen and outrageous markups,” the company notes in a press release. They have partnered with the digital health care company Truepill, which built and powers the pharmacy’s website.
At its launch, the pharmacy offered 109 generic medications. So far, the generics offered for oncology include generic anastrozole, letrozole, raloxifene, and tamoxifen for use in breast cancer, as well as the chemotherapy methotrexate and generic imatinib, as mentioned above. All of the drugs sold through the MCCPDC have prices much lower than in the standard marketplace. Becker’s Hospital Review recently published a list of the 50 drugs with the biggest savings at Cuban’s pharmacy.
At the top of the list was albendazole, an anthelmintic that retails for $6,565. In contrast, the MCCPDC price is $453, which translates to a savings of more than $6,000 for a 30-count supply.
The second-largest savings was for imatinib.
For the other cancer drugs, the savings were less substantial, reflecting their much lower retail price, but savings still ranged between $66 and $200 per product.
Overall, 14 of the top 50 discounted drugs are slated to save consumers more than $500 for a 30-count supply when purchased from MCCPDC.
Medicare could save billions
Medicare would save billions if it used this online pharmacy, say researchers from Harvard University, who recently published a study in Annals of Internal Medicine giving some estimates.
The team analyzed 89 generic drugs listed at MCCPDC and found that Medicare Part D could have saved more than $3 billion in 2020 if they had purchased them at these prices. For example, aripiprazole, a commonly used psychiatric medication, was purchased for more than $2 per pill, while the same generic formulation of the drug is sold by Cuban’s company for $0.24 per pill. Overall, just with this one drug, Medicare could have saved $233 million in 2020.
“We found that Medicare spent $9.6 billion on 89 generic drugs in 2020,” commented lead author Hussain S. Lalani, MD, MPH in a tweet. “It could have saved up to $3.6 billion on 77 of the 89 drugs if it purchased them at the largest quantity sold by Mark Cuban’s Cost Plus Drug Company. The other 12 drugs ($1.5B) did not offer savings.”
Dr. Lalani pointed out that the price transparency provided by MCCPDC is “helping us to understand the cost of many generic drugs and highlights inefficiencies in the supply chain for generic drugs.”
In standard practice, there are “multiple actors” involved in distributing the drug from the pharmaceutical manufacturer to the patient, he explained. “Mark Cuban’s company does not accept health insurance, buys from the manufacturer, and sells it directly to consumers online!”
He added that innovation and policy reform are needed. “We know that many drug prices are outrageous, and the supply chain is also expensive & NOT working right,” he tweeted. “We need a system that delivers innovative, affordable, and accessible medicines for all Americans.”
Commenting on Dr. Lalani’s Twitter thread, Eric Topol, MD, Medscape’s editor-in-chief, said that “the many billions the U.S. could save each year by MCCPDC is remarkable.”
Dr. Topol also noted that the savings estimated in the Annals of Internal Medicine paper were based on fewer than 100 generic drugs that are currently available, but he said that “there will be >1,000 more offered in the next year.”
No insurance, no PBMs
Prior to launching the online pharmacy, Mr. Cuban established a pharmacy benefit manager (PBM) operation to serve companies providing prescription coverage in their employee benefit plans. According to a press release, MCCPDC has pledged to be “radically transparent” in its own negotiations as a PBM, revealing the true costs it pays for drugs and eliminating spread pricing and misaligned rebate incentives. MCCPDC anticipates that its PBM could save companies millions of dollars with no changes to its benefits, as it will eliminate the traditional PBM model.
However, the online pharmacy is a cash-only venture, because MCCPDC refuses to pay third-party PBMs in order to be allowed to process insurance claims. But the model allows patients to immediately purchase medications at a cost that is often less than what they might pay when having to deal with deductible and copay requirements.
In the future, MCCPDC plans to start manufacturing medications. The company is currently building a state-of-the-art pharmaceutical facility in Dallas, at which it plans to produce its own high-quality medicines at the lowest possible prices.
A version of this article first appeared on Medscape.com.
Don’t wait for a cyberattack; know what coverage you have now
Barbara L. McAneny, MD, CEO of New Mexico Oncology Hematology Consultants, experienced a data breach about 10 years ago, when a laptop was stolen from her large practice.
She and the other physicians were upset and worried that the individual would attempt to log in to the computer system and hack their patients’ private health information.
Dr. McAneny was also worried that the practice would have to pay a hefty fine to the government for having unsecured private health information on a laptop. She could have paid from $50,000 to more than $1.9 million for lost and stolen devices (although that didn’t happen).
Dr. McAneny had a standard cyber liability benefit in her med-mal policy that covered up to $50,000 of the data breach costs. That covered the legal advice The Doctors Company provided about state and federal reporting requirements when a data breach occurs and the costs the practice incurred from mailing letters to all of its patients notifying them of the data breach, says Dr. McAneny.
“The data breach taught me a lot. Our practice spent a lot of money on increasing our internal controls, cybersecurity, and monitoring. Our IT department started testing our computer firewalls periodically, and that’s how we discovered that cybercriminals were attempting to break into our computer system at least 100 times daily,” says Dr. McAneny.
That discovery changed how she thought about insurance. “I decided the med-mal benefit wasn’t enough. I bought the best cybersecurity policy we could afford to protect against future breaches, especially malware or ransomware attacks.”
Her practice also had to make its electronic health records (EHRs) more secure to comply with the Department of Health & Human Services Office of Civil Rights standards for protected health information. The cost of increased security wasn’t covered by her cyber benefit.
Cyberattacks increasing in health care
Despite having comprehensive coverage, Dr. McAneny worries that the cybercriminals are a step ahead of the cybersecurity experts and her practice will eventually have another data breach.
“The policy only covers things that we know about today. As we upgrade our defenses, criminals are finding new ways to breach firewalls and work around our defenses,” she says.
So far this year, nearly 200 medical groups have reported cyberattacks involving 500 or more of their patients’ medical records to the federal government.
EHRs are valuable targets to cybercriminals because of the protected health information they contain. Cybercriminals grab information such as Social Security numbers, dates of birth, medical procedures and results, and in some cases billing and financial information and sell it on the dark web.
They typically bundle the information and sell it to other criminals who later use it for various kinds of fraud and extortion such as banking and credit fraud, health care fraud, identity theft, and ransom extortion.
What do most doctors have?
The vast majority (82%) of doctors polled by the Medical Group Management Association last year said they had cyber insurance, compared with 54% in 2018.
For those who answered “yes,” many said they have coverage through their malpractice insurance carrier.
David Zetter, president of Zetter HealthCare Management Consultants, recommends that physicians speak with their malpractice carrier to determine what coverage they have, if any, within their malpractice policy.
A typical cybersecurity benefit is limited to what is needed to fix and resolve the hacking incident, says Raj Shah, senior regulatory attorney and policyholder advisor at MagMutual, which insures medical practices for malpractice and cyber liability.
That usually covers investigating the cause of the breach and the extent of the damage, legal advice about federal and state reporting requirements, whether to pay a ransom, and a public relations professional to handle patient communication, says Mr. Shah.
The benefit doesn’t cover lost patient revenue when practices have to shut down their operations, the cost of replacing damaged computers, or the ransom payment, he says.
Mr. Zetter advises doctors to consider buying cybersecurity coverage. “I recommend that they speak with an insurance broker who is experienced with cybersecurity policies sold to health care professionals to determine what type of coverage and how much coverage they may need. Their malpractice carrier may also be able to provide some answers,” says Mr. Zetter.
The physician will need to be able to answer questions about their network and how many staff they have and may need to involve their IT vendor too, he adds.
How does comprehensive coverage compare?
Ransomware attacks continue to be one of the most frequent types of attacks, and the amount criminals are demanding has risen significantly. The median ransom payment was $5,000 in the fourth quarter of 2018, compared with over $300,000 during the fourth quarter of 2021.
Cybercriminals now engage in “double extortion” – demanding a ransom payment to hand over the code that will unlock their encrypted data – and then another ransom payment to not post patients’ sensitive medical information they copied onto the dark web.
Comprehensive cybersecurity insurance will cover “double extortion” payments, legal costs that may arise from defending against patient lawsuits, and the costs of meeting federal and state privacy requirements, including notifying patients of the data breach and regulatory investigations, says Michael Carr, head of risk engineering for North America for Coalition, a cyber insurance firm.
Cyber insurers also contract with vendors who sell bitcoin, which is the currency cybercriminals typically demand for ransom payments, and work with ransom negotiators.
For example, once Coalition decided to pay the ransom on behalf of a health care client, it negotiated the ransom demand down by nearly 75% from $750,000 to $200,000, and proceeded to help the company restore all of its data.
The costs to respond to the incident, to recover lost data, and to pay the extortion, together with the lost business income resulting from the incident, were covered by Coalition’s cyber insurance policy.
Other clients have had their funds retrieved before a fraudulent wire transfer was completed. “Medical practices have vendors they pay regularly. A cybercriminal may compromise your email or take over a bank account and then impersonate a vendor asking to be paid for services they didn’t provide,” says Mr. Carr.
How much coverage do you need? Cost?
Dr. McAneny has increased her cybersecurity coverage every year. “It’s expensive, but I think it’s worth it. But you can never buy enough protection due to the coverage limits.”
She worries that the costs could exceed the limits if a ransomware attack disrupts her practice for days, weeks, or longer, or if the Office for Civil Rights fines her practice $10,000 per patient chart – the practice has 100,000 health records. “That can run several millions of dollars and ruin a practice,” she says.
Health systems and hospitals need massive amounts of coverage, which often runs from $20 million to $30 million, says Mr. Shah. However, practices insured through MagMutual have lower coverage limits that range from $1 million to $5 million, he says.
“A large practice does not necessarily need more than $1,000,000 in coverage if they have limited loss in this area and strong internal processes and controls. Most large practices also have a dedicated information security director, which reduces their risk, so they may be comfortable with $1,000,000 in coverage,” says Mr. Shah.
Premiums are based on the number of patient health records per practice, which translates into higher premiums for larger practices.
Other factors that come into play include the underlying coverage, risk controls the practice has implemented, and its claims history, says Mr. Shah.
However, the cost for cyber liability insurance has increased, and practices can expect to pay higher premiums and deductibles. For example, a practice that paid $10,000 in premiums for a new policy last year will have to pay $20,000 this year, says Dan Hanson, senior vice president of management liability and client experience at Marsh & McLennon Agency, a risk management firm that sells cyber insurance policies.
“We saw 71% of our self-insured clients experience higher deductibles over last year due to increased claim activity and the lack of capacity in the market. The carriers are saying they will set limits, but you are going to pay a lot more, and you are going to participate more in losses through the higher deductibles,” says Mr. Hanson.
Are you eligible?
Cyber insurance companies have a vested interest in avoiding claims. With increasing cyberattacks and larger payouts, many insurers are requiring practices to implement some defensive measures before they insure them. Some insurers, such as Coalition, say they may still insure small practices for comprehensive coverage, but it may impact the pricing or what’s covered, says Mr. Carr.
Here are some of the security measures that cyber insurers are looking for:
- Multifactorial authentication (MFA) requires an extra layer of security to access the system. For example, when logging into your organization’s EHR platform, instead of just using a username and password to access the platform, MFA would require you to input an additional unique login credential before you can access the EHR. A secondary login credential may include security questions, a one-time PIN, or biometrics.
- Removing a terminated employee’s login credentials quickly from the computer system. “One of the most damaging and expensive types of attacks are by disgruntled employees who still have their login credentials and take revenge by logging back into the system and planting malware,” says Mr. Shah.
- Automatic system updates (patches). “Phishing email compromises usually result from a failure to fix vulnerabilities. When a system needs to restart, it should be set to automatically update any potential security loopholes within programs or products,” says Mr. Carr. The firewall settings should also be updated.
- Prior hacking incidents: Are the attackers out of your system? Once criminals hack into the system, your practice is vulnerable to repeat attacks. “If a cyberattack is not completely addressed, threat actors will maintain access to or a presence on the compromised network. In general, we will work with the insured to ensure that the initial point of compromise has been addressed and that any threat actor presence in the network has been removed,” says Mr. Carr.
When doctors compare cybersecurity policies, experts recommend avoiding companies that may offer lower prices but lack a proven track record of handling claims and do not offer resources that can detect a threat, such as ongoing network monitoring and employee training with simulated exercises.
“Practices tend to think, ‘It won’t happen to me.’ Every practice needs to take this seriously,” says Dr. McAneny.
A version of this article first appeared on Medscape.com.
Barbara L. McAneny, MD, CEO of New Mexico Oncology Hematology Consultants, experienced a data breach about 10 years ago, when a laptop was stolen from her large practice.
She and the other physicians were upset and worried that the individual would attempt to log in to the computer system and hack their patients’ private health information.
Dr. McAneny was also worried that the practice would have to pay a hefty fine to the government for having unsecured private health information on a laptop. She could have paid from $50,000 to more than $1.9 million for lost and stolen devices (although that didn’t happen).
Dr. McAneny had a standard cyber liability benefit in her med-mal policy that covered up to $50,000 of the data breach costs. That covered the legal advice The Doctors Company provided about state and federal reporting requirements when a data breach occurs and the costs the practice incurred from mailing letters to all of its patients notifying them of the data breach, says Dr. McAneny.
“The data breach taught me a lot. Our practice spent a lot of money on increasing our internal controls, cybersecurity, and monitoring. Our IT department started testing our computer firewalls periodically, and that’s how we discovered that cybercriminals were attempting to break into our computer system at least 100 times daily,” says Dr. McAneny.
That discovery changed how she thought about insurance. “I decided the med-mal benefit wasn’t enough. I bought the best cybersecurity policy we could afford to protect against future breaches, especially malware or ransomware attacks.”
Her practice also had to make its electronic health records (EHRs) more secure to comply with the Department of Health & Human Services Office of Civil Rights standards for protected health information. The cost of increased security wasn’t covered by her cyber benefit.
Cyberattacks increasing in health care
Despite having comprehensive coverage, Dr. McAneny worries that the cybercriminals are a step ahead of the cybersecurity experts and her practice will eventually have another data breach.
“The policy only covers things that we know about today. As we upgrade our defenses, criminals are finding new ways to breach firewalls and work around our defenses,” she says.
So far this year, nearly 200 medical groups have reported cyberattacks involving 500 or more of their patients’ medical records to the federal government.
EHRs are valuable targets to cybercriminals because of the protected health information they contain. Cybercriminals grab information such as Social Security numbers, dates of birth, medical procedures and results, and in some cases billing and financial information and sell it on the dark web.
They typically bundle the information and sell it to other criminals who later use it for various kinds of fraud and extortion such as banking and credit fraud, health care fraud, identity theft, and ransom extortion.
What do most doctors have?
The vast majority (82%) of doctors polled by the Medical Group Management Association last year said they had cyber insurance, compared with 54% in 2018.
For those who answered “yes,” many said they have coverage through their malpractice insurance carrier.
David Zetter, president of Zetter HealthCare Management Consultants, recommends that physicians speak with their malpractice carrier to determine what coverage they have, if any, within their malpractice policy.
A typical cybersecurity benefit is limited to what is needed to fix and resolve the hacking incident, says Raj Shah, senior regulatory attorney and policyholder advisor at MagMutual, which insures medical practices for malpractice and cyber liability.
That usually covers investigating the cause of the breach and the extent of the damage, legal advice about federal and state reporting requirements, whether to pay a ransom, and a public relations professional to handle patient communication, says Mr. Shah.
The benefit doesn’t cover lost patient revenue when practices have to shut down their operations, the cost of replacing damaged computers, or the ransom payment, he says.
Mr. Zetter advises doctors to consider buying cybersecurity coverage. “I recommend that they speak with an insurance broker who is experienced with cybersecurity policies sold to health care professionals to determine what type of coverage and how much coverage they may need. Their malpractice carrier may also be able to provide some answers,” says Mr. Zetter.
The physician will need to be able to answer questions about their network and how many staff they have and may need to involve their IT vendor too, he adds.
How does comprehensive coverage compare?
Ransomware attacks continue to be one of the most frequent types of attacks, and the amount criminals are demanding has risen significantly. The median ransom payment was $5,000 in the fourth quarter of 2018, compared with over $300,000 during the fourth quarter of 2021.
Cybercriminals now engage in “double extortion” – demanding a ransom payment to hand over the code that will unlock their encrypted data – and then another ransom payment to not post patients’ sensitive medical information they copied onto the dark web.
Comprehensive cybersecurity insurance will cover “double extortion” payments, legal costs that may arise from defending against patient lawsuits, and the costs of meeting federal and state privacy requirements, including notifying patients of the data breach and regulatory investigations, says Michael Carr, head of risk engineering for North America for Coalition, a cyber insurance firm.
Cyber insurers also contract with vendors who sell bitcoin, which is the currency cybercriminals typically demand for ransom payments, and work with ransom negotiators.
For example, once Coalition decided to pay the ransom on behalf of a health care client, it negotiated the ransom demand down by nearly 75% from $750,000 to $200,000, and proceeded to help the company restore all of its data.
The costs to respond to the incident, to recover lost data, and to pay the extortion, together with the lost business income resulting from the incident, were covered by Coalition’s cyber insurance policy.
Other clients have had their funds retrieved before a fraudulent wire transfer was completed. “Medical practices have vendors they pay regularly. A cybercriminal may compromise your email or take over a bank account and then impersonate a vendor asking to be paid for services they didn’t provide,” says Mr. Carr.
How much coverage do you need? Cost?
Dr. McAneny has increased her cybersecurity coverage every year. “It’s expensive, but I think it’s worth it. But you can never buy enough protection due to the coverage limits.”
She worries that the costs could exceed the limits if a ransomware attack disrupts her practice for days, weeks, or longer, or if the Office for Civil Rights fines her practice $10,000 per patient chart – the practice has 100,000 health records. “That can run several millions of dollars and ruin a practice,” she says.
Health systems and hospitals need massive amounts of coverage, which often runs from $20 million to $30 million, says Mr. Shah. However, practices insured through MagMutual have lower coverage limits that range from $1 million to $5 million, he says.
“A large practice does not necessarily need more than $1,000,000 in coverage if they have limited loss in this area and strong internal processes and controls. Most large practices also have a dedicated information security director, which reduces their risk, so they may be comfortable with $1,000,000 in coverage,” says Mr. Shah.
Premiums are based on the number of patient health records per practice, which translates into higher premiums for larger practices.
Other factors that come into play include the underlying coverage, risk controls the practice has implemented, and its claims history, says Mr. Shah.
However, the cost for cyber liability insurance has increased, and practices can expect to pay higher premiums and deductibles. For example, a practice that paid $10,000 in premiums for a new policy last year will have to pay $20,000 this year, says Dan Hanson, senior vice president of management liability and client experience at Marsh & McLennon Agency, a risk management firm that sells cyber insurance policies.
“We saw 71% of our self-insured clients experience higher deductibles over last year due to increased claim activity and the lack of capacity in the market. The carriers are saying they will set limits, but you are going to pay a lot more, and you are going to participate more in losses through the higher deductibles,” says Mr. Hanson.
Are you eligible?
Cyber insurance companies have a vested interest in avoiding claims. With increasing cyberattacks and larger payouts, many insurers are requiring practices to implement some defensive measures before they insure them. Some insurers, such as Coalition, say they may still insure small practices for comprehensive coverage, but it may impact the pricing or what’s covered, says Mr. Carr.
Here are some of the security measures that cyber insurers are looking for:
- Multifactorial authentication (MFA) requires an extra layer of security to access the system. For example, when logging into your organization’s EHR platform, instead of just using a username and password to access the platform, MFA would require you to input an additional unique login credential before you can access the EHR. A secondary login credential may include security questions, a one-time PIN, or biometrics.
- Removing a terminated employee’s login credentials quickly from the computer system. “One of the most damaging and expensive types of attacks are by disgruntled employees who still have their login credentials and take revenge by logging back into the system and planting malware,” says Mr. Shah.
- Automatic system updates (patches). “Phishing email compromises usually result from a failure to fix vulnerabilities. When a system needs to restart, it should be set to automatically update any potential security loopholes within programs or products,” says Mr. Carr. The firewall settings should also be updated.
- Prior hacking incidents: Are the attackers out of your system? Once criminals hack into the system, your practice is vulnerable to repeat attacks. “If a cyberattack is not completely addressed, threat actors will maintain access to or a presence on the compromised network. In general, we will work with the insured to ensure that the initial point of compromise has been addressed and that any threat actor presence in the network has been removed,” says Mr. Carr.
When doctors compare cybersecurity policies, experts recommend avoiding companies that may offer lower prices but lack a proven track record of handling claims and do not offer resources that can detect a threat, such as ongoing network monitoring and employee training with simulated exercises.
“Practices tend to think, ‘It won’t happen to me.’ Every practice needs to take this seriously,” says Dr. McAneny.
A version of this article first appeared on Medscape.com.
Barbara L. McAneny, MD, CEO of New Mexico Oncology Hematology Consultants, experienced a data breach about 10 years ago, when a laptop was stolen from her large practice.
She and the other physicians were upset and worried that the individual would attempt to log in to the computer system and hack their patients’ private health information.
Dr. McAneny was also worried that the practice would have to pay a hefty fine to the government for having unsecured private health information on a laptop. She could have paid from $50,000 to more than $1.9 million for lost and stolen devices (although that didn’t happen).
Dr. McAneny had a standard cyber liability benefit in her med-mal policy that covered up to $50,000 of the data breach costs. That covered the legal advice The Doctors Company provided about state and federal reporting requirements when a data breach occurs and the costs the practice incurred from mailing letters to all of its patients notifying them of the data breach, says Dr. McAneny.
“The data breach taught me a lot. Our practice spent a lot of money on increasing our internal controls, cybersecurity, and monitoring. Our IT department started testing our computer firewalls periodically, and that’s how we discovered that cybercriminals were attempting to break into our computer system at least 100 times daily,” says Dr. McAneny.
That discovery changed how she thought about insurance. “I decided the med-mal benefit wasn’t enough. I bought the best cybersecurity policy we could afford to protect against future breaches, especially malware or ransomware attacks.”
Her practice also had to make its electronic health records (EHRs) more secure to comply with the Department of Health & Human Services Office of Civil Rights standards for protected health information. The cost of increased security wasn’t covered by her cyber benefit.
Cyberattacks increasing in health care
Despite having comprehensive coverage, Dr. McAneny worries that the cybercriminals are a step ahead of the cybersecurity experts and her practice will eventually have another data breach.
“The policy only covers things that we know about today. As we upgrade our defenses, criminals are finding new ways to breach firewalls and work around our defenses,” she says.
So far this year, nearly 200 medical groups have reported cyberattacks involving 500 or more of their patients’ medical records to the federal government.
EHRs are valuable targets to cybercriminals because of the protected health information they contain. Cybercriminals grab information such as Social Security numbers, dates of birth, medical procedures and results, and in some cases billing and financial information and sell it on the dark web.
They typically bundle the information and sell it to other criminals who later use it for various kinds of fraud and extortion such as banking and credit fraud, health care fraud, identity theft, and ransom extortion.
What do most doctors have?
The vast majority (82%) of doctors polled by the Medical Group Management Association last year said they had cyber insurance, compared with 54% in 2018.
For those who answered “yes,” many said they have coverage through their malpractice insurance carrier.
David Zetter, president of Zetter HealthCare Management Consultants, recommends that physicians speak with their malpractice carrier to determine what coverage they have, if any, within their malpractice policy.
A typical cybersecurity benefit is limited to what is needed to fix and resolve the hacking incident, says Raj Shah, senior regulatory attorney and policyholder advisor at MagMutual, which insures medical practices for malpractice and cyber liability.
That usually covers investigating the cause of the breach and the extent of the damage, legal advice about federal and state reporting requirements, whether to pay a ransom, and a public relations professional to handle patient communication, says Mr. Shah.
The benefit doesn’t cover lost patient revenue when practices have to shut down their operations, the cost of replacing damaged computers, or the ransom payment, he says.
Mr. Zetter advises doctors to consider buying cybersecurity coverage. “I recommend that they speak with an insurance broker who is experienced with cybersecurity policies sold to health care professionals to determine what type of coverage and how much coverage they may need. Their malpractice carrier may also be able to provide some answers,” says Mr. Zetter.
The physician will need to be able to answer questions about their network and how many staff they have and may need to involve their IT vendor too, he adds.
How does comprehensive coverage compare?
Ransomware attacks continue to be one of the most frequent types of attacks, and the amount criminals are demanding has risen significantly. The median ransom payment was $5,000 in the fourth quarter of 2018, compared with over $300,000 during the fourth quarter of 2021.
Cybercriminals now engage in “double extortion” – demanding a ransom payment to hand over the code that will unlock their encrypted data – and then another ransom payment to not post patients’ sensitive medical information they copied onto the dark web.
Comprehensive cybersecurity insurance will cover “double extortion” payments, legal costs that may arise from defending against patient lawsuits, and the costs of meeting federal and state privacy requirements, including notifying patients of the data breach and regulatory investigations, says Michael Carr, head of risk engineering for North America for Coalition, a cyber insurance firm.
Cyber insurers also contract with vendors who sell bitcoin, which is the currency cybercriminals typically demand for ransom payments, and work with ransom negotiators.
For example, once Coalition decided to pay the ransom on behalf of a health care client, it negotiated the ransom demand down by nearly 75% from $750,000 to $200,000, and proceeded to help the company restore all of its data.
The costs to respond to the incident, to recover lost data, and to pay the extortion, together with the lost business income resulting from the incident, were covered by Coalition’s cyber insurance policy.
Other clients have had their funds retrieved before a fraudulent wire transfer was completed. “Medical practices have vendors they pay regularly. A cybercriminal may compromise your email or take over a bank account and then impersonate a vendor asking to be paid for services they didn’t provide,” says Mr. Carr.
How much coverage do you need? Cost?
Dr. McAneny has increased her cybersecurity coverage every year. “It’s expensive, but I think it’s worth it. But you can never buy enough protection due to the coverage limits.”
She worries that the costs could exceed the limits if a ransomware attack disrupts her practice for days, weeks, or longer, or if the Office for Civil Rights fines her practice $10,000 per patient chart – the practice has 100,000 health records. “That can run several millions of dollars and ruin a practice,” she says.
Health systems and hospitals need massive amounts of coverage, which often runs from $20 million to $30 million, says Mr. Shah. However, practices insured through MagMutual have lower coverage limits that range from $1 million to $5 million, he says.
“A large practice does not necessarily need more than $1,000,000 in coverage if they have limited loss in this area and strong internal processes and controls. Most large practices also have a dedicated information security director, which reduces their risk, so they may be comfortable with $1,000,000 in coverage,” says Mr. Shah.
Premiums are based on the number of patient health records per practice, which translates into higher premiums for larger practices.
Other factors that come into play include the underlying coverage, risk controls the practice has implemented, and its claims history, says Mr. Shah.
However, the cost for cyber liability insurance has increased, and practices can expect to pay higher premiums and deductibles. For example, a practice that paid $10,000 in premiums for a new policy last year will have to pay $20,000 this year, says Dan Hanson, senior vice president of management liability and client experience at Marsh & McLennon Agency, a risk management firm that sells cyber insurance policies.
“We saw 71% of our self-insured clients experience higher deductibles over last year due to increased claim activity and the lack of capacity in the market. The carriers are saying they will set limits, but you are going to pay a lot more, and you are going to participate more in losses through the higher deductibles,” says Mr. Hanson.
Are you eligible?
Cyber insurance companies have a vested interest in avoiding claims. With increasing cyberattacks and larger payouts, many insurers are requiring practices to implement some defensive measures before they insure them. Some insurers, such as Coalition, say they may still insure small practices for comprehensive coverage, but it may impact the pricing or what’s covered, says Mr. Carr.
Here are some of the security measures that cyber insurers are looking for:
- Multifactorial authentication (MFA) requires an extra layer of security to access the system. For example, when logging into your organization’s EHR platform, instead of just using a username and password to access the platform, MFA would require you to input an additional unique login credential before you can access the EHR. A secondary login credential may include security questions, a one-time PIN, or biometrics.
- Removing a terminated employee’s login credentials quickly from the computer system. “One of the most damaging and expensive types of attacks are by disgruntled employees who still have their login credentials and take revenge by logging back into the system and planting malware,” says Mr. Shah.
- Automatic system updates (patches). “Phishing email compromises usually result from a failure to fix vulnerabilities. When a system needs to restart, it should be set to automatically update any potential security loopholes within programs or products,” says Mr. Carr. The firewall settings should also be updated.
- Prior hacking incidents: Are the attackers out of your system? Once criminals hack into the system, your practice is vulnerable to repeat attacks. “If a cyberattack is not completely addressed, threat actors will maintain access to or a presence on the compromised network. In general, we will work with the insured to ensure that the initial point of compromise has been addressed and that any threat actor presence in the network has been removed,” says Mr. Carr.
When doctors compare cybersecurity policies, experts recommend avoiding companies that may offer lower prices but lack a proven track record of handling claims and do not offer resources that can detect a threat, such as ongoing network monitoring and employee training with simulated exercises.
“Practices tend to think, ‘It won’t happen to me.’ Every practice needs to take this seriously,” says Dr. McAneny.
A version of this article first appeared on Medscape.com.
Amniotic fluid embolism: Management using a checklist
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
High deductible insurance linked to delayed advanced cancer diagnosis
In oncology, delayed care may result in a failed opportunity to achieve remission. Delays in diagnosis can result in patients having to undergo more extensive surgery, radiation exposure, or more intensive drug therapy than if their disease had been detected at an early stage.
Now, researchers at Harvard Medical School, Boston, report that
Using national insurance claims data, the authors conducted an observational study to examine what happened when some workers with employer-based insurance were switched from low-deductible to high-deductible plans, compared with a control group of workers who remained on low-deductible plans.
After the switch, workers shunted into high-deductible plans had a longer time to first diagnosis of a metastatic cancer, indicating delayed detection of advanced disease, compared with controls. The difference translated into a delay in diagnosis of metastatic disease of nearly 5 months, reported Nico Trad, BA, a fourth-year medical student at Dana-Farber Cancer Institute, Boston.
“The takeaway here is that these plans were associated with delayed detection of metastatic cancer. We did not assess the mechanism, but it’s a reasonable assumption to make that increased cost-sharing is having some adverse impacts on people’s willingness to seek care. And although we didn’t study potential impacts, we might anticipate that a delayed diagnosis might also lead to delayed engagement with palliative care,” he said in an oral abstract presentation at the annual meeting of the American Society of Clinical Oncology.
“A delay in initiation of symptom-relieving therapies and a delayed presentation might also lead to greater dissemination of disease throughout the body, which also has the potential to limit therapeutic options,” he added.
‘Deductible relief day’
Mr. Trad said that in 2022 more than half of employees are covered by high-deductible health plans, compared with only about 10% in 2006.
This major shift in cost burden coincided with President Joseph Biden’s announcement in early 2022 of the “Cancer Moonshot,” program with the goal of reducing cancer mortality by 50% over the next 25 years.
“Part of that is cancer prevention and control, which involves timely detection of cancer so that we can treat it early and have better outcomes,” he said.
High-deductible health plans ostensibly provide motivation for patients to shop for lower-priced care and avoid unnecessary or low-quality care, but making patients shell out more upfront before their insurance kicks in, while it reduced health care utilization, can also reduce the quality of care, he said.
In 2022, “Deductible Relief Day,” the day in which the average patient has satisfied the deductible and insurance starts to pick up more of the tab, occurred in mid-May, compared with late February in 2006.
Insurance claims data
Mr. Trad and colleagues used health insurance claims data from a nationally representative cohort of privately insured patients in a national commercial and Medicare Advantage database. They excluded patients 65 and older who were eligible for Medicare because it does not have high-deductible options.
The study cohort included 345,401 adults from the ages of 18 to 64 whose employers mandated a switch from a low-deductible plan which was defined as $500 or less, to a high-deductible plan defined as $1,000 or more. Controls were 1,654,775 contemporaneous adults whose employers offered only low-deductible plans. Both groups had a 1-year baseline period when all members were enrolled in low deductible plans.
To minimize the possibility of confounding, the investigators matched the participants by age, gender, race/ethnicity, morbidity according to Adjusted Clinical Group score, poverty level, geographic region, employer size, baseline primary cancer, baseline medical and pharmacy costs, and follow-up duration.
During the baseline period, the hazard ratio for time to a first observed metastatic cancer diagnosis in the main cohort, compared with controls, was 0.96 with a nonsignificant P value, indicating no difference in the time to diagnosis between the groups.
During a maximum 13.5 years of follow-up, however, the participants who had been switched after a year to a high-deductible plan had a significantly longer time to first metastatic diagnosis (HR, 0.88; P = .01), indicating delayed diagnosis relative to controls. This difference translated to a delay of 4.6 months associated with the higher out-of-pocket costs plans.
According to a systematic review and meta-analysis published online in 2020, a 1-month delay in treatment for many types of cancer can translate into a 6% to 13% higher risk for death, a risk that continues to increase with further delays.
The investigators acknowledged that the study was limited by the use of retrospective claims-based data, which not contain information on how the patients fared after diagnosis.
“I would say in terms of policy relevance that this really points to the need for new and innovative insurance models that, No. 1, reduce the cost-sharing burden for patients so that they’re not deterred from seeking care, and No. 2, that align rather than contradict the goal of improving population-level survival from cancer,” Mr. Trad said.
Further evidence of a flawed system
The study adds to an already strong body of evidence showing that high-deductible plans can have a negative impact on health, said Sara R. Collins, vice president for health care coverage and access at the Commonwealth Fund, a New York–based private foundation dedicated to improving health care.
“This is really the latest evidence on top of years of research that shows that high-deductible health plans lead people to make decisions that are not in the best interest of their health,” said Ms. Collins, who is not affiliated with the study presented at ASCO.
“We have a health care cost problem in the United States that far exceeds that of other high-income countries. Insurers try to solve it by shifting the costs to consumers and using other measures to restrict people’s use of health care, and often needed health care like this. The result is less access to needed care, and long-term adverse health consequences and their associated costs to patients and the health system generally,” she said.
The real driver of health care costs is not utilization, but the prices that insurers and providers negotiate in their service contracts, she explained.
“Prices are the central problem, insurers have control over those prices in their negotiations with providers. So unless we can gain control of that driver, patients are going to continue to suffer unnecessarily from both the short- and long-term effects of insurers who use tools to reduce their access to care,” she said.
In oncology, delayed care may result in a failed opportunity to achieve remission. Delays in diagnosis can result in patients having to undergo more extensive surgery, radiation exposure, or more intensive drug therapy than if their disease had been detected at an early stage.
Now, researchers at Harvard Medical School, Boston, report that
Using national insurance claims data, the authors conducted an observational study to examine what happened when some workers with employer-based insurance were switched from low-deductible to high-deductible plans, compared with a control group of workers who remained on low-deductible plans.
After the switch, workers shunted into high-deductible plans had a longer time to first diagnosis of a metastatic cancer, indicating delayed detection of advanced disease, compared with controls. The difference translated into a delay in diagnosis of metastatic disease of nearly 5 months, reported Nico Trad, BA, a fourth-year medical student at Dana-Farber Cancer Institute, Boston.
“The takeaway here is that these plans were associated with delayed detection of metastatic cancer. We did not assess the mechanism, but it’s a reasonable assumption to make that increased cost-sharing is having some adverse impacts on people’s willingness to seek care. And although we didn’t study potential impacts, we might anticipate that a delayed diagnosis might also lead to delayed engagement with palliative care,” he said in an oral abstract presentation at the annual meeting of the American Society of Clinical Oncology.
“A delay in initiation of symptom-relieving therapies and a delayed presentation might also lead to greater dissemination of disease throughout the body, which also has the potential to limit therapeutic options,” he added.
‘Deductible relief day’
Mr. Trad said that in 2022 more than half of employees are covered by high-deductible health plans, compared with only about 10% in 2006.
This major shift in cost burden coincided with President Joseph Biden’s announcement in early 2022 of the “Cancer Moonshot,” program with the goal of reducing cancer mortality by 50% over the next 25 years.
“Part of that is cancer prevention and control, which involves timely detection of cancer so that we can treat it early and have better outcomes,” he said.
High-deductible health plans ostensibly provide motivation for patients to shop for lower-priced care and avoid unnecessary or low-quality care, but making patients shell out more upfront before their insurance kicks in, while it reduced health care utilization, can also reduce the quality of care, he said.
In 2022, “Deductible Relief Day,” the day in which the average patient has satisfied the deductible and insurance starts to pick up more of the tab, occurred in mid-May, compared with late February in 2006.
Insurance claims data
Mr. Trad and colleagues used health insurance claims data from a nationally representative cohort of privately insured patients in a national commercial and Medicare Advantage database. They excluded patients 65 and older who were eligible for Medicare because it does not have high-deductible options.
The study cohort included 345,401 adults from the ages of 18 to 64 whose employers mandated a switch from a low-deductible plan which was defined as $500 or less, to a high-deductible plan defined as $1,000 or more. Controls were 1,654,775 contemporaneous adults whose employers offered only low-deductible plans. Both groups had a 1-year baseline period when all members were enrolled in low deductible plans.
To minimize the possibility of confounding, the investigators matched the participants by age, gender, race/ethnicity, morbidity according to Adjusted Clinical Group score, poverty level, geographic region, employer size, baseline primary cancer, baseline medical and pharmacy costs, and follow-up duration.
During the baseline period, the hazard ratio for time to a first observed metastatic cancer diagnosis in the main cohort, compared with controls, was 0.96 with a nonsignificant P value, indicating no difference in the time to diagnosis between the groups.
During a maximum 13.5 years of follow-up, however, the participants who had been switched after a year to a high-deductible plan had a significantly longer time to first metastatic diagnosis (HR, 0.88; P = .01), indicating delayed diagnosis relative to controls. This difference translated to a delay of 4.6 months associated with the higher out-of-pocket costs plans.
According to a systematic review and meta-analysis published online in 2020, a 1-month delay in treatment for many types of cancer can translate into a 6% to 13% higher risk for death, a risk that continues to increase with further delays.
The investigators acknowledged that the study was limited by the use of retrospective claims-based data, which not contain information on how the patients fared after diagnosis.
“I would say in terms of policy relevance that this really points to the need for new and innovative insurance models that, No. 1, reduce the cost-sharing burden for patients so that they’re not deterred from seeking care, and No. 2, that align rather than contradict the goal of improving population-level survival from cancer,” Mr. Trad said.
Further evidence of a flawed system
The study adds to an already strong body of evidence showing that high-deductible plans can have a negative impact on health, said Sara R. Collins, vice president for health care coverage and access at the Commonwealth Fund, a New York–based private foundation dedicated to improving health care.
“This is really the latest evidence on top of years of research that shows that high-deductible health plans lead people to make decisions that are not in the best interest of their health,” said Ms. Collins, who is not affiliated with the study presented at ASCO.
“We have a health care cost problem in the United States that far exceeds that of other high-income countries. Insurers try to solve it by shifting the costs to consumers and using other measures to restrict people’s use of health care, and often needed health care like this. The result is less access to needed care, and long-term adverse health consequences and their associated costs to patients and the health system generally,” she said.
The real driver of health care costs is not utilization, but the prices that insurers and providers negotiate in their service contracts, she explained.
“Prices are the central problem, insurers have control over those prices in their negotiations with providers. So unless we can gain control of that driver, patients are going to continue to suffer unnecessarily from both the short- and long-term effects of insurers who use tools to reduce their access to care,” she said.
In oncology, delayed care may result in a failed opportunity to achieve remission. Delays in diagnosis can result in patients having to undergo more extensive surgery, radiation exposure, or more intensive drug therapy than if their disease had been detected at an early stage.
Now, researchers at Harvard Medical School, Boston, report that
Using national insurance claims data, the authors conducted an observational study to examine what happened when some workers with employer-based insurance were switched from low-deductible to high-deductible plans, compared with a control group of workers who remained on low-deductible plans.
After the switch, workers shunted into high-deductible plans had a longer time to first diagnosis of a metastatic cancer, indicating delayed detection of advanced disease, compared with controls. The difference translated into a delay in diagnosis of metastatic disease of nearly 5 months, reported Nico Trad, BA, a fourth-year medical student at Dana-Farber Cancer Institute, Boston.
“The takeaway here is that these plans were associated with delayed detection of metastatic cancer. We did not assess the mechanism, but it’s a reasonable assumption to make that increased cost-sharing is having some adverse impacts on people’s willingness to seek care. And although we didn’t study potential impacts, we might anticipate that a delayed diagnosis might also lead to delayed engagement with palliative care,” he said in an oral abstract presentation at the annual meeting of the American Society of Clinical Oncology.
“A delay in initiation of symptom-relieving therapies and a delayed presentation might also lead to greater dissemination of disease throughout the body, which also has the potential to limit therapeutic options,” he added.
‘Deductible relief day’
Mr. Trad said that in 2022 more than half of employees are covered by high-deductible health plans, compared with only about 10% in 2006.
This major shift in cost burden coincided with President Joseph Biden’s announcement in early 2022 of the “Cancer Moonshot,” program with the goal of reducing cancer mortality by 50% over the next 25 years.
“Part of that is cancer prevention and control, which involves timely detection of cancer so that we can treat it early and have better outcomes,” he said.
High-deductible health plans ostensibly provide motivation for patients to shop for lower-priced care and avoid unnecessary or low-quality care, but making patients shell out more upfront before their insurance kicks in, while it reduced health care utilization, can also reduce the quality of care, he said.
In 2022, “Deductible Relief Day,” the day in which the average patient has satisfied the deductible and insurance starts to pick up more of the tab, occurred in mid-May, compared with late February in 2006.
Insurance claims data
Mr. Trad and colleagues used health insurance claims data from a nationally representative cohort of privately insured patients in a national commercial and Medicare Advantage database. They excluded patients 65 and older who were eligible for Medicare because it does not have high-deductible options.
The study cohort included 345,401 adults from the ages of 18 to 64 whose employers mandated a switch from a low-deductible plan which was defined as $500 or less, to a high-deductible plan defined as $1,000 or more. Controls were 1,654,775 contemporaneous adults whose employers offered only low-deductible plans. Both groups had a 1-year baseline period when all members were enrolled in low deductible plans.
To minimize the possibility of confounding, the investigators matched the participants by age, gender, race/ethnicity, morbidity according to Adjusted Clinical Group score, poverty level, geographic region, employer size, baseline primary cancer, baseline medical and pharmacy costs, and follow-up duration.
During the baseline period, the hazard ratio for time to a first observed metastatic cancer diagnosis in the main cohort, compared with controls, was 0.96 with a nonsignificant P value, indicating no difference in the time to diagnosis between the groups.
During a maximum 13.5 years of follow-up, however, the participants who had been switched after a year to a high-deductible plan had a significantly longer time to first metastatic diagnosis (HR, 0.88; P = .01), indicating delayed diagnosis relative to controls. This difference translated to a delay of 4.6 months associated with the higher out-of-pocket costs plans.
According to a systematic review and meta-analysis published online in 2020, a 1-month delay in treatment for many types of cancer can translate into a 6% to 13% higher risk for death, a risk that continues to increase with further delays.
The investigators acknowledged that the study was limited by the use of retrospective claims-based data, which not contain information on how the patients fared after diagnosis.
“I would say in terms of policy relevance that this really points to the need for new and innovative insurance models that, No. 1, reduce the cost-sharing burden for patients so that they’re not deterred from seeking care, and No. 2, that align rather than contradict the goal of improving population-level survival from cancer,” Mr. Trad said.
Further evidence of a flawed system
The study adds to an already strong body of evidence showing that high-deductible plans can have a negative impact on health, said Sara R. Collins, vice president for health care coverage and access at the Commonwealth Fund, a New York–based private foundation dedicated to improving health care.
“This is really the latest evidence on top of years of research that shows that high-deductible health plans lead people to make decisions that are not in the best interest of their health,” said Ms. Collins, who is not affiliated with the study presented at ASCO.
“We have a health care cost problem in the United States that far exceeds that of other high-income countries. Insurers try to solve it by shifting the costs to consumers and using other measures to restrict people’s use of health care, and often needed health care like this. The result is less access to needed care, and long-term adverse health consequences and their associated costs to patients and the health system generally,” she said.
The real driver of health care costs is not utilization, but the prices that insurers and providers negotiate in their service contracts, she explained.
“Prices are the central problem, insurers have control over those prices in their negotiations with providers. So unless we can gain control of that driver, patients are going to continue to suffer unnecessarily from both the short- and long-term effects of insurers who use tools to reduce their access to care,” she said.
FROM ASCO 2022
Inflation and health care: The prognosis for doctors
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Docs reveal perils of giving medical advice to friends and family
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
CMS unveils replacement for the Oncology Care Model
that ended on June 30.
The OCM’s successor, known as the Enhancing Oncology Model (EOM), will begin next year on July 1, and run for 5 years.
Like the OCM, the EOM will align payment incentives with care quality, and focus on value-based, patient-centered care for those undergoing chemotherapy based on 6-month episodes of care. The EOM will focus on health equity, and participants will include oncology practices that treat Medicare beneficiaries receiving chemotherapy for seven types of cancer: breast cancer, chronic leukemia, lung cancer, lymphoma, multiple myeloma, prostate cancer, and small intestine/colorectal cancer.
The new model will build on lessons learned from the OCM, incorporating successful elements of the previous model, such as patient navigation and care planning, and will introduce new elements, including gradually implementing electronic Patient-Reported Outcomes and activities that promote health equity.
In a statement, CMS Administrator Chiquita Brooks-LaSure noted that the EOM will “incentivize participating oncology practices – including those in rural and underserved areas – to improve the provision of high-quality, coordinated care that addresses patients’ social needs and improves patient and caregiver support.”
The goal, Ms. Brooks-LaSure added, is to address “stark inequities in the ability of people with cancer across race, gender, region, and income to access cancer screening, diagnostics, and treatment. CMS is working to advance President Biden’s Cancer Moonshot goals by helping Medicare cancer patients better navigate a challenging and often overwhelming journey.”
Applauds and concerns
The American Society of Clinical Oncology, the Association of Community Cancer Centers, and the Community Oncology Alliance all issued statements applauding the new model and the fact that it is voluntary. But they have also voiced several concerns.
The COA, for example, noted that the CMS Innovation Center plans to cut the Monthly Enhanced Oncology Services payments in the EOM by more than half ($70 vs $160 for the OCM), but at the same time, expects more work from practices.
While COA is “extremely supportive” of screening for health-related social needs and electronic patient-reported outcomes, “it seems unfair to burden practices with more work but pay less for it, particularly as practices are dealing with the return of the Medicare sequester cut, inflation, and ongoing COVID-19 practice challenges,” Ted Okon, executive director of COA, wrote in a statement.
COA also expressed concern with the 1-year gap between the end of the OCM and the start of EOM.
“During this time practices will have to shoulder the extensive investments and operational changes put in place to benefit patients without reimbursement,” Mr. Okon said.
ASCO echoed COA’s concerns and the ACCC expressed unease with some of the structural elements of the program.
The EOM includes two risk arrangements with different degrees of downside risk. However, requiring participants to accept downside risk from the start of the model “will be a significant barrier to enrollment given the current reimbursement landscape,” the ACCC said in a statement. This risk “may not make financial sense for smaller oncology programs, particularly those who care for underserved patients and those that have not previously participated in OCM.”
Instead, CMS should “endeavor to provide as much information on proposed payment methodologies, cost data, and benchmark amounts as early as possible so that practices can make informed decisions around participation,” the ACCC wrote.
An improvement over OCM?
The OCM represented the largest alternative payment model to address value-based payment for cancer care. More than 3,200 oncologists and 201 physician practices voluntarily entered the program, which lasted 6 years.
But since its implementation, studies assessing the success of the program have yielded mixed results.
A 2018 analysis, for instance, revealed that one large community practice saved Medicare $3 million over a year after adopting the OCM.
However, a 2021 study found that, while community practices experienced lower drug costs in lung and prostate cancer and lower office-based costs after implementing the program, the difference was not statistically significant when accounting for all costs.
Another analysis also revealed more mixed results, reporting cost reductions for all cancers, but also finding those savings were offset by administrative expenses. Overall, this study found the OCM led to a $155 million net loss to Medicare over 4 years.
Will the EOM improve upon the OCM?
According to the CMS, “the central goal of EOM is to better support patients and improve their care experience.”
Participating Physician Group Practices will take accountability for health care quality and total spending during 6-month episodes of care for Medicare patients with certain cancers.
CMS will give participants the option to bill for Monthly Enhanced Oncology Services payment for services provided to eligible beneficiaries. This payment will be higher for beneficiaries dually eligible for Medicare and Medicaid.
EOM participants will have the opportunity to earn a retrospective performance-based payment based on quality and savings. Participants will be required to take on downside risk from the start of the model, with the potential to owe CMS a performance-based recoupment.
EOM participants will be required to implement participant redesign activities, including 24/7 access to care, patient navigation, care planning, use of evidence-based guidelines, use of electronic Patient Reported Outcomes, screening for health-related social needs, use of data for quality improvement, and use of certified electronic health record technology.
“No one should have to battle cancer without access to high-quality, coordinated care,” said Health & Human Services Secretary Xavier Becerra, in a statement. “With this new Innovation Center model for oncology care, we are delivering on President Biden’s call to action to mobilize every option to address cancer, and creating a system of care that supports all patients and their families.”
A detailed payment methodology paper will be published for EOM this summer and will be available on the Innovation Center’s website.
A version of this article first appeared on Medscape.com.
that ended on June 30.
The OCM’s successor, known as the Enhancing Oncology Model (EOM), will begin next year on July 1, and run for 5 years.
Like the OCM, the EOM will align payment incentives with care quality, and focus on value-based, patient-centered care for those undergoing chemotherapy based on 6-month episodes of care. The EOM will focus on health equity, and participants will include oncology practices that treat Medicare beneficiaries receiving chemotherapy for seven types of cancer: breast cancer, chronic leukemia, lung cancer, lymphoma, multiple myeloma, prostate cancer, and small intestine/colorectal cancer.
The new model will build on lessons learned from the OCM, incorporating successful elements of the previous model, such as patient navigation and care planning, and will introduce new elements, including gradually implementing electronic Patient-Reported Outcomes and activities that promote health equity.
In a statement, CMS Administrator Chiquita Brooks-LaSure noted that the EOM will “incentivize participating oncology practices – including those in rural and underserved areas – to improve the provision of high-quality, coordinated care that addresses patients’ social needs and improves patient and caregiver support.”
The goal, Ms. Brooks-LaSure added, is to address “stark inequities in the ability of people with cancer across race, gender, region, and income to access cancer screening, diagnostics, and treatment. CMS is working to advance President Biden’s Cancer Moonshot goals by helping Medicare cancer patients better navigate a challenging and often overwhelming journey.”
Applauds and concerns
The American Society of Clinical Oncology, the Association of Community Cancer Centers, and the Community Oncology Alliance all issued statements applauding the new model and the fact that it is voluntary. But they have also voiced several concerns.
The COA, for example, noted that the CMS Innovation Center plans to cut the Monthly Enhanced Oncology Services payments in the EOM by more than half ($70 vs $160 for the OCM), but at the same time, expects more work from practices.
While COA is “extremely supportive” of screening for health-related social needs and electronic patient-reported outcomes, “it seems unfair to burden practices with more work but pay less for it, particularly as practices are dealing with the return of the Medicare sequester cut, inflation, and ongoing COVID-19 practice challenges,” Ted Okon, executive director of COA, wrote in a statement.
COA also expressed concern with the 1-year gap between the end of the OCM and the start of EOM.
“During this time practices will have to shoulder the extensive investments and operational changes put in place to benefit patients without reimbursement,” Mr. Okon said.
ASCO echoed COA’s concerns and the ACCC expressed unease with some of the structural elements of the program.
The EOM includes two risk arrangements with different degrees of downside risk. However, requiring participants to accept downside risk from the start of the model “will be a significant barrier to enrollment given the current reimbursement landscape,” the ACCC said in a statement. This risk “may not make financial sense for smaller oncology programs, particularly those who care for underserved patients and those that have not previously participated in OCM.”
Instead, CMS should “endeavor to provide as much information on proposed payment methodologies, cost data, and benchmark amounts as early as possible so that practices can make informed decisions around participation,” the ACCC wrote.
An improvement over OCM?
The OCM represented the largest alternative payment model to address value-based payment for cancer care. More than 3,200 oncologists and 201 physician practices voluntarily entered the program, which lasted 6 years.
But since its implementation, studies assessing the success of the program have yielded mixed results.
A 2018 analysis, for instance, revealed that one large community practice saved Medicare $3 million over a year after adopting the OCM.
However, a 2021 study found that, while community practices experienced lower drug costs in lung and prostate cancer and lower office-based costs after implementing the program, the difference was not statistically significant when accounting for all costs.
Another analysis also revealed more mixed results, reporting cost reductions for all cancers, but also finding those savings were offset by administrative expenses. Overall, this study found the OCM led to a $155 million net loss to Medicare over 4 years.
Will the EOM improve upon the OCM?
According to the CMS, “the central goal of EOM is to better support patients and improve their care experience.”
Participating Physician Group Practices will take accountability for health care quality and total spending during 6-month episodes of care for Medicare patients with certain cancers.
CMS will give participants the option to bill for Monthly Enhanced Oncology Services payment for services provided to eligible beneficiaries. This payment will be higher for beneficiaries dually eligible for Medicare and Medicaid.
EOM participants will have the opportunity to earn a retrospective performance-based payment based on quality and savings. Participants will be required to take on downside risk from the start of the model, with the potential to owe CMS a performance-based recoupment.
EOM participants will be required to implement participant redesign activities, including 24/7 access to care, patient navigation, care planning, use of evidence-based guidelines, use of electronic Patient Reported Outcomes, screening for health-related social needs, use of data for quality improvement, and use of certified electronic health record technology.
“No one should have to battle cancer without access to high-quality, coordinated care,” said Health & Human Services Secretary Xavier Becerra, in a statement. “With this new Innovation Center model for oncology care, we are delivering on President Biden’s call to action to mobilize every option to address cancer, and creating a system of care that supports all patients and their families.”
A detailed payment methodology paper will be published for EOM this summer and will be available on the Innovation Center’s website.
A version of this article first appeared on Medscape.com.
that ended on June 30.
The OCM’s successor, known as the Enhancing Oncology Model (EOM), will begin next year on July 1, and run for 5 years.
Like the OCM, the EOM will align payment incentives with care quality, and focus on value-based, patient-centered care for those undergoing chemotherapy based on 6-month episodes of care. The EOM will focus on health equity, and participants will include oncology practices that treat Medicare beneficiaries receiving chemotherapy for seven types of cancer: breast cancer, chronic leukemia, lung cancer, lymphoma, multiple myeloma, prostate cancer, and small intestine/colorectal cancer.
The new model will build on lessons learned from the OCM, incorporating successful elements of the previous model, such as patient navigation and care planning, and will introduce new elements, including gradually implementing electronic Patient-Reported Outcomes and activities that promote health equity.
In a statement, CMS Administrator Chiquita Brooks-LaSure noted that the EOM will “incentivize participating oncology practices – including those in rural and underserved areas – to improve the provision of high-quality, coordinated care that addresses patients’ social needs and improves patient and caregiver support.”
The goal, Ms. Brooks-LaSure added, is to address “stark inequities in the ability of people with cancer across race, gender, region, and income to access cancer screening, diagnostics, and treatment. CMS is working to advance President Biden’s Cancer Moonshot goals by helping Medicare cancer patients better navigate a challenging and often overwhelming journey.”
Applauds and concerns
The American Society of Clinical Oncology, the Association of Community Cancer Centers, and the Community Oncology Alliance all issued statements applauding the new model and the fact that it is voluntary. But they have also voiced several concerns.
The COA, for example, noted that the CMS Innovation Center plans to cut the Monthly Enhanced Oncology Services payments in the EOM by more than half ($70 vs $160 for the OCM), but at the same time, expects more work from practices.
While COA is “extremely supportive” of screening for health-related social needs and electronic patient-reported outcomes, “it seems unfair to burden practices with more work but pay less for it, particularly as practices are dealing with the return of the Medicare sequester cut, inflation, and ongoing COVID-19 practice challenges,” Ted Okon, executive director of COA, wrote in a statement.
COA also expressed concern with the 1-year gap between the end of the OCM and the start of EOM.
“During this time practices will have to shoulder the extensive investments and operational changes put in place to benefit patients without reimbursement,” Mr. Okon said.
ASCO echoed COA’s concerns and the ACCC expressed unease with some of the structural elements of the program.
The EOM includes two risk arrangements with different degrees of downside risk. However, requiring participants to accept downside risk from the start of the model “will be a significant barrier to enrollment given the current reimbursement landscape,” the ACCC said in a statement. This risk “may not make financial sense for smaller oncology programs, particularly those who care for underserved patients and those that have not previously participated in OCM.”
Instead, CMS should “endeavor to provide as much information on proposed payment methodologies, cost data, and benchmark amounts as early as possible so that practices can make informed decisions around participation,” the ACCC wrote.
An improvement over OCM?
The OCM represented the largest alternative payment model to address value-based payment for cancer care. More than 3,200 oncologists and 201 physician practices voluntarily entered the program, which lasted 6 years.
But since its implementation, studies assessing the success of the program have yielded mixed results.
A 2018 analysis, for instance, revealed that one large community practice saved Medicare $3 million over a year after adopting the OCM.
However, a 2021 study found that, while community practices experienced lower drug costs in lung and prostate cancer and lower office-based costs after implementing the program, the difference was not statistically significant when accounting for all costs.
Another analysis also revealed more mixed results, reporting cost reductions for all cancers, but also finding those savings were offset by administrative expenses. Overall, this study found the OCM led to a $155 million net loss to Medicare over 4 years.
Will the EOM improve upon the OCM?
According to the CMS, “the central goal of EOM is to better support patients and improve their care experience.”
Participating Physician Group Practices will take accountability for health care quality and total spending during 6-month episodes of care for Medicare patients with certain cancers.
CMS will give participants the option to bill for Monthly Enhanced Oncology Services payment for services provided to eligible beneficiaries. This payment will be higher for beneficiaries dually eligible for Medicare and Medicaid.
EOM participants will have the opportunity to earn a retrospective performance-based payment based on quality and savings. Participants will be required to take on downside risk from the start of the model, with the potential to owe CMS a performance-based recoupment.
EOM participants will be required to implement participant redesign activities, including 24/7 access to care, patient navigation, care planning, use of evidence-based guidelines, use of electronic Patient Reported Outcomes, screening for health-related social needs, use of data for quality improvement, and use of certified electronic health record technology.
“No one should have to battle cancer without access to high-quality, coordinated care,” said Health & Human Services Secretary Xavier Becerra, in a statement. “With this new Innovation Center model for oncology care, we are delivering on President Biden’s call to action to mobilize every option to address cancer, and creating a system of care that supports all patients and their families.”
A detailed payment methodology paper will be published for EOM this summer and will be available on the Innovation Center’s website.
A version of this article first appeared on Medscape.com.