User login
AHA targets rising prevalence of obstructive sleep apnea in children
Obstructive sleep apnea is becoming more common in children and adolescents as the prevalence of obesity increases, but it may also be a preventable risk factor for cardiovascular disease, according to a new scientific statement from the American Heart Association.
The statement focuses on the links between OSA and CVD risk factors in children and adolescents, and reviews diagnostic strategies and treatments. The writing committee reported that 1%-6% of children and adolescents have OSA, as do up to 60% of adolescents considered obese.
The statement was created by the AHA’s Atherosclerosis, Hypertension, and Obesity in the Young subcommittee of the Council on Cardiovascular Disease in the Young and was published online in the Journal of the American Heart Association.
Carissa M. Baker-Smith, MD, chair of the writing group chair and director of pediatric preventive cardiology at Nemours Cardiac Center, Alfred I. duPont Hospital for Children, Wilmington, Del., explained the rationale for issuing the statement at this time, noting that the relationship between OSA and CVD in adults is well documented.
“There has been less focus on the importance of recognizing and treating sleep apnea in youth,” she said in an interview. “Thus, we felt that it was vitally important to get the word out to parents and to providers that paying attention to the quality and duration of your child’s sleep is vitally important to a child’s long-term heart health. Risk factors for heart disease, when present in childhood, can persist into adulthood.”
Clarity on polysomnography
For making the diagnosis of OSA in children, the statement provides clarity on the use of polysomnography and the role of the apnea-hypopnea index, which is lower in children with OSA than in adults. “One controversy, or at least as I saw it, was whether or not polysomnography testing is always required to make the diagnosis of OSA and before proceeding with tonsil and adenoid removal among children for whom enlarged tonsils and adenoids are present,” Dr. Baker-Smith said. “Polysomnography testing is not always needed before an ear, nose, and throat surgeon may recommend surgery.”
The statement also noted that history and physical examination may not yield enough reliable information to distinguish OSA from snoring.
In areas where sleep laboratories that work with children aren’t available, alternative tests such as daytime nap polysomnography, nocturnal oximetry, and nocturnal video recording may be used – with a caveat. “These alternative tests have weaker positive and negative predictive values when compared with polysomnography,” the writing committee noted. Home sleep apnea tests aren’t recommended in children. Questionnaires “are useful as screening, but not as diagnostic tools.”
Pediatric patients being evaluated for OSA should also be screened for hypertension and metabolic syndrome, as well as central nervous system and behavioral disorders. Diagnosing OSA in children and adolescents requires “a high index of suspicion,” the committee wrote.
Pediatricians and pediatric cardiologists should exercise that high index of suspicion when receiving referrals for cardiac evaluations for attention deficit hyperactivity disorder medication, Dr. Baker-Smith said. “Take the time to ask about a child’s sleep – snoring, apnea, etc. – especially if the child has obesity, difficulty focusing during the day, and if there is evidence of systemic hypertension or other signs of metabolic syndrome,” she said.
Risk factors for OSA in children
The statement also reviewed risk factors for OSA, among them obesity, particularly among children younger than 6 years. Other risk factors include upper and lower airway disease, hypotonia, parental history of hyperplasia of the adenoids and tonsils, craniofacial malformations, and neuromuscular disorders. However, the committee cited “limited data” to support that children with congenital heart disease may be at greater risk for OSA and sleep-disordered breathing (SDB).
Black children are at significantly greater risk, and socioeconomic factors “may be potential confounders,” the committee stated. Other risk factors include allergic rhinitis and sickle cell disease.
But the statement underscores that “obesity is the main risk factor” for OSA in children and adolescents, and that the presence of increased inflammation may explain this relationship. Steroids may alleviate these symptoms, even in nonobese children, and removal of the adenoids or tonsils is an option to reduce inflammation in children with OSA.
“Obesity is a significant risk factor for sleep disturbances and obstructive sleep apnea, and the severity of sleep apnea may be improved by weight-loss interventions, which then improves metabolic syndrome factors such as insulin sensitivity,” Dr. Baker-Smith said. “We need to increase awareness about how the rising prevalence of obesity may be impacting sleep quality in kids and recognize sleep-disordered breathing as something that could contribute to risks for hypertension and later cardiovascular disease.”
Children in whom OSA is suspected should also undergo screening for metabolic syndrome, and central nervous system and behavioral disorders.
Cardiovascular risks
The statement explores the connection between cardiovascular complications and SDB and OSA in depth.
“Inadequate sleep duration of < 5 hours per night in children and adolescents has been linked to an increased risk of hypertension and is also associated with an increased prevalence of obesity,” the committee wrote.
However, the statement left one question hanging: whether OSA alone or obesity cause higher BP in younger patients with OSA. But the committee concluded that BP levels increase with the severity of OSA, although the effects can vary with age. OSA in children peaks between ages 2 and 8, corresponding to the peak prevalence of hypertrophy of the tonsils and adenoids. Children aged 10-11 with more severe OSA may have BP dysregulation, while older adolescents develop higher sustained BP. Obesity may be a confounder for daytime BP elevations, while nighttime hypertension depends less on obesity and more on OSA severity.
“OSA is associated with abnormal BP in youth and, in particular, higher nighttime blood pressures and loss of the normal decline in BP that should occur during sleep,” Dr. Baker-Smith said. “Children with OSA appear to have higher BP than controls during both sleep and wake times, and BP levels increase with increasing severity of OSA.”
Nonetheless, children with OSA are at greater risk for other cardiovascular problems. Left ventricular hypertrophy may be a secondary outcome. “The presence of obstructive sleep apnea in children is associated with an 11-fold increased risk for LVH in children, a relationship not seen in the presence of primary snoring alone,” Dr. Baker-Smith said.
Dr. Baker-Smith had no relevant disclosures. Coauthor Amal Isaiah, MD, is coinventor of an imaging system for sleep apnea and receives royalties from the University of Maryland. The other coauthors have no relevant financial relationships to disclose.
Obstructive sleep apnea is becoming more common in children and adolescents as the prevalence of obesity increases, but it may also be a preventable risk factor for cardiovascular disease, according to a new scientific statement from the American Heart Association.
The statement focuses on the links between OSA and CVD risk factors in children and adolescents, and reviews diagnostic strategies and treatments. The writing committee reported that 1%-6% of children and adolescents have OSA, as do up to 60% of adolescents considered obese.
The statement was created by the AHA’s Atherosclerosis, Hypertension, and Obesity in the Young subcommittee of the Council on Cardiovascular Disease in the Young and was published online in the Journal of the American Heart Association.
Carissa M. Baker-Smith, MD, chair of the writing group chair and director of pediatric preventive cardiology at Nemours Cardiac Center, Alfred I. duPont Hospital for Children, Wilmington, Del., explained the rationale for issuing the statement at this time, noting that the relationship between OSA and CVD in adults is well documented.
“There has been less focus on the importance of recognizing and treating sleep apnea in youth,” she said in an interview. “Thus, we felt that it was vitally important to get the word out to parents and to providers that paying attention to the quality and duration of your child’s sleep is vitally important to a child’s long-term heart health. Risk factors for heart disease, when present in childhood, can persist into adulthood.”
Clarity on polysomnography
For making the diagnosis of OSA in children, the statement provides clarity on the use of polysomnography and the role of the apnea-hypopnea index, which is lower in children with OSA than in adults. “One controversy, or at least as I saw it, was whether or not polysomnography testing is always required to make the diagnosis of OSA and before proceeding with tonsil and adenoid removal among children for whom enlarged tonsils and adenoids are present,” Dr. Baker-Smith said. “Polysomnography testing is not always needed before an ear, nose, and throat surgeon may recommend surgery.”
The statement also noted that history and physical examination may not yield enough reliable information to distinguish OSA from snoring.
In areas where sleep laboratories that work with children aren’t available, alternative tests such as daytime nap polysomnography, nocturnal oximetry, and nocturnal video recording may be used – with a caveat. “These alternative tests have weaker positive and negative predictive values when compared with polysomnography,” the writing committee noted. Home sleep apnea tests aren’t recommended in children. Questionnaires “are useful as screening, but not as diagnostic tools.”
Pediatric patients being evaluated for OSA should also be screened for hypertension and metabolic syndrome, as well as central nervous system and behavioral disorders. Diagnosing OSA in children and adolescents requires “a high index of suspicion,” the committee wrote.
Pediatricians and pediatric cardiologists should exercise that high index of suspicion when receiving referrals for cardiac evaluations for attention deficit hyperactivity disorder medication, Dr. Baker-Smith said. “Take the time to ask about a child’s sleep – snoring, apnea, etc. – especially if the child has obesity, difficulty focusing during the day, and if there is evidence of systemic hypertension or other signs of metabolic syndrome,” she said.
Risk factors for OSA in children
The statement also reviewed risk factors for OSA, among them obesity, particularly among children younger than 6 years. Other risk factors include upper and lower airway disease, hypotonia, parental history of hyperplasia of the adenoids and tonsils, craniofacial malformations, and neuromuscular disorders. However, the committee cited “limited data” to support that children with congenital heart disease may be at greater risk for OSA and sleep-disordered breathing (SDB).
Black children are at significantly greater risk, and socioeconomic factors “may be potential confounders,” the committee stated. Other risk factors include allergic rhinitis and sickle cell disease.
But the statement underscores that “obesity is the main risk factor” for OSA in children and adolescents, and that the presence of increased inflammation may explain this relationship. Steroids may alleviate these symptoms, even in nonobese children, and removal of the adenoids or tonsils is an option to reduce inflammation in children with OSA.
“Obesity is a significant risk factor for sleep disturbances and obstructive sleep apnea, and the severity of sleep apnea may be improved by weight-loss interventions, which then improves metabolic syndrome factors such as insulin sensitivity,” Dr. Baker-Smith said. “We need to increase awareness about how the rising prevalence of obesity may be impacting sleep quality in kids and recognize sleep-disordered breathing as something that could contribute to risks for hypertension and later cardiovascular disease.”
Children in whom OSA is suspected should also undergo screening for metabolic syndrome, and central nervous system and behavioral disorders.
Cardiovascular risks
The statement explores the connection between cardiovascular complications and SDB and OSA in depth.
“Inadequate sleep duration of < 5 hours per night in children and adolescents has been linked to an increased risk of hypertension and is also associated with an increased prevalence of obesity,” the committee wrote.
However, the statement left one question hanging: whether OSA alone or obesity cause higher BP in younger patients with OSA. But the committee concluded that BP levels increase with the severity of OSA, although the effects can vary with age. OSA in children peaks between ages 2 and 8, corresponding to the peak prevalence of hypertrophy of the tonsils and adenoids. Children aged 10-11 with more severe OSA may have BP dysregulation, while older adolescents develop higher sustained BP. Obesity may be a confounder for daytime BP elevations, while nighttime hypertension depends less on obesity and more on OSA severity.
“OSA is associated with abnormal BP in youth and, in particular, higher nighttime blood pressures and loss of the normal decline in BP that should occur during sleep,” Dr. Baker-Smith said. “Children with OSA appear to have higher BP than controls during both sleep and wake times, and BP levels increase with increasing severity of OSA.”
Nonetheless, children with OSA are at greater risk for other cardiovascular problems. Left ventricular hypertrophy may be a secondary outcome. “The presence of obstructive sleep apnea in children is associated with an 11-fold increased risk for LVH in children, a relationship not seen in the presence of primary snoring alone,” Dr. Baker-Smith said.
Dr. Baker-Smith had no relevant disclosures. Coauthor Amal Isaiah, MD, is coinventor of an imaging system for sleep apnea and receives royalties from the University of Maryland. The other coauthors have no relevant financial relationships to disclose.
Obstructive sleep apnea is becoming more common in children and adolescents as the prevalence of obesity increases, but it may also be a preventable risk factor for cardiovascular disease, according to a new scientific statement from the American Heart Association.
The statement focuses on the links between OSA and CVD risk factors in children and adolescents, and reviews diagnostic strategies and treatments. The writing committee reported that 1%-6% of children and adolescents have OSA, as do up to 60% of adolescents considered obese.
The statement was created by the AHA’s Atherosclerosis, Hypertension, and Obesity in the Young subcommittee of the Council on Cardiovascular Disease in the Young and was published online in the Journal of the American Heart Association.
Carissa M. Baker-Smith, MD, chair of the writing group chair and director of pediatric preventive cardiology at Nemours Cardiac Center, Alfred I. duPont Hospital for Children, Wilmington, Del., explained the rationale for issuing the statement at this time, noting that the relationship between OSA and CVD in adults is well documented.
“There has been less focus on the importance of recognizing and treating sleep apnea in youth,” she said in an interview. “Thus, we felt that it was vitally important to get the word out to parents and to providers that paying attention to the quality and duration of your child’s sleep is vitally important to a child’s long-term heart health. Risk factors for heart disease, when present in childhood, can persist into adulthood.”
Clarity on polysomnography
For making the diagnosis of OSA in children, the statement provides clarity on the use of polysomnography and the role of the apnea-hypopnea index, which is lower in children with OSA than in adults. “One controversy, or at least as I saw it, was whether or not polysomnography testing is always required to make the diagnosis of OSA and before proceeding with tonsil and adenoid removal among children for whom enlarged tonsils and adenoids are present,” Dr. Baker-Smith said. “Polysomnography testing is not always needed before an ear, nose, and throat surgeon may recommend surgery.”
The statement also noted that history and physical examination may not yield enough reliable information to distinguish OSA from snoring.
In areas where sleep laboratories that work with children aren’t available, alternative tests such as daytime nap polysomnography, nocturnal oximetry, and nocturnal video recording may be used – with a caveat. “These alternative tests have weaker positive and negative predictive values when compared with polysomnography,” the writing committee noted. Home sleep apnea tests aren’t recommended in children. Questionnaires “are useful as screening, but not as diagnostic tools.”
Pediatric patients being evaluated for OSA should also be screened for hypertension and metabolic syndrome, as well as central nervous system and behavioral disorders. Diagnosing OSA in children and adolescents requires “a high index of suspicion,” the committee wrote.
Pediatricians and pediatric cardiologists should exercise that high index of suspicion when receiving referrals for cardiac evaluations for attention deficit hyperactivity disorder medication, Dr. Baker-Smith said. “Take the time to ask about a child’s sleep – snoring, apnea, etc. – especially if the child has obesity, difficulty focusing during the day, and if there is evidence of systemic hypertension or other signs of metabolic syndrome,” she said.
Risk factors for OSA in children
The statement also reviewed risk factors for OSA, among them obesity, particularly among children younger than 6 years. Other risk factors include upper and lower airway disease, hypotonia, parental history of hyperplasia of the adenoids and tonsils, craniofacial malformations, and neuromuscular disorders. However, the committee cited “limited data” to support that children with congenital heart disease may be at greater risk for OSA and sleep-disordered breathing (SDB).
Black children are at significantly greater risk, and socioeconomic factors “may be potential confounders,” the committee stated. Other risk factors include allergic rhinitis and sickle cell disease.
But the statement underscores that “obesity is the main risk factor” for OSA in children and adolescents, and that the presence of increased inflammation may explain this relationship. Steroids may alleviate these symptoms, even in nonobese children, and removal of the adenoids or tonsils is an option to reduce inflammation in children with OSA.
“Obesity is a significant risk factor for sleep disturbances and obstructive sleep apnea, and the severity of sleep apnea may be improved by weight-loss interventions, which then improves metabolic syndrome factors such as insulin sensitivity,” Dr. Baker-Smith said. “We need to increase awareness about how the rising prevalence of obesity may be impacting sleep quality in kids and recognize sleep-disordered breathing as something that could contribute to risks for hypertension and later cardiovascular disease.”
Children in whom OSA is suspected should also undergo screening for metabolic syndrome, and central nervous system and behavioral disorders.
Cardiovascular risks
The statement explores the connection between cardiovascular complications and SDB and OSA in depth.
“Inadequate sleep duration of < 5 hours per night in children and adolescents has been linked to an increased risk of hypertension and is also associated with an increased prevalence of obesity,” the committee wrote.
However, the statement left one question hanging: whether OSA alone or obesity cause higher BP in younger patients with OSA. But the committee concluded that BP levels increase with the severity of OSA, although the effects can vary with age. OSA in children peaks between ages 2 and 8, corresponding to the peak prevalence of hypertrophy of the tonsils and adenoids. Children aged 10-11 with more severe OSA may have BP dysregulation, while older adolescents develop higher sustained BP. Obesity may be a confounder for daytime BP elevations, while nighttime hypertension depends less on obesity and more on OSA severity.
“OSA is associated with abnormal BP in youth and, in particular, higher nighttime blood pressures and loss of the normal decline in BP that should occur during sleep,” Dr. Baker-Smith said. “Children with OSA appear to have higher BP than controls during both sleep and wake times, and BP levels increase with increasing severity of OSA.”
Nonetheless, children with OSA are at greater risk for other cardiovascular problems. Left ventricular hypertrophy may be a secondary outcome. “The presence of obstructive sleep apnea in children is associated with an 11-fold increased risk for LVH in children, a relationship not seen in the presence of primary snoring alone,” Dr. Baker-Smith said.
Dr. Baker-Smith had no relevant disclosures. Coauthor Amal Isaiah, MD, is coinventor of an imaging system for sleep apnea and receives royalties from the University of Maryland. The other coauthors have no relevant financial relationships to disclose.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
Managing sleep in the elderly
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
FROM FOCUS ON NEUROPSYCHIATRY 2021
Brain memory signals appear to regulate metabolism
Rhythmic brain signals that help encode memories also appear to influence blood sugar levels and may regulate the timing of the release of hormones, early, pre-clinical research shows.
“Our study is the first to show how clusters of brain cell firing in the hippocampus may directly regulate metabolism,” senior author György Buzsáki, MD, PhD, professor, department of neuroscience and physiology, NYU Grossman School of Medicine and NYU Langone Health, said in a news release.
“Evidence suggests that the brain evolved, for reasons of efficiency, to use the same signals to achieve two very different functions in terms of memory and hormonal regulation,” added corresponding author David Tingley, PhD, a post-doctoral scholar in Dr. Buzsáki’s lab.
The study was published online August 11 in Nature.
It’s recently been discovered that populations of hippocampal neurons fire within milliseconds of each other in cycles. This firing pattern is called a “sharp wave ripple” for the shape it takes when captured graphically by electroencephalogram.
In their study, Dr. Buzsáki, Dr. Tingley, and colleagues observed that clusters of sharp wave ripples recorded from the hippocampus of rats were “reliably” and rapidly, followed by decreases in blood sugar concentrations in the animals.
“This correlation was not dependent on circadian, ultradian, or meal-triggered fluctuations; it could be mimicked with optogenetically induced ripples in the hippocampus, but not in the parietal cortex, and was attenuated to chance levels by pharmacogenetically suppressing activity of the lateral septum (LS), the major conduit between the hippocampus and hypothalamus,” the researchers report.
These observations suggest that hippocampal sharp wave ripples may regulate the timing of the release of hormones, possibly including insulin, by the pancreas and liver, as well as other hormones by the pituitary gland, the researchers note.
As sharp wave ripples mostly occur during non-rapid eye movement sleep, the impact of sleep disturbance on sharp wave ripples may provide a mechanistic link between poor sleep and high blood sugar levels seen in type 2 diabetes, they suggest.
“There are a couple of experimental studies showing that if you deprive a young healthy person from sleep [for 48 hours], their glucose tolerance resembles” that of a person with diabetes, Dr. Buzsáki noted in an interview.
Moving forward, the researchers will seek to extend their theory that several hormones could be affected by nightly sharp wave ripples.
The research was funded by National Institutes of Health. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rhythmic brain signals that help encode memories also appear to influence blood sugar levels and may regulate the timing of the release of hormones, early, pre-clinical research shows.
“Our study is the first to show how clusters of brain cell firing in the hippocampus may directly regulate metabolism,” senior author György Buzsáki, MD, PhD, professor, department of neuroscience and physiology, NYU Grossman School of Medicine and NYU Langone Health, said in a news release.
“Evidence suggests that the brain evolved, for reasons of efficiency, to use the same signals to achieve two very different functions in terms of memory and hormonal regulation,” added corresponding author David Tingley, PhD, a post-doctoral scholar in Dr. Buzsáki’s lab.
The study was published online August 11 in Nature.
It’s recently been discovered that populations of hippocampal neurons fire within milliseconds of each other in cycles. This firing pattern is called a “sharp wave ripple” for the shape it takes when captured graphically by electroencephalogram.
In their study, Dr. Buzsáki, Dr. Tingley, and colleagues observed that clusters of sharp wave ripples recorded from the hippocampus of rats were “reliably” and rapidly, followed by decreases in blood sugar concentrations in the animals.
“This correlation was not dependent on circadian, ultradian, or meal-triggered fluctuations; it could be mimicked with optogenetically induced ripples in the hippocampus, but not in the parietal cortex, and was attenuated to chance levels by pharmacogenetically suppressing activity of the lateral septum (LS), the major conduit between the hippocampus and hypothalamus,” the researchers report.
These observations suggest that hippocampal sharp wave ripples may regulate the timing of the release of hormones, possibly including insulin, by the pancreas and liver, as well as other hormones by the pituitary gland, the researchers note.
As sharp wave ripples mostly occur during non-rapid eye movement sleep, the impact of sleep disturbance on sharp wave ripples may provide a mechanistic link between poor sleep and high blood sugar levels seen in type 2 diabetes, they suggest.
“There are a couple of experimental studies showing that if you deprive a young healthy person from sleep [for 48 hours], their glucose tolerance resembles” that of a person with diabetes, Dr. Buzsáki noted in an interview.
Moving forward, the researchers will seek to extend their theory that several hormones could be affected by nightly sharp wave ripples.
The research was funded by National Institutes of Health. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rhythmic brain signals that help encode memories also appear to influence blood sugar levels and may regulate the timing of the release of hormones, early, pre-clinical research shows.
“Our study is the first to show how clusters of brain cell firing in the hippocampus may directly regulate metabolism,” senior author György Buzsáki, MD, PhD, professor, department of neuroscience and physiology, NYU Grossman School of Medicine and NYU Langone Health, said in a news release.
“Evidence suggests that the brain evolved, for reasons of efficiency, to use the same signals to achieve two very different functions in terms of memory and hormonal regulation,” added corresponding author David Tingley, PhD, a post-doctoral scholar in Dr. Buzsáki’s lab.
The study was published online August 11 in Nature.
It’s recently been discovered that populations of hippocampal neurons fire within milliseconds of each other in cycles. This firing pattern is called a “sharp wave ripple” for the shape it takes when captured graphically by electroencephalogram.
In their study, Dr. Buzsáki, Dr. Tingley, and colleagues observed that clusters of sharp wave ripples recorded from the hippocampus of rats were “reliably” and rapidly, followed by decreases in blood sugar concentrations in the animals.
“This correlation was not dependent on circadian, ultradian, or meal-triggered fluctuations; it could be mimicked with optogenetically induced ripples in the hippocampus, but not in the parietal cortex, and was attenuated to chance levels by pharmacogenetically suppressing activity of the lateral septum (LS), the major conduit between the hippocampus and hypothalamus,” the researchers report.
These observations suggest that hippocampal sharp wave ripples may regulate the timing of the release of hormones, possibly including insulin, by the pancreas and liver, as well as other hormones by the pituitary gland, the researchers note.
As sharp wave ripples mostly occur during non-rapid eye movement sleep, the impact of sleep disturbance on sharp wave ripples may provide a mechanistic link between poor sleep and high blood sugar levels seen in type 2 diabetes, they suggest.
“There are a couple of experimental studies showing that if you deprive a young healthy person from sleep [for 48 hours], their glucose tolerance resembles” that of a person with diabetes, Dr. Buzsáki noted in an interview.
Moving forward, the researchers will seek to extend their theory that several hormones could be affected by nightly sharp wave ripples.
The research was funded by National Institutes of Health. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves first drug for idiopathic hypersomnia
, the company announced in a news release.
It marks the second approval for Xywav. The FDA approved it last year for the treatment of cataplexy or excessive daytime sleepiness in patients with narcolepsy as young as 7 years of age.
This recent approval is the first for a treatment for idiopathic hypersomnia.
“Idiopathic hypersomnia can have a significant impact on the social, educational, and occupational functioning of people living with the condition,” Diane Powell, board chair and CEO of the Hypersomnia Foundation, noted in the release.
This FDA approval “is a major milestone for the entire idiopathic hypersomnia community as Xywav becomes the first medicine approved to manage this chronic sleep disorder,” said Ms. Powell.
Low sodium oxybate product
Xywav is a novel oxybate product with a unique composition of cations. It contains 92% less sodium than sodium oxybate (Xyrem) at the recommended adult dosage range of 6 to 9 g, the company noted in a news release.
An estimated 37,000 people in the United States have been diagnosed with idiopathic hypersomnia, a neurologic sleep disorder characterized by chronic excessive daytime sleepiness.
Other symptoms of the disorder may include severe sleep inertia or sleep drunkenness (prolonged difficulty waking with frequent re-entries into sleep, confusion, and irritability), as well as prolonged, nonrestorative night-time sleep, cognitive impairment, and long and unrefreshing naps.
The approval was based on findings from a phase 3, double-blind, multicenter, placebo-controlled, randomized withdrawal study.
Results showed “statistically significant and clinically meaningful” differences compared with placebo in change in the primary endpoint of Epworth Sleepiness Scale score (P < .0001) and the secondary endpoints of Patient Global Impression of Change (P < .0001) and the Idiopathic Hypersomnia Severity Scale (P < .0001), the company reported.
The most common adverse reactions were nausea, headache, dizziness, anxiety, insomnia, decreased appetite, hyperhidrosis, vomiting, diarrhea, dry mouth, parasomnia, somnolence, fatigue, and tremor.
The novel agent can be administered once or twice nightly for the treatment of idiopathic hypersomnia in adults.
“To optimize response, a patient’s health care provider may consider prescribing a twice-nightly regimen in equally or unequally divided doses at bedtime and 2.5 to 4 hours later and gradually titrate Xywav so that a patient may receive an individualized dose and regimen based on efficacy and tolerability,” the company said.
Xywav carries a boxed warning because it is a central nervous system depressant and because there is potential for abuse and misuse. The drug is only available through a risk evaluation and mitigation strategy (REMS) program.
The company plans to make Xywav available to patients with idiopathic hypersomnia later this year following implementation of the REMS program.
A version of this article first appeared on Medscape.com.
, the company announced in a news release.
It marks the second approval for Xywav. The FDA approved it last year for the treatment of cataplexy or excessive daytime sleepiness in patients with narcolepsy as young as 7 years of age.
This recent approval is the first for a treatment for idiopathic hypersomnia.
“Idiopathic hypersomnia can have a significant impact on the social, educational, and occupational functioning of people living with the condition,” Diane Powell, board chair and CEO of the Hypersomnia Foundation, noted in the release.
This FDA approval “is a major milestone for the entire idiopathic hypersomnia community as Xywav becomes the first medicine approved to manage this chronic sleep disorder,” said Ms. Powell.
Low sodium oxybate product
Xywav is a novel oxybate product with a unique composition of cations. It contains 92% less sodium than sodium oxybate (Xyrem) at the recommended adult dosage range of 6 to 9 g, the company noted in a news release.
An estimated 37,000 people in the United States have been diagnosed with idiopathic hypersomnia, a neurologic sleep disorder characterized by chronic excessive daytime sleepiness.
Other symptoms of the disorder may include severe sleep inertia or sleep drunkenness (prolonged difficulty waking with frequent re-entries into sleep, confusion, and irritability), as well as prolonged, nonrestorative night-time sleep, cognitive impairment, and long and unrefreshing naps.
The approval was based on findings from a phase 3, double-blind, multicenter, placebo-controlled, randomized withdrawal study.
Results showed “statistically significant and clinically meaningful” differences compared with placebo in change in the primary endpoint of Epworth Sleepiness Scale score (P < .0001) and the secondary endpoints of Patient Global Impression of Change (P < .0001) and the Idiopathic Hypersomnia Severity Scale (P < .0001), the company reported.
The most common adverse reactions were nausea, headache, dizziness, anxiety, insomnia, decreased appetite, hyperhidrosis, vomiting, diarrhea, dry mouth, parasomnia, somnolence, fatigue, and tremor.
The novel agent can be administered once or twice nightly for the treatment of idiopathic hypersomnia in adults.
“To optimize response, a patient’s health care provider may consider prescribing a twice-nightly regimen in equally or unequally divided doses at bedtime and 2.5 to 4 hours later and gradually titrate Xywav so that a patient may receive an individualized dose and regimen based on efficacy and tolerability,” the company said.
Xywav carries a boxed warning because it is a central nervous system depressant and because there is potential for abuse and misuse. The drug is only available through a risk evaluation and mitigation strategy (REMS) program.
The company plans to make Xywav available to patients with idiopathic hypersomnia later this year following implementation of the REMS program.
A version of this article first appeared on Medscape.com.
, the company announced in a news release.
It marks the second approval for Xywav. The FDA approved it last year for the treatment of cataplexy or excessive daytime sleepiness in patients with narcolepsy as young as 7 years of age.
This recent approval is the first for a treatment for idiopathic hypersomnia.
“Idiopathic hypersomnia can have a significant impact on the social, educational, and occupational functioning of people living with the condition,” Diane Powell, board chair and CEO of the Hypersomnia Foundation, noted in the release.
This FDA approval “is a major milestone for the entire idiopathic hypersomnia community as Xywav becomes the first medicine approved to manage this chronic sleep disorder,” said Ms. Powell.
Low sodium oxybate product
Xywav is a novel oxybate product with a unique composition of cations. It contains 92% less sodium than sodium oxybate (Xyrem) at the recommended adult dosage range of 6 to 9 g, the company noted in a news release.
An estimated 37,000 people in the United States have been diagnosed with idiopathic hypersomnia, a neurologic sleep disorder characterized by chronic excessive daytime sleepiness.
Other symptoms of the disorder may include severe sleep inertia or sleep drunkenness (prolonged difficulty waking with frequent re-entries into sleep, confusion, and irritability), as well as prolonged, nonrestorative night-time sleep, cognitive impairment, and long and unrefreshing naps.
The approval was based on findings from a phase 3, double-blind, multicenter, placebo-controlled, randomized withdrawal study.
Results showed “statistically significant and clinically meaningful” differences compared with placebo in change in the primary endpoint of Epworth Sleepiness Scale score (P < .0001) and the secondary endpoints of Patient Global Impression of Change (P < .0001) and the Idiopathic Hypersomnia Severity Scale (P < .0001), the company reported.
The most common adverse reactions were nausea, headache, dizziness, anxiety, insomnia, decreased appetite, hyperhidrosis, vomiting, diarrhea, dry mouth, parasomnia, somnolence, fatigue, and tremor.
The novel agent can be administered once or twice nightly for the treatment of idiopathic hypersomnia in adults.
“To optimize response, a patient’s health care provider may consider prescribing a twice-nightly regimen in equally or unequally divided doses at bedtime and 2.5 to 4 hours later and gradually titrate Xywav so that a patient may receive an individualized dose and regimen based on efficacy and tolerability,” the company said.
Xywav carries a boxed warning because it is a central nervous system depressant and because there is potential for abuse and misuse. The drug is only available through a risk evaluation and mitigation strategy (REMS) program.
The company plans to make Xywav available to patients with idiopathic hypersomnia later this year following implementation of the REMS program.
A version of this article first appeared on Medscape.com.
Late-onset, treatment-resistant anxiety and depression
CASE Anxious and can’t sleep
Mr. A, age 41, presents to his primary care physician (PCP) with anxiety and insomnia. He describes having generalized anxiety with initial and middle insomnia, and says he is sleeping an average of 2 hours per night. He denies any other psychiatric symptoms. Mr. A has no significant psychiatric or medical history.
Mr. A is initiated on zolpidem tartrate, 12.5 mg every night at bedtime, and paroxetine, 20 mg every night at bedtime, for anxiety and insomnia, but these medications result in little to no improvement.
During a 4-month period, he is treated with trials of alprazolam, 0.5 mg every 8 hours as needed; diazepam 5 mg twice a day as needed; diphenhydramine, 50 mg at bedtime; and eszopiclone, 3 mg at bedtime. Despite these treatments, he experiences increased anxiety and insomnia, and develops depressive symptoms, including depressed mood, poor concentration, general malaise, extreme fatigue, a 15-pound unintentional weight loss, erectile dysfunction, and decreased libido. Mr. A denies having suicidal or homicidal ideations. Additionally, he typically goes to the gym approximately 3 times per week, and has noticed that the amount of weight he is able to lift has decreased, which is distressing. Previously, he had been able to lift 300 pounds, but now he can only lift 200 pounds.
[polldaddy:10891920]
The authors’ observations
Insomnia, anxiety, and depression are common chief complaints in medical settings. However, some psychiatric presentations may have an underlying medical etiology.
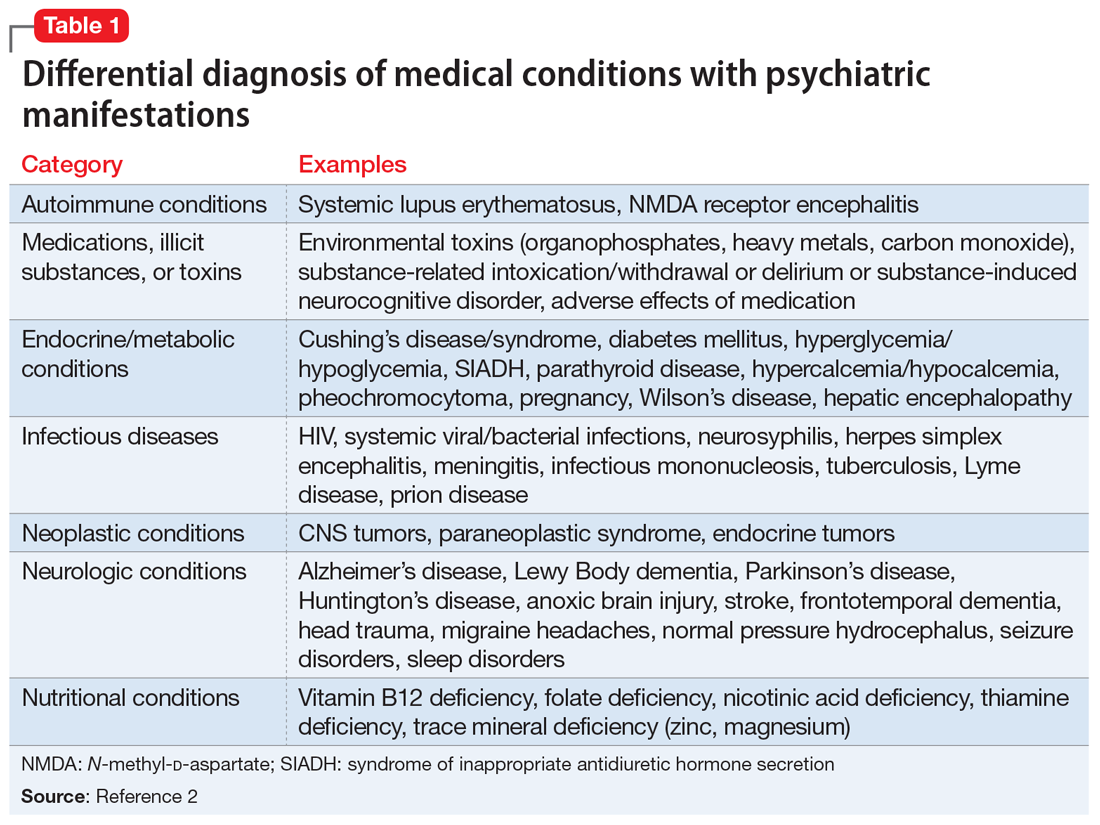
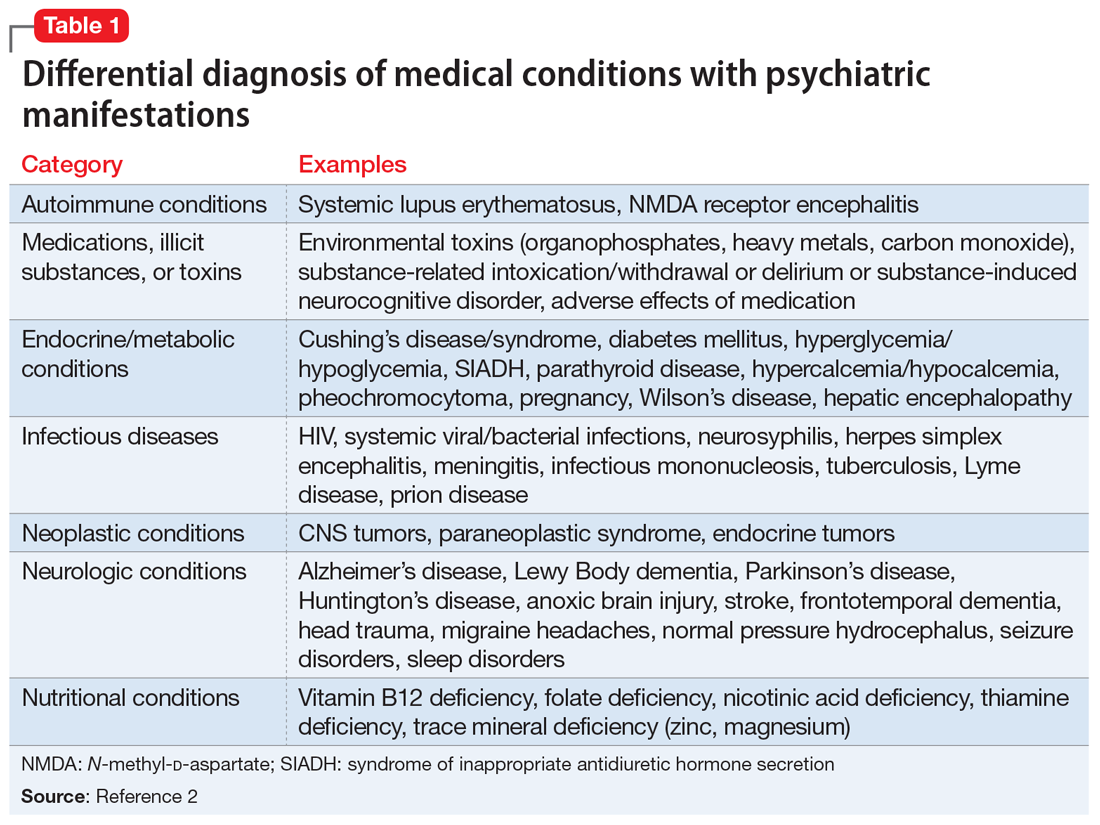
DSM-5 requires that medical conditions be ruled out in order for a patient to meet criteria for a psychiatric diagnosis.1 Medical differential diagnoses for patients with psychiatric symptoms can include autoimmune, drug/toxin, metabolic, infectious, neoplastic, neurologic, and nutritional etiologies (Table 12). To rule out the possibility of an underlying medical etiology, general screening guidelines include complete blood count, complete metabolic panel, urinalysis, and urine drug screen with alcohol. Human immunodeficiency virus testing and thyroid hormone testing are also commonly ordered.3 Further laboratory testing and imaging is typically not warranted in the absence of historical or physical findings because they are not advocated as cost-effective, so health care professionals must use their clinical judgment to determine appropriate further evaluation. The onset of anxiety most commonly occurs in late adolescence early and adulthood, but Mr. A experienced his first symptoms of anxiety at age 41.2 Mr. A’s age, lack of psychiatric or family history of mental illness, acute onset of symptoms, and failure of symptoms to abate with standard psychiatric treatments warrant a more extensive workup.
EVALUATION Imaging reveals an important finding
Because Mr. A’s symptoms do not improve with standard psychiatric treatments, his PCP orders standard laboratory bloodwork to investigate a possible medical etiology; however, his results are all within normal range.
After the PCP’s niece is coincidentally diagnosed with a pituitary macroadenoma, the PCP orders brain imaging for Mr. A. Results of an MRI show that Mr. A has a 1.6-cm macroadenoma of the pituitary. He is referred to an endocrinologist, who orders additional laboratory tests that show an elevated 24-hour free urine cortisol level of 73 μg/24 h (normal range: 3.5 to 45 μg/24 h), suggesting that Mr. A’s anxiety may be due to Cushing’s disease or that his anxiety caused falsely elevated urinary cortisol levels. Four weeks later, bloodwork is repeated and shows an abnormal dexamethasone suppression test, and 2 more elevated 24-hour free urine cortisol levels of 76 μg/24 h and 150 μg/24 h. A repeat MRI shows a 1.8-cm, mostly cystic sellar mass, indicating the need for surgical intervention. Although the tumor is large and shows optic nerve compression, Mr. A does not complain of headaches or changes in vision.
Continue to: Two months later...
Two months later, Mr. A undergoes a transsphenoidal tumor resection of the pituitary adenoma, and biopsy results confirm an adrenocorticotropic hormone (ACTH)-secreting pituitary macroadenoma, which is consistent with Cushing’s disease. Following surgery, steroid treatment with dexamethasone is discontinued due to a persistently elevated
[polldaddy:10891923]
The authors’ observations
Chronic excess glucocorticoid production is the underlying pathophysiology of Cushing’s disease, which is most commonly caused by an ACTH-producing adenoma.4,5 When these hormones become dysregulated, the result can be over- or underproduction of cortisol, which can lead to physical and psychiatric manifestations.6
Cushing’s disease most commonly manifests with the physical symptoms of centripetal fat deposition, abdominal striae, facial plethora, muscle atrophy, bone density loss, immunosuppression, and cardiovascular complications.5
Hypercortisolism can precipitate anxiety (12% to 79%), mood disorders (50% to 70%), and (less commonly) psychotic disorders; however, in a clinical setting, if a patient presented with one of these as a chief complaint, they would likely first be treated psychiatrically rather than worked up medically for a rare medical condition.5,7-13
Mr. A’s initial bloodwork was unremarkable, but cortisol levels were not obtained at that time because testing for cortisol levels to rule out an underlying medical condition is not routine in patients with depression and anxiety. In Mr. A’s case, a neuroendocrine workup was only ordered once his PCP’s niece coincidentally was diagnosed with a pituitary adenoma.
Continue to: For Mr. A...
For Mr. A, Cushing’s disease presented as a psychiatric disorder with anxiety and insomnia that were resistant to numerous psychiatric medications during an 8-month period. If Mr. A’s PCP had not ordered a brain MRI, he may have continued to receive ineffective psychiatric treatment for some time. Many of Mr. A’s physical symptoms were consistent with Cushing’s disease and mental illness, including erectile dysfunction, fatigue, and muscle weakness; however, his 15-pound weight loss pointed more toward psychiatric illness and further disguised his underlying medical diagnosis, because sudden weight gain is commonly seen in Cushing’s disease (Table 24,5,7,9).
TREATMENT Persistent psychiatric symptoms, then finally relief
Four weeks after surgery, Mr. A’s psychiatric symptoms gradually intensify, which prompts him to see a psychiatrist. A mental status examination (MSE) shows that he is well-nourished, with normal activity, appropriate behavior, and coherent thought process, but depressed mood and flat affect. He denies suicidal or homicidal ideation. He reports that despite being advised to have realistic expectations, he had high hopes that the surgery would lead to remission of all his symptoms, and expresses disappointment that he does not feel “back to normal.”
Six days later, Mr. A’s wife takes him to the hospital. His MSE shows that he has a tense appearance, fidgety activity, depressed and anxious mood, restricted affect, circumstantial thought process, and paranoid delusions that his wife was plotting against him. He says he still is experiencing insomnia. He also discloses having suicidal ideations with a plan and intent to overdose on medication, as well as homicidal ideations about killing his wife and children. Mr. A provides reasons for why he would want to hurt his family, and does not appear to be bothered by these thoughts.
Mr. A is admitted to the inpatient psychiatric unit and is prescribed quetiapine, 100 mg every night at bedtime. During the next 2 days, quetiapine is titrated to 300 mg every night at bedtime. On hospital Day 3, Mr. A says he is feeling worse than the previous days. He is still having vague suicidal thoughts and feels agitated, guilty, and depressed. To treat these persistent symptoms, quetiapine is further increased to 400 mg every night at bedtime, and he is initiated on bupropion XL, 150 mg, to treat persistent symptoms.
After 1 week of hospitalization, the treatment team meets with Mr. A and his wife, who has been supportive throughout her husband’s hospitalization. During the meeting, they both agree that Mr. A has experienced some improvement because he is no longer having suicidal or homicidal thoughts, but he is still feeling depressed and frustrated by his continued insomnia. Following the meeting, Mr. A’s quetiapine is further increased to 450 mg every night at bedtime to address continued insomnia, and bupropion XL is increased to 300 mg/d to address continued depressive symptoms. During the next few days, his affective symptoms improve; however, his initial insomnia continues, and quetiapine is further increased to 500 mg every night at bedtime.
Continue to: On hospital Day 20...
On hospital Day 20, Mr. A is discharged back to his outpatient psychiatrist and receives quetiapine, 500 mg every night at bedtime, and bupropion XL, 300 mg/d. Although Mr. A’s depression and anxiety continue to be well controlled, his insomnia persists. Sleep hygiene is addressed, and alprazolam, 0.5 mg every night at bedtime, is added to his regimen, which proves to be effective.
OUTCOME A slow remission
After a year of treatment, Mr. A is slowly tapered off of all medications. Two years later, he is in complete remission of all psychiatric symptoms and no longer requires any psychotropic medications.
The authors’ observations
Treatment for hypercortisolism in patients with psychiatric symptoms triggered by glucocorticoid imbalance has typically resulted in a decrease in the severity of their psychiatric symptoms.9,11 A prospective longitudinal study examining 33 patients found that correction of hypercortisolism in patients with Cushing’s syndrome often led to resolution of their psychiatric symptoms, with 87.9% of patients back to baseline within 1 year.14 However, to our knowledge, few reports have described the management of patients whose symptoms are resistant to treatment of hypercortisolism.
In our case, after transsphenoidal resection of an adenoma, Mr. A became suicidal and paranoid, and his anxiety and insomnia also persisted. A possible explanation for the worsening of Mr. A’s symptoms after surgery could be the slow recovery of the hypothalamic-pituitary-adrenal (HPA) axis and therefore a temporary deficiency in glucocorticoid, which caused an increase in catecholamines, leading to an increase in stress.14 This concept of a “slow recovery” is supported by the fact that Mr. A was successfully weaned off all medication after 1 year of treatment, and achieved complete remission of psychiatric symptoms for >2 years. Furthermore, the severity of Mr. A’s symptoms appeared to correlate with his 24-hour urine cortisol and
Future research should evaluate the utility of screening all patients with treatment-resistant anxiety and/or insomnia for hypercortisolism. Even without other clues to endocrinopathies, serum cortisol levels can be used as a screening tool for diagnosing underlying medical causes in patients with anxiety and depression.2 A greater understanding of the relationship between medical and psychiatric manifestations will allow clinicians to better care for patients. Further research is needed to elucidate the quantitative relationship between cortisol levels and anxiety to evaluate severity, guide treatment planning, and follow treatment response for patients with anxiety. It may be useful to determine the threshold between elevated cortisol levels due to anxiety vs elevated cortisol due to an underlying medical pathology such as Cushing’s disease. Additionally, little research has been conducted to compare how psychiatric symptoms respond to pituitary macroadenoma resection alone, pharmaceutical intervention alone, or a combination of these approaches. It would be beneficial to evaluate these treatment strategies to elucidate the most effective method to reduce psychiatric symptoms in patients with hypercortisolism, and perhaps to reduce the incidence of post-resection worsening of psychiatric symptoms.
Continue to: This case was challenging...
This case was challenging because Mr. A did not initially respond to psychiatric intervention, his psychiatric symptoms worsened after transsphenoidal resection of the pituitary adenoma, and his symptoms were alleviated only after psychiatric medications were re-initiated following surgery. This case highlights the importance of considering an underlying medically diagnosable and treatable cause of psychiatric illness, and illustrates the complex ongoing management that may be necessary to help a patient with this condition achieve their baseline. Further, Mr. A’s case shows that the absence of response to standard psychiatric therapies should warrant earlier laboratory and/or imaging evaluation prior to or in conjunction with psychiatric referral. Additionally, testing for cortisol levels is not typically done for a patient with treatment-resistant anxiety, and this case highlights the importance of considering hypercortisolism in such circumstances.
Bottom Line
Consider testing cortisol levels in patients with treatment-resistant anxiety and insomnia, because cortisol plays a role in Cushing’s disease and anxiety. The severity of psychiatric manifestations of Cushing’s disease may correlate with cortisol levels. Treatment should focus on symptomatic management and underlying etiology.
Related Resources
- Roberts LW, Hales RE, Yudofsky SC, ed. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019.
- Rotham J. Cushing’s syndrome: a tale of frequent misdiagnosis. National Center for Health Research. 2020. www.center4research.org/cushings-syndrome-frequent-misdiagnosis/
- Middleman D. Psychiatric issues of Cushing’s patients: coping with Cushing’s. Cushing’s Support and Research Foundation. www.csrf.net/coping-with-cushings/psychiatric-issues-of-cushings-patients/
Drug Brand Names
Alprazolam • Xanax
Bupropion • Wellbutrin
Dexamethasone • Decadron
Diazepam • Valium
Eszopiclone • Lunesta
Paroxetine • Paxil
Quetiapine • Seroquel
Zolpidem tartrate • Ambien CR
1. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
2. Sadock BJ, Sadock VA, Ruiz P, et al. Neural sciences. In: Sadock BJ, Sadock VA, Ruiz P, et al. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Wolters Kluwer; 2015.
3. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry. 1992;14(4):248-257.
4. Fehm HL, Voigt KH. Pathophysiology of Cushing’s disease. Pathobiol Annu. 1979;9:225-255.
5. Fujii Y, Mizoguchi Y, Masuoka J, et al. Cushing’s syndrome and psychosis: a case report and literature review. Prim Care Companion CNS Disord. 2018;20(5):18.
6. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing’s syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2011;4(2):739-769.
7. Santos A, Resimini E, Pascual JC, et al. Psychiatric symptoms in patients with Cushing’s syndrome: prevalence diagnosis, and management. Drugs. 2017;77(8):829-842.
8. Arnaldi G, Angeli A, Atkinson B, et al. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593-5602.
9. Sonino N, Fava GA. Psychosomatic aspects of Cushing’s disease. Psychother Psychosom. 1998;67(3):140-146.
10. Loosen PT, Chambliss B, DeBold CR, et al. Psychiatric phenomenology in Cushing’s disease. Pharmacopsychiatry. 1992;25(4):192-198.
11. Kelly WF, Kelly MJ, Faragher B. A prospective study of psychiatric and psychological aspects of Cushing’s syndrome. Clin Endocrinol. 1996;45(6):715-720.
12. Katho RG, Delahunt JW, Hannah L. Transition from bipolar affective disorder to intermittent Cushing’s syndrome: case report. J Clin Psychiatry. 1985;46(5):194-196.
13. Hirsh D, Orr G, Kantarovich V, et al. Cushing’s syndrome presenting as a schizophrenia-like psychotic state. Isr J Psychiatry Relat Sci. 2000;37(1):46-50.
14. Dorn LD, Burgess ES, Friedman TC, et al. The longitudinal course of psychopathology in Cushing’s syndrome after correction of hypercortisolism. J Clin Endocrinol Metab. 1997;82(3):912-919.
15. Starkman MN, Schteingart DE, Schork MA. Cushing’s syndrome after treatment: changes in cortisol and ACTH levels, and amelioration of the depressive syndrome. Psychiatry Res. 1986;19(3):177-178.
CASE Anxious and can’t sleep
Mr. A, age 41, presents to his primary care physician (PCP) with anxiety and insomnia. He describes having generalized anxiety with initial and middle insomnia, and says he is sleeping an average of 2 hours per night. He denies any other psychiatric symptoms. Mr. A has no significant psychiatric or medical history.
Mr. A is initiated on zolpidem tartrate, 12.5 mg every night at bedtime, and paroxetine, 20 mg every night at bedtime, for anxiety and insomnia, but these medications result in little to no improvement.
During a 4-month period, he is treated with trials of alprazolam, 0.5 mg every 8 hours as needed; diazepam 5 mg twice a day as needed; diphenhydramine, 50 mg at bedtime; and eszopiclone, 3 mg at bedtime. Despite these treatments, he experiences increased anxiety and insomnia, and develops depressive symptoms, including depressed mood, poor concentration, general malaise, extreme fatigue, a 15-pound unintentional weight loss, erectile dysfunction, and decreased libido. Mr. A denies having suicidal or homicidal ideations. Additionally, he typically goes to the gym approximately 3 times per week, and has noticed that the amount of weight he is able to lift has decreased, which is distressing. Previously, he had been able to lift 300 pounds, but now he can only lift 200 pounds.
[polldaddy:10891920]
The authors’ observations
Insomnia, anxiety, and depression are common chief complaints in medical settings. However, some psychiatric presentations may have an underlying medical etiology.
DSM-5 requires that medical conditions be ruled out in order for a patient to meet criteria for a psychiatric diagnosis.1 Medical differential diagnoses for patients with psychiatric symptoms can include autoimmune, drug/toxin, metabolic, infectious, neoplastic, neurologic, and nutritional etiologies (Table 12). To rule out the possibility of an underlying medical etiology, general screening guidelines include complete blood count, complete metabolic panel, urinalysis, and urine drug screen with alcohol. Human immunodeficiency virus testing and thyroid hormone testing are also commonly ordered.3 Further laboratory testing and imaging is typically not warranted in the absence of historical or physical findings because they are not advocated as cost-effective, so health care professionals must use their clinical judgment to determine appropriate further evaluation. The onset of anxiety most commonly occurs in late adolescence early and adulthood, but Mr. A experienced his first symptoms of anxiety at age 41.2 Mr. A’s age, lack of psychiatric or family history of mental illness, acute onset of symptoms, and failure of symptoms to abate with standard psychiatric treatments warrant a more extensive workup.
EVALUATION Imaging reveals an important finding
Because Mr. A’s symptoms do not improve with standard psychiatric treatments, his PCP orders standard laboratory bloodwork to investigate a possible medical etiology; however, his results are all within normal range.
After the PCP’s niece is coincidentally diagnosed with a pituitary macroadenoma, the PCP orders brain imaging for Mr. A. Results of an MRI show that Mr. A has a 1.6-cm macroadenoma of the pituitary. He is referred to an endocrinologist, who orders additional laboratory tests that show an elevated 24-hour free urine cortisol level of 73 μg/24 h (normal range: 3.5 to 45 μg/24 h), suggesting that Mr. A’s anxiety may be due to Cushing’s disease or that his anxiety caused falsely elevated urinary cortisol levels. Four weeks later, bloodwork is repeated and shows an abnormal dexamethasone suppression test, and 2 more elevated 24-hour free urine cortisol levels of 76 μg/24 h and 150 μg/24 h. A repeat MRI shows a 1.8-cm, mostly cystic sellar mass, indicating the need for surgical intervention. Although the tumor is large and shows optic nerve compression, Mr. A does not complain of headaches or changes in vision.
Continue to: Two months later...
Two months later, Mr. A undergoes a transsphenoidal tumor resection of the pituitary adenoma, and biopsy results confirm an adrenocorticotropic hormone (ACTH)-secreting pituitary macroadenoma, which is consistent with Cushing’s disease. Following surgery, steroid treatment with dexamethasone is discontinued due to a persistently elevated
[polldaddy:10891923]
The authors’ observations
Chronic excess glucocorticoid production is the underlying pathophysiology of Cushing’s disease, which is most commonly caused by an ACTH-producing adenoma.4,5 When these hormones become dysregulated, the result can be over- or underproduction of cortisol, which can lead to physical and psychiatric manifestations.6
Cushing’s disease most commonly manifests with the physical symptoms of centripetal fat deposition, abdominal striae, facial plethora, muscle atrophy, bone density loss, immunosuppression, and cardiovascular complications.5
Hypercortisolism can precipitate anxiety (12% to 79%), mood disorders (50% to 70%), and (less commonly) psychotic disorders; however, in a clinical setting, if a patient presented with one of these as a chief complaint, they would likely first be treated psychiatrically rather than worked up medically for a rare medical condition.5,7-13
Mr. A’s initial bloodwork was unremarkable, but cortisol levels were not obtained at that time because testing for cortisol levels to rule out an underlying medical condition is not routine in patients with depression and anxiety. In Mr. A’s case, a neuroendocrine workup was only ordered once his PCP’s niece coincidentally was diagnosed with a pituitary adenoma.
Continue to: For Mr. A...
For Mr. A, Cushing’s disease presented as a psychiatric disorder with anxiety and insomnia that were resistant to numerous psychiatric medications during an 8-month period. If Mr. A’s PCP had not ordered a brain MRI, he may have continued to receive ineffective psychiatric treatment for some time. Many of Mr. A’s physical symptoms were consistent with Cushing’s disease and mental illness, including erectile dysfunction, fatigue, and muscle weakness; however, his 15-pound weight loss pointed more toward psychiatric illness and further disguised his underlying medical diagnosis, because sudden weight gain is commonly seen in Cushing’s disease (Table 24,5,7,9).
TREATMENT Persistent psychiatric symptoms, then finally relief
Four weeks after surgery, Mr. A’s psychiatric symptoms gradually intensify, which prompts him to see a psychiatrist. A mental status examination (MSE) shows that he is well-nourished, with normal activity, appropriate behavior, and coherent thought process, but depressed mood and flat affect. He denies suicidal or homicidal ideation. He reports that despite being advised to have realistic expectations, he had high hopes that the surgery would lead to remission of all his symptoms, and expresses disappointment that he does not feel “back to normal.”
Six days later, Mr. A’s wife takes him to the hospital. His MSE shows that he has a tense appearance, fidgety activity, depressed and anxious mood, restricted affect, circumstantial thought process, and paranoid delusions that his wife was plotting against him. He says he still is experiencing insomnia. He also discloses having suicidal ideations with a plan and intent to overdose on medication, as well as homicidal ideations about killing his wife and children. Mr. A provides reasons for why he would want to hurt his family, and does not appear to be bothered by these thoughts.
Mr. A is admitted to the inpatient psychiatric unit and is prescribed quetiapine, 100 mg every night at bedtime. During the next 2 days, quetiapine is titrated to 300 mg every night at bedtime. On hospital Day 3, Mr. A says he is feeling worse than the previous days. He is still having vague suicidal thoughts and feels agitated, guilty, and depressed. To treat these persistent symptoms, quetiapine is further increased to 400 mg every night at bedtime, and he is initiated on bupropion XL, 150 mg, to treat persistent symptoms.
After 1 week of hospitalization, the treatment team meets with Mr. A and his wife, who has been supportive throughout her husband’s hospitalization. During the meeting, they both agree that Mr. A has experienced some improvement because he is no longer having suicidal or homicidal thoughts, but he is still feeling depressed and frustrated by his continued insomnia. Following the meeting, Mr. A’s quetiapine is further increased to 450 mg every night at bedtime to address continued insomnia, and bupropion XL is increased to 300 mg/d to address continued depressive symptoms. During the next few days, his affective symptoms improve; however, his initial insomnia continues, and quetiapine is further increased to 500 mg every night at bedtime.
Continue to: On hospital Day 20...
On hospital Day 20, Mr. A is discharged back to his outpatient psychiatrist and receives quetiapine, 500 mg every night at bedtime, and bupropion XL, 300 mg/d. Although Mr. A’s depression and anxiety continue to be well controlled, his insomnia persists. Sleep hygiene is addressed, and alprazolam, 0.5 mg every night at bedtime, is added to his regimen, which proves to be effective.
OUTCOME A slow remission
After a year of treatment, Mr. A is slowly tapered off of all medications. Two years later, he is in complete remission of all psychiatric symptoms and no longer requires any psychotropic medications.
The authors’ observations
Treatment for hypercortisolism in patients with psychiatric symptoms triggered by glucocorticoid imbalance has typically resulted in a decrease in the severity of their psychiatric symptoms.9,11 A prospective longitudinal study examining 33 patients found that correction of hypercortisolism in patients with Cushing’s syndrome often led to resolution of their psychiatric symptoms, with 87.9% of patients back to baseline within 1 year.14 However, to our knowledge, few reports have described the management of patients whose symptoms are resistant to treatment of hypercortisolism.
In our case, after transsphenoidal resection of an adenoma, Mr. A became suicidal and paranoid, and his anxiety and insomnia also persisted. A possible explanation for the worsening of Mr. A’s symptoms after surgery could be the slow recovery of the hypothalamic-pituitary-adrenal (HPA) axis and therefore a temporary deficiency in glucocorticoid, which caused an increase in catecholamines, leading to an increase in stress.14 This concept of a “slow recovery” is supported by the fact that Mr. A was successfully weaned off all medication after 1 year of treatment, and achieved complete remission of psychiatric symptoms for >2 years. Furthermore, the severity of Mr. A’s symptoms appeared to correlate with his 24-hour urine cortisol and
Future research should evaluate the utility of screening all patients with treatment-resistant anxiety and/or insomnia for hypercortisolism. Even without other clues to endocrinopathies, serum cortisol levels can be used as a screening tool for diagnosing underlying medical causes in patients with anxiety and depression.2 A greater understanding of the relationship between medical and psychiatric manifestations will allow clinicians to better care for patients. Further research is needed to elucidate the quantitative relationship between cortisol levels and anxiety to evaluate severity, guide treatment planning, and follow treatment response for patients with anxiety. It may be useful to determine the threshold between elevated cortisol levels due to anxiety vs elevated cortisol due to an underlying medical pathology such as Cushing’s disease. Additionally, little research has been conducted to compare how psychiatric symptoms respond to pituitary macroadenoma resection alone, pharmaceutical intervention alone, or a combination of these approaches. It would be beneficial to evaluate these treatment strategies to elucidate the most effective method to reduce psychiatric symptoms in patients with hypercortisolism, and perhaps to reduce the incidence of post-resection worsening of psychiatric symptoms.
Continue to: This case was challenging...
This case was challenging because Mr. A did not initially respond to psychiatric intervention, his psychiatric symptoms worsened after transsphenoidal resection of the pituitary adenoma, and his symptoms were alleviated only after psychiatric medications were re-initiated following surgery. This case highlights the importance of considering an underlying medically diagnosable and treatable cause of psychiatric illness, and illustrates the complex ongoing management that may be necessary to help a patient with this condition achieve their baseline. Further, Mr. A’s case shows that the absence of response to standard psychiatric therapies should warrant earlier laboratory and/or imaging evaluation prior to or in conjunction with psychiatric referral. Additionally, testing for cortisol levels is not typically done for a patient with treatment-resistant anxiety, and this case highlights the importance of considering hypercortisolism in such circumstances.
Bottom Line
Consider testing cortisol levels in patients with treatment-resistant anxiety and insomnia, because cortisol plays a role in Cushing’s disease and anxiety. The severity of psychiatric manifestations of Cushing’s disease may correlate with cortisol levels. Treatment should focus on symptomatic management and underlying etiology.
Related Resources
- Roberts LW, Hales RE, Yudofsky SC, ed. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019.
- Rotham J. Cushing’s syndrome: a tale of frequent misdiagnosis. National Center for Health Research. 2020. www.center4research.org/cushings-syndrome-frequent-misdiagnosis/
- Middleman D. Psychiatric issues of Cushing’s patients: coping with Cushing’s. Cushing’s Support and Research Foundation. www.csrf.net/coping-with-cushings/psychiatric-issues-of-cushings-patients/
Drug Brand Names
Alprazolam • Xanax
Bupropion • Wellbutrin
Dexamethasone • Decadron
Diazepam • Valium
Eszopiclone • Lunesta
Paroxetine • Paxil
Quetiapine • Seroquel
Zolpidem tartrate • Ambien CR
CASE Anxious and can’t sleep
Mr. A, age 41, presents to his primary care physician (PCP) with anxiety and insomnia. He describes having generalized anxiety with initial and middle insomnia, and says he is sleeping an average of 2 hours per night. He denies any other psychiatric symptoms. Mr. A has no significant psychiatric or medical history.
Mr. A is initiated on zolpidem tartrate, 12.5 mg every night at bedtime, and paroxetine, 20 mg every night at bedtime, for anxiety and insomnia, but these medications result in little to no improvement.
During a 4-month period, he is treated with trials of alprazolam, 0.5 mg every 8 hours as needed; diazepam 5 mg twice a day as needed; diphenhydramine, 50 mg at bedtime; and eszopiclone, 3 mg at bedtime. Despite these treatments, he experiences increased anxiety and insomnia, and develops depressive symptoms, including depressed mood, poor concentration, general malaise, extreme fatigue, a 15-pound unintentional weight loss, erectile dysfunction, and decreased libido. Mr. A denies having suicidal or homicidal ideations. Additionally, he typically goes to the gym approximately 3 times per week, and has noticed that the amount of weight he is able to lift has decreased, which is distressing. Previously, he had been able to lift 300 pounds, but now he can only lift 200 pounds.
[polldaddy:10891920]
The authors’ observations
Insomnia, anxiety, and depression are common chief complaints in medical settings. However, some psychiatric presentations may have an underlying medical etiology.
DSM-5 requires that medical conditions be ruled out in order for a patient to meet criteria for a psychiatric diagnosis.1 Medical differential diagnoses for patients with psychiatric symptoms can include autoimmune, drug/toxin, metabolic, infectious, neoplastic, neurologic, and nutritional etiologies (Table 12). To rule out the possibility of an underlying medical etiology, general screening guidelines include complete blood count, complete metabolic panel, urinalysis, and urine drug screen with alcohol. Human immunodeficiency virus testing and thyroid hormone testing are also commonly ordered.3 Further laboratory testing and imaging is typically not warranted in the absence of historical or physical findings because they are not advocated as cost-effective, so health care professionals must use their clinical judgment to determine appropriate further evaluation. The onset of anxiety most commonly occurs in late adolescence early and adulthood, but Mr. A experienced his first symptoms of anxiety at age 41.2 Mr. A’s age, lack of psychiatric or family history of mental illness, acute onset of symptoms, and failure of symptoms to abate with standard psychiatric treatments warrant a more extensive workup.
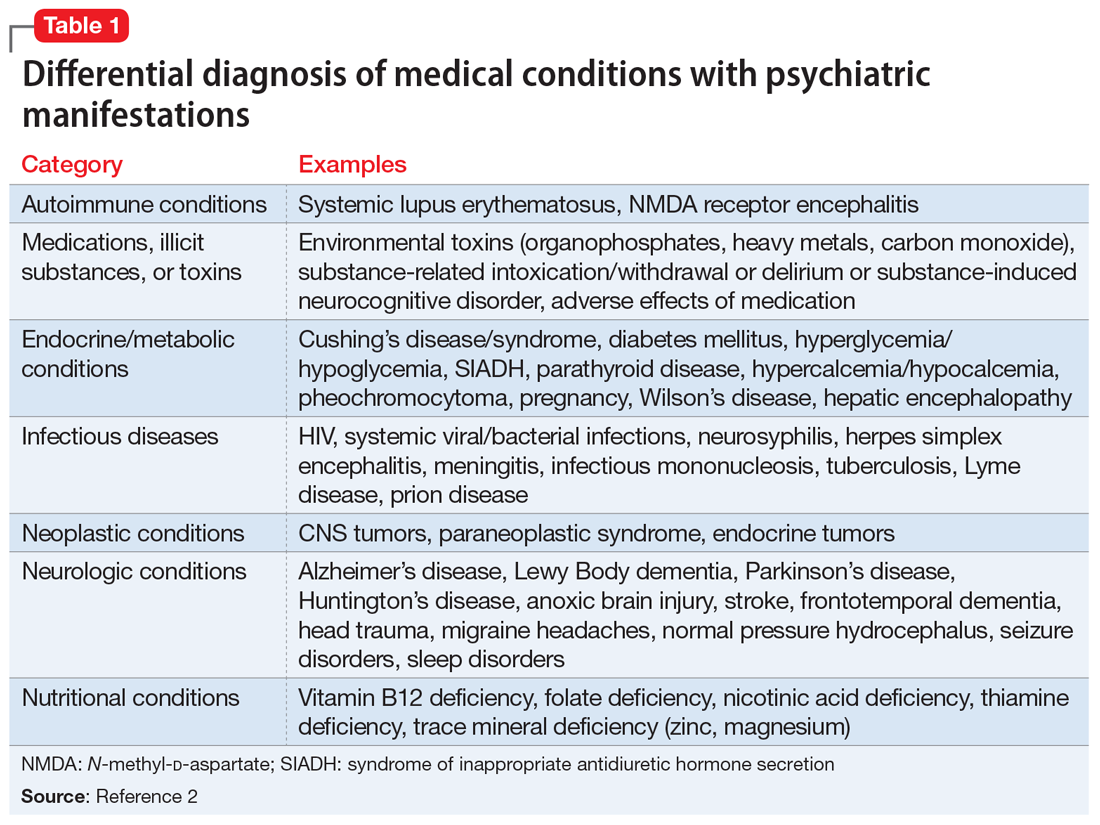
EVALUATION Imaging reveals an important finding
Because Mr. A’s symptoms do not improve with standard psychiatric treatments, his PCP orders standard laboratory bloodwork to investigate a possible medical etiology; however, his results are all within normal range.
After the PCP’s niece is coincidentally diagnosed with a pituitary macroadenoma, the PCP orders brain imaging for Mr. A. Results of an MRI show that Mr. A has a 1.6-cm macroadenoma of the pituitary. He is referred to an endocrinologist, who orders additional laboratory tests that show an elevated 24-hour free urine cortisol level of 73 μg/24 h (normal range: 3.5 to 45 μg/24 h), suggesting that Mr. A’s anxiety may be due to Cushing’s disease or that his anxiety caused falsely elevated urinary cortisol levels. Four weeks later, bloodwork is repeated and shows an abnormal dexamethasone suppression test, and 2 more elevated 24-hour free urine cortisol levels of 76 μg/24 h and 150 μg/24 h. A repeat MRI shows a 1.8-cm, mostly cystic sellar mass, indicating the need for surgical intervention. Although the tumor is large and shows optic nerve compression, Mr. A does not complain of headaches or changes in vision.
Continue to: Two months later...
Two months later, Mr. A undergoes a transsphenoidal tumor resection of the pituitary adenoma, and biopsy results confirm an adrenocorticotropic hormone (ACTH)-secreting pituitary macroadenoma, which is consistent with Cushing’s disease. Following surgery, steroid treatment with dexamethasone is discontinued due to a persistently elevated
[polldaddy:10891923]
The authors’ observations
Chronic excess glucocorticoid production is the underlying pathophysiology of Cushing’s disease, which is most commonly caused by an ACTH-producing adenoma.4,5 When these hormones become dysregulated, the result can be over- or underproduction of cortisol, which can lead to physical and psychiatric manifestations.6
Cushing’s disease most commonly manifests with the physical symptoms of centripetal fat deposition, abdominal striae, facial plethora, muscle atrophy, bone density loss, immunosuppression, and cardiovascular complications.5
Hypercortisolism can precipitate anxiety (12% to 79%), mood disorders (50% to 70%), and (less commonly) psychotic disorders; however, in a clinical setting, if a patient presented with one of these as a chief complaint, they would likely first be treated psychiatrically rather than worked up medically for a rare medical condition.5,7-13
Mr. A’s initial bloodwork was unremarkable, but cortisol levels were not obtained at that time because testing for cortisol levels to rule out an underlying medical condition is not routine in patients with depression and anxiety. In Mr. A’s case, a neuroendocrine workup was only ordered once his PCP’s niece coincidentally was diagnosed with a pituitary adenoma.
Continue to: For Mr. A...
For Mr. A, Cushing’s disease presented as a psychiatric disorder with anxiety and insomnia that were resistant to numerous psychiatric medications during an 8-month period. If Mr. A’s PCP had not ordered a brain MRI, he may have continued to receive ineffective psychiatric treatment for some time. Many of Mr. A’s physical symptoms were consistent with Cushing’s disease and mental illness, including erectile dysfunction, fatigue, and muscle weakness; however, his 15-pound weight loss pointed more toward psychiatric illness and further disguised his underlying medical diagnosis, because sudden weight gain is commonly seen in Cushing’s disease (Table 24,5,7,9).
TREATMENT Persistent psychiatric symptoms, then finally relief
Four weeks after surgery, Mr. A’s psychiatric symptoms gradually intensify, which prompts him to see a psychiatrist. A mental status examination (MSE) shows that he is well-nourished, with normal activity, appropriate behavior, and coherent thought process, but depressed mood and flat affect. He denies suicidal or homicidal ideation. He reports that despite being advised to have realistic expectations, he had high hopes that the surgery would lead to remission of all his symptoms, and expresses disappointment that he does not feel “back to normal.”
Six days later, Mr. A’s wife takes him to the hospital. His MSE shows that he has a tense appearance, fidgety activity, depressed and anxious mood, restricted affect, circumstantial thought process, and paranoid delusions that his wife was plotting against him. He says he still is experiencing insomnia. He also discloses having suicidal ideations with a plan and intent to overdose on medication, as well as homicidal ideations about killing his wife and children. Mr. A provides reasons for why he would want to hurt his family, and does not appear to be bothered by these thoughts.
Mr. A is admitted to the inpatient psychiatric unit and is prescribed quetiapine, 100 mg every night at bedtime. During the next 2 days, quetiapine is titrated to 300 mg every night at bedtime. On hospital Day 3, Mr. A says he is feeling worse than the previous days. He is still having vague suicidal thoughts and feels agitated, guilty, and depressed. To treat these persistent symptoms, quetiapine is further increased to 400 mg every night at bedtime, and he is initiated on bupropion XL, 150 mg, to treat persistent symptoms.
After 1 week of hospitalization, the treatment team meets with Mr. A and his wife, who has been supportive throughout her husband’s hospitalization. During the meeting, they both agree that Mr. A has experienced some improvement because he is no longer having suicidal or homicidal thoughts, but he is still feeling depressed and frustrated by his continued insomnia. Following the meeting, Mr. A’s quetiapine is further increased to 450 mg every night at bedtime to address continued insomnia, and bupropion XL is increased to 300 mg/d to address continued depressive symptoms. During the next few days, his affective symptoms improve; however, his initial insomnia continues, and quetiapine is further increased to 500 mg every night at bedtime.
Continue to: On hospital Day 20...
On hospital Day 20, Mr. A is discharged back to his outpatient psychiatrist and receives quetiapine, 500 mg every night at bedtime, and bupropion XL, 300 mg/d. Although Mr. A’s depression and anxiety continue to be well controlled, his insomnia persists. Sleep hygiene is addressed, and alprazolam, 0.5 mg every night at bedtime, is added to his regimen, which proves to be effective.
OUTCOME A slow remission
After a year of treatment, Mr. A is slowly tapered off of all medications. Two years later, he is in complete remission of all psychiatric symptoms and no longer requires any psychotropic medications.
The authors’ observations
Treatment for hypercortisolism in patients with psychiatric symptoms triggered by glucocorticoid imbalance has typically resulted in a decrease in the severity of their psychiatric symptoms.9,11 A prospective longitudinal study examining 33 patients found that correction of hypercortisolism in patients with Cushing’s syndrome often led to resolution of their psychiatric symptoms, with 87.9% of patients back to baseline within 1 year.14 However, to our knowledge, few reports have described the management of patients whose symptoms are resistant to treatment of hypercortisolism.
In our case, after transsphenoidal resection of an adenoma, Mr. A became suicidal and paranoid, and his anxiety and insomnia also persisted. A possible explanation for the worsening of Mr. A’s symptoms after surgery could be the slow recovery of the hypothalamic-pituitary-adrenal (HPA) axis and therefore a temporary deficiency in glucocorticoid, which caused an increase in catecholamines, leading to an increase in stress.14 This concept of a “slow recovery” is supported by the fact that Mr. A was successfully weaned off all medication after 1 year of treatment, and achieved complete remission of psychiatric symptoms for >2 years. Furthermore, the severity of Mr. A’s symptoms appeared to correlate with his 24-hour urine cortisol and
Future research should evaluate the utility of screening all patients with treatment-resistant anxiety and/or insomnia for hypercortisolism. Even without other clues to endocrinopathies, serum cortisol levels can be used as a screening tool for diagnosing underlying medical causes in patients with anxiety and depression.2 A greater understanding of the relationship between medical and psychiatric manifestations will allow clinicians to better care for patients. Further research is needed to elucidate the quantitative relationship between cortisol levels and anxiety to evaluate severity, guide treatment planning, and follow treatment response for patients with anxiety. It may be useful to determine the threshold between elevated cortisol levels due to anxiety vs elevated cortisol due to an underlying medical pathology such as Cushing’s disease. Additionally, little research has been conducted to compare how psychiatric symptoms respond to pituitary macroadenoma resection alone, pharmaceutical intervention alone, or a combination of these approaches. It would be beneficial to evaluate these treatment strategies to elucidate the most effective method to reduce psychiatric symptoms in patients with hypercortisolism, and perhaps to reduce the incidence of post-resection worsening of psychiatric symptoms.
Continue to: This case was challenging...
This case was challenging because Mr. A did not initially respond to psychiatric intervention, his psychiatric symptoms worsened after transsphenoidal resection of the pituitary adenoma, and his symptoms were alleviated only after psychiatric medications were re-initiated following surgery. This case highlights the importance of considering an underlying medically diagnosable and treatable cause of psychiatric illness, and illustrates the complex ongoing management that may be necessary to help a patient with this condition achieve their baseline. Further, Mr. A’s case shows that the absence of response to standard psychiatric therapies should warrant earlier laboratory and/or imaging evaluation prior to or in conjunction with psychiatric referral. Additionally, testing for cortisol levels is not typically done for a patient with treatment-resistant anxiety, and this case highlights the importance of considering hypercortisolism in such circumstances.
Bottom Line
Consider testing cortisol levels in patients with treatment-resistant anxiety and insomnia, because cortisol plays a role in Cushing’s disease and anxiety. The severity of psychiatric manifestations of Cushing’s disease may correlate with cortisol levels. Treatment should focus on symptomatic management and underlying etiology.
Related Resources
- Roberts LW, Hales RE, Yudofsky SC, ed. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019.
- Rotham J. Cushing’s syndrome: a tale of frequent misdiagnosis. National Center for Health Research. 2020. www.center4research.org/cushings-syndrome-frequent-misdiagnosis/
- Middleman D. Psychiatric issues of Cushing’s patients: coping with Cushing’s. Cushing’s Support and Research Foundation. www.csrf.net/coping-with-cushings/psychiatric-issues-of-cushings-patients/
Drug Brand Names
Alprazolam • Xanax
Bupropion • Wellbutrin
Dexamethasone • Decadron
Diazepam • Valium
Eszopiclone • Lunesta
Paroxetine • Paxil
Quetiapine • Seroquel
Zolpidem tartrate • Ambien CR
1. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
2. Sadock BJ, Sadock VA, Ruiz P, et al. Neural sciences. In: Sadock BJ, Sadock VA, Ruiz P, et al. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Wolters Kluwer; 2015.
3. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry. 1992;14(4):248-257.
4. Fehm HL, Voigt KH. Pathophysiology of Cushing’s disease. Pathobiol Annu. 1979;9:225-255.
5. Fujii Y, Mizoguchi Y, Masuoka J, et al. Cushing’s syndrome and psychosis: a case report and literature review. Prim Care Companion CNS Disord. 2018;20(5):18.
6. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing’s syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2011;4(2):739-769.
7. Santos A, Resimini E, Pascual JC, et al. Psychiatric symptoms in patients with Cushing’s syndrome: prevalence diagnosis, and management. Drugs. 2017;77(8):829-842.
8. Arnaldi G, Angeli A, Atkinson B, et al. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593-5602.
9. Sonino N, Fava GA. Psychosomatic aspects of Cushing’s disease. Psychother Psychosom. 1998;67(3):140-146.
10. Loosen PT, Chambliss B, DeBold CR, et al. Psychiatric phenomenology in Cushing’s disease. Pharmacopsychiatry. 1992;25(4):192-198.
11. Kelly WF, Kelly MJ, Faragher B. A prospective study of psychiatric and psychological aspects of Cushing’s syndrome. Clin Endocrinol. 1996;45(6):715-720.
12. Katho RG, Delahunt JW, Hannah L. Transition from bipolar affective disorder to intermittent Cushing’s syndrome: case report. J Clin Psychiatry. 1985;46(5):194-196.
13. Hirsh D, Orr G, Kantarovich V, et al. Cushing’s syndrome presenting as a schizophrenia-like psychotic state. Isr J Psychiatry Relat Sci. 2000;37(1):46-50.
14. Dorn LD, Burgess ES, Friedman TC, et al. The longitudinal course of psychopathology in Cushing’s syndrome after correction of hypercortisolism. J Clin Endocrinol Metab. 1997;82(3):912-919.
15. Starkman MN, Schteingart DE, Schork MA. Cushing’s syndrome after treatment: changes in cortisol and ACTH levels, and amelioration of the depressive syndrome. Psychiatry Res. 1986;19(3):177-178.
1. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
2. Sadock BJ, Sadock VA, Ruiz P, et al. Neural sciences. In: Sadock BJ, Sadock VA, Ruiz P, et al. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Wolters Kluwer; 2015.
3. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry. 1992;14(4):248-257.
4. Fehm HL, Voigt KH. Pathophysiology of Cushing’s disease. Pathobiol Annu. 1979;9:225-255.
5. Fujii Y, Mizoguchi Y, Masuoka J, et al. Cushing’s syndrome and psychosis: a case report and literature review. Prim Care Companion CNS Disord. 2018;20(5):18.
6. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing’s syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2011;4(2):739-769.
7. Santos A, Resimini E, Pascual JC, et al. Psychiatric symptoms in patients with Cushing’s syndrome: prevalence diagnosis, and management. Drugs. 2017;77(8):829-842.
8. Arnaldi G, Angeli A, Atkinson B, et al. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593-5602.
9. Sonino N, Fava GA. Psychosomatic aspects of Cushing’s disease. Psychother Psychosom. 1998;67(3):140-146.
10. Loosen PT, Chambliss B, DeBold CR, et al. Psychiatric phenomenology in Cushing’s disease. Pharmacopsychiatry. 1992;25(4):192-198.
11. Kelly WF, Kelly MJ, Faragher B. A prospective study of psychiatric and psychological aspects of Cushing’s syndrome. Clin Endocrinol. 1996;45(6):715-720.
12. Katho RG, Delahunt JW, Hannah L. Transition from bipolar affective disorder to intermittent Cushing’s syndrome: case report. J Clin Psychiatry. 1985;46(5):194-196.
13. Hirsh D, Orr G, Kantarovich V, et al. Cushing’s syndrome presenting as a schizophrenia-like psychotic state. Isr J Psychiatry Relat Sci. 2000;37(1):46-50.
14. Dorn LD, Burgess ES, Friedman TC, et al. The longitudinal course of psychopathology in Cushing’s syndrome after correction of hypercortisolism. J Clin Endocrinol Metab. 1997;82(3):912-919.
15. Starkman MN, Schteingart DE, Schork MA. Cushing’s syndrome after treatment: changes in cortisol and ACTH levels, and amelioration of the depressive syndrome. Psychiatry Res. 1986;19(3):177-178.
Short sleep is linked to future dementia
, according to a new analysis of data from the Whitehall II cohort study.
Previous work had identified links between short sleep duration and dementia risk, but few studies examined sleep habits long before onset of dementia. Those that did produced inconsistent results, according to Séverine Sabia, PhD, who is a research associate at Inserm (France) and the University College London.
“One potential reason for these inconstancies is the large range of ages of the study populations, and the small number of participants within each sleep duration group. The novelty of our study is to examine this association among almost 8,000 participants with a follow-up of 30 years, using repeated measures of sleep duration starting in midlife to consider sleep duration at specific ages,” Dr. Sabia said in an interview. She presented the research at the 2021 Alzheimer’s Association International Conference.
Those previous studies found a U-shaped association between sleep duration and dementia risk, with lowest risk associated with 7-8 hours of sleep, but greater risk for shorter and longer durations. However, because the studies had follow-up periods shorter than 10 years, they are at greater risk of reverse causation bias. Longer follow-up studies tended to have small sample sizes or to focus on older adults.
The longer follow-up in the current study makes for a more compelling case, said Claire Sexton, DPhil, director of Scientific Programs & Outreach for the Alzheimer’s Association. Observations of short or long sleep closer to the onset of symptoms could just be a warning sign of dementia. “But looking at age 50, age 60 ... if you’re seeing those relationships, then it’s less likely that it is just purely prodromal,” said Dr. Sexton. But it still doesn’t necessarily confirm causation. “It could also be a risk factor,” Dr. Sexton added.
Multifactorial risk
Dr. Sabia also noted that the magnitude of risk was similar to that seen with smoking or obesity, and many factors play a role in dementia risk. “Even if the risk of dementia was 30% higher in those with persistent short sleep duration, in absolute terms, the percentage of those with persistent short duration who developed dementia was 8%, and 6% in those with persistent sleep duration of 7 hours. Dementia is a multifactorial disease, which means that several factors are likely to influence its onset. Sleep duration is one of them, but if a person has poor sleep and does not manage to increase it, there are other important prevention measures. It is important to keep a healthy lifestyle and cardiometabolic measures in the normal range. All together it is likely to be beneficial for brain health in later life,” she said.
Dr. Sexton agreed. “With sleep we’re still trying to tease apart what aspect of sleep is important. Is it the sleep duration? Is it the quality of sleep? Is it certain sleep stages?” she said.
Regardless of sleep’s potential influence on dementia risk, both Dr. Sexton and Dr. Sabia noted the importance of sleep for general health. “These types of problems are very prevalent, so it’s good for people to be aware of them. And then if they notice any problems with their sleep, or any changes, to go and see their health care provider, and to be discussing them, and then to be investigating the cause, and to see whether changes in sleep hygiene and treatments for insomnia could address these sleep problems,” said Dr. Sexton.
Decades of data
During the Whitehall II study, researchers assessed average sleep duration (“How many hours of sleep do you have on an average weeknight?”) six times over 30 years of follow-up. Dr. Sabia’s group extracted self-reported sleep duration data at ages 50, 60, and 70. Short sleep duration was defined as fewer than 5 hours, or 6 hours. Normal sleep duration was defined as 7 hours. Long duration was defined as 8 hours or more.
A questioner during the Q&A period noted that this grouping is a little unusual. Many studies define 7-8 hours as normal. Dr. Sabia answered that they were unable to examine periods of 9 hours or more due to the nature of the data, and the lowest associated risk was found at 7 hours.
The researchers analyzed data from 7,959 participants (33.0% women). At age 50, compared with 7 hours of sleep, 6 or few hours of sleep was associated with a higher risk of dementia over the ensuing 25 years of follow-up (hazard ratio [HR], 1.22; 95% confidence interval [CI], 1.01-1.48). The same was true at age 60 (15 years of follow-up HR, 1.37; 95% CI, 1.10-1.72). There was a trend at age 70 (8 years follow-up; HR, 1.24; 95% CI, 0.98-1.57). For 8 or more hours of sleep, there were trends toward increased risk at age 50 (HR, 1.25; 95% CI, 0.98-1.60). Long sleep at age 60 and 70 was associated with heightened risk, but the confidence intervals were well outside statistical significance.
Twenty percent of participants had persistent short sleep over the course of follow-up, 37% had persistent normal sleep, and 7% had persistent long sleep. Seven percent of participants experienced a change from normal sleep to short sleep, 16% had a change from short sleep to normal sleep, and 13% had a change from normal sleep to long sleep.
Persistent short sleep between age 50 and 70 was associated with a 30% increased risk of dementia (HR, 1.30; 95% CI, 1.00-1.69). There were no statistically significant associations between dementia risk and any of the changing sleep pattern groups.
Dr. Sabia and Dr. Sexton have no relevant financial disclosures.
, according to a new analysis of data from the Whitehall II cohort study.
Previous work had identified links between short sleep duration and dementia risk, but few studies examined sleep habits long before onset of dementia. Those that did produced inconsistent results, according to Séverine Sabia, PhD, who is a research associate at Inserm (France) and the University College London.
“One potential reason for these inconstancies is the large range of ages of the study populations, and the small number of participants within each sleep duration group. The novelty of our study is to examine this association among almost 8,000 participants with a follow-up of 30 years, using repeated measures of sleep duration starting in midlife to consider sleep duration at specific ages,” Dr. Sabia said in an interview. She presented the research at the 2021 Alzheimer’s Association International Conference.
Those previous studies found a U-shaped association between sleep duration and dementia risk, with lowest risk associated with 7-8 hours of sleep, but greater risk for shorter and longer durations. However, because the studies had follow-up periods shorter than 10 years, they are at greater risk of reverse causation bias. Longer follow-up studies tended to have small sample sizes or to focus on older adults.
The longer follow-up in the current study makes for a more compelling case, said Claire Sexton, DPhil, director of Scientific Programs & Outreach for the Alzheimer’s Association. Observations of short or long sleep closer to the onset of symptoms could just be a warning sign of dementia. “But looking at age 50, age 60 ... if you’re seeing those relationships, then it’s less likely that it is just purely prodromal,” said Dr. Sexton. But it still doesn’t necessarily confirm causation. “It could also be a risk factor,” Dr. Sexton added.
Multifactorial risk
Dr. Sabia also noted that the magnitude of risk was similar to that seen with smoking or obesity, and many factors play a role in dementia risk. “Even if the risk of dementia was 30% higher in those with persistent short sleep duration, in absolute terms, the percentage of those with persistent short duration who developed dementia was 8%, and 6% in those with persistent sleep duration of 7 hours. Dementia is a multifactorial disease, which means that several factors are likely to influence its onset. Sleep duration is one of them, but if a person has poor sleep and does not manage to increase it, there are other important prevention measures. It is important to keep a healthy lifestyle and cardiometabolic measures in the normal range. All together it is likely to be beneficial for brain health in later life,” she said.
Dr. Sexton agreed. “With sleep we’re still trying to tease apart what aspect of sleep is important. Is it the sleep duration? Is it the quality of sleep? Is it certain sleep stages?” she said.
Regardless of sleep’s potential influence on dementia risk, both Dr. Sexton and Dr. Sabia noted the importance of sleep for general health. “These types of problems are very prevalent, so it’s good for people to be aware of them. And then if they notice any problems with their sleep, or any changes, to go and see their health care provider, and to be discussing them, and then to be investigating the cause, and to see whether changes in sleep hygiene and treatments for insomnia could address these sleep problems,” said Dr. Sexton.
Decades of data
During the Whitehall II study, researchers assessed average sleep duration (“How many hours of sleep do you have on an average weeknight?”) six times over 30 years of follow-up. Dr. Sabia’s group extracted self-reported sleep duration data at ages 50, 60, and 70. Short sleep duration was defined as fewer than 5 hours, or 6 hours. Normal sleep duration was defined as 7 hours. Long duration was defined as 8 hours or more.
A questioner during the Q&A period noted that this grouping is a little unusual. Many studies define 7-8 hours as normal. Dr. Sabia answered that they were unable to examine periods of 9 hours or more due to the nature of the data, and the lowest associated risk was found at 7 hours.
The researchers analyzed data from 7,959 participants (33.0% women). At age 50, compared with 7 hours of sleep, 6 or few hours of sleep was associated with a higher risk of dementia over the ensuing 25 years of follow-up (hazard ratio [HR], 1.22; 95% confidence interval [CI], 1.01-1.48). The same was true at age 60 (15 years of follow-up HR, 1.37; 95% CI, 1.10-1.72). There was a trend at age 70 (8 years follow-up; HR, 1.24; 95% CI, 0.98-1.57). For 8 or more hours of sleep, there were trends toward increased risk at age 50 (HR, 1.25; 95% CI, 0.98-1.60). Long sleep at age 60 and 70 was associated with heightened risk, but the confidence intervals were well outside statistical significance.
Twenty percent of participants had persistent short sleep over the course of follow-up, 37% had persistent normal sleep, and 7% had persistent long sleep. Seven percent of participants experienced a change from normal sleep to short sleep, 16% had a change from short sleep to normal sleep, and 13% had a change from normal sleep to long sleep.
Persistent short sleep between age 50 and 70 was associated with a 30% increased risk of dementia (HR, 1.30; 95% CI, 1.00-1.69). There were no statistically significant associations between dementia risk and any of the changing sleep pattern groups.
Dr. Sabia and Dr. Sexton have no relevant financial disclosures.
, according to a new analysis of data from the Whitehall II cohort study.
Previous work had identified links between short sleep duration and dementia risk, but few studies examined sleep habits long before onset of dementia. Those that did produced inconsistent results, according to Séverine Sabia, PhD, who is a research associate at Inserm (France) and the University College London.
“One potential reason for these inconstancies is the large range of ages of the study populations, and the small number of participants within each sleep duration group. The novelty of our study is to examine this association among almost 8,000 participants with a follow-up of 30 years, using repeated measures of sleep duration starting in midlife to consider sleep duration at specific ages,” Dr. Sabia said in an interview. She presented the research at the 2021 Alzheimer’s Association International Conference.
Those previous studies found a U-shaped association between sleep duration and dementia risk, with lowest risk associated with 7-8 hours of sleep, but greater risk for shorter and longer durations. However, because the studies had follow-up periods shorter than 10 years, they are at greater risk of reverse causation bias. Longer follow-up studies tended to have small sample sizes or to focus on older adults.
The longer follow-up in the current study makes for a more compelling case, said Claire Sexton, DPhil, director of Scientific Programs & Outreach for the Alzheimer’s Association. Observations of short or long sleep closer to the onset of symptoms could just be a warning sign of dementia. “But looking at age 50, age 60 ... if you’re seeing those relationships, then it’s less likely that it is just purely prodromal,” said Dr. Sexton. But it still doesn’t necessarily confirm causation. “It could also be a risk factor,” Dr. Sexton added.
Multifactorial risk
Dr. Sabia also noted that the magnitude of risk was similar to that seen with smoking or obesity, and many factors play a role in dementia risk. “Even if the risk of dementia was 30% higher in those with persistent short sleep duration, in absolute terms, the percentage of those with persistent short duration who developed dementia was 8%, and 6% in those with persistent sleep duration of 7 hours. Dementia is a multifactorial disease, which means that several factors are likely to influence its onset. Sleep duration is one of them, but if a person has poor sleep and does not manage to increase it, there are other important prevention measures. It is important to keep a healthy lifestyle and cardiometabolic measures in the normal range. All together it is likely to be beneficial for brain health in later life,” she said.
Dr. Sexton agreed. “With sleep we’re still trying to tease apart what aspect of sleep is important. Is it the sleep duration? Is it the quality of sleep? Is it certain sleep stages?” she said.
Regardless of sleep’s potential influence on dementia risk, both Dr. Sexton and Dr. Sabia noted the importance of sleep for general health. “These types of problems are very prevalent, so it’s good for people to be aware of them. And then if they notice any problems with their sleep, or any changes, to go and see their health care provider, and to be discussing them, and then to be investigating the cause, and to see whether changes in sleep hygiene and treatments for insomnia could address these sleep problems,” said Dr. Sexton.
Decades of data
During the Whitehall II study, researchers assessed average sleep duration (“How many hours of sleep do you have on an average weeknight?”) six times over 30 years of follow-up. Dr. Sabia’s group extracted self-reported sleep duration data at ages 50, 60, and 70. Short sleep duration was defined as fewer than 5 hours, or 6 hours. Normal sleep duration was defined as 7 hours. Long duration was defined as 8 hours or more.
A questioner during the Q&A period noted that this grouping is a little unusual. Many studies define 7-8 hours as normal. Dr. Sabia answered that they were unable to examine periods of 9 hours or more due to the nature of the data, and the lowest associated risk was found at 7 hours.
The researchers analyzed data from 7,959 participants (33.0% women). At age 50, compared with 7 hours of sleep, 6 or few hours of sleep was associated with a higher risk of dementia over the ensuing 25 years of follow-up (hazard ratio [HR], 1.22; 95% confidence interval [CI], 1.01-1.48). The same was true at age 60 (15 years of follow-up HR, 1.37; 95% CI, 1.10-1.72). There was a trend at age 70 (8 years follow-up; HR, 1.24; 95% CI, 0.98-1.57). For 8 or more hours of sleep, there were trends toward increased risk at age 50 (HR, 1.25; 95% CI, 0.98-1.60). Long sleep at age 60 and 70 was associated with heightened risk, but the confidence intervals were well outside statistical significance.
Twenty percent of participants had persistent short sleep over the course of follow-up, 37% had persistent normal sleep, and 7% had persistent long sleep. Seven percent of participants experienced a change from normal sleep to short sleep, 16% had a change from short sleep to normal sleep, and 13% had a change from normal sleep to long sleep.
Persistent short sleep between age 50 and 70 was associated with a 30% increased risk of dementia (HR, 1.30; 95% CI, 1.00-1.69). There were no statistically significant associations between dementia risk and any of the changing sleep pattern groups.
Dr. Sabia and Dr. Sexton have no relevant financial disclosures.
FROM AAIC 2021
Lucid abductions and Candy Crush addiction
I dream of alien abductions
There he goes! It’s lunchtime and your colleague Tom is going on and on again about that time he was abducted by aliens. It sounds ridiculous, but he does make some convincing arguments. Tom thinks it was real, but could it have all just been in his head?
Lucid dreaming may help explain alleged alien abductions. During a lucid dream, people know that they’re dreaming, and can also have some control over how the dreams play out. During some dream states, a person can feel intense sensations, such as terror and paralysis, so it’s no wonder these dreams feel so real.
In a recent study, scientists encouraged 152 participants who had self-identified as lucid dreamers to dream about aliens. Many (75%) of the participants were able to dream about alien encounters, and 15% “achieved relatively realistic experiences,” the investigators reported.
So cut Tom some slack. He’s not crazy, he might just have lucid dreaming privileges. Tell him he should dream about something more fun, like a vacation in the Bahamas.
Follow your heart: Drink more coffee
It seems like the world is divided into coffee drinkers and non–coffee drinkers. Then there’s decaf and regular drinkers. Whichever camp you fall into, know this: The widespread belief that caffeine consumption has an effect on your heart is all beans.
In what is the largest investigation of its kind, researchers from the University of California, San Francisco, looked into whether drinking caffeinated coffee was linked to a risk for heart arrhythmia. They also researched whether patients with genetic variants that affect their metabolism could change that association. Almost 400,000 people with a mean age of 56 years participated in the study. More than half of the participants were women.
The investigators analyzed the participants’ self-reported coffee consumption using a technique called Mendelian randomization to leverage genetic data with the participants’ relationship with caffeine, making it an even field and not relying on the participant consumption self-reporting for outcomes as in previous studies.
What they found, after the 4-year follow up, was nothing short of myth busting.
“We found no evidence that caffeine consumption leads to a greater risk of arrhythmias,” said senior and corresponding author Gregory Marcus, MD. “Our population-based study provides reassurance that common prohibitions against caffeine to reduce arrhythmia risk are likely unwarranted.”
There was no evidence of a heightened risk of arrhythmias in participants who were genetically predisposed to metabolize caffeine differently from those who were not. And, there was a 3% reduction of arrhythmias in patients who consumed higher amounts of coffee.
We are not lobbying for Big Caffeine, but this study adds to the reported health benefits linked to coffee, which already include reduced risk for cancer, diabetes, and Parkinson’s disease, with an added bonus of anti-inflammatory benefits. So, the next time you’re hesitant to pour that second cup of Joe, just go for it. Your heart can take it.
Bored? Feeling down? Don’t play Candy Crush
Now hang on, aren’t those the perfect times to play video games? If there’s nothing else to do, why not open Candy Crush and mindlessly power through the levels?
Because, according to a study by a group of Canadian researchers, it’s actually the worst thing you can do. Well, maybe not literally, but it’s not helpful. Researchers recruited 60 Candy Crush players who were at various levels in the game. They had the participants play early levels that were far too easy or levels balanced with their gameplay abilities.
Players in the easy-level group got bored and quit far earlier than did those in the advanced-level group. The group playing to their abilities were able to access a “flow” state and focus all their attention on the game. While this is all well and good for their gaming performance, according to the researchers, it confirms the theory that playing to escape boredom or negative emotions is more likely to lead to addiction. As with all addictions, the temporary high can give way to a self-repeating loop, causing patients to ignore real life and deepen depression.
The researchers hope their findings will encourage game developers to “consider implementing responsible video gaming tools directly within their games.” Comedy gold. Perhaps Canadians’ idea of capitalism is a little different from that of those south of the border.
Hiccups and vaccine refusal
Tonight, LOTME News dives into the fetid cesspool that is international politics and comes out with … hiccups?
But first, a word from our sponsor, Fearless Boxing Club of South Etobicoke, Ontario.
Are you looking to flout public health restrictions? Do you want to spend time in an enclosed space with other people who haven’t gotten the COVID-19 vaccine? Do you “feel safer waiting until more research is done on the side effects being discovered right now”? (We are not making this up.)
Then join the Fearless Boxing Club, because we “will not be accepting any vaccinated members.” Our founders, Mohammed Abedeen and Krystal Glazier-Roscoe, are working hard to exclude “those who received the experimental COVID vaccine.” (Still not making it up.)
And now, back to the news.
Brazilian president Jair Bolsonaro was hospitalized recently for a severe case of hiccups that may have been related to a stab wound he received in 2018. [Nope, didn’t make that up, either.]
Mr. Bolsonaro had been hiccuping for 10 days, and was experiencing abdominal pain and difficulty speaking, when he entered the hospital on July 14. Since being stabbed while on the campaign trail, he has undergone several operations, which may have led to the partial intestinal obstruction that caused his latest symptoms.
His medical team advised Mr. Bolsonaro to go on a diet to aid his recovery, but when he was released on July 18 he said, “I hope in 10 days I’ll be eating barbecued ribs.” (Maybe this is all just a lucid dream. Probably shouldn’t have had ribs right before bed.)
I dream of alien abductions
There he goes! It’s lunchtime and your colleague Tom is going on and on again about that time he was abducted by aliens. It sounds ridiculous, but he does make some convincing arguments. Tom thinks it was real, but could it have all just been in his head?
Lucid dreaming may help explain alleged alien abductions. During a lucid dream, people know that they’re dreaming, and can also have some control over how the dreams play out. During some dream states, a person can feel intense sensations, such as terror and paralysis, so it’s no wonder these dreams feel so real.
In a recent study, scientists encouraged 152 participants who had self-identified as lucid dreamers to dream about aliens. Many (75%) of the participants were able to dream about alien encounters, and 15% “achieved relatively realistic experiences,” the investigators reported.
So cut Tom some slack. He’s not crazy, he might just have lucid dreaming privileges. Tell him he should dream about something more fun, like a vacation in the Bahamas.
Follow your heart: Drink more coffee
It seems like the world is divided into coffee drinkers and non–coffee drinkers. Then there’s decaf and regular drinkers. Whichever camp you fall into, know this: The widespread belief that caffeine consumption has an effect on your heart is all beans.
In what is the largest investigation of its kind, researchers from the University of California, San Francisco, looked into whether drinking caffeinated coffee was linked to a risk for heart arrhythmia. They also researched whether patients with genetic variants that affect their metabolism could change that association. Almost 400,000 people with a mean age of 56 years participated in the study. More than half of the participants were women.
The investigators analyzed the participants’ self-reported coffee consumption using a technique called Mendelian randomization to leverage genetic data with the participants’ relationship with caffeine, making it an even field and not relying on the participant consumption self-reporting for outcomes as in previous studies.
What they found, after the 4-year follow up, was nothing short of myth busting.
“We found no evidence that caffeine consumption leads to a greater risk of arrhythmias,” said senior and corresponding author Gregory Marcus, MD. “Our population-based study provides reassurance that common prohibitions against caffeine to reduce arrhythmia risk are likely unwarranted.”
There was no evidence of a heightened risk of arrhythmias in participants who were genetically predisposed to metabolize caffeine differently from those who were not. And, there was a 3% reduction of arrhythmias in patients who consumed higher amounts of coffee.
We are not lobbying for Big Caffeine, but this study adds to the reported health benefits linked to coffee, which already include reduced risk for cancer, diabetes, and Parkinson’s disease, with an added bonus of anti-inflammatory benefits. So, the next time you’re hesitant to pour that second cup of Joe, just go for it. Your heart can take it.
Bored? Feeling down? Don’t play Candy Crush
Now hang on, aren’t those the perfect times to play video games? If there’s nothing else to do, why not open Candy Crush and mindlessly power through the levels?
Because, according to a study by a group of Canadian researchers, it’s actually the worst thing you can do. Well, maybe not literally, but it’s not helpful. Researchers recruited 60 Candy Crush players who were at various levels in the game. They had the participants play early levels that were far too easy or levels balanced with their gameplay abilities.
Players in the easy-level group got bored and quit far earlier than did those in the advanced-level group. The group playing to their abilities were able to access a “flow” state and focus all their attention on the game. While this is all well and good for their gaming performance, according to the researchers, it confirms the theory that playing to escape boredom or negative emotions is more likely to lead to addiction. As with all addictions, the temporary high can give way to a self-repeating loop, causing patients to ignore real life and deepen depression.
The researchers hope their findings will encourage game developers to “consider implementing responsible video gaming tools directly within their games.” Comedy gold. Perhaps Canadians’ idea of capitalism is a little different from that of those south of the border.
Hiccups and vaccine refusal
Tonight, LOTME News dives into the fetid cesspool that is international politics and comes out with … hiccups?
But first, a word from our sponsor, Fearless Boxing Club of South Etobicoke, Ontario.
Are you looking to flout public health restrictions? Do you want to spend time in an enclosed space with other people who haven’t gotten the COVID-19 vaccine? Do you “feel safer waiting until more research is done on the side effects being discovered right now”? (We are not making this up.)
Then join the Fearless Boxing Club, because we “will not be accepting any vaccinated members.” Our founders, Mohammed Abedeen and Krystal Glazier-Roscoe, are working hard to exclude “those who received the experimental COVID vaccine.” (Still not making it up.)
And now, back to the news.
Brazilian president Jair Bolsonaro was hospitalized recently for a severe case of hiccups that may have been related to a stab wound he received in 2018. [Nope, didn’t make that up, either.]
Mr. Bolsonaro had been hiccuping for 10 days, and was experiencing abdominal pain and difficulty speaking, when he entered the hospital on July 14. Since being stabbed while on the campaign trail, he has undergone several operations, which may have led to the partial intestinal obstruction that caused his latest symptoms.
His medical team advised Mr. Bolsonaro to go on a diet to aid his recovery, but when he was released on July 18 he said, “I hope in 10 days I’ll be eating barbecued ribs.” (Maybe this is all just a lucid dream. Probably shouldn’t have had ribs right before bed.)
I dream of alien abductions
There he goes! It’s lunchtime and your colleague Tom is going on and on again about that time he was abducted by aliens. It sounds ridiculous, but he does make some convincing arguments. Tom thinks it was real, but could it have all just been in his head?
Lucid dreaming may help explain alleged alien abductions. During a lucid dream, people know that they’re dreaming, and can also have some control over how the dreams play out. During some dream states, a person can feel intense sensations, such as terror and paralysis, so it’s no wonder these dreams feel so real.
In a recent study, scientists encouraged 152 participants who had self-identified as lucid dreamers to dream about aliens. Many (75%) of the participants were able to dream about alien encounters, and 15% “achieved relatively realistic experiences,” the investigators reported.
So cut Tom some slack. He’s not crazy, he might just have lucid dreaming privileges. Tell him he should dream about something more fun, like a vacation in the Bahamas.
Follow your heart: Drink more coffee
It seems like the world is divided into coffee drinkers and non–coffee drinkers. Then there’s decaf and regular drinkers. Whichever camp you fall into, know this: The widespread belief that caffeine consumption has an effect on your heart is all beans.
In what is the largest investigation of its kind, researchers from the University of California, San Francisco, looked into whether drinking caffeinated coffee was linked to a risk for heart arrhythmia. They also researched whether patients with genetic variants that affect their metabolism could change that association. Almost 400,000 people with a mean age of 56 years participated in the study. More than half of the participants were women.
The investigators analyzed the participants’ self-reported coffee consumption using a technique called Mendelian randomization to leverage genetic data with the participants’ relationship with caffeine, making it an even field and not relying on the participant consumption self-reporting for outcomes as in previous studies.
What they found, after the 4-year follow up, was nothing short of myth busting.
“We found no evidence that caffeine consumption leads to a greater risk of arrhythmias,” said senior and corresponding author Gregory Marcus, MD. “Our population-based study provides reassurance that common prohibitions against caffeine to reduce arrhythmia risk are likely unwarranted.”
There was no evidence of a heightened risk of arrhythmias in participants who were genetically predisposed to metabolize caffeine differently from those who were not. And, there was a 3% reduction of arrhythmias in patients who consumed higher amounts of coffee.
We are not lobbying for Big Caffeine, but this study adds to the reported health benefits linked to coffee, which already include reduced risk for cancer, diabetes, and Parkinson’s disease, with an added bonus of anti-inflammatory benefits. So, the next time you’re hesitant to pour that second cup of Joe, just go for it. Your heart can take it.
Bored? Feeling down? Don’t play Candy Crush
Now hang on, aren’t those the perfect times to play video games? If there’s nothing else to do, why not open Candy Crush and mindlessly power through the levels?
Because, according to a study by a group of Canadian researchers, it’s actually the worst thing you can do. Well, maybe not literally, but it’s not helpful. Researchers recruited 60 Candy Crush players who were at various levels in the game. They had the participants play early levels that were far too easy or levels balanced with their gameplay abilities.
Players in the easy-level group got bored and quit far earlier than did those in the advanced-level group. The group playing to their abilities were able to access a “flow” state and focus all their attention on the game. While this is all well and good for their gaming performance, according to the researchers, it confirms the theory that playing to escape boredom or negative emotions is more likely to lead to addiction. As with all addictions, the temporary high can give way to a self-repeating loop, causing patients to ignore real life and deepen depression.
The researchers hope their findings will encourage game developers to “consider implementing responsible video gaming tools directly within their games.” Comedy gold. Perhaps Canadians’ idea of capitalism is a little different from that of those south of the border.
Hiccups and vaccine refusal
Tonight, LOTME News dives into the fetid cesspool that is international politics and comes out with … hiccups?
But first, a word from our sponsor, Fearless Boxing Club of South Etobicoke, Ontario.
Are you looking to flout public health restrictions? Do you want to spend time in an enclosed space with other people who haven’t gotten the COVID-19 vaccine? Do you “feel safer waiting until more research is done on the side effects being discovered right now”? (We are not making this up.)
Then join the Fearless Boxing Club, because we “will not be accepting any vaccinated members.” Our founders, Mohammed Abedeen and Krystal Glazier-Roscoe, are working hard to exclude “those who received the experimental COVID vaccine.” (Still not making it up.)
And now, back to the news.
Brazilian president Jair Bolsonaro was hospitalized recently for a severe case of hiccups that may have been related to a stab wound he received in 2018. [Nope, didn’t make that up, either.]
Mr. Bolsonaro had been hiccuping for 10 days, and was experiencing abdominal pain and difficulty speaking, when he entered the hospital on July 14. Since being stabbed while on the campaign trail, he has undergone several operations, which may have led to the partial intestinal obstruction that caused his latest symptoms.
His medical team advised Mr. Bolsonaro to go on a diet to aid his recovery, but when he was released on July 18 he said, “I hope in 10 days I’ll be eating barbecued ribs.” (Maybe this is all just a lucid dream. Probably shouldn’t have had ribs right before bed.)
Medicare rules for CPAP penalize low-income patients for nonadherence
Report from the CHEST Health Policy and Advocacy Committee (HPAC) Conference
The relationship between adherence and benefit for those prescribed continuous positive airway pressure (CPAP) devices is clear. However, a Medicare-reimbursement rule that demands adherence blind to circumstances appears to be denying access to many low-income patients, according to an analysis delivered at the annual CHEST Health Policy and Advocacy Committee (HPAC) conference sponsored by the American College of Chest Physicians.
Over the past several years, adherence to CPAP has improved substantially following a series of studies that demonstrated the device must be used at least 4 hours per night to achieve improved outcomes. Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (21 nights) during a consecutive 30-day period any time in the first 3 months of initial usage.
However, the studies that show improved adherence show a lag among those in the lowest income quartile, according to Sairam Parthasarathy, MD, FCCP, of the Center for Sleep and Circadian Sciences at the University of Arizona, Tucson.
When patients are followed for a year after being prescribed CPAP, the lag for the low-income patients is not seen immediately. Rather, adherence studies show a steady climb in adherence in all income groups initially, but “right at 90 days, there is a marked change,” according to Dr. Parthasarathy.
This change happens to coincide with Medicare policy that denies reimbursement for CPAP after 90 days if patients are not using CPAP at least 4 hours per night, which is the threshold associated with benefit.
The correlation between this policy and income disparity is “observational” rather than proven, but Dr. Parthasarathy is confident it is valid. He believes it is a prime example of a health inequity driven by poorly conceived policy.
“The 90-day rule needs to go,” he said, calling the choice of threshold “man-made.”
“This is the only disease condition for which a therapy is withheld if it is not used according to some magical threshold,” he said. “I cannot think of a more draconian policy.”
In an effort to illustrate the problem, he likened this policy to withholding insulin in a diabetes patient judged nonadherent because of a persistently elevated Hb1Ac.
At 90 days, adherence rates remain at a relatively early point in their upwards trajectory in all income groups. One year later, adherence rates are more than twice as high in the highest income relative to the lowest quartile and approaching twofold greater in quartiles 2 and 3.
“It takes time to get used to these devices,” Dr. Parthasarathy explained. Given studies demonstrating that “more is better” with CPAP, whether measured by sleep scales or quality of life, Dr. Parthasarathy advocates strategies to improve adherence, but he questioned an approach that penalizes low-income patients for a definition of nonadherence at an arbitrary point in time. He suggested it is just one example of health policies that ultimately penalize individuals with lower incomes.
“There are millions of dollars spent every year on understanding the genetics of disease, but the biggest influence on how long you live is the ZIP code of where you live,” said Dr. Parthasarathy, referring to zip codes as a surrogate for socioeconomic status.
This is not to imply, however, that genetics are irrelevant, Dr. Parthasarathy said. He pointed to data linking genetic traits that determine melanin levels and circadian rhythms. He noted one genotype associated with later bedtimes that is more commonly found in African Americans and Hispanics. This has relevance to a variety of sleep disorders and other health conditions, but it might serve as a fundamental disadvantage for children with this genotype, Dr. Parthasarathy maintained. He cited a study conducted at his center that found Hispanic children sleep on average 30 minutes less than white children (Sleep Med. 2016;18:61-66). The reason was simple. Hispanic children went to bed 30 minutes later but rose at the same time.
The later bedtimes and reduced sleep could potentially be one obstacle among many, such as the need for lower income patients to hold several jobs, that prevent these patients from becoming accustomed to CPAP at the same speed as wealthier patients, according to Dr. Parthasarathy.
The current Medicare policy that withholds CPAP on the basis of a single definition of nonadherence appears to lead directly to an inequity in treatment of sleep apnea, Dr. Parthasarathy maintained. Dr. Parthasarathy, who was a coauthor of a recently published paper on addressing disparities in sleep health (Chest. 2021;159:1232-40), described this issue as part of a larger problem of the failure to deliver health care that is sensitive to the cultural and racial differences underlying these inequities.
Kathleen Sarmiento, MD, FCCP, Director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System, agreed. Dr. Sarmiento, a member of the CHEST Health Policy and Advocacy Committee and the moderator of the session in which Dr. Parthasarathy presented his data, said, “This type of issue is exactly what our Committee [HPAC] would like to address.”
The association between the 90-day Medicare rule for CPAP reimbursement and reduced access to this therapy among patients of lower economic status is compelling, she indicated. Within the goal of advocacy for health policies that will reduce inequities, Dr. Sarmiento explained that the committee is attempting to identify and reverse the source of these types of disparity.
“Specific rules or regulations are actionable targets to effect broader change in health care access and health care delivery,” said Dr. Sarmiento, alluding to the mission of HPAC.
Dr. Parthasarathy and Dr. Sarmiento report no relevant conflicts of interest.
Report from the CHEST Health Policy and Advocacy Committee (HPAC) Conference
Report from the CHEST Health Policy and Advocacy Committee (HPAC) Conference
The relationship between adherence and benefit for those prescribed continuous positive airway pressure (CPAP) devices is clear. However, a Medicare-reimbursement rule that demands adherence blind to circumstances appears to be denying access to many low-income patients, according to an analysis delivered at the annual CHEST Health Policy and Advocacy Committee (HPAC) conference sponsored by the American College of Chest Physicians.
Over the past several years, adherence to CPAP has improved substantially following a series of studies that demonstrated the device must be used at least 4 hours per night to achieve improved outcomes. Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (21 nights) during a consecutive 30-day period any time in the first 3 months of initial usage.
However, the studies that show improved adherence show a lag among those in the lowest income quartile, according to Sairam Parthasarathy, MD, FCCP, of the Center for Sleep and Circadian Sciences at the University of Arizona, Tucson.
When patients are followed for a year after being prescribed CPAP, the lag for the low-income patients is not seen immediately. Rather, adherence studies show a steady climb in adherence in all income groups initially, but “right at 90 days, there is a marked change,” according to Dr. Parthasarathy.
This change happens to coincide with Medicare policy that denies reimbursement for CPAP after 90 days if patients are not using CPAP at least 4 hours per night, which is the threshold associated with benefit.
The correlation between this policy and income disparity is “observational” rather than proven, but Dr. Parthasarathy is confident it is valid. He believes it is a prime example of a health inequity driven by poorly conceived policy.
“The 90-day rule needs to go,” he said, calling the choice of threshold “man-made.”
“This is the only disease condition for which a therapy is withheld if it is not used according to some magical threshold,” he said. “I cannot think of a more draconian policy.”
In an effort to illustrate the problem, he likened this policy to withholding insulin in a diabetes patient judged nonadherent because of a persistently elevated Hb1Ac.
At 90 days, adherence rates remain at a relatively early point in their upwards trajectory in all income groups. One year later, adherence rates are more than twice as high in the highest income relative to the lowest quartile and approaching twofold greater in quartiles 2 and 3.
“It takes time to get used to these devices,” Dr. Parthasarathy explained. Given studies demonstrating that “more is better” with CPAP, whether measured by sleep scales or quality of life, Dr. Parthasarathy advocates strategies to improve adherence, but he questioned an approach that penalizes low-income patients for a definition of nonadherence at an arbitrary point in time. He suggested it is just one example of health policies that ultimately penalize individuals with lower incomes.
“There are millions of dollars spent every year on understanding the genetics of disease, but the biggest influence on how long you live is the ZIP code of where you live,” said Dr. Parthasarathy, referring to zip codes as a surrogate for socioeconomic status.
This is not to imply, however, that genetics are irrelevant, Dr. Parthasarathy said. He pointed to data linking genetic traits that determine melanin levels and circadian rhythms. He noted one genotype associated with later bedtimes that is more commonly found in African Americans and Hispanics. This has relevance to a variety of sleep disorders and other health conditions, but it might serve as a fundamental disadvantage for children with this genotype, Dr. Parthasarathy maintained. He cited a study conducted at his center that found Hispanic children sleep on average 30 minutes less than white children (Sleep Med. 2016;18:61-66). The reason was simple. Hispanic children went to bed 30 minutes later but rose at the same time.
The later bedtimes and reduced sleep could potentially be one obstacle among many, such as the need for lower income patients to hold several jobs, that prevent these patients from becoming accustomed to CPAP at the same speed as wealthier patients, according to Dr. Parthasarathy.
The current Medicare policy that withholds CPAP on the basis of a single definition of nonadherence appears to lead directly to an inequity in treatment of sleep apnea, Dr. Parthasarathy maintained. Dr. Parthasarathy, who was a coauthor of a recently published paper on addressing disparities in sleep health (Chest. 2021;159:1232-40), described this issue as part of a larger problem of the failure to deliver health care that is sensitive to the cultural and racial differences underlying these inequities.
Kathleen Sarmiento, MD, FCCP, Director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System, agreed. Dr. Sarmiento, a member of the CHEST Health Policy and Advocacy Committee and the moderator of the session in which Dr. Parthasarathy presented his data, said, “This type of issue is exactly what our Committee [HPAC] would like to address.”
The association between the 90-day Medicare rule for CPAP reimbursement and reduced access to this therapy among patients of lower economic status is compelling, she indicated. Within the goal of advocacy for health policies that will reduce inequities, Dr. Sarmiento explained that the committee is attempting to identify and reverse the source of these types of disparity.
“Specific rules or regulations are actionable targets to effect broader change in health care access and health care delivery,” said Dr. Sarmiento, alluding to the mission of HPAC.
Dr. Parthasarathy and Dr. Sarmiento report no relevant conflicts of interest.
The relationship between adherence and benefit for those prescribed continuous positive airway pressure (CPAP) devices is clear. However, a Medicare-reimbursement rule that demands adherence blind to circumstances appears to be denying access to many low-income patients, according to an analysis delivered at the annual CHEST Health Policy and Advocacy Committee (HPAC) conference sponsored by the American College of Chest Physicians.
Over the past several years, adherence to CPAP has improved substantially following a series of studies that demonstrated the device must be used at least 4 hours per night to achieve improved outcomes. Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (21 nights) during a consecutive 30-day period any time in the first 3 months of initial usage.
However, the studies that show improved adherence show a lag among those in the lowest income quartile, according to Sairam Parthasarathy, MD, FCCP, of the Center for Sleep and Circadian Sciences at the University of Arizona, Tucson.
When patients are followed for a year after being prescribed CPAP, the lag for the low-income patients is not seen immediately. Rather, adherence studies show a steady climb in adherence in all income groups initially, but “right at 90 days, there is a marked change,” according to Dr. Parthasarathy.
This change happens to coincide with Medicare policy that denies reimbursement for CPAP after 90 days if patients are not using CPAP at least 4 hours per night, which is the threshold associated with benefit.
The correlation between this policy and income disparity is “observational” rather than proven, but Dr. Parthasarathy is confident it is valid. He believes it is a prime example of a health inequity driven by poorly conceived policy.
“The 90-day rule needs to go,” he said, calling the choice of threshold “man-made.”
“This is the only disease condition for which a therapy is withheld if it is not used according to some magical threshold,” he said. “I cannot think of a more draconian policy.”
In an effort to illustrate the problem, he likened this policy to withholding insulin in a diabetes patient judged nonadherent because of a persistently elevated Hb1Ac.
At 90 days, adherence rates remain at a relatively early point in their upwards trajectory in all income groups. One year later, adherence rates are more than twice as high in the highest income relative to the lowest quartile and approaching twofold greater in quartiles 2 and 3.
“It takes time to get used to these devices,” Dr. Parthasarathy explained. Given studies demonstrating that “more is better” with CPAP, whether measured by sleep scales or quality of life, Dr. Parthasarathy advocates strategies to improve adherence, but he questioned an approach that penalizes low-income patients for a definition of nonadherence at an arbitrary point in time. He suggested it is just one example of health policies that ultimately penalize individuals with lower incomes.
“There are millions of dollars spent every year on understanding the genetics of disease, but the biggest influence on how long you live is the ZIP code of where you live,” said Dr. Parthasarathy, referring to zip codes as a surrogate for socioeconomic status.
This is not to imply, however, that genetics are irrelevant, Dr. Parthasarathy said. He pointed to data linking genetic traits that determine melanin levels and circadian rhythms. He noted one genotype associated with later bedtimes that is more commonly found in African Americans and Hispanics. This has relevance to a variety of sleep disorders and other health conditions, but it might serve as a fundamental disadvantage for children with this genotype, Dr. Parthasarathy maintained. He cited a study conducted at his center that found Hispanic children sleep on average 30 minutes less than white children (Sleep Med. 2016;18:61-66). The reason was simple. Hispanic children went to bed 30 minutes later but rose at the same time.
The later bedtimes and reduced sleep could potentially be one obstacle among many, such as the need for lower income patients to hold several jobs, that prevent these patients from becoming accustomed to CPAP at the same speed as wealthier patients, according to Dr. Parthasarathy.
The current Medicare policy that withholds CPAP on the basis of a single definition of nonadherence appears to lead directly to an inequity in treatment of sleep apnea, Dr. Parthasarathy maintained. Dr. Parthasarathy, who was a coauthor of a recently published paper on addressing disparities in sleep health (Chest. 2021;159:1232-40), described this issue as part of a larger problem of the failure to deliver health care that is sensitive to the cultural and racial differences underlying these inequities.
Kathleen Sarmiento, MD, FCCP, Director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System, agreed. Dr. Sarmiento, a member of the CHEST Health Policy and Advocacy Committee and the moderator of the session in which Dr. Parthasarathy presented his data, said, “This type of issue is exactly what our Committee [HPAC] would like to address.”
The association between the 90-day Medicare rule for CPAP reimbursement and reduced access to this therapy among patients of lower economic status is compelling, she indicated. Within the goal of advocacy for health policies that will reduce inequities, Dr. Sarmiento explained that the committee is attempting to identify and reverse the source of these types of disparity.
“Specific rules or regulations are actionable targets to effect broader change in health care access and health care delivery,” said Dr. Sarmiento, alluding to the mission of HPAC.
Dr. Parthasarathy and Dr. Sarmiento report no relevant conflicts of interest.
Political support of permanent DST concerns sleep scientists
The reintroduction of congressional bills that aim to end seasonal time change and move permanently to daylight saving time (DST) – and action on the issue by 19 states in the last 4 years – signal political momentum and up the ante on sleep medicine to educate others and to more uniformly weigh in on the health consequences of such a change.
This was the message of several sleep scientists and physicians who participated in moderated discussions of DST at the virtual annual meeting of the Associated Professional Sleep Societies.
A position paper issued about a year ago by the American Academy of Sleep Medicine objected to the proposed switch and instead called for elimination of DST in favor of permanent standard time (ST). While there are detrimental health effects with time changes in either direction, there is “abundant” evidence that the transition from standard time to daylight saving time is worse, the AASM statement says.
Some experts have questioned, however, whether the evidence is weighty and comprehensive enough to drive a change in national policy. Others, such as SLEEP 2021 discussant Karin Johnson, MD, say there is unawareness outside of sleep medicine – and even within – of a growing body of literature on circadian misalignment and its associated health risks.
“There’s an educational gap for what’s out there [in the literature],” Dr. Johnson, medical director of the Baystate Health regional sleep program and Baystate Medical Center sleep laboratory in Springfield, Mass., said in an interview after the meeting.
Calls for more research, particularly on the chronic effects of DST and ST, are concerning because discussions of abolishing seasonal time change are “moving forward with or without us,” Kenneth Wright Jr., PhD, director of the chronobiology laboratory at the University of Colorado in Boulder and professor in the university’s department of integrative biology, said at the meeting.
“We don’t have time ... to have the studies we’d need to prove unequivocally that permanent standard time [is best]. We need to consider the scientific evidence before us – what’s known about human biology and health with respect to light and circadian timing,” Dr. Wright said. “The argument that pushing our clocks later is going to be healthier is not tenable. We cannot support that given the vast amount of scientific evidence we have from circadian and sleep science.”
Underscoring the sense of urgency to be engaged in the issue were the messages of Rep. Raymond Ward, MD, PhD, a Utah legislator in the state’s House of Representatives who introduced a bill to permanently observe DST, pending the amendment of federal law to permit such a change, and provided that five other Western states enact the same legislation.
“I chose to support DST because I became convinced this is the only thing that’s politically possible,” said Rep. Ward, a family practice physician at the Ogden Clinic in Bountiful. National polls have shown a “strong preference” to end seasonal time change, he said, and a poll conducted in his district showed that nearly 80% “wanted to stop changing the clocks, and 65% wanted the summer time schedule.”
“To me, the train seems to be moving in one direction,” said Rep. Ward. “The bills open in Congress in both the House and the Senate don’t have enough support yet, but every time another state legislature passes [legislation to establish permanent DST], they pick up a few more supporters.”
The Sunshine Protection Act of 2021 introduced in the House in January by Rep. Vern Buchanan (R-Fla.) has 23 cosponsors, and a bill of the same name introduced in the Senate in March by Marco Rubio (R-Fla.) has 14 cosponsors. Both bills have bipartisan support and are reintroductions of legislation initially put forth in 2019. A press release issued by Sen. Rubio’s office says that “extending DST can benefit the economy and our overall health.”
According to the National Conference of State Legislatures, 19 states have enacted legislation or passed resolutions in the last several years to provide for year-round DST, if Congress were to allow such a change. And according to a Congressional Research Service (CRS) report on DST updated in September 2020, at least 45 states have, since 2015, proposed legislation to change their observance of DST.
These efforts include proposals to exempt a state from DST observance, which is allowable under existing law, and proposals that would establish permanent DST, which would require Congress to amend the Uniform Time Act of 1966, the CRS report says.
The state of the science
Shifting from ST to DST has been associated with an increase in cardiovascular morbidity (heart attacks and atrial fibrillation), increased missed medical appointments, increased ED visits, increased mood disturbances and suicide risk, increased risk of fatal car crashes and medical errors – and sleep loss, said Elizabeth Klerman, MD, PhD, professor of neurology in the division of sleep medicine at Harvard Medical School, Boston.
These associations are covered in AASM statement, along with acknowledgment that most studies on the chronic effects of DST have “either been retrospective or addressed the issue indirectly.”
For Dr. Johnson, who refers to DST as “sleep deprivation time,” the most convincing data regarding the dangers of permanent DST come from studies comparing locations within time zones. “The farther you’re off from the meridian, the more you have that ‘social jet lag’ or circadian misalignment [between the innate circadian rhythm, which is synchronized with solar time, and school or work schedules],” she said at the meeting.
Researchers reported in 2017, for instance, that the risk for all cancers and many specific cancers increased from east to west within a time zone, as solar time is progressively delayed. “They documented changes in risk for every 5 degrees west from the meridian,” she said.
Dr. Johnson is a case in point of the “educational gap” that she believes needs attention. Two years ago, as chair of the sleep section of the American Academy of Neurology, she delved into the literature after the AAN asked the section whether it should endorse the AASM’s position paper on DST. “I didn’t know the literature even as a sleep scientist until I got into this,” she said.
“If you’re asked me 2 years ago,” she added in the later interview, “I would have said that permanent DST is fine.”
The sleep section recommended that the AAN endorse permanent ST, but the AAN ultimately decided it “didn’t feel strongly enough to say that standard time is unequivocally the better option,” Dr. Johnson said in an interview. “They agreed that there’s science [in favor of it], but ... it’s a big public policy decision.”
Jamie Zeitzer, PhD, associate professor of psychiatry and behavioral sciences at Stanford (Calif.) University’s Center for Sleep Sciences and Medicine, voiced similar concerns at the meeting about currently advocating a shift in either direction. It’s “absolutely clear that switching clocks, especially since it’s occurring at a population level, is deleterious and we need to get rid of it,” he said. “But before we put forth dictates on public health [with a shift to permanent ST], I think we better be sure we’re correct.”
“I think we’re getting close. I think the data thus far [are indicating] that permanent standard time is better for health,” Dr. Zeitzer said. “But I don’t think there’s a cumulative amount of evidence to really say that we have to subvert all other interests because this is so important for public health. We need at least a few more studies.”
There is not enough evidence, for instance, to conclude that the body clock does not eventually adjust to DST, he said, and it is not yet clear what roles electric light and sunlight each play in the body’s circadian time.
“And we need to think about north-south. What may be important for the upper Midwest, and for Maine, and for Washington, may not be ... good for Florida and Texas and southern California,” Dr. Zeitzer said. “You have very different patterns of light exposure, especially when it deals with seasons.”
Historical considerations
In his comments at the meeting, Muhammad Rishi, MBBS, the lead author of the AASM’s position statement, added that circadian misalignment – that “asynchrony between the internal and external clocks” – is associated in studies with an increased risk of obesity, metabolic syndrome, and depression.
But he also emphasized that the “historical evidence” against permanent DST is at least as strong as the medical evidence.
“The U.S. has gone on permanent daylight savings time several times in the past, most recently in the 1970s during the OPEC [oil embargo], and it was so unpopular,” said Dr. Rishi, of the department of pulmonology, critical care and sleep medicine at the Mayo Clinic Health System in Eau Claire, Wis. “England also did it in the 1960s and then abolished it, and most recently Russia did it ... it became so unpopular with increased depression and mood disorders that they abolished it.”
Rep. Ward said that China has offered a large natural experiment with its move decades ago from five time zones to one time zone – Beijing time. “I don’t think we’ve seen any sweeping changes in their health because they have one large time zone,” he said.
Dr. Klerman took issue, saying she “knows someone in China who is trying to get that data about health outcomes and is unable to get it.”
Arguments that DST saves energy hold little to no weight upon scrutiny of the data, Dr. Johnson said. Moreover, research other than oft-cited, older Department of Transportation studies suggests that “permanent DST is bad for energy and bad for the climate,” she said. “This really needs to be more fully evaluated by the government and others.”
Dr. Johnson said after the meeting that it’s important for experts from the energy and climate sectors, education, and medicine – including pediatrics, oncology, and other specialties with “a stake in this” – to come together and share information so “we won’t all be in our silos.” She and other sleep experts in the neurology field are planning to host a summit in 2022 to do just this.
Dr. Johnson and Kin Yuen, MD, of the Sleep Disorders Center at the University of California, San Francisco, both expressed concern at the meeting that adoption of permanent DST would negate the benefits of delayed school start times in middle and high school students.
There is some evidence that delayed start times have led to decreased tardiness and absences, Dr. Yuen said. To have the same impact with permanent DST, “instead of starting at 8:30 a.m., you’d have to start at 9:30,” Dr. Johnson added after the meeting.
The first discussion of DST at the SLEEP 2021 meeting was led by Erin E. Flynn-Evans, PhD, MPH, director of the Fatigue Countermeasures Laboratory at the National Aeronautics and Space Administration Ames Research Center. Dr. Yuen led a later second question-and-answer session. They and each of the eight participants reported that they had no relevant conflicts of interest.
Dr. Yuen and Dr. Flynn-Evans are both coauthors of the AASM’s position statement on DST. Dr. Klerman is a coauthor of the Society for Research on Biological Rhythms 2019 position paper on DST.
The AASM’s statement has been endorsed by 19 organizations, including the American College of Chest Physicians, the SRBR, the American Academy of Cardiovascular Sleep Medicine, the Society of Behavioral Sleep Medicine, the National PTA, and the American College of Occupational and Environmental Medicine.
The reintroduction of congressional bills that aim to end seasonal time change and move permanently to daylight saving time (DST) – and action on the issue by 19 states in the last 4 years – signal political momentum and up the ante on sleep medicine to educate others and to more uniformly weigh in on the health consequences of such a change.
This was the message of several sleep scientists and physicians who participated in moderated discussions of DST at the virtual annual meeting of the Associated Professional Sleep Societies.
A position paper issued about a year ago by the American Academy of Sleep Medicine objected to the proposed switch and instead called for elimination of DST in favor of permanent standard time (ST). While there are detrimental health effects with time changes in either direction, there is “abundant” evidence that the transition from standard time to daylight saving time is worse, the AASM statement says.
Some experts have questioned, however, whether the evidence is weighty and comprehensive enough to drive a change in national policy. Others, such as SLEEP 2021 discussant Karin Johnson, MD, say there is unawareness outside of sleep medicine – and even within – of a growing body of literature on circadian misalignment and its associated health risks.
“There’s an educational gap for what’s out there [in the literature],” Dr. Johnson, medical director of the Baystate Health regional sleep program and Baystate Medical Center sleep laboratory in Springfield, Mass., said in an interview after the meeting.
Calls for more research, particularly on the chronic effects of DST and ST, are concerning because discussions of abolishing seasonal time change are “moving forward with or without us,” Kenneth Wright Jr., PhD, director of the chronobiology laboratory at the University of Colorado in Boulder and professor in the university’s department of integrative biology, said at the meeting.
“We don’t have time ... to have the studies we’d need to prove unequivocally that permanent standard time [is best]. We need to consider the scientific evidence before us – what’s known about human biology and health with respect to light and circadian timing,” Dr. Wright said. “The argument that pushing our clocks later is going to be healthier is not tenable. We cannot support that given the vast amount of scientific evidence we have from circadian and sleep science.”
Underscoring the sense of urgency to be engaged in the issue were the messages of Rep. Raymond Ward, MD, PhD, a Utah legislator in the state’s House of Representatives who introduced a bill to permanently observe DST, pending the amendment of federal law to permit such a change, and provided that five other Western states enact the same legislation.
“I chose to support DST because I became convinced this is the only thing that’s politically possible,” said Rep. Ward, a family practice physician at the Ogden Clinic in Bountiful. National polls have shown a “strong preference” to end seasonal time change, he said, and a poll conducted in his district showed that nearly 80% “wanted to stop changing the clocks, and 65% wanted the summer time schedule.”
“To me, the train seems to be moving in one direction,” said Rep. Ward. “The bills open in Congress in both the House and the Senate don’t have enough support yet, but every time another state legislature passes [legislation to establish permanent DST], they pick up a few more supporters.”
The Sunshine Protection Act of 2021 introduced in the House in January by Rep. Vern Buchanan (R-Fla.) has 23 cosponsors, and a bill of the same name introduced in the Senate in March by Marco Rubio (R-Fla.) has 14 cosponsors. Both bills have bipartisan support and are reintroductions of legislation initially put forth in 2019. A press release issued by Sen. Rubio’s office says that “extending DST can benefit the economy and our overall health.”
According to the National Conference of State Legislatures, 19 states have enacted legislation or passed resolutions in the last several years to provide for year-round DST, if Congress were to allow such a change. And according to a Congressional Research Service (CRS) report on DST updated in September 2020, at least 45 states have, since 2015, proposed legislation to change their observance of DST.
These efforts include proposals to exempt a state from DST observance, which is allowable under existing law, and proposals that would establish permanent DST, which would require Congress to amend the Uniform Time Act of 1966, the CRS report says.
The state of the science
Shifting from ST to DST has been associated with an increase in cardiovascular morbidity (heart attacks and atrial fibrillation), increased missed medical appointments, increased ED visits, increased mood disturbances and suicide risk, increased risk of fatal car crashes and medical errors – and sleep loss, said Elizabeth Klerman, MD, PhD, professor of neurology in the division of sleep medicine at Harvard Medical School, Boston.
These associations are covered in AASM statement, along with acknowledgment that most studies on the chronic effects of DST have “either been retrospective or addressed the issue indirectly.”
For Dr. Johnson, who refers to DST as “sleep deprivation time,” the most convincing data regarding the dangers of permanent DST come from studies comparing locations within time zones. “The farther you’re off from the meridian, the more you have that ‘social jet lag’ or circadian misalignment [between the innate circadian rhythm, which is synchronized with solar time, and school or work schedules],” she said at the meeting.
Researchers reported in 2017, for instance, that the risk for all cancers and many specific cancers increased from east to west within a time zone, as solar time is progressively delayed. “They documented changes in risk for every 5 degrees west from the meridian,” she said.
Dr. Johnson is a case in point of the “educational gap” that she believes needs attention. Two years ago, as chair of the sleep section of the American Academy of Neurology, she delved into the literature after the AAN asked the section whether it should endorse the AASM’s position paper on DST. “I didn’t know the literature even as a sleep scientist until I got into this,” she said.
“If you’re asked me 2 years ago,” she added in the later interview, “I would have said that permanent DST is fine.”
The sleep section recommended that the AAN endorse permanent ST, but the AAN ultimately decided it “didn’t feel strongly enough to say that standard time is unequivocally the better option,” Dr. Johnson said in an interview. “They agreed that there’s science [in favor of it], but ... it’s a big public policy decision.”
Jamie Zeitzer, PhD, associate professor of psychiatry and behavioral sciences at Stanford (Calif.) University’s Center for Sleep Sciences and Medicine, voiced similar concerns at the meeting about currently advocating a shift in either direction. It’s “absolutely clear that switching clocks, especially since it’s occurring at a population level, is deleterious and we need to get rid of it,” he said. “But before we put forth dictates on public health [with a shift to permanent ST], I think we better be sure we’re correct.”
“I think we’re getting close. I think the data thus far [are indicating] that permanent standard time is better for health,” Dr. Zeitzer said. “But I don’t think there’s a cumulative amount of evidence to really say that we have to subvert all other interests because this is so important for public health. We need at least a few more studies.”
There is not enough evidence, for instance, to conclude that the body clock does not eventually adjust to DST, he said, and it is not yet clear what roles electric light and sunlight each play in the body’s circadian time.
“And we need to think about north-south. What may be important for the upper Midwest, and for Maine, and for Washington, may not be ... good for Florida and Texas and southern California,” Dr. Zeitzer said. “You have very different patterns of light exposure, especially when it deals with seasons.”
Historical considerations
In his comments at the meeting, Muhammad Rishi, MBBS, the lead author of the AASM’s position statement, added that circadian misalignment – that “asynchrony between the internal and external clocks” – is associated in studies with an increased risk of obesity, metabolic syndrome, and depression.
But he also emphasized that the “historical evidence” against permanent DST is at least as strong as the medical evidence.
“The U.S. has gone on permanent daylight savings time several times in the past, most recently in the 1970s during the OPEC [oil embargo], and it was so unpopular,” said Dr. Rishi, of the department of pulmonology, critical care and sleep medicine at the Mayo Clinic Health System in Eau Claire, Wis. “England also did it in the 1960s and then abolished it, and most recently Russia did it ... it became so unpopular with increased depression and mood disorders that they abolished it.”
Rep. Ward said that China has offered a large natural experiment with its move decades ago from five time zones to one time zone – Beijing time. “I don’t think we’ve seen any sweeping changes in their health because they have one large time zone,” he said.
Dr. Klerman took issue, saying she “knows someone in China who is trying to get that data about health outcomes and is unable to get it.”
Arguments that DST saves energy hold little to no weight upon scrutiny of the data, Dr. Johnson said. Moreover, research other than oft-cited, older Department of Transportation studies suggests that “permanent DST is bad for energy and bad for the climate,” she said. “This really needs to be more fully evaluated by the government and others.”
Dr. Johnson said after the meeting that it’s important for experts from the energy and climate sectors, education, and medicine – including pediatrics, oncology, and other specialties with “a stake in this” – to come together and share information so “we won’t all be in our silos.” She and other sleep experts in the neurology field are planning to host a summit in 2022 to do just this.
Dr. Johnson and Kin Yuen, MD, of the Sleep Disorders Center at the University of California, San Francisco, both expressed concern at the meeting that adoption of permanent DST would negate the benefits of delayed school start times in middle and high school students.
There is some evidence that delayed start times have led to decreased tardiness and absences, Dr. Yuen said. To have the same impact with permanent DST, “instead of starting at 8:30 a.m., you’d have to start at 9:30,” Dr. Johnson added after the meeting.
The first discussion of DST at the SLEEP 2021 meeting was led by Erin E. Flynn-Evans, PhD, MPH, director of the Fatigue Countermeasures Laboratory at the National Aeronautics and Space Administration Ames Research Center. Dr. Yuen led a later second question-and-answer session. They and each of the eight participants reported that they had no relevant conflicts of interest.
Dr. Yuen and Dr. Flynn-Evans are both coauthors of the AASM’s position statement on DST. Dr. Klerman is a coauthor of the Society for Research on Biological Rhythms 2019 position paper on DST.
The AASM’s statement has been endorsed by 19 organizations, including the American College of Chest Physicians, the SRBR, the American Academy of Cardiovascular Sleep Medicine, the Society of Behavioral Sleep Medicine, the National PTA, and the American College of Occupational and Environmental Medicine.
The reintroduction of congressional bills that aim to end seasonal time change and move permanently to daylight saving time (DST) – and action on the issue by 19 states in the last 4 years – signal political momentum and up the ante on sleep medicine to educate others and to more uniformly weigh in on the health consequences of such a change.
This was the message of several sleep scientists and physicians who participated in moderated discussions of DST at the virtual annual meeting of the Associated Professional Sleep Societies.
A position paper issued about a year ago by the American Academy of Sleep Medicine objected to the proposed switch and instead called for elimination of DST in favor of permanent standard time (ST). While there are detrimental health effects with time changes in either direction, there is “abundant” evidence that the transition from standard time to daylight saving time is worse, the AASM statement says.
Some experts have questioned, however, whether the evidence is weighty and comprehensive enough to drive a change in national policy. Others, such as SLEEP 2021 discussant Karin Johnson, MD, say there is unawareness outside of sleep medicine – and even within – of a growing body of literature on circadian misalignment and its associated health risks.
“There’s an educational gap for what’s out there [in the literature],” Dr. Johnson, medical director of the Baystate Health regional sleep program and Baystate Medical Center sleep laboratory in Springfield, Mass., said in an interview after the meeting.
Calls for more research, particularly on the chronic effects of DST and ST, are concerning because discussions of abolishing seasonal time change are “moving forward with or without us,” Kenneth Wright Jr., PhD, director of the chronobiology laboratory at the University of Colorado in Boulder and professor in the university’s department of integrative biology, said at the meeting.
“We don’t have time ... to have the studies we’d need to prove unequivocally that permanent standard time [is best]. We need to consider the scientific evidence before us – what’s known about human biology and health with respect to light and circadian timing,” Dr. Wright said. “The argument that pushing our clocks later is going to be healthier is not tenable. We cannot support that given the vast amount of scientific evidence we have from circadian and sleep science.”
Underscoring the sense of urgency to be engaged in the issue were the messages of Rep. Raymond Ward, MD, PhD, a Utah legislator in the state’s House of Representatives who introduced a bill to permanently observe DST, pending the amendment of federal law to permit such a change, and provided that five other Western states enact the same legislation.
“I chose to support DST because I became convinced this is the only thing that’s politically possible,” said Rep. Ward, a family practice physician at the Ogden Clinic in Bountiful. National polls have shown a “strong preference” to end seasonal time change, he said, and a poll conducted in his district showed that nearly 80% “wanted to stop changing the clocks, and 65% wanted the summer time schedule.”
“To me, the train seems to be moving in one direction,” said Rep. Ward. “The bills open in Congress in both the House and the Senate don’t have enough support yet, but every time another state legislature passes [legislation to establish permanent DST], they pick up a few more supporters.”
The Sunshine Protection Act of 2021 introduced in the House in January by Rep. Vern Buchanan (R-Fla.) has 23 cosponsors, and a bill of the same name introduced in the Senate in March by Marco Rubio (R-Fla.) has 14 cosponsors. Both bills have bipartisan support and are reintroductions of legislation initially put forth in 2019. A press release issued by Sen. Rubio’s office says that “extending DST can benefit the economy and our overall health.”
According to the National Conference of State Legislatures, 19 states have enacted legislation or passed resolutions in the last several years to provide for year-round DST, if Congress were to allow such a change. And according to a Congressional Research Service (CRS) report on DST updated in September 2020, at least 45 states have, since 2015, proposed legislation to change their observance of DST.
These efforts include proposals to exempt a state from DST observance, which is allowable under existing law, and proposals that would establish permanent DST, which would require Congress to amend the Uniform Time Act of 1966, the CRS report says.
The state of the science
Shifting from ST to DST has been associated with an increase in cardiovascular morbidity (heart attacks and atrial fibrillation), increased missed medical appointments, increased ED visits, increased mood disturbances and suicide risk, increased risk of fatal car crashes and medical errors – and sleep loss, said Elizabeth Klerman, MD, PhD, professor of neurology in the division of sleep medicine at Harvard Medical School, Boston.
These associations are covered in AASM statement, along with acknowledgment that most studies on the chronic effects of DST have “either been retrospective or addressed the issue indirectly.”
For Dr. Johnson, who refers to DST as “sleep deprivation time,” the most convincing data regarding the dangers of permanent DST come from studies comparing locations within time zones. “The farther you’re off from the meridian, the more you have that ‘social jet lag’ or circadian misalignment [between the innate circadian rhythm, which is synchronized with solar time, and school or work schedules],” she said at the meeting.
Researchers reported in 2017, for instance, that the risk for all cancers and many specific cancers increased from east to west within a time zone, as solar time is progressively delayed. “They documented changes in risk for every 5 degrees west from the meridian,” she said.
Dr. Johnson is a case in point of the “educational gap” that she believes needs attention. Two years ago, as chair of the sleep section of the American Academy of Neurology, she delved into the literature after the AAN asked the section whether it should endorse the AASM’s position paper on DST. “I didn’t know the literature even as a sleep scientist until I got into this,” she said.
“If you’re asked me 2 years ago,” she added in the later interview, “I would have said that permanent DST is fine.”
The sleep section recommended that the AAN endorse permanent ST, but the AAN ultimately decided it “didn’t feel strongly enough to say that standard time is unequivocally the better option,” Dr. Johnson said in an interview. “They agreed that there’s science [in favor of it], but ... it’s a big public policy decision.”
Jamie Zeitzer, PhD, associate professor of psychiatry and behavioral sciences at Stanford (Calif.) University’s Center for Sleep Sciences and Medicine, voiced similar concerns at the meeting about currently advocating a shift in either direction. It’s “absolutely clear that switching clocks, especially since it’s occurring at a population level, is deleterious and we need to get rid of it,” he said. “But before we put forth dictates on public health [with a shift to permanent ST], I think we better be sure we’re correct.”
“I think we’re getting close. I think the data thus far [are indicating] that permanent standard time is better for health,” Dr. Zeitzer said. “But I don’t think there’s a cumulative amount of evidence to really say that we have to subvert all other interests because this is so important for public health. We need at least a few more studies.”
There is not enough evidence, for instance, to conclude that the body clock does not eventually adjust to DST, he said, and it is not yet clear what roles electric light and sunlight each play in the body’s circadian time.
“And we need to think about north-south. What may be important for the upper Midwest, and for Maine, and for Washington, may not be ... good for Florida and Texas and southern California,” Dr. Zeitzer said. “You have very different patterns of light exposure, especially when it deals with seasons.”
Historical considerations
In his comments at the meeting, Muhammad Rishi, MBBS, the lead author of the AASM’s position statement, added that circadian misalignment – that “asynchrony between the internal and external clocks” – is associated in studies with an increased risk of obesity, metabolic syndrome, and depression.
But he also emphasized that the “historical evidence” against permanent DST is at least as strong as the medical evidence.
“The U.S. has gone on permanent daylight savings time several times in the past, most recently in the 1970s during the OPEC [oil embargo], and it was so unpopular,” said Dr. Rishi, of the department of pulmonology, critical care and sleep medicine at the Mayo Clinic Health System in Eau Claire, Wis. “England also did it in the 1960s and then abolished it, and most recently Russia did it ... it became so unpopular with increased depression and mood disorders that they abolished it.”
Rep. Ward said that China has offered a large natural experiment with its move decades ago from five time zones to one time zone – Beijing time. “I don’t think we’ve seen any sweeping changes in their health because they have one large time zone,” he said.
Dr. Klerman took issue, saying she “knows someone in China who is trying to get that data about health outcomes and is unable to get it.”
Arguments that DST saves energy hold little to no weight upon scrutiny of the data, Dr. Johnson said. Moreover, research other than oft-cited, older Department of Transportation studies suggests that “permanent DST is bad for energy and bad for the climate,” she said. “This really needs to be more fully evaluated by the government and others.”
Dr. Johnson said after the meeting that it’s important for experts from the energy and climate sectors, education, and medicine – including pediatrics, oncology, and other specialties with “a stake in this” – to come together and share information so “we won’t all be in our silos.” She and other sleep experts in the neurology field are planning to host a summit in 2022 to do just this.
Dr. Johnson and Kin Yuen, MD, of the Sleep Disorders Center at the University of California, San Francisco, both expressed concern at the meeting that adoption of permanent DST would negate the benefits of delayed school start times in middle and high school students.
There is some evidence that delayed start times have led to decreased tardiness and absences, Dr. Yuen said. To have the same impact with permanent DST, “instead of starting at 8:30 a.m., you’d have to start at 9:30,” Dr. Johnson added after the meeting.
The first discussion of DST at the SLEEP 2021 meeting was led by Erin E. Flynn-Evans, PhD, MPH, director of the Fatigue Countermeasures Laboratory at the National Aeronautics and Space Administration Ames Research Center. Dr. Yuen led a later second question-and-answer session. They and each of the eight participants reported that they had no relevant conflicts of interest.
Dr. Yuen and Dr. Flynn-Evans are both coauthors of the AASM’s position statement on DST. Dr. Klerman is a coauthor of the Society for Research on Biological Rhythms 2019 position paper on DST.
The AASM’s statement has been endorsed by 19 organizations, including the American College of Chest Physicians, the SRBR, the American Academy of Cardiovascular Sleep Medicine, the Society of Behavioral Sleep Medicine, the National PTA, and the American College of Occupational and Environmental Medicine.
FROM SLEEP 2021
Updates on COVID-19 guidance for sleep medicine
Background
Well into its second year, the worldwide COVID-19 pandemic continues to pose substantial challenges for health care access and delivery. Regulatory agencies such as the Centers for Disease Control (CDC) do not currently have guidance related to COVID-19 specific to sleep centers and laboratories. In March 2020, within days of the World Health Organization pandemic declaration, the American Academy of Sleep Medicine (AASM) posted detailed guidance on mitigation strategies for sleep medicine practices (COVID-19 Resources).
This initial guidance has been previously reported in this publication (Sullivan S, Gurubhagavatula I. CHEST Physician 2020 May 8), and the guidance has been periodically updated during the pandemic. It was restructured in mid-2020 to include sections summarizing CDC recommendations germane for sleep practices; additional sleep medicine-specific guidance from the AASM COVID-19 Task Force (TF); and a frequently asked questions (FAQ) section. The last major update from the task force occurred on Jan. 18, 2021, though subsequent posts – especially related to recent CDC changes in masking guidelines – were made in May 2021. The purpose of this article is to summarize these updates and to call attention to areas of ongoing interest to sleep medicine. Notably, the AASM Task Force guidance is nonbinding and offered as a framework for considering best practices in this evolving situation, acknowledging the importance of weighing local factors, conditions, and regulations, as well as the interests of and risks to the patient, staff, and providers.
Key updates
Data on exposure and transmission risks specific to sleep medicine
Measures for reducing viral transmission have been central to managing the spread of the virus in clinical settings. In its last major update, the AASM TF noted that no known outbreaks of COVID-19 related to sleep center exposure have been reported. A perspective and data published in the Journal of the American Medical Association concluded that hospital transmission of the virus “in the setting of universal masking is likely rare, even during periods of high community prevalence.” It also concluded that hospital-based outbreaks are more likely to occur in small workrooms and during mealtime when staff are less adherent to masking and physical distancing (Richterman A, et al. JAMA. 2020;324[21]:2155-6). The TF elaborated on considerations to reduce transmission, which include not just telework and foundational infection control practices, but also broader workplace considerations such as optimizing ventilation, taking advantage of outdoor spaces (e.g., for breaks and eating), scheduling to reduce interactions between personnel from different teams, minimizing contact in meeting/break rooms, removing tables and chairs from lounge areas, and following CDC guidance for effective facility operations.
Vaccination
In the January update, the AASM COVID-19 TF stated that, “sleep facility leaders should encourage staff and patients to be vaccinated in accordance with CDC guidance.” The role of the sleep medicine community in encouraging healthy sleep habits before and after vaccination was emphasized, pointing to evidence linking sleep and immunity, specifically between sleep duration and vaccination response (Healthy sleep and immune response to COVID-19 vaccination. 2021 Jan.).
In an FAQ update from March 26, 2021, considering whether continued COVID-19 testing was needed following full vaccination, the AASM advised testing prior to potential aerosol-generating procedures should be made on the basis of a risk-benefit assessment by the sleep clinician. Several considerations were highlighted, including recent COVID-19 infection, vaccination status of contacts, local prevalence of newer variants, and whether individuals are receiving positive airway pressure therapy. The TF focused on the vigilance for residents and staff in long-term care facilities, which have been associated with a number of outbreaks.
Masking in the context of the COVID-19 vaccine
The most significant change in recommendations is the recent relaxation of masking guidance by the CDC in the setting of the approval and distribution of COVID-19 vaccinations. In May, the CDC stated that fully vaccinated individuals can resume activities without masking or physically distancing except in scenarios of travel and where required by laws, regulations, and local businesses, due to the efficacy of the vaccines, increasing evidence of reduced asymptomatic carriage and transmission after vaccination, and anticipated increased uptake of vaccination. However, the CDC also noted that these updates did not apply to health care facilities, where the recommendation remains that patients and visitors should continue to mask throughout their stay. Additionally, fully vaccinated health care workers should continue to practice infection control measures while working with patients. On May 14, the AASM TF provided a detailed FAQ acknowledging the CDC’s new guidance, emphasizing that masking guidance in health care facilities remains unchanged, and encouraging individuals to follow CDC guidance regarding vaccination, noting that emergence of newer variants continues to be monitored, and existing vaccines still appear to induce neutralizing antibodies even if to a somewhat lower degree. The situation for pediatric sleep centers has been highlighted in particular because the potential risk posed by newer variants to children remains under investigation, and children under age 12 are not approved for vaccination.
Important caveats to discussions around vaccination status are the lack of a centralized method to identify vaccinated individuals, the unknown duration of immunity, and reports of the use of fake vaccine cards. At this time, in health care settings, vaccination status should not exempt mask usage for any individual.
Sleep medicine care for those with COVID-19
Regarding the duration of isolation and precautions for adults with COVID-19, the TF highlighted the CDC’s symptom-based strategy, rather than test-based strategy, for ending isolation of these patients, availing them of sleep medicine services in person.
In line with the CDC guidance, this approach indicates that scheduling in-person care such as polysomnography for a COVID-19–positive patient may be appropriate at least 10 days after symptom onset (or after a positive test if the patient never developed symptoms); or at least 20 days after symptom onset if the illness was severe; or if at least 90 days have elapsed since symptom onset, consider preappointment COVID-19 screening. In the context of immunocompromised individuals, involvement from infectious disease specialists may be needed to help guide decisions.
Patient communications
For many, a repercussion of the pandemic has been delaying care or avoiding addressing medical issues, including sleep disorders. The AASM encouraged practices to consider communicating with patients that delaying needed care can increase health risks; COVID-19 transmission to patients in health care settings has been low; effective safety procedures are in place; and whether remote/telehealth services are available.
Disparities in care
In addition to the specific guidance above, there are ongoing concerns regarding disparities in care resulting from a variety of sources and becoming more evident during the pandemic. Complex factors, ranging from economic, geographic, contextual, occupational, and others contribute to disparities that health care systems – and sleep medicine - have not been able to adequately address (Jackson CL and Johnson DA. J Clin Sleep Med. 16[8]:1401-2). More specific differences may include Internet access, reduced access due to socioeconomic barriers, transportation limitations, medical mistrust, and membership in a medically vulnerable group such as children, the elderly, and those with high acuity needs. For example, in pediatric patients there exist few evidence-based alternatives and guidelines to in-lab testing and care, which may have negatively impacted access to needed sleep medicine services (Sullivan S et al. J Clin Sleep Med. 2021 Mar 1;17[3]:361-2).
Economics in the COVID-19 pandemic
The economic effects of COVID-19 on medical institutions and in sleep medicine is a story that continues to unfold. Reductions in patient visits and elective procedures, infection control measures limiting capacity, increased costs to maintain such measures, and variability of responses by payer and region are just a few of the issues. The Centers for Medicare & Medicaid Services has employed waivers to increased flexibility and promote safe and effective care including the use of telemedicine during the public health emergency, but the future of these waivers remains uncertain. Alarmingly, a sizeable portion of sleep practices reported financial solvency concerns related to the pandemic (Ramar K. J Clin Sleep Med. 2020;16[11]:1939-42).
Conclusion
As the COVID-19 pandemic and related public health guidance continues to evolve, sleep medicine practices continue to adapt. Vaccination, new variants, changes in mask guidance, new outbreaks around the globe, financial and staffing uncertainties, as well as addressing disparities in care and outcomes that may be augmented by the pandemic remain salient areas of ongoing development.
Dr. Lee is a Postdoctoral and Pediatric Pulmonary Fellow, Department of Pediatrics, Division of Pulmonary, Asthma, and Sleep Medicine, Stanford University School of Medicine; Dr. Sullivan is Clinical Professor, Department of Pediatrics, Division of Pulmonary, Asthma, and Sleep Medicine, and by courtesy, Division of Sleep Medicine, Department of Psychiatry, Stanford University School of Medicine, Palo Alto, CA.
Background
Well into its second year, the worldwide COVID-19 pandemic continues to pose substantial challenges for health care access and delivery. Regulatory agencies such as the Centers for Disease Control (CDC) do not currently have guidance related to COVID-19 specific to sleep centers and laboratories. In March 2020, within days of the World Health Organization pandemic declaration, the American Academy of Sleep Medicine (AASM) posted detailed guidance on mitigation strategies for sleep medicine practices (COVID-19 Resources).
This initial guidance has been previously reported in this publication (Sullivan S, Gurubhagavatula I. CHEST Physician 2020 May 8), and the guidance has been periodically updated during the pandemic. It was restructured in mid-2020 to include sections summarizing CDC recommendations germane for sleep practices; additional sleep medicine-specific guidance from the AASM COVID-19 Task Force (TF); and a frequently asked questions (FAQ) section. The last major update from the task force occurred on Jan. 18, 2021, though subsequent posts – especially related to recent CDC changes in masking guidelines – were made in May 2021. The purpose of this article is to summarize these updates and to call attention to areas of ongoing interest to sleep medicine. Notably, the AASM Task Force guidance is nonbinding and offered as a framework for considering best practices in this evolving situation, acknowledging the importance of weighing local factors, conditions, and regulations, as well as the interests of and risks to the patient, staff, and providers.
Key updates
Data on exposure and transmission risks specific to sleep medicine
Measures for reducing viral transmission have been central to managing the spread of the virus in clinical settings. In its last major update, the AASM TF noted that no known outbreaks of COVID-19 related to sleep center exposure have been reported. A perspective and data published in the Journal of the American Medical Association concluded that hospital transmission of the virus “in the setting of universal masking is likely rare, even during periods of high community prevalence.” It also concluded that hospital-based outbreaks are more likely to occur in small workrooms and during mealtime when staff are less adherent to masking and physical distancing (Richterman A, et al. JAMA. 2020;324[21]:2155-6). The TF elaborated on considerations to reduce transmission, which include not just telework and foundational infection control practices, but also broader workplace considerations such as optimizing ventilation, taking advantage of outdoor spaces (e.g., for breaks and eating), scheduling to reduce interactions between personnel from different teams, minimizing contact in meeting/break rooms, removing tables and chairs from lounge areas, and following CDC guidance for effective facility operations.
Vaccination
In the January update, the AASM COVID-19 TF stated that, “sleep facility leaders should encourage staff and patients to be vaccinated in accordance with CDC guidance.” The role of the sleep medicine community in encouraging healthy sleep habits before and after vaccination was emphasized, pointing to evidence linking sleep and immunity, specifically between sleep duration and vaccination response (Healthy sleep and immune response to COVID-19 vaccination. 2021 Jan.).
In an FAQ update from March 26, 2021, considering whether continued COVID-19 testing was needed following full vaccination, the AASM advised testing prior to potential aerosol-generating procedures should be made on the basis of a risk-benefit assessment by the sleep clinician. Several considerations were highlighted, including recent COVID-19 infection, vaccination status of contacts, local prevalence of newer variants, and whether individuals are receiving positive airway pressure therapy. The TF focused on the vigilance for residents and staff in long-term care facilities, which have been associated with a number of outbreaks.
Masking in the context of the COVID-19 vaccine
The most significant change in recommendations is the recent relaxation of masking guidance by the CDC in the setting of the approval and distribution of COVID-19 vaccinations. In May, the CDC stated that fully vaccinated individuals can resume activities without masking or physically distancing except in scenarios of travel and where required by laws, regulations, and local businesses, due to the efficacy of the vaccines, increasing evidence of reduced asymptomatic carriage and transmission after vaccination, and anticipated increased uptake of vaccination. However, the CDC also noted that these updates did not apply to health care facilities, where the recommendation remains that patients and visitors should continue to mask throughout their stay. Additionally, fully vaccinated health care workers should continue to practice infection control measures while working with patients. On May 14, the AASM TF provided a detailed FAQ acknowledging the CDC’s new guidance, emphasizing that masking guidance in health care facilities remains unchanged, and encouraging individuals to follow CDC guidance regarding vaccination, noting that emergence of newer variants continues to be monitored, and existing vaccines still appear to induce neutralizing antibodies even if to a somewhat lower degree. The situation for pediatric sleep centers has been highlighted in particular because the potential risk posed by newer variants to children remains under investigation, and children under age 12 are not approved for vaccination.
Important caveats to discussions around vaccination status are the lack of a centralized method to identify vaccinated individuals, the unknown duration of immunity, and reports of the use of fake vaccine cards. At this time, in health care settings, vaccination status should not exempt mask usage for any individual.
Sleep medicine care for those with COVID-19
Regarding the duration of isolation and precautions for adults with COVID-19, the TF highlighted the CDC’s symptom-based strategy, rather than test-based strategy, for ending isolation of these patients, availing them of sleep medicine services in person.
In line with the CDC guidance, this approach indicates that scheduling in-person care such as polysomnography for a COVID-19–positive patient may be appropriate at least 10 days after symptom onset (or after a positive test if the patient never developed symptoms); or at least 20 days after symptom onset if the illness was severe; or if at least 90 days have elapsed since symptom onset, consider preappointment COVID-19 screening. In the context of immunocompromised individuals, involvement from infectious disease specialists may be needed to help guide decisions.
Patient communications
For many, a repercussion of the pandemic has been delaying care or avoiding addressing medical issues, including sleep disorders. The AASM encouraged practices to consider communicating with patients that delaying needed care can increase health risks; COVID-19 transmission to patients in health care settings has been low; effective safety procedures are in place; and whether remote/telehealth services are available.
Disparities in care
In addition to the specific guidance above, there are ongoing concerns regarding disparities in care resulting from a variety of sources and becoming more evident during the pandemic. Complex factors, ranging from economic, geographic, contextual, occupational, and others contribute to disparities that health care systems – and sleep medicine - have not been able to adequately address (Jackson CL and Johnson DA. J Clin Sleep Med. 16[8]:1401-2). More specific differences may include Internet access, reduced access due to socioeconomic barriers, transportation limitations, medical mistrust, and membership in a medically vulnerable group such as children, the elderly, and those with high acuity needs. For example, in pediatric patients there exist few evidence-based alternatives and guidelines to in-lab testing and care, which may have negatively impacted access to needed sleep medicine services (Sullivan S et al. J Clin Sleep Med. 2021 Mar 1;17[3]:361-2).
Economics in the COVID-19 pandemic
The economic effects of COVID-19 on medical institutions and in sleep medicine is a story that continues to unfold. Reductions in patient visits and elective procedures, infection control measures limiting capacity, increased costs to maintain such measures, and variability of responses by payer and region are just a few of the issues. The Centers for Medicare & Medicaid Services has employed waivers to increased flexibility and promote safe and effective care including the use of telemedicine during the public health emergency, but the future of these waivers remains uncertain. Alarmingly, a sizeable portion of sleep practices reported financial solvency concerns related to the pandemic (Ramar K. J Clin Sleep Med. 2020;16[11]:1939-42).
Conclusion
As the COVID-19 pandemic and related public health guidance continues to evolve, sleep medicine practices continue to adapt. Vaccination, new variants, changes in mask guidance, new outbreaks around the globe, financial and staffing uncertainties, as well as addressing disparities in care and outcomes that may be augmented by the pandemic remain salient areas of ongoing development.
Dr. Lee is a Postdoctoral and Pediatric Pulmonary Fellow, Department of Pediatrics, Division of Pulmonary, Asthma, and Sleep Medicine, Stanford University School of Medicine; Dr. Sullivan is Clinical Professor, Department of Pediatrics, Division of Pulmonary, Asthma, and Sleep Medicine, and by courtesy, Division of Sleep Medicine, Department of Psychiatry, Stanford University School of Medicine, Palo Alto, CA.
Background
Well into its second year, the worldwide COVID-19 pandemic continues to pose substantial challenges for health care access and delivery. Regulatory agencies such as the Centers for Disease Control (CDC) do not currently have guidance related to COVID-19 specific to sleep centers and laboratories. In March 2020, within days of the World Health Organization pandemic declaration, the American Academy of Sleep Medicine (AASM) posted detailed guidance on mitigation strategies for sleep medicine practices (COVID-19 Resources).
This initial guidance has been previously reported in this publication (Sullivan S, Gurubhagavatula I. CHEST Physician 2020 May 8), and the guidance has been periodically updated during the pandemic. It was restructured in mid-2020 to include sections summarizing CDC recommendations germane for sleep practices; additional sleep medicine-specific guidance from the AASM COVID-19 Task Force (TF); and a frequently asked questions (FAQ) section. The last major update from the task force occurred on Jan. 18, 2021, though subsequent posts – especially related to recent CDC changes in masking guidelines – were made in May 2021. The purpose of this article is to summarize these updates and to call attention to areas of ongoing interest to sleep medicine. Notably, the AASM Task Force guidance is nonbinding and offered as a framework for considering best practices in this evolving situation, acknowledging the importance of weighing local factors, conditions, and regulations, as well as the interests of and risks to the patient, staff, and providers.
Key updates
Data on exposure and transmission risks specific to sleep medicine
Measures for reducing viral transmission have been central to managing the spread of the virus in clinical settings. In its last major update, the AASM TF noted that no known outbreaks of COVID-19 related to sleep center exposure have been reported. A perspective and data published in the Journal of the American Medical Association concluded that hospital transmission of the virus “in the setting of universal masking is likely rare, even during periods of high community prevalence.” It also concluded that hospital-based outbreaks are more likely to occur in small workrooms and during mealtime when staff are less adherent to masking and physical distancing (Richterman A, et al. JAMA. 2020;324[21]:2155-6). The TF elaborated on considerations to reduce transmission, which include not just telework and foundational infection control practices, but also broader workplace considerations such as optimizing ventilation, taking advantage of outdoor spaces (e.g., for breaks and eating), scheduling to reduce interactions between personnel from different teams, minimizing contact in meeting/break rooms, removing tables and chairs from lounge areas, and following CDC guidance for effective facility operations.
Vaccination
In the January update, the AASM COVID-19 TF stated that, “sleep facility leaders should encourage staff and patients to be vaccinated in accordance with CDC guidance.” The role of the sleep medicine community in encouraging healthy sleep habits before and after vaccination was emphasized, pointing to evidence linking sleep and immunity, specifically between sleep duration and vaccination response (Healthy sleep and immune response to COVID-19 vaccination. 2021 Jan.).
In an FAQ update from March 26, 2021, considering whether continued COVID-19 testing was needed following full vaccination, the AASM advised testing prior to potential aerosol-generating procedures should be made on the basis of a risk-benefit assessment by the sleep clinician. Several considerations were highlighted, including recent COVID-19 infection, vaccination status of contacts, local prevalence of newer variants, and whether individuals are receiving positive airway pressure therapy. The TF focused on the vigilance for residents and staff in long-term care facilities, which have been associated with a number of outbreaks.
Masking in the context of the COVID-19 vaccine
The most significant change in recommendations is the recent relaxation of masking guidance by the CDC in the setting of the approval and distribution of COVID-19 vaccinations. In May, the CDC stated that fully vaccinated individuals can resume activities without masking or physically distancing except in scenarios of travel and where required by laws, regulations, and local businesses, due to the efficacy of the vaccines, increasing evidence of reduced asymptomatic carriage and transmission after vaccination, and anticipated increased uptake of vaccination. However, the CDC also noted that these updates did not apply to health care facilities, where the recommendation remains that patients and visitors should continue to mask throughout their stay. Additionally, fully vaccinated health care workers should continue to practice infection control measures while working with patients. On May 14, the AASM TF provided a detailed FAQ acknowledging the CDC’s new guidance, emphasizing that masking guidance in health care facilities remains unchanged, and encouraging individuals to follow CDC guidance regarding vaccination, noting that emergence of newer variants continues to be monitored, and existing vaccines still appear to induce neutralizing antibodies even if to a somewhat lower degree. The situation for pediatric sleep centers has been highlighted in particular because the potential risk posed by newer variants to children remains under investigation, and children under age 12 are not approved for vaccination.
Important caveats to discussions around vaccination status are the lack of a centralized method to identify vaccinated individuals, the unknown duration of immunity, and reports of the use of fake vaccine cards. At this time, in health care settings, vaccination status should not exempt mask usage for any individual.
Sleep medicine care for those with COVID-19
Regarding the duration of isolation and precautions for adults with COVID-19, the TF highlighted the CDC’s symptom-based strategy, rather than test-based strategy, for ending isolation of these patients, availing them of sleep medicine services in person.
In line with the CDC guidance, this approach indicates that scheduling in-person care such as polysomnography for a COVID-19–positive patient may be appropriate at least 10 days after symptom onset (or after a positive test if the patient never developed symptoms); or at least 20 days after symptom onset if the illness was severe; or if at least 90 days have elapsed since symptom onset, consider preappointment COVID-19 screening. In the context of immunocompromised individuals, involvement from infectious disease specialists may be needed to help guide decisions.
Patient communications
For many, a repercussion of the pandemic has been delaying care or avoiding addressing medical issues, including sleep disorders. The AASM encouraged practices to consider communicating with patients that delaying needed care can increase health risks; COVID-19 transmission to patients in health care settings has been low; effective safety procedures are in place; and whether remote/telehealth services are available.
Disparities in care
In addition to the specific guidance above, there are ongoing concerns regarding disparities in care resulting from a variety of sources and becoming more evident during the pandemic. Complex factors, ranging from economic, geographic, contextual, occupational, and others contribute to disparities that health care systems – and sleep medicine - have not been able to adequately address (Jackson CL and Johnson DA. J Clin Sleep Med. 16[8]:1401-2). More specific differences may include Internet access, reduced access due to socioeconomic barriers, transportation limitations, medical mistrust, and membership in a medically vulnerable group such as children, the elderly, and those with high acuity needs. For example, in pediatric patients there exist few evidence-based alternatives and guidelines to in-lab testing and care, which may have negatively impacted access to needed sleep medicine services (Sullivan S et al. J Clin Sleep Med. 2021 Mar 1;17[3]:361-2).
Economics in the COVID-19 pandemic
The economic effects of COVID-19 on medical institutions and in sleep medicine is a story that continues to unfold. Reductions in patient visits and elective procedures, infection control measures limiting capacity, increased costs to maintain such measures, and variability of responses by payer and region are just a few of the issues. The Centers for Medicare & Medicaid Services has employed waivers to increased flexibility and promote safe and effective care including the use of telemedicine during the public health emergency, but the future of these waivers remains uncertain. Alarmingly, a sizeable portion of sleep practices reported financial solvency concerns related to the pandemic (Ramar K. J Clin Sleep Med. 2020;16[11]:1939-42).
Conclusion
As the COVID-19 pandemic and related public health guidance continues to evolve, sleep medicine practices continue to adapt. Vaccination, new variants, changes in mask guidance, new outbreaks around the globe, financial and staffing uncertainties, as well as addressing disparities in care and outcomes that may be augmented by the pandemic remain salient areas of ongoing development.
Dr. Lee is a Postdoctoral and Pediatric Pulmonary Fellow, Department of Pediatrics, Division of Pulmonary, Asthma, and Sleep Medicine, Stanford University School of Medicine; Dr. Sullivan is Clinical Professor, Department of Pediatrics, Division of Pulmonary, Asthma, and Sleep Medicine, and by courtesy, Division of Sleep Medicine, Department of Psychiatry, Stanford University School of Medicine, Palo Alto, CA.