User login
A ‘crisis’ of suicidal thoughts, attempts in transgender youth
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
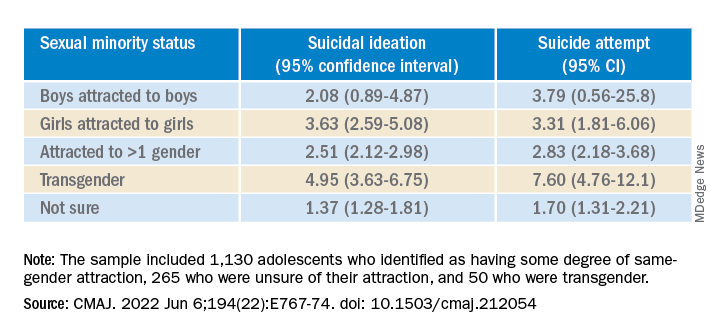
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
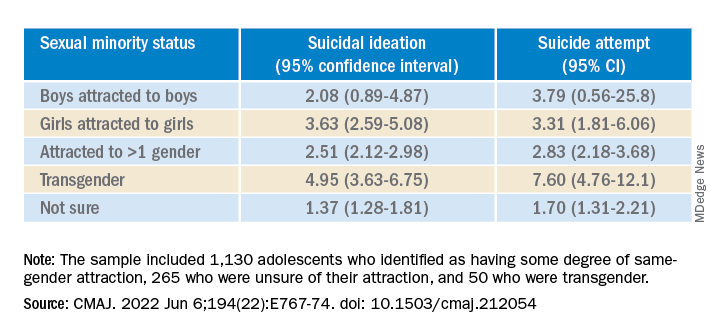
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
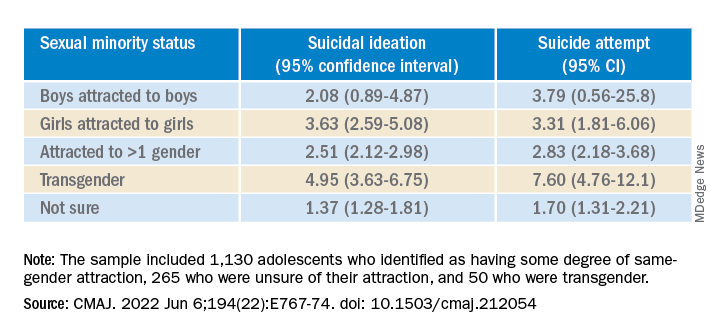
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
New studies show growing number of trans, nonbinary youth in U.S.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Trans teens less likely to commit acts of sexual violence, says new study
Transgender and nonbinary adolescents are twice as likely to experience sexual violence as their cisgendered peers but are less likely to attempt rape or commit sexual assault, researchers have found.
The study, which was published online in JAMA Network Open, is among the first on the sexual violence that trans, nonbinary, and other gender nonconforming adolescents experience. Previous studies have focused on adults.
“In the busy world of clinical care, it is essential that clinicians be aware of potential disparities their patients are navigating,” said Michele Ybarra, PhD, MPH, president and research director of the Center for Innovative Public Health Research, San Clemente, California, who led the study. “This includes sexual violence victimization for gender minority youth and the need to talk about consent and boundaries for youth of all genders.”
Dr. Ybarra said that while clinicians may be aware that transgender young people face stigma, discrimination, and bullying, they may not be aware that trans youth are also the targets of sexual violence.
Studies indicate that health care providers and communities have significant misconceptions about sexually explicit behavior among trans and nonbinary teens. Misconceptions can lead to discrimination, resulting in higher rates of drug abuse, dropping out of school, suicide, and homelessness.
Dr. Ybarra and her colleagues surveyed 911 trans, nonbinary, or questioning youth on Instagram and Facebook through a collaboration with Growing Up With Media, a national longitudinal survey designed to investigate sexual violence during adolescence.
They also surveyed 3,282 cisgender persons aged 14-16 years who were recruited to the study between June 2018 and March 2020. The term “cisgender” refers to youth who identify with their gender at birth.
The questionnaires asked teens about gender identity, race, economic status, and support systems at home. Factors associated with not experiencing sexual violence included having a strong network of friends, family, and educators; involvement in the community; and having people close who affirm their gender identity.
More than three-fourths (78%) of youth surveyed identified as cisgender, 13.9% identified as questioning, and 7.9% identified as transgender.
Roughly two-thirds (67%) of transgender adolescents said they had experienced serious sexual violence, 73% reported experiencing violence in their communities, and 63% said they had been exposed to aggressive behavior. In contrast, 6.7% of trans youth said they had ever committed sexual violence, while 7.4% of cisgender teens surveyed, or 243 students, said they had done so.
“The relative lack of visibility of gender minority youth in sexual violence research is unacceptable,” Dr. Ybarra told this news organization. “To be counted, one needs to be seen. We aimed to start addressing this exclusion with the current study.”
The findings provide a lens into the levels of sexual violence that LGBTQIA+ youth experience and an opportunity to provide more inclusive care, according to Elizabeth Miller, MD, PhD, FSAHM, Distinguished Professor of Pediatrics, director of the Division of Adolescent and Young Adult Medicine, and medical director of community and population health at UPMC Children’s Hospital of Pittsburgh, who was not involved in the study.
“There are unfortunately pervasive and harmful stereotypes in our society about the ‘sexual deviancy’ attributed to LGBTQIA+ individuals,” Dr. Miller told this news organization. “This study adds to the research literature that counters and challenges these harmful – and inaccurate – perceptions.”
Dr. Miller said clinicians can help this population by offering youth accurate information about relevant support and services, including how to help a friend.
Programs that providers could incorporate include gender transformative approaches, which guide youth to examine gender norms and inequities and that develop leadership skills.
Such programs are more common outside the United States and have been shown to decrease LGBTQIA+ youth exposure to sexual violence, she said.
Dr. Miller said more research is needed to understand the contexts in which gender minority youth experience sexual violence to guide prevention efforts: “We need to move beyond individual-focused interventions to considering community-level interventions to create safer and more inclusive spaces for all youth.”
Dr. Miller has received royalties for writing content for UptoDate Wolters Kluwer outside of the current study. Dr. Ybarra has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender and nonbinary adolescents are twice as likely to experience sexual violence as their cisgendered peers but are less likely to attempt rape or commit sexual assault, researchers have found.
The study, which was published online in JAMA Network Open, is among the first on the sexual violence that trans, nonbinary, and other gender nonconforming adolescents experience. Previous studies have focused on adults.
“In the busy world of clinical care, it is essential that clinicians be aware of potential disparities their patients are navigating,” said Michele Ybarra, PhD, MPH, president and research director of the Center for Innovative Public Health Research, San Clemente, California, who led the study. “This includes sexual violence victimization for gender minority youth and the need to talk about consent and boundaries for youth of all genders.”
Dr. Ybarra said that while clinicians may be aware that transgender young people face stigma, discrimination, and bullying, they may not be aware that trans youth are also the targets of sexual violence.
Studies indicate that health care providers and communities have significant misconceptions about sexually explicit behavior among trans and nonbinary teens. Misconceptions can lead to discrimination, resulting in higher rates of drug abuse, dropping out of school, suicide, and homelessness.
Dr. Ybarra and her colleagues surveyed 911 trans, nonbinary, or questioning youth on Instagram and Facebook through a collaboration with Growing Up With Media, a national longitudinal survey designed to investigate sexual violence during adolescence.
They also surveyed 3,282 cisgender persons aged 14-16 years who were recruited to the study between June 2018 and March 2020. The term “cisgender” refers to youth who identify with their gender at birth.
The questionnaires asked teens about gender identity, race, economic status, and support systems at home. Factors associated with not experiencing sexual violence included having a strong network of friends, family, and educators; involvement in the community; and having people close who affirm their gender identity.
More than three-fourths (78%) of youth surveyed identified as cisgender, 13.9% identified as questioning, and 7.9% identified as transgender.
Roughly two-thirds (67%) of transgender adolescents said they had experienced serious sexual violence, 73% reported experiencing violence in their communities, and 63% said they had been exposed to aggressive behavior. In contrast, 6.7% of trans youth said they had ever committed sexual violence, while 7.4% of cisgender teens surveyed, or 243 students, said they had done so.
“The relative lack of visibility of gender minority youth in sexual violence research is unacceptable,” Dr. Ybarra told this news organization. “To be counted, one needs to be seen. We aimed to start addressing this exclusion with the current study.”
The findings provide a lens into the levels of sexual violence that LGBTQIA+ youth experience and an opportunity to provide more inclusive care, according to Elizabeth Miller, MD, PhD, FSAHM, Distinguished Professor of Pediatrics, director of the Division of Adolescent and Young Adult Medicine, and medical director of community and population health at UPMC Children’s Hospital of Pittsburgh, who was not involved in the study.
“There are unfortunately pervasive and harmful stereotypes in our society about the ‘sexual deviancy’ attributed to LGBTQIA+ individuals,” Dr. Miller told this news organization. “This study adds to the research literature that counters and challenges these harmful – and inaccurate – perceptions.”
Dr. Miller said clinicians can help this population by offering youth accurate information about relevant support and services, including how to help a friend.
Programs that providers could incorporate include gender transformative approaches, which guide youth to examine gender norms and inequities and that develop leadership skills.
Such programs are more common outside the United States and have been shown to decrease LGBTQIA+ youth exposure to sexual violence, she said.
Dr. Miller said more research is needed to understand the contexts in which gender minority youth experience sexual violence to guide prevention efforts: “We need to move beyond individual-focused interventions to considering community-level interventions to create safer and more inclusive spaces for all youth.”
Dr. Miller has received royalties for writing content for UptoDate Wolters Kluwer outside of the current study. Dr. Ybarra has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender and nonbinary adolescents are twice as likely to experience sexual violence as their cisgendered peers but are less likely to attempt rape or commit sexual assault, researchers have found.
The study, which was published online in JAMA Network Open, is among the first on the sexual violence that trans, nonbinary, and other gender nonconforming adolescents experience. Previous studies have focused on adults.
“In the busy world of clinical care, it is essential that clinicians be aware of potential disparities their patients are navigating,” said Michele Ybarra, PhD, MPH, president and research director of the Center for Innovative Public Health Research, San Clemente, California, who led the study. “This includes sexual violence victimization for gender minority youth and the need to talk about consent and boundaries for youth of all genders.”
Dr. Ybarra said that while clinicians may be aware that transgender young people face stigma, discrimination, and bullying, they may not be aware that trans youth are also the targets of sexual violence.
Studies indicate that health care providers and communities have significant misconceptions about sexually explicit behavior among trans and nonbinary teens. Misconceptions can lead to discrimination, resulting in higher rates of drug abuse, dropping out of school, suicide, and homelessness.
Dr. Ybarra and her colleagues surveyed 911 trans, nonbinary, or questioning youth on Instagram and Facebook through a collaboration with Growing Up With Media, a national longitudinal survey designed to investigate sexual violence during adolescence.
They also surveyed 3,282 cisgender persons aged 14-16 years who were recruited to the study between June 2018 and March 2020. The term “cisgender” refers to youth who identify with their gender at birth.
The questionnaires asked teens about gender identity, race, economic status, and support systems at home. Factors associated with not experiencing sexual violence included having a strong network of friends, family, and educators; involvement in the community; and having people close who affirm their gender identity.
More than three-fourths (78%) of youth surveyed identified as cisgender, 13.9% identified as questioning, and 7.9% identified as transgender.
Roughly two-thirds (67%) of transgender adolescents said they had experienced serious sexual violence, 73% reported experiencing violence in their communities, and 63% said they had been exposed to aggressive behavior. In contrast, 6.7% of trans youth said they had ever committed sexual violence, while 7.4% of cisgender teens surveyed, or 243 students, said they had done so.
“The relative lack of visibility of gender minority youth in sexual violence research is unacceptable,” Dr. Ybarra told this news organization. “To be counted, one needs to be seen. We aimed to start addressing this exclusion with the current study.”
The findings provide a lens into the levels of sexual violence that LGBTQIA+ youth experience and an opportunity to provide more inclusive care, according to Elizabeth Miller, MD, PhD, FSAHM, Distinguished Professor of Pediatrics, director of the Division of Adolescent and Young Adult Medicine, and medical director of community and population health at UPMC Children’s Hospital of Pittsburgh, who was not involved in the study.
“There are unfortunately pervasive and harmful stereotypes in our society about the ‘sexual deviancy’ attributed to LGBTQIA+ individuals,” Dr. Miller told this news organization. “This study adds to the research literature that counters and challenges these harmful – and inaccurate – perceptions.”
Dr. Miller said clinicians can help this population by offering youth accurate information about relevant support and services, including how to help a friend.
Programs that providers could incorporate include gender transformative approaches, which guide youth to examine gender norms and inequities and that develop leadership skills.
Such programs are more common outside the United States and have been shown to decrease LGBTQIA+ youth exposure to sexual violence, she said.
Dr. Miller said more research is needed to understand the contexts in which gender minority youth experience sexual violence to guide prevention efforts: “We need to move beyond individual-focused interventions to considering community-level interventions to create safer and more inclusive spaces for all youth.”
Dr. Miller has received royalties for writing content for UptoDate Wolters Kluwer outside of the current study. Dr. Ybarra has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Urinary incontinence in transfeminine patients
Whether your patient is a cisgender female or a transfeminine patient, urinary incontinence is unfortunately common and can have a significant negative effect on a person’s quality of life. While the incidence of incontinence is relatively well established in the cisgender population, these statistics remain elusive among transfeminine individuals. Many studies today currently examine cosmetic results, sexual function, and major complications rates, and are now starting to explore the long-term effects of these surgeries on the urinary tract.1
As gender-affirming surgery increases in prevalence, our knowledge regarding long-term outcomes impacting quality of life needs to subsequently improve. A few small studies have examined the rates of incontinence and urinary dysfunction among transfeminine patients. In one study, changes in voiding were reported in 32% of patients, with 19% reporting worse voiding and 19% reporting some degree of incontinence.2 A small series of 52 transgender female patients found rates of urinary urgency to be 24.6% and stress incontinence 23%.1,3 Another study of only 18 patients demonstrated a significant rate of incontinence at 33%, which was due to stress urinary incontinence and overactive bladder.1,4 Other studies noted postvoid dribbling to be as high as 79%.1,2
Obtaining a thorough history is essential in evaluating patients with incontinence. Compared with cisgender females, risk factors for urinary incontinence in cisgender males are naturally different. For example, increasing age, parity, vaginal delivery, history of hysterectomy, and obesity are some risk factors for incontinence in cisgender women.1,6 However, in men, overall rates are lower and tend to be associated with factors such as a history of stroke, diabetes, and injury to the urethral sphincter – which can occur in radical prostatectomy.1
In addition to asking standard questions, such as caffeine use, beverage consumption, medication changes, physical activity, etc., the relationship of a patient’s symptoms to her vaginoplasty is crucial. Providers should elucidate whether patients experienced urinary symptoms prior to surgery, note the type of vaginoplasty performed, and determine if any temporal relationship exists with dilation or intercourse.
Communicating with the original surgeon and obtaining operative reports is often necessary to understand the flaps utilized and the current anatomic structures that were altered during surgery. Creation of the neovagina involves dissection through the levator ani, which can lead to neurologic injury and subsequently predispose patients to incontinence. The surgeon must be meticulous in their creation of the neovaginal space, particularly between the rectum and the prostatic urethra. As the dissection continues in a cephalad direction to the peritoneal reflection, the bladder can also suffer an iatrogenic injury.
In cases of the penile inversion vaginoplasty, a skin graft is typically used to line the neovaginal canal. If this graft fails to take appropriately it can prolapse and can contribute to urinary incontinence symptoms. Some surgeons will suspend the apical portion of the neovagina; however, the effect on rates of incontinence is mixed.
The physical exam of a transfeminine patient should consist of a general health assessment, neurological, abdominal, and genitourinary examinations. Palpation of the prostate is performed through the neovaginal canal if patent. During the urinary exam, the provider should make note of stenosis at the urethral meatus or urethral hypermobility. For patients reporting symptoms of stress incontinence, a cough stress test is useful. The neovagina should be carefully examined for fistula formation or any other structural abnormality.
Testing for urinary incontinence is similar to the evaluation in cisgender females in that every patient should undergo a urinalysis and a postvoid residual volume measurement, and should maintain a voiding diary. Indications for urodynamic testing are the same for transfeminine women and cisgender women – symptoms do not correlate with objective findings, failure to improve with treatment, prior incontinence from pelvic floor surgery, difficult diagnostic evaluation with unclear diagnosis.5,6 Cystoscopy is useful for patients experiencing hematuria, before anti-incontinence surgery, or prior to transurethral prostate intervention.1
Treatment is tailored to the type of incontinence diagnosed; however, there are no specific guidelines that are evidence-based for transfeminine patients after vaginoplasty. The therapies available are extrapolated from the general patient population. All patients can benefit from dietary modifications such as avoiding bladder irritants, monitoring fluid and caffeine intake, timed voiding, and pelvic floor exercises.1,6 If patients do not experience improvement from conservative measures, the mainstay treatment for overactive bladder is antimuscarinic agents. However, in cisgender male patients who have a prostate, these agents can lead to urinary retention related to bladder outlet obstruction, although the rates of urinary retention are low.1 Overall, these agents are relatively safe and effective in cisgender men with a prostate and by extension should be utilized in transfeminine patients when indicated.
In patients diagnosed with stress urinary incontinence, conservative options with weight loss, smoking cessation, and pelvic floor exercises should be attempted. If these measures fail in cisgender women, surgical treatment is often recommended. However, surgical treatment in transfeminine patients is significantly less straightforward and beyond the scope of this article.
Obstetrician/gynecologists are familiar with assessing and treating cisgender female patients reporting incontinence and should use this same knowledge for diagnosing and treating transfeminine patients. In addition, providers should be aware of complications of these procedures in evaluating patients presenting for symptoms of incontinence, as these complications directly contribute to incontinence in this patient population.1
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Email her at [email protected] .
References
1. Ginzburg N. Care of transgender patients: Incontinence. In: Nikolavsky D, Blakley SA, eds. Urological Care for the Transgender Patient: A Comprehensive Guide. Syracuse, NY: Springer, 2021:203-17.
2. Hoebeke P et al. Eur Urol. 2005;47(3):398-402.
3. Kuhn A et al. Fertil Steril. 2011;95(7):2379-82.
4. Kuhn A et al. Eur J Obstet Gynecol Reprod Biol. 2007;131(2):226-30.
5. Winters JC et al. J Urol. 2012;188(6s):2464-72.
6. Practice Bulletin No. 155. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;126:e66-81.
Whether your patient is a cisgender female or a transfeminine patient, urinary incontinence is unfortunately common and can have a significant negative effect on a person’s quality of life. While the incidence of incontinence is relatively well established in the cisgender population, these statistics remain elusive among transfeminine individuals. Many studies today currently examine cosmetic results, sexual function, and major complications rates, and are now starting to explore the long-term effects of these surgeries on the urinary tract.1
As gender-affirming surgery increases in prevalence, our knowledge regarding long-term outcomes impacting quality of life needs to subsequently improve. A few small studies have examined the rates of incontinence and urinary dysfunction among transfeminine patients. In one study, changes in voiding were reported in 32% of patients, with 19% reporting worse voiding and 19% reporting some degree of incontinence.2 A small series of 52 transgender female patients found rates of urinary urgency to be 24.6% and stress incontinence 23%.1,3 Another study of only 18 patients demonstrated a significant rate of incontinence at 33%, which was due to stress urinary incontinence and overactive bladder.1,4 Other studies noted postvoid dribbling to be as high as 79%.1,2
Obtaining a thorough history is essential in evaluating patients with incontinence. Compared with cisgender females, risk factors for urinary incontinence in cisgender males are naturally different. For example, increasing age, parity, vaginal delivery, history of hysterectomy, and obesity are some risk factors for incontinence in cisgender women.1,6 However, in men, overall rates are lower and tend to be associated with factors such as a history of stroke, diabetes, and injury to the urethral sphincter – which can occur in radical prostatectomy.1
In addition to asking standard questions, such as caffeine use, beverage consumption, medication changes, physical activity, etc., the relationship of a patient’s symptoms to her vaginoplasty is crucial. Providers should elucidate whether patients experienced urinary symptoms prior to surgery, note the type of vaginoplasty performed, and determine if any temporal relationship exists with dilation or intercourse.
Communicating with the original surgeon and obtaining operative reports is often necessary to understand the flaps utilized and the current anatomic structures that were altered during surgery. Creation of the neovagina involves dissection through the levator ani, which can lead to neurologic injury and subsequently predispose patients to incontinence. The surgeon must be meticulous in their creation of the neovaginal space, particularly between the rectum and the prostatic urethra. As the dissection continues in a cephalad direction to the peritoneal reflection, the bladder can also suffer an iatrogenic injury.
In cases of the penile inversion vaginoplasty, a skin graft is typically used to line the neovaginal canal. If this graft fails to take appropriately it can prolapse and can contribute to urinary incontinence symptoms. Some surgeons will suspend the apical portion of the neovagina; however, the effect on rates of incontinence is mixed.
The physical exam of a transfeminine patient should consist of a general health assessment, neurological, abdominal, and genitourinary examinations. Palpation of the prostate is performed through the neovaginal canal if patent. During the urinary exam, the provider should make note of stenosis at the urethral meatus or urethral hypermobility. For patients reporting symptoms of stress incontinence, a cough stress test is useful. The neovagina should be carefully examined for fistula formation or any other structural abnormality.
Testing for urinary incontinence is similar to the evaluation in cisgender females in that every patient should undergo a urinalysis and a postvoid residual volume measurement, and should maintain a voiding diary. Indications for urodynamic testing are the same for transfeminine women and cisgender women – symptoms do not correlate with objective findings, failure to improve with treatment, prior incontinence from pelvic floor surgery, difficult diagnostic evaluation with unclear diagnosis.5,6 Cystoscopy is useful for patients experiencing hematuria, before anti-incontinence surgery, or prior to transurethral prostate intervention.1
Treatment is tailored to the type of incontinence diagnosed; however, there are no specific guidelines that are evidence-based for transfeminine patients after vaginoplasty. The therapies available are extrapolated from the general patient population. All patients can benefit from dietary modifications such as avoiding bladder irritants, monitoring fluid and caffeine intake, timed voiding, and pelvic floor exercises.1,6 If patients do not experience improvement from conservative measures, the mainstay treatment for overactive bladder is antimuscarinic agents. However, in cisgender male patients who have a prostate, these agents can lead to urinary retention related to bladder outlet obstruction, although the rates of urinary retention are low.1 Overall, these agents are relatively safe and effective in cisgender men with a prostate and by extension should be utilized in transfeminine patients when indicated.
In patients diagnosed with stress urinary incontinence, conservative options with weight loss, smoking cessation, and pelvic floor exercises should be attempted. If these measures fail in cisgender women, surgical treatment is often recommended. However, surgical treatment in transfeminine patients is significantly less straightforward and beyond the scope of this article.
Obstetrician/gynecologists are familiar with assessing and treating cisgender female patients reporting incontinence and should use this same knowledge for diagnosing and treating transfeminine patients. In addition, providers should be aware of complications of these procedures in evaluating patients presenting for symptoms of incontinence, as these complications directly contribute to incontinence in this patient population.1
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Email her at [email protected] .
References
1. Ginzburg N. Care of transgender patients: Incontinence. In: Nikolavsky D, Blakley SA, eds. Urological Care for the Transgender Patient: A Comprehensive Guide. Syracuse, NY: Springer, 2021:203-17.
2. Hoebeke P et al. Eur Urol. 2005;47(3):398-402.
3. Kuhn A et al. Fertil Steril. 2011;95(7):2379-82.
4. Kuhn A et al. Eur J Obstet Gynecol Reprod Biol. 2007;131(2):226-30.
5. Winters JC et al. J Urol. 2012;188(6s):2464-72.
6. Practice Bulletin No. 155. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;126:e66-81.
Whether your patient is a cisgender female or a transfeminine patient, urinary incontinence is unfortunately common and can have a significant negative effect on a person’s quality of life. While the incidence of incontinence is relatively well established in the cisgender population, these statistics remain elusive among transfeminine individuals. Many studies today currently examine cosmetic results, sexual function, and major complications rates, and are now starting to explore the long-term effects of these surgeries on the urinary tract.1
As gender-affirming surgery increases in prevalence, our knowledge regarding long-term outcomes impacting quality of life needs to subsequently improve. A few small studies have examined the rates of incontinence and urinary dysfunction among transfeminine patients. In one study, changes in voiding were reported in 32% of patients, with 19% reporting worse voiding and 19% reporting some degree of incontinence.2 A small series of 52 transgender female patients found rates of urinary urgency to be 24.6% and stress incontinence 23%.1,3 Another study of only 18 patients demonstrated a significant rate of incontinence at 33%, which was due to stress urinary incontinence and overactive bladder.1,4 Other studies noted postvoid dribbling to be as high as 79%.1,2
Obtaining a thorough history is essential in evaluating patients with incontinence. Compared with cisgender females, risk factors for urinary incontinence in cisgender males are naturally different. For example, increasing age, parity, vaginal delivery, history of hysterectomy, and obesity are some risk factors for incontinence in cisgender women.1,6 However, in men, overall rates are lower and tend to be associated with factors such as a history of stroke, diabetes, and injury to the urethral sphincter – which can occur in radical prostatectomy.1
In addition to asking standard questions, such as caffeine use, beverage consumption, medication changes, physical activity, etc., the relationship of a patient’s symptoms to her vaginoplasty is crucial. Providers should elucidate whether patients experienced urinary symptoms prior to surgery, note the type of vaginoplasty performed, and determine if any temporal relationship exists with dilation or intercourse.
Communicating with the original surgeon and obtaining operative reports is often necessary to understand the flaps utilized and the current anatomic structures that were altered during surgery. Creation of the neovagina involves dissection through the levator ani, which can lead to neurologic injury and subsequently predispose patients to incontinence. The surgeon must be meticulous in their creation of the neovaginal space, particularly between the rectum and the prostatic urethra. As the dissection continues in a cephalad direction to the peritoneal reflection, the bladder can also suffer an iatrogenic injury.
In cases of the penile inversion vaginoplasty, a skin graft is typically used to line the neovaginal canal. If this graft fails to take appropriately it can prolapse and can contribute to urinary incontinence symptoms. Some surgeons will suspend the apical portion of the neovagina; however, the effect on rates of incontinence is mixed.
The physical exam of a transfeminine patient should consist of a general health assessment, neurological, abdominal, and genitourinary examinations. Palpation of the prostate is performed through the neovaginal canal if patent. During the urinary exam, the provider should make note of stenosis at the urethral meatus or urethral hypermobility. For patients reporting symptoms of stress incontinence, a cough stress test is useful. The neovagina should be carefully examined for fistula formation or any other structural abnormality.
Testing for urinary incontinence is similar to the evaluation in cisgender females in that every patient should undergo a urinalysis and a postvoid residual volume measurement, and should maintain a voiding diary. Indications for urodynamic testing are the same for transfeminine women and cisgender women – symptoms do not correlate with objective findings, failure to improve with treatment, prior incontinence from pelvic floor surgery, difficult diagnostic evaluation with unclear diagnosis.5,6 Cystoscopy is useful for patients experiencing hematuria, before anti-incontinence surgery, or prior to transurethral prostate intervention.1
Treatment is tailored to the type of incontinence diagnosed; however, there are no specific guidelines that are evidence-based for transfeminine patients after vaginoplasty. The therapies available are extrapolated from the general patient population. All patients can benefit from dietary modifications such as avoiding bladder irritants, monitoring fluid and caffeine intake, timed voiding, and pelvic floor exercises.1,6 If patients do not experience improvement from conservative measures, the mainstay treatment for overactive bladder is antimuscarinic agents. However, in cisgender male patients who have a prostate, these agents can lead to urinary retention related to bladder outlet obstruction, although the rates of urinary retention are low.1 Overall, these agents are relatively safe and effective in cisgender men with a prostate and by extension should be utilized in transfeminine patients when indicated.
In patients diagnosed with stress urinary incontinence, conservative options with weight loss, smoking cessation, and pelvic floor exercises should be attempted. If these measures fail in cisgender women, surgical treatment is often recommended. However, surgical treatment in transfeminine patients is significantly less straightforward and beyond the scope of this article.
Obstetrician/gynecologists are familiar with assessing and treating cisgender female patients reporting incontinence and should use this same knowledge for diagnosing and treating transfeminine patients. In addition, providers should be aware of complications of these procedures in evaluating patients presenting for symptoms of incontinence, as these complications directly contribute to incontinence in this patient population.1
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Email her at [email protected] .
References
1. Ginzburg N. Care of transgender patients: Incontinence. In: Nikolavsky D, Blakley SA, eds. Urological Care for the Transgender Patient: A Comprehensive Guide. Syracuse, NY: Springer, 2021:203-17.
2. Hoebeke P et al. Eur Urol. 2005;47(3):398-402.
3. Kuhn A et al. Fertil Steril. 2011;95(7):2379-82.
4. Kuhn A et al. Eur J Obstet Gynecol Reprod Biol. 2007;131(2):226-30.
5. Winters JC et al. J Urol. 2012;188(6s):2464-72.
6. Practice Bulletin No. 155. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;126:e66-81.
Few children with early social gender transition change their minds
Approximately 7% of youth who chose gender identity social transition in early childhood had retransitioned 5 years later, based on data from 317 individuals.
“Increasing numbers of children are socially transitioning to live in line with their gender identity, rather than the gender assumed by their sex at birth – a process that typically involves changing a child’s pronouns, first name, hairstyle, and clothing,” wrote Kristina R. Olson, PhD, of Princeton (N.J.) University, and colleagues.
The question of whether early childhood social transitions will result in high rates of retransition continues to be a subject for debate, and long-term data on retransition rates and identity outcomes in children who transition are limited, they said.
To examine retransition in early-transitioning children, the researchers identified 317 binary socially transitioned transgender children to participate in a longitudinal study known as the Trans Youth Project (TYP) between July 2013 and December 2017. The study was published in Pediatrics. The mean age at baseline was 8 years. At study entry, participants had to have made a complete binary social transition, including changing their pronouns from those used at birth. During the 5-year follow-up period, children and parents were asked about use of puberty blockers and/or gender-affirming hormones. At study entry, 37 children had begun some type of puberty blockers. A total of 124 children initially socially transitioned before 6 years of age, and 193 initially socially transitioned at 6 years or older.
The study did not evaluate whether the participants met the DSM-5 criteria for gender dysphoria in childhood, the researchers noted. “Based on data collected at their initial visit, we do know that these participants showed signs of gender identification and gender-typed preferences commonly associated with their gender, not their sex assigned at birth,” they wrote.
Participants were classified as binary transgender, nonbinary, or cisgender based on their pronouns at follow-up. Binary transgender pronouns were associated with the other binary assigned sex, nonbinary pronouns were they/them or a mix of they/them and binary pronouns, and cisgender pronouns were those associated with assigned sex.
Overall, 7.3% of the participants had retransitioned at least once by 5 years after their initial binary social transition. The majority (94%) were living as binary transgender youth, including 1.3% who retransitioned to cisgender or nonbinary and then back to binary transgender during the follow-up period. A total of 2.5% were living as cisgender youth and 3.5% were living as nonbinary youth. These rates were similar across the initial population, as well as the 291 participants who continue to be in contact with the researchers, the 200 who had gone at least 5 years since their initial social transition, and the 280 participants who began the study before starting puberty blockers.
The researchers found no differences in retransition rates related to participant sex at birth. Rates of retransition were slightly higher among participants who made their initial social transition before 6 years of age, but these rates were low, the researchers noted.
The study findings were limited by several factors including the use of a volunteer community sample, with the potential for bias that may not generalize to the population at large, the researchers noted. Other limitations included the use of pronouns as the main criteria for retransition, and the classification of a change from binary transgender to nonbinary as a transition, they said. “Many nonbinary people consider themselves to be transgender,” they noted.
“If we had used a stricter criterion of retransition, more similar to the common use of terms like “detransition” or “desistence,” referring only to youth who are living as cisgender, then our retransition rate would have been lower (2.5%),” the researchers explained. Another limitation was the disproportionate number of trans girls, the researchers said. However, because no significant gender effect appeared in terms of retransition rates, “we do not predict any change in pattern of results if we had a different ratio of participants by sex at birth,” they said.
The researchers stated that they intend to follow the cohort through adolescence and into adulthood.
“As more youth are coming out and being supported in their transitions early in development, it is increasingly critical that clinicians understand the experiences of this cohort and not make assumptions about them as a function of older data from youth who lived under different circumstances,” the researchers emphasized. “Though we can never predict the exact gender trajectory of any child, these data suggest that many youth who identify as transgender early, and are supported through a social transition, will continue to identify as transgender 5 years after initial social transition.” They concluded that more research is needed to determine how best to support initial and later gender transitions in youth.
Study offers support for family discussions
“This study is important to help provide more data regarding the experiences of gender-diverse youth,” M. Brett Cooper, MD, of UT Southwestern Medical Center, Dallas, said in an interview. “The results of a study like this can be used by clinicians to help provide advice and guidance to parents and families as they support their children through their gender journey,” said Dr. Cooper, who was not involved in the study. The current study “also provides evidence to support that persistent, insistent, and consistent youth have an extremely low rate of retransition to a gender that aligns with their sex assigned at birth. This refutes suggestions by politicians and others that those who seek medical care have a high rate of regret or retransition,” Dr. Cooper emphasized.
“I was not surprised at all by their findings,” said Dr. Cooper. “These are very similar to what I have seen in my own panel of gender-diverse patients and what has been seen in other studies,” he noted.
The take-home message of the current study does not suggest any change in clinical practice, Dr. Cooper said. “Guidance already suggests supporting these youth on their gender journey and that for some youth, this may mean retransitioning to identify with their sex assigned at birth,” he explained.
The study was supported in part by grants to the researchers from the National Institutes of Health, the National Science Foundation, the Arcus Foundation, and the MacArthur Foundation. The researchers had no financial conflicts to disclose.
Approximately 7% of youth who chose gender identity social transition in early childhood had retransitioned 5 years later, based on data from 317 individuals.
“Increasing numbers of children are socially transitioning to live in line with their gender identity, rather than the gender assumed by their sex at birth – a process that typically involves changing a child’s pronouns, first name, hairstyle, and clothing,” wrote Kristina R. Olson, PhD, of Princeton (N.J.) University, and colleagues.
The question of whether early childhood social transitions will result in high rates of retransition continues to be a subject for debate, and long-term data on retransition rates and identity outcomes in children who transition are limited, they said.
To examine retransition in early-transitioning children, the researchers identified 317 binary socially transitioned transgender children to participate in a longitudinal study known as the Trans Youth Project (TYP) between July 2013 and December 2017. The study was published in Pediatrics. The mean age at baseline was 8 years. At study entry, participants had to have made a complete binary social transition, including changing their pronouns from those used at birth. During the 5-year follow-up period, children and parents were asked about use of puberty blockers and/or gender-affirming hormones. At study entry, 37 children had begun some type of puberty blockers. A total of 124 children initially socially transitioned before 6 years of age, and 193 initially socially transitioned at 6 years or older.
The study did not evaluate whether the participants met the DSM-5 criteria for gender dysphoria in childhood, the researchers noted. “Based on data collected at their initial visit, we do know that these participants showed signs of gender identification and gender-typed preferences commonly associated with their gender, not their sex assigned at birth,” they wrote.
Participants were classified as binary transgender, nonbinary, or cisgender based on their pronouns at follow-up. Binary transgender pronouns were associated with the other binary assigned sex, nonbinary pronouns were they/them or a mix of they/them and binary pronouns, and cisgender pronouns were those associated with assigned sex.
Overall, 7.3% of the participants had retransitioned at least once by 5 years after their initial binary social transition. The majority (94%) were living as binary transgender youth, including 1.3% who retransitioned to cisgender or nonbinary and then back to binary transgender during the follow-up period. A total of 2.5% were living as cisgender youth and 3.5% were living as nonbinary youth. These rates were similar across the initial population, as well as the 291 participants who continue to be in contact with the researchers, the 200 who had gone at least 5 years since their initial social transition, and the 280 participants who began the study before starting puberty blockers.
The researchers found no differences in retransition rates related to participant sex at birth. Rates of retransition were slightly higher among participants who made their initial social transition before 6 years of age, but these rates were low, the researchers noted.
The study findings were limited by several factors including the use of a volunteer community sample, with the potential for bias that may not generalize to the population at large, the researchers noted. Other limitations included the use of pronouns as the main criteria for retransition, and the classification of a change from binary transgender to nonbinary as a transition, they said. “Many nonbinary people consider themselves to be transgender,” they noted.
“If we had used a stricter criterion of retransition, more similar to the common use of terms like “detransition” or “desistence,” referring only to youth who are living as cisgender, then our retransition rate would have been lower (2.5%),” the researchers explained. Another limitation was the disproportionate number of trans girls, the researchers said. However, because no significant gender effect appeared in terms of retransition rates, “we do not predict any change in pattern of results if we had a different ratio of participants by sex at birth,” they said.
The researchers stated that they intend to follow the cohort through adolescence and into adulthood.
“As more youth are coming out and being supported in their transitions early in development, it is increasingly critical that clinicians understand the experiences of this cohort and not make assumptions about them as a function of older data from youth who lived under different circumstances,” the researchers emphasized. “Though we can never predict the exact gender trajectory of any child, these data suggest that many youth who identify as transgender early, and are supported through a social transition, will continue to identify as transgender 5 years after initial social transition.” They concluded that more research is needed to determine how best to support initial and later gender transitions in youth.
Study offers support for family discussions
“This study is important to help provide more data regarding the experiences of gender-diverse youth,” M. Brett Cooper, MD, of UT Southwestern Medical Center, Dallas, said in an interview. “The results of a study like this can be used by clinicians to help provide advice and guidance to parents and families as they support their children through their gender journey,” said Dr. Cooper, who was not involved in the study. The current study “also provides evidence to support that persistent, insistent, and consistent youth have an extremely low rate of retransition to a gender that aligns with their sex assigned at birth. This refutes suggestions by politicians and others that those who seek medical care have a high rate of regret or retransition,” Dr. Cooper emphasized.
“I was not surprised at all by their findings,” said Dr. Cooper. “These are very similar to what I have seen in my own panel of gender-diverse patients and what has been seen in other studies,” he noted.
The take-home message of the current study does not suggest any change in clinical practice, Dr. Cooper said. “Guidance already suggests supporting these youth on their gender journey and that for some youth, this may mean retransitioning to identify with their sex assigned at birth,” he explained.
The study was supported in part by grants to the researchers from the National Institutes of Health, the National Science Foundation, the Arcus Foundation, and the MacArthur Foundation. The researchers had no financial conflicts to disclose.
Approximately 7% of youth who chose gender identity social transition in early childhood had retransitioned 5 years later, based on data from 317 individuals.
“Increasing numbers of children are socially transitioning to live in line with their gender identity, rather than the gender assumed by their sex at birth – a process that typically involves changing a child’s pronouns, first name, hairstyle, and clothing,” wrote Kristina R. Olson, PhD, of Princeton (N.J.) University, and colleagues.
The question of whether early childhood social transitions will result in high rates of retransition continues to be a subject for debate, and long-term data on retransition rates and identity outcomes in children who transition are limited, they said.
To examine retransition in early-transitioning children, the researchers identified 317 binary socially transitioned transgender children to participate in a longitudinal study known as the Trans Youth Project (TYP) between July 2013 and December 2017. The study was published in Pediatrics. The mean age at baseline was 8 years. At study entry, participants had to have made a complete binary social transition, including changing their pronouns from those used at birth. During the 5-year follow-up period, children and parents were asked about use of puberty blockers and/or gender-affirming hormones. At study entry, 37 children had begun some type of puberty blockers. A total of 124 children initially socially transitioned before 6 years of age, and 193 initially socially transitioned at 6 years or older.
The study did not evaluate whether the participants met the DSM-5 criteria for gender dysphoria in childhood, the researchers noted. “Based on data collected at their initial visit, we do know that these participants showed signs of gender identification and gender-typed preferences commonly associated with their gender, not their sex assigned at birth,” they wrote.
Participants were classified as binary transgender, nonbinary, or cisgender based on their pronouns at follow-up. Binary transgender pronouns were associated with the other binary assigned sex, nonbinary pronouns were they/them or a mix of they/them and binary pronouns, and cisgender pronouns were those associated with assigned sex.
Overall, 7.3% of the participants had retransitioned at least once by 5 years after their initial binary social transition. The majority (94%) were living as binary transgender youth, including 1.3% who retransitioned to cisgender or nonbinary and then back to binary transgender during the follow-up period. A total of 2.5% were living as cisgender youth and 3.5% were living as nonbinary youth. These rates were similar across the initial population, as well as the 291 participants who continue to be in contact with the researchers, the 200 who had gone at least 5 years since their initial social transition, and the 280 participants who began the study before starting puberty blockers.
The researchers found no differences in retransition rates related to participant sex at birth. Rates of retransition were slightly higher among participants who made their initial social transition before 6 years of age, but these rates were low, the researchers noted.
The study findings were limited by several factors including the use of a volunteer community sample, with the potential for bias that may not generalize to the population at large, the researchers noted. Other limitations included the use of pronouns as the main criteria for retransition, and the classification of a change from binary transgender to nonbinary as a transition, they said. “Many nonbinary people consider themselves to be transgender,” they noted.
“If we had used a stricter criterion of retransition, more similar to the common use of terms like “detransition” or “desistence,” referring only to youth who are living as cisgender, then our retransition rate would have been lower (2.5%),” the researchers explained. Another limitation was the disproportionate number of trans girls, the researchers said. However, because no significant gender effect appeared in terms of retransition rates, “we do not predict any change in pattern of results if we had a different ratio of participants by sex at birth,” they said.
The researchers stated that they intend to follow the cohort through adolescence and into adulthood.
“As more youth are coming out and being supported in their transitions early in development, it is increasingly critical that clinicians understand the experiences of this cohort and not make assumptions about them as a function of older data from youth who lived under different circumstances,” the researchers emphasized. “Though we can never predict the exact gender trajectory of any child, these data suggest that many youth who identify as transgender early, and are supported through a social transition, will continue to identify as transgender 5 years after initial social transition.” They concluded that more research is needed to determine how best to support initial and later gender transitions in youth.
Study offers support for family discussions
“This study is important to help provide more data regarding the experiences of gender-diverse youth,” M. Brett Cooper, MD, of UT Southwestern Medical Center, Dallas, said in an interview. “The results of a study like this can be used by clinicians to help provide advice and guidance to parents and families as they support their children through their gender journey,” said Dr. Cooper, who was not involved in the study. The current study “also provides evidence to support that persistent, insistent, and consistent youth have an extremely low rate of retransition to a gender that aligns with their sex assigned at birth. This refutes suggestions by politicians and others that those who seek medical care have a high rate of regret or retransition,” Dr. Cooper emphasized.
“I was not surprised at all by their findings,” said Dr. Cooper. “These are very similar to what I have seen in my own panel of gender-diverse patients and what has been seen in other studies,” he noted.
The take-home message of the current study does not suggest any change in clinical practice, Dr. Cooper said. “Guidance already suggests supporting these youth on their gender journey and that for some youth, this may mean retransitioning to identify with their sex assigned at birth,” he explained.
The study was supported in part by grants to the researchers from the National Institutes of Health, the National Science Foundation, the Arcus Foundation, and the MacArthur Foundation. The researchers had no financial conflicts to disclose.
FROM PEDIATRICS
How gender-affirming care is provided to adolescents in the United States
“Texas investigates parents of transgender teen.” “Court did not force dad to allow chemical castration of son.” Headlines such as these are becoming more common as transgender adolescents and young adults, as well as their families, continue to come under attack from state and local governments. In the 2021 state legislative sessions, more than 100 anti-trans bills were filed across 35 state legislatures. Texas alone saw 13 anti-trans bills, covering everything from sports participation to criminalization of best-practice medical care.1 Many of these bills are introduced under the guise of “protecting” these adolescents and young adults but are detrimental to their health. They also contain descriptions of gender-affirming care that do not reflect the evidence-based standards of care followed by clinicians across the country. Below is scientifically accurate information on gender-affirming care.
Gender identity development
Trajectories of gender identity are diverse. In a large sample of transgender adults (n = 27,715), 10% started to realize they were transgender at age 5 or younger, 16% between ages 6 and 10, 28% between 11 and 15, 29% between 16 and 20, and 18% at age 21 or older.2 In childhood, cross-gender play and preferences are a normal part of gender expression and many gender-nonconforming children will go on to identify with the sex they were assigned at birth (labeled cisgender). However, some children explicitly identify with a gender different than the sex they were assigned at birth (labeled transgender). Children who are consistent, insistent, and persistent in this identity appear likely to remain so into adolescence and adulthood. It is important to note that there is no evidence that discouraging gender nonconformity decreases the likelihood that a child will identify as transgender. In fact, this practice is no longer considered ethical, as it can have damaging effects on self-esteem and mental health. In addition, not all transgender people are noticeably gender nonconforming in childhood and that lack of childhood gender nonconformity does not invalidate someone’s transgender identity.
Gender-affirming care
For youth who identify as transgender, all steps in transition prior to puberty are social. This includes steps like changing hairstyles or clothing and using a different (affirmed) name and/or pronouns. This time period allows youth to explore their gender identity and expression. In one large study of 10,000 LGBTQ youth, among youth who reported “all or most people” used their affirmed pronoun, 12% reported a history of suicide attempt.3 In comparison, among those who reported that “no one” used their affirmed pronoun, the suicide attempt rate was 28%. Further, 14% of youth who reported that they were able to make changes in their clothing and appearance reported a past suicide attempt in comparison to 26% of those who were not able to. Many of these youth also are under the care of mental health professionals during this time.
At the onset of puberty, transgender youth are eligible for medical management, if needed, to address gender dysphoria (i.e., distress with one’s sex characteristics that is consistent and impairing). It is important to recognize that not all people who identify as transgender experience gender dysphoria or desire a medical transition. For those who do seek medical care, puberty must be confirmed either by breast/testicular exam or checking gonadotropin levels. Standards of care suggest that prior to pubertal suppression with GnRH agonists, such as leuprolide or histrelin, adolescents undergo a thorough psychosocial evaluation by a qualified, licensed clinician. After this evaluation, pubertal suppression may be initiated. These adolescents are monitored by their physicians every 3-6 months for side effects and continuing evaluation of their gender identity. GnRH agonists pause any further pubertal development while the adolescent continues to explore his/her/their gender identity. GnRH agonists are fully reversible and if they are stopped, the child’s natal puberty would recommence.
If an adolescent desires to start gender-affirming hormones, these are started as early as age 14, depending on their maturity, when they desire to start, and/or their ability to obtain parental consent. If a patient has not begun GnRH agonists and undergone a previous psychosocial evaluation, a thorough psychosocial evaluation by a qualified, licensed clinician would take place prior to initiating gender-affirming hormones. Prior to initiating hormones, a thorough informed-consent process occurs between the clinician, patient, and family. This process reviews reversible versus irreversible effects, as well of any side effects of the medication(s). Adolescents who begin hormonal treatment are then monitored every 3-6 months for medication side effects, efficacy, satisfaction with treatment, and by continued mental health assessments. Engagement in mental health therapy is not required beyond the initial evaluation (as many adolescents are well adjusted), but it is encouraged for support during the adolescent’s transition.4 It is important to note that the decision to begin hormones, or not, as well as how to adjust dosing over time, is nuanced and is individualized to each patient’s particular goals for his/her/their transition.
Care for transmasculine identified adolescents (those who were assigned female at birth) typically involves testosterone, delivered via subcutaneous injection, transdermal patch, or transdermal gel. Care for transfeminine individuals (those who were assigned male at birth) typically involves estradiol, delivered via daily pill, weekly or twice weekly transdermal patch, or intramuscular injection, as well as an androgen blocker. This is because estradiol by itself is a weak androgen inhibitor. Antiandrogen medication is delivered by daily oral spironolactone, daily oral bicalutamide (an androgen receptor blocker), or GnRH agonists similar to those used for puberty blockade.
Outcomes
At least 13 studies have documented an improvement in gender dysphoria and/or mental health for adolescents and young adults after beginning gender affirming medical care.5 A recent study by Turban et al. showed that access to gender affirming hormones during adolescence or early adulthood was associated with decreased odds of past month suicidal ideation than for those who did not have access to gender-affirming hormones.6 Tordoff et al. found that receipt of gender-affirming care, including medications, led to a 60% decrease in depressive symptoms and a 73% decrease in suicidality.7 One other question that often arises is whether youth who undergo medical treatment for their transition regret their transition or retransition back to the sex they were assigned at birth. In a large study at a gender clinic in the United Kingdom, they found a regret rate of only 0.47% (16 of 3,398 adolescents aged 13-20).8 This is similar to other studies that have also found low rates of regret. Regret is often due to lack of acceptance in society rather than lack of transgender identity.
The care of gender diverse youth takes place on a spectrum, including options that do not include medical treatment. By supporting youth where they are on their gender journey, there is a significant reduction in adverse mental health outcomes. Gender-affirming hormonal treatment is individualized and a thorough multidisciplinary evaluation and informed consent are obtained prior to initiation. There are careful, nuanced discussions with patients and their families to individualize care based on individual goals. By following established evidence-based standards of care, physicians can support their gender-diverse patients throughout their gender journey. Just like other medical treatments, procedures, or surgeries, gender-affirming care should be undertaken in the context of the sacred patient-physician relationship.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Equality Texas. Legislative Bill Tracker.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC: National Center for Transgender Equality.
3. The Trevor Project. 2020. National Survey on LGBTQ Mental Health.
4. Lopez X et al. Curr Opin Pediatrics. 2017;29(4):475-80.
5. Turban J. The evidence for trans youth gender-affirming medical care. Psychology Today. 2022 Jan 24.
6. Turban J et al. Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLOS ONE. 2022;17(1).
7. Tordoff DM et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5(2).
8. Davies S et al. Detransition rates in a national UK gender identity clinic. Inside Matters. On Law, Ethics, and Religion. 2019 Apr 11.
“Texas investigates parents of transgender teen.” “Court did not force dad to allow chemical castration of son.” Headlines such as these are becoming more common as transgender adolescents and young adults, as well as their families, continue to come under attack from state and local governments. In the 2021 state legislative sessions, more than 100 anti-trans bills were filed across 35 state legislatures. Texas alone saw 13 anti-trans bills, covering everything from sports participation to criminalization of best-practice medical care.1 Many of these bills are introduced under the guise of “protecting” these adolescents and young adults but are detrimental to their health. They also contain descriptions of gender-affirming care that do not reflect the evidence-based standards of care followed by clinicians across the country. Below is scientifically accurate information on gender-affirming care.
Gender identity development
Trajectories of gender identity are diverse. In a large sample of transgender adults (n = 27,715), 10% started to realize they were transgender at age 5 or younger, 16% between ages 6 and 10, 28% between 11 and 15, 29% between 16 and 20, and 18% at age 21 or older.2 In childhood, cross-gender play and preferences are a normal part of gender expression and many gender-nonconforming children will go on to identify with the sex they were assigned at birth (labeled cisgender). However, some children explicitly identify with a gender different than the sex they were assigned at birth (labeled transgender). Children who are consistent, insistent, and persistent in this identity appear likely to remain so into adolescence and adulthood. It is important to note that there is no evidence that discouraging gender nonconformity decreases the likelihood that a child will identify as transgender. In fact, this practice is no longer considered ethical, as it can have damaging effects on self-esteem and mental health. In addition, not all transgender people are noticeably gender nonconforming in childhood and that lack of childhood gender nonconformity does not invalidate someone’s transgender identity.
Gender-affirming care
For youth who identify as transgender, all steps in transition prior to puberty are social. This includes steps like changing hairstyles or clothing and using a different (affirmed) name and/or pronouns. This time period allows youth to explore their gender identity and expression. In one large study of 10,000 LGBTQ youth, among youth who reported “all or most people” used their affirmed pronoun, 12% reported a history of suicide attempt.3 In comparison, among those who reported that “no one” used their affirmed pronoun, the suicide attempt rate was 28%. Further, 14% of youth who reported that they were able to make changes in their clothing and appearance reported a past suicide attempt in comparison to 26% of those who were not able to. Many of these youth also are under the care of mental health professionals during this time.
At the onset of puberty, transgender youth are eligible for medical management, if needed, to address gender dysphoria (i.e., distress with one’s sex characteristics that is consistent and impairing). It is important to recognize that not all people who identify as transgender experience gender dysphoria or desire a medical transition. For those who do seek medical care, puberty must be confirmed either by breast/testicular exam or checking gonadotropin levels. Standards of care suggest that prior to pubertal suppression with GnRH agonists, such as leuprolide or histrelin, adolescents undergo a thorough psychosocial evaluation by a qualified, licensed clinician. After this evaluation, pubertal suppression may be initiated. These adolescents are monitored by their physicians every 3-6 months for side effects and continuing evaluation of their gender identity. GnRH agonists pause any further pubertal development while the adolescent continues to explore his/her/their gender identity. GnRH agonists are fully reversible and if they are stopped, the child’s natal puberty would recommence.
If an adolescent desires to start gender-affirming hormones, these are started as early as age 14, depending on their maturity, when they desire to start, and/or their ability to obtain parental consent. If a patient has not begun GnRH agonists and undergone a previous psychosocial evaluation, a thorough psychosocial evaluation by a qualified, licensed clinician would take place prior to initiating gender-affirming hormones. Prior to initiating hormones, a thorough informed-consent process occurs between the clinician, patient, and family. This process reviews reversible versus irreversible effects, as well of any side effects of the medication(s). Adolescents who begin hormonal treatment are then monitored every 3-6 months for medication side effects, efficacy, satisfaction with treatment, and by continued mental health assessments. Engagement in mental health therapy is not required beyond the initial evaluation (as many adolescents are well adjusted), but it is encouraged for support during the adolescent’s transition.4 It is important to note that the decision to begin hormones, or not, as well as how to adjust dosing over time, is nuanced and is individualized to each patient’s particular goals for his/her/their transition.
Care for transmasculine identified adolescents (those who were assigned female at birth) typically involves testosterone, delivered via subcutaneous injection, transdermal patch, or transdermal gel. Care for transfeminine individuals (those who were assigned male at birth) typically involves estradiol, delivered via daily pill, weekly or twice weekly transdermal patch, or intramuscular injection, as well as an androgen blocker. This is because estradiol by itself is a weak androgen inhibitor. Antiandrogen medication is delivered by daily oral spironolactone, daily oral bicalutamide (an androgen receptor blocker), or GnRH agonists similar to those used for puberty blockade.
Outcomes
At least 13 studies have documented an improvement in gender dysphoria and/or mental health for adolescents and young adults after beginning gender affirming medical care.5 A recent study by Turban et al. showed that access to gender affirming hormones during adolescence or early adulthood was associated with decreased odds of past month suicidal ideation than for those who did not have access to gender-affirming hormones.6 Tordoff et al. found that receipt of gender-affirming care, including medications, led to a 60% decrease in depressive symptoms and a 73% decrease in suicidality.7 One other question that often arises is whether youth who undergo medical treatment for their transition regret their transition or retransition back to the sex they were assigned at birth. In a large study at a gender clinic in the United Kingdom, they found a regret rate of only 0.47% (16 of 3,398 adolescents aged 13-20).8 This is similar to other studies that have also found low rates of regret. Regret is often due to lack of acceptance in society rather than lack of transgender identity.
The care of gender diverse youth takes place on a spectrum, including options that do not include medical treatment. By supporting youth where they are on their gender journey, there is a significant reduction in adverse mental health outcomes. Gender-affirming hormonal treatment is individualized and a thorough multidisciplinary evaluation and informed consent are obtained prior to initiation. There are careful, nuanced discussions with patients and their families to individualize care based on individual goals. By following established evidence-based standards of care, physicians can support their gender-diverse patients throughout their gender journey. Just like other medical treatments, procedures, or surgeries, gender-affirming care should be undertaken in the context of the sacred patient-physician relationship.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Equality Texas. Legislative Bill Tracker.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC: National Center for Transgender Equality.
3. The Trevor Project. 2020. National Survey on LGBTQ Mental Health.
4. Lopez X et al. Curr Opin Pediatrics. 2017;29(4):475-80.
5. Turban J. The evidence for trans youth gender-affirming medical care. Psychology Today. 2022 Jan 24.
6. Turban J et al. Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLOS ONE. 2022;17(1).
7. Tordoff DM et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5(2).
8. Davies S et al. Detransition rates in a national UK gender identity clinic. Inside Matters. On Law, Ethics, and Religion. 2019 Apr 11.
“Texas investigates parents of transgender teen.” “Court did not force dad to allow chemical castration of son.” Headlines such as these are becoming more common as transgender adolescents and young adults, as well as their families, continue to come under attack from state and local governments. In the 2021 state legislative sessions, more than 100 anti-trans bills were filed across 35 state legislatures. Texas alone saw 13 anti-trans bills, covering everything from sports participation to criminalization of best-practice medical care.1 Many of these bills are introduced under the guise of “protecting” these adolescents and young adults but are detrimental to their health. They also contain descriptions of gender-affirming care that do not reflect the evidence-based standards of care followed by clinicians across the country. Below is scientifically accurate information on gender-affirming care.
Gender identity development
Trajectories of gender identity are diverse. In a large sample of transgender adults (n = 27,715), 10% started to realize they were transgender at age 5 or younger, 16% between ages 6 and 10, 28% between 11 and 15, 29% between 16 and 20, and 18% at age 21 or older.2 In childhood, cross-gender play and preferences are a normal part of gender expression and many gender-nonconforming children will go on to identify with the sex they were assigned at birth (labeled cisgender). However, some children explicitly identify with a gender different than the sex they were assigned at birth (labeled transgender). Children who are consistent, insistent, and persistent in this identity appear likely to remain so into adolescence and adulthood. It is important to note that there is no evidence that discouraging gender nonconformity decreases the likelihood that a child will identify as transgender. In fact, this practice is no longer considered ethical, as it can have damaging effects on self-esteem and mental health. In addition, not all transgender people are noticeably gender nonconforming in childhood and that lack of childhood gender nonconformity does not invalidate someone’s transgender identity.
Gender-affirming care
For youth who identify as transgender, all steps in transition prior to puberty are social. This includes steps like changing hairstyles or clothing and using a different (affirmed) name and/or pronouns. This time period allows youth to explore their gender identity and expression. In one large study of 10,000 LGBTQ youth, among youth who reported “all or most people” used their affirmed pronoun, 12% reported a history of suicide attempt.3 In comparison, among those who reported that “no one” used their affirmed pronoun, the suicide attempt rate was 28%. Further, 14% of youth who reported that they were able to make changes in their clothing and appearance reported a past suicide attempt in comparison to 26% of those who were not able to. Many of these youth also are under the care of mental health professionals during this time.
At the onset of puberty, transgender youth are eligible for medical management, if needed, to address gender dysphoria (i.e., distress with one’s sex characteristics that is consistent and impairing). It is important to recognize that not all people who identify as transgender experience gender dysphoria or desire a medical transition. For those who do seek medical care, puberty must be confirmed either by breast/testicular exam or checking gonadotropin levels. Standards of care suggest that prior to pubertal suppression with GnRH agonists, such as leuprolide or histrelin, adolescents undergo a thorough psychosocial evaluation by a qualified, licensed clinician. After this evaluation, pubertal suppression may be initiated. These adolescents are monitored by their physicians every 3-6 months for side effects and continuing evaluation of their gender identity. GnRH agonists pause any further pubertal development while the adolescent continues to explore his/her/their gender identity. GnRH agonists are fully reversible and if they are stopped, the child’s natal puberty would recommence.
If an adolescent desires to start gender-affirming hormones, these are started as early as age 14, depending on their maturity, when they desire to start, and/or their ability to obtain parental consent. If a patient has not begun GnRH agonists and undergone a previous psychosocial evaluation, a thorough psychosocial evaluation by a qualified, licensed clinician would take place prior to initiating gender-affirming hormones. Prior to initiating hormones, a thorough informed-consent process occurs between the clinician, patient, and family. This process reviews reversible versus irreversible effects, as well of any side effects of the medication(s). Adolescents who begin hormonal treatment are then monitored every 3-6 months for medication side effects, efficacy, satisfaction with treatment, and by continued mental health assessments. Engagement in mental health therapy is not required beyond the initial evaluation (as many adolescents are well adjusted), but it is encouraged for support during the adolescent’s transition.4 It is important to note that the decision to begin hormones, or not, as well as how to adjust dosing over time, is nuanced and is individualized to each patient’s particular goals for his/her/their transition.
Care for transmasculine identified adolescents (those who were assigned female at birth) typically involves testosterone, delivered via subcutaneous injection, transdermal patch, or transdermal gel. Care for transfeminine individuals (those who were assigned male at birth) typically involves estradiol, delivered via daily pill, weekly or twice weekly transdermal patch, or intramuscular injection, as well as an androgen blocker. This is because estradiol by itself is a weak androgen inhibitor. Antiandrogen medication is delivered by daily oral spironolactone, daily oral bicalutamide (an androgen receptor blocker), or GnRH agonists similar to those used for puberty blockade.
Outcomes
At least 13 studies have documented an improvement in gender dysphoria and/or mental health for adolescents and young adults after beginning gender affirming medical care.5 A recent study by Turban et al. showed that access to gender affirming hormones during adolescence or early adulthood was associated with decreased odds of past month suicidal ideation than for those who did not have access to gender-affirming hormones.6 Tordoff et al. found that receipt of gender-affirming care, including medications, led to a 60% decrease in depressive symptoms and a 73% decrease in suicidality.7 One other question that often arises is whether youth who undergo medical treatment for their transition regret their transition or retransition back to the sex they were assigned at birth. In a large study at a gender clinic in the United Kingdom, they found a regret rate of only 0.47% (16 of 3,398 adolescents aged 13-20).8 This is similar to other studies that have also found low rates of regret. Regret is often due to lack of acceptance in society rather than lack of transgender identity.
The care of gender diverse youth takes place on a spectrum, including options that do not include medical treatment. By supporting youth where they are on their gender journey, there is a significant reduction in adverse mental health outcomes. Gender-affirming hormonal treatment is individualized and a thorough multidisciplinary evaluation and informed consent are obtained prior to initiation. There are careful, nuanced discussions with patients and their families to individualize care based on individual goals. By following established evidence-based standards of care, physicians can support their gender-diverse patients throughout their gender journey. Just like other medical treatments, procedures, or surgeries, gender-affirming care should be undertaken in the context of the sacred patient-physician relationship.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Equality Texas. Legislative Bill Tracker.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC: National Center for Transgender Equality.
3. The Trevor Project. 2020. National Survey on LGBTQ Mental Health.
4. Lopez X et al. Curr Opin Pediatrics. 2017;29(4):475-80.
5. Turban J. The evidence for trans youth gender-affirming medical care. Psychology Today. 2022 Jan 24.
6. Turban J et al. Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLOS ONE. 2022;17(1).
7. Tordoff DM et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5(2).
8. Davies S et al. Detransition rates in a national UK gender identity clinic. Inside Matters. On Law, Ethics, and Religion. 2019 Apr 11.
Trans women in female sports: A sports scientist’s take
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
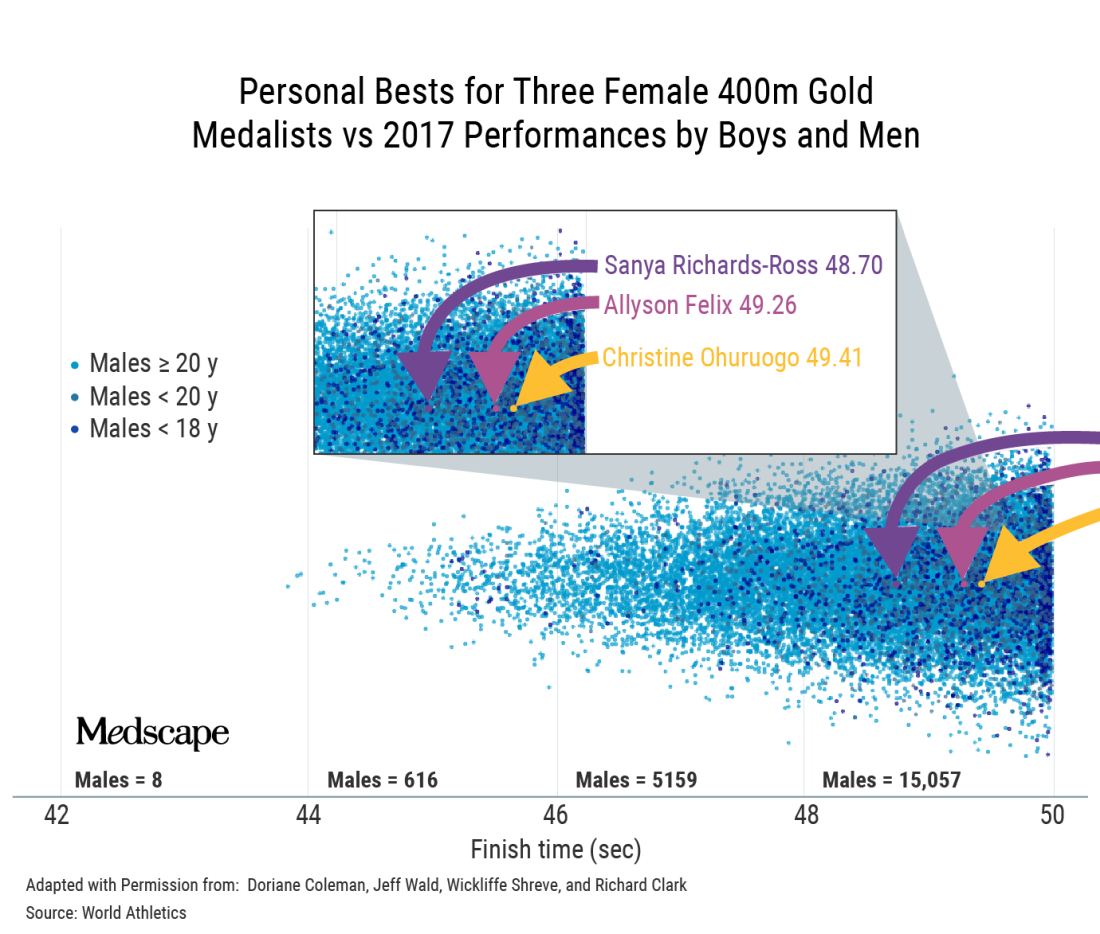
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
An interview with Ross Tucker, PhD
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
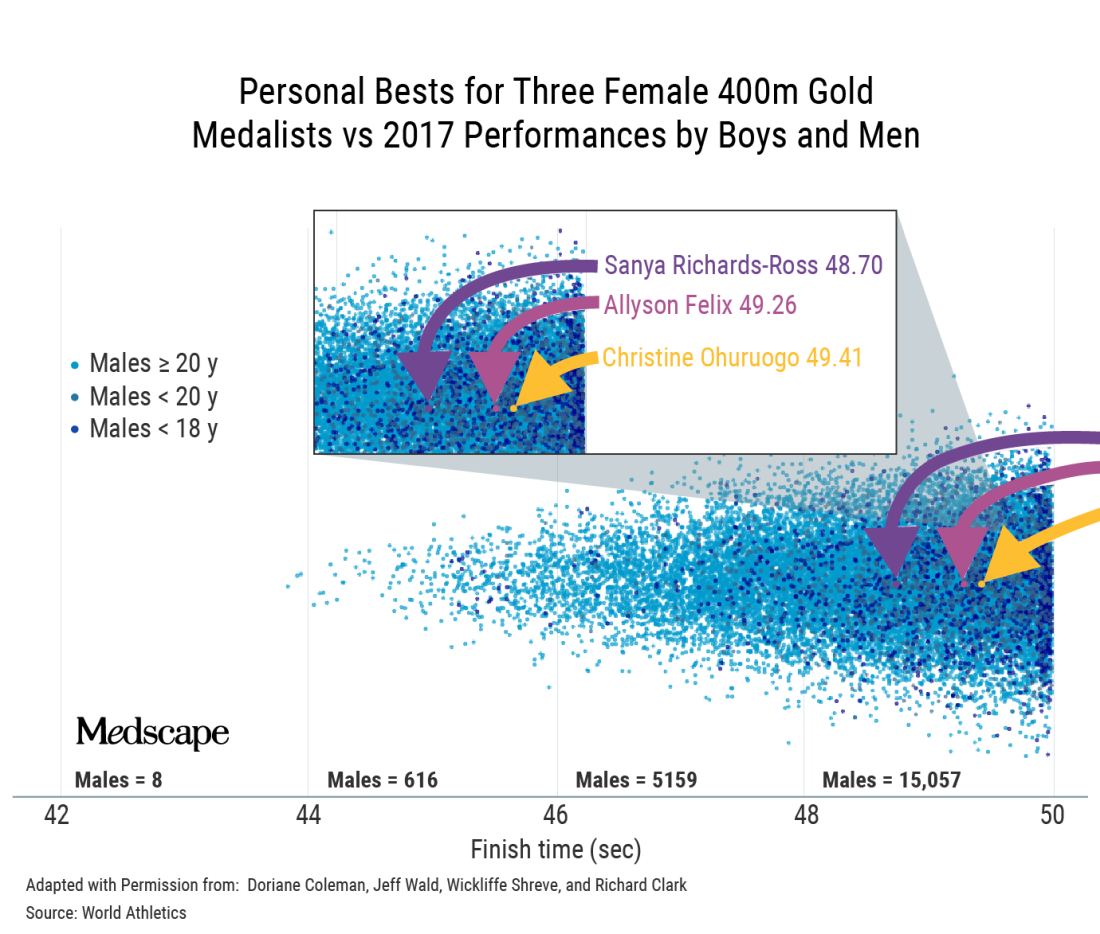
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
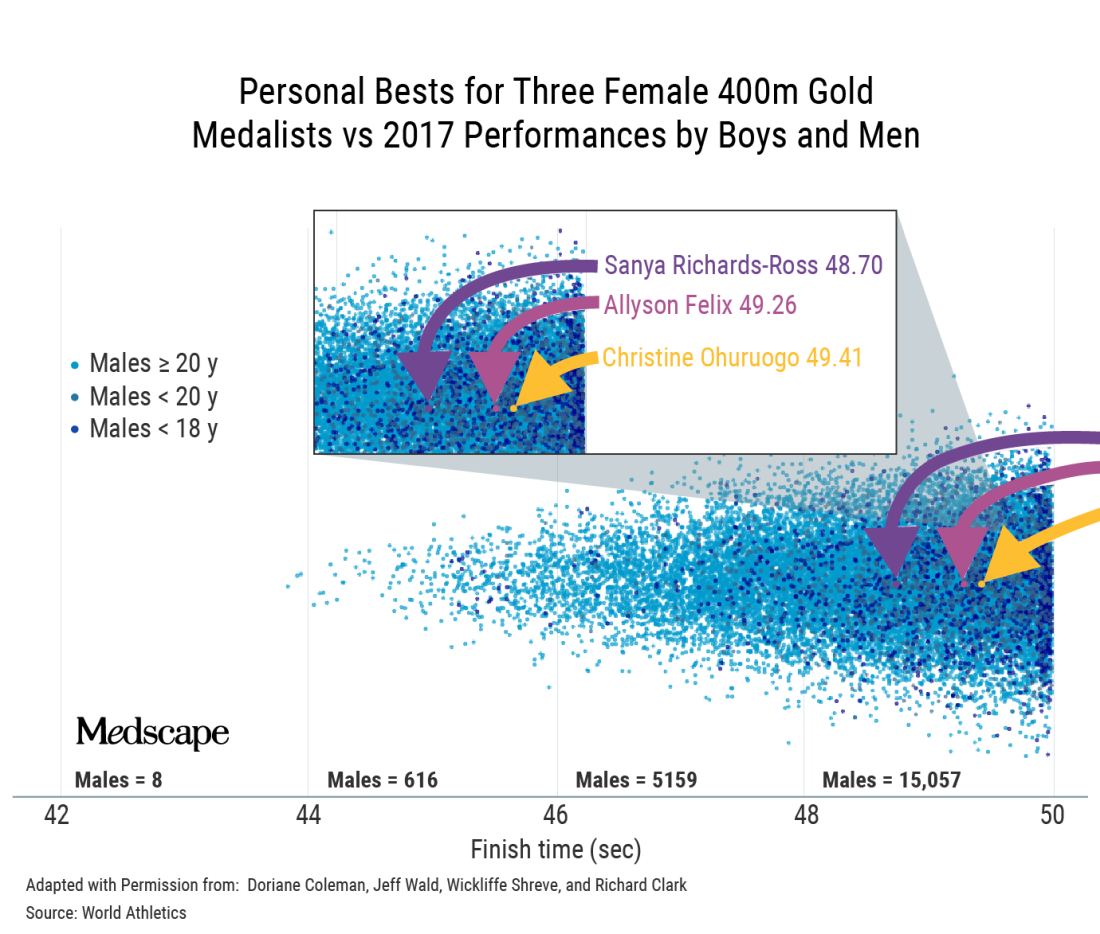
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
Breast anatomy and augmentation in transfeminine individuals
Augmentation mammaplasty, otherwise known as a breast augmentation, is one of the most common cosmetic procedures performed in cisgender females. Gynecologists routinely perform annual breast examinations and order screening mammography in cisgender women with breast implants. Similarly, there is an increasing number of transgender women seeking breast augmentation – with approximately 60%-70% of patients having desired or undergone the procedure.1 Consequently, these patients are instructed by their surgeons to follow up with gynecologists for annual examinations and screening. While there are many similarities in technique and procedure, there are nuances in patient demographics, anatomy, and surgical technique that obstetricians/gynecologists should be aware of when examining these patients or prior to referring them to a surgeon for augmentation.2
Many patients who are dissatisfied with breast size from hormone therapy alone will seek out augmentation mammaplasty. In patients taking estrogen for hormone therapy, breast growth will commence around 2-3 months and peak over 1-2 years.3 Unlike chest surgery for transmasculine individuals, it is recommended that transfeminine patients seeking breast augmentation wait a minimum of 12 months before to surgery to allow for maximum breast enlargement. As with breast growth in cisgender females, the extent of breast development is multifactorial and varies from individual to individual. Current literature does not suggest that estrogen type or dose affects the ultimate breast size; however, younger age, tissue sensitivity, and body weight may affect breast volume.3 Referral to a genetic counselor and preoperative imaging may be necessary if a patient has a history concerning for a genetic or familial predisposition to breast cancer.
Implant selection and placement is determined by a variety of factors. While the overall principles of augmentation mammaplasty are essentially the same, there are anatomic differences in transfeminine patients that surgeons must take into consideration at the time of the consultation and during the surgery itself. For example, the pectoralis major muscle is more defined, there is a longer sternal notch-to-nipple distance, the chest wall is broader and more barrel-shaped, and there is a shorter distance between the nipple and the inframammary crease.2-4 As a result of the broader chest wall, it is extremely difficult to achieve central cleavage even with larger implant selection. The surgeon must also ensure that the nipple and areola overlie the implant centrally. Medial placement of the implant will result in lateral displacement of the nipples, which can have an unsatisfactory cosmetic appearance.
Incision location can be axillary, inframammary, or even transareolar, although the latter is less common due to the smaller areolar size and larger implant choice.3 If the inframammary incision is used, it should be placed lower than the natural inframammary fold because the distance between the inferior areolar margin and inframammary fold is shorter and will expand after the implant is placed.4 While both saline and silicone implants are available, many surgeons (myself included), favor more form-stable silicone implants. Given the association between anaplastic large-cell lymphoma and textured implants, many surgeons also use nontextured, or smooth, cohesive gel silicone implants.5
Pocket selection of the implant itself can be subglandular – directly under the breast mound – or subpectoral – behind the pectoralis muscle. For patients with a pinch test of greater than 1.5 cm (outside of the area of the breast bud), good skin softening, and marked pectoralis hypertrophy, subglandular placement is reasonable.6 In thin patients with minimal breast development, subglandular placement can result in a “double-mound” appearance and can lead to visible implant edges on the periphery.6 Use of the subpectoral plane is more common and is associated with less implant visibility due to an increased amount of soft-tissue coverage and has lower rates of capsular contracture.4 However, due to the more robust pectoralis muscle in transfeminine patients, implant displacement can occur more frequently compared to subglandular placement. The surgeon and patient must have a thorough discussion about the location of the incision, implant material, and pocket placement along with the benefits and complications of the surgical plan.
Complications of augmentation mammaplasty are rare. However, when they occur it can include capsular contracture, breast asymmetry, hematoma formation, loss of nipple sensation, implant malposition, implant displacement below the inframammary crease, implant rupture, and need for revisional surgery.7 If an obstetrician/gynecologist observes any of the aforementioned findings in a postoperative patient, consultation and referral to a plastic surgeon is imperative.
Postoperative assessment and screening are mandatory in all patients who undergo breast augmentation. It is important for the gynecologist to note the incision placement, know the type of implant used (saline or silicone), and delineate where the implant was placed. If silicone implants are used, breast MRI is more sensitive in detecting implant rupture compared to mammography alone. Given the relatively poor epidemiologic data on breast cancer in transgender women, the Endocrine Society recommends that these patients follow the same screening guidelines as cisgender women.4,6
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Wierckx K et al. J Sex Med. 2014;11(5):1240-7.
2. Mehra G et al. Plast Reconstr Surg Glob Open 2021 Jan 21;9(1):e3362. doi: 10.1097/GOX.0000000000003362.
3. Schecter LS, Schechter RB. Breast and chest surgery for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia, PA: Elsevier, 2020:73-81.
4. Colebunders B et al. Top surgery. In: Salgado CJ et al. ed. Gender Affirmation: Medical and Surgical Perspectives. New York, NY: Thieme, 2017:51-66.
5. De Boer M et al. Aesthet Surg J. 2017;37:NP83-NP87.
6. Coon D et al. Plast Reconstr Surg. 2020 Jun;145(6):1343-53.
7. Kanhai RC et al. Br J Plast Surg. 2000;53:209-11.
Augmentation mammaplasty, otherwise known as a breast augmentation, is one of the most common cosmetic procedures performed in cisgender females. Gynecologists routinely perform annual breast examinations and order screening mammography in cisgender women with breast implants. Similarly, there is an increasing number of transgender women seeking breast augmentation – with approximately 60%-70% of patients having desired or undergone the procedure.1 Consequently, these patients are instructed by their surgeons to follow up with gynecologists for annual examinations and screening. While there are many similarities in technique and procedure, there are nuances in patient demographics, anatomy, and surgical technique that obstetricians/gynecologists should be aware of when examining these patients or prior to referring them to a surgeon for augmentation.2
Many patients who are dissatisfied with breast size from hormone therapy alone will seek out augmentation mammaplasty. In patients taking estrogen for hormone therapy, breast growth will commence around 2-3 months and peak over 1-2 years.3 Unlike chest surgery for transmasculine individuals, it is recommended that transfeminine patients seeking breast augmentation wait a minimum of 12 months before to surgery to allow for maximum breast enlargement. As with breast growth in cisgender females, the extent of breast development is multifactorial and varies from individual to individual. Current literature does not suggest that estrogen type or dose affects the ultimate breast size; however, younger age, tissue sensitivity, and body weight may affect breast volume.3 Referral to a genetic counselor and preoperative imaging may be necessary if a patient has a history concerning for a genetic or familial predisposition to breast cancer.
Implant selection and placement is determined by a variety of factors. While the overall principles of augmentation mammaplasty are essentially the same, there are anatomic differences in transfeminine patients that surgeons must take into consideration at the time of the consultation and during the surgery itself. For example, the pectoralis major muscle is more defined, there is a longer sternal notch-to-nipple distance, the chest wall is broader and more barrel-shaped, and there is a shorter distance between the nipple and the inframammary crease.2-4 As a result of the broader chest wall, it is extremely difficult to achieve central cleavage even with larger implant selection. The surgeon must also ensure that the nipple and areola overlie the implant centrally. Medial placement of the implant will result in lateral displacement of the nipples, which can have an unsatisfactory cosmetic appearance.
Incision location can be axillary, inframammary, or even transareolar, although the latter is less common due to the smaller areolar size and larger implant choice.3 If the inframammary incision is used, it should be placed lower than the natural inframammary fold because the distance between the inferior areolar margin and inframammary fold is shorter and will expand after the implant is placed.4 While both saline and silicone implants are available, many surgeons (myself included), favor more form-stable silicone implants. Given the association between anaplastic large-cell lymphoma and textured implants, many surgeons also use nontextured, or smooth, cohesive gel silicone implants.5
Pocket selection of the implant itself can be subglandular – directly under the breast mound – or subpectoral – behind the pectoralis muscle. For patients with a pinch test of greater than 1.5 cm (outside of the area of the breast bud), good skin softening, and marked pectoralis hypertrophy, subglandular placement is reasonable.6 In thin patients with minimal breast development, subglandular placement can result in a “double-mound” appearance and can lead to visible implant edges on the periphery.6 Use of the subpectoral plane is more common and is associated with less implant visibility due to an increased amount of soft-tissue coverage and has lower rates of capsular contracture.4 However, due to the more robust pectoralis muscle in transfeminine patients, implant displacement can occur more frequently compared to subglandular placement. The surgeon and patient must have a thorough discussion about the location of the incision, implant material, and pocket placement along with the benefits and complications of the surgical plan.
Complications of augmentation mammaplasty are rare. However, when they occur it can include capsular contracture, breast asymmetry, hematoma formation, loss of nipple sensation, implant malposition, implant displacement below the inframammary crease, implant rupture, and need for revisional surgery.7 If an obstetrician/gynecologist observes any of the aforementioned findings in a postoperative patient, consultation and referral to a plastic surgeon is imperative.
Postoperative assessment and screening are mandatory in all patients who undergo breast augmentation. It is important for the gynecologist to note the incision placement, know the type of implant used (saline or silicone), and delineate where the implant was placed. If silicone implants are used, breast MRI is more sensitive in detecting implant rupture compared to mammography alone. Given the relatively poor epidemiologic data on breast cancer in transgender women, the Endocrine Society recommends that these patients follow the same screening guidelines as cisgender women.4,6
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Wierckx K et al. J Sex Med. 2014;11(5):1240-7.
2. Mehra G et al. Plast Reconstr Surg Glob Open 2021 Jan 21;9(1):e3362. doi: 10.1097/GOX.0000000000003362.
3. Schecter LS, Schechter RB. Breast and chest surgery for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia, PA: Elsevier, 2020:73-81.
4. Colebunders B et al. Top surgery. In: Salgado CJ et al. ed. Gender Affirmation: Medical and Surgical Perspectives. New York, NY: Thieme, 2017:51-66.
5. De Boer M et al. Aesthet Surg J. 2017;37:NP83-NP87.
6. Coon D et al. Plast Reconstr Surg. 2020 Jun;145(6):1343-53.
7. Kanhai RC et al. Br J Plast Surg. 2000;53:209-11.
Augmentation mammaplasty, otherwise known as a breast augmentation, is one of the most common cosmetic procedures performed in cisgender females. Gynecologists routinely perform annual breast examinations and order screening mammography in cisgender women with breast implants. Similarly, there is an increasing number of transgender women seeking breast augmentation – with approximately 60%-70% of patients having desired or undergone the procedure.1 Consequently, these patients are instructed by their surgeons to follow up with gynecologists for annual examinations and screening. While there are many similarities in technique and procedure, there are nuances in patient demographics, anatomy, and surgical technique that obstetricians/gynecologists should be aware of when examining these patients or prior to referring them to a surgeon for augmentation.2
Many patients who are dissatisfied with breast size from hormone therapy alone will seek out augmentation mammaplasty. In patients taking estrogen for hormone therapy, breast growth will commence around 2-3 months and peak over 1-2 years.3 Unlike chest surgery for transmasculine individuals, it is recommended that transfeminine patients seeking breast augmentation wait a minimum of 12 months before to surgery to allow for maximum breast enlargement. As with breast growth in cisgender females, the extent of breast development is multifactorial and varies from individual to individual. Current literature does not suggest that estrogen type or dose affects the ultimate breast size; however, younger age, tissue sensitivity, and body weight may affect breast volume.3 Referral to a genetic counselor and preoperative imaging may be necessary if a patient has a history concerning for a genetic or familial predisposition to breast cancer.
Implant selection and placement is determined by a variety of factors. While the overall principles of augmentation mammaplasty are essentially the same, there are anatomic differences in transfeminine patients that surgeons must take into consideration at the time of the consultation and during the surgery itself. For example, the pectoralis major muscle is more defined, there is a longer sternal notch-to-nipple distance, the chest wall is broader and more barrel-shaped, and there is a shorter distance between the nipple and the inframammary crease.2-4 As a result of the broader chest wall, it is extremely difficult to achieve central cleavage even with larger implant selection. The surgeon must also ensure that the nipple and areola overlie the implant centrally. Medial placement of the implant will result in lateral displacement of the nipples, which can have an unsatisfactory cosmetic appearance.
Incision location can be axillary, inframammary, or even transareolar, although the latter is less common due to the smaller areolar size and larger implant choice.3 If the inframammary incision is used, it should be placed lower than the natural inframammary fold because the distance between the inferior areolar margin and inframammary fold is shorter and will expand after the implant is placed.4 While both saline and silicone implants are available, many surgeons (myself included), favor more form-stable silicone implants. Given the association between anaplastic large-cell lymphoma and textured implants, many surgeons also use nontextured, or smooth, cohesive gel silicone implants.5
Pocket selection of the implant itself can be subglandular – directly under the breast mound – or subpectoral – behind the pectoralis muscle. For patients with a pinch test of greater than 1.5 cm (outside of the area of the breast bud), good skin softening, and marked pectoralis hypertrophy, subglandular placement is reasonable.6 In thin patients with minimal breast development, subglandular placement can result in a “double-mound” appearance and can lead to visible implant edges on the periphery.6 Use of the subpectoral plane is more common and is associated with less implant visibility due to an increased amount of soft-tissue coverage and has lower rates of capsular contracture.4 However, due to the more robust pectoralis muscle in transfeminine patients, implant displacement can occur more frequently compared to subglandular placement. The surgeon and patient must have a thorough discussion about the location of the incision, implant material, and pocket placement along with the benefits and complications of the surgical plan.
Complications of augmentation mammaplasty are rare. However, when they occur it can include capsular contracture, breast asymmetry, hematoma formation, loss of nipple sensation, implant malposition, implant displacement below the inframammary crease, implant rupture, and need for revisional surgery.7 If an obstetrician/gynecologist observes any of the aforementioned findings in a postoperative patient, consultation and referral to a plastic surgeon is imperative.
Postoperative assessment and screening are mandatory in all patients who undergo breast augmentation. It is important for the gynecologist to note the incision placement, know the type of implant used (saline or silicone), and delineate where the implant was placed. If silicone implants are used, breast MRI is more sensitive in detecting implant rupture compared to mammography alone. Given the relatively poor epidemiologic data on breast cancer in transgender women, the Endocrine Society recommends that these patients follow the same screening guidelines as cisgender women.4,6
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Wierckx K et al. J Sex Med. 2014;11(5):1240-7.
2. Mehra G et al. Plast Reconstr Surg Glob Open 2021 Jan 21;9(1):e3362. doi: 10.1097/GOX.0000000000003362.
3. Schecter LS, Schechter RB. Breast and chest surgery for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia, PA: Elsevier, 2020:73-81.
4. Colebunders B et al. Top surgery. In: Salgado CJ et al. ed. Gender Affirmation: Medical and Surgical Perspectives. New York, NY: Thieme, 2017:51-66.
5. De Boer M et al. Aesthet Surg J. 2017;37:NP83-NP87.
6. Coon D et al. Plast Reconstr Surg. 2020 Jun;145(6):1343-53.
7. Kanhai RC et al. Br J Plast Surg. 2000;53:209-11.
More medical schools build training in transgender care
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Transgender youth: Bringing evidence to the political debates
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.








