User login
Pandemic adds more weight to burden of obesity in children
according to a new report from the Robert Wood Johnson Foundation.
“Our nation’s safety net is fragile, outdated, and out of reach for millions of eligible kids and caregivers,” said Jamie Bussel, senior program officer at the RWJF, and senior author of the report. She added that the pandemic further fractured an already broken system that disproportionately overlooks “children of color and those who live farthest from economic opportunity”.
It’s time to think ‘bigger and better’
Ms. Bussel said, during a press conference, that congress responded to the pandemic with “an array of policy solutions,” but it’s now time to think ‘bigger and better.’
“There have been huge flexibilities deployed across the safety net program and these have been really important reliefs, but the fact is many of them are temporary emergency relief measures,” she explained.
For the past 3 years, the RWJF’s annual State of Childhood Obesity report has drawn national and state obesity data from large surveys including the National Survey of Children’s Health, the Youth Risk Behavior Surveillance System, the WIC Participant and Program Characteristics Survey, and the National Health and Nutrition Examination Survey.
Similar to in past years, this year’s data show that rates of obesity and overweight have remained relatively steady and have been highest among minority and low-income populations. For example, data from the 2019-2020 National Survey of Children’s Health, along with an analysis conducted by the Health Resources and Services Administration’s Maternal and Child Health Bureau, show that one in six – or 16.2% – of youth aged 10-17 years have obesity.
While non-Hispanic Asian children had the lowest obesity rate (8.1%), followed by non-Hispanic White children (12.1%), rates were significantly higher for Hispanic (21.4%), non-Hispanic Black (23.8%), and non-Hispanic American Indian/Alaska Native (28.7%) children, according to the report.
“Additional years of data are needed to assess whether obesity rates changed after the onset of the pandemic,” explained Ms. Bussel.
Digging deeper
Other studies included in this year’s report were specifically designed to measure the impact of the pandemic, and show a distinct rise in overweight and obesity, especially in younger children. For example, a retrospective cohort study using data from Kaiser Permanente Southern California showed the rate of overweight and obesity in children aged 5-11 years rose to 45.7% between March 2020 and January 2021, up from 36.2% before the pandemic.
Another of these studies, which was based on national electronic health records of more than 430,000 children, showed the obesity rate crept from 19.3% to 22.4% between August 2019 and August 2020.
“The lid we had been trying desperately to put on the obesity epidemic has come off again,” said Sandra G Hassink, MD, MSc, who is medical director of the American Academy of Pediatrics Institute for Healthy Childhood Weight.
“In the absence of COVID we had been seeing slow upticks in the numbers – and in some groups we’d been thinking maybe we were headed toward stabilization – but these numbers blow that out of the water ... COVID has escalated the rates,” she said in an interview.
“Unfortunately, these two crises – the COVID pandemic, the childhood obesity epidemic – in so many ways have exacerbated one another,” said Ms. Bussel. “It’s not a huge surprise that we’re seeing an increase in childhood obesity rates given the complete and utter disruption of every single system that circumscribes our lives.”
The systems that feed obesity
Addressing childhood obesity requires targeting far beyond healthy eating and physical activity, Ms. Bussel said.
“As important is whether that child has a safe place to call home. Does mom or dad or their care provider have a stable income? Is there reliable transportation? Is their access to health insurance? Is there access to high-quality health care? ... All of those factors influence the child and the family’s opportunities to live well, be healthy, and be at a healthy weight,” she noted.
The report includes a list of five main policy recommendations.
- Making free, universal school meal programs permanent.
- Extending eligibility for WIC, the Special Supplemental Nutrition Program for Women, Infants, and Children, to postpartum mothers and to children through age 6.
- Extending and expanding other programs, such as the Child Tax Credit.
- Closing the Medicaid coverage gap.
- Developing a consistent approach to collecting obesity data organized by race, ethnicity, and income level.
“Collectively, over at least the course of the last generation or two, our policy approach to obesity prevention has not been sufficient. But that doesn’t mean all of our policy approaches have been failures,” Ms. Bussel said during an interview. “Policy change does not always need to be dramatic to have a real impact on families.”
Fighting complacency
For Dr. Hassink, one of the barriers to change is society’s level of acceptance. She said an identifiable explanation for pandemic weight gain doesn’t mean society should simply shrug it off.
“If we regarded childhood obesity as the population level catastrophe that it is for chronic disease maybe people would be activated around these policy changes,” she said.
“We’re accepting a disease process that wreaks havoc on people,” noted Dr. Hassink, who was not involved in the new report. “I think it’s hard for people to realize the magnitude of the disease burden that we’re seeing. If you’re in a weight management clinic or any pediatrician’s office you would see it – you would see kids coming in with liver disease, 9-year-olds on [continuous positive airway pressure] for sleep apnea, kids needing their hips pinned because they had a hip fracture because of obesity.
“So, those of us that see the disease burden see what’s behind those numbers. The sadness of what we’re talking about is we know a lot about what could push the dial and help reduce this epidemic and we’re not doing what we already know,” added Dr. Hassink.
Ms. Bussel and Dr. Hassink reported no conflicts.
according to a new report from the Robert Wood Johnson Foundation.
“Our nation’s safety net is fragile, outdated, and out of reach for millions of eligible kids and caregivers,” said Jamie Bussel, senior program officer at the RWJF, and senior author of the report. She added that the pandemic further fractured an already broken system that disproportionately overlooks “children of color and those who live farthest from economic opportunity”.
It’s time to think ‘bigger and better’
Ms. Bussel said, during a press conference, that congress responded to the pandemic with “an array of policy solutions,” but it’s now time to think ‘bigger and better.’
“There have been huge flexibilities deployed across the safety net program and these have been really important reliefs, but the fact is many of them are temporary emergency relief measures,” she explained.
For the past 3 years, the RWJF’s annual State of Childhood Obesity report has drawn national and state obesity data from large surveys including the National Survey of Children’s Health, the Youth Risk Behavior Surveillance System, the WIC Participant and Program Characteristics Survey, and the National Health and Nutrition Examination Survey.
Similar to in past years, this year’s data show that rates of obesity and overweight have remained relatively steady and have been highest among minority and low-income populations. For example, data from the 2019-2020 National Survey of Children’s Health, along with an analysis conducted by the Health Resources and Services Administration’s Maternal and Child Health Bureau, show that one in six – or 16.2% – of youth aged 10-17 years have obesity.
While non-Hispanic Asian children had the lowest obesity rate (8.1%), followed by non-Hispanic White children (12.1%), rates were significantly higher for Hispanic (21.4%), non-Hispanic Black (23.8%), and non-Hispanic American Indian/Alaska Native (28.7%) children, according to the report.
“Additional years of data are needed to assess whether obesity rates changed after the onset of the pandemic,” explained Ms. Bussel.
Digging deeper
Other studies included in this year’s report were specifically designed to measure the impact of the pandemic, and show a distinct rise in overweight and obesity, especially in younger children. For example, a retrospective cohort study using data from Kaiser Permanente Southern California showed the rate of overweight and obesity in children aged 5-11 years rose to 45.7% between March 2020 and January 2021, up from 36.2% before the pandemic.
Another of these studies, which was based on national electronic health records of more than 430,000 children, showed the obesity rate crept from 19.3% to 22.4% between August 2019 and August 2020.
“The lid we had been trying desperately to put on the obesity epidemic has come off again,” said Sandra G Hassink, MD, MSc, who is medical director of the American Academy of Pediatrics Institute for Healthy Childhood Weight.
“In the absence of COVID we had been seeing slow upticks in the numbers – and in some groups we’d been thinking maybe we were headed toward stabilization – but these numbers blow that out of the water ... COVID has escalated the rates,” she said in an interview.
“Unfortunately, these two crises – the COVID pandemic, the childhood obesity epidemic – in so many ways have exacerbated one another,” said Ms. Bussel. “It’s not a huge surprise that we’re seeing an increase in childhood obesity rates given the complete and utter disruption of every single system that circumscribes our lives.”
The systems that feed obesity
Addressing childhood obesity requires targeting far beyond healthy eating and physical activity, Ms. Bussel said.
“As important is whether that child has a safe place to call home. Does mom or dad or their care provider have a stable income? Is there reliable transportation? Is their access to health insurance? Is there access to high-quality health care? ... All of those factors influence the child and the family’s opportunities to live well, be healthy, and be at a healthy weight,” she noted.
The report includes a list of five main policy recommendations.
- Making free, universal school meal programs permanent.
- Extending eligibility for WIC, the Special Supplemental Nutrition Program for Women, Infants, and Children, to postpartum mothers and to children through age 6.
- Extending and expanding other programs, such as the Child Tax Credit.
- Closing the Medicaid coverage gap.
- Developing a consistent approach to collecting obesity data organized by race, ethnicity, and income level.
“Collectively, over at least the course of the last generation or two, our policy approach to obesity prevention has not been sufficient. But that doesn’t mean all of our policy approaches have been failures,” Ms. Bussel said during an interview. “Policy change does not always need to be dramatic to have a real impact on families.”
Fighting complacency
For Dr. Hassink, one of the barriers to change is society’s level of acceptance. She said an identifiable explanation for pandemic weight gain doesn’t mean society should simply shrug it off.
“If we regarded childhood obesity as the population level catastrophe that it is for chronic disease maybe people would be activated around these policy changes,” she said.
“We’re accepting a disease process that wreaks havoc on people,” noted Dr. Hassink, who was not involved in the new report. “I think it’s hard for people to realize the magnitude of the disease burden that we’re seeing. If you’re in a weight management clinic or any pediatrician’s office you would see it – you would see kids coming in with liver disease, 9-year-olds on [continuous positive airway pressure] for sleep apnea, kids needing their hips pinned because they had a hip fracture because of obesity.
“So, those of us that see the disease burden see what’s behind those numbers. The sadness of what we’re talking about is we know a lot about what could push the dial and help reduce this epidemic and we’re not doing what we already know,” added Dr. Hassink.
Ms. Bussel and Dr. Hassink reported no conflicts.
according to a new report from the Robert Wood Johnson Foundation.
“Our nation’s safety net is fragile, outdated, and out of reach for millions of eligible kids and caregivers,” said Jamie Bussel, senior program officer at the RWJF, and senior author of the report. She added that the pandemic further fractured an already broken system that disproportionately overlooks “children of color and those who live farthest from economic opportunity”.
It’s time to think ‘bigger and better’
Ms. Bussel said, during a press conference, that congress responded to the pandemic with “an array of policy solutions,” but it’s now time to think ‘bigger and better.’
“There have been huge flexibilities deployed across the safety net program and these have been really important reliefs, but the fact is many of them are temporary emergency relief measures,” she explained.
For the past 3 years, the RWJF’s annual State of Childhood Obesity report has drawn national and state obesity data from large surveys including the National Survey of Children’s Health, the Youth Risk Behavior Surveillance System, the WIC Participant and Program Characteristics Survey, and the National Health and Nutrition Examination Survey.
Similar to in past years, this year’s data show that rates of obesity and overweight have remained relatively steady and have been highest among minority and low-income populations. For example, data from the 2019-2020 National Survey of Children’s Health, along with an analysis conducted by the Health Resources and Services Administration’s Maternal and Child Health Bureau, show that one in six – or 16.2% – of youth aged 10-17 years have obesity.
While non-Hispanic Asian children had the lowest obesity rate (8.1%), followed by non-Hispanic White children (12.1%), rates were significantly higher for Hispanic (21.4%), non-Hispanic Black (23.8%), and non-Hispanic American Indian/Alaska Native (28.7%) children, according to the report.
“Additional years of data are needed to assess whether obesity rates changed after the onset of the pandemic,” explained Ms. Bussel.
Digging deeper
Other studies included in this year’s report were specifically designed to measure the impact of the pandemic, and show a distinct rise in overweight and obesity, especially in younger children. For example, a retrospective cohort study using data from Kaiser Permanente Southern California showed the rate of overweight and obesity in children aged 5-11 years rose to 45.7% between March 2020 and January 2021, up from 36.2% before the pandemic.
Another of these studies, which was based on national electronic health records of more than 430,000 children, showed the obesity rate crept from 19.3% to 22.4% between August 2019 and August 2020.
“The lid we had been trying desperately to put on the obesity epidemic has come off again,” said Sandra G Hassink, MD, MSc, who is medical director of the American Academy of Pediatrics Institute for Healthy Childhood Weight.
“In the absence of COVID we had been seeing slow upticks in the numbers – and in some groups we’d been thinking maybe we were headed toward stabilization – but these numbers blow that out of the water ... COVID has escalated the rates,” she said in an interview.
“Unfortunately, these two crises – the COVID pandemic, the childhood obesity epidemic – in so many ways have exacerbated one another,” said Ms. Bussel. “It’s not a huge surprise that we’re seeing an increase in childhood obesity rates given the complete and utter disruption of every single system that circumscribes our lives.”
The systems that feed obesity
Addressing childhood obesity requires targeting far beyond healthy eating and physical activity, Ms. Bussel said.
“As important is whether that child has a safe place to call home. Does mom or dad or their care provider have a stable income? Is there reliable transportation? Is their access to health insurance? Is there access to high-quality health care? ... All of those factors influence the child and the family’s opportunities to live well, be healthy, and be at a healthy weight,” she noted.
The report includes a list of five main policy recommendations.
- Making free, universal school meal programs permanent.
- Extending eligibility for WIC, the Special Supplemental Nutrition Program for Women, Infants, and Children, to postpartum mothers and to children through age 6.
- Extending and expanding other programs, such as the Child Tax Credit.
- Closing the Medicaid coverage gap.
- Developing a consistent approach to collecting obesity data organized by race, ethnicity, and income level.
“Collectively, over at least the course of the last generation or two, our policy approach to obesity prevention has not been sufficient. But that doesn’t mean all of our policy approaches have been failures,” Ms. Bussel said during an interview. “Policy change does not always need to be dramatic to have a real impact on families.”
Fighting complacency
For Dr. Hassink, one of the barriers to change is society’s level of acceptance. She said an identifiable explanation for pandemic weight gain doesn’t mean society should simply shrug it off.
“If we regarded childhood obesity as the population level catastrophe that it is for chronic disease maybe people would be activated around these policy changes,” she said.
“We’re accepting a disease process that wreaks havoc on people,” noted Dr. Hassink, who was not involved in the new report. “I think it’s hard for people to realize the magnitude of the disease burden that we’re seeing. If you’re in a weight management clinic or any pediatrician’s office you would see it – you would see kids coming in with liver disease, 9-year-olds on [continuous positive airway pressure] for sleep apnea, kids needing their hips pinned because they had a hip fracture because of obesity.
“So, those of us that see the disease burden see what’s behind those numbers. The sadness of what we’re talking about is we know a lot about what could push the dial and help reduce this epidemic and we’re not doing what we already know,” added Dr. Hassink.
Ms. Bussel and Dr. Hassink reported no conflicts.
Old wives’ tales, traditional medicine, and science
Sixteen-year-old Ana and is sitting on the bench with her science teacher, Ms. Tehrani, waiting for the bus to take them back to their village after school. Ana wants to hear her science teacher’s opinion about her grandmother.
Do you respect your grandmother?
Why yes, of course, why to do you ask?
So you think my grandmother is wise when she tells me old wife tales?
Like what?
Well, she says not to take my medicine because it will have bad effects and that I should take her remedies instead.
What else does she tell you?
Well, she says that people are born how they are and that they belong to either God or the Devil, not to their parents.
What else?
She thinks I am a fay child; she has always said that about me.
What does that mean?
It means that I have my own ways, fairy ways, and that I should go out in the forest and listen.
Do you?
Yes.
What do you hear?
I hear about my destiny.
What do you hear?
I hear that I must wash in witch hazel. My grandmother taught me how to find it and how to prepare it. She said I should sit in the forest and wait for a sign.
What sign?
I don’t know.
Well, what do you think about your grandmother?
I love her but …
But what?
I think she might be wrong about all of this, you know, science and all that.
But you do it, anyway?
Yes.
Why?
Aren’t we supposed to respect our elders, and aren’t they supposed to be wise?
Ms. Tehrani is in a bind. What to say? She has no ready answer, feeling caught between two beliefs: the unscientific basis of ineffective old wives’ treatments and the purported wisdom of our elders. She knows Ana’s family and that there are women in that family going back generations who are identified as medicine women or women with the special powers of the forest.
Ana wants to study science but she is being groomed as the family wise mother. Ana is caught between the ways of the past and the ways of the future. She sees that to go with the future is to devalue her family tradition. If she chooses to study medicine, can she keep the balance between magical ways and the ways of science?
Ms. Tehrani decides to expose her class to Indigenous and preindustrial cultural practices and what science has to say. She describes how knowledge is passed down through the generations, and how some of this knowledge has now been proved correct by science, such as the use of opium for pain management and how some knowledge has been corrected by science. She asks the class: What myths have been passed down in your family that science has shown to be effective or ineffective? What does science have to say about how we live our lives?
After a baby in the village dies, Ms. Tehrani asks the local health center to think about implementing a teaching course on caring for babies, a course that will discuss tradition and science. She is well aware of the fact that Black mothers tend not to follow the advice of the pediatricians who now recommend that parents put babies to sleep on their backs. Black women trust the advice of their paternal and maternal grandmothers more than the advice of health care providers, research by Deborah Stiffler, PhD, RN, CNM, shows (J Spec Pediatr Nurs. 2018 Apr;23[2]:e12213). While new Black mothers feel that they have limited knowledge and are eager to learn about safe sleep practices, their grandmothers were skeptical – and the grandmothers often won that argument. Black mothers believed that their own mothers knew best, based on their experience raising infants.
In Dr. Stiffler’s study, one grandmother commented: “Girls today need a mother to help them take care of their babies. They don’t know how to do anything. When I was growing up, our moms helped us.”
One new mother said: I “listen more to the elderly people because like the social workers and stuff some of them don’t have kids. They just go by the book … so I feel like I listen more to like my grandparents.”
Integrating traditions
When Ana enters medical school she is faced with the task of integration of traditional practice and Western medicine. Ana looks to the National Center for Complementary and Integrative Health (NCCIH), the U.S. government’s lead agency for scientific research on complementary and integrative health approaches for support in her task. The NCCIH was established in 1998 with the mission of determining the usefulness and safety of complementary and integrative health approaches, and their roles in improving health and health care.
The NCCIH notes that more than 30% of adults use health care approaches that are not part of conventional medical care or that have origins outside of usual Western practice, and 17.7% of American adults had used a dietary supplement other than vitamins and minerals in the past year, most commonly fish oil. This agency notes that large rigorous research studies extend to only a few dietary supplements, with results showing that the products didn’t work for the conditions studied. The work of the NCCIH is mirrored worldwide.
The 2008 Beijing Declaration called on World Health Organization member states and other stakeholders to integrate traditional medicine and complementary alternative medicines into national health care systems. The WHO Congress on Traditional Medicine recognizes that traditional medicine (TM) may be more affordable and accessible than Western medicine, and that it plays an important role in meeting the demands of primary health care in many developing countries. From 70% to 80% of the population in India and Ethiopia depend on TM for primary health care, and 70% of the population in Canada and 80% in Germany are reported to have used TM as complementary and/or alternative medical treatment.
After graduation and residency, Ana returns to her village and helps her science teacher consider how best to shape the intergenerational transmission of knowledge, so that it is both honored by the elders and also shaped by the science of medicine.
Every village, regardless of where it is in the world, has to contend with finding the balance between the traditional medical knowledge that is passed down through the family and the discoveries of science. When it comes to practicing medicine and psychiatry, a respect for family tradition must be weighed against the application of science: this is a long conversation that is well worth its time.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). Dr. Heru has no conflicts of interest. Contact Dr. Heru at [email protected].
Sixteen-year-old Ana and is sitting on the bench with her science teacher, Ms. Tehrani, waiting for the bus to take them back to their village after school. Ana wants to hear her science teacher’s opinion about her grandmother.
Do you respect your grandmother?
Why yes, of course, why to do you ask?
So you think my grandmother is wise when she tells me old wife tales?
Like what?
Well, she says not to take my medicine because it will have bad effects and that I should take her remedies instead.
What else does she tell you?
Well, she says that people are born how they are and that they belong to either God or the Devil, not to their parents.
What else?
She thinks I am a fay child; she has always said that about me.
What does that mean?
It means that I have my own ways, fairy ways, and that I should go out in the forest and listen.
Do you?
Yes.
What do you hear?
I hear about my destiny.
What do you hear?
I hear that I must wash in witch hazel. My grandmother taught me how to find it and how to prepare it. She said I should sit in the forest and wait for a sign.
What sign?
I don’t know.
Well, what do you think about your grandmother?
I love her but …
But what?
I think she might be wrong about all of this, you know, science and all that.
But you do it, anyway?
Yes.
Why?
Aren’t we supposed to respect our elders, and aren’t they supposed to be wise?
Ms. Tehrani is in a bind. What to say? She has no ready answer, feeling caught between two beliefs: the unscientific basis of ineffective old wives’ treatments and the purported wisdom of our elders. She knows Ana’s family and that there are women in that family going back generations who are identified as medicine women or women with the special powers of the forest.
Ana wants to study science but she is being groomed as the family wise mother. Ana is caught between the ways of the past and the ways of the future. She sees that to go with the future is to devalue her family tradition. If she chooses to study medicine, can she keep the balance between magical ways and the ways of science?
Ms. Tehrani decides to expose her class to Indigenous and preindustrial cultural practices and what science has to say. She describes how knowledge is passed down through the generations, and how some of this knowledge has now been proved correct by science, such as the use of opium for pain management and how some knowledge has been corrected by science. She asks the class: What myths have been passed down in your family that science has shown to be effective or ineffective? What does science have to say about how we live our lives?
After a baby in the village dies, Ms. Tehrani asks the local health center to think about implementing a teaching course on caring for babies, a course that will discuss tradition and science. She is well aware of the fact that Black mothers tend not to follow the advice of the pediatricians who now recommend that parents put babies to sleep on their backs. Black women trust the advice of their paternal and maternal grandmothers more than the advice of health care providers, research by Deborah Stiffler, PhD, RN, CNM, shows (J Spec Pediatr Nurs. 2018 Apr;23[2]:e12213). While new Black mothers feel that they have limited knowledge and are eager to learn about safe sleep practices, their grandmothers were skeptical – and the grandmothers often won that argument. Black mothers believed that their own mothers knew best, based on their experience raising infants.
In Dr. Stiffler’s study, one grandmother commented: “Girls today need a mother to help them take care of their babies. They don’t know how to do anything. When I was growing up, our moms helped us.”
One new mother said: I “listen more to the elderly people because like the social workers and stuff some of them don’t have kids. They just go by the book … so I feel like I listen more to like my grandparents.”
Integrating traditions
When Ana enters medical school she is faced with the task of integration of traditional practice and Western medicine. Ana looks to the National Center for Complementary and Integrative Health (NCCIH), the U.S. government’s lead agency for scientific research on complementary and integrative health approaches for support in her task. The NCCIH was established in 1998 with the mission of determining the usefulness and safety of complementary and integrative health approaches, and their roles in improving health and health care.
The NCCIH notes that more than 30% of adults use health care approaches that are not part of conventional medical care or that have origins outside of usual Western practice, and 17.7% of American adults had used a dietary supplement other than vitamins and minerals in the past year, most commonly fish oil. This agency notes that large rigorous research studies extend to only a few dietary supplements, with results showing that the products didn’t work for the conditions studied. The work of the NCCIH is mirrored worldwide.
The 2008 Beijing Declaration called on World Health Organization member states and other stakeholders to integrate traditional medicine and complementary alternative medicines into national health care systems. The WHO Congress on Traditional Medicine recognizes that traditional medicine (TM) may be more affordable and accessible than Western medicine, and that it plays an important role in meeting the demands of primary health care in many developing countries. From 70% to 80% of the population in India and Ethiopia depend on TM for primary health care, and 70% of the population in Canada and 80% in Germany are reported to have used TM as complementary and/or alternative medical treatment.
After graduation and residency, Ana returns to her village and helps her science teacher consider how best to shape the intergenerational transmission of knowledge, so that it is both honored by the elders and also shaped by the science of medicine.
Every village, regardless of where it is in the world, has to contend with finding the balance between the traditional medical knowledge that is passed down through the family and the discoveries of science. When it comes to practicing medicine and psychiatry, a respect for family tradition must be weighed against the application of science: this is a long conversation that is well worth its time.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). Dr. Heru has no conflicts of interest. Contact Dr. Heru at [email protected].
Sixteen-year-old Ana and is sitting on the bench with her science teacher, Ms. Tehrani, waiting for the bus to take them back to their village after school. Ana wants to hear her science teacher’s opinion about her grandmother.
Do you respect your grandmother?
Why yes, of course, why to do you ask?
So you think my grandmother is wise when she tells me old wife tales?
Like what?
Well, she says not to take my medicine because it will have bad effects and that I should take her remedies instead.
What else does she tell you?
Well, she says that people are born how they are and that they belong to either God or the Devil, not to their parents.
What else?
She thinks I am a fay child; she has always said that about me.
What does that mean?
It means that I have my own ways, fairy ways, and that I should go out in the forest and listen.
Do you?
Yes.
What do you hear?
I hear about my destiny.
What do you hear?
I hear that I must wash in witch hazel. My grandmother taught me how to find it and how to prepare it. She said I should sit in the forest and wait for a sign.
What sign?
I don’t know.
Well, what do you think about your grandmother?
I love her but …
But what?
I think she might be wrong about all of this, you know, science and all that.
But you do it, anyway?
Yes.
Why?
Aren’t we supposed to respect our elders, and aren’t they supposed to be wise?
Ms. Tehrani is in a bind. What to say? She has no ready answer, feeling caught between two beliefs: the unscientific basis of ineffective old wives’ treatments and the purported wisdom of our elders. She knows Ana’s family and that there are women in that family going back generations who are identified as medicine women or women with the special powers of the forest.
Ana wants to study science but she is being groomed as the family wise mother. Ana is caught between the ways of the past and the ways of the future. She sees that to go with the future is to devalue her family tradition. If she chooses to study medicine, can she keep the balance between magical ways and the ways of science?
Ms. Tehrani decides to expose her class to Indigenous and preindustrial cultural practices and what science has to say. She describes how knowledge is passed down through the generations, and how some of this knowledge has now been proved correct by science, such as the use of opium for pain management and how some knowledge has been corrected by science. She asks the class: What myths have been passed down in your family that science has shown to be effective or ineffective? What does science have to say about how we live our lives?
After a baby in the village dies, Ms. Tehrani asks the local health center to think about implementing a teaching course on caring for babies, a course that will discuss tradition and science. She is well aware of the fact that Black mothers tend not to follow the advice of the pediatricians who now recommend that parents put babies to sleep on their backs. Black women trust the advice of their paternal and maternal grandmothers more than the advice of health care providers, research by Deborah Stiffler, PhD, RN, CNM, shows (J Spec Pediatr Nurs. 2018 Apr;23[2]:e12213). While new Black mothers feel that they have limited knowledge and are eager to learn about safe sleep practices, their grandmothers were skeptical – and the grandmothers often won that argument. Black mothers believed that their own mothers knew best, based on their experience raising infants.
In Dr. Stiffler’s study, one grandmother commented: “Girls today need a mother to help them take care of their babies. They don’t know how to do anything. When I was growing up, our moms helped us.”
One new mother said: I “listen more to the elderly people because like the social workers and stuff some of them don’t have kids. They just go by the book … so I feel like I listen more to like my grandparents.”
Integrating traditions
When Ana enters medical school she is faced with the task of integration of traditional practice and Western medicine. Ana looks to the National Center for Complementary and Integrative Health (NCCIH), the U.S. government’s lead agency for scientific research on complementary and integrative health approaches for support in her task. The NCCIH was established in 1998 with the mission of determining the usefulness and safety of complementary and integrative health approaches, and their roles in improving health and health care.
The NCCIH notes that more than 30% of adults use health care approaches that are not part of conventional medical care or that have origins outside of usual Western practice, and 17.7% of American adults had used a dietary supplement other than vitamins and minerals in the past year, most commonly fish oil. This agency notes that large rigorous research studies extend to only a few dietary supplements, with results showing that the products didn’t work for the conditions studied. The work of the NCCIH is mirrored worldwide.
The 2008 Beijing Declaration called on World Health Organization member states and other stakeholders to integrate traditional medicine and complementary alternative medicines into national health care systems. The WHO Congress on Traditional Medicine recognizes that traditional medicine (TM) may be more affordable and accessible than Western medicine, and that it plays an important role in meeting the demands of primary health care in many developing countries. From 70% to 80% of the population in India and Ethiopia depend on TM for primary health care, and 70% of the population in Canada and 80% in Germany are reported to have used TM as complementary and/or alternative medical treatment.
After graduation and residency, Ana returns to her village and helps her science teacher consider how best to shape the intergenerational transmission of knowledge, so that it is both honored by the elders and also shaped by the science of medicine.
Every village, regardless of where it is in the world, has to contend with finding the balance between the traditional medical knowledge that is passed down through the family and the discoveries of science. When it comes to practicing medicine and psychiatry, a respect for family tradition must be weighed against the application of science: this is a long conversation that is well worth its time.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). Dr. Heru has no conflicts of interest. Contact Dr. Heru at [email protected].
The Long-term Effects of Underdiagnosed Conditions in Sleep Disorders
Jessie Wrobel is a board-certified Family Nurse Practitioner. She earned a Bachelor of Science in Nursing from Southern Connecticut State University, concurrently graduating from their Honor’s College in 2009 and spent 9 years at the bedside focusing on heart failure and stroke populations. She then obtained a Master of Science in Nursing from Southern Connecticut State University and holds a certification with the American Academy of Nurse Practitioners (AANP) as a family nurse practitioner. She has since worked at Yale-New Haven’s Sleep Medicine Center where she follows patients for sleep disordered breathing, narcolepsy, parasomnias, restless leg syndrome and insomnia.
Jessie Wrobel is a board-certified Family Nurse Practitioner. She earned a Bachelor of Science in Nursing from Southern Connecticut State University, concurrently graduating from their Honor’s College in 2009 and spent 9 years at the bedside focusing on heart failure and stroke populations. She then obtained a Master of Science in Nursing from Southern Connecticut State University and holds a certification with the American Academy of Nurse Practitioners (AANP) as a family nurse practitioner. She has since worked at Yale-New Haven’s Sleep Medicine Center where she follows patients for sleep disordered breathing, narcolepsy, parasomnias, restless leg syndrome and insomnia.
Jessie Wrobel is a board-certified Family Nurse Practitioner. She earned a Bachelor of Science in Nursing from Southern Connecticut State University, concurrently graduating from their Honor’s College in 2009 and spent 9 years at the bedside focusing on heart failure and stroke populations. She then obtained a Master of Science in Nursing from Southern Connecticut State University and holds a certification with the American Academy of Nurse Practitioners (AANP) as a family nurse practitioner. She has since worked at Yale-New Haven’s Sleep Medicine Center where she follows patients for sleep disordered breathing, narcolepsy, parasomnias, restless leg syndrome and insomnia.
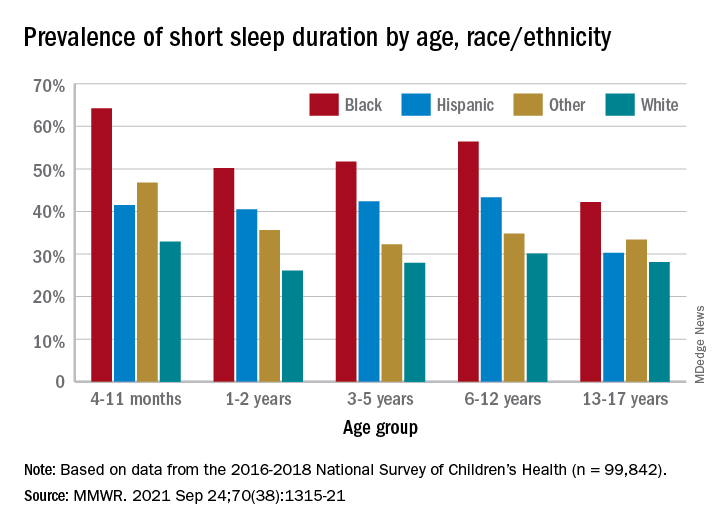
One in three children fall short of sleep recommendations
Just over one-third of children in the United States get less sleep than recommended, with higher rates occurring among several racial/ethnic and socioeconomic groups, according to a report from the Centers for Disease Control and Prevention.
, Anne G. Wheaton, PhD, and Angelika H. Claussen, PhD, said in the Morbidity and Mortality Weekly Report.
Unlike previous reports, this analysis showed that adolescents were less likely than infants to have short sleep duration, 31.2% vs. 40.3%. These latest data are based on the 2016-2018 editions of the National Survey of Children’s Health, and the “difference might be explained by NSCH’s reliance on parent report rather than self-report with Youth Risk Behavior Surveys,” they suggested.
Black children had the highest prevalence of any group included in the study, as parents reported that 50.8% of all ages were not getting the recommended amount of sleep, compared with 39.1% among Hispanics, 34.6% for other races, and 28.8% for Whites. The figure for Black infants was 64.2%, almost double the prevalence for White infants (32.9%), said Dr. Wheaton and Dr. Claussen of the CDC.
Short sleep duration also was more common in children from lower-income families and among those with less educated parents. Geography had an effect as well, with prevalence “highest in the Southeast, similar to geographic variation in adequate sleep observed for adults,” they noted.
Previous research has shown that “sleep disparity was associated with various social determinants of health (e.g., poverty, food insecurity, and perceived racism), which can increase chronic and acute stress and result in environmental and psychological factors that negatively affect sleep duration and can compound long-term health risks,” the investigators wrote.
Short sleep duration by age group was defined as less the following amounts: Twelve hours for infants (4-11 months), 11 hours for children aged 1-2 years, 10 hours for children aged 3-5 years, 9 hours for children aged 6-12, and 8 hours for adolescents (13-17 years), they explained. Responses for the survey’s sleep-duration question totaled 99,842 for the 3 years included.
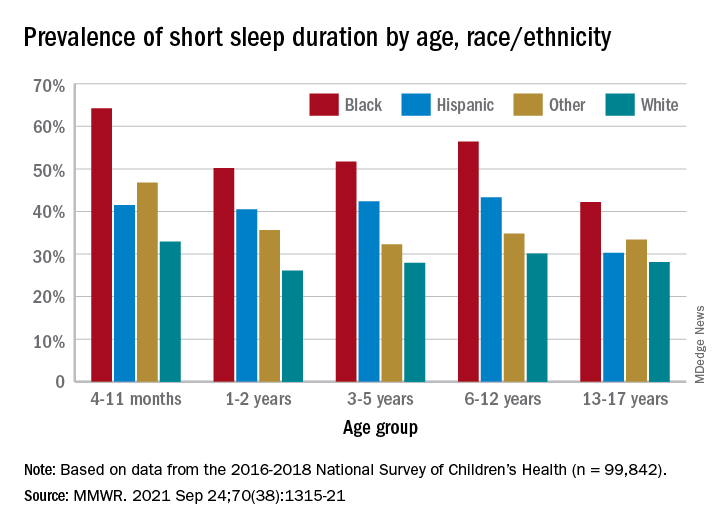
Just over one-third of children in the United States get less sleep than recommended, with higher rates occurring among several racial/ethnic and socioeconomic groups, according to a report from the Centers for Disease Control and Prevention.
, Anne G. Wheaton, PhD, and Angelika H. Claussen, PhD, said in the Morbidity and Mortality Weekly Report.
Unlike previous reports, this analysis showed that adolescents were less likely than infants to have short sleep duration, 31.2% vs. 40.3%. These latest data are based on the 2016-2018 editions of the National Survey of Children’s Health, and the “difference might be explained by NSCH’s reliance on parent report rather than self-report with Youth Risk Behavior Surveys,” they suggested.
Black children had the highest prevalence of any group included in the study, as parents reported that 50.8% of all ages were not getting the recommended amount of sleep, compared with 39.1% among Hispanics, 34.6% for other races, and 28.8% for Whites. The figure for Black infants was 64.2%, almost double the prevalence for White infants (32.9%), said Dr. Wheaton and Dr. Claussen of the CDC.
Short sleep duration also was more common in children from lower-income families and among those with less educated parents. Geography had an effect as well, with prevalence “highest in the Southeast, similar to geographic variation in adequate sleep observed for adults,” they noted.
Previous research has shown that “sleep disparity was associated with various social determinants of health (e.g., poverty, food insecurity, and perceived racism), which can increase chronic and acute stress and result in environmental and psychological factors that negatively affect sleep duration and can compound long-term health risks,” the investigators wrote.
Short sleep duration by age group was defined as less the following amounts: Twelve hours for infants (4-11 months), 11 hours for children aged 1-2 years, 10 hours for children aged 3-5 years, 9 hours for children aged 6-12, and 8 hours for adolescents (13-17 years), they explained. Responses for the survey’s sleep-duration question totaled 99,842 for the 3 years included.
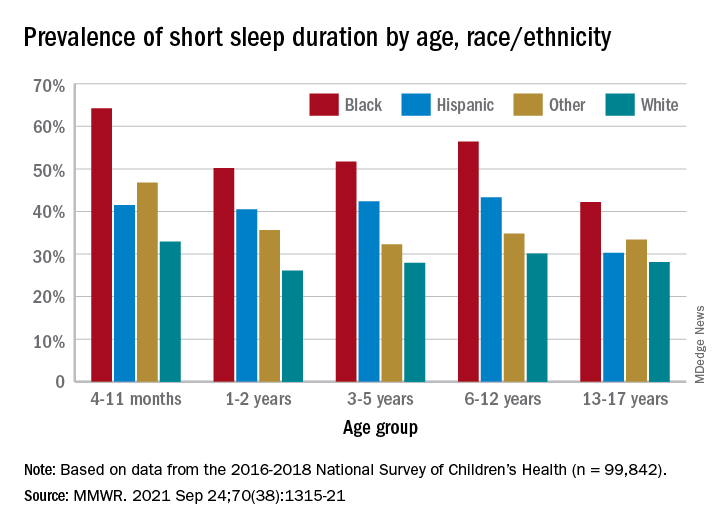
Just over one-third of children in the United States get less sleep than recommended, with higher rates occurring among several racial/ethnic and socioeconomic groups, according to a report from the Centers for Disease Control and Prevention.
, Anne G. Wheaton, PhD, and Angelika H. Claussen, PhD, said in the Morbidity and Mortality Weekly Report.
Unlike previous reports, this analysis showed that adolescents were less likely than infants to have short sleep duration, 31.2% vs. 40.3%. These latest data are based on the 2016-2018 editions of the National Survey of Children’s Health, and the “difference might be explained by NSCH’s reliance on parent report rather than self-report with Youth Risk Behavior Surveys,” they suggested.
Black children had the highest prevalence of any group included in the study, as parents reported that 50.8% of all ages were not getting the recommended amount of sleep, compared with 39.1% among Hispanics, 34.6% for other races, and 28.8% for Whites. The figure for Black infants was 64.2%, almost double the prevalence for White infants (32.9%), said Dr. Wheaton and Dr. Claussen of the CDC.
Short sleep duration also was more common in children from lower-income families and among those with less educated parents. Geography had an effect as well, with prevalence “highest in the Southeast, similar to geographic variation in adequate sleep observed for adults,” they noted.
Previous research has shown that “sleep disparity was associated with various social determinants of health (e.g., poverty, food insecurity, and perceived racism), which can increase chronic and acute stress and result in environmental and psychological factors that negatively affect sleep duration and can compound long-term health risks,” the investigators wrote.
Short sleep duration by age group was defined as less the following amounts: Twelve hours for infants (4-11 months), 11 hours for children aged 1-2 years, 10 hours for children aged 3-5 years, 9 hours for children aged 6-12, and 8 hours for adolescents (13-17 years), they explained. Responses for the survey’s sleep-duration question totaled 99,842 for the 3 years included.
FROM MMWR
Nature versus nurture: Seasonal affective disorder
With summer coming to an end, and pumpkin spice lattes trending again, we might also expect to say hello to an old friend ... seasonal affective disorder (SAD).
Have you ever woken up one morning during the fall or winter and felt out of it for a prolonged period, not your regular self? I’m not referring to a day here and there, but consistently experiencing this “down mood” around the same time each year? At some point in their life, it is estimated that 2-3% of Canadians will experience SAD. To add to that, 15% of individuals will experience milder (and less impairing) SAD.
Seasonal affective disorder can be thought of as a type of depression that occurs during a specific time of the year, usually the winter or fall (with remission outside this period). It is typically characterized by symptoms of clinical depression such as low energy, difficulty with concentration, sleep problems, extreme fatigue, and agitation. While the evidence related to the risk factors for SAD are limited, it is suggested that a family history of SAD, female sex, location farther from the equator (that is, fewer days of sunlight), and being between the ages of 18-30 increase your risk for SAD.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) does not provide a separate and distinct categorization for SAD. Rather, SAD is categorized as a subtype of depression. However,
Nature versus nurture: An evolutionary perspective
The pathophysiology of SAD is not yet well understood. However, it is hypothesized that SAD is an adaptive response related to physiologic and behavioral patterns of reproduction and childrearing.
Historically, reproduction was closely linked to food and natural resource availability (for example, water, sunlight). Males primarily handled the hunting, while females were primarily responsible for agricultural work, a job closely tied to the seasons. With this in mind, it would logically follow that natural selection favored reproduction during times of food abundance and did not favor reproduction during times of food scarcity (that is, low energy).
Consequently, conception would occur when the growing season began (around the summer), giving females the chance to rest when heavily pregnant in the winter, and give birth in the spring. Accordingly, from an evolutionary perspective, greater seasonal variation in mood and behavior is a function of historic patterns of reproduction and food gathering.
An alternative hypothesis of SAD is the dual vulnerability hypothesis. This hypothesis posits that SAD is the result of seasonality and depression (or “vulnerability traits”). Seasonality refers to external environmental factors such as light availability.
It’s quite well known, and perhaps your personal experience can speak to this topic as well, that shorter days may trigger SAD because reduced light exposure is associated with phase-delayed circadian rhythms. As a result, less dopamine is produced, and relatively higher levels of melatonin are produced, compared to individuals without SAD. “Vulnerability traits” refer to a genetic predisposition, or external effects (for example, stress).
A disorder of the past?
By nature of natural selection, SAD is likely not to be considered an advantageous adaptive trait that would help with survival and reproduction. In fact, it could be considered a maladaptive trait. In that case, will SAD eventually fall to natural selection?
Leanna M.W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
With summer coming to an end, and pumpkin spice lattes trending again, we might also expect to say hello to an old friend ... seasonal affective disorder (SAD).
Have you ever woken up one morning during the fall or winter and felt out of it for a prolonged period, not your regular self? I’m not referring to a day here and there, but consistently experiencing this “down mood” around the same time each year? At some point in their life, it is estimated that 2-3% of Canadians will experience SAD. To add to that, 15% of individuals will experience milder (and less impairing) SAD.
Seasonal affective disorder can be thought of as a type of depression that occurs during a specific time of the year, usually the winter or fall (with remission outside this period). It is typically characterized by symptoms of clinical depression such as low energy, difficulty with concentration, sleep problems, extreme fatigue, and agitation. While the evidence related to the risk factors for SAD are limited, it is suggested that a family history of SAD, female sex, location farther from the equator (that is, fewer days of sunlight), and being between the ages of 18-30 increase your risk for SAD.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) does not provide a separate and distinct categorization for SAD. Rather, SAD is categorized as a subtype of depression. However,
Nature versus nurture: An evolutionary perspective
The pathophysiology of SAD is not yet well understood. However, it is hypothesized that SAD is an adaptive response related to physiologic and behavioral patterns of reproduction and childrearing.
Historically, reproduction was closely linked to food and natural resource availability (for example, water, sunlight). Males primarily handled the hunting, while females were primarily responsible for agricultural work, a job closely tied to the seasons. With this in mind, it would logically follow that natural selection favored reproduction during times of food abundance and did not favor reproduction during times of food scarcity (that is, low energy).
Consequently, conception would occur when the growing season began (around the summer), giving females the chance to rest when heavily pregnant in the winter, and give birth in the spring. Accordingly, from an evolutionary perspective, greater seasonal variation in mood and behavior is a function of historic patterns of reproduction and food gathering.
An alternative hypothesis of SAD is the dual vulnerability hypothesis. This hypothesis posits that SAD is the result of seasonality and depression (or “vulnerability traits”). Seasonality refers to external environmental factors such as light availability.
It’s quite well known, and perhaps your personal experience can speak to this topic as well, that shorter days may trigger SAD because reduced light exposure is associated with phase-delayed circadian rhythms. As a result, less dopamine is produced, and relatively higher levels of melatonin are produced, compared to individuals without SAD. “Vulnerability traits” refer to a genetic predisposition, or external effects (for example, stress).
A disorder of the past?
By nature of natural selection, SAD is likely not to be considered an advantageous adaptive trait that would help with survival and reproduction. In fact, it could be considered a maladaptive trait. In that case, will SAD eventually fall to natural selection?
Leanna M.W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
With summer coming to an end, and pumpkin spice lattes trending again, we might also expect to say hello to an old friend ... seasonal affective disorder (SAD).
Have you ever woken up one morning during the fall or winter and felt out of it for a prolonged period, not your regular self? I’m not referring to a day here and there, but consistently experiencing this “down mood” around the same time each year? At some point in their life, it is estimated that 2-3% of Canadians will experience SAD. To add to that, 15% of individuals will experience milder (and less impairing) SAD.
Seasonal affective disorder can be thought of as a type of depression that occurs during a specific time of the year, usually the winter or fall (with remission outside this period). It is typically characterized by symptoms of clinical depression such as low energy, difficulty with concentration, sleep problems, extreme fatigue, and agitation. While the evidence related to the risk factors for SAD are limited, it is suggested that a family history of SAD, female sex, location farther from the equator (that is, fewer days of sunlight), and being between the ages of 18-30 increase your risk for SAD.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) does not provide a separate and distinct categorization for SAD. Rather, SAD is categorized as a subtype of depression. However,
Nature versus nurture: An evolutionary perspective
The pathophysiology of SAD is not yet well understood. However, it is hypothesized that SAD is an adaptive response related to physiologic and behavioral patterns of reproduction and childrearing.
Historically, reproduction was closely linked to food and natural resource availability (for example, water, sunlight). Males primarily handled the hunting, while females were primarily responsible for agricultural work, a job closely tied to the seasons. With this in mind, it would logically follow that natural selection favored reproduction during times of food abundance and did not favor reproduction during times of food scarcity (that is, low energy).
Consequently, conception would occur when the growing season began (around the summer), giving females the chance to rest when heavily pregnant in the winter, and give birth in the spring. Accordingly, from an evolutionary perspective, greater seasonal variation in mood and behavior is a function of historic patterns of reproduction and food gathering.
An alternative hypothesis of SAD is the dual vulnerability hypothesis. This hypothesis posits that SAD is the result of seasonality and depression (or “vulnerability traits”). Seasonality refers to external environmental factors such as light availability.
It’s quite well known, and perhaps your personal experience can speak to this topic as well, that shorter days may trigger SAD because reduced light exposure is associated with phase-delayed circadian rhythms. As a result, less dopamine is produced, and relatively higher levels of melatonin are produced, compared to individuals without SAD. “Vulnerability traits” refer to a genetic predisposition, or external effects (for example, stress).
A disorder of the past?
By nature of natural selection, SAD is likely not to be considered an advantageous adaptive trait that would help with survival and reproduction. In fact, it could be considered a maladaptive trait. In that case, will SAD eventually fall to natural selection?
Leanna M.W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
COVID wars, part nine: The rise of iodine
Onions and iodine and COVID, oh my!
As surely as the sun rises, anti-vaxxers will come up with some wacky and dangerous new idea to prevent COVID. While perhaps nothing will top horse medication, gargling iodine (or spraying it into the nose) is also not a great idea.
Multiple social media posts have extolled the virtues of gargling Betadine (povidone iodine), which is a TOPICAL disinfectant commonly used in EDs and operating rooms. One post cited a paper by a Bangladeshi plastic surgeon who hypothesized on the subject, and if that’s not a peer-reviewed, rigorously researched source, we don’t know what is.
Perhaps unsurprisingly, actual medical experts do not recommend using Betadine to prevent COVID. Ingesting it can cause iodine poisoning and plenty of nasty GI side effects; while Betadine does make a diluted product safe for gargling use (used for the treatment of sore throats), it has not shown any effectiveness against viruses or COVID in particular.
A New York ED doctor summed it up best in the Rolling Stone article when he was told anti-vaxxers were gargling iodine: He offered a choice four-letter expletive, then said, “Of course they are.”
But wait! We’ve got a two-for-one deal on dubious COVID cures this week. Health experts in Myanmar (Burma to all the “Seinfeld” fans) and Thailand have been combating social media posts claiming that onion fumes will cure COVID. All you need to do is slice an onion in half, sniff it for a while, then chew on a second onion, and your COVID will be cured!
In what is surely the most radical understatement of the year, a professor in the department of preventive and social medicine at Chulalongkorn University, Bangkok, said in the AFP article that there is “no solid evidence” to support onion sniffing from “any clinical research.”
We’re just going to assume the expletives that surely followed were kept off the record.
Pro-Trump state governor encourages vaccination
Clearly, the politics of COVID-19 have been working against the science of COVID-19. Politicians can’t, or won’t, agree on what to do about it, and many prominent Republicans have been actively resisting vaccine and mask mandates.
There is at least one Republican governor who has wholeheartedly encouraged vaccination in his pro-Trump state. We’re talking about Gov. Jim Justice of West Virginia, and not for the first time.
The Washington Post has detailed his efforts to promote the COVID vaccine, and we would like to share a couple of examples.
In June he suggested that people who didn’t get vaccinated were “entering the death drawing.” He followed that by saying, “If I knew for certain that there was going to be eight or nine people die by next Tuesday, and I could be one of them if I don’t take the vaccine ... What in the world do you think I would do? I mean, I would run over top of somebody.”
More recently, Gov. Justice took on vaccine conspiracy theories.
“For God’s sakes a livin’, how difficult is this to understand? Why in the world do we have to come up with these crazy ideas – and they’re crazy ideas – that the vaccine’s got something in it and it’s tracing people wherever they go? And the very same people that are saying that are carrying their cellphones around. I mean, come on. Come on.”
Nuff said.
Jet lag may be a gut feeling
After a week-long vacation halfway around the world, it’s time to go back to your usual routine and time zone. But don’t forget about that free souvenir, jet lag. A disrupted circadian rhythm can be a real bummer, but researchers may have found the fix in your belly.
In a study funded by the U.S. Navy, researchers at the University of Colorado, Boulder, looked into how the presence of a prebiotic in one’s diet can have on the disrupted biological clocks. They’re not the same as probiotics, which help you stay regular in another way. Prebiotics work as food to help the good gut bacteria you already have. An earlier study had suggested that prebiotics may have a positive effect on the brain.
To test the theory, the researchers gave one group of rats their regular food while another group received food with two different prebiotics. After manipulating the rats’ light-dark cycle for 8 weeks to give the illusion of traveling to a time zone 12 hours ahead every week, they found that the rats who ate the prebiotics were able to bounce back faster.
The possibility of ingesting something to keep your body clock regular sounds like a dream, but the researchers don’t really advise you to snatch all the supplements you can at your local pharmacy just yet.
“If you know you are going to come into a challenge, you could take a look at some of the prebiotics that are available. Just realize that they are not customized yet, so it might work for you but it won’t work for your neighbor,” said senior author Monika Fleshner.
Until there’s more conclusive research, just be good to your bacteria.
How to make stuff up and influence people
You’ve probably heard that we use only 10% of our brain. It’s right up there with “the Earth is flat” and “an apple a day keeps the doctor away.”
The idea that we use only 10% of our brains can probably be traced back to the early 1900s, suggests Discover magazine, when psychologist William James wrote, “Compared with what we ought to be, we are only half awake. Our fires are damped, our drafts are checked. We are making use of only a small part of our possible mental and physical resources.”
There are many different takes on it, but it is indeed a myth that we use only 10% of our brains. Dale Carnegie, the public speaking teacher, seems to be the one who put the specific number of 10% on James’ idea in his 1936 book, “How to Win Friends and Influence People.”
“We think that people are excited by this pseudo fact because it’s very optimistic,” neuroscientist Sandra Aamodt told Discover. “Wouldn’t we all love to think our brains had some giant pool of untapped potential that we’re not using?”
The reality is, we do use our whole brain. Functional MRI shows that different parts of the brain are used for different things such as language and memories. “Not all at the same time, of course. But every part of the brain has a job to do,” the Discover article explained.
There are many things we don’t know about how the brain works, but at least you know you use more than 10%. After all, a brain just told you so.
Onions and iodine and COVID, oh my!
As surely as the sun rises, anti-vaxxers will come up with some wacky and dangerous new idea to prevent COVID. While perhaps nothing will top horse medication, gargling iodine (or spraying it into the nose) is also not a great idea.
Multiple social media posts have extolled the virtues of gargling Betadine (povidone iodine), which is a TOPICAL disinfectant commonly used in EDs and operating rooms. One post cited a paper by a Bangladeshi plastic surgeon who hypothesized on the subject, and if that’s not a peer-reviewed, rigorously researched source, we don’t know what is.
Perhaps unsurprisingly, actual medical experts do not recommend using Betadine to prevent COVID. Ingesting it can cause iodine poisoning and plenty of nasty GI side effects; while Betadine does make a diluted product safe for gargling use (used for the treatment of sore throats), it has not shown any effectiveness against viruses or COVID in particular.
A New York ED doctor summed it up best in the Rolling Stone article when he was told anti-vaxxers were gargling iodine: He offered a choice four-letter expletive, then said, “Of course they are.”
But wait! We’ve got a two-for-one deal on dubious COVID cures this week. Health experts in Myanmar (Burma to all the “Seinfeld” fans) and Thailand have been combating social media posts claiming that onion fumes will cure COVID. All you need to do is slice an onion in half, sniff it for a while, then chew on a second onion, and your COVID will be cured!
In what is surely the most radical understatement of the year, a professor in the department of preventive and social medicine at Chulalongkorn University, Bangkok, said in the AFP article that there is “no solid evidence” to support onion sniffing from “any clinical research.”
We’re just going to assume the expletives that surely followed were kept off the record.
Pro-Trump state governor encourages vaccination
Clearly, the politics of COVID-19 have been working against the science of COVID-19. Politicians can’t, or won’t, agree on what to do about it, and many prominent Republicans have been actively resisting vaccine and mask mandates.
There is at least one Republican governor who has wholeheartedly encouraged vaccination in his pro-Trump state. We’re talking about Gov. Jim Justice of West Virginia, and not for the first time.
The Washington Post has detailed his efforts to promote the COVID vaccine, and we would like to share a couple of examples.
In June he suggested that people who didn’t get vaccinated were “entering the death drawing.” He followed that by saying, “If I knew for certain that there was going to be eight or nine people die by next Tuesday, and I could be one of them if I don’t take the vaccine ... What in the world do you think I would do? I mean, I would run over top of somebody.”
More recently, Gov. Justice took on vaccine conspiracy theories.
“For God’s sakes a livin’, how difficult is this to understand? Why in the world do we have to come up with these crazy ideas – and they’re crazy ideas – that the vaccine’s got something in it and it’s tracing people wherever they go? And the very same people that are saying that are carrying their cellphones around. I mean, come on. Come on.”
Nuff said.
Jet lag may be a gut feeling
After a week-long vacation halfway around the world, it’s time to go back to your usual routine and time zone. But don’t forget about that free souvenir, jet lag. A disrupted circadian rhythm can be a real bummer, but researchers may have found the fix in your belly.
In a study funded by the U.S. Navy, researchers at the University of Colorado, Boulder, looked into how the presence of a prebiotic in one’s diet can have on the disrupted biological clocks. They’re not the same as probiotics, which help you stay regular in another way. Prebiotics work as food to help the good gut bacteria you already have. An earlier study had suggested that prebiotics may have a positive effect on the brain.
To test the theory, the researchers gave one group of rats their regular food while another group received food with two different prebiotics. After manipulating the rats’ light-dark cycle for 8 weeks to give the illusion of traveling to a time zone 12 hours ahead every week, they found that the rats who ate the prebiotics were able to bounce back faster.
The possibility of ingesting something to keep your body clock regular sounds like a dream, but the researchers don’t really advise you to snatch all the supplements you can at your local pharmacy just yet.
“If you know you are going to come into a challenge, you could take a look at some of the prebiotics that are available. Just realize that they are not customized yet, so it might work for you but it won’t work for your neighbor,” said senior author Monika Fleshner.
Until there’s more conclusive research, just be good to your bacteria.
How to make stuff up and influence people
You’ve probably heard that we use only 10% of our brain. It’s right up there with “the Earth is flat” and “an apple a day keeps the doctor away.”
The idea that we use only 10% of our brains can probably be traced back to the early 1900s, suggests Discover magazine, when psychologist William James wrote, “Compared with what we ought to be, we are only half awake. Our fires are damped, our drafts are checked. We are making use of only a small part of our possible mental and physical resources.”
There are many different takes on it, but it is indeed a myth that we use only 10% of our brains. Dale Carnegie, the public speaking teacher, seems to be the one who put the specific number of 10% on James’ idea in his 1936 book, “How to Win Friends and Influence People.”
“We think that people are excited by this pseudo fact because it’s very optimistic,” neuroscientist Sandra Aamodt told Discover. “Wouldn’t we all love to think our brains had some giant pool of untapped potential that we’re not using?”
The reality is, we do use our whole brain. Functional MRI shows that different parts of the brain are used for different things such as language and memories. “Not all at the same time, of course. But every part of the brain has a job to do,” the Discover article explained.
There are many things we don’t know about how the brain works, but at least you know you use more than 10%. After all, a brain just told you so.
Onions and iodine and COVID, oh my!
As surely as the sun rises, anti-vaxxers will come up with some wacky and dangerous new idea to prevent COVID. While perhaps nothing will top horse medication, gargling iodine (or spraying it into the nose) is also not a great idea.
Multiple social media posts have extolled the virtues of gargling Betadine (povidone iodine), which is a TOPICAL disinfectant commonly used in EDs and operating rooms. One post cited a paper by a Bangladeshi plastic surgeon who hypothesized on the subject, and if that’s not a peer-reviewed, rigorously researched source, we don’t know what is.
Perhaps unsurprisingly, actual medical experts do not recommend using Betadine to prevent COVID. Ingesting it can cause iodine poisoning and plenty of nasty GI side effects; while Betadine does make a diluted product safe for gargling use (used for the treatment of sore throats), it has not shown any effectiveness against viruses or COVID in particular.
A New York ED doctor summed it up best in the Rolling Stone article when he was told anti-vaxxers were gargling iodine: He offered a choice four-letter expletive, then said, “Of course they are.”
But wait! We’ve got a two-for-one deal on dubious COVID cures this week. Health experts in Myanmar (Burma to all the “Seinfeld” fans) and Thailand have been combating social media posts claiming that onion fumes will cure COVID. All you need to do is slice an onion in half, sniff it for a while, then chew on a second onion, and your COVID will be cured!
In what is surely the most radical understatement of the year, a professor in the department of preventive and social medicine at Chulalongkorn University, Bangkok, said in the AFP article that there is “no solid evidence” to support onion sniffing from “any clinical research.”
We’re just going to assume the expletives that surely followed were kept off the record.
Pro-Trump state governor encourages vaccination
Clearly, the politics of COVID-19 have been working against the science of COVID-19. Politicians can’t, or won’t, agree on what to do about it, and many prominent Republicans have been actively resisting vaccine and mask mandates.
There is at least one Republican governor who has wholeheartedly encouraged vaccination in his pro-Trump state. We’re talking about Gov. Jim Justice of West Virginia, and not for the first time.
The Washington Post has detailed his efforts to promote the COVID vaccine, and we would like to share a couple of examples.
In June he suggested that people who didn’t get vaccinated were “entering the death drawing.” He followed that by saying, “If I knew for certain that there was going to be eight or nine people die by next Tuesday, and I could be one of them if I don’t take the vaccine ... What in the world do you think I would do? I mean, I would run over top of somebody.”
More recently, Gov. Justice took on vaccine conspiracy theories.
“For God’s sakes a livin’, how difficult is this to understand? Why in the world do we have to come up with these crazy ideas – and they’re crazy ideas – that the vaccine’s got something in it and it’s tracing people wherever they go? And the very same people that are saying that are carrying their cellphones around. I mean, come on. Come on.”
Nuff said.
Jet lag may be a gut feeling
After a week-long vacation halfway around the world, it’s time to go back to your usual routine and time zone. But don’t forget about that free souvenir, jet lag. A disrupted circadian rhythm can be a real bummer, but researchers may have found the fix in your belly.
In a study funded by the U.S. Navy, researchers at the University of Colorado, Boulder, looked into how the presence of a prebiotic in one’s diet can have on the disrupted biological clocks. They’re not the same as probiotics, which help you stay regular in another way. Prebiotics work as food to help the good gut bacteria you already have. An earlier study had suggested that prebiotics may have a positive effect on the brain.
To test the theory, the researchers gave one group of rats their regular food while another group received food with two different prebiotics. After manipulating the rats’ light-dark cycle for 8 weeks to give the illusion of traveling to a time zone 12 hours ahead every week, they found that the rats who ate the prebiotics were able to bounce back faster.
The possibility of ingesting something to keep your body clock regular sounds like a dream, but the researchers don’t really advise you to snatch all the supplements you can at your local pharmacy just yet.
“If you know you are going to come into a challenge, you could take a look at some of the prebiotics that are available. Just realize that they are not customized yet, so it might work for you but it won’t work for your neighbor,” said senior author Monika Fleshner.
Until there’s more conclusive research, just be good to your bacteria.
How to make stuff up and influence people
You’ve probably heard that we use only 10% of our brain. It’s right up there with “the Earth is flat” and “an apple a day keeps the doctor away.”
The idea that we use only 10% of our brains can probably be traced back to the early 1900s, suggests Discover magazine, when psychologist William James wrote, “Compared with what we ought to be, we are only half awake. Our fires are damped, our drafts are checked. We are making use of only a small part of our possible mental and physical resources.”
There are many different takes on it, but it is indeed a myth that we use only 10% of our brains. Dale Carnegie, the public speaking teacher, seems to be the one who put the specific number of 10% on James’ idea in his 1936 book, “How to Win Friends and Influence People.”
“We think that people are excited by this pseudo fact because it’s very optimistic,” neuroscientist Sandra Aamodt told Discover. “Wouldn’t we all love to think our brains had some giant pool of untapped potential that we’re not using?”
The reality is, we do use our whole brain. Functional MRI shows that different parts of the brain are used for different things such as language and memories. “Not all at the same time, of course. But every part of the brain has a job to do,” the Discover article explained.
There are many things we don’t know about how the brain works, but at least you know you use more than 10%. After all, a brain just told you so.
CBT via telehealth or in-person: Which is best for insomnia?
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Staying up to date with consumer sleep technology
With Siri and Alexa sitting at our kitchen tables and listening to our conversations, we have all but forgotten about the before times – when we had to use the Yellow Pages to look up a number or address and when we had no idea how many steps we took in a given day. Wearable technology has become ubiquitous and has us watching not only our step count but also our sleep. Did I get enough deep sleep? What does my sleep score of 82 mean? Should I be worried?
As clinicians, we must also navigate how this information impacts our clinical decision-making and consider how our patients are interpreting these data on a daily basis. There is an inherent assumption that we, as sleep clinicians, will understand the nuances of each consumer-facing sleep technology (CST) whether it is a wearable, a nearable (a device that sits near the body but not on the body), or an app. Very little validation data exist, as most of these technologies are marketed as wellness devices and are not intended to render a diagnosis. It therefore falls to us to determine how to utilize this information in an already busy clinic.
One strategy is to use these technologies as patient engagement tools – a way to increase public awareness of the importance of sleep. While this certainly should be beneficial, oftentimes, the data are confusing and can lead to misunderstandings about what normal sleep should look like. Approaching these data as partners to our patients allows us to set expectations around normal sleep cycles and sleep duration. It also allows us to discuss appropriate sleep timing and sleep hygiene.
Many wearable devices have incorporated oximetry into their metrics, and some claim to have accuracy that is better than hospital-grade oximeters. Many of these companies are no longer in business. Others specify higher accuracy in dark-skinned individuals (“CIRCUL Ring Pulse Oximeter in Dark-Pigmented Individuals: Clinical Study Validates Efficacy and Reliability,” Medical Device News Magazine, Feb. 26, 2021).
Despite these claims, they are registered as wellness devices with the FDA and are not diagnostic devices. Logically, if one of these devices demonstrates worrisome data, then it can prompt further clinical queries and, potentially, objective testing for obstructive sleep apnea (OSA). The reverse, however, cannot be claimed. A normal reading by CST does not obviate the need for objective testing if the clinical symptoms warrant it.
There are CSTs that have been created around very specific needs - such as jet lag- and provide guidance for how to quickly acclimate to the destination time zone by providing nudges for light exposure and timed melatonin or dark glasses (https://www.timeshifter.com/).
Others analyze the sleep space for extrinsic sounds (https://www.sleepcycle.com/), while a plethora of apps provides advice for how to optimize your sleep environment and wind-down routine. There is even a sleep robot designed to facilitate sleep onset (https://somnox.com/). This bean-shaped device is designed to “breathe” as you hold it, and the user is meant to emulate those same breathing patterns. It is a take on the 4-7-8 breathing pattern long endorsed by yogis.
Although validation data are lacking for the vast majority of CST, a recent study (www.ncbi.nlm.nih.gov/pmc/articles/PMC8120339/pdf/zsaa291.pdf).demonstrated that CST had high performance when compared with actigraphy in assessing sleep and wakefulness and, as such, may improve the evaluation of sleep and wake opportunities prior to MSLT or improve identification of circadian sleep-wake disorders. Many practices do not currently utilize actigraphy due to its expense and very limited potential for reimbursement. Using a patient’s sleep-tracking device may allow access to these data without financial outlay. While these data demonstrate the ability of CST to potentially differentiate sleep from wakefulness, it is notable that this study also found that the determination of individual sleep stages is less robust. In general, CST cannot identify an underlying sleep disorder, however, may raise awareness that a disorder might be present.
This leads to more reflection on the role of CST in a typical sleep clinic. Many years ago, discussion around this technology was primarily patient-initiated and often times met with skepticism on the part of the clinician. As technology has improved and has become more accessible, there appears to be more acceptance among our colleagues – not, perhaps, in terms of absolute actionable data, but rather as an opportunity to discuss sleep with our patients and to support their own efforts at improving their sleep. Trends in the data in response to CBT-I or medications can be observed. Abnormalities identified via CST often serve as the initial prompt for a clinical visit and, as such, should not be eschewed. Rather, reframing the use of this information while also addressing other sleep issues is likely to be the more appropriate path forward.
Assessing this information can be time-consuming, and best practice suggests establishing expectations around this process (J Clin Sleep Med 2018 May 15. doi: 10.5664/jcsm.7128).
Agreements can be made with patients that the data are reviewed in the context of a clinical visit rather than longitudinally as data are uploaded and then sent via messaging unless such an understanding has already been agreed upon. RPM billing codes may ultimately allow for reimbursement and recognition of this workload. At the present time, RPM billing is limited to FDA-cleared, prescription devices, and CST does not yet qualify.
There also needs to be recognition of potential harm from CST. Inevitably, some patients will develop orthosomnia, a term coined by Dr. Kelly Baron, where patients become so fixated on achieving perfect sleep scores that it contributes to insomnia. In this case, identification of orthosomnia is made via the clinical visit and patients are advised to stop tracking their sleep for a set period of time. This allows the anxiety around achieving “perfect sleep” to dissipate.
Google and the AASM recently announced a partnership. Essentially, the Google Nest Hub will serve to detect sleep concerns (such as timing of sleep, snoring, insufficient sleep, etc.) and will direct the user to educational resources such as www.sleepeducation.org. The idea behind this is that people are often unaware of an underlying sleep disorder such as OSA and don’t know what to search for. The Nest Hub uses information it collects and directs users to appropriate resources, thus obviating the need to know what to Google.
Clearly, big tech has invested heavily in our field. Between the copious wearables, nearables, and apps that are sleep-focused, these industry giants obviously believe that sleep is worthy of such a significant allocation of resources. This has improved the overall awareness of the importance of sleep and of identifying and treating sleep disorders. While these technologies are no replacement for a clinical evaluation, they can serve as patient engagement tools, as well as potentially large-scale OSA screening tools and may help us improve the percentage of patients with undiagnosed OSA, estimated to be 80% (Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, 2016).
CST may allow us to better identify circadian sleep-wake disorders and evaluate sleep satiation prior to MLST that no longer requires investment in expensive actigraphy devices. They also allow us to partner with our patients by meeting them where they are and recognizing the efforts they have already made to improve their sleep before we even meet them.
Dr. Khosla is Medical Director, North Dakota Center for Sleep, Fargo, North Dakota.
With Siri and Alexa sitting at our kitchen tables and listening to our conversations, we have all but forgotten about the before times – when we had to use the Yellow Pages to look up a number or address and when we had no idea how many steps we took in a given day. Wearable technology has become ubiquitous and has us watching not only our step count but also our sleep. Did I get enough deep sleep? What does my sleep score of 82 mean? Should I be worried?
As clinicians, we must also navigate how this information impacts our clinical decision-making and consider how our patients are interpreting these data on a daily basis. There is an inherent assumption that we, as sleep clinicians, will understand the nuances of each consumer-facing sleep technology (CST) whether it is a wearable, a nearable (a device that sits near the body but not on the body), or an app. Very little validation data exist, as most of these technologies are marketed as wellness devices and are not intended to render a diagnosis. It therefore falls to us to determine how to utilize this information in an already busy clinic.
One strategy is to use these technologies as patient engagement tools – a way to increase public awareness of the importance of sleep. While this certainly should be beneficial, oftentimes, the data are confusing and can lead to misunderstandings about what normal sleep should look like. Approaching these data as partners to our patients allows us to set expectations around normal sleep cycles and sleep duration. It also allows us to discuss appropriate sleep timing and sleep hygiene.
Many wearable devices have incorporated oximetry into their metrics, and some claim to have accuracy that is better than hospital-grade oximeters. Many of these companies are no longer in business. Others specify higher accuracy in dark-skinned individuals (“CIRCUL Ring Pulse Oximeter in Dark-Pigmented Individuals: Clinical Study Validates Efficacy and Reliability,” Medical Device News Magazine, Feb. 26, 2021).
Despite these claims, they are registered as wellness devices with the FDA and are not diagnostic devices. Logically, if one of these devices demonstrates worrisome data, then it can prompt further clinical queries and, potentially, objective testing for obstructive sleep apnea (OSA). The reverse, however, cannot be claimed. A normal reading by CST does not obviate the need for objective testing if the clinical symptoms warrant it.
There are CSTs that have been created around very specific needs - such as jet lag- and provide guidance for how to quickly acclimate to the destination time zone by providing nudges for light exposure and timed melatonin or dark glasses (https://www.timeshifter.com/).
Others analyze the sleep space for extrinsic sounds (https://www.sleepcycle.com/), while a plethora of apps provides advice for how to optimize your sleep environment and wind-down routine. There is even a sleep robot designed to facilitate sleep onset (https://somnox.com/). This bean-shaped device is designed to “breathe” as you hold it, and the user is meant to emulate those same breathing patterns. It is a take on the 4-7-8 breathing pattern long endorsed by yogis.
Although validation data are lacking for the vast majority of CST, a recent study (www.ncbi.nlm.nih.gov/pmc/articles/PMC8120339/pdf/zsaa291.pdf).demonstrated that CST had high performance when compared with actigraphy in assessing sleep and wakefulness and, as such, may improve the evaluation of sleep and wake opportunities prior to MSLT or improve identification of circadian sleep-wake disorders. Many practices do not currently utilize actigraphy due to its expense and very limited potential for reimbursement. Using a patient’s sleep-tracking device may allow access to these data without financial outlay. While these data demonstrate the ability of CST to potentially differentiate sleep from wakefulness, it is notable that this study also found that the determination of individual sleep stages is less robust. In general, CST cannot identify an underlying sleep disorder, however, may raise awareness that a disorder might be present.
This leads to more reflection on the role of CST in a typical sleep clinic. Many years ago, discussion around this technology was primarily patient-initiated and often times met with skepticism on the part of the clinician. As technology has improved and has become more accessible, there appears to be more acceptance among our colleagues – not, perhaps, in terms of absolute actionable data, but rather as an opportunity to discuss sleep with our patients and to support their own efforts at improving their sleep. Trends in the data in response to CBT-I or medications can be observed. Abnormalities identified via CST often serve as the initial prompt for a clinical visit and, as such, should not be eschewed. Rather, reframing the use of this information while also addressing other sleep issues is likely to be the more appropriate path forward.
Assessing this information can be time-consuming, and best practice suggests establishing expectations around this process (J Clin Sleep Med 2018 May 15. doi: 10.5664/jcsm.7128).
Agreements can be made with patients that the data are reviewed in the context of a clinical visit rather than longitudinally as data are uploaded and then sent via messaging unless such an understanding has already been agreed upon. RPM billing codes may ultimately allow for reimbursement and recognition of this workload. At the present time, RPM billing is limited to FDA-cleared, prescription devices, and CST does not yet qualify.
There also needs to be recognition of potential harm from CST. Inevitably, some patients will develop orthosomnia, a term coined by Dr. Kelly Baron, where patients become so fixated on achieving perfect sleep scores that it contributes to insomnia. In this case, identification of orthosomnia is made via the clinical visit and patients are advised to stop tracking their sleep for a set period of time. This allows the anxiety around achieving “perfect sleep” to dissipate.
Google and the AASM recently announced a partnership. Essentially, the Google Nest Hub will serve to detect sleep concerns (such as timing of sleep, snoring, insufficient sleep, etc.) and will direct the user to educational resources such as www.sleepeducation.org. The idea behind this is that people are often unaware of an underlying sleep disorder such as OSA and don’t know what to search for. The Nest Hub uses information it collects and directs users to appropriate resources, thus obviating the need to know what to Google.
Clearly, big tech has invested heavily in our field. Between the copious wearables, nearables, and apps that are sleep-focused, these industry giants obviously believe that sleep is worthy of such a significant allocation of resources. This has improved the overall awareness of the importance of sleep and of identifying and treating sleep disorders. While these technologies are no replacement for a clinical evaluation, they can serve as patient engagement tools, as well as potentially large-scale OSA screening tools and may help us improve the percentage of patients with undiagnosed OSA, estimated to be 80% (Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, 2016).
CST may allow us to better identify circadian sleep-wake disorders and evaluate sleep satiation prior to MLST that no longer requires investment in expensive actigraphy devices. They also allow us to partner with our patients by meeting them where they are and recognizing the efforts they have already made to improve their sleep before we even meet them.
Dr. Khosla is Medical Director, North Dakota Center for Sleep, Fargo, North Dakota.
With Siri and Alexa sitting at our kitchen tables and listening to our conversations, we have all but forgotten about the before times – when we had to use the Yellow Pages to look up a number or address and when we had no idea how many steps we took in a given day. Wearable technology has become ubiquitous and has us watching not only our step count but also our sleep. Did I get enough deep sleep? What does my sleep score of 82 mean? Should I be worried?
As clinicians, we must also navigate how this information impacts our clinical decision-making and consider how our patients are interpreting these data on a daily basis. There is an inherent assumption that we, as sleep clinicians, will understand the nuances of each consumer-facing sleep technology (CST) whether it is a wearable, a nearable (a device that sits near the body but not on the body), or an app. Very little validation data exist, as most of these technologies are marketed as wellness devices and are not intended to render a diagnosis. It therefore falls to us to determine how to utilize this information in an already busy clinic.
One strategy is to use these technologies as patient engagement tools – a way to increase public awareness of the importance of sleep. While this certainly should be beneficial, oftentimes, the data are confusing and can lead to misunderstandings about what normal sleep should look like. Approaching these data as partners to our patients allows us to set expectations around normal sleep cycles and sleep duration. It also allows us to discuss appropriate sleep timing and sleep hygiene.
Many wearable devices have incorporated oximetry into their metrics, and some claim to have accuracy that is better than hospital-grade oximeters. Many of these companies are no longer in business. Others specify higher accuracy in dark-skinned individuals (“CIRCUL Ring Pulse Oximeter in Dark-Pigmented Individuals: Clinical Study Validates Efficacy and Reliability,” Medical Device News Magazine, Feb. 26, 2021).
Despite these claims, they are registered as wellness devices with the FDA and are not diagnostic devices. Logically, if one of these devices demonstrates worrisome data, then it can prompt further clinical queries and, potentially, objective testing for obstructive sleep apnea (OSA). The reverse, however, cannot be claimed. A normal reading by CST does not obviate the need for objective testing if the clinical symptoms warrant it.
There are CSTs that have been created around very specific needs - such as jet lag- and provide guidance for how to quickly acclimate to the destination time zone by providing nudges for light exposure and timed melatonin or dark glasses (https://www.timeshifter.com/).
Others analyze the sleep space for extrinsic sounds (https://www.sleepcycle.com/), while a plethora of apps provides advice for how to optimize your sleep environment and wind-down routine. There is even a sleep robot designed to facilitate sleep onset (https://somnox.com/). This bean-shaped device is designed to “breathe” as you hold it, and the user is meant to emulate those same breathing patterns. It is a take on the 4-7-8 breathing pattern long endorsed by yogis.
Although validation data are lacking for the vast majority of CST, a recent study (www.ncbi.nlm.nih.gov/pmc/articles/PMC8120339/pdf/zsaa291.pdf).demonstrated that CST had high performance when compared with actigraphy in assessing sleep and wakefulness and, as such, may improve the evaluation of sleep and wake opportunities prior to MSLT or improve identification of circadian sleep-wake disorders. Many practices do not currently utilize actigraphy due to its expense and very limited potential for reimbursement. Using a patient’s sleep-tracking device may allow access to these data without financial outlay. While these data demonstrate the ability of CST to potentially differentiate sleep from wakefulness, it is notable that this study also found that the determination of individual sleep stages is less robust. In general, CST cannot identify an underlying sleep disorder, however, may raise awareness that a disorder might be present.
This leads to more reflection on the role of CST in a typical sleep clinic. Many years ago, discussion around this technology was primarily patient-initiated and often times met with skepticism on the part of the clinician. As technology has improved and has become more accessible, there appears to be more acceptance among our colleagues – not, perhaps, in terms of absolute actionable data, but rather as an opportunity to discuss sleep with our patients and to support their own efforts at improving their sleep. Trends in the data in response to CBT-I or medications can be observed. Abnormalities identified via CST often serve as the initial prompt for a clinical visit and, as such, should not be eschewed. Rather, reframing the use of this information while also addressing other sleep issues is likely to be the more appropriate path forward.
Assessing this information can be time-consuming, and best practice suggests establishing expectations around this process (J Clin Sleep Med 2018 May 15. doi: 10.5664/jcsm.7128).
Agreements can be made with patients that the data are reviewed in the context of a clinical visit rather than longitudinally as data are uploaded and then sent via messaging unless such an understanding has already been agreed upon. RPM billing codes may ultimately allow for reimbursement and recognition of this workload. At the present time, RPM billing is limited to FDA-cleared, prescription devices, and CST does not yet qualify.
There also needs to be recognition of potential harm from CST. Inevitably, some patients will develop orthosomnia, a term coined by Dr. Kelly Baron, where patients become so fixated on achieving perfect sleep scores that it contributes to insomnia. In this case, identification of orthosomnia is made via the clinical visit and patients are advised to stop tracking their sleep for a set period of time. This allows the anxiety around achieving “perfect sleep” to dissipate.
Google and the AASM recently announced a partnership. Essentially, the Google Nest Hub will serve to detect sleep concerns (such as timing of sleep, snoring, insufficient sleep, etc.) and will direct the user to educational resources such as www.sleepeducation.org. The idea behind this is that people are often unaware of an underlying sleep disorder such as OSA and don’t know what to search for. The Nest Hub uses information it collects and directs users to appropriate resources, thus obviating the need to know what to Google.
Clearly, big tech has invested heavily in our field. Between the copious wearables, nearables, and apps that are sleep-focused, these industry giants obviously believe that sleep is worthy of such a significant allocation of resources. This has improved the overall awareness of the importance of sleep and of identifying and treating sleep disorders. While these technologies are no replacement for a clinical evaluation, they can serve as patient engagement tools, as well as potentially large-scale OSA screening tools and may help us improve the percentage of patients with undiagnosed OSA, estimated to be 80% (Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, 2016).
CST may allow us to better identify circadian sleep-wake disorders and evaluate sleep satiation prior to MLST that no longer requires investment in expensive actigraphy devices. They also allow us to partner with our patients by meeting them where they are and recognizing the efforts they have already made to improve their sleep before we even meet them.
Dr. Khosla is Medical Director, North Dakota Center for Sleep, Fargo, North Dakota.
The future of Advanced Practice Providers (APPs) in sleep clinics and telemedicine post-pandemic
Loretta J. Colvin, APRN, ACNP-BC, is a Nurse Practitioner at Sleep Services, SSM Health Medical Group, specializing in the treatment of sleep disorders. Her focus is on insomnia, narcolepsy, obstructive sleep apnea, parasomnias, periodic leg movement disorder, restless leg syndrome, sleep disorders, snoring and telehealth.
Q: As a nurse practitioner and a specialist at a clinic focused on identifying sleep related disorders, what do you feel is the overall value of such a clinic as a therapeutic need for patients?
Ms. Colvin: Well, for us in sleep, we've experienced a growth in our field, and anticipate further growth. We know that many people remain undiagnosed with their sleep disorders. So, we see our role as filling a need for the public in providing more personalized and specialized care for those that have a sleep problem.
Patients get to us via many routes, including self-referral or referral by their primary care provider or specialist. We help these patients identify their sleep problems, guide them in testing and treatment decisions, and provide on-going treatment support.
Currently, there are two areas in which there is a particular need. With current stressors impacting our society, there is an increased need for patients to discuss their insomnia or sleep difficulty concerns with a healthcare provider. We are seeing more patients bring up insomnia concerns to their primary care providers or coming directly to our sleep clinic for discussion of these concerns. As the recognition of the importance of diagnosing and treatment sleep apnea continues to grow, we see more patients coming to us for care, including those with less obvious symptoms but high risk of sleep apnea due to their comorbid diseases.
Q: Given current predictions that the outpatient health care structure will change and the number of APRNs and PAs will increase, what is your perspective on role and utilization of APPs, as well as the need to plan for the future care of patients with sleep disorders?
Ms. Colvin: First, let me talk about the national landscape with regards to structure. Nationally, the APP role and the number of professionals in that role is growing, so that's going to help meet some of the needs of our society for providing health care, whether it be primary care or specialty care, like I do, or acute care in the hospital. At present, there are a significant number of places where we fill a needed role but within the area of sleep, there is a likely to be an increase in need for APPs as a result of attrition in the field as well as a shift in how many physicians are available to provide care in our ever-expanding specialty. What we then need to do is figure out how do we train these Providers in a specialty? This is not a specialty that is a large part of our basic education, so how do we train people into that specialty? And how do we prepare them for their role and ensure that we are offering opportunities to expand their capabilities over time?
An example of this can be seen with regards to the opportunities now being offered in telehealth in behavioral sleep medicine and in working with conditions like insomnia, or with people who have difficulty in trying to adjust to Continuous Positive Airway Pressure (CPAP) therapy and might need additional assistance and coaching.
Within my organization, physicians will refer patients directly to me who have struggled to use PAP in the past. With specialized guidance, these past struggles can often be overcome thanks to improvements in our equipment and technology, patient knowledge and acceptance combined with personalized specialty care. I have had good success with helping patients who were not successful using PAP 10 or 20 years ago to become successful through guidance and coaching. When we encounter anxiety or claustrophobia with PAP, we can incorporate behavioral sleep principles into the patient’s care to help them better acclimate to PAP therapy or consider alternative therapies.
Q: With more than 70 million US adults affected by sleep disorders and a growing number of clinicians and sleep practitioners gaining expertise in virtual models for diagnosis and treatments, what is your approach to using the telehealth to provide the same level of support, education, and therapy at home versus in the office?
Ms. Colvin: The pandemic definitely pushed us farther along in how we use telehealth. Before the pandemic, I was utilizing it in small increments, but there were some limits as a result of either regulation or reimbursement that caused it to not be included as a larger part of our program. However, now that we've experienced this shift with the pandemic, our health system has invested more in technology, and exposed more patients to the experience, I think telehealth and our usage of it will be different once we come out on the other side of this public health crisis. So, now we must decide, how are we going to use this mode as an alternative model of care?
I see two main focuses for us in sleep—expanding patient access and patient convenience. As technology improves, it will expand access for patients with less accessibility to technology and the internet, such as those in rural areas. And with smartphones becoming even more readily available and more capable of doing virtual care, we see potential to reach out and treat patients who we would otherwise not be able to offer treatment to.
Patient convenience is also very important. With virtual visits, we may be able to keep patients from having to leave work as they may be able to just ‘pop out’ at lunch, have a visit, and then go right back to work. Doing so also helps if patients have care giving responsibilities as they don't have to, for example, find a babysitter to come in for an office visit as they can make the necessary arrangements from home.
In lockstep with patient access and convenience, I am interested to see how telehealth, over time, manifests for patients with disabilities but we are already seeing the benefits of its application within this population.
I have a patient who is confined to a wheelchair so for this patient to get to a visit requires significant planning time to get into the van and be driven to the clinic by his caregiver, who has to schedule time off from work. So, it is not an easy process for this patient to come in and see me for a quick visit. With telehealth, this simple visit doesn’t have to be a whole- or half-day affair as it can be a quick check-in. If an in-person visit is warranted, we can always arrange that but usually we can accomplish what we need to on video and audio.
Another example is with those patients with hearing impairments. Depending on the impairment, certain patients may be able to use Bluetooth or audio enhancement with their hearing aids and can actually hear me better in a video environment than they can in the clinic; especially at this point in time as we are masked when in the office.
Q: In what ways do you think the telemedicine diagnosis process might be impacted post-pandemic?
Ms. Colvin: At-home sleep testing became available several years ago, but it has a limited role as it is specifically for the diagnosis of sleep apnea in the uncomplicated patient. Telehealth offers some convenience in enabling patients to be tested in their home and it is also more affordable for the patient and for insurance. In fact, this is seen as one of the disruptors in our field that will continue to expand in the appropriate patient populations. But we will always have to acknowledge that it won't serve all patient needs because our more complex patients still need to come in for in-person testing.
Q: Overall, in what ways do sleep professionals support the value of having a specialist care model versus a generalist PCP model to perform patient care within the US as well as other countries?
Ms. Colvin: From my view, I see that our PCPs are already stretched thin in their ability to provide easily accessible care and I think it would be difficult for them to also provide the specialty care that patients with sleep disorders need. Some of the less complex patients might be able to stay within a primary care environment but as technology, as well as the software training that is required to be able to communicate with the devices our patients use for treatment or for diagnosis, continues to become more complex, it can become difficult to manage through the primary care environment.
The question then goes back to, how can we be as accessible as possible in an underserved area or where the specialty clinic is not easy to access? I think this is where telehealth may give us new options for expanding access to patients who can use the technology that is available.
Loretta J. Colvin, APRN, ACNP-BC, is a Nurse Practitioner at Sleep Services, SSM Health Medical Group, specializing in the treatment of sleep disorders. Her focus is on insomnia, narcolepsy, obstructive sleep apnea, parasomnias, periodic leg movement disorder, restless leg syndrome, sleep disorders, snoring and telehealth.
Q: As a nurse practitioner and a specialist at a clinic focused on identifying sleep related disorders, what do you feel is the overall value of such a clinic as a therapeutic need for patients?
Ms. Colvin: Well, for us in sleep, we've experienced a growth in our field, and anticipate further growth. We know that many people remain undiagnosed with their sleep disorders. So, we see our role as filling a need for the public in providing more personalized and specialized care for those that have a sleep problem.
Patients get to us via many routes, including self-referral or referral by their primary care provider or specialist. We help these patients identify their sleep problems, guide them in testing and treatment decisions, and provide on-going treatment support.
Currently, there are two areas in which there is a particular need. With current stressors impacting our society, there is an increased need for patients to discuss their insomnia or sleep difficulty concerns with a healthcare provider. We are seeing more patients bring up insomnia concerns to their primary care providers or coming directly to our sleep clinic for discussion of these concerns. As the recognition of the importance of diagnosing and treatment sleep apnea continues to grow, we see more patients coming to us for care, including those with less obvious symptoms but high risk of sleep apnea due to their comorbid diseases.
Q: Given current predictions that the outpatient health care structure will change and the number of APRNs and PAs will increase, what is your perspective on role and utilization of APPs, as well as the need to plan for the future care of patients with sleep disorders?
Ms. Colvin: First, let me talk about the national landscape with regards to structure. Nationally, the APP role and the number of professionals in that role is growing, so that's going to help meet some of the needs of our society for providing health care, whether it be primary care or specialty care, like I do, or acute care in the hospital. At present, there are a significant number of places where we fill a needed role but within the area of sleep, there is a likely to be an increase in need for APPs as a result of attrition in the field as well as a shift in how many physicians are available to provide care in our ever-expanding specialty. What we then need to do is figure out how do we train these Providers in a specialty? This is not a specialty that is a large part of our basic education, so how do we train people into that specialty? And how do we prepare them for their role and ensure that we are offering opportunities to expand their capabilities over time?
An example of this can be seen with regards to the opportunities now being offered in telehealth in behavioral sleep medicine and in working with conditions like insomnia, or with people who have difficulty in trying to adjust to Continuous Positive Airway Pressure (CPAP) therapy and might need additional assistance and coaching.
Within my organization, physicians will refer patients directly to me who have struggled to use PAP in the past. With specialized guidance, these past struggles can often be overcome thanks to improvements in our equipment and technology, patient knowledge and acceptance combined with personalized specialty care. I have had good success with helping patients who were not successful using PAP 10 or 20 years ago to become successful through guidance and coaching. When we encounter anxiety or claustrophobia with PAP, we can incorporate behavioral sleep principles into the patient’s care to help them better acclimate to PAP therapy or consider alternative therapies.
Q: With more than 70 million US adults affected by sleep disorders and a growing number of clinicians and sleep practitioners gaining expertise in virtual models for diagnosis and treatments, what is your approach to using the telehealth to provide the same level of support, education, and therapy at home versus in the office?
Ms. Colvin: The pandemic definitely pushed us farther along in how we use telehealth. Before the pandemic, I was utilizing it in small increments, but there were some limits as a result of either regulation or reimbursement that caused it to not be included as a larger part of our program. However, now that we've experienced this shift with the pandemic, our health system has invested more in technology, and exposed more patients to the experience, I think telehealth and our usage of it will be different once we come out on the other side of this public health crisis. So, now we must decide, how are we going to use this mode as an alternative model of care?
I see two main focuses for us in sleep—expanding patient access and patient convenience. As technology improves, it will expand access for patients with less accessibility to technology and the internet, such as those in rural areas. And with smartphones becoming even more readily available and more capable of doing virtual care, we see potential to reach out and treat patients who we would otherwise not be able to offer treatment to.
Patient convenience is also very important. With virtual visits, we may be able to keep patients from having to leave work as they may be able to just ‘pop out’ at lunch, have a visit, and then go right back to work. Doing so also helps if patients have care giving responsibilities as they don't have to, for example, find a babysitter to come in for an office visit as they can make the necessary arrangements from home.
In lockstep with patient access and convenience, I am interested to see how telehealth, over time, manifests for patients with disabilities but we are already seeing the benefits of its application within this population.
I have a patient who is confined to a wheelchair so for this patient to get to a visit requires significant planning time to get into the van and be driven to the clinic by his caregiver, who has to schedule time off from work. So, it is not an easy process for this patient to come in and see me for a quick visit. With telehealth, this simple visit doesn’t have to be a whole- or half-day affair as it can be a quick check-in. If an in-person visit is warranted, we can always arrange that but usually we can accomplish what we need to on video and audio.
Another example is with those patients with hearing impairments. Depending on the impairment, certain patients may be able to use Bluetooth or audio enhancement with their hearing aids and can actually hear me better in a video environment than they can in the clinic; especially at this point in time as we are masked when in the office.
Q: In what ways do you think the telemedicine diagnosis process might be impacted post-pandemic?
Ms. Colvin: At-home sleep testing became available several years ago, but it has a limited role as it is specifically for the diagnosis of sleep apnea in the uncomplicated patient. Telehealth offers some convenience in enabling patients to be tested in their home and it is also more affordable for the patient and for insurance. In fact, this is seen as one of the disruptors in our field that will continue to expand in the appropriate patient populations. But we will always have to acknowledge that it won't serve all patient needs because our more complex patients still need to come in for in-person testing.
Q: Overall, in what ways do sleep professionals support the value of having a specialist care model versus a generalist PCP model to perform patient care within the US as well as other countries?
Ms. Colvin: From my view, I see that our PCPs are already stretched thin in their ability to provide easily accessible care and I think it would be difficult for them to also provide the specialty care that patients with sleep disorders need. Some of the less complex patients might be able to stay within a primary care environment but as technology, as well as the software training that is required to be able to communicate with the devices our patients use for treatment or for diagnosis, continues to become more complex, it can become difficult to manage through the primary care environment.
The question then goes back to, how can we be as accessible as possible in an underserved area or where the specialty clinic is not easy to access? I think this is where telehealth may give us new options for expanding access to patients who can use the technology that is available.
Loretta J. Colvin, APRN, ACNP-BC, is a Nurse Practitioner at Sleep Services, SSM Health Medical Group, specializing in the treatment of sleep disorders. Her focus is on insomnia, narcolepsy, obstructive sleep apnea, parasomnias, periodic leg movement disorder, restless leg syndrome, sleep disorders, snoring and telehealth.
Q: As a nurse practitioner and a specialist at a clinic focused on identifying sleep related disorders, what do you feel is the overall value of such a clinic as a therapeutic need for patients?
Ms. Colvin: Well, for us in sleep, we've experienced a growth in our field, and anticipate further growth. We know that many people remain undiagnosed with their sleep disorders. So, we see our role as filling a need for the public in providing more personalized and specialized care for those that have a sleep problem.
Patients get to us via many routes, including self-referral or referral by their primary care provider or specialist. We help these patients identify their sleep problems, guide them in testing and treatment decisions, and provide on-going treatment support.
Currently, there are two areas in which there is a particular need. With current stressors impacting our society, there is an increased need for patients to discuss their insomnia or sleep difficulty concerns with a healthcare provider. We are seeing more patients bring up insomnia concerns to their primary care providers or coming directly to our sleep clinic for discussion of these concerns. As the recognition of the importance of diagnosing and treatment sleep apnea continues to grow, we see more patients coming to us for care, including those with less obvious symptoms but high risk of sleep apnea due to their comorbid diseases.
Q: Given current predictions that the outpatient health care structure will change and the number of APRNs and PAs will increase, what is your perspective on role and utilization of APPs, as well as the need to plan for the future care of patients with sleep disorders?
Ms. Colvin: First, let me talk about the national landscape with regards to structure. Nationally, the APP role and the number of professionals in that role is growing, so that's going to help meet some of the needs of our society for providing health care, whether it be primary care or specialty care, like I do, or acute care in the hospital. At present, there are a significant number of places where we fill a needed role but within the area of sleep, there is a likely to be an increase in need for APPs as a result of attrition in the field as well as a shift in how many physicians are available to provide care in our ever-expanding specialty. What we then need to do is figure out how do we train these Providers in a specialty? This is not a specialty that is a large part of our basic education, so how do we train people into that specialty? And how do we prepare them for their role and ensure that we are offering opportunities to expand their capabilities over time?
An example of this can be seen with regards to the opportunities now being offered in telehealth in behavioral sleep medicine and in working with conditions like insomnia, or with people who have difficulty in trying to adjust to Continuous Positive Airway Pressure (CPAP) therapy and might need additional assistance and coaching.
Within my organization, physicians will refer patients directly to me who have struggled to use PAP in the past. With specialized guidance, these past struggles can often be overcome thanks to improvements in our equipment and technology, patient knowledge and acceptance combined with personalized specialty care. I have had good success with helping patients who were not successful using PAP 10 or 20 years ago to become successful through guidance and coaching. When we encounter anxiety or claustrophobia with PAP, we can incorporate behavioral sleep principles into the patient’s care to help them better acclimate to PAP therapy or consider alternative therapies.
Q: With more than 70 million US adults affected by sleep disorders and a growing number of clinicians and sleep practitioners gaining expertise in virtual models for diagnosis and treatments, what is your approach to using the telehealth to provide the same level of support, education, and therapy at home versus in the office?
Ms. Colvin: The pandemic definitely pushed us farther along in how we use telehealth. Before the pandemic, I was utilizing it in small increments, but there were some limits as a result of either regulation or reimbursement that caused it to not be included as a larger part of our program. However, now that we've experienced this shift with the pandemic, our health system has invested more in technology, and exposed more patients to the experience, I think telehealth and our usage of it will be different once we come out on the other side of this public health crisis. So, now we must decide, how are we going to use this mode as an alternative model of care?
I see two main focuses for us in sleep—expanding patient access and patient convenience. As technology improves, it will expand access for patients with less accessibility to technology and the internet, such as those in rural areas. And with smartphones becoming even more readily available and more capable of doing virtual care, we see potential to reach out and treat patients who we would otherwise not be able to offer treatment to.
Patient convenience is also very important. With virtual visits, we may be able to keep patients from having to leave work as they may be able to just ‘pop out’ at lunch, have a visit, and then go right back to work. Doing so also helps if patients have care giving responsibilities as they don't have to, for example, find a babysitter to come in for an office visit as they can make the necessary arrangements from home.
In lockstep with patient access and convenience, I am interested to see how telehealth, over time, manifests for patients with disabilities but we are already seeing the benefits of its application within this population.
I have a patient who is confined to a wheelchair so for this patient to get to a visit requires significant planning time to get into the van and be driven to the clinic by his caregiver, who has to schedule time off from work. So, it is not an easy process for this patient to come in and see me for a quick visit. With telehealth, this simple visit doesn’t have to be a whole- or half-day affair as it can be a quick check-in. If an in-person visit is warranted, we can always arrange that but usually we can accomplish what we need to on video and audio.
Another example is with those patients with hearing impairments. Depending on the impairment, certain patients may be able to use Bluetooth or audio enhancement with their hearing aids and can actually hear me better in a video environment than they can in the clinic; especially at this point in time as we are masked when in the office.
Q: In what ways do you think the telemedicine diagnosis process might be impacted post-pandemic?
Ms. Colvin: At-home sleep testing became available several years ago, but it has a limited role as it is specifically for the diagnosis of sleep apnea in the uncomplicated patient. Telehealth offers some convenience in enabling patients to be tested in their home and it is also more affordable for the patient and for insurance. In fact, this is seen as one of the disruptors in our field that will continue to expand in the appropriate patient populations. But we will always have to acknowledge that it won't serve all patient needs because our more complex patients still need to come in for in-person testing.
Q: Overall, in what ways do sleep professionals support the value of having a specialist care model versus a generalist PCP model to perform patient care within the US as well as other countries?
Ms. Colvin: From my view, I see that our PCPs are already stretched thin in their ability to provide easily accessible care and I think it would be difficult for them to also provide the specialty care that patients with sleep disorders need. Some of the less complex patients might be able to stay within a primary care environment but as technology, as well as the software training that is required to be able to communicate with the devices our patients use for treatment or for diagnosis, continues to become more complex, it can become difficult to manage through the primary care environment.
The question then goes back to, how can we be as accessible as possible in an underserved area or where the specialty clinic is not easy to access? I think this is where telehealth may give us new options for expanding access to patients who can use the technology that is available.
Nonmotor symptoms common in Parkinson’s
The hallmark of Parkinson’s disease is the accompanying motor symptoms, but the condition can bring other challenges. Among those are nonmotor symptoms, including depression, dementia, and even psychosis.
The culprit is Lewy bodies, which are also responsible for Lewy body dementia. “What we call Lewy body dementia and Parkinson’s disease are caused by the same pathological process – the formation of Lewy bodies in the brain,” Leslie Citrome, MD, MPH, said in an interview. Dr. Citrome discussed some of the psychiatric comorbidities associated with Parkinson’s disease at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In fact, the association goes both ways. “Many people with Parkinson’s disease develop a dementia. Many people with Lewy body dementia develop motor symptoms that look just like Parkinson’s disease,” said Dr. Citrome, professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, and president of the American Society for Clinical Psychopharmacology.
The motor symptoms of Parkinson’s disease are generally attributable to loss of striatal dopaminergic neurons, while nonmotor symptoms can be traced to loss of neurons in nondopaminergic regions. Nonmotor symptoms – often including sleep disorders, depression, cognitive changes, and psychosis – may occur before motor symptoms. Other problems may include autonomic dysfunction, such as constipation, sexual dysfunction, sweating, or urinary retention.
Patients might not be aware that nonmotor symptoms can occur with Parkinson’s disease and may not even consider mentioning mood changes or hallucinations to their neurologist. Family members may also be unaware.
Sleep problems are common in Parkinson’s disease, including rapid eye-movement sleep behavior disorders, vivid dreams, restless legs syndrome, insomnia, and daytime somnolence. Dopamine agonists may also cause unintended sleep.
Depression is extremely common, affecting up to 90% of Parkinson’s disease patients, and this may be related to dopaminergic losses. Antidepressant medications can worsen Parkinson’s disease symptoms: Tricyclic antidepressants increase risk of adverse events from anticholinergic drugs. Selective serotonin reuptake inhibitors (SSRIs) can exacerbate tremor and may increase risk of serotonin syndrome when combined with MAO‐B inhibitors.
Dr. Citrome was not aware of any antidepressant drugs that have been tested specifically in Parkinson’s disease patients, though “I’d be surprised if there wasn’t,” he said during the Q&A session. “There’s no one perfect antidepressant for people with depression associated with Parkinson’s disease. I would make sure to select one that they would tolerate and be willing to take and that doesn’t interfere with their treatment of their movement disorder, and (I would make sure) that there’s no drug-drug interaction,” he said.
This can include reduced working memory, learning, and planning, and generally does not manifest until at least 1 year after motor symptoms have begun. Rivastigmine is Food and Drug Administration–approved for treatment of cognitive impairment in Parkinson’s disease.
As many as 60% of Parkinson’s disease patients suffer from psychosis at some point, often visual hallucinations or delusions, which can include beliefs of spousal infidelity.
Many clinicians prescribe quetiapine off label, but there are not compelling data to support that it reduces intensity and frequency of hallucinations and delusions, according to Dr. Citrome. However, it is relatively easy to prescribe, requiring no preauthorizations, it is inexpensive, and it may improve sleep.
The FDA approved pimavanserin in 2016 for hallucinations and delusions in Parkinson’s disease, and it doesn’t worsen motor symptoms, Dr. Citrome said. That’s because pimavanserin is a highly selective antagonist of the 5-HT2A receptor, with no effect on dopaminergic, histaminergic, adrenergic, or muscarinic receptors.
The drug improves positive symptoms beginning at days 29 and 43, compared with placebo. An analysis by Dr. Citrome’s group found a number needed to treat (NNT) of 7 to gain a benefit over placebo if the metric is a ≥ 30% reduction in baseline symptom score. The drug had an NNT of 9 to achieve a ≥ 50% reduction, and an NNT of 5 to achieve a score of much improved or very much improved on the Clinical Global Impression–Improvement (CGI-I) scale. In general, an NNT less than 10 suggests that a drug is clinically useful.
In contrast, the number needed to harm (NNH) represents the number of patients who would need to receive a therapy to add one adverse event, compared with placebo. A number greater than 10 indicates that the therapy may be tolerable.
Using various measures, the NNH was well over 10 for pimavanserin. With respect to somnolence, the NNH over placebo was 138, and for a weight gain of 7% or more, the NNH was 594.
Overall, the study found that 4 patients would need to be treated to achieve a benefit over placebo with respect to a ≥ 3–point improvement in the Scale of Positive Symptoms–Parkinson’s Disease (SAPS-PD), while 21 would need to receive the drug to lead to one additional discontinuation because of an adverse event, compared to placebo.
When researchers compared pimavanserin to off-label use of quetiapine, olanzapine, and clozapine, they found a Cohen’s d value of 0.50, which was better than quetiapine and olanzapine, but lower than for clozapine. However, there is no requirement of blood monitoring, and clozapine can potentially worsen motor symptoms.
Dr. Citrome’s presentation should be a reminder to neurologists that psychiatric disorders are an important patient concern, said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati, who moderated the session.
“I think this serves as a model to recognize that many neurological disorders actually present with numerous psychiatric disorders,” Dr. Nasrallah said during the meeting, presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Dr. Citrome has consulted for AbbVie, Acadia, Alkermes, Allergan, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer-Ingelheim, Cadent Therapeutics, Eisai, Impel, Intra-Cellular, Janssen, Karuna, Lundbeck, Lyndra, MedAvante-ProPhase, Merck, Neurocrine, Noven, Otsuka, Ovid, Relmada, Sage, Sunovion, and Teva. He has been a speaker for most of those companies, and he holds stock in Bristol Myers Squibb, Eli Lilly, J&J, Merck, and Pfizer.
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has served on a speakers bureau for most of those companies, in addition to that of Noven.
The hallmark of Parkinson’s disease is the accompanying motor symptoms, but the condition can bring other challenges. Among those are nonmotor symptoms, including depression, dementia, and even psychosis.
The culprit is Lewy bodies, which are also responsible for Lewy body dementia. “What we call Lewy body dementia and Parkinson’s disease are caused by the same pathological process – the formation of Lewy bodies in the brain,” Leslie Citrome, MD, MPH, said in an interview. Dr. Citrome discussed some of the psychiatric comorbidities associated with Parkinson’s disease at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In fact, the association goes both ways. “Many people with Parkinson’s disease develop a dementia. Many people with Lewy body dementia develop motor symptoms that look just like Parkinson’s disease,” said Dr. Citrome, professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, and president of the American Society for Clinical Psychopharmacology.
The motor symptoms of Parkinson’s disease are generally attributable to loss of striatal dopaminergic neurons, while nonmotor symptoms can be traced to loss of neurons in nondopaminergic regions. Nonmotor symptoms – often including sleep disorders, depression, cognitive changes, and psychosis – may occur before motor symptoms. Other problems may include autonomic dysfunction, such as constipation, sexual dysfunction, sweating, or urinary retention.
Patients might not be aware that nonmotor symptoms can occur with Parkinson’s disease and may not even consider mentioning mood changes or hallucinations to their neurologist. Family members may also be unaware.
Sleep problems are common in Parkinson’s disease, including rapid eye-movement sleep behavior disorders, vivid dreams, restless legs syndrome, insomnia, and daytime somnolence. Dopamine agonists may also cause unintended sleep.
Depression is extremely common, affecting up to 90% of Parkinson’s disease patients, and this may be related to dopaminergic losses. Antidepressant medications can worsen Parkinson’s disease symptoms: Tricyclic antidepressants increase risk of adverse events from anticholinergic drugs. Selective serotonin reuptake inhibitors (SSRIs) can exacerbate tremor and may increase risk of serotonin syndrome when combined with MAO‐B inhibitors.
Dr. Citrome was not aware of any antidepressant drugs that have been tested specifically in Parkinson’s disease patients, though “I’d be surprised if there wasn’t,” he said during the Q&A session. “There’s no one perfect antidepressant for people with depression associated with Parkinson’s disease. I would make sure to select one that they would tolerate and be willing to take and that doesn’t interfere with their treatment of their movement disorder, and (I would make sure) that there’s no drug-drug interaction,” he said.
This can include reduced working memory, learning, and planning, and generally does not manifest until at least 1 year after motor symptoms have begun. Rivastigmine is Food and Drug Administration–approved for treatment of cognitive impairment in Parkinson’s disease.
As many as 60% of Parkinson’s disease patients suffer from psychosis at some point, often visual hallucinations or delusions, which can include beliefs of spousal infidelity.
Many clinicians prescribe quetiapine off label, but there are not compelling data to support that it reduces intensity and frequency of hallucinations and delusions, according to Dr. Citrome. However, it is relatively easy to prescribe, requiring no preauthorizations, it is inexpensive, and it may improve sleep.
The FDA approved pimavanserin in 2016 for hallucinations and delusions in Parkinson’s disease, and it doesn’t worsen motor symptoms, Dr. Citrome said. That’s because pimavanserin is a highly selective antagonist of the 5-HT2A receptor, with no effect on dopaminergic, histaminergic, adrenergic, or muscarinic receptors.
The drug improves positive symptoms beginning at days 29 and 43, compared with placebo. An analysis by Dr. Citrome’s group found a number needed to treat (NNT) of 7 to gain a benefit over placebo if the metric is a ≥ 30% reduction in baseline symptom score. The drug had an NNT of 9 to achieve a ≥ 50% reduction, and an NNT of 5 to achieve a score of much improved or very much improved on the Clinical Global Impression–Improvement (CGI-I) scale. In general, an NNT less than 10 suggests that a drug is clinically useful.
In contrast, the number needed to harm (NNH) represents the number of patients who would need to receive a therapy to add one adverse event, compared with placebo. A number greater than 10 indicates that the therapy may be tolerable.
Using various measures, the NNH was well over 10 for pimavanserin. With respect to somnolence, the NNH over placebo was 138, and for a weight gain of 7% or more, the NNH was 594.
Overall, the study found that 4 patients would need to be treated to achieve a benefit over placebo with respect to a ≥ 3–point improvement in the Scale of Positive Symptoms–Parkinson’s Disease (SAPS-PD), while 21 would need to receive the drug to lead to one additional discontinuation because of an adverse event, compared to placebo.
When researchers compared pimavanserin to off-label use of quetiapine, olanzapine, and clozapine, they found a Cohen’s d value of 0.50, which was better than quetiapine and olanzapine, but lower than for clozapine. However, there is no requirement of blood monitoring, and clozapine can potentially worsen motor symptoms.
Dr. Citrome’s presentation should be a reminder to neurologists that psychiatric disorders are an important patient concern, said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati, who moderated the session.
“I think this serves as a model to recognize that many neurological disorders actually present with numerous psychiatric disorders,” Dr. Nasrallah said during the meeting, presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Dr. Citrome has consulted for AbbVie, Acadia, Alkermes, Allergan, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer-Ingelheim, Cadent Therapeutics, Eisai, Impel, Intra-Cellular, Janssen, Karuna, Lundbeck, Lyndra, MedAvante-ProPhase, Merck, Neurocrine, Noven, Otsuka, Ovid, Relmada, Sage, Sunovion, and Teva. He has been a speaker for most of those companies, and he holds stock in Bristol Myers Squibb, Eli Lilly, J&J, Merck, and Pfizer.
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has served on a speakers bureau for most of those companies, in addition to that of Noven.
The hallmark of Parkinson’s disease is the accompanying motor symptoms, but the condition can bring other challenges. Among those are nonmotor symptoms, including depression, dementia, and even psychosis.
The culprit is Lewy bodies, which are also responsible for Lewy body dementia. “What we call Lewy body dementia and Parkinson’s disease are caused by the same pathological process – the formation of Lewy bodies in the brain,” Leslie Citrome, MD, MPH, said in an interview. Dr. Citrome discussed some of the psychiatric comorbidities associated with Parkinson’s disease at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In fact, the association goes both ways. “Many people with Parkinson’s disease develop a dementia. Many people with Lewy body dementia develop motor symptoms that look just like Parkinson’s disease,” said Dr. Citrome, professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, and president of the American Society for Clinical Psychopharmacology.
The motor symptoms of Parkinson’s disease are generally attributable to loss of striatal dopaminergic neurons, while nonmotor symptoms can be traced to loss of neurons in nondopaminergic regions. Nonmotor symptoms – often including sleep disorders, depression, cognitive changes, and psychosis – may occur before motor symptoms. Other problems may include autonomic dysfunction, such as constipation, sexual dysfunction, sweating, or urinary retention.
Patients might not be aware that nonmotor symptoms can occur with Parkinson’s disease and may not even consider mentioning mood changes or hallucinations to their neurologist. Family members may also be unaware.
Sleep problems are common in Parkinson’s disease, including rapid eye-movement sleep behavior disorders, vivid dreams, restless legs syndrome, insomnia, and daytime somnolence. Dopamine agonists may also cause unintended sleep.
Depression is extremely common, affecting up to 90% of Parkinson’s disease patients, and this may be related to dopaminergic losses. Antidepressant medications can worsen Parkinson’s disease symptoms: Tricyclic antidepressants increase risk of adverse events from anticholinergic drugs. Selective serotonin reuptake inhibitors (SSRIs) can exacerbate tremor and may increase risk of serotonin syndrome when combined with MAO‐B inhibitors.
Dr. Citrome was not aware of any antidepressant drugs that have been tested specifically in Parkinson’s disease patients, though “I’d be surprised if there wasn’t,” he said during the Q&A session. “There’s no one perfect antidepressant for people with depression associated with Parkinson’s disease. I would make sure to select one that they would tolerate and be willing to take and that doesn’t interfere with their treatment of their movement disorder, and (I would make sure) that there’s no drug-drug interaction,” he said.
This can include reduced working memory, learning, and planning, and generally does not manifest until at least 1 year after motor symptoms have begun. Rivastigmine is Food and Drug Administration–approved for treatment of cognitive impairment in Parkinson’s disease.
As many as 60% of Parkinson’s disease patients suffer from psychosis at some point, often visual hallucinations or delusions, which can include beliefs of spousal infidelity.
Many clinicians prescribe quetiapine off label, but there are not compelling data to support that it reduces intensity and frequency of hallucinations and delusions, according to Dr. Citrome. However, it is relatively easy to prescribe, requiring no preauthorizations, it is inexpensive, and it may improve sleep.
The FDA approved pimavanserin in 2016 for hallucinations and delusions in Parkinson’s disease, and it doesn’t worsen motor symptoms, Dr. Citrome said. That’s because pimavanserin is a highly selective antagonist of the 5-HT2A receptor, with no effect on dopaminergic, histaminergic, adrenergic, or muscarinic receptors.
The drug improves positive symptoms beginning at days 29 and 43, compared with placebo. An analysis by Dr. Citrome’s group found a number needed to treat (NNT) of 7 to gain a benefit over placebo if the metric is a ≥ 30% reduction in baseline symptom score. The drug had an NNT of 9 to achieve a ≥ 50% reduction, and an NNT of 5 to achieve a score of much improved or very much improved on the Clinical Global Impression–Improvement (CGI-I) scale. In general, an NNT less than 10 suggests that a drug is clinically useful.
In contrast, the number needed to harm (NNH) represents the number of patients who would need to receive a therapy to add one adverse event, compared with placebo. A number greater than 10 indicates that the therapy may be tolerable.
Using various measures, the NNH was well over 10 for pimavanserin. With respect to somnolence, the NNH over placebo was 138, and for a weight gain of 7% or more, the NNH was 594.
Overall, the study found that 4 patients would need to be treated to achieve a benefit over placebo with respect to a ≥ 3–point improvement in the Scale of Positive Symptoms–Parkinson’s Disease (SAPS-PD), while 21 would need to receive the drug to lead to one additional discontinuation because of an adverse event, compared to placebo.
When researchers compared pimavanserin to off-label use of quetiapine, olanzapine, and clozapine, they found a Cohen’s d value of 0.50, which was better than quetiapine and olanzapine, but lower than for clozapine. However, there is no requirement of blood monitoring, and clozapine can potentially worsen motor symptoms.
Dr. Citrome’s presentation should be a reminder to neurologists that psychiatric disorders are an important patient concern, said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati, who moderated the session.
“I think this serves as a model to recognize that many neurological disorders actually present with numerous psychiatric disorders,” Dr. Nasrallah said during the meeting, presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Dr. Citrome has consulted for AbbVie, Acadia, Alkermes, Allergan, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer-Ingelheim, Cadent Therapeutics, Eisai, Impel, Intra-Cellular, Janssen, Karuna, Lundbeck, Lyndra, MedAvante-ProPhase, Merck, Neurocrine, Noven, Otsuka, Ovid, Relmada, Sage, Sunovion, and Teva. He has been a speaker for most of those companies, and he holds stock in Bristol Myers Squibb, Eli Lilly, J&J, Merck, and Pfizer.
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has served on a speakers bureau for most of those companies, in addition to that of Noven.
FROM FOCUS ON NEUROPSYCHIATRY 2021