User login
A nurse’s view: Blood test for severe preeclampsia will save lives
There is amazing news for the world of obstetrics and for all pregnant women. Severe preeclampsia is a critical obstetrical condition that can have serious outcomes for a mother and baby. It can lead to eclampsia, an obstetrical emergency, which often results in death of the mother and/or baby.
Based on research published in the Journal of the American Heart Association, the incidence of new‐onset hypertensive disorders of pregnancy (gestational hypertension and preeclampsia/eclampsia) have nearly doubled in the United States from 2007 to 2019. And they continue to climb.
According to the Preeclampsia Foundation, 5%-8% of all pregnancies in the United States will result in preeclampsia. Black women are at a 60% higher risk than white women, and according to various sources, other risk groups include those who became pregnant via in vitro fertilization, mothers of multiples (twins and triplets), women with gestational diabetes, women over age 35, women with chronic hypertension, obesity, polycystic ovary syndrome, sickle cell disease, rheumatoid arthritis, lupus, migraines, antiphospholipid syndrome, previous pregnancy with preeclampsia, family history, and scleroderma.
Screening and treatment
Preeclampsia is a multiorgan disease of pregnancy, and can be mild, but may quickly progress to severe, which can be life-threatening for mother and baby. It was previously referred to as toxemia or the high blood pressure disease of pregnancy. It primarily involves the cardiovascular, neurologic and renal systems, and the liver. Patients typically present with elevated blood pressures, but other symptoms may include headache, swelling of hands and feet, blurry/double vision or seeing spots, nausea/vomiting, and epigastric pain. It is diagnosed with elevated blood pressures, blood work, and protein in the urine.
Early screening for preeclampsia is done in the first trimester. Presently, a combination of prenatal blood work, blood pressure monitoring, and recognition of high-risk groups is used to determine a treatment plan going forward. The American Congress of Obstetricians and Gynecologists recommends women that fall into this group for potentially developing preeclampsia take daily aspirin as a preventative measure.
In its milder form, a pregnant woman can be observed as an outpatient – monitored with antepartum testing, lab work, and patient education to report significant symptoms as listed above. Teaching patients about fetal kick counts to monitor their baby’s movements is equally important. Women with mild preeclampsia usually can safely deliver at term, being induced between 37-39 weeks’ gestation.
On the other hand, if mild preeclampsia progresses to severe preeclampsia, delivery may be preterm for the safety of mother and baby. Severe preeclampsia can lead to maternal organ damage, seizures, and even death of mother and/or baby.
About 20% of women with severe preeclampsia will develop HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelets) syndrome, a life-threatening disease that often warrants immediate delivery. According to the National Library of Medicine, the mortality rate of women with HELLP syndrome is up to 24% and the perinatal death rate is up as high as 37%. These serious conditions can cause ineffective maternal clotting, liver rupture, placental abruption, and postpartum hemorrhage. It is most prevalent in the third trimester but can occur within 48 hours of delivery.
The only cure for preeclampsia in any form is delivery.
Patients with severe preeclampsia are hospitalized until delivery – sometimes a few days to a couple of weeks. Mother and baby are closely watched for further progression, including signs of organ damage in the mother and changes to the well-being of the baby. If the mother’s health is severely compromised, then the baby will be compromised as well. A preterm delivery may be necessary.
Impact of the new test
The National Institute of Health states that preterm babies born from preeclamptic mothers can suffer many health problems including cerebral palsy, deafness, blindness, epilepsy, and a host of other respiratory, cardiovascular, and endocrine issues. But the biggest issue is preterm birth, defined as birth before 37 weeks gestation. Being born preterm can require a long stay in the intensive care nursery.
This is where the first-of-its-kind prognostic blood test comes into play. The test’s ability to predict severe preeclampsia within 2 weeks can help save lives. The test can offer health care providers the ability to administer steroids for fetal lung maturity before delivery and be more prepared to care for what could be a very compromised newborn.
The blood test, which is recommended between 23-35 weeks gestation, involves analyzing a ratio between two proteins from the placenta, sFlt1 and PIGF. The higher the ratio, the higher the risk that severe preeclampsia will develop. Results can be available within 30 minutes, which is critical when contemplating treatment.
An example of the use of this ratio is illustrated with chronic hypertension in pregnancy, which is defined as elevated blood pressure before 20 weeks or even before conception. Since chronic hypertension can be a primary precursor to preeclampsia, patients with this condition are at higher risk. The FDA-approved blood test would be helpful in determining the plan of care; that is, delivery versus hospitalization versus monitor as an outpatient.
With a positive test result, a pregnant woman can be immediately hospitalized where she can get the care she and baby need as they await delivery. Since health care providers already know the high-risk groups, surveillance can begin early, utilizing this blood test to predict the progression to severe preeclampsia. Conversely, if the test is negative, a treatment plan can be made as an outpatient and the pregnancy continues.
Not all hospitals are equipped to care for premature babies. If delivery is not imminent, providers can use this blood test to identify those that should be transferred to a tertiary center for observation and monitoring. Mother and baby would then not be separated after birth.
We really don’t know who will develop severe preeclampsia and who won’t. This new blood test will be a critical tool as pregnant patients go through their second and third trimesters. It will be especially pivotal for these women, but important for all pregnant women in reducing maternal and fetal mortality and morbidity.
Ms. Barnett is a registered nurse in the department of obstetrics, Mills-Peninsula Medical Center, Burlingame, Calif. She has disclosed no relevant financial relationships.
There is amazing news for the world of obstetrics and for all pregnant women. Severe preeclampsia is a critical obstetrical condition that can have serious outcomes for a mother and baby. It can lead to eclampsia, an obstetrical emergency, which often results in death of the mother and/or baby.
Based on research published in the Journal of the American Heart Association, the incidence of new‐onset hypertensive disorders of pregnancy (gestational hypertension and preeclampsia/eclampsia) have nearly doubled in the United States from 2007 to 2019. And they continue to climb.
According to the Preeclampsia Foundation, 5%-8% of all pregnancies in the United States will result in preeclampsia. Black women are at a 60% higher risk than white women, and according to various sources, other risk groups include those who became pregnant via in vitro fertilization, mothers of multiples (twins and triplets), women with gestational diabetes, women over age 35, women with chronic hypertension, obesity, polycystic ovary syndrome, sickle cell disease, rheumatoid arthritis, lupus, migraines, antiphospholipid syndrome, previous pregnancy with preeclampsia, family history, and scleroderma.
Screening and treatment
Preeclampsia is a multiorgan disease of pregnancy, and can be mild, but may quickly progress to severe, which can be life-threatening for mother and baby. It was previously referred to as toxemia or the high blood pressure disease of pregnancy. It primarily involves the cardiovascular, neurologic and renal systems, and the liver. Patients typically present with elevated blood pressures, but other symptoms may include headache, swelling of hands and feet, blurry/double vision or seeing spots, nausea/vomiting, and epigastric pain. It is diagnosed with elevated blood pressures, blood work, and protein in the urine.
Early screening for preeclampsia is done in the first trimester. Presently, a combination of prenatal blood work, blood pressure monitoring, and recognition of high-risk groups is used to determine a treatment plan going forward. The American Congress of Obstetricians and Gynecologists recommends women that fall into this group for potentially developing preeclampsia take daily aspirin as a preventative measure.
In its milder form, a pregnant woman can be observed as an outpatient – monitored with antepartum testing, lab work, and patient education to report significant symptoms as listed above. Teaching patients about fetal kick counts to monitor their baby’s movements is equally important. Women with mild preeclampsia usually can safely deliver at term, being induced between 37-39 weeks’ gestation.
On the other hand, if mild preeclampsia progresses to severe preeclampsia, delivery may be preterm for the safety of mother and baby. Severe preeclampsia can lead to maternal organ damage, seizures, and even death of mother and/or baby.
About 20% of women with severe preeclampsia will develop HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelets) syndrome, a life-threatening disease that often warrants immediate delivery. According to the National Library of Medicine, the mortality rate of women with HELLP syndrome is up to 24% and the perinatal death rate is up as high as 37%. These serious conditions can cause ineffective maternal clotting, liver rupture, placental abruption, and postpartum hemorrhage. It is most prevalent in the third trimester but can occur within 48 hours of delivery.
The only cure for preeclampsia in any form is delivery.
Patients with severe preeclampsia are hospitalized until delivery – sometimes a few days to a couple of weeks. Mother and baby are closely watched for further progression, including signs of organ damage in the mother and changes to the well-being of the baby. If the mother’s health is severely compromised, then the baby will be compromised as well. A preterm delivery may be necessary.
Impact of the new test
The National Institute of Health states that preterm babies born from preeclamptic mothers can suffer many health problems including cerebral palsy, deafness, blindness, epilepsy, and a host of other respiratory, cardiovascular, and endocrine issues. But the biggest issue is preterm birth, defined as birth before 37 weeks gestation. Being born preterm can require a long stay in the intensive care nursery.
This is where the first-of-its-kind prognostic blood test comes into play. The test’s ability to predict severe preeclampsia within 2 weeks can help save lives. The test can offer health care providers the ability to administer steroids for fetal lung maturity before delivery and be more prepared to care for what could be a very compromised newborn.
The blood test, which is recommended between 23-35 weeks gestation, involves analyzing a ratio between two proteins from the placenta, sFlt1 and PIGF. The higher the ratio, the higher the risk that severe preeclampsia will develop. Results can be available within 30 minutes, which is critical when contemplating treatment.
An example of the use of this ratio is illustrated with chronic hypertension in pregnancy, which is defined as elevated blood pressure before 20 weeks or even before conception. Since chronic hypertension can be a primary precursor to preeclampsia, patients with this condition are at higher risk. The FDA-approved blood test would be helpful in determining the plan of care; that is, delivery versus hospitalization versus monitor as an outpatient.
With a positive test result, a pregnant woman can be immediately hospitalized where she can get the care she and baby need as they await delivery. Since health care providers already know the high-risk groups, surveillance can begin early, utilizing this blood test to predict the progression to severe preeclampsia. Conversely, if the test is negative, a treatment plan can be made as an outpatient and the pregnancy continues.
Not all hospitals are equipped to care for premature babies. If delivery is not imminent, providers can use this blood test to identify those that should be transferred to a tertiary center for observation and monitoring. Mother and baby would then not be separated after birth.
We really don’t know who will develop severe preeclampsia and who won’t. This new blood test will be a critical tool as pregnant patients go through their second and third trimesters. It will be especially pivotal for these women, but important for all pregnant women in reducing maternal and fetal mortality and morbidity.
Ms. Barnett is a registered nurse in the department of obstetrics, Mills-Peninsula Medical Center, Burlingame, Calif. She has disclosed no relevant financial relationships.
There is amazing news for the world of obstetrics and for all pregnant women. Severe preeclampsia is a critical obstetrical condition that can have serious outcomes for a mother and baby. It can lead to eclampsia, an obstetrical emergency, which often results in death of the mother and/or baby.
Based on research published in the Journal of the American Heart Association, the incidence of new‐onset hypertensive disorders of pregnancy (gestational hypertension and preeclampsia/eclampsia) have nearly doubled in the United States from 2007 to 2019. And they continue to climb.
According to the Preeclampsia Foundation, 5%-8% of all pregnancies in the United States will result in preeclampsia. Black women are at a 60% higher risk than white women, and according to various sources, other risk groups include those who became pregnant via in vitro fertilization, mothers of multiples (twins and triplets), women with gestational diabetes, women over age 35, women with chronic hypertension, obesity, polycystic ovary syndrome, sickle cell disease, rheumatoid arthritis, lupus, migraines, antiphospholipid syndrome, previous pregnancy with preeclampsia, family history, and scleroderma.
Screening and treatment
Preeclampsia is a multiorgan disease of pregnancy, and can be mild, but may quickly progress to severe, which can be life-threatening for mother and baby. It was previously referred to as toxemia or the high blood pressure disease of pregnancy. It primarily involves the cardiovascular, neurologic and renal systems, and the liver. Patients typically present with elevated blood pressures, but other symptoms may include headache, swelling of hands and feet, blurry/double vision or seeing spots, nausea/vomiting, and epigastric pain. It is diagnosed with elevated blood pressures, blood work, and protein in the urine.
Early screening for preeclampsia is done in the first trimester. Presently, a combination of prenatal blood work, blood pressure monitoring, and recognition of high-risk groups is used to determine a treatment plan going forward. The American Congress of Obstetricians and Gynecologists recommends women that fall into this group for potentially developing preeclampsia take daily aspirin as a preventative measure.
In its milder form, a pregnant woman can be observed as an outpatient – monitored with antepartum testing, lab work, and patient education to report significant symptoms as listed above. Teaching patients about fetal kick counts to monitor their baby’s movements is equally important. Women with mild preeclampsia usually can safely deliver at term, being induced between 37-39 weeks’ gestation.
On the other hand, if mild preeclampsia progresses to severe preeclampsia, delivery may be preterm for the safety of mother and baby. Severe preeclampsia can lead to maternal organ damage, seizures, and even death of mother and/or baby.
About 20% of women with severe preeclampsia will develop HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelets) syndrome, a life-threatening disease that often warrants immediate delivery. According to the National Library of Medicine, the mortality rate of women with HELLP syndrome is up to 24% and the perinatal death rate is up as high as 37%. These serious conditions can cause ineffective maternal clotting, liver rupture, placental abruption, and postpartum hemorrhage. It is most prevalent in the third trimester but can occur within 48 hours of delivery.
The only cure for preeclampsia in any form is delivery.
Patients with severe preeclampsia are hospitalized until delivery – sometimes a few days to a couple of weeks. Mother and baby are closely watched for further progression, including signs of organ damage in the mother and changes to the well-being of the baby. If the mother’s health is severely compromised, then the baby will be compromised as well. A preterm delivery may be necessary.
Impact of the new test
The National Institute of Health states that preterm babies born from preeclamptic mothers can suffer many health problems including cerebral palsy, deafness, blindness, epilepsy, and a host of other respiratory, cardiovascular, and endocrine issues. But the biggest issue is preterm birth, defined as birth before 37 weeks gestation. Being born preterm can require a long stay in the intensive care nursery.
This is where the first-of-its-kind prognostic blood test comes into play. The test’s ability to predict severe preeclampsia within 2 weeks can help save lives. The test can offer health care providers the ability to administer steroids for fetal lung maturity before delivery and be more prepared to care for what could be a very compromised newborn.
The blood test, which is recommended between 23-35 weeks gestation, involves analyzing a ratio between two proteins from the placenta, sFlt1 and PIGF. The higher the ratio, the higher the risk that severe preeclampsia will develop. Results can be available within 30 minutes, which is critical when contemplating treatment.
An example of the use of this ratio is illustrated with chronic hypertension in pregnancy, which is defined as elevated blood pressure before 20 weeks or even before conception. Since chronic hypertension can be a primary precursor to preeclampsia, patients with this condition are at higher risk. The FDA-approved blood test would be helpful in determining the plan of care; that is, delivery versus hospitalization versus monitor as an outpatient.
With a positive test result, a pregnant woman can be immediately hospitalized where she can get the care she and baby need as they await delivery. Since health care providers already know the high-risk groups, surveillance can begin early, utilizing this blood test to predict the progression to severe preeclampsia. Conversely, if the test is negative, a treatment plan can be made as an outpatient and the pregnancy continues.
Not all hospitals are equipped to care for premature babies. If delivery is not imminent, providers can use this blood test to identify those that should be transferred to a tertiary center for observation and monitoring. Mother and baby would then not be separated after birth.
We really don’t know who will develop severe preeclampsia and who won’t. This new blood test will be a critical tool as pregnant patients go through their second and third trimesters. It will be especially pivotal for these women, but important for all pregnant women in reducing maternal and fetal mortality and morbidity.
Ms. Barnett is a registered nurse in the department of obstetrics, Mills-Peninsula Medical Center, Burlingame, Calif. She has disclosed no relevant financial relationships.
Prenatal sleep problems, depression linked to poorer outcomes
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Together, the two studies suggest that commonly overlooked experiences in the prenatal period can have negative effects down the line if clinicians aren’t asking patients about them and addressing the issue.
”I think the national conversation around mental health in general will hopefully carry us forward to better supporting the patients who are coming in with preexisting conditions,” lead author Minnie Jang, a 4th-year medical student at Johns Hopkins University, Baltimore, said in an interview.
Most of the attention on mood disorders of pregnancy focus on the postpartum period, but preexisting or new-onset depression during pregnancy deserves more attention, Ms. Jang told attendees. ACOG recommends that clinicians screen all patients at least once during the perinatal period, but that could be anywhere from early pregnancy to the postpartum period. Ms. Jang would like to see recommendations addressing both early pregnancy and the postpartum period.
“I think there’s this framing that postpartum depression is a distinct entity from other mental health conditions whereas it’s really part of a continuum,” Ms. Jang said in an interview.
She retrospectively analyzed the medical records of all pregnant women who completed the Edinburgh Postnatal Depression Scale (EPDS) during their first or second trimesters between 2002 and 2021 at Johns Hopkins Hospital. Among the 718 women who were screened in early pregnancy, 44.6% were Black or African American, 39.7% were white, and 15.7% were of a different race. Nearly all (94%) were not Hispanic/Latino.
Most (59%) were partnered, employed (68%), and had private insurance (58%). Only 7% used tobacco while 11% used alcohol and 6% used illicit drugs.
Twelve percent of the patients scored positive for depression, with a score of at least 10 or an affirmative answer to question 10 regarding self-harm. These women tended to be younger (P = .034), with an median age of 28 at their first visit versus 31 for those who screened negative, and were more likely to be publicly insured (P = .013) and without a partner (P = .005).
Patients who screened positive were more likely to have a history of substance use or history of a previous psychiatric diagnosis (P < .0001 for both). In addition, more patients who screened positive (49%) than those who screened negative (26%) had fetal complications (P < .001).
”There are some interesting subgroups of patients who are screening positive for depressive symptoms early on in pregnancy,” Ms. Jang said. Some come into pregnancy with preexisting mental health conditions while others have situational depressive symptoms, such as the subgroup referred to social work who had diagnosed fetal complications, she said. “Then there’s a whole other group of patients who are developing new symptoms during pregnancy.”
Patients who screened positive tended to start prenatal care later, at a median 12.3 weeks gestational age, than patients who screened negative, at a median 10.7 weeks gestational age (P = .002), the analysis found.
The number of routine prenatal care visits did not significantly differ between those who screened positive and those who screened negative, but patients with positive depression screens were almost half as likely to complete glucose tolerance testing (odds ratio, 0.6) or group B streptococcus testing (OR, 0.56) after adjusting for insurance status, gravidity, and gestational age at the patient’s first visit.
The researchers also identified a significant positive association between higher EPDS scores and the number of labor and delivery triage visits (P = .006). There were no significant differences in the rates of Tdap vaccination or screening for sexually transmitted infections between the two groups.
Poor sleep linked to later depression
The other study was prospective, using data from the PATCH Prenatal Care and Maternal and Child Health Outcomes study, which initially “compared health outcomes and satisfaction with prenatal care between patients receiving Centering Pregnancy group prenatal care and patients receiving traditional prenatal care,” the authors explained. This secondary analysis looked at sleep problems and postpartum depression.
“We don’t routinely ask patients about sleep or screen patients for sleeping issues,” lead author Carolyn Sinow, MD, a 4th-year resident at Kaiser Permanente Santa Clara (Calif.) Medical Center, said in an interview. “I think that we need to take sleep complaints more seriously overall, especially in early pregnancy.” While sleep problems in the third trimester often have more to do with discomforts from pregnancy itself, better sleep “in the first and second trimester is something we can really target with good sleep hygiene,” she added.
The 336 pregnant participants were recruited from Health Connect as long as they had a singleton pregnancy, were receiving prenatal care from Kaiser Permanente Northern California, and completed baseline questionnaires about their sleep and depression and anxiety symptoms during their first trimester between August 2020 and April 2021. Those with clinical depression or a high-risk pregnancy were excluded. The participants then completed the questionnaires again between 4 and 8 weeks post partum.
After adjusting for baseline depression and potential confounders, patients with poor sleep quality, indicated by a score greater than 5 on the Pittsburgh Sleep Quality Index (PSQI), were 12% more likely to develop postpartum depression, indicated by a score on the Patient Health Questionnaire depression scale (PHQ-8) of 10 or greater (relative risk, 1.12; 95% confidence interval, 1.01-1.25).
The two aspects of sleep that specifically correlated with postpartum depression were sleep quality and sleep latency, or taking a long time to fall asleep. Those reporting poor sleep quality were twice as likely to develop postpartum depression (relative risk, 2.18; 95% CI, 1.22-3.91), and those who took a while to fall asleep were 52% more likely to develop postpartum depression (RR, 1.52; 95% CI, 1.06-2.17).
Though the study also found prenatal sleep problems correlated with higher postpartum anxiety scores on the General Anxiety Disorder scale (GAD-7), the results were not statistically significant.
Kathleen Morrell, MD, MPH, an ob.gyn. in New York, was not involved in the study and said she was surprised it wasn’t something that had been studied much before because it makes sense.
“I always like it when studies confirm what we think should make sense, so it’s nice to see it,” Dr. Morrell said in an interview. “I think anytime you put something out, research it, and define it with numbers for doctors, that sometimes allows us to [realize], ‘Oh, that’s probably something we should be paying more attention to, especially if we have available treatments for it,’” she added.
“The clinical takeaway is that we really need to be screening for sleep pattern disruptions early in pregnancy, because even though it makes logical sense, it might not be something on our radar to think about,” Dr. Morrell said. “If people aren’t sleeping, well, their mental health is negatively affected.”
The most promising therapy for sleep issues currently is cognitive-behavioral therapy, which can accessed through various apps, Dr. Sinow said in an interview. “There are also safe interventions, such as melatonin and Unisom, that are totally safe in pregnancy that we can use to target sleep in early pregnancy.”
Dr. Morrell added that vitamin B6, often taken for nausea and vomiting during pregnancy, can also sometimes help people sleep and is safe during pregnancy.
“We know that postpartum depression does not necessarily only have a negative effect on the mother, but also has a negative effect on the infant and the family dynamic as well,” Dr. Morrell said. “So, we should be looking and screening for it so that we can offer people potential treatment because we know it can have long-term effects.”
Ms. Jang and Dr. Sinow did not have any disclosures. Dr. Morrell has done training for Nexplanon. Neither study noted external funding.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Together, the two studies suggest that commonly overlooked experiences in the prenatal period can have negative effects down the line if clinicians aren’t asking patients about them and addressing the issue.
”I think the national conversation around mental health in general will hopefully carry us forward to better supporting the patients who are coming in with preexisting conditions,” lead author Minnie Jang, a 4th-year medical student at Johns Hopkins University, Baltimore, said in an interview.
Most of the attention on mood disorders of pregnancy focus on the postpartum period, but preexisting or new-onset depression during pregnancy deserves more attention, Ms. Jang told attendees. ACOG recommends that clinicians screen all patients at least once during the perinatal period, but that could be anywhere from early pregnancy to the postpartum period. Ms. Jang would like to see recommendations addressing both early pregnancy and the postpartum period.
“I think there’s this framing that postpartum depression is a distinct entity from other mental health conditions whereas it’s really part of a continuum,” Ms. Jang said in an interview.
She retrospectively analyzed the medical records of all pregnant women who completed the Edinburgh Postnatal Depression Scale (EPDS) during their first or second trimesters between 2002 and 2021 at Johns Hopkins Hospital. Among the 718 women who were screened in early pregnancy, 44.6% were Black or African American, 39.7% were white, and 15.7% were of a different race. Nearly all (94%) were not Hispanic/Latino.
Most (59%) were partnered, employed (68%), and had private insurance (58%). Only 7% used tobacco while 11% used alcohol and 6% used illicit drugs.
Twelve percent of the patients scored positive for depression, with a score of at least 10 or an affirmative answer to question 10 regarding self-harm. These women tended to be younger (P = .034), with an median age of 28 at their first visit versus 31 for those who screened negative, and were more likely to be publicly insured (P = .013) and without a partner (P = .005).
Patients who screened positive were more likely to have a history of substance use or history of a previous psychiatric diagnosis (P < .0001 for both). In addition, more patients who screened positive (49%) than those who screened negative (26%) had fetal complications (P < .001).
”There are some interesting subgroups of patients who are screening positive for depressive symptoms early on in pregnancy,” Ms. Jang said. Some come into pregnancy with preexisting mental health conditions while others have situational depressive symptoms, such as the subgroup referred to social work who had diagnosed fetal complications, she said. “Then there’s a whole other group of patients who are developing new symptoms during pregnancy.”
Patients who screened positive tended to start prenatal care later, at a median 12.3 weeks gestational age, than patients who screened negative, at a median 10.7 weeks gestational age (P = .002), the analysis found.
The number of routine prenatal care visits did not significantly differ between those who screened positive and those who screened negative, but patients with positive depression screens were almost half as likely to complete glucose tolerance testing (odds ratio, 0.6) or group B streptococcus testing (OR, 0.56) after adjusting for insurance status, gravidity, and gestational age at the patient’s first visit.
The researchers also identified a significant positive association between higher EPDS scores and the number of labor and delivery triage visits (P = .006). There were no significant differences in the rates of Tdap vaccination or screening for sexually transmitted infections between the two groups.
Poor sleep linked to later depression
The other study was prospective, using data from the PATCH Prenatal Care and Maternal and Child Health Outcomes study, which initially “compared health outcomes and satisfaction with prenatal care between patients receiving Centering Pregnancy group prenatal care and patients receiving traditional prenatal care,” the authors explained. This secondary analysis looked at sleep problems and postpartum depression.
“We don’t routinely ask patients about sleep or screen patients for sleeping issues,” lead author Carolyn Sinow, MD, a 4th-year resident at Kaiser Permanente Santa Clara (Calif.) Medical Center, said in an interview. “I think that we need to take sleep complaints more seriously overall, especially in early pregnancy.” While sleep problems in the third trimester often have more to do with discomforts from pregnancy itself, better sleep “in the first and second trimester is something we can really target with good sleep hygiene,” she added.
The 336 pregnant participants were recruited from Health Connect as long as they had a singleton pregnancy, were receiving prenatal care from Kaiser Permanente Northern California, and completed baseline questionnaires about their sleep and depression and anxiety symptoms during their first trimester between August 2020 and April 2021. Those with clinical depression or a high-risk pregnancy were excluded. The participants then completed the questionnaires again between 4 and 8 weeks post partum.
After adjusting for baseline depression and potential confounders, patients with poor sleep quality, indicated by a score greater than 5 on the Pittsburgh Sleep Quality Index (PSQI), were 12% more likely to develop postpartum depression, indicated by a score on the Patient Health Questionnaire depression scale (PHQ-8) of 10 or greater (relative risk, 1.12; 95% confidence interval, 1.01-1.25).
The two aspects of sleep that specifically correlated with postpartum depression were sleep quality and sleep latency, or taking a long time to fall asleep. Those reporting poor sleep quality were twice as likely to develop postpartum depression (relative risk, 2.18; 95% CI, 1.22-3.91), and those who took a while to fall asleep were 52% more likely to develop postpartum depression (RR, 1.52; 95% CI, 1.06-2.17).
Though the study also found prenatal sleep problems correlated with higher postpartum anxiety scores on the General Anxiety Disorder scale (GAD-7), the results were not statistically significant.
Kathleen Morrell, MD, MPH, an ob.gyn. in New York, was not involved in the study and said she was surprised it wasn’t something that had been studied much before because it makes sense.
“I always like it when studies confirm what we think should make sense, so it’s nice to see it,” Dr. Morrell said in an interview. “I think anytime you put something out, research it, and define it with numbers for doctors, that sometimes allows us to [realize], ‘Oh, that’s probably something we should be paying more attention to, especially if we have available treatments for it,’” she added.
“The clinical takeaway is that we really need to be screening for sleep pattern disruptions early in pregnancy, because even though it makes logical sense, it might not be something on our radar to think about,” Dr. Morrell said. “If people aren’t sleeping, well, their mental health is negatively affected.”
The most promising therapy for sleep issues currently is cognitive-behavioral therapy, which can accessed through various apps, Dr. Sinow said in an interview. “There are also safe interventions, such as melatonin and Unisom, that are totally safe in pregnancy that we can use to target sleep in early pregnancy.”
Dr. Morrell added that vitamin B6, often taken for nausea and vomiting during pregnancy, can also sometimes help people sleep and is safe during pregnancy.
“We know that postpartum depression does not necessarily only have a negative effect on the mother, but also has a negative effect on the infant and the family dynamic as well,” Dr. Morrell said. “So, we should be looking and screening for it so that we can offer people potential treatment because we know it can have long-term effects.”
Ms. Jang and Dr. Sinow did not have any disclosures. Dr. Morrell has done training for Nexplanon. Neither study noted external funding.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Together, the two studies suggest that commonly overlooked experiences in the prenatal period can have negative effects down the line if clinicians aren’t asking patients about them and addressing the issue.
”I think the national conversation around mental health in general will hopefully carry us forward to better supporting the patients who are coming in with preexisting conditions,” lead author Minnie Jang, a 4th-year medical student at Johns Hopkins University, Baltimore, said in an interview.
Most of the attention on mood disorders of pregnancy focus on the postpartum period, but preexisting or new-onset depression during pregnancy deserves more attention, Ms. Jang told attendees. ACOG recommends that clinicians screen all patients at least once during the perinatal period, but that could be anywhere from early pregnancy to the postpartum period. Ms. Jang would like to see recommendations addressing both early pregnancy and the postpartum period.
“I think there’s this framing that postpartum depression is a distinct entity from other mental health conditions whereas it’s really part of a continuum,” Ms. Jang said in an interview.
She retrospectively analyzed the medical records of all pregnant women who completed the Edinburgh Postnatal Depression Scale (EPDS) during their first or second trimesters between 2002 and 2021 at Johns Hopkins Hospital. Among the 718 women who were screened in early pregnancy, 44.6% were Black or African American, 39.7% were white, and 15.7% were of a different race. Nearly all (94%) were not Hispanic/Latino.
Most (59%) were partnered, employed (68%), and had private insurance (58%). Only 7% used tobacco while 11% used alcohol and 6% used illicit drugs.
Twelve percent of the patients scored positive for depression, with a score of at least 10 or an affirmative answer to question 10 regarding self-harm. These women tended to be younger (P = .034), with an median age of 28 at their first visit versus 31 for those who screened negative, and were more likely to be publicly insured (P = .013) and without a partner (P = .005).
Patients who screened positive were more likely to have a history of substance use or history of a previous psychiatric diagnosis (P < .0001 for both). In addition, more patients who screened positive (49%) than those who screened negative (26%) had fetal complications (P < .001).
”There are some interesting subgroups of patients who are screening positive for depressive symptoms early on in pregnancy,” Ms. Jang said. Some come into pregnancy with preexisting mental health conditions while others have situational depressive symptoms, such as the subgroup referred to social work who had diagnosed fetal complications, she said. “Then there’s a whole other group of patients who are developing new symptoms during pregnancy.”
Patients who screened positive tended to start prenatal care later, at a median 12.3 weeks gestational age, than patients who screened negative, at a median 10.7 weeks gestational age (P = .002), the analysis found.
The number of routine prenatal care visits did not significantly differ between those who screened positive and those who screened negative, but patients with positive depression screens were almost half as likely to complete glucose tolerance testing (odds ratio, 0.6) or group B streptococcus testing (OR, 0.56) after adjusting for insurance status, gravidity, and gestational age at the patient’s first visit.
The researchers also identified a significant positive association between higher EPDS scores and the number of labor and delivery triage visits (P = .006). There were no significant differences in the rates of Tdap vaccination or screening for sexually transmitted infections between the two groups.
Poor sleep linked to later depression
The other study was prospective, using data from the PATCH Prenatal Care and Maternal and Child Health Outcomes study, which initially “compared health outcomes and satisfaction with prenatal care between patients receiving Centering Pregnancy group prenatal care and patients receiving traditional prenatal care,” the authors explained. This secondary analysis looked at sleep problems and postpartum depression.
“We don’t routinely ask patients about sleep or screen patients for sleeping issues,” lead author Carolyn Sinow, MD, a 4th-year resident at Kaiser Permanente Santa Clara (Calif.) Medical Center, said in an interview. “I think that we need to take sleep complaints more seriously overall, especially in early pregnancy.” While sleep problems in the third trimester often have more to do with discomforts from pregnancy itself, better sleep “in the first and second trimester is something we can really target with good sleep hygiene,” she added.
The 336 pregnant participants were recruited from Health Connect as long as they had a singleton pregnancy, were receiving prenatal care from Kaiser Permanente Northern California, and completed baseline questionnaires about their sleep and depression and anxiety symptoms during their first trimester between August 2020 and April 2021. Those with clinical depression or a high-risk pregnancy were excluded. The participants then completed the questionnaires again between 4 and 8 weeks post partum.
After adjusting for baseline depression and potential confounders, patients with poor sleep quality, indicated by a score greater than 5 on the Pittsburgh Sleep Quality Index (PSQI), were 12% more likely to develop postpartum depression, indicated by a score on the Patient Health Questionnaire depression scale (PHQ-8) of 10 or greater (relative risk, 1.12; 95% confidence interval, 1.01-1.25).
The two aspects of sleep that specifically correlated with postpartum depression were sleep quality and sleep latency, or taking a long time to fall asleep. Those reporting poor sleep quality were twice as likely to develop postpartum depression (relative risk, 2.18; 95% CI, 1.22-3.91), and those who took a while to fall asleep were 52% more likely to develop postpartum depression (RR, 1.52; 95% CI, 1.06-2.17).
Though the study also found prenatal sleep problems correlated with higher postpartum anxiety scores on the General Anxiety Disorder scale (GAD-7), the results were not statistically significant.
Kathleen Morrell, MD, MPH, an ob.gyn. in New York, was not involved in the study and said she was surprised it wasn’t something that had been studied much before because it makes sense.
“I always like it when studies confirm what we think should make sense, so it’s nice to see it,” Dr. Morrell said in an interview. “I think anytime you put something out, research it, and define it with numbers for doctors, that sometimes allows us to [realize], ‘Oh, that’s probably something we should be paying more attention to, especially if we have available treatments for it,’” she added.
“The clinical takeaway is that we really need to be screening for sleep pattern disruptions early in pregnancy, because even though it makes logical sense, it might not be something on our radar to think about,” Dr. Morrell said. “If people aren’t sleeping, well, their mental health is negatively affected.”
The most promising therapy for sleep issues currently is cognitive-behavioral therapy, which can accessed through various apps, Dr. Sinow said in an interview. “There are also safe interventions, such as melatonin and Unisom, that are totally safe in pregnancy that we can use to target sleep in early pregnancy.”
Dr. Morrell added that vitamin B6, often taken for nausea and vomiting during pregnancy, can also sometimes help people sleep and is safe during pregnancy.
“We know that postpartum depression does not necessarily only have a negative effect on the mother, but also has a negative effect on the infant and the family dynamic as well,” Dr. Morrell said. “So, we should be looking and screening for it so that we can offer people potential treatment because we know it can have long-term effects.”
Ms. Jang and Dr. Sinow did not have any disclosures. Dr. Morrell has done training for Nexplanon. Neither study noted external funding.
AT ACOG 2023
Investigating the etiology of recurrent pregnancy loss
With attention to the timing of loss
Introduction: Reassurance through pregnancy loss and workups
Pregnancy loss is not an uncommon complication but it can be associated with significant stress among parents and loved ones when it occurs. Especially when recurrent, it also becomes a medical dilemma for physicians and nurses because the cause is not always obvious immediately, and even with exploration, the cause may not always be found.
First and foremost, it is important that physicians provide counseling and reassurance to families experiencing loss, and that they encourage a level of patience while the investigation for loss is done. Investigations tend not to be linear. One must look at a number of diagnostic areas including genetics, anatomy, immunology, and infections.
Even with an extensive workup, what often is found are potential associations rather than precise causes. For instance, one may find that certain antibodies or certain conditions are present, or that certain anatomic structures are abnormal. While such findings are not necessarily causative, there are therapeutic interventions that we can offer to address many of the conditions (e.g., surgical correction of the septate uterus, and low-dose aspirin and heparin for antiphospholipid syndrome).
Less than 1% of couples experience recurrent pregnancy loss (traditionally defined as three or more losses), so parents who experience one loss should be given reassurance that their loss was likely a sporadic miscarriage and that chances of recurrence will be low. Even as workups proceed, reassurance is important.
For this month’s Master Class in Obstetrics we’ve invited Wendy L. Kinzler, MD, and Anthony Vintzileos, MD, both of whom have expertise in the area of recurrent pregnancy loss, to review the potential causes and the management approach. They focus on the first trimester, when genetic causes predominate, and the early second trimester, when undetected uterine factors can be at play. They explain that the gestational age at which recurrent losses occur is an important factor in decoding etiology and management.
Dr. Kinzler is associate dean, graduate medical education, and professor of obstetrics and gynecology at NYU Long Island School of Medicine, Mineola, N.Y., and Dr. Vintzileos is chief patient safety officer for obstetrics, Northwell Health–Western Region, and professor in the department of obstetrics and gynecology in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, N.Y. Dr. Kinzler and Dr. Vintzileos reported no relevant disclosures.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at [email protected].
Investigating the etiology of recurrent pregnancy loss
Pregnancy loss is defined as a loss occurring at < 20 weeks’ gestation.
Consideration of the timing of the pregnancy loss can provide a useful guide to this evaluation, as etiologies vary depending on when in gestation losses occur. In this Master Class, we will address the evaluation of pregnancy loss at < 20 weeks’ gestation, with particular attention to first trimester and early second trimester causes. Literature on the role of the cervix and intra-amniotic infection in midtrimester loss is extensive and will not be covered here.
Although early first trimester miscarriage is common, occurring in approximately 15% of clinically recognized pregnancies, only 2%-3% of couples experience two or more miscarriages and 0.5%-1% experience three or more.
When to begin a diagnostic workup should be part of a shared decision-making process, taking into consideration future family planning, parity, number of previous losses, and notably, the gestational age at which loss(es) occurred. Recurrence rates for first trimester miscarriage are similar after two versus three consecutive losses and either situation usually prompts an evaluation, whereas any second-trimester loss should be evaluated.
Increasingly, we are appreciating the value of a more targeted, gestational age–driven approach to the evaluation of pregnancy loss in an attempt to provide grieving parents with useful information without subjecting them to a wide array of expensive and unnecessary tests.
Genetic causes
The earlier the pregnancy loss, the more likely it is the result of abnormal fetal genetics. Genetic factors should be considered as the most likely cause for first trimester pregnancy losses (especially those occurring at < 10 weeks’ gestation), the most frequent being autosomal trisomies or monosomy X. The vast majority of trisomy conceptuses are sporadic in nature and are related to the natural aging process of the ovary (increasing the rate of meiotic nondisjunction).
If fetal aneuploidy is identified in a pregnancy loss, couples can be counseled about the definitive cause of the loss and can be counseled about recurrence based on age-related risks and/or tests of ovarian reserve. Recurrent pregnancy loss (RPL) is only rarely associated with a parental translocation (< 5%). Testing parental karyotypes should be reserved for cases in which the fetal karyotypes are unknown or in which an unbalanced translocation was identified in the fetus.
When a first trimester pregnancy loss is diagnosed, chorionic villus sampling (CVS) with microarray testing is the most reliable and comprehensive method for evaluating potential genetic causes. It provides valuable information even when cells are not viable and reduces the risk of maternal cell contamination – two significant limitations to standard karyotype analysis performed on tissue passed spontaneously or at the time of D&C. Studies of products of conception (POC) testing with microarray have documented the detection of abnormalities in an additional 10%-15% of cases compared with traditional karyotype analysis.
When CVS is not feasible, testing maternal serum for cell-free DNA is a reasonable alternative. In a prospective cohort study of 50 maternal blood samples taken after fetal demise, 76% of samples yielded cell-free DNA results, meaning fetal fractions were within the detectable range. The higher the gestational age at the time of loss, the higher the chance of obtaining a result: Findings in the study were possible in 88% of samples when the gestational age was 8 weeks or greater, and in 53% of cases involving a lower gestational age. The time from demise to blood draw did not affect the likelihood of obtaining a result (Obstet Gynecol. 2015 Jun;125[6]:1321-29).
When neither CVS nor cell-free DNA analysis is feasible, analysis of either spontaneously passed tissue or tissue obtained at the time of a D&C may still be worthwhile. Maternal cell contamination, of course, is the main downside.
A paper published in 2020 documented the value of refocusing the initial workup. Researchers reported that 57% of 1,400 cases of recurrent pregnancy loss went unexplained using the 2012 ASRM guidelines, which included parental karyotyping but not POC cytogenetic analysis. When parental karyotypes were omitted from the initial workup and POC analysis with 24-chromosome microarray was added, at least one potential explanation for loss could be identified in 92% of cases. Only 8% were left “unexplained” (Curr Opin Obstet Gynecol. 2020 Oct;32[5]:371-9).
When genetics are ruled out
Issues that are top of mind when we lack genetic information or when genetic causes are ruled out include maternal metabolic disorders (uncontrolled diabetes, obesity, uncontrolled thyroid disease), environmental exposures (smoking), uterine abnormalities, and antiphospholipid syndrome.
Thorough evaluation of the uterine cavity after recurrent first trimester miscarriage – or after any second trimester loss – is too often a missing element of investigation. It is a vital component of the evaluation, and information about uterine structure is easily obtained.
A saline infusion sonogram (SIS) allows us to look at the external contour of the uterus, assess the myometrium for muscular abnormalities, visualize the uterine lining, and assess uterine orientation. Performed in the nonpregnant state, and ideally coupled with 3D technology, this relatively simple test can identify congenital uterine anomalies, intracavitary abnormalities (such as fibroids, polyps, or synechiae) which can surgically be removed prior to another pregnancy, a retroverted uterus that may be predisposed to incarceration during pregnancy, and other potentially impactful conditions, such as adenomyosis.
Structural anomalies
Congenital uterine anomalies are associated with first trimester miscarriage, second trimester pregnancy loss, and preterm birth. A uterine septum is of particular concern for early miscarriage, as the early embryo can implant on the relatively avascular septum.
Other congenital uterine anomalies (bicornuate, didelphys, unicornuate) can be associated with concomitant cervical structural abnormalities leading to cervical insufficiency and/or result in pathologic uterine stretch of a space-limited cavity, leading to midtrimester loss or preterm birth. The diagnosis of these anomalies is an important part of the evaluation of pregnancy loss, as it can guide monitoring in future pregnancies, or can be surgically corrected, as in the case of a uterine septum, significantly improving pregnancy outcomes.
A short cervix can result either congenitally or from injury or trauma and may also be associated with cervical insufficiency and miscarriage. It can be evaluated and monitored by ultrasound and, in some cases, treated by surgical cerclage. Pregnancy losses due to cervical insufficiency usually occur after 16 weeks of gestation and frequently are associated with intra-amniotic infections.
Incarcerated uterus and adenomyosis
Other uterine factors that can contribute to pregnancy loss and that are largely underdiagnosed or undiagnosed are an incarcerated retroverted uterus and adenomyosis.
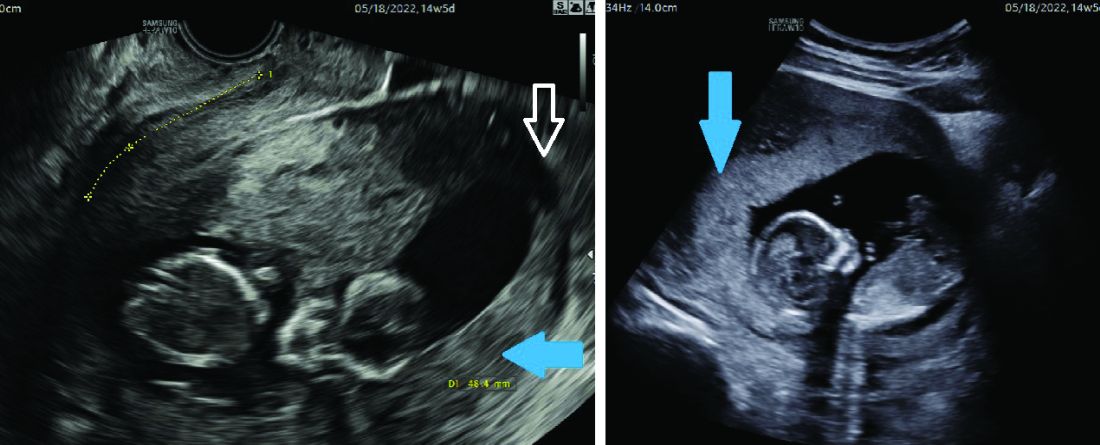
Most of the time, a retroverted uterus naturally assumes an anteverted position by the late first trimester or early second trimester, allowing for continued growth of the uterus and developing fetus. In approximately 10% of cases, however, the retroverted uterus becomes “stuck” or incarcerated in the posterior pelvis. This is more likely if there are large uterine fibroids or in the presence of pelvic adhesions due to endometriosis or previous pelvic surgery.
When this occurs, the fundus is wedged on the sacral promontory (may cause pelvic discomfort and constipation) and the cervix is markedly displaced anteriorly under the pubic symphysis (causing bladder outlet obstruction and urinary retention).
It is critical that ob.gyns. and emergency medicine providers are aware of this condition, which typically presents between 12 and 16 weeks’ gestation. The most frequent complaint is lower abdominal discomfort due to distended bladder and inability to void, which usually leads to bladder catheterization with drainage of large amounts of urine. An incarcerated uterus can predispose to pregnancy loss during this time (few other conditions cause loss during this time window), presumably due to impaired uterine artery blood flow.
Once the diagnosis is made, uterine incarceration may be corrected by elevating the gravid uterus out of the pelvis either manually, or by using a transvaginal ultrasound probe. (The latter minimally invasive approach was described in March at the American Institute of Ultrasound in Medicine’s annual conference by Martin Chavez, MD, and coinvestigators. More invasive approaches are rarely required but include CO2 intraperitoneal insufflation, as used prior to laparoscopy, or laparotomy.
The later in gestation the condition is allowed to persist, the less likely correction will be possible due to the enlarging fundus. Correction between 14 and 16 weeks, or earlier if symptoms develop, is recommended.
Adenomyosis, another poorly understood condition impacting pregnancy outcomes, has been associated with increased rates of miscarriage after in vitro fertilization (in addition to lower implantation rates); a meta-analysis published almost a decade ago found a risk ratio of miscarriage of 2.12 (95% confidence interval, 1.2-3.75) in women with adenomyosis versus those without (Hum Reprod. 2014 May;29[5]:964-77). However, outside of reproductive endocrinology, its impact on pregnancy outcomes in the obstetrical literature is not well recognized.
Although more research is necessary, we believe that adenomyosis should be considered a risk factor for pregnancy loss in the second trimester. The presence of endometrial glands within the myometrium, predisposing for an inflammatory environment, can lead to abnormal implantation, poor uterine distensibility, sterile inflammation, and early cervical insufficiency. As the prevalence of adenomyosis increases with age and maternal ages are increasing, this is an important condition to consider.
Diagnosis is typically made with MRI (although pathology of a hysterectomy specimen is the gold standard). Ultrasound findings consistent with adenomyosis are not routinely assessed and have not been studied in a gravid uterus. Nonetheless, a heightened sense of awareness about this possible contributor to pregnancy loss is very important.
A word about antiphospholipid syndrome
Antiphospholipid syndrome can cause a variety of adverse pregnancy outcomes, including first and second trimester pregnancy loss, fetal demise, fetal growth restriction, preeclampsia, preterm birth, and maternal thromboembolism. The classical presentation of miscarriage due to untreated antiphospholipid antibody syndrome is early severe fetal growth restriction, oligohydramnios, and IUFD in the second trimester.
The diagnosis requires at least one clinical criterion and one laboratory criterion. The mere presence of low level antibodies does not make the diagnosis of antiphospholipid antibody syndrome, and care should be taken to consider both the clinical and laboratory diagnostic criteria to make an accurate diagnosis.
When present, close maternal and fetal surveillance and a combination of low-dose aspirin and heparin are mainstays of treatment. The majority of studies suggest that low-molecular weight heparin (LMWH) and unfractionated heparin have comparable clinical efficacy. However, if a recurrent loss is experienced despite treatment with LMWH, the use of unfractionated heparin in a subsequent pregnancy should be considered.
With attention to the timing of loss
With attention to the timing of loss
Introduction: Reassurance through pregnancy loss and workups
Pregnancy loss is not an uncommon complication but it can be associated with significant stress among parents and loved ones when it occurs. Especially when recurrent, it also becomes a medical dilemma for physicians and nurses because the cause is not always obvious immediately, and even with exploration, the cause may not always be found.
First and foremost, it is important that physicians provide counseling and reassurance to families experiencing loss, and that they encourage a level of patience while the investigation for loss is done. Investigations tend not to be linear. One must look at a number of diagnostic areas including genetics, anatomy, immunology, and infections.
Even with an extensive workup, what often is found are potential associations rather than precise causes. For instance, one may find that certain antibodies or certain conditions are present, or that certain anatomic structures are abnormal. While such findings are not necessarily causative, there are therapeutic interventions that we can offer to address many of the conditions (e.g., surgical correction of the septate uterus, and low-dose aspirin and heparin for antiphospholipid syndrome).
Less than 1% of couples experience recurrent pregnancy loss (traditionally defined as three or more losses), so parents who experience one loss should be given reassurance that their loss was likely a sporadic miscarriage and that chances of recurrence will be low. Even as workups proceed, reassurance is important.
For this month’s Master Class in Obstetrics we’ve invited Wendy L. Kinzler, MD, and Anthony Vintzileos, MD, both of whom have expertise in the area of recurrent pregnancy loss, to review the potential causes and the management approach. They focus on the first trimester, when genetic causes predominate, and the early second trimester, when undetected uterine factors can be at play. They explain that the gestational age at which recurrent losses occur is an important factor in decoding etiology and management.
Dr. Kinzler is associate dean, graduate medical education, and professor of obstetrics and gynecology at NYU Long Island School of Medicine, Mineola, N.Y., and Dr. Vintzileos is chief patient safety officer for obstetrics, Northwell Health–Western Region, and professor in the department of obstetrics and gynecology in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, N.Y. Dr. Kinzler and Dr. Vintzileos reported no relevant disclosures.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at [email protected].
Investigating the etiology of recurrent pregnancy loss
Pregnancy loss is defined as a loss occurring at < 20 weeks’ gestation.
Consideration of the timing of the pregnancy loss can provide a useful guide to this evaluation, as etiologies vary depending on when in gestation losses occur. In this Master Class, we will address the evaluation of pregnancy loss at < 20 weeks’ gestation, with particular attention to first trimester and early second trimester causes. Literature on the role of the cervix and intra-amniotic infection in midtrimester loss is extensive and will not be covered here.
Although early first trimester miscarriage is common, occurring in approximately 15% of clinically recognized pregnancies, only 2%-3% of couples experience two or more miscarriages and 0.5%-1% experience three or more.
When to begin a diagnostic workup should be part of a shared decision-making process, taking into consideration future family planning, parity, number of previous losses, and notably, the gestational age at which loss(es) occurred. Recurrence rates for first trimester miscarriage are similar after two versus three consecutive losses and either situation usually prompts an evaluation, whereas any second-trimester loss should be evaluated.
Increasingly, we are appreciating the value of a more targeted, gestational age–driven approach to the evaluation of pregnancy loss in an attempt to provide grieving parents with useful information without subjecting them to a wide array of expensive and unnecessary tests.
Genetic causes
The earlier the pregnancy loss, the more likely it is the result of abnormal fetal genetics. Genetic factors should be considered as the most likely cause for first trimester pregnancy losses (especially those occurring at < 10 weeks’ gestation), the most frequent being autosomal trisomies or monosomy X. The vast majority of trisomy conceptuses are sporadic in nature and are related to the natural aging process of the ovary (increasing the rate of meiotic nondisjunction).
If fetal aneuploidy is identified in a pregnancy loss, couples can be counseled about the definitive cause of the loss and can be counseled about recurrence based on age-related risks and/or tests of ovarian reserve. Recurrent pregnancy loss (RPL) is only rarely associated with a parental translocation (< 5%). Testing parental karyotypes should be reserved for cases in which the fetal karyotypes are unknown or in which an unbalanced translocation was identified in the fetus.
When a first trimester pregnancy loss is diagnosed, chorionic villus sampling (CVS) with microarray testing is the most reliable and comprehensive method for evaluating potential genetic causes. It provides valuable information even when cells are not viable and reduces the risk of maternal cell contamination – two significant limitations to standard karyotype analysis performed on tissue passed spontaneously or at the time of D&C. Studies of products of conception (POC) testing with microarray have documented the detection of abnormalities in an additional 10%-15% of cases compared with traditional karyotype analysis.
When CVS is not feasible, testing maternal serum for cell-free DNA is a reasonable alternative. In a prospective cohort study of 50 maternal blood samples taken after fetal demise, 76% of samples yielded cell-free DNA results, meaning fetal fractions were within the detectable range. The higher the gestational age at the time of loss, the higher the chance of obtaining a result: Findings in the study were possible in 88% of samples when the gestational age was 8 weeks or greater, and in 53% of cases involving a lower gestational age. The time from demise to blood draw did not affect the likelihood of obtaining a result (Obstet Gynecol. 2015 Jun;125[6]:1321-29).
When neither CVS nor cell-free DNA analysis is feasible, analysis of either spontaneously passed tissue or tissue obtained at the time of a D&C may still be worthwhile. Maternal cell contamination, of course, is the main downside.
A paper published in 2020 documented the value of refocusing the initial workup. Researchers reported that 57% of 1,400 cases of recurrent pregnancy loss went unexplained using the 2012 ASRM guidelines, which included parental karyotyping but not POC cytogenetic analysis. When parental karyotypes were omitted from the initial workup and POC analysis with 24-chromosome microarray was added, at least one potential explanation for loss could be identified in 92% of cases. Only 8% were left “unexplained” (Curr Opin Obstet Gynecol. 2020 Oct;32[5]:371-9).
When genetics are ruled out
Issues that are top of mind when we lack genetic information or when genetic causes are ruled out include maternal metabolic disorders (uncontrolled diabetes, obesity, uncontrolled thyroid disease), environmental exposures (smoking), uterine abnormalities, and antiphospholipid syndrome.
Thorough evaluation of the uterine cavity after recurrent first trimester miscarriage – or after any second trimester loss – is too often a missing element of investigation. It is a vital component of the evaluation, and information about uterine structure is easily obtained.
A saline infusion sonogram (SIS) allows us to look at the external contour of the uterus, assess the myometrium for muscular abnormalities, visualize the uterine lining, and assess uterine orientation. Performed in the nonpregnant state, and ideally coupled with 3D technology, this relatively simple test can identify congenital uterine anomalies, intracavitary abnormalities (such as fibroids, polyps, or synechiae) which can surgically be removed prior to another pregnancy, a retroverted uterus that may be predisposed to incarceration during pregnancy, and other potentially impactful conditions, such as adenomyosis.
Structural anomalies
Congenital uterine anomalies are associated with first trimester miscarriage, second trimester pregnancy loss, and preterm birth. A uterine septum is of particular concern for early miscarriage, as the early embryo can implant on the relatively avascular septum.
Other congenital uterine anomalies (bicornuate, didelphys, unicornuate) can be associated with concomitant cervical structural abnormalities leading to cervical insufficiency and/or result in pathologic uterine stretch of a space-limited cavity, leading to midtrimester loss or preterm birth. The diagnosis of these anomalies is an important part of the evaluation of pregnancy loss, as it can guide monitoring in future pregnancies, or can be surgically corrected, as in the case of a uterine septum, significantly improving pregnancy outcomes.
A short cervix can result either congenitally or from injury or trauma and may also be associated with cervical insufficiency and miscarriage. It can be evaluated and monitored by ultrasound and, in some cases, treated by surgical cerclage. Pregnancy losses due to cervical insufficiency usually occur after 16 weeks of gestation and frequently are associated with intra-amniotic infections.
Incarcerated uterus and adenomyosis
Other uterine factors that can contribute to pregnancy loss and that are largely underdiagnosed or undiagnosed are an incarcerated retroverted uterus and adenomyosis.
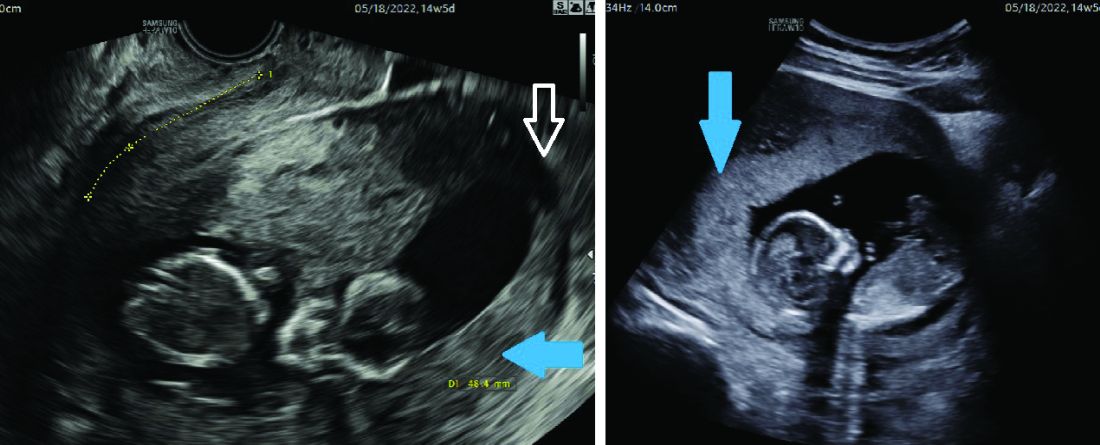
Most of the time, a retroverted uterus naturally assumes an anteverted position by the late first trimester or early second trimester, allowing for continued growth of the uterus and developing fetus. In approximately 10% of cases, however, the retroverted uterus becomes “stuck” or incarcerated in the posterior pelvis. This is more likely if there are large uterine fibroids or in the presence of pelvic adhesions due to endometriosis or previous pelvic surgery.
When this occurs, the fundus is wedged on the sacral promontory (may cause pelvic discomfort and constipation) and the cervix is markedly displaced anteriorly under the pubic symphysis (causing bladder outlet obstruction and urinary retention).
It is critical that ob.gyns. and emergency medicine providers are aware of this condition, which typically presents between 12 and 16 weeks’ gestation. The most frequent complaint is lower abdominal discomfort due to distended bladder and inability to void, which usually leads to bladder catheterization with drainage of large amounts of urine. An incarcerated uterus can predispose to pregnancy loss during this time (few other conditions cause loss during this time window), presumably due to impaired uterine artery blood flow.
Once the diagnosis is made, uterine incarceration may be corrected by elevating the gravid uterus out of the pelvis either manually, or by using a transvaginal ultrasound probe. (The latter minimally invasive approach was described in March at the American Institute of Ultrasound in Medicine’s annual conference by Martin Chavez, MD, and coinvestigators. More invasive approaches are rarely required but include CO2 intraperitoneal insufflation, as used prior to laparoscopy, or laparotomy.
The later in gestation the condition is allowed to persist, the less likely correction will be possible due to the enlarging fundus. Correction between 14 and 16 weeks, or earlier if symptoms develop, is recommended.
Adenomyosis, another poorly understood condition impacting pregnancy outcomes, has been associated with increased rates of miscarriage after in vitro fertilization (in addition to lower implantation rates); a meta-analysis published almost a decade ago found a risk ratio of miscarriage of 2.12 (95% confidence interval, 1.2-3.75) in women with adenomyosis versus those without (Hum Reprod. 2014 May;29[5]:964-77). However, outside of reproductive endocrinology, its impact on pregnancy outcomes in the obstetrical literature is not well recognized.
Although more research is necessary, we believe that adenomyosis should be considered a risk factor for pregnancy loss in the second trimester. The presence of endometrial glands within the myometrium, predisposing for an inflammatory environment, can lead to abnormal implantation, poor uterine distensibility, sterile inflammation, and early cervical insufficiency. As the prevalence of adenomyosis increases with age and maternal ages are increasing, this is an important condition to consider.
Diagnosis is typically made with MRI (although pathology of a hysterectomy specimen is the gold standard). Ultrasound findings consistent with adenomyosis are not routinely assessed and have not been studied in a gravid uterus. Nonetheless, a heightened sense of awareness about this possible contributor to pregnancy loss is very important.
A word about antiphospholipid syndrome
Antiphospholipid syndrome can cause a variety of adverse pregnancy outcomes, including first and second trimester pregnancy loss, fetal demise, fetal growth restriction, preeclampsia, preterm birth, and maternal thromboembolism. The classical presentation of miscarriage due to untreated antiphospholipid antibody syndrome is early severe fetal growth restriction, oligohydramnios, and IUFD in the second trimester.
The diagnosis requires at least one clinical criterion and one laboratory criterion. The mere presence of low level antibodies does not make the diagnosis of antiphospholipid antibody syndrome, and care should be taken to consider both the clinical and laboratory diagnostic criteria to make an accurate diagnosis.
When present, close maternal and fetal surveillance and a combination of low-dose aspirin and heparin are mainstays of treatment. The majority of studies suggest that low-molecular weight heparin (LMWH) and unfractionated heparin have comparable clinical efficacy. However, if a recurrent loss is experienced despite treatment with LMWH, the use of unfractionated heparin in a subsequent pregnancy should be considered.
Introduction: Reassurance through pregnancy loss and workups
Pregnancy loss is not an uncommon complication but it can be associated with significant stress among parents and loved ones when it occurs. Especially when recurrent, it also becomes a medical dilemma for physicians and nurses because the cause is not always obvious immediately, and even with exploration, the cause may not always be found.
First and foremost, it is important that physicians provide counseling and reassurance to families experiencing loss, and that they encourage a level of patience while the investigation for loss is done. Investigations tend not to be linear. One must look at a number of diagnostic areas including genetics, anatomy, immunology, and infections.
Even with an extensive workup, what often is found are potential associations rather than precise causes. For instance, one may find that certain antibodies or certain conditions are present, or that certain anatomic structures are abnormal. While such findings are not necessarily causative, there are therapeutic interventions that we can offer to address many of the conditions (e.g., surgical correction of the septate uterus, and low-dose aspirin and heparin for antiphospholipid syndrome).
Less than 1% of couples experience recurrent pregnancy loss (traditionally defined as three or more losses), so parents who experience one loss should be given reassurance that their loss was likely a sporadic miscarriage and that chances of recurrence will be low. Even as workups proceed, reassurance is important.
For this month’s Master Class in Obstetrics we’ve invited Wendy L. Kinzler, MD, and Anthony Vintzileos, MD, both of whom have expertise in the area of recurrent pregnancy loss, to review the potential causes and the management approach. They focus on the first trimester, when genetic causes predominate, and the early second trimester, when undetected uterine factors can be at play. They explain that the gestational age at which recurrent losses occur is an important factor in decoding etiology and management.
Dr. Kinzler is associate dean, graduate medical education, and professor of obstetrics and gynecology at NYU Long Island School of Medicine, Mineola, N.Y., and Dr. Vintzileos is chief patient safety officer for obstetrics, Northwell Health–Western Region, and professor in the department of obstetrics and gynecology in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, N.Y. Dr. Kinzler and Dr. Vintzileos reported no relevant disclosures.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at [email protected].
Investigating the etiology of recurrent pregnancy loss
Pregnancy loss is defined as a loss occurring at < 20 weeks’ gestation.
Consideration of the timing of the pregnancy loss can provide a useful guide to this evaluation, as etiologies vary depending on when in gestation losses occur. In this Master Class, we will address the evaluation of pregnancy loss at < 20 weeks’ gestation, with particular attention to first trimester and early second trimester causes. Literature on the role of the cervix and intra-amniotic infection in midtrimester loss is extensive and will not be covered here.
Although early first trimester miscarriage is common, occurring in approximately 15% of clinically recognized pregnancies, only 2%-3% of couples experience two or more miscarriages and 0.5%-1% experience three or more.
When to begin a diagnostic workup should be part of a shared decision-making process, taking into consideration future family planning, parity, number of previous losses, and notably, the gestational age at which loss(es) occurred. Recurrence rates for first trimester miscarriage are similar after two versus three consecutive losses and either situation usually prompts an evaluation, whereas any second-trimester loss should be evaluated.
Increasingly, we are appreciating the value of a more targeted, gestational age–driven approach to the evaluation of pregnancy loss in an attempt to provide grieving parents with useful information without subjecting them to a wide array of expensive and unnecessary tests.
Genetic causes
The earlier the pregnancy loss, the more likely it is the result of abnormal fetal genetics. Genetic factors should be considered as the most likely cause for first trimester pregnancy losses (especially those occurring at < 10 weeks’ gestation), the most frequent being autosomal trisomies or monosomy X. The vast majority of trisomy conceptuses are sporadic in nature and are related to the natural aging process of the ovary (increasing the rate of meiotic nondisjunction).
If fetal aneuploidy is identified in a pregnancy loss, couples can be counseled about the definitive cause of the loss and can be counseled about recurrence based on age-related risks and/or tests of ovarian reserve. Recurrent pregnancy loss (RPL) is only rarely associated with a parental translocation (< 5%). Testing parental karyotypes should be reserved for cases in which the fetal karyotypes are unknown or in which an unbalanced translocation was identified in the fetus.
When a first trimester pregnancy loss is diagnosed, chorionic villus sampling (CVS) with microarray testing is the most reliable and comprehensive method for evaluating potential genetic causes. It provides valuable information even when cells are not viable and reduces the risk of maternal cell contamination – two significant limitations to standard karyotype analysis performed on tissue passed spontaneously or at the time of D&C. Studies of products of conception (POC) testing with microarray have documented the detection of abnormalities in an additional 10%-15% of cases compared with traditional karyotype analysis.
When CVS is not feasible, testing maternal serum for cell-free DNA is a reasonable alternative. In a prospective cohort study of 50 maternal blood samples taken after fetal demise, 76% of samples yielded cell-free DNA results, meaning fetal fractions were within the detectable range. The higher the gestational age at the time of loss, the higher the chance of obtaining a result: Findings in the study were possible in 88% of samples when the gestational age was 8 weeks or greater, and in 53% of cases involving a lower gestational age. The time from demise to blood draw did not affect the likelihood of obtaining a result (Obstet Gynecol. 2015 Jun;125[6]:1321-29).
When neither CVS nor cell-free DNA analysis is feasible, analysis of either spontaneously passed tissue or tissue obtained at the time of a D&C may still be worthwhile. Maternal cell contamination, of course, is the main downside.
A paper published in 2020 documented the value of refocusing the initial workup. Researchers reported that 57% of 1,400 cases of recurrent pregnancy loss went unexplained using the 2012 ASRM guidelines, which included parental karyotyping but not POC cytogenetic analysis. When parental karyotypes were omitted from the initial workup and POC analysis with 24-chromosome microarray was added, at least one potential explanation for loss could be identified in 92% of cases. Only 8% were left “unexplained” (Curr Opin Obstet Gynecol. 2020 Oct;32[5]:371-9).
When genetics are ruled out
Issues that are top of mind when we lack genetic information or when genetic causes are ruled out include maternal metabolic disorders (uncontrolled diabetes, obesity, uncontrolled thyroid disease), environmental exposures (smoking), uterine abnormalities, and antiphospholipid syndrome.
Thorough evaluation of the uterine cavity after recurrent first trimester miscarriage – or after any second trimester loss – is too often a missing element of investigation. It is a vital component of the evaluation, and information about uterine structure is easily obtained.
A saline infusion sonogram (SIS) allows us to look at the external contour of the uterus, assess the myometrium for muscular abnormalities, visualize the uterine lining, and assess uterine orientation. Performed in the nonpregnant state, and ideally coupled with 3D technology, this relatively simple test can identify congenital uterine anomalies, intracavitary abnormalities (such as fibroids, polyps, or synechiae) which can surgically be removed prior to another pregnancy, a retroverted uterus that may be predisposed to incarceration during pregnancy, and other potentially impactful conditions, such as adenomyosis.
Structural anomalies
Congenital uterine anomalies are associated with first trimester miscarriage, second trimester pregnancy loss, and preterm birth. A uterine septum is of particular concern for early miscarriage, as the early embryo can implant on the relatively avascular septum.
Other congenital uterine anomalies (bicornuate, didelphys, unicornuate) can be associated with concomitant cervical structural abnormalities leading to cervical insufficiency and/or result in pathologic uterine stretch of a space-limited cavity, leading to midtrimester loss or preterm birth. The diagnosis of these anomalies is an important part of the evaluation of pregnancy loss, as it can guide monitoring in future pregnancies, or can be surgically corrected, as in the case of a uterine septum, significantly improving pregnancy outcomes.
A short cervix can result either congenitally or from injury or trauma and may also be associated with cervical insufficiency and miscarriage. It can be evaluated and monitored by ultrasound and, in some cases, treated by surgical cerclage. Pregnancy losses due to cervical insufficiency usually occur after 16 weeks of gestation and frequently are associated with intra-amniotic infections.
Incarcerated uterus and adenomyosis
Other uterine factors that can contribute to pregnancy loss and that are largely underdiagnosed or undiagnosed are an incarcerated retroverted uterus and adenomyosis.
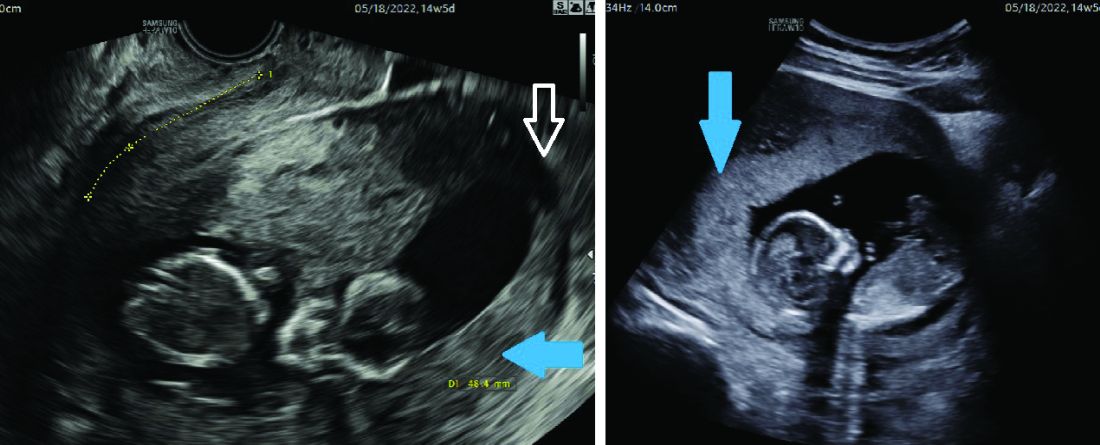
Most of the time, a retroverted uterus naturally assumes an anteverted position by the late first trimester or early second trimester, allowing for continued growth of the uterus and developing fetus. In approximately 10% of cases, however, the retroverted uterus becomes “stuck” or incarcerated in the posterior pelvis. This is more likely if there are large uterine fibroids or in the presence of pelvic adhesions due to endometriosis or previous pelvic surgery.
When this occurs, the fundus is wedged on the sacral promontory (may cause pelvic discomfort and constipation) and the cervix is markedly displaced anteriorly under the pubic symphysis (causing bladder outlet obstruction and urinary retention).
It is critical that ob.gyns. and emergency medicine providers are aware of this condition, which typically presents between 12 and 16 weeks’ gestation. The most frequent complaint is lower abdominal discomfort due to distended bladder and inability to void, which usually leads to bladder catheterization with drainage of large amounts of urine. An incarcerated uterus can predispose to pregnancy loss during this time (few other conditions cause loss during this time window), presumably due to impaired uterine artery blood flow.
Once the diagnosis is made, uterine incarceration may be corrected by elevating the gravid uterus out of the pelvis either manually, or by using a transvaginal ultrasound probe. (The latter minimally invasive approach was described in March at the American Institute of Ultrasound in Medicine’s annual conference by Martin Chavez, MD, and coinvestigators. More invasive approaches are rarely required but include CO2 intraperitoneal insufflation, as used prior to laparoscopy, or laparotomy.
The later in gestation the condition is allowed to persist, the less likely correction will be possible due to the enlarging fundus. Correction between 14 and 16 weeks, or earlier if symptoms develop, is recommended.
Adenomyosis, another poorly understood condition impacting pregnancy outcomes, has been associated with increased rates of miscarriage after in vitro fertilization (in addition to lower implantation rates); a meta-analysis published almost a decade ago found a risk ratio of miscarriage of 2.12 (95% confidence interval, 1.2-3.75) in women with adenomyosis versus those without (Hum Reprod. 2014 May;29[5]:964-77). However, outside of reproductive endocrinology, its impact on pregnancy outcomes in the obstetrical literature is not well recognized.
Although more research is necessary, we believe that adenomyosis should be considered a risk factor for pregnancy loss in the second trimester. The presence of endometrial glands within the myometrium, predisposing for an inflammatory environment, can lead to abnormal implantation, poor uterine distensibility, sterile inflammation, and early cervical insufficiency. As the prevalence of adenomyosis increases with age and maternal ages are increasing, this is an important condition to consider.
Diagnosis is typically made with MRI (although pathology of a hysterectomy specimen is the gold standard). Ultrasound findings consistent with adenomyosis are not routinely assessed and have not been studied in a gravid uterus. Nonetheless, a heightened sense of awareness about this possible contributor to pregnancy loss is very important.
A word about antiphospholipid syndrome
Antiphospholipid syndrome can cause a variety of adverse pregnancy outcomes, including first and second trimester pregnancy loss, fetal demise, fetal growth restriction, preeclampsia, preterm birth, and maternal thromboembolism. The classical presentation of miscarriage due to untreated antiphospholipid antibody syndrome is early severe fetal growth restriction, oligohydramnios, and IUFD in the second trimester.
The diagnosis requires at least one clinical criterion and one laboratory criterion. The mere presence of low level antibodies does not make the diagnosis of antiphospholipid antibody syndrome, and care should be taken to consider both the clinical and laboratory diagnostic criteria to make an accurate diagnosis.
When present, close maternal and fetal surveillance and a combination of low-dose aspirin and heparin are mainstays of treatment. The majority of studies suggest that low-molecular weight heparin (LMWH) and unfractionated heparin have comparable clinical efficacy. However, if a recurrent loss is experienced despite treatment with LMWH, the use of unfractionated heparin in a subsequent pregnancy should be considered.
Routine third-trimester ultrasounds can detect likely breech births
Implementing universal ultrasound during the third trimester of pregnancy significantly reduced the number of undiagnosed breech presentations, according to a study published in PLOS Medicine. The effects held if sonographers used a traditional ultrasound machine or if midwives used a handheld ultrasound tool to perform what is known as a point-of-care ultrasound (POCUS) procedure.
“Giving pregnant women a third-trimester scan reduces the rate of undetected breech in labor by over two-thirds, which reduces the chances of harm to the baby,” said Asma Khalil, MBBCh, MD, professor of obstetrics and maternal-fetal medicine at the University of London’s St. George’s Hospital, and a coauthor of the new study.
Routine ultrasounds typically are performed from the 10th to the 13th week of pregnancy, not during the third trimester, when the risk for a breech birth would be most apparent. Breech births occur in 3%-4% of pregnancies, raising the risk that babies will experience broken bones or hemorrhage. Knowing that breech is possible before birth enables physicians to discuss options with the pregnant woman in advance, Dr. Khalil said. These steps include rotating the baby in the uterus or conducting a cesarean delivery. Such counseling is not possible if breech is undetected until spontaneous or induced labor.
“Breech presentation at term is not very common, but diagnosing it prior to the onset of labor or induction of labor offers patients much more flexibility in terms of options and planning,” said Cecilia B. Leggett, MD, a resident in obstetrics and gynecology at Cedars-Sinai in Los Angeles. Dr. Leggett, who was not involved in the study, has shown that handheld devices are as accurate at assessing fetal weight as are standard ultrasound machines.
Two tools, same result
Dr. Khalil and her colleagues compared the rates of undiagnosed breech presentations before and after implementing universal third-semester ultrasound at two hospitals in the United Kingdom. The requirement began in 2020; the study compared the rate of undiagnosed breeches from the period of 2016-2020 with that of 2020-2021.
St. George’s Hospital in London used a traditional ultrasound machine that is read by a sonographer, whereas the Norfolk and Norwich University Hospitals, in Norwich, England, employed midwives to use a handheld ultrasound device.
The rate of undiagnosed breech cases declined from 14.2% at St. George’s before the universal ultrasound requirement (82 missed cases of 578 breech births) to 2.8% after the requirement began (7 missed cases of 251 breech births). The story was similar at Norfolk and Norwich, where 16.2% missed breech cases occurred before the requirement (27 of 167) and 3.5% missed cases were reported after it (5 of 142).
The increased accuracy of breech diagnosis before labor probably led to fewer cases of impaired blood flow to a baby’s brain at birth, Dr. Khalil’s group reported, as well as a probable reduction in the number of stillborn babies or those who die extremely young.
Traditional ultrasound scans read by sonographers are expensive, Dr. Khalil noted, whereas the portable handheld devices are much cheaper and could be used widely to improve detection of breech births. That step would require robust training about how to properly use these devices, Dr. Leggett said.
“As we see more and more studies come out about technology for POCUS, I think it’s important to keep in mind that we need the education about the tools to be as accessible as the tools themselves,” she said.
Dr. Leggett had no relevant financial relationships. Dr. Khalil is a vice president of the Royal College of Obstetricians and Gynaecologists, is a trustee and the treasurer of the International Society of Ultrasound in Obstetrics and Gynecology, and has lectured at and consulted in several ultrasound-based projects, webinars, and educational events.
A version of this article first appeared on Medscape.com.
Implementing universal ultrasound during the third trimester of pregnancy significantly reduced the number of undiagnosed breech presentations, according to a study published in PLOS Medicine. The effects held if sonographers used a traditional ultrasound machine or if midwives used a handheld ultrasound tool to perform what is known as a point-of-care ultrasound (POCUS) procedure.
“Giving pregnant women a third-trimester scan reduces the rate of undetected breech in labor by over two-thirds, which reduces the chances of harm to the baby,” said Asma Khalil, MBBCh, MD, professor of obstetrics and maternal-fetal medicine at the University of London’s St. George’s Hospital, and a coauthor of the new study.
Routine ultrasounds typically are performed from the 10th to the 13th week of pregnancy, not during the third trimester, when the risk for a breech birth would be most apparent. Breech births occur in 3%-4% of pregnancies, raising the risk that babies will experience broken bones or hemorrhage. Knowing that breech is possible before birth enables physicians to discuss options with the pregnant woman in advance, Dr. Khalil said. These steps include rotating the baby in the uterus or conducting a cesarean delivery. Such counseling is not possible if breech is undetected until spontaneous or induced labor.
“Breech presentation at term is not very common, but diagnosing it prior to the onset of labor or induction of labor offers patients much more flexibility in terms of options and planning,” said Cecilia B. Leggett, MD, a resident in obstetrics and gynecology at Cedars-Sinai in Los Angeles. Dr. Leggett, who was not involved in the study, has shown that handheld devices are as accurate at assessing fetal weight as are standard ultrasound machines.
Two tools, same result
Dr. Khalil and her colleagues compared the rates of undiagnosed breech presentations before and after implementing universal third-semester ultrasound at two hospitals in the United Kingdom. The requirement began in 2020; the study compared the rate of undiagnosed breeches from the period of 2016-2020 with that of 2020-2021.
St. George’s Hospital in London used a traditional ultrasound machine that is read by a sonographer, whereas the Norfolk and Norwich University Hospitals, in Norwich, England, employed midwives to use a handheld ultrasound device.
The rate of undiagnosed breech cases declined from 14.2% at St. George’s before the universal ultrasound requirement (82 missed cases of 578 breech births) to 2.8% after the requirement began (7 missed cases of 251 breech births). The story was similar at Norfolk and Norwich, where 16.2% missed breech cases occurred before the requirement (27 of 167) and 3.5% missed cases were reported after it (5 of 142).
The increased accuracy of breech diagnosis before labor probably led to fewer cases of impaired blood flow to a baby’s brain at birth, Dr. Khalil’s group reported, as well as a probable reduction in the number of stillborn babies or those who die extremely young.
Traditional ultrasound scans read by sonographers are expensive, Dr. Khalil noted, whereas the portable handheld devices are much cheaper and could be used widely to improve detection of breech births. That step would require robust training about how to properly use these devices, Dr. Leggett said.
“As we see more and more studies come out about technology for POCUS, I think it’s important to keep in mind that we need the education about the tools to be as accessible as the tools themselves,” she said.
Dr. Leggett had no relevant financial relationships. Dr. Khalil is a vice president of the Royal College of Obstetricians and Gynaecologists, is a trustee and the treasurer of the International Society of Ultrasound in Obstetrics and Gynecology, and has lectured at and consulted in several ultrasound-based projects, webinars, and educational events.
A version of this article first appeared on Medscape.com.
Implementing universal ultrasound during the third trimester of pregnancy significantly reduced the number of undiagnosed breech presentations, according to a study published in PLOS Medicine. The effects held if sonographers used a traditional ultrasound machine or if midwives used a handheld ultrasound tool to perform what is known as a point-of-care ultrasound (POCUS) procedure.
“Giving pregnant women a third-trimester scan reduces the rate of undetected breech in labor by over two-thirds, which reduces the chances of harm to the baby,” said Asma Khalil, MBBCh, MD, professor of obstetrics and maternal-fetal medicine at the University of London’s St. George’s Hospital, and a coauthor of the new study.
Routine ultrasounds typically are performed from the 10th to the 13th week of pregnancy, not during the third trimester, when the risk for a breech birth would be most apparent. Breech births occur in 3%-4% of pregnancies, raising the risk that babies will experience broken bones or hemorrhage. Knowing that breech is possible before birth enables physicians to discuss options with the pregnant woman in advance, Dr. Khalil said. These steps include rotating the baby in the uterus or conducting a cesarean delivery. Such counseling is not possible if breech is undetected until spontaneous or induced labor.
“Breech presentation at term is not very common, but diagnosing it prior to the onset of labor or induction of labor offers patients much more flexibility in terms of options and planning,” said Cecilia B. Leggett, MD, a resident in obstetrics and gynecology at Cedars-Sinai in Los Angeles. Dr. Leggett, who was not involved in the study, has shown that handheld devices are as accurate at assessing fetal weight as are standard ultrasound machines.
Two tools, same result
Dr. Khalil and her colleagues compared the rates of undiagnosed breech presentations before and after implementing universal third-semester ultrasound at two hospitals in the United Kingdom. The requirement began in 2020; the study compared the rate of undiagnosed breeches from the period of 2016-2020 with that of 2020-2021.
St. George’s Hospital in London used a traditional ultrasound machine that is read by a sonographer, whereas the Norfolk and Norwich University Hospitals, in Norwich, England, employed midwives to use a handheld ultrasound device.
The rate of undiagnosed breech cases declined from 14.2% at St. George’s before the universal ultrasound requirement (82 missed cases of 578 breech births) to 2.8% after the requirement began (7 missed cases of 251 breech births). The story was similar at Norfolk and Norwich, where 16.2% missed breech cases occurred before the requirement (27 of 167) and 3.5% missed cases were reported after it (5 of 142).
The increased accuracy of breech diagnosis before labor probably led to fewer cases of impaired blood flow to a baby’s brain at birth, Dr. Khalil’s group reported, as well as a probable reduction in the number of stillborn babies or those who die extremely young.
Traditional ultrasound scans read by sonographers are expensive, Dr. Khalil noted, whereas the portable handheld devices are much cheaper and could be used widely to improve detection of breech births. That step would require robust training about how to properly use these devices, Dr. Leggett said.
“As we see more and more studies come out about technology for POCUS, I think it’s important to keep in mind that we need the education about the tools to be as accessible as the tools themselves,” she said.
Dr. Leggett had no relevant financial relationships. Dr. Khalil is a vice president of the Royal College of Obstetricians and Gynaecologists, is a trustee and the treasurer of the International Society of Ultrasound in Obstetrics and Gynecology, and has lectured at and consulted in several ultrasound-based projects, webinars, and educational events.
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE
NICU use up, birth weights down in babies of mothers with HCV
Infants born to women infected with the hepatitis C virus (HCV) faced twice the risk of stays in the neonatal ICU (NICU) and 2.7 times the risk of low birth weight, a new analysis finds, even when researchers adjusted their data to control for injectable drug use and maternal medical comorbidity.
Clinicians should be “aware that the infants of pregnant people with HCV may have a high rate of need for higher-level pediatric care,” said Brenna L. Hughes, MD, MSc, chief of maternal fetal medicine at Duke University Medical Center, Durham, N.C. She spoke in an interview about the findings, which were presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
As Dr. Hughes noted, “HCV remains a serious problem in pregnancy because it often goes undiagnosed and/or untreated prior to pregnancy. It can be passed to infants, and this can cause significant health-related outcomes for children as they age.”
For the multicenter U.S. study, researchers identified 249 pregnant mothers with HCV from a 2012-2018 cohort and matched them by gestational age to controls (n = 486). The average age was 28; 71.1% of the cases were non-Hispanic White versus 41.6% of the controls; 8.4% of cases were non-Hispanic Black versus 32.1% of controls (P < .001 for race/ethnicity analysis); and 73% of cases were smokers versus 18% of controls (P < .001). More than 19% of cases reported injectable drug use during pregnancy versus 0.2% of controls (P < .001).
The researchers adjusted their findings for maternal age, body mass index, injectable drug use, and maternal comorbidity.
An earlier analysis of the study data found that 6% of pregnant women with HCV passed it on to their infants, especially those with high levels of virus in their systems. For the new study, researchers focused on various outcomes to test the assumption that “adverse pregnancy outcomes associated with HCV are related to prematurity or to ongoing use of injection drugs,” Dr. Hughes said.
There was no increase in rates of preterm birth or adverse maternal outcomes in the HCV cases. However, infants born to women with HCV were more likely than the controls to require a stay in the NICU (45% vs. 19%; adjusted relative risk, 1.99; 95% confidence interval, 1.54-2.58). They were also more likely to have lower birth weights (small for gestational age < 5th percentile) (10.6% vs. 3.1%; ARR, 2.72; 95% CI, 1.38-5.34).
No difference in outcomes was seen when HCV cases with viremia (33%) were excluded.
“The most surprising finding was that the need for higher-level pediatric care was so high even though there wasn’t an increased risk of prematurity,” Dr. Hughes said.
She added it’s not clear why NICU stays and low birth weights were more common in infants of women with HCV. “It is possible that the higher risk of need for higher-level pediatric care was related to a need for observation or treatment due to use of opioid replacement therapies with opioid agonists.” As for lower birth weight, “there may be other unmeasured risk factors.”
Tatyana Kushner, MD, MSCE, of the division of liver diseases at Icahn School of Medicine at Mount Sinai, New York, said in an interview that the study adds to limited data about HCV in pregnancy. “These findings have been demonstrated in prior studies, and it would be important to tease apart whether [low birth weight] is related to the virus itself or more related to other confounding associated factors such as maternal substance use as well as other associated social determinants of health among women with HCV.”
As for the study’s message, Dr. Kushner said it makes it clear that “hepatitis C adversely impacts outcomes of pregnancy and it is important to identify women of childbearing age for treatment early, ideally prior to pregnancy, in order to improve their pregnancy outcomes. In addition, treatment of hepatitis C during pregnancy should be explored further to determine if treatment during pregnancy can improve outcomes.”
At the moment, she said, “there are ongoing studies to delineate the safety and efficacy of hepatitis C treatment during pregnancy. Given that we are screening for hepatitis C during pregnancy, we need clear recommendations on the use of direct-acting antivirals in people who screen positive.”
The study was funded by the National Institute of Child Health and Human Development. The authors have no disclosures. Dr. Kushner disclosed research support (Gilead) and advisory board service (Gilead, AbbVie, Bausch, GlaxoSmithKline, and Eiger).
Infants born to women infected with the hepatitis C virus (HCV) faced twice the risk of stays in the neonatal ICU (NICU) and 2.7 times the risk of low birth weight, a new analysis finds, even when researchers adjusted their data to control for injectable drug use and maternal medical comorbidity.
Clinicians should be “aware that the infants of pregnant people with HCV may have a high rate of need for higher-level pediatric care,” said Brenna L. Hughes, MD, MSc, chief of maternal fetal medicine at Duke University Medical Center, Durham, N.C. She spoke in an interview about the findings, which were presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
As Dr. Hughes noted, “HCV remains a serious problem in pregnancy because it often goes undiagnosed and/or untreated prior to pregnancy. It can be passed to infants, and this can cause significant health-related outcomes for children as they age.”
For the multicenter U.S. study, researchers identified 249 pregnant mothers with HCV from a 2012-2018 cohort and matched them by gestational age to controls (n = 486). The average age was 28; 71.1% of the cases were non-Hispanic White versus 41.6% of the controls; 8.4% of cases were non-Hispanic Black versus 32.1% of controls (P < .001 for race/ethnicity analysis); and 73% of cases were smokers versus 18% of controls (P < .001). More than 19% of cases reported injectable drug use during pregnancy versus 0.2% of controls (P < .001).
The researchers adjusted their findings for maternal age, body mass index, injectable drug use, and maternal comorbidity.
An earlier analysis of the study data found that 6% of pregnant women with HCV passed it on to their infants, especially those with high levels of virus in their systems. For the new study, researchers focused on various outcomes to test the assumption that “adverse pregnancy outcomes associated with HCV are related to prematurity or to ongoing use of injection drugs,” Dr. Hughes said.
There was no increase in rates of preterm birth or adverse maternal outcomes in the HCV cases. However, infants born to women with HCV were more likely than the controls to require a stay in the NICU (45% vs. 19%; adjusted relative risk, 1.99; 95% confidence interval, 1.54-2.58). They were also more likely to have lower birth weights (small for gestational age < 5th percentile) (10.6% vs. 3.1%; ARR, 2.72; 95% CI, 1.38-5.34).
No difference in outcomes was seen when HCV cases with viremia (33%) were excluded.
“The most surprising finding was that the need for higher-level pediatric care was so high even though there wasn’t an increased risk of prematurity,” Dr. Hughes said.
She added it’s not clear why NICU stays and low birth weights were more common in infants of women with HCV. “It is possible that the higher risk of need for higher-level pediatric care was related to a need for observation or treatment due to use of opioid replacement therapies with opioid agonists.” As for lower birth weight, “there may be other unmeasured risk factors.”
Tatyana Kushner, MD, MSCE, of the division of liver diseases at Icahn School of Medicine at Mount Sinai, New York, said in an interview that the study adds to limited data about HCV in pregnancy. “These findings have been demonstrated in prior studies, and it would be important to tease apart whether [low birth weight] is related to the virus itself or more related to other confounding associated factors such as maternal substance use as well as other associated social determinants of health among women with HCV.”
As for the study’s message, Dr. Kushner said it makes it clear that “hepatitis C adversely impacts outcomes of pregnancy and it is important to identify women of childbearing age for treatment early, ideally prior to pregnancy, in order to improve their pregnancy outcomes. In addition, treatment of hepatitis C during pregnancy should be explored further to determine if treatment during pregnancy can improve outcomes.”
At the moment, she said, “there are ongoing studies to delineate the safety and efficacy of hepatitis C treatment during pregnancy. Given that we are screening for hepatitis C during pregnancy, we need clear recommendations on the use of direct-acting antivirals in people who screen positive.”
The study was funded by the National Institute of Child Health and Human Development. The authors have no disclosures. Dr. Kushner disclosed research support (Gilead) and advisory board service (Gilead, AbbVie, Bausch, GlaxoSmithKline, and Eiger).
Infants born to women infected with the hepatitis C virus (HCV) faced twice the risk of stays in the neonatal ICU (NICU) and 2.7 times the risk of low birth weight, a new analysis finds, even when researchers adjusted their data to control for injectable drug use and maternal medical comorbidity.
Clinicians should be “aware that the infants of pregnant people with HCV may have a high rate of need for higher-level pediatric care,” said Brenna L. Hughes, MD, MSc, chief of maternal fetal medicine at Duke University Medical Center, Durham, N.C. She spoke in an interview about the findings, which were presented at the meeting sponsored by the Society for Maternal-Fetal Medicine.
As Dr. Hughes noted, “HCV remains a serious problem in pregnancy because it often goes undiagnosed and/or untreated prior to pregnancy. It can be passed to infants, and this can cause significant health-related outcomes for children as they age.”
For the multicenter U.S. study, researchers identified 249 pregnant mothers with HCV from a 2012-2018 cohort and matched them by gestational age to controls (n = 486). The average age was 28; 71.1% of the cases were non-Hispanic White versus 41.6% of the controls; 8.4% of cases were non-Hispanic Black versus 32.1% of controls (P < .001 for race/ethnicity analysis); and 73% of cases were smokers versus 18% of controls (P < .001). More than 19% of cases reported injectable drug use during pregnancy versus 0.2% of controls (P < .001).
The researchers adjusted their findings for maternal age, body mass index, injectable drug use, and maternal comorbidity.
An earlier analysis of the study data found that 6% of pregnant women with HCV passed it on to their infants, especially those with high levels of virus in their systems. For the new study, researchers focused on various outcomes to test the assumption that “adverse pregnancy outcomes associated with HCV are related to prematurity or to ongoing use of injection drugs,” Dr. Hughes said.
There was no increase in rates of preterm birth or adverse maternal outcomes in the HCV cases. However, infants born to women with HCV were more likely than the controls to require a stay in the NICU (45% vs. 19%; adjusted relative risk, 1.99; 95% confidence interval, 1.54-2.58). They were also more likely to have lower birth weights (small for gestational age < 5th percentile) (10.6% vs. 3.1%; ARR, 2.72; 95% CI, 1.38-5.34).
No difference in outcomes was seen when HCV cases with viremia (33%) were excluded.
“The most surprising finding was that the need for higher-level pediatric care was so high even though there wasn’t an increased risk of prematurity,” Dr. Hughes said.
She added it’s not clear why NICU stays and low birth weights were more common in infants of women with HCV. “It is possible that the higher risk of need for higher-level pediatric care was related to a need for observation or treatment due to use of opioid replacement therapies with opioid agonists.” As for lower birth weight, “there may be other unmeasured risk factors.”
Tatyana Kushner, MD, MSCE, of the division of liver diseases at Icahn School of Medicine at Mount Sinai, New York, said in an interview that the study adds to limited data about HCV in pregnancy. “These findings have been demonstrated in prior studies, and it would be important to tease apart whether [low birth weight] is related to the virus itself or more related to other confounding associated factors such as maternal substance use as well as other associated social determinants of health among women with HCV.”
As for the study’s message, Dr. Kushner said it makes it clear that “hepatitis C adversely impacts outcomes of pregnancy and it is important to identify women of childbearing age for treatment early, ideally prior to pregnancy, in order to improve their pregnancy outcomes. In addition, treatment of hepatitis C during pregnancy should be explored further to determine if treatment during pregnancy can improve outcomes.”
At the moment, she said, “there are ongoing studies to delineate the safety and efficacy of hepatitis C treatment during pregnancy. Given that we are screening for hepatitis C during pregnancy, we need clear recommendations on the use of direct-acting antivirals in people who screen positive.”
The study was funded by the National Institute of Child Health and Human Development. The authors have no disclosures. Dr. Kushner disclosed research support (Gilead) and advisory board service (Gilead, AbbVie, Bausch, GlaxoSmithKline, and Eiger).
FROM THE PREGNANCY MEETING
Health risks low for children exposed in utero to cancer and chemo
Children who were exposed in utero to maternal cancer and treatment do not appear to have any long-term health consequences as a result of this exposure, a nationwide Danish study suggests.
The study evaluated live-born children between January 1978 and December 2018 whose mothers were diagnosed with cancer during pregnancy. Compared with unexposed fetuses, children exposed in utero had no higher overall mortality and no increased risk of congenital malformations.
Researchers also determined that exposure to chemotherapy was not associated with somatic diseases and congenital malformations when compared with in utero exposure to maternal cancer without chemotherapy.
“These findings suggest that fetal exposure to maternal cancer and treatment did not have implications for the long-term somatic and psychiatric health of the children, which is reassuring for the affected families and their health care providers,” the researchers commented.
The paper was published online in the Journal of Clinical Oncology.
Approached for comment, Katherine Van Loon, MD, MPH, director of the Global Cancer Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, said the results offer “promising news.”
“In the balance between administering needed oncologic therapy to save a mother’s life versus considering potential risks to the fetus, this data is reassuring that there is not an increased risk of catastrophic outcomes for the fetus,” Dr. Van Loon said. She noted, however, that the exposed children were not prospectively evaluated for adverse outcomes, which may have been more subtle that this study could detect.
The authors used data from the Danish Civil Registration System and Danish Medical Birth Register. They found that of 2,526,163 live-born children, 690 (0.03%) were exposed to maternal cancer in utero. Children born to mothers younger than 15 years or older than 54 years and children with an outcome diagnosis were excluded from the study.
Researchers found that children exposed to maternal cancer in utero did not demonstrate a higher overall mortality than the unexposed reference group; adjusted hazard ratio, 0.8 (95% confidence interval, 0.4-1.5). There was also no excess of congenital malformations (aHR, 1.0 [95% CI, 0.8-1.2]). In addition, there were no excesses of puberty disturbances or respiratory, cardiovascular, urinary tract, or neurologic disease.
Researchers also conducted a subgroup analysis on in utero exposure to chemotherapy, which involved 1,053,109 children born after 2002. There were 378 (0.03%) children exposed to maternal cancer in utero, and 42 (12.5%) who were exposed to chemotherapy. Chemotherapy was given during the second trimester in 73.8% of the mothers and during the third trimester in 26.2%.
No deaths or events of cancer, autism spectrum disorder, ADHD, hearing loss, or suppressed myelopoiesis were identified during follow-up of the 42 children exposed to chemotherapy in utero.
Dr. Van Loon said many cancer treatments are safe during pregnancy but added that every situation is nuanced with a number of variables to consider.
“All treatment decisions must take into account the diagnosis and prognosis of the mother, the gestational age of the fetus, and the potential teratogenic effects of the proposed treatments,” she said.
The study was supported by grants from the Research Fund of Rigshospitalet, Copenhagen University Hospital, the Novo Nordisk Foundation, Johannes Clemmesen Research Foundation, Helsefonden, Holm Memorial Foundation, and the Danish Cancer Research Foundation. Researcher disclosures are listed in the study paper.
A version of this article first appeared on Medscape.com.
Children who were exposed in utero to maternal cancer and treatment do not appear to have any long-term health consequences as a result of this exposure, a nationwide Danish study suggests.
The study evaluated live-born children between January 1978 and December 2018 whose mothers were diagnosed with cancer during pregnancy. Compared with unexposed fetuses, children exposed in utero had no higher overall mortality and no increased risk of congenital malformations.
Researchers also determined that exposure to chemotherapy was not associated with somatic diseases and congenital malformations when compared with in utero exposure to maternal cancer without chemotherapy.
“These findings suggest that fetal exposure to maternal cancer and treatment did not have implications for the long-term somatic and psychiatric health of the children, which is reassuring for the affected families and their health care providers,” the researchers commented.
The paper was published online in the Journal of Clinical Oncology.
Approached for comment, Katherine Van Loon, MD, MPH, director of the Global Cancer Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, said the results offer “promising news.”
“In the balance between administering needed oncologic therapy to save a mother’s life versus considering potential risks to the fetus, this data is reassuring that there is not an increased risk of catastrophic outcomes for the fetus,” Dr. Van Loon said. She noted, however, that the exposed children were not prospectively evaluated for adverse outcomes, which may have been more subtle that this study could detect.
The authors used data from the Danish Civil Registration System and Danish Medical Birth Register. They found that of 2,526,163 live-born children, 690 (0.03%) were exposed to maternal cancer in utero. Children born to mothers younger than 15 years or older than 54 years and children with an outcome diagnosis were excluded from the study.
Researchers found that children exposed to maternal cancer in utero did not demonstrate a higher overall mortality than the unexposed reference group; adjusted hazard ratio, 0.8 (95% confidence interval, 0.4-1.5). There was also no excess of congenital malformations (aHR, 1.0 [95% CI, 0.8-1.2]). In addition, there were no excesses of puberty disturbances or respiratory, cardiovascular, urinary tract, or neurologic disease.
Researchers also conducted a subgroup analysis on in utero exposure to chemotherapy, which involved 1,053,109 children born after 2002. There were 378 (0.03%) children exposed to maternal cancer in utero, and 42 (12.5%) who were exposed to chemotherapy. Chemotherapy was given during the second trimester in 73.8% of the mothers and during the third trimester in 26.2%.
No deaths or events of cancer, autism spectrum disorder, ADHD, hearing loss, or suppressed myelopoiesis were identified during follow-up of the 42 children exposed to chemotherapy in utero.
Dr. Van Loon said many cancer treatments are safe during pregnancy but added that every situation is nuanced with a number of variables to consider.
“All treatment decisions must take into account the diagnosis and prognosis of the mother, the gestational age of the fetus, and the potential teratogenic effects of the proposed treatments,” she said.
The study was supported by grants from the Research Fund of Rigshospitalet, Copenhagen University Hospital, the Novo Nordisk Foundation, Johannes Clemmesen Research Foundation, Helsefonden, Holm Memorial Foundation, and the Danish Cancer Research Foundation. Researcher disclosures are listed in the study paper.
A version of this article first appeared on Medscape.com.
Children who were exposed in utero to maternal cancer and treatment do not appear to have any long-term health consequences as a result of this exposure, a nationwide Danish study suggests.
The study evaluated live-born children between January 1978 and December 2018 whose mothers were diagnosed with cancer during pregnancy. Compared with unexposed fetuses, children exposed in utero had no higher overall mortality and no increased risk of congenital malformations.
Researchers also determined that exposure to chemotherapy was not associated with somatic diseases and congenital malformations when compared with in utero exposure to maternal cancer without chemotherapy.
“These findings suggest that fetal exposure to maternal cancer and treatment did not have implications for the long-term somatic and psychiatric health of the children, which is reassuring for the affected families and their health care providers,” the researchers commented.
The paper was published online in the Journal of Clinical Oncology.
Approached for comment, Katherine Van Loon, MD, MPH, director of the Global Cancer Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, said the results offer “promising news.”
“In the balance between administering needed oncologic therapy to save a mother’s life versus considering potential risks to the fetus, this data is reassuring that there is not an increased risk of catastrophic outcomes for the fetus,” Dr. Van Loon said. She noted, however, that the exposed children were not prospectively evaluated for adverse outcomes, which may have been more subtle that this study could detect.
The authors used data from the Danish Civil Registration System and Danish Medical Birth Register. They found that of 2,526,163 live-born children, 690 (0.03%) were exposed to maternal cancer in utero. Children born to mothers younger than 15 years or older than 54 years and children with an outcome diagnosis were excluded from the study.
Researchers found that children exposed to maternal cancer in utero did not demonstrate a higher overall mortality than the unexposed reference group; adjusted hazard ratio, 0.8 (95% confidence interval, 0.4-1.5). There was also no excess of congenital malformations (aHR, 1.0 [95% CI, 0.8-1.2]). In addition, there were no excesses of puberty disturbances or respiratory, cardiovascular, urinary tract, or neurologic disease.
Researchers also conducted a subgroup analysis on in utero exposure to chemotherapy, which involved 1,053,109 children born after 2002. There were 378 (0.03%) children exposed to maternal cancer in utero, and 42 (12.5%) who were exposed to chemotherapy. Chemotherapy was given during the second trimester in 73.8% of the mothers and during the third trimester in 26.2%.
No deaths or events of cancer, autism spectrum disorder, ADHD, hearing loss, or suppressed myelopoiesis were identified during follow-up of the 42 children exposed to chemotherapy in utero.
Dr. Van Loon said many cancer treatments are safe during pregnancy but added that every situation is nuanced with a number of variables to consider.
“All treatment decisions must take into account the diagnosis and prognosis of the mother, the gestational age of the fetus, and the potential teratogenic effects of the proposed treatments,” she said.
The study was supported by grants from the Research Fund of Rigshospitalet, Copenhagen University Hospital, the Novo Nordisk Foundation, Johannes Clemmesen Research Foundation, Helsefonden, Holm Memorial Foundation, and the Danish Cancer Research Foundation. Researcher disclosures are listed in the study paper.
A version of this article first appeared on Medscape.com.
They trusted their prenatal test. They didn’t know the industry is an unregulated ‘Wild West.’
Amanda wanted to warn someone. In June 2021, her daughter – the one she and her husband had tried for 3 years to conceive – had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the light bulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests – including certain tests for COVID-19 or, say, pregnancy – the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong – sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in 6 years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, the New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings – and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University, Washington, law professor specializing in bioethics.
The stakes for families are increasing. Upward of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last 2 decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
‘They started using it on humans, and then they went back and said: “Was our test accurate?” ’
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as 9 weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex – a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Dr. Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about 2 months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’ ” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money, and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai Medical Center in Los Angeles. The push left many ob.gyns. and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in 1 year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after 5 months in 2016.
The rep, who requested anonymity because she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests – for Down syndrome and trisomy 18 – often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at the University of California, San Francisco, Medical Center’s prenatal diagnostic center. Considered a leading researcher in the field, she was an author of many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested, and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value – that is, the probability that a positive screening result will turn out to be correct – will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took 5 agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.
‘I can’t believe I didn’t say more’
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as 1 of 20 concerning tests.
But, over the next 2 years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Mr. Clement has reportedly commanded rates of $1,350 per hour. He and Mr. Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress – and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Mr. Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’ ” Mr. Lurie later told ProPublica. (After leaving the agency, Mr. Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the coauthors had disclosed no conflicts of interest. But two of the four coauthors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third coauthor with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in 5 months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Dr. Norton, who coauthored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, 4 months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known – known, or should have been known – for 10 years,” she said.
‘It had me so messed up’
With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits – and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
The screenings showed the baby was a girl – but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.
The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to 4 more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time – ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there’s a false positive, they say, ‘Well, we’re not diagnostic.’ ”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.
Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones – those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus,” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value (PPV) of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” because of the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
‘The margin of error is a human life’
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home – one who lives past the first 2 nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out – after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Amanda wanted to warn someone. In June 2021, her daughter – the one she and her husband had tried for 3 years to conceive – had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the light bulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests – including certain tests for COVID-19 or, say, pregnancy – the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong – sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in 6 years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, the New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings – and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University, Washington, law professor specializing in bioethics.
The stakes for families are increasing. Upward of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last 2 decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
‘They started using it on humans, and then they went back and said: “Was our test accurate?” ’
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as 9 weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex – a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Dr. Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about 2 months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’ ” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money, and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai Medical Center in Los Angeles. The push left many ob.gyns. and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in 1 year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after 5 months in 2016.
The rep, who requested anonymity because she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests – for Down syndrome and trisomy 18 – often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at the University of California, San Francisco, Medical Center’s prenatal diagnostic center. Considered a leading researcher in the field, she was an author of many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested, and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value – that is, the probability that a positive screening result will turn out to be correct – will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took 5 agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.
‘I can’t believe I didn’t say more’
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as 1 of 20 concerning tests.
But, over the next 2 years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Mr. Clement has reportedly commanded rates of $1,350 per hour. He and Mr. Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress – and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Mr. Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’ ” Mr. Lurie later told ProPublica. (After leaving the agency, Mr. Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the coauthors had disclosed no conflicts of interest. But two of the four coauthors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third coauthor with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in 5 months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Dr. Norton, who coauthored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, 4 months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known – known, or should have been known – for 10 years,” she said.
‘It had me so messed up’
With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits – and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
The screenings showed the baby was a girl – but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.
The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to 4 more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time – ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there’s a false positive, they say, ‘Well, we’re not diagnostic.’ ”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.
Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones – those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus,” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value (PPV) of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” because of the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
‘The margin of error is a human life’
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home – one who lives past the first 2 nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out – after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Amanda wanted to warn someone. In June 2021, her daughter – the one she and her husband had tried for 3 years to conceive – had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the light bulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests – including certain tests for COVID-19 or, say, pregnancy – the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong – sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in 6 years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, the New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings – and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University, Washington, law professor specializing in bioethics.
The stakes for families are increasing. Upward of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last 2 decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
‘They started using it on humans, and then they went back and said: “Was our test accurate?” ’
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as 9 weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex – a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Dr. Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about 2 months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’ ” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money, and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai Medical Center in Los Angeles. The push left many ob.gyns. and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in 1 year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after 5 months in 2016.
The rep, who requested anonymity because she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests – for Down syndrome and trisomy 18 – often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at the University of California, San Francisco, Medical Center’s prenatal diagnostic center. Considered a leading researcher in the field, she was an author of many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested, and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value – that is, the probability that a positive screening result will turn out to be correct – will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took 5 agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.
‘I can’t believe I didn’t say more’
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as 1 of 20 concerning tests.
But, over the next 2 years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Mr. Clement has reportedly commanded rates of $1,350 per hour. He and Mr. Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress – and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Mr. Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’ ” Mr. Lurie later told ProPublica. (After leaving the agency, Mr. Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the coauthors had disclosed no conflicts of interest. But two of the four coauthors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third coauthor with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in 5 months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Dr. Norton, who coauthored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, 4 months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known – known, or should have been known – for 10 years,” she said.
‘It had me so messed up’
With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits – and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
The screenings showed the baby was a girl – but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.
The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to 4 more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time – ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there’s a false positive, they say, ‘Well, we’re not diagnostic.’ ”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.
Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones – those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus,” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value (PPV) of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” because of the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
‘The margin of error is a human life’
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home – one who lives past the first 2 nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out – after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Pregnant, postpartum women with disabilities at higher risk for violence
Pregnant or postpartum women with disabilities are at relatively high risk of experiencing violence, often from the people closest to them, new research suggests.
The researchers set out to measure risk of interpersonal violence, which the World Health Organization defines as “the intentional use of physical force or power against an individual by an intimate partner, family member, or other community member.”
Hilary K. Brown, PhD, with the department of health & society, University of Toronto, led the study published online in Obstetrics and Gynecology.
Large, population-based dataset
The population study included people 15-49 years old with births in Ontario from 2004 to 2019. They included 147,414 people with physical disabilities; 47,459 people with intellectual disabilities; 2,557 with developmental disabilities; and 9,598 with multiple disabilities.
The control group was 1,594,441 million people without disabilities.
The outcome measured was “any emergency department visit, hospital admission, or death related to physical, sexual, or psychological violence between fertilization and 365 days post partum.”
Researchers found that the adjusted relative risk of interpersonal violence for those with disabilities, compared with those with no disabilities was 1.40 (95% confidence interval, 1.31-1.50) in those with physical disabilities; 2.39 (95% CI, 1.98-2.88) in those with intellectual or developmental disabilities; and 1.96 (95% CI, 1.66-2.30) in those with multiple disabilities.
History of violence means higher risk
Those with a history of interpersonal violence and a disability were at particularly high risk for perinatal violence.
The authors note that pregnancy is a high-risk period for interpersonal violence for all women, particularly by an intimate partner.
“More than 30% of intimate partner violence begins during pregnancy, and preexisting violence tends to escalate perinatally,” they write.
The authors cite previous research that found women with disabilities experience higher rates of abuse overall and by an intimate partner – two to four times rates reported by those without disabilities.
Opportunities for provider intervention
Since the period surrounding pregnancy is a time of increased contact with medical providers and resources, there may be opportunities for identifying abuse and providing interventions.
Those might include better screening, access to violence-related information and services, and education of health care professionals to support people with disabilities. For example, “Tools used for violence screening perinatally do not include items about forms of violence that are unique to individuals with disabilities, such as refusal to assist with activities of daily living.”
The authors add: “[G]iven that the strongest risk factor for interpersonal violence in the perinatal period, particularly in those with disabilities, was a prepregnancy history of interpersonal violence, our findings suggest that more could be done before pregnancy to offer screening and support at the index encounter.”
Violence can lead to adverse outcomes
Implications are important as the violence can result in barriers to care and adverse perinatal outcomes.
Jeanne L. Alhusen, PhD, CRNP, RN, University of Virginia Medical Center professor of nursing and associate dean for research, was not part of this research but wrote a paper earlier this year on the subject and had similar conclusions.
She said before this study by Brown et al., “our understanding of the risk of violence by disability type throughout the perinatal period, on a population-based level, was quite limited.”
With the size of this dataset, she said, this paper provides critical information for health care providers. It extends physicians’ ability to examine risk of violence by disability type as well as these patients’ risk of experiencing different types of violence.
She pointed out that the Pregnancy Risk Assessment Monitoring System (PRAMS) recently incorporated a disability supplement that allows better understanding of pregnancy risks in people with disabilities.
“It will be critical that U.S. states continue to incorporate the disability questions into their PRAMS administration [because] without that information, persons with disabilities will continue to experience unconscionable inequities,” she said.
Barriers to equitable care
Dr. Alhusen added that people with disabilities experience significant barriers in accessing equitable care – both at the provider and the system level.
She said it is critical that we recognize and address the sexual and reproductive health needs of all persons with disability. “This includes screening every person for violence and [ensuring] the tools we utilize are accessible and include items specific to disability-related abuse. In our qualitative studies, we have heard from pregnant persons that they were never screened or that they were screened with their abusive partner sitting next to them.”
Screening questions to ask
The American College of Obstetricians and Gynecologists provides examples of screening questions that are specific to people with disabilities such as asking if a partner has ever prevented the individual from using an assistive device (for example, a wheelchair, cane, or respirator) or refused to help with an important personal need, such as taking medication or getting out of bed.
“For many reasons, people with disabilities are less likely to disclose violence, and health care professionals are less likely to ask them about it,” said coauthor of the current study, Yona Lunsky, PhD, clinician-scientist, Centre for Addiction and Mental Health, Toronto, in a statement. Based on the findings, she said, she hopes clinicians will see the need to develop disability-informed screening tools to capture abuse and identify the appropriate resources for this population before, during, and after pregnancy.
Coauthor Dr. Natasha Saunders receives an honorarium from the BMJ Group (Archives of Diseases in Childhood). Coauthor Dr. Simone N. Vigod receives royalties from UpToDate for authorship of materials related to depression and pregnancy. The other authors did not report any potential conflicts of interest. Dr. Alhusen reported no relevant financial relationships.
Pregnant or postpartum women with disabilities are at relatively high risk of experiencing violence, often from the people closest to them, new research suggests.
The researchers set out to measure risk of interpersonal violence, which the World Health Organization defines as “the intentional use of physical force or power against an individual by an intimate partner, family member, or other community member.”
Hilary K. Brown, PhD, with the department of health & society, University of Toronto, led the study published online in Obstetrics and Gynecology.
Large, population-based dataset
The population study included people 15-49 years old with births in Ontario from 2004 to 2019. They included 147,414 people with physical disabilities; 47,459 people with intellectual disabilities; 2,557 with developmental disabilities; and 9,598 with multiple disabilities.
The control group was 1,594,441 million people without disabilities.
The outcome measured was “any emergency department visit, hospital admission, or death related to physical, sexual, or psychological violence between fertilization and 365 days post partum.”
Researchers found that the adjusted relative risk of interpersonal violence for those with disabilities, compared with those with no disabilities was 1.40 (95% confidence interval, 1.31-1.50) in those with physical disabilities; 2.39 (95% CI, 1.98-2.88) in those with intellectual or developmental disabilities; and 1.96 (95% CI, 1.66-2.30) in those with multiple disabilities.
History of violence means higher risk
Those with a history of interpersonal violence and a disability were at particularly high risk for perinatal violence.
The authors note that pregnancy is a high-risk period for interpersonal violence for all women, particularly by an intimate partner.
“More than 30% of intimate partner violence begins during pregnancy, and preexisting violence tends to escalate perinatally,” they write.
The authors cite previous research that found women with disabilities experience higher rates of abuse overall and by an intimate partner – two to four times rates reported by those without disabilities.
Opportunities for provider intervention
Since the period surrounding pregnancy is a time of increased contact with medical providers and resources, there may be opportunities for identifying abuse and providing interventions.
Those might include better screening, access to violence-related information and services, and education of health care professionals to support people with disabilities. For example, “Tools used for violence screening perinatally do not include items about forms of violence that are unique to individuals with disabilities, such as refusal to assist with activities of daily living.”
The authors add: “[G]iven that the strongest risk factor for interpersonal violence in the perinatal period, particularly in those with disabilities, was a prepregnancy history of interpersonal violence, our findings suggest that more could be done before pregnancy to offer screening and support at the index encounter.”
Violence can lead to adverse outcomes
Implications are important as the violence can result in barriers to care and adverse perinatal outcomes.
Jeanne L. Alhusen, PhD, CRNP, RN, University of Virginia Medical Center professor of nursing and associate dean for research, was not part of this research but wrote a paper earlier this year on the subject and had similar conclusions.
She said before this study by Brown et al., “our understanding of the risk of violence by disability type throughout the perinatal period, on a population-based level, was quite limited.”
With the size of this dataset, she said, this paper provides critical information for health care providers. It extends physicians’ ability to examine risk of violence by disability type as well as these patients’ risk of experiencing different types of violence.
She pointed out that the Pregnancy Risk Assessment Monitoring System (PRAMS) recently incorporated a disability supplement that allows better understanding of pregnancy risks in people with disabilities.
“It will be critical that U.S. states continue to incorporate the disability questions into their PRAMS administration [because] without that information, persons with disabilities will continue to experience unconscionable inequities,” she said.
Barriers to equitable care
Dr. Alhusen added that people with disabilities experience significant barriers in accessing equitable care – both at the provider and the system level.
She said it is critical that we recognize and address the sexual and reproductive health needs of all persons with disability. “This includes screening every person for violence and [ensuring] the tools we utilize are accessible and include items specific to disability-related abuse. In our qualitative studies, we have heard from pregnant persons that they were never screened or that they were screened with their abusive partner sitting next to them.”
Screening questions to ask
The American College of Obstetricians and Gynecologists provides examples of screening questions that are specific to people with disabilities such as asking if a partner has ever prevented the individual from using an assistive device (for example, a wheelchair, cane, or respirator) or refused to help with an important personal need, such as taking medication or getting out of bed.
“For many reasons, people with disabilities are less likely to disclose violence, and health care professionals are less likely to ask them about it,” said coauthor of the current study, Yona Lunsky, PhD, clinician-scientist, Centre for Addiction and Mental Health, Toronto, in a statement. Based on the findings, she said, she hopes clinicians will see the need to develop disability-informed screening tools to capture abuse and identify the appropriate resources for this population before, during, and after pregnancy.
Coauthor Dr. Natasha Saunders receives an honorarium from the BMJ Group (Archives of Diseases in Childhood). Coauthor Dr. Simone N. Vigod receives royalties from UpToDate for authorship of materials related to depression and pregnancy. The other authors did not report any potential conflicts of interest. Dr. Alhusen reported no relevant financial relationships.
Pregnant or postpartum women with disabilities are at relatively high risk of experiencing violence, often from the people closest to them, new research suggests.
The researchers set out to measure risk of interpersonal violence, which the World Health Organization defines as “the intentional use of physical force or power against an individual by an intimate partner, family member, or other community member.”
Hilary K. Brown, PhD, with the department of health & society, University of Toronto, led the study published online in Obstetrics and Gynecology.
Large, population-based dataset
The population study included people 15-49 years old with births in Ontario from 2004 to 2019. They included 147,414 people with physical disabilities; 47,459 people with intellectual disabilities; 2,557 with developmental disabilities; and 9,598 with multiple disabilities.
The control group was 1,594,441 million people without disabilities.
The outcome measured was “any emergency department visit, hospital admission, or death related to physical, sexual, or psychological violence between fertilization and 365 days post partum.”
Researchers found that the adjusted relative risk of interpersonal violence for those with disabilities, compared with those with no disabilities was 1.40 (95% confidence interval, 1.31-1.50) in those with physical disabilities; 2.39 (95% CI, 1.98-2.88) in those with intellectual or developmental disabilities; and 1.96 (95% CI, 1.66-2.30) in those with multiple disabilities.
History of violence means higher risk
Those with a history of interpersonal violence and a disability were at particularly high risk for perinatal violence.
The authors note that pregnancy is a high-risk period for interpersonal violence for all women, particularly by an intimate partner.
“More than 30% of intimate partner violence begins during pregnancy, and preexisting violence tends to escalate perinatally,” they write.
The authors cite previous research that found women with disabilities experience higher rates of abuse overall and by an intimate partner – two to four times rates reported by those without disabilities.
Opportunities for provider intervention
Since the period surrounding pregnancy is a time of increased contact with medical providers and resources, there may be opportunities for identifying abuse and providing interventions.
Those might include better screening, access to violence-related information and services, and education of health care professionals to support people with disabilities. For example, “Tools used for violence screening perinatally do not include items about forms of violence that are unique to individuals with disabilities, such as refusal to assist with activities of daily living.”
The authors add: “[G]iven that the strongest risk factor for interpersonal violence in the perinatal period, particularly in those with disabilities, was a prepregnancy history of interpersonal violence, our findings suggest that more could be done before pregnancy to offer screening and support at the index encounter.”
Violence can lead to adverse outcomes
Implications are important as the violence can result in barriers to care and adverse perinatal outcomes.
Jeanne L. Alhusen, PhD, CRNP, RN, University of Virginia Medical Center professor of nursing and associate dean for research, was not part of this research but wrote a paper earlier this year on the subject and had similar conclusions.
She said before this study by Brown et al., “our understanding of the risk of violence by disability type throughout the perinatal period, on a population-based level, was quite limited.”
With the size of this dataset, she said, this paper provides critical information for health care providers. It extends physicians’ ability to examine risk of violence by disability type as well as these patients’ risk of experiencing different types of violence.
She pointed out that the Pregnancy Risk Assessment Monitoring System (PRAMS) recently incorporated a disability supplement that allows better understanding of pregnancy risks in people with disabilities.
“It will be critical that U.S. states continue to incorporate the disability questions into their PRAMS administration [because] without that information, persons with disabilities will continue to experience unconscionable inequities,” she said.
Barriers to equitable care
Dr. Alhusen added that people with disabilities experience significant barriers in accessing equitable care – both at the provider and the system level.
She said it is critical that we recognize and address the sexual and reproductive health needs of all persons with disability. “This includes screening every person for violence and [ensuring] the tools we utilize are accessible and include items specific to disability-related abuse. In our qualitative studies, we have heard from pregnant persons that they were never screened or that they were screened with their abusive partner sitting next to them.”
Screening questions to ask
The American College of Obstetricians and Gynecologists provides examples of screening questions that are specific to people with disabilities such as asking if a partner has ever prevented the individual from using an assistive device (for example, a wheelchair, cane, or respirator) or refused to help with an important personal need, such as taking medication or getting out of bed.
“For many reasons, people with disabilities are less likely to disclose violence, and health care professionals are less likely to ask them about it,” said coauthor of the current study, Yona Lunsky, PhD, clinician-scientist, Centre for Addiction and Mental Health, Toronto, in a statement. Based on the findings, she said, she hopes clinicians will see the need to develop disability-informed screening tools to capture abuse and identify the appropriate resources for this population before, during, and after pregnancy.
Coauthor Dr. Natasha Saunders receives an honorarium from the BMJ Group (Archives of Diseases in Childhood). Coauthor Dr. Simone N. Vigod receives royalties from UpToDate for authorship of materials related to depression and pregnancy. The other authors did not report any potential conflicts of interest. Dr. Alhusen reported no relevant financial relationships.
FROM OBSTETRICS AND GYNECOLOGY
Lasker awardee pioneered prenatal DNA testing
For Yuk Ming Dennis Lo, BM BCh, DPhil, a 1996 paper showing the detection of tumor DNA in blood plasma would prove a turning point.
Since the 1960s, clinicians had been searching for a way to glimpse into a fetus’ genetic makeup without disturbing the pregnancy – a fascination Dr. Lo, at the time a graduate student in the United Kingdom, shared.
But the article triggered a thought. If cancer cells could release their DNA into blood plasma, then maybe fetuses could, too. “I had the strange thought that the cancer growing in the patients is a little bit like the placenta that has implanted into the uterus,” he told The New York Times.
The answer was yes. In 1997, having returned home to Hong Kong, Dr. Lo published a seminal article showing that cell-free fetal DNA could be detected in maternal blood.
He went on to devise methods to detect markers for Down syndrome, creating a noninvasive test that is more than 99% accurate for ruling out the disorder, along with screenings for trisomy 18 (Edwards syndrome), trisomy 13 (Patau syndrome), and other chromosome abnormalities.
With the commercial launch of noninvasive prenatal testing (NIPT) in 2011, health care centers around the world quickly embraced the technology as a safe alternative to more invasive methods, such as amniocentesis, for identifying fetal abnormalities. NIPT is now available in over 60 countries and is widely used by clinicians, according to the Lasker Foundation, which granted him the 2022 Lasker DeBakey Clinical Medical Research Award, along with a $250,000 prize.
“I am pleased that since its launch, noninvasive prenatal testing has become a standard of care,” Dr. Lo, chair of the department of chemical pathology at The Chinese University of Hong Kong, said in a video on the Lasker website. “It has also stimulated a global interest in the diagnostic applications of plasma DNA, especially in the area of cancer liquid biopsies and transplantation monitoring. I look forward to seeing these and other yet to be developed applications improving health care worldwide.”
Dr. Lo’s work has inspired clinical advances and applications, including Rh factor assessments, innovations in cancer technology, transplantation, and beyond, according to Lasker.
Iris Krishna, MD, MPH, director of Perinatal Quality in the Emory Perinatal Center at Emory University School of Medicine, Atlanta, said Dr. Lo’s work has also provided opportunities to screen for other genetic disorders, such as microdeletion syndromes and single gene disorders
“As we continue to learn about the possibilities of this technology, it is imperative for the clinician to be knowledgeable of the benefits and limitations of cell-free DNA screening to be able to counsel their patients appropriately,” Dr. Krishna said.
A COVID clearinghouse
Lauren Gardner, PhD, professor in the department of civil and systems engineering at Johns Hopkins University, Baltimore, received the Lasker Bloomberg Public Service Award for her work on the Johns Hopkins’ COVID-19 dashboard, a critical tool for the dissemination of public health data in real time.
According to the Los Angeles Times, Ensheng Dong, Dr. Gardner’s graduate student, approached her about tracking cases of the emerging infection in his home country of China. Mr. Dong mined Chinese websites for early cases of COVID-19 and created online maps using the information. At Dr. Gardner’s suggestion, he expanded the database to include global data.
At the time, according to Lasker, no other institution was providing this information. The World Health Organization created summaries of daily COVID-19 counts, but the data were not as accessible. Dr. Gardner said timely and obtainable information was crucial to craft nimble and rational strategies for combating the pandemic.
“Given the amount of misinformation in circulation and the highly politicized nature of the COVID-19 public health crisis, our work enabled individuals to access the information they needed to make informed decisions to protect themselves, which was especially critical in those locations with delayed or nonexistent policies in place,” Dr. Gardner said in a statement.
Dr. Gardner said she was excited to pursue additional data-centric projects. “I am optimistic that in the future, timely public health information will become increasingly available, especially in times of crisis,” she said. “Moving forward, I am excited to build on our learnings from COVID-19 and transfer that knowledge to address other problems facing societies.”
New knowledge of cells, immunology, and disease
The 2022 Albert Lasker Basic Research Award honored three scientists who helped identify a family of proteins that connect cells and assist the immune system in attaching to its targets. The proteins, called integrins, are needed for cells to interact with each other to build complex structures in the body. They are also key to the process T cells undergo to recognize and attack cancer cells.
Awardees Richard O. Hynes, MA, PhD, distinguished professor of cancer research at Massachusetts Institute of Technology; Erkki Ruoslahti, MD, PhD, distinguished professor emeritus at Sanford Burnham Prebys Medical Discovery Institute, La Jolla, California; and Timothy A. Springer, PhD, professor of biological chemistry and molecular biology at Boston Children’s Hospital and Harvard Medical School, independently identified a cell-surface–associated protein that helps cells attach to the extracellular matrix.
“Many of the mysteries of how integrins work are only being discovered today,” Dr. Springer said in his acceptance remarks online.
The discoveries related to integrins have led to several clinical advances, including the development of drugs like the eyedrops lifitegrast, the biologic agent vedolizumab (made using integrins Springer discovered), and tirofiban, a medication used to hamper clotting in cardiovascular diseases.
A version of this article first appeared on Medscape.com.
For Yuk Ming Dennis Lo, BM BCh, DPhil, a 1996 paper showing the detection of tumor DNA in blood plasma would prove a turning point.
Since the 1960s, clinicians had been searching for a way to glimpse into a fetus’ genetic makeup without disturbing the pregnancy – a fascination Dr. Lo, at the time a graduate student in the United Kingdom, shared.
But the article triggered a thought. If cancer cells could release their DNA into blood plasma, then maybe fetuses could, too. “I had the strange thought that the cancer growing in the patients is a little bit like the placenta that has implanted into the uterus,” he told The New York Times.
The answer was yes. In 1997, having returned home to Hong Kong, Dr. Lo published a seminal article showing that cell-free fetal DNA could be detected in maternal blood.
He went on to devise methods to detect markers for Down syndrome, creating a noninvasive test that is more than 99% accurate for ruling out the disorder, along with screenings for trisomy 18 (Edwards syndrome), trisomy 13 (Patau syndrome), and other chromosome abnormalities.
With the commercial launch of noninvasive prenatal testing (NIPT) in 2011, health care centers around the world quickly embraced the technology as a safe alternative to more invasive methods, such as amniocentesis, for identifying fetal abnormalities. NIPT is now available in over 60 countries and is widely used by clinicians, according to the Lasker Foundation, which granted him the 2022 Lasker DeBakey Clinical Medical Research Award, along with a $250,000 prize.
“I am pleased that since its launch, noninvasive prenatal testing has become a standard of care,” Dr. Lo, chair of the department of chemical pathology at The Chinese University of Hong Kong, said in a video on the Lasker website. “It has also stimulated a global interest in the diagnostic applications of plasma DNA, especially in the area of cancer liquid biopsies and transplantation monitoring. I look forward to seeing these and other yet to be developed applications improving health care worldwide.”
Dr. Lo’s work has inspired clinical advances and applications, including Rh factor assessments, innovations in cancer technology, transplantation, and beyond, according to Lasker.
Iris Krishna, MD, MPH, director of Perinatal Quality in the Emory Perinatal Center at Emory University School of Medicine, Atlanta, said Dr. Lo’s work has also provided opportunities to screen for other genetic disorders, such as microdeletion syndromes and single gene disorders
“As we continue to learn about the possibilities of this technology, it is imperative for the clinician to be knowledgeable of the benefits and limitations of cell-free DNA screening to be able to counsel their patients appropriately,” Dr. Krishna said.
A COVID clearinghouse
Lauren Gardner, PhD, professor in the department of civil and systems engineering at Johns Hopkins University, Baltimore, received the Lasker Bloomberg Public Service Award for her work on the Johns Hopkins’ COVID-19 dashboard, a critical tool for the dissemination of public health data in real time.
According to the Los Angeles Times, Ensheng Dong, Dr. Gardner’s graduate student, approached her about tracking cases of the emerging infection in his home country of China. Mr. Dong mined Chinese websites for early cases of COVID-19 and created online maps using the information. At Dr. Gardner’s suggestion, he expanded the database to include global data.
At the time, according to Lasker, no other institution was providing this information. The World Health Organization created summaries of daily COVID-19 counts, but the data were not as accessible. Dr. Gardner said timely and obtainable information was crucial to craft nimble and rational strategies for combating the pandemic.
“Given the amount of misinformation in circulation and the highly politicized nature of the COVID-19 public health crisis, our work enabled individuals to access the information they needed to make informed decisions to protect themselves, which was especially critical in those locations with delayed or nonexistent policies in place,” Dr. Gardner said in a statement.
Dr. Gardner said she was excited to pursue additional data-centric projects. “I am optimistic that in the future, timely public health information will become increasingly available, especially in times of crisis,” she said. “Moving forward, I am excited to build on our learnings from COVID-19 and transfer that knowledge to address other problems facing societies.”
New knowledge of cells, immunology, and disease
The 2022 Albert Lasker Basic Research Award honored three scientists who helped identify a family of proteins that connect cells and assist the immune system in attaching to its targets. The proteins, called integrins, are needed for cells to interact with each other to build complex structures in the body. They are also key to the process T cells undergo to recognize and attack cancer cells.
Awardees Richard O. Hynes, MA, PhD, distinguished professor of cancer research at Massachusetts Institute of Technology; Erkki Ruoslahti, MD, PhD, distinguished professor emeritus at Sanford Burnham Prebys Medical Discovery Institute, La Jolla, California; and Timothy A. Springer, PhD, professor of biological chemistry and molecular biology at Boston Children’s Hospital and Harvard Medical School, independently identified a cell-surface–associated protein that helps cells attach to the extracellular matrix.
“Many of the mysteries of how integrins work are only being discovered today,” Dr. Springer said in his acceptance remarks online.
The discoveries related to integrins have led to several clinical advances, including the development of drugs like the eyedrops lifitegrast, the biologic agent vedolizumab (made using integrins Springer discovered), and tirofiban, a medication used to hamper clotting in cardiovascular diseases.
A version of this article first appeared on Medscape.com.
For Yuk Ming Dennis Lo, BM BCh, DPhil, a 1996 paper showing the detection of tumor DNA in blood plasma would prove a turning point.
Since the 1960s, clinicians had been searching for a way to glimpse into a fetus’ genetic makeup without disturbing the pregnancy – a fascination Dr. Lo, at the time a graduate student in the United Kingdom, shared.
But the article triggered a thought. If cancer cells could release their DNA into blood plasma, then maybe fetuses could, too. “I had the strange thought that the cancer growing in the patients is a little bit like the placenta that has implanted into the uterus,” he told The New York Times.
The answer was yes. In 1997, having returned home to Hong Kong, Dr. Lo published a seminal article showing that cell-free fetal DNA could be detected in maternal blood.
He went on to devise methods to detect markers for Down syndrome, creating a noninvasive test that is more than 99% accurate for ruling out the disorder, along with screenings for trisomy 18 (Edwards syndrome), trisomy 13 (Patau syndrome), and other chromosome abnormalities.
With the commercial launch of noninvasive prenatal testing (NIPT) in 2011, health care centers around the world quickly embraced the technology as a safe alternative to more invasive methods, such as amniocentesis, for identifying fetal abnormalities. NIPT is now available in over 60 countries and is widely used by clinicians, according to the Lasker Foundation, which granted him the 2022 Lasker DeBakey Clinical Medical Research Award, along with a $250,000 prize.
“I am pleased that since its launch, noninvasive prenatal testing has become a standard of care,” Dr. Lo, chair of the department of chemical pathology at The Chinese University of Hong Kong, said in a video on the Lasker website. “It has also stimulated a global interest in the diagnostic applications of plasma DNA, especially in the area of cancer liquid biopsies and transplantation monitoring. I look forward to seeing these and other yet to be developed applications improving health care worldwide.”
Dr. Lo’s work has inspired clinical advances and applications, including Rh factor assessments, innovations in cancer technology, transplantation, and beyond, according to Lasker.
Iris Krishna, MD, MPH, director of Perinatal Quality in the Emory Perinatal Center at Emory University School of Medicine, Atlanta, said Dr. Lo’s work has also provided opportunities to screen for other genetic disorders, such as microdeletion syndromes and single gene disorders
“As we continue to learn about the possibilities of this technology, it is imperative for the clinician to be knowledgeable of the benefits and limitations of cell-free DNA screening to be able to counsel their patients appropriately,” Dr. Krishna said.
A COVID clearinghouse
Lauren Gardner, PhD, professor in the department of civil and systems engineering at Johns Hopkins University, Baltimore, received the Lasker Bloomberg Public Service Award for her work on the Johns Hopkins’ COVID-19 dashboard, a critical tool for the dissemination of public health data in real time.
According to the Los Angeles Times, Ensheng Dong, Dr. Gardner’s graduate student, approached her about tracking cases of the emerging infection in his home country of China. Mr. Dong mined Chinese websites for early cases of COVID-19 and created online maps using the information. At Dr. Gardner’s suggestion, he expanded the database to include global data.
At the time, according to Lasker, no other institution was providing this information. The World Health Organization created summaries of daily COVID-19 counts, but the data were not as accessible. Dr. Gardner said timely and obtainable information was crucial to craft nimble and rational strategies for combating the pandemic.
“Given the amount of misinformation in circulation and the highly politicized nature of the COVID-19 public health crisis, our work enabled individuals to access the information they needed to make informed decisions to protect themselves, which was especially critical in those locations with delayed or nonexistent policies in place,” Dr. Gardner said in a statement.
Dr. Gardner said she was excited to pursue additional data-centric projects. “I am optimistic that in the future, timely public health information will become increasingly available, especially in times of crisis,” she said. “Moving forward, I am excited to build on our learnings from COVID-19 and transfer that knowledge to address other problems facing societies.”
New knowledge of cells, immunology, and disease
The 2022 Albert Lasker Basic Research Award honored three scientists who helped identify a family of proteins that connect cells and assist the immune system in attaching to its targets. The proteins, called integrins, are needed for cells to interact with each other to build complex structures in the body. They are also key to the process T cells undergo to recognize and attack cancer cells.
Awardees Richard O. Hynes, MA, PhD, distinguished professor of cancer research at Massachusetts Institute of Technology; Erkki Ruoslahti, MD, PhD, distinguished professor emeritus at Sanford Burnham Prebys Medical Discovery Institute, La Jolla, California; and Timothy A. Springer, PhD, professor of biological chemistry and molecular biology at Boston Children’s Hospital and Harvard Medical School, independently identified a cell-surface–associated protein that helps cells attach to the extracellular matrix.
“Many of the mysteries of how integrins work are only being discovered today,” Dr. Springer said in his acceptance remarks online.
The discoveries related to integrins have led to several clinical advances, including the development of drugs like the eyedrops lifitegrast, the biologic agent vedolizumab (made using integrins Springer discovered), and tirofiban, a medication used to hamper clotting in cardiovascular diseases.
A version of this article first appeared on Medscape.com.
Congenital cytomegalovirus declined in wake of COVID-19
Congenital cytomegalovirus cases declined significantly during the COVID-19 pandemic, compared with a period before the pandemic, based on data from nearly 20,000 newborns.
A study originated to explore racial and ethnic differences in congenital cytomegalovirus (cCMV) began in 2016, but was halted in April 2020 because of the COVID-19 pandemic, wrote Mark R. Schleiss, MD, of the University of Minnesota, Minneapolis, and colleagues. The study resumed for a period from August 2020 to December 2021, and the researchers compared data on cCMV before and during the pandemic. The prepandemic period included data from April 2016 to March 2020.
“We have been screening for congenital CMV infection in Minnesota for 6 years as a part of a multicenter collaborative study that I lead as the primary investigator,” Dr. Schleiss said in an interview. “Our efforts have contributed to the decision, vetted through the Minnesota Legislature and signed into law in 2021 (the “Vivian Act”), to begin universal screening for all newborns in Minnesota in 2023. In the context of this ongoing screening/surveillance study, it was important and scientifically very interesting to examine the impact of the COVID-19 pandemic on the risk of congenital CMV infection,” he explained.
The findings were published in a research letter in JAMA Network Open. A total of 15,697 newborns were screened before the pandemic and 4,222 were screened during the pandemic period at six hospitals. The majority of the mothers participating during the prepandemic and pandemic periods were non-Hispanic White (71% and 60%, respectively).
Overall, the percentage screened prevalence for cCMV was 79% in the prepandemic period and 21% during the pandemic, with rates of 4.5 per 1,000 and 1.4 per 1,000, respectively.
Although the highest percentage of cCMV cases occurred in newborns of mothers aged 25 years and older (86%), the prevalence was highest among newborns of mothers aged 24 years and younger (6.0 per 1,000). The prevalence of cCMV overall was higher in infants of non-Hispanic Black mothers vs. non-Hispanic White mothers, but not significantly different (5.1 per 1,000 vs. 4.6 per 1,000) and among second newborns vs. first newborns (6.0 vs. 3.2 per 1,000, respectively).
Factors related to COVID-19, including reduced day care attendance, behavioral changes, and mitigation measures at childcare facilities such as smaller classes and increased hand hygiene and disinfection may have contributed to this decrease in cCMV in the pandemic period, the researchers wrote in their discussion.
The comparable prevalence in newborns of non-Hispanic Black and White mothers contrasts with previous studies showing a higher prevalence in children of non-Hispanic Black mothers, the researchers noted in their discussion.
The study was limited by several factors, including the variation in time points for enrollment at different sites and the exclusion of families in the newborn nursery with positive COVID-19 results during the pandemic, they wrote. More research is needed on the potential effects of behavioral interventions to reduce CMV risk during pregnancy, as well as future CMV vaccination for childbearing-aged women and young children, they concluded.
However, the researchers were surprised by the impact of COVID-19 on the prevalence of cCMV, Dr. Schleiss said in an interview. “We have had the knowledge for many years that CMV infections in young women are commonly acquired through interactions with their toddlers. These interactions – sharing food, wiping drool and nasal discharge from the toddler’s nose, changing diapers, kissing the child on the mouth – can transmit CMV,” he said. In addition, toddlers may acquire CMV from group day care; the child then sheds CMV and transmits the virus to their pregnant mother, who then transmits the virus across the placenta, leading to cCMV infection in the newborn, Dr. Schleiss explained.
Although the researchers expected a decrease in CMV in the wake of closures of group day care, increased home schooling, decreased interactions among children, hygienic precautions, and social isolation, the decrease exceeded their expectations, said Dr. Schleiss. “Our previous work showed that in the 5-year period leading up to the pandemic, about one baby in every 200 births was born with CMV. Between August 2020 and December 2021, the number decreased to one baby in every 1,000 births,” a difference he and his team found striking.
The message from the study is that CMV can be prevented, said Dr. Schleiss. “Hygienic precautions during pregnancy had a big impact. Since congenital CMV infection is the most common congenital infection in the United States, and probably globally, that causes disabilities in children, the implications are highly significant,” he said. “The hygienic precautions we all have engaged in during the pandemic, such as masking, handwashing, and infection prevention behaviors, were almost certainly responsible for the reduction in CMV transmission, which in turn protected mothers and newborns from the potentially devastating effects of the CMV virus,” he noted.
Looking ahead, “Vaccines are moving forward in clinical trials that aim to confer immunity on young women of childbearing age to protect future pregnancies against transmission of CMV to the newborn infant; it would be very important to examine in future studies whether hygienic precautions would have the same impact as a potential vaccine,” Dr. Schleiss said. More research is needed to examine the effect of education of women about CMV transmission, he added. “We think it is very important to share this knowledge from our study with the pediatric community, since pediatricians can be important in counseling women about future pregnancies and the risks of CMV acquisition and transmission,” he noted.
Implications for other viruses
Although CMV poses minimal risk for healthy populations, irreversible complications for infants born with congenital CMV, especially hearing loss, are very concerning, said Catherine Haut, DNP, CPNP-AC/PC, a pediatric nurse practitioner in Rehoboth Beach, Del., in an interview.
“The study of viral transmission during a time of isolation, masking, and other mitigation procedures for COVID-19 assists in awareness that other viruses may also be limited with the use of these measures,” she said.
Dr. Haut was not surprised by the findings, given that CMV is transmitted primarily through direct contact with body fluids and that more than 50% of American adults have been infected by age 40, according to the Centers for Disease Control and Prevention, she said.
The take-home message for pediatricians, Dr. Haut said, is measures to prevent transmission of viral infection can yield significant positive health outcomes for the pediatric population; however, the effect of isolation, which has been associated with a higher rate of mental health problems, should not be ignored.
“Despite appropriate statistical analyses and presentation of findings in this study, the population sampled during the pandemic was less than 30% of the pre-COVID sampling, representing a study limitation,” and conducting research in a single state limits generalizability, Dr. Haut noted. “I agree with the authors that additional study is necessary to better understand prevention measures and apply these methods to reduce CMV transmission. Pursuit of CMV immunization opportunities is also needed,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Vaccine Program Office, the Minnesota Department of Health Newborn Screening Program, and the University of South Carolina Disability Research and Dissemination Center. Lead author Dr. Schleiss disclosed grants from the CDC, the National Institutes of Health, and the DRDC during the conduct of the study; he also disclosed receiving personal fees from Moderna, Sanofi, GlaxoSmithKline, and Merck unrelated to the study. Dr. Haut had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
Congenital cytomegalovirus cases declined significantly during the COVID-19 pandemic, compared with a period before the pandemic, based on data from nearly 20,000 newborns.
A study originated to explore racial and ethnic differences in congenital cytomegalovirus (cCMV) began in 2016, but was halted in April 2020 because of the COVID-19 pandemic, wrote Mark R. Schleiss, MD, of the University of Minnesota, Minneapolis, and colleagues. The study resumed for a period from August 2020 to December 2021, and the researchers compared data on cCMV before and during the pandemic. The prepandemic period included data from April 2016 to March 2020.
“We have been screening for congenital CMV infection in Minnesota for 6 years as a part of a multicenter collaborative study that I lead as the primary investigator,” Dr. Schleiss said in an interview. “Our efforts have contributed to the decision, vetted through the Minnesota Legislature and signed into law in 2021 (the “Vivian Act”), to begin universal screening for all newborns in Minnesota in 2023. In the context of this ongoing screening/surveillance study, it was important and scientifically very interesting to examine the impact of the COVID-19 pandemic on the risk of congenital CMV infection,” he explained.
The findings were published in a research letter in JAMA Network Open. A total of 15,697 newborns were screened before the pandemic and 4,222 were screened during the pandemic period at six hospitals. The majority of the mothers participating during the prepandemic and pandemic periods were non-Hispanic White (71% and 60%, respectively).
Overall, the percentage screened prevalence for cCMV was 79% in the prepandemic period and 21% during the pandemic, with rates of 4.5 per 1,000 and 1.4 per 1,000, respectively.
Although the highest percentage of cCMV cases occurred in newborns of mothers aged 25 years and older (86%), the prevalence was highest among newborns of mothers aged 24 years and younger (6.0 per 1,000). The prevalence of cCMV overall was higher in infants of non-Hispanic Black mothers vs. non-Hispanic White mothers, but not significantly different (5.1 per 1,000 vs. 4.6 per 1,000) and among second newborns vs. first newborns (6.0 vs. 3.2 per 1,000, respectively).
Factors related to COVID-19, including reduced day care attendance, behavioral changes, and mitigation measures at childcare facilities such as smaller classes and increased hand hygiene and disinfection may have contributed to this decrease in cCMV in the pandemic period, the researchers wrote in their discussion.
The comparable prevalence in newborns of non-Hispanic Black and White mothers contrasts with previous studies showing a higher prevalence in children of non-Hispanic Black mothers, the researchers noted in their discussion.
The study was limited by several factors, including the variation in time points for enrollment at different sites and the exclusion of families in the newborn nursery with positive COVID-19 results during the pandemic, they wrote. More research is needed on the potential effects of behavioral interventions to reduce CMV risk during pregnancy, as well as future CMV vaccination for childbearing-aged women and young children, they concluded.
However, the researchers were surprised by the impact of COVID-19 on the prevalence of cCMV, Dr. Schleiss said in an interview. “We have had the knowledge for many years that CMV infections in young women are commonly acquired through interactions with their toddlers. These interactions – sharing food, wiping drool and nasal discharge from the toddler’s nose, changing diapers, kissing the child on the mouth – can transmit CMV,” he said. In addition, toddlers may acquire CMV from group day care; the child then sheds CMV and transmits the virus to their pregnant mother, who then transmits the virus across the placenta, leading to cCMV infection in the newborn, Dr. Schleiss explained.
Although the researchers expected a decrease in CMV in the wake of closures of group day care, increased home schooling, decreased interactions among children, hygienic precautions, and social isolation, the decrease exceeded their expectations, said Dr. Schleiss. “Our previous work showed that in the 5-year period leading up to the pandemic, about one baby in every 200 births was born with CMV. Between August 2020 and December 2021, the number decreased to one baby in every 1,000 births,” a difference he and his team found striking.
The message from the study is that CMV can be prevented, said Dr. Schleiss. “Hygienic precautions during pregnancy had a big impact. Since congenital CMV infection is the most common congenital infection in the United States, and probably globally, that causes disabilities in children, the implications are highly significant,” he said. “The hygienic precautions we all have engaged in during the pandemic, such as masking, handwashing, and infection prevention behaviors, were almost certainly responsible for the reduction in CMV transmission, which in turn protected mothers and newborns from the potentially devastating effects of the CMV virus,” he noted.
Looking ahead, “Vaccines are moving forward in clinical trials that aim to confer immunity on young women of childbearing age to protect future pregnancies against transmission of CMV to the newborn infant; it would be very important to examine in future studies whether hygienic precautions would have the same impact as a potential vaccine,” Dr. Schleiss said. More research is needed to examine the effect of education of women about CMV transmission, he added. “We think it is very important to share this knowledge from our study with the pediatric community, since pediatricians can be important in counseling women about future pregnancies and the risks of CMV acquisition and transmission,” he noted.
Implications for other viruses
Although CMV poses minimal risk for healthy populations, irreversible complications for infants born with congenital CMV, especially hearing loss, are very concerning, said Catherine Haut, DNP, CPNP-AC/PC, a pediatric nurse practitioner in Rehoboth Beach, Del., in an interview.
“The study of viral transmission during a time of isolation, masking, and other mitigation procedures for COVID-19 assists in awareness that other viruses may also be limited with the use of these measures,” she said.
Dr. Haut was not surprised by the findings, given that CMV is transmitted primarily through direct contact with body fluids and that more than 50% of American adults have been infected by age 40, according to the Centers for Disease Control and Prevention, she said.
The take-home message for pediatricians, Dr. Haut said, is measures to prevent transmission of viral infection can yield significant positive health outcomes for the pediatric population; however, the effect of isolation, which has been associated with a higher rate of mental health problems, should not be ignored.
“Despite appropriate statistical analyses and presentation of findings in this study, the population sampled during the pandemic was less than 30% of the pre-COVID sampling, representing a study limitation,” and conducting research in a single state limits generalizability, Dr. Haut noted. “I agree with the authors that additional study is necessary to better understand prevention measures and apply these methods to reduce CMV transmission. Pursuit of CMV immunization opportunities is also needed,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Vaccine Program Office, the Minnesota Department of Health Newborn Screening Program, and the University of South Carolina Disability Research and Dissemination Center. Lead author Dr. Schleiss disclosed grants from the CDC, the National Institutes of Health, and the DRDC during the conduct of the study; he also disclosed receiving personal fees from Moderna, Sanofi, GlaxoSmithKline, and Merck unrelated to the study. Dr. Haut had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
Congenital cytomegalovirus cases declined significantly during the COVID-19 pandemic, compared with a period before the pandemic, based on data from nearly 20,000 newborns.
A study originated to explore racial and ethnic differences in congenital cytomegalovirus (cCMV) began in 2016, but was halted in April 2020 because of the COVID-19 pandemic, wrote Mark R. Schleiss, MD, of the University of Minnesota, Minneapolis, and colleagues. The study resumed for a period from August 2020 to December 2021, and the researchers compared data on cCMV before and during the pandemic. The prepandemic period included data from April 2016 to March 2020.
“We have been screening for congenital CMV infection in Minnesota for 6 years as a part of a multicenter collaborative study that I lead as the primary investigator,” Dr. Schleiss said in an interview. “Our efforts have contributed to the decision, vetted through the Minnesota Legislature and signed into law in 2021 (the “Vivian Act”), to begin universal screening for all newborns in Minnesota in 2023. In the context of this ongoing screening/surveillance study, it was important and scientifically very interesting to examine the impact of the COVID-19 pandemic on the risk of congenital CMV infection,” he explained.
The findings were published in a research letter in JAMA Network Open. A total of 15,697 newborns were screened before the pandemic and 4,222 were screened during the pandemic period at six hospitals. The majority of the mothers participating during the prepandemic and pandemic periods were non-Hispanic White (71% and 60%, respectively).
Overall, the percentage screened prevalence for cCMV was 79% in the prepandemic period and 21% during the pandemic, with rates of 4.5 per 1,000 and 1.4 per 1,000, respectively.
Although the highest percentage of cCMV cases occurred in newborns of mothers aged 25 years and older (86%), the prevalence was highest among newborns of mothers aged 24 years and younger (6.0 per 1,000). The prevalence of cCMV overall was higher in infants of non-Hispanic Black mothers vs. non-Hispanic White mothers, but not significantly different (5.1 per 1,000 vs. 4.6 per 1,000) and among second newborns vs. first newborns (6.0 vs. 3.2 per 1,000, respectively).
Factors related to COVID-19, including reduced day care attendance, behavioral changes, and mitigation measures at childcare facilities such as smaller classes and increased hand hygiene and disinfection may have contributed to this decrease in cCMV in the pandemic period, the researchers wrote in their discussion.
The comparable prevalence in newborns of non-Hispanic Black and White mothers contrasts with previous studies showing a higher prevalence in children of non-Hispanic Black mothers, the researchers noted in their discussion.
The study was limited by several factors, including the variation in time points for enrollment at different sites and the exclusion of families in the newborn nursery with positive COVID-19 results during the pandemic, they wrote. More research is needed on the potential effects of behavioral interventions to reduce CMV risk during pregnancy, as well as future CMV vaccination for childbearing-aged women and young children, they concluded.
However, the researchers were surprised by the impact of COVID-19 on the prevalence of cCMV, Dr. Schleiss said in an interview. “We have had the knowledge for many years that CMV infections in young women are commonly acquired through interactions with their toddlers. These interactions – sharing food, wiping drool and nasal discharge from the toddler’s nose, changing diapers, kissing the child on the mouth – can transmit CMV,” he said. In addition, toddlers may acquire CMV from group day care; the child then sheds CMV and transmits the virus to their pregnant mother, who then transmits the virus across the placenta, leading to cCMV infection in the newborn, Dr. Schleiss explained.
Although the researchers expected a decrease in CMV in the wake of closures of group day care, increased home schooling, decreased interactions among children, hygienic precautions, and social isolation, the decrease exceeded their expectations, said Dr. Schleiss. “Our previous work showed that in the 5-year period leading up to the pandemic, about one baby in every 200 births was born with CMV. Between August 2020 and December 2021, the number decreased to one baby in every 1,000 births,” a difference he and his team found striking.
The message from the study is that CMV can be prevented, said Dr. Schleiss. “Hygienic precautions during pregnancy had a big impact. Since congenital CMV infection is the most common congenital infection in the United States, and probably globally, that causes disabilities in children, the implications are highly significant,” he said. “The hygienic precautions we all have engaged in during the pandemic, such as masking, handwashing, and infection prevention behaviors, were almost certainly responsible for the reduction in CMV transmission, which in turn protected mothers and newborns from the potentially devastating effects of the CMV virus,” he noted.
Looking ahead, “Vaccines are moving forward in clinical trials that aim to confer immunity on young women of childbearing age to protect future pregnancies against transmission of CMV to the newborn infant; it would be very important to examine in future studies whether hygienic precautions would have the same impact as a potential vaccine,” Dr. Schleiss said. More research is needed to examine the effect of education of women about CMV transmission, he added. “We think it is very important to share this knowledge from our study with the pediatric community, since pediatricians can be important in counseling women about future pregnancies and the risks of CMV acquisition and transmission,” he noted.
Implications for other viruses
Although CMV poses minimal risk for healthy populations, irreversible complications for infants born with congenital CMV, especially hearing loss, are very concerning, said Catherine Haut, DNP, CPNP-AC/PC, a pediatric nurse practitioner in Rehoboth Beach, Del., in an interview.
“The study of viral transmission during a time of isolation, masking, and other mitigation procedures for COVID-19 assists in awareness that other viruses may also be limited with the use of these measures,” she said.
Dr. Haut was not surprised by the findings, given that CMV is transmitted primarily through direct contact with body fluids and that more than 50% of American adults have been infected by age 40, according to the Centers for Disease Control and Prevention, she said.
The take-home message for pediatricians, Dr. Haut said, is measures to prevent transmission of viral infection can yield significant positive health outcomes for the pediatric population; however, the effect of isolation, which has been associated with a higher rate of mental health problems, should not be ignored.
“Despite appropriate statistical analyses and presentation of findings in this study, the population sampled during the pandemic was less than 30% of the pre-COVID sampling, representing a study limitation,” and conducting research in a single state limits generalizability, Dr. Haut noted. “I agree with the authors that additional study is necessary to better understand prevention measures and apply these methods to reduce CMV transmission. Pursuit of CMV immunization opportunities is also needed,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Vaccine Program Office, the Minnesota Department of Health Newborn Screening Program, and the University of South Carolina Disability Research and Dissemination Center. Lead author Dr. Schleiss disclosed grants from the CDC, the National Institutes of Health, and the DRDC during the conduct of the study; he also disclosed receiving personal fees from Moderna, Sanofi, GlaxoSmithKline, and Merck unrelated to the study. Dr. Haut had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
FROM JAMA NETWORK OPEN




