User login
Sleep, chronic pain, and OUD have a complex relationship
MILWAUKEE – Individuals with chronic pain frequently have disrupted sleep and also may be at risk for opioid use disorder. However, even with advanced monitoring, it’s not clear how sleep modulates pain and opioid cravings.
Sleep has an impact on positive and negative affect, but new research shows that the link between sleep and mood states that may contribute to opioid use disorder is not straightforward. At the scientific meeting of the American Pain Society, Patrick Finan, PhD, of Johns Hopkins University, Baltimore, discussed how sleep and mood affect cravings for opioids among those in treatment for opioid use disorder (OUD).
said Dr. Finan, who told attendees that one key question he and his colleagues were seeking to answer was whether those with OUD and chronic pain had more disturbed sleep than those with OUD alone. Also, the researchers wanted to know whether the ups and downs of sleep on a day-to-day basis were reflected in pain scores among those with OUD, as would be predicted by prevailing models.
Finally, two “proximal indicators” of relapse risk, affect and heroin craving, might be affected by both sleep and pain, and Dr. Finan and collaborators sought to explore that association.
The work was part of a larger study looking at the natural history of OUD and OUD with comorbid chronic pain. To participate in this parent study, adults with OUD had to be seeking treatment or currently enrolled in methadone or buprenorphine maintenance treatment, and without current major depressive disorder. Also, patients could not have a history of significant mental illness, cognitive impairment, or a medical condition that would interfere with study participation. A total of 56 patients participated, and 20 of these individuals also had chronic pain.
Those with OUD and chronic pain qualified if they had pain (not related to opioid withdrawal) averaging above 3 on a 0-10 pain rating scale over the past week; additional criteria included pain for at least the past 3 months, with 10 or more days per month of pain.
Pain ratings were captured via a smartphone app that prompted participants to enter a pain rating at three random times during each day. Each evening, patients also completed a sleep diary giving information about bedtime, sleep onset latency, waking after sleep onset, and wake time for the preceding day.
A self-applied ambulatory electroencephalogram applied to the forehead was used for up to 7 consecutive nights to capture sleep continuity estimates; the device has been validated against polysomnography data in other work. Participants were given incentives to use the device, and this “yielded strong adherence,” with an average of 5 nights of use per participant, Dr. Finan said.
Patients were an average age of about 49 years, and were 75% male. African American participants made up just over half of the cohort, and 43% were white. Participants were roughly evenly divided in the type of maintenance therapy they were taking. Overall, 39% of participants had a positive urine toxicology screen.
For patients with chronic pain, 45% of all momentary pain reports had a pain score over zero, with a mean of 32 days of pain. Looking at the data another way, 58% of all patient-days had at least one momentary report of pain greater than zero, said Dr. Finan. On average, participants recorded a pain score of 2.27.
Brief Pain Inventory scores at baseline showed a mean severity of 5, and a pain interference score of 5.07.
Participants with OUD and chronic pain did not differ across any EEG-recorded sleep measures, compared with those with OUD alone. However, subjective reports of sleep were actually better overall for those with chronic pain than the objective EEG reports. The EEG recordings captured an average of 9.11 minutes more of waking after sleep onset (P less than .001). Also, total sleep time was 10.37 minutes shorter as recorded by the EEG than by self-report (P less than .001). Overall sleep efficiency was also worse by 5.96 minutes according to the EEG, compared with self-report (P less than .001).
“Sleep is objectively poor but subjectively ‘normal’ and variable in opioid use disorder patients,” Dr. Finan said. In aggregate, however, neither diary-based subjective nor EEG-based objective sleep measures differed between those with and without chronic pain in the research cohort. This phenomenon of sleep efficiency being self-reported as higher than objective measures capture sleep has also been seen in those newly abstinent from cocaine, Dr. Finan said, adding that it’s possible individuals with substance use disorder who are new to treatment simply feel better than they have in some time along many dimensions, with sleep being one such domain.
Pain on a given day didn’t predict poor sleep on that night, except that sleep onset took slightly longer (P = .01), said Dr. Finan. He noted that “there was no substantive effect on other sleep continuity parameters.”
Looking at how negative affect mediated craving for heroin, Dr. Finan and colleagues found that negative affect–related craving was significantly greater for those with chronic pain (P less than .001). Unlike findings in patients without OUD, having disrupted sleep continuity was more associated with increased daily negative affect, rather than decreased positive affect. And this increased negative affect was associated with heroin cravings, said Dr. Finan. “In the past few years, we’ve seen quite a few studies that have found some abnormalities in the reward system in patients with chronic pain.” Whether poor sleep is a mediator of these abnormalities deserves further study.
The study was supported by the National Institutes of Health. Dr. Finan reported no outside sources of funding.
MILWAUKEE – Individuals with chronic pain frequently have disrupted sleep and also may be at risk for opioid use disorder. However, even with advanced monitoring, it’s not clear how sleep modulates pain and opioid cravings.
Sleep has an impact on positive and negative affect, but new research shows that the link between sleep and mood states that may contribute to opioid use disorder is not straightforward. At the scientific meeting of the American Pain Society, Patrick Finan, PhD, of Johns Hopkins University, Baltimore, discussed how sleep and mood affect cravings for opioids among those in treatment for opioid use disorder (OUD).
said Dr. Finan, who told attendees that one key question he and his colleagues were seeking to answer was whether those with OUD and chronic pain had more disturbed sleep than those with OUD alone. Also, the researchers wanted to know whether the ups and downs of sleep on a day-to-day basis were reflected in pain scores among those with OUD, as would be predicted by prevailing models.
Finally, two “proximal indicators” of relapse risk, affect and heroin craving, might be affected by both sleep and pain, and Dr. Finan and collaborators sought to explore that association.
The work was part of a larger study looking at the natural history of OUD and OUD with comorbid chronic pain. To participate in this parent study, adults with OUD had to be seeking treatment or currently enrolled in methadone or buprenorphine maintenance treatment, and without current major depressive disorder. Also, patients could not have a history of significant mental illness, cognitive impairment, or a medical condition that would interfere with study participation. A total of 56 patients participated, and 20 of these individuals also had chronic pain.
Those with OUD and chronic pain qualified if they had pain (not related to opioid withdrawal) averaging above 3 on a 0-10 pain rating scale over the past week; additional criteria included pain for at least the past 3 months, with 10 or more days per month of pain.
Pain ratings were captured via a smartphone app that prompted participants to enter a pain rating at three random times during each day. Each evening, patients also completed a sleep diary giving information about bedtime, sleep onset latency, waking after sleep onset, and wake time for the preceding day.
A self-applied ambulatory electroencephalogram applied to the forehead was used for up to 7 consecutive nights to capture sleep continuity estimates; the device has been validated against polysomnography data in other work. Participants were given incentives to use the device, and this “yielded strong adherence,” with an average of 5 nights of use per participant, Dr. Finan said.
Patients were an average age of about 49 years, and were 75% male. African American participants made up just over half of the cohort, and 43% were white. Participants were roughly evenly divided in the type of maintenance therapy they were taking. Overall, 39% of participants had a positive urine toxicology screen.
For patients with chronic pain, 45% of all momentary pain reports had a pain score over zero, with a mean of 32 days of pain. Looking at the data another way, 58% of all patient-days had at least one momentary report of pain greater than zero, said Dr. Finan. On average, participants recorded a pain score of 2.27.
Brief Pain Inventory scores at baseline showed a mean severity of 5, and a pain interference score of 5.07.
Participants with OUD and chronic pain did not differ across any EEG-recorded sleep measures, compared with those with OUD alone. However, subjective reports of sleep were actually better overall for those with chronic pain than the objective EEG reports. The EEG recordings captured an average of 9.11 minutes more of waking after sleep onset (P less than .001). Also, total sleep time was 10.37 minutes shorter as recorded by the EEG than by self-report (P less than .001). Overall sleep efficiency was also worse by 5.96 minutes according to the EEG, compared with self-report (P less than .001).
“Sleep is objectively poor but subjectively ‘normal’ and variable in opioid use disorder patients,” Dr. Finan said. In aggregate, however, neither diary-based subjective nor EEG-based objective sleep measures differed between those with and without chronic pain in the research cohort. This phenomenon of sleep efficiency being self-reported as higher than objective measures capture sleep has also been seen in those newly abstinent from cocaine, Dr. Finan said, adding that it’s possible individuals with substance use disorder who are new to treatment simply feel better than they have in some time along many dimensions, with sleep being one such domain.
Pain on a given day didn’t predict poor sleep on that night, except that sleep onset took slightly longer (P = .01), said Dr. Finan. He noted that “there was no substantive effect on other sleep continuity parameters.”
Looking at how negative affect mediated craving for heroin, Dr. Finan and colleagues found that negative affect–related craving was significantly greater for those with chronic pain (P less than .001). Unlike findings in patients without OUD, having disrupted sleep continuity was more associated with increased daily negative affect, rather than decreased positive affect. And this increased negative affect was associated with heroin cravings, said Dr. Finan. “In the past few years, we’ve seen quite a few studies that have found some abnormalities in the reward system in patients with chronic pain.” Whether poor sleep is a mediator of these abnormalities deserves further study.
The study was supported by the National Institutes of Health. Dr. Finan reported no outside sources of funding.
MILWAUKEE – Individuals with chronic pain frequently have disrupted sleep and also may be at risk for opioid use disorder. However, even with advanced monitoring, it’s not clear how sleep modulates pain and opioid cravings.
Sleep has an impact on positive and negative affect, but new research shows that the link between sleep and mood states that may contribute to opioid use disorder is not straightforward. At the scientific meeting of the American Pain Society, Patrick Finan, PhD, of Johns Hopkins University, Baltimore, discussed how sleep and mood affect cravings for opioids among those in treatment for opioid use disorder (OUD).
said Dr. Finan, who told attendees that one key question he and his colleagues were seeking to answer was whether those with OUD and chronic pain had more disturbed sleep than those with OUD alone. Also, the researchers wanted to know whether the ups and downs of sleep on a day-to-day basis were reflected in pain scores among those with OUD, as would be predicted by prevailing models.
Finally, two “proximal indicators” of relapse risk, affect and heroin craving, might be affected by both sleep and pain, and Dr. Finan and collaborators sought to explore that association.
The work was part of a larger study looking at the natural history of OUD and OUD with comorbid chronic pain. To participate in this parent study, adults with OUD had to be seeking treatment or currently enrolled in methadone or buprenorphine maintenance treatment, and without current major depressive disorder. Also, patients could not have a history of significant mental illness, cognitive impairment, or a medical condition that would interfere with study participation. A total of 56 patients participated, and 20 of these individuals also had chronic pain.
Those with OUD and chronic pain qualified if they had pain (not related to opioid withdrawal) averaging above 3 on a 0-10 pain rating scale over the past week; additional criteria included pain for at least the past 3 months, with 10 or more days per month of pain.
Pain ratings were captured via a smartphone app that prompted participants to enter a pain rating at three random times during each day. Each evening, patients also completed a sleep diary giving information about bedtime, sleep onset latency, waking after sleep onset, and wake time for the preceding day.
A self-applied ambulatory electroencephalogram applied to the forehead was used for up to 7 consecutive nights to capture sleep continuity estimates; the device has been validated against polysomnography data in other work. Participants were given incentives to use the device, and this “yielded strong adherence,” with an average of 5 nights of use per participant, Dr. Finan said.
Patients were an average age of about 49 years, and were 75% male. African American participants made up just over half of the cohort, and 43% were white. Participants were roughly evenly divided in the type of maintenance therapy they were taking. Overall, 39% of participants had a positive urine toxicology screen.
For patients with chronic pain, 45% of all momentary pain reports had a pain score over zero, with a mean of 32 days of pain. Looking at the data another way, 58% of all patient-days had at least one momentary report of pain greater than zero, said Dr. Finan. On average, participants recorded a pain score of 2.27.
Brief Pain Inventory scores at baseline showed a mean severity of 5, and a pain interference score of 5.07.
Participants with OUD and chronic pain did not differ across any EEG-recorded sleep measures, compared with those with OUD alone. However, subjective reports of sleep were actually better overall for those with chronic pain than the objective EEG reports. The EEG recordings captured an average of 9.11 minutes more of waking after sleep onset (P less than .001). Also, total sleep time was 10.37 minutes shorter as recorded by the EEG than by self-report (P less than .001). Overall sleep efficiency was also worse by 5.96 minutes according to the EEG, compared with self-report (P less than .001).
“Sleep is objectively poor but subjectively ‘normal’ and variable in opioid use disorder patients,” Dr. Finan said. In aggregate, however, neither diary-based subjective nor EEG-based objective sleep measures differed between those with and without chronic pain in the research cohort. This phenomenon of sleep efficiency being self-reported as higher than objective measures capture sleep has also been seen in those newly abstinent from cocaine, Dr. Finan said, adding that it’s possible individuals with substance use disorder who are new to treatment simply feel better than they have in some time along many dimensions, with sleep being one such domain.
Pain on a given day didn’t predict poor sleep on that night, except that sleep onset took slightly longer (P = .01), said Dr. Finan. He noted that “there was no substantive effect on other sleep continuity parameters.”
Looking at how negative affect mediated craving for heroin, Dr. Finan and colleagues found that negative affect–related craving was significantly greater for those with chronic pain (P less than .001). Unlike findings in patients without OUD, having disrupted sleep continuity was more associated with increased daily negative affect, rather than decreased positive affect. And this increased negative affect was associated with heroin cravings, said Dr. Finan. “In the past few years, we’ve seen quite a few studies that have found some abnormalities in the reward system in patients with chronic pain.” Whether poor sleep is a mediator of these abnormalities deserves further study.
The study was supported by the National Institutes of Health. Dr. Finan reported no outside sources of funding.
REPORTING FROM APS 2019
Sleep apnea is linked with tau accumulation in the brain
PHILADELPHIA – according to data that will be presented at the annual meeting of the American Academy of Neurology. Tau accumulation is a biomarker of Alzheimer’s disease, and the finding suggests a possible explanation for the apparent association between sleep disruption and dementia.
“Our research results raise the possibility that sleep apnea affects tau accumulation,” said Diego Z. Carvalho, MD, of the Mayo Clinic in Rochester, Minn., in a press release. “But it is also possible that higher levels of tau in other regions may predispose a person to sleep apnea, so longer studies are now needed to solve this chicken-and-egg problem.”
Previous research had suggested an association between sleep disruption and increased risk of dementia. Obstructive sleep apnea in particular has been associated with this increased risk. The pathological processes that account for this association are unknown, however.
Dr. Carvalho and colleagues decided to evaluate whether apneas during sleep, reported by the patient or an informant, were associated with high levels of tau in cognitively normal elderly individuals. The investigators identified 288 participants in the Mayo Clinic Study of Aging for their analysis. Eligible participants were aged 65 years or older, had no cognitive impairment, had undergone tau PET and amyloid PET scans, and had completed a questionnaire that solicited information about witnessed apneas during sleep (either from patients or bed partners). Dr. Carvalho’s group took the entorhinal cortex as its region of interest because it is highly susceptible to tau accumulation. The entorhinal cortex is involved in memory, navigation, and the perception of time. They chose the cerebellum crus as their reference region.
The investigators created a linear model to evaluate the association between tau in the entorhinal cortex and witnessed apneas. They controlled the data for age, sex, years of education, body mass index, hypertension, hyperlipidemia, diabetes, reduced sleep, excessive daytime sleepiness, and global amyloid.
In all, 43 participants (15%) had witnessed apneas during sleep. Witnessed apneas were significantly associated with tau in the entorhinal cortex. After controlling for potential confounders, Dr. Carvalho and colleagues estimated a 0.049 elevation in the entorhinal cortex tau standardized uptake value ratio (95% confidence interval, 0.011–0.087; P = 0.012).
The study had a relatively small sample size, and its results require validation. Other important limitations include the absence of sleep studies to confirm the presence and severity of sleep apnea and a lack of information about whether participants already were receiving treatment for sleep apnea.
The National Institutes of Health supported the study.
SOURCE: Carvalho D et al. AAN 2019, Abstract P3.6-021.
PHILADELPHIA – according to data that will be presented at the annual meeting of the American Academy of Neurology. Tau accumulation is a biomarker of Alzheimer’s disease, and the finding suggests a possible explanation for the apparent association between sleep disruption and dementia.
“Our research results raise the possibility that sleep apnea affects tau accumulation,” said Diego Z. Carvalho, MD, of the Mayo Clinic in Rochester, Minn., in a press release. “But it is also possible that higher levels of tau in other regions may predispose a person to sleep apnea, so longer studies are now needed to solve this chicken-and-egg problem.”
Previous research had suggested an association between sleep disruption and increased risk of dementia. Obstructive sleep apnea in particular has been associated with this increased risk. The pathological processes that account for this association are unknown, however.
Dr. Carvalho and colleagues decided to evaluate whether apneas during sleep, reported by the patient or an informant, were associated with high levels of tau in cognitively normal elderly individuals. The investigators identified 288 participants in the Mayo Clinic Study of Aging for their analysis. Eligible participants were aged 65 years or older, had no cognitive impairment, had undergone tau PET and amyloid PET scans, and had completed a questionnaire that solicited information about witnessed apneas during sleep (either from patients or bed partners). Dr. Carvalho’s group took the entorhinal cortex as its region of interest because it is highly susceptible to tau accumulation. The entorhinal cortex is involved in memory, navigation, and the perception of time. They chose the cerebellum crus as their reference region.
The investigators created a linear model to evaluate the association between tau in the entorhinal cortex and witnessed apneas. They controlled the data for age, sex, years of education, body mass index, hypertension, hyperlipidemia, diabetes, reduced sleep, excessive daytime sleepiness, and global amyloid.
In all, 43 participants (15%) had witnessed apneas during sleep. Witnessed apneas were significantly associated with tau in the entorhinal cortex. After controlling for potential confounders, Dr. Carvalho and colleagues estimated a 0.049 elevation in the entorhinal cortex tau standardized uptake value ratio (95% confidence interval, 0.011–0.087; P = 0.012).
The study had a relatively small sample size, and its results require validation. Other important limitations include the absence of sleep studies to confirm the presence and severity of sleep apnea and a lack of information about whether participants already were receiving treatment for sleep apnea.
The National Institutes of Health supported the study.
SOURCE: Carvalho D et al. AAN 2019, Abstract P3.6-021.
PHILADELPHIA – according to data that will be presented at the annual meeting of the American Academy of Neurology. Tau accumulation is a biomarker of Alzheimer’s disease, and the finding suggests a possible explanation for the apparent association between sleep disruption and dementia.
“Our research results raise the possibility that sleep apnea affects tau accumulation,” said Diego Z. Carvalho, MD, of the Mayo Clinic in Rochester, Minn., in a press release. “But it is also possible that higher levels of tau in other regions may predispose a person to sleep apnea, so longer studies are now needed to solve this chicken-and-egg problem.”
Previous research had suggested an association between sleep disruption and increased risk of dementia. Obstructive sleep apnea in particular has been associated with this increased risk. The pathological processes that account for this association are unknown, however.
Dr. Carvalho and colleagues decided to evaluate whether apneas during sleep, reported by the patient or an informant, were associated with high levels of tau in cognitively normal elderly individuals. The investigators identified 288 participants in the Mayo Clinic Study of Aging for their analysis. Eligible participants were aged 65 years or older, had no cognitive impairment, had undergone tau PET and amyloid PET scans, and had completed a questionnaire that solicited information about witnessed apneas during sleep (either from patients or bed partners). Dr. Carvalho’s group took the entorhinal cortex as its region of interest because it is highly susceptible to tau accumulation. The entorhinal cortex is involved in memory, navigation, and the perception of time. They chose the cerebellum crus as their reference region.
The investigators created a linear model to evaluate the association between tau in the entorhinal cortex and witnessed apneas. They controlled the data for age, sex, years of education, body mass index, hypertension, hyperlipidemia, diabetes, reduced sleep, excessive daytime sleepiness, and global amyloid.
In all, 43 participants (15%) had witnessed apneas during sleep. Witnessed apneas were significantly associated with tau in the entorhinal cortex. After controlling for potential confounders, Dr. Carvalho and colleagues estimated a 0.049 elevation in the entorhinal cortex tau standardized uptake value ratio (95% confidence interval, 0.011–0.087; P = 0.012).
The study had a relatively small sample size, and its results require validation. Other important limitations include the absence of sleep studies to confirm the presence and severity of sleep apnea and a lack of information about whether participants already were receiving treatment for sleep apnea.
The National Institutes of Health supported the study.
SOURCE: Carvalho D et al. AAN 2019, Abstract P3.6-021.
FROM AAN 2019
PAP may reduce mortality in patients with obesity and severe OSA
according to the results of a cohort study published in JAMA Otolaryngology–Head & Neck Surgery.
The association becomes evident several years after positive airway pressure (PAP) initiation, according to the researchers. Obstructive sleep apnea (OSA) is among the top 10 modifiable cardiovascular risk factors, and is associated with increased risks of coronary artery disease, stroke, and death. PAP is the most effective treatment for OSA, but this treatment’s effect on all-cause and cardiovascular mortality is uncertain. Randomized trials have yielded inconclusive answers to this question, and evidence from observational studies has been weak.
To investigate the association between PAP prescription and mortality in patients with obesity and severe OSA, Quentin Lisan, MD, of the Paris Cardiovascular Research Center and his colleagues conducted a multicenter, population-based cohort study. The researchers examined data for 392 participants in the Sleep Heart Health Study, in which adult men and women age 40 years or older were recruited from nine population-based studies between 1995 and 1998 and followed for a mean of 11.1 years. With each participant who had been prescribed PAP, the investigators matched as many as four participants who had not been prescribed PAP, on the basis of age, sex, and apnea-hypopnea index. Of this sample, 81 patients were prescribed PAP, and 311 were not.
All participants had a clinic visit and underwent overnight polysomnography at baseline. At 2-3 years, participants had a follow-up visit or phone call, during which they were asked whether their physicians had prescribed PAP. Participants were monitored for cardiovascular and all-cause mortality.
In all, 319 of the 392 participants were men; the population’s mean age was 63 years. Patients who had received a PAP prescription had a higher body mass index and more education, compared with patients who had not received a prescription. Mean follow-up duration was 11.6 years in the PAP-prescribed group and 10.9 years in the nonprescribed group.
A total of 96 deaths occurred during follow-up: 12 in the PAP-prescribed group and 84 in the nonprescribed PAP group. The crude incidence rate of mortality was 24.7 deaths per 1,000 person-years in the nonprescribed group and 12.8 deaths per 1,000 person-years in the PAP-prescribed group. The difference in survival between the prescribed and nonprescribed groups was evident in survival curves after 6-7 years of follow-up. After adjustments for prevalent cardiovascular disease, hypertension, diabetes, body mass index, education level, smoking status, and alcohol consumption, the hazard ratio of all-cause mortality for the prescribed group was 0.38, compared with the nonprescribed group.
Dr. Lisan and his colleagues identified 27 deaths of cardiovascular origin, one of which occurred in the prescribed group. After adjusting for prevalent cardiovascular disease, the hazard ratio of cardiovascular mortality for the prescribed group was 0.06, compared with the nonprescribed group.
One reason that the reduction in mortality associated with PAP was not found in previous randomized, controlled trials could be that their mean length of follow-up was not long enough, the researchers wrote. For example, the mean length of follow-up in the SAVE trial was 3.7 years, but the survival benefit was not apparent in the present analysis until 6-7 years after treatment initiation.
These results are exploratory and require confirmation in future research, Dr. Lisan and his colleagues wrote. No information on adherence to PAP was available, and the researchers could not account for initiation and interruption of PAP therapy. Nevertheless, “prescribing PAP in patients with OSA should be pursued and encouraged, given its potential major public health implication,” they concluded.
The Sleep Heart Health Study was supported by grants from the National Institutes of Health.
SOURCE: Lisan Q et al. JAMA Otolaryngol Head Neck Surg. 2019 Apr 11. doi: 10.1001/jamaoto.2019.0281.
Further confirmation of the benefits of positive airway pressure (PAP) on mortality in patients with obstructive sleep apnea (OSA) may follow the results published by Lisan et al., wrote Clete A. Kushida, MD, PhD, in an accompanying editorial. Dr. Kushida is a professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Of the study limitations described by Lisan et al., a major factor is the participants’ use of PAP therapy: The participants self-reported if they were prescribed PAP therapy, but their PAP adherence data (i.e., duration and frequency of PAP use) were unknown. Discrepancies exist between self-reported versus objective PAP adherence, as well as between patterns of PAP adherence over time, and the lack of adherence data would be expected to limit our understanding of the effects of PAP therapy on mortality.” A further limitation is that the study’s findings are restricted to patients with obesity and severe OSA.
“Even taking into consideration the technological improvement in size, comfort, and convenience of these devices since PAP was first tried on patients with OSA, every knowledgeable sleep specialist has had difficulty in convincing some patients of the need to treat their OSA with these devices, and/or the need to improve their use of the devices once they have been prescribed,” Dr. Kushida continued. “Although at this point experienced sleep specialists cannot say with certainty that use of PAP improves survival, the study by Lisan et al. will undoubtedly make these clinicians’ jobs a little easier by enabling them to present to their patients evidence that PAP may be associated with reduced mortality, particularly in those with severe OSA and comorbid obesity.”
Dr. Kushida receives salary support from a contract between Stanford University and Philips-Respironics for the conduct of a clinical trial. These comments are from an accompanying editorial (JAMA Otolaryngol Head Neck Surg. 2019 April 11. doi: 10.1001/jamaoto.2019.0345).
Further confirmation of the benefits of positive airway pressure (PAP) on mortality in patients with obstructive sleep apnea (OSA) may follow the results published by Lisan et al., wrote Clete A. Kushida, MD, PhD, in an accompanying editorial. Dr. Kushida is a professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Of the study limitations described by Lisan et al., a major factor is the participants’ use of PAP therapy: The participants self-reported if they were prescribed PAP therapy, but their PAP adherence data (i.e., duration and frequency of PAP use) were unknown. Discrepancies exist between self-reported versus objective PAP adherence, as well as between patterns of PAP adherence over time, and the lack of adherence data would be expected to limit our understanding of the effects of PAP therapy on mortality.” A further limitation is that the study’s findings are restricted to patients with obesity and severe OSA.
“Even taking into consideration the technological improvement in size, comfort, and convenience of these devices since PAP was first tried on patients with OSA, every knowledgeable sleep specialist has had difficulty in convincing some patients of the need to treat their OSA with these devices, and/or the need to improve their use of the devices once they have been prescribed,” Dr. Kushida continued. “Although at this point experienced sleep specialists cannot say with certainty that use of PAP improves survival, the study by Lisan et al. will undoubtedly make these clinicians’ jobs a little easier by enabling them to present to their patients evidence that PAP may be associated with reduced mortality, particularly in those with severe OSA and comorbid obesity.”
Dr. Kushida receives salary support from a contract between Stanford University and Philips-Respironics for the conduct of a clinical trial. These comments are from an accompanying editorial (JAMA Otolaryngol Head Neck Surg. 2019 April 11. doi: 10.1001/jamaoto.2019.0345).
Further confirmation of the benefits of positive airway pressure (PAP) on mortality in patients with obstructive sleep apnea (OSA) may follow the results published by Lisan et al., wrote Clete A. Kushida, MD, PhD, in an accompanying editorial. Dr. Kushida is a professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Of the study limitations described by Lisan et al., a major factor is the participants’ use of PAP therapy: The participants self-reported if they were prescribed PAP therapy, but their PAP adherence data (i.e., duration and frequency of PAP use) were unknown. Discrepancies exist between self-reported versus objective PAP adherence, as well as between patterns of PAP adherence over time, and the lack of adherence data would be expected to limit our understanding of the effects of PAP therapy on mortality.” A further limitation is that the study’s findings are restricted to patients with obesity and severe OSA.
“Even taking into consideration the technological improvement in size, comfort, and convenience of these devices since PAP was first tried on patients with OSA, every knowledgeable sleep specialist has had difficulty in convincing some patients of the need to treat their OSA with these devices, and/or the need to improve their use of the devices once they have been prescribed,” Dr. Kushida continued. “Although at this point experienced sleep specialists cannot say with certainty that use of PAP improves survival, the study by Lisan et al. will undoubtedly make these clinicians’ jobs a little easier by enabling them to present to their patients evidence that PAP may be associated with reduced mortality, particularly in those with severe OSA and comorbid obesity.”
Dr. Kushida receives salary support from a contract between Stanford University and Philips-Respironics for the conduct of a clinical trial. These comments are from an accompanying editorial (JAMA Otolaryngol Head Neck Surg. 2019 April 11. doi: 10.1001/jamaoto.2019.0345).
according to the results of a cohort study published in JAMA Otolaryngology–Head & Neck Surgery.
The association becomes evident several years after positive airway pressure (PAP) initiation, according to the researchers. Obstructive sleep apnea (OSA) is among the top 10 modifiable cardiovascular risk factors, and is associated with increased risks of coronary artery disease, stroke, and death. PAP is the most effective treatment for OSA, but this treatment’s effect on all-cause and cardiovascular mortality is uncertain. Randomized trials have yielded inconclusive answers to this question, and evidence from observational studies has been weak.
To investigate the association between PAP prescription and mortality in patients with obesity and severe OSA, Quentin Lisan, MD, of the Paris Cardiovascular Research Center and his colleagues conducted a multicenter, population-based cohort study. The researchers examined data for 392 participants in the Sleep Heart Health Study, in which adult men and women age 40 years or older were recruited from nine population-based studies between 1995 and 1998 and followed for a mean of 11.1 years. With each participant who had been prescribed PAP, the investigators matched as many as four participants who had not been prescribed PAP, on the basis of age, sex, and apnea-hypopnea index. Of this sample, 81 patients were prescribed PAP, and 311 were not.
All participants had a clinic visit and underwent overnight polysomnography at baseline. At 2-3 years, participants had a follow-up visit or phone call, during which they were asked whether their physicians had prescribed PAP. Participants were monitored for cardiovascular and all-cause mortality.
In all, 319 of the 392 participants were men; the population’s mean age was 63 years. Patients who had received a PAP prescription had a higher body mass index and more education, compared with patients who had not received a prescription. Mean follow-up duration was 11.6 years in the PAP-prescribed group and 10.9 years in the nonprescribed group.
A total of 96 deaths occurred during follow-up: 12 in the PAP-prescribed group and 84 in the nonprescribed PAP group. The crude incidence rate of mortality was 24.7 deaths per 1,000 person-years in the nonprescribed group and 12.8 deaths per 1,000 person-years in the PAP-prescribed group. The difference in survival between the prescribed and nonprescribed groups was evident in survival curves after 6-7 years of follow-up. After adjustments for prevalent cardiovascular disease, hypertension, diabetes, body mass index, education level, smoking status, and alcohol consumption, the hazard ratio of all-cause mortality for the prescribed group was 0.38, compared with the nonprescribed group.
Dr. Lisan and his colleagues identified 27 deaths of cardiovascular origin, one of which occurred in the prescribed group. After adjusting for prevalent cardiovascular disease, the hazard ratio of cardiovascular mortality for the prescribed group was 0.06, compared with the nonprescribed group.
One reason that the reduction in mortality associated with PAP was not found in previous randomized, controlled trials could be that their mean length of follow-up was not long enough, the researchers wrote. For example, the mean length of follow-up in the SAVE trial was 3.7 years, but the survival benefit was not apparent in the present analysis until 6-7 years after treatment initiation.
These results are exploratory and require confirmation in future research, Dr. Lisan and his colleagues wrote. No information on adherence to PAP was available, and the researchers could not account for initiation and interruption of PAP therapy. Nevertheless, “prescribing PAP in patients with OSA should be pursued and encouraged, given its potential major public health implication,” they concluded.
The Sleep Heart Health Study was supported by grants from the National Institutes of Health.
SOURCE: Lisan Q et al. JAMA Otolaryngol Head Neck Surg. 2019 Apr 11. doi: 10.1001/jamaoto.2019.0281.
according to the results of a cohort study published in JAMA Otolaryngology–Head & Neck Surgery.
The association becomes evident several years after positive airway pressure (PAP) initiation, according to the researchers. Obstructive sleep apnea (OSA) is among the top 10 modifiable cardiovascular risk factors, and is associated with increased risks of coronary artery disease, stroke, and death. PAP is the most effective treatment for OSA, but this treatment’s effect on all-cause and cardiovascular mortality is uncertain. Randomized trials have yielded inconclusive answers to this question, and evidence from observational studies has been weak.
To investigate the association between PAP prescription and mortality in patients with obesity and severe OSA, Quentin Lisan, MD, of the Paris Cardiovascular Research Center and his colleagues conducted a multicenter, population-based cohort study. The researchers examined data for 392 participants in the Sleep Heart Health Study, in which adult men and women age 40 years or older were recruited from nine population-based studies between 1995 and 1998 and followed for a mean of 11.1 years. With each participant who had been prescribed PAP, the investigators matched as many as four participants who had not been prescribed PAP, on the basis of age, sex, and apnea-hypopnea index. Of this sample, 81 patients were prescribed PAP, and 311 were not.
All participants had a clinic visit and underwent overnight polysomnography at baseline. At 2-3 years, participants had a follow-up visit or phone call, during which they were asked whether their physicians had prescribed PAP. Participants were monitored for cardiovascular and all-cause mortality.
In all, 319 of the 392 participants were men; the population’s mean age was 63 years. Patients who had received a PAP prescription had a higher body mass index and more education, compared with patients who had not received a prescription. Mean follow-up duration was 11.6 years in the PAP-prescribed group and 10.9 years in the nonprescribed group.
A total of 96 deaths occurred during follow-up: 12 in the PAP-prescribed group and 84 in the nonprescribed PAP group. The crude incidence rate of mortality was 24.7 deaths per 1,000 person-years in the nonprescribed group and 12.8 deaths per 1,000 person-years in the PAP-prescribed group. The difference in survival between the prescribed and nonprescribed groups was evident in survival curves after 6-7 years of follow-up. After adjustments for prevalent cardiovascular disease, hypertension, diabetes, body mass index, education level, smoking status, and alcohol consumption, the hazard ratio of all-cause mortality for the prescribed group was 0.38, compared with the nonprescribed group.
Dr. Lisan and his colleagues identified 27 deaths of cardiovascular origin, one of which occurred in the prescribed group. After adjusting for prevalent cardiovascular disease, the hazard ratio of cardiovascular mortality for the prescribed group was 0.06, compared with the nonprescribed group.
One reason that the reduction in mortality associated with PAP was not found in previous randomized, controlled trials could be that their mean length of follow-up was not long enough, the researchers wrote. For example, the mean length of follow-up in the SAVE trial was 3.7 years, but the survival benefit was not apparent in the present analysis until 6-7 years after treatment initiation.
These results are exploratory and require confirmation in future research, Dr. Lisan and his colleagues wrote. No information on adherence to PAP was available, and the researchers could not account for initiation and interruption of PAP therapy. Nevertheless, “prescribing PAP in patients with OSA should be pursued and encouraged, given its potential major public health implication,” they concluded.
The Sleep Heart Health Study was supported by grants from the National Institutes of Health.
SOURCE: Lisan Q et al. JAMA Otolaryngol Head Neck Surg. 2019 Apr 11. doi: 10.1001/jamaoto.2019.0281.
FROM JAMA OTOLARYNGOLOGY–HEAD & NECK SURGERY
New sleep apnea guidelines offer evidence-based recommendations
New guidelines on treating obstructive sleep apnea with positive airway pressure include recommendations for using positive airway pressure (PAP) versus no therapy, using either continuous PAP (CPAP) or automatic PAP (APAP) for ongoing treatment, and providing educational interventions to patients starting PAP. The complete guidelines, issued by the American Academy of Sleep Medicine, were published in the Journal of Clinical Sleep Medicine.
The guidelines were driven by improvements in PAP adherence and device technology, wrote lead author Susheel P. Patil, MD, of Johns Hopkins University, Baltimore, and his colleagues.
The guidelines begin with a pair of Good Practice Statements to ensure effective and appropriate management of obstructive sleep apnea (OSA) in adults. First, “Treatment of OSA with PAP therapy should be based on a diagnosis of OSA established using objective sleep apnea testing.” Second, “Adequate follow-up, including troubleshooting and monitoring of objective efficacy and usage data to ensure adequate treatment and adherence, should occur following PAP therapy initiation and during treatment of OSA.”
The nine recommendations, approved by the AASM board of directors, include four strong recommendations that clinicians should follow under most circumstances, and five conditional recommendations that are suggested but lack strong clinical support for their appropriateness for all patients in all circumstances.
The first of the strong recommendations, for using PAP versus no therapy to treat adults with OSA and excessive sleepiness, was based on a high level of evidence from a meta-analysis of 38 randomized, controlled trials and the conclusion that the benefits of PAP outweighed the harms.
The second strong recommendation for using either CPAP or APAP for ongoing treatment was based on data from 26 trials that showed no clinically significant difference between the two. The third strong recommendation that PAP therapy be initiated using either APAP at home or in-laboratory PAP titration in adults with OSA and no significant comorbidities was supported by a meta-analysis of 10 trials that showed no clinically significant difference between at-home and laboratory initiation, and that each option has its benefits. The authors noted that “the majority of well-informed adult patients with OSA and without significant comorbidities would prefer initiation of PAP using the most rapid, convenient, and cost-effective strategy.” This comment supports the fourth strong recommendation for providing educational interventions to patients starting PAP.
The conditional recommendations include using PAP versus no therapy for adults with OSA and impaired quality of life related to poor sleep, such as insomnia, snoring, morning headaches, and daytime fatigue. Other conditional recommendations include using PAP versus no therapy for adults with OSA and comorbid hypertension, choosing CPAP or APAP over bilateral PAP for routine treatment of OSA in adults, providing behavioral interventions or troubleshooting during patients’ initial use of PAP, and using telemonitoring-guided interventions to monitor patients during their initial use of PAP.
“The ultimate judgment regarding any specific care must be made by the treating clinician and the patient, taking into consideration the individual circumstances of the patient, available treatment options, and resources,” the authors noted.
“When implementing the recommendations, providers should consider additional strategies that will maximize the individual patient’s comfort and adherence such as nasal/intranasal over oronasal mask interface and heated humidification,” they added.
The guidelines were developed by a task force commissioned by the AASM that included board-certified sleep specialists and experts in PAP use, and will be reviewed and updated as new information surfaces, the authors wrote.
Dr. Patil reported no financial conflicts; several coauthors reported conflicts that were managed by their not voting on guidelines related to those conflicts.
SOURCE: Patil SP et al. J Clin Sleep Med. 2018 Feb 15;15(2):335-43.
Octavian C. Ioachimescu, MD, FCCP, comments: The last guidelines and practice parameters for the use of positive airway pressure (PAP) as therapy for adult patients with obstructive sleep apnea, were published in 2006 and 2008, respectively. Since then, new technological advances, an ever-growing body of literature, and shifting practice patterns led to an acute need for a thorough reassessment, a comprehensive update of the previous recommendations, and the potential of issuing new ones for emerging areas. As such, the American Academy of Sleep Medicine commissioned a task force of content experts to review the existing evidence, to issue new guidelines and to publish an associated systematic review and a meta-analysis of the literature on this topic.
A welcome recommendation is the endorsement by the task force of the use of telemedicine capabilities in monitoring patients’ adherence to PAP therapy. Another interesting aspect is that, while our literature is represented by a mix of both randomized and nonrandomized controlled trials, occasionally there seems to be an interesting dichotomy in the results: Randomized trials tend to point in one direction, while nonrandomized studies pooled in the meta-analysis seem to point to the contrary or to give the impression of more definitive effects. While this is clearly not the place to make an extensive analysis of the strengths and the potential pitfalls of randomized versus nonrandomized studies, this clearly raises some issues. One is that our randomized studies are typically small, underpowered, and hence with nonconvincing risk or hazard reduction assessments. Second, the dichotomy in the results may be driven by publication bias, expense, and difficulty in performing adequately-powered, long-term trials that essentially may be studying small effects.
Guidelines are not intended to be used in an Occam’s razor approach, but in a fashion that would allow individualization of therapy while critically appraising the existing evidence for various interventions in specific conditions and maintaining a very stringent and critical view on generalizability, expected results, and adequate management of reasonable expectations. In addition, the areas that are unclear, with conflicting evidence or in which the guidelines allow “too much” latitude to the treating clinician, may be seen as either an invitation to remain “creative,” or one for abstaining from action in the name of equipoise. I would advise that both extremes are to be avoided.
Octavian C. Ioachimescu, MD, FCCP, comments: The last guidelines and practice parameters for the use of positive airway pressure (PAP) as therapy for adult patients with obstructive sleep apnea, were published in 2006 and 2008, respectively. Since then, new technological advances, an ever-growing body of literature, and shifting practice patterns led to an acute need for a thorough reassessment, a comprehensive update of the previous recommendations, and the potential of issuing new ones for emerging areas. As such, the American Academy of Sleep Medicine commissioned a task force of content experts to review the existing evidence, to issue new guidelines and to publish an associated systematic review and a meta-analysis of the literature on this topic.
A welcome recommendation is the endorsement by the task force of the use of telemedicine capabilities in monitoring patients’ adherence to PAP therapy. Another interesting aspect is that, while our literature is represented by a mix of both randomized and nonrandomized controlled trials, occasionally there seems to be an interesting dichotomy in the results: Randomized trials tend to point in one direction, while nonrandomized studies pooled in the meta-analysis seem to point to the contrary or to give the impression of more definitive effects. While this is clearly not the place to make an extensive analysis of the strengths and the potential pitfalls of randomized versus nonrandomized studies, this clearly raises some issues. One is that our randomized studies are typically small, underpowered, and hence with nonconvincing risk or hazard reduction assessments. Second, the dichotomy in the results may be driven by publication bias, expense, and difficulty in performing adequately-powered, long-term trials that essentially may be studying small effects.
Guidelines are not intended to be used in an Occam’s razor approach, but in a fashion that would allow individualization of therapy while critically appraising the existing evidence for various interventions in specific conditions and maintaining a very stringent and critical view on generalizability, expected results, and adequate management of reasonable expectations. In addition, the areas that are unclear, with conflicting evidence or in which the guidelines allow “too much” latitude to the treating clinician, may be seen as either an invitation to remain “creative,” or one for abstaining from action in the name of equipoise. I would advise that both extremes are to be avoided.
Octavian C. Ioachimescu, MD, FCCP, comments: The last guidelines and practice parameters for the use of positive airway pressure (PAP) as therapy for adult patients with obstructive sleep apnea, were published in 2006 and 2008, respectively. Since then, new technological advances, an ever-growing body of literature, and shifting practice patterns led to an acute need for a thorough reassessment, a comprehensive update of the previous recommendations, and the potential of issuing new ones for emerging areas. As such, the American Academy of Sleep Medicine commissioned a task force of content experts to review the existing evidence, to issue new guidelines and to publish an associated systematic review and a meta-analysis of the literature on this topic.
A welcome recommendation is the endorsement by the task force of the use of telemedicine capabilities in monitoring patients’ adherence to PAP therapy. Another interesting aspect is that, while our literature is represented by a mix of both randomized and nonrandomized controlled trials, occasionally there seems to be an interesting dichotomy in the results: Randomized trials tend to point in one direction, while nonrandomized studies pooled in the meta-analysis seem to point to the contrary or to give the impression of more definitive effects. While this is clearly not the place to make an extensive analysis of the strengths and the potential pitfalls of randomized versus nonrandomized studies, this clearly raises some issues. One is that our randomized studies are typically small, underpowered, and hence with nonconvincing risk or hazard reduction assessments. Second, the dichotomy in the results may be driven by publication bias, expense, and difficulty in performing adequately-powered, long-term trials that essentially may be studying small effects.
Guidelines are not intended to be used in an Occam’s razor approach, but in a fashion that would allow individualization of therapy while critically appraising the existing evidence for various interventions in specific conditions and maintaining a very stringent and critical view on generalizability, expected results, and adequate management of reasonable expectations. In addition, the areas that are unclear, with conflicting evidence or in which the guidelines allow “too much” latitude to the treating clinician, may be seen as either an invitation to remain “creative,” or one for abstaining from action in the name of equipoise. I would advise that both extremes are to be avoided.
New guidelines on treating obstructive sleep apnea with positive airway pressure include recommendations for using positive airway pressure (PAP) versus no therapy, using either continuous PAP (CPAP) or automatic PAP (APAP) for ongoing treatment, and providing educational interventions to patients starting PAP. The complete guidelines, issued by the American Academy of Sleep Medicine, were published in the Journal of Clinical Sleep Medicine.
The guidelines were driven by improvements in PAP adherence and device technology, wrote lead author Susheel P. Patil, MD, of Johns Hopkins University, Baltimore, and his colleagues.
The guidelines begin with a pair of Good Practice Statements to ensure effective and appropriate management of obstructive sleep apnea (OSA) in adults. First, “Treatment of OSA with PAP therapy should be based on a diagnosis of OSA established using objective sleep apnea testing.” Second, “Adequate follow-up, including troubleshooting and monitoring of objective efficacy and usage data to ensure adequate treatment and adherence, should occur following PAP therapy initiation and during treatment of OSA.”
The nine recommendations, approved by the AASM board of directors, include four strong recommendations that clinicians should follow under most circumstances, and five conditional recommendations that are suggested but lack strong clinical support for their appropriateness for all patients in all circumstances.
The first of the strong recommendations, for using PAP versus no therapy to treat adults with OSA and excessive sleepiness, was based on a high level of evidence from a meta-analysis of 38 randomized, controlled trials and the conclusion that the benefits of PAP outweighed the harms.
The second strong recommendation for using either CPAP or APAP for ongoing treatment was based on data from 26 trials that showed no clinically significant difference between the two. The third strong recommendation that PAP therapy be initiated using either APAP at home or in-laboratory PAP titration in adults with OSA and no significant comorbidities was supported by a meta-analysis of 10 trials that showed no clinically significant difference between at-home and laboratory initiation, and that each option has its benefits. The authors noted that “the majority of well-informed adult patients with OSA and without significant comorbidities would prefer initiation of PAP using the most rapid, convenient, and cost-effective strategy.” This comment supports the fourth strong recommendation for providing educational interventions to patients starting PAP.
The conditional recommendations include using PAP versus no therapy for adults with OSA and impaired quality of life related to poor sleep, such as insomnia, snoring, morning headaches, and daytime fatigue. Other conditional recommendations include using PAP versus no therapy for adults with OSA and comorbid hypertension, choosing CPAP or APAP over bilateral PAP for routine treatment of OSA in adults, providing behavioral interventions or troubleshooting during patients’ initial use of PAP, and using telemonitoring-guided interventions to monitor patients during their initial use of PAP.
“The ultimate judgment regarding any specific care must be made by the treating clinician and the patient, taking into consideration the individual circumstances of the patient, available treatment options, and resources,” the authors noted.
“When implementing the recommendations, providers should consider additional strategies that will maximize the individual patient’s comfort and adherence such as nasal/intranasal over oronasal mask interface and heated humidification,” they added.
The guidelines were developed by a task force commissioned by the AASM that included board-certified sleep specialists and experts in PAP use, and will be reviewed and updated as new information surfaces, the authors wrote.
Dr. Patil reported no financial conflicts; several coauthors reported conflicts that were managed by their not voting on guidelines related to those conflicts.
SOURCE: Patil SP et al. J Clin Sleep Med. 2018 Feb 15;15(2):335-43.
New guidelines on treating obstructive sleep apnea with positive airway pressure include recommendations for using positive airway pressure (PAP) versus no therapy, using either continuous PAP (CPAP) or automatic PAP (APAP) for ongoing treatment, and providing educational interventions to patients starting PAP. The complete guidelines, issued by the American Academy of Sleep Medicine, were published in the Journal of Clinical Sleep Medicine.
The guidelines were driven by improvements in PAP adherence and device technology, wrote lead author Susheel P. Patil, MD, of Johns Hopkins University, Baltimore, and his colleagues.
The guidelines begin with a pair of Good Practice Statements to ensure effective and appropriate management of obstructive sleep apnea (OSA) in adults. First, “Treatment of OSA with PAP therapy should be based on a diagnosis of OSA established using objective sleep apnea testing.” Second, “Adequate follow-up, including troubleshooting and monitoring of objective efficacy and usage data to ensure adequate treatment and adherence, should occur following PAP therapy initiation and during treatment of OSA.”
The nine recommendations, approved by the AASM board of directors, include four strong recommendations that clinicians should follow under most circumstances, and five conditional recommendations that are suggested but lack strong clinical support for their appropriateness for all patients in all circumstances.
The first of the strong recommendations, for using PAP versus no therapy to treat adults with OSA and excessive sleepiness, was based on a high level of evidence from a meta-analysis of 38 randomized, controlled trials and the conclusion that the benefits of PAP outweighed the harms.
The second strong recommendation for using either CPAP or APAP for ongoing treatment was based on data from 26 trials that showed no clinically significant difference between the two. The third strong recommendation that PAP therapy be initiated using either APAP at home or in-laboratory PAP titration in adults with OSA and no significant comorbidities was supported by a meta-analysis of 10 trials that showed no clinically significant difference between at-home and laboratory initiation, and that each option has its benefits. The authors noted that “the majority of well-informed adult patients with OSA and without significant comorbidities would prefer initiation of PAP using the most rapid, convenient, and cost-effective strategy.” This comment supports the fourth strong recommendation for providing educational interventions to patients starting PAP.
The conditional recommendations include using PAP versus no therapy for adults with OSA and impaired quality of life related to poor sleep, such as insomnia, snoring, morning headaches, and daytime fatigue. Other conditional recommendations include using PAP versus no therapy for adults with OSA and comorbid hypertension, choosing CPAP or APAP over bilateral PAP for routine treatment of OSA in adults, providing behavioral interventions or troubleshooting during patients’ initial use of PAP, and using telemonitoring-guided interventions to monitor patients during their initial use of PAP.
“The ultimate judgment regarding any specific care must be made by the treating clinician and the patient, taking into consideration the individual circumstances of the patient, available treatment options, and resources,” the authors noted.
“When implementing the recommendations, providers should consider additional strategies that will maximize the individual patient’s comfort and adherence such as nasal/intranasal over oronasal mask interface and heated humidification,” they added.
The guidelines were developed by a task force commissioned by the AASM that included board-certified sleep specialists and experts in PAP use, and will be reviewed and updated as new information surfaces, the authors wrote.
Dr. Patil reported no financial conflicts; several coauthors reported conflicts that were managed by their not voting on guidelines related to those conflicts.
SOURCE: Patil SP et al. J Clin Sleep Med. 2018 Feb 15;15(2):335-43.
FROM THE JOURNAL OF CLINICAL SLEEP MEDICINE
Depression, antidepressant use may be common among patients with OSA
About a quarter of patients with obstructive sleep apnea also had clinical depression and used antidepressants, recent research has shown.
Although patients in the study associated their sleep disorder with poorer quality of life as well as symptoms of anxiety and depression, it is unclear whether treating their obstructive sleep apnea (OSA) with continuous positive airway pressure (CPAP) would alleviate these symptoms, said Melinda L. Jackson, PhD, from Monash University in Clayton, Victoria, Australia, and her colleagues.
“OSA is a modifiable factor that, if treated, may reduce the economic, health care, and personal burden of depression,” Dr. Jackson and her colleagues wrote in their study, recently published in the journal Sleep Medicine. “Findings from the treatment phase of this study will help us determine whether clinical depression is alleviated with CPAP use, taking into account antidepressant use; whether there are subgroups of patients who respond better to treatment; and what are the characteristics of patients who respond compared to those who remain depressed.”
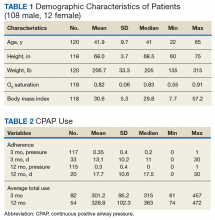
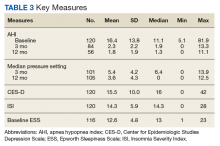
The researchers used baseline data from 109 patients in the CPAP for OSA and Depression trial who were diagnosed with OSA. Participants (mean age, 52.6 years; 43.1% female) consecutively presented to a sleep laboratory where they answered interview questions to assess clinical depression and sleep habits. Data were collected using the structured clinical interview for depression (SCID-IV), Hospital Anxiety and Depression Scale, Pittsburgh Sleep Quality Index (PSQI), Functional Outcomes of Sleep Questionnaire (FOSQ), Epworth Sleepiness Scale, and Assessment of Quality of Life questionnaire. In addition, the researchers performed a meta-analysis of seven studies, including the current study, to determine the prevalence of clinical depression among patients with untreated OSA.
Overall, SCID-IV scores identified clinical depression in 25 participants (22.7%), and these participants said they had greater sleep disturbance and reported higher depressive, anxiety and stress as well as lower quality of life as a result of their clinical depression. Researchers found these participants also had significantly worse quality of sleep (P less than .05) and daytime dysfunction (P less than .05) as identified by PSQI scores, while FOSQ results showed participants with clinical depression had significantly lower activity levels, social outcomes, and general productivity, compared with patients without clinical depression (P less than .05). In a meta-analysis, Dr. Jackson and her colleagues found a pooled prevalence of 23% for clinical depression among participants with OSA.
Participants using antidepressants were examined separately from participants who had clinical depression. The researchers found 27 participants (24.8%) using antidepressants who also had reported higher symptoms of anxiety, depression and stress, lower quality of life, and poorer sleep outcomes. Participants using antidepressants also were more likely to have bipolar disorder or a condition such as hypertension, chronic obstructive pulmonary disease, high cholesterol, or type 2 diabetes, and 75% of these participants reported having some type of comorbid condition.
Dr. Jackson and her colleagues noted they were uncertain whether depression or OSA occurred first, or whether depression exacerbated symptoms of OSA through other factors such as weight gain, sleep disruption, inactivity, or alcohol use. Depression and OSA may also present independently of one another, they added.
“Development of scales to better capture information about when symptoms commenced and the length of time an individual has experienced OSA will provide a clearer understanding of the consequences of OSA on psychological and medical conditions,” the researchers said.
This study was funded by the Austin Medical Research Fund, and one authors reported support from an National Health and Medical Research Council Early Career Fellowship. The authors report no relevant conflicts of interest.
SOURCE: Jackson ML et al. Sleep Med. 2019 Mar 27. doi: 10.1016/j.sleep.2019.03.011.
About a quarter of patients with obstructive sleep apnea also had clinical depression and used antidepressants, recent research has shown.
Although patients in the study associated their sleep disorder with poorer quality of life as well as symptoms of anxiety and depression, it is unclear whether treating their obstructive sleep apnea (OSA) with continuous positive airway pressure (CPAP) would alleviate these symptoms, said Melinda L. Jackson, PhD, from Monash University in Clayton, Victoria, Australia, and her colleagues.
“OSA is a modifiable factor that, if treated, may reduce the economic, health care, and personal burden of depression,” Dr. Jackson and her colleagues wrote in their study, recently published in the journal Sleep Medicine. “Findings from the treatment phase of this study will help us determine whether clinical depression is alleviated with CPAP use, taking into account antidepressant use; whether there are subgroups of patients who respond better to treatment; and what are the characteristics of patients who respond compared to those who remain depressed.”
The researchers used baseline data from 109 patients in the CPAP for OSA and Depression trial who were diagnosed with OSA. Participants (mean age, 52.6 years; 43.1% female) consecutively presented to a sleep laboratory where they answered interview questions to assess clinical depression and sleep habits. Data were collected using the structured clinical interview for depression (SCID-IV), Hospital Anxiety and Depression Scale, Pittsburgh Sleep Quality Index (PSQI), Functional Outcomes of Sleep Questionnaire (FOSQ), Epworth Sleepiness Scale, and Assessment of Quality of Life questionnaire. In addition, the researchers performed a meta-analysis of seven studies, including the current study, to determine the prevalence of clinical depression among patients with untreated OSA.
Overall, SCID-IV scores identified clinical depression in 25 participants (22.7%), and these participants said they had greater sleep disturbance and reported higher depressive, anxiety and stress as well as lower quality of life as a result of their clinical depression. Researchers found these participants also had significantly worse quality of sleep (P less than .05) and daytime dysfunction (P less than .05) as identified by PSQI scores, while FOSQ results showed participants with clinical depression had significantly lower activity levels, social outcomes, and general productivity, compared with patients without clinical depression (P less than .05). In a meta-analysis, Dr. Jackson and her colleagues found a pooled prevalence of 23% for clinical depression among participants with OSA.
Participants using antidepressants were examined separately from participants who had clinical depression. The researchers found 27 participants (24.8%) using antidepressants who also had reported higher symptoms of anxiety, depression and stress, lower quality of life, and poorer sleep outcomes. Participants using antidepressants also were more likely to have bipolar disorder or a condition such as hypertension, chronic obstructive pulmonary disease, high cholesterol, or type 2 diabetes, and 75% of these participants reported having some type of comorbid condition.
Dr. Jackson and her colleagues noted they were uncertain whether depression or OSA occurred first, or whether depression exacerbated symptoms of OSA through other factors such as weight gain, sleep disruption, inactivity, or alcohol use. Depression and OSA may also present independently of one another, they added.
“Development of scales to better capture information about when symptoms commenced and the length of time an individual has experienced OSA will provide a clearer understanding of the consequences of OSA on psychological and medical conditions,” the researchers said.
This study was funded by the Austin Medical Research Fund, and one authors reported support from an National Health and Medical Research Council Early Career Fellowship. The authors report no relevant conflicts of interest.
SOURCE: Jackson ML et al. Sleep Med. 2019 Mar 27. doi: 10.1016/j.sleep.2019.03.011.
About a quarter of patients with obstructive sleep apnea also had clinical depression and used antidepressants, recent research has shown.
Although patients in the study associated their sleep disorder with poorer quality of life as well as symptoms of anxiety and depression, it is unclear whether treating their obstructive sleep apnea (OSA) with continuous positive airway pressure (CPAP) would alleviate these symptoms, said Melinda L. Jackson, PhD, from Monash University in Clayton, Victoria, Australia, and her colleagues.
“OSA is a modifiable factor that, if treated, may reduce the economic, health care, and personal burden of depression,” Dr. Jackson and her colleagues wrote in their study, recently published in the journal Sleep Medicine. “Findings from the treatment phase of this study will help us determine whether clinical depression is alleviated with CPAP use, taking into account antidepressant use; whether there are subgroups of patients who respond better to treatment; and what are the characteristics of patients who respond compared to those who remain depressed.”
The researchers used baseline data from 109 patients in the CPAP for OSA and Depression trial who were diagnosed with OSA. Participants (mean age, 52.6 years; 43.1% female) consecutively presented to a sleep laboratory where they answered interview questions to assess clinical depression and sleep habits. Data were collected using the structured clinical interview for depression (SCID-IV), Hospital Anxiety and Depression Scale, Pittsburgh Sleep Quality Index (PSQI), Functional Outcomes of Sleep Questionnaire (FOSQ), Epworth Sleepiness Scale, and Assessment of Quality of Life questionnaire. In addition, the researchers performed a meta-analysis of seven studies, including the current study, to determine the prevalence of clinical depression among patients with untreated OSA.
Overall, SCID-IV scores identified clinical depression in 25 participants (22.7%), and these participants said they had greater sleep disturbance and reported higher depressive, anxiety and stress as well as lower quality of life as a result of their clinical depression. Researchers found these participants also had significantly worse quality of sleep (P less than .05) and daytime dysfunction (P less than .05) as identified by PSQI scores, while FOSQ results showed participants with clinical depression had significantly lower activity levels, social outcomes, and general productivity, compared with patients without clinical depression (P less than .05). In a meta-analysis, Dr. Jackson and her colleagues found a pooled prevalence of 23% for clinical depression among participants with OSA.
Participants using antidepressants were examined separately from participants who had clinical depression. The researchers found 27 participants (24.8%) using antidepressants who also had reported higher symptoms of anxiety, depression and stress, lower quality of life, and poorer sleep outcomes. Participants using antidepressants also were more likely to have bipolar disorder or a condition such as hypertension, chronic obstructive pulmonary disease, high cholesterol, or type 2 diabetes, and 75% of these participants reported having some type of comorbid condition.
Dr. Jackson and her colleagues noted they were uncertain whether depression or OSA occurred first, or whether depression exacerbated symptoms of OSA through other factors such as weight gain, sleep disruption, inactivity, or alcohol use. Depression and OSA may also present independently of one another, they added.
“Development of scales to better capture information about when symptoms commenced and the length of time an individual has experienced OSA will provide a clearer understanding of the consequences of OSA on psychological and medical conditions,” the researchers said.
This study was funded by the Austin Medical Research Fund, and one authors reported support from an National Health and Medical Research Council Early Career Fellowship. The authors report no relevant conflicts of interest.
SOURCE: Jackson ML et al. Sleep Med. 2019 Mar 27. doi: 10.1016/j.sleep.2019.03.011.
FROM SLEEP MEDICINE
Long-term CPAP use not linked to weight gain
Continuous positive airway pressure (CPAP) over several years did not lead to clinically concerning levels of weight gain among patients with obstructive sleep apnea and comorbid cardiovascular disease enrolled in a large international trial, findings from a large, multicenter trial show.
No differences in weight, body mass index (BMI), or other body measurements were found when comparing CPAP and control groups in a post hoc analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) trial, which included 2,483 adults enrolled at 89 centers in seven countries.
In a subanalysis, there was a small but statistically significant weight gain of less than 400 g in men who used CPAP at least 4 hours per night as compared to matched controls. However, there were no differences in BMI or neck and waist circumferences for these men, and no such changes were observed in women, according to the investigators, led by Qiong Ou, MD, of Guangdong (China) General Hospital and R. Doug McEvoy, MD, of the Adelaide Institute for Sleep Health at Flinders University, Adelaide, Australia.
“Such a small change in weight, even with good adherence over several years, is highly unlikely to have any serious clinical ramifications,” wrote the investigators of the study published in Chest.
“Taken together, these results indicate that long-term CPAP treatment is unlikely to exacerbate the problems of overweight and obesity that are common among patients with OSA,” they added.
In a previous meta-analysis of randomized trials, investigators concluded that CPAP promoted significant increases in BMI and weight. However, the median study duration was only 3 months.
In contrast, the analysis of the SAVE trial included adults who had regular body measurements over a mean follow-up of nearly 4 years.
That long-term follow-up provided an “ideal opportunity” to assess whether CPAP treatment promotes weight gain in OSA patients over the course of several years, the authors of the SAVE trial analysis wrote.
For men in the SAVE trial, the difference in weight change for the CPAP group vs. the control group was just 0.07 kg (95% confidence interval, –0.40 to 0.54; P = .773) while in women, the difference for CPAP vs. controls was –0.14 kg (95% CI, –0.37 to 0.09; P = .233), the investigators reported.
Weight gain was significantly higher among men with good CPAP adherence, defined as use for at least 4 hours per night, investigators said, noting a mean difference of 0.38 kg (95% CI, 0.04-0.73; P = .031), though no other differences were found in body measurements for men, and no such associations were found in women with good CPAP adherence.
It’s not exactly clear why this SAVE analysis would find no evidence of CPAP promoting weight gain over the long term, in contrast to the earlier meta-analysis of short-term studies finding a significant risk of weight gain.
However, it is possible that differences in study populations such as ethnicity, age, or comorbidities contributed to the differences, said investigators.
For example, results of regression analysis in the present study showed that, compared with recruitment in Australia, recruitment in China and India was significantly linked to weight loss, while recruitment in New Zealand was linked to weight gain.
Dr. Ou had no disclosures related to the study, while Dr. McEvoy reported disclosures related to Philips Respironics, ResMed, Fisher & Paykel, Air Liquide, and the National Health and Medical Research Council of Australia.
SOURCE: Ou Q et al. Chest. 2019 Apr;155(4):720-9.
This analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) trial had several strengths and a reassuring conclusion regarding lack of weight gain with long-term use of CPAP in patients with obstructive sleep apnea (OSA) and comorbid cardiovascular disease. However, the findings may be difficult to extrapolate to Western countries, according to authors of an editorial.
“It is conceivable that the results of the study would have been different if the predominant race of the participants had been Caucasian and had a higher BMI,” said Rohit Budhiraja, MBBS, and Stuart F. Quan, MD, in the editorial. Two-thirds of the patients in the were enrolled in China, the authors said, noting that it is “well established” that Asians with OSA are less often obese compared with Caucasians with OSA in Western countries.
For clinicians, the most important message of this analysis of the SAVE trial should be that weight loss did not occur, according to Dr. Budhiraja and Dr. Quan.
“A comprehensive approach to weight loss should be used, instead of the optimistic view that improved sleep quality and daytime symptoms will automatically translate into increase physical activity, better nutrition and weight loss,” they concluded in their editorial.
Dr. Budhiraja is affiliated with the Brigham and Women’s Hospital, and Harvard Medical School, both in Boston; Dr. Quan is affiliated with Harvard Medical School, Boston, and the University of Arizona Tucson. Their editorial appears in Chest ( 2019 Apr;155[4] 657-8 ). Dr. Budhiraja reported no conflicts of interest. Dr. Quan reported serving as a consultant for Jazz Pharmaceuticals and Best Doctors, along with grant funding from the National Institutes of Health.
This analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) trial had several strengths and a reassuring conclusion regarding lack of weight gain with long-term use of CPAP in patients with obstructive sleep apnea (OSA) and comorbid cardiovascular disease. However, the findings may be difficult to extrapolate to Western countries, according to authors of an editorial.
“It is conceivable that the results of the study would have been different if the predominant race of the participants had been Caucasian and had a higher BMI,” said Rohit Budhiraja, MBBS, and Stuart F. Quan, MD, in the editorial. Two-thirds of the patients in the were enrolled in China, the authors said, noting that it is “well established” that Asians with OSA are less often obese compared with Caucasians with OSA in Western countries.
For clinicians, the most important message of this analysis of the SAVE trial should be that weight loss did not occur, according to Dr. Budhiraja and Dr. Quan.
“A comprehensive approach to weight loss should be used, instead of the optimistic view that improved sleep quality and daytime symptoms will automatically translate into increase physical activity, better nutrition and weight loss,” they concluded in their editorial.
Dr. Budhiraja is affiliated with the Brigham and Women’s Hospital, and Harvard Medical School, both in Boston; Dr. Quan is affiliated with Harvard Medical School, Boston, and the University of Arizona Tucson. Their editorial appears in Chest ( 2019 Apr;155[4] 657-8 ). Dr. Budhiraja reported no conflicts of interest. Dr. Quan reported serving as a consultant for Jazz Pharmaceuticals and Best Doctors, along with grant funding from the National Institutes of Health.
This analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) trial had several strengths and a reassuring conclusion regarding lack of weight gain with long-term use of CPAP in patients with obstructive sleep apnea (OSA) and comorbid cardiovascular disease. However, the findings may be difficult to extrapolate to Western countries, according to authors of an editorial.
“It is conceivable that the results of the study would have been different if the predominant race of the participants had been Caucasian and had a higher BMI,” said Rohit Budhiraja, MBBS, and Stuart F. Quan, MD, in the editorial. Two-thirds of the patients in the were enrolled in China, the authors said, noting that it is “well established” that Asians with OSA are less often obese compared with Caucasians with OSA in Western countries.
For clinicians, the most important message of this analysis of the SAVE trial should be that weight loss did not occur, according to Dr. Budhiraja and Dr. Quan.
“A comprehensive approach to weight loss should be used, instead of the optimistic view that improved sleep quality and daytime symptoms will automatically translate into increase physical activity, better nutrition and weight loss,” they concluded in their editorial.
Dr. Budhiraja is affiliated with the Brigham and Women’s Hospital, and Harvard Medical School, both in Boston; Dr. Quan is affiliated with Harvard Medical School, Boston, and the University of Arizona Tucson. Their editorial appears in Chest ( 2019 Apr;155[4] 657-8 ). Dr. Budhiraja reported no conflicts of interest. Dr. Quan reported serving as a consultant for Jazz Pharmaceuticals and Best Doctors, along with grant funding from the National Institutes of Health.
Continuous positive airway pressure (CPAP) over several years did not lead to clinically concerning levels of weight gain among patients with obstructive sleep apnea and comorbid cardiovascular disease enrolled in a large international trial, findings from a large, multicenter trial show.
No differences in weight, body mass index (BMI), or other body measurements were found when comparing CPAP and control groups in a post hoc analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) trial, which included 2,483 adults enrolled at 89 centers in seven countries.
In a subanalysis, there was a small but statistically significant weight gain of less than 400 g in men who used CPAP at least 4 hours per night as compared to matched controls. However, there were no differences in BMI or neck and waist circumferences for these men, and no such changes were observed in women, according to the investigators, led by Qiong Ou, MD, of Guangdong (China) General Hospital and R. Doug McEvoy, MD, of the Adelaide Institute for Sleep Health at Flinders University, Adelaide, Australia.
“Such a small change in weight, even with good adherence over several years, is highly unlikely to have any serious clinical ramifications,” wrote the investigators of the study published in Chest.
“Taken together, these results indicate that long-term CPAP treatment is unlikely to exacerbate the problems of overweight and obesity that are common among patients with OSA,” they added.
In a previous meta-analysis of randomized trials, investigators concluded that CPAP promoted significant increases in BMI and weight. However, the median study duration was only 3 months.
In contrast, the analysis of the SAVE trial included adults who had regular body measurements over a mean follow-up of nearly 4 years.
That long-term follow-up provided an “ideal opportunity” to assess whether CPAP treatment promotes weight gain in OSA patients over the course of several years, the authors of the SAVE trial analysis wrote.
For men in the SAVE trial, the difference in weight change for the CPAP group vs. the control group was just 0.07 kg (95% confidence interval, –0.40 to 0.54; P = .773) while in women, the difference for CPAP vs. controls was –0.14 kg (95% CI, –0.37 to 0.09; P = .233), the investigators reported.
Weight gain was significantly higher among men with good CPAP adherence, defined as use for at least 4 hours per night, investigators said, noting a mean difference of 0.38 kg (95% CI, 0.04-0.73; P = .031), though no other differences were found in body measurements for men, and no such associations were found in women with good CPAP adherence.
It’s not exactly clear why this SAVE analysis would find no evidence of CPAP promoting weight gain over the long term, in contrast to the earlier meta-analysis of short-term studies finding a significant risk of weight gain.
However, it is possible that differences in study populations such as ethnicity, age, or comorbidities contributed to the differences, said investigators.
For example, results of regression analysis in the present study showed that, compared with recruitment in Australia, recruitment in China and India was significantly linked to weight loss, while recruitment in New Zealand was linked to weight gain.
Dr. Ou had no disclosures related to the study, while Dr. McEvoy reported disclosures related to Philips Respironics, ResMed, Fisher & Paykel, Air Liquide, and the National Health and Medical Research Council of Australia.
SOURCE: Ou Q et al. Chest. 2019 Apr;155(4):720-9.
Continuous positive airway pressure (CPAP) over several years did not lead to clinically concerning levels of weight gain among patients with obstructive sleep apnea and comorbid cardiovascular disease enrolled in a large international trial, findings from a large, multicenter trial show.
No differences in weight, body mass index (BMI), or other body measurements were found when comparing CPAP and control groups in a post hoc analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) trial, which included 2,483 adults enrolled at 89 centers in seven countries.
In a subanalysis, there was a small but statistically significant weight gain of less than 400 g in men who used CPAP at least 4 hours per night as compared to matched controls. However, there were no differences in BMI or neck and waist circumferences for these men, and no such changes were observed in women, according to the investigators, led by Qiong Ou, MD, of Guangdong (China) General Hospital and R. Doug McEvoy, MD, of the Adelaide Institute for Sleep Health at Flinders University, Adelaide, Australia.
“Such a small change in weight, even with good adherence over several years, is highly unlikely to have any serious clinical ramifications,” wrote the investigators of the study published in Chest.
“Taken together, these results indicate that long-term CPAP treatment is unlikely to exacerbate the problems of overweight and obesity that are common among patients with OSA,” they added.
In a previous meta-analysis of randomized trials, investigators concluded that CPAP promoted significant increases in BMI and weight. However, the median study duration was only 3 months.
In contrast, the analysis of the SAVE trial included adults who had regular body measurements over a mean follow-up of nearly 4 years.
That long-term follow-up provided an “ideal opportunity” to assess whether CPAP treatment promotes weight gain in OSA patients over the course of several years, the authors of the SAVE trial analysis wrote.
For men in the SAVE trial, the difference in weight change for the CPAP group vs. the control group was just 0.07 kg (95% confidence interval, –0.40 to 0.54; P = .773) while in women, the difference for CPAP vs. controls was –0.14 kg (95% CI, –0.37 to 0.09; P = .233), the investigators reported.
Weight gain was significantly higher among men with good CPAP adherence, defined as use for at least 4 hours per night, investigators said, noting a mean difference of 0.38 kg (95% CI, 0.04-0.73; P = .031), though no other differences were found in body measurements for men, and no such associations were found in women with good CPAP adherence.
It’s not exactly clear why this SAVE analysis would find no evidence of CPAP promoting weight gain over the long term, in contrast to the earlier meta-analysis of short-term studies finding a significant risk of weight gain.
However, it is possible that differences in study populations such as ethnicity, age, or comorbidities contributed to the differences, said investigators.
For example, results of regression analysis in the present study showed that, compared with recruitment in Australia, recruitment in China and India was significantly linked to weight loss, while recruitment in New Zealand was linked to weight gain.
Dr. Ou had no disclosures related to the study, while Dr. McEvoy reported disclosures related to Philips Respironics, ResMed, Fisher & Paykel, Air Liquide, and the National Health and Medical Research Council of Australia.
SOURCE: Ou Q et al. Chest. 2019 Apr;155(4):720-9.
FROM CHEST
CPAP use associated with greater weight loss in obese patients with sleep apnea
NEW ORLEANS – Contrary to previously published data suggesting continuous positive airway pressure (CPAP) produces weight gain in patients with obstructive sleep apnea (OSA), new study findings presented at the annual meeting of the Endocrine Society provided data supporting the exact opposite conclusion.
“We think the data are strong enough to conclude that combining CPAP with a weight-loss program should be considered for all OSA patients. The weight-loss advantage is substantial,” reported Yuanjie Mao, MD, PhD, of the University of Arkansas for Medical Sciences, Little Rock.
Both weight loss and CPAP have been shown to be effective for the treatment of OSA, but concern that CPAP produces a counterproductive gain in weight was raised by findings in a meta-analysis in which CPAP was associated with increased body mass index (Thorax. 2015 Mar;70:258-64). As a result of that finding, some guidelines subsequently advised intensifying a weight-loss program at the time that CPAP is initiated to mitigate the weight gain effect, according to Dr. Mao. However, he noted that prospective data were never collected, so a causal relationship was never proven. Now, his data support the opposite conclusion.
In the more recent study, 300 patients who had participated in an intensive weight-loss program at his institution were divided into three groups: OSA patients who had been treated with CPAP, symptomatic OSA patients who had not been treated with CPAP, and asymptomatic OSA patients not treated with CPAP. They were compared retrospectively for weight change over a 16-week period.
“This was a very simple study,” said Dr. Mao, who explained that several exclusions, such as thyroid dysfunction, active infection, and uncontrolled diabetes, were used to reduce variables that might also affect weight change. At the end of 16 weeks, the median absolute weight loss in the CPAP group was 26.7 lb (12.1 kg), compared with 21 lb (9.5 kg) for the symptomatic OSA group and 19.2 lb (8.7 kg) for the asymptomatic OSA group. The weight loss was significantly greater for the CPAP group (P less than .01), compared with either of the other two groups, but not significantly different between the groups that were not treated with CPAP.
“The differences remained significant after adjusting for baseline BMI [body mass index], age, and gender,” Dr. Mao reported.
Asked why his data contradicted the previously reported data, Dr. Mao said that the previous studies were not evaluating CPAP in the context of a weight-loss program. He contends that when CPAP is combined with a rigorous weight-reduction regimen, there is an additive benefit from CPAP.
According to Dr. Mao, these data bring the value of CPAP for weight loss full circle. Before publication of the 2015 meta-analysis, it was widely assumed that CPAP helped with weight loss based on the expectation that better sleep quality would increase daytime activity. However, in the absence of strong data confirming that effect, Dr. Mao believes the unexpected results of the 2015 study easily pushed the pendulum in the opposite direction.
“The conclusion that CPAP increases weight was drawn from studies not designed to evaluate a weight-loss effect in those participating in a weight-loss program,” Dr. Mao explained. His study suggests that it is this combination that is important. He believes the observed effect from better sleep quality associated with CPAP is not necessarily related to better daytime function alone.
“Patients who sleep well also have more favorable diurnal changes in factors that might be important to weight change, such as leptin resistance and hormonal secretion,” he said. Although more work is needed to determine whether these purported mechanisms are important, he thinks his study has an immediate clinical message.
“Patients with OSA who are prescribed weight loss should also be considered for CPAP for the goal of weight loss,” Dr. Mao said. “We think this therapy should be started right away.”
SOURCE: Mao Y et al. ENDO 2019, Session SAT-095.
NEW ORLEANS – Contrary to previously published data suggesting continuous positive airway pressure (CPAP) produces weight gain in patients with obstructive sleep apnea (OSA), new study findings presented at the annual meeting of the Endocrine Society provided data supporting the exact opposite conclusion.
“We think the data are strong enough to conclude that combining CPAP with a weight-loss program should be considered for all OSA patients. The weight-loss advantage is substantial,” reported Yuanjie Mao, MD, PhD, of the University of Arkansas for Medical Sciences, Little Rock.
Both weight loss and CPAP have been shown to be effective for the treatment of OSA, but concern that CPAP produces a counterproductive gain in weight was raised by findings in a meta-analysis in which CPAP was associated with increased body mass index (Thorax. 2015 Mar;70:258-64). As a result of that finding, some guidelines subsequently advised intensifying a weight-loss program at the time that CPAP is initiated to mitigate the weight gain effect, according to Dr. Mao. However, he noted that prospective data were never collected, so a causal relationship was never proven. Now, his data support the opposite conclusion.
In the more recent study, 300 patients who had participated in an intensive weight-loss program at his institution were divided into three groups: OSA patients who had been treated with CPAP, symptomatic OSA patients who had not been treated with CPAP, and asymptomatic OSA patients not treated with CPAP. They were compared retrospectively for weight change over a 16-week period.
“This was a very simple study,” said Dr. Mao, who explained that several exclusions, such as thyroid dysfunction, active infection, and uncontrolled diabetes, were used to reduce variables that might also affect weight change. At the end of 16 weeks, the median absolute weight loss in the CPAP group was 26.7 lb (12.1 kg), compared with 21 lb (9.5 kg) for the symptomatic OSA group and 19.2 lb (8.7 kg) for the asymptomatic OSA group. The weight loss was significantly greater for the CPAP group (P less than .01), compared with either of the other two groups, but not significantly different between the groups that were not treated with CPAP.
“The differences remained significant after adjusting for baseline BMI [body mass index], age, and gender,” Dr. Mao reported.
Asked why his data contradicted the previously reported data, Dr. Mao said that the previous studies were not evaluating CPAP in the context of a weight-loss program. He contends that when CPAP is combined with a rigorous weight-reduction regimen, there is an additive benefit from CPAP.
According to Dr. Mao, these data bring the value of CPAP for weight loss full circle. Before publication of the 2015 meta-analysis, it was widely assumed that CPAP helped with weight loss based on the expectation that better sleep quality would increase daytime activity. However, in the absence of strong data confirming that effect, Dr. Mao believes the unexpected results of the 2015 study easily pushed the pendulum in the opposite direction.
“The conclusion that CPAP increases weight was drawn from studies not designed to evaluate a weight-loss effect in those participating in a weight-loss program,” Dr. Mao explained. His study suggests that it is this combination that is important. He believes the observed effect from better sleep quality associated with CPAP is not necessarily related to better daytime function alone.
“Patients who sleep well also have more favorable diurnal changes in factors that might be important to weight change, such as leptin resistance and hormonal secretion,” he said. Although more work is needed to determine whether these purported mechanisms are important, he thinks his study has an immediate clinical message.
“Patients with OSA who are prescribed weight loss should also be considered for CPAP for the goal of weight loss,” Dr. Mao said. “We think this therapy should be started right away.”
SOURCE: Mao Y et al. ENDO 2019, Session SAT-095.
NEW ORLEANS – Contrary to previously published data suggesting continuous positive airway pressure (CPAP) produces weight gain in patients with obstructive sleep apnea (OSA), new study findings presented at the annual meeting of the Endocrine Society provided data supporting the exact opposite conclusion.
“We think the data are strong enough to conclude that combining CPAP with a weight-loss program should be considered for all OSA patients. The weight-loss advantage is substantial,” reported Yuanjie Mao, MD, PhD, of the University of Arkansas for Medical Sciences, Little Rock.
Both weight loss and CPAP have been shown to be effective for the treatment of OSA, but concern that CPAP produces a counterproductive gain in weight was raised by findings in a meta-analysis in which CPAP was associated with increased body mass index (Thorax. 2015 Mar;70:258-64). As a result of that finding, some guidelines subsequently advised intensifying a weight-loss program at the time that CPAP is initiated to mitigate the weight gain effect, according to Dr. Mao. However, he noted that prospective data were never collected, so a causal relationship was never proven. Now, his data support the opposite conclusion.
In the more recent study, 300 patients who had participated in an intensive weight-loss program at his institution were divided into three groups: OSA patients who had been treated with CPAP, symptomatic OSA patients who had not been treated with CPAP, and asymptomatic OSA patients not treated with CPAP. They were compared retrospectively for weight change over a 16-week period.
“This was a very simple study,” said Dr. Mao, who explained that several exclusions, such as thyroid dysfunction, active infection, and uncontrolled diabetes, were used to reduce variables that might also affect weight change. At the end of 16 weeks, the median absolute weight loss in the CPAP group was 26.7 lb (12.1 kg), compared with 21 lb (9.5 kg) for the symptomatic OSA group and 19.2 lb (8.7 kg) for the asymptomatic OSA group. The weight loss was significantly greater for the CPAP group (P less than .01), compared with either of the other two groups, but not significantly different between the groups that were not treated with CPAP.
“The differences remained significant after adjusting for baseline BMI [body mass index], age, and gender,” Dr. Mao reported.
Asked why his data contradicted the previously reported data, Dr. Mao said that the previous studies were not evaluating CPAP in the context of a weight-loss program. He contends that when CPAP is combined with a rigorous weight-reduction regimen, there is an additive benefit from CPAP.
According to Dr. Mao, these data bring the value of CPAP for weight loss full circle. Before publication of the 2015 meta-analysis, it was widely assumed that CPAP helped with weight loss based on the expectation that better sleep quality would increase daytime activity. However, in the absence of strong data confirming that effect, Dr. Mao believes the unexpected results of the 2015 study easily pushed the pendulum in the opposite direction.
“The conclusion that CPAP increases weight was drawn from studies not designed to evaluate a weight-loss effect in those participating in a weight-loss program,” Dr. Mao explained. His study suggests that it is this combination that is important. He believes the observed effect from better sleep quality associated with CPAP is not necessarily related to better daytime function alone.
“Patients who sleep well also have more favorable diurnal changes in factors that might be important to weight change, such as leptin resistance and hormonal secretion,” he said. Although more work is needed to determine whether these purported mechanisms are important, he thinks his study has an immediate clinical message.
“Patients with OSA who are prescribed weight loss should also be considered for CPAP for the goal of weight loss,” Dr. Mao said. “We think this therapy should be started right away.”
SOURCE: Mao Y et al. ENDO 2019, Session SAT-095.
REPORTING FROM ENDO 2019
FDA approves solriamfetol for daytime sleepiness treatment
The. It is the first dopamine and norepinephrine reuptake inhibitor approved to treat those conditions.
Approval was based on results from TONES (Treatment of Obstructive Sleep Apnea and Narcolepsy Excessive Sleepiness), a phase 3 study that combined four randomized, placebo-controlled trials assessing solriamfetol at various doses, compared with a placebo. After 12 weeks, 68%-74% of patients taking solriamfetol at 75 mg and 78%-90% of those taking solriamfetol at 150 mg reported improvement as assessed by the Patient Global Impression of Change scale.
Solriamfetol is approved at 75 mg and 150 mg for patients with narcolepsy and at 37.5 mg, 75 mg, and 150 mg for patients with obstructive sleep apnea. The most common adverse events associated with solriamfetol are headache, nausea, decreased appetite, and anxiety.
“Excessive daytime sleepiness can negatively impact the daily lives of people living with narcolepsy or obstructive sleep apnea at work, at home, or in daily activities. With this approval, a new, daytime medicine that can provide sustained wakefulness throughout the day will be available for patients,” Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals, said in the press release.
Find the full press release on the Jazz Pharmaceuticals website.
The. It is the first dopamine and norepinephrine reuptake inhibitor approved to treat those conditions.
Approval was based on results from TONES (Treatment of Obstructive Sleep Apnea and Narcolepsy Excessive Sleepiness), a phase 3 study that combined four randomized, placebo-controlled trials assessing solriamfetol at various doses, compared with a placebo. After 12 weeks, 68%-74% of patients taking solriamfetol at 75 mg and 78%-90% of those taking solriamfetol at 150 mg reported improvement as assessed by the Patient Global Impression of Change scale.
Solriamfetol is approved at 75 mg and 150 mg for patients with narcolepsy and at 37.5 mg, 75 mg, and 150 mg for patients with obstructive sleep apnea. The most common adverse events associated with solriamfetol are headache, nausea, decreased appetite, and anxiety.
“Excessive daytime sleepiness can negatively impact the daily lives of people living with narcolepsy or obstructive sleep apnea at work, at home, or in daily activities. With this approval, a new, daytime medicine that can provide sustained wakefulness throughout the day will be available for patients,” Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals, said in the press release.
Find the full press release on the Jazz Pharmaceuticals website.
The. It is the first dopamine and norepinephrine reuptake inhibitor approved to treat those conditions.
Approval was based on results from TONES (Treatment of Obstructive Sleep Apnea and Narcolepsy Excessive Sleepiness), a phase 3 study that combined four randomized, placebo-controlled trials assessing solriamfetol at various doses, compared with a placebo. After 12 weeks, 68%-74% of patients taking solriamfetol at 75 mg and 78%-90% of those taking solriamfetol at 150 mg reported improvement as assessed by the Patient Global Impression of Change scale.
Solriamfetol is approved at 75 mg and 150 mg for patients with narcolepsy and at 37.5 mg, 75 mg, and 150 mg for patients with obstructive sleep apnea. The most common adverse events associated with solriamfetol are headache, nausea, decreased appetite, and anxiety.
“Excessive daytime sleepiness can negatively impact the daily lives of people living with narcolepsy or obstructive sleep apnea at work, at home, or in daily activities. With this approval, a new, daytime medicine that can provide sustained wakefulness throughout the day will be available for patients,” Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals, said in the press release.
Find the full press release on the Jazz Pharmaceuticals website.
Effects of Insomnia and Depression on CPAP Adherence in a Military Population
Continuous positive airway pressure therapy (CPAP) is the first-line treatment for obstructive sleep apnea (OSA) recommended by the American College of Physicians and the American Academy of Sleep Medicine.1,2 CPAP reduces the apnea hypopnea index (AHI), improves oxyhemoglobin desaturation, and reduces cortical arousals associated with apneic/hypopneic events.3 Despite being an effective treatment for OSA, a significant limitation of CPAP is treatment adherence. Factors associated with CPAP adherence include disease and patient characteristics, perceived self-efficacy, treatment titration procedure, device technology factors, adverse effects, and psychosocial factors.4
Recent studies suggest that insomnia and depression may be associated with OSA. According to a review by Luyster and colleagues, insomnia is present in 39% to 58% of patients with OSA.5 Since OSA may disturb sleep by the number of nightly awakenings, OSA may cause or worsen insomnia. Furthermore, insomnia may exacerbate sleep apnea thus impeding the effectiveness of sleep apnea treatment.
In some studies, the presence of insomnia symptoms prior to initiating CPAP treatment has been found to be associated with reduced CPAP adherence. For example, in 2010, Wickwire and colleagues found that there was a negative association with the average nightly minutes of CPAP use for those patients with OSA that reported symptoms of sleep maintenance insomnia.6 This was not found for those patients with OSA who reported symptoms of sleep onset insomnia or reported no insomnia at all. In another study by Pieh and colleagues, self-reported insomnia symptoms were predictive of CPAP adherence (defined as < 4 hours use/night) at a 6-month follow-up.7 However, results from a separate study indicated that insomnia was not associated with 6-month CPAP adherence.8
Depressive symptoms are commonly reported by patients with OSA, and higher rates of depressive symptomatology in patients with OSA have been observed in a number of prevalence studies when compared with the general population.9,10 Between 15% and 56% of patients with OSA are diagnosed with a depressive disorder compared with 6.6% of the general population.11 OSA may be causally related with depression or coexist as a separate disorder. Apnea severity has been shown to exacerbate depressive symptoms, and treatment with CPAP can improve depressive symptoms.12,13 Unfortunately, depression has been found to reduce CPAP adherence. For example, Law and colleagues found that depression was independently associated with poorer adherence during home-based auto-PAP titration.14 Furthermore, in a study by Gurlanick and colleagues, depressive symptoms were independently associated with reduced CPAP adherence in surgical patients with OSA.15
To the best of our knowledge, the combined impact of both insomnia and depression on CPAP adherence has not been investigated. In military populations this may be especially important as CPAP adherence has been reported to be worse in military patients with posttraumatic stress disorder (PTSD) and other psychiatric disorders, and there are increasing rates of insomnia and OSA in the military.16,17 We hypothesize that active-duty and retired military patients with self-reported insomnia and depression will have reduced short and long-term CPAP adherence.
Methods
This is a retrospective cohort study that reviewed charts of active-duty and retired military members diagnosed with OSA by the Sleep Medicine Clinic at Naval Medical Center San Diego in California using a home sleep test (HST). The HSTs were interpreted by board-certified physicians in sleep medicine. Prior to the HST, all patients completed a sleep questionnaire that included self-reports of daytime sleepiness, using the Epworth Sleepiness Scale (ESS), depression using the Center for Epidemiologic Studies Depression Scale (CES-D) and insomnia using the Insomnia Severity Index (ISI).
The study population included active-duty and veteran patients diagnosed with OSA who chose treatment with a CPAP and attended the sleep clinic’s OSA educational class, which discussed the diagnosis and treatment of OSA. Inclusion criteria were patients aged > 18 years and diagnosed with OSA at the Naval Medical Center San Diego sleep lab between June 2014 and June 2015.
The study population was stratified into 4 groups: (1) those with OSA but no self-reported depression or insomnia; (2) those with OSA and self-reported depression but no insomnia; (3) those with OSA and insomnia but no depression; and (4) those with OSA and self-reported depression and insomnia. Charts were excluded from the review if there were incomplete data or if the patient selected an alternative treatment for OSA, such as an oral appliance. A total of 120 charts were included in the final review. This study was approved by the Naval Medical Center San Diego Institutional Review Board.
Data Collection
Data collected included the individual’s age, sex, minimum oxygen saturation during sleep, body mass index (BMI), height, weight, ESS score at time of diagnosis, date of HST, and date of attendance at the clinic’s OSA group treatment class. Diagnosis of OSA was based on the patient’s ≥ 5 AHI. OSA severity was divided into mild (AHI 5-14), moderate (AHI 15-29), or severe (AHI ≥ 30). A patient with a CES-D score > 14 was considered to have clinically significant depression, and a patient with an ISI score of > 14 was considered to have clinically significant insomnia. ISI is a reliable and valid instrument to quantify perceived insomnia severity.18 The CES-D was used only as an indicator of symptoms relating to depression, not to clinically diagnose depression. It also has been used extensively to investigate levels of depression without a psychiatric diagnosis.19
Follow-up CPAP adherence was collected at 3- and 12-month intervals after the date of the patient’s OSA treatment group class and included AHI, median pressure setting, median days used, average time used per night, and percentage of days used for more than 4 hours for the previous 30 days. Data were obtained through Sleep Data and ResMed websites, which receive patient adherence data directly from the patient’s CPAP device. Patients were considered to be adherent with CPAP usage based on the Medicare definition: Use of the CPAP device > 4 hours per night for at least 70% of nights during a 30-day period). The 3-month time frame was used as a short interval because that is when patients are seen in the pulmonary clinic for their initial follow-up appointment. Patients are seen again at 12 months because durable medical equipment supplies must be reordered after 12 months, which requires a patient visit.
Statistical Analysis
Linear regression methods were used to characterize any potential relationships between the predictor variables and the target outcome variables associated with CPAP adherence at 3 and 12 months. Scatterplots were produced to assess whether linear structure was sufficient to characterize any detectable relationships, or whether there existed more complex, nonlinear relationships. The best-fitting linear regression line was examined in relation to the confidence bands of the corresponding LOESS line to determine whether a more complicated model structure was needed to capture the relationship.
Standard tests of assumptions required for these methods were also carried out: QQ plots of residuals to test for normality, the Durbin-Watson test for independence of residuals, and the nonconstant variance score test for heteroskedasticity (ie, Breusch-Pagan test). The results of these assumptions tests are reported only in cases in which the assumptions were revealed to be untenable. In cases in which suspicious outlying observations may have biased analyses, robust versions of the corresponding models were constructed. In no cases did the resulting conclusions change; only the results of the original analysis are reported. All analyses were carried out in R (R Foundation, r-project.org). Statistical significance was defined as P < .05.
Results
Our study population was predominately male (90%) with a median age of 41 years (range 22-65) and BMI of 29.8 (range 7.7-57.2)(Table 1).
Predictors of CPAP Adherence
OSA severity, as measured by the AHI, was the only promising predictor of CPAP use at 3 months (b, 2.128; t80, 2.854; P = .005; adjusted R2, 0.081). The severity of self-reported daytime sleepiness prior to a diagnosis of OSA, as measured by the ESS, did not predict 3-month CPAP adherence (b, 0.688; t77, 0.300; P = .765; adjusted R2, -0.012). Self-reported depression as measured by the CES-D also did not predict CPAP use at 3 months (b, -0.078; t80, -0.014; P = .941; adjusted R2, -0.012). Similarly, self-reported insomnia, as measured by the ISI, did not predict 3-month CPAP adherence (b, 1.765; t80, 0.939; P = .350; adjusted R2, -0.001). Furthermore, a model that incorporated both depression and insomnia proved no better at accounting for variation in 3-month CPAP use (R2, -0.012). Demographic variables, such as age, sex, or BMI did not predict 3-month CPAP adherence (all Ps > .20). Finally, median CPAP pressure approached statistical significance as a predictor of 3-month CPAP adherence (b, 9.493; t66, 1.881; P = .064; adjusted R2, 0.037) (Figure 1).
CPAP Use at 12 months
The results for CPAP use at 12 months mirrored the results for 3 months with one main exception: OSA severity, as measured by the AHI, did not predict CPAP use at 12 months (b, 1.158; t52, 1.245; P = .219; adjusted R2, 0.010). Neither adding a quadratic predictor nor log transforming the AHI values produced a better model (R2, -0.0007 vs R2, 0.0089, respectively). The severity of self-reported daytime sleepiness, as measured by the ESS, did not predict 12-month CPAP adherence (b, -2.201; t50, -0.752; P = .456; adjusted R2 = -0.0086). Self-reported depression as measured by the CES-D also did not predict CPAP use at 12 months (b, 0.034, t52, 0.022; P = .983; adjusted R2, -0.092). Self-reported insomnia, as measured by the ISI, also did not predict 12-month CPAP adherence (b, 1.765; t80, 0.939; P = .350; adjusted R2 = -0.001). Furthermore, a model that incorporated both depression and insomnia proved no better at accounting for variation in 12-month CPAP use, (R2, -0.0298).
Discussion
Our study did not provide evidence that self-reported depressive and insomnia symptoms, as measured by the CES-D and ISI, can serve as useful predictors of short and long-term CPAP adherence in a sample of active-duty and retired military. OSA severity, as measured by the AHI, was the only promising predictor of CPAP adherence at 3 months.
Insomnia has been shown to improve with the use of CPAP. In a pilot study, Krakow and colleagues investigated the use of CPAP, oral appliances, or bilateral turbinectomy on patients with OSA and chronic insomnia.20 Objective measures of insomnia improved with 1 night of CPAP titration. Björnsdóttir and colleagues evaluated the long-term effects of positive airway pressure (PAP) treatment on 705 adults with middle insomnia.21 They found after 2 years of PAP treatment combined with cognitive behavioral therapy for insomnia, patients had reduced symptoms of middle insomnia. It is possible that persistent insomnia is associated with more severe OSA which was not studied in our population.22
As reported in other studies, it is possible that patients with depressive symptoms can improve with CPAP use, suggesting that depression and CPAP use are not totally unrelated. Edwards and colleagues studied the impact of CPAP on depressive symptoms in men and woman. They found that depressive symptoms are common in OSA and markedly improve with CPAP.23 Bopparaju and colleagues found a high prevalence of anxiety and depression in patients with OSA but did not influence CPAP adherence.24
The results of this study differ from some previous findings where depression was found to predict CPAP adherence.10 This may be due in part to differences in the type of instrument used to assess depression. Wells and colleagues found that baseline depressive symptoms did not correlate with CPAP adherence and that patients with greater CPAP adherence had improvement in OSA and depressive symptoms.25 Furthermore, patients with residual OSA symptoms using CPAP had more depressive symptoms, suggesting that it is the improvement in OSA symptoms that may be correlated with the improvement in depressive symptoms. Although soldiers with PTSD may have reduced CPAP adherence, use of CPAP is associated with improvement in PTSD symptoms.11,26
Limitations
This study had several limitations, including a small sample size. Study patients were also from a single institution, and the majority of patients had mild-to-moderate OSA. A multicenter prospective study with a larger sample size that included more severe patients with OSA may have shown different results. The participants in this study were limited to members from the active-duty and retired military population. The findings in this population may not be transferrable to the general public. Another study limitation was that the ISI and the CES-D were only administered prior to the initiation of CPAP. If the CES-D and ISI were administered at the 3- and 12-month follow-up visits, we could determine whether short and long-term CPAP improved these symptoms or whether there was no association between CPAP adherence with insomnia and depressive symptoms. Another limitation is that we did not have access to information about potential PTSD symptomatology, which has been associated with reduced CPAP adherence and is more common in a military and veteran population.11
Conclusion
This study found little evidence that symptoms of depression and insomnia are useful predictors of CPAP adherence, in either short- or long-term use, in an active-duty and retired military sample. Although these were not found to be predictors of CPAP adherence, further research will be necessary to determine whether CPAP adherence improves symptoms of depression and insomnia in military and veteran populations. Apnea severity did predict CPAP adherence in the short term, but not for any length of time beyond 3 months. More research is needed to explore strategies to improve CPAP adherence in military populations.
1. Qaseem A, Holty JE, Owens DK, Dallas P, Starkey M, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Management of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159(7):471-483.
2. Epstein LJ, Kristo D, Strollo PJ, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-276.
3. Gay P, Weaver T, Loube D, Iber C; Positive Airway Pressure Task Force; Standards of Practice Committee; American Academy of Sleep Medicine. Evaluation of positive airway pressure treatment for sleep-related breathing disorders in adults. Sleep. 2006;29(3):381-401.
4. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver T. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343-356.
5. Luyster FS; Buysse DJ; Strollo PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196-204.
6. Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772-776
7. Pieh C, Bach M, Popp R, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99-104.
8. Nguyên XL, Chaskalovic J, Rakotonanahary D, Fleury B. Insomnia symptoms and CPAP compliance in OSAS patients: a descriptive study using data mining methods. Sleep Med. 2010;11(8):777-784.
9. Yilmaz E, Sedky K, Bennett DS. The relationship between depressive symptoms and obstructive sleep apnea in pediatric populations: a meta-analysis. J Clin Sleep Med. 2013;9(11):1213-1220.
10. Chen YH, Keller JK, Kang JH, Hsieh HJ, Lin HC. Obstructive sleep apnea and the subsequent risk of depressive disorder: a population-based follow-up study. J Clin Sleep Med. 2013;9(5):417-423.
11. Kessler RC, Berglund P, Demler O, et al; National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003:289(23):3095-3105
12. Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13(6):437-444.
13. Schwartz D, Kohler W, Karatinos G. Symptoms of depression in individuals with obstructive sleep apnea may be amendable to treatment with continuous positive airway pressure. Chest. 2005;128(3):1304-1309
14. Law M, Naughton M, Ho S, Roebuck T, Dabscheck E. Depression may reduce adherence during CPAP titration trial. J Clin Sleep Med. 2014;10(2):163-169.
15. Guralnick AS, Pant M, Minhaj M, Sweitzer BJ, Mokhlesi B. CPAP adherence in patients with newly diagnosed obstructive sleep apnea prior to elective surgery. J Clin Sleep Med. 2012;8(5):501-506
16. Collen JF, Lettieri CJ, Hoffman M. The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med. 2012;8(6):667-672.
17. Caldwell A, Knapik JJ, Lieberman HR. Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. J Sleep Res. 2017;26(5):665-670.
18. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307.
19. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychological Measurement. 1977;1(3):385-401.
20. Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath. 2004;8(1):15-29.
21. Björnsdóttir E, Janson C, Sigurdsson JF, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901-1909.
22. Glidewell RN, Renn BN, Roby E, Orr WC. Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med. 2014;15(8):899-905.
23. Edwards C, Mukherjee S, Simpson L, Palmer LJ, Almeida OP, Hillman DR. Depressive symptoms before and after treatment of obstructive sleep apnea in men and women. J Clin Sleep Med. 2015;11(9):1029-1038.
24. Bopparaju S, Casturi L, Guntupalli B, Surani S, Subramanian S. Anxiety and depression in obstructive sleep apnea: Effect of CPAP therapy and influence on CPAP compliance. Presented at: American College of Chest Physicians Annual Meeting, October 31-November 05, 2009; San Diego, CA. Chest. 2009;136(4, meeting abstracts):71S.
25. Wells RD, Freedland KE, Carney RM, Duntley SP, Stepanski EJ. Adherence, reports of benefits, and depression among patients treated with continuous positive airway pressure. Psychosom Med. 2007;69(5):449-454.
26. Orr JE, Smales C, Alexander TH, et al. Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med. 2017;13(1):57-63.
Continuous positive airway pressure therapy (CPAP) is the first-line treatment for obstructive sleep apnea (OSA) recommended by the American College of Physicians and the American Academy of Sleep Medicine.1,2 CPAP reduces the apnea hypopnea index (AHI), improves oxyhemoglobin desaturation, and reduces cortical arousals associated with apneic/hypopneic events.3 Despite being an effective treatment for OSA, a significant limitation of CPAP is treatment adherence. Factors associated with CPAP adherence include disease and patient characteristics, perceived self-efficacy, treatment titration procedure, device technology factors, adverse effects, and psychosocial factors.4
Recent studies suggest that insomnia and depression may be associated with OSA. According to a review by Luyster and colleagues, insomnia is present in 39% to 58% of patients with OSA.5 Since OSA may disturb sleep by the number of nightly awakenings, OSA may cause or worsen insomnia. Furthermore, insomnia may exacerbate sleep apnea thus impeding the effectiveness of sleep apnea treatment.
In some studies, the presence of insomnia symptoms prior to initiating CPAP treatment has been found to be associated with reduced CPAP adherence. For example, in 2010, Wickwire and colleagues found that there was a negative association with the average nightly minutes of CPAP use for those patients with OSA that reported symptoms of sleep maintenance insomnia.6 This was not found for those patients with OSA who reported symptoms of sleep onset insomnia or reported no insomnia at all. In another study by Pieh and colleagues, self-reported insomnia symptoms were predictive of CPAP adherence (defined as < 4 hours use/night) at a 6-month follow-up.7 However, results from a separate study indicated that insomnia was not associated with 6-month CPAP adherence.8
Depressive symptoms are commonly reported by patients with OSA, and higher rates of depressive symptomatology in patients with OSA have been observed in a number of prevalence studies when compared with the general population.9,10 Between 15% and 56% of patients with OSA are diagnosed with a depressive disorder compared with 6.6% of the general population.11 OSA may be causally related with depression or coexist as a separate disorder. Apnea severity has been shown to exacerbate depressive symptoms, and treatment with CPAP can improve depressive symptoms.12,13 Unfortunately, depression has been found to reduce CPAP adherence. For example, Law and colleagues found that depression was independently associated with poorer adherence during home-based auto-PAP titration.14 Furthermore, in a study by Gurlanick and colleagues, depressive symptoms were independently associated with reduced CPAP adherence in surgical patients with OSA.15
To the best of our knowledge, the combined impact of both insomnia and depression on CPAP adherence has not been investigated. In military populations this may be especially important as CPAP adherence has been reported to be worse in military patients with posttraumatic stress disorder (PTSD) and other psychiatric disorders, and there are increasing rates of insomnia and OSA in the military.16,17 We hypothesize that active-duty and retired military patients with self-reported insomnia and depression will have reduced short and long-term CPAP adherence.
Methods
This is a retrospective cohort study that reviewed charts of active-duty and retired military members diagnosed with OSA by the Sleep Medicine Clinic at Naval Medical Center San Diego in California using a home sleep test (HST). The HSTs were interpreted by board-certified physicians in sleep medicine. Prior to the HST, all patients completed a sleep questionnaire that included self-reports of daytime sleepiness, using the Epworth Sleepiness Scale (ESS), depression using the Center for Epidemiologic Studies Depression Scale (CES-D) and insomnia using the Insomnia Severity Index (ISI).
The study population included active-duty and veteran patients diagnosed with OSA who chose treatment with a CPAP and attended the sleep clinic’s OSA educational class, which discussed the diagnosis and treatment of OSA. Inclusion criteria were patients aged > 18 years and diagnosed with OSA at the Naval Medical Center San Diego sleep lab between June 2014 and June 2015.
The study population was stratified into 4 groups: (1) those with OSA but no self-reported depression or insomnia; (2) those with OSA and self-reported depression but no insomnia; (3) those with OSA and insomnia but no depression; and (4) those with OSA and self-reported depression and insomnia. Charts were excluded from the review if there were incomplete data or if the patient selected an alternative treatment for OSA, such as an oral appliance. A total of 120 charts were included in the final review. This study was approved by the Naval Medical Center San Diego Institutional Review Board.
Data Collection
Data collected included the individual’s age, sex, minimum oxygen saturation during sleep, body mass index (BMI), height, weight, ESS score at time of diagnosis, date of HST, and date of attendance at the clinic’s OSA group treatment class. Diagnosis of OSA was based on the patient’s ≥ 5 AHI. OSA severity was divided into mild (AHI 5-14), moderate (AHI 15-29), or severe (AHI ≥ 30). A patient with a CES-D score > 14 was considered to have clinically significant depression, and a patient with an ISI score of > 14 was considered to have clinically significant insomnia. ISI is a reliable and valid instrument to quantify perceived insomnia severity.18 The CES-D was used only as an indicator of symptoms relating to depression, not to clinically diagnose depression. It also has been used extensively to investigate levels of depression without a psychiatric diagnosis.19
Follow-up CPAP adherence was collected at 3- and 12-month intervals after the date of the patient’s OSA treatment group class and included AHI, median pressure setting, median days used, average time used per night, and percentage of days used for more than 4 hours for the previous 30 days. Data were obtained through Sleep Data and ResMed websites, which receive patient adherence data directly from the patient’s CPAP device. Patients were considered to be adherent with CPAP usage based on the Medicare definition: Use of the CPAP device > 4 hours per night for at least 70% of nights during a 30-day period). The 3-month time frame was used as a short interval because that is when patients are seen in the pulmonary clinic for their initial follow-up appointment. Patients are seen again at 12 months because durable medical equipment supplies must be reordered after 12 months, which requires a patient visit.
Statistical Analysis
Linear regression methods were used to characterize any potential relationships between the predictor variables and the target outcome variables associated with CPAP adherence at 3 and 12 months. Scatterplots were produced to assess whether linear structure was sufficient to characterize any detectable relationships, or whether there existed more complex, nonlinear relationships. The best-fitting linear regression line was examined in relation to the confidence bands of the corresponding LOESS line to determine whether a more complicated model structure was needed to capture the relationship.
Standard tests of assumptions required for these methods were also carried out: QQ plots of residuals to test for normality, the Durbin-Watson test for independence of residuals, and the nonconstant variance score test for heteroskedasticity (ie, Breusch-Pagan test). The results of these assumptions tests are reported only in cases in which the assumptions were revealed to be untenable. In cases in which suspicious outlying observations may have biased analyses, robust versions of the corresponding models were constructed. In no cases did the resulting conclusions change; only the results of the original analysis are reported. All analyses were carried out in R (R Foundation, r-project.org). Statistical significance was defined as P < .05.
Results
Our study population was predominately male (90%) with a median age of 41 years (range 22-65) and BMI of 29.8 (range 7.7-57.2)(Table 1).
Predictors of CPAP Adherence
OSA severity, as measured by the AHI, was the only promising predictor of CPAP use at 3 months (b, 2.128; t80, 2.854; P = .005; adjusted R2, 0.081). The severity of self-reported daytime sleepiness prior to a diagnosis of OSA, as measured by the ESS, did not predict 3-month CPAP adherence (b, 0.688; t77, 0.300; P = .765; adjusted R2, -0.012). Self-reported depression as measured by the CES-D also did not predict CPAP use at 3 months (b, -0.078; t80, -0.014; P = .941; adjusted R2, -0.012). Similarly, self-reported insomnia, as measured by the ISI, did not predict 3-month CPAP adherence (b, 1.765; t80, 0.939; P = .350; adjusted R2, -0.001). Furthermore, a model that incorporated both depression and insomnia proved no better at accounting for variation in 3-month CPAP use (R2, -0.012). Demographic variables, such as age, sex, or BMI did not predict 3-month CPAP adherence (all Ps > .20). Finally, median CPAP pressure approached statistical significance as a predictor of 3-month CPAP adherence (b, 9.493; t66, 1.881; P = .064; adjusted R2, 0.037) (Figure 1).
CPAP Use at 12 months
The results for CPAP use at 12 months mirrored the results for 3 months with one main exception: OSA severity, as measured by the AHI, did not predict CPAP use at 12 months (b, 1.158; t52, 1.245; P = .219; adjusted R2, 0.010). Neither adding a quadratic predictor nor log transforming the AHI values produced a better model (R2, -0.0007 vs R2, 0.0089, respectively). The severity of self-reported daytime sleepiness, as measured by the ESS, did not predict 12-month CPAP adherence (b, -2.201; t50, -0.752; P = .456; adjusted R2 = -0.0086). Self-reported depression as measured by the CES-D also did not predict CPAP use at 12 months (b, 0.034, t52, 0.022; P = .983; adjusted R2, -0.092). Self-reported insomnia, as measured by the ISI, also did not predict 12-month CPAP adherence (b, 1.765; t80, 0.939; P = .350; adjusted R2 = -0.001). Furthermore, a model that incorporated both depression and insomnia proved no better at accounting for variation in 12-month CPAP use, (R2, -0.0298).
Discussion
Our study did not provide evidence that self-reported depressive and insomnia symptoms, as measured by the CES-D and ISI, can serve as useful predictors of short and long-term CPAP adherence in a sample of active-duty and retired military. OSA severity, as measured by the AHI, was the only promising predictor of CPAP adherence at 3 months.
Insomnia has been shown to improve with the use of CPAP. In a pilot study, Krakow and colleagues investigated the use of CPAP, oral appliances, or bilateral turbinectomy on patients with OSA and chronic insomnia.20 Objective measures of insomnia improved with 1 night of CPAP titration. Björnsdóttir and colleagues evaluated the long-term effects of positive airway pressure (PAP) treatment on 705 adults with middle insomnia.21 They found after 2 years of PAP treatment combined with cognitive behavioral therapy for insomnia, patients had reduced symptoms of middle insomnia. It is possible that persistent insomnia is associated with more severe OSA which was not studied in our population.22
As reported in other studies, it is possible that patients with depressive symptoms can improve with CPAP use, suggesting that depression and CPAP use are not totally unrelated. Edwards and colleagues studied the impact of CPAP on depressive symptoms in men and woman. They found that depressive symptoms are common in OSA and markedly improve with CPAP.23 Bopparaju and colleagues found a high prevalence of anxiety and depression in patients with OSA but did not influence CPAP adherence.24
The results of this study differ from some previous findings where depression was found to predict CPAP adherence.10 This may be due in part to differences in the type of instrument used to assess depression. Wells and colleagues found that baseline depressive symptoms did not correlate with CPAP adherence and that patients with greater CPAP adherence had improvement in OSA and depressive symptoms.25 Furthermore, patients with residual OSA symptoms using CPAP had more depressive symptoms, suggesting that it is the improvement in OSA symptoms that may be correlated with the improvement in depressive symptoms. Although soldiers with PTSD may have reduced CPAP adherence, use of CPAP is associated with improvement in PTSD symptoms.11,26
Limitations
This study had several limitations, including a small sample size. Study patients were also from a single institution, and the majority of patients had mild-to-moderate OSA. A multicenter prospective study with a larger sample size that included more severe patients with OSA may have shown different results. The participants in this study were limited to members from the active-duty and retired military population. The findings in this population may not be transferrable to the general public. Another study limitation was that the ISI and the CES-D were only administered prior to the initiation of CPAP. If the CES-D and ISI were administered at the 3- and 12-month follow-up visits, we could determine whether short and long-term CPAP improved these symptoms or whether there was no association between CPAP adherence with insomnia and depressive symptoms. Another limitation is that we did not have access to information about potential PTSD symptomatology, which has been associated with reduced CPAP adherence and is more common in a military and veteran population.11
Conclusion
This study found little evidence that symptoms of depression and insomnia are useful predictors of CPAP adherence, in either short- or long-term use, in an active-duty and retired military sample. Although these were not found to be predictors of CPAP adherence, further research will be necessary to determine whether CPAP adherence improves symptoms of depression and insomnia in military and veteran populations. Apnea severity did predict CPAP adherence in the short term, but not for any length of time beyond 3 months. More research is needed to explore strategies to improve CPAP adherence in military populations.
Continuous positive airway pressure therapy (CPAP) is the first-line treatment for obstructive sleep apnea (OSA) recommended by the American College of Physicians and the American Academy of Sleep Medicine.1,2 CPAP reduces the apnea hypopnea index (AHI), improves oxyhemoglobin desaturation, and reduces cortical arousals associated with apneic/hypopneic events.3 Despite being an effective treatment for OSA, a significant limitation of CPAP is treatment adherence. Factors associated with CPAP adherence include disease and patient characteristics, perceived self-efficacy, treatment titration procedure, device technology factors, adverse effects, and psychosocial factors.4
Recent studies suggest that insomnia and depression may be associated with OSA. According to a review by Luyster and colleagues, insomnia is present in 39% to 58% of patients with OSA.5 Since OSA may disturb sleep by the number of nightly awakenings, OSA may cause or worsen insomnia. Furthermore, insomnia may exacerbate sleep apnea thus impeding the effectiveness of sleep apnea treatment.
In some studies, the presence of insomnia symptoms prior to initiating CPAP treatment has been found to be associated with reduced CPAP adherence. For example, in 2010, Wickwire and colleagues found that there was a negative association with the average nightly minutes of CPAP use for those patients with OSA that reported symptoms of sleep maintenance insomnia.6 This was not found for those patients with OSA who reported symptoms of sleep onset insomnia or reported no insomnia at all. In another study by Pieh and colleagues, self-reported insomnia symptoms were predictive of CPAP adherence (defined as < 4 hours use/night) at a 6-month follow-up.7 However, results from a separate study indicated that insomnia was not associated with 6-month CPAP adherence.8
Depressive symptoms are commonly reported by patients with OSA, and higher rates of depressive symptomatology in patients with OSA have been observed in a number of prevalence studies when compared with the general population.9,10 Between 15% and 56% of patients with OSA are diagnosed with a depressive disorder compared with 6.6% of the general population.11 OSA may be causally related with depression or coexist as a separate disorder. Apnea severity has been shown to exacerbate depressive symptoms, and treatment with CPAP can improve depressive symptoms.12,13 Unfortunately, depression has been found to reduce CPAP adherence. For example, Law and colleagues found that depression was independently associated with poorer adherence during home-based auto-PAP titration.14 Furthermore, in a study by Gurlanick and colleagues, depressive symptoms were independently associated with reduced CPAP adherence in surgical patients with OSA.15
To the best of our knowledge, the combined impact of both insomnia and depression on CPAP adherence has not been investigated. In military populations this may be especially important as CPAP adherence has been reported to be worse in military patients with posttraumatic stress disorder (PTSD) and other psychiatric disorders, and there are increasing rates of insomnia and OSA in the military.16,17 We hypothesize that active-duty and retired military patients with self-reported insomnia and depression will have reduced short and long-term CPAP adherence.
Methods
This is a retrospective cohort study that reviewed charts of active-duty and retired military members diagnosed with OSA by the Sleep Medicine Clinic at Naval Medical Center San Diego in California using a home sleep test (HST). The HSTs were interpreted by board-certified physicians in sleep medicine. Prior to the HST, all patients completed a sleep questionnaire that included self-reports of daytime sleepiness, using the Epworth Sleepiness Scale (ESS), depression using the Center for Epidemiologic Studies Depression Scale (CES-D) and insomnia using the Insomnia Severity Index (ISI).
The study population included active-duty and veteran patients diagnosed with OSA who chose treatment with a CPAP and attended the sleep clinic’s OSA educational class, which discussed the diagnosis and treatment of OSA. Inclusion criteria were patients aged > 18 years and diagnosed with OSA at the Naval Medical Center San Diego sleep lab between June 2014 and June 2015.
The study population was stratified into 4 groups: (1) those with OSA but no self-reported depression or insomnia; (2) those with OSA and self-reported depression but no insomnia; (3) those with OSA and insomnia but no depression; and (4) those with OSA and self-reported depression and insomnia. Charts were excluded from the review if there were incomplete data or if the patient selected an alternative treatment for OSA, such as an oral appliance. A total of 120 charts were included in the final review. This study was approved by the Naval Medical Center San Diego Institutional Review Board.
Data Collection
Data collected included the individual’s age, sex, minimum oxygen saturation during sleep, body mass index (BMI), height, weight, ESS score at time of diagnosis, date of HST, and date of attendance at the clinic’s OSA group treatment class. Diagnosis of OSA was based on the patient’s ≥ 5 AHI. OSA severity was divided into mild (AHI 5-14), moderate (AHI 15-29), or severe (AHI ≥ 30). A patient with a CES-D score > 14 was considered to have clinically significant depression, and a patient with an ISI score of > 14 was considered to have clinically significant insomnia. ISI is a reliable and valid instrument to quantify perceived insomnia severity.18 The CES-D was used only as an indicator of symptoms relating to depression, not to clinically diagnose depression. It also has been used extensively to investigate levels of depression without a psychiatric diagnosis.19
Follow-up CPAP adherence was collected at 3- and 12-month intervals after the date of the patient’s OSA treatment group class and included AHI, median pressure setting, median days used, average time used per night, and percentage of days used for more than 4 hours for the previous 30 days. Data were obtained through Sleep Data and ResMed websites, which receive patient adherence data directly from the patient’s CPAP device. Patients were considered to be adherent with CPAP usage based on the Medicare definition: Use of the CPAP device > 4 hours per night for at least 70% of nights during a 30-day period). The 3-month time frame was used as a short interval because that is when patients are seen in the pulmonary clinic for their initial follow-up appointment. Patients are seen again at 12 months because durable medical equipment supplies must be reordered after 12 months, which requires a patient visit.
Statistical Analysis
Linear regression methods were used to characterize any potential relationships between the predictor variables and the target outcome variables associated with CPAP adherence at 3 and 12 months. Scatterplots were produced to assess whether linear structure was sufficient to characterize any detectable relationships, or whether there existed more complex, nonlinear relationships. The best-fitting linear regression line was examined in relation to the confidence bands of the corresponding LOESS line to determine whether a more complicated model structure was needed to capture the relationship.
Standard tests of assumptions required for these methods were also carried out: QQ plots of residuals to test for normality, the Durbin-Watson test for independence of residuals, and the nonconstant variance score test for heteroskedasticity (ie, Breusch-Pagan test). The results of these assumptions tests are reported only in cases in which the assumptions were revealed to be untenable. In cases in which suspicious outlying observations may have biased analyses, robust versions of the corresponding models were constructed. In no cases did the resulting conclusions change; only the results of the original analysis are reported. All analyses were carried out in R (R Foundation, r-project.org). Statistical significance was defined as P < .05.
Results
Our study population was predominately male (90%) with a median age of 41 years (range 22-65) and BMI of 29.8 (range 7.7-57.2)(Table 1).
Predictors of CPAP Adherence
OSA severity, as measured by the AHI, was the only promising predictor of CPAP use at 3 months (b, 2.128; t80, 2.854; P = .005; adjusted R2, 0.081). The severity of self-reported daytime sleepiness prior to a diagnosis of OSA, as measured by the ESS, did not predict 3-month CPAP adherence (b, 0.688; t77, 0.300; P = .765; adjusted R2, -0.012). Self-reported depression as measured by the CES-D also did not predict CPAP use at 3 months (b, -0.078; t80, -0.014; P = .941; adjusted R2, -0.012). Similarly, self-reported insomnia, as measured by the ISI, did not predict 3-month CPAP adherence (b, 1.765; t80, 0.939; P = .350; adjusted R2, -0.001). Furthermore, a model that incorporated both depression and insomnia proved no better at accounting for variation in 3-month CPAP use (R2, -0.012). Demographic variables, such as age, sex, or BMI did not predict 3-month CPAP adherence (all Ps > .20). Finally, median CPAP pressure approached statistical significance as a predictor of 3-month CPAP adherence (b, 9.493; t66, 1.881; P = .064; adjusted R2, 0.037) (Figure 1).
CPAP Use at 12 months
The results for CPAP use at 12 months mirrored the results for 3 months with one main exception: OSA severity, as measured by the AHI, did not predict CPAP use at 12 months (b, 1.158; t52, 1.245; P = .219; adjusted R2, 0.010). Neither adding a quadratic predictor nor log transforming the AHI values produced a better model (R2, -0.0007 vs R2, 0.0089, respectively). The severity of self-reported daytime sleepiness, as measured by the ESS, did not predict 12-month CPAP adherence (b, -2.201; t50, -0.752; P = .456; adjusted R2 = -0.0086). Self-reported depression as measured by the CES-D also did not predict CPAP use at 12 months (b, 0.034, t52, 0.022; P = .983; adjusted R2, -0.092). Self-reported insomnia, as measured by the ISI, also did not predict 12-month CPAP adherence (b, 1.765; t80, 0.939; P = .350; adjusted R2 = -0.001). Furthermore, a model that incorporated both depression and insomnia proved no better at accounting for variation in 12-month CPAP use, (R2, -0.0298).
Discussion
Our study did not provide evidence that self-reported depressive and insomnia symptoms, as measured by the CES-D and ISI, can serve as useful predictors of short and long-term CPAP adherence in a sample of active-duty and retired military. OSA severity, as measured by the AHI, was the only promising predictor of CPAP adherence at 3 months.
Insomnia has been shown to improve with the use of CPAP. In a pilot study, Krakow and colleagues investigated the use of CPAP, oral appliances, or bilateral turbinectomy on patients with OSA and chronic insomnia.20 Objective measures of insomnia improved with 1 night of CPAP titration. Björnsdóttir and colleagues evaluated the long-term effects of positive airway pressure (PAP) treatment on 705 adults with middle insomnia.21 They found after 2 years of PAP treatment combined with cognitive behavioral therapy for insomnia, patients had reduced symptoms of middle insomnia. It is possible that persistent insomnia is associated with more severe OSA which was not studied in our population.22
As reported in other studies, it is possible that patients with depressive symptoms can improve with CPAP use, suggesting that depression and CPAP use are not totally unrelated. Edwards and colleagues studied the impact of CPAP on depressive symptoms in men and woman. They found that depressive symptoms are common in OSA and markedly improve with CPAP.23 Bopparaju and colleagues found a high prevalence of anxiety and depression in patients with OSA but did not influence CPAP adherence.24
The results of this study differ from some previous findings where depression was found to predict CPAP adherence.10 This may be due in part to differences in the type of instrument used to assess depression. Wells and colleagues found that baseline depressive symptoms did not correlate with CPAP adherence and that patients with greater CPAP adherence had improvement in OSA and depressive symptoms.25 Furthermore, patients with residual OSA symptoms using CPAP had more depressive symptoms, suggesting that it is the improvement in OSA symptoms that may be correlated with the improvement in depressive symptoms. Although soldiers with PTSD may have reduced CPAP adherence, use of CPAP is associated with improvement in PTSD symptoms.11,26
Limitations
This study had several limitations, including a small sample size. Study patients were also from a single institution, and the majority of patients had mild-to-moderate OSA. A multicenter prospective study with a larger sample size that included more severe patients with OSA may have shown different results. The participants in this study were limited to members from the active-duty and retired military population. The findings in this population may not be transferrable to the general public. Another study limitation was that the ISI and the CES-D were only administered prior to the initiation of CPAP. If the CES-D and ISI were administered at the 3- and 12-month follow-up visits, we could determine whether short and long-term CPAP improved these symptoms or whether there was no association between CPAP adherence with insomnia and depressive symptoms. Another limitation is that we did not have access to information about potential PTSD symptomatology, which has been associated with reduced CPAP adherence and is more common in a military and veteran population.11
Conclusion
This study found little evidence that symptoms of depression and insomnia are useful predictors of CPAP adherence, in either short- or long-term use, in an active-duty and retired military sample. Although these were not found to be predictors of CPAP adherence, further research will be necessary to determine whether CPAP adherence improves symptoms of depression and insomnia in military and veteran populations. Apnea severity did predict CPAP adherence in the short term, but not for any length of time beyond 3 months. More research is needed to explore strategies to improve CPAP adherence in military populations.
1. Qaseem A, Holty JE, Owens DK, Dallas P, Starkey M, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Management of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159(7):471-483.
2. Epstein LJ, Kristo D, Strollo PJ, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-276.
3. Gay P, Weaver T, Loube D, Iber C; Positive Airway Pressure Task Force; Standards of Practice Committee; American Academy of Sleep Medicine. Evaluation of positive airway pressure treatment for sleep-related breathing disorders in adults. Sleep. 2006;29(3):381-401.
4. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver T. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343-356.
5. Luyster FS; Buysse DJ; Strollo PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196-204.
6. Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772-776
7. Pieh C, Bach M, Popp R, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99-104.
8. Nguyên XL, Chaskalovic J, Rakotonanahary D, Fleury B. Insomnia symptoms and CPAP compliance in OSAS patients: a descriptive study using data mining methods. Sleep Med. 2010;11(8):777-784.
9. Yilmaz E, Sedky K, Bennett DS. The relationship between depressive symptoms and obstructive sleep apnea in pediatric populations: a meta-analysis. J Clin Sleep Med. 2013;9(11):1213-1220.
10. Chen YH, Keller JK, Kang JH, Hsieh HJ, Lin HC. Obstructive sleep apnea and the subsequent risk of depressive disorder: a population-based follow-up study. J Clin Sleep Med. 2013;9(5):417-423.
11. Kessler RC, Berglund P, Demler O, et al; National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003:289(23):3095-3105
12. Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13(6):437-444.
13. Schwartz D, Kohler W, Karatinos G. Symptoms of depression in individuals with obstructive sleep apnea may be amendable to treatment with continuous positive airway pressure. Chest. 2005;128(3):1304-1309
14. Law M, Naughton M, Ho S, Roebuck T, Dabscheck E. Depression may reduce adherence during CPAP titration trial. J Clin Sleep Med. 2014;10(2):163-169.
15. Guralnick AS, Pant M, Minhaj M, Sweitzer BJ, Mokhlesi B. CPAP adherence in patients with newly diagnosed obstructive sleep apnea prior to elective surgery. J Clin Sleep Med. 2012;8(5):501-506
16. Collen JF, Lettieri CJ, Hoffman M. The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med. 2012;8(6):667-672.
17. Caldwell A, Knapik JJ, Lieberman HR. Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. J Sleep Res. 2017;26(5):665-670.
18. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307.
19. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychological Measurement. 1977;1(3):385-401.
20. Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath. 2004;8(1):15-29.
21. Björnsdóttir E, Janson C, Sigurdsson JF, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901-1909.
22. Glidewell RN, Renn BN, Roby E, Orr WC. Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med. 2014;15(8):899-905.
23. Edwards C, Mukherjee S, Simpson L, Palmer LJ, Almeida OP, Hillman DR. Depressive symptoms before and after treatment of obstructive sleep apnea in men and women. J Clin Sleep Med. 2015;11(9):1029-1038.
24. Bopparaju S, Casturi L, Guntupalli B, Surani S, Subramanian S. Anxiety and depression in obstructive sleep apnea: Effect of CPAP therapy and influence on CPAP compliance. Presented at: American College of Chest Physicians Annual Meeting, October 31-November 05, 2009; San Diego, CA. Chest. 2009;136(4, meeting abstracts):71S.
25. Wells RD, Freedland KE, Carney RM, Duntley SP, Stepanski EJ. Adherence, reports of benefits, and depression among patients treated with continuous positive airway pressure. Psychosom Med. 2007;69(5):449-454.
26. Orr JE, Smales C, Alexander TH, et al. Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med. 2017;13(1):57-63.
1. Qaseem A, Holty JE, Owens DK, Dallas P, Starkey M, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Management of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159(7):471-483.
2. Epstein LJ, Kristo D, Strollo PJ, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-276.
3. Gay P, Weaver T, Loube D, Iber C; Positive Airway Pressure Task Force; Standards of Practice Committee; American Academy of Sleep Medicine. Evaluation of positive airway pressure treatment for sleep-related breathing disorders in adults. Sleep. 2006;29(3):381-401.
4. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver T. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343-356.
5. Luyster FS; Buysse DJ; Strollo PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196-204.
6. Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772-776
7. Pieh C, Bach M, Popp R, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99-104.
8. Nguyên XL, Chaskalovic J, Rakotonanahary D, Fleury B. Insomnia symptoms and CPAP compliance in OSAS patients: a descriptive study using data mining methods. Sleep Med. 2010;11(8):777-784.
9. Yilmaz E, Sedky K, Bennett DS. The relationship between depressive symptoms and obstructive sleep apnea in pediatric populations: a meta-analysis. J Clin Sleep Med. 2013;9(11):1213-1220.
10. Chen YH, Keller JK, Kang JH, Hsieh HJ, Lin HC. Obstructive sleep apnea and the subsequent risk of depressive disorder: a population-based follow-up study. J Clin Sleep Med. 2013;9(5):417-423.
11. Kessler RC, Berglund P, Demler O, et al; National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003:289(23):3095-3105
12. Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13(6):437-444.
13. Schwartz D, Kohler W, Karatinos G. Symptoms of depression in individuals with obstructive sleep apnea may be amendable to treatment with continuous positive airway pressure. Chest. 2005;128(3):1304-1309
14. Law M, Naughton M, Ho S, Roebuck T, Dabscheck E. Depression may reduce adherence during CPAP titration trial. J Clin Sleep Med. 2014;10(2):163-169.
15. Guralnick AS, Pant M, Minhaj M, Sweitzer BJ, Mokhlesi B. CPAP adherence in patients with newly diagnosed obstructive sleep apnea prior to elective surgery. J Clin Sleep Med. 2012;8(5):501-506
16. Collen JF, Lettieri CJ, Hoffman M. The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med. 2012;8(6):667-672.
17. Caldwell A, Knapik JJ, Lieberman HR. Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. J Sleep Res. 2017;26(5):665-670.
18. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307.
19. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychological Measurement. 1977;1(3):385-401.
20. Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath. 2004;8(1):15-29.
21. Björnsdóttir E, Janson C, Sigurdsson JF, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901-1909.
22. Glidewell RN, Renn BN, Roby E, Orr WC. Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med. 2014;15(8):899-905.
23. Edwards C, Mukherjee S, Simpson L, Palmer LJ, Almeida OP, Hillman DR. Depressive symptoms before and after treatment of obstructive sleep apnea in men and women. J Clin Sleep Med. 2015;11(9):1029-1038.
24. Bopparaju S, Casturi L, Guntupalli B, Surani S, Subramanian S. Anxiety and depression in obstructive sleep apnea: Effect of CPAP therapy and influence on CPAP compliance. Presented at: American College of Chest Physicians Annual Meeting, October 31-November 05, 2009; San Diego, CA. Chest. 2009;136(4, meeting abstracts):71S.
25. Wells RD, Freedland KE, Carney RM, Duntley SP, Stepanski EJ. Adherence, reports of benefits, and depression among patients treated with continuous positive airway pressure. Psychosom Med. 2007;69(5):449-454.
26. Orr JE, Smales C, Alexander TH, et al. Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med. 2017;13(1):57-63.
Sleep Strategies
Compared with obstructive sleep apnea (OSA), the prevalence of central sleep apnea (CSA) is low in the general population. However, in adults, CSA may be highly prevalent in certain conditions, most commonly among those with left ventricular systolic dysfunction, left ventricular diastolic dysfunction, atrial fibrillation, stroke, and opioid users (Javaheri S, et al. J Am Coll Cardiol. 2017; 69:841). CSA may also be found in patients with carotid artery stenosis, cervical neck injury, and renal dysfunction. CSA can occur when OSA is treated (treatment-emergent central sleep apnea, or TECA), notably, and most frequently, with continuous positive airway pressure (CPAP) devices. Though in many individuals, this frequently resolves with continued use of the device.
In addition, unlike OSA, adequate treatment of CSA has proven difficult. Specifically, the response to CPAP, oxygen, theophylline, acetazolamide, and adaptive-servo ventilation (ASV) is highly variable, with individuals who respond well, and individuals in whom therapy fails to fully suppress the disorder.
Our interest in phrenic nerve stimulation increased after it was shown that CPAP therapy failed to improve morbidity and mortality of CSA in patients with heart failure and reduced ejection fraction (HFrEF) (CANPAP trial, Bradley et al. N Engl J Med. 2005;353(19):2025). In fact, in this trial, treatment with CPAP was associated with significantly increased mortality during the first few months of therapy. We reason that a potential mechanism was positive airway pressure that had adverse cardiovascular effects (Javaheri S. J Clin Sleep Med. 2006;2:399). This is because positive airway pressure therapy decreases venous return to the right side of the heart and increases lung volume. This could increase pulmonary vascular resistance (right ventricular afterload), which is lung volume-dependent. Therefore, the subgroup of individuals with heart failure whose right ventricular function is preload-dependent and has pulmonary hypertension is at risk for premature mortality with any PAP device.
Interestingly, investigators of the SERVE-HF trial (Cowie MR, et al. N Engl J Med. 2015;373:1095) also hypothesized that one reason for excess mortality associated with ASV use might have been due to an ASV-associated excessive rise in intrathoracic pressure, similar to the hypothesis we proposed earlier for CPAP. We expanded on this hypothesis and reasoned that based on the algorithm of the device, in some patients, it could have generated excessive minute ventilation and pressure contributing to excess mortality, either at night or daytime (Javaheri S, et al. Chest. 2016;149:900). Other deficiencies of the algorithm of the ASV device could have contributed to excess mortality as well (Javaheri S, et al. Chest. 2014;146:514). These deficiencies of the ASV device used in the SERVE-HF trial have been significantly improved in the new generation of ASV devices.
Undoubtedly, therefore, mask therapy with positive airway pressures increases intrathoracic pressure and will adversely affect cardiovascular function in some patients with heart failure. Another issue for mask therapy is adherence to the device remains poor, as demonstrated both in the CANPAP and SERVE-HF trials, confirming the need for new approaches utilizing non-mask therapies both for CSA and OSA.
Given the limitations of mask-based therapies, over the last several years, we have performed studies exploring the use of oxygen, acetazolamide, theophylline, and, most recently, phrenic nerve stimulation (PNS). In general, these therapies are devoid of increasing intrathoracic pressure and are expected to be less reliant on patients’ adherence than PAP therapy. Long-term randomized clinical trials are needed, and, most recently, the NIH approved a phase 3 trial for a randomized placebo-controlled low flow oxygen therapy for treatment of CSA in HFrEF. This is a modified trial proposed by one of us more than 20 years ago!
Regarding PNS, CSA is characterized by intermittent phrenic nerve (and intercostal nerves) deactivation. It, therefore, makes sense to have an implanted stimulator for the phrenic nerve to prevent development of central apneas during sleep. This is not a new idea. In 1948, Sarnoff and colleagues demonstrated for the first time that artificial respiration could be effectively administered to the cat, dog, monkey, and rabbit in the absence of spontaneous respiration by electrical stimulation of one (or both) phrenic nerves (Sarnoff SJ, et al. Science. 1948;108:482). In later experiments, these investigators showed that unilateral phrenic nerve stimulation is also equally effective in man as that shown in animal models.
The phrenic nerves comes in contact with veins on both the right (brachiocephalic) and the left (pericardiophrenic vein) side of the mediastinum. Like a cardiac pacemaker, an electrophysiologist places the stimulator within the vein at the point of encounter with the phrenic nerve. Only unilateral stimulation is needed for the therapy. The device is typically placed on the right side of the chest as many patients may already have a cardiac implanted electronic device such as a pacemaker. Like the hypoglossal nerve stimulation, the FDA approved this device for the treatment of OSA. The system can be programmed using an external programmer in the office.
Phrenic nerve stimulation system is initially activated 1 month after the device is placed. It is programmed to be automatically activated at night when the patient is at rest. First, a time is set on the device for when the patient typically goes to bed and awakens. This allows the therapy to activate. The device contains a position sensor and accelerometer, which determine position and activity level. Once appropriate time, position, and activity are confirmed, the device activates automatically. Therapy comes on and can increase in level over several minutes. The device senses transthoracic impedance and can use this measurement to make changes in the therapy output and activity. If the patient gets up at night, the device automatically stops and restarts when the patient is back in a sleeping position. How quickly the therapy restarts and at what energy is programmable. The device may allow from 1 to 15 minutes for the patient to get back to sleep before beginning therapy. These programming changes allow for patient acceptance and comfort with the therapy even in very sensitive patients. Importantly, no patient activation is needed, so that therapy delivery is independent of patient’s adherence over time.
In the prospective, randomized pivotal trial (Costanzo et al. Lancet. 2016;388:974), 151 eligible patients with moderate-severe central sleep apnea were implanted and randomly assigned to the treatment (n=73) or control (n=78) groups. Participants in the active arm received PNS for 6 months. All polysomnograms were centrally and blindly scored. There were significant decreases in AHI (50 to 26/per hour of sleep), CAI (32 to 6), arousal index (46 to 25), and ODI (44 to 25). Two points should be emphasized: first, changes in AHI with PNS are similar to those in CANPAP trial, and there remained a significant number of hypopneas (some of these hypopneas are at least in part related to the speed of the titration when the subject sits up and the device automatically is deactivated, only to resume therapy in supine position); second, in contrast to the CANPAP trial, there was a significant reduction in arousals. Probably for this reason, subjective daytime sleepiness, as measured by the ESS, improved. In addition, PNS improved quality of life, in contrast to lack of effect of CPAP or ASV in this domain. Regarding side effects, 138 (91%) of 151 patients had no serious-related adverse events at 12 months. Seven (9%) cases of related-serious adverse events occurred in the control group and six (8%) cases were reported in the treatment group.—3.4% needed lead repositioning, a rate which is like that of cardiac implantable devices. Seven patients died (unrelated to implant, system, or therapy), four deaths (two in treatment group and two in control group) during the 6-month randomization period when neurostimulation was delivered to only the treatment and was off in the control group, and three deaths between 6 months and 12 months of follow-up when all patients received neurostimulation. Of 73 patients in the treatment group, 27 (37%) reported nonserious therapy-related discomfort that was resolved with simple system reprogramming in 26 (36%) patients but was unresolved in one (1%) patient.
Long-term studies have shown sustained effects of PNS on CSA with improvement in both sleep metrics and QOL, as measured by the Minnesota Living with Heart Failure Questionnaire (MLWHF) and patient global assessment (PGA). Furthermore, in the subgroup of patients with concomitant heart failure with LVEF ≤ 45%, PNS was associated with both improvements in LVEF and a trend toward lower hospitalization rates (Costanzo et al. Eur J Heart Fail. 2018; doi:10.1002/ejhf.1312).
Several issues must be emphasized. One advantage of PNS is complete adherence resulting in a major reduction in apnea burden across the whole night. Second, the mechanism of action prevents any potential adverse consequences related to increased intrathoracic pressure. However, the cost of this therapy is high, similar to that of hypoglossal nerve stimulation. Large scale, long-term studies related to mortality are not yet available, and continued research should help identify those patients most likely to benefit from this therapeutic approach.
Compared with obstructive sleep apnea (OSA), the prevalence of central sleep apnea (CSA) is low in the general population. However, in adults, CSA may be highly prevalent in certain conditions, most commonly among those with left ventricular systolic dysfunction, left ventricular diastolic dysfunction, atrial fibrillation, stroke, and opioid users (Javaheri S, et al. J Am Coll Cardiol. 2017; 69:841). CSA may also be found in patients with carotid artery stenosis, cervical neck injury, and renal dysfunction. CSA can occur when OSA is treated (treatment-emergent central sleep apnea, or TECA), notably, and most frequently, with continuous positive airway pressure (CPAP) devices. Though in many individuals, this frequently resolves with continued use of the device.
In addition, unlike OSA, adequate treatment of CSA has proven difficult. Specifically, the response to CPAP, oxygen, theophylline, acetazolamide, and adaptive-servo ventilation (ASV) is highly variable, with individuals who respond well, and individuals in whom therapy fails to fully suppress the disorder.
Our interest in phrenic nerve stimulation increased after it was shown that CPAP therapy failed to improve morbidity and mortality of CSA in patients with heart failure and reduced ejection fraction (HFrEF) (CANPAP trial, Bradley et al. N Engl J Med. 2005;353(19):2025). In fact, in this trial, treatment with CPAP was associated with significantly increased mortality during the first few months of therapy. We reason that a potential mechanism was positive airway pressure that had adverse cardiovascular effects (Javaheri S. J Clin Sleep Med. 2006;2:399). This is because positive airway pressure therapy decreases venous return to the right side of the heart and increases lung volume. This could increase pulmonary vascular resistance (right ventricular afterload), which is lung volume-dependent. Therefore, the subgroup of individuals with heart failure whose right ventricular function is preload-dependent and has pulmonary hypertension is at risk for premature mortality with any PAP device.
Interestingly, investigators of the SERVE-HF trial (Cowie MR, et al. N Engl J Med. 2015;373:1095) also hypothesized that one reason for excess mortality associated with ASV use might have been due to an ASV-associated excessive rise in intrathoracic pressure, similar to the hypothesis we proposed earlier for CPAP. We expanded on this hypothesis and reasoned that based on the algorithm of the device, in some patients, it could have generated excessive minute ventilation and pressure contributing to excess mortality, either at night or daytime (Javaheri S, et al. Chest. 2016;149:900). Other deficiencies of the algorithm of the ASV device could have contributed to excess mortality as well (Javaheri S, et al. Chest. 2014;146:514). These deficiencies of the ASV device used in the SERVE-HF trial have been significantly improved in the new generation of ASV devices.
Undoubtedly, therefore, mask therapy with positive airway pressures increases intrathoracic pressure and will adversely affect cardiovascular function in some patients with heart failure. Another issue for mask therapy is adherence to the device remains poor, as demonstrated both in the CANPAP and SERVE-HF trials, confirming the need for new approaches utilizing non-mask therapies both for CSA and OSA.
Given the limitations of mask-based therapies, over the last several years, we have performed studies exploring the use of oxygen, acetazolamide, theophylline, and, most recently, phrenic nerve stimulation (PNS). In general, these therapies are devoid of increasing intrathoracic pressure and are expected to be less reliant on patients’ adherence than PAP therapy. Long-term randomized clinical trials are needed, and, most recently, the NIH approved a phase 3 trial for a randomized placebo-controlled low flow oxygen therapy for treatment of CSA in HFrEF. This is a modified trial proposed by one of us more than 20 years ago!
Regarding PNS, CSA is characterized by intermittent phrenic nerve (and intercostal nerves) deactivation. It, therefore, makes sense to have an implanted stimulator for the phrenic nerve to prevent development of central apneas during sleep. This is not a new idea. In 1948, Sarnoff and colleagues demonstrated for the first time that artificial respiration could be effectively administered to the cat, dog, monkey, and rabbit in the absence of spontaneous respiration by electrical stimulation of one (or both) phrenic nerves (Sarnoff SJ, et al. Science. 1948;108:482). In later experiments, these investigators showed that unilateral phrenic nerve stimulation is also equally effective in man as that shown in animal models.
The phrenic nerves comes in contact with veins on both the right (brachiocephalic) and the left (pericardiophrenic vein) side of the mediastinum. Like a cardiac pacemaker, an electrophysiologist places the stimulator within the vein at the point of encounter with the phrenic nerve. Only unilateral stimulation is needed for the therapy. The device is typically placed on the right side of the chest as many patients may already have a cardiac implanted electronic device such as a pacemaker. Like the hypoglossal nerve stimulation, the FDA approved this device for the treatment of OSA. The system can be programmed using an external programmer in the office.
Phrenic nerve stimulation system is initially activated 1 month after the device is placed. It is programmed to be automatically activated at night when the patient is at rest. First, a time is set on the device for when the patient typically goes to bed and awakens. This allows the therapy to activate. The device contains a position sensor and accelerometer, which determine position and activity level. Once appropriate time, position, and activity are confirmed, the device activates automatically. Therapy comes on and can increase in level over several minutes. The device senses transthoracic impedance and can use this measurement to make changes in the therapy output and activity. If the patient gets up at night, the device automatically stops and restarts when the patient is back in a sleeping position. How quickly the therapy restarts and at what energy is programmable. The device may allow from 1 to 15 minutes for the patient to get back to sleep before beginning therapy. These programming changes allow for patient acceptance and comfort with the therapy even in very sensitive patients. Importantly, no patient activation is needed, so that therapy delivery is independent of patient’s adherence over time.
In the prospective, randomized pivotal trial (Costanzo et al. Lancet. 2016;388:974), 151 eligible patients with moderate-severe central sleep apnea were implanted and randomly assigned to the treatment (n=73) or control (n=78) groups. Participants in the active arm received PNS for 6 months. All polysomnograms were centrally and blindly scored. There were significant decreases in AHI (50 to 26/per hour of sleep), CAI (32 to 6), arousal index (46 to 25), and ODI (44 to 25). Two points should be emphasized: first, changes in AHI with PNS are similar to those in CANPAP trial, and there remained a significant number of hypopneas (some of these hypopneas are at least in part related to the speed of the titration when the subject sits up and the device automatically is deactivated, only to resume therapy in supine position); second, in contrast to the CANPAP trial, there was a significant reduction in arousals. Probably for this reason, subjective daytime sleepiness, as measured by the ESS, improved. In addition, PNS improved quality of life, in contrast to lack of effect of CPAP or ASV in this domain. Regarding side effects, 138 (91%) of 151 patients had no serious-related adverse events at 12 months. Seven (9%) cases of related-serious adverse events occurred in the control group and six (8%) cases were reported in the treatment group.—3.4% needed lead repositioning, a rate which is like that of cardiac implantable devices. Seven patients died (unrelated to implant, system, or therapy), four deaths (two in treatment group and two in control group) during the 6-month randomization period when neurostimulation was delivered to only the treatment and was off in the control group, and three deaths between 6 months and 12 months of follow-up when all patients received neurostimulation. Of 73 patients in the treatment group, 27 (37%) reported nonserious therapy-related discomfort that was resolved with simple system reprogramming in 26 (36%) patients but was unresolved in one (1%) patient.
Long-term studies have shown sustained effects of PNS on CSA with improvement in both sleep metrics and QOL, as measured by the Minnesota Living with Heart Failure Questionnaire (MLWHF) and patient global assessment (PGA). Furthermore, in the subgroup of patients with concomitant heart failure with LVEF ≤ 45%, PNS was associated with both improvements in LVEF and a trend toward lower hospitalization rates (Costanzo et al. Eur J Heart Fail. 2018; doi:10.1002/ejhf.1312).
Several issues must be emphasized. One advantage of PNS is complete adherence resulting in a major reduction in apnea burden across the whole night. Second, the mechanism of action prevents any potential adverse consequences related to increased intrathoracic pressure. However, the cost of this therapy is high, similar to that of hypoglossal nerve stimulation. Large scale, long-term studies related to mortality are not yet available, and continued research should help identify those patients most likely to benefit from this therapeutic approach.
Compared with obstructive sleep apnea (OSA), the prevalence of central sleep apnea (CSA) is low in the general population. However, in adults, CSA may be highly prevalent in certain conditions, most commonly among those with left ventricular systolic dysfunction, left ventricular diastolic dysfunction, atrial fibrillation, stroke, and opioid users (Javaheri S, et al. J Am Coll Cardiol. 2017; 69:841). CSA may also be found in patients with carotid artery stenosis, cervical neck injury, and renal dysfunction. CSA can occur when OSA is treated (treatment-emergent central sleep apnea, or TECA), notably, and most frequently, with continuous positive airway pressure (CPAP) devices. Though in many individuals, this frequently resolves with continued use of the device.
In addition, unlike OSA, adequate treatment of CSA has proven difficult. Specifically, the response to CPAP, oxygen, theophylline, acetazolamide, and adaptive-servo ventilation (ASV) is highly variable, with individuals who respond well, and individuals in whom therapy fails to fully suppress the disorder.
Our interest in phrenic nerve stimulation increased after it was shown that CPAP therapy failed to improve morbidity and mortality of CSA in patients with heart failure and reduced ejection fraction (HFrEF) (CANPAP trial, Bradley et al. N Engl J Med. 2005;353(19):2025). In fact, in this trial, treatment with CPAP was associated with significantly increased mortality during the first few months of therapy. We reason that a potential mechanism was positive airway pressure that had adverse cardiovascular effects (Javaheri S. J Clin Sleep Med. 2006;2:399). This is because positive airway pressure therapy decreases venous return to the right side of the heart and increases lung volume. This could increase pulmonary vascular resistance (right ventricular afterload), which is lung volume-dependent. Therefore, the subgroup of individuals with heart failure whose right ventricular function is preload-dependent and has pulmonary hypertension is at risk for premature mortality with any PAP device.
Interestingly, investigators of the SERVE-HF trial (Cowie MR, et al. N Engl J Med. 2015;373:1095) also hypothesized that one reason for excess mortality associated with ASV use might have been due to an ASV-associated excessive rise in intrathoracic pressure, similar to the hypothesis we proposed earlier for CPAP. We expanded on this hypothesis and reasoned that based on the algorithm of the device, in some patients, it could have generated excessive minute ventilation and pressure contributing to excess mortality, either at night or daytime (Javaheri S, et al. Chest. 2016;149:900). Other deficiencies of the algorithm of the ASV device could have contributed to excess mortality as well (Javaheri S, et al. Chest. 2014;146:514). These deficiencies of the ASV device used in the SERVE-HF trial have been significantly improved in the new generation of ASV devices.
Undoubtedly, therefore, mask therapy with positive airway pressures increases intrathoracic pressure and will adversely affect cardiovascular function in some patients with heart failure. Another issue for mask therapy is adherence to the device remains poor, as demonstrated both in the CANPAP and SERVE-HF trials, confirming the need for new approaches utilizing non-mask therapies both for CSA and OSA.
Given the limitations of mask-based therapies, over the last several years, we have performed studies exploring the use of oxygen, acetazolamide, theophylline, and, most recently, phrenic nerve stimulation (PNS). In general, these therapies are devoid of increasing intrathoracic pressure and are expected to be less reliant on patients’ adherence than PAP therapy. Long-term randomized clinical trials are needed, and, most recently, the NIH approved a phase 3 trial for a randomized placebo-controlled low flow oxygen therapy for treatment of CSA in HFrEF. This is a modified trial proposed by one of us more than 20 years ago!
Regarding PNS, CSA is characterized by intermittent phrenic nerve (and intercostal nerves) deactivation. It, therefore, makes sense to have an implanted stimulator for the phrenic nerve to prevent development of central apneas during sleep. This is not a new idea. In 1948, Sarnoff and colleagues demonstrated for the first time that artificial respiration could be effectively administered to the cat, dog, monkey, and rabbit in the absence of spontaneous respiration by electrical stimulation of one (or both) phrenic nerves (Sarnoff SJ, et al. Science. 1948;108:482). In later experiments, these investigators showed that unilateral phrenic nerve stimulation is also equally effective in man as that shown in animal models.
The phrenic nerves comes in contact with veins on both the right (brachiocephalic) and the left (pericardiophrenic vein) side of the mediastinum. Like a cardiac pacemaker, an electrophysiologist places the stimulator within the vein at the point of encounter with the phrenic nerve. Only unilateral stimulation is needed for the therapy. The device is typically placed on the right side of the chest as many patients may already have a cardiac implanted electronic device such as a pacemaker. Like the hypoglossal nerve stimulation, the FDA approved this device for the treatment of OSA. The system can be programmed using an external programmer in the office.
Phrenic nerve stimulation system is initially activated 1 month after the device is placed. It is programmed to be automatically activated at night when the patient is at rest. First, a time is set on the device for when the patient typically goes to bed and awakens. This allows the therapy to activate. The device contains a position sensor and accelerometer, which determine position and activity level. Once appropriate time, position, and activity are confirmed, the device activates automatically. Therapy comes on and can increase in level over several minutes. The device senses transthoracic impedance and can use this measurement to make changes in the therapy output and activity. If the patient gets up at night, the device automatically stops and restarts when the patient is back in a sleeping position. How quickly the therapy restarts and at what energy is programmable. The device may allow from 1 to 15 minutes for the patient to get back to sleep before beginning therapy. These programming changes allow for patient acceptance and comfort with the therapy even in very sensitive patients. Importantly, no patient activation is needed, so that therapy delivery is independent of patient’s adherence over time.
In the prospective, randomized pivotal trial (Costanzo et al. Lancet. 2016;388:974), 151 eligible patients with moderate-severe central sleep apnea were implanted and randomly assigned to the treatment (n=73) or control (n=78) groups. Participants in the active arm received PNS for 6 months. All polysomnograms were centrally and blindly scored. There were significant decreases in AHI (50 to 26/per hour of sleep), CAI (32 to 6), arousal index (46 to 25), and ODI (44 to 25). Two points should be emphasized: first, changes in AHI with PNS are similar to those in CANPAP trial, and there remained a significant number of hypopneas (some of these hypopneas are at least in part related to the speed of the titration when the subject sits up and the device automatically is deactivated, only to resume therapy in supine position); second, in contrast to the CANPAP trial, there was a significant reduction in arousals. Probably for this reason, subjective daytime sleepiness, as measured by the ESS, improved. In addition, PNS improved quality of life, in contrast to lack of effect of CPAP or ASV in this domain. Regarding side effects, 138 (91%) of 151 patients had no serious-related adverse events at 12 months. Seven (9%) cases of related-serious adverse events occurred in the control group and six (8%) cases were reported in the treatment group.—3.4% needed lead repositioning, a rate which is like that of cardiac implantable devices. Seven patients died (unrelated to implant, system, or therapy), four deaths (two in treatment group and two in control group) during the 6-month randomization period when neurostimulation was delivered to only the treatment and was off in the control group, and three deaths between 6 months and 12 months of follow-up when all patients received neurostimulation. Of 73 patients in the treatment group, 27 (37%) reported nonserious therapy-related discomfort that was resolved with simple system reprogramming in 26 (36%) patients but was unresolved in one (1%) patient.
Long-term studies have shown sustained effects of PNS on CSA with improvement in both sleep metrics and QOL, as measured by the Minnesota Living with Heart Failure Questionnaire (MLWHF) and patient global assessment (PGA). Furthermore, in the subgroup of patients with concomitant heart failure with LVEF ≤ 45%, PNS was associated with both improvements in LVEF and a trend toward lower hospitalization rates (Costanzo et al. Eur J Heart Fail. 2018; doi:10.1002/ejhf.1312).
Several issues must be emphasized. One advantage of PNS is complete adherence resulting in a major reduction in apnea burden across the whole night. Second, the mechanism of action prevents any potential adverse consequences related to increased intrathoracic pressure. However, the cost of this therapy is high, similar to that of hypoglossal nerve stimulation. Large scale, long-term studies related to mortality are not yet available, and continued research should help identify those patients most likely to benefit from this therapeutic approach.