User login
Timing Pneumococcal Vaccination in Patients with RA Starting Methotrexate: When’s Best?
VIENNA — Pneumococcal vaccination administered 1 month prior to starting methotrexate (MTX) in patients with rheumatoid arthritis (RA) allows a significantly higher immunological response at 1 month and does not affect disease control at 1 year, compared with starting MTX simultaneously with the vaccination, according to data from a randomized trial presented at the annual European Congress of Rheumatology.
“Our patients are more susceptible to infection due to immunosuppressive therapy, and it’s recommended they receive vaccination against pneumococcal infection,” the lead author Jacques Morel, MD, PhD, said in his presentation of results from the VACIMRA study.
Timing the vaccination against pneumococcal disease when initiating MTX in clinical practice has been a point of uncertainty, noted Dr. Morel, a rheumatologist from Centre Hospitalier Universitaire, Montpellier, France.
“How can we deal with this in clinical practice where one recommendation is to vaccine before initiation of methotrexate, but it is also recommended to start methotrexate as soon as the diagnosis of RA is made?” he asked.
Comparing Humoral Response of MTX Started Immediately or 1 Month Post-Vaccination
The prospective, randomized, multicenter trial aimed to compare the rate of humoral immunological response against pneumococcal 13-valent conjugate vaccine (PCV13) in patients with RA who had a Disease Activity Score in 28 joints (DAS28) > 3.2, never taken MTX, and never been vaccinated against pneumococcus. Patients were vaccinated either 1 month before MTX initiation (n = 126) or simultaneously with MTX (n = 123). Oral glucocorticoids were allowed but only at < 10 mg/d. Following PCV13 vaccination, all patients also received the 23-valent pneumococcal polysaccharide vaccine (PPV23) 2 months later.
Concentrations of immunoglobulin (Ig) G antibodies against the 13 serotypes contained within PCV13 were measured using enzyme-linked immunosorbent assay (ELISA) and opsonophagocytic killing assay (OPA) at baseline and during follow-up at 1, 3, 6, and 12 months.
Positive antibody response was defined as a twofold or more increase in the IgG concentration using ELISA. The main outcome was the responder rates at 1 month after PCV13, defined by at least three positive antibody responses out of five of the target PVC13 serotypes (1, 3, 5, 7F, and 19A) using ELISA or OPA. Secondary outcomes included comparisons of the percentage of patients responding to each of the 13 vaccine serotypes at 1 month and after the boost with PPV23 and at 3, 6, and 12 months after vaccination with PCV13. The researchers also measured disease activity, infections, and side effects throughout the study.
Dr. Morel highlighted that all the patients had very early RA of less than 6 months, and that their characteristics at baseline were similar in both groups with 70% women, mean age 55.6 years, RA duration 2 months, 69% positive for anticitrullinated protein antibodies, 21% with erosive disease, and a DAS28 based on C-reactive protein of 4.6.
Response rates in those receiving MTX 1 month after vaccination were significantly higher at 88% with ELISA than those at 75% for immediate vaccination (P < .01) and 96% vs 88% with OPA (P = .02). These responder proportions persisted at the 12-month follow-up measurements, remaining higher in the delayed MTX group for both assays and across the 13 serotypes.
Showing a graph of the antibody responses, Dr. Morel explained that “at 12 months, the curves start to converge, but the difference in antibody titers were still significant for eight of the 13 serotypes.”
Disease Activity Not Adversely Affected by Starting MTX 1 Month Later
Regarding medication doses at 12 months, the cumulative glucocorticoid doses were similar between groups during the follow-up. As expected, the 1-year cumulative dose of MTX was higher in those given the drug immediately after vaccination vs delayed (826 vs 734 mg), but the weekly mean doses of MTX were similar at 3, 6, and 12 months between the two groups, and likewise, the use of targeted disease-modifying antirheumatic drugs (DMARDs) at 1 year was comparable. The cumulative glucocorticoid dose at 12 months was similar at 1716 mg with delayed MTX and 1613 mg with immediate MTX.
Not unexpectedly, at 1 month, DAS28 scores were higher with delayed vs immediate MTX at 3.95 vs 3.38 for DAS28-ESR and 3.54 vs 3.01 for DAS28-CRP (P < .01), but after the first month, DAS28 scores were similar between the two groups.
No significant differences were found between the groups for adverse event rates within 7 days of receiving PCV13, with local and systemic reactions occurring at 60%-61% and 50%-58%, respectively; fever at 0%-4%; and severe infections at 12%.
Finally, no difference was found in terms of serious adverse events between groups, with one pneumococcal infection with delayed MTX during follow-up, and there were no unexpected side effects observed with the PCV13 and PPV23 vaccinations.
Rheumatologists’ Reactions
Ernest Choy, MD, head of rheumatology and translational research at the Institute of Infection and Immunity, Cardiff University School of Medicine, Cardiff, Wales, asked if any individual showed no humoral response at all rather than a reduced response. “I ask because if there is no humoral response, then they are at very high risk, and there will be clinical relevance to that.”
Dr. Morel replied that “one serotype showed no response, at least according to the assays used, but we don’t know why. We analyzed at the population [level], not at the individual level, so it is difficult to answer the question.”
Another delegate asked what the participants thought about delaying MTX by 1 month. “When we tell the patient we need to vaccinate before we can use methotrexate [because] otherwise, we will reduce the response to the vaccination, then patient accepts it,” said Dr. Morel, adding that, “we allowed a minimal dose of steroids, and we saw from the results that the DAS28 at 1 month had changed.”
Co-moderator Katerina Chatzidionysiou, MD, PhD, a consultant rheumatologist and head of the Clinical Trial Department Rheumatology Unit, Karolinska University Hospital, Stockholm, Sweden, said that “As a physician, I’d feel uncomfortable delaying MTX if they had very active disease even for a short period of time.”
Dr. Morel replied that, “Today, we have so many drugs that can control the disease, for example, the targeted DMARDs. Progression does not show much variation, and we know x-ray progression with today’s drugs is a lot less than previously.”
Dr. Morel reported financial relationships with AbbVie, Amgen, Biogen, Bristol Myers Squibb, Fresenius Kabi, Galapagos, GlaxoSmithKline, Lilly, Medac, Nordic Pharma, Novartis, Pfizer, Sandoz, Sanofi, Boehringer Ingelheim, and Servier. Dr. Choy had no relevant financial relationships of relevance to this study.
A version of this article appeared on Medscape.com.
VIENNA — Pneumococcal vaccination administered 1 month prior to starting methotrexate (MTX) in patients with rheumatoid arthritis (RA) allows a significantly higher immunological response at 1 month and does not affect disease control at 1 year, compared with starting MTX simultaneously with the vaccination, according to data from a randomized trial presented at the annual European Congress of Rheumatology.
“Our patients are more susceptible to infection due to immunosuppressive therapy, and it’s recommended they receive vaccination against pneumococcal infection,” the lead author Jacques Morel, MD, PhD, said in his presentation of results from the VACIMRA study.
Timing the vaccination against pneumococcal disease when initiating MTX in clinical practice has been a point of uncertainty, noted Dr. Morel, a rheumatologist from Centre Hospitalier Universitaire, Montpellier, France.
“How can we deal with this in clinical practice where one recommendation is to vaccine before initiation of methotrexate, but it is also recommended to start methotrexate as soon as the diagnosis of RA is made?” he asked.
Comparing Humoral Response of MTX Started Immediately or 1 Month Post-Vaccination
The prospective, randomized, multicenter trial aimed to compare the rate of humoral immunological response against pneumococcal 13-valent conjugate vaccine (PCV13) in patients with RA who had a Disease Activity Score in 28 joints (DAS28) > 3.2, never taken MTX, and never been vaccinated against pneumococcus. Patients were vaccinated either 1 month before MTX initiation (n = 126) or simultaneously with MTX (n = 123). Oral glucocorticoids were allowed but only at < 10 mg/d. Following PCV13 vaccination, all patients also received the 23-valent pneumococcal polysaccharide vaccine (PPV23) 2 months later.
Concentrations of immunoglobulin (Ig) G antibodies against the 13 serotypes contained within PCV13 were measured using enzyme-linked immunosorbent assay (ELISA) and opsonophagocytic killing assay (OPA) at baseline and during follow-up at 1, 3, 6, and 12 months.
Positive antibody response was defined as a twofold or more increase in the IgG concentration using ELISA. The main outcome was the responder rates at 1 month after PCV13, defined by at least three positive antibody responses out of five of the target PVC13 serotypes (1, 3, 5, 7F, and 19A) using ELISA or OPA. Secondary outcomes included comparisons of the percentage of patients responding to each of the 13 vaccine serotypes at 1 month and after the boost with PPV23 and at 3, 6, and 12 months after vaccination with PCV13. The researchers also measured disease activity, infections, and side effects throughout the study.
Dr. Morel highlighted that all the patients had very early RA of less than 6 months, and that their characteristics at baseline were similar in both groups with 70% women, mean age 55.6 years, RA duration 2 months, 69% positive for anticitrullinated protein antibodies, 21% with erosive disease, and a DAS28 based on C-reactive protein of 4.6.
Response rates in those receiving MTX 1 month after vaccination were significantly higher at 88% with ELISA than those at 75% for immediate vaccination (P < .01) and 96% vs 88% with OPA (P = .02). These responder proportions persisted at the 12-month follow-up measurements, remaining higher in the delayed MTX group for both assays and across the 13 serotypes.
Showing a graph of the antibody responses, Dr. Morel explained that “at 12 months, the curves start to converge, but the difference in antibody titers were still significant for eight of the 13 serotypes.”
Disease Activity Not Adversely Affected by Starting MTX 1 Month Later
Regarding medication doses at 12 months, the cumulative glucocorticoid doses were similar between groups during the follow-up. As expected, the 1-year cumulative dose of MTX was higher in those given the drug immediately after vaccination vs delayed (826 vs 734 mg), but the weekly mean doses of MTX were similar at 3, 6, and 12 months between the two groups, and likewise, the use of targeted disease-modifying antirheumatic drugs (DMARDs) at 1 year was comparable. The cumulative glucocorticoid dose at 12 months was similar at 1716 mg with delayed MTX and 1613 mg with immediate MTX.
Not unexpectedly, at 1 month, DAS28 scores were higher with delayed vs immediate MTX at 3.95 vs 3.38 for DAS28-ESR and 3.54 vs 3.01 for DAS28-CRP (P < .01), but after the first month, DAS28 scores were similar between the two groups.
No significant differences were found between the groups for adverse event rates within 7 days of receiving PCV13, with local and systemic reactions occurring at 60%-61% and 50%-58%, respectively; fever at 0%-4%; and severe infections at 12%.
Finally, no difference was found in terms of serious adverse events between groups, with one pneumococcal infection with delayed MTX during follow-up, and there were no unexpected side effects observed with the PCV13 and PPV23 vaccinations.
Rheumatologists’ Reactions
Ernest Choy, MD, head of rheumatology and translational research at the Institute of Infection and Immunity, Cardiff University School of Medicine, Cardiff, Wales, asked if any individual showed no humoral response at all rather than a reduced response. “I ask because if there is no humoral response, then they are at very high risk, and there will be clinical relevance to that.”
Dr. Morel replied that “one serotype showed no response, at least according to the assays used, but we don’t know why. We analyzed at the population [level], not at the individual level, so it is difficult to answer the question.”
Another delegate asked what the participants thought about delaying MTX by 1 month. “When we tell the patient we need to vaccinate before we can use methotrexate [because] otherwise, we will reduce the response to the vaccination, then patient accepts it,” said Dr. Morel, adding that, “we allowed a minimal dose of steroids, and we saw from the results that the DAS28 at 1 month had changed.”
Co-moderator Katerina Chatzidionysiou, MD, PhD, a consultant rheumatologist and head of the Clinical Trial Department Rheumatology Unit, Karolinska University Hospital, Stockholm, Sweden, said that “As a physician, I’d feel uncomfortable delaying MTX if they had very active disease even for a short period of time.”
Dr. Morel replied that, “Today, we have so many drugs that can control the disease, for example, the targeted DMARDs. Progression does not show much variation, and we know x-ray progression with today’s drugs is a lot less than previously.”
Dr. Morel reported financial relationships with AbbVie, Amgen, Biogen, Bristol Myers Squibb, Fresenius Kabi, Galapagos, GlaxoSmithKline, Lilly, Medac, Nordic Pharma, Novartis, Pfizer, Sandoz, Sanofi, Boehringer Ingelheim, and Servier. Dr. Choy had no relevant financial relationships of relevance to this study.
A version of this article appeared on Medscape.com.
VIENNA — Pneumococcal vaccination administered 1 month prior to starting methotrexate (MTX) in patients with rheumatoid arthritis (RA) allows a significantly higher immunological response at 1 month and does not affect disease control at 1 year, compared with starting MTX simultaneously with the vaccination, according to data from a randomized trial presented at the annual European Congress of Rheumatology.
“Our patients are more susceptible to infection due to immunosuppressive therapy, and it’s recommended they receive vaccination against pneumococcal infection,” the lead author Jacques Morel, MD, PhD, said in his presentation of results from the VACIMRA study.
Timing the vaccination against pneumococcal disease when initiating MTX in clinical practice has been a point of uncertainty, noted Dr. Morel, a rheumatologist from Centre Hospitalier Universitaire, Montpellier, France.
“How can we deal with this in clinical practice where one recommendation is to vaccine before initiation of methotrexate, but it is also recommended to start methotrexate as soon as the diagnosis of RA is made?” he asked.
Comparing Humoral Response of MTX Started Immediately or 1 Month Post-Vaccination
The prospective, randomized, multicenter trial aimed to compare the rate of humoral immunological response against pneumococcal 13-valent conjugate vaccine (PCV13) in patients with RA who had a Disease Activity Score in 28 joints (DAS28) > 3.2, never taken MTX, and never been vaccinated against pneumococcus. Patients were vaccinated either 1 month before MTX initiation (n = 126) or simultaneously with MTX (n = 123). Oral glucocorticoids were allowed but only at < 10 mg/d. Following PCV13 vaccination, all patients also received the 23-valent pneumococcal polysaccharide vaccine (PPV23) 2 months later.
Concentrations of immunoglobulin (Ig) G antibodies against the 13 serotypes contained within PCV13 were measured using enzyme-linked immunosorbent assay (ELISA) and opsonophagocytic killing assay (OPA) at baseline and during follow-up at 1, 3, 6, and 12 months.
Positive antibody response was defined as a twofold or more increase in the IgG concentration using ELISA. The main outcome was the responder rates at 1 month after PCV13, defined by at least three positive antibody responses out of five of the target PVC13 serotypes (1, 3, 5, 7F, and 19A) using ELISA or OPA. Secondary outcomes included comparisons of the percentage of patients responding to each of the 13 vaccine serotypes at 1 month and after the boost with PPV23 and at 3, 6, and 12 months after vaccination with PCV13. The researchers also measured disease activity, infections, and side effects throughout the study.
Dr. Morel highlighted that all the patients had very early RA of less than 6 months, and that their characteristics at baseline were similar in both groups with 70% women, mean age 55.6 years, RA duration 2 months, 69% positive for anticitrullinated protein antibodies, 21% with erosive disease, and a DAS28 based on C-reactive protein of 4.6.
Response rates in those receiving MTX 1 month after vaccination were significantly higher at 88% with ELISA than those at 75% for immediate vaccination (P < .01) and 96% vs 88% with OPA (P = .02). These responder proportions persisted at the 12-month follow-up measurements, remaining higher in the delayed MTX group for both assays and across the 13 serotypes.
Showing a graph of the antibody responses, Dr. Morel explained that “at 12 months, the curves start to converge, but the difference in antibody titers were still significant for eight of the 13 serotypes.”
Disease Activity Not Adversely Affected by Starting MTX 1 Month Later
Regarding medication doses at 12 months, the cumulative glucocorticoid doses were similar between groups during the follow-up. As expected, the 1-year cumulative dose of MTX was higher in those given the drug immediately after vaccination vs delayed (826 vs 734 mg), but the weekly mean doses of MTX were similar at 3, 6, and 12 months between the two groups, and likewise, the use of targeted disease-modifying antirheumatic drugs (DMARDs) at 1 year was comparable. The cumulative glucocorticoid dose at 12 months was similar at 1716 mg with delayed MTX and 1613 mg with immediate MTX.
Not unexpectedly, at 1 month, DAS28 scores were higher with delayed vs immediate MTX at 3.95 vs 3.38 for DAS28-ESR and 3.54 vs 3.01 for DAS28-CRP (P < .01), but after the first month, DAS28 scores were similar between the two groups.
No significant differences were found between the groups for adverse event rates within 7 days of receiving PCV13, with local and systemic reactions occurring at 60%-61% and 50%-58%, respectively; fever at 0%-4%; and severe infections at 12%.
Finally, no difference was found in terms of serious adverse events between groups, with one pneumococcal infection with delayed MTX during follow-up, and there were no unexpected side effects observed with the PCV13 and PPV23 vaccinations.
Rheumatologists’ Reactions
Ernest Choy, MD, head of rheumatology and translational research at the Institute of Infection and Immunity, Cardiff University School of Medicine, Cardiff, Wales, asked if any individual showed no humoral response at all rather than a reduced response. “I ask because if there is no humoral response, then they are at very high risk, and there will be clinical relevance to that.”
Dr. Morel replied that “one serotype showed no response, at least according to the assays used, but we don’t know why. We analyzed at the population [level], not at the individual level, so it is difficult to answer the question.”
Another delegate asked what the participants thought about delaying MTX by 1 month. “When we tell the patient we need to vaccinate before we can use methotrexate [because] otherwise, we will reduce the response to the vaccination, then patient accepts it,” said Dr. Morel, adding that, “we allowed a minimal dose of steroids, and we saw from the results that the DAS28 at 1 month had changed.”
Co-moderator Katerina Chatzidionysiou, MD, PhD, a consultant rheumatologist and head of the Clinical Trial Department Rheumatology Unit, Karolinska University Hospital, Stockholm, Sweden, said that “As a physician, I’d feel uncomfortable delaying MTX if they had very active disease even for a short period of time.”
Dr. Morel replied that, “Today, we have so many drugs that can control the disease, for example, the targeted DMARDs. Progression does not show much variation, and we know x-ray progression with today’s drugs is a lot less than previously.”
Dr. Morel reported financial relationships with AbbVie, Amgen, Biogen, Bristol Myers Squibb, Fresenius Kabi, Galapagos, GlaxoSmithKline, Lilly, Medac, Nordic Pharma, Novartis, Pfizer, Sandoz, Sanofi, Boehringer Ingelheim, and Servier. Dr. Choy had no relevant financial relationships of relevance to this study.
A version of this article appeared on Medscape.com.
FROM EULAR 2024
Autoantibodies Nonspecific to Systemic Sclerosis May Play Role in ILD Prediction
VIENNA — Anti-Ro/SSA antibodies may help predict which patients with systemic sclerosis (SSc) are at a greater risk for interstitial lung disease (ILD) and may serve as a biomarker to guide screening, according to an analysis of data from a large European cohort.
The researchers were led by Blaž Burja, MD, PhD, a physician-scientist at the Center of Experimental Rheumatology, University Hospital Zürich, Switzerland, who reported that anti-Ro/SSA antibodies are a risk factor for ILD, with an odds ratio of 1.24, in patients with SSc.
At the annual European Congress of Rheumatology, he presented the findings of the study that aimed to find out if SSc-nonspecific antibodies might help better risk-stratify patients with SSc, focusing on lung involvement. “Among them, anti-Ro/SSA antibodies have been shown to be associated with interstitial lung disease in different connective tissue diseases,” Dr. Burja pointed out.
“A total of 15% of all patients in the SSc cohort presented with anti-Ro/SSA antibodies, and this subgroup presented with distinct clinical features: Importantly, higher prevalence of ILD and lower DLCO% [diffusing capacity of the lungs for carbon monoxide] in patients with established ILD,” reported Dr. Burja. “However, these anti-Ro/SSA antibodies do not predict ILD progression, death, or overall disease progression.”
Based on the findings, Dr. Burja suggested that these antibodies be incorporated into routine clinical practice to identify patients with SSc who have a high risk for ILD. He noted that “this has specific importance in clinical settings without availability of high-resolution computed tomography (HRCT), where anti-Ro/SSA antibodies could represent an additional biomarker to guide the screening process, in particular, in patients without SSc-specific antibodies.”
Caroline Ospelt, MD, PhD, co-moderator of the session and scientific program chair of EULAR 2024, told this news organization that the study was unique in its approach to studying ILD risk by “looking outside the box, so not just at specific antibodies but whether cross-disease antibodies may have value in stratifying patients and help predict risk of lung involvement and possibly monitor these patients.”
Dr. Ospelt, professor of experimental rheumatology at University Hospital Zürich, who was not involved in the study, noted: “It might also be the case that we could adapt this concept and use these antibodies in other rheumatic diseases, too, not just systemic sclerosis, to predict lung involvement.”
Risk-Stratifying With SSc-Nonspecific Antibodies
Dr. Burja explained that despite better stratification of patients with SSc with SSc-specific antibodies, “in clinical practice, we see large heterogeneity, and individual prognosis with regards to outcomes is still unpredictable, so we wanted to know whether by using nonspecific autoantibodies we might be better able to risk-stratify these patients.”
A study population of 4421 with at least one follow-up visit, including 3060 patients with available follow-up serologic data, was drawn from the European Scleroderma Trials and Research group database (n = 22,482). Of these 3060 patients, 461 were positive for anti-Ro/SSA antibodies and 2599 were negative. The researchers analyzed the relationships between baseline characteristics and the development or progression of ILD over 2.7 years of follow-up. Incident, de novo ILD was defined based on its presence on HRCT, and progression was defined by whether the percentage of predicted forced vital capacity (FVC%) dropped ≥ 10%, FVC% dropped 5%-9% in association with a DLCO% drop ≥ 15%, or FVC% dropped > 5%. Deaths from all causes and prognostic factors for the progression of lung fibrosis during follow-up were recorded.
High Prevalence of ILD With Anti-Ro/SSA Antibodies in SSc
At baseline, patients with anti-Ro/SSA antibodies were aged 55-56 years, 84%-87% were women, and muscular involvement was present in 18% of patients positive for anti-Ro/SSA antibodies and 12.5% of those who were negative (P < .001). According to HRCT, ILD was present in 56.2% of patients positive for anti-Ro/SSA antibodies and in 47.8% of those who were negative (P = .001). FVC% was 92.5% in patients positive for anti-Ro/SSA antibodies and 95.7% in those who were negative (P = .002). DLCO% was 66.9% in patients positive for anti-Ro/SSA antibodies and 71% in those who were negative (P < .001).
“A total of 15% of all SSc patients presented as positive for anti-Ro/SSA antibodies, and these patients all presented with higher prevalence of SSA-nonspecific antibodies, too: Of note, those with anti-La/SSB and anti-U1/RNP and rheumatoid factor,” Dr. Burja reported.
In patients with anti-U1/RNP autoantibodies, 1% were positive and 4% were negative for anti-Ro/SSA antibodies; in those with anti-La/SSB autoantibodies, 17% were positive and 1% were negative for anti-Ro/SSA antibodies; and in those with rheumatoid factor, 28% were positive and 14% were negative for anti-Ro/SSA antibodies.
Dr. Burja pointed out that the average disease duration in the study cohort at baseline was 7 years, “and at this timepoint, we expect to see some common disease manifestations. Specifically, higher muscular involvement and higher ILD based on HRCT.
“We decided to focus on patients with established ILD at baseline,” said Dr. Burja. “Anti-Ro/SSA-positive patients with established ILD at baseline presented with lower DLCO values at 59% in patients positive for anti-Ro/SSA antibodies and 61% for those who were negative.”
After conducting a multivariable analysis of 14,066 healthcare visits and adjusting for known risk factors for ILD, the researchers concluded that anti-Ro/SSA antibodies are an independent risk factor for ILD, with an odds ratio of 1.24 (95% CI, 1.07-1.44; P = .006). They also determined that anti-Ro/SSA antibodies are a risk factor for lower DLCO values in patients with ILD, with a regression coefficient of −1.93.
The researchers then explored the progression of ILD and overall disease progression and survival during the follow-up period in a longitudinal analysis. “However, anti-Ro/SSA antibodies were not found to predict the progression of ILD,” reported Dr. Burja, adding that this was true regardless of the definition of ILD progression used. “Nor did anti-Ro/SSA antibodies do not predict survival or overall disease progression.”
Dr. Burja pointed out the limitations in his study, including the lack of standardized criteria for all centers to assess anti-Ro/SSA positivity; there was a lack of discrimination between anti-Ro52 and anti-Ro60 subtypes, and there were no standardized applicable criteria to study lung progression in SSc.
Dr. Burja and Dr. Ospelt had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
VIENNA — Anti-Ro/SSA antibodies may help predict which patients with systemic sclerosis (SSc) are at a greater risk for interstitial lung disease (ILD) and may serve as a biomarker to guide screening, according to an analysis of data from a large European cohort.
The researchers were led by Blaž Burja, MD, PhD, a physician-scientist at the Center of Experimental Rheumatology, University Hospital Zürich, Switzerland, who reported that anti-Ro/SSA antibodies are a risk factor for ILD, with an odds ratio of 1.24, in patients with SSc.
At the annual European Congress of Rheumatology, he presented the findings of the study that aimed to find out if SSc-nonspecific antibodies might help better risk-stratify patients with SSc, focusing on lung involvement. “Among them, anti-Ro/SSA antibodies have been shown to be associated with interstitial lung disease in different connective tissue diseases,” Dr. Burja pointed out.
“A total of 15% of all patients in the SSc cohort presented with anti-Ro/SSA antibodies, and this subgroup presented with distinct clinical features: Importantly, higher prevalence of ILD and lower DLCO% [diffusing capacity of the lungs for carbon monoxide] in patients with established ILD,” reported Dr. Burja. “However, these anti-Ro/SSA antibodies do not predict ILD progression, death, or overall disease progression.”
Based on the findings, Dr. Burja suggested that these antibodies be incorporated into routine clinical practice to identify patients with SSc who have a high risk for ILD. He noted that “this has specific importance in clinical settings without availability of high-resolution computed tomography (HRCT), where anti-Ro/SSA antibodies could represent an additional biomarker to guide the screening process, in particular, in patients without SSc-specific antibodies.”
Caroline Ospelt, MD, PhD, co-moderator of the session and scientific program chair of EULAR 2024, told this news organization that the study was unique in its approach to studying ILD risk by “looking outside the box, so not just at specific antibodies but whether cross-disease antibodies may have value in stratifying patients and help predict risk of lung involvement and possibly monitor these patients.”
Dr. Ospelt, professor of experimental rheumatology at University Hospital Zürich, who was not involved in the study, noted: “It might also be the case that we could adapt this concept and use these antibodies in other rheumatic diseases, too, not just systemic sclerosis, to predict lung involvement.”
Risk-Stratifying With SSc-Nonspecific Antibodies
Dr. Burja explained that despite better stratification of patients with SSc with SSc-specific antibodies, “in clinical practice, we see large heterogeneity, and individual prognosis with regards to outcomes is still unpredictable, so we wanted to know whether by using nonspecific autoantibodies we might be better able to risk-stratify these patients.”
A study population of 4421 with at least one follow-up visit, including 3060 patients with available follow-up serologic data, was drawn from the European Scleroderma Trials and Research group database (n = 22,482). Of these 3060 patients, 461 were positive for anti-Ro/SSA antibodies and 2599 were negative. The researchers analyzed the relationships between baseline characteristics and the development or progression of ILD over 2.7 years of follow-up. Incident, de novo ILD was defined based on its presence on HRCT, and progression was defined by whether the percentage of predicted forced vital capacity (FVC%) dropped ≥ 10%, FVC% dropped 5%-9% in association with a DLCO% drop ≥ 15%, or FVC% dropped > 5%. Deaths from all causes and prognostic factors for the progression of lung fibrosis during follow-up were recorded.
High Prevalence of ILD With Anti-Ro/SSA Antibodies in SSc
At baseline, patients with anti-Ro/SSA antibodies were aged 55-56 years, 84%-87% were women, and muscular involvement was present in 18% of patients positive for anti-Ro/SSA antibodies and 12.5% of those who were negative (P < .001). According to HRCT, ILD was present in 56.2% of patients positive for anti-Ro/SSA antibodies and in 47.8% of those who were negative (P = .001). FVC% was 92.5% in patients positive for anti-Ro/SSA antibodies and 95.7% in those who were negative (P = .002). DLCO% was 66.9% in patients positive for anti-Ro/SSA antibodies and 71% in those who were negative (P < .001).
“A total of 15% of all SSc patients presented as positive for anti-Ro/SSA antibodies, and these patients all presented with higher prevalence of SSA-nonspecific antibodies, too: Of note, those with anti-La/SSB and anti-U1/RNP and rheumatoid factor,” Dr. Burja reported.
In patients with anti-U1/RNP autoantibodies, 1% were positive and 4% were negative for anti-Ro/SSA antibodies; in those with anti-La/SSB autoantibodies, 17% were positive and 1% were negative for anti-Ro/SSA antibodies; and in those with rheumatoid factor, 28% were positive and 14% were negative for anti-Ro/SSA antibodies.
Dr. Burja pointed out that the average disease duration in the study cohort at baseline was 7 years, “and at this timepoint, we expect to see some common disease manifestations. Specifically, higher muscular involvement and higher ILD based on HRCT.
“We decided to focus on patients with established ILD at baseline,” said Dr. Burja. “Anti-Ro/SSA-positive patients with established ILD at baseline presented with lower DLCO values at 59% in patients positive for anti-Ro/SSA antibodies and 61% for those who were negative.”
After conducting a multivariable analysis of 14,066 healthcare visits and adjusting for known risk factors for ILD, the researchers concluded that anti-Ro/SSA antibodies are an independent risk factor for ILD, with an odds ratio of 1.24 (95% CI, 1.07-1.44; P = .006). They also determined that anti-Ro/SSA antibodies are a risk factor for lower DLCO values in patients with ILD, with a regression coefficient of −1.93.
The researchers then explored the progression of ILD and overall disease progression and survival during the follow-up period in a longitudinal analysis. “However, anti-Ro/SSA antibodies were not found to predict the progression of ILD,” reported Dr. Burja, adding that this was true regardless of the definition of ILD progression used. “Nor did anti-Ro/SSA antibodies do not predict survival or overall disease progression.”
Dr. Burja pointed out the limitations in his study, including the lack of standardized criteria for all centers to assess anti-Ro/SSA positivity; there was a lack of discrimination between anti-Ro52 and anti-Ro60 subtypes, and there were no standardized applicable criteria to study lung progression in SSc.
Dr. Burja and Dr. Ospelt had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
VIENNA — Anti-Ro/SSA antibodies may help predict which patients with systemic sclerosis (SSc) are at a greater risk for interstitial lung disease (ILD) and may serve as a biomarker to guide screening, according to an analysis of data from a large European cohort.
The researchers were led by Blaž Burja, MD, PhD, a physician-scientist at the Center of Experimental Rheumatology, University Hospital Zürich, Switzerland, who reported that anti-Ro/SSA antibodies are a risk factor for ILD, with an odds ratio of 1.24, in patients with SSc.
At the annual European Congress of Rheumatology, he presented the findings of the study that aimed to find out if SSc-nonspecific antibodies might help better risk-stratify patients with SSc, focusing on lung involvement. “Among them, anti-Ro/SSA antibodies have been shown to be associated with interstitial lung disease in different connective tissue diseases,” Dr. Burja pointed out.
“A total of 15% of all patients in the SSc cohort presented with anti-Ro/SSA antibodies, and this subgroup presented with distinct clinical features: Importantly, higher prevalence of ILD and lower DLCO% [diffusing capacity of the lungs for carbon monoxide] in patients with established ILD,” reported Dr. Burja. “However, these anti-Ro/SSA antibodies do not predict ILD progression, death, or overall disease progression.”
Based on the findings, Dr. Burja suggested that these antibodies be incorporated into routine clinical practice to identify patients with SSc who have a high risk for ILD. He noted that “this has specific importance in clinical settings without availability of high-resolution computed tomography (HRCT), where anti-Ro/SSA antibodies could represent an additional biomarker to guide the screening process, in particular, in patients without SSc-specific antibodies.”
Caroline Ospelt, MD, PhD, co-moderator of the session and scientific program chair of EULAR 2024, told this news organization that the study was unique in its approach to studying ILD risk by “looking outside the box, so not just at specific antibodies but whether cross-disease antibodies may have value in stratifying patients and help predict risk of lung involvement and possibly monitor these patients.”
Dr. Ospelt, professor of experimental rheumatology at University Hospital Zürich, who was not involved in the study, noted: “It might also be the case that we could adapt this concept and use these antibodies in other rheumatic diseases, too, not just systemic sclerosis, to predict lung involvement.”
Risk-Stratifying With SSc-Nonspecific Antibodies
Dr. Burja explained that despite better stratification of patients with SSc with SSc-specific antibodies, “in clinical practice, we see large heterogeneity, and individual prognosis with regards to outcomes is still unpredictable, so we wanted to know whether by using nonspecific autoantibodies we might be better able to risk-stratify these patients.”
A study population of 4421 with at least one follow-up visit, including 3060 patients with available follow-up serologic data, was drawn from the European Scleroderma Trials and Research group database (n = 22,482). Of these 3060 patients, 461 were positive for anti-Ro/SSA antibodies and 2599 were negative. The researchers analyzed the relationships between baseline characteristics and the development or progression of ILD over 2.7 years of follow-up. Incident, de novo ILD was defined based on its presence on HRCT, and progression was defined by whether the percentage of predicted forced vital capacity (FVC%) dropped ≥ 10%, FVC% dropped 5%-9% in association with a DLCO% drop ≥ 15%, or FVC% dropped > 5%. Deaths from all causes and prognostic factors for the progression of lung fibrosis during follow-up were recorded.
High Prevalence of ILD With Anti-Ro/SSA Antibodies in SSc
At baseline, patients with anti-Ro/SSA antibodies were aged 55-56 years, 84%-87% were women, and muscular involvement was present in 18% of patients positive for anti-Ro/SSA antibodies and 12.5% of those who were negative (P < .001). According to HRCT, ILD was present in 56.2% of patients positive for anti-Ro/SSA antibodies and in 47.8% of those who were negative (P = .001). FVC% was 92.5% in patients positive for anti-Ro/SSA antibodies and 95.7% in those who were negative (P = .002). DLCO% was 66.9% in patients positive for anti-Ro/SSA antibodies and 71% in those who were negative (P < .001).
“A total of 15% of all SSc patients presented as positive for anti-Ro/SSA antibodies, and these patients all presented with higher prevalence of SSA-nonspecific antibodies, too: Of note, those with anti-La/SSB and anti-U1/RNP and rheumatoid factor,” Dr. Burja reported.
In patients with anti-U1/RNP autoantibodies, 1% were positive and 4% were negative for anti-Ro/SSA antibodies; in those with anti-La/SSB autoantibodies, 17% were positive and 1% were negative for anti-Ro/SSA antibodies; and in those with rheumatoid factor, 28% were positive and 14% were negative for anti-Ro/SSA antibodies.
Dr. Burja pointed out that the average disease duration in the study cohort at baseline was 7 years, “and at this timepoint, we expect to see some common disease manifestations. Specifically, higher muscular involvement and higher ILD based on HRCT.
“We decided to focus on patients with established ILD at baseline,” said Dr. Burja. “Anti-Ro/SSA-positive patients with established ILD at baseline presented with lower DLCO values at 59% in patients positive for anti-Ro/SSA antibodies and 61% for those who were negative.”
After conducting a multivariable analysis of 14,066 healthcare visits and adjusting for known risk factors for ILD, the researchers concluded that anti-Ro/SSA antibodies are an independent risk factor for ILD, with an odds ratio of 1.24 (95% CI, 1.07-1.44; P = .006). They also determined that anti-Ro/SSA antibodies are a risk factor for lower DLCO values in patients with ILD, with a regression coefficient of −1.93.
The researchers then explored the progression of ILD and overall disease progression and survival during the follow-up period in a longitudinal analysis. “However, anti-Ro/SSA antibodies were not found to predict the progression of ILD,” reported Dr. Burja, adding that this was true regardless of the definition of ILD progression used. “Nor did anti-Ro/SSA antibodies do not predict survival or overall disease progression.”
Dr. Burja pointed out the limitations in his study, including the lack of standardized criteria for all centers to assess anti-Ro/SSA positivity; there was a lack of discrimination between anti-Ro52 and anti-Ro60 subtypes, and there were no standardized applicable criteria to study lung progression in SSc.
Dr. Burja and Dr. Ospelt had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
FROM EULAR 2024
Low Infection Risk, Apart from Herpes Zoster, Seen in Real-World JAK Inhibitor Data for RA
VIENNA — In patients with rheumatoid arthritis (RA), Janus kinase inhibitors (JAKi) are associated with a substantially greater risk for herpes zoster, but the risk for other types of infections is about the same and often numerically lower relative to biologic disease-modifying antirheumatic drugs (bDMARDs), according to new data from the JAK-pot study.
“In the real world, we found no significantly greater risk of serious or nonserious infections, with the exception of herpes zoster,” said Romain Aymon, a statistician in the Department of Rheumatology at the University Hospital of Geneva, Switzerland.
This finding is the latest analysis generated by JAK-pot, a collaboration of 20 national registries to answer real-world questions about the efficacy and safety of JAKi in rheumatic diseases. These data have already been used to address such issues as relative rates of discontinuation for JAKi vs bDMARDs and to compare outcomes of RA patients who are switched to a bDMARD vs those who are cycled to another JAKi.
The main conclusion — that JAKi, relative to bDMARDs for RA, is associated with an increased risk for herpes zoster but not other types of infections — is not a surprise, according to Floris A. van Gaalen, MD, PhD, a clinician and researcher in the Department of Rheumatology, Leiden University in the Netherlands.
“There are a number of risks with JAK inhibitors that have generated concern, but I think most clinicians are aware that they should be warning patients about herpes zoster,” said Dr. van Gaalen, who was not involved in the study. He believes the risk is sufficient to warrant a discussion with patients about taking the herpes zoster vaccine prior to treatment.
“It is nice to have data indicating that risk of other infections is no higher with JAKi than other treatment options, but I am not sure this has been a big concern,” he said. “But I do think more information about other types of risks would be helpful.”
Relative Risk for Infection on JAKi Is Unclear
Although the greater risk for herpes zoster with JAKi vs bDMARDs is well established, the relative risk for other types of infections has been unclear, according to Mr. Aymon. One reason is that some, but not all, of the initial pivotal trials and safety studies associated JAKi with an increased risk for opportunistic infections, Mr. Aymon said.
The JAK-pot data, presented at the annual European Congress of Rheumatology, provide real-world data that shed light on this controversy, Mr. Aymon said.
Of the 20 national registries now providing data to JAK-pot, only 14 were included in this analysis. The study required data on infection rates from the time that JAKi became commercially available, which narrowed the data pool.
For this analysis, JAKi, which included tofacitinib (Xeljanz), baricitinib (Olumiant), upadacitinib (Rinvoq), and filgotinib (Jyseleca), were compared separately and together with two groups of bDMARDs. One consisted of the tumor necrosis factor inhibitors (TNFi), infliximab, etanercept, adalimumab, certolizumab pegol, or golimumab. The other was composed of bDMARDs with other modes of action (OMA). This group included abatacept, rituximab, sarilumab, and tocilizumab.
More Than 50,000 Exposures Included in Analysis
From the pooled registry, data were gathered from 13,374 courses of JAKi, 25,049 courses of TNFi, and 16,482 courses of OMA. There were some differences between these groups, including a significantly lower median age for those in the JAKi pool (57.1 years vs 58.3 and 60.5 years for TNFi and OMA, respectively) and median disease duration (8.3 years vs 11.0 and 11.9 years, respectively).
A greater proportion of patients on TNFi were naive to therapy (44.6%), compared with either JAKi (20.2%) or OMA (16.1%). More patients in the TNFi pool (60.0%) were also on concomitant therapy than those in the JAKi pool (49.5%) or the OMA pool (51.9%).
Other characteristics such as disease activity, body mass index, and percentage of smokers were comparable.
When TNFi was used as the reference, there were no significant differences in the rate of all infections, the rate of all infections excluding herpes zoster, and all serious infections. In all three groups, the incidence rates were numerically but not significantly lower in patients on JAKi vs OMA. With the exception of serious infections, for which the adjusted incidence of JAKi was 0.99 relative to TNFi, both JAKi and OMA had numerically higher incidence rate ratios than TNFi.
Herpes Zoster Risk on JAKi Is > Twofold Higher
Because the CIs overlapped in all cases, none of the differences were significant. The exception was herpes zoster. The 1.07 incidence rate ratio for OMA was not significantly different than the TNFi reference, but the 2.27 rate ratio for JAKi far exceeded either of the other two comparators (95% CI, 1.17-3.02).
In a separate analysis of patients at least 55 years of age with at least one cardiovascular risk factor, the numerical differences between groups were narrower and thus did not reach statistical significance, even for herpes zoster. Although the herpes zoster rate ratio was 1.62 for JAKi vs 1.23 for OMA (TNFi as the reference was 1.0), the CI for JAKi (0.86-3.03) overlapped both.
Based on a Poisson regression analysis, this study took into account a wide variety of variables, including age, disease activity, comorbidities, and tobacco use, Mr. Aymon said. He noted that the analyses were performed on data from each registry as well as with the pooled data, and the data were reasonably consistent.
Initially, the investigators had planned to evaluate differences between therapy groups, if any, for COVID-19 infection, but differences in the availability and use of vaccinations among the countries where the registries were maintained made this analysis too complicated to conduct.
Mr. Aymon reported no potential conflicts of interest, but some coauthors reported financial relationships with manufacturers of both bDMARDs and JAKi. Dr. van Gaalen reported financial relationships with AbbVie, Bristol Myers Squibb, Eli Lilly, Merck Sharp & Dohme, Novartis, and UCB.
A version of this article appeared on Medscape.com.
VIENNA — In patients with rheumatoid arthritis (RA), Janus kinase inhibitors (JAKi) are associated with a substantially greater risk for herpes zoster, but the risk for other types of infections is about the same and often numerically lower relative to biologic disease-modifying antirheumatic drugs (bDMARDs), according to new data from the JAK-pot study.
“In the real world, we found no significantly greater risk of serious or nonserious infections, with the exception of herpes zoster,” said Romain Aymon, a statistician in the Department of Rheumatology at the University Hospital of Geneva, Switzerland.
This finding is the latest analysis generated by JAK-pot, a collaboration of 20 national registries to answer real-world questions about the efficacy and safety of JAKi in rheumatic diseases. These data have already been used to address such issues as relative rates of discontinuation for JAKi vs bDMARDs and to compare outcomes of RA patients who are switched to a bDMARD vs those who are cycled to another JAKi.
The main conclusion — that JAKi, relative to bDMARDs for RA, is associated with an increased risk for herpes zoster but not other types of infections — is not a surprise, according to Floris A. van Gaalen, MD, PhD, a clinician and researcher in the Department of Rheumatology, Leiden University in the Netherlands.
“There are a number of risks with JAK inhibitors that have generated concern, but I think most clinicians are aware that they should be warning patients about herpes zoster,” said Dr. van Gaalen, who was not involved in the study. He believes the risk is sufficient to warrant a discussion with patients about taking the herpes zoster vaccine prior to treatment.
“It is nice to have data indicating that risk of other infections is no higher with JAKi than other treatment options, but I am not sure this has been a big concern,” he said. “But I do think more information about other types of risks would be helpful.”
Relative Risk for Infection on JAKi Is Unclear
Although the greater risk for herpes zoster with JAKi vs bDMARDs is well established, the relative risk for other types of infections has been unclear, according to Mr. Aymon. One reason is that some, but not all, of the initial pivotal trials and safety studies associated JAKi with an increased risk for opportunistic infections, Mr. Aymon said.
The JAK-pot data, presented at the annual European Congress of Rheumatology, provide real-world data that shed light on this controversy, Mr. Aymon said.
Of the 20 national registries now providing data to JAK-pot, only 14 were included in this analysis. The study required data on infection rates from the time that JAKi became commercially available, which narrowed the data pool.
For this analysis, JAKi, which included tofacitinib (Xeljanz), baricitinib (Olumiant), upadacitinib (Rinvoq), and filgotinib (Jyseleca), were compared separately and together with two groups of bDMARDs. One consisted of the tumor necrosis factor inhibitors (TNFi), infliximab, etanercept, adalimumab, certolizumab pegol, or golimumab. The other was composed of bDMARDs with other modes of action (OMA). This group included abatacept, rituximab, sarilumab, and tocilizumab.
More Than 50,000 Exposures Included in Analysis
From the pooled registry, data were gathered from 13,374 courses of JAKi, 25,049 courses of TNFi, and 16,482 courses of OMA. There were some differences between these groups, including a significantly lower median age for those in the JAKi pool (57.1 years vs 58.3 and 60.5 years for TNFi and OMA, respectively) and median disease duration (8.3 years vs 11.0 and 11.9 years, respectively).
A greater proportion of patients on TNFi were naive to therapy (44.6%), compared with either JAKi (20.2%) or OMA (16.1%). More patients in the TNFi pool (60.0%) were also on concomitant therapy than those in the JAKi pool (49.5%) or the OMA pool (51.9%).
Other characteristics such as disease activity, body mass index, and percentage of smokers were comparable.
When TNFi was used as the reference, there were no significant differences in the rate of all infections, the rate of all infections excluding herpes zoster, and all serious infections. In all three groups, the incidence rates were numerically but not significantly lower in patients on JAKi vs OMA. With the exception of serious infections, for which the adjusted incidence of JAKi was 0.99 relative to TNFi, both JAKi and OMA had numerically higher incidence rate ratios than TNFi.
Herpes Zoster Risk on JAKi Is > Twofold Higher
Because the CIs overlapped in all cases, none of the differences were significant. The exception was herpes zoster. The 1.07 incidence rate ratio for OMA was not significantly different than the TNFi reference, but the 2.27 rate ratio for JAKi far exceeded either of the other two comparators (95% CI, 1.17-3.02).
In a separate analysis of patients at least 55 years of age with at least one cardiovascular risk factor, the numerical differences between groups were narrower and thus did not reach statistical significance, even for herpes zoster. Although the herpes zoster rate ratio was 1.62 for JAKi vs 1.23 for OMA (TNFi as the reference was 1.0), the CI for JAKi (0.86-3.03) overlapped both.
Based on a Poisson regression analysis, this study took into account a wide variety of variables, including age, disease activity, comorbidities, and tobacco use, Mr. Aymon said. He noted that the analyses were performed on data from each registry as well as with the pooled data, and the data were reasonably consistent.
Initially, the investigators had planned to evaluate differences between therapy groups, if any, for COVID-19 infection, but differences in the availability and use of vaccinations among the countries where the registries were maintained made this analysis too complicated to conduct.
Mr. Aymon reported no potential conflicts of interest, but some coauthors reported financial relationships with manufacturers of both bDMARDs and JAKi. Dr. van Gaalen reported financial relationships with AbbVie, Bristol Myers Squibb, Eli Lilly, Merck Sharp & Dohme, Novartis, and UCB.
A version of this article appeared on Medscape.com.
VIENNA — In patients with rheumatoid arthritis (RA), Janus kinase inhibitors (JAKi) are associated with a substantially greater risk for herpes zoster, but the risk for other types of infections is about the same and often numerically lower relative to biologic disease-modifying antirheumatic drugs (bDMARDs), according to new data from the JAK-pot study.
“In the real world, we found no significantly greater risk of serious or nonserious infections, with the exception of herpes zoster,” said Romain Aymon, a statistician in the Department of Rheumatology at the University Hospital of Geneva, Switzerland.
This finding is the latest analysis generated by JAK-pot, a collaboration of 20 national registries to answer real-world questions about the efficacy and safety of JAKi in rheumatic diseases. These data have already been used to address such issues as relative rates of discontinuation for JAKi vs bDMARDs and to compare outcomes of RA patients who are switched to a bDMARD vs those who are cycled to another JAKi.
The main conclusion — that JAKi, relative to bDMARDs for RA, is associated with an increased risk for herpes zoster but not other types of infections — is not a surprise, according to Floris A. van Gaalen, MD, PhD, a clinician and researcher in the Department of Rheumatology, Leiden University in the Netherlands.
“There are a number of risks with JAK inhibitors that have generated concern, but I think most clinicians are aware that they should be warning patients about herpes zoster,” said Dr. van Gaalen, who was not involved in the study. He believes the risk is sufficient to warrant a discussion with patients about taking the herpes zoster vaccine prior to treatment.
“It is nice to have data indicating that risk of other infections is no higher with JAKi than other treatment options, but I am not sure this has been a big concern,” he said. “But I do think more information about other types of risks would be helpful.”
Relative Risk for Infection on JAKi Is Unclear
Although the greater risk for herpes zoster with JAKi vs bDMARDs is well established, the relative risk for other types of infections has been unclear, according to Mr. Aymon. One reason is that some, but not all, of the initial pivotal trials and safety studies associated JAKi with an increased risk for opportunistic infections, Mr. Aymon said.
The JAK-pot data, presented at the annual European Congress of Rheumatology, provide real-world data that shed light on this controversy, Mr. Aymon said.
Of the 20 national registries now providing data to JAK-pot, only 14 were included in this analysis. The study required data on infection rates from the time that JAKi became commercially available, which narrowed the data pool.
For this analysis, JAKi, which included tofacitinib (Xeljanz), baricitinib (Olumiant), upadacitinib (Rinvoq), and filgotinib (Jyseleca), were compared separately and together with two groups of bDMARDs. One consisted of the tumor necrosis factor inhibitors (TNFi), infliximab, etanercept, adalimumab, certolizumab pegol, or golimumab. The other was composed of bDMARDs with other modes of action (OMA). This group included abatacept, rituximab, sarilumab, and tocilizumab.
More Than 50,000 Exposures Included in Analysis
From the pooled registry, data were gathered from 13,374 courses of JAKi, 25,049 courses of TNFi, and 16,482 courses of OMA. There were some differences between these groups, including a significantly lower median age for those in the JAKi pool (57.1 years vs 58.3 and 60.5 years for TNFi and OMA, respectively) and median disease duration (8.3 years vs 11.0 and 11.9 years, respectively).
A greater proportion of patients on TNFi were naive to therapy (44.6%), compared with either JAKi (20.2%) or OMA (16.1%). More patients in the TNFi pool (60.0%) were also on concomitant therapy than those in the JAKi pool (49.5%) or the OMA pool (51.9%).
Other characteristics such as disease activity, body mass index, and percentage of smokers were comparable.
When TNFi was used as the reference, there were no significant differences in the rate of all infections, the rate of all infections excluding herpes zoster, and all serious infections. In all three groups, the incidence rates were numerically but not significantly lower in patients on JAKi vs OMA. With the exception of serious infections, for which the adjusted incidence of JAKi was 0.99 relative to TNFi, both JAKi and OMA had numerically higher incidence rate ratios than TNFi.
Herpes Zoster Risk on JAKi Is > Twofold Higher
Because the CIs overlapped in all cases, none of the differences were significant. The exception was herpes zoster. The 1.07 incidence rate ratio for OMA was not significantly different than the TNFi reference, but the 2.27 rate ratio for JAKi far exceeded either of the other two comparators (95% CI, 1.17-3.02).
In a separate analysis of patients at least 55 years of age with at least one cardiovascular risk factor, the numerical differences between groups were narrower and thus did not reach statistical significance, even for herpes zoster. Although the herpes zoster rate ratio was 1.62 for JAKi vs 1.23 for OMA (TNFi as the reference was 1.0), the CI for JAKi (0.86-3.03) overlapped both.
Based on a Poisson regression analysis, this study took into account a wide variety of variables, including age, disease activity, comorbidities, and tobacco use, Mr. Aymon said. He noted that the analyses were performed on data from each registry as well as with the pooled data, and the data were reasonably consistent.
Initially, the investigators had planned to evaluate differences between therapy groups, if any, for COVID-19 infection, but differences in the availability and use of vaccinations among the countries where the registries were maintained made this analysis too complicated to conduct.
Mr. Aymon reported no potential conflicts of interest, but some coauthors reported financial relationships with manufacturers of both bDMARDs and JAKi. Dr. van Gaalen reported financial relationships with AbbVie, Bristol Myers Squibb, Eli Lilly, Merck Sharp & Dohme, Novartis, and UCB.
A version of this article appeared on Medscape.com.
FROM EULAR 2024
Upadacitinib Proves Successful in First JAK Inhibitor Trial for Giant Cell Arteritis
VIENNA — Results from the phase 3 SELECT-GCA study showed that the Janus kinase (JAK) inhibitor upadacitinib (Rinvoq) induces significant and sustained remission in people with new-onset or relapsing giant cell arteritis (GCA).
The primary endpoint of sustained remission — the absence of GCA signs or symptoms from weeks 12 to 52 together with adherence to a steroid-tapering regimen — occurred in 46% of 210 individuals randomly assigned to treatment treated with a once-daily 15-mg dose of upadacitinib and 29% of 105 randomly assigned to placebo (P = .0019).
Nine of the 11 secondary endpoints were also positive for upadacitinib 15 mg vs placebo, and no new safety concerns were identified in a late-breaking abstract presented at the at the annual European Congress of Rheumatology.
First JAK Trial in GCA
This is the first trial to look at the use of a JAK inhibitor for the treatment of GCA, and it is addressing a real unmet need, the presenting study investigator Daniel Blockmans, MD, PhD, of University Hospitals Leuven in Belgium, told this news organization.
Glucocorticoids remain the mainstay of treatment, and tocilizumab has been licensed for use, but people don’t always get better or can relapse, he explained.
“I have the impression that these only suppress the disease but do not cure it,” Dr. Blockmans said, adding that “patients get very well soon after these treatments are started, but there are more and more reports that there is a kind of smoldering vasculitis that exists, and this can lead to dilatation of the aorta.”
Upadacitinib inhibits two JAK-dependent cytokines, interleukin 6 and interferon gamma, which have been implicated in the pathogenesis of GCA. The latter could be particularly important, Dr. Blockmans suggested.
Study Details
SELECT-GCA is an ongoing multicenter, randomized, double-blind, placebo-controlled study designed to evaluate the safety and efficacy of upadacitinib vs placebo in patients with GCA.
A total of 428 patients have been included: 210 were randomly allocated to treatment with upadacitinib 15 mg, 105 to upadacitinib 7.5 mg, and 105 to placebo. The inclusion of the lower “minimally effective” upadacitinib dose was a requirement of the regulatory authorities, Dr. Blockmans said; the licensed dose in rheumatoid arthritis (RA) is 15 mg.
Dr. Blockmans reported data from the first 52 weeks of the trial during which all patients underwent glucocorticoid tapering — 26 weeks for upadacitinib and 52 weeks for placebo.
No imaging was done in this trial, which Dr. Blockmans said should be considered for future studies.
Secondary Endpoints
One of the key secondary endpoints was sustained complete remission, defined as sustained remission plus a normalized erythrocyte sedimentation rate to ≤ 30 mm/h and reducing high-sensitivity C-reactive protein to < 1 mg/dL.
Sustained complete remission occurred in 37% and 16% of patients treated with upadacitinib 15 mg and placebo, respectively (P < .0001).
Additionally, a significantly lower proportion of upadacitinib 15 mg- than placebo-treated patients experienced at least one disease flare through week 52 (34% vs 56%, P = .0014).
Other positive secondary endpoints for upadacitinib 15 mg vs placebo out to week 52 were the number of disease flares per patient, cumulative glucocorticoid exposure, and complete remission (also at week 24).
And significant changes in SF-36 and FACIT-Fatigue from baseline to week 52 were seen for upadacitinib 15 mg.
The only secondary endpoints not showing a clear benefit for upadacitinib 15 mg were the changes in the Treatment Satisfaction Questionnaire for Medication at 52 weeks and the rate of glucocorticoid-related adverse events through week 52.
As for the 7.5-mg dose of upadacitinib, neither the primary nor secondary endpoints were significantly better vs placebo.
‘Life-Changing’
The study’s findings could be “really life-changing” for patients with this type of vasculitis if upadacitinib gets approval for use in this indication, Milena Bond, MD, PhD, of Brunico Hospital in Italy, told this news organization at the meeting.
“Unfortunately, nowadays, we still have only a few options for treating these patients,” she said. “So, this drug could be really, really important.”
Dr. Bond added: “The data ... also shows there is a very good safety profile, which was a main concern given the class of the drug. So, I’m very positive about this treatment and very excited to see the preliminary results.”
After his presentation, Dr. Blockmans said, “Of course, if we already had an ideal treatment for GCA, there would be no need for a JAK inhibitor, but I don’t think that steroid treatment or tocilizumab treatment is the ideal treatment.”
Judicious Use Still Warranted
Upadacitinib still needs to be used cautiously, following appropriate guidance from the European Medicines Agency (EMA) and the US Food and Drug Administration.
Dr. Bond said: “It is not advised to use to the drug when people are older than 65 years old,” according to the EMA, for example, and “given the rules that we have, I would not use this drug as a first-line treatment. We do not do that for rheumatoid arthritis.”
But, she added, “As for arthritis, when you fail treating patients with the other alternatives, you could use this drug, and you have to discuss risks with the patients.”
Dr. Blockmans reported there had been no increased risk for major adverse cardiovascular events or venous thromboembolism associated with upadacitinib relative to placebo in the population of patients studied, and he pointed out that they had a much higher risk for these events than perhaps an RA population.
He said: “It’s effective, and it’s apparently safe in these older people, despite what we heard about tofacitinib in the ORAL [Surveillance] study; we didn’t see these problems here in this elderly population.”
The SELECT-GCA trial was funded by AbbVie, and the company participated in all aspects of the study, including its design, conduct, interpretation of data, and reporting. Dr. Blockmans received no funding or other honoraria from the company but reported a research grant from Roche and consulting fees from GlaxoSmithKline. Most of his coauthors reported financial relationships with AbbVie, and some are employees of the company. Dr. Bond reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
VIENNA — Results from the phase 3 SELECT-GCA study showed that the Janus kinase (JAK) inhibitor upadacitinib (Rinvoq) induces significant and sustained remission in people with new-onset or relapsing giant cell arteritis (GCA).
The primary endpoint of sustained remission — the absence of GCA signs or symptoms from weeks 12 to 52 together with adherence to a steroid-tapering regimen — occurred in 46% of 210 individuals randomly assigned to treatment treated with a once-daily 15-mg dose of upadacitinib and 29% of 105 randomly assigned to placebo (P = .0019).
Nine of the 11 secondary endpoints were also positive for upadacitinib 15 mg vs placebo, and no new safety concerns were identified in a late-breaking abstract presented at the at the annual European Congress of Rheumatology.
First JAK Trial in GCA
This is the first trial to look at the use of a JAK inhibitor for the treatment of GCA, and it is addressing a real unmet need, the presenting study investigator Daniel Blockmans, MD, PhD, of University Hospitals Leuven in Belgium, told this news organization.
Glucocorticoids remain the mainstay of treatment, and tocilizumab has been licensed for use, but people don’t always get better or can relapse, he explained.
“I have the impression that these only suppress the disease but do not cure it,” Dr. Blockmans said, adding that “patients get very well soon after these treatments are started, but there are more and more reports that there is a kind of smoldering vasculitis that exists, and this can lead to dilatation of the aorta.”
Upadacitinib inhibits two JAK-dependent cytokines, interleukin 6 and interferon gamma, which have been implicated in the pathogenesis of GCA. The latter could be particularly important, Dr. Blockmans suggested.
Study Details
SELECT-GCA is an ongoing multicenter, randomized, double-blind, placebo-controlled study designed to evaluate the safety and efficacy of upadacitinib vs placebo in patients with GCA.
A total of 428 patients have been included: 210 were randomly allocated to treatment with upadacitinib 15 mg, 105 to upadacitinib 7.5 mg, and 105 to placebo. The inclusion of the lower “minimally effective” upadacitinib dose was a requirement of the regulatory authorities, Dr. Blockmans said; the licensed dose in rheumatoid arthritis (RA) is 15 mg.
Dr. Blockmans reported data from the first 52 weeks of the trial during which all patients underwent glucocorticoid tapering — 26 weeks for upadacitinib and 52 weeks for placebo.
No imaging was done in this trial, which Dr. Blockmans said should be considered for future studies.
Secondary Endpoints
One of the key secondary endpoints was sustained complete remission, defined as sustained remission plus a normalized erythrocyte sedimentation rate to ≤ 30 mm/h and reducing high-sensitivity C-reactive protein to < 1 mg/dL.
Sustained complete remission occurred in 37% and 16% of patients treated with upadacitinib 15 mg and placebo, respectively (P < .0001).
Additionally, a significantly lower proportion of upadacitinib 15 mg- than placebo-treated patients experienced at least one disease flare through week 52 (34% vs 56%, P = .0014).
Other positive secondary endpoints for upadacitinib 15 mg vs placebo out to week 52 were the number of disease flares per patient, cumulative glucocorticoid exposure, and complete remission (also at week 24).
And significant changes in SF-36 and FACIT-Fatigue from baseline to week 52 were seen for upadacitinib 15 mg.
The only secondary endpoints not showing a clear benefit for upadacitinib 15 mg were the changes in the Treatment Satisfaction Questionnaire for Medication at 52 weeks and the rate of glucocorticoid-related adverse events through week 52.
As for the 7.5-mg dose of upadacitinib, neither the primary nor secondary endpoints were significantly better vs placebo.
‘Life-Changing’
The study’s findings could be “really life-changing” for patients with this type of vasculitis if upadacitinib gets approval for use in this indication, Milena Bond, MD, PhD, of Brunico Hospital in Italy, told this news organization at the meeting.
“Unfortunately, nowadays, we still have only a few options for treating these patients,” she said. “So, this drug could be really, really important.”
Dr. Bond added: “The data ... also shows there is a very good safety profile, which was a main concern given the class of the drug. So, I’m very positive about this treatment and very excited to see the preliminary results.”
After his presentation, Dr. Blockmans said, “Of course, if we already had an ideal treatment for GCA, there would be no need for a JAK inhibitor, but I don’t think that steroid treatment or tocilizumab treatment is the ideal treatment.”
Judicious Use Still Warranted
Upadacitinib still needs to be used cautiously, following appropriate guidance from the European Medicines Agency (EMA) and the US Food and Drug Administration.
Dr. Bond said: “It is not advised to use to the drug when people are older than 65 years old,” according to the EMA, for example, and “given the rules that we have, I would not use this drug as a first-line treatment. We do not do that for rheumatoid arthritis.”
But, she added, “As for arthritis, when you fail treating patients with the other alternatives, you could use this drug, and you have to discuss risks with the patients.”
Dr. Blockmans reported there had been no increased risk for major adverse cardiovascular events or venous thromboembolism associated with upadacitinib relative to placebo in the population of patients studied, and he pointed out that they had a much higher risk for these events than perhaps an RA population.
He said: “It’s effective, and it’s apparently safe in these older people, despite what we heard about tofacitinib in the ORAL [Surveillance] study; we didn’t see these problems here in this elderly population.”
The SELECT-GCA trial was funded by AbbVie, and the company participated in all aspects of the study, including its design, conduct, interpretation of data, and reporting. Dr. Blockmans received no funding or other honoraria from the company but reported a research grant from Roche and consulting fees from GlaxoSmithKline. Most of his coauthors reported financial relationships with AbbVie, and some are employees of the company. Dr. Bond reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
VIENNA — Results from the phase 3 SELECT-GCA study showed that the Janus kinase (JAK) inhibitor upadacitinib (Rinvoq) induces significant and sustained remission in people with new-onset or relapsing giant cell arteritis (GCA).
The primary endpoint of sustained remission — the absence of GCA signs or symptoms from weeks 12 to 52 together with adherence to a steroid-tapering regimen — occurred in 46% of 210 individuals randomly assigned to treatment treated with a once-daily 15-mg dose of upadacitinib and 29% of 105 randomly assigned to placebo (P = .0019).
Nine of the 11 secondary endpoints were also positive for upadacitinib 15 mg vs placebo, and no new safety concerns were identified in a late-breaking abstract presented at the at the annual European Congress of Rheumatology.
First JAK Trial in GCA
This is the first trial to look at the use of a JAK inhibitor for the treatment of GCA, and it is addressing a real unmet need, the presenting study investigator Daniel Blockmans, MD, PhD, of University Hospitals Leuven in Belgium, told this news organization.
Glucocorticoids remain the mainstay of treatment, and tocilizumab has been licensed for use, but people don’t always get better or can relapse, he explained.
“I have the impression that these only suppress the disease but do not cure it,” Dr. Blockmans said, adding that “patients get very well soon after these treatments are started, but there are more and more reports that there is a kind of smoldering vasculitis that exists, and this can lead to dilatation of the aorta.”
Upadacitinib inhibits two JAK-dependent cytokines, interleukin 6 and interferon gamma, which have been implicated in the pathogenesis of GCA. The latter could be particularly important, Dr. Blockmans suggested.
Study Details
SELECT-GCA is an ongoing multicenter, randomized, double-blind, placebo-controlled study designed to evaluate the safety and efficacy of upadacitinib vs placebo in patients with GCA.
A total of 428 patients have been included: 210 were randomly allocated to treatment with upadacitinib 15 mg, 105 to upadacitinib 7.5 mg, and 105 to placebo. The inclusion of the lower “minimally effective” upadacitinib dose was a requirement of the regulatory authorities, Dr. Blockmans said; the licensed dose in rheumatoid arthritis (RA) is 15 mg.
Dr. Blockmans reported data from the first 52 weeks of the trial during which all patients underwent glucocorticoid tapering — 26 weeks for upadacitinib and 52 weeks for placebo.
No imaging was done in this trial, which Dr. Blockmans said should be considered for future studies.
Secondary Endpoints
One of the key secondary endpoints was sustained complete remission, defined as sustained remission plus a normalized erythrocyte sedimentation rate to ≤ 30 mm/h and reducing high-sensitivity C-reactive protein to < 1 mg/dL.
Sustained complete remission occurred in 37% and 16% of patients treated with upadacitinib 15 mg and placebo, respectively (P < .0001).
Additionally, a significantly lower proportion of upadacitinib 15 mg- than placebo-treated patients experienced at least one disease flare through week 52 (34% vs 56%, P = .0014).
Other positive secondary endpoints for upadacitinib 15 mg vs placebo out to week 52 were the number of disease flares per patient, cumulative glucocorticoid exposure, and complete remission (also at week 24).
And significant changes in SF-36 and FACIT-Fatigue from baseline to week 52 were seen for upadacitinib 15 mg.
The only secondary endpoints not showing a clear benefit for upadacitinib 15 mg were the changes in the Treatment Satisfaction Questionnaire for Medication at 52 weeks and the rate of glucocorticoid-related adverse events through week 52.
As for the 7.5-mg dose of upadacitinib, neither the primary nor secondary endpoints were significantly better vs placebo.
‘Life-Changing’
The study’s findings could be “really life-changing” for patients with this type of vasculitis if upadacitinib gets approval for use in this indication, Milena Bond, MD, PhD, of Brunico Hospital in Italy, told this news organization at the meeting.
“Unfortunately, nowadays, we still have only a few options for treating these patients,” she said. “So, this drug could be really, really important.”
Dr. Bond added: “The data ... also shows there is a very good safety profile, which was a main concern given the class of the drug. So, I’m very positive about this treatment and very excited to see the preliminary results.”
After his presentation, Dr. Blockmans said, “Of course, if we already had an ideal treatment for GCA, there would be no need for a JAK inhibitor, but I don’t think that steroid treatment or tocilizumab treatment is the ideal treatment.”
Judicious Use Still Warranted
Upadacitinib still needs to be used cautiously, following appropriate guidance from the European Medicines Agency (EMA) and the US Food and Drug Administration.
Dr. Bond said: “It is not advised to use to the drug when people are older than 65 years old,” according to the EMA, for example, and “given the rules that we have, I would not use this drug as a first-line treatment. We do not do that for rheumatoid arthritis.”
But, she added, “As for arthritis, when you fail treating patients with the other alternatives, you could use this drug, and you have to discuss risks with the patients.”
Dr. Blockmans reported there had been no increased risk for major adverse cardiovascular events or venous thromboembolism associated with upadacitinib relative to placebo in the population of patients studied, and he pointed out that they had a much higher risk for these events than perhaps an RA population.
He said: “It’s effective, and it’s apparently safe in these older people, despite what we heard about tofacitinib in the ORAL [Surveillance] study; we didn’t see these problems here in this elderly population.”
The SELECT-GCA trial was funded by AbbVie, and the company participated in all aspects of the study, including its design, conduct, interpretation of data, and reporting. Dr. Blockmans received no funding or other honoraria from the company but reported a research grant from Roche and consulting fees from GlaxoSmithKline. Most of his coauthors reported financial relationships with AbbVie, and some are employees of the company. Dr. Bond reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM EULAR 2024
USPSTF Draft Recommendations Support More Options for Osteoporosis Screening, Seek More Research in Men
An influential US panel may largely reaffirm its current recommendation in favor of screening older women to prevent osteoporotic fractures, while also repeating its call for more research to try to determine whether men would benefit from this kind of routine testing.
The US Preventive Services Task Force (USPSTF) on June 11 released a draft update of its recommendations on osteoporosis screening. The task force will accept comments on the draft through July 8. Federal law gives the USPSTF recommendations extra clout, requiring insurers to cover — without co-pay — services that get top marks “A” or “B” from the task force.
The task force intends to maintain a “B” recommendation on screening of older women, indicating that the evidence gathered to date suggests a moderate net benefit. But the draft includes a shift in the approach to this screening.
The USPSTF proposed saying that it recommends screening for osteoporosis in both women aged 65 years and older and postmenopausal women younger than 65 years who are at an increased risk for an osteoporotic fracture. The current recommendation, finalized in 2018, advises “screening for osteoporosis with bone measurement testing [emphasis added]” for these groups.
The proposed change in language — dropping the phrase “with bone measurement testing” — is intended to expand flexibility for clinicians, Esa Davis, MD, MPH, a member of USPSTF and a professor at the University of Maryland School of Medicine, Baltimore, told this news organization.
“It provides them with more options instead of telling them, ‘You have to do it this way,’ ” Dr. Davis said.
The task force’s draft recommendation is not meant to apply to people with secondary osteoporosis due to an underlying medical condition such as cancer, metabolic bone diseases or hyperthyroidism, or chronic use of a medication associated with bone loss.
Rajesh K. Jain, MD, who was not involved with the USPSTF work, read the draft recommendations at the request of this news organization. In an email, he said he generally agreed with the decision to largely stick to the 2018 recommendations for women.
He also noted that there’s still a lack of a clear direction for physicians about assessing osteoporosis risk in men. But multiple randomized control trials of osteoporosis drugs seem to suggest these medicines work for both sexes, said Dr. Jain, who is the endocrinology fellowship program director at University of Chicago Medicine, Chicago.
The USPSTF draft also would reiterate the current “I” grade about screening men for osteoporosis.
An “I” grade means the task force found the current body of available evidence is insufficient to assess the balance of benefits and harms of screening for osteoporosis to prevent osteoporotic fractures in men.
“Since there is no recommendation right now, it would have seemed sensible to include a recommendation to screen men with prior fracture or other risk factors for osteoporosis, much like they do for younger women,” Dr. Jain said.
Insufficient Evidence
The USPSTF’s “I” grade is different from a “D” grade, which is what the task force uses to recommend against the use of a service.
A “D” grade means the USPSTF says there is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. (The USPSTF makes it easy to search online for grades given to preventive services, including those that got a “D.”)
The USPSTF is calling for more studies on the benefits and harms of screening for osteoporosis to prevent fractures and related morbidity and mortality in men.
“Men do get osteoporosis,” Dr. Davis said. “But unfortunately, the evidence isn’t there” to allow USPSTF to make a recommendation on screening approaches.
“Any man who has concerns about bone health should certainly talk to his clinician and figure out what is the best form of screening” he might want to do, she said.
There’s been a growing interest in the question of whether to screen men for osteoporosis and bone health. For example, Osteoporosis Canada last year updated a guideline to emphasize the need to assess older patients of both sexes for the risk for fractures. But the Canadian Task Force on Preventive Health Care in 2023 came to a conclusion in line with the USPSTF draft.
The Canadian task force recommended against routine screening in men, while adding that clinicians should be alert to changes in health that may indicate the patient has experienced or is at a higher risk for fragility fracture.
Risk Factors, Concerns About Tests
The USPSTF said that risk factors associated with fragility fractures are similar in men and women. These include:
- Increasing age
- Low body mass index
- Excessive alcohol intake
- Current smoking
- Chronic corticosteroid use
- History of prior fractures, falls within the past year, cerebrovascular accident, and diabetes
- Hypogonadism
The process of updating the USPSTF recommendations can serve as a chance to expand public awareness about osteoporosis, as many men may not know to raise the question of their fracture risk during medical appointments, Dr. Davis said.
“Clinicians need to be aware of the risk factors and to be able to have conversations with men,” she said.
Dr. Davis also cautioned about the need to be aware of limitations with clinical risk assessment tools. In the draft recommendation statement, the USPSTF noted that some tools and approaches may be less likely to identify Black, Hispanic, and Asian people as high risk, and subsequently, clinicians may be less likely to offer treatment to them compared with White people of the same age, bone mineral density, and clinical risk profile.
Dr. Davis had no relevant financial relationships. Dr. Jain received research funding from the Amgen Foundation.
A version of this article appeared on Medscape.com.
An influential US panel may largely reaffirm its current recommendation in favor of screening older women to prevent osteoporotic fractures, while also repeating its call for more research to try to determine whether men would benefit from this kind of routine testing.
The US Preventive Services Task Force (USPSTF) on June 11 released a draft update of its recommendations on osteoporosis screening. The task force will accept comments on the draft through July 8. Federal law gives the USPSTF recommendations extra clout, requiring insurers to cover — without co-pay — services that get top marks “A” or “B” from the task force.
The task force intends to maintain a “B” recommendation on screening of older women, indicating that the evidence gathered to date suggests a moderate net benefit. But the draft includes a shift in the approach to this screening.
The USPSTF proposed saying that it recommends screening for osteoporosis in both women aged 65 years and older and postmenopausal women younger than 65 years who are at an increased risk for an osteoporotic fracture. The current recommendation, finalized in 2018, advises “screening for osteoporosis with bone measurement testing [emphasis added]” for these groups.
The proposed change in language — dropping the phrase “with bone measurement testing” — is intended to expand flexibility for clinicians, Esa Davis, MD, MPH, a member of USPSTF and a professor at the University of Maryland School of Medicine, Baltimore, told this news organization.
“It provides them with more options instead of telling them, ‘You have to do it this way,’ ” Dr. Davis said.
The task force’s draft recommendation is not meant to apply to people with secondary osteoporosis due to an underlying medical condition such as cancer, metabolic bone diseases or hyperthyroidism, or chronic use of a medication associated with bone loss.
Rajesh K. Jain, MD, who was not involved with the USPSTF work, read the draft recommendations at the request of this news organization. In an email, he said he generally agreed with the decision to largely stick to the 2018 recommendations for women.
He also noted that there’s still a lack of a clear direction for physicians about assessing osteoporosis risk in men. But multiple randomized control trials of osteoporosis drugs seem to suggest these medicines work for both sexes, said Dr. Jain, who is the endocrinology fellowship program director at University of Chicago Medicine, Chicago.
The USPSTF draft also would reiterate the current “I” grade about screening men for osteoporosis.
An “I” grade means the task force found the current body of available evidence is insufficient to assess the balance of benefits and harms of screening for osteoporosis to prevent osteoporotic fractures in men.
“Since there is no recommendation right now, it would have seemed sensible to include a recommendation to screen men with prior fracture or other risk factors for osteoporosis, much like they do for younger women,” Dr. Jain said.
Insufficient Evidence
The USPSTF’s “I” grade is different from a “D” grade, which is what the task force uses to recommend against the use of a service.
A “D” grade means the USPSTF says there is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. (The USPSTF makes it easy to search online for grades given to preventive services, including those that got a “D.”)
The USPSTF is calling for more studies on the benefits and harms of screening for osteoporosis to prevent fractures and related morbidity and mortality in men.
“Men do get osteoporosis,” Dr. Davis said. “But unfortunately, the evidence isn’t there” to allow USPSTF to make a recommendation on screening approaches.
“Any man who has concerns about bone health should certainly talk to his clinician and figure out what is the best form of screening” he might want to do, she said.
There’s been a growing interest in the question of whether to screen men for osteoporosis and bone health. For example, Osteoporosis Canada last year updated a guideline to emphasize the need to assess older patients of both sexes for the risk for fractures. But the Canadian Task Force on Preventive Health Care in 2023 came to a conclusion in line with the USPSTF draft.
The Canadian task force recommended against routine screening in men, while adding that clinicians should be alert to changes in health that may indicate the patient has experienced or is at a higher risk for fragility fracture.
Risk Factors, Concerns About Tests
The USPSTF said that risk factors associated with fragility fractures are similar in men and women. These include:
- Increasing age
- Low body mass index
- Excessive alcohol intake
- Current smoking
- Chronic corticosteroid use
- History of prior fractures, falls within the past year, cerebrovascular accident, and diabetes
- Hypogonadism
The process of updating the USPSTF recommendations can serve as a chance to expand public awareness about osteoporosis, as many men may not know to raise the question of their fracture risk during medical appointments, Dr. Davis said.
“Clinicians need to be aware of the risk factors and to be able to have conversations with men,” she said.
Dr. Davis also cautioned about the need to be aware of limitations with clinical risk assessment tools. In the draft recommendation statement, the USPSTF noted that some tools and approaches may be less likely to identify Black, Hispanic, and Asian people as high risk, and subsequently, clinicians may be less likely to offer treatment to them compared with White people of the same age, bone mineral density, and clinical risk profile.
Dr. Davis had no relevant financial relationships. Dr. Jain received research funding from the Amgen Foundation.
A version of this article appeared on Medscape.com.
An influential US panel may largely reaffirm its current recommendation in favor of screening older women to prevent osteoporotic fractures, while also repeating its call for more research to try to determine whether men would benefit from this kind of routine testing.
The US Preventive Services Task Force (USPSTF) on June 11 released a draft update of its recommendations on osteoporosis screening. The task force will accept comments on the draft through July 8. Federal law gives the USPSTF recommendations extra clout, requiring insurers to cover — without co-pay — services that get top marks “A” or “B” from the task force.
The task force intends to maintain a “B” recommendation on screening of older women, indicating that the evidence gathered to date suggests a moderate net benefit. But the draft includes a shift in the approach to this screening.
The USPSTF proposed saying that it recommends screening for osteoporosis in both women aged 65 years and older and postmenopausal women younger than 65 years who are at an increased risk for an osteoporotic fracture. The current recommendation, finalized in 2018, advises “screening for osteoporosis with bone measurement testing [emphasis added]” for these groups.
The proposed change in language — dropping the phrase “with bone measurement testing” — is intended to expand flexibility for clinicians, Esa Davis, MD, MPH, a member of USPSTF and a professor at the University of Maryland School of Medicine, Baltimore, told this news organization.
“It provides them with more options instead of telling them, ‘You have to do it this way,’ ” Dr. Davis said.
The task force’s draft recommendation is not meant to apply to people with secondary osteoporosis due to an underlying medical condition such as cancer, metabolic bone diseases or hyperthyroidism, or chronic use of a medication associated with bone loss.
Rajesh K. Jain, MD, who was not involved with the USPSTF work, read the draft recommendations at the request of this news organization. In an email, he said he generally agreed with the decision to largely stick to the 2018 recommendations for women.
He also noted that there’s still a lack of a clear direction for physicians about assessing osteoporosis risk in men. But multiple randomized control trials of osteoporosis drugs seem to suggest these medicines work for both sexes, said Dr. Jain, who is the endocrinology fellowship program director at University of Chicago Medicine, Chicago.
The USPSTF draft also would reiterate the current “I” grade about screening men for osteoporosis.
An “I” grade means the task force found the current body of available evidence is insufficient to assess the balance of benefits and harms of screening for osteoporosis to prevent osteoporotic fractures in men.
“Since there is no recommendation right now, it would have seemed sensible to include a recommendation to screen men with prior fracture or other risk factors for osteoporosis, much like they do for younger women,” Dr. Jain said.
Insufficient Evidence
The USPSTF’s “I” grade is different from a “D” grade, which is what the task force uses to recommend against the use of a service.
A “D” grade means the USPSTF says there is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. (The USPSTF makes it easy to search online for grades given to preventive services, including those that got a “D.”)
The USPSTF is calling for more studies on the benefits and harms of screening for osteoporosis to prevent fractures and related morbidity and mortality in men.
“Men do get osteoporosis,” Dr. Davis said. “But unfortunately, the evidence isn’t there” to allow USPSTF to make a recommendation on screening approaches.
“Any man who has concerns about bone health should certainly talk to his clinician and figure out what is the best form of screening” he might want to do, she said.
There’s been a growing interest in the question of whether to screen men for osteoporosis and bone health. For example, Osteoporosis Canada last year updated a guideline to emphasize the need to assess older patients of both sexes for the risk for fractures. But the Canadian Task Force on Preventive Health Care in 2023 came to a conclusion in line with the USPSTF draft.
The Canadian task force recommended against routine screening in men, while adding that clinicians should be alert to changes in health that may indicate the patient has experienced or is at a higher risk for fragility fracture.
Risk Factors, Concerns About Tests
The USPSTF said that risk factors associated with fragility fractures are similar in men and women. These include:
- Increasing age
- Low body mass index
- Excessive alcohol intake
- Current smoking
- Chronic corticosteroid use
- History of prior fractures, falls within the past year, cerebrovascular accident, and diabetes
- Hypogonadism
The process of updating the USPSTF recommendations can serve as a chance to expand public awareness about osteoporosis, as many men may not know to raise the question of their fracture risk during medical appointments, Dr. Davis said.
“Clinicians need to be aware of the risk factors and to be able to have conversations with men,” she said.
Dr. Davis also cautioned about the need to be aware of limitations with clinical risk assessment tools. In the draft recommendation statement, the USPSTF noted that some tools and approaches may be less likely to identify Black, Hispanic, and Asian people as high risk, and subsequently, clinicians may be less likely to offer treatment to them compared with White people of the same age, bone mineral density, and clinical risk profile.
Dr. Davis had no relevant financial relationships. Dr. Jain received research funding from the Amgen Foundation.
A version of this article appeared on Medscape.com.
EULAR 2024 Preview: Therapeutics in Development Take Center Stage
The European Alliance of Associations for Rheumatology (EULAR) 2024 European Congress of Rheumatology annual meeting is about to take place in Vienna, Austria. From June 12 to 15, some of the world’s leading researchers and clinicians will convene to present and learn about data on some of the new and innovative treatments for people with rheumatic and musculoskeletal diseases (RMDs) as well as to discuss how to use and optimize existing approaches.
Ahead of the Congress, this news organization asked the Congress Committee’s Scientific Programme Chair Caroline Ospelt, MD, PhD, and Abstract Chair Christian Dejaco, MD, PhD, MBA, to discuss some of their highlights of this year’s meeting.
From Bench to Bedside
“For me, the beauty at EULAR is really that you have the latest on basic research, how this can be translated in clinical trials, and then the last step would be how EULAR recommends it to be used in clinical practice,” Dr. Ospelt, professor of experimental rheumatology at University Hospital Zurich, said in an interview.
“So, if you go to EULAR continuously, you can actually follow the whole story of how novelty comes into clinical practice,” she added.
In a separate interview, Dr. Dejaco, a consultant rheumatologist and associate professor at the Medical University of Graz in Austria, said: “There are several new drug trials that are going to be presented.”
One of his highlights on the use of new drugs for the treatment of giant cell arteritis will be the phase 3 SELECT-GCA trial of the Janus kinase (JAK) inhibitor upadacitinib (LBA0001).
“It’s a trial that hopefully will lead to the approval of this drug in this indication,” Dr. Dejaco said.
Late-Breaking Abstracts
Dr. Ospelt noted: “We had a lot of good late-breaking abstracts this year.”
Some of these include:
- Real-world data on the comparative effectiveness of five different classes of drugs used to treat psoriatic arthritis (PsA; LBA0002)
- The 16-week results of a phase 2b/3 study with the novel interleukin (IL)–17A inhibitor izokibep in people with PsA (LBA0005)
- Data from the COSPIRIT-JIA trial on the efficacy and safety of ixekizumab (Taltz) in juvenile idiopathic arthritis (LBA0009)
- Phase 2 data on the safety and efficacy of the CD38-targeting monoclonal antibody daratumumab in systemic lupus erythematosus (LBA0007)
- Results of the phase 2 DAHLIAS study of the anti–neonatal Fc receptor monoclonal antibody nipocalimab in people with primary Sjögren disease (LBA0010)
- Safety and immunogenicity data from a phase 1 study of an active anti–IL-6 immunotherapy in people with knee osteoarthritis (LBA0011)
The latter is “really interesting,” Dr. Ospelt said. As of now, there is no approved treatment for osteoarthritis, and there is no immunotherapy, “so this would be the first.”
But it’s not just the late-breaker abstracts to look out for. Dr. Dejaco highlighted two abstracts that will be presented during the Abstract Plenary:
- A phase 3 study of a new selective JAK1 inhibitor, SHR0302, in rheumatoid arthritis (OP0037)
- A multi-omics analysis and targeted gene-editing study in people with , which causes inflammatory and hematologic changes (OP0073)
Of the latter, he said, “this disease is still incompletely understood, and this abstract really helps to better understand the mechanisms underlying this disease.”
One to Watch: CAR T-Cell Therapy
Dr. Ospelt said that the scientific program is about 80% clinical and 20% basic science overall. However, more sessions are being held jointly because data are starting to move from the bench to bedside.
One of the basic science areas that has had “a real buzz” around it and is now producing results in the clinic is the use of chimeric antigen receptor (CAR) T cells. In one of the first, and perhaps aptly titled What Is New, or WIN, sessions of the congress, Georg Schett, MD, vice president of research at Friedrich-Alexander-Universität Erlangen-Nüremberg in Germany, will discuss the use of CAR T-cell therapy for inflammatory RMDs. There are also multiple abstract presentations on this topic.
In-depth tissue analysis and prediction of treatment response is another interesting approach, Dr. Ospelt said. “I think that’s the way to go, that we come from the blood, we go into the tissue.” A “very nice” example of this approach will be presented during the Abstract Plenary session on Wednesday, June 12, looking at how synovial tissue macrophages may be able to give information on likely treatment response in treatment-naive rheumatoid arthritis (OP0062). There are also some further findings related to the tissue biopsy–driven treatment trial R4RA that are being presented at the meeting (OP0218, OP0242, and POS0351).
EULAR Highlighted Sessions
Among the highlighted sessions on the EULAR 2024 website is one on axial involvement in PsA and spondyloarthritis (SpA).
“Axial involvement in psoriatic arthritis and peripheral involvement in axial spondyloarthritis is quite a hot topic at the moment,” Dr. Ospelt said. There are lots of questions: “How connected are they? How different are they? Do we need different treatment for axial involvement compared to peripheral involvement?”
Another EULAR highlighted session is the 75th anniversary of glucocorticoid treatment, during which Past President of EULAR and Emeritus Professor of Rheumatology Josef S. Smolen, MD, will overview the “past, present, and future” of glucocorticoids in RMDs. Consultant rheumatologist Frank Buttgereit, MD, from the German Rheumatism Research Center in Berlin, will discuss the practicalities of using these drugs in clinical practice.
Dr. Dejaco noted: “Glucocorticoids have been one of the most important treatments for a very long time, and they’re still the most important treatment for the acute treatment of systemic inflammatory diseases.”
For a long time, there was no alternative to using steroids, he added, but steroid-sparing options now exist, and there will be data presented on a new type of drug that could potentially be used to control cortisol levels in the body (OP0335).
Recommendations and More
Dr. Ospelt and Dr. Dejaco both pointed out other sessions that are likely to be very popular, such as the first and second EULAR Recommendations sessions, a session on rheumatoid arthritis prevention, as well as the many presentations and sessions on digital health and nonpharmacologic interventions such as exercise.
With over 5242 submitted abstracts, there is going to be no shortage of data being presented at EULAR 2024. Alongside the traditional abstract submission categories, this year there is a new clinical case reports category.
“We had about 578 submissions for that category,” Dr. Dejaco said. There were 3315 abstracts submitted for the clinical research category, 812 for the basic and translational research category, 283 from health professionals in rheumatology, 152 from patient groups, and 102 in the field of pediatric rheumatology.
Join in On-Site, Watch on Demand
EULAR 2024 reverts to an on-site–only meeting this year. Some of the more lighthearted yet educational elements of the program for those attending include the second edition of the EMEUNET Rheumatology Quiz and, new for this year, two escape rooms. These rooms will provide an interactive experience where small teams will have to solve rheumatologic conundrums in order to escape the room within the hour, Dr. Dejaco explained. There will also be a morning run on Friday, June 14. “It’s not a race, it’s simply to meet and run together,” Dr. Dejaco said.
But if you cannot make the congress in person, the EULAR 2024 Livestream will be broadcasting throughout the congress. Anyone registered by June 30 will have on-demand access to the recorded content from June 17 until December 31, 2024.
Abstracts for the meeting will be published as a supplement to Annals of the Rheumatic Diseases, the official journal of EULAR.
Dr. Ospelt reported no relevant financial relationships. Dr. Dejaco has received consulting/speaker fees from AbbVie, Eli Lilly, Janssen, Sparrow, Novartis, Pfizer, Roche, Galapagos, and Sanofi.
A version of this article appeared on Medscape.com.
The European Alliance of Associations for Rheumatology (EULAR) 2024 European Congress of Rheumatology annual meeting is about to take place in Vienna, Austria. From June 12 to 15, some of the world’s leading researchers and clinicians will convene to present and learn about data on some of the new and innovative treatments for people with rheumatic and musculoskeletal diseases (RMDs) as well as to discuss how to use and optimize existing approaches.
Ahead of the Congress, this news organization asked the Congress Committee’s Scientific Programme Chair Caroline Ospelt, MD, PhD, and Abstract Chair Christian Dejaco, MD, PhD, MBA, to discuss some of their highlights of this year’s meeting.
From Bench to Bedside
“For me, the beauty at EULAR is really that you have the latest on basic research, how this can be translated in clinical trials, and then the last step would be how EULAR recommends it to be used in clinical practice,” Dr. Ospelt, professor of experimental rheumatology at University Hospital Zurich, said in an interview.
“So, if you go to EULAR continuously, you can actually follow the whole story of how novelty comes into clinical practice,” she added.
In a separate interview, Dr. Dejaco, a consultant rheumatologist and associate professor at the Medical University of Graz in Austria, said: “There are several new drug trials that are going to be presented.”
One of his highlights on the use of new drugs for the treatment of giant cell arteritis will be the phase 3 SELECT-GCA trial of the Janus kinase (JAK) inhibitor upadacitinib (LBA0001).
“It’s a trial that hopefully will lead to the approval of this drug in this indication,” Dr. Dejaco said.
Late-Breaking Abstracts
Dr. Ospelt noted: “We had a lot of good late-breaking abstracts this year.”
Some of these include:
- Real-world data on the comparative effectiveness of five different classes of drugs used to treat psoriatic arthritis (PsA; LBA0002)
- The 16-week results of a phase 2b/3 study with the novel interleukin (IL)–17A inhibitor izokibep in people with PsA (LBA0005)
- Data from the COSPIRIT-JIA trial on the efficacy and safety of ixekizumab (Taltz) in juvenile idiopathic arthritis (LBA0009)
- Phase 2 data on the safety and efficacy of the CD38-targeting monoclonal antibody daratumumab in systemic lupus erythematosus (LBA0007)
- Results of the phase 2 DAHLIAS study of the anti–neonatal Fc receptor monoclonal antibody nipocalimab in people with primary Sjögren disease (LBA0010)
- Safety and immunogenicity data from a phase 1 study of an active anti–IL-6 immunotherapy in people with knee osteoarthritis (LBA0011)
The latter is “really interesting,” Dr. Ospelt said. As of now, there is no approved treatment for osteoarthritis, and there is no immunotherapy, “so this would be the first.”
But it’s not just the late-breaker abstracts to look out for. Dr. Dejaco highlighted two abstracts that will be presented during the Abstract Plenary:
- A phase 3 study of a new selective JAK1 inhibitor, SHR0302, in rheumatoid arthritis (OP0037)
- A multi-omics analysis and targeted gene-editing study in people with , which causes inflammatory and hematologic changes (OP0073)
Of the latter, he said, “this disease is still incompletely understood, and this abstract really helps to better understand the mechanisms underlying this disease.”
One to Watch: CAR T-Cell Therapy
Dr. Ospelt said that the scientific program is about 80% clinical and 20% basic science overall. However, more sessions are being held jointly because data are starting to move from the bench to bedside.
One of the basic science areas that has had “a real buzz” around it and is now producing results in the clinic is the use of chimeric antigen receptor (CAR) T cells. In one of the first, and perhaps aptly titled What Is New, or WIN, sessions of the congress, Georg Schett, MD, vice president of research at Friedrich-Alexander-Universität Erlangen-Nüremberg in Germany, will discuss the use of CAR T-cell therapy for inflammatory RMDs. There are also multiple abstract presentations on this topic.
In-depth tissue analysis and prediction of treatment response is another interesting approach, Dr. Ospelt said. “I think that’s the way to go, that we come from the blood, we go into the tissue.” A “very nice” example of this approach will be presented during the Abstract Plenary session on Wednesday, June 12, looking at how synovial tissue macrophages may be able to give information on likely treatment response in treatment-naive rheumatoid arthritis (OP0062). There are also some further findings related to the tissue biopsy–driven treatment trial R4RA that are being presented at the meeting (OP0218, OP0242, and POS0351).
EULAR Highlighted Sessions
Among the highlighted sessions on the EULAR 2024 website is one on axial involvement in PsA and spondyloarthritis (SpA).
“Axial involvement in psoriatic arthritis and peripheral involvement in axial spondyloarthritis is quite a hot topic at the moment,” Dr. Ospelt said. There are lots of questions: “How connected are they? How different are they? Do we need different treatment for axial involvement compared to peripheral involvement?”
Another EULAR highlighted session is the 75th anniversary of glucocorticoid treatment, during which Past President of EULAR and Emeritus Professor of Rheumatology Josef S. Smolen, MD, will overview the “past, present, and future” of glucocorticoids in RMDs. Consultant rheumatologist Frank Buttgereit, MD, from the German Rheumatism Research Center in Berlin, will discuss the practicalities of using these drugs in clinical practice.
Dr. Dejaco noted: “Glucocorticoids have been one of the most important treatments for a very long time, and they’re still the most important treatment for the acute treatment of systemic inflammatory diseases.”
For a long time, there was no alternative to using steroids, he added, but steroid-sparing options now exist, and there will be data presented on a new type of drug that could potentially be used to control cortisol levels in the body (OP0335).
Recommendations and More
Dr. Ospelt and Dr. Dejaco both pointed out other sessions that are likely to be very popular, such as the first and second EULAR Recommendations sessions, a session on rheumatoid arthritis prevention, as well as the many presentations and sessions on digital health and nonpharmacologic interventions such as exercise.
With over 5242 submitted abstracts, there is going to be no shortage of data being presented at EULAR 2024. Alongside the traditional abstract submission categories, this year there is a new clinical case reports category.
“We had about 578 submissions for that category,” Dr. Dejaco said. There were 3315 abstracts submitted for the clinical research category, 812 for the basic and translational research category, 283 from health professionals in rheumatology, 152 from patient groups, and 102 in the field of pediatric rheumatology.
Join in On-Site, Watch on Demand
EULAR 2024 reverts to an on-site–only meeting this year. Some of the more lighthearted yet educational elements of the program for those attending include the second edition of the EMEUNET Rheumatology Quiz and, new for this year, two escape rooms. These rooms will provide an interactive experience where small teams will have to solve rheumatologic conundrums in order to escape the room within the hour, Dr. Dejaco explained. There will also be a morning run on Friday, June 14. “It’s not a race, it’s simply to meet and run together,” Dr. Dejaco said.
But if you cannot make the congress in person, the EULAR 2024 Livestream will be broadcasting throughout the congress. Anyone registered by June 30 will have on-demand access to the recorded content from June 17 until December 31, 2024.
Abstracts for the meeting will be published as a supplement to Annals of the Rheumatic Diseases, the official journal of EULAR.
Dr. Ospelt reported no relevant financial relationships. Dr. Dejaco has received consulting/speaker fees from AbbVie, Eli Lilly, Janssen, Sparrow, Novartis, Pfizer, Roche, Galapagos, and Sanofi.
A version of this article appeared on Medscape.com.
The European Alliance of Associations for Rheumatology (EULAR) 2024 European Congress of Rheumatology annual meeting is about to take place in Vienna, Austria. From June 12 to 15, some of the world’s leading researchers and clinicians will convene to present and learn about data on some of the new and innovative treatments for people with rheumatic and musculoskeletal diseases (RMDs) as well as to discuss how to use and optimize existing approaches.
Ahead of the Congress, this news organization asked the Congress Committee’s Scientific Programme Chair Caroline Ospelt, MD, PhD, and Abstract Chair Christian Dejaco, MD, PhD, MBA, to discuss some of their highlights of this year’s meeting.
From Bench to Bedside
“For me, the beauty at EULAR is really that you have the latest on basic research, how this can be translated in clinical trials, and then the last step would be how EULAR recommends it to be used in clinical practice,” Dr. Ospelt, professor of experimental rheumatology at University Hospital Zurich, said in an interview.
“So, if you go to EULAR continuously, you can actually follow the whole story of how novelty comes into clinical practice,” she added.
In a separate interview, Dr. Dejaco, a consultant rheumatologist and associate professor at the Medical University of Graz in Austria, said: “There are several new drug trials that are going to be presented.”
One of his highlights on the use of new drugs for the treatment of giant cell arteritis will be the phase 3 SELECT-GCA trial of the Janus kinase (JAK) inhibitor upadacitinib (LBA0001).
“It’s a trial that hopefully will lead to the approval of this drug in this indication,” Dr. Dejaco said.
Late-Breaking Abstracts
Dr. Ospelt noted: “We had a lot of good late-breaking abstracts this year.”
Some of these include:
- Real-world data on the comparative effectiveness of five different classes of drugs used to treat psoriatic arthritis (PsA; LBA0002)
- The 16-week results of a phase 2b/3 study with the novel interleukin (IL)–17A inhibitor izokibep in people with PsA (LBA0005)
- Data from the COSPIRIT-JIA trial on the efficacy and safety of ixekizumab (Taltz) in juvenile idiopathic arthritis (LBA0009)
- Phase 2 data on the safety and efficacy of the CD38-targeting monoclonal antibody daratumumab in systemic lupus erythematosus (LBA0007)
- Results of the phase 2 DAHLIAS study of the anti–neonatal Fc receptor monoclonal antibody nipocalimab in people with primary Sjögren disease (LBA0010)
- Safety and immunogenicity data from a phase 1 study of an active anti–IL-6 immunotherapy in people with knee osteoarthritis (LBA0011)
The latter is “really interesting,” Dr. Ospelt said. As of now, there is no approved treatment for osteoarthritis, and there is no immunotherapy, “so this would be the first.”
But it’s not just the late-breaker abstracts to look out for. Dr. Dejaco highlighted two abstracts that will be presented during the Abstract Plenary:
- A phase 3 study of a new selective JAK1 inhibitor, SHR0302, in rheumatoid arthritis (OP0037)
- A multi-omics analysis and targeted gene-editing study in people with , which causes inflammatory and hematologic changes (OP0073)
Of the latter, he said, “this disease is still incompletely understood, and this abstract really helps to better understand the mechanisms underlying this disease.”
One to Watch: CAR T-Cell Therapy
Dr. Ospelt said that the scientific program is about 80% clinical and 20% basic science overall. However, more sessions are being held jointly because data are starting to move from the bench to bedside.
One of the basic science areas that has had “a real buzz” around it and is now producing results in the clinic is the use of chimeric antigen receptor (CAR) T cells. In one of the first, and perhaps aptly titled What Is New, or WIN, sessions of the congress, Georg Schett, MD, vice president of research at Friedrich-Alexander-Universität Erlangen-Nüremberg in Germany, will discuss the use of CAR T-cell therapy for inflammatory RMDs. There are also multiple abstract presentations on this topic.
In-depth tissue analysis and prediction of treatment response is another interesting approach, Dr. Ospelt said. “I think that’s the way to go, that we come from the blood, we go into the tissue.” A “very nice” example of this approach will be presented during the Abstract Plenary session on Wednesday, June 12, looking at how synovial tissue macrophages may be able to give information on likely treatment response in treatment-naive rheumatoid arthritis (OP0062). There are also some further findings related to the tissue biopsy–driven treatment trial R4RA that are being presented at the meeting (OP0218, OP0242, and POS0351).
EULAR Highlighted Sessions
Among the highlighted sessions on the EULAR 2024 website is one on axial involvement in PsA and spondyloarthritis (SpA).
“Axial involvement in psoriatic arthritis and peripheral involvement in axial spondyloarthritis is quite a hot topic at the moment,” Dr. Ospelt said. There are lots of questions: “How connected are they? How different are they? Do we need different treatment for axial involvement compared to peripheral involvement?”
Another EULAR highlighted session is the 75th anniversary of glucocorticoid treatment, during which Past President of EULAR and Emeritus Professor of Rheumatology Josef S. Smolen, MD, will overview the “past, present, and future” of glucocorticoids in RMDs. Consultant rheumatologist Frank Buttgereit, MD, from the German Rheumatism Research Center in Berlin, will discuss the practicalities of using these drugs in clinical practice.
Dr. Dejaco noted: “Glucocorticoids have been one of the most important treatments for a very long time, and they’re still the most important treatment for the acute treatment of systemic inflammatory diseases.”
For a long time, there was no alternative to using steroids, he added, but steroid-sparing options now exist, and there will be data presented on a new type of drug that could potentially be used to control cortisol levels in the body (OP0335).
Recommendations and More
Dr. Ospelt and Dr. Dejaco both pointed out other sessions that are likely to be very popular, such as the first and second EULAR Recommendations sessions, a session on rheumatoid arthritis prevention, as well as the many presentations and sessions on digital health and nonpharmacologic interventions such as exercise.
With over 5242 submitted abstracts, there is going to be no shortage of data being presented at EULAR 2024. Alongside the traditional abstract submission categories, this year there is a new clinical case reports category.
“We had about 578 submissions for that category,” Dr. Dejaco said. There were 3315 abstracts submitted for the clinical research category, 812 for the basic and translational research category, 283 from health professionals in rheumatology, 152 from patient groups, and 102 in the field of pediatric rheumatology.
Join in On-Site, Watch on Demand
EULAR 2024 reverts to an on-site–only meeting this year. Some of the more lighthearted yet educational elements of the program for those attending include the second edition of the EMEUNET Rheumatology Quiz and, new for this year, two escape rooms. These rooms will provide an interactive experience where small teams will have to solve rheumatologic conundrums in order to escape the room within the hour, Dr. Dejaco explained. There will also be a morning run on Friday, June 14. “It’s not a race, it’s simply to meet and run together,” Dr. Dejaco said.
But if you cannot make the congress in person, the EULAR 2024 Livestream will be broadcasting throughout the congress. Anyone registered by June 30 will have on-demand access to the recorded content from June 17 until December 31, 2024.
Abstracts for the meeting will be published as a supplement to Annals of the Rheumatic Diseases, the official journal of EULAR.
Dr. Ospelt reported no relevant financial relationships. Dr. Dejaco has received consulting/speaker fees from AbbVie, Eli Lilly, Janssen, Sparrow, Novartis, Pfizer, Roche, Galapagos, and Sanofi.
A version of this article appeared on Medscape.com.
Clear Coverage Preference for Humira Over Biosimilars Seen in Most Medicare Part D Plans
Despite the influx of adalimumab biosimilars entering the market in 2023, Humira remains on top.
As of January 2024, both high and low concentrations of Humira, the originator adalimumab product, are nearly universally covered by Medicare Part D plans, while only half of these plans covered adalimumab biosimilars, according to a new research letter published online on June 6, 2024, in JAMA.
Of the plans that covered both, only 1.5% had lower-tier placement for biosimilars.
“This study of formulary coverage helps explain limited uptake of adalimumab biosimilars,” wrote the authors, led by Matthew J. Klebanoff, MD, of the University of Pennsylvania, Philadelphia. “Subpar biosimilar adoption will not only undermine their potential to reduce spending but also may deter investments in biosimilar development.”
The analysis included the formulary and enrollment files for 5609 Medicare Part D plans, representing 44.4 million beneficiaries. Drug list prices and whole acquisition costs (WAC) were pulled from the Red Book database, which provides prices for prescription and over-the-counter drugs as well as medical devices and supplies.
Nearly all (98.9%) of Part D plans covered the high-concentration (100 mg/mL) version of adalimumab with a WAC of $6923. This higher concentration is the most popular formulation of the drug, making up an estimated 85% of prescriptions. By comparison, 26.8% of plans covered the high-concentration version of adalimumab-adaz (Hyrimoz), with a WAC 5% less than the reference product.
The unbranded version of adalimumab-adaz, sold at an 81% discount from the reference product, was covered by 13% of plans. Only 4.6% of plans covered high-concentration adalimumab-bwwd (Hadlima), manufactured by Samsung Bioepis.
In January 2024, no high-concentration adalimumab biosimilar had been granted interchangeability status by the US Food and Drug Administration (FDA). Adalimumab-ryvk (Simlandi) was the first biosimilar to receive this designation and was launched in late May 2024.
Coverage for the lower concentration of adalimumab was nearly universal (98.7% of plans). About half of the plans (50.7%) covered adalimumab-adbm (Cyltezo) at a 5% discount. Adalimumab-adbm (Boehringer Ingelheim) was the first interchangeable Humira biosimilar approved by the FDA, but it is only interchangeable with the less popular, lower concentration formulation of adalimumab.
All other biosimilars were covered by less than 5% of Medicare Part D plans, even with some having a WAC 86% below Humira.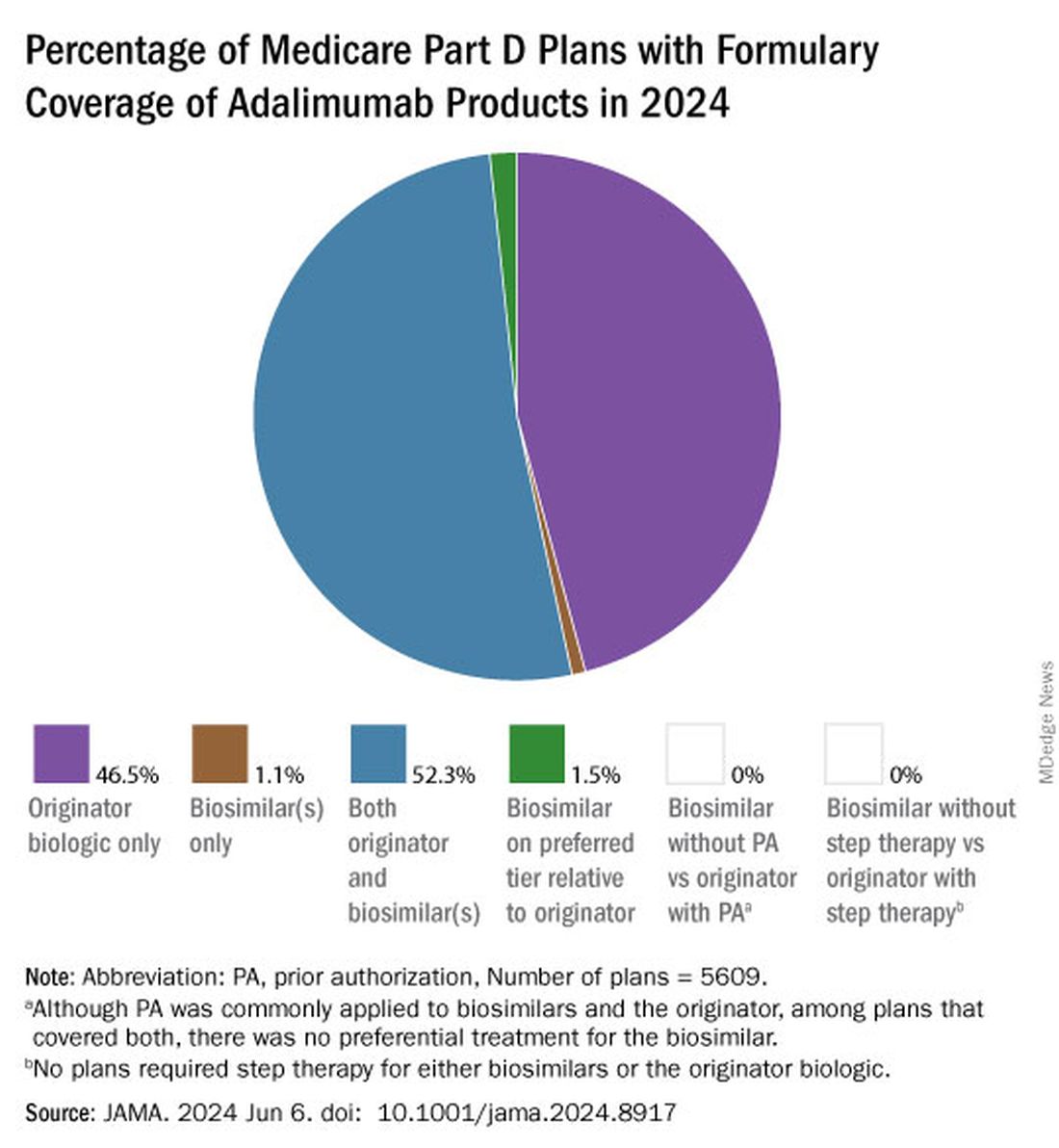
Few plans (1.5%) had biosimilars on preferred tiers compared with the reference product, and no plans used prior authorization to incentivize use of biosimilars. Most plans preferred the higher-priced version of adalimumab biosimilars, which appeals to pharmacy benefit managers who can therefore receive higher rebates, the authors noted.
“Ultimately, biosimilars’ true effect on spending will depend not on their list price but rather on their net price (after rebates) and their influence on originator biologics’ net price,” they wrote. They pointed to the 38% drop in Humira’s annual net price at the end of 2023 compared with the prior year.
“Despite this price decrease, biosimilars offer far greater potential savings: Several adalimumab biosimilars have list prices that are less than half of Humira’s net price,” the authors continued, and encouraged policy makers to mandate coverage for these lower-priced options.
Dr. Klebanoff was supported by a grant from the Health Resources and Services Administration. Two coauthors were supported by a grant from the National Institute on Aging. One author reported receiving consulting fees from AbbVie, which manufactures Humira.
A version of this article appeared on Medscape.com .
Despite the influx of adalimumab biosimilars entering the market in 2023, Humira remains on top.
As of January 2024, both high and low concentrations of Humira, the originator adalimumab product, are nearly universally covered by Medicare Part D plans, while only half of these plans covered adalimumab biosimilars, according to a new research letter published online on June 6, 2024, in JAMA.
Of the plans that covered both, only 1.5% had lower-tier placement for biosimilars.
“This study of formulary coverage helps explain limited uptake of adalimumab biosimilars,” wrote the authors, led by Matthew J. Klebanoff, MD, of the University of Pennsylvania, Philadelphia. “Subpar biosimilar adoption will not only undermine their potential to reduce spending but also may deter investments in biosimilar development.”
The analysis included the formulary and enrollment files for 5609 Medicare Part D plans, representing 44.4 million beneficiaries. Drug list prices and whole acquisition costs (WAC) were pulled from the Red Book database, which provides prices for prescription and over-the-counter drugs as well as medical devices and supplies.
Nearly all (98.9%) of Part D plans covered the high-concentration (100 mg/mL) version of adalimumab with a WAC of $6923. This higher concentration is the most popular formulation of the drug, making up an estimated 85% of prescriptions. By comparison, 26.8% of plans covered the high-concentration version of adalimumab-adaz (Hyrimoz), with a WAC 5% less than the reference product.
The unbranded version of adalimumab-adaz, sold at an 81% discount from the reference product, was covered by 13% of plans. Only 4.6% of plans covered high-concentration adalimumab-bwwd (Hadlima), manufactured by Samsung Bioepis.
In January 2024, no high-concentration adalimumab biosimilar had been granted interchangeability status by the US Food and Drug Administration (FDA). Adalimumab-ryvk (Simlandi) was the first biosimilar to receive this designation and was launched in late May 2024.
Coverage for the lower concentration of adalimumab was nearly universal (98.7% of plans). About half of the plans (50.7%) covered adalimumab-adbm (Cyltezo) at a 5% discount. Adalimumab-adbm (Boehringer Ingelheim) was the first interchangeable Humira biosimilar approved by the FDA, but it is only interchangeable with the less popular, lower concentration formulation of adalimumab.
All other biosimilars were covered by less than 5% of Medicare Part D plans, even with some having a WAC 86% below Humira.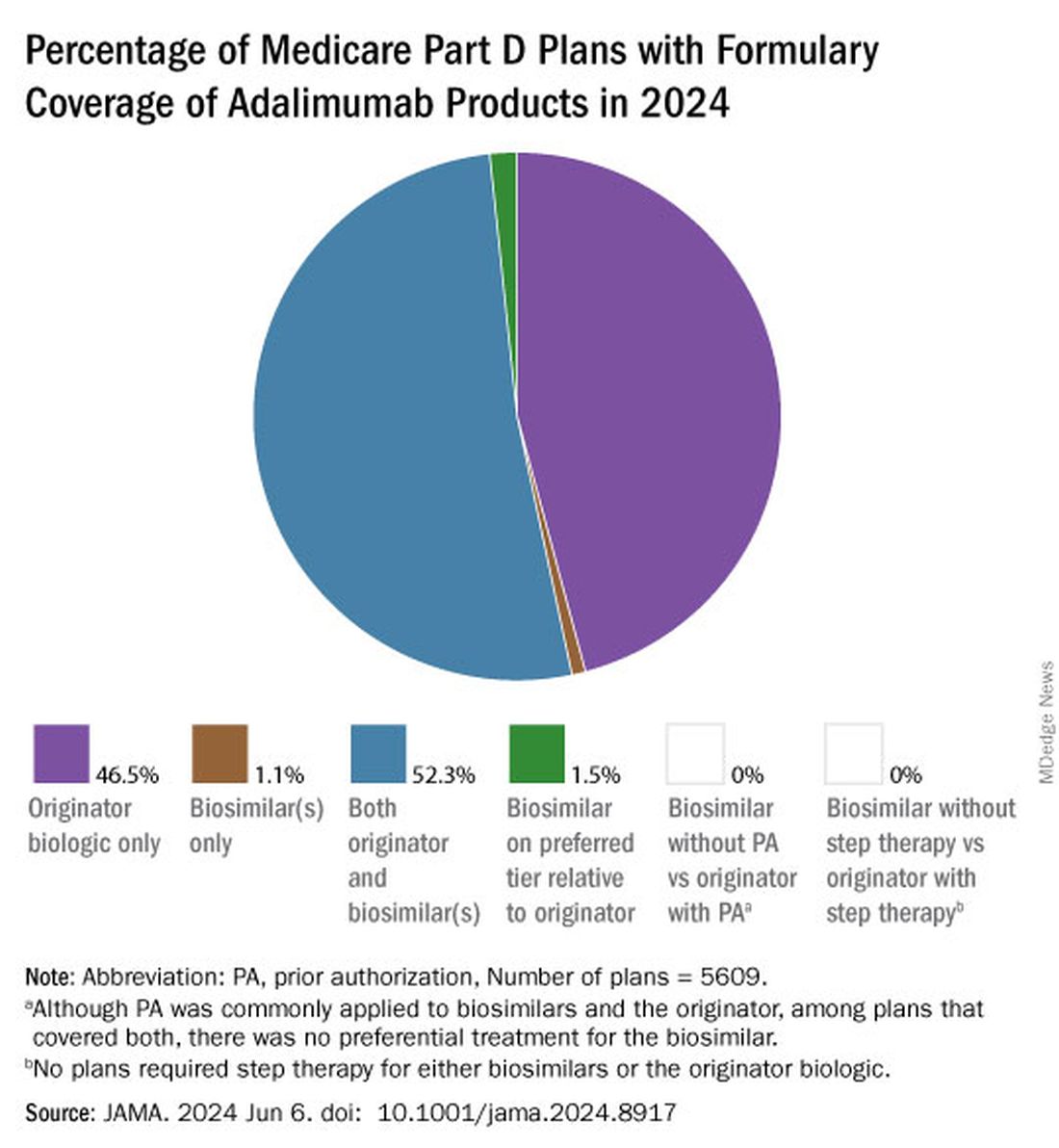
Few plans (1.5%) had biosimilars on preferred tiers compared with the reference product, and no plans used prior authorization to incentivize use of biosimilars. Most plans preferred the higher-priced version of adalimumab biosimilars, which appeals to pharmacy benefit managers who can therefore receive higher rebates, the authors noted.
“Ultimately, biosimilars’ true effect on spending will depend not on their list price but rather on their net price (after rebates) and their influence on originator biologics’ net price,” they wrote. They pointed to the 38% drop in Humira’s annual net price at the end of 2023 compared with the prior year.
“Despite this price decrease, biosimilars offer far greater potential savings: Several adalimumab biosimilars have list prices that are less than half of Humira’s net price,” the authors continued, and encouraged policy makers to mandate coverage for these lower-priced options.
Dr. Klebanoff was supported by a grant from the Health Resources and Services Administration. Two coauthors were supported by a grant from the National Institute on Aging. One author reported receiving consulting fees from AbbVie, which manufactures Humira.
A version of this article appeared on Medscape.com .
Despite the influx of adalimumab biosimilars entering the market in 2023, Humira remains on top.
As of January 2024, both high and low concentrations of Humira, the originator adalimumab product, are nearly universally covered by Medicare Part D plans, while only half of these plans covered adalimumab biosimilars, according to a new research letter published online on June 6, 2024, in JAMA.
Of the plans that covered both, only 1.5% had lower-tier placement for biosimilars.
“This study of formulary coverage helps explain limited uptake of adalimumab biosimilars,” wrote the authors, led by Matthew J. Klebanoff, MD, of the University of Pennsylvania, Philadelphia. “Subpar biosimilar adoption will not only undermine their potential to reduce spending but also may deter investments in biosimilar development.”
The analysis included the formulary and enrollment files for 5609 Medicare Part D plans, representing 44.4 million beneficiaries. Drug list prices and whole acquisition costs (WAC) were pulled from the Red Book database, which provides prices for prescription and over-the-counter drugs as well as medical devices and supplies.
Nearly all (98.9%) of Part D plans covered the high-concentration (100 mg/mL) version of adalimumab with a WAC of $6923. This higher concentration is the most popular formulation of the drug, making up an estimated 85% of prescriptions. By comparison, 26.8% of plans covered the high-concentration version of adalimumab-adaz (Hyrimoz), with a WAC 5% less than the reference product.
The unbranded version of adalimumab-adaz, sold at an 81% discount from the reference product, was covered by 13% of plans. Only 4.6% of plans covered high-concentration adalimumab-bwwd (Hadlima), manufactured by Samsung Bioepis.
In January 2024, no high-concentration adalimumab biosimilar had been granted interchangeability status by the US Food and Drug Administration (FDA). Adalimumab-ryvk (Simlandi) was the first biosimilar to receive this designation and was launched in late May 2024.
Coverage for the lower concentration of adalimumab was nearly universal (98.7% of plans). About half of the plans (50.7%) covered adalimumab-adbm (Cyltezo) at a 5% discount. Adalimumab-adbm (Boehringer Ingelheim) was the first interchangeable Humira biosimilar approved by the FDA, but it is only interchangeable with the less popular, lower concentration formulation of adalimumab.
All other biosimilars were covered by less than 5% of Medicare Part D plans, even with some having a WAC 86% below Humira.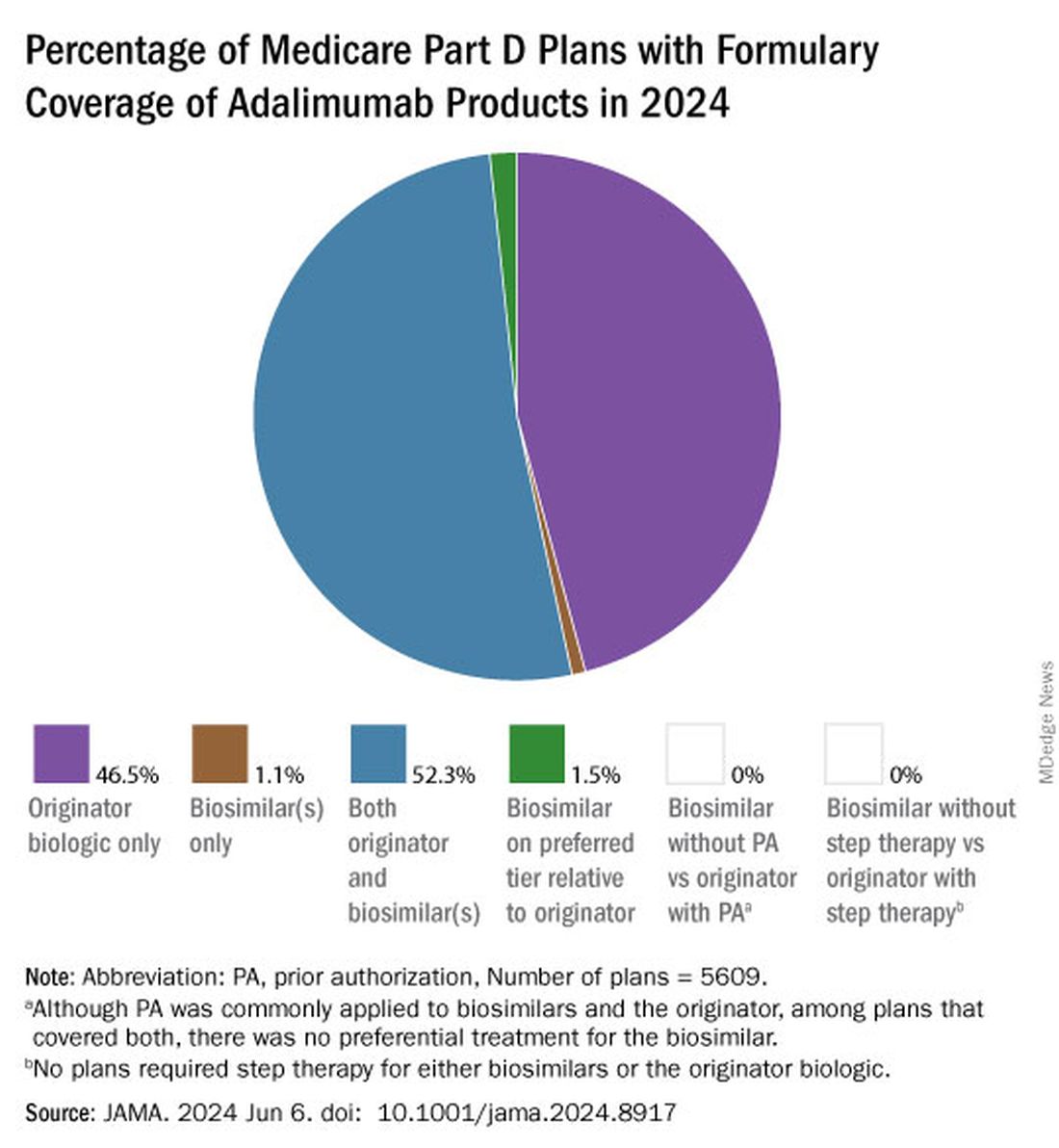
Few plans (1.5%) had biosimilars on preferred tiers compared with the reference product, and no plans used prior authorization to incentivize use of biosimilars. Most plans preferred the higher-priced version of adalimumab biosimilars, which appeals to pharmacy benefit managers who can therefore receive higher rebates, the authors noted.
“Ultimately, biosimilars’ true effect on spending will depend not on their list price but rather on their net price (after rebates) and their influence on originator biologics’ net price,” they wrote. They pointed to the 38% drop in Humira’s annual net price at the end of 2023 compared with the prior year.
“Despite this price decrease, biosimilars offer far greater potential savings: Several adalimumab biosimilars have list prices that are less than half of Humira’s net price,” the authors continued, and encouraged policy makers to mandate coverage for these lower-priced options.
Dr. Klebanoff was supported by a grant from the Health Resources and Services Administration. Two coauthors were supported by a grant from the National Institute on Aging. One author reported receiving consulting fees from AbbVie, which manufactures Humira.
A version of this article appeared on Medscape.com .
FROM JAMA
FDA Grants New Pediatric Arthritis Indications for Upadacitinib
Upadacitinib (Rinvoq) is now indicated for patients aged 2 years or older with active polyarticular juvenile idiopathic arthritis (pJIA) and psoriatic arthritis (PsA) who cannot tolerate or achieve adequate disease response with one or more tumor necrosis factor (TNF) blockers, according to a press release from manufacturer AbbVie.
For the youngest patients, upadacitinib is also available as a weight-based oral solution (Rinvoq LQ) in addition to the previously available tablets, according to the company. JIA, which includes pJIA and juvenile PsA, affects nearly 300,000 children and adolescents in the United States, and alternatives to TNF inhibitor (TNFi) therapy are limited, according to the company.
“Pediatric patients with pJIA and PsA can be severely limited in their ability to complete daily physical tasks and participate in everyday activities. Understanding their needs today and knowing the likelihood of disease in adulthood underscores the need for additional treatment options,” Aarat Patel, MD, a pediatric rheumatologist at Bon Secours Rheumatology Center, Richmond, Virginia, said in the press release. “Having a treatment option available for patients who do not respond well to a TNFi addresses a need for the healthcare community, patients, and their families,” he said.
Upadacitinib, a Janus kinase (JAK) inhibitor, is being studied for multiple immune-mediated inflammatory diseases. The new indication was supported by data from adults with rheumatoid arthritis (RA) and PsA, 51 pediatric patients with pJIA and active polyarthritis, and safety data from 83 pediatric patients aged 2 years to younger than 18 years with pJIA and active polyarthritis.
In the studies, the drug’s safety in pediatric patients was similar to the known safety profile in adults, which includes increased risk for serious infections such as tuberculosis, cancer, immune system problems, blood clots, and serious allergic reactions to components of the drug, according to the press release. However, the safety and effectiveness of upadacitinib for pJIA and PsA in patients younger than 2 years are unknown.
“Upadacitinib plasma exposures in pediatric patients with pJIA and PsA at the recommended dosage are predicted to be comparable to those observed in adults with RA and PsA based on population pharmacokinetic modeling and simulation,” according to the press release.
Currently, upadacitinib’s only other pediatric indication is for moderate to severe atopic dermatitis in children aged 12 years or older. Upadacitinib also is indicated for treatment of adults with moderate to severe RA, active PsA, active ankylosing spondylitis, active nonradiographic axial spondyloarthritis, and moderate to severe ulcerative colitis and Crohn’s disease, but safety and efficacy for its use in treatment of these conditions in children and adolescents is unknown.
Upadacitinib also is being studied in phase 3 trials for treatment of conditions including alopecia areata, ankylosing spondylitis, atopic dermatitis, axial spondyloarthritis, Crohn’s disease, giant cell arteritis, hidradenitis suppurativa, psoriatic arthritis, RA, systemic lupus erythematosus, Takayasu arteritis, ulcerative colitis, and vitiligo, according to the press release.
Full prescribing information and safety data for upadacitinib are available here.
A version of this article appeared on Medscape.com.
Upadacitinib (Rinvoq) is now indicated for patients aged 2 years or older with active polyarticular juvenile idiopathic arthritis (pJIA) and psoriatic arthritis (PsA) who cannot tolerate or achieve adequate disease response with one or more tumor necrosis factor (TNF) blockers, according to a press release from manufacturer AbbVie.
For the youngest patients, upadacitinib is also available as a weight-based oral solution (Rinvoq LQ) in addition to the previously available tablets, according to the company. JIA, which includes pJIA and juvenile PsA, affects nearly 300,000 children and adolescents in the United States, and alternatives to TNF inhibitor (TNFi) therapy are limited, according to the company.
“Pediatric patients with pJIA and PsA can be severely limited in their ability to complete daily physical tasks and participate in everyday activities. Understanding their needs today and knowing the likelihood of disease in adulthood underscores the need for additional treatment options,” Aarat Patel, MD, a pediatric rheumatologist at Bon Secours Rheumatology Center, Richmond, Virginia, said in the press release. “Having a treatment option available for patients who do not respond well to a TNFi addresses a need for the healthcare community, patients, and their families,” he said.
Upadacitinib, a Janus kinase (JAK) inhibitor, is being studied for multiple immune-mediated inflammatory diseases. The new indication was supported by data from adults with rheumatoid arthritis (RA) and PsA, 51 pediatric patients with pJIA and active polyarthritis, and safety data from 83 pediatric patients aged 2 years to younger than 18 years with pJIA and active polyarthritis.
In the studies, the drug’s safety in pediatric patients was similar to the known safety profile in adults, which includes increased risk for serious infections such as tuberculosis, cancer, immune system problems, blood clots, and serious allergic reactions to components of the drug, according to the press release. However, the safety and effectiveness of upadacitinib for pJIA and PsA in patients younger than 2 years are unknown.
“Upadacitinib plasma exposures in pediatric patients with pJIA and PsA at the recommended dosage are predicted to be comparable to those observed in adults with RA and PsA based on population pharmacokinetic modeling and simulation,” according to the press release.
Currently, upadacitinib’s only other pediatric indication is for moderate to severe atopic dermatitis in children aged 12 years or older. Upadacitinib also is indicated for treatment of adults with moderate to severe RA, active PsA, active ankylosing spondylitis, active nonradiographic axial spondyloarthritis, and moderate to severe ulcerative colitis and Crohn’s disease, but safety and efficacy for its use in treatment of these conditions in children and adolescents is unknown.
Upadacitinib also is being studied in phase 3 trials for treatment of conditions including alopecia areata, ankylosing spondylitis, atopic dermatitis, axial spondyloarthritis, Crohn’s disease, giant cell arteritis, hidradenitis suppurativa, psoriatic arthritis, RA, systemic lupus erythematosus, Takayasu arteritis, ulcerative colitis, and vitiligo, according to the press release.
Full prescribing information and safety data for upadacitinib are available here.
A version of this article appeared on Medscape.com.
Upadacitinib (Rinvoq) is now indicated for patients aged 2 years or older with active polyarticular juvenile idiopathic arthritis (pJIA) and psoriatic arthritis (PsA) who cannot tolerate or achieve adequate disease response with one or more tumor necrosis factor (TNF) blockers, according to a press release from manufacturer AbbVie.
For the youngest patients, upadacitinib is also available as a weight-based oral solution (Rinvoq LQ) in addition to the previously available tablets, according to the company. JIA, which includes pJIA and juvenile PsA, affects nearly 300,000 children and adolescents in the United States, and alternatives to TNF inhibitor (TNFi) therapy are limited, according to the company.
“Pediatric patients with pJIA and PsA can be severely limited in their ability to complete daily physical tasks and participate in everyday activities. Understanding their needs today and knowing the likelihood of disease in adulthood underscores the need for additional treatment options,” Aarat Patel, MD, a pediatric rheumatologist at Bon Secours Rheumatology Center, Richmond, Virginia, said in the press release. “Having a treatment option available for patients who do not respond well to a TNFi addresses a need for the healthcare community, patients, and their families,” he said.
Upadacitinib, a Janus kinase (JAK) inhibitor, is being studied for multiple immune-mediated inflammatory diseases. The new indication was supported by data from adults with rheumatoid arthritis (RA) and PsA, 51 pediatric patients with pJIA and active polyarthritis, and safety data from 83 pediatric patients aged 2 years to younger than 18 years with pJIA and active polyarthritis.
In the studies, the drug’s safety in pediatric patients was similar to the known safety profile in adults, which includes increased risk for serious infections such as tuberculosis, cancer, immune system problems, blood clots, and serious allergic reactions to components of the drug, according to the press release. However, the safety and effectiveness of upadacitinib for pJIA and PsA in patients younger than 2 years are unknown.
“Upadacitinib plasma exposures in pediatric patients with pJIA and PsA at the recommended dosage are predicted to be comparable to those observed in adults with RA and PsA based on population pharmacokinetic modeling and simulation,” according to the press release.
Currently, upadacitinib’s only other pediatric indication is for moderate to severe atopic dermatitis in children aged 12 years or older. Upadacitinib also is indicated for treatment of adults with moderate to severe RA, active PsA, active ankylosing spondylitis, active nonradiographic axial spondyloarthritis, and moderate to severe ulcerative colitis and Crohn’s disease, but safety and efficacy for its use in treatment of these conditions in children and adolescents is unknown.
Upadacitinib also is being studied in phase 3 trials for treatment of conditions including alopecia areata, ankylosing spondylitis, atopic dermatitis, axial spondyloarthritis, Crohn’s disease, giant cell arteritis, hidradenitis suppurativa, psoriatic arthritis, RA, systemic lupus erythematosus, Takayasu arteritis, ulcerative colitis, and vitiligo, according to the press release.
Full prescribing information and safety data for upadacitinib are available here.
A version of this article appeared on Medscape.com.
Spondyloarthritis Screening Study Finds ‘High Burden of Need’ in Patients With Inflammatory Bowel Disease
More than 40% of patients with inflammatory bowel disease (IBD) screened positive for joint pain symptomatic of spondyloarthritis (SpA), according to a new study.
Of these patients, 75% did not have any history of arthritis.
“What we know is that a substantial proportion of patients with IBD do report musculoskeletal symptoms, and inflammatory back pain stands out as being one of the more frequent symptoms reported,” said Reem Jan, MBBS, a rheumatologist at the University of Chicago Medicine. She presented the study findings during the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN) in Cleveland.
“Yet a minority of these patients are evaluated by rheumatologists. So that suggests there’s a high burden of need in the IBD population to have this joint pain evaluated and addressed,” she said during her presentation.
She presented preliminary data from an ongoing project to better understand the prevalence of inflammatory arthritis in IBD — estimates range from 17% to 39%— and the risk factors for developing arthritis in this patient population.
Study Details
Researchers enrolled patients from outpatient gastroenterology clinics or procedure units at NYU Langone Health, New York City; Brigham and Women’s Hospital, Boston; University of Colorado Anschutz Medical Campus, Aurora, Colorado; Mayo Clinic, Rochester, Minnesota; University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago; and Icahn School of Medicine at Mount Sinai, New York City. Additional patients were recruited from Mercy Health, a community health system in Ohio.
Upon entry into the study, participants completed a survey documenting their history with joint pain. The survey combined questions from the DETAIL and the IBIS questionnaires.
Between January 2021 and December 2022, 669 patients joined the study. In total, 41% of patients (n = 275) screened positive.
“What really stood out to us was that of all the positive screens, only about a quarter of those patients were known to have SpA,” Dr. Jan said during her presentation. “[This] means 75% of the patients who screened positive were not known to have any type of arthritic disease.”
In addition, only 24% (n = 65) of all patients who screened positive — including those with a SpA diagnosis — had seen a rheumatologist in the previous year.
Among these patients, inflammatory back pain was the most commonly reported symptom, followed by painful swelling of peripheral joints and heel pain.
Excluding patients with a SpA diagnosis, researchers also investigated which characteristics were associated with a higher likelihood of screening positive in the questionnaire. The analysis, including 588 patients, identified the following risk factors:
- Female sex: Odds ratio (OR), 2.0; 95% CI, 1.4-2.9
- Older age: OR, 1.02; 95% CI, 1.01-1.4
- History of smoking: OR, 1.7; 95% CI, 1.1-2.6
- History of prior IBD-related surgery: OR, 1.60; 95% CI, 1.1-2.5
- History of biologic or small molecule therapy: OR, 2.3; 95% CI, 1.4-4.0
Future Directions
Commenting on the study, Mark Hwang, MD, a rheumatologist at UTHealth Houston, noted that it was “very interesting to see the fairly large, positive rates” of joint pain in patients with IBD, which certainly have clinical implications. However, it is not yet known if any of these patients went on to be diagnosed with SpA.
Jan noted that potential next steps include a follow-up analysis of patients who screened positive to see how many went on to see a rheumatologist and which patients were ultimately diagnosed with SpA or other inflammatory arthritis conditions.
These findings are a first step, Dr. Hwang said, and will likely “help further establish some of the validity of these questionnaires by testing in different patient populations,” he noted.
The ultimate goal is to “develop really good strategies to risk stratify IBD patients with the greatest need of rheumatologist consultation,” Dr. Jan said. “We certainly don’t want to see all these patients, so how can we figure out who really needs to be seen?”
Funding information was not available for this study. Dr. Hwang is conducting two clinical trials for psoriatic arthritis sponsored by Janssen and Eli Lilly. Dr. Jan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
More than 40% of patients with inflammatory bowel disease (IBD) screened positive for joint pain symptomatic of spondyloarthritis (SpA), according to a new study.
Of these patients, 75% did not have any history of arthritis.
“What we know is that a substantial proportion of patients with IBD do report musculoskeletal symptoms, and inflammatory back pain stands out as being one of the more frequent symptoms reported,” said Reem Jan, MBBS, a rheumatologist at the University of Chicago Medicine. She presented the study findings during the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN) in Cleveland.
“Yet a minority of these patients are evaluated by rheumatologists. So that suggests there’s a high burden of need in the IBD population to have this joint pain evaluated and addressed,” she said during her presentation.
She presented preliminary data from an ongoing project to better understand the prevalence of inflammatory arthritis in IBD — estimates range from 17% to 39%— and the risk factors for developing arthritis in this patient population.
Study Details
Researchers enrolled patients from outpatient gastroenterology clinics or procedure units at NYU Langone Health, New York City; Brigham and Women’s Hospital, Boston; University of Colorado Anschutz Medical Campus, Aurora, Colorado; Mayo Clinic, Rochester, Minnesota; University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago; and Icahn School of Medicine at Mount Sinai, New York City. Additional patients were recruited from Mercy Health, a community health system in Ohio.
Upon entry into the study, participants completed a survey documenting their history with joint pain. The survey combined questions from the DETAIL and the IBIS questionnaires.
Between January 2021 and December 2022, 669 patients joined the study. In total, 41% of patients (n = 275) screened positive.
“What really stood out to us was that of all the positive screens, only about a quarter of those patients were known to have SpA,” Dr. Jan said during her presentation. “[This] means 75% of the patients who screened positive were not known to have any type of arthritic disease.”
In addition, only 24% (n = 65) of all patients who screened positive — including those with a SpA diagnosis — had seen a rheumatologist in the previous year.
Among these patients, inflammatory back pain was the most commonly reported symptom, followed by painful swelling of peripheral joints and heel pain.
Excluding patients with a SpA diagnosis, researchers also investigated which characteristics were associated with a higher likelihood of screening positive in the questionnaire. The analysis, including 588 patients, identified the following risk factors:
- Female sex: Odds ratio (OR), 2.0; 95% CI, 1.4-2.9
- Older age: OR, 1.02; 95% CI, 1.01-1.4
- History of smoking: OR, 1.7; 95% CI, 1.1-2.6
- History of prior IBD-related surgery: OR, 1.60; 95% CI, 1.1-2.5
- History of biologic or small molecule therapy: OR, 2.3; 95% CI, 1.4-4.0
Future Directions
Commenting on the study, Mark Hwang, MD, a rheumatologist at UTHealth Houston, noted that it was “very interesting to see the fairly large, positive rates” of joint pain in patients with IBD, which certainly have clinical implications. However, it is not yet known if any of these patients went on to be diagnosed with SpA.
Jan noted that potential next steps include a follow-up analysis of patients who screened positive to see how many went on to see a rheumatologist and which patients were ultimately diagnosed with SpA or other inflammatory arthritis conditions.
These findings are a first step, Dr. Hwang said, and will likely “help further establish some of the validity of these questionnaires by testing in different patient populations,” he noted.
The ultimate goal is to “develop really good strategies to risk stratify IBD patients with the greatest need of rheumatologist consultation,” Dr. Jan said. “We certainly don’t want to see all these patients, so how can we figure out who really needs to be seen?”
Funding information was not available for this study. Dr. Hwang is conducting two clinical trials for psoriatic arthritis sponsored by Janssen and Eli Lilly. Dr. Jan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
More than 40% of patients with inflammatory bowel disease (IBD) screened positive for joint pain symptomatic of spondyloarthritis (SpA), according to a new study.
Of these patients, 75% did not have any history of arthritis.
“What we know is that a substantial proportion of patients with IBD do report musculoskeletal symptoms, and inflammatory back pain stands out as being one of the more frequent symptoms reported,” said Reem Jan, MBBS, a rheumatologist at the University of Chicago Medicine. She presented the study findings during the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN) in Cleveland.
“Yet a minority of these patients are evaluated by rheumatologists. So that suggests there’s a high burden of need in the IBD population to have this joint pain evaluated and addressed,” she said during her presentation.
She presented preliminary data from an ongoing project to better understand the prevalence of inflammatory arthritis in IBD — estimates range from 17% to 39%— and the risk factors for developing arthritis in this patient population.
Study Details
Researchers enrolled patients from outpatient gastroenterology clinics or procedure units at NYU Langone Health, New York City; Brigham and Women’s Hospital, Boston; University of Colorado Anschutz Medical Campus, Aurora, Colorado; Mayo Clinic, Rochester, Minnesota; University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago; and Icahn School of Medicine at Mount Sinai, New York City. Additional patients were recruited from Mercy Health, a community health system in Ohio.
Upon entry into the study, participants completed a survey documenting their history with joint pain. The survey combined questions from the DETAIL and the IBIS questionnaires.
Between January 2021 and December 2022, 669 patients joined the study. In total, 41% of patients (n = 275) screened positive.
“What really stood out to us was that of all the positive screens, only about a quarter of those patients were known to have SpA,” Dr. Jan said during her presentation. “[This] means 75% of the patients who screened positive were not known to have any type of arthritic disease.”
In addition, only 24% (n = 65) of all patients who screened positive — including those with a SpA diagnosis — had seen a rheumatologist in the previous year.
Among these patients, inflammatory back pain was the most commonly reported symptom, followed by painful swelling of peripheral joints and heel pain.
Excluding patients with a SpA diagnosis, researchers also investigated which characteristics were associated with a higher likelihood of screening positive in the questionnaire. The analysis, including 588 patients, identified the following risk factors:
- Female sex: Odds ratio (OR), 2.0; 95% CI, 1.4-2.9
- Older age: OR, 1.02; 95% CI, 1.01-1.4
- History of smoking: OR, 1.7; 95% CI, 1.1-2.6
- History of prior IBD-related surgery: OR, 1.60; 95% CI, 1.1-2.5
- History of biologic or small molecule therapy: OR, 2.3; 95% CI, 1.4-4.0
Future Directions
Commenting on the study, Mark Hwang, MD, a rheumatologist at UTHealth Houston, noted that it was “very interesting to see the fairly large, positive rates” of joint pain in patients with IBD, which certainly have clinical implications. However, it is not yet known if any of these patients went on to be diagnosed with SpA.
Jan noted that potential next steps include a follow-up analysis of patients who screened positive to see how many went on to see a rheumatologist and which patients were ultimately diagnosed with SpA or other inflammatory arthritis conditions.
These findings are a first step, Dr. Hwang said, and will likely “help further establish some of the validity of these questionnaires by testing in different patient populations,” he noted.
The ultimate goal is to “develop really good strategies to risk stratify IBD patients with the greatest need of rheumatologist consultation,” Dr. Jan said. “We certainly don’t want to see all these patients, so how can we figure out who really needs to be seen?”
Funding information was not available for this study. Dr. Hwang is conducting two clinical trials for psoriatic arthritis sponsored by Janssen and Eli Lilly. Dr. Jan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM SPARTAN 2024
No Increased Risk for Fractures Seen With Frequent Steroid Injections for Musculoskeletal Conditions
TOPLINE:
The cumulative effect of frequent corticosteroid injections (CSIs), a common treatment for musculoskeletal pain, does not appear to increase the risk for fractures.
METHODOLOGY:
- Researchers utilized an institutional electronic health record database to identify adults in Olmsted County, Minnesota, receiving corticosteroid injections from May 1, 2018, to July 1, 2022.
- Corticosteroid equivalents were calculated for medications injected, including methylprednisolone, triamcinolone, betamethasone, and dexamethasone.
- Patients were excluded if they had a prescription for oral prednisone equivalents greater than 2.5 mg/day for more than 30 days.
- Fracture events were identified using ICD-9 and ICD-10 codes and were included only if they occurred after the first corticosteroid injection.
TAKEAWAY:
- A total of 7197 patients were analyzed, with a mean age of 64.4 years, and of these patients, 346 (4.8%) had a new fracture in a mean time of 329 days from the first corticosteroid injection, including 149 (43.1%) in classic osteoporotic locations.
- The study reported no increased fracture risk associated with corticosteroid injections and no significant difference in fracture rates across cumulative corticosteroid injection dose quartiles, regardless of osteoporosis status.
- Factors such as previous fractures, age, and Charlson Comorbidity Index were associated with a higher risk for fractures, not corticosteroid injections.
IN PRACTICE:
“Clinicians should be reassured that frequent CSI is not associated with higher fracture risk and should not withhold these important pain treatments owing to concern for fracture,” wrote the authors of the study.
SOURCE:
The study was led by Terin T. Sytsma, MD, Division of Community Internal Medicine, Geriatrics, and Palliative Care, Mayo Clinic, Rochester, Minnesota. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s retrospective cohort design and its focus on a predominantly White population in a single community may limit the generalizability of the findings. Confounding variables such as smoking status, alcohol intake, and physical activity were acknowledged as potential contributors to fracture risk. Only clinically apparent fractures were considered, excluding silent vertebral fractures, and differences in corticosteroid formulation were not delineated.
DISCLOSURES:
The study was supported by a Mayo Clinic Catalyst Award to Dr. Sytsma. The authors had no conflicts of interest to report.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
The cumulative effect of frequent corticosteroid injections (CSIs), a common treatment for musculoskeletal pain, does not appear to increase the risk for fractures.
METHODOLOGY:
- Researchers utilized an institutional electronic health record database to identify adults in Olmsted County, Minnesota, receiving corticosteroid injections from May 1, 2018, to July 1, 2022.
- Corticosteroid equivalents were calculated for medications injected, including methylprednisolone, triamcinolone, betamethasone, and dexamethasone.
- Patients were excluded if they had a prescription for oral prednisone equivalents greater than 2.5 mg/day for more than 30 days.
- Fracture events were identified using ICD-9 and ICD-10 codes and were included only if they occurred after the first corticosteroid injection.
TAKEAWAY:
- A total of 7197 patients were analyzed, with a mean age of 64.4 years, and of these patients, 346 (4.8%) had a new fracture in a mean time of 329 days from the first corticosteroid injection, including 149 (43.1%) in classic osteoporotic locations.
- The study reported no increased fracture risk associated with corticosteroid injections and no significant difference in fracture rates across cumulative corticosteroid injection dose quartiles, regardless of osteoporosis status.
- Factors such as previous fractures, age, and Charlson Comorbidity Index were associated with a higher risk for fractures, not corticosteroid injections.
IN PRACTICE:
“Clinicians should be reassured that frequent CSI is not associated with higher fracture risk and should not withhold these important pain treatments owing to concern for fracture,” wrote the authors of the study.
SOURCE:
The study was led by Terin T. Sytsma, MD, Division of Community Internal Medicine, Geriatrics, and Palliative Care, Mayo Clinic, Rochester, Minnesota. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s retrospective cohort design and its focus on a predominantly White population in a single community may limit the generalizability of the findings. Confounding variables such as smoking status, alcohol intake, and physical activity were acknowledged as potential contributors to fracture risk. Only clinically apparent fractures were considered, excluding silent vertebral fractures, and differences in corticosteroid formulation were not delineated.
DISCLOSURES:
The study was supported by a Mayo Clinic Catalyst Award to Dr. Sytsma. The authors had no conflicts of interest to report.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
The cumulative effect of frequent corticosteroid injections (CSIs), a common treatment for musculoskeletal pain, does not appear to increase the risk for fractures.
METHODOLOGY:
- Researchers utilized an institutional electronic health record database to identify adults in Olmsted County, Minnesota, receiving corticosteroid injections from May 1, 2018, to July 1, 2022.
- Corticosteroid equivalents were calculated for medications injected, including methylprednisolone, triamcinolone, betamethasone, and dexamethasone.
- Patients were excluded if they had a prescription for oral prednisone equivalents greater than 2.5 mg/day for more than 30 days.
- Fracture events were identified using ICD-9 and ICD-10 codes and were included only if they occurred after the first corticosteroid injection.
TAKEAWAY:
- A total of 7197 patients were analyzed, with a mean age of 64.4 years, and of these patients, 346 (4.8%) had a new fracture in a mean time of 329 days from the first corticosteroid injection, including 149 (43.1%) in classic osteoporotic locations.
- The study reported no increased fracture risk associated with corticosteroid injections and no significant difference in fracture rates across cumulative corticosteroid injection dose quartiles, regardless of osteoporosis status.
- Factors such as previous fractures, age, and Charlson Comorbidity Index were associated with a higher risk for fractures, not corticosteroid injections.
IN PRACTICE:
“Clinicians should be reassured that frequent CSI is not associated with higher fracture risk and should not withhold these important pain treatments owing to concern for fracture,” wrote the authors of the study.
SOURCE:
The study was led by Terin T. Sytsma, MD, Division of Community Internal Medicine, Geriatrics, and Palliative Care, Mayo Clinic, Rochester, Minnesota. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s retrospective cohort design and its focus on a predominantly White population in a single community may limit the generalizability of the findings. Confounding variables such as smoking status, alcohol intake, and physical activity were acknowledged as potential contributors to fracture risk. Only clinically apparent fractures were considered, excluding silent vertebral fractures, and differences in corticosteroid formulation were not delineated.
DISCLOSURES:
The study was supported by a Mayo Clinic Catalyst Award to Dr. Sytsma. The authors had no conflicts of interest to report.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.








