User login
Medtronic recalls HawkOne directional atherectomy system
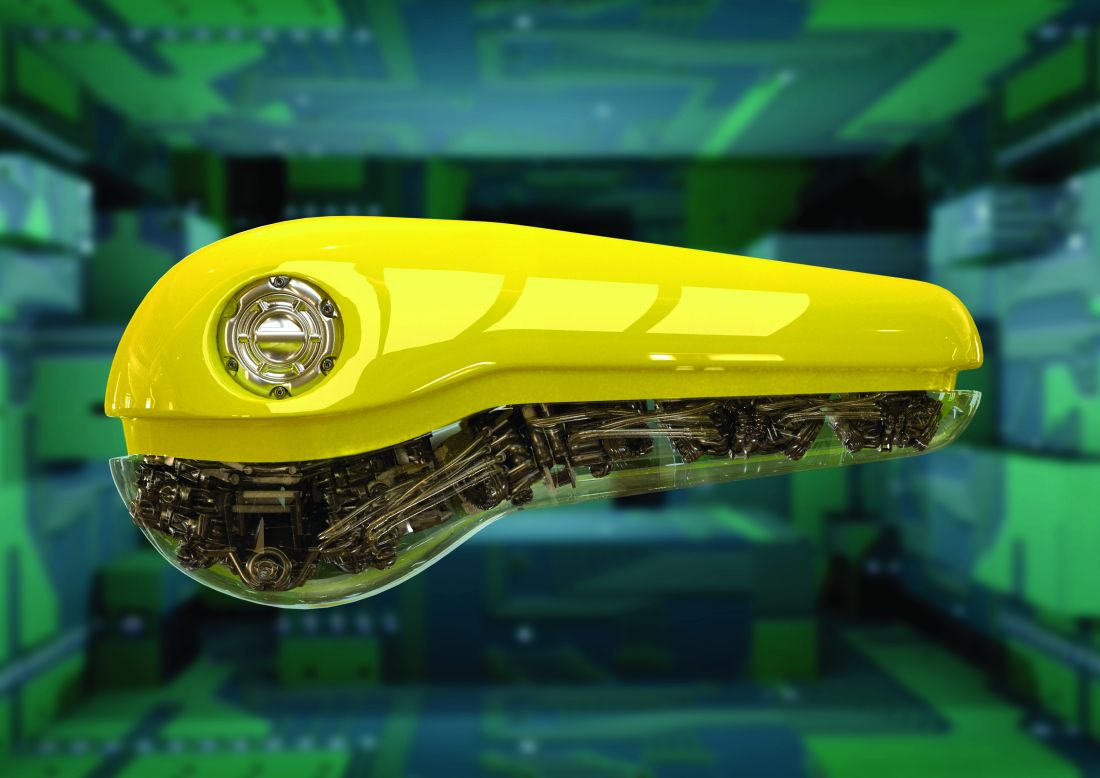
Medtronic has recalled 95,110 HawkOne Directional Atherectomy Systems because of the risk of the guidewire within the catheter moving downward or prolapsing during use, which may damage the tip of the catheter.
The U.S. Food and Drug Administration has identified this as a Class I recall, the most serious type, because of the potential for serious injury or death.
The HawkOne Directional Atherectomy system is used during procedures intended to remove blockage from peripheral arteries and improve blood flow.
If the guideline moves downward or prolapses during use, the “catheter tip may break off or separate, and this could lead to serious adverse events, including a tear along the inside wall of an artery (arterial dissection), a rupture or breakage of an artery (arterial rupture), decrease in blood flow to a part of the body because of a blocked artery (ischemia), and/or blood vessel complications that could require surgical repair and additional procedures to capture and remove the detached and/or migrated (embolized) tip,” the FDA says in a recall notice posted today on its website.
To date, there have been 55 injuries, no deaths, and 163 complaints reported for this device.
The recalled devices were distributed in the United States between Jan. 22, 2018 and Oct. 4, 2021. Product codes and lot numbers pertaining to the devices are listed on the FDA website.
Medtronic sent an urgent field safety notice to customers Dec. 6, 2021, requesting that they alert parties of the defect, review the instructions for use before using the device, and note the warnings and precautions listed in the letter.
Customers were also asked to complete the enclosed confirmation form and email to [email protected].
Health care providers can report adverse reactions or quality problems they experience using these devices to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Medtronic has recalled 95,110 HawkOne Directional Atherectomy Systems because of the risk of the guidewire within the catheter moving downward or prolapsing during use, which may damage the tip of the catheter.
The U.S. Food and Drug Administration has identified this as a Class I recall, the most serious type, because of the potential for serious injury or death.
The HawkOne Directional Atherectomy system is used during procedures intended to remove blockage from peripheral arteries and improve blood flow.
If the guideline moves downward or prolapses during use, the “catheter tip may break off or separate, and this could lead to serious adverse events, including a tear along the inside wall of an artery (arterial dissection), a rupture or breakage of an artery (arterial rupture), decrease in blood flow to a part of the body because of a blocked artery (ischemia), and/or blood vessel complications that could require surgical repair and additional procedures to capture and remove the detached and/or migrated (embolized) tip,” the FDA says in a recall notice posted today on its website.
To date, there have been 55 injuries, no deaths, and 163 complaints reported for this device.
The recalled devices were distributed in the United States between Jan. 22, 2018 and Oct. 4, 2021. Product codes and lot numbers pertaining to the devices are listed on the FDA website.
Medtronic sent an urgent field safety notice to customers Dec. 6, 2021, requesting that they alert parties of the defect, review the instructions for use before using the device, and note the warnings and precautions listed in the letter.
Customers were also asked to complete the enclosed confirmation form and email to [email protected].
Health care providers can report adverse reactions or quality problems they experience using these devices to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Medtronic has recalled 95,110 HawkOne Directional Atherectomy Systems because of the risk of the guidewire within the catheter moving downward or prolapsing during use, which may damage the tip of the catheter.
The U.S. Food and Drug Administration has identified this as a Class I recall, the most serious type, because of the potential for serious injury or death.
The HawkOne Directional Atherectomy system is used during procedures intended to remove blockage from peripheral arteries and improve blood flow.
If the guideline moves downward or prolapses during use, the “catheter tip may break off or separate, and this could lead to serious adverse events, including a tear along the inside wall of an artery (arterial dissection), a rupture or breakage of an artery (arterial rupture), decrease in blood flow to a part of the body because of a blocked artery (ischemia), and/or blood vessel complications that could require surgical repair and additional procedures to capture and remove the detached and/or migrated (embolized) tip,” the FDA says in a recall notice posted today on its website.
To date, there have been 55 injuries, no deaths, and 163 complaints reported for this device.
The recalled devices were distributed in the United States between Jan. 22, 2018 and Oct. 4, 2021. Product codes and lot numbers pertaining to the devices are listed on the FDA website.
Medtronic sent an urgent field safety notice to customers Dec. 6, 2021, requesting that they alert parties of the defect, review the instructions for use before using the device, and note the warnings and precautions listed in the letter.
Customers were also asked to complete the enclosed confirmation form and email to [email protected].
Health care providers can report adverse reactions or quality problems they experience using these devices to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
‘We just have to keep them alive’: Transitioning youth with type 1 diabetes
“No one has asked young people what they want,” said Tabitha Randell, MBChB, an endocrinologist with Nottingham (England) University Hospitals NHS Trust, who specializes in treating teenagers with type 1 diabetes as they transition to adult care.
Dr. Randell, who has set up a very successful specialist service in her hospital for such patients, said: “We consistently have the best, or the second best, outcomes in this country for our diabetes patients.” She believes this is one of the most important issues in modern endocrinology today.
Speaking at the Diabetes Professional Care conference in London at the end of 2021, and sharing her thoughts afterward with this news organization, she noted that in general there are “virtually no published outcomes” on how best to transition a patient with type 1 diabetes from pediatric to adult care.
“If you actually get them to transition – because some just drop out and disengage and there’s nothing you can do – none of them get lost. Some of them disengage in the adult clinic, but if you’re in the young diabetes service [in England] the rules are that if you miss a diabetes appointment you do not get discharged, as compared with the adult clinic, where if you miss an appointment, you are discharged.”
In the young diabetes clinic, doctors will “carry on trying to contact you, and get you back,” she explained. “And the patients do eventually come back in – it might be a year or 2, but they do come back. We’ve just got to keep them alive in the meantime!”
This issue needs tackling all over the world. Dr. Randell said she’s not aware of any one country – although there may be “pockets” of good care within a given country – that is doing this perfectly.
Across the pond, Grazia Aleppo, MD, division of endocrinology at Northwestern University, Chicago, agreed that transitioning pediatric patients with type 1 diabetes to adult care presents “unique challenges.”
Challenges when transitioning from pediatric to adult care
During childhood, type 1 diabetes management is largely supervised by patients’ parents and members of the pediatric diabetes care team, which may include diabetes educators, psychologists, or social workers, as well as pediatric endocrinologists.
When the patient with type 1 diabetes becomes a young adult and takes over management of their own health, Dr. Aleppo said, the care team may diminish along with the time spent in provider visits.
The adult endocrinology setting focuses more on self-management and autonomous functioning of the individual with diabetes.
Adult appointments are typically shorter, and the patient is usually expected to follow doctors’ suggestions independently, she noted. They are also expected to manage the practical aspects of their diabetes care, including prescriptions, diabetes supplies, laboratory tests, scheduling, and keeping appointments.
At the same time that the emerging adult needs to start asserting independence over their health care, they will also be going through a myriad of other important lifestyle changes, such as attending college, living on their own for the first time, and starting a career.
“With these fundamental differences and challenges, competing priorities, such as college, work and relationships, medical care may become of secondary importance and patients may become disengaged,” Dr. Aleppo explained.
As Dr. Randell has said, loss to follow-up is a big problem with this patient population, with disengagement from specialist services and worsening A1c across the transition, Dr. Aleppo noted. This makes addressing these patients’ specific needs extremely important.
Engage with kid, not disease; don’t palm them off on new recruits
“The really key thing these kids say is, ‘I do not want to be a disease,’” Dr. Randell said. “They want you to know that they are a person. Engage these kids!” she suggested. “Ask them: ‘How is your exam revision going?’ Find something positive to say, even if it’s just: ‘I’m glad you came today.’ ”
“If the first thing that you do is tell them off [for poor diabetes care], you are never going to see them again,” she cautioned.
Dr. Randell also said that role models with type 1 diabetes, such as Lila Moss – daughter of British supermodel Kate Moss – who was recently pictured wearing an insulin pump on her leg on the catwalk, are helping youngsters not feel so self-conscious about their diabetes.
“Let them know it’s not the end of the world, having [type 1] diabetes,” she emphasized.
And Partha Kar, MBBS, OBE, national specialty advisor, diabetes with NHS England, agreed wholeheartedly with Dr. Randall.
Reminiscing about his early days as a newly qualified endocrinologist, Dr. Kar, who works at Portsmouth (England) Hospital NHS Trust, noted that as a new member of staff he was given the youth with type 1 diabetes – those getting ready to transition to adult care – to look after.
But this is the exact opposite of what should be happening, he emphasized. “If you don’t think transition care is important, you shouldn’t be treating type 1 diabetes.”
He believes that every diabetes center “must have a young-adult team lead” and this job must not be given to the least experienced member of staff.
This lead “doesn’t need to be a doctor,” Dr. Kar stressed. “It can be a psychologist, or a diabetes nurse, or a pharmacist, or a dietician.”
In short, it must be someone experienced who loves working with this age group.
Dr. Randell agreed: “Make sure the team is interested in young people. It shouldn’t be the last person in who gets the job no one else wants.” Teens “are my favorite group to work with. They don’t take any nonsense.”
And she explained: “Young people like to get to know the person who’s going to take care of them. So, stay with them for their young adult years.” This can be “quite a fluid period,” with it normally extending to age 25, but in some cases, “it can be up to 32 years old.”
Preparing for the transition
To ease pediatric patients into the transition to adult care, Dr. Aleppo recommended that the pediatric diabetes team provide enough time so that any concerns the patient and their family may have can be addressed.
This should also include transferring management responsibilities to the young adult rather than their parent.
The pediatric provider should discuss with the patient available potential adult colleagues, personalizing these options to their needs, she said.
And the adult and pediatric clinicians should collaborate and provide important information beyond medical records or health summaries.
Adult providers should guide young adults on how to navigate the new practices, from scheduling follow-up appointments to policies regarding medication refills or supplies, to providing information about urgent numbers or email addresses for after-hours communications.
Dr. Kar reiterated that there are too few published outcomes in this patient group to guide the establishment of good transition services.
“Without data, we are dead on the ground. Without data, it’s all conjecture, anecdotes,” he said.
What he does know is that, in the latest national type 1 diabetes audit for England, “Diabetic ketoacidosis admissions ... are up in this age group,” which suggests these patients are not receiving adequate care.
Be a guide, not a gatekeeper
Dr. Kar stressed that, of the 8,760 hours in a year, the average patient with type 1 diabetes in the United Kingdom gets just “1-2 hours with you as a clinician, based on four appointments per year of 30 minutes each.”
“So you spend 0.02% of their time with individuals with type 1 diabetes. So, what’s the one thing you can do with that minimal contact? Be nice!”
Dr. Kar said he always has his email open to his adult patients and they are very respectful of his time. “They don’t email you at 1 a.m. That means every one of my patients has got support [from me]. Don’t be a barrier.”
“We have to fundamentally change the narrative. Doctors must have more empathy,” he said, stating that the one thing adolescents have constantly given feedback on has been, “Why don’t appointments start with: ‘How are you?’
“For a teenager, if you throw type 1 diabetes into the loop, it’s not easy,” he stressed. “Talk to them about something else. As a clinician, be a guide, not a gatekeeper. Give people the tools to self-manage better.”
Adult providers can meet these young adult patients “at their level,” Dr. Aleppo agreed.
“Pay attention to their immediate needs and focus on their present circumstances – whether how to get through their next semester in college, navigating job interviews, or handling having diabetes in the workplace.”
Paying attention to the mental health needs of these young patients is equally “paramount,” Dr. Aleppo said.
While access to mental health professionals may be challenging in the adult setting, providers should bring it up with their patients and offer counseling referrals.
“Diabetes impacts everything, and office appointments and conversations carry weight on these patients’ lives as a whole, not just on their diabetes,” she stressed. “A patient told me recently: ‘We’re learning to be adults,’ which can be hard enough, and with diabetes it can be even more challenging. Adult providers need to be aware of the patient’s ‘diabetes language’ in that often it is not what a patient is saying, rather how they are saying it that gives us information on what they truly need.
“As adult providers, we need to also train and teach our young patients to advocate for themselves on where to find resources that can help them navigate adulthood with diabetes,” she added.
One particularly helpful resource in the United States is the College Diabetes Network, a not-for-profit organization whose mission is to equip young adults with type 1 diabetes to successfully manage the challenging transition to independence at college and beyond.
“The sweetest thing that can happen to us as adult diabetes providers is when a patient – seen as an emerging adult during college – returns to your practice 10 years later after moving back and seeks you out for their diabetes care because of the relationship and trust you developed in those transitioning years,” Dr. Aleppo said.
Another resource is a freely available comic book series cocreated by Dr. Kar and colleague Mayank Patel, MBBS, an endocrinologist from University Hospital Southampton NHS Foundation Trust.
As detailed by this news organization in 2021, the series consists of three volumes: the first, Type 1: Origins, focuses on actual experiences of patients who have type 1 diabetes; the second, Type 1: Attack of the Ketones, is aimed at professionals who may provide care but have limited understanding of type 1 diabetes; and the third, Type 1 Mission 3: S.T.I.G.M.A., addresses the stigmas and misconceptions that patients with type 1 diabetes may face.
The idea for the first comic was inspired by a patient who compared having diabetes to being like the Marvel character The Hulk, said Dr. Kar, and has been expanded to include the additional volumes.
Dr. Kar and Dr. Patel have also just launched the fourth comic in the series, Type 1: Generations, to mark the 100-year anniversary since insulin was first given to a human.
“This is high priority”
Dr. Kar said the NHS in England has just appointed a national lead for type 1 diabetes in youth, Fulya Mehta, MD, of Alder Hey Children’s NHS Foundation Trust, Liverpool, England.
“If you have a plan, bring it to us,” he told the audience at the DPC conference, and “tell us, what is the one thing you would change? This is not a session we are doing just to tick a box. This is high priority.
“Encourage your colleagues to think about transition services. This is an absolute priority. We will be asking every center [in England] who is your transitioning lead?”
And he once again stressed that “a lead of transition service does not have to be a medic. This should be a multidisciplinary team. But they do need to be comfortable in that space. To that teenager, your job title means nothing. Give them time and space.”
Dr. Randell summed it up: “If we can work together, it’s only going to result in better outcomes. We need to blaze the trail for young people.”
Dr. Aleppo has reported serving as a consultant to Dexcom and Insulet and receiving support to Northwestern University from AstraZeneca, Dexcom, Eli Lilly, Fractyl Health, Insulet, and Novo Nordisk. Dr. Randell and Dr. Kar have no conflicts of interest.
A version of this article first appeared on Medscape.com.
“No one has asked young people what they want,” said Tabitha Randell, MBChB, an endocrinologist with Nottingham (England) University Hospitals NHS Trust, who specializes in treating teenagers with type 1 diabetes as they transition to adult care.
Dr. Randell, who has set up a very successful specialist service in her hospital for such patients, said: “We consistently have the best, or the second best, outcomes in this country for our diabetes patients.” She believes this is one of the most important issues in modern endocrinology today.
Speaking at the Diabetes Professional Care conference in London at the end of 2021, and sharing her thoughts afterward with this news organization, she noted that in general there are “virtually no published outcomes” on how best to transition a patient with type 1 diabetes from pediatric to adult care.
“If you actually get them to transition – because some just drop out and disengage and there’s nothing you can do – none of them get lost. Some of them disengage in the adult clinic, but if you’re in the young diabetes service [in England] the rules are that if you miss a diabetes appointment you do not get discharged, as compared with the adult clinic, where if you miss an appointment, you are discharged.”
In the young diabetes clinic, doctors will “carry on trying to contact you, and get you back,” she explained. “And the patients do eventually come back in – it might be a year or 2, but they do come back. We’ve just got to keep them alive in the meantime!”
This issue needs tackling all over the world. Dr. Randell said she’s not aware of any one country – although there may be “pockets” of good care within a given country – that is doing this perfectly.
Across the pond, Grazia Aleppo, MD, division of endocrinology at Northwestern University, Chicago, agreed that transitioning pediatric patients with type 1 diabetes to adult care presents “unique challenges.”
Challenges when transitioning from pediatric to adult care
During childhood, type 1 diabetes management is largely supervised by patients’ parents and members of the pediatric diabetes care team, which may include diabetes educators, psychologists, or social workers, as well as pediatric endocrinologists.
When the patient with type 1 diabetes becomes a young adult and takes over management of their own health, Dr. Aleppo said, the care team may diminish along with the time spent in provider visits.
The adult endocrinology setting focuses more on self-management and autonomous functioning of the individual with diabetes.
Adult appointments are typically shorter, and the patient is usually expected to follow doctors’ suggestions independently, she noted. They are also expected to manage the practical aspects of their diabetes care, including prescriptions, diabetes supplies, laboratory tests, scheduling, and keeping appointments.
At the same time that the emerging adult needs to start asserting independence over their health care, they will also be going through a myriad of other important lifestyle changes, such as attending college, living on their own for the first time, and starting a career.
“With these fundamental differences and challenges, competing priorities, such as college, work and relationships, medical care may become of secondary importance and patients may become disengaged,” Dr. Aleppo explained.
As Dr. Randell has said, loss to follow-up is a big problem with this patient population, with disengagement from specialist services and worsening A1c across the transition, Dr. Aleppo noted. This makes addressing these patients’ specific needs extremely important.
Engage with kid, not disease; don’t palm them off on new recruits
“The really key thing these kids say is, ‘I do not want to be a disease,’” Dr. Randell said. “They want you to know that they are a person. Engage these kids!” she suggested. “Ask them: ‘How is your exam revision going?’ Find something positive to say, even if it’s just: ‘I’m glad you came today.’ ”
“If the first thing that you do is tell them off [for poor diabetes care], you are never going to see them again,” she cautioned.
Dr. Randell also said that role models with type 1 diabetes, such as Lila Moss – daughter of British supermodel Kate Moss – who was recently pictured wearing an insulin pump on her leg on the catwalk, are helping youngsters not feel so self-conscious about their diabetes.
“Let them know it’s not the end of the world, having [type 1] diabetes,” she emphasized.
And Partha Kar, MBBS, OBE, national specialty advisor, diabetes with NHS England, agreed wholeheartedly with Dr. Randall.
Reminiscing about his early days as a newly qualified endocrinologist, Dr. Kar, who works at Portsmouth (England) Hospital NHS Trust, noted that as a new member of staff he was given the youth with type 1 diabetes – those getting ready to transition to adult care – to look after.
But this is the exact opposite of what should be happening, he emphasized. “If you don’t think transition care is important, you shouldn’t be treating type 1 diabetes.”
He believes that every diabetes center “must have a young-adult team lead” and this job must not be given to the least experienced member of staff.
This lead “doesn’t need to be a doctor,” Dr. Kar stressed. “It can be a psychologist, or a diabetes nurse, or a pharmacist, or a dietician.”
In short, it must be someone experienced who loves working with this age group.
Dr. Randell agreed: “Make sure the team is interested in young people. It shouldn’t be the last person in who gets the job no one else wants.” Teens “are my favorite group to work with. They don’t take any nonsense.”
And she explained: “Young people like to get to know the person who’s going to take care of them. So, stay with them for their young adult years.” This can be “quite a fluid period,” with it normally extending to age 25, but in some cases, “it can be up to 32 years old.”
Preparing for the transition
To ease pediatric patients into the transition to adult care, Dr. Aleppo recommended that the pediatric diabetes team provide enough time so that any concerns the patient and their family may have can be addressed.
This should also include transferring management responsibilities to the young adult rather than their parent.
The pediatric provider should discuss with the patient available potential adult colleagues, personalizing these options to their needs, she said.
And the adult and pediatric clinicians should collaborate and provide important information beyond medical records or health summaries.
Adult providers should guide young adults on how to navigate the new practices, from scheduling follow-up appointments to policies regarding medication refills or supplies, to providing information about urgent numbers or email addresses for after-hours communications.
Dr. Kar reiterated that there are too few published outcomes in this patient group to guide the establishment of good transition services.
“Without data, we are dead on the ground. Without data, it’s all conjecture, anecdotes,” he said.
What he does know is that, in the latest national type 1 diabetes audit for England, “Diabetic ketoacidosis admissions ... are up in this age group,” which suggests these patients are not receiving adequate care.
Be a guide, not a gatekeeper
Dr. Kar stressed that, of the 8,760 hours in a year, the average patient with type 1 diabetes in the United Kingdom gets just “1-2 hours with you as a clinician, based on four appointments per year of 30 minutes each.”
“So you spend 0.02% of their time with individuals with type 1 diabetes. So, what’s the one thing you can do with that minimal contact? Be nice!”
Dr. Kar said he always has his email open to his adult patients and they are very respectful of his time. “They don’t email you at 1 a.m. That means every one of my patients has got support [from me]. Don’t be a barrier.”
“We have to fundamentally change the narrative. Doctors must have more empathy,” he said, stating that the one thing adolescents have constantly given feedback on has been, “Why don’t appointments start with: ‘How are you?’
“For a teenager, if you throw type 1 diabetes into the loop, it’s not easy,” he stressed. “Talk to them about something else. As a clinician, be a guide, not a gatekeeper. Give people the tools to self-manage better.”
Adult providers can meet these young adult patients “at their level,” Dr. Aleppo agreed.
“Pay attention to their immediate needs and focus on their present circumstances – whether how to get through their next semester in college, navigating job interviews, or handling having diabetes in the workplace.”
Paying attention to the mental health needs of these young patients is equally “paramount,” Dr. Aleppo said.
While access to mental health professionals may be challenging in the adult setting, providers should bring it up with their patients and offer counseling referrals.
“Diabetes impacts everything, and office appointments and conversations carry weight on these patients’ lives as a whole, not just on their diabetes,” she stressed. “A patient told me recently: ‘We’re learning to be adults,’ which can be hard enough, and with diabetes it can be even more challenging. Adult providers need to be aware of the patient’s ‘diabetes language’ in that often it is not what a patient is saying, rather how they are saying it that gives us information on what they truly need.
“As adult providers, we need to also train and teach our young patients to advocate for themselves on where to find resources that can help them navigate adulthood with diabetes,” she added.
One particularly helpful resource in the United States is the College Diabetes Network, a not-for-profit organization whose mission is to equip young adults with type 1 diabetes to successfully manage the challenging transition to independence at college and beyond.
“The sweetest thing that can happen to us as adult diabetes providers is when a patient – seen as an emerging adult during college – returns to your practice 10 years later after moving back and seeks you out for their diabetes care because of the relationship and trust you developed in those transitioning years,” Dr. Aleppo said.
Another resource is a freely available comic book series cocreated by Dr. Kar and colleague Mayank Patel, MBBS, an endocrinologist from University Hospital Southampton NHS Foundation Trust.
As detailed by this news organization in 2021, the series consists of three volumes: the first, Type 1: Origins, focuses on actual experiences of patients who have type 1 diabetes; the second, Type 1: Attack of the Ketones, is aimed at professionals who may provide care but have limited understanding of type 1 diabetes; and the third, Type 1 Mission 3: S.T.I.G.M.A., addresses the stigmas and misconceptions that patients with type 1 diabetes may face.
The idea for the first comic was inspired by a patient who compared having diabetes to being like the Marvel character The Hulk, said Dr. Kar, and has been expanded to include the additional volumes.
Dr. Kar and Dr. Patel have also just launched the fourth comic in the series, Type 1: Generations, to mark the 100-year anniversary since insulin was first given to a human.
“This is high priority”
Dr. Kar said the NHS in England has just appointed a national lead for type 1 diabetes in youth, Fulya Mehta, MD, of Alder Hey Children’s NHS Foundation Trust, Liverpool, England.
“If you have a plan, bring it to us,” he told the audience at the DPC conference, and “tell us, what is the one thing you would change? This is not a session we are doing just to tick a box. This is high priority.
“Encourage your colleagues to think about transition services. This is an absolute priority. We will be asking every center [in England] who is your transitioning lead?”
And he once again stressed that “a lead of transition service does not have to be a medic. This should be a multidisciplinary team. But they do need to be comfortable in that space. To that teenager, your job title means nothing. Give them time and space.”
Dr. Randell summed it up: “If we can work together, it’s only going to result in better outcomes. We need to blaze the trail for young people.”
Dr. Aleppo has reported serving as a consultant to Dexcom and Insulet and receiving support to Northwestern University from AstraZeneca, Dexcom, Eli Lilly, Fractyl Health, Insulet, and Novo Nordisk. Dr. Randell and Dr. Kar have no conflicts of interest.
A version of this article first appeared on Medscape.com.
“No one has asked young people what they want,” said Tabitha Randell, MBChB, an endocrinologist with Nottingham (England) University Hospitals NHS Trust, who specializes in treating teenagers with type 1 diabetes as they transition to adult care.
Dr. Randell, who has set up a very successful specialist service in her hospital for such patients, said: “We consistently have the best, or the second best, outcomes in this country for our diabetes patients.” She believes this is one of the most important issues in modern endocrinology today.
Speaking at the Diabetes Professional Care conference in London at the end of 2021, and sharing her thoughts afterward with this news organization, she noted that in general there are “virtually no published outcomes” on how best to transition a patient with type 1 diabetes from pediatric to adult care.
“If you actually get them to transition – because some just drop out and disengage and there’s nothing you can do – none of them get lost. Some of them disengage in the adult clinic, but if you’re in the young diabetes service [in England] the rules are that if you miss a diabetes appointment you do not get discharged, as compared with the adult clinic, where if you miss an appointment, you are discharged.”
In the young diabetes clinic, doctors will “carry on trying to contact you, and get you back,” she explained. “And the patients do eventually come back in – it might be a year or 2, but they do come back. We’ve just got to keep them alive in the meantime!”
This issue needs tackling all over the world. Dr. Randell said she’s not aware of any one country – although there may be “pockets” of good care within a given country – that is doing this perfectly.
Across the pond, Grazia Aleppo, MD, division of endocrinology at Northwestern University, Chicago, agreed that transitioning pediatric patients with type 1 diabetes to adult care presents “unique challenges.”
Challenges when transitioning from pediatric to adult care
During childhood, type 1 diabetes management is largely supervised by patients’ parents and members of the pediatric diabetes care team, which may include diabetes educators, psychologists, or social workers, as well as pediatric endocrinologists.
When the patient with type 1 diabetes becomes a young adult and takes over management of their own health, Dr. Aleppo said, the care team may diminish along with the time spent in provider visits.
The adult endocrinology setting focuses more on self-management and autonomous functioning of the individual with diabetes.
Adult appointments are typically shorter, and the patient is usually expected to follow doctors’ suggestions independently, she noted. They are also expected to manage the practical aspects of their diabetes care, including prescriptions, diabetes supplies, laboratory tests, scheduling, and keeping appointments.
At the same time that the emerging adult needs to start asserting independence over their health care, they will also be going through a myriad of other important lifestyle changes, such as attending college, living on their own for the first time, and starting a career.
“With these fundamental differences and challenges, competing priorities, such as college, work and relationships, medical care may become of secondary importance and patients may become disengaged,” Dr. Aleppo explained.
As Dr. Randell has said, loss to follow-up is a big problem with this patient population, with disengagement from specialist services and worsening A1c across the transition, Dr. Aleppo noted. This makes addressing these patients’ specific needs extremely important.
Engage with kid, not disease; don’t palm them off on new recruits
“The really key thing these kids say is, ‘I do not want to be a disease,’” Dr. Randell said. “They want you to know that they are a person. Engage these kids!” she suggested. “Ask them: ‘How is your exam revision going?’ Find something positive to say, even if it’s just: ‘I’m glad you came today.’ ”
“If the first thing that you do is tell them off [for poor diabetes care], you are never going to see them again,” she cautioned.
Dr. Randell also said that role models with type 1 diabetes, such as Lila Moss – daughter of British supermodel Kate Moss – who was recently pictured wearing an insulin pump on her leg on the catwalk, are helping youngsters not feel so self-conscious about their diabetes.
“Let them know it’s not the end of the world, having [type 1] diabetes,” she emphasized.
And Partha Kar, MBBS, OBE, national specialty advisor, diabetes with NHS England, agreed wholeheartedly with Dr. Randall.
Reminiscing about his early days as a newly qualified endocrinologist, Dr. Kar, who works at Portsmouth (England) Hospital NHS Trust, noted that as a new member of staff he was given the youth with type 1 diabetes – those getting ready to transition to adult care – to look after.
But this is the exact opposite of what should be happening, he emphasized. “If you don’t think transition care is important, you shouldn’t be treating type 1 diabetes.”
He believes that every diabetes center “must have a young-adult team lead” and this job must not be given to the least experienced member of staff.
This lead “doesn’t need to be a doctor,” Dr. Kar stressed. “It can be a psychologist, or a diabetes nurse, or a pharmacist, or a dietician.”
In short, it must be someone experienced who loves working with this age group.
Dr. Randell agreed: “Make sure the team is interested in young people. It shouldn’t be the last person in who gets the job no one else wants.” Teens “are my favorite group to work with. They don’t take any nonsense.”
And she explained: “Young people like to get to know the person who’s going to take care of them. So, stay with them for their young adult years.” This can be “quite a fluid period,” with it normally extending to age 25, but in some cases, “it can be up to 32 years old.”
Preparing for the transition
To ease pediatric patients into the transition to adult care, Dr. Aleppo recommended that the pediatric diabetes team provide enough time so that any concerns the patient and their family may have can be addressed.
This should also include transferring management responsibilities to the young adult rather than their parent.
The pediatric provider should discuss with the patient available potential adult colleagues, personalizing these options to their needs, she said.
And the adult and pediatric clinicians should collaborate and provide important information beyond medical records or health summaries.
Adult providers should guide young adults on how to navigate the new practices, from scheduling follow-up appointments to policies regarding medication refills or supplies, to providing information about urgent numbers or email addresses for after-hours communications.
Dr. Kar reiterated that there are too few published outcomes in this patient group to guide the establishment of good transition services.
“Without data, we are dead on the ground. Without data, it’s all conjecture, anecdotes,” he said.
What he does know is that, in the latest national type 1 diabetes audit for England, “Diabetic ketoacidosis admissions ... are up in this age group,” which suggests these patients are not receiving adequate care.
Be a guide, not a gatekeeper
Dr. Kar stressed that, of the 8,760 hours in a year, the average patient with type 1 diabetes in the United Kingdom gets just “1-2 hours with you as a clinician, based on four appointments per year of 30 minutes each.”
“So you spend 0.02% of their time with individuals with type 1 diabetes. So, what’s the one thing you can do with that minimal contact? Be nice!”
Dr. Kar said he always has his email open to his adult patients and they are very respectful of his time. “They don’t email you at 1 a.m. That means every one of my patients has got support [from me]. Don’t be a barrier.”
“We have to fundamentally change the narrative. Doctors must have more empathy,” he said, stating that the one thing adolescents have constantly given feedback on has been, “Why don’t appointments start with: ‘How are you?’
“For a teenager, if you throw type 1 diabetes into the loop, it’s not easy,” he stressed. “Talk to them about something else. As a clinician, be a guide, not a gatekeeper. Give people the tools to self-manage better.”
Adult providers can meet these young adult patients “at their level,” Dr. Aleppo agreed.
“Pay attention to their immediate needs and focus on their present circumstances – whether how to get through their next semester in college, navigating job interviews, or handling having diabetes in the workplace.”
Paying attention to the mental health needs of these young patients is equally “paramount,” Dr. Aleppo said.
While access to mental health professionals may be challenging in the adult setting, providers should bring it up with their patients and offer counseling referrals.
“Diabetes impacts everything, and office appointments and conversations carry weight on these patients’ lives as a whole, not just on their diabetes,” she stressed. “A patient told me recently: ‘We’re learning to be adults,’ which can be hard enough, and with diabetes it can be even more challenging. Adult providers need to be aware of the patient’s ‘diabetes language’ in that often it is not what a patient is saying, rather how they are saying it that gives us information on what they truly need.
“As adult providers, we need to also train and teach our young patients to advocate for themselves on where to find resources that can help them navigate adulthood with diabetes,” she added.
One particularly helpful resource in the United States is the College Diabetes Network, a not-for-profit organization whose mission is to equip young adults with type 1 diabetes to successfully manage the challenging transition to independence at college and beyond.
“The sweetest thing that can happen to us as adult diabetes providers is when a patient – seen as an emerging adult during college – returns to your practice 10 years later after moving back and seeks you out for their diabetes care because of the relationship and trust you developed in those transitioning years,” Dr. Aleppo said.
Another resource is a freely available comic book series cocreated by Dr. Kar and colleague Mayank Patel, MBBS, an endocrinologist from University Hospital Southampton NHS Foundation Trust.
As detailed by this news organization in 2021, the series consists of three volumes: the first, Type 1: Origins, focuses on actual experiences of patients who have type 1 diabetes; the second, Type 1: Attack of the Ketones, is aimed at professionals who may provide care but have limited understanding of type 1 diabetes; and the third, Type 1 Mission 3: S.T.I.G.M.A., addresses the stigmas and misconceptions that patients with type 1 diabetes may face.
The idea for the first comic was inspired by a patient who compared having diabetes to being like the Marvel character The Hulk, said Dr. Kar, and has been expanded to include the additional volumes.
Dr. Kar and Dr. Patel have also just launched the fourth comic in the series, Type 1: Generations, to mark the 100-year anniversary since insulin was first given to a human.
“This is high priority”
Dr. Kar said the NHS in England has just appointed a national lead for type 1 diabetes in youth, Fulya Mehta, MD, of Alder Hey Children’s NHS Foundation Trust, Liverpool, England.
“If you have a plan, bring it to us,” he told the audience at the DPC conference, and “tell us, what is the one thing you would change? This is not a session we are doing just to tick a box. This is high priority.
“Encourage your colleagues to think about transition services. This is an absolute priority. We will be asking every center [in England] who is your transitioning lead?”
And he once again stressed that “a lead of transition service does not have to be a medic. This should be a multidisciplinary team. But they do need to be comfortable in that space. To that teenager, your job title means nothing. Give them time and space.”
Dr. Randell summed it up: “If we can work together, it’s only going to result in better outcomes. We need to blaze the trail for young people.”
Dr. Aleppo has reported serving as a consultant to Dexcom and Insulet and receiving support to Northwestern University from AstraZeneca, Dexcom, Eli Lilly, Fractyl Health, Insulet, and Novo Nordisk. Dr. Randell and Dr. Kar have no conflicts of interest.
A version of this article first appeared on Medscape.com.
‘Artificial pancreas’ life-changing in kids with type 1 diabetes
A semiautomated insulin delivery system improved glycemic control in young children with type 1 diabetes aged 1-7 years without increasing hypoglycemia.
“Hybrid closed-loop” systems – comprising an insulin pump, a continuous glucose monitor (CGM), and software enabling communication that semiautomates insulin delivery based on glucose levels – have been shown to improve glucose control in older children and adults.
The technology, also known as an artificial pancreas, has been less studied in very young children even though it may uniquely benefit them, said the authors of the new study, led by Julia Ware, MD, of the Wellcome Trust–Medical Research Council Institute of Metabolic Science and the University of Cambridge (England). The findings were published online Jan. 19, 2022, in the New England Journal of Medicine.
“Very young children are extremely vulnerable to changes in their blood sugar levels. High levels in particular can have potentially lasting consequences to their brain development. On top of that, diabetes is very challenging to manage in this age group, creating a huge burden for families,” she said in a University of Cambridge statement.
There is “high variability of insulin requirements, marked insulin sensitivity, and unpredictable eating and activity patterns,” Dr. Ware and colleagues noted.
“Caregiver fear of hypoglycemia, particularly overnight, is common and, coupled with young children’s unawareness that hypoglycemia is occurring, contributes to children not meeting the recommended glycemic targets or having difficulty maintaining recommended glycemic control unless caregivers can provide constant monitoring. These issues often lead to ... reduced quality of life for the whole family,” they added.
Except for mealtimes, device is fully automated
The new multicenter, randomized, crossover trial was conducted at seven centers across Austria, Germany, Luxembourg, and the United Kingdom in 2019-2020.
The trial compared the safety and efficacy of hybrid closed-loop therapy with sensor-augmented pump therapy (that is, without the device communication, as a control). All 74 children used the CamAPS FX hybrid closed-loop system for 16 weeks, and then used the control treatment for 16 weeks. The children were a mean age of 5.6 years and had a baseline hemoglobin A1c of 7.3% (56.6 mmol/mol).
The hybrid closed-loop system consisted of components that are commercially available in Europe: the Sooil insulin pump (Dana Diabecare RS) and the Dexcom G6 CGM, along with an unlocked Samsung Galaxy 8 smartphone housing an app (CamAPS FX, CamDiab) that runs the Cambridge proprietary model predictive control algorithm.
The smartphone communicates wirelessly with both the pump and the CGM transmitter and automatically adjusts the pump’s insulin delivery based on real-time sensor glucose readings. It also issues alarms if glucose levels fall below or rise above user-specified thresholds. This functionality was disabled during the study control periods.
Senior investigator Roman Hovorka, PhD, who developed the CamAPS FX app, explained in the University of Cambridge statement that the app “makes predictions about what it thinks is likely to happen next based on past experience. It learns how much insulin the child needs per day and how this changes at different times of the day.
“It then uses this [information] to adjust insulin levels to help achieve ideal blood sugar levels. Other than at mealtimes, it is fully automated, so parents do not need to continually monitor their child’s blood sugar levels.”
Indeed, the time spent in target glucose range (70-180 mg/dL) during the 16-week closed-loop period was 8.7 percentage points higher than during the control period (P < .001).
That difference translates to “a clinically meaningful 125 minutes per day,” and represented around three-quarters of their day (71.6%) in the target range, the investigators wrote.
The mean adjusted difference in time spent above 180 mg/dL was 8.5 percentage points lower with the closed-loop, also a significant difference (P < .001). Time spent below 70 mg/dL did not differ significantly between the two interventions (P = .74).
At the end of the study periods, the mean adjusted between-treatment difference in A1c was –0.4 percentage points, significantly lower following the closed-loop, compared with the control period (P < .001).
That percentage point difference (equivalent to 3.9 mmol/mol) “is important in a population of patients who had tight glycemic control at baseline. This result was observed without an increase in the time spent in a hypoglycemic state,” Dr. Ware and colleagues noted.
Median glucose sensor use was 99% during the closed-loop period and 96% during the control periods. During the closed-loop periods, the system was in closed-loop mode 95% of the time.
This finding supports longer-term usability in this age group and compares well with use in older children, they said.
One serious hypoglycemic episode, attributed to parental error rather than system malfunction, occurred during the closed-loop period. There were no episodes of diabetic ketoacidosis. Rates of other adverse events didn’t differ between the two periods.
“CamAPS FX led to improvements in several measures, including hyperglycemia and average blood sugar levels, without increasing the risk of hypos. This is likely to have important benefits for those children who use it,” Dr. Ware summarized.
Sleep quality could improve for children and caregivers
Reductions in time spent in hyperglycemia without increasing hypoglycemia could minimize the risk for neurocognitive deficits that have been reported among young children with type 1 diabetes, the authors speculated.
In addition, they noted that because 80% of overnight sensor readings were within target range and less than 3% were below 70 mg/dL, sleep quality could improve for both the children and their parents. This, in turn, “would confer associated quality of life benefits.”
“Parents have described our artificial pancreas as ‘life changing’ as it meant they were able to relax and spend less time worrying about their child’s blood sugar levels, particularly at nighttime. They tell us it gives them more time to do what any ‘normal’ family can do, to play and do fun things with their children,” observed Dr. Ware.
The CamAPS FX has been commercialized by CamDiab, a spin-out company set up by Dr. Hovorka. It is currently available through several NHS trusts across the United Kingdom, including Cambridge University Hospitals NHS Foundation Trust, and is expected to be more widely available soon.
The study was supported by the European Commission within the Horizon 2020 Framework Program, the NIHR Cambridge Biomedical Research Centre, and JDRF. Dr. Ware had no further disclosures. Dr. Hovorka has reported acting as consultant for Abbott Diabetes Care, BD, Dexcom, being a speaker for Novo Nordisk and Eli Lilly, and receiving royalty payments from B. Braun for software. He is director of CamDiab.
A version of this article first appeared on Medscape.com.
A semiautomated insulin delivery system improved glycemic control in young children with type 1 diabetes aged 1-7 years without increasing hypoglycemia.
“Hybrid closed-loop” systems – comprising an insulin pump, a continuous glucose monitor (CGM), and software enabling communication that semiautomates insulin delivery based on glucose levels – have been shown to improve glucose control in older children and adults.
The technology, also known as an artificial pancreas, has been less studied in very young children even though it may uniquely benefit them, said the authors of the new study, led by Julia Ware, MD, of the Wellcome Trust–Medical Research Council Institute of Metabolic Science and the University of Cambridge (England). The findings were published online Jan. 19, 2022, in the New England Journal of Medicine.
“Very young children are extremely vulnerable to changes in their blood sugar levels. High levels in particular can have potentially lasting consequences to their brain development. On top of that, diabetes is very challenging to manage in this age group, creating a huge burden for families,” she said in a University of Cambridge statement.
There is “high variability of insulin requirements, marked insulin sensitivity, and unpredictable eating and activity patterns,” Dr. Ware and colleagues noted.
“Caregiver fear of hypoglycemia, particularly overnight, is common and, coupled with young children’s unawareness that hypoglycemia is occurring, contributes to children not meeting the recommended glycemic targets or having difficulty maintaining recommended glycemic control unless caregivers can provide constant monitoring. These issues often lead to ... reduced quality of life for the whole family,” they added.
Except for mealtimes, device is fully automated
The new multicenter, randomized, crossover trial was conducted at seven centers across Austria, Germany, Luxembourg, and the United Kingdom in 2019-2020.
The trial compared the safety and efficacy of hybrid closed-loop therapy with sensor-augmented pump therapy (that is, without the device communication, as a control). All 74 children used the CamAPS FX hybrid closed-loop system for 16 weeks, and then used the control treatment for 16 weeks. The children were a mean age of 5.6 years and had a baseline hemoglobin A1c of 7.3% (56.6 mmol/mol).
The hybrid closed-loop system consisted of components that are commercially available in Europe: the Sooil insulin pump (Dana Diabecare RS) and the Dexcom G6 CGM, along with an unlocked Samsung Galaxy 8 smartphone housing an app (CamAPS FX, CamDiab) that runs the Cambridge proprietary model predictive control algorithm.
The smartphone communicates wirelessly with both the pump and the CGM transmitter and automatically adjusts the pump’s insulin delivery based on real-time sensor glucose readings. It also issues alarms if glucose levels fall below or rise above user-specified thresholds. This functionality was disabled during the study control periods.
Senior investigator Roman Hovorka, PhD, who developed the CamAPS FX app, explained in the University of Cambridge statement that the app “makes predictions about what it thinks is likely to happen next based on past experience. It learns how much insulin the child needs per day and how this changes at different times of the day.
“It then uses this [information] to adjust insulin levels to help achieve ideal blood sugar levels. Other than at mealtimes, it is fully automated, so parents do not need to continually monitor their child’s blood sugar levels.”
Indeed, the time spent in target glucose range (70-180 mg/dL) during the 16-week closed-loop period was 8.7 percentage points higher than during the control period (P < .001).
That difference translates to “a clinically meaningful 125 minutes per day,” and represented around three-quarters of their day (71.6%) in the target range, the investigators wrote.
The mean adjusted difference in time spent above 180 mg/dL was 8.5 percentage points lower with the closed-loop, also a significant difference (P < .001). Time spent below 70 mg/dL did not differ significantly between the two interventions (P = .74).
At the end of the study periods, the mean adjusted between-treatment difference in A1c was –0.4 percentage points, significantly lower following the closed-loop, compared with the control period (P < .001).
That percentage point difference (equivalent to 3.9 mmol/mol) “is important in a population of patients who had tight glycemic control at baseline. This result was observed without an increase in the time spent in a hypoglycemic state,” Dr. Ware and colleagues noted.
Median glucose sensor use was 99% during the closed-loop period and 96% during the control periods. During the closed-loop periods, the system was in closed-loop mode 95% of the time.
This finding supports longer-term usability in this age group and compares well with use in older children, they said.
One serious hypoglycemic episode, attributed to parental error rather than system malfunction, occurred during the closed-loop period. There were no episodes of diabetic ketoacidosis. Rates of other adverse events didn’t differ between the two periods.
“CamAPS FX led to improvements in several measures, including hyperglycemia and average blood sugar levels, without increasing the risk of hypos. This is likely to have important benefits for those children who use it,” Dr. Ware summarized.
Sleep quality could improve for children and caregivers
Reductions in time spent in hyperglycemia without increasing hypoglycemia could minimize the risk for neurocognitive deficits that have been reported among young children with type 1 diabetes, the authors speculated.
In addition, they noted that because 80% of overnight sensor readings were within target range and less than 3% were below 70 mg/dL, sleep quality could improve for both the children and their parents. This, in turn, “would confer associated quality of life benefits.”
“Parents have described our artificial pancreas as ‘life changing’ as it meant they were able to relax and spend less time worrying about their child’s blood sugar levels, particularly at nighttime. They tell us it gives them more time to do what any ‘normal’ family can do, to play and do fun things with their children,” observed Dr. Ware.
The CamAPS FX has been commercialized by CamDiab, a spin-out company set up by Dr. Hovorka. It is currently available through several NHS trusts across the United Kingdom, including Cambridge University Hospitals NHS Foundation Trust, and is expected to be more widely available soon.
The study was supported by the European Commission within the Horizon 2020 Framework Program, the NIHR Cambridge Biomedical Research Centre, and JDRF. Dr. Ware had no further disclosures. Dr. Hovorka has reported acting as consultant for Abbott Diabetes Care, BD, Dexcom, being a speaker for Novo Nordisk and Eli Lilly, and receiving royalty payments from B. Braun for software. He is director of CamDiab.
A version of this article first appeared on Medscape.com.
A semiautomated insulin delivery system improved glycemic control in young children with type 1 diabetes aged 1-7 years without increasing hypoglycemia.
“Hybrid closed-loop” systems – comprising an insulin pump, a continuous glucose monitor (CGM), and software enabling communication that semiautomates insulin delivery based on glucose levels – have been shown to improve glucose control in older children and adults.
The technology, also known as an artificial pancreas, has been less studied in very young children even though it may uniquely benefit them, said the authors of the new study, led by Julia Ware, MD, of the Wellcome Trust–Medical Research Council Institute of Metabolic Science and the University of Cambridge (England). The findings were published online Jan. 19, 2022, in the New England Journal of Medicine.
“Very young children are extremely vulnerable to changes in their blood sugar levels. High levels in particular can have potentially lasting consequences to their brain development. On top of that, diabetes is very challenging to manage in this age group, creating a huge burden for families,” she said in a University of Cambridge statement.
There is “high variability of insulin requirements, marked insulin sensitivity, and unpredictable eating and activity patterns,” Dr. Ware and colleagues noted.
“Caregiver fear of hypoglycemia, particularly overnight, is common and, coupled with young children’s unawareness that hypoglycemia is occurring, contributes to children not meeting the recommended glycemic targets or having difficulty maintaining recommended glycemic control unless caregivers can provide constant monitoring. These issues often lead to ... reduced quality of life for the whole family,” they added.
Except for mealtimes, device is fully automated
The new multicenter, randomized, crossover trial was conducted at seven centers across Austria, Germany, Luxembourg, and the United Kingdom in 2019-2020.
The trial compared the safety and efficacy of hybrid closed-loop therapy with sensor-augmented pump therapy (that is, without the device communication, as a control). All 74 children used the CamAPS FX hybrid closed-loop system for 16 weeks, and then used the control treatment for 16 weeks. The children were a mean age of 5.6 years and had a baseline hemoglobin A1c of 7.3% (56.6 mmol/mol).
The hybrid closed-loop system consisted of components that are commercially available in Europe: the Sooil insulin pump (Dana Diabecare RS) and the Dexcom G6 CGM, along with an unlocked Samsung Galaxy 8 smartphone housing an app (CamAPS FX, CamDiab) that runs the Cambridge proprietary model predictive control algorithm.
The smartphone communicates wirelessly with both the pump and the CGM transmitter and automatically adjusts the pump’s insulin delivery based on real-time sensor glucose readings. It also issues alarms if glucose levels fall below or rise above user-specified thresholds. This functionality was disabled during the study control periods.
Senior investigator Roman Hovorka, PhD, who developed the CamAPS FX app, explained in the University of Cambridge statement that the app “makes predictions about what it thinks is likely to happen next based on past experience. It learns how much insulin the child needs per day and how this changes at different times of the day.
“It then uses this [information] to adjust insulin levels to help achieve ideal blood sugar levels. Other than at mealtimes, it is fully automated, so parents do not need to continually monitor their child’s blood sugar levels.”
Indeed, the time spent in target glucose range (70-180 mg/dL) during the 16-week closed-loop period was 8.7 percentage points higher than during the control period (P < .001).
That difference translates to “a clinically meaningful 125 minutes per day,” and represented around three-quarters of their day (71.6%) in the target range, the investigators wrote.
The mean adjusted difference in time spent above 180 mg/dL was 8.5 percentage points lower with the closed-loop, also a significant difference (P < .001). Time spent below 70 mg/dL did not differ significantly between the two interventions (P = .74).
At the end of the study periods, the mean adjusted between-treatment difference in A1c was –0.4 percentage points, significantly lower following the closed-loop, compared with the control period (P < .001).
That percentage point difference (equivalent to 3.9 mmol/mol) “is important in a population of patients who had tight glycemic control at baseline. This result was observed without an increase in the time spent in a hypoglycemic state,” Dr. Ware and colleagues noted.
Median glucose sensor use was 99% during the closed-loop period and 96% during the control periods. During the closed-loop periods, the system was in closed-loop mode 95% of the time.
This finding supports longer-term usability in this age group and compares well with use in older children, they said.
One serious hypoglycemic episode, attributed to parental error rather than system malfunction, occurred during the closed-loop period. There were no episodes of diabetic ketoacidosis. Rates of other adverse events didn’t differ between the two periods.
“CamAPS FX led to improvements in several measures, including hyperglycemia and average blood sugar levels, without increasing the risk of hypos. This is likely to have important benefits for those children who use it,” Dr. Ware summarized.
Sleep quality could improve for children and caregivers
Reductions in time spent in hyperglycemia without increasing hypoglycemia could minimize the risk for neurocognitive deficits that have been reported among young children with type 1 diabetes, the authors speculated.
In addition, they noted that because 80% of overnight sensor readings were within target range and less than 3% were below 70 mg/dL, sleep quality could improve for both the children and their parents. This, in turn, “would confer associated quality of life benefits.”
“Parents have described our artificial pancreas as ‘life changing’ as it meant they were able to relax and spend less time worrying about their child’s blood sugar levels, particularly at nighttime. They tell us it gives them more time to do what any ‘normal’ family can do, to play and do fun things with their children,” observed Dr. Ware.
The CamAPS FX has been commercialized by CamDiab, a spin-out company set up by Dr. Hovorka. It is currently available through several NHS trusts across the United Kingdom, including Cambridge University Hospitals NHS Foundation Trust, and is expected to be more widely available soon.
The study was supported by the European Commission within the Horizon 2020 Framework Program, the NIHR Cambridge Biomedical Research Centre, and JDRF. Dr. Ware had no further disclosures. Dr. Hovorka has reported acting as consultant for Abbott Diabetes Care, BD, Dexcom, being a speaker for Novo Nordisk and Eli Lilly, and receiving royalty payments from B. Braun for software. He is director of CamDiab.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Advances in Diabetes and Cardiovascular Care
Real-World Experience With Automated Insulin Pumps
Continuous Blood Glucose Monitoring for T2DM
Statin-Induced Adverse Effects
Long QT and Cardiac Arrest After Pulmonary Edema
And more online
• Clinical Impact of U-500 Insulin Initiation
• Diabetes Self-Management Education
• SGLT2 Inhibitors, T2DM, and Heart Failure
• Alirocumab Use in Statin-Intolerant Veterans
• K Pneumoniae-Induced Aortitis
Real-World Experience With Automated Insulin Pumps
Continuous Blood Glucose Monitoring for T2DM
Statin-Induced Adverse Effects
Long QT and Cardiac Arrest After Pulmonary Edema
And more online
• Clinical Impact of U-500 Insulin Initiation
• Diabetes Self-Management Education
• SGLT2 Inhibitors, T2DM, and Heart Failure
• Alirocumab Use in Statin-Intolerant Veterans
• K Pneumoniae-Induced Aortitis
Real-World Experience With Automated Insulin Pumps
Continuous Blood Glucose Monitoring for T2DM
Statin-Induced Adverse Effects
Long QT and Cardiac Arrest After Pulmonary Edema
And more online
• Clinical Impact of U-500 Insulin Initiation
• Diabetes Self-Management Education
• SGLT2 Inhibitors, T2DM, and Heart Failure
• Alirocumab Use in Statin-Intolerant Veterans
• K Pneumoniae-Induced Aortitis
Program targets preschoolers to promote heart health
Creators of a pilot program that educates preschoolers about good heart health have validated a template for successful early childhood intervention that, they claim, provides a pathway for translating scientific evidence into the community and classroom for educational purposes to encourage long-lasting lifestyle changes.
That validation supports the creators' plans to take the program into more schools.
They reported key lessons in crafting the program, known as the SI! Program (for Salud Integral-Comprehensive Health), online in the Journal of the American College of Cardiology.
“This is a research-based program that uses randomized clinical trial evidence with implementation strategies to design educational health promotion programs,” senior author Valentin Fuster, MD, PhD, founder and trustees chairman of the Foundation for Science, Health, and Education (SHE) based in Barcelona, under whose aegis the SI! Program was implemented, said in an interview. Dr. Fuster is also director of Mount Sinai Heart and physician-in-chief at Mount Sinai Hospital in New York, and general director of the National Center for Cardiovascular Investigation (CNIC) in Madrid, Spain’s equivalent of the National Heart, Lung, and Blood Institute.
“There are specific times in a child’s life when improvements can be made to enhance long-term cardiovascular health status,” said Rodrigo Fernández-Jiménez, MD, PhD, group leader of the cardiovascular health and imaging lab at CNIC and study coauthor. “Our review, and previous studies, suggest that 4-5 years of age is the most favorable time to start a school-based intervention focused on healthy habits.”
A key piece of the SI! Program used a Sesame Street character, known as Dr. Ruster, a Muppet based on Dr. Fuster, to introduce and convey most messages and activities to the preschool children. The program also used a heart-shaped mascot named “Cardio” to teach about healthy behaviors. Other components include video segments, a colorful storybook, an interactive board game, flash cards, and a teacher’s guide. The activities and messages were tailored based on the country in which the program was implemented.
A decade of experience
The review evaluated 10 years of experience with the preschool-based program, drawing upon cluster-randomized clinical trials of the program in three countries with different socioeconomic conditions: Colombia, Spain, and the United States. The studies randomized schools to receive the SI! Program for 4 months or to a control group and included more than 3,800 children from 50 schools, along with their parents or caregivers and teachers. The studies found significant increases in preschoolers’ knowledge, attitudes, and habits toward healthy eating and living an active lifestyle. Now, the SI! Program is expanding into more than 250 schools in Spain and more than 40 schools in all five boroughs of New York City.
“This is a multidimensional program,” Dr. Fuster said. The review identified five stages for implementing the program: dissemination; adoption; implementation; evaluation; and institutionalization.
Dissemination involves three substages for intervention: components, design, and strategy. With regard to the components, said Dr. Fuster, “We’re targeting children to educate them in four topics: how the body works; nutritional and dietary requirements; physical activity; and the need to control emotions – to say no in the future when they’re confronted with alcohol, drugs, and tobacco.”
Design involved a multidisciplinary team of experts to develop the intervention, Dr. Fuster said. The strategy itself enlists parents and teachers in the implementation, but goes beyond that. “This is a community,” Dr. Fuster said. Hence, the school environment and classroom itself are also engaged to support the message of the four topics.
Dr. Fuster said future research should look at knowledge, attitude, and habits and biological outcomes in children who’ve been in the SI! Program when they reach adolescence. “Our hypothesis is that we can do this in older children, but when they reach age 10 we want to reintervene in them,” Dr. Fuster said. “Humans need reintervention. Our findings don’t get into sustainability.” He added that further research should also identify socioeconomic factors that influence child health.
Expanding the program across the New York City’s five boroughs “offers a unique opportunity to explore which socioeconomic factors, at both the family and borough level, and may eventually affect children’s health, how they are implicated in the intervention’s effectiveness, and how they can be addressed to reduce the gap in health inequalities,” he said.
Karalyn Kinsella, MD, a pediatrician affiliated with Yale New Haven (Conn.) Medical Center, noted the program’s multidimensional nature is an important element. “I think what is so important about this intervention is that it is not one single intervention but a curriculum that takes a significant amount of time (up to 50 hours) that allows for repetition of the information, which allows it to become remembered,” she said in an interview. “I also think incorporating families in the intervention is key as that is where change often has to happen.”
While she said the program may provide a template for a mental health curriculum, she added, “My concern is that teachers are already feeling overwhelmed and this may be viewed as another burden.”
The American Heart Association provided funding for the study in the United States. Dr Fernández-Jiménez has received funding from the Fondo de Investigación Sanitaria–Instituto de Salud Carlos III, which is cofunded by the European Regional Development Fund/European Social Fund. Dr. Fuster and Dr. Kinsella have no relevant disclosures.
Creators of a pilot program that educates preschoolers about good heart health have validated a template for successful early childhood intervention that, they claim, provides a pathway for translating scientific evidence into the community and classroom for educational purposes to encourage long-lasting lifestyle changes.
That validation supports the creators' plans to take the program into more schools.
They reported key lessons in crafting the program, known as the SI! Program (for Salud Integral-Comprehensive Health), online in the Journal of the American College of Cardiology.
“This is a research-based program that uses randomized clinical trial evidence with implementation strategies to design educational health promotion programs,” senior author Valentin Fuster, MD, PhD, founder and trustees chairman of the Foundation for Science, Health, and Education (SHE) based in Barcelona, under whose aegis the SI! Program was implemented, said in an interview. Dr. Fuster is also director of Mount Sinai Heart and physician-in-chief at Mount Sinai Hospital in New York, and general director of the National Center for Cardiovascular Investigation (CNIC) in Madrid, Spain’s equivalent of the National Heart, Lung, and Blood Institute.
“There are specific times in a child’s life when improvements can be made to enhance long-term cardiovascular health status,” said Rodrigo Fernández-Jiménez, MD, PhD, group leader of the cardiovascular health and imaging lab at CNIC and study coauthor. “Our review, and previous studies, suggest that 4-5 years of age is the most favorable time to start a school-based intervention focused on healthy habits.”
A key piece of the SI! Program used a Sesame Street character, known as Dr. Ruster, a Muppet based on Dr. Fuster, to introduce and convey most messages and activities to the preschool children. The program also used a heart-shaped mascot named “Cardio” to teach about healthy behaviors. Other components include video segments, a colorful storybook, an interactive board game, flash cards, and a teacher’s guide. The activities and messages were tailored based on the country in which the program was implemented.
A decade of experience
The review evaluated 10 years of experience with the preschool-based program, drawing upon cluster-randomized clinical trials of the program in three countries with different socioeconomic conditions: Colombia, Spain, and the United States. The studies randomized schools to receive the SI! Program for 4 months or to a control group and included more than 3,800 children from 50 schools, along with their parents or caregivers and teachers. The studies found significant increases in preschoolers’ knowledge, attitudes, and habits toward healthy eating and living an active lifestyle. Now, the SI! Program is expanding into more than 250 schools in Spain and more than 40 schools in all five boroughs of New York City.
“This is a multidimensional program,” Dr. Fuster said. The review identified five stages for implementing the program: dissemination; adoption; implementation; evaluation; and institutionalization.
Dissemination involves three substages for intervention: components, design, and strategy. With regard to the components, said Dr. Fuster, “We’re targeting children to educate them in four topics: how the body works; nutritional and dietary requirements; physical activity; and the need to control emotions – to say no in the future when they’re confronted with alcohol, drugs, and tobacco.”
Design involved a multidisciplinary team of experts to develop the intervention, Dr. Fuster said. The strategy itself enlists parents and teachers in the implementation, but goes beyond that. “This is a community,” Dr. Fuster said. Hence, the school environment and classroom itself are also engaged to support the message of the four topics.
Dr. Fuster said future research should look at knowledge, attitude, and habits and biological outcomes in children who’ve been in the SI! Program when they reach adolescence. “Our hypothesis is that we can do this in older children, but when they reach age 10 we want to reintervene in them,” Dr. Fuster said. “Humans need reintervention. Our findings don’t get into sustainability.” He added that further research should also identify socioeconomic factors that influence child health.
Expanding the program across the New York City’s five boroughs “offers a unique opportunity to explore which socioeconomic factors, at both the family and borough level, and may eventually affect children’s health, how they are implicated in the intervention’s effectiveness, and how they can be addressed to reduce the gap in health inequalities,” he said.
Karalyn Kinsella, MD, a pediatrician affiliated with Yale New Haven (Conn.) Medical Center, noted the program’s multidimensional nature is an important element. “I think what is so important about this intervention is that it is not one single intervention but a curriculum that takes a significant amount of time (up to 50 hours) that allows for repetition of the information, which allows it to become remembered,” she said in an interview. “I also think incorporating families in the intervention is key as that is where change often has to happen.”
While she said the program may provide a template for a mental health curriculum, she added, “My concern is that teachers are already feeling overwhelmed and this may be viewed as another burden.”
The American Heart Association provided funding for the study in the United States. Dr Fernández-Jiménez has received funding from the Fondo de Investigación Sanitaria–Instituto de Salud Carlos III, which is cofunded by the European Regional Development Fund/European Social Fund. Dr. Fuster and Dr. Kinsella have no relevant disclosures.
Creators of a pilot program that educates preschoolers about good heart health have validated a template for successful early childhood intervention that, they claim, provides a pathway for translating scientific evidence into the community and classroom for educational purposes to encourage long-lasting lifestyle changes.
That validation supports the creators' plans to take the program into more schools.
They reported key lessons in crafting the program, known as the SI! Program (for Salud Integral-Comprehensive Health), online in the Journal of the American College of Cardiology.
“This is a research-based program that uses randomized clinical trial evidence with implementation strategies to design educational health promotion programs,” senior author Valentin Fuster, MD, PhD, founder and trustees chairman of the Foundation for Science, Health, and Education (SHE) based in Barcelona, under whose aegis the SI! Program was implemented, said in an interview. Dr. Fuster is also director of Mount Sinai Heart and physician-in-chief at Mount Sinai Hospital in New York, and general director of the National Center for Cardiovascular Investigation (CNIC) in Madrid, Spain’s equivalent of the National Heart, Lung, and Blood Institute.
“There are specific times in a child’s life when improvements can be made to enhance long-term cardiovascular health status,” said Rodrigo Fernández-Jiménez, MD, PhD, group leader of the cardiovascular health and imaging lab at CNIC and study coauthor. “Our review, and previous studies, suggest that 4-5 years of age is the most favorable time to start a school-based intervention focused on healthy habits.”
A key piece of the SI! Program used a Sesame Street character, known as Dr. Ruster, a Muppet based on Dr. Fuster, to introduce and convey most messages and activities to the preschool children. The program also used a heart-shaped mascot named “Cardio” to teach about healthy behaviors. Other components include video segments, a colorful storybook, an interactive board game, flash cards, and a teacher’s guide. The activities and messages were tailored based on the country in which the program was implemented.
A decade of experience
The review evaluated 10 years of experience with the preschool-based program, drawing upon cluster-randomized clinical trials of the program in three countries with different socioeconomic conditions: Colombia, Spain, and the United States. The studies randomized schools to receive the SI! Program for 4 months or to a control group and included more than 3,800 children from 50 schools, along with their parents or caregivers and teachers. The studies found significant increases in preschoolers’ knowledge, attitudes, and habits toward healthy eating and living an active lifestyle. Now, the SI! Program is expanding into more than 250 schools in Spain and more than 40 schools in all five boroughs of New York City.
“This is a multidimensional program,” Dr. Fuster said. The review identified five stages for implementing the program: dissemination; adoption; implementation; evaluation; and institutionalization.
Dissemination involves three substages for intervention: components, design, and strategy. With regard to the components, said Dr. Fuster, “We’re targeting children to educate them in four topics: how the body works; nutritional and dietary requirements; physical activity; and the need to control emotions – to say no in the future when they’re confronted with alcohol, drugs, and tobacco.”
Design involved a multidisciplinary team of experts to develop the intervention, Dr. Fuster said. The strategy itself enlists parents and teachers in the implementation, but goes beyond that. “This is a community,” Dr. Fuster said. Hence, the school environment and classroom itself are also engaged to support the message of the four topics.
Dr. Fuster said future research should look at knowledge, attitude, and habits and biological outcomes in children who’ve been in the SI! Program when they reach adolescence. “Our hypothesis is that we can do this in older children, but when they reach age 10 we want to reintervene in them,” Dr. Fuster said. “Humans need reintervention. Our findings don’t get into sustainability.” He added that further research should also identify socioeconomic factors that influence child health.
Expanding the program across the New York City’s five boroughs “offers a unique opportunity to explore which socioeconomic factors, at both the family and borough level, and may eventually affect children’s health, how they are implicated in the intervention’s effectiveness, and how they can be addressed to reduce the gap in health inequalities,” he said.
Karalyn Kinsella, MD, a pediatrician affiliated with Yale New Haven (Conn.) Medical Center, noted the program’s multidimensional nature is an important element. “I think what is so important about this intervention is that it is not one single intervention but a curriculum that takes a significant amount of time (up to 50 hours) that allows for repetition of the information, which allows it to become remembered,” she said in an interview. “I also think incorporating families in the intervention is key as that is where change often has to happen.”
While she said the program may provide a template for a mental health curriculum, she added, “My concern is that teachers are already feeling overwhelmed and this may be viewed as another burden.”
The American Heart Association provided funding for the study in the United States. Dr Fernández-Jiménez has received funding from the Fondo de Investigación Sanitaria–Instituto de Salud Carlos III, which is cofunded by the European Regional Development Fund/European Social Fund. Dr. Fuster and Dr. Kinsella have no relevant disclosures.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Semaglutide tops sibling liraglutide for weight loss
A study showing that once-weekly subcutaneous semaglutide 2.4 mg (Wegovy, Novo Nordisk) produces greater long-term weight loss than once-daily injected liraglutide 3.0 mg (Saxenda, Novo Nordisk) among adults with overweight or obesity without diabetes has now been published.
The data, previously reported at Obesity Week 2021, were published online Jan. 11 in JAMA.
The findings are from the phase 3 Semaglutide Treatment Effect in People with Obesity (STEP) 8 trial by Domenica M. Rubino, MD, of the Washington Center for Weight Management and Research, Arlington, Virginia, and colleagues.
Semaglutide and liraglutide, subcutaneously injectable glucagon-like peptide-1 (GLP-1) agonists, were both first approved for the treatment of type 2 diabetes in the United States and elsewhere, but are now also approved, in different doses, for chronic weight management and in people with obesity or overweight and comorbidities. A phase 2 trial demonstrated that once-daily semaglutide 0.4 mg produced significantly more weight loss than liraglutide 3.0 mg.
“Semaglutide and liraglutide induce weight loss by lowering energy intake. However, the reduction in caloric intake versus placebo appears to be larger with semaglutide (35%) than liraglutide (approximately 16%),” say Dr. Rubino and colleagues.
“Semaglutide has also been associated with reductions in food cravings, which is less evident with liraglutide, suggesting different mechanisms of energy intake regulation,” they add.
Novo Nordisk has recently reported that there may be supply problems with Wegovy, as a contract manufacturer that fills syringes for pens to inject the drug temporarily halted deliveries and manufacturing after issues related to good manufacturing practice.
The company is also developing an oral form of semaglutide for weight loss. The oral form has already been approved in doses of 7 or 14 mg/day for the treatment of type 2 diabetes in the United States as Rybelsus.
Individualize treatment for those with obesity
STEP 8 was a randomized, open-label, 68-week phase 3b trial of 338 adults randomized to once-weekly semaglutide 2.4 mg (n = 126), once-daily liraglutide 3.0 mg (n = 127), or matched injected placebo (n = 85) for 68 weeks, all provided with counseling on diet and physical activity.
The primary outcome – estimated mean change in body weight at week 68 – was –15.8% with semaglutide versus –6.4% with liraglutide, a significant difference (P < .001). The proportions of patients achieving loss of body weight of 10%, 15%, or 20% were 70.9%, 55.6%, and 38.5% with semaglutide versus 25.6%, 12.0%, and 6.0% with liraglutide, respectively.
Significantly greater reductions were also seen at 68 weeks for weekly semaglutide versus daily liraglutide in absolute body weight, waist circumference, diastolic blood pressure, total cholesterol, very low-density cholesterol, triglycerides, A1c, fasting plasma glucose, and C-reactive protein. Differences in systolic blood pressure, LDL and HDL cholesterol, free fatty acids, and fasting serum insulin did not achieve significance.
Overall, 19.8% of patients permanently discontinued treatment, with the most discontinuations in the liraglutide group (27.6%), followed by placebo (17.6%) and semaglutide (3.5%). Time to first and permanent discontinuation were shorter with liraglutide than with semaglutide or placebo.
Adverse events were reported by 95.2% of patients with semaglutide, 96.1% with liraglutide, and 95.3% with placebo. Gastrointestinal disorders were the most common with the two active drugs, reported by 84.1% with semaglutide and 82.7% with liraglutide versus 55.3% with placebo.
Most side effects were mild to moderate and resolved without treatment discontinuation. Severe gastrointestinal adverse events were reported by only 3.2%, 2.4%, and 3.5% of patients with semaglutide, liraglutide, and placebo, respectively.
“This trial found weight loss with semaglutide was significantly greater than with liraglutide. However, the variability in treatment response means an individual’s tolerance and sensitivity to a specific treatment is important for obesity management,” the researchers observe.
“Therefore, having multiple antiobesity medications proven to lower body weight through different mechanisms, with different adverse effect profiles and dosing regimens, can only benefit clinicians and patients,” they conclude.
The trial was funded by Novo Nordisk. Dr. Rubino has reported being a clinical investigator for Boehringer Ingelheim, AstraZeneca, and Novo Nordisk; receiving honoraria from WebMD; receiving speaker fees, consulting fees, scientific advisory fees, and honoraria from Novo Nordisk; receiving grants from SARL and personal fees from Medscape, PeerView, and the Endocrine Society; and being a shareholder in Novo Nordisk.
A version of this article first appeared on Medscape.com.
A study showing that once-weekly subcutaneous semaglutide 2.4 mg (Wegovy, Novo Nordisk) produces greater long-term weight loss than once-daily injected liraglutide 3.0 mg (Saxenda, Novo Nordisk) among adults with overweight or obesity without diabetes has now been published.
The data, previously reported at Obesity Week 2021, were published online Jan. 11 in JAMA.
The findings are from the phase 3 Semaglutide Treatment Effect in People with Obesity (STEP) 8 trial by Domenica M. Rubino, MD, of the Washington Center for Weight Management and Research, Arlington, Virginia, and colleagues.
Semaglutide and liraglutide, subcutaneously injectable glucagon-like peptide-1 (GLP-1) agonists, were both first approved for the treatment of type 2 diabetes in the United States and elsewhere, but are now also approved, in different doses, for chronic weight management and in people with obesity or overweight and comorbidities. A phase 2 trial demonstrated that once-daily semaglutide 0.4 mg produced significantly more weight loss than liraglutide 3.0 mg.
“Semaglutide and liraglutide induce weight loss by lowering energy intake. However, the reduction in caloric intake versus placebo appears to be larger with semaglutide (35%) than liraglutide (approximately 16%),” say Dr. Rubino and colleagues.
“Semaglutide has also been associated with reductions in food cravings, which is less evident with liraglutide, suggesting different mechanisms of energy intake regulation,” they add.
Novo Nordisk has recently reported that there may be supply problems with Wegovy, as a contract manufacturer that fills syringes for pens to inject the drug temporarily halted deliveries and manufacturing after issues related to good manufacturing practice.
The company is also developing an oral form of semaglutide for weight loss. The oral form has already been approved in doses of 7 or 14 mg/day for the treatment of type 2 diabetes in the United States as Rybelsus.
Individualize treatment for those with obesity
STEP 8 was a randomized, open-label, 68-week phase 3b trial of 338 adults randomized to once-weekly semaglutide 2.4 mg (n = 126), once-daily liraglutide 3.0 mg (n = 127), or matched injected placebo (n = 85) for 68 weeks, all provided with counseling on diet and physical activity.
The primary outcome – estimated mean change in body weight at week 68 – was –15.8% with semaglutide versus –6.4% with liraglutide, a significant difference (P < .001). The proportions of patients achieving loss of body weight of 10%, 15%, or 20% were 70.9%, 55.6%, and 38.5% with semaglutide versus 25.6%, 12.0%, and 6.0% with liraglutide, respectively.
Significantly greater reductions were also seen at 68 weeks for weekly semaglutide versus daily liraglutide in absolute body weight, waist circumference, diastolic blood pressure, total cholesterol, very low-density cholesterol, triglycerides, A1c, fasting plasma glucose, and C-reactive protein. Differences in systolic blood pressure, LDL and HDL cholesterol, free fatty acids, and fasting serum insulin did not achieve significance.
Overall, 19.8% of patients permanently discontinued treatment, with the most discontinuations in the liraglutide group (27.6%), followed by placebo (17.6%) and semaglutide (3.5%). Time to first and permanent discontinuation were shorter with liraglutide than with semaglutide or placebo.
Adverse events were reported by 95.2% of patients with semaglutide, 96.1% with liraglutide, and 95.3% with placebo. Gastrointestinal disorders were the most common with the two active drugs, reported by 84.1% with semaglutide and 82.7% with liraglutide versus 55.3% with placebo.
Most side effects were mild to moderate and resolved without treatment discontinuation. Severe gastrointestinal adverse events were reported by only 3.2%, 2.4%, and 3.5% of patients with semaglutide, liraglutide, and placebo, respectively.
“This trial found weight loss with semaglutide was significantly greater than with liraglutide. However, the variability in treatment response means an individual’s tolerance and sensitivity to a specific treatment is important for obesity management,” the researchers observe.
“Therefore, having multiple antiobesity medications proven to lower body weight through different mechanisms, with different adverse effect profiles and dosing regimens, can only benefit clinicians and patients,” they conclude.
The trial was funded by Novo Nordisk. Dr. Rubino has reported being a clinical investigator for Boehringer Ingelheim, AstraZeneca, and Novo Nordisk; receiving honoraria from WebMD; receiving speaker fees, consulting fees, scientific advisory fees, and honoraria from Novo Nordisk; receiving grants from SARL and personal fees from Medscape, PeerView, and the Endocrine Society; and being a shareholder in Novo Nordisk.
A version of this article first appeared on Medscape.com.
A study showing that once-weekly subcutaneous semaglutide 2.4 mg (Wegovy, Novo Nordisk) produces greater long-term weight loss than once-daily injected liraglutide 3.0 mg (Saxenda, Novo Nordisk) among adults with overweight or obesity without diabetes has now been published.
The data, previously reported at Obesity Week 2021, were published online Jan. 11 in JAMA.
The findings are from the phase 3 Semaglutide Treatment Effect in People with Obesity (STEP) 8 trial by Domenica M. Rubino, MD, of the Washington Center for Weight Management and Research, Arlington, Virginia, and colleagues.
Semaglutide and liraglutide, subcutaneously injectable glucagon-like peptide-1 (GLP-1) agonists, were both first approved for the treatment of type 2 diabetes in the United States and elsewhere, but are now also approved, in different doses, for chronic weight management and in people with obesity or overweight and comorbidities. A phase 2 trial demonstrated that once-daily semaglutide 0.4 mg produced significantly more weight loss than liraglutide 3.0 mg.
“Semaglutide and liraglutide induce weight loss by lowering energy intake. However, the reduction in caloric intake versus placebo appears to be larger with semaglutide (35%) than liraglutide (approximately 16%),” say Dr. Rubino and colleagues.
“Semaglutide has also been associated with reductions in food cravings, which is less evident with liraglutide, suggesting different mechanisms of energy intake regulation,” they add.
Novo Nordisk has recently reported that there may be supply problems with Wegovy, as a contract manufacturer that fills syringes for pens to inject the drug temporarily halted deliveries and manufacturing after issues related to good manufacturing practice.
The company is also developing an oral form of semaglutide for weight loss. The oral form has already been approved in doses of 7 or 14 mg/day for the treatment of type 2 diabetes in the United States as Rybelsus.
Individualize treatment for those with obesity
STEP 8 was a randomized, open-label, 68-week phase 3b trial of 338 adults randomized to once-weekly semaglutide 2.4 mg (n = 126), once-daily liraglutide 3.0 mg (n = 127), or matched injected placebo (n = 85) for 68 weeks, all provided with counseling on diet and physical activity.
The primary outcome – estimated mean change in body weight at week 68 – was –15.8% with semaglutide versus –6.4% with liraglutide, a significant difference (P < .001). The proportions of patients achieving loss of body weight of 10%, 15%, or 20% were 70.9%, 55.6%, and 38.5% with semaglutide versus 25.6%, 12.0%, and 6.0% with liraglutide, respectively.
Significantly greater reductions were also seen at 68 weeks for weekly semaglutide versus daily liraglutide in absolute body weight, waist circumference, diastolic blood pressure, total cholesterol, very low-density cholesterol, triglycerides, A1c, fasting plasma glucose, and C-reactive protein. Differences in systolic blood pressure, LDL and HDL cholesterol, free fatty acids, and fasting serum insulin did not achieve significance.
Overall, 19.8% of patients permanently discontinued treatment, with the most discontinuations in the liraglutide group (27.6%), followed by placebo (17.6%) and semaglutide (3.5%). Time to first and permanent discontinuation were shorter with liraglutide than with semaglutide or placebo.
Adverse events were reported by 95.2% of patients with semaglutide, 96.1% with liraglutide, and 95.3% with placebo. Gastrointestinal disorders were the most common with the two active drugs, reported by 84.1% with semaglutide and 82.7% with liraglutide versus 55.3% with placebo.
Most side effects were mild to moderate and resolved without treatment discontinuation. Severe gastrointestinal adverse events were reported by only 3.2%, 2.4%, and 3.5% of patients with semaglutide, liraglutide, and placebo, respectively.
“This trial found weight loss with semaglutide was significantly greater than with liraglutide. However, the variability in treatment response means an individual’s tolerance and sensitivity to a specific treatment is important for obesity management,” the researchers observe.
“Therefore, having multiple antiobesity medications proven to lower body weight through different mechanisms, with different adverse effect profiles and dosing regimens, can only benefit clinicians and patients,” they conclude.
The trial was funded by Novo Nordisk. Dr. Rubino has reported being a clinical investigator for Boehringer Ingelheim, AstraZeneca, and Novo Nordisk; receiving honoraria from WebMD; receiving speaker fees, consulting fees, scientific advisory fees, and honoraria from Novo Nordisk; receiving grants from SARL and personal fees from Medscape, PeerView, and the Endocrine Society; and being a shareholder in Novo Nordisk.
A version of this article first appeared on Medscape.com.
FROM JAMA
Lifestyle changes can lead to remission, but not a cure, in type 2 diabetes
Whenever I get a new patient with type 2 diabetes, who is generally on metformin, one of the very first questions they ask me is, “Can I get off my medication?” Everybody, it seems, who gets diabetes wants to not have diabetes.
So, what does this really mean? What does this mean to me as a clinician? And what does this mean to my patients? The American Diabetes Association recently came out with a consensus statement that defines and interprets the definition of remission in people with type 2 diabetes. Basically, if the hemoglobin A1c is less than 6.5% without diabetes medications for at least 3 months, that’s considered remission.
There are other considerations, such as metabolic surgery, that can lead to remission. But again, such patients should be 3 months post surgery and at least 3 months off diabetes medication. As for a lifestyle intervention, the authors state that remission really happens within about 6 months.
That leads me to wonder: What is remission? Remission really means temporary recovery, so it doesn’t mean a cure. Now, I’m not against curing diabetes. In fact, I’m all for it. But when somebody gets diabetes – and honestly, it doesn’t matter whether it’s type 1 or type 2 – the first thing I think of, and I think the first thing that my patients are taught, is how important it is to have a healthy lifestyle. This healthy lifestyle isn’t just for people with diabetes; it largely means the healthy lifestyle that all of us should follow, one where we eat fewer simple carbs, less processed food, more vegetables, more lean proteins and meats – all of the things that we know we should do. And all of the things that keep us healthy. To some degree, I don’t think you can ever get “remission” from diabetes, because if having diabetes points an individual toward having a healthier lifestyle, I think that’s great.
I think people should exercise more. When it comes to treating diabetes, exercise is key. When you think about obesity, we want to help people who are overweight or obese lose weight as part of their treatment for diabetes. And that doesn’t go away, either.
So, no, people who are diagnosed with diabetes don’t really go into remission if they keep their same old habits and don’t lose weight and don’t exercise. But many people with diabetes can get off medication if they do those things.
However, it’s not true for everybody, and I don’t want people to get unrealistic expectations because I think there are probably about a thousand different subtypes of type 2 diabetes. And I’ve definitely seen people who are lean with type 2 diabetes who don’t respond as well to a lifestyle intervention, or people who are more insulin deficient, who also need medication.
I think it’s really important to frame the expectation that, if remission means going back to the way it was before, when they didn’t have to think about what they ate or whether or not they exercised, that’s not going to happen. I think diabetes should really be a wake-up call that people need to be healthier in terms of their lifestyle habits.
The issue of medication is really an individual one, and I think we need to help patients look for what’s best for the individual, what their targets are, what their goals are. But we also have to think that diabetes isn’t just about glucose.
So remission in terms of the ADA’s definition looks at glucose, but I look at more than glucose. You have to look at lipids and blood pressure. And, as I mentioned earlier, you have to look at whether or not a person has preexisting cardiovascular disease or has the presence of microvascular complications that need to be screened for and treated.
I actually think that, in some ways, the diagnosis of diabetes is helpful simply because it helps put people on a better path to health. I don’t want people to think that remission means that they can go back to unhealthy habits. I really encourage all people to live a healthier lifestyle, and if it leads to improvements in glucose levels and getting off medication, I think that’s wonderful and a worthy goal. But remember, health and meeting one’s targets remain key in the treatment of type 2 diabetes.
Dr. Peters is a professor in the department of clinical medicine at the University of Southern California, Los Angeles. She reported serving on the advisory board or speakers’ bureau of Medscape and several pharmaceutical companies, and has received research support from Dexcom, MannKind, and AstraZeneca. This perspective and an accompanying video first appeared on Medscape.com.
Whenever I get a new patient with type 2 diabetes, who is generally on metformin, one of the very first questions they ask me is, “Can I get off my medication?” Everybody, it seems, who gets diabetes wants to not have diabetes.
So, what does this really mean? What does this mean to me as a clinician? And what does this mean to my patients? The American Diabetes Association recently came out with a consensus statement that defines and interprets the definition of remission in people with type 2 diabetes. Basically, if the hemoglobin A1c is less than 6.5% without diabetes medications for at least 3 months, that’s considered remission.
There are other considerations, such as metabolic surgery, that can lead to remission. But again, such patients should be 3 months post surgery and at least 3 months off diabetes medication. As for a lifestyle intervention, the authors state that remission really happens within about 6 months.
That leads me to wonder: What is remission? Remission really means temporary recovery, so it doesn’t mean a cure. Now, I’m not against curing diabetes. In fact, I’m all for it. But when somebody gets diabetes – and honestly, it doesn’t matter whether it’s type 1 or type 2 – the first thing I think of, and I think the first thing that my patients are taught, is how important it is to have a healthy lifestyle. This healthy lifestyle isn’t just for people with diabetes; it largely means the healthy lifestyle that all of us should follow, one where we eat fewer simple carbs, less processed food, more vegetables, more lean proteins and meats – all of the things that we know we should do. And all of the things that keep us healthy. To some degree, I don’t think you can ever get “remission” from diabetes, because if having diabetes points an individual toward having a healthier lifestyle, I think that’s great.
I think people should exercise more. When it comes to treating diabetes, exercise is key. When you think about obesity, we want to help people who are overweight or obese lose weight as part of their treatment for diabetes. And that doesn’t go away, either.
So, no, people who are diagnosed with diabetes don’t really go into remission if they keep their same old habits and don’t lose weight and don’t exercise. But many people with diabetes can get off medication if they do those things.
However, it’s not true for everybody, and I don’t want people to get unrealistic expectations because I think there are probably about a thousand different subtypes of type 2 diabetes. And I’ve definitely seen people who are lean with type 2 diabetes who don’t respond as well to a lifestyle intervention, or people who are more insulin deficient, who also need medication.
I think it’s really important to frame the expectation that, if remission means going back to the way it was before, when they didn’t have to think about what they ate or whether or not they exercised, that’s not going to happen. I think diabetes should really be a wake-up call that people need to be healthier in terms of their lifestyle habits.
The issue of medication is really an individual one, and I think we need to help patients look for what’s best for the individual, what their targets are, what their goals are. But we also have to think that diabetes isn’t just about glucose.
So remission in terms of the ADA’s definition looks at glucose, but I look at more than glucose. You have to look at lipids and blood pressure. And, as I mentioned earlier, you have to look at whether or not a person has preexisting cardiovascular disease or has the presence of microvascular complications that need to be screened for and treated.
I actually think that, in some ways, the diagnosis of diabetes is helpful simply because it helps put people on a better path to health. I don’t want people to think that remission means that they can go back to unhealthy habits. I really encourage all people to live a healthier lifestyle, and if it leads to improvements in glucose levels and getting off medication, I think that’s wonderful and a worthy goal. But remember, health and meeting one’s targets remain key in the treatment of type 2 diabetes.
Dr. Peters is a professor in the department of clinical medicine at the University of Southern California, Los Angeles. She reported serving on the advisory board or speakers’ bureau of Medscape and several pharmaceutical companies, and has received research support from Dexcom, MannKind, and AstraZeneca. This perspective and an accompanying video first appeared on Medscape.com.
Whenever I get a new patient with type 2 diabetes, who is generally on metformin, one of the very first questions they ask me is, “Can I get off my medication?” Everybody, it seems, who gets diabetes wants to not have diabetes.
So, what does this really mean? What does this mean to me as a clinician? And what does this mean to my patients? The American Diabetes Association recently came out with a consensus statement that defines and interprets the definition of remission in people with type 2 diabetes. Basically, if the hemoglobin A1c is less than 6.5% without diabetes medications for at least 3 months, that’s considered remission.
There are other considerations, such as metabolic surgery, that can lead to remission. But again, such patients should be 3 months post surgery and at least 3 months off diabetes medication. As for a lifestyle intervention, the authors state that remission really happens within about 6 months.
That leads me to wonder: What is remission? Remission really means temporary recovery, so it doesn’t mean a cure. Now, I’m not against curing diabetes. In fact, I’m all for it. But when somebody gets diabetes – and honestly, it doesn’t matter whether it’s type 1 or type 2 – the first thing I think of, and I think the first thing that my patients are taught, is how important it is to have a healthy lifestyle. This healthy lifestyle isn’t just for people with diabetes; it largely means the healthy lifestyle that all of us should follow, one where we eat fewer simple carbs, less processed food, more vegetables, more lean proteins and meats – all of the things that we know we should do. And all of the things that keep us healthy. To some degree, I don’t think you can ever get “remission” from diabetes, because if having diabetes points an individual toward having a healthier lifestyle, I think that’s great.
I think people should exercise more. When it comes to treating diabetes, exercise is key. When you think about obesity, we want to help people who are overweight or obese lose weight as part of their treatment for diabetes. And that doesn’t go away, either.
So, no, people who are diagnosed with diabetes don’t really go into remission if they keep their same old habits and don’t lose weight and don’t exercise. But many people with diabetes can get off medication if they do those things.
However, it’s not true for everybody, and I don’t want people to get unrealistic expectations because I think there are probably about a thousand different subtypes of type 2 diabetes. And I’ve definitely seen people who are lean with type 2 diabetes who don’t respond as well to a lifestyle intervention, or people who are more insulin deficient, who also need medication.
I think it’s really important to frame the expectation that, if remission means going back to the way it was before, when they didn’t have to think about what they ate or whether or not they exercised, that’s not going to happen. I think diabetes should really be a wake-up call that people need to be healthier in terms of their lifestyle habits.
The issue of medication is really an individual one, and I think we need to help patients look for what’s best for the individual, what their targets are, what their goals are. But we also have to think that diabetes isn’t just about glucose.
So remission in terms of the ADA’s definition looks at glucose, but I look at more than glucose. You have to look at lipids and blood pressure. And, as I mentioned earlier, you have to look at whether or not a person has preexisting cardiovascular disease or has the presence of microvascular complications that need to be screened for and treated.
I actually think that, in some ways, the diagnosis of diabetes is helpful simply because it helps put people on a better path to health. I don’t want people to think that remission means that they can go back to unhealthy habits. I really encourage all people to live a healthier lifestyle, and if it leads to improvements in glucose levels and getting off medication, I think that’s wonderful and a worthy goal. But remember, health and meeting one’s targets remain key in the treatment of type 2 diabetes.
Dr. Peters is a professor in the department of clinical medicine at the University of Southern California, Los Angeles. She reported serving on the advisory board or speakers’ bureau of Medscape and several pharmaceutical companies, and has received research support from Dexcom, MannKind, and AstraZeneca. This perspective and an accompanying video first appeared on Medscape.com.
Heavy snoring in early pregnancy linked to increased insulin resistance
Severe maternal sleep-disordered breathing (SDB) is a known risk factor for gestational diabetes, which is commonly diagnosed in the second or third trimester of pregnancy.
Now, a new study suggests that increases in insulin resistance, a precursor for gestational diabetes, may take place as early as the first trimester of pregnancy in women with risk factors for obstructive sleep apnea (OSA), such as overweight and habitual snoring.
This finding could potentially provide physicians with a window of opportunity to improve outcomes by screening at-risk women early in pregnancy or even prior to conception, Laura Sanapo, MD, assistant professor of medicine (research) at Brown University, Providence, R.I., and colleagues wrote in Sleep.
“Further studies are needed to investigate the association and its impact on the development of gestational diabetes, and to establish whether early-gestation or pregestational treatment of SDB would improve glucose metabolic outcomes in pregnancy,” they wrote.
”What this paper demonstrates is that the changes that predate gestational diabetes are seen much earlier in pregnancy,” senior study author Ghada Bourjeily, MD, professor of medicine at Brown University, said in an interview. Women should be screened for SDB rather than insulin resistance in early pregnancy since continuous positive airway pressure therapy (CPAP) is a highly effective intervention.
Waiting until midpregnancy to screen for OSA “is too late to make significant changes in the care of these women,” said Dr. Bourjeily, who is also director of research and training at the Women’s Medicine Collaborative at The Miriam Hospital in Providence, R.I. “By the time you diagnose gestational diabetes, the cat is out of the bag.”
For the study, women with early singleton pregnancies and risk factors for OSA such as habitual snoring and a median body mass index (BMI) of at least 27 kg/m2 were recruited from two prospective clinical trial studies enriched for OSA positivity. Women with a history of pregestational diabetes and those using CPAP or receiving chronic steroid therapy were excluded from the current study.
A total of 192 study participants underwent in-home sleep study (HSAT) and homeostatic model assessment (HOMA) between 11 and 15 gestational weeks, respectively. The association between continuous measures of SDB as a respiratory-event index as well as oxygen-desaturation index and glucose metabolism parameters such as insulin resistance (HOMA-IR) were analyzed after adjusting for gestational age, maternal age, BMI, ethnicity, race, and parity.
In all, 61 women (32%) were diagnosed with OSA based on respiratory event index values greater than or equal to five events per hour. These participants were more likely to be older, to have a high BMI, and to be multipara, compared with women who didn’t have a diagnosis of OSA. Women with a diagnosis of OSA exhibited higher glucose and C-peptide values and a higher degree of insulin resistance, compared with women without OSA, the researchers found. An increase of 0.3 in HOMA-IR related to maternal SDB in early pregnancy may significantly affect glucose metabolism.
Although the findings of the current study cannot be extrapolated to women who don’t have overweight or obesity, some women with normal-range BMI (18.5-24.9) are also at increased risk of glucose metabolism changes, Dr. Bourjeily pointed out. This includes those of Southeast Asian descent. “We found that the association of SDB parameters with insulin resistance was actually happening independently of BMI and other factors.”
Ideally, screening for SDB would begin prior to pregnancy, Dr. Bourjeily said. A BMI greater than 25 should be taken into account and patients asked if they snore and if so, whether it’s loud enough to wake their partner. They should also be asked about experiencing daytime sleepiness.
“Based on these answers, especially in women screened prior to pregnancy, there will be time to make the diagnosis of sleep apnea and get the patient on CPAP,” Dr. Bourjeily said.
“This is an interesting study and one of the rare ones looking at early pregnancy and some of the mechanisms that could possibly be contributing to gestational diabetes,” commented Grenye O’Malley, MD, assistant professor in the division of endocrinology, diabetes, and bone disease at the Icahn School of Medicine at Mount Sinai, New York. Dr. O’Malley was not involved in the study.
“It confirms our suspicions that there’s probably a lot of things happening earlier in pregnancy before a diagnosis of gestational diabetes. It also confirms that some of the mechanisms are probably very similar to those involved in the association between disordered sleep and the development of type 2 diabetes.”
However, it’s too early to determine whether screening for SDB and the use of CPAP will prevent glycemic changes, Dr. O’Malley said in an interview. “Whenever we screen, we ask whether we have an intervention that changes outcomes and we don’t know that yet.”
Some of the symptoms of SDB are also common in early pregnancy, such as a BMI greater than 25 and daytime sleepiness, Dr. O’Malley pointed out. It was unclear whether the study participants had a propensity to develop type 2 diabetes or whether they were at risk of gestational diabetes.
This study was funded by the National Heart, Lung, and Blood Institute; the National Institute for Child Health; and the National Institute of General Medical Sciences. Dr. Bourjeily and colleagues, as well as Dr. O’Malley, reported having no potential financial conflicts of interest.
Severe maternal sleep-disordered breathing (SDB) is a known risk factor for gestational diabetes, which is commonly diagnosed in the second or third trimester of pregnancy.
Now, a new study suggests that increases in insulin resistance, a precursor for gestational diabetes, may take place as early as the first trimester of pregnancy in women with risk factors for obstructive sleep apnea (OSA), such as overweight and habitual snoring.
This finding could potentially provide physicians with a window of opportunity to improve outcomes by screening at-risk women early in pregnancy or even prior to conception, Laura Sanapo, MD, assistant professor of medicine (research) at Brown University, Providence, R.I., and colleagues wrote in Sleep.
“Further studies are needed to investigate the association and its impact on the development of gestational diabetes, and to establish whether early-gestation or pregestational treatment of SDB would improve glucose metabolic outcomes in pregnancy,” they wrote.
”What this paper demonstrates is that the changes that predate gestational diabetes are seen much earlier in pregnancy,” senior study author Ghada Bourjeily, MD, professor of medicine at Brown University, said in an interview. Women should be screened for SDB rather than insulin resistance in early pregnancy since continuous positive airway pressure therapy (CPAP) is a highly effective intervention.
Waiting until midpregnancy to screen for OSA “is too late to make significant changes in the care of these women,” said Dr. Bourjeily, who is also director of research and training at the Women’s Medicine Collaborative at The Miriam Hospital in Providence, R.I. “By the time you diagnose gestational diabetes, the cat is out of the bag.”
For the study, women with early singleton pregnancies and risk factors for OSA such as habitual snoring and a median body mass index (BMI) of at least 27 kg/m2 were recruited from two prospective clinical trial studies enriched for OSA positivity. Women with a history of pregestational diabetes and those using CPAP or receiving chronic steroid therapy were excluded from the current study.
A total of 192 study participants underwent in-home sleep study (HSAT) and homeostatic model assessment (HOMA) between 11 and 15 gestational weeks, respectively. The association between continuous measures of SDB as a respiratory-event index as well as oxygen-desaturation index and glucose metabolism parameters such as insulin resistance (HOMA-IR) were analyzed after adjusting for gestational age, maternal age, BMI, ethnicity, race, and parity.
In all, 61 women (32%) were diagnosed with OSA based on respiratory event index values greater than or equal to five events per hour. These participants were more likely to be older, to have a high BMI, and to be multipara, compared with women who didn’t have a diagnosis of OSA. Women with a diagnosis of OSA exhibited higher glucose and C-peptide values and a higher degree of insulin resistance, compared with women without OSA, the researchers found. An increase of 0.3 in HOMA-IR related to maternal SDB in early pregnancy may significantly affect glucose metabolism.
Although the findings of the current study cannot be extrapolated to women who don’t have overweight or obesity, some women with normal-range BMI (18.5-24.9) are also at increased risk of glucose metabolism changes, Dr. Bourjeily pointed out. This includes those of Southeast Asian descent. “We found that the association of SDB parameters with insulin resistance was actually happening independently of BMI and other factors.”
Ideally, screening for SDB would begin prior to pregnancy, Dr. Bourjeily said. A BMI greater than 25 should be taken into account and patients asked if they snore and if so, whether it’s loud enough to wake their partner. They should also be asked about experiencing daytime sleepiness.
“Based on these answers, especially in women screened prior to pregnancy, there will be time to make the diagnosis of sleep apnea and get the patient on CPAP,” Dr. Bourjeily said.
“This is an interesting study and one of the rare ones looking at early pregnancy and some of the mechanisms that could possibly be contributing to gestational diabetes,” commented Grenye O’Malley, MD, assistant professor in the division of endocrinology, diabetes, and bone disease at the Icahn School of Medicine at Mount Sinai, New York. Dr. O’Malley was not involved in the study.
“It confirms our suspicions that there’s probably a lot of things happening earlier in pregnancy before a diagnosis of gestational diabetes. It also confirms that some of the mechanisms are probably very similar to those involved in the association between disordered sleep and the development of type 2 diabetes.”
However, it’s too early to determine whether screening for SDB and the use of CPAP will prevent glycemic changes, Dr. O’Malley said in an interview. “Whenever we screen, we ask whether we have an intervention that changes outcomes and we don’t know that yet.”
Some of the symptoms of SDB are also common in early pregnancy, such as a BMI greater than 25 and daytime sleepiness, Dr. O’Malley pointed out. It was unclear whether the study participants had a propensity to develop type 2 diabetes or whether they were at risk of gestational diabetes.
This study was funded by the National Heart, Lung, and Blood Institute; the National Institute for Child Health; and the National Institute of General Medical Sciences. Dr. Bourjeily and colleagues, as well as Dr. O’Malley, reported having no potential financial conflicts of interest.
Severe maternal sleep-disordered breathing (SDB) is a known risk factor for gestational diabetes, which is commonly diagnosed in the second or third trimester of pregnancy.
Now, a new study suggests that increases in insulin resistance, a precursor for gestational diabetes, may take place as early as the first trimester of pregnancy in women with risk factors for obstructive sleep apnea (OSA), such as overweight and habitual snoring.
This finding could potentially provide physicians with a window of opportunity to improve outcomes by screening at-risk women early in pregnancy or even prior to conception, Laura Sanapo, MD, assistant professor of medicine (research) at Brown University, Providence, R.I., and colleagues wrote in Sleep.
“Further studies are needed to investigate the association and its impact on the development of gestational diabetes, and to establish whether early-gestation or pregestational treatment of SDB would improve glucose metabolic outcomes in pregnancy,” they wrote.
”What this paper demonstrates is that the changes that predate gestational diabetes are seen much earlier in pregnancy,” senior study author Ghada Bourjeily, MD, professor of medicine at Brown University, said in an interview. Women should be screened for SDB rather than insulin resistance in early pregnancy since continuous positive airway pressure therapy (CPAP) is a highly effective intervention.
Waiting until midpregnancy to screen for OSA “is too late to make significant changes in the care of these women,” said Dr. Bourjeily, who is also director of research and training at the Women’s Medicine Collaborative at The Miriam Hospital in Providence, R.I. “By the time you diagnose gestational diabetes, the cat is out of the bag.”
For the study, women with early singleton pregnancies and risk factors for OSA such as habitual snoring and a median body mass index (BMI) of at least 27 kg/m2 were recruited from two prospective clinical trial studies enriched for OSA positivity. Women with a history of pregestational diabetes and those using CPAP or receiving chronic steroid therapy were excluded from the current study.
A total of 192 study participants underwent in-home sleep study (HSAT) and homeostatic model assessment (HOMA) between 11 and 15 gestational weeks, respectively. The association between continuous measures of SDB as a respiratory-event index as well as oxygen-desaturation index and glucose metabolism parameters such as insulin resistance (HOMA-IR) were analyzed after adjusting for gestational age, maternal age, BMI, ethnicity, race, and parity.
In all, 61 women (32%) were diagnosed with OSA based on respiratory event index values greater than or equal to five events per hour. These participants were more likely to be older, to have a high BMI, and to be multipara, compared with women who didn’t have a diagnosis of OSA. Women with a diagnosis of OSA exhibited higher glucose and C-peptide values and a higher degree of insulin resistance, compared with women without OSA, the researchers found. An increase of 0.3 in HOMA-IR related to maternal SDB in early pregnancy may significantly affect glucose metabolism.
Although the findings of the current study cannot be extrapolated to women who don’t have overweight or obesity, some women with normal-range BMI (18.5-24.9) are also at increased risk of glucose metabolism changes, Dr. Bourjeily pointed out. This includes those of Southeast Asian descent. “We found that the association of SDB parameters with insulin resistance was actually happening independently of BMI and other factors.”
Ideally, screening for SDB would begin prior to pregnancy, Dr. Bourjeily said. A BMI greater than 25 should be taken into account and patients asked if they snore and if so, whether it’s loud enough to wake their partner. They should also be asked about experiencing daytime sleepiness.
“Based on these answers, especially in women screened prior to pregnancy, there will be time to make the diagnosis of sleep apnea and get the patient on CPAP,” Dr. Bourjeily said.
“This is an interesting study and one of the rare ones looking at early pregnancy and some of the mechanisms that could possibly be contributing to gestational diabetes,” commented Grenye O’Malley, MD, assistant professor in the division of endocrinology, diabetes, and bone disease at the Icahn School of Medicine at Mount Sinai, New York. Dr. O’Malley was not involved in the study.
“It confirms our suspicions that there’s probably a lot of things happening earlier in pregnancy before a diagnosis of gestational diabetes. It also confirms that some of the mechanisms are probably very similar to those involved in the association between disordered sleep and the development of type 2 diabetes.”
However, it’s too early to determine whether screening for SDB and the use of CPAP will prevent glycemic changes, Dr. O’Malley said in an interview. “Whenever we screen, we ask whether we have an intervention that changes outcomes and we don’t know that yet.”
Some of the symptoms of SDB are also common in early pregnancy, such as a BMI greater than 25 and daytime sleepiness, Dr. O’Malley pointed out. It was unclear whether the study participants had a propensity to develop type 2 diabetes or whether they were at risk of gestational diabetes.
This study was funded by the National Heart, Lung, and Blood Institute; the National Institute for Child Health; and the National Institute of General Medical Sciences. Dr. Bourjeily and colleagues, as well as Dr. O’Malley, reported having no potential financial conflicts of interest.
FROM SLEEP
AHA advice for diabetes patients to stay heart healthy
A new document from the American Heart Association summarizes the latest research on cardiovascular risk factor management in type 2 diabetes, including medications, lifestyle, and social determinants of health.
Despite the availability of effective therapies for improving cardiovascular risk, in the United States fewer than one in five people with type 2 diabetes and without known cardiovascular disease meet control targets for a combination of A1c, blood pressure, LDL cholesterol, and nonsmoking status.
That proportion drops to less than 1 in 10 if body mass index less than 30 kg/m2 is included among the targets, and even less than that among individuals with established atherosclerotic cardiovascular disease, Joshua J. Joseph, MD, and colleagues point out in their paper, published online Jan. 10 in Circulation.
“This new scientific statement is an urgent call to action to follow the latest evidence-based approaches and to develop new best practices to advance type 2 diabetes treatment and care and reduce cardiovascular disease risk,” wrote Dr. Joseph, assistant professor of medicine in the division of endocrinology, diabetes, and metabolism at The Ohio State University, Columbus, Ohio, and coauthors.
The statement is not a guideline but an expert analysis that may inform future clinical practice guidelines, according to a press release from the AHA.
The new statement reviews evidence through June 2020 for lifestyle management of diabetes and weight, glycemic targets and control, blood pressure management, lipid management, antithrombotic therapy, and screening for cardiovascular and renal complications, including imaging. It also discusses the clinical implications of recent cardiovascular outcomes trials of newer glucose-lowering medications.
However, Dr. Joseph and colleagues point out, clinical care and treatment account for just 10%-20% of modifiable contributors to health outcomes. The other 80%-90% relate to social determinants of health, including health-related behaviors, socioeconomic factors, environmental factors, and racism.
“If we are to continue to advance the management of cardiovascular risk factors, we must also address the [social determinants of health] in the delivery of health care,” they noted.
Overall, they advise a patient-centered approach, meaning “reframing our clinical encounters to think about patients as people who live in families, communities, and societies that must be considered in their cardiovascular risk management.”
“People with [type 2 diabetes] face numerous barriers to health including access to care and equitable care, which must be considered when developing individualized care plans with our patients,” Dr. Joseph said in the AHA press release.
Lifestyle, medications for lowering A1c, BP, lipids
For lifestyle management, the authors say, “culturally appropriate recommendations through diabetes self-management education and support and medical nutrition therapy are key to meeting individualized goals for behavioral change and diabetes self-management.”
The document summarizes recommendations from other professional societies regarding glycemic targets and glucose lowering medications, i.e., target A1c levels of either < 7% or < 6.5% for the majority, with adjustments based on individual factors, such as life expectancy. It advises on use of metformin as first-line therapy followed by a sodium-glucose cotransporter-2 inhibitor or a glucagon-like peptide-1 agonist for those with established cardiovascular disease or risk factors.
“Cost may be a barrier to taking some [type 2 diabetes] medications as prescribed; however, many of these medications are now more commonly covered by more health insurance plans,” Dr. Joseph said.
“Another barrier is recognition by patients that these newer [type 2 diabetes] medications are also effective in reducing the risk of heart disease, stroke, heart failure, and kidney disease.”
Blood pressure treatment guidelines differ between those of the AHA/American College of Cardiology (ACC) and the American Diabetes Association (ADA), most notably that the AHA/ACC guidelines advise a general target of < 130/80 mm Hg, whereas ADA advises < 140/90 mm Hg or < 130/80 mm Hg for those with high risk if it can be safely achieved.
The decision should be “patient-centered with shared decision-making,” Dr. Joseph and colleagues advised.
For lipid-lowering, the document cites the 2018 ACC/AHA cholesterol guidelines, which include advising statins as first-line therapy for both primary and secondary prevention in diabetes, with highest intensity statins used in those at highest risk. But again, treatment should be individualized, and other agents should be used for patients in whom statins don’t work or aren’t tolerated.
And while use of antiplatelets – that is, aspirin – is well established as secondary prevention in type 2 diabetes, given new data suggesting that the risk for major bleeding could outweigh the benefits for primary prevention, “the relative benefits of antithrombotic approaches need to be weighed carefully against risks using a patient-centered approach,” the authors advised.
Among the many imaging tests available to facilitate cardiovascular risk stratification in type 2 diabetes, coronary artery calcification (CAC) CT screening is one of the few with sufficient data to support routine use in selected patients. The National Lipid Association, for example, recommends escalation to high-intensity statin for CAC > 100.
“One avenue to continue to address and advance diabetes management is through breaking down the four walls of the clinic or hospital through community engagement, clinic-to-community connections, and academic-community-government partnerships that may help address and support modifiable lifestyle behaviors such as physical activity, nutrition, smoking cessation and stress management,” Dr. Joseph concluded.
The AHA receives funding primarily from individuals. Foundations and corporations, including pharmaceutical, device manufacturers, and other companies, also make donations and fund AHA programs and events. The AHA’s strict policies prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers, and health insurance providers and the AHA’s financial information are available on the association’s website. Dr. Joseph has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new document from the American Heart Association summarizes the latest research on cardiovascular risk factor management in type 2 diabetes, including medications, lifestyle, and social determinants of health.
Despite the availability of effective therapies for improving cardiovascular risk, in the United States fewer than one in five people with type 2 diabetes and without known cardiovascular disease meet control targets for a combination of A1c, blood pressure, LDL cholesterol, and nonsmoking status.
That proportion drops to less than 1 in 10 if body mass index less than 30 kg/m2 is included among the targets, and even less than that among individuals with established atherosclerotic cardiovascular disease, Joshua J. Joseph, MD, and colleagues point out in their paper, published online Jan. 10 in Circulation.
“This new scientific statement is an urgent call to action to follow the latest evidence-based approaches and to develop new best practices to advance type 2 diabetes treatment and care and reduce cardiovascular disease risk,” wrote Dr. Joseph, assistant professor of medicine in the division of endocrinology, diabetes, and metabolism at The Ohio State University, Columbus, Ohio, and coauthors.
The statement is not a guideline but an expert analysis that may inform future clinical practice guidelines, according to a press release from the AHA.
The new statement reviews evidence through June 2020 for lifestyle management of diabetes and weight, glycemic targets and control, blood pressure management, lipid management, antithrombotic therapy, and screening for cardiovascular and renal complications, including imaging. It also discusses the clinical implications of recent cardiovascular outcomes trials of newer glucose-lowering medications.
However, Dr. Joseph and colleagues point out, clinical care and treatment account for just 10%-20% of modifiable contributors to health outcomes. The other 80%-90% relate to social determinants of health, including health-related behaviors, socioeconomic factors, environmental factors, and racism.
“If we are to continue to advance the management of cardiovascular risk factors, we must also address the [social determinants of health] in the delivery of health care,” they noted.
Overall, they advise a patient-centered approach, meaning “reframing our clinical encounters to think about patients as people who live in families, communities, and societies that must be considered in their cardiovascular risk management.”
“People with [type 2 diabetes] face numerous barriers to health including access to care and equitable care, which must be considered when developing individualized care plans with our patients,” Dr. Joseph said in the AHA press release.
Lifestyle, medications for lowering A1c, BP, lipids
For lifestyle management, the authors say, “culturally appropriate recommendations through diabetes self-management education and support and medical nutrition therapy are key to meeting individualized goals for behavioral change and diabetes self-management.”
The document summarizes recommendations from other professional societies regarding glycemic targets and glucose lowering medications, i.e., target A1c levels of either < 7% or < 6.5% for the majority, with adjustments based on individual factors, such as life expectancy. It advises on use of metformin as first-line therapy followed by a sodium-glucose cotransporter-2 inhibitor or a glucagon-like peptide-1 agonist for those with established cardiovascular disease or risk factors.
“Cost may be a barrier to taking some [type 2 diabetes] medications as prescribed; however, many of these medications are now more commonly covered by more health insurance plans,” Dr. Joseph said.
“Another barrier is recognition by patients that these newer [type 2 diabetes] medications are also effective in reducing the risk of heart disease, stroke, heart failure, and kidney disease.”
Blood pressure treatment guidelines differ between those of the AHA/American College of Cardiology (ACC) and the American Diabetes Association (ADA), most notably that the AHA/ACC guidelines advise a general target of < 130/80 mm Hg, whereas ADA advises < 140/90 mm Hg or < 130/80 mm Hg for those with high risk if it can be safely achieved.
The decision should be “patient-centered with shared decision-making,” Dr. Joseph and colleagues advised.
For lipid-lowering, the document cites the 2018 ACC/AHA cholesterol guidelines, which include advising statins as first-line therapy for both primary and secondary prevention in diabetes, with highest intensity statins used in those at highest risk. But again, treatment should be individualized, and other agents should be used for patients in whom statins don’t work or aren’t tolerated.
And while use of antiplatelets – that is, aspirin – is well established as secondary prevention in type 2 diabetes, given new data suggesting that the risk for major bleeding could outweigh the benefits for primary prevention, “the relative benefits of antithrombotic approaches need to be weighed carefully against risks using a patient-centered approach,” the authors advised.
Among the many imaging tests available to facilitate cardiovascular risk stratification in type 2 diabetes, coronary artery calcification (CAC) CT screening is one of the few with sufficient data to support routine use in selected patients. The National Lipid Association, for example, recommends escalation to high-intensity statin for CAC > 100.
“One avenue to continue to address and advance diabetes management is through breaking down the four walls of the clinic or hospital through community engagement, clinic-to-community connections, and academic-community-government partnerships that may help address and support modifiable lifestyle behaviors such as physical activity, nutrition, smoking cessation and stress management,” Dr. Joseph concluded.
The AHA receives funding primarily from individuals. Foundations and corporations, including pharmaceutical, device manufacturers, and other companies, also make donations and fund AHA programs and events. The AHA’s strict policies prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers, and health insurance providers and the AHA’s financial information are available on the association’s website. Dr. Joseph has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new document from the American Heart Association summarizes the latest research on cardiovascular risk factor management in type 2 diabetes, including medications, lifestyle, and social determinants of health.
Despite the availability of effective therapies for improving cardiovascular risk, in the United States fewer than one in five people with type 2 diabetes and without known cardiovascular disease meet control targets for a combination of A1c, blood pressure, LDL cholesterol, and nonsmoking status.
That proportion drops to less than 1 in 10 if body mass index less than 30 kg/m2 is included among the targets, and even less than that among individuals with established atherosclerotic cardiovascular disease, Joshua J. Joseph, MD, and colleagues point out in their paper, published online Jan. 10 in Circulation.
“This new scientific statement is an urgent call to action to follow the latest evidence-based approaches and to develop new best practices to advance type 2 diabetes treatment and care and reduce cardiovascular disease risk,” wrote Dr. Joseph, assistant professor of medicine in the division of endocrinology, diabetes, and metabolism at The Ohio State University, Columbus, Ohio, and coauthors.
The statement is not a guideline but an expert analysis that may inform future clinical practice guidelines, according to a press release from the AHA.
The new statement reviews evidence through June 2020 for lifestyle management of diabetes and weight, glycemic targets and control, blood pressure management, lipid management, antithrombotic therapy, and screening for cardiovascular and renal complications, including imaging. It also discusses the clinical implications of recent cardiovascular outcomes trials of newer glucose-lowering medications.
However, Dr. Joseph and colleagues point out, clinical care and treatment account for just 10%-20% of modifiable contributors to health outcomes. The other 80%-90% relate to social determinants of health, including health-related behaviors, socioeconomic factors, environmental factors, and racism.
“If we are to continue to advance the management of cardiovascular risk factors, we must also address the [social determinants of health] in the delivery of health care,” they noted.
Overall, they advise a patient-centered approach, meaning “reframing our clinical encounters to think about patients as people who live in families, communities, and societies that must be considered in their cardiovascular risk management.”
“People with [type 2 diabetes] face numerous barriers to health including access to care and equitable care, which must be considered when developing individualized care plans with our patients,” Dr. Joseph said in the AHA press release.
Lifestyle, medications for lowering A1c, BP, lipids
For lifestyle management, the authors say, “culturally appropriate recommendations through diabetes self-management education and support and medical nutrition therapy are key to meeting individualized goals for behavioral change and diabetes self-management.”
The document summarizes recommendations from other professional societies regarding glycemic targets and glucose lowering medications, i.e., target A1c levels of either < 7% or < 6.5% for the majority, with adjustments based on individual factors, such as life expectancy. It advises on use of metformin as first-line therapy followed by a sodium-glucose cotransporter-2 inhibitor or a glucagon-like peptide-1 agonist for those with established cardiovascular disease or risk factors.
“Cost may be a barrier to taking some [type 2 diabetes] medications as prescribed; however, many of these medications are now more commonly covered by more health insurance plans,” Dr. Joseph said.
“Another barrier is recognition by patients that these newer [type 2 diabetes] medications are also effective in reducing the risk of heart disease, stroke, heart failure, and kidney disease.”
Blood pressure treatment guidelines differ between those of the AHA/American College of Cardiology (ACC) and the American Diabetes Association (ADA), most notably that the AHA/ACC guidelines advise a general target of < 130/80 mm Hg, whereas ADA advises < 140/90 mm Hg or < 130/80 mm Hg for those with high risk if it can be safely achieved.
The decision should be “patient-centered with shared decision-making,” Dr. Joseph and colleagues advised.
For lipid-lowering, the document cites the 2018 ACC/AHA cholesterol guidelines, which include advising statins as first-line therapy for both primary and secondary prevention in diabetes, with highest intensity statins used in those at highest risk. But again, treatment should be individualized, and other agents should be used for patients in whom statins don’t work or aren’t tolerated.
And while use of antiplatelets – that is, aspirin – is well established as secondary prevention in type 2 diabetes, given new data suggesting that the risk for major bleeding could outweigh the benefits for primary prevention, “the relative benefits of antithrombotic approaches need to be weighed carefully against risks using a patient-centered approach,” the authors advised.
Among the many imaging tests available to facilitate cardiovascular risk stratification in type 2 diabetes, coronary artery calcification (CAC) CT screening is one of the few with sufficient data to support routine use in selected patients. The National Lipid Association, for example, recommends escalation to high-intensity statin for CAC > 100.
“One avenue to continue to address and advance diabetes management is through breaking down the four walls of the clinic or hospital through community engagement, clinic-to-community connections, and academic-community-government partnerships that may help address and support modifiable lifestyle behaviors such as physical activity, nutrition, smoking cessation and stress management,” Dr. Joseph concluded.
The AHA receives funding primarily from individuals. Foundations and corporations, including pharmaceutical, device manufacturers, and other companies, also make donations and fund AHA programs and events. The AHA’s strict policies prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers, and health insurance providers and the AHA’s financial information are available on the association’s website. Dr. Joseph has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 linked to increased diabetes risk in youth
SARS-CoV-2 infection was associated with an increased risk for diabetes among youth, whereas other acute respiratory infections were not, new data from the U.S. Centers for Disease Control and Prevention indicate.
The results from two large U.S. health claims databases were published in an early release in the CDC’s Morbidity and Mortality Weekly Report by Catherine E. Barrett, PhD, and colleagues of the CDC’s COVID-19 Emergency Response Team and Division of Diabetes Translation.
Clinicians should monitor individuals younger than 18 years in the months following a SARS-CoV-2 infection for new diabetes onset, they advise.
The findings, which are supported by independent studies in adults, “underscore the importance of COVID-19 prevention among all age groups, including vaccination for all eligible children and adolescents, and chronic disease prevention and treatment,” Dr. Barrett and colleagues say.
Diabetes type couldn’t be reliably distinguished from the databases, which is noted as an important study limitation.
“SARS-CoV-2 infection might lead to type 1 or type 2 diabetes through complex and differing mechanisms,” they say.
Emerging evidence began to suggest, in mid-2020, that COVID-19 may trigger the onset of diabetes in healthy people. A new global registry was subsequently established to collect data on patients with COVID-19–related diabetes, called the CoviDiab registry.
Not clear if diabetes after COVID-19 is transient or permanent
From one of the databases used in the new study, known as IQVIA, 80,893 individuals aged younger than 18 years diagnosed with COVID-19 during March 2020 to February 26, 2021, were compared with age- and sex-matched people during that period who did not have COVID-19 and to prepandemic groups with and without a diagnosis of acute respiratory illness during March 1, 2017, to February 26, 2018.
From the second database, HealthVerity, 439,439 youth diagnosed with COVID-19 during March 1, 2020, to June 28, 2021, were compared with age- and sex-matched youth without COVID-19. Here, there was no prepandemic comparison group.
Diabetes diagnoses were coded in 0.08% with COVID-19 vs. 0.03% without COVID-19 in IQVIA and in 0.25% vs. 0.19% in HealthVerity.
Thus, new diabetes diagnoses were 166% and 31% more likely to occur in those with COVID-19 in IQVIA and HealthVerity, respectively. And in IQVIA, those with COVID-19 were 116% more likely to develop diabetes than were those with prepandemic acute respiratory illnesses. Those differences were all significant, whereas non–SARS-CoV-2 respiratory infections were not associated with diabetes, Dr. Barrett and colleagues say.
In both databases, diabetic ketoacidosis (DKA) was more common at diabetes onset among those with, vs. without, COVID-19: 48.5% vs. 13.6% in IQVIA and 40.2% vs. 29.7% in HealthVerity. In IQVIA, 22.0% with prepandemic acute respiratory illness presented with DKA.
Dr. Barrett and colleagues offer several potential explanations for the observed association between COVID-19 and diabetes, including a direct attack on pancreatic beta cells expressing angiotensin-converting enzyme 2 receptors, or via stress hyperglycemia resulting from cytokine storm and alterations in glucose metabolism.
Another possibility is the precipitation to diabetes from prediabetes; the latter is a condition present in one in five U.S. adolescents.
Steroid treatment during hospitalization might have led to transient hyperglycemia, but only 1.5% to 2.2% of diabetes codes were for drug- or chemical-induced diabetes. The majority were for type 1 or 2.
Alternatively, pandemic-associated weight gain might have also contributed to risks for both severe COVID-19 and type 2 diabetes.
“Although this study can provide information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition,” Dr. Barrett and colleagues conclude.
A version of this article first appeared on Medscape.com.
SARS-CoV-2 infection was associated with an increased risk for diabetes among youth, whereas other acute respiratory infections were not, new data from the U.S. Centers for Disease Control and Prevention indicate.
The results from two large U.S. health claims databases were published in an early release in the CDC’s Morbidity and Mortality Weekly Report by Catherine E. Barrett, PhD, and colleagues of the CDC’s COVID-19 Emergency Response Team and Division of Diabetes Translation.
Clinicians should monitor individuals younger than 18 years in the months following a SARS-CoV-2 infection for new diabetes onset, they advise.
The findings, which are supported by independent studies in adults, “underscore the importance of COVID-19 prevention among all age groups, including vaccination for all eligible children and adolescents, and chronic disease prevention and treatment,” Dr. Barrett and colleagues say.
Diabetes type couldn’t be reliably distinguished from the databases, which is noted as an important study limitation.
“SARS-CoV-2 infection might lead to type 1 or type 2 diabetes through complex and differing mechanisms,” they say.
Emerging evidence began to suggest, in mid-2020, that COVID-19 may trigger the onset of diabetes in healthy people. A new global registry was subsequently established to collect data on patients with COVID-19–related diabetes, called the CoviDiab registry.
Not clear if diabetes after COVID-19 is transient or permanent
From one of the databases used in the new study, known as IQVIA, 80,893 individuals aged younger than 18 years diagnosed with COVID-19 during March 2020 to February 26, 2021, were compared with age- and sex-matched people during that period who did not have COVID-19 and to prepandemic groups with and without a diagnosis of acute respiratory illness during March 1, 2017, to February 26, 2018.
From the second database, HealthVerity, 439,439 youth diagnosed with COVID-19 during March 1, 2020, to June 28, 2021, were compared with age- and sex-matched youth without COVID-19. Here, there was no prepandemic comparison group.
Diabetes diagnoses were coded in 0.08% with COVID-19 vs. 0.03% without COVID-19 in IQVIA and in 0.25% vs. 0.19% in HealthVerity.
Thus, new diabetes diagnoses were 166% and 31% more likely to occur in those with COVID-19 in IQVIA and HealthVerity, respectively. And in IQVIA, those with COVID-19 were 116% more likely to develop diabetes than were those with prepandemic acute respiratory illnesses. Those differences were all significant, whereas non–SARS-CoV-2 respiratory infections were not associated with diabetes, Dr. Barrett and colleagues say.
In both databases, diabetic ketoacidosis (DKA) was more common at diabetes onset among those with, vs. without, COVID-19: 48.5% vs. 13.6% in IQVIA and 40.2% vs. 29.7% in HealthVerity. In IQVIA, 22.0% with prepandemic acute respiratory illness presented with DKA.
Dr. Barrett and colleagues offer several potential explanations for the observed association between COVID-19 and diabetes, including a direct attack on pancreatic beta cells expressing angiotensin-converting enzyme 2 receptors, or via stress hyperglycemia resulting from cytokine storm and alterations in glucose metabolism.
Another possibility is the precipitation to diabetes from prediabetes; the latter is a condition present in one in five U.S. adolescents.
Steroid treatment during hospitalization might have led to transient hyperglycemia, but only 1.5% to 2.2% of diabetes codes were for drug- or chemical-induced diabetes. The majority were for type 1 or 2.
Alternatively, pandemic-associated weight gain might have also contributed to risks for both severe COVID-19 and type 2 diabetes.
“Although this study can provide information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition,” Dr. Barrett and colleagues conclude.
A version of this article first appeared on Medscape.com.
SARS-CoV-2 infection was associated with an increased risk for diabetes among youth, whereas other acute respiratory infections were not, new data from the U.S. Centers for Disease Control and Prevention indicate.
The results from two large U.S. health claims databases were published in an early release in the CDC’s Morbidity and Mortality Weekly Report by Catherine E. Barrett, PhD, and colleagues of the CDC’s COVID-19 Emergency Response Team and Division of Diabetes Translation.
Clinicians should monitor individuals younger than 18 years in the months following a SARS-CoV-2 infection for new diabetes onset, they advise.
The findings, which are supported by independent studies in adults, “underscore the importance of COVID-19 prevention among all age groups, including vaccination for all eligible children and adolescents, and chronic disease prevention and treatment,” Dr. Barrett and colleagues say.
Diabetes type couldn’t be reliably distinguished from the databases, which is noted as an important study limitation.
“SARS-CoV-2 infection might lead to type 1 or type 2 diabetes through complex and differing mechanisms,” they say.
Emerging evidence began to suggest, in mid-2020, that COVID-19 may trigger the onset of diabetes in healthy people. A new global registry was subsequently established to collect data on patients with COVID-19–related diabetes, called the CoviDiab registry.
Not clear if diabetes after COVID-19 is transient or permanent
From one of the databases used in the new study, known as IQVIA, 80,893 individuals aged younger than 18 years diagnosed with COVID-19 during March 2020 to February 26, 2021, were compared with age- and sex-matched people during that period who did not have COVID-19 and to prepandemic groups with and without a diagnosis of acute respiratory illness during March 1, 2017, to February 26, 2018.
From the second database, HealthVerity, 439,439 youth diagnosed with COVID-19 during March 1, 2020, to June 28, 2021, were compared with age- and sex-matched youth without COVID-19. Here, there was no prepandemic comparison group.
Diabetes diagnoses were coded in 0.08% with COVID-19 vs. 0.03% without COVID-19 in IQVIA and in 0.25% vs. 0.19% in HealthVerity.
Thus, new diabetes diagnoses were 166% and 31% more likely to occur in those with COVID-19 in IQVIA and HealthVerity, respectively. And in IQVIA, those with COVID-19 were 116% more likely to develop diabetes than were those with prepandemic acute respiratory illnesses. Those differences were all significant, whereas non–SARS-CoV-2 respiratory infections were not associated with diabetes, Dr. Barrett and colleagues say.
In both databases, diabetic ketoacidosis (DKA) was more common at diabetes onset among those with, vs. without, COVID-19: 48.5% vs. 13.6% in IQVIA and 40.2% vs. 29.7% in HealthVerity. In IQVIA, 22.0% with prepandemic acute respiratory illness presented with DKA.
Dr. Barrett and colleagues offer several potential explanations for the observed association between COVID-19 and diabetes, including a direct attack on pancreatic beta cells expressing angiotensin-converting enzyme 2 receptors, or via stress hyperglycemia resulting from cytokine storm and alterations in glucose metabolism.
Another possibility is the precipitation to diabetes from prediabetes; the latter is a condition present in one in five U.S. adolescents.
Steroid treatment during hospitalization might have led to transient hyperglycemia, but only 1.5% to 2.2% of diabetes codes were for drug- or chemical-induced diabetes. The majority were for type 1 or 2.
Alternatively, pandemic-associated weight gain might have also contributed to risks for both severe COVID-19 and type 2 diabetes.
“Although this study can provide information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition,” Dr. Barrett and colleagues conclude.
A version of this article first appeared on Medscape.com.
FROM MMWR