User login
Risk factors for death from COVID-19 identified in Wuhan patients
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
WHO declares COVID-19 outbreak a pandemic
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
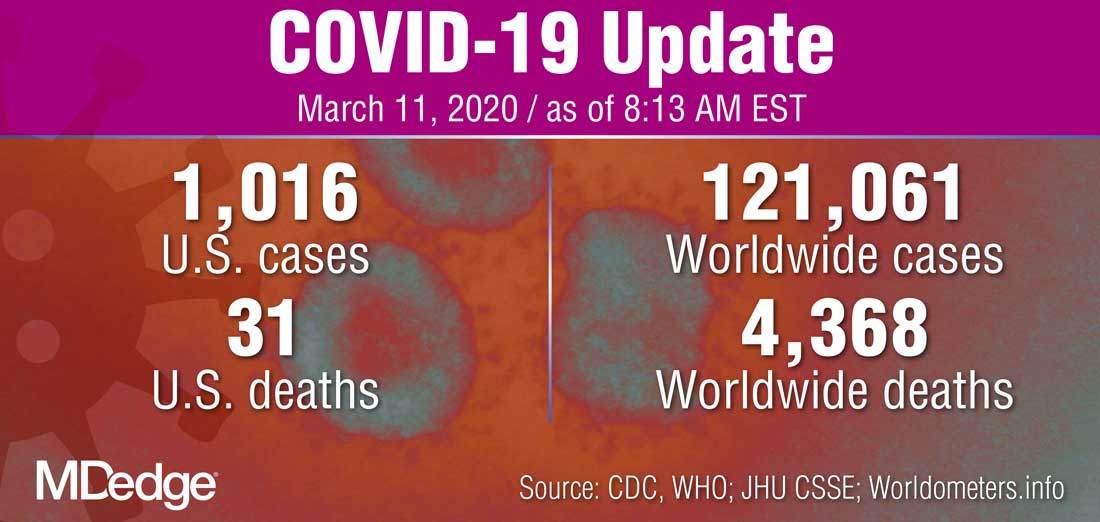
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
FDA broadens nintedanib interstitial lung disease indication
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
Managing children’s fear, anxiety in the age of COVID-19
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
COVID-19 update: Transmission 5% or less among close contacts
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
FROM CROI 2020
Know the 15% rule in scleroderma
MAUI, HAWAII – The 15% rule in scleroderma is a handy tool that raises awareness of the disease’s associated prevalence of various severe organ complications so clinicians can screen appropriately, Janet Pope, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
Dr. Pope and colleagues in the Canadian Scleroderma Research Group developed the 15% rule because they recognized that scleroderma is rare enough that most physicians practicing outside of a few specialized centers don’t see many affected patients. The systemic autoimmune disease is marked by numerous possible expressions of vascular inflammation and malfunction, fibrosis, and autoimmunity in different organ systems.
“A lot of clinicians do not know how common this stuff is,” according to Dr. Pope, professor of medicine at the University of Western Ontario and head of the division of rheumatology at St. Joseph’s Health Center in London, Ont.
Basically, the 15% rule holds that, at any given time, a patient with scleroderma has roughly a 15% chance – or one in six – of having any of an extensive array of severe organ complications. That means a 15% chance of having prevalent clinically significant pulmonary hypertension as defined by a systolic pulmonary artery pressure of 45 mm Hg or more on Doppler echocardiography, a 15% likelihood of interstitial lung disease or clinically significant pulmonary fibrosis as suggested by a forced vital capacity less than 70% of predicted, a 15% prevalence of Sjögren’s syndrome, a 15% likelihood of having pulmonary artery hypertension upon right heart catheterization, a 15% chance of inflammatory arthritis, and a one-in-six chance of having a myopathy or myositis. Also, diastolic dysfunction, 15%. Ditto symptomatic arrhythmias.
“It’s a good little rule of thumb,” Dr. Pope commented.
The odds of having a current digital ulcer on any given day? Again, about 15%. In addition, scleroderma patients have a 15% lifetime risk of developing a complicated digital ulcer requiring hospitalization and/or amputation, she continued.
And while the prevalence of scleroderma renal crisis in the overall population with scleroderma is low, at 3%, in the subgroup with diffuse cutaneous systemic sclerosis, it climbs to 12%-15%.
Every rule has its exceptions. The 15% rule doesn’t apply to Raynaud’s phenomenon, which is present in nearly all patients with scleroderma, nor to gastroesophageal reflux disease or dysphagia, present in roughly 80% of patients.
Dr. Pope and coinvestigators developed the 15% rule pertaining to the prevalence of serious organ complications in scleroderma by conducting a systematic review of 69 published studies, each including a minimum of 50 scleroderma patients. The detailed results of the systematic review have been published.
Dr. Pope reported receiving research grants from and/or serving as a consultant to more than a dozen pharmaceutical companies.
MAUI, HAWAII – The 15% rule in scleroderma is a handy tool that raises awareness of the disease’s associated prevalence of various severe organ complications so clinicians can screen appropriately, Janet Pope, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
Dr. Pope and colleagues in the Canadian Scleroderma Research Group developed the 15% rule because they recognized that scleroderma is rare enough that most physicians practicing outside of a few specialized centers don’t see many affected patients. The systemic autoimmune disease is marked by numerous possible expressions of vascular inflammation and malfunction, fibrosis, and autoimmunity in different organ systems.
“A lot of clinicians do not know how common this stuff is,” according to Dr. Pope, professor of medicine at the University of Western Ontario and head of the division of rheumatology at St. Joseph’s Health Center in London, Ont.
Basically, the 15% rule holds that, at any given time, a patient with scleroderma has roughly a 15% chance – or one in six – of having any of an extensive array of severe organ complications. That means a 15% chance of having prevalent clinically significant pulmonary hypertension as defined by a systolic pulmonary artery pressure of 45 mm Hg or more on Doppler echocardiography, a 15% likelihood of interstitial lung disease or clinically significant pulmonary fibrosis as suggested by a forced vital capacity less than 70% of predicted, a 15% prevalence of Sjögren’s syndrome, a 15% likelihood of having pulmonary artery hypertension upon right heart catheterization, a 15% chance of inflammatory arthritis, and a one-in-six chance of having a myopathy or myositis. Also, diastolic dysfunction, 15%. Ditto symptomatic arrhythmias.
“It’s a good little rule of thumb,” Dr. Pope commented.
The odds of having a current digital ulcer on any given day? Again, about 15%. In addition, scleroderma patients have a 15% lifetime risk of developing a complicated digital ulcer requiring hospitalization and/or amputation, she continued.
And while the prevalence of scleroderma renal crisis in the overall population with scleroderma is low, at 3%, in the subgroup with diffuse cutaneous systemic sclerosis, it climbs to 12%-15%.
Every rule has its exceptions. The 15% rule doesn’t apply to Raynaud’s phenomenon, which is present in nearly all patients with scleroderma, nor to gastroesophageal reflux disease or dysphagia, present in roughly 80% of patients.
Dr. Pope and coinvestigators developed the 15% rule pertaining to the prevalence of serious organ complications in scleroderma by conducting a systematic review of 69 published studies, each including a minimum of 50 scleroderma patients. The detailed results of the systematic review have been published.
Dr. Pope reported receiving research grants from and/or serving as a consultant to more than a dozen pharmaceutical companies.
MAUI, HAWAII – The 15% rule in scleroderma is a handy tool that raises awareness of the disease’s associated prevalence of various severe organ complications so clinicians can screen appropriately, Janet Pope, MD, said at the 2020 Rheumatology Winter Clinical Symposium.
Dr. Pope and colleagues in the Canadian Scleroderma Research Group developed the 15% rule because they recognized that scleroderma is rare enough that most physicians practicing outside of a few specialized centers don’t see many affected patients. The systemic autoimmune disease is marked by numerous possible expressions of vascular inflammation and malfunction, fibrosis, and autoimmunity in different organ systems.
“A lot of clinicians do not know how common this stuff is,” according to Dr. Pope, professor of medicine at the University of Western Ontario and head of the division of rheumatology at St. Joseph’s Health Center in London, Ont.
Basically, the 15% rule holds that, at any given time, a patient with scleroderma has roughly a 15% chance – or one in six – of having any of an extensive array of severe organ complications. That means a 15% chance of having prevalent clinically significant pulmonary hypertension as defined by a systolic pulmonary artery pressure of 45 mm Hg or more on Doppler echocardiography, a 15% likelihood of interstitial lung disease or clinically significant pulmonary fibrosis as suggested by a forced vital capacity less than 70% of predicted, a 15% prevalence of Sjögren’s syndrome, a 15% likelihood of having pulmonary artery hypertension upon right heart catheterization, a 15% chance of inflammatory arthritis, and a one-in-six chance of having a myopathy or myositis. Also, diastolic dysfunction, 15%. Ditto symptomatic arrhythmias.
“It’s a good little rule of thumb,” Dr. Pope commented.
The odds of having a current digital ulcer on any given day? Again, about 15%. In addition, scleroderma patients have a 15% lifetime risk of developing a complicated digital ulcer requiring hospitalization and/or amputation, she continued.
And while the prevalence of scleroderma renal crisis in the overall population with scleroderma is low, at 3%, in the subgroup with diffuse cutaneous systemic sclerosis, it climbs to 12%-15%.
Every rule has its exceptions. The 15% rule doesn’t apply to Raynaud’s phenomenon, which is present in nearly all patients with scleroderma, nor to gastroesophageal reflux disease or dysphagia, present in roughly 80% of patients.
Dr. Pope and coinvestigators developed the 15% rule pertaining to the prevalence of serious organ complications in scleroderma by conducting a systematic review of 69 published studies, each including a minimum of 50 scleroderma patients. The detailed results of the systematic review have been published.
Dr. Pope reported receiving research grants from and/or serving as a consultant to more than a dozen pharmaceutical companies.
REPORTING FROM RWCS 2020
Some infected patients could show COVID-19 symptoms after quarantine
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Some individuals who are infected with the novel coronavirus could become symptomatic after the active 14-day quarantine period.
Major finding: The median incubation period was 5.1 days, with 97.5% of patients developing symptoms within 11.5 days, implying that 101 of every 10,000 cases (99th percentile) would develop symptoms beyond the quarantine period.
Study details: Analysis of 181 confirmed COVID-19 cases identified outside of the outbreak epicenter, Wuhan, China.
Disclosures: The study was supported by the U.S. Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
Source: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi: 10.1101/2020.02.02.20020016.
New RA diagnosis prompts patients to quit smoking
Health care factors, such as type of health system and being newly diagnosed, rather than patient socioeconomic factors, were significant predictors of smoking cessation in patients with RA, according to findings published in Arthritis Care & Research.
Smoking is a known risk factor for poor outcomes in RA, but data on factors that predict smoking cessation in these patients are limited, wrote Maria Schletzbaum, a student in the MD-PhD program at the University of Wisconsin–Madison, and colleagues. “Further, most patients with RA are not aware of the associations between smoking and RA development and complications, although such knowledge could influence cessation attempts.”
To identify predictors of smoking cessation, the investigators reviewed the 2005-2016 electronic medical records for 3,577 adults aged 18 years or older and with at least two RA diagnosis codes. The records were from two health systems, one urban and one rural.
Overall, patients who were baseline smokers and who were new to rheumatology care were 60% more likely to quit smoking (adjusted odds ratio, 1.60). However, patients who were seropositive and baseline smokers were 43% less likely to quit (aOR, 0.57). Demographic factors, including age, race, and sex, were not significantly associated with smoking cessation.
“The observed increased likelihood of quitting in patients new to rheumatology care may partially be due to cessation following a new RA diagnosis, a phenomenon previously reported in RA and other chronic diseases,” the researchers noted. Notably, the significance of being new to rheumatology disappeared in an analysis controlling for health system, “potentially suggesting greater importance of system-level factors versus individual patient factors.”
In addition, patients in the rural community health system were 66% more likely to quit smoking, possibly because about half of the patients in that system were covered by the systems’ insurance, and therefore qualified for various smoking cessation interventions, they wrote.
The study population included 915 former smokers and 507 current smokers. Seropositivity was most common in current smokers (71%), followed by former smokers (64%) and never smokers (59%). The disinclination of seropositive patients to quit smoking may reflect greater smoking intensity, and these patients may need greater support, the researchers wrote.
The study findings were limited by several factors; for example, some differences in patient populations, such as education and income levels, were not measured, and there was a lack of complete information on cumulative smoking exposure. However, the results were strengthened by the large sample size and use of data from two centers and support national guidelines for health system interventions in smoking cessation for RA patients, they noted.
The study was funded in part by the Rheumatology Research Foundation, the University of Wisconsin Medical Scientist Training Program, and the University of Wisconsin Clinical and Translational Science Award. The authors did not report any financial conflicts of interest.
SOURCE: Schletzbaum M et al. Arthritis Car Res. 2020 Mar 3. doi: 10.1002/ACR.24154.
Health care factors, such as type of health system and being newly diagnosed, rather than patient socioeconomic factors, were significant predictors of smoking cessation in patients with RA, according to findings published in Arthritis Care & Research.
Smoking is a known risk factor for poor outcomes in RA, but data on factors that predict smoking cessation in these patients are limited, wrote Maria Schletzbaum, a student in the MD-PhD program at the University of Wisconsin–Madison, and colleagues. “Further, most patients with RA are not aware of the associations between smoking and RA development and complications, although such knowledge could influence cessation attempts.”
To identify predictors of smoking cessation, the investigators reviewed the 2005-2016 electronic medical records for 3,577 adults aged 18 years or older and with at least two RA diagnosis codes. The records were from two health systems, one urban and one rural.
Overall, patients who were baseline smokers and who were new to rheumatology care were 60% more likely to quit smoking (adjusted odds ratio, 1.60). However, patients who were seropositive and baseline smokers were 43% less likely to quit (aOR, 0.57). Demographic factors, including age, race, and sex, were not significantly associated with smoking cessation.
“The observed increased likelihood of quitting in patients new to rheumatology care may partially be due to cessation following a new RA diagnosis, a phenomenon previously reported in RA and other chronic diseases,” the researchers noted. Notably, the significance of being new to rheumatology disappeared in an analysis controlling for health system, “potentially suggesting greater importance of system-level factors versus individual patient factors.”
In addition, patients in the rural community health system were 66% more likely to quit smoking, possibly because about half of the patients in that system were covered by the systems’ insurance, and therefore qualified for various smoking cessation interventions, they wrote.
The study population included 915 former smokers and 507 current smokers. Seropositivity was most common in current smokers (71%), followed by former smokers (64%) and never smokers (59%). The disinclination of seropositive patients to quit smoking may reflect greater smoking intensity, and these patients may need greater support, the researchers wrote.
The study findings were limited by several factors; for example, some differences in patient populations, such as education and income levels, were not measured, and there was a lack of complete information on cumulative smoking exposure. However, the results were strengthened by the large sample size and use of data from two centers and support national guidelines for health system interventions in smoking cessation for RA patients, they noted.
The study was funded in part by the Rheumatology Research Foundation, the University of Wisconsin Medical Scientist Training Program, and the University of Wisconsin Clinical and Translational Science Award. The authors did not report any financial conflicts of interest.
SOURCE: Schletzbaum M et al. Arthritis Car Res. 2020 Mar 3. doi: 10.1002/ACR.24154.
Health care factors, such as type of health system and being newly diagnosed, rather than patient socioeconomic factors, were significant predictors of smoking cessation in patients with RA, according to findings published in Arthritis Care & Research.
Smoking is a known risk factor for poor outcomes in RA, but data on factors that predict smoking cessation in these patients are limited, wrote Maria Schletzbaum, a student in the MD-PhD program at the University of Wisconsin–Madison, and colleagues. “Further, most patients with RA are not aware of the associations between smoking and RA development and complications, although such knowledge could influence cessation attempts.”
To identify predictors of smoking cessation, the investigators reviewed the 2005-2016 electronic medical records for 3,577 adults aged 18 years or older and with at least two RA diagnosis codes. The records were from two health systems, one urban and one rural.
Overall, patients who were baseline smokers and who were new to rheumatology care were 60% more likely to quit smoking (adjusted odds ratio, 1.60). However, patients who were seropositive and baseline smokers were 43% less likely to quit (aOR, 0.57). Demographic factors, including age, race, and sex, were not significantly associated with smoking cessation.
“The observed increased likelihood of quitting in patients new to rheumatology care may partially be due to cessation following a new RA diagnosis, a phenomenon previously reported in RA and other chronic diseases,” the researchers noted. Notably, the significance of being new to rheumatology disappeared in an analysis controlling for health system, “potentially suggesting greater importance of system-level factors versus individual patient factors.”
In addition, patients in the rural community health system were 66% more likely to quit smoking, possibly because about half of the patients in that system were covered by the systems’ insurance, and therefore qualified for various smoking cessation interventions, they wrote.
The study population included 915 former smokers and 507 current smokers. Seropositivity was most common in current smokers (71%), followed by former smokers (64%) and never smokers (59%). The disinclination of seropositive patients to quit smoking may reflect greater smoking intensity, and these patients may need greater support, the researchers wrote.
The study findings were limited by several factors; for example, some differences in patient populations, such as education and income levels, were not measured, and there was a lack of complete information on cumulative smoking exposure. However, the results were strengthened by the large sample size and use of data from two centers and support national guidelines for health system interventions in smoking cessation for RA patients, they noted.
The study was funded in part by the Rheumatology Research Foundation, the University of Wisconsin Medical Scientist Training Program, and the University of Wisconsin Clinical and Translational Science Award. The authors did not report any financial conflicts of interest.
SOURCE: Schletzbaum M et al. Arthritis Car Res. 2020 Mar 3. doi: 10.1002/ACR.24154.
FROM ARTHRITIS CARE & RESEARCH
Flu activity declines again but remains high

Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.

Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.

Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
Novel coronavirus may cause environmental contamination through fecal shedding
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
FROM JAMA