User login
Antibiotics use and vaccine antibody levels
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).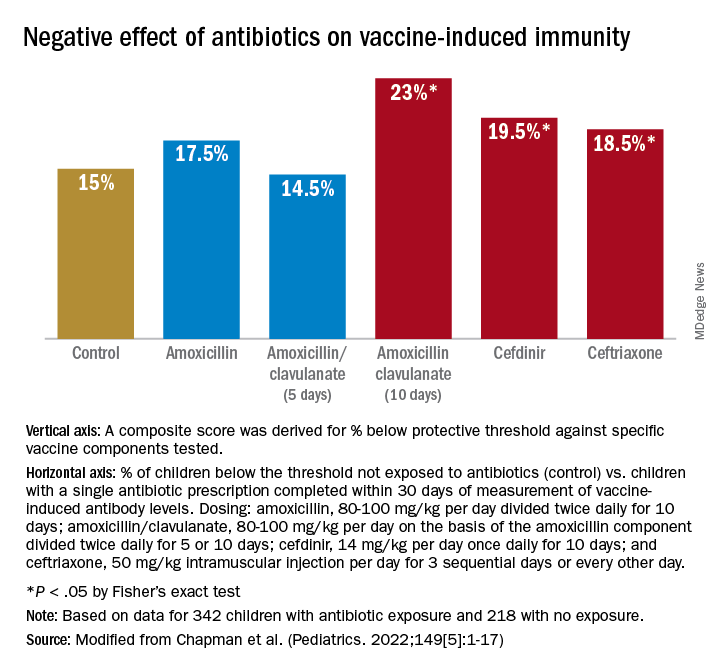
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).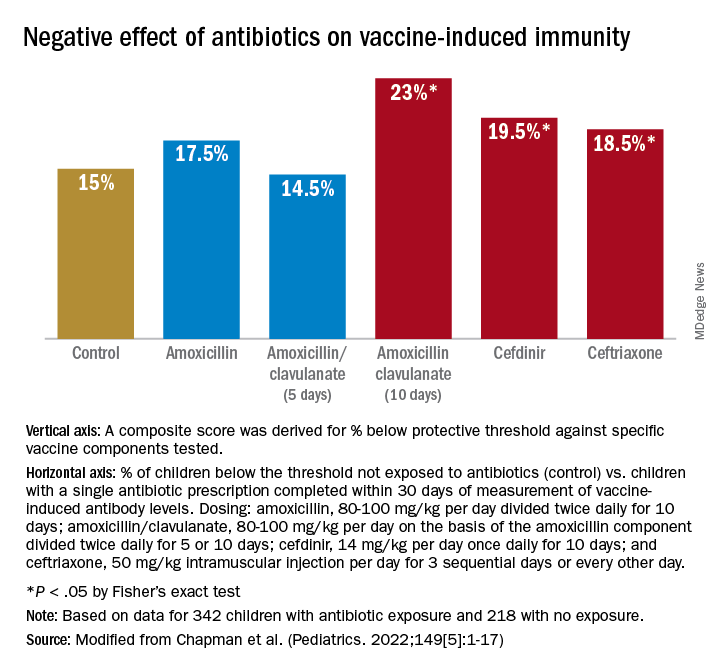
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).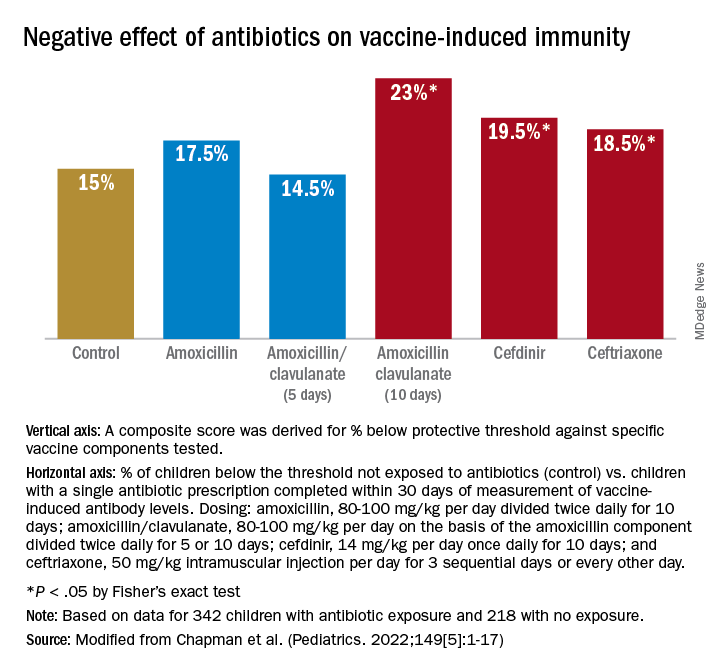
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
Kindergarten vaccination rates dip below 95% target
Vaccination rates among kindergartners in the United States dipped below the Healthy People 2030 target of 95% in 2020-2021, according to the latest figures from the Centers for Disease Control and Prevention.
Data from 47 states and the District of Columbia, reported in the Morbidity and Mortality Weekly Report, showed the rates dipped by about 1 percentage point, compared with the previous school year for state-required vaccines. Coverage nationally was 93.9% for two doses of the MMR vaccine, 93.6% for the required number of doses of DTaP, and 93.6% for the state-required doses of varicella vaccine.
“This might not sound like much,” Georgina Peacock, MD, MPH, acting director of CDC’s immunization services division said in a press briefing. “But it amounts to at least 35,000 more children across the United States that entered kindergarten without documentation of complete vaccination against common diseases like measles, whooping cough, and chickenpox.”
The report authors, led by Ranee Seither, MPH, with the immunization services division of the CDC’s National Center for Immunization and Respiratory Diseases, said the COVID-19 pandemic played a large part in the dip as children missed doctors’ appointments and states relaxed requirements with remote instruction.
States reported reluctance by parents to schedule well-child appointments and reduced access to office visits as well as longer grace periods or provisional enrollment. There was also less submission of documentation by parents, less time for school nurses to follow-up with students to document vaccines, fewer staff members to conduct kindergarten vaccination coverage assessment, lower response rates from schools, and both extended and compressed kindergarten vaccination coverage data collection schedules.
“There’s a greater proportion of parents who are questioning routine vaccines,” Jason V. Terk, MD, a Texas pediatrician and a spokesman for the American Academy of Pediatrics, told the New York Times. He said misinformation “fed the fire of distrust and skepticism that is really sort of the new pandemic of hesitancy for routine vaccines.”
The authors of the CDC report wrote: “As schools continue to return to in-person learning, enforcement of vaccination policies and follow-up with undervaccinated students are important to improve vaccination coverage.”
They urged schools and immunization programs to reach out to first-time students, including kindergartners and first-graders, and follow up with undervaccinated students.
The rate of people having an exemption from at least one vaccine remained low at 2.2% and the percentage of children with exemptions decreased in 37 states. However, an additional 3.9% who did not have a vaccine exemption were not up to date for MMR, according to the report.
Mississippi and New York had the smallest percentage of exemptions (0.1%) and Idaho had the most (8.2%). In the 2019-2020 school year, 2.5% reported an exemption from at least one vaccine. Nationally, 0.2% of kindergartners had a medical exemption and 1.9% had a nonmedical exemption.
Vaccination rates also differed among states. The New York Times noted that Maryland had a 10% drop in MMR vaccine coverage, while Wisconsin, Georgia, Wyoming, and Kentucky had declines of about 5%.
Among states reporting the measures in 2020-2021, the proportion of kindergartners attending school with no documentation of required vaccinations or exemptions ranged from 0.1% (Pennsylvania and Virginia) to 8.3% (Maryland). The state with the lowest proportion of kindergarteners out of compliance was Florida (0.2%) and Indiana had the highest out-of-compliance rate at 16.6%.
Comparing states’ performance is difficult, the authors noted, because they vary as to which vaccine and number of doses they require and by what date and what documentation they require. They also vary by data collection methods; exemptions allowed; grace period rules and provisional enrollment.
The authors, Dr. Peacock, and Dr. Terk reported no relevant financial disclosures.
Vaccination rates among kindergartners in the United States dipped below the Healthy People 2030 target of 95% in 2020-2021, according to the latest figures from the Centers for Disease Control and Prevention.
Data from 47 states and the District of Columbia, reported in the Morbidity and Mortality Weekly Report, showed the rates dipped by about 1 percentage point, compared with the previous school year for state-required vaccines. Coverage nationally was 93.9% for two doses of the MMR vaccine, 93.6% for the required number of doses of DTaP, and 93.6% for the state-required doses of varicella vaccine.
“This might not sound like much,” Georgina Peacock, MD, MPH, acting director of CDC’s immunization services division said in a press briefing. “But it amounts to at least 35,000 more children across the United States that entered kindergarten without documentation of complete vaccination against common diseases like measles, whooping cough, and chickenpox.”
The report authors, led by Ranee Seither, MPH, with the immunization services division of the CDC’s National Center for Immunization and Respiratory Diseases, said the COVID-19 pandemic played a large part in the dip as children missed doctors’ appointments and states relaxed requirements with remote instruction.
States reported reluctance by parents to schedule well-child appointments and reduced access to office visits as well as longer grace periods or provisional enrollment. There was also less submission of documentation by parents, less time for school nurses to follow-up with students to document vaccines, fewer staff members to conduct kindergarten vaccination coverage assessment, lower response rates from schools, and both extended and compressed kindergarten vaccination coverage data collection schedules.
“There’s a greater proportion of parents who are questioning routine vaccines,” Jason V. Terk, MD, a Texas pediatrician and a spokesman for the American Academy of Pediatrics, told the New York Times. He said misinformation “fed the fire of distrust and skepticism that is really sort of the new pandemic of hesitancy for routine vaccines.”
The authors of the CDC report wrote: “As schools continue to return to in-person learning, enforcement of vaccination policies and follow-up with undervaccinated students are important to improve vaccination coverage.”
They urged schools and immunization programs to reach out to first-time students, including kindergartners and first-graders, and follow up with undervaccinated students.
The rate of people having an exemption from at least one vaccine remained low at 2.2% and the percentage of children with exemptions decreased in 37 states. However, an additional 3.9% who did not have a vaccine exemption were not up to date for MMR, according to the report.
Mississippi and New York had the smallest percentage of exemptions (0.1%) and Idaho had the most (8.2%). In the 2019-2020 school year, 2.5% reported an exemption from at least one vaccine. Nationally, 0.2% of kindergartners had a medical exemption and 1.9% had a nonmedical exemption.
Vaccination rates also differed among states. The New York Times noted that Maryland had a 10% drop in MMR vaccine coverage, while Wisconsin, Georgia, Wyoming, and Kentucky had declines of about 5%.
Among states reporting the measures in 2020-2021, the proportion of kindergartners attending school with no documentation of required vaccinations or exemptions ranged from 0.1% (Pennsylvania and Virginia) to 8.3% (Maryland). The state with the lowest proportion of kindergarteners out of compliance was Florida (0.2%) and Indiana had the highest out-of-compliance rate at 16.6%.
Comparing states’ performance is difficult, the authors noted, because they vary as to which vaccine and number of doses they require and by what date and what documentation they require. They also vary by data collection methods; exemptions allowed; grace period rules and provisional enrollment.
The authors, Dr. Peacock, and Dr. Terk reported no relevant financial disclosures.
Vaccination rates among kindergartners in the United States dipped below the Healthy People 2030 target of 95% in 2020-2021, according to the latest figures from the Centers for Disease Control and Prevention.
Data from 47 states and the District of Columbia, reported in the Morbidity and Mortality Weekly Report, showed the rates dipped by about 1 percentage point, compared with the previous school year for state-required vaccines. Coverage nationally was 93.9% for two doses of the MMR vaccine, 93.6% for the required number of doses of DTaP, and 93.6% for the state-required doses of varicella vaccine.
“This might not sound like much,” Georgina Peacock, MD, MPH, acting director of CDC’s immunization services division said in a press briefing. “But it amounts to at least 35,000 more children across the United States that entered kindergarten without documentation of complete vaccination against common diseases like measles, whooping cough, and chickenpox.”
The report authors, led by Ranee Seither, MPH, with the immunization services division of the CDC’s National Center for Immunization and Respiratory Diseases, said the COVID-19 pandemic played a large part in the dip as children missed doctors’ appointments and states relaxed requirements with remote instruction.
States reported reluctance by parents to schedule well-child appointments and reduced access to office visits as well as longer grace periods or provisional enrollment. There was also less submission of documentation by parents, less time for school nurses to follow-up with students to document vaccines, fewer staff members to conduct kindergarten vaccination coverage assessment, lower response rates from schools, and both extended and compressed kindergarten vaccination coverage data collection schedules.
“There’s a greater proportion of parents who are questioning routine vaccines,” Jason V. Terk, MD, a Texas pediatrician and a spokesman for the American Academy of Pediatrics, told the New York Times. He said misinformation “fed the fire of distrust and skepticism that is really sort of the new pandemic of hesitancy for routine vaccines.”
The authors of the CDC report wrote: “As schools continue to return to in-person learning, enforcement of vaccination policies and follow-up with undervaccinated students are important to improve vaccination coverage.”
They urged schools and immunization programs to reach out to first-time students, including kindergartners and first-graders, and follow up with undervaccinated students.
The rate of people having an exemption from at least one vaccine remained low at 2.2% and the percentage of children with exemptions decreased in 37 states. However, an additional 3.9% who did not have a vaccine exemption were not up to date for MMR, according to the report.
Mississippi and New York had the smallest percentage of exemptions (0.1%) and Idaho had the most (8.2%). In the 2019-2020 school year, 2.5% reported an exemption from at least one vaccine. Nationally, 0.2% of kindergartners had a medical exemption and 1.9% had a nonmedical exemption.
Vaccination rates also differed among states. The New York Times noted that Maryland had a 10% drop in MMR vaccine coverage, while Wisconsin, Georgia, Wyoming, and Kentucky had declines of about 5%.
Among states reporting the measures in 2020-2021, the proportion of kindergartners attending school with no documentation of required vaccinations or exemptions ranged from 0.1% (Pennsylvania and Virginia) to 8.3% (Maryland). The state with the lowest proportion of kindergarteners out of compliance was Florida (0.2%) and Indiana had the highest out-of-compliance rate at 16.6%.
Comparing states’ performance is difficult, the authors noted, because they vary as to which vaccine and number of doses they require and by what date and what documentation they require. They also vary by data collection methods; exemptions allowed; grace period rules and provisional enrollment.
The authors, Dr. Peacock, and Dr. Terk reported no relevant financial disclosures.
FROM THE MMWR
More antibodies with longer intervals between COVID vaccine doses
An overall ninefold increase in COVID-19 antibody levels can be seen with a longer interval between first and second doses of the Pfizer/BioNTech (BNT162b2) vaccine in people without prior infection, according to data from the U.K. government’s SIREN (SARS-CoV-2 Immunity and Reinfection Evaluation) study.
This interval-dependent antibody level varied by age, with those aged 45-54 years showing an 11-fold increase with a longer dosing interval (greater than 10 weeks vs. 2-4 weeks). People younger than age 25 years showed a 13-fold increase with the longer interval, but participant numbers were low in this sub-group.
Overall antibody levels in infection-naive participants were 1,268.72 Binding Antibody Units (BAU)/mL (1,043.25-1,542.91) in those with a 2-4–week interval, compared with 11,479.73 BAU/mL (10,742.78-12,267.24) (P < .0001), in those with at least a 10-week interval between doses.
The work is the latest analysis from SIREN, which measured antibody levels in the blood from nearly 6,000 health care workers from across the United Kingdom. Study lead Ashley Otter, PhD, technical lead for SIREN serology at the UK Health Security Agency (UKHSA), will present the work on Tuesday at the 2022 European Congress of Clinical Microbiology & Infectious Diseases (ECCMID), Lisbon.
In an interview, Dr. Otter noted that, “it is important to remember that antibody levels are only one aspect of the immune response, and in our recent vaccine effectiveness analysis, we found that dosing intervals did not affect protection against infection.”
The study, which appeared in the March issue of the New England Journal of Medicine, also found that after the second dose of vaccine, there was about a 2.5–fold difference in antibody levels between those who had prior infection of 16.052 (14.071-18.312) BAU/mL, compared with 7.050 (6.634-7.491) BAU/mL in infection-naive individuals (P < .0001).
Following the first dose only, antibody levels were up to 10 times higher in participants who were previously infected, compared with infection-naive individuals. This effect lasted up to 8 months and then began to plateau.
Natural infection increased antibody levels
Dr. Otter remarked that, “COVID-19 antibody levels are high in those people who were previously naturally infected and vaccinated, highlighting that vaccination provides an additional benefit to these individuals.”
This news organization asked Charlotte Thålin, PhD, an immunologist from the Karolinska Institute, Stockholm, to comment on the study. Dr. Thålin studies a cohort similar to SIREN, called the Swedish COMMUNITY health care worker cohort. “The new data from the SIREN emphasizes the importance of the number of antigenic exposures and the time interval between them, whether it be exposure through vaccination or exposure through infection.”
“We see similar data in our Swedish COMMUNITY health care worker cohort,” Dr. Thålin continued, “where infection prior to vaccination yields a more than twofold enhancement in antibodies, neutralizing breadth, and T cell responses, and an even larger increase with a longer time interval between infection and vaccination.”
However, she cautioned that they now see a high rate of Omicron vaccine breakthrough infections, and this is also true in people with previous infection and three vaccine doses.
“As we approach a second booster – a fourth vaccine dose – we need to consider that many individuals will have had up to five to six antigen exposures within a short period of time, sometimes within a year,” she pointed out. “This is a whole new scenario, with a lot of different combinations of vaccine and infection-induced immunity. We do not yet know the impact of these frequent immune exposures, and we now need to monitor immune responses following Omicron and booster doses closely.”
SIREN originally aimed to understand how much protection people got after developing a primary infection and why they might become reinfected with COVID-19. Following the rollout of the United Kingdom’s vaccination program, the protective effects of vaccination against COVID-19 were investigated, as well as why some people still become ill after being vaccinated, Dr. Otter explained.
In this latest analysis, Dr. Otter and colleagues assessed anti-spike binding antibodies in serum samples from a total of 5,871 health care workers, with 3,989 after one dose (at least 21 days) and 1,882 after two doses (at least 14 days).
Most participants were women (82.3%), of White ethnicity (87%), and came from across the United Kingdom.
Participants were also categorized into those who had evidence of natural COVID-19 infection (confirmed by a PCR test or assumed because of their antibody profile) or those who were infection-naive. Almost all (> 99%) of those who were infection-naive seroconverted after vaccination.
The primary outcome was anti-spike antibody levels assessed according to dose, previous infection, dosing interval, age, ethnicity, and comorbidities, including immunosuppressive disease such as immune system cancers, rheumatologic disease, chronic respiratory diseases, diabetes, obesity, and chronic neurologic disease.
In the infection-naive group, the mean antibody (anti-S titer) was 75.48 BAU/mL after the first vaccine dose, and this rose to 7,049.76 BAU/mL after the second dose.
The much higher antibody titer with the second dose in infection-naive individuals “is what gives you the most protection, as your antibody titers are at their peak. They then start to gradually wane from this peak,” said Dr. Otter.
In the post-infection group, antibody titers also rose (2,111.08 BAU/mL after first dose and 16,052.39 BAU/mL after second dose), although less so than in the infection-naive group, because of the additional exposure of infection, added Dr. Otter.
Antibody levels also varied according to time elapsed between natural infection and dose 1 of vaccination. With a 3-month interval, antibody levels were 1,970.83 (1,506.01-2,579.1) BAU/mL, compared with 13,759.31 (8,097.78-23,379.09) BAU/mL after a 9-month interval. Antibody levels after one dose in those previously infected are higher than the infection-naive because “previous infection, then vaccination, is likely explained by T-cell expansion upon a boost with a second antigen exposure, and then a maturing memory B-cell response that has been demonstrated up to 6 months,” explained Dr. Otter.
Timing of fourth dose
By March of this year, 86.2% of the U.K. population aged over 12 years had received at least two doses, but with rises in disease prevalence and the spread of variants of concern, further work is ongoing to understand the waning of the immune response, level of protection, and why some individuals develop COVID-19 even when double-vaccinated.
This news organization asked Susanna Dunachie, BMChB, professor of infectious diseases, University of Oxford, U.K., what the interval findings might mean for the timing of the fourth dose of vaccine across the U.K. population.
In the United Kingdom, fourth doses are being given to people who are 75 years and older, residents in care homes for older people, and those with weakened immune systems. “To make decisions about fourth doses for healthy people, we need to see how quickly antibody and T-cell responses drop,” said Ms. Dunachie, who is part of the large SIREN study team but was not involved in the analysis led by Dr. Otter. “Current research suggests that the T-cell response may be better maintained than the antibody response, and less affected by variants like Omicron.”
She explained the balance between antibody and T-cell responses to vaccination. “It is likely that antibodies that neutralize the virus are important for preventing any infection at all, and these unfortunately do fall in time, but T-cell responses are better sustained and help keep people out of [the] hospital,” she said.
Ms. Dunachie added that it was necessary to wait and observe what happens next with SARS-CoV-2 evolution, as well as wait for longer follow-up after the third dose in healthy people. “On current evidence, my estimate is we postpone decisions on fourth doses in healthy people to late summer/autumn.”
A version of this article first appeared on Medscape.com.
An overall ninefold increase in COVID-19 antibody levels can be seen with a longer interval between first and second doses of the Pfizer/BioNTech (BNT162b2) vaccine in people without prior infection, according to data from the U.K. government’s SIREN (SARS-CoV-2 Immunity and Reinfection Evaluation) study.
This interval-dependent antibody level varied by age, with those aged 45-54 years showing an 11-fold increase with a longer dosing interval (greater than 10 weeks vs. 2-4 weeks). People younger than age 25 years showed a 13-fold increase with the longer interval, but participant numbers were low in this sub-group.
Overall antibody levels in infection-naive participants were 1,268.72 Binding Antibody Units (BAU)/mL (1,043.25-1,542.91) in those with a 2-4–week interval, compared with 11,479.73 BAU/mL (10,742.78-12,267.24) (P < .0001), in those with at least a 10-week interval between doses.
The work is the latest analysis from SIREN, which measured antibody levels in the blood from nearly 6,000 health care workers from across the United Kingdom. Study lead Ashley Otter, PhD, technical lead for SIREN serology at the UK Health Security Agency (UKHSA), will present the work on Tuesday at the 2022 European Congress of Clinical Microbiology & Infectious Diseases (ECCMID), Lisbon.
In an interview, Dr. Otter noted that, “it is important to remember that antibody levels are only one aspect of the immune response, and in our recent vaccine effectiveness analysis, we found that dosing intervals did not affect protection against infection.”
The study, which appeared in the March issue of the New England Journal of Medicine, also found that after the second dose of vaccine, there was about a 2.5–fold difference in antibody levels between those who had prior infection of 16.052 (14.071-18.312) BAU/mL, compared with 7.050 (6.634-7.491) BAU/mL in infection-naive individuals (P < .0001).
Following the first dose only, antibody levels were up to 10 times higher in participants who were previously infected, compared with infection-naive individuals. This effect lasted up to 8 months and then began to plateau.
Natural infection increased antibody levels
Dr. Otter remarked that, “COVID-19 antibody levels are high in those people who were previously naturally infected and vaccinated, highlighting that vaccination provides an additional benefit to these individuals.”
This news organization asked Charlotte Thålin, PhD, an immunologist from the Karolinska Institute, Stockholm, to comment on the study. Dr. Thålin studies a cohort similar to SIREN, called the Swedish COMMUNITY health care worker cohort. “The new data from the SIREN emphasizes the importance of the number of antigenic exposures and the time interval between them, whether it be exposure through vaccination or exposure through infection.”
“We see similar data in our Swedish COMMUNITY health care worker cohort,” Dr. Thålin continued, “where infection prior to vaccination yields a more than twofold enhancement in antibodies, neutralizing breadth, and T cell responses, and an even larger increase with a longer time interval between infection and vaccination.”
However, she cautioned that they now see a high rate of Omicron vaccine breakthrough infections, and this is also true in people with previous infection and three vaccine doses.
“As we approach a second booster – a fourth vaccine dose – we need to consider that many individuals will have had up to five to six antigen exposures within a short period of time, sometimes within a year,” she pointed out. “This is a whole new scenario, with a lot of different combinations of vaccine and infection-induced immunity. We do not yet know the impact of these frequent immune exposures, and we now need to monitor immune responses following Omicron and booster doses closely.”
SIREN originally aimed to understand how much protection people got after developing a primary infection and why they might become reinfected with COVID-19. Following the rollout of the United Kingdom’s vaccination program, the protective effects of vaccination against COVID-19 were investigated, as well as why some people still become ill after being vaccinated, Dr. Otter explained.
In this latest analysis, Dr. Otter and colleagues assessed anti-spike binding antibodies in serum samples from a total of 5,871 health care workers, with 3,989 after one dose (at least 21 days) and 1,882 after two doses (at least 14 days).
Most participants were women (82.3%), of White ethnicity (87%), and came from across the United Kingdom.
Participants were also categorized into those who had evidence of natural COVID-19 infection (confirmed by a PCR test or assumed because of their antibody profile) or those who were infection-naive. Almost all (> 99%) of those who were infection-naive seroconverted after vaccination.
The primary outcome was anti-spike antibody levels assessed according to dose, previous infection, dosing interval, age, ethnicity, and comorbidities, including immunosuppressive disease such as immune system cancers, rheumatologic disease, chronic respiratory diseases, diabetes, obesity, and chronic neurologic disease.
In the infection-naive group, the mean antibody (anti-S titer) was 75.48 BAU/mL after the first vaccine dose, and this rose to 7,049.76 BAU/mL after the second dose.
The much higher antibody titer with the second dose in infection-naive individuals “is what gives you the most protection, as your antibody titers are at their peak. They then start to gradually wane from this peak,” said Dr. Otter.
In the post-infection group, antibody titers also rose (2,111.08 BAU/mL after first dose and 16,052.39 BAU/mL after second dose), although less so than in the infection-naive group, because of the additional exposure of infection, added Dr. Otter.
Antibody levels also varied according to time elapsed between natural infection and dose 1 of vaccination. With a 3-month interval, antibody levels were 1,970.83 (1,506.01-2,579.1) BAU/mL, compared with 13,759.31 (8,097.78-23,379.09) BAU/mL after a 9-month interval. Antibody levels after one dose in those previously infected are higher than the infection-naive because “previous infection, then vaccination, is likely explained by T-cell expansion upon a boost with a second antigen exposure, and then a maturing memory B-cell response that has been demonstrated up to 6 months,” explained Dr. Otter.
Timing of fourth dose
By March of this year, 86.2% of the U.K. population aged over 12 years had received at least two doses, but with rises in disease prevalence and the spread of variants of concern, further work is ongoing to understand the waning of the immune response, level of protection, and why some individuals develop COVID-19 even when double-vaccinated.
This news organization asked Susanna Dunachie, BMChB, professor of infectious diseases, University of Oxford, U.K., what the interval findings might mean for the timing of the fourth dose of vaccine across the U.K. population.
In the United Kingdom, fourth doses are being given to people who are 75 years and older, residents in care homes for older people, and those with weakened immune systems. “To make decisions about fourth doses for healthy people, we need to see how quickly antibody and T-cell responses drop,” said Ms. Dunachie, who is part of the large SIREN study team but was not involved in the analysis led by Dr. Otter. “Current research suggests that the T-cell response may be better maintained than the antibody response, and less affected by variants like Omicron.”
She explained the balance between antibody and T-cell responses to vaccination. “It is likely that antibodies that neutralize the virus are important for preventing any infection at all, and these unfortunately do fall in time, but T-cell responses are better sustained and help keep people out of [the] hospital,” she said.
Ms. Dunachie added that it was necessary to wait and observe what happens next with SARS-CoV-2 evolution, as well as wait for longer follow-up after the third dose in healthy people. “On current evidence, my estimate is we postpone decisions on fourth doses in healthy people to late summer/autumn.”
A version of this article first appeared on Medscape.com.
An overall ninefold increase in COVID-19 antibody levels can be seen with a longer interval between first and second doses of the Pfizer/BioNTech (BNT162b2) vaccine in people without prior infection, according to data from the U.K. government’s SIREN (SARS-CoV-2 Immunity and Reinfection Evaluation) study.
This interval-dependent antibody level varied by age, with those aged 45-54 years showing an 11-fold increase with a longer dosing interval (greater than 10 weeks vs. 2-4 weeks). People younger than age 25 years showed a 13-fold increase with the longer interval, but participant numbers were low in this sub-group.
Overall antibody levels in infection-naive participants were 1,268.72 Binding Antibody Units (BAU)/mL (1,043.25-1,542.91) in those with a 2-4–week interval, compared with 11,479.73 BAU/mL (10,742.78-12,267.24) (P < .0001), in those with at least a 10-week interval between doses.
The work is the latest analysis from SIREN, which measured antibody levels in the blood from nearly 6,000 health care workers from across the United Kingdom. Study lead Ashley Otter, PhD, technical lead for SIREN serology at the UK Health Security Agency (UKHSA), will present the work on Tuesday at the 2022 European Congress of Clinical Microbiology & Infectious Diseases (ECCMID), Lisbon.
In an interview, Dr. Otter noted that, “it is important to remember that antibody levels are only one aspect of the immune response, and in our recent vaccine effectiveness analysis, we found that dosing intervals did not affect protection against infection.”
The study, which appeared in the March issue of the New England Journal of Medicine, also found that after the second dose of vaccine, there was about a 2.5–fold difference in antibody levels between those who had prior infection of 16.052 (14.071-18.312) BAU/mL, compared with 7.050 (6.634-7.491) BAU/mL in infection-naive individuals (P < .0001).
Following the first dose only, antibody levels were up to 10 times higher in participants who were previously infected, compared with infection-naive individuals. This effect lasted up to 8 months and then began to plateau.
Natural infection increased antibody levels
Dr. Otter remarked that, “COVID-19 antibody levels are high in those people who were previously naturally infected and vaccinated, highlighting that vaccination provides an additional benefit to these individuals.”
This news organization asked Charlotte Thålin, PhD, an immunologist from the Karolinska Institute, Stockholm, to comment on the study. Dr. Thålin studies a cohort similar to SIREN, called the Swedish COMMUNITY health care worker cohort. “The new data from the SIREN emphasizes the importance of the number of antigenic exposures and the time interval between them, whether it be exposure through vaccination or exposure through infection.”
“We see similar data in our Swedish COMMUNITY health care worker cohort,” Dr. Thålin continued, “where infection prior to vaccination yields a more than twofold enhancement in antibodies, neutralizing breadth, and T cell responses, and an even larger increase with a longer time interval between infection and vaccination.”
However, she cautioned that they now see a high rate of Omicron vaccine breakthrough infections, and this is also true in people with previous infection and three vaccine doses.
“As we approach a second booster – a fourth vaccine dose – we need to consider that many individuals will have had up to five to six antigen exposures within a short period of time, sometimes within a year,” she pointed out. “This is a whole new scenario, with a lot of different combinations of vaccine and infection-induced immunity. We do not yet know the impact of these frequent immune exposures, and we now need to monitor immune responses following Omicron and booster doses closely.”
SIREN originally aimed to understand how much protection people got after developing a primary infection and why they might become reinfected with COVID-19. Following the rollout of the United Kingdom’s vaccination program, the protective effects of vaccination against COVID-19 were investigated, as well as why some people still become ill after being vaccinated, Dr. Otter explained.
In this latest analysis, Dr. Otter and colleagues assessed anti-spike binding antibodies in serum samples from a total of 5,871 health care workers, with 3,989 after one dose (at least 21 days) and 1,882 after two doses (at least 14 days).
Most participants were women (82.3%), of White ethnicity (87%), and came from across the United Kingdom.
Participants were also categorized into those who had evidence of natural COVID-19 infection (confirmed by a PCR test or assumed because of their antibody profile) or those who were infection-naive. Almost all (> 99%) of those who were infection-naive seroconverted after vaccination.
The primary outcome was anti-spike antibody levels assessed according to dose, previous infection, dosing interval, age, ethnicity, and comorbidities, including immunosuppressive disease such as immune system cancers, rheumatologic disease, chronic respiratory diseases, diabetes, obesity, and chronic neurologic disease.
In the infection-naive group, the mean antibody (anti-S titer) was 75.48 BAU/mL after the first vaccine dose, and this rose to 7,049.76 BAU/mL after the second dose.
The much higher antibody titer with the second dose in infection-naive individuals “is what gives you the most protection, as your antibody titers are at their peak. They then start to gradually wane from this peak,” said Dr. Otter.
In the post-infection group, antibody titers also rose (2,111.08 BAU/mL after first dose and 16,052.39 BAU/mL after second dose), although less so than in the infection-naive group, because of the additional exposure of infection, added Dr. Otter.
Antibody levels also varied according to time elapsed between natural infection and dose 1 of vaccination. With a 3-month interval, antibody levels were 1,970.83 (1,506.01-2,579.1) BAU/mL, compared with 13,759.31 (8,097.78-23,379.09) BAU/mL after a 9-month interval. Antibody levels after one dose in those previously infected are higher than the infection-naive because “previous infection, then vaccination, is likely explained by T-cell expansion upon a boost with a second antigen exposure, and then a maturing memory B-cell response that has been demonstrated up to 6 months,” explained Dr. Otter.
Timing of fourth dose
By March of this year, 86.2% of the U.K. population aged over 12 years had received at least two doses, but with rises in disease prevalence and the spread of variants of concern, further work is ongoing to understand the waning of the immune response, level of protection, and why some individuals develop COVID-19 even when double-vaccinated.
This news organization asked Susanna Dunachie, BMChB, professor of infectious diseases, University of Oxford, U.K., what the interval findings might mean for the timing of the fourth dose of vaccine across the U.K. population.
In the United Kingdom, fourth doses are being given to people who are 75 years and older, residents in care homes for older people, and those with weakened immune systems. “To make decisions about fourth doses for healthy people, we need to see how quickly antibody and T-cell responses drop,” said Ms. Dunachie, who is part of the large SIREN study team but was not involved in the analysis led by Dr. Otter. “Current research suggests that the T-cell response may be better maintained than the antibody response, and less affected by variants like Omicron.”
She explained the balance between antibody and T-cell responses to vaccination. “It is likely that antibodies that neutralize the virus are important for preventing any infection at all, and these unfortunately do fall in time, but T-cell responses are better sustained and help keep people out of [the] hospital,” she said.
Ms. Dunachie added that it was necessary to wait and observe what happens next with SARS-CoV-2 evolution, as well as wait for longer follow-up after the third dose in healthy people. “On current evidence, my estimate is we postpone decisions on fourth doses in healthy people to late summer/autumn.”
A version of this article first appeared on Medscape.com.
Meningococcal vaccine shows moderate protective effect against gonorrhea
A widely approved vaccine for meningitis may provide up to 40% protection against gonorrhea in young adults and adolescents, according to new research. This moderate efficacy paired with a targeted risk-based approach could reduce cases as well as lead to health care savings over 10 years, an additional modeling study showed.
The results – in three linked papers – were published in The Lancet Infectious Diseases.
Gonorrhea, caused by the bacterium Neisseria gonorrhoeae, is the second most commonly reported sexually transmitted infection in the United States, according to the Centers for Disease Control and Prevention. Globally, the World Health Organization estimates that there were 82.4 million new cases in people aged 15-49 in 2020. At the same time, it is becoming more difficult to treat the infection because of the increasing prevalence of drug-resistant strains of N. gonorrhoeae.
“New approaches, such as vaccination, are needed as long-term strategies to prevent gonorrhea and address the emerging threat of antimicrobial resistance,” Winston Abara, MD, PhD, Division of STD Prevention, Centers for Disease Control and Prevention, and colleagues wrote.
While there is currently no vaccine for gonorrhea, observational studies have found an association between a meningococcal serogroup B vaccine and reduced gonorrhea cases. One study in New Zealand found that people vaccinated with the MeNZB vaccine, which was produced to control an outbreak of meningococcal disease in the country, were 31% less likely to contract gonorrhea.
This cross-reactivity comes about because Neisseria meningitidis, the bacterium that can cause meningitis, is closely related to N. gonorrhoeae, Joseph Alex Duncan, MD, PhD, associate professor of medicine, Division of Infectious Diseases, University of North Carolina School of Medicine, Chapel Hill, said in an interview. He was not involved with the research. The thought is that “a large proportion of the proteins that are in the vaccine also recognize proteins from Neisseria gonorrhea, because the bacteria are so similar at the genetic level,” he said.
To see if this association was still found for the four-component serogroup B meningococcal vaccine (MenB-4C), which is now widely available, Dr. Abara and colleagues looked through health records to identify laboratory-confirmed gonorrhea and chlamydia infections in adolescents and young adults in New York City and Philadelphia. All individuals included in the analysis were age 16-23 and all infections occurred between Jan. 1, 2016, and Dec. 31, 2018. These infections were then linked to vaccination records to determine individuals’ MenB-4C vaccination status. Complete vaccination was defined as two MenB-4C doses, delivered 30-180 days apart.
The research team identified over 167,700 infections, including 18,099 gonococcal infections, 124,876 chlamydial infections, and 24,731 coinfections, among 109,737 individuals. A total of 7,692 individuals had received at least one shot of the vaccine, and 3,660 people were fully vaccinated. Full MenB-4C vaccination was estimated to be 40% protective (APR 0.60; P < .0001) against gonorrhea, and partial vaccination was 26% protective (APR 0.74; P = .0012).
“The findings of our study add to the body of evidence that demonstrates that the MenB-4C may offer cross-protection against Neisseria gonorrhoeae, and it supports feasibility of an effective gonococcal vaccine with implications for gonorrhea prevention and control,” Dr. Abara told this news organization.
A second study conducted in South Australia looked at the effectiveness of the MenB-4C vaccine against meningitis and gonorrhea as part of a vaccination program. Using infection data from the Government of South Australia and vaccination records from the Australian Immunization Register, researchers identified individuals born between Feb. 1, 1998, and Feb. 1, 2005, with a documented gonorrhea or chlamydia infection between Feb. 1, 2019, and Jan. 31, 2021. Individuals with chlamydia served as the controls to account for similar sexual behavioral risks.
The analysis included 512 individuals with 575 cases of gonorrhea and 3,140 individuals with 3,847 episodes of chlamydia. In this group, the estimated vaccine effectiveness against gonorrhea was 32.7% (95% confidence interval, 8.3-50.6) in individuals who were fully vaccinated and 32.6% (95% CI, 10.6-49.1) in those who had received at least one dose of the MenB-4C.
While these findings are “confirmatory” because they showed results similar to those in previous observational studies, they are still exciting, Dr. Duncan said. “Up until now, we really haven’t had any real progress in knowing what type of immune responses could actually be protective from the disease,” he said. “These observational studies have really reinvigorated the Neisseria gonorrhea vaccine research community.”
A vaccine with moderate efficacy – like the protection demonstrated in both studies – could lead to a significant reduction in cases, he noted. A 2015 Australian modeling study estimated that a nonwaning vaccine with 20% efficacy could reduce cases by 40% over 20 years. Focusing on vaccinating higher-risk groups could also have an “outsize impact,” said Jeanne Marrazzo, MD, director, Division of Infectious Diseases, UAB Medicine, Birmingham, Alabama, in an interview. In the third study published in The Lancet, researchers estimated the possible reduction of cases and the potential health care cost savings in England in a vaccination effort focusing on men who have sex with men (MSM) at high risk for gonorrhea infection. They predicted that a vaccine with 31% efficacy could prevent 110,200 cases in MSM and save about £8 million ($10.4 million) over 10 years.
Both Dr. Duncan and Dr. Marrazzo agreed that clinical trials are needed to tease out whether the decrease in gonorrhea cases is due to the MenB-4C vaccine or the association is incidental. There are two ongoing clinical trials, one in Australia and one in the United States. Dr. Marrazzo leads the U.S. multicenter study, which also has two locations in Bangkok. The trial will also look at whether vaccination protection varies by the location of gonococcal infection: urethra, rectum, cervix, or pharynx. The two new observational studies did not distinguish the different sites of infection.
Dr. Marrazzo’s trial has enrolled almost 500 individuals so far, with the goal of enrolling over 2,000 participants in total. She hopes to see results by late 2023. “It’s a pretty ambitious effort, but I’m hoping it will give us not only a definitive answer in terms of reduction in infection by anatomic site,” she said, but “also give us a lot of information about how the immune response works to protect you from getting gonorrhea if you do get the vaccine.”
Dr. Duncan has received research grants from the National Institutes of Health. Dr. Marrazzo leads a clinical trial of the MenB-4C vaccine sponsored by the National Institute of Allergy and Infectious Diseases.
A version of this article first appeared on Medscape.com.
A widely approved vaccine for meningitis may provide up to 40% protection against gonorrhea in young adults and adolescents, according to new research. This moderate efficacy paired with a targeted risk-based approach could reduce cases as well as lead to health care savings over 10 years, an additional modeling study showed.
The results – in three linked papers – were published in The Lancet Infectious Diseases.
Gonorrhea, caused by the bacterium Neisseria gonorrhoeae, is the second most commonly reported sexually transmitted infection in the United States, according to the Centers for Disease Control and Prevention. Globally, the World Health Organization estimates that there were 82.4 million new cases in people aged 15-49 in 2020. At the same time, it is becoming more difficult to treat the infection because of the increasing prevalence of drug-resistant strains of N. gonorrhoeae.
“New approaches, such as vaccination, are needed as long-term strategies to prevent gonorrhea and address the emerging threat of antimicrobial resistance,” Winston Abara, MD, PhD, Division of STD Prevention, Centers for Disease Control and Prevention, and colleagues wrote.
While there is currently no vaccine for gonorrhea, observational studies have found an association between a meningococcal serogroup B vaccine and reduced gonorrhea cases. One study in New Zealand found that people vaccinated with the MeNZB vaccine, which was produced to control an outbreak of meningococcal disease in the country, were 31% less likely to contract gonorrhea.
This cross-reactivity comes about because Neisseria meningitidis, the bacterium that can cause meningitis, is closely related to N. gonorrhoeae, Joseph Alex Duncan, MD, PhD, associate professor of medicine, Division of Infectious Diseases, University of North Carolina School of Medicine, Chapel Hill, said in an interview. He was not involved with the research. The thought is that “a large proportion of the proteins that are in the vaccine also recognize proteins from Neisseria gonorrhea, because the bacteria are so similar at the genetic level,” he said.
To see if this association was still found for the four-component serogroup B meningococcal vaccine (MenB-4C), which is now widely available, Dr. Abara and colleagues looked through health records to identify laboratory-confirmed gonorrhea and chlamydia infections in adolescents and young adults in New York City and Philadelphia. All individuals included in the analysis were age 16-23 and all infections occurred between Jan. 1, 2016, and Dec. 31, 2018. These infections were then linked to vaccination records to determine individuals’ MenB-4C vaccination status. Complete vaccination was defined as two MenB-4C doses, delivered 30-180 days apart.
The research team identified over 167,700 infections, including 18,099 gonococcal infections, 124,876 chlamydial infections, and 24,731 coinfections, among 109,737 individuals. A total of 7,692 individuals had received at least one shot of the vaccine, and 3,660 people were fully vaccinated. Full MenB-4C vaccination was estimated to be 40% protective (APR 0.60; P < .0001) against gonorrhea, and partial vaccination was 26% protective (APR 0.74; P = .0012).
“The findings of our study add to the body of evidence that demonstrates that the MenB-4C may offer cross-protection against Neisseria gonorrhoeae, and it supports feasibility of an effective gonococcal vaccine with implications for gonorrhea prevention and control,” Dr. Abara told this news organization.
A second study conducted in South Australia looked at the effectiveness of the MenB-4C vaccine against meningitis and gonorrhea as part of a vaccination program. Using infection data from the Government of South Australia and vaccination records from the Australian Immunization Register, researchers identified individuals born between Feb. 1, 1998, and Feb. 1, 2005, with a documented gonorrhea or chlamydia infection between Feb. 1, 2019, and Jan. 31, 2021. Individuals with chlamydia served as the controls to account for similar sexual behavioral risks.
The analysis included 512 individuals with 575 cases of gonorrhea and 3,140 individuals with 3,847 episodes of chlamydia. In this group, the estimated vaccine effectiveness against gonorrhea was 32.7% (95% confidence interval, 8.3-50.6) in individuals who were fully vaccinated and 32.6% (95% CI, 10.6-49.1) in those who had received at least one dose of the MenB-4C.
While these findings are “confirmatory” because they showed results similar to those in previous observational studies, they are still exciting, Dr. Duncan said. “Up until now, we really haven’t had any real progress in knowing what type of immune responses could actually be protective from the disease,” he said. “These observational studies have really reinvigorated the Neisseria gonorrhea vaccine research community.”
A vaccine with moderate efficacy – like the protection demonstrated in both studies – could lead to a significant reduction in cases, he noted. A 2015 Australian modeling study estimated that a nonwaning vaccine with 20% efficacy could reduce cases by 40% over 20 years. Focusing on vaccinating higher-risk groups could also have an “outsize impact,” said Jeanne Marrazzo, MD, director, Division of Infectious Diseases, UAB Medicine, Birmingham, Alabama, in an interview. In the third study published in The Lancet, researchers estimated the possible reduction of cases and the potential health care cost savings in England in a vaccination effort focusing on men who have sex with men (MSM) at high risk for gonorrhea infection. They predicted that a vaccine with 31% efficacy could prevent 110,200 cases in MSM and save about £8 million ($10.4 million) over 10 years.
Both Dr. Duncan and Dr. Marrazzo agreed that clinical trials are needed to tease out whether the decrease in gonorrhea cases is due to the MenB-4C vaccine or the association is incidental. There are two ongoing clinical trials, one in Australia and one in the United States. Dr. Marrazzo leads the U.S. multicenter study, which also has two locations in Bangkok. The trial will also look at whether vaccination protection varies by the location of gonococcal infection: urethra, rectum, cervix, or pharynx. The two new observational studies did not distinguish the different sites of infection.
Dr. Marrazzo’s trial has enrolled almost 500 individuals so far, with the goal of enrolling over 2,000 participants in total. She hopes to see results by late 2023. “It’s a pretty ambitious effort, but I’m hoping it will give us not only a definitive answer in terms of reduction in infection by anatomic site,” she said, but “also give us a lot of information about how the immune response works to protect you from getting gonorrhea if you do get the vaccine.”
Dr. Duncan has received research grants from the National Institutes of Health. Dr. Marrazzo leads a clinical trial of the MenB-4C vaccine sponsored by the National Institute of Allergy and Infectious Diseases.
A version of this article first appeared on Medscape.com.
A widely approved vaccine for meningitis may provide up to 40% protection against gonorrhea in young adults and adolescents, according to new research. This moderate efficacy paired with a targeted risk-based approach could reduce cases as well as lead to health care savings over 10 years, an additional modeling study showed.
The results – in three linked papers – were published in The Lancet Infectious Diseases.
Gonorrhea, caused by the bacterium Neisseria gonorrhoeae, is the second most commonly reported sexually transmitted infection in the United States, according to the Centers for Disease Control and Prevention. Globally, the World Health Organization estimates that there were 82.4 million new cases in people aged 15-49 in 2020. At the same time, it is becoming more difficult to treat the infection because of the increasing prevalence of drug-resistant strains of N. gonorrhoeae.
“New approaches, such as vaccination, are needed as long-term strategies to prevent gonorrhea and address the emerging threat of antimicrobial resistance,” Winston Abara, MD, PhD, Division of STD Prevention, Centers for Disease Control and Prevention, and colleagues wrote.
While there is currently no vaccine for gonorrhea, observational studies have found an association between a meningococcal serogroup B vaccine and reduced gonorrhea cases. One study in New Zealand found that people vaccinated with the MeNZB vaccine, which was produced to control an outbreak of meningococcal disease in the country, were 31% less likely to contract gonorrhea.
This cross-reactivity comes about because Neisseria meningitidis, the bacterium that can cause meningitis, is closely related to N. gonorrhoeae, Joseph Alex Duncan, MD, PhD, associate professor of medicine, Division of Infectious Diseases, University of North Carolina School of Medicine, Chapel Hill, said in an interview. He was not involved with the research. The thought is that “a large proportion of the proteins that are in the vaccine also recognize proteins from Neisseria gonorrhea, because the bacteria are so similar at the genetic level,” he said.
To see if this association was still found for the four-component serogroup B meningococcal vaccine (MenB-4C), which is now widely available, Dr. Abara and colleagues looked through health records to identify laboratory-confirmed gonorrhea and chlamydia infections in adolescents and young adults in New York City and Philadelphia. All individuals included in the analysis were age 16-23 and all infections occurred between Jan. 1, 2016, and Dec. 31, 2018. These infections were then linked to vaccination records to determine individuals’ MenB-4C vaccination status. Complete vaccination was defined as two MenB-4C doses, delivered 30-180 days apart.
The research team identified over 167,700 infections, including 18,099 gonococcal infections, 124,876 chlamydial infections, and 24,731 coinfections, among 109,737 individuals. A total of 7,692 individuals had received at least one shot of the vaccine, and 3,660 people were fully vaccinated. Full MenB-4C vaccination was estimated to be 40% protective (APR 0.60; P < .0001) against gonorrhea, and partial vaccination was 26% protective (APR 0.74; P = .0012).
“The findings of our study add to the body of evidence that demonstrates that the MenB-4C may offer cross-protection against Neisseria gonorrhoeae, and it supports feasibility of an effective gonococcal vaccine with implications for gonorrhea prevention and control,” Dr. Abara told this news organization.
A second study conducted in South Australia looked at the effectiveness of the MenB-4C vaccine against meningitis and gonorrhea as part of a vaccination program. Using infection data from the Government of South Australia and vaccination records from the Australian Immunization Register, researchers identified individuals born between Feb. 1, 1998, and Feb. 1, 2005, with a documented gonorrhea or chlamydia infection between Feb. 1, 2019, and Jan. 31, 2021. Individuals with chlamydia served as the controls to account for similar sexual behavioral risks.
The analysis included 512 individuals with 575 cases of gonorrhea and 3,140 individuals with 3,847 episodes of chlamydia. In this group, the estimated vaccine effectiveness against gonorrhea was 32.7% (95% confidence interval, 8.3-50.6) in individuals who were fully vaccinated and 32.6% (95% CI, 10.6-49.1) in those who had received at least one dose of the MenB-4C.
While these findings are “confirmatory” because they showed results similar to those in previous observational studies, they are still exciting, Dr. Duncan said. “Up until now, we really haven’t had any real progress in knowing what type of immune responses could actually be protective from the disease,” he said. “These observational studies have really reinvigorated the Neisseria gonorrhea vaccine research community.”
A vaccine with moderate efficacy – like the protection demonstrated in both studies – could lead to a significant reduction in cases, he noted. A 2015 Australian modeling study estimated that a nonwaning vaccine with 20% efficacy could reduce cases by 40% over 20 years. Focusing on vaccinating higher-risk groups could also have an “outsize impact,” said Jeanne Marrazzo, MD, director, Division of Infectious Diseases, UAB Medicine, Birmingham, Alabama, in an interview. In the third study published in The Lancet, researchers estimated the possible reduction of cases and the potential health care cost savings in England in a vaccination effort focusing on men who have sex with men (MSM) at high risk for gonorrhea infection. They predicted that a vaccine with 31% efficacy could prevent 110,200 cases in MSM and save about £8 million ($10.4 million) over 10 years.
Both Dr. Duncan and Dr. Marrazzo agreed that clinical trials are needed to tease out whether the decrease in gonorrhea cases is due to the MenB-4C vaccine or the association is incidental. There are two ongoing clinical trials, one in Australia and one in the United States. Dr. Marrazzo leads the U.S. multicenter study, which also has two locations in Bangkok. The trial will also look at whether vaccination protection varies by the location of gonococcal infection: urethra, rectum, cervix, or pharynx. The two new observational studies did not distinguish the different sites of infection.
Dr. Marrazzo’s trial has enrolled almost 500 individuals so far, with the goal of enrolling over 2,000 participants in total. She hopes to see results by late 2023. “It’s a pretty ambitious effort, but I’m hoping it will give us not only a definitive answer in terms of reduction in infection by anatomic site,” she said, but “also give us a lot of information about how the immune response works to protect you from getting gonorrhea if you do get the vaccine.”
Dr. Duncan has received research grants from the National Institutes of Health. Dr. Marrazzo leads a clinical trial of the MenB-4C vaccine sponsored by the National Institute of Allergy and Infectious Diseases.
A version of this article first appeared on Medscape.com.
FROM THE LANCET INFECTIOUS DISEASES
CDC recommends hep B vaccination for most adults
It also added that adults aged 60 years or older without known risk factors for hepatitis B may get vaccinated.
The agency earlier recommended the vaccination for all infants and children under the age of 19 years and for adults aged 60 years or older with known risk factors.
The CDC said it wants to expand vaccinations because, after decades of progress, the number of new hepatitis B infections is increasing among adults. Acute hepatitis B infections among adults lead to chronic hepatitis B disease in an estimated 2%-6% of cases, and can result in cirrhosis, liver cancer, and death.
Among adults aged 40-49 years, the rate of cases increased from 1.9 per 100,000 people in 2011 to 2.7 per 100,000 in 2019. Among adults aged 50-59 years, the rate increased during this period from 1.1 to 1.6 per 100,000.
Most adults aren’t vaccinated. Among adults aged 19 years or older, only 30.0% reported that they’d received at least the three recommended doses of the vaccine. The rate was 40.3% for adults aged 19-49 years, and 19.1% for adults aged 50 years or older.
Hepatitis B infection rates are particularly elevated among African Americans.
Even among adults with chronic liver disease, the vaccination rate is only 33.0%. And, among travelers to countries where the virus has been endemic since 1995, only 38.9% were vaccinated.
In a 2018 survey of internal medicine and family physicians, 68% said their patients had not told them about risk factors, making it difficult to assess whether the patients needed the vaccine according to the recommendations at the time. These risk factors include injection drug use, incarceration, and multiple sex partners, experiences the patients may not have been willing to discuss.
CDC researchers calculated that universal adult hepatitis B vaccination would cost $153,000 for every quality-adjusted life-year (QALY) gained. For adults aged 19-59 years, a QALY would cost $117,000 because infections are more prevalent in that age group.
The CDC specified that it intends its new guidelines to prompt physicians to offer the vaccine to adults aged 60 years or older rather than wait for them to request it.
The Food and Drug Administration has approved both three-dose and two-dose hepatitis B vaccines, with evidence showing similar seroprotection and adverse events.
People who have already completed their vaccination or have a history of hepatitis B infection should only receive additional vaccinations in specific cases, as detailed in the CDC’s 2018 recommendations.
A version of this article first appeared on Medscape.com.
It also added that adults aged 60 years or older without known risk factors for hepatitis B may get vaccinated.
The agency earlier recommended the vaccination for all infants and children under the age of 19 years and for adults aged 60 years or older with known risk factors.
The CDC said it wants to expand vaccinations because, after decades of progress, the number of new hepatitis B infections is increasing among adults. Acute hepatitis B infections among adults lead to chronic hepatitis B disease in an estimated 2%-6% of cases, and can result in cirrhosis, liver cancer, and death.
Among adults aged 40-49 years, the rate of cases increased from 1.9 per 100,000 people in 2011 to 2.7 per 100,000 in 2019. Among adults aged 50-59 years, the rate increased during this period from 1.1 to 1.6 per 100,000.
Most adults aren’t vaccinated. Among adults aged 19 years or older, only 30.0% reported that they’d received at least the three recommended doses of the vaccine. The rate was 40.3% for adults aged 19-49 years, and 19.1% for adults aged 50 years or older.
Hepatitis B infection rates are particularly elevated among African Americans.
Even among adults with chronic liver disease, the vaccination rate is only 33.0%. And, among travelers to countries where the virus has been endemic since 1995, only 38.9% were vaccinated.
In a 2018 survey of internal medicine and family physicians, 68% said their patients had not told them about risk factors, making it difficult to assess whether the patients needed the vaccine according to the recommendations at the time. These risk factors include injection drug use, incarceration, and multiple sex partners, experiences the patients may not have been willing to discuss.
CDC researchers calculated that universal adult hepatitis B vaccination would cost $153,000 for every quality-adjusted life-year (QALY) gained. For adults aged 19-59 years, a QALY would cost $117,000 because infections are more prevalent in that age group.
The CDC specified that it intends its new guidelines to prompt physicians to offer the vaccine to adults aged 60 years or older rather than wait for them to request it.
The Food and Drug Administration has approved both three-dose and two-dose hepatitis B vaccines, with evidence showing similar seroprotection and adverse events.
People who have already completed their vaccination or have a history of hepatitis B infection should only receive additional vaccinations in specific cases, as detailed in the CDC’s 2018 recommendations.
A version of this article first appeared on Medscape.com.
It also added that adults aged 60 years or older without known risk factors for hepatitis B may get vaccinated.
The agency earlier recommended the vaccination for all infants and children under the age of 19 years and for adults aged 60 years or older with known risk factors.
The CDC said it wants to expand vaccinations because, after decades of progress, the number of new hepatitis B infections is increasing among adults. Acute hepatitis B infections among adults lead to chronic hepatitis B disease in an estimated 2%-6% of cases, and can result in cirrhosis, liver cancer, and death.
Among adults aged 40-49 years, the rate of cases increased from 1.9 per 100,000 people in 2011 to 2.7 per 100,000 in 2019. Among adults aged 50-59 years, the rate increased during this period from 1.1 to 1.6 per 100,000.
Most adults aren’t vaccinated. Among adults aged 19 years or older, only 30.0% reported that they’d received at least the three recommended doses of the vaccine. The rate was 40.3% for adults aged 19-49 years, and 19.1% for adults aged 50 years or older.
Hepatitis B infection rates are particularly elevated among African Americans.
Even among adults with chronic liver disease, the vaccination rate is only 33.0%. And, among travelers to countries where the virus has been endemic since 1995, only 38.9% were vaccinated.
In a 2018 survey of internal medicine and family physicians, 68% said their patients had not told them about risk factors, making it difficult to assess whether the patients needed the vaccine according to the recommendations at the time. These risk factors include injection drug use, incarceration, and multiple sex partners, experiences the patients may not have been willing to discuss.
CDC researchers calculated that universal adult hepatitis B vaccination would cost $153,000 for every quality-adjusted life-year (QALY) gained. For adults aged 19-59 years, a QALY would cost $117,000 because infections are more prevalent in that age group.
The CDC specified that it intends its new guidelines to prompt physicians to offer the vaccine to adults aged 60 years or older rather than wait for them to request it.
The Food and Drug Administration has approved both three-dose and two-dose hepatitis B vaccines, with evidence showing similar seroprotection and adverse events.
People who have already completed their vaccination or have a history of hepatitis B infection should only receive additional vaccinations in specific cases, as detailed in the CDC’s 2018 recommendations.
A version of this article first appeared on Medscape.com.
FROM THE MMWR
Polio: Five African countries vaccinating 23 million children
When polio paralyzed a 3-year-old girl in Lilongwe, Malawi, in November 2021, public health experts in Malawi’s Ministry of Health responded quickly. The ministry partnered with the Global Polio Eradication Initiative, the World Health Organization, and the United Nations International Children’s Emergency Fund to mobilize a surge team of personnel and resources to vaccinate all 2.9 million Malawian children aged under 5 years, WHO reported in a news release.
The first of four sequential campaigns began on March 20 and expanded on March 24 to neighboring Mozambique, Tanzania, and Zambia. The multinational, multiagency effort aims to include Zimbabwean children as well and deliver over 80 million supplemental doses of bivalent oral polio vaccines to over 23 million children in these five countries by July.
Because it takes multiple polio vaccine doses to become fully immunized, the children are expected to receive four rounds of vaccine regardless of their vaccination history.
“It is important to conduct the campaigns now to boost the immunity of our children,” Annie Chauma-Mwale, MBBS, MPH, the chief medical officer of epidemiology and surveillance in Malawi’s Ministry of Health in Lilongwe, said in an interview. “Polio is not only a medical issue. Polio is also a socioeconomic issue with long-term impacts on the child, the country, and the globe.
“In Malawi, we are using our community health and health care facility structures to ensure we do not miss any eligible child,” explained Dr. Chauma-Mwale, who is also the deputy incident manager of the poliovirus outbreak response. “We aim to play our role in the global eradication of polio by protecting the vulnerable and curtailing any potential transmission as early as possible.”
Of the three variants of wild, naturally occurring poliovirus, types 2 and 3 have been eradicated, but wild poliovirus type 1 (WPV1) remains endemic in Afghanistan and Pakistan.
As reported recently by this news organization, the girl in Malawi was infected with a WPV1 strain that had been circulating for years in Pakistan’s Sindh Province.
Malawi’s most recent clinically confirmed WPV1 case was reported in 1992, and this is the first WPV1 case detected in Africa since 2016. The continent was declared free of indigenous wild polio in 2020 and is still considered free of wild poliovirus because the child’s illness was imported from elsewhere.
The 3-year-old girl developed acute flaccid paralysis in November 2021. In February 2022, virus from her stool was sequenced by the National Institute of Communicable Disease in South Africa and the U.S. Centers for Disease Control and Prevention. On Feb. 16, Malawi was notified of the case, which was genetically linked to a sequence detected in Sindh Province around 2 years earlier.
‘Do not ignore polio’
Within 24 hours, the Government of Malawi declared a public health emergency and activated the national Emergency Operations Centre. Within 72 hours, the GPEI rapid response team arrived in the country. The Ministry of Health partnered with GPEI, WHO, and UNICEF to mobilize the campaign and begin vaccinating children on March 20.
‘’We rely on clinicians to support the surveillance of polio through case searches, both active and passive,” Mike Nenani Chisema, MBBS, MPH, the program manager of the expanded program on immunization and the polio response operations manager in Malawi’s Ministry of Health, said in an interview.
He noted that the young girl was diagnosed correctly and millions of children are now being protected against the disease, thanks to the acumen of one hospital clinician.
“Remember, we still have polio in some countries, and every country is at risk,” he cautioned. “Don’t forget to look for the obvious and do not ignore polio, regardless of economic status.’’
According to GPEI, all countries – especially those with weak immunization and other public health programs whose residents trade or travel to and from endemic countries – are at risk for imported polio.
Anita Gupta, DO, MPP, PharmD, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at the Johns Hopkins University, Baltimore, said that she welcomes this effort.
“Given the decades of published evidence and understanding on the vaccine’s safety and efficacy, this program in Malawi is the right step to take,” Gupta, who is not involved in the campaigns, said in an interview. “Polio is preventable, and acting now will prevent spread later.”
Dr. Chauma-Mwale and Dr. Chisema are employees of Malawi’s Ministry of Health. Dr. Gupta disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When polio paralyzed a 3-year-old girl in Lilongwe, Malawi, in November 2021, public health experts in Malawi’s Ministry of Health responded quickly. The ministry partnered with the Global Polio Eradication Initiative, the World Health Organization, and the United Nations International Children’s Emergency Fund to mobilize a surge team of personnel and resources to vaccinate all 2.9 million Malawian children aged under 5 years, WHO reported in a news release.
The first of four sequential campaigns began on March 20 and expanded on March 24 to neighboring Mozambique, Tanzania, and Zambia. The multinational, multiagency effort aims to include Zimbabwean children as well and deliver over 80 million supplemental doses of bivalent oral polio vaccines to over 23 million children in these five countries by July.
Because it takes multiple polio vaccine doses to become fully immunized, the children are expected to receive four rounds of vaccine regardless of their vaccination history.
“It is important to conduct the campaigns now to boost the immunity of our children,” Annie Chauma-Mwale, MBBS, MPH, the chief medical officer of epidemiology and surveillance in Malawi’s Ministry of Health in Lilongwe, said in an interview. “Polio is not only a medical issue. Polio is also a socioeconomic issue with long-term impacts on the child, the country, and the globe.
“In Malawi, we are using our community health and health care facility structures to ensure we do not miss any eligible child,” explained Dr. Chauma-Mwale, who is also the deputy incident manager of the poliovirus outbreak response. “We aim to play our role in the global eradication of polio by protecting the vulnerable and curtailing any potential transmission as early as possible.”
Of the three variants of wild, naturally occurring poliovirus, types 2 and 3 have been eradicated, but wild poliovirus type 1 (WPV1) remains endemic in Afghanistan and Pakistan.
As reported recently by this news organization, the girl in Malawi was infected with a WPV1 strain that had been circulating for years in Pakistan’s Sindh Province.
Malawi’s most recent clinically confirmed WPV1 case was reported in 1992, and this is the first WPV1 case detected in Africa since 2016. The continent was declared free of indigenous wild polio in 2020 and is still considered free of wild poliovirus because the child’s illness was imported from elsewhere.
The 3-year-old girl developed acute flaccid paralysis in November 2021. In February 2022, virus from her stool was sequenced by the National Institute of Communicable Disease in South Africa and the U.S. Centers for Disease Control and Prevention. On Feb. 16, Malawi was notified of the case, which was genetically linked to a sequence detected in Sindh Province around 2 years earlier.
‘Do not ignore polio’
Within 24 hours, the Government of Malawi declared a public health emergency and activated the national Emergency Operations Centre. Within 72 hours, the GPEI rapid response team arrived in the country. The Ministry of Health partnered with GPEI, WHO, and UNICEF to mobilize the campaign and begin vaccinating children on March 20.
‘’We rely on clinicians to support the surveillance of polio through case searches, both active and passive,” Mike Nenani Chisema, MBBS, MPH, the program manager of the expanded program on immunization and the polio response operations manager in Malawi’s Ministry of Health, said in an interview.
He noted that the young girl was diagnosed correctly and millions of children are now being protected against the disease, thanks to the acumen of one hospital clinician.
“Remember, we still have polio in some countries, and every country is at risk,” he cautioned. “Don’t forget to look for the obvious and do not ignore polio, regardless of economic status.’’
According to GPEI, all countries – especially those with weak immunization and other public health programs whose residents trade or travel to and from endemic countries – are at risk for imported polio.
Anita Gupta, DO, MPP, PharmD, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at the Johns Hopkins University, Baltimore, said that she welcomes this effort.
“Given the decades of published evidence and understanding on the vaccine’s safety and efficacy, this program in Malawi is the right step to take,” Gupta, who is not involved in the campaigns, said in an interview. “Polio is preventable, and acting now will prevent spread later.”
Dr. Chauma-Mwale and Dr. Chisema are employees of Malawi’s Ministry of Health. Dr. Gupta disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When polio paralyzed a 3-year-old girl in Lilongwe, Malawi, in November 2021, public health experts in Malawi’s Ministry of Health responded quickly. The ministry partnered with the Global Polio Eradication Initiative, the World Health Organization, and the United Nations International Children’s Emergency Fund to mobilize a surge team of personnel and resources to vaccinate all 2.9 million Malawian children aged under 5 years, WHO reported in a news release.
The first of four sequential campaigns began on March 20 and expanded on March 24 to neighboring Mozambique, Tanzania, and Zambia. The multinational, multiagency effort aims to include Zimbabwean children as well and deliver over 80 million supplemental doses of bivalent oral polio vaccines to over 23 million children in these five countries by July.
Because it takes multiple polio vaccine doses to become fully immunized, the children are expected to receive four rounds of vaccine regardless of their vaccination history.
“It is important to conduct the campaigns now to boost the immunity of our children,” Annie Chauma-Mwale, MBBS, MPH, the chief medical officer of epidemiology and surveillance in Malawi’s Ministry of Health in Lilongwe, said in an interview. “Polio is not only a medical issue. Polio is also a socioeconomic issue with long-term impacts on the child, the country, and the globe.
“In Malawi, we are using our community health and health care facility structures to ensure we do not miss any eligible child,” explained Dr. Chauma-Mwale, who is also the deputy incident manager of the poliovirus outbreak response. “We aim to play our role in the global eradication of polio by protecting the vulnerable and curtailing any potential transmission as early as possible.”
Of the three variants of wild, naturally occurring poliovirus, types 2 and 3 have been eradicated, but wild poliovirus type 1 (WPV1) remains endemic in Afghanistan and Pakistan.
As reported recently by this news organization, the girl in Malawi was infected with a WPV1 strain that had been circulating for years in Pakistan’s Sindh Province.
Malawi’s most recent clinically confirmed WPV1 case was reported in 1992, and this is the first WPV1 case detected in Africa since 2016. The continent was declared free of indigenous wild polio in 2020 and is still considered free of wild poliovirus because the child’s illness was imported from elsewhere.
The 3-year-old girl developed acute flaccid paralysis in November 2021. In February 2022, virus from her stool was sequenced by the National Institute of Communicable Disease in South Africa and the U.S. Centers for Disease Control and Prevention. On Feb. 16, Malawi was notified of the case, which was genetically linked to a sequence detected in Sindh Province around 2 years earlier.
‘Do not ignore polio’
Within 24 hours, the Government of Malawi declared a public health emergency and activated the national Emergency Operations Centre. Within 72 hours, the GPEI rapid response team arrived in the country. The Ministry of Health partnered with GPEI, WHO, and UNICEF to mobilize the campaign and begin vaccinating children on March 20.
‘’We rely on clinicians to support the surveillance of polio through case searches, both active and passive,” Mike Nenani Chisema, MBBS, MPH, the program manager of the expanded program on immunization and the polio response operations manager in Malawi’s Ministry of Health, said in an interview.
He noted that the young girl was diagnosed correctly and millions of children are now being protected against the disease, thanks to the acumen of one hospital clinician.
“Remember, we still have polio in some countries, and every country is at risk,” he cautioned. “Don’t forget to look for the obvious and do not ignore polio, regardless of economic status.’’
According to GPEI, all countries – especially those with weak immunization and other public health programs whose residents trade or travel to and from endemic countries – are at risk for imported polio.
Anita Gupta, DO, MPP, PharmD, an adjunct assistant professor of anesthesiology and critical care medicine and pain medicine at the Johns Hopkins University, Baltimore, said that she welcomes this effort.
“Given the decades of published evidence and understanding on the vaccine’s safety and efficacy, this program in Malawi is the right step to take,” Gupta, who is not involved in the campaigns, said in an interview. “Polio is preventable, and acting now will prevent spread later.”
Dr. Chauma-Mwale and Dr. Chisema are employees of Malawi’s Ministry of Health. Dr. Gupta disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As FDA OKs another COVID booster, some experts question need
, even though many top infectious disease experts questioned the need before the agency’s decision.
The FDA granted emergency use authorization for both Pfizer and Moderna to offer the second booster – and fourth shot overall – for adults over 50 as well as those over 18 with compromised immune systems.
The Centers for Control and Prevention must still sign off before those doses start reaching American arms. That approval could come at any time.
“The general consensus, certainly the CDC’s consensus, is that the current vaccines are still really quite effective against Omicron and this new BA.2 variant in keeping people out of the hospital, and preventing the development of severe disease,” William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville said prior to the FDA’s announcement March 29.
Of the 217.4 million Americans who are “fully vaccinated,” i.e., received two doses of either Pfizer or Moderna’s vaccines or one dose of the Johnson & Johnson vaccine, only 45% have also received a booster shot, according to the CDC.
“Given that, there’s no need at the moment for the general population to get a fourth inoculation,” Dr. Schaffner says. “Our current focus ought to be on making sure that as many people as possible get that [first] booster who are eligible.”
Monica Gandhi, MD, an infectious disease specialist at the University of California, San Francisco, agreed that another booster for everyone was unnecessary. The only people who would need a fourth shot (or third, if they had the Johnson & Johnson vaccine initially) are those over age 65 or 70 years, Dr. Gandhi says.
“Older people need those antibodies up high because they’re more susceptible to severe breakthroughs,” she said, also before the latest development.
To boost or not to boost
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham & Women’s Hospital in Boston, said the timing of a booster and who should be eligible depends on what the nation is trying to achieve with its vaccination strategy.
“Is the goal to prevent any symptomatic infection with COVID-19, is the goal to prevent the spread of COVID-19, or is the goal to prevent severe disease that requires hospitalization?” asked Dr. Kuritzkes.
The current vaccine — with a booster — has prevented severe disease, he said.
An Israeli study showed, for instance, that a third Pfizer dose was 93% effective against hospitalization, 92% effective against severe illness, and 81% effective against death.
A just-published study in the New England Journal of Medicine found that a booster of the Pfizer vaccine was 95% effective against COVID-19 infection and that it did not raise any new safety issues.
A small Israeli study, also published in NEJM, of a fourth Pfizer dose given to health care workers found that it prevented symptomatic infection and illness, but that it was much less effective than previous doses — maybe 65% effective against symptomatic illness, the authors write.
Giving Americans another booster now — which has been shown to lose some effectiveness after about 4 months — means it might not offer protection this fall and winter, when there could be a seasonal surge of the virus, Dr. Kuritzkes says.
And, even if people receive boosters every few months, they are still likely to get a mild respiratory virus infection, he said.
“I’m pretty convinced that we cannot boost ourselves out of this pandemic,” said Dr. Kuritzkes. “We need to first of all ensure there’s global immunization so that all the people who have not been vaccinated at all get vaccinated. That’s far more important than boosting people a fourth time.”
Booster confusion
The April 6 FDA meeting of the agency’s Vaccines and Related Biological Products Advisory Committee comes as the two major COVID vaccine makers — Pfizer and Moderna — have applied for emergency use authorization for an additional booster.
Pfizer had asked for authorization for a fourth shot in patients over age 65 years, while Moderna wanted a booster to be available to all Americans over 18. The FDA instead granted authorization to both companies for those over 50 and anyone 18 or older who is immunocompromised.
What this means for the committee’s April 6 meeting is not clear. The original agenda says the committee will consider the evidence on safety and effectiveness of the additional vaccine doses and discuss how to set up a process — similar to that used for the influenza vaccine — to be able to determine the makeup of COVID vaccines as new variants emerge. That could lay the groundwork for an annual COVID shot, if needed.
The FDA advisers will not make recommendations nor vote on whether — and which — Americans should get a COVID booster. That is the job of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The last time a booster was considered, CDC Director Rochelle Walensky, MD, overrode the committee and recommended that all Americans — not just older individuals — get an additional COVID shot, which became the first booster.
That past action worries Dr. Gandhi, who calls it confusing, and says it may have contributed to the fact that less than half of Americans have since chosen to get a booster.
Dr. Schaffner says he expects the FDA to authorize emergency use for fourth doses of the Pfizer and Moderna vaccines, but he doesn’t think the CDC committee will recommend routine use. As was seen before, however, the CDC director does not have to follow the committee’s advice.
The members of ACIP “might be more conservative or narrower in scope in terms of recommending who needs to be boosted and when boosting is appropriate,” Dr. Kuritzkes says.
Dr. Gandhi says she’s concerned the FDA’s deliberations could be swayed by Moderna and Pfizer’s influence and that “pharmaceutical companies are going to have more of a say than they should in the scientific process.”
There are similar worries for Dr. Schaffner. He says he’s “a bit grumpy” that the vaccine makers have been using press releases to argue for boosters.
“Press releases are no way to make vaccine recommendations,” Dr. Schaffner said, adding that he “would advise [vaccine makers] to sit down and be quiet and let the FDA and CDC advisory committee do their thing.”
Moderna Chief Medical Officer Paul Burton, MD, however, told WebMD last week that the signs point to why a fourth shot may be needed.
“We see waning of effectiveness, antibody levels come down, and certainly effectiveness against Omicron comes down in 3 to 6 months,” Burton said. “The natural history, from what we’re seeing around the world, is that BA.2 is definitely here, it’s highly transmissible, and I think we are going to get an additional wave of BA.2 here in the United States.”
Another wave is coming, he said, and “I think there will be waning of effectiveness. We need to be prepared for that, so that’s why we need the fourth dose.”
Supply issues?
Meanwhile, the United Kingdom has begun offering boosters to anyone over 75, and Sweden’s health authority has recommended a fourth shot to people over age 80.
That puts pressure on the United States — at least on its politicians and policymakers — to, in a sense, keep up, said the infectious disease specialists.
Indeed, the White House has been keeping fourth shots in the news, warning that it is running out of money to ensure that all Americans would have access to one, if recommended.
On March 23, outgoing White House COVID-19 Response Coordinator Jeff Zients said the federal government had enough vaccine for the immunocompromised to get a fourth dose “and, if authorized in the coming weeks, enough supply for fourth doses for our most vulnerable, including seniors.”
But he warned that without congressional approval of a COVID-19 funding package, “We can’t procure the necessary vaccine supply to support fourth shots for all Americans.”
Mr. Zients also noted that other countries, including Japan, Vietnam, and the Philippines had already secured future booster doses and added, “We should be securing additional supply right now.”
Dr. Schaffner says that while it would be nice to “have a booster on the shelf,” the United States needs to put more effort into creating a globally-coordinated process for ensuring that vaccines match circulating strains and that they are manufactured on a timely basis.
He says he and others “have been reminding the public that the COVID pandemic may indeed be diminishing and moving into the endemic, but that doesn’t mean COVID is over or finished or disappeared.”
Dr. Schaffner says that it may be that “perhaps we’d need a periodic reminder to our immune system to remain protected. In other words, we might have to get boosted perhaps annually like we do with influenza.”
A version of this article first appeared on WebMD.com.
, even though many top infectious disease experts questioned the need before the agency’s decision.
The FDA granted emergency use authorization for both Pfizer and Moderna to offer the second booster – and fourth shot overall – for adults over 50 as well as those over 18 with compromised immune systems.
The Centers for Control and Prevention must still sign off before those doses start reaching American arms. That approval could come at any time.
“The general consensus, certainly the CDC’s consensus, is that the current vaccines are still really quite effective against Omicron and this new BA.2 variant in keeping people out of the hospital, and preventing the development of severe disease,” William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville said prior to the FDA’s announcement March 29.
Of the 217.4 million Americans who are “fully vaccinated,” i.e., received two doses of either Pfizer or Moderna’s vaccines or one dose of the Johnson & Johnson vaccine, only 45% have also received a booster shot, according to the CDC.
“Given that, there’s no need at the moment for the general population to get a fourth inoculation,” Dr. Schaffner says. “Our current focus ought to be on making sure that as many people as possible get that [first] booster who are eligible.”
Monica Gandhi, MD, an infectious disease specialist at the University of California, San Francisco, agreed that another booster for everyone was unnecessary. The only people who would need a fourth shot (or third, if they had the Johnson & Johnson vaccine initially) are those over age 65 or 70 years, Dr. Gandhi says.
“Older people need those antibodies up high because they’re more susceptible to severe breakthroughs,” she said, also before the latest development.
To boost or not to boost
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham & Women’s Hospital in Boston, said the timing of a booster and who should be eligible depends on what the nation is trying to achieve with its vaccination strategy.
“Is the goal to prevent any symptomatic infection with COVID-19, is the goal to prevent the spread of COVID-19, or is the goal to prevent severe disease that requires hospitalization?” asked Dr. Kuritzkes.
The current vaccine — with a booster — has prevented severe disease, he said.
An Israeli study showed, for instance, that a third Pfizer dose was 93% effective against hospitalization, 92% effective against severe illness, and 81% effective against death.
A just-published study in the New England Journal of Medicine found that a booster of the Pfizer vaccine was 95% effective against COVID-19 infection and that it did not raise any new safety issues.
A small Israeli study, also published in NEJM, of a fourth Pfizer dose given to health care workers found that it prevented symptomatic infection and illness, but that it was much less effective than previous doses — maybe 65% effective against symptomatic illness, the authors write.
Giving Americans another booster now — which has been shown to lose some effectiveness after about 4 months — means it might not offer protection this fall and winter, when there could be a seasonal surge of the virus, Dr. Kuritzkes says.
And, even if people receive boosters every few months, they are still likely to get a mild respiratory virus infection, he said.
“I’m pretty convinced that we cannot boost ourselves out of this pandemic,” said Dr. Kuritzkes. “We need to first of all ensure there’s global immunization so that all the people who have not been vaccinated at all get vaccinated. That’s far more important than boosting people a fourth time.”
Booster confusion
The April 6 FDA meeting of the agency’s Vaccines and Related Biological Products Advisory Committee comes as the two major COVID vaccine makers — Pfizer and Moderna — have applied for emergency use authorization for an additional booster.
Pfizer had asked for authorization for a fourth shot in patients over age 65 years, while Moderna wanted a booster to be available to all Americans over 18. The FDA instead granted authorization to both companies for those over 50 and anyone 18 or older who is immunocompromised.
What this means for the committee’s April 6 meeting is not clear. The original agenda says the committee will consider the evidence on safety and effectiveness of the additional vaccine doses and discuss how to set up a process — similar to that used for the influenza vaccine — to be able to determine the makeup of COVID vaccines as new variants emerge. That could lay the groundwork for an annual COVID shot, if needed.
The FDA advisers will not make recommendations nor vote on whether — and which — Americans should get a COVID booster. That is the job of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The last time a booster was considered, CDC Director Rochelle Walensky, MD, overrode the committee and recommended that all Americans — not just older individuals — get an additional COVID shot, which became the first booster.
That past action worries Dr. Gandhi, who calls it confusing, and says it may have contributed to the fact that less than half of Americans have since chosen to get a booster.
Dr. Schaffner says he expects the FDA to authorize emergency use for fourth doses of the Pfizer and Moderna vaccines, but he doesn’t think the CDC committee will recommend routine use. As was seen before, however, the CDC director does not have to follow the committee’s advice.
The members of ACIP “might be more conservative or narrower in scope in terms of recommending who needs to be boosted and when boosting is appropriate,” Dr. Kuritzkes says.
Dr. Gandhi says she’s concerned the FDA’s deliberations could be swayed by Moderna and Pfizer’s influence and that “pharmaceutical companies are going to have more of a say than they should in the scientific process.”
There are similar worries for Dr. Schaffner. He says he’s “a bit grumpy” that the vaccine makers have been using press releases to argue for boosters.
“Press releases are no way to make vaccine recommendations,” Dr. Schaffner said, adding that he “would advise [vaccine makers] to sit down and be quiet and let the FDA and CDC advisory committee do their thing.”
Moderna Chief Medical Officer Paul Burton, MD, however, told WebMD last week that the signs point to why a fourth shot may be needed.
“We see waning of effectiveness, antibody levels come down, and certainly effectiveness against Omicron comes down in 3 to 6 months,” Burton said. “The natural history, from what we’re seeing around the world, is that BA.2 is definitely here, it’s highly transmissible, and I think we are going to get an additional wave of BA.2 here in the United States.”
Another wave is coming, he said, and “I think there will be waning of effectiveness. We need to be prepared for that, so that’s why we need the fourth dose.”
Supply issues?
Meanwhile, the United Kingdom has begun offering boosters to anyone over 75, and Sweden’s health authority has recommended a fourth shot to people over age 80.
That puts pressure on the United States — at least on its politicians and policymakers — to, in a sense, keep up, said the infectious disease specialists.
Indeed, the White House has been keeping fourth shots in the news, warning that it is running out of money to ensure that all Americans would have access to one, if recommended.
On March 23, outgoing White House COVID-19 Response Coordinator Jeff Zients said the federal government had enough vaccine for the immunocompromised to get a fourth dose “and, if authorized in the coming weeks, enough supply for fourth doses for our most vulnerable, including seniors.”
But he warned that without congressional approval of a COVID-19 funding package, “We can’t procure the necessary vaccine supply to support fourth shots for all Americans.”
Mr. Zients also noted that other countries, including Japan, Vietnam, and the Philippines had already secured future booster doses and added, “We should be securing additional supply right now.”
Dr. Schaffner says that while it would be nice to “have a booster on the shelf,” the United States needs to put more effort into creating a globally-coordinated process for ensuring that vaccines match circulating strains and that they are manufactured on a timely basis.
He says he and others “have been reminding the public that the COVID pandemic may indeed be diminishing and moving into the endemic, but that doesn’t mean COVID is over or finished or disappeared.”
Dr. Schaffner says that it may be that “perhaps we’d need a periodic reminder to our immune system to remain protected. In other words, we might have to get boosted perhaps annually like we do with influenza.”
A version of this article first appeared on WebMD.com.
, even though many top infectious disease experts questioned the need before the agency’s decision.
The FDA granted emergency use authorization for both Pfizer and Moderna to offer the second booster – and fourth shot overall – for adults over 50 as well as those over 18 with compromised immune systems.
The Centers for Control and Prevention must still sign off before those doses start reaching American arms. That approval could come at any time.
“The general consensus, certainly the CDC’s consensus, is that the current vaccines are still really quite effective against Omicron and this new BA.2 variant in keeping people out of the hospital, and preventing the development of severe disease,” William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville said prior to the FDA’s announcement March 29.
Of the 217.4 million Americans who are “fully vaccinated,” i.e., received two doses of either Pfizer or Moderna’s vaccines or one dose of the Johnson & Johnson vaccine, only 45% have also received a booster shot, according to the CDC.
“Given that, there’s no need at the moment for the general population to get a fourth inoculation,” Dr. Schaffner says. “Our current focus ought to be on making sure that as many people as possible get that [first] booster who are eligible.”
Monica Gandhi, MD, an infectious disease specialist at the University of California, San Francisco, agreed that another booster for everyone was unnecessary. The only people who would need a fourth shot (or third, if they had the Johnson & Johnson vaccine initially) are those over age 65 or 70 years, Dr. Gandhi says.
“Older people need those antibodies up high because they’re more susceptible to severe breakthroughs,” she said, also before the latest development.
To boost or not to boost
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham & Women’s Hospital in Boston, said the timing of a booster and who should be eligible depends on what the nation is trying to achieve with its vaccination strategy.
“Is the goal to prevent any symptomatic infection with COVID-19, is the goal to prevent the spread of COVID-19, or is the goal to prevent severe disease that requires hospitalization?” asked Dr. Kuritzkes.
The current vaccine — with a booster — has prevented severe disease, he said.
An Israeli study showed, for instance, that a third Pfizer dose was 93% effective against hospitalization, 92% effective against severe illness, and 81% effective against death.
A just-published study in the New England Journal of Medicine found that a booster of the Pfizer vaccine was 95% effective against COVID-19 infection and that it did not raise any new safety issues.
A small Israeli study, also published in NEJM, of a fourth Pfizer dose given to health care workers found that it prevented symptomatic infection and illness, but that it was much less effective than previous doses — maybe 65% effective against symptomatic illness, the authors write.
Giving Americans another booster now — which has been shown to lose some effectiveness after about 4 months — means it might not offer protection this fall and winter, when there could be a seasonal surge of the virus, Dr. Kuritzkes says.
And, even if people receive boosters every few months, they are still likely to get a mild respiratory virus infection, he said.
“I’m pretty convinced that we cannot boost ourselves out of this pandemic,” said Dr. Kuritzkes. “We need to first of all ensure there’s global immunization so that all the people who have not been vaccinated at all get vaccinated. That’s far more important than boosting people a fourth time.”
Booster confusion
The April 6 FDA meeting of the agency’s Vaccines and Related Biological Products Advisory Committee comes as the two major COVID vaccine makers — Pfizer and Moderna — have applied for emergency use authorization for an additional booster.
Pfizer had asked for authorization for a fourth shot in patients over age 65 years, while Moderna wanted a booster to be available to all Americans over 18. The FDA instead granted authorization to both companies for those over 50 and anyone 18 or older who is immunocompromised.
What this means for the committee’s April 6 meeting is not clear. The original agenda says the committee will consider the evidence on safety and effectiveness of the additional vaccine doses and discuss how to set up a process — similar to that used for the influenza vaccine — to be able to determine the makeup of COVID vaccines as new variants emerge. That could lay the groundwork for an annual COVID shot, if needed.
The FDA advisers will not make recommendations nor vote on whether — and which — Americans should get a COVID booster. That is the job of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The last time a booster was considered, CDC Director Rochelle Walensky, MD, overrode the committee and recommended that all Americans — not just older individuals — get an additional COVID shot, which became the first booster.
That past action worries Dr. Gandhi, who calls it confusing, and says it may have contributed to the fact that less than half of Americans have since chosen to get a booster.
Dr. Schaffner says he expects the FDA to authorize emergency use for fourth doses of the Pfizer and Moderna vaccines, but he doesn’t think the CDC committee will recommend routine use. As was seen before, however, the CDC director does not have to follow the committee’s advice.
The members of ACIP “might be more conservative or narrower in scope in terms of recommending who needs to be boosted and when boosting is appropriate,” Dr. Kuritzkes says.
Dr. Gandhi says she’s concerned the FDA’s deliberations could be swayed by Moderna and Pfizer’s influence and that “pharmaceutical companies are going to have more of a say than they should in the scientific process.”
There are similar worries for Dr. Schaffner. He says he’s “a bit grumpy” that the vaccine makers have been using press releases to argue for boosters.
“Press releases are no way to make vaccine recommendations,” Dr. Schaffner said, adding that he “would advise [vaccine makers] to sit down and be quiet and let the FDA and CDC advisory committee do their thing.”
Moderna Chief Medical Officer Paul Burton, MD, however, told WebMD last week that the signs point to why a fourth shot may be needed.
“We see waning of effectiveness, antibody levels come down, and certainly effectiveness against Omicron comes down in 3 to 6 months,” Burton said. “The natural history, from what we’re seeing around the world, is that BA.2 is definitely here, it’s highly transmissible, and I think we are going to get an additional wave of BA.2 here in the United States.”
Another wave is coming, he said, and “I think there will be waning of effectiveness. We need to be prepared for that, so that’s why we need the fourth dose.”
Supply issues?
Meanwhile, the United Kingdom has begun offering boosters to anyone over 75, and Sweden’s health authority has recommended a fourth shot to people over age 80.
That puts pressure on the United States — at least on its politicians and policymakers — to, in a sense, keep up, said the infectious disease specialists.
Indeed, the White House has been keeping fourth shots in the news, warning that it is running out of money to ensure that all Americans would have access to one, if recommended.
On March 23, outgoing White House COVID-19 Response Coordinator Jeff Zients said the federal government had enough vaccine for the immunocompromised to get a fourth dose “and, if authorized in the coming weeks, enough supply for fourth doses for our most vulnerable, including seniors.”
But he warned that without congressional approval of a COVID-19 funding package, “We can’t procure the necessary vaccine supply to support fourth shots for all Americans.”
Mr. Zients also noted that other countries, including Japan, Vietnam, and the Philippines had already secured future booster doses and added, “We should be securing additional supply right now.”
Dr. Schaffner says that while it would be nice to “have a booster on the shelf,” the United States needs to put more effort into creating a globally-coordinated process for ensuring that vaccines match circulating strains and that they are manufactured on a timely basis.
He says he and others “have been reminding the public that the COVID pandemic may indeed be diminishing and moving into the endemic, but that doesn’t mean COVID is over or finished or disappeared.”
Dr. Schaffner says that it may be that “perhaps we’d need a periodic reminder to our immune system to remain protected. In other words, we might have to get boosted perhaps annually like we do with influenza.”
A version of this article first appeared on WebMD.com.
Aluminum named allergen of the year
BOSTON – The . Aluminum salts, which are the major cause of allergic reactions, are “ubiquitous,” Donald Belsito, MD, professor of dermatology at Columbia University, New York, said at the annual meeting of the American Contact Dermatitis Society.
These salts can be found in sunscreen, cosmetics, dental restorations, and food, to name a few, though the most commonly identified reactions are from aluminum hydroxide, which can be found in some vaccines or preparations for allergen-specific immunotherapy. “It’s the aluminum hydroxide that seems to be more allergenic than other aluminum salts,” Dr. Belsito said in an interview.
“It’s not a dangerous allergy; It’s not a threat,” he said, “but it’s something that dermatologists need to be aware of.”
These reactions normally present as itchy nodules that can last for months and even years, like some reactions from patch testing. “We’re not talking about a vaccine allergy in such a way where people are getting anaphylaxis,” JiaDe Yu, MD, a pediatric dermatologist specializing in allergic contact dermatitis at Massachusetts General Hospital, Boston, said in an interview. “An itchy rash is what we tend to see.”
There have also been occasional reports of atopic dermatitis from aluminum in antiperspirants, astringents, as well as from the metallic aluminum.
Dr. Yu noted that aluminum allergies are not thought to be very common, but the overall prevalence is not known. Studies do suggest, however, that the allergy may be more prevalent in children. In one recent study in Sweden, 5% of children and 0.9% of adults who underwent patch testing had an aluminum contact allergy.
Recommendations for testing
Aluminum is not included in baseline patch testing in the United States, though a recent report about the allergen in the journal Dermatitis argued for its inclusion for pediatric patch testing. Both Dr. Belsito and Dr. Yu agreed that the best approach is to do targeted testing. “If there is a suspicion for it, absolutely test for it,” Dr. Yu said, but if a patient comes in with something like eyelid dermatitis or a rash after a hair care appointment, an aluminum allergy is not very likely.
Because aluminum is also present in Finn Chambers for patch testing, Dr. Belsito advised using plastic chambers in people suspected of having an aluminum allergy. He now uses only plastic chambers in children, he said, as some patients have had reactions to the Finn Chambers even if they have no history of reactions to vaccines or other aluminum-containing products.
While aluminum chloride hexahydrate (ACH) 2% in petrolatum is the commercially available preparation in patch testing, a preparation with ACH 10% is more sensitive, Dr. Belsito said. If a physician strongly suspects an aluminum allergy in a patient but the test with the ACH 2% is negative, he or she should then try a 10% solution, he noted, adding that 7-day readings are also necessary to maximize accuracy.
Vaccine safety
One of the concerns about naming aluminum as the allergen of the year is the potential to cause anxiety around vaccines. “We want to make sure that we’re not giving more fuel to people who have an excuse not to get a vaccine,” Dr. Yu said. “We certainly want to reinforce that fact that it is safe.” Dr. Belsito noted that COVID-19 vaccines do not contain aluminum.
Even on the rare chance that a patient does have a reaction to an aluminum-containing vaccine, these subcutaneous nodules resolve over time, Dr. Belsito said. In his own clinical experience, “99.99% of the time they resolve and there is no residual.” He did add that overreacting to the rash by prescribing injectable steroids can lead to steroid atrophy. In these cases, a topical steroid may be more appropriate.
All unexpected or clinically significant vaccine reactions should be reported to the Vaccine Adverse Event Reporting System, cosponsored by the Centers for Disease Control and Prevention and the Food and Drug Administration. The Clinical Immunization Project Safety Assessment Project, from the CDC, also can provide expertise and advice on aluminum-free alternatives for some vaccines.
Dr. Belsito and Dr. Yu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – The . Aluminum salts, which are the major cause of allergic reactions, are “ubiquitous,” Donald Belsito, MD, professor of dermatology at Columbia University, New York, said at the annual meeting of the American Contact Dermatitis Society.
These salts can be found in sunscreen, cosmetics, dental restorations, and food, to name a few, though the most commonly identified reactions are from aluminum hydroxide, which can be found in some vaccines or preparations for allergen-specific immunotherapy. “It’s the aluminum hydroxide that seems to be more allergenic than other aluminum salts,” Dr. Belsito said in an interview.
“It’s not a dangerous allergy; It’s not a threat,” he said, “but it’s something that dermatologists need to be aware of.”
These reactions normally present as itchy nodules that can last for months and even years, like some reactions from patch testing. “We’re not talking about a vaccine allergy in such a way where people are getting anaphylaxis,” JiaDe Yu, MD, a pediatric dermatologist specializing in allergic contact dermatitis at Massachusetts General Hospital, Boston, said in an interview. “An itchy rash is what we tend to see.”
There have also been occasional reports of atopic dermatitis from aluminum in antiperspirants, astringents, as well as from the metallic aluminum.
Dr. Yu noted that aluminum allergies are not thought to be very common, but the overall prevalence is not known. Studies do suggest, however, that the allergy may be more prevalent in children. In one recent study in Sweden, 5% of children and 0.9% of adults who underwent patch testing had an aluminum contact allergy.
Recommendations for testing
Aluminum is not included in baseline patch testing in the United States, though a recent report about the allergen in the journal Dermatitis argued for its inclusion for pediatric patch testing. Both Dr. Belsito and Dr. Yu agreed that the best approach is to do targeted testing. “If there is a suspicion for it, absolutely test for it,” Dr. Yu said, but if a patient comes in with something like eyelid dermatitis or a rash after a hair care appointment, an aluminum allergy is not very likely.
Because aluminum is also present in Finn Chambers for patch testing, Dr. Belsito advised using plastic chambers in people suspected of having an aluminum allergy. He now uses only plastic chambers in children, he said, as some patients have had reactions to the Finn Chambers even if they have no history of reactions to vaccines or other aluminum-containing products.
While aluminum chloride hexahydrate (ACH) 2% in petrolatum is the commercially available preparation in patch testing, a preparation with ACH 10% is more sensitive, Dr. Belsito said. If a physician strongly suspects an aluminum allergy in a patient but the test with the ACH 2% is negative, he or she should then try a 10% solution, he noted, adding that 7-day readings are also necessary to maximize accuracy.
Vaccine safety
One of the concerns about naming aluminum as the allergen of the year is the potential to cause anxiety around vaccines. “We want to make sure that we’re not giving more fuel to people who have an excuse not to get a vaccine,” Dr. Yu said. “We certainly want to reinforce that fact that it is safe.” Dr. Belsito noted that COVID-19 vaccines do not contain aluminum.
Even on the rare chance that a patient does have a reaction to an aluminum-containing vaccine, these subcutaneous nodules resolve over time, Dr. Belsito said. In his own clinical experience, “99.99% of the time they resolve and there is no residual.” He did add that overreacting to the rash by prescribing injectable steroids can lead to steroid atrophy. In these cases, a topical steroid may be more appropriate.
All unexpected or clinically significant vaccine reactions should be reported to the Vaccine Adverse Event Reporting System, cosponsored by the Centers for Disease Control and Prevention and the Food and Drug Administration. The Clinical Immunization Project Safety Assessment Project, from the CDC, also can provide expertise and advice on aluminum-free alternatives for some vaccines.
Dr. Belsito and Dr. Yu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – The . Aluminum salts, which are the major cause of allergic reactions, are “ubiquitous,” Donald Belsito, MD, professor of dermatology at Columbia University, New York, said at the annual meeting of the American Contact Dermatitis Society.
These salts can be found in sunscreen, cosmetics, dental restorations, and food, to name a few, though the most commonly identified reactions are from aluminum hydroxide, which can be found in some vaccines or preparations for allergen-specific immunotherapy. “It’s the aluminum hydroxide that seems to be more allergenic than other aluminum salts,” Dr. Belsito said in an interview.
“It’s not a dangerous allergy; It’s not a threat,” he said, “but it’s something that dermatologists need to be aware of.”
These reactions normally present as itchy nodules that can last for months and even years, like some reactions from patch testing. “We’re not talking about a vaccine allergy in such a way where people are getting anaphylaxis,” JiaDe Yu, MD, a pediatric dermatologist specializing in allergic contact dermatitis at Massachusetts General Hospital, Boston, said in an interview. “An itchy rash is what we tend to see.”
There have also been occasional reports of atopic dermatitis from aluminum in antiperspirants, astringents, as well as from the metallic aluminum.
Dr. Yu noted that aluminum allergies are not thought to be very common, but the overall prevalence is not known. Studies do suggest, however, that the allergy may be more prevalent in children. In one recent study in Sweden, 5% of children and 0.9% of adults who underwent patch testing had an aluminum contact allergy.
Recommendations for testing
Aluminum is not included in baseline patch testing in the United States, though a recent report about the allergen in the journal Dermatitis argued for its inclusion for pediatric patch testing. Both Dr. Belsito and Dr. Yu agreed that the best approach is to do targeted testing. “If there is a suspicion for it, absolutely test for it,” Dr. Yu said, but if a patient comes in with something like eyelid dermatitis or a rash after a hair care appointment, an aluminum allergy is not very likely.
Because aluminum is also present in Finn Chambers for patch testing, Dr. Belsito advised using plastic chambers in people suspected of having an aluminum allergy. He now uses only plastic chambers in children, he said, as some patients have had reactions to the Finn Chambers even if they have no history of reactions to vaccines or other aluminum-containing products.
While aluminum chloride hexahydrate (ACH) 2% in petrolatum is the commercially available preparation in patch testing, a preparation with ACH 10% is more sensitive, Dr. Belsito said. If a physician strongly suspects an aluminum allergy in a patient but the test with the ACH 2% is negative, he or she should then try a 10% solution, he noted, adding that 7-day readings are also necessary to maximize accuracy.
Vaccine safety
One of the concerns about naming aluminum as the allergen of the year is the potential to cause anxiety around vaccines. “We want to make sure that we’re not giving more fuel to people who have an excuse not to get a vaccine,” Dr. Yu said. “We certainly want to reinforce that fact that it is safe.” Dr. Belsito noted that COVID-19 vaccines do not contain aluminum.
Even on the rare chance that a patient does have a reaction to an aluminum-containing vaccine, these subcutaneous nodules resolve over time, Dr. Belsito said. In his own clinical experience, “99.99% of the time they resolve and there is no residual.” He did add that overreacting to the rash by prescribing injectable steroids can lead to steroid atrophy. In these cases, a topical steroid may be more appropriate.
All unexpected or clinically significant vaccine reactions should be reported to the Vaccine Adverse Event Reporting System, cosponsored by the Centers for Disease Control and Prevention and the Food and Drug Administration. The Clinical Immunization Project Safety Assessment Project, from the CDC, also can provide expertise and advice on aluminum-free alternatives for some vaccines.
Dr. Belsito and Dr. Yu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ACDS 2022
Natural, vaccine-induced, and hybrid immunity to COVID-19
Seroprevalence surveys suggest that, from the beginning of the pandemic to 2022, more than a third of the global population had been infected with SARS-CoV-2. As large numbers of people continue to be infected, the efficacy and duration of natural immunity, in terms of protection against SARS-CoV-2 reinfections and severe disease, are of crucial significance. The virus’s epidemiologic trajectory will be influenced by the trends in vaccine-induced and hybrid immunity.
Omicron’s immune evasion
Cases of SARS-CoV-2 reinfection are increasing around the world. According to data from the U.K. Health Security Agency, 650,000 people in England have been infected twice, and most of them were reinfected in the past 2 months. Before mid-November 2021, reinfections accounted for about 1% of reported cases, but the rate has now increased to around 10%. The reinfection risk was 16 times higher between mid-December 2021 and early January 2022. Experts believe that this spike in reinfections is related to the spread of Omicron, which overtook Delta as the dominant variant. Nonetheless, other aspects should also be considered.
Omicron’s greater propensity to spread is not unrelated to its ability to evade the body’s immune defenses. This aspect was raised in a letter recently published in the New England Journal of Medicine. The authors reported that the effectiveness of previous infection in preventing reinfection against the Alpha, Beta, and Delta variants was around 90%, but it was only 56% against Omicron.
Natural immunity
Natural immunity showed roughly similar effectiveness regarding protection against reinfection across different SARS-CoV-2 variants, with the exception of the Omicron variant. The risk of hospitalization and death was also reduced in SARS-CoV-2 reinfections versus primary infections. Observational studies indicate that natural immunity may offer equal or greater protection against SARS-CoV-2 infections, compared with immunization with two doses of an mRNA vaccine, but the data are not fully consistent.
Natural immunity seems to be relatively long-lasting. Data from Denmark and Austria show no evidence that protection against reinfections wanes after 6 months. Some investigations indicate that protection against reinfection is lowest 4-5 months after initial infection and increases thereafter, a finding that might hypothetically be explained by persistent viral shedding; that is, misclassification of prolonged SARS-CoV-2 infections as reinfections. While no comparison was made against information pertaining to unvaccinated, not previously-infected individuals, preliminary data from Israel suggest that protection from reinfection can decrease from 6 to more than 12 months after the first SARS-CoV-2 infection. Taken together, epidemiologic studies indicate that protection against reinfections by natural immunity lasts over 1 year with only moderate, if any, decline over this period. Among older individuals, immunocompromised patients, and those with certain comorbidities or exposure risk (for example, health care workers), rates of reinfection may be higher. It is plausible that reinfection risk may be a function of exposure risk.
There is accumulating evidence that reinfections may be significantly less severe than primary infections with SARS-CoV-2. Reduced clinical severity of SARS-CoV-2 reinfections naturally also makes sense from a biologic point of view, inasmuch as a previously primed immune system should be better prepared for a rechallenge with this virus.
Vaccine-induced immunity
The short-term (<4 months) efficacy of mRNA vaccines against SARS-CoV-2 is high and varies from 94.1% (Moderna) to 95% (BioNTech/Pfizer). This has been confirmed by randomized controlled trials and was subsequently confirmed in effectiveness studies in real-world settings. Waning efficacy was observed with respect to protection against SARS-CoV-2 infections (for example, only approximately 20% after about half a year in Qatar), whereas protection against severe disease was either sustained or showed only a moderate decline.
In individuals who received two doses of the BioNTech/Pfizer vaccine at least 5 months earlier, an additional vaccine dose, a so-called booster, significantly lowered mortality and severe illness. These findings suggest that the booster restored and probably exceeded the initial short-term efficacy of the initial vaccination.
Data are still emerging regarding the efficacy of boosters against the Omicron variants. Preliminary data suggest a far lower ability to restore protection from infection and vaccination. However, fatalities and hospitalizations remain low.
Natural immunity vs. vaccine-induced immunity
Comparisons of natural immunity with vaccine-induced immunity are complicated by a series of biases and by combinations of biases – for example, the biases of comparisons between infected and uninfected, plus the biases of comparisons between vaccinated and nonvaccinated, with strong potential selection biases and confounding. Of particular note, the proportion of people previously infected and/or vaccinated may influence estimates of effectiveness. Regarding this point, one study compared unvaccinated patients with a prior SARS-CoV-2 infection and vaccinated individuals followed up from a week after the second vaccine dose onward versus a group of unvaccinated, not previously infected individuals. The findings showed that, compared with unvaccinated, not previously infected individuals, the natural immunity group and the vaccinated group had similar protection of 94.8% and 92.8% against infection, of 94.1% and 94.2% against hospitalization, and of 96.4% and 94.4% against severe illness, respectively.
Hybrid immunity
The combination of a previous SARS-CoV-2 infection and a respective vaccination is called hybrid immunity. This combination seems to confer the greatest protection against SARS-CoV-2 infections, but several knowledge gaps remain regarding this issue.
Data from Israel showed that, when the time since the last immunity-conferring event (either primary infection or vaccination) was the same, the rates of SARS-CoV-2 infections were similar in the following groups: individuals who had a previous infection and no vaccination, individuals who had an infection and were then vaccinated with a single dose after at least 3 months, and individuals who were vaccinated (two doses) and then infected. Severe disease was relatively rare overall.
Data on the efficacy of hybrid immunity point in the direction of hybrid immunity being superior, as compared with either vaccine-induced (without a booster) immunity or natural immunity alone. Timing and mode of vaccination of previously infected individuals to achieve optimal hybrid immunity are central questions that remain to be addressed in future studies.
Given that vaccination rates are continuously increasing and that, by the beginning of 2022, perhaps half or more of the global population had already been infected with SARS-CoV-2, with the vast majority of this group not being officially detected, it would appear logical that future infection waves, even with highly transmissible variants of SARS-CoV-2, may be limited with respect to their maximum potential health burden. The advent of Omicron suggests that massive surges can occur even in populations with extremely high rates of previous vaccination and variable rates of prior infections. However, even then, the accompanying burden of hospitalizations and deaths is far less than what was seen in 2020 and 2021. One may argue that the pandemic has already transitioned to the endemic phase and that Omicron is an endemic wave occurring in the setting of already widespread population immunity.
A version of this article first appeared on Medscape.com.
Seroprevalence surveys suggest that, from the beginning of the pandemic to 2022, more than a third of the global population had been infected with SARS-CoV-2. As large numbers of people continue to be infected, the efficacy and duration of natural immunity, in terms of protection against SARS-CoV-2 reinfections and severe disease, are of crucial significance. The virus’s epidemiologic trajectory will be influenced by the trends in vaccine-induced and hybrid immunity.
Omicron’s immune evasion
Cases of SARS-CoV-2 reinfection are increasing around the world. According to data from the U.K. Health Security Agency, 650,000 people in England have been infected twice, and most of them were reinfected in the past 2 months. Before mid-November 2021, reinfections accounted for about 1% of reported cases, but the rate has now increased to around 10%. The reinfection risk was 16 times higher between mid-December 2021 and early January 2022. Experts believe that this spike in reinfections is related to the spread of Omicron, which overtook Delta as the dominant variant. Nonetheless, other aspects should also be considered.
Omicron’s greater propensity to spread is not unrelated to its ability to evade the body’s immune defenses. This aspect was raised in a letter recently published in the New England Journal of Medicine. The authors reported that the effectiveness of previous infection in preventing reinfection against the Alpha, Beta, and Delta variants was around 90%, but it was only 56% against Omicron.
Natural immunity
Natural immunity showed roughly similar effectiveness regarding protection against reinfection across different SARS-CoV-2 variants, with the exception of the Omicron variant. The risk of hospitalization and death was also reduced in SARS-CoV-2 reinfections versus primary infections. Observational studies indicate that natural immunity may offer equal or greater protection against SARS-CoV-2 infections, compared with immunization with two doses of an mRNA vaccine, but the data are not fully consistent.
Natural immunity seems to be relatively long-lasting. Data from Denmark and Austria show no evidence that protection against reinfections wanes after 6 months. Some investigations indicate that protection against reinfection is lowest 4-5 months after initial infection and increases thereafter, a finding that might hypothetically be explained by persistent viral shedding; that is, misclassification of prolonged SARS-CoV-2 infections as reinfections. While no comparison was made against information pertaining to unvaccinated, not previously-infected individuals, preliminary data from Israel suggest that protection from reinfection can decrease from 6 to more than 12 months after the first SARS-CoV-2 infection. Taken together, epidemiologic studies indicate that protection against reinfections by natural immunity lasts over 1 year with only moderate, if any, decline over this period. Among older individuals, immunocompromised patients, and those with certain comorbidities or exposure risk (for example, health care workers), rates of reinfection may be higher. It is plausible that reinfection risk may be a function of exposure risk.
There is accumulating evidence that reinfections may be significantly less severe than primary infections with SARS-CoV-2. Reduced clinical severity of SARS-CoV-2 reinfections naturally also makes sense from a biologic point of view, inasmuch as a previously primed immune system should be better prepared for a rechallenge with this virus.
Vaccine-induced immunity
The short-term (<4 months) efficacy of mRNA vaccines against SARS-CoV-2 is high and varies from 94.1% (Moderna) to 95% (BioNTech/Pfizer). This has been confirmed by randomized controlled trials and was subsequently confirmed in effectiveness studies in real-world settings. Waning efficacy was observed with respect to protection against SARS-CoV-2 infections (for example, only approximately 20% after about half a year in Qatar), whereas protection against severe disease was either sustained or showed only a moderate decline.
In individuals who received two doses of the BioNTech/Pfizer vaccine at least 5 months earlier, an additional vaccine dose, a so-called booster, significantly lowered mortality and severe illness. These findings suggest that the booster restored and probably exceeded the initial short-term efficacy of the initial vaccination.
Data are still emerging regarding the efficacy of boosters against the Omicron variants. Preliminary data suggest a far lower ability to restore protection from infection and vaccination. However, fatalities and hospitalizations remain low.
Natural immunity vs. vaccine-induced immunity
Comparisons of natural immunity with vaccine-induced immunity are complicated by a series of biases and by combinations of biases – for example, the biases of comparisons between infected and uninfected, plus the biases of comparisons between vaccinated and nonvaccinated, with strong potential selection biases and confounding. Of particular note, the proportion of people previously infected and/or vaccinated may influence estimates of effectiveness. Regarding this point, one study compared unvaccinated patients with a prior SARS-CoV-2 infection and vaccinated individuals followed up from a week after the second vaccine dose onward versus a group of unvaccinated, not previously infected individuals. The findings showed that, compared with unvaccinated, not previously infected individuals, the natural immunity group and the vaccinated group had similar protection of 94.8% and 92.8% against infection, of 94.1% and 94.2% against hospitalization, and of 96.4% and 94.4% against severe illness, respectively.
Hybrid immunity
The combination of a previous SARS-CoV-2 infection and a respective vaccination is called hybrid immunity. This combination seems to confer the greatest protection against SARS-CoV-2 infections, but several knowledge gaps remain regarding this issue.
Data from Israel showed that, when the time since the last immunity-conferring event (either primary infection or vaccination) was the same, the rates of SARS-CoV-2 infections were similar in the following groups: individuals who had a previous infection and no vaccination, individuals who had an infection and were then vaccinated with a single dose after at least 3 months, and individuals who were vaccinated (two doses) and then infected. Severe disease was relatively rare overall.
Data on the efficacy of hybrid immunity point in the direction of hybrid immunity being superior, as compared with either vaccine-induced (without a booster) immunity or natural immunity alone. Timing and mode of vaccination of previously infected individuals to achieve optimal hybrid immunity are central questions that remain to be addressed in future studies.
Given that vaccination rates are continuously increasing and that, by the beginning of 2022, perhaps half or more of the global population had already been infected with SARS-CoV-2, with the vast majority of this group not being officially detected, it would appear logical that future infection waves, even with highly transmissible variants of SARS-CoV-2, may be limited with respect to their maximum potential health burden. The advent of Omicron suggests that massive surges can occur even in populations with extremely high rates of previous vaccination and variable rates of prior infections. However, even then, the accompanying burden of hospitalizations and deaths is far less than what was seen in 2020 and 2021. One may argue that the pandemic has already transitioned to the endemic phase and that Omicron is an endemic wave occurring in the setting of already widespread population immunity.
A version of this article first appeared on Medscape.com.
Seroprevalence surveys suggest that, from the beginning of the pandemic to 2022, more than a third of the global population had been infected with SARS-CoV-2. As large numbers of people continue to be infected, the efficacy and duration of natural immunity, in terms of protection against SARS-CoV-2 reinfections and severe disease, are of crucial significance. The virus’s epidemiologic trajectory will be influenced by the trends in vaccine-induced and hybrid immunity.
Omicron’s immune evasion
Cases of SARS-CoV-2 reinfection are increasing around the world. According to data from the U.K. Health Security Agency, 650,000 people in England have been infected twice, and most of them were reinfected in the past 2 months. Before mid-November 2021, reinfections accounted for about 1% of reported cases, but the rate has now increased to around 10%. The reinfection risk was 16 times higher between mid-December 2021 and early January 2022. Experts believe that this spike in reinfections is related to the spread of Omicron, which overtook Delta as the dominant variant. Nonetheless, other aspects should also be considered.
Omicron’s greater propensity to spread is not unrelated to its ability to evade the body’s immune defenses. This aspect was raised in a letter recently published in the New England Journal of Medicine. The authors reported that the effectiveness of previous infection in preventing reinfection against the Alpha, Beta, and Delta variants was around 90%, but it was only 56% against Omicron.
Natural immunity
Natural immunity showed roughly similar effectiveness regarding protection against reinfection across different SARS-CoV-2 variants, with the exception of the Omicron variant. The risk of hospitalization and death was also reduced in SARS-CoV-2 reinfections versus primary infections. Observational studies indicate that natural immunity may offer equal or greater protection against SARS-CoV-2 infections, compared with immunization with two doses of an mRNA vaccine, but the data are not fully consistent.
Natural immunity seems to be relatively long-lasting. Data from Denmark and Austria show no evidence that protection against reinfections wanes after 6 months. Some investigations indicate that protection against reinfection is lowest 4-5 months after initial infection and increases thereafter, a finding that might hypothetically be explained by persistent viral shedding; that is, misclassification of prolonged SARS-CoV-2 infections as reinfections. While no comparison was made against information pertaining to unvaccinated, not previously-infected individuals, preliminary data from Israel suggest that protection from reinfection can decrease from 6 to more than 12 months after the first SARS-CoV-2 infection. Taken together, epidemiologic studies indicate that protection against reinfections by natural immunity lasts over 1 year with only moderate, if any, decline over this period. Among older individuals, immunocompromised patients, and those with certain comorbidities or exposure risk (for example, health care workers), rates of reinfection may be higher. It is plausible that reinfection risk may be a function of exposure risk.
There is accumulating evidence that reinfections may be significantly less severe than primary infections with SARS-CoV-2. Reduced clinical severity of SARS-CoV-2 reinfections naturally also makes sense from a biologic point of view, inasmuch as a previously primed immune system should be better prepared for a rechallenge with this virus.
Vaccine-induced immunity
The short-term (<4 months) efficacy of mRNA vaccines against SARS-CoV-2 is high and varies from 94.1% (Moderna) to 95% (BioNTech/Pfizer). This has been confirmed by randomized controlled trials and was subsequently confirmed in effectiveness studies in real-world settings. Waning efficacy was observed with respect to protection against SARS-CoV-2 infections (for example, only approximately 20% after about half a year in Qatar), whereas protection against severe disease was either sustained or showed only a moderate decline.
In individuals who received two doses of the BioNTech/Pfizer vaccine at least 5 months earlier, an additional vaccine dose, a so-called booster, significantly lowered mortality and severe illness. These findings suggest that the booster restored and probably exceeded the initial short-term efficacy of the initial vaccination.
Data are still emerging regarding the efficacy of boosters against the Omicron variants. Preliminary data suggest a far lower ability to restore protection from infection and vaccination. However, fatalities and hospitalizations remain low.
Natural immunity vs. vaccine-induced immunity
Comparisons of natural immunity with vaccine-induced immunity are complicated by a series of biases and by combinations of biases – for example, the biases of comparisons between infected and uninfected, plus the biases of comparisons between vaccinated and nonvaccinated, with strong potential selection biases and confounding. Of particular note, the proportion of people previously infected and/or vaccinated may influence estimates of effectiveness. Regarding this point, one study compared unvaccinated patients with a prior SARS-CoV-2 infection and vaccinated individuals followed up from a week after the second vaccine dose onward versus a group of unvaccinated, not previously infected individuals. The findings showed that, compared with unvaccinated, not previously infected individuals, the natural immunity group and the vaccinated group had similar protection of 94.8% and 92.8% against infection, of 94.1% and 94.2% against hospitalization, and of 96.4% and 94.4% against severe illness, respectively.
Hybrid immunity
The combination of a previous SARS-CoV-2 infection and a respective vaccination is called hybrid immunity. This combination seems to confer the greatest protection against SARS-CoV-2 infections, but several knowledge gaps remain regarding this issue.
Data from Israel showed that, when the time since the last immunity-conferring event (either primary infection or vaccination) was the same, the rates of SARS-CoV-2 infections were similar in the following groups: individuals who had a previous infection and no vaccination, individuals who had an infection and were then vaccinated with a single dose after at least 3 months, and individuals who were vaccinated (two doses) and then infected. Severe disease was relatively rare overall.
Data on the efficacy of hybrid immunity point in the direction of hybrid immunity being superior, as compared with either vaccine-induced (without a booster) immunity or natural immunity alone. Timing and mode of vaccination of previously infected individuals to achieve optimal hybrid immunity are central questions that remain to be addressed in future studies.
Given that vaccination rates are continuously increasing and that, by the beginning of 2022, perhaps half or more of the global population had already been infected with SARS-CoV-2, with the vast majority of this group not being officially detected, it would appear logical that future infection waves, even with highly transmissible variants of SARS-CoV-2, may be limited with respect to their maximum potential health burden. The advent of Omicron suggests that massive surges can occur even in populations with extremely high rates of previous vaccination and variable rates of prior infections. However, even then, the accompanying burden of hospitalizations and deaths is far less than what was seen in 2020 and 2021. One may argue that the pandemic has already transitioned to the endemic phase and that Omicron is an endemic wave occurring in the setting of already widespread population immunity.
A version of this article first appeared on Medscape.com.
Moderna reports positive COVID-19 vaccine response in kids down to 6 months
Moderna on March 23 released interim results indicating that its mRNA-1273 COVID vaccine produced “robust” neutralizing antibody titers in children aged 6 months to 6 years – levels similar to those seen in adults.
Vaccine efficacy against infection was 43.7% in children aged 6 months to 2 years and 37.5% among children aged 2-6 years, the new data from its phase 2/3 KidCOVE study show.
The company explained the lower efficacy numbers by noting that its study involving these younger children was conducted during the Omicron wave. The same decrease in efficacy against infection was reported in adults during the Omicron surge.
A majority of COVID-19 cases were mild in the approximately 6,900 children aged 6 months to 6 years in the study. No severe COVID-19 cases, hospitalizations, or deaths were reported.
The primary series of two 25-mcg doses of the vaccine given 28 days apart was generally well tolerated. Most adverse events were mild to moderate. For example, temperature greater than 38° C (>100.4° F) was reported for 17.0% of the 6-month-old to 2-year-old group and for 14.6% of the 2- to 6-year-old group. A few children, 0.2% of each group, experienced a temperature greater than 40° C (>104° F).
Moderna plans to include these response, efficacy, and safety data in an application to the Food and Drug Administration for emergency use authorization (EUA) of the vaccine in these younger children in the coming weeks.
“We now have clinical data on the performance of our vaccine from infants 6 months of age through older adults,” Moderna CEO Stephane Bancel said in a news release. He described the interim results as “good news for parents of children under 6 years of age.”
In other news
Moderna also announced that it began the FDA EUA submission process for a 50-μg two-dose primary series for children aged 6-12 years.
The company is also updating its EUA submission for a 100-mcg two-dose primary series for children and adolescents aged 12-18 years.
Similar to its booster research in adults, Moderna plans to evaluate the potential of a booster dose for all pediatric populations, including those aged 6 months to 6 years, 6-12 years, and adolescents. The company is evaluating both a booster dose of mRNA-1273 and its bivalent booster candidate (mRNA1273.214), which includes an Omicron variant booster and mRNA-1273.
A version of this article first appeared on Medscape.com.
Moderna on March 23 released interim results indicating that its mRNA-1273 COVID vaccine produced “robust” neutralizing antibody titers in children aged 6 months to 6 years – levels similar to those seen in adults.
Vaccine efficacy against infection was 43.7% in children aged 6 months to 2 years and 37.5% among children aged 2-6 years, the new data from its phase 2/3 KidCOVE study show.
The company explained the lower efficacy numbers by noting that its study involving these younger children was conducted during the Omicron wave. The same decrease in efficacy against infection was reported in adults during the Omicron surge.
A majority of COVID-19 cases were mild in the approximately 6,900 children aged 6 months to 6 years in the study. No severe COVID-19 cases, hospitalizations, or deaths were reported.
The primary series of two 25-mcg doses of the vaccine given 28 days apart was generally well tolerated. Most adverse events were mild to moderate. For example, temperature greater than 38° C (>100.4° F) was reported for 17.0% of the 6-month-old to 2-year-old group and for 14.6% of the 2- to 6-year-old group. A few children, 0.2% of each group, experienced a temperature greater than 40° C (>104° F).
Moderna plans to include these response, efficacy, and safety data in an application to the Food and Drug Administration for emergency use authorization (EUA) of the vaccine in these younger children in the coming weeks.
“We now have clinical data on the performance of our vaccine from infants 6 months of age through older adults,” Moderna CEO Stephane Bancel said in a news release. He described the interim results as “good news for parents of children under 6 years of age.”
In other news
Moderna also announced that it began the FDA EUA submission process for a 50-μg two-dose primary series for children aged 6-12 years.
The company is also updating its EUA submission for a 100-mcg two-dose primary series for children and adolescents aged 12-18 years.
Similar to its booster research in adults, Moderna plans to evaluate the potential of a booster dose for all pediatric populations, including those aged 6 months to 6 years, 6-12 years, and adolescents. The company is evaluating both a booster dose of mRNA-1273 and its bivalent booster candidate (mRNA1273.214), which includes an Omicron variant booster and mRNA-1273.
A version of this article first appeared on Medscape.com.
Moderna on March 23 released interim results indicating that its mRNA-1273 COVID vaccine produced “robust” neutralizing antibody titers in children aged 6 months to 6 years – levels similar to those seen in adults.
Vaccine efficacy against infection was 43.7% in children aged 6 months to 2 years and 37.5% among children aged 2-6 years, the new data from its phase 2/3 KidCOVE study show.
The company explained the lower efficacy numbers by noting that its study involving these younger children was conducted during the Omicron wave. The same decrease in efficacy against infection was reported in adults during the Omicron surge.
A majority of COVID-19 cases were mild in the approximately 6,900 children aged 6 months to 6 years in the study. No severe COVID-19 cases, hospitalizations, or deaths were reported.
The primary series of two 25-mcg doses of the vaccine given 28 days apart was generally well tolerated. Most adverse events were mild to moderate. For example, temperature greater than 38° C (>100.4° F) was reported for 17.0% of the 6-month-old to 2-year-old group and for 14.6% of the 2- to 6-year-old group. A few children, 0.2% of each group, experienced a temperature greater than 40° C (>104° F).
Moderna plans to include these response, efficacy, and safety data in an application to the Food and Drug Administration for emergency use authorization (EUA) of the vaccine in these younger children in the coming weeks.
“We now have clinical data on the performance of our vaccine from infants 6 months of age through older adults,” Moderna CEO Stephane Bancel said in a news release. He described the interim results as “good news for parents of children under 6 years of age.”
In other news
Moderna also announced that it began the FDA EUA submission process for a 50-μg two-dose primary series for children aged 6-12 years.
The company is also updating its EUA submission for a 100-mcg two-dose primary series for children and adolescents aged 12-18 years.
Similar to its booster research in adults, Moderna plans to evaluate the potential of a booster dose for all pediatric populations, including those aged 6 months to 6 years, 6-12 years, and adolescents. The company is evaluating both a booster dose of mRNA-1273 and its bivalent booster candidate (mRNA1273.214), which includes an Omicron variant booster and mRNA-1273.
A version of this article first appeared on Medscape.com.

