User login
Resurgence of black lung among U.S. coal miners
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Advances in technology over the last century, as well as the exportation of many high exposure jobs, nearly eliminated lung diseases caused by occupational exposure to respirable dust (the pneumoconioses) in the United States. One such example of this near elimination is black lung, or coal workers' pneumoconiosis (CWP), following the 1969 Federal Coal Mine Health and Safety Act. The Act established permissible exposure limits to respirable dust, designed to prevent the most severe forms of CWP from occurring, and a national respiratory health screening program for underground coal miners. Between 1970 and the mid-1990s, disease prevalence plummeted from nearly 35% to less than 5% prevalence among longer tenured miners, and from 3% to less than 1% in miners with less than 10 years of mining tenure (Hall NB, et al. Curr Environ Health Rep. 2019;6[3]:137).
Many assumed that this was the last we'd hear of black lung - that the cases of disease existing in the 1990s were likely caused by exposures that occurred prior to the 1969 Act, and within a few years, no further cases would be detected. This appeared to be an entirely reasonable assumption in the 1990s given the 30 years of declining prevalence and the continuous technological advances designed to continue reductions in dust exposures. In fact, the precipitous decline in black lung was briefly viewed as a public health triumph, as the most severe forms appeared to be near eradication in the United States just 2 decades ago (Attfield MD, et al. Am J Public Health. 1992;82[7]:971; Attfield MD, et al. Am J Public Health. 1992;82[7]:964). However, what has since been observed is a strong and ongoing resurgence of the potentially deadly fibrotic interstitial disease starting in the early 2000s (Figure 1), with the most striking increase observed in the Central Appalachian states of Kentucky, Virginia, and West Virginia (Blackley DJ, et al. Am J Respir Crit Care Med. 2014;190[6]:708; Blackley DJ, et al. Am J Public Health. 2018;108[9]:1220).
Of great concern is the resurgence of complicated Black Lung (progressive massive fibrosis [PMF]), which is completely disabling and leads to premature mortality. The prevalence of PMF is higher today than when NIOSH started formally tracking the disease in the 1970s, especially among specific populations.
Since the mid-2000s, NIOSH and others have described the following(Hall NB, et al. Curr Environ Health Rep. 2019;6[3]:137):
· Increasing prevalence and severity of CWP both nationwide and specifically in Central Appalachia.
· Rapid progression of CWP.
· Increases in the frequency of lung transplantation for CWP.
· Severe disease among surface coal miners with no underground mining tenure.
· Increased severity of disease among former and retired miners.
· Hundreds of cases of PMF among coal miners seeking care at clinics in eastern Kentucky and southwestern Virginia.
· Increasing numbers of miners with PMF filing for federal black lung compensation.
· Radiologic and pathologic indications of increased respirable silica exposure among coal miners.
· Premature mortality in miners diagnosed with CWP.
· Underutilization of a secondary prevention worker removal program designed to reduce the exposure of miners with disease.
· Former miners with severe disease describing extreme pressure to operate. outside of applicable protective federal standards in order to increase productivity
In our surveillance work, we have talked to many miners who, after having months or years' worth of extensive workups for pneumonia, sarcoidosis, lung cancer, and/or diseases other than the pneumoconioses, have eventually learned that they actually had dust-induced lung disease attributable to their work. Additionally, through our evaluation of the transplantation data, it has become clear that dust-related lung disease is likely underreported or underrecognized among those receiving lung transplants. Finally, through analysis of mortality data, it is apparent that CWP is also underreported as a cause of death among miners with black lung. We mention these points to emphasize how important it is to document a full occupational history for proper diagnoses, early intervention, and improved public health information to inform primary and secondary disease prevention efforts.
Resources for clinicians
CWP is most commonly identified using plain posterior-anterior chest radiography and presence/severity of fibrotic change is described using an international standard established by the International Labour Office (International Labour Office. Guidelines for the use of the ILO international classification of radiographs of pneumoconioses. Geneva: International Labour Office; 2011). In the United States, NIOSH operates the B Reader Training and Certification Program, which offers a free self-study syllabus, https://www.cdc.gov/niosh/topics/chestradiography/breader.html, and in-person training courses on occasion, to assist physicians in learning and demonstrating continuous competency in classifying chest radiographs of dust-exposed workers according to the ILO Standards (Halldin CN, et al. J Occup Environ Med. 2019;61[12]:1045). The B Reader Program and ILO Standards are currently undergoing a decade-long revision process where both will feature digitally acquired chest radiograph images. This process should be fully complete in the following months.
To educate miners, mine operators, and others about the risks of respirable dust, NIOSH produced an educational video, Faces of Black Lung, in 2008 that featured two miners in their 50s and 60s who had complicated Black Lung. Because of the resurgence of disease and particularly severe cases being identified among much younger miners, NIOSH recently released an updated version of the video, Faces of Black Lung II, where three Kentucky underground miners, ages 39, 42, and 48, describe the incredible disability and quality of life lost due to a disease caused by gross overexposure of respirable coal mine dust.
Unfortunately, the 42-year-old miner died from complications stemming from Black Lung less than a year after filming his part in the video, and the other two miners have been advised to be evaluated for lung transplantation. We hope that these men's stories will help younger miners relate to the risks of respirable coal mine dust and help others understand the severity of disease as all three of these men struggled to breathe just describing their day to day tasks.
Parting message
No one should ever have to consider a lung transplant at the age of 40 because they went to work attempting to provide for their family. No one should ever be faced with end-of-life planning while their kids are in grade school because of a disease they acquired at work. Respirable coal mine dust is the only cause of black lung, and the coal mining industry has the necessary technology and tools to prevent harmful exposures to respirable dust, and, together with miners, must successfully and consistently implement dust suppression controls. There is no cure for black lung; it's irreversible and can be first recognized and continue to progress even after a miner has left exposure. However, early identification and appropriate intervention can prevent progression to the most disabling manifestations. The role of the clinician is to be part of the early identification of black lung through including CWP in the differential diagnosis for unusual or unexpected respiratory illness in otherwise healthy primarily working aged miners. The public health community must continue to monitor disease prevalence in working populations and implement policies and recommendations to support the efforts of those on the frontline - the miners, industry, and health-care workers.
The Energy Information Agency projects that coal will continue to be a substantial source of U.S. energy production and consumption well into the mid- to late-century. Unfortunately, Black Lung has made a resurgence and is killing miners, and each of us has a role to play in eliminating it once and for all. We will continue to carry out our mandate to screen working coal miners for respiratory disease; however, given the continued contraction of the coal mining industry, it's much more likely for cases of disease to be recognized in the clinic setting. Therefore, we reiterate our previous plea to clinicians: when identifying an individual with interstitial fibrosis consider their full occupational history.
Dr. Halldin and Dr. Laney are from the Surveillance Branch, Respiratory Health Division, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Morgantown, WV.
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Advances in technology over the last century, as well as the exportation of many high exposure jobs, nearly eliminated lung diseases caused by occupational exposure to respirable dust (the pneumoconioses) in the United States. One such example of this near elimination is black lung, or coal workers' pneumoconiosis (CWP), following the 1969 Federal Coal Mine Health and Safety Act. The Act established permissible exposure limits to respirable dust, designed to prevent the most severe forms of CWP from occurring, and a national respiratory health screening program for underground coal miners. Between 1970 and the mid-1990s, disease prevalence plummeted from nearly 35% to less than 5% prevalence among longer tenured miners, and from 3% to less than 1% in miners with less than 10 years of mining tenure (Hall NB, et al. Curr Environ Health Rep. 2019;6[3]:137).
Many assumed that this was the last we'd hear of black lung - that the cases of disease existing in the 1990s were likely caused by exposures that occurred prior to the 1969 Act, and within a few years, no further cases would be detected. This appeared to be an entirely reasonable assumption in the 1990s given the 30 years of declining prevalence and the continuous technological advances designed to continue reductions in dust exposures. In fact, the precipitous decline in black lung was briefly viewed as a public health triumph, as the most severe forms appeared to be near eradication in the United States just 2 decades ago (Attfield MD, et al. Am J Public Health. 1992;82[7]:971; Attfield MD, et al. Am J Public Health. 1992;82[7]:964). However, what has since been observed is a strong and ongoing resurgence of the potentially deadly fibrotic interstitial disease starting in the early 2000s (Figure 1), with the most striking increase observed in the Central Appalachian states of Kentucky, Virginia, and West Virginia (Blackley DJ, et al. Am J Respir Crit Care Med. 2014;190[6]:708; Blackley DJ, et al. Am J Public Health. 2018;108[9]:1220).
Of great concern is the resurgence of complicated Black Lung (progressive massive fibrosis [PMF]), which is completely disabling and leads to premature mortality. The prevalence of PMF is higher today than when NIOSH started formally tracking the disease in the 1970s, especially among specific populations.
Since the mid-2000s, NIOSH and others have described the following(Hall NB, et al. Curr Environ Health Rep. 2019;6[3]:137):
· Increasing prevalence and severity of CWP both nationwide and specifically in Central Appalachia.
· Rapid progression of CWP.
· Increases in the frequency of lung transplantation for CWP.
· Severe disease among surface coal miners with no underground mining tenure.
· Increased severity of disease among former and retired miners.
· Hundreds of cases of PMF among coal miners seeking care at clinics in eastern Kentucky and southwestern Virginia.
· Increasing numbers of miners with PMF filing for federal black lung compensation.
· Radiologic and pathologic indications of increased respirable silica exposure among coal miners.
· Premature mortality in miners diagnosed with CWP.
· Underutilization of a secondary prevention worker removal program designed to reduce the exposure of miners with disease.
· Former miners with severe disease describing extreme pressure to operate. outside of applicable protective federal standards in order to increase productivity
In our surveillance work, we have talked to many miners who, after having months or years' worth of extensive workups for pneumonia, sarcoidosis, lung cancer, and/or diseases other than the pneumoconioses, have eventually learned that they actually had dust-induced lung disease attributable to their work. Additionally, through our evaluation of the transplantation data, it has become clear that dust-related lung disease is likely underreported or underrecognized among those receiving lung transplants. Finally, through analysis of mortality data, it is apparent that CWP is also underreported as a cause of death among miners with black lung. We mention these points to emphasize how important it is to document a full occupational history for proper diagnoses, early intervention, and improved public health information to inform primary and secondary disease prevention efforts.
Resources for clinicians
CWP is most commonly identified using plain posterior-anterior chest radiography and presence/severity of fibrotic change is described using an international standard established by the International Labour Office (International Labour Office. Guidelines for the use of the ILO international classification of radiographs of pneumoconioses. Geneva: International Labour Office; 2011). In the United States, NIOSH operates the B Reader Training and Certification Program, which offers a free self-study syllabus, https://www.cdc.gov/niosh/topics/chestradiography/breader.html, and in-person training courses on occasion, to assist physicians in learning and demonstrating continuous competency in classifying chest radiographs of dust-exposed workers according to the ILO Standards (Halldin CN, et al. J Occup Environ Med. 2019;61[12]:1045). The B Reader Program and ILO Standards are currently undergoing a decade-long revision process where both will feature digitally acquired chest radiograph images. This process should be fully complete in the following months.
To educate miners, mine operators, and others about the risks of respirable dust, NIOSH produced an educational video, Faces of Black Lung, in 2008 that featured two miners in their 50s and 60s who had complicated Black Lung. Because of the resurgence of disease and particularly severe cases being identified among much younger miners, NIOSH recently released an updated version of the video, Faces of Black Lung II, where three Kentucky underground miners, ages 39, 42, and 48, describe the incredible disability and quality of life lost due to a disease caused by gross overexposure of respirable coal mine dust.
Unfortunately, the 42-year-old miner died from complications stemming from Black Lung less than a year after filming his part in the video, and the other two miners have been advised to be evaluated for lung transplantation. We hope that these men's stories will help younger miners relate to the risks of respirable coal mine dust and help others understand the severity of disease as all three of these men struggled to breathe just describing their day to day tasks.
Parting message
No one should ever have to consider a lung transplant at the age of 40 because they went to work attempting to provide for their family. No one should ever be faced with end-of-life planning while their kids are in grade school because of a disease they acquired at work. Respirable coal mine dust is the only cause of black lung, and the coal mining industry has the necessary technology and tools to prevent harmful exposures to respirable dust, and, together with miners, must successfully and consistently implement dust suppression controls. There is no cure for black lung; it's irreversible and can be first recognized and continue to progress even after a miner has left exposure. However, early identification and appropriate intervention can prevent progression to the most disabling manifestations. The role of the clinician is to be part of the early identification of black lung through including CWP in the differential diagnosis for unusual or unexpected respiratory illness in otherwise healthy primarily working aged miners. The public health community must continue to monitor disease prevalence in working populations and implement policies and recommendations to support the efforts of those on the frontline - the miners, industry, and health-care workers.
The Energy Information Agency projects that coal will continue to be a substantial source of U.S. energy production and consumption well into the mid- to late-century. Unfortunately, Black Lung has made a resurgence and is killing miners, and each of us has a role to play in eliminating it once and for all. We will continue to carry out our mandate to screen working coal miners for respiratory disease; however, given the continued contraction of the coal mining industry, it's much more likely for cases of disease to be recognized in the clinic setting. Therefore, we reiterate our previous plea to clinicians: when identifying an individual with interstitial fibrosis consider their full occupational history.
Dr. Halldin and Dr. Laney are from the Surveillance Branch, Respiratory Health Division, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Morgantown, WV.
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Advances in technology over the last century, as well as the exportation of many high exposure jobs, nearly eliminated lung diseases caused by occupational exposure to respirable dust (the pneumoconioses) in the United States. One such example of this near elimination is black lung, or coal workers' pneumoconiosis (CWP), following the 1969 Federal Coal Mine Health and Safety Act. The Act established permissible exposure limits to respirable dust, designed to prevent the most severe forms of CWP from occurring, and a national respiratory health screening program for underground coal miners. Between 1970 and the mid-1990s, disease prevalence plummeted from nearly 35% to less than 5% prevalence among longer tenured miners, and from 3% to less than 1% in miners with less than 10 years of mining tenure (Hall NB, et al. Curr Environ Health Rep. 2019;6[3]:137).
Many assumed that this was the last we'd hear of black lung - that the cases of disease existing in the 1990s were likely caused by exposures that occurred prior to the 1969 Act, and within a few years, no further cases would be detected. This appeared to be an entirely reasonable assumption in the 1990s given the 30 years of declining prevalence and the continuous technological advances designed to continue reductions in dust exposures. In fact, the precipitous decline in black lung was briefly viewed as a public health triumph, as the most severe forms appeared to be near eradication in the United States just 2 decades ago (Attfield MD, et al. Am J Public Health. 1992;82[7]:971; Attfield MD, et al. Am J Public Health. 1992;82[7]:964). However, what has since been observed is a strong and ongoing resurgence of the potentially deadly fibrotic interstitial disease starting in the early 2000s (Figure 1), with the most striking increase observed in the Central Appalachian states of Kentucky, Virginia, and West Virginia (Blackley DJ, et al. Am J Respir Crit Care Med. 2014;190[6]:708; Blackley DJ, et al. Am J Public Health. 2018;108[9]:1220).
Of great concern is the resurgence of complicated Black Lung (progressive massive fibrosis [PMF]), which is completely disabling and leads to premature mortality. The prevalence of PMF is higher today than when NIOSH started formally tracking the disease in the 1970s, especially among specific populations.
Since the mid-2000s, NIOSH and others have described the following(Hall NB, et al. Curr Environ Health Rep. 2019;6[3]:137):
· Increasing prevalence and severity of CWP both nationwide and specifically in Central Appalachia.
· Rapid progression of CWP.
· Increases in the frequency of lung transplantation for CWP.
· Severe disease among surface coal miners with no underground mining tenure.
· Increased severity of disease among former and retired miners.
· Hundreds of cases of PMF among coal miners seeking care at clinics in eastern Kentucky and southwestern Virginia.
· Increasing numbers of miners with PMF filing for federal black lung compensation.
· Radiologic and pathologic indications of increased respirable silica exposure among coal miners.
· Premature mortality in miners diagnosed with CWP.
· Underutilization of a secondary prevention worker removal program designed to reduce the exposure of miners with disease.
· Former miners with severe disease describing extreme pressure to operate. outside of applicable protective federal standards in order to increase productivity
In our surveillance work, we have talked to many miners who, after having months or years' worth of extensive workups for pneumonia, sarcoidosis, lung cancer, and/or diseases other than the pneumoconioses, have eventually learned that they actually had dust-induced lung disease attributable to their work. Additionally, through our evaluation of the transplantation data, it has become clear that dust-related lung disease is likely underreported or underrecognized among those receiving lung transplants. Finally, through analysis of mortality data, it is apparent that CWP is also underreported as a cause of death among miners with black lung. We mention these points to emphasize how important it is to document a full occupational history for proper diagnoses, early intervention, and improved public health information to inform primary and secondary disease prevention efforts.
Resources for clinicians
CWP is most commonly identified using plain posterior-anterior chest radiography and presence/severity of fibrotic change is described using an international standard established by the International Labour Office (International Labour Office. Guidelines for the use of the ILO international classification of radiographs of pneumoconioses. Geneva: International Labour Office; 2011). In the United States, NIOSH operates the B Reader Training and Certification Program, which offers a free self-study syllabus, https://www.cdc.gov/niosh/topics/chestradiography/breader.html, and in-person training courses on occasion, to assist physicians in learning and demonstrating continuous competency in classifying chest radiographs of dust-exposed workers according to the ILO Standards (Halldin CN, et al. J Occup Environ Med. 2019;61[12]:1045). The B Reader Program and ILO Standards are currently undergoing a decade-long revision process where both will feature digitally acquired chest radiograph images. This process should be fully complete in the following months.
To educate miners, mine operators, and others about the risks of respirable dust, NIOSH produced an educational video, Faces of Black Lung, in 2008 that featured two miners in their 50s and 60s who had complicated Black Lung. Because of the resurgence of disease and particularly severe cases being identified among much younger miners, NIOSH recently released an updated version of the video, Faces of Black Lung II, where three Kentucky underground miners, ages 39, 42, and 48, describe the incredible disability and quality of life lost due to a disease caused by gross overexposure of respirable coal mine dust.
Unfortunately, the 42-year-old miner died from complications stemming from Black Lung less than a year after filming his part in the video, and the other two miners have been advised to be evaluated for lung transplantation. We hope that these men's stories will help younger miners relate to the risks of respirable coal mine dust and help others understand the severity of disease as all three of these men struggled to breathe just describing their day to day tasks.
Parting message
No one should ever have to consider a lung transplant at the age of 40 because they went to work attempting to provide for their family. No one should ever be faced with end-of-life planning while their kids are in grade school because of a disease they acquired at work. Respirable coal mine dust is the only cause of black lung, and the coal mining industry has the necessary technology and tools to prevent harmful exposures to respirable dust, and, together with miners, must successfully and consistently implement dust suppression controls. There is no cure for black lung; it's irreversible and can be first recognized and continue to progress even after a miner has left exposure. However, early identification and appropriate intervention can prevent progression to the most disabling manifestations. The role of the clinician is to be part of the early identification of black lung through including CWP in the differential diagnosis for unusual or unexpected respiratory illness in otherwise healthy primarily working aged miners. The public health community must continue to monitor disease prevalence in working populations and implement policies and recommendations to support the efforts of those on the frontline - the miners, industry, and health-care workers.
The Energy Information Agency projects that coal will continue to be a substantial source of U.S. energy production and consumption well into the mid- to late-century. Unfortunately, Black Lung has made a resurgence and is killing miners, and each of us has a role to play in eliminating it once and for all. We will continue to carry out our mandate to screen working coal miners for respiratory disease; however, given the continued contraction of the coal mining industry, it's much more likely for cases of disease to be recognized in the clinic setting. Therefore, we reiterate our previous plea to clinicians: when identifying an individual with interstitial fibrosis consider their full occupational history.
Dr. Halldin and Dr. Laney are from the Surveillance Branch, Respiratory Health Division, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Morgantown, WV.
Stopping smoking allows healthy lung cells to proliferate
New research results reinforce the benefits of quitting smoking.
Not only does it stop further damage to the lungs, it appears that it also allows new, , say researchers.
The findings were published online in Nature (2020 Jan 29. doi: 10.1038/s41586-020-1961-1).
The team performed whole-genome sequencing on healthy airway cells collected (during a bronchoscopy for clinical indications) from current smokers and ex-smokers, as well as from adult never-smokers and children.
The investigators found, as expected, that the cells from current and ex-smokers had a far higher mutational burden than those of never-smokers and children, including an increased number of “driver” mutations, which increase the potential of cells to become cancerous.
However, they also found that in ex-smokers – but not in current smokers – up to 40% of the cells were near normal, with far less genetic damage and a low risk of developing cancer.
“People who have smoked heavily for 30, 40 or more years often say to me that it’s too late to stop smoking – the damage is already done,” commented senior author Peter J. Campbell, PhD, Cancer Genome Project, Wellcome Trust Sanger Institute, Hinxton, England.
“What is so exciting about our study is that it shows that it’s never too late to quit. Some of the people in our study had smoked more than 15,000 packs of cigarettes over their life, but within a few years of quitting, many of the cells lining their airways showed no evidence of damage from tobacco,” he said. The comments appear in a press release issued by Cancer Research UK, which partly funded the study.
This study has “broadened our understanding of the effects of tobacco smoke on normal epithelial cells in the human lung,” Gerd P. Pfeifer, PhD, at the Center for Epigenetics, Van Andel Institute, Grand Rapids, Michigan, writes in an accompanying comment.
“It has shed light on how the protective effect of smoking cessation plays out at the molecular level in human lung tissue and raises many interesting questions worthy of future investigation,” he added.
‘Important public health message’
Joint senior author Sam M. Janes, PhD, Lungs for Living Research Center, UCL Respiratory, University College London, added that the study has “an important public health message.
“Stopping smoking at any age does not just slow the accumulation of further damage but could reawaken cells unharmed by past lifestyle choices,” he said.
“Further research into this process could help to understand how these cells protect against cancer and could potentially lead to new avenues of research into anticancer therapeutics,” Dr. James added.
In an interview, Dr. Campbell said that the team would next like to try “to find where this reservoir of normal cells hides out while the patient is smoking. We have some ideas from mouse models and we think, by adapting the methods we used in this study, we will be able to test that hypothesis directly.”
He continued: “If we can find this stem cell niche, then we can study the biology of the cells living in there and what makes them expand when a patient stops smoking.
“Once we understand that biology, we can think about therapies to target that population of cells in beneficial ways.”
Dr. Campbell concluded that they are “a long way away yet, but the toolkit exists for getting there.”
Tobacco and mutagenesis
In their article, the team notes that the model explaining how tobacco exposure causes lung cancer centers on the notion that the 60-plus carcinogens in cigarette smoke directly cause mutagenesis, which combines with the indirect effects of inflammation, immune suppression, and infection to lead to cancer.
However, this does not explain why individuals who stop smoking in middle age or earlier “avoid most of the risk of tobacco-associated lung cancer.”
They questioned the relationship between tobacco and mutagenesis. For two people who smoke the same number of cigarettes over their lifetime, the observation that the person with longer duration of cessation has a lower risk for lung cancer is difficult to explain if carcinogenesis is induced exclusively by an increase in the mutational burden, they noted.
To investigate further, the team set out to examine the “landscape” of somatic mutations in normal bronchial epithelium. They recruited 16 individuals: three children, four never-smokers, six ex-smokers, and three current smokers.
All the participants underwent bronchoscopy for clinical indications. Samples of airway epithelium were obtained from biopsies or brushings of main or secondary bronchi.
The researchers performed whole-genome sequencing of 632 colonies derived from single bronchial epithelial cells. In addition, cells from squamous cell carcinoma or carcinoma in situ from three of the patients were sequenced.
Cells show different mutational burdens
The results showed there was “considerable heterogeneity” in mutational burden both between patients and in individual patients.
Moreover, single-base substitutions increased significantly with age, at an estimated rate of 22 per cell per year (P = 10–8). In addition, previous and current smoking substantially increased the substitution burden by an estimated 2,330 per cell in ex-smokers and 5,300 per cell in current smokers.
The team was surprised to find that smoking also increased the variability of the mutational burden from cell to cell, “even within the same individual.”
They calculated that, even between cells from a small biopsy sample of normal airway, the standard deviation in mutational burden was 2,350 per cell in ex-smokers and 2,100 per cell in current smokers, but only 140 per cell in children and 290 per cell in adult never-smokers (P less than 10–16 for within-subject heterogeneity).
Between individuals, the mean substitution burden was 1,200 per cell in ex-smokers, 1,260 per cell in current smokers, and 90 per cell for nonsmokers (P = 10–8 for heterogeneity).
Driver mutations were also more common in individuals who had a history of smoking. In those persons, they were seen in at least 25% of cells vs. 4%-14% of cells from adult never-smokers and none of the cells from children.
It was calculated that current smokers had a 2.1-fold increase in the number of driver mutations per cell in comparison with never-smokers (P = .04).
In addition, the number of driver mutations per cell increased 1.5-fold with every decade of life (P = .004) and twofold for every 5,000 extra somatic mutations per cell (P = .0003).
However, the team also found that some patients among the ex-smokers and current smokers had cells with a near-normal mutational burden, similar to that seen for never-smokers of the equivalent age.
Although these cells were rare in current smokers, their relative frequency was, the team reports, an average fourfold higher in ex-smokers and accounted for between 20% and 40% of all cells studied.
Further analysis showed that these near-normal cells had less damage from tobacco-specific mutational processes than other cells and that they had longer telomeres.
“Two points remain unclear: how these cells have avoided the high rates of mutations that are exhibited by neighbouring cells, and why this particular population of cells expands after smoking cessation,” the team writes.
They argue that the presence of longer telomeres suggests they are “recent descendants of quiescent stem cells,” which have been found in mice but “remain elusive” in human lungs.
“The apparent expansion of the near-normal cells could represent the expected physiology of a two-compartment model in which relatively short-lived proliferative progenitors are slowly replenished from a pool of quiescent stem cells, but the progenitors are more exposed to tobacco carcinogens,” they suggest.
“Only in ex-smokers would the difference in mutagenic environment be sufficient to distinguish newly produced progenitors from long-term occupants of the bronchial epithelial surface,” they add.
However, in his commentary, Dr. Pfeifer highlights that a “potential caveat” of the study is the small number of individuals (n = 16) from whom cells were taken.
In addition, Dr. Pfeifer notes that the “lack of knowledge” about the suggested “long-lived stem cells and information about the longevity of the different cell types in the human lung make it difficult to explain what occurred in the ex-smokers’ cells with few mutations.”
The study was supported by a Cancer Research UK Grand Challenge Award and the Wellcome Trust. Dr. Campbell and Dr. Janes are Wellcome Trust senior clinical fellows. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
New research results reinforce the benefits of quitting smoking.
Not only does it stop further damage to the lungs, it appears that it also allows new, , say researchers.
The findings were published online in Nature (2020 Jan 29. doi: 10.1038/s41586-020-1961-1).
The team performed whole-genome sequencing on healthy airway cells collected (during a bronchoscopy for clinical indications) from current smokers and ex-smokers, as well as from adult never-smokers and children.
The investigators found, as expected, that the cells from current and ex-smokers had a far higher mutational burden than those of never-smokers and children, including an increased number of “driver” mutations, which increase the potential of cells to become cancerous.
However, they also found that in ex-smokers – but not in current smokers – up to 40% of the cells were near normal, with far less genetic damage and a low risk of developing cancer.
“People who have smoked heavily for 30, 40 or more years often say to me that it’s too late to stop smoking – the damage is already done,” commented senior author Peter J. Campbell, PhD, Cancer Genome Project, Wellcome Trust Sanger Institute, Hinxton, England.
“What is so exciting about our study is that it shows that it’s never too late to quit. Some of the people in our study had smoked more than 15,000 packs of cigarettes over their life, but within a few years of quitting, many of the cells lining their airways showed no evidence of damage from tobacco,” he said. The comments appear in a press release issued by Cancer Research UK, which partly funded the study.
This study has “broadened our understanding of the effects of tobacco smoke on normal epithelial cells in the human lung,” Gerd P. Pfeifer, PhD, at the Center for Epigenetics, Van Andel Institute, Grand Rapids, Michigan, writes in an accompanying comment.
“It has shed light on how the protective effect of smoking cessation plays out at the molecular level in human lung tissue and raises many interesting questions worthy of future investigation,” he added.
‘Important public health message’
Joint senior author Sam M. Janes, PhD, Lungs for Living Research Center, UCL Respiratory, University College London, added that the study has “an important public health message.
“Stopping smoking at any age does not just slow the accumulation of further damage but could reawaken cells unharmed by past lifestyle choices,” he said.
“Further research into this process could help to understand how these cells protect against cancer and could potentially lead to new avenues of research into anticancer therapeutics,” Dr. James added.
In an interview, Dr. Campbell said that the team would next like to try “to find where this reservoir of normal cells hides out while the patient is smoking. We have some ideas from mouse models and we think, by adapting the methods we used in this study, we will be able to test that hypothesis directly.”
He continued: “If we can find this stem cell niche, then we can study the biology of the cells living in there and what makes them expand when a patient stops smoking.
“Once we understand that biology, we can think about therapies to target that population of cells in beneficial ways.”
Dr. Campbell concluded that they are “a long way away yet, but the toolkit exists for getting there.”
Tobacco and mutagenesis
In their article, the team notes that the model explaining how tobacco exposure causes lung cancer centers on the notion that the 60-plus carcinogens in cigarette smoke directly cause mutagenesis, which combines with the indirect effects of inflammation, immune suppression, and infection to lead to cancer.
However, this does not explain why individuals who stop smoking in middle age or earlier “avoid most of the risk of tobacco-associated lung cancer.”
They questioned the relationship between tobacco and mutagenesis. For two people who smoke the same number of cigarettes over their lifetime, the observation that the person with longer duration of cessation has a lower risk for lung cancer is difficult to explain if carcinogenesis is induced exclusively by an increase in the mutational burden, they noted.
To investigate further, the team set out to examine the “landscape” of somatic mutations in normal bronchial epithelium. They recruited 16 individuals: three children, four never-smokers, six ex-smokers, and three current smokers.
All the participants underwent bronchoscopy for clinical indications. Samples of airway epithelium were obtained from biopsies or brushings of main or secondary bronchi.
The researchers performed whole-genome sequencing of 632 colonies derived from single bronchial epithelial cells. In addition, cells from squamous cell carcinoma or carcinoma in situ from three of the patients were sequenced.
Cells show different mutational burdens
The results showed there was “considerable heterogeneity” in mutational burden both between patients and in individual patients.
Moreover, single-base substitutions increased significantly with age, at an estimated rate of 22 per cell per year (P = 10–8). In addition, previous and current smoking substantially increased the substitution burden by an estimated 2,330 per cell in ex-smokers and 5,300 per cell in current smokers.
The team was surprised to find that smoking also increased the variability of the mutational burden from cell to cell, “even within the same individual.”
They calculated that, even between cells from a small biopsy sample of normal airway, the standard deviation in mutational burden was 2,350 per cell in ex-smokers and 2,100 per cell in current smokers, but only 140 per cell in children and 290 per cell in adult never-smokers (P less than 10–16 for within-subject heterogeneity).
Between individuals, the mean substitution burden was 1,200 per cell in ex-smokers, 1,260 per cell in current smokers, and 90 per cell for nonsmokers (P = 10–8 for heterogeneity).
Driver mutations were also more common in individuals who had a history of smoking. In those persons, they were seen in at least 25% of cells vs. 4%-14% of cells from adult never-smokers and none of the cells from children.
It was calculated that current smokers had a 2.1-fold increase in the number of driver mutations per cell in comparison with never-smokers (P = .04).
In addition, the number of driver mutations per cell increased 1.5-fold with every decade of life (P = .004) and twofold for every 5,000 extra somatic mutations per cell (P = .0003).
However, the team also found that some patients among the ex-smokers and current smokers had cells with a near-normal mutational burden, similar to that seen for never-smokers of the equivalent age.
Although these cells were rare in current smokers, their relative frequency was, the team reports, an average fourfold higher in ex-smokers and accounted for between 20% and 40% of all cells studied.
Further analysis showed that these near-normal cells had less damage from tobacco-specific mutational processes than other cells and that they had longer telomeres.
“Two points remain unclear: how these cells have avoided the high rates of mutations that are exhibited by neighbouring cells, and why this particular population of cells expands after smoking cessation,” the team writes.
They argue that the presence of longer telomeres suggests they are “recent descendants of quiescent stem cells,” which have been found in mice but “remain elusive” in human lungs.
“The apparent expansion of the near-normal cells could represent the expected physiology of a two-compartment model in which relatively short-lived proliferative progenitors are slowly replenished from a pool of quiescent stem cells, but the progenitors are more exposed to tobacco carcinogens,” they suggest.
“Only in ex-smokers would the difference in mutagenic environment be sufficient to distinguish newly produced progenitors from long-term occupants of the bronchial epithelial surface,” they add.
However, in his commentary, Dr. Pfeifer highlights that a “potential caveat” of the study is the small number of individuals (n = 16) from whom cells were taken.
In addition, Dr. Pfeifer notes that the “lack of knowledge” about the suggested “long-lived stem cells and information about the longevity of the different cell types in the human lung make it difficult to explain what occurred in the ex-smokers’ cells with few mutations.”
The study was supported by a Cancer Research UK Grand Challenge Award and the Wellcome Trust. Dr. Campbell and Dr. Janes are Wellcome Trust senior clinical fellows. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
New research results reinforce the benefits of quitting smoking.
Not only does it stop further damage to the lungs, it appears that it also allows new, , say researchers.
The findings were published online in Nature (2020 Jan 29. doi: 10.1038/s41586-020-1961-1).
The team performed whole-genome sequencing on healthy airway cells collected (during a bronchoscopy for clinical indications) from current smokers and ex-smokers, as well as from adult never-smokers and children.
The investigators found, as expected, that the cells from current and ex-smokers had a far higher mutational burden than those of never-smokers and children, including an increased number of “driver” mutations, which increase the potential of cells to become cancerous.
However, they also found that in ex-smokers – but not in current smokers – up to 40% of the cells were near normal, with far less genetic damage and a low risk of developing cancer.
“People who have smoked heavily for 30, 40 or more years often say to me that it’s too late to stop smoking – the damage is already done,” commented senior author Peter J. Campbell, PhD, Cancer Genome Project, Wellcome Trust Sanger Institute, Hinxton, England.
“What is so exciting about our study is that it shows that it’s never too late to quit. Some of the people in our study had smoked more than 15,000 packs of cigarettes over their life, but within a few years of quitting, many of the cells lining their airways showed no evidence of damage from tobacco,” he said. The comments appear in a press release issued by Cancer Research UK, which partly funded the study.
This study has “broadened our understanding of the effects of tobacco smoke on normal epithelial cells in the human lung,” Gerd P. Pfeifer, PhD, at the Center for Epigenetics, Van Andel Institute, Grand Rapids, Michigan, writes in an accompanying comment.
“It has shed light on how the protective effect of smoking cessation plays out at the molecular level in human lung tissue and raises many interesting questions worthy of future investigation,” he added.
‘Important public health message’
Joint senior author Sam M. Janes, PhD, Lungs for Living Research Center, UCL Respiratory, University College London, added that the study has “an important public health message.
“Stopping smoking at any age does not just slow the accumulation of further damage but could reawaken cells unharmed by past lifestyle choices,” he said.
“Further research into this process could help to understand how these cells protect against cancer and could potentially lead to new avenues of research into anticancer therapeutics,” Dr. James added.
In an interview, Dr. Campbell said that the team would next like to try “to find where this reservoir of normal cells hides out while the patient is smoking. We have some ideas from mouse models and we think, by adapting the methods we used in this study, we will be able to test that hypothesis directly.”
He continued: “If we can find this stem cell niche, then we can study the biology of the cells living in there and what makes them expand when a patient stops smoking.
“Once we understand that biology, we can think about therapies to target that population of cells in beneficial ways.”
Dr. Campbell concluded that they are “a long way away yet, but the toolkit exists for getting there.”
Tobacco and mutagenesis
In their article, the team notes that the model explaining how tobacco exposure causes lung cancer centers on the notion that the 60-plus carcinogens in cigarette smoke directly cause mutagenesis, which combines with the indirect effects of inflammation, immune suppression, and infection to lead to cancer.
However, this does not explain why individuals who stop smoking in middle age or earlier “avoid most of the risk of tobacco-associated lung cancer.”
They questioned the relationship between tobacco and mutagenesis. For two people who smoke the same number of cigarettes over their lifetime, the observation that the person with longer duration of cessation has a lower risk for lung cancer is difficult to explain if carcinogenesis is induced exclusively by an increase in the mutational burden, they noted.
To investigate further, the team set out to examine the “landscape” of somatic mutations in normal bronchial epithelium. They recruited 16 individuals: three children, four never-smokers, six ex-smokers, and three current smokers.
All the participants underwent bronchoscopy for clinical indications. Samples of airway epithelium were obtained from biopsies or brushings of main or secondary bronchi.
The researchers performed whole-genome sequencing of 632 colonies derived from single bronchial epithelial cells. In addition, cells from squamous cell carcinoma or carcinoma in situ from three of the patients were sequenced.
Cells show different mutational burdens
The results showed there was “considerable heterogeneity” in mutational burden both between patients and in individual patients.
Moreover, single-base substitutions increased significantly with age, at an estimated rate of 22 per cell per year (P = 10–8). In addition, previous and current smoking substantially increased the substitution burden by an estimated 2,330 per cell in ex-smokers and 5,300 per cell in current smokers.
The team was surprised to find that smoking also increased the variability of the mutational burden from cell to cell, “even within the same individual.”
They calculated that, even between cells from a small biopsy sample of normal airway, the standard deviation in mutational burden was 2,350 per cell in ex-smokers and 2,100 per cell in current smokers, but only 140 per cell in children and 290 per cell in adult never-smokers (P less than 10–16 for within-subject heterogeneity).
Between individuals, the mean substitution burden was 1,200 per cell in ex-smokers, 1,260 per cell in current smokers, and 90 per cell for nonsmokers (P = 10–8 for heterogeneity).
Driver mutations were also more common in individuals who had a history of smoking. In those persons, they were seen in at least 25% of cells vs. 4%-14% of cells from adult never-smokers and none of the cells from children.
It was calculated that current smokers had a 2.1-fold increase in the number of driver mutations per cell in comparison with never-smokers (P = .04).
In addition, the number of driver mutations per cell increased 1.5-fold with every decade of life (P = .004) and twofold for every 5,000 extra somatic mutations per cell (P = .0003).
However, the team also found that some patients among the ex-smokers and current smokers had cells with a near-normal mutational burden, similar to that seen for never-smokers of the equivalent age.
Although these cells were rare in current smokers, their relative frequency was, the team reports, an average fourfold higher in ex-smokers and accounted for between 20% and 40% of all cells studied.
Further analysis showed that these near-normal cells had less damage from tobacco-specific mutational processes than other cells and that they had longer telomeres.
“Two points remain unclear: how these cells have avoided the high rates of mutations that are exhibited by neighbouring cells, and why this particular population of cells expands after smoking cessation,” the team writes.
They argue that the presence of longer telomeres suggests they are “recent descendants of quiescent stem cells,” which have been found in mice but “remain elusive” in human lungs.
“The apparent expansion of the near-normal cells could represent the expected physiology of a two-compartment model in which relatively short-lived proliferative progenitors are slowly replenished from a pool of quiescent stem cells, but the progenitors are more exposed to tobacco carcinogens,” they suggest.
“Only in ex-smokers would the difference in mutagenic environment be sufficient to distinguish newly produced progenitors from long-term occupants of the bronchial epithelial surface,” they add.
However, in his commentary, Dr. Pfeifer highlights that a “potential caveat” of the study is the small number of individuals (n = 16) from whom cells were taken.
In addition, Dr. Pfeifer notes that the “lack of knowledge” about the suggested “long-lived stem cells and information about the longevity of the different cell types in the human lung make it difficult to explain what occurred in the ex-smokers’ cells with few mutations.”
The study was supported by a Cancer Research UK Grand Challenge Award and the Wellcome Trust. Dr. Campbell and Dr. Janes are Wellcome Trust senior clinical fellows. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
FROM NATURE
Medicare study evaluates impact of U.S. Hospital Readmissions Reduction Program
Research offers evidence against calls to curtail the program
Among Medicare beneficiaries admitted to the hospital between 2008 and 2016, there was an increase in postdischarge 30-day mortality for patients with heart failure, but not for those with acute myocardial infarction or pneumonia.
The finding comes from an effort to evaluate the use of services soon after discharge for conditions targeted in the U.S. Hospital Readmissions Reduction Program (HRRP), and patients’ outcomes.
“The announcement and implementation of the HRRP were associated with a reduction in readmissions within 30 days of discharge for heart failure, acute myocardial infarction, and pneumonia, as shown by a decrease in the overall national rate of readmissions,” first author Rohan Khera, MD, and colleagues wrote in a study published online Jan. 15, 2020, in the British Medical Journal (doi:10.1136/bmj.l6831).
“Concerns existed that pressures to reduce readmissions had led to the evolution of care patterns that may have adverse consequences through reducing access to care in appropriate settings. Therefore, determining whether patients who are seen in acute care settings, but not admitted to hospital, experience an increased risk of mortality is essential.”
Dr. Khera, a cardiologist at the University of Texas Southwestern Medical Center, Dallas, and colleagues limited the analysis to Medicare claims data from patients who were admitted to the hospital with heart failure, acute myocardial infarction (MI), or pneumonia between 2008 and 2016. Key outcomes of interest were: (1) postdischarge 30-day mortality; and (2) acute care utilization in inpatient units, observation units, and the ED during the postdischarge period.
During the study period there were 3,772,924 hospital admissions for heart failure, 1,570,113 for acute MI, and 3,131,162 for pneumonia. The greatest number of readmissions within 30 days of discharge was for heart failure patients (22.5%), followed by acute MI (17.5%), and pneumonia (17.2%).
The overall rates of observation stays were 1.7% for heart failure, 2.6% for acute MI, and 1.4% for pneumonia, while the overall rates of emergency department visits were 6.4% for heart failure, 6.8% for acute MI, and 6.3% for pneumonia. Cumulatively, about one-third of all admissions – 30.7% for heart failure, 26.9% for acute MI, and 24.8% for pneumonia – received postdischarge care in any acute care setting.
Dr. Khera and colleagues found that overall postdischarge 30-day mortality was 8.7% for heart failure, 7.3% for acute MI, and 8.4% for pneumonia. At the same time, postdischarge 30-day mortality was higher in patients with readmissions (13.2% for heart failure, 12.7% for acute MI, and 15.3% for pneumonia), compared with those who had observation stays (4.5% for heart failure, 2.7% for acute MI, and 4.6% for pneumonia), emergency department visits (9.7% for heart failure, 8.8% for acute MI, and 7.8% for pneumonia), or no postdischarge acute care (7.2% for heart failure, 6.0% for acute MI, and 6.9% for pneumonia). Risk adjusted mortality increased annually by 0.05% only for heart failure, while it decreased by 0.06% for acute MI, and did not significantly change for pneumonia.
“The study strongly suggests that the HRRP did not lead to harm through inappropriate triage of patients at high risk to observation units and the emergency department, and therefore provides evidence against calls to curtail the program owing to this theoretical concern (see JAMA 2018;320:2539-41),” the researchers concluded.
They acknowledged certain limitations of the study, including the fact that they were “unable to identify patterns of acute care during the index hospital admission that would be associated with a higher rate of postdischarge acute care in observation units and emergency departments and whether these visits represented avenues for planned postdischarge follow-up care. Moreover, the proportion of these care encounters that were preventable remains poorly understood.”
Dr. Khera disclosed that he is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. His coauthors reported having numerous disclosures.
SOURCE: Khera et al. BMJ 2020;368:l6831.
Research offers evidence against calls to curtail the program
Research offers evidence against calls to curtail the program
Among Medicare beneficiaries admitted to the hospital between 2008 and 2016, there was an increase in postdischarge 30-day mortality for patients with heart failure, but not for those with acute myocardial infarction or pneumonia.
The finding comes from an effort to evaluate the use of services soon after discharge for conditions targeted in the U.S. Hospital Readmissions Reduction Program (HRRP), and patients’ outcomes.
“The announcement and implementation of the HRRP were associated with a reduction in readmissions within 30 days of discharge for heart failure, acute myocardial infarction, and pneumonia, as shown by a decrease in the overall national rate of readmissions,” first author Rohan Khera, MD, and colleagues wrote in a study published online Jan. 15, 2020, in the British Medical Journal (doi:10.1136/bmj.l6831).
“Concerns existed that pressures to reduce readmissions had led to the evolution of care patterns that may have adverse consequences through reducing access to care in appropriate settings. Therefore, determining whether patients who are seen in acute care settings, but not admitted to hospital, experience an increased risk of mortality is essential.”
Dr. Khera, a cardiologist at the University of Texas Southwestern Medical Center, Dallas, and colleagues limited the analysis to Medicare claims data from patients who were admitted to the hospital with heart failure, acute myocardial infarction (MI), or pneumonia between 2008 and 2016. Key outcomes of interest were: (1) postdischarge 30-day mortality; and (2) acute care utilization in inpatient units, observation units, and the ED during the postdischarge period.
During the study period there were 3,772,924 hospital admissions for heart failure, 1,570,113 for acute MI, and 3,131,162 for pneumonia. The greatest number of readmissions within 30 days of discharge was for heart failure patients (22.5%), followed by acute MI (17.5%), and pneumonia (17.2%).
The overall rates of observation stays were 1.7% for heart failure, 2.6% for acute MI, and 1.4% for pneumonia, while the overall rates of emergency department visits were 6.4% for heart failure, 6.8% for acute MI, and 6.3% for pneumonia. Cumulatively, about one-third of all admissions – 30.7% for heart failure, 26.9% for acute MI, and 24.8% for pneumonia – received postdischarge care in any acute care setting.
Dr. Khera and colleagues found that overall postdischarge 30-day mortality was 8.7% for heart failure, 7.3% for acute MI, and 8.4% for pneumonia. At the same time, postdischarge 30-day mortality was higher in patients with readmissions (13.2% for heart failure, 12.7% for acute MI, and 15.3% for pneumonia), compared with those who had observation stays (4.5% for heart failure, 2.7% for acute MI, and 4.6% for pneumonia), emergency department visits (9.7% for heart failure, 8.8% for acute MI, and 7.8% for pneumonia), or no postdischarge acute care (7.2% for heart failure, 6.0% for acute MI, and 6.9% for pneumonia). Risk adjusted mortality increased annually by 0.05% only for heart failure, while it decreased by 0.06% for acute MI, and did not significantly change for pneumonia.
“The study strongly suggests that the HRRP did not lead to harm through inappropriate triage of patients at high risk to observation units and the emergency department, and therefore provides evidence against calls to curtail the program owing to this theoretical concern (see JAMA 2018;320:2539-41),” the researchers concluded.
They acknowledged certain limitations of the study, including the fact that they were “unable to identify patterns of acute care during the index hospital admission that would be associated with a higher rate of postdischarge acute care in observation units and emergency departments and whether these visits represented avenues for planned postdischarge follow-up care. Moreover, the proportion of these care encounters that were preventable remains poorly understood.”
Dr. Khera disclosed that he is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. His coauthors reported having numerous disclosures.
SOURCE: Khera et al. BMJ 2020;368:l6831.
Among Medicare beneficiaries admitted to the hospital between 2008 and 2016, there was an increase in postdischarge 30-day mortality for patients with heart failure, but not for those with acute myocardial infarction or pneumonia.
The finding comes from an effort to evaluate the use of services soon after discharge for conditions targeted in the U.S. Hospital Readmissions Reduction Program (HRRP), and patients’ outcomes.
“The announcement and implementation of the HRRP were associated with a reduction in readmissions within 30 days of discharge for heart failure, acute myocardial infarction, and pneumonia, as shown by a decrease in the overall national rate of readmissions,” first author Rohan Khera, MD, and colleagues wrote in a study published online Jan. 15, 2020, in the British Medical Journal (doi:10.1136/bmj.l6831).
“Concerns existed that pressures to reduce readmissions had led to the evolution of care patterns that may have adverse consequences through reducing access to care in appropriate settings. Therefore, determining whether patients who are seen in acute care settings, but not admitted to hospital, experience an increased risk of mortality is essential.”
Dr. Khera, a cardiologist at the University of Texas Southwestern Medical Center, Dallas, and colleagues limited the analysis to Medicare claims data from patients who were admitted to the hospital with heart failure, acute myocardial infarction (MI), or pneumonia between 2008 and 2016. Key outcomes of interest were: (1) postdischarge 30-day mortality; and (2) acute care utilization in inpatient units, observation units, and the ED during the postdischarge period.
During the study period there were 3,772,924 hospital admissions for heart failure, 1,570,113 for acute MI, and 3,131,162 for pneumonia. The greatest number of readmissions within 30 days of discharge was for heart failure patients (22.5%), followed by acute MI (17.5%), and pneumonia (17.2%).
The overall rates of observation stays were 1.7% for heart failure, 2.6% for acute MI, and 1.4% for pneumonia, while the overall rates of emergency department visits were 6.4% for heart failure, 6.8% for acute MI, and 6.3% for pneumonia. Cumulatively, about one-third of all admissions – 30.7% for heart failure, 26.9% for acute MI, and 24.8% for pneumonia – received postdischarge care in any acute care setting.
Dr. Khera and colleagues found that overall postdischarge 30-day mortality was 8.7% for heart failure, 7.3% for acute MI, and 8.4% for pneumonia. At the same time, postdischarge 30-day mortality was higher in patients with readmissions (13.2% for heart failure, 12.7% for acute MI, and 15.3% for pneumonia), compared with those who had observation stays (4.5% for heart failure, 2.7% for acute MI, and 4.6% for pneumonia), emergency department visits (9.7% for heart failure, 8.8% for acute MI, and 7.8% for pneumonia), or no postdischarge acute care (7.2% for heart failure, 6.0% for acute MI, and 6.9% for pneumonia). Risk adjusted mortality increased annually by 0.05% only for heart failure, while it decreased by 0.06% for acute MI, and did not significantly change for pneumonia.
“The study strongly suggests that the HRRP did not lead to harm through inappropriate triage of patients at high risk to observation units and the emergency department, and therefore provides evidence against calls to curtail the program owing to this theoretical concern (see JAMA 2018;320:2539-41),” the researchers concluded.
They acknowledged certain limitations of the study, including the fact that they were “unable to identify patterns of acute care during the index hospital admission that would be associated with a higher rate of postdischarge acute care in observation units and emergency departments and whether these visits represented avenues for planned postdischarge follow-up care. Moreover, the proportion of these care encounters that were preventable remains poorly understood.”
Dr. Khera disclosed that he is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. His coauthors reported having numerous disclosures.
SOURCE: Khera et al. BMJ 2020;368:l6831.
FROM BMJ
Flu activity increases for third straight week
For the second time during the 2019-2020 flu season, activity measures have climbed into noteworthy territory.

The proportion of outpatient visits for influenza-like illness (ILI) reached its highest December level, 7.1%, since 2003 and then dropped for 2 weeks. Three weeks of increases since then, however, have the outpatient-visit rate at 6.7% for the week ending Feb. 1, 2020, the Centers for Disease Control and Prevention reported. The baseline rate for the United States is 2.4%.
That rate of 6.7% is already above the highest rates recorded in eight of the last nine flu seasons, and another increase could mean a second, separate trip above 7.0% in the 2019-2020 season – something that has not occurred since national tracking began in 1997, CDC data show.
Those same data also show that,
Another important measure on the rise, the proportion of respiratory specimens testing positive for influenza, reached a new high for the season, 29.8%, during the week of Feb. 1, the CDC’s influenza division said.
Tests at clinical laboratories also show that predominance is continuing to switch from type B (45.6%) to type A (54.4%), the influenza division noted. Overall predominance for the season, however, continues to favor type B, 59.3% to 40.7%.
The percentage of deaths caused by pneumonia and influenza, which passed the threshold for epidemic of 7.2% back in early January, has been trending downward for the last 3 weeks and was 7.1% as of Feb. 1, according to the influenza division.
ILI-related deaths among children continue to remain high, with a total count of 78 for the season after another 10 deaths were reported during the week ending Feb. 1, the CDC reported. Comparable numbers for the last three seasons are 44 (2018-2019), 97 (2017-2018), and 35 (2016-2017).
The CDC estimates put the total number of ILIs at around 22 million for the season so far, leading to 210,000 hospitalizations. The agency said that it expects to release estimates of vaccine effectiveness later this month.
For the second time during the 2019-2020 flu season, activity measures have climbed into noteworthy territory.

The proportion of outpatient visits for influenza-like illness (ILI) reached its highest December level, 7.1%, since 2003 and then dropped for 2 weeks. Three weeks of increases since then, however, have the outpatient-visit rate at 6.7% for the week ending Feb. 1, 2020, the Centers for Disease Control and Prevention reported. The baseline rate for the United States is 2.4%.
That rate of 6.7% is already above the highest rates recorded in eight of the last nine flu seasons, and another increase could mean a second, separate trip above 7.0% in the 2019-2020 season – something that has not occurred since national tracking began in 1997, CDC data show.
Those same data also show that,
Another important measure on the rise, the proportion of respiratory specimens testing positive for influenza, reached a new high for the season, 29.8%, during the week of Feb. 1, the CDC’s influenza division said.
Tests at clinical laboratories also show that predominance is continuing to switch from type B (45.6%) to type A (54.4%), the influenza division noted. Overall predominance for the season, however, continues to favor type B, 59.3% to 40.7%.
The percentage of deaths caused by pneumonia and influenza, which passed the threshold for epidemic of 7.2% back in early January, has been trending downward for the last 3 weeks and was 7.1% as of Feb. 1, according to the influenza division.
ILI-related deaths among children continue to remain high, with a total count of 78 for the season after another 10 deaths were reported during the week ending Feb. 1, the CDC reported. Comparable numbers for the last three seasons are 44 (2018-2019), 97 (2017-2018), and 35 (2016-2017).
The CDC estimates put the total number of ILIs at around 22 million for the season so far, leading to 210,000 hospitalizations. The agency said that it expects to release estimates of vaccine effectiveness later this month.
For the second time during the 2019-2020 flu season, activity measures have climbed into noteworthy territory.

The proportion of outpatient visits for influenza-like illness (ILI) reached its highest December level, 7.1%, since 2003 and then dropped for 2 weeks. Three weeks of increases since then, however, have the outpatient-visit rate at 6.7% for the week ending Feb. 1, 2020, the Centers for Disease Control and Prevention reported. The baseline rate for the United States is 2.4%.
That rate of 6.7% is already above the highest rates recorded in eight of the last nine flu seasons, and another increase could mean a second, separate trip above 7.0% in the 2019-2020 season – something that has not occurred since national tracking began in 1997, CDC data show.
Those same data also show that,
Another important measure on the rise, the proportion of respiratory specimens testing positive for influenza, reached a new high for the season, 29.8%, during the week of Feb. 1, the CDC’s influenza division said.
Tests at clinical laboratories also show that predominance is continuing to switch from type B (45.6%) to type A (54.4%), the influenza division noted. Overall predominance for the season, however, continues to favor type B, 59.3% to 40.7%.
The percentage of deaths caused by pneumonia and influenza, which passed the threshold for epidemic of 7.2% back in early January, has been trending downward for the last 3 weeks and was 7.1% as of Feb. 1, according to the influenza division.
ILI-related deaths among children continue to remain high, with a total count of 78 for the season after another 10 deaths were reported during the week ending Feb. 1, the CDC reported. Comparable numbers for the last three seasons are 44 (2018-2019), 97 (2017-2018), and 35 (2016-2017).
The CDC estimates put the total number of ILIs at around 22 million for the season so far, leading to 210,000 hospitalizations. The agency said that it expects to release estimates of vaccine effectiveness later this month.
Remdesivir under study as treatment for novel coronavirus
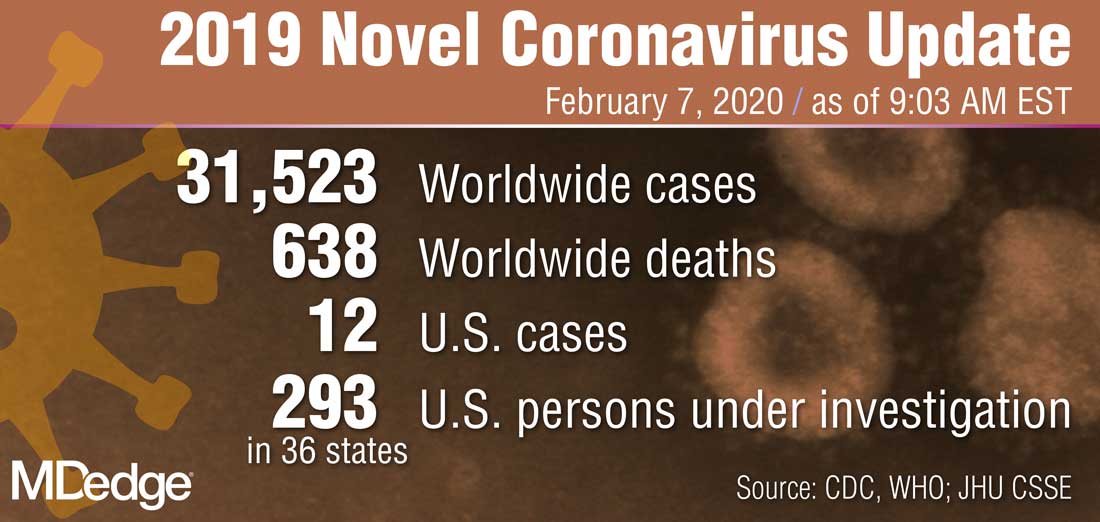
“What they’re looking at is the effect of this drug -- either the drug plus standard of care versus standard of care alone,” Anthony S. Fauci, MD, reported Feb. 7 during a press briefing held by members of President Trump’s Coronavirus Task Force. “I think pretty soon we are going to get a definitive answer, whether one of these among several drugs works.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases, added that several organizations and individual investigators are developing vaccines for 2019-nCoV. In one such effort, the National Institutes of Health is working with Moderna Inc. to develop a vaccine built on a messenger RNA platform. “One of the first steps is to successfully get that [novel coronavirus] gene and insert it into the messenger RNA platform successfully and allow it to express proteins,” Dr. Fauci explained. “We’ve succeeded in that. The next [step] is to put it in a mouse animal model to induce immunogenicity, and to get the company to make [gold nanoparticle] products. All of those have been successfully implemented. There have been no glitches so far. If that continues, we will be in Phase 1 trials in people within the next two-and-a-half months.”
In another development on the same day, Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, announced that Heath & Human Services issued an interim final rule to amend foreign quarantine regulations in the wake of the public health threat posed by the 2019-nCoV. “This will enable CDC to collect certain contact information data regarding airline passengers and crew when they arrive from other countries. . .and may be exposed to communicable disease,” Dr. Redfield said. “This action is part of our multi-layered approach to the U.S. response and demonstrates our commitment to take all necessary actions to protect the American people.”
According to Alex Azar, secretary of Health and Human Services, and chair of President Trump’s Coronavirus Task Force, there are 12 confirmed cases of the novel coronavirus in the United States, including two cases of transmission to people who had not recently been in China. “Although the virus represents a potentially very serious public health threat, and we expect to continue seeing more cases here, the immediate risk to the American public is low at this time,” Mr. Azar said. “We are working as quickly as possible on the many unanswered questions about this virus. That includes exactly how it spreads, how deadly it is, whether it’s commonly transmitted by patients who are not yet displaying symptoms, and other issues.”
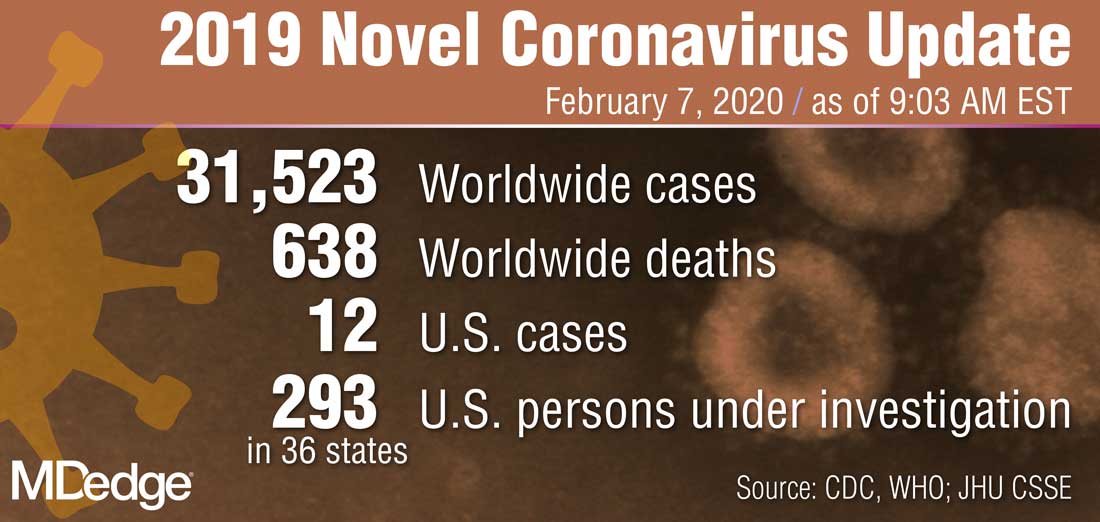
“What they’re looking at is the effect of this drug -- either the drug plus standard of care versus standard of care alone,” Anthony S. Fauci, MD, reported Feb. 7 during a press briefing held by members of President Trump’s Coronavirus Task Force. “I think pretty soon we are going to get a definitive answer, whether one of these among several drugs works.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases, added that several organizations and individual investigators are developing vaccines for 2019-nCoV. In one such effort, the National Institutes of Health is working with Moderna Inc. to develop a vaccine built on a messenger RNA platform. “One of the first steps is to successfully get that [novel coronavirus] gene and insert it into the messenger RNA platform successfully and allow it to express proteins,” Dr. Fauci explained. “We’ve succeeded in that. The next [step] is to put it in a mouse animal model to induce immunogenicity, and to get the company to make [gold nanoparticle] products. All of those have been successfully implemented. There have been no glitches so far. If that continues, we will be in Phase 1 trials in people within the next two-and-a-half months.”
In another development on the same day, Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, announced that Heath & Human Services issued an interim final rule to amend foreign quarantine regulations in the wake of the public health threat posed by the 2019-nCoV. “This will enable CDC to collect certain contact information data regarding airline passengers and crew when they arrive from other countries. . .and may be exposed to communicable disease,” Dr. Redfield said. “This action is part of our multi-layered approach to the U.S. response and demonstrates our commitment to take all necessary actions to protect the American people.”
According to Alex Azar, secretary of Health and Human Services, and chair of President Trump’s Coronavirus Task Force, there are 12 confirmed cases of the novel coronavirus in the United States, including two cases of transmission to people who had not recently been in China. “Although the virus represents a potentially very serious public health threat, and we expect to continue seeing more cases here, the immediate risk to the American public is low at this time,” Mr. Azar said. “We are working as quickly as possible on the many unanswered questions about this virus. That includes exactly how it spreads, how deadly it is, whether it’s commonly transmitted by patients who are not yet displaying symptoms, and other issues.”
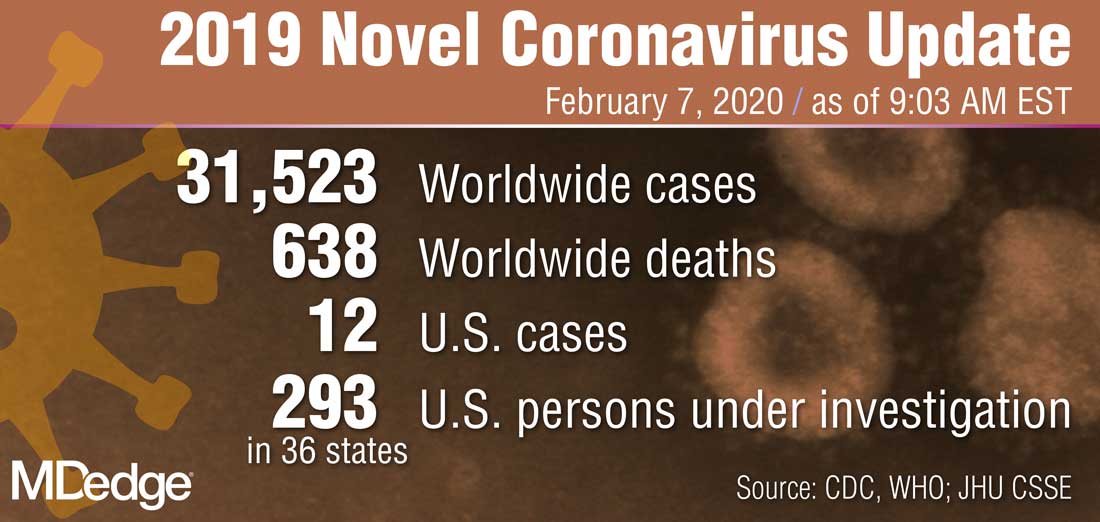
“What they’re looking at is the effect of this drug -- either the drug plus standard of care versus standard of care alone,” Anthony S. Fauci, MD, reported Feb. 7 during a press briefing held by members of President Trump’s Coronavirus Task Force. “I think pretty soon we are going to get a definitive answer, whether one of these among several drugs works.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases, added that several organizations and individual investigators are developing vaccines for 2019-nCoV. In one such effort, the National Institutes of Health is working with Moderna Inc. to develop a vaccine built on a messenger RNA platform. “One of the first steps is to successfully get that [novel coronavirus] gene and insert it into the messenger RNA platform successfully and allow it to express proteins,” Dr. Fauci explained. “We’ve succeeded in that. The next [step] is to put it in a mouse animal model to induce immunogenicity, and to get the company to make [gold nanoparticle] products. All of those have been successfully implemented. There have been no glitches so far. If that continues, we will be in Phase 1 trials in people within the next two-and-a-half months.”
In another development on the same day, Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, announced that Heath & Human Services issued an interim final rule to amend foreign quarantine regulations in the wake of the public health threat posed by the 2019-nCoV. “This will enable CDC to collect certain contact information data regarding airline passengers and crew when they arrive from other countries. . .and may be exposed to communicable disease,” Dr. Redfield said. “This action is part of our multi-layered approach to the U.S. response and demonstrates our commitment to take all necessary actions to protect the American people.”
According to Alex Azar, secretary of Health and Human Services, and chair of President Trump’s Coronavirus Task Force, there are 12 confirmed cases of the novel coronavirus in the United States, including two cases of transmission to people who had not recently been in China. “Although the virus represents a potentially very serious public health threat, and we expect to continue seeing more cases here, the immediate risk to the American public is low at this time,” Mr. Azar said. “We are working as quickly as possible on the many unanswered questions about this virus. That includes exactly how it spreads, how deadly it is, whether it’s commonly transmitted by patients who are not yet displaying symptoms, and other issues.”
Report chastises government for allowing flavored e-cigarettes
according to a report on federal and state policies.
In its annual “State of Tobacco Control” report, the American Lung Association called out the federal government for issuing “inadequate guidance on flavored e-cigarettes that leaves thousands of flavored e-cigarettes on the market.” The organization urged Congress and the Food and Drug Administration “to eliminate all flavored tobacco products from the marketplace, including menthol cigarettes, flavored cigars, and e-cigarettes,” in 2020.
“Flavored tobacco products cause kids to become hooked, and now more than one in four teens (27.5%) are vaping, a staggering 135% increase over the past 2 years,” the association wrote in a news release. Federal guidance on Jan. 2, 2020, permits the sale of flavored e-cigarettes that do not use cartridges. This guidance represented a reversal after officials said in a prior announcement that regulators would “clear the market” of flavored e-cigarettes.
Graphic warning labels
The report also asked the FDA to reject product marketing applications that fail to meet public health standards, calls on the U.S. Department of Health & Human Services to “clarify and ensure that all tobacco users have access to a comprehensive tobacco cessation benefit,” and urges Congress to increase federal funding for the Centers for Disease Control and Prevention’s Office on Smoking and Health to help stop youth e-cigarette use.
“Raising the federal minimum age of sale to 21, which took effect immediately on Dec. 30, was an important first step forward,” the report says. “The American Lung Association successfully advocated for the legislation to be comprehensive and to close state exemptions, such as for military personnel, while also not limiting states from pursuing stronger protections. Additional rules from FDA to provide guidance on the law’s implementation are forthcoming.”
The FDA is expected to release graphic warning labels for cigarette packs in March. After legal setbacks to the Tobacco Control Act of 2009, which required the FDA to ensure all cigarette packs had graphic warning labels by 2011, a judgment “compels FDA to release final graphic warnings by March 15, 2020, with the warning labels appearing on all cigarette packs by June of 2021,” the American Lung Association report said.
“While the American Lung Association recognizes the federal government with an A grade for passage of a strong federal Tobacco 21 law [raising the minimum age of purchase], it also earns an F for its failure to comprehensively oversee tobacco products,” said Harold P. Wimmer, national president and CEO of the American Lung Association, in the news release. “Without meaningful actions by the federal government, the health and the future of our nation’s children are being compromised.”
The federal government received an F for its tobacco tax policies, a D for cessation coverage, and an A for its mass media campaigns, “Tips from Former Smokers” and “The Real Cost.”
Grading states
In addition, the report graded each state and the District of Columbia in terms of funding for tobacco prevention programs, strength of smoke-free workplace laws, level of state tobacco taxes, and coverage of and access to services to quit tobacco. None scored all A’s, but California, the District of Columbia, Maine, New York, and Vermont ranked the highest. Alabama, Mississippi, and North Carolina, on the other hand, received all F’s.
In November, Massachusetts became the first state to prohibit the sale of flavored tobacco products, including menthol cigarettes, and more states should follow suit, according to the association.
according to a report on federal and state policies.
In its annual “State of Tobacco Control” report, the American Lung Association called out the federal government for issuing “inadequate guidance on flavored e-cigarettes that leaves thousands of flavored e-cigarettes on the market.” The organization urged Congress and the Food and Drug Administration “to eliminate all flavored tobacco products from the marketplace, including menthol cigarettes, flavored cigars, and e-cigarettes,” in 2020.
“Flavored tobacco products cause kids to become hooked, and now more than one in four teens (27.5%) are vaping, a staggering 135% increase over the past 2 years,” the association wrote in a news release. Federal guidance on Jan. 2, 2020, permits the sale of flavored e-cigarettes that do not use cartridges. This guidance represented a reversal after officials said in a prior announcement that regulators would “clear the market” of flavored e-cigarettes.
Graphic warning labels
The report also asked the FDA to reject product marketing applications that fail to meet public health standards, calls on the U.S. Department of Health & Human Services to “clarify and ensure that all tobacco users have access to a comprehensive tobacco cessation benefit,” and urges Congress to increase federal funding for the Centers for Disease Control and Prevention’s Office on Smoking and Health to help stop youth e-cigarette use.
“Raising the federal minimum age of sale to 21, which took effect immediately on Dec. 30, was an important first step forward,” the report says. “The American Lung Association successfully advocated for the legislation to be comprehensive and to close state exemptions, such as for military personnel, while also not limiting states from pursuing stronger protections. Additional rules from FDA to provide guidance on the law’s implementation are forthcoming.”
The FDA is expected to release graphic warning labels for cigarette packs in March. After legal setbacks to the Tobacco Control Act of 2009, which required the FDA to ensure all cigarette packs had graphic warning labels by 2011, a judgment “compels FDA to release final graphic warnings by March 15, 2020, with the warning labels appearing on all cigarette packs by June of 2021,” the American Lung Association report said.
“While the American Lung Association recognizes the federal government with an A grade for passage of a strong federal Tobacco 21 law [raising the minimum age of purchase], it also earns an F for its failure to comprehensively oversee tobacco products,” said Harold P. Wimmer, national president and CEO of the American Lung Association, in the news release. “Without meaningful actions by the federal government, the health and the future of our nation’s children are being compromised.”
The federal government received an F for its tobacco tax policies, a D for cessation coverage, and an A for its mass media campaigns, “Tips from Former Smokers” and “The Real Cost.”
Grading states
In addition, the report graded each state and the District of Columbia in terms of funding for tobacco prevention programs, strength of smoke-free workplace laws, level of state tobacco taxes, and coverage of and access to services to quit tobacco. None scored all A’s, but California, the District of Columbia, Maine, New York, and Vermont ranked the highest. Alabama, Mississippi, and North Carolina, on the other hand, received all F’s.
In November, Massachusetts became the first state to prohibit the sale of flavored tobacco products, including menthol cigarettes, and more states should follow suit, according to the association.
according to a report on federal and state policies.
In its annual “State of Tobacco Control” report, the American Lung Association called out the federal government for issuing “inadequate guidance on flavored e-cigarettes that leaves thousands of flavored e-cigarettes on the market.” The organization urged Congress and the Food and Drug Administration “to eliminate all flavored tobacco products from the marketplace, including menthol cigarettes, flavored cigars, and e-cigarettes,” in 2020.
“Flavored tobacco products cause kids to become hooked, and now more than one in four teens (27.5%) are vaping, a staggering 135% increase over the past 2 years,” the association wrote in a news release. Federal guidance on Jan. 2, 2020, permits the sale of flavored e-cigarettes that do not use cartridges. This guidance represented a reversal after officials said in a prior announcement that regulators would “clear the market” of flavored e-cigarettes.
Graphic warning labels
The report also asked the FDA to reject product marketing applications that fail to meet public health standards, calls on the U.S. Department of Health & Human Services to “clarify and ensure that all tobacco users have access to a comprehensive tobacco cessation benefit,” and urges Congress to increase federal funding for the Centers for Disease Control and Prevention’s Office on Smoking and Health to help stop youth e-cigarette use.
“Raising the federal minimum age of sale to 21, which took effect immediately on Dec. 30, was an important first step forward,” the report says. “The American Lung Association successfully advocated for the legislation to be comprehensive and to close state exemptions, such as for military personnel, while also not limiting states from pursuing stronger protections. Additional rules from FDA to provide guidance on the law’s implementation are forthcoming.”
The FDA is expected to release graphic warning labels for cigarette packs in March. After legal setbacks to the Tobacco Control Act of 2009, which required the FDA to ensure all cigarette packs had graphic warning labels by 2011, a judgment “compels FDA to release final graphic warnings by March 15, 2020, with the warning labels appearing on all cigarette packs by June of 2021,” the American Lung Association report said.
“While the American Lung Association recognizes the federal government with an A grade for passage of a strong federal Tobacco 21 law [raising the minimum age of purchase], it also earns an F for its failure to comprehensively oversee tobacco products,” said Harold P. Wimmer, national president and CEO of the American Lung Association, in the news release. “Without meaningful actions by the federal government, the health and the future of our nation’s children are being compromised.”
The federal government received an F for its tobacco tax policies, a D for cessation coverage, and an A for its mass media campaigns, “Tips from Former Smokers” and “The Real Cost.”
Grading states
In addition, the report graded each state and the District of Columbia in terms of funding for tobacco prevention programs, strength of smoke-free workplace laws, level of state tobacco taxes, and coverage of and access to services to quit tobacco. None scored all A’s, but California, the District of Columbia, Maine, New York, and Vermont ranked the highest. Alabama, Mississippi, and North Carolina, on the other hand, received all F’s.
In November, Massachusetts became the first state to prohibit the sale of flavored tobacco products, including menthol cigarettes, and more states should follow suit, according to the association.
Funding failures: Tobacco prevention and cessation
When it comes to state funding for tobacco prevention and cessation, the American Lung Association grades on a curve. It did not help.

Each state’s annual funding for tobacco prevention and cessation was calculated and then compared with the Centers for Disease Control and Prevention’s recommended spending level. That percentage became the grade, with any level of funding at 80% or more of the CDC’s recommendation getting an A and anything below 50% getting an F, the ALA explained.
The three A’s went to Alaska – which spent $10.14 million, or 99.4% of the CDC-recommended $10.2 million – California (96.0%), and Maine (83.5%). The lowest levels of spending came from Georgia, which spend just 2.8% of the CDC’s recommendation of $106 million, and Missouri, which spent 3.0%, the ALA reported.
States’ grades were generally better in the four other areas of tobacco-control policy: There were 24 A’s and 9 F’s for smoke-free air laws, 1 A and 35 F’s for tobacco excise taxes, 3 A’s and 17 F’s for access to cessation treatment, and 10 A’s and 30 F’s for laws to raise the tobacco sales age to 21 years, the ALA said in the report.
Despite an overall grade of F, the federal government managed to earn some praise in that last area: “In what could only be described as unimaginable even 2 years ago, in December 2019, Congress passed bipartisan legislation to raise the minimum age of sale for tobacco products to 21,” the ALA said.
The federal government was strongly criticized on the subject of e-cigarettes. “The Trump Administration failed to prioritize public health over the tobacco industry with its Jan. 2, 2020, announcement that will leave thousands of flavored e-cigarettes on the market,” the ALA said, while concluding that the rising use of e-cigarettes in recent years “is a real-world demonstration of the failure of the U.S. Food and Drug Administration to properly oversee all tobacco products. … This failure places the lung health and lives of Americans at risk.”
When it comes to state funding for tobacco prevention and cessation, the American Lung Association grades on a curve. It did not help.

Each state’s annual funding for tobacco prevention and cessation was calculated and then compared with the Centers for Disease Control and Prevention’s recommended spending level. That percentage became the grade, with any level of funding at 80% or more of the CDC’s recommendation getting an A and anything below 50% getting an F, the ALA explained.
The three A’s went to Alaska – which spent $10.14 million, or 99.4% of the CDC-recommended $10.2 million – California (96.0%), and Maine (83.5%). The lowest levels of spending came from Georgia, which spend just 2.8% of the CDC’s recommendation of $106 million, and Missouri, which spent 3.0%, the ALA reported.
States’ grades were generally better in the four other areas of tobacco-control policy: There were 24 A’s and 9 F’s for smoke-free air laws, 1 A and 35 F’s for tobacco excise taxes, 3 A’s and 17 F’s for access to cessation treatment, and 10 A’s and 30 F’s for laws to raise the tobacco sales age to 21 years, the ALA said in the report.
Despite an overall grade of F, the federal government managed to earn some praise in that last area: “In what could only be described as unimaginable even 2 years ago, in December 2019, Congress passed bipartisan legislation to raise the minimum age of sale for tobacco products to 21,” the ALA said.
The federal government was strongly criticized on the subject of e-cigarettes. “The Trump Administration failed to prioritize public health over the tobacco industry with its Jan. 2, 2020, announcement that will leave thousands of flavored e-cigarettes on the market,” the ALA said, while concluding that the rising use of e-cigarettes in recent years “is a real-world demonstration of the failure of the U.S. Food and Drug Administration to properly oversee all tobacco products. … This failure places the lung health and lives of Americans at risk.”
When it comes to state funding for tobacco prevention and cessation, the American Lung Association grades on a curve. It did not help.

Each state’s annual funding for tobacco prevention and cessation was calculated and then compared with the Centers for Disease Control and Prevention’s recommended spending level. That percentage became the grade, with any level of funding at 80% or more of the CDC’s recommendation getting an A and anything below 50% getting an F, the ALA explained.
The three A’s went to Alaska – which spent $10.14 million, or 99.4% of the CDC-recommended $10.2 million – California (96.0%), and Maine (83.5%). The lowest levels of spending came from Georgia, which spend just 2.8% of the CDC’s recommendation of $106 million, and Missouri, which spent 3.0%, the ALA reported.
States’ grades were generally better in the four other areas of tobacco-control policy: There were 24 A’s and 9 F’s for smoke-free air laws, 1 A and 35 F’s for tobacco excise taxes, 3 A’s and 17 F’s for access to cessation treatment, and 10 A’s and 30 F’s for laws to raise the tobacco sales age to 21 years, the ALA said in the report.
Despite an overall grade of F, the federal government managed to earn some praise in that last area: “In what could only be described as unimaginable even 2 years ago, in December 2019, Congress passed bipartisan legislation to raise the minimum age of sale for tobacco products to 21,” the ALA said.
The federal government was strongly criticized on the subject of e-cigarettes. “The Trump Administration failed to prioritize public health over the tobacco industry with its Jan. 2, 2020, announcement that will leave thousands of flavored e-cigarettes on the market,” the ALA said, while concluding that the rising use of e-cigarettes in recent years “is a real-world demonstration of the failure of the U.S. Food and Drug Administration to properly oversee all tobacco products. … This failure places the lung health and lives of Americans at risk.”
Uptick in lung cancer in younger women, not related to smoking
A study of lung cancer in younger adults (less than 50 years) has found a recent trend of higher lung cancer rates in women, compared with men. The increase is driven by cases of adenocarcinoma of the lung.
The “emerging pattern of higher lung cancer incidence in young females” is not confined to geographic areas and income levels and “is not fully explained by sex-differences in smoking prevalence,” the authors comment.
Miranda M. Fidler-Benaoudia, PhD, Cancer Control Alberta, Alberta Health Services, Calgary, and colleagues examined lung cancer cases in 40 countries from 1993 to 2012.
They found that the female-to-male incidence rate ratio (IRR) had significantly crossed over from men to women in six countries, including the United States and Canada, and had nonsignificantly crossed over in a further 23 countries.
The research was published online Feb. 5 in the International Journal of Cancer.
These findings “forewarn of a higher lung cancer burden in women than men at older ages in the decades to follow, especially in higher-income settings,” write the authors. They highlight “the need for etiologic studies.”
Historically, lung cancer higher in men
Historically, lung cancer rates have been higher among men than women, owing to the fact that men start smoking in large numbers earlier and smoke at higher rates, the researchers comment.
However, there has been a convergence in lung cancer incidence between men and women. A recent study suggests that, in the United States, the incidence in young women is higher than that in their male counterparts.
To determine the degree to which this phenomenon is occurring globally, the team used national or subnational registry data from Cancer Incidence in Five Continents, volumes VIII–XI.
These included lung and bronchial cancer cases in 40 countries from 1993 to 2012, divided into 5-year periods. Individuals were categorized into 5-year age bands.
In addition, the team used the Global Health Data Exchange to extract data from the Global Burden of Disease Study 2015 and derive country- and sex-specific daily smoking prevalence rates.
The researchers found that among young men and women, there were three patterns in the occurrence of lung cancer between the periods 1993-1997 and 2008-2012:
- A significant crossover from male to female dominance, seen in six countries.
- An insignificant crossover from male to female dominance, found in 23 countries.
- A continued male dominance, observed in 11 countries.
Higher incidence in women in six countries
The six countries with significant crossover from male to female dominance were Canada, Denmark, Germany, New Zealand, the Netherlands, and the United States.
Further analysis showed that, in general, age-specific lung cancer incidence rates decreased in successive male birth cohorts in these six countries. There was more variation across female birth cohorts.
Calculating female-to-male incidence rate ratios, the team found, for example, the IRR increased in New Zealand from 1.0 in the 1953 birth cohort to 1.6 in the 1968 birth cohort for people aged 40-44 years.
In addition, among adults aged 45-49 years in the Netherlands, the IRR rose from 0.7 in those born in the circa 1948 cohort to 1.4 in those from the circa 1958 cohort.
Overall, female-to-male IRRs increased notably among the following groups:
- Individuals aged 30-34 years in Canada, Denmark, and Germany.
- Those aged 40-44 years in Germany, the Netherlands, and the United States.
- Those aged 44-50 years in the Netherlands and the United States.
- Those aged 50-54 years in Canada, Denmark, and New Zealand.
Countries with an insignificant crossover from male to female dominance of lung cancer were located across Africa, the Americas, Asia, Europe, and Oceania.
Again, incidence rates were typically characterized by falling rates of lung cancer among men in more recent birth cohorts, and lung cancer incidence trends were more variable in women.
The team writes: “Of note, the six countries demonstrating a significant crossover are among those considered to be more advanced in the tobacco epidemic.
“Many of the countries where the crossover was insignificant or when there was no crossover are considered to be late adopters of the tobacco epidemic, with the effects of the epidemic on the burden of lung cancer and other smoking-related diseases beginning to manifest more recently, or perhaps yet to come.”
They suggest that low- and middle-resource countries may not follow the tobacco epidemic pattern of high-income countries, and so “we may not see higher lung cancer incidence rates in women than men for the foreseeable future in these countries.”
No funding for the study has been disclosed. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
A study of lung cancer in younger adults (less than 50 years) has found a recent trend of higher lung cancer rates in women, compared with men. The increase is driven by cases of adenocarcinoma of the lung.
The “emerging pattern of higher lung cancer incidence in young females” is not confined to geographic areas and income levels and “is not fully explained by sex-differences in smoking prevalence,” the authors comment.
Miranda M. Fidler-Benaoudia, PhD, Cancer Control Alberta, Alberta Health Services, Calgary, and colleagues examined lung cancer cases in 40 countries from 1993 to 2012.
They found that the female-to-male incidence rate ratio (IRR) had significantly crossed over from men to women in six countries, including the United States and Canada, and had nonsignificantly crossed over in a further 23 countries.
The research was published online Feb. 5 in the International Journal of Cancer.
These findings “forewarn of a higher lung cancer burden in women than men at older ages in the decades to follow, especially in higher-income settings,” write the authors. They highlight “the need for etiologic studies.”
Historically, lung cancer higher in men
Historically, lung cancer rates have been higher among men than women, owing to the fact that men start smoking in large numbers earlier and smoke at higher rates, the researchers comment.
However, there has been a convergence in lung cancer incidence between men and women. A recent study suggests that, in the United States, the incidence in young women is higher than that in their male counterparts.
To determine the degree to which this phenomenon is occurring globally, the team used national or subnational registry data from Cancer Incidence in Five Continents, volumes VIII–XI.
These included lung and bronchial cancer cases in 40 countries from 1993 to 2012, divided into 5-year periods. Individuals were categorized into 5-year age bands.
In addition, the team used the Global Health Data Exchange to extract data from the Global Burden of Disease Study 2015 and derive country- and sex-specific daily smoking prevalence rates.
The researchers found that among young men and women, there were three patterns in the occurrence of lung cancer between the periods 1993-1997 and 2008-2012:
- A significant crossover from male to female dominance, seen in six countries.
- An insignificant crossover from male to female dominance, found in 23 countries.
- A continued male dominance, observed in 11 countries.
Higher incidence in women in six countries
The six countries with significant crossover from male to female dominance were Canada, Denmark, Germany, New Zealand, the Netherlands, and the United States.
Further analysis showed that, in general, age-specific lung cancer incidence rates decreased in successive male birth cohorts in these six countries. There was more variation across female birth cohorts.
Calculating female-to-male incidence rate ratios, the team found, for example, the IRR increased in New Zealand from 1.0 in the 1953 birth cohort to 1.6 in the 1968 birth cohort for people aged 40-44 years.
In addition, among adults aged 45-49 years in the Netherlands, the IRR rose from 0.7 in those born in the circa 1948 cohort to 1.4 in those from the circa 1958 cohort.
Overall, female-to-male IRRs increased notably among the following groups:
- Individuals aged 30-34 years in Canada, Denmark, and Germany.
- Those aged 40-44 years in Germany, the Netherlands, and the United States.
- Those aged 44-50 years in the Netherlands and the United States.
- Those aged 50-54 years in Canada, Denmark, and New Zealand.
Countries with an insignificant crossover from male to female dominance of lung cancer were located across Africa, the Americas, Asia, Europe, and Oceania.
Again, incidence rates were typically characterized by falling rates of lung cancer among men in more recent birth cohorts, and lung cancer incidence trends were more variable in women.
The team writes: “Of note, the six countries demonstrating a significant crossover are among those considered to be more advanced in the tobacco epidemic.
“Many of the countries where the crossover was insignificant or when there was no crossover are considered to be late adopters of the tobacco epidemic, with the effects of the epidemic on the burden of lung cancer and other smoking-related diseases beginning to manifest more recently, or perhaps yet to come.”
They suggest that low- and middle-resource countries may not follow the tobacco epidemic pattern of high-income countries, and so “we may not see higher lung cancer incidence rates in women than men for the foreseeable future in these countries.”
No funding for the study has been disclosed. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
A study of lung cancer in younger adults (less than 50 years) has found a recent trend of higher lung cancer rates in women, compared with men. The increase is driven by cases of adenocarcinoma of the lung.
The “emerging pattern of higher lung cancer incidence in young females” is not confined to geographic areas and income levels and “is not fully explained by sex-differences in smoking prevalence,” the authors comment.
Miranda M. Fidler-Benaoudia, PhD, Cancer Control Alberta, Alberta Health Services, Calgary, and colleagues examined lung cancer cases in 40 countries from 1993 to 2012.
They found that the female-to-male incidence rate ratio (IRR) had significantly crossed over from men to women in six countries, including the United States and Canada, and had nonsignificantly crossed over in a further 23 countries.
The research was published online Feb. 5 in the International Journal of Cancer.
These findings “forewarn of a higher lung cancer burden in women than men at older ages in the decades to follow, especially in higher-income settings,” write the authors. They highlight “the need for etiologic studies.”
Historically, lung cancer higher in men
Historically, lung cancer rates have been higher among men than women, owing to the fact that men start smoking in large numbers earlier and smoke at higher rates, the researchers comment.
However, there has been a convergence in lung cancer incidence between men and women. A recent study suggests that, in the United States, the incidence in young women is higher than that in their male counterparts.
To determine the degree to which this phenomenon is occurring globally, the team used national or subnational registry data from Cancer Incidence in Five Continents, volumes VIII–XI.
These included lung and bronchial cancer cases in 40 countries from 1993 to 2012, divided into 5-year periods. Individuals were categorized into 5-year age bands.
In addition, the team used the Global Health Data Exchange to extract data from the Global Burden of Disease Study 2015 and derive country- and sex-specific daily smoking prevalence rates.
The researchers found that among young men and women, there were three patterns in the occurrence of lung cancer between the periods 1993-1997 and 2008-2012:
- A significant crossover from male to female dominance, seen in six countries.
- An insignificant crossover from male to female dominance, found in 23 countries.
- A continued male dominance, observed in 11 countries.
Higher incidence in women in six countries
The six countries with significant crossover from male to female dominance were Canada, Denmark, Germany, New Zealand, the Netherlands, and the United States.
Further analysis showed that, in general, age-specific lung cancer incidence rates decreased in successive male birth cohorts in these six countries. There was more variation across female birth cohorts.
Calculating female-to-male incidence rate ratios, the team found, for example, the IRR increased in New Zealand from 1.0 in the 1953 birth cohort to 1.6 in the 1968 birth cohort for people aged 40-44 years.
In addition, among adults aged 45-49 years in the Netherlands, the IRR rose from 0.7 in those born in the circa 1948 cohort to 1.4 in those from the circa 1958 cohort.
Overall, female-to-male IRRs increased notably among the following groups:
- Individuals aged 30-34 years in Canada, Denmark, and Germany.
- Those aged 40-44 years in Germany, the Netherlands, and the United States.
- Those aged 44-50 years in the Netherlands and the United States.
- Those aged 50-54 years in Canada, Denmark, and New Zealand.
Countries with an insignificant crossover from male to female dominance of lung cancer were located across Africa, the Americas, Asia, Europe, and Oceania.
Again, incidence rates were typically characterized by falling rates of lung cancer among men in more recent birth cohorts, and lung cancer incidence trends were more variable in women.
The team writes: “Of note, the six countries demonstrating a significant crossover are among those considered to be more advanced in the tobacco epidemic.
“Many of the countries where the crossover was insignificant or when there was no crossover are considered to be late adopters of the tobacco epidemic, with the effects of the epidemic on the burden of lung cancer and other smoking-related diseases beginning to manifest more recently, or perhaps yet to come.”
They suggest that low- and middle-resource countries may not follow the tobacco epidemic pattern of high-income countries, and so “we may not see higher lung cancer incidence rates in women than men for the foreseeable future in these countries.”
No funding for the study has been disclosed. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Delaying flu vaccine didn’t drop fever rate for childhood immunizations
according to a randomized trial.
An increased risk for febrile seizures had been seen when the three vaccines were administered together, wrote Emmanuel B. Walter, MD, MPH, and coauthors, so they constructed a trial that compared a simultaneous administration strategy that delayed inactivated influenza vaccine (IIV) administration by about 2 weeks.
In all, 221 children aged 12-16 months were enrolled in the randomized study. A total of 110 children received quadrivalent IIV (IIV4), DTaP, and 13-valent pneumococcal conjugate vaccine (PCV13) simultaneously and returned for a dental health education visit 2 weeks later. For 111 children, DTaP and PCV13 were administered at study visit 1, and IIV4 was given along with dental health education 2 weeks later. Most children in both groups also received at least one nonstudy vaccine at the first study visit. Eleven children in the simultaneous group and four in the sequential group didn’t complete the study.
There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87; 95% confidence interval, 0.36-2.10).
However, children in the simultaneous group were more likely to receive antipyretic medication in the first 2 days after visit 1 (37% versus 22%; P = .020), reported Dr. Walter, professor of pediatrics at Duke University, Durham, N.C., and coauthors. Because it’s rare for febrile seizures to occur after immunization, the authors didn’t make the occurrence of febrile seizure a primary or secondary endpoint of the study; no seizures occurred in study participants. They did hypothesize that the total proportion of children having fever would be higher in the simultaneous than in the sequential group – a hypothesis not supported by the study findings.
Children were excluded, or their study vaccinations were delayed, if they had received antipyretic medication within the 72 hours preceding the visit or at the study visit, or if they had a temperature of 38° C or more.
Parents monitored participants’ temperatures for 8 days after visits by using a study-provided temporal thermometer once daily at about the same time, and also by checking the temperature if their child felt feverish. Parents also recorded any antipyretic use, medical care, other symptoms, and febrile seizures.
The study was stopped earlier than anticipated because unexpectedly high levels of influenza activity made it unethical to delay influenza immunization, explained Dr. Walter and coauthors.
Participants were a median 15 months old; most were non-Hispanic white and had private insurance. Most participants didn’t attend day care.
“Nearly all fever episodes and days of fever on days 1-2 after the study visits occurred after visit 1,” reported Dr. Walter and coinvestigators. They saw no difference between groups in the proportion of children who had a fever of 38.6° C on days 1-2 after either study visit.
The mean peak temperature – about 38.5° C – on combined study visits 1 and 2 didn’t differ between groups. Similarly, for those participants who had a fever, the mean postvisit fever duration of 1.3 days was identical between groups.
Parents also were asked about their perceptions of the vaccination schedule their children received. Over half of parents overall (56%) reported that they disliked having to bring their child in for two separate clinic visits, with more parents in the sequential group than the simultaneous group reporting this (65% versus 48%).
Generalizability of the findings and comparison with previous studies are limited, noted Dr. Walter and coinvestigators, because the composition of influenza vaccine varies from year to year. No signal for seizures was seen in the Vaccine Safety Datalink after IIV during the 2017-2018 influenza season, wrote the investigators. The 2010-2011 influenza season’s IIV formulation was associated with increased febrile seizure risk, indicating that the IIV formulation for that year may have been more pyrogenic than the 2017-2018 formulation.
Also, children deemed at higher risk of febrile seizure were excluded from the study, so findings may have limited applicability to these children. The lack of parental blinding also may have influenced antipyretic administration or other symptom reporting, although objective temperature measurement should not have been affected by the lack of blinding, wrote Dr. Walker and collaborators.
The study was funded by the Centers for Disease Control and Prevention. One coauthor reported potential conflicts of interest from financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune. The remaining authors have no relevant financial disclosures.
SOURCE: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
according to a randomized trial.
An increased risk for febrile seizures had been seen when the three vaccines were administered together, wrote Emmanuel B. Walter, MD, MPH, and coauthors, so they constructed a trial that compared a simultaneous administration strategy that delayed inactivated influenza vaccine (IIV) administration by about 2 weeks.
In all, 221 children aged 12-16 months were enrolled in the randomized study. A total of 110 children received quadrivalent IIV (IIV4), DTaP, and 13-valent pneumococcal conjugate vaccine (PCV13) simultaneously and returned for a dental health education visit 2 weeks later. For 111 children, DTaP and PCV13 were administered at study visit 1, and IIV4 was given along with dental health education 2 weeks later. Most children in both groups also received at least one nonstudy vaccine at the first study visit. Eleven children in the simultaneous group and four in the sequential group didn’t complete the study.
There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87; 95% confidence interval, 0.36-2.10).
However, children in the simultaneous group were more likely to receive antipyretic medication in the first 2 days after visit 1 (37% versus 22%; P = .020), reported Dr. Walter, professor of pediatrics at Duke University, Durham, N.C., and coauthors. Because it’s rare for febrile seizures to occur after immunization, the authors didn’t make the occurrence of febrile seizure a primary or secondary endpoint of the study; no seizures occurred in study participants. They did hypothesize that the total proportion of children having fever would be higher in the simultaneous than in the sequential group – a hypothesis not supported by the study findings.
Children were excluded, or their study vaccinations were delayed, if they had received antipyretic medication within the 72 hours preceding the visit or at the study visit, or if they had a temperature of 38° C or more.
Parents monitored participants’ temperatures for 8 days after visits by using a study-provided temporal thermometer once daily at about the same time, and also by checking the temperature if their child felt feverish. Parents also recorded any antipyretic use, medical care, other symptoms, and febrile seizures.
The study was stopped earlier than anticipated because unexpectedly high levels of influenza activity made it unethical to delay influenza immunization, explained Dr. Walter and coauthors.
Participants were a median 15 months old; most were non-Hispanic white and had private insurance. Most participants didn’t attend day care.
“Nearly all fever episodes and days of fever on days 1-2 after the study visits occurred after visit 1,” reported Dr. Walter and coinvestigators. They saw no difference between groups in the proportion of children who had a fever of 38.6° C on days 1-2 after either study visit.
The mean peak temperature – about 38.5° C – on combined study visits 1 and 2 didn’t differ between groups. Similarly, for those participants who had a fever, the mean postvisit fever duration of 1.3 days was identical between groups.
Parents also were asked about their perceptions of the vaccination schedule their children received. Over half of parents overall (56%) reported that they disliked having to bring their child in for two separate clinic visits, with more parents in the sequential group than the simultaneous group reporting this (65% versus 48%).
Generalizability of the findings and comparison with previous studies are limited, noted Dr. Walter and coinvestigators, because the composition of influenza vaccine varies from year to year. No signal for seizures was seen in the Vaccine Safety Datalink after IIV during the 2017-2018 influenza season, wrote the investigators. The 2010-2011 influenza season’s IIV formulation was associated with increased febrile seizure risk, indicating that the IIV formulation for that year may have been more pyrogenic than the 2017-2018 formulation.
Also, children deemed at higher risk of febrile seizure were excluded from the study, so findings may have limited applicability to these children. The lack of parental blinding also may have influenced antipyretic administration or other symptom reporting, although objective temperature measurement should not have been affected by the lack of blinding, wrote Dr. Walker and collaborators.
The study was funded by the Centers for Disease Control and Prevention. One coauthor reported potential conflicts of interest from financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune. The remaining authors have no relevant financial disclosures.
SOURCE: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
according to a randomized trial.
An increased risk for febrile seizures had been seen when the three vaccines were administered together, wrote Emmanuel B. Walter, MD, MPH, and coauthors, so they constructed a trial that compared a simultaneous administration strategy that delayed inactivated influenza vaccine (IIV) administration by about 2 weeks.
In all, 221 children aged 12-16 months were enrolled in the randomized study. A total of 110 children received quadrivalent IIV (IIV4), DTaP, and 13-valent pneumococcal conjugate vaccine (PCV13) simultaneously and returned for a dental health education visit 2 weeks later. For 111 children, DTaP and PCV13 were administered at study visit 1, and IIV4 was given along with dental health education 2 weeks later. Most children in both groups also received at least one nonstudy vaccine at the first study visit. Eleven children in the simultaneous group and four in the sequential group didn’t complete the study.
There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87; 95% confidence interval, 0.36-2.10).
However, children in the simultaneous group were more likely to receive antipyretic medication in the first 2 days after visit 1 (37% versus 22%; P = .020), reported Dr. Walter, professor of pediatrics at Duke University, Durham, N.C., and coauthors. Because it’s rare for febrile seizures to occur after immunization, the authors didn’t make the occurrence of febrile seizure a primary or secondary endpoint of the study; no seizures occurred in study participants. They did hypothesize that the total proportion of children having fever would be higher in the simultaneous than in the sequential group – a hypothesis not supported by the study findings.
Children were excluded, or their study vaccinations were delayed, if they had received antipyretic medication within the 72 hours preceding the visit or at the study visit, or if they had a temperature of 38° C or more.
Parents monitored participants’ temperatures for 8 days after visits by using a study-provided temporal thermometer once daily at about the same time, and also by checking the temperature if their child felt feverish. Parents also recorded any antipyretic use, medical care, other symptoms, and febrile seizures.
The study was stopped earlier than anticipated because unexpectedly high levels of influenza activity made it unethical to delay influenza immunization, explained Dr. Walter and coauthors.
Participants were a median 15 months old; most were non-Hispanic white and had private insurance. Most participants didn’t attend day care.
“Nearly all fever episodes and days of fever on days 1-2 after the study visits occurred after visit 1,” reported Dr. Walter and coinvestigators. They saw no difference between groups in the proportion of children who had a fever of 38.6° C on days 1-2 after either study visit.
The mean peak temperature – about 38.5° C – on combined study visits 1 and 2 didn’t differ between groups. Similarly, for those participants who had a fever, the mean postvisit fever duration of 1.3 days was identical between groups.
Parents also were asked about their perceptions of the vaccination schedule their children received. Over half of parents overall (56%) reported that they disliked having to bring their child in for two separate clinic visits, with more parents in the sequential group than the simultaneous group reporting this (65% versus 48%).
Generalizability of the findings and comparison with previous studies are limited, noted Dr. Walter and coinvestigators, because the composition of influenza vaccine varies from year to year. No signal for seizures was seen in the Vaccine Safety Datalink after IIV during the 2017-2018 influenza season, wrote the investigators. The 2010-2011 influenza season’s IIV formulation was associated with increased febrile seizure risk, indicating that the IIV formulation for that year may have been more pyrogenic than the 2017-2018 formulation.
Also, children deemed at higher risk of febrile seizure were excluded from the study, so findings may have limited applicability to these children. The lack of parental blinding also may have influenced antipyretic administration or other symptom reporting, although objective temperature measurement should not have been affected by the lack of blinding, wrote Dr. Walker and collaborators.
The study was funded by the Centers for Disease Control and Prevention. One coauthor reported potential conflicts of interest from financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune. The remaining authors have no relevant financial disclosures.
SOURCE: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
FROM PEDIATRICS
Key clinical point: Fevers were no less common when influenza vaccine was delayed for children receiving DTaP and pneumococcal vaccinations.
Major finding: There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87).
Study details: Randomized, nonblinded trial of 221 children aged 12-16 months receiving scheduled vaccinations.
Disclosures: The study was funded by the Centers for Disease Control and Prevention. One coauthor reported financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune.
Source: Walter EB et al. Pediatrics. 2020;145(3):e20191909.







