User login
Official Newspaper of the American College of Surgeons
Home discharge with total artificial heart is feasible, safe
LOS ANGELES – Some patients with a total artificial heart can safely go home with the use of a small portable driver while awaiting heart transplantation, according to data from the first U.S. patient cohort in whom this was attempted.
Investigators assessed outcomes in 13 total artificial heart recipients who were stable enough clinically to be transitioned from the usual driver to SynCardia Systems’ investigational portable driver, the Freedom Driver System. The driver weighs 14 pounds and allows several hours of untethered activity.
Eight of the patients were able to go home for an average of 5.5 months, lead investigator Dr. Vigneshwar Kasirajan reported at the annual meeting of the Society of Thoracic Surgeons.
They had a low rate of major bleeding and no major infections. There were roughly five device malfunctions per patient-year, but in all cases, patients were able to switch to a backup driver uneventfully.
Twelve of the 13 total patients ultimately underwent transplantation, for a transplantation rate of 92%.
"The Freedom driver is effective in supporting circulation with a total artificial heart. Discharge home is safe and feasible," commented Dr. Kasirajan, who is director of heart transplantation, heart-lung transplantation, and mechanical circulatory support at Virginia Commonwealth University in Richmond.
"Further data on the completion of this study will help to demonstrate the efficacy and safety of the driver. In addition, important data on exercise capacity and quality of life will be valuable in finally moving the artificial heart technology to more widespread use," he said.
Session comoderator Dr. Todd M. Dewey, a cardiothoracic surgeon with Medical City Specialists in Dallas, noted, "The majority of patients on axial-flow left ventricular assist devices are discharged home. What percentage of total artificial heart patients do you think will ultimately leave the hospital?"
"We are close to 80% of our patients going home right now, at least in high-volume institutions," Dr. Kasirajan replied. Two patients have been at home for more than 2 years without readmissions related to the device, he added.
A pivotal study previously showed that the total artificial heart can be used as a bridge to transplantation in patients with irreversible biventricular failure (N. Engl. J. Med. 2004;351:859-67).
"Unfortunately, ... the widespread use of this technology is limited because of the inability to discharge these patients home, and that relates to the fact that the circulatory support system console has to be powered by compressed air either from the hospital or via a cylinder," Dr. Kasirajan explained.
However, once patients are stable, the driver settings need little adjustment, which spurred development of the portable driver. "The driver has two batteries that allow up to 3 hours of untethered activity. These can be charged in place using an alternating current output or car charger," he said.
The ongoing study of the driver will enroll up to 60 patients from 30 international sites. Patients are required to be wait-listed for heart transplantation and receive a total artificial heart, and to be clinically stable on the circulatory support system, with a cardiac index of at least 2.2 L/min/m2. They are then switched to the portable driver with the intent of discharge from the hospital.
Dr. Kasirajan reported results for the first 13 patients enrolled from four U.S. sites. Overall, 5 of the patients remained in the hospital (because of medical reasons, discharge logistics, or personal preference), whereas 8 went home with the driver. The median duration out of the hospital in the latter group was 162 days (range, 39-437 days).
The 13 patients had maintenance of cardiac function, with a cardiac index averaging 3.3 L/min/m2, and their laboratory values remained stable between baseline and 90 days. "Particularly, there was no evidence of hemolysis that was worse than at the beginning," he noted. "Increasing albumin levels reflect the increasing nutritional status in these patients."
The in-hospital group had a very similar rate of adverse events relative to an earlier comparison cohort of stable patients with a total artificial heart followed as part of postmarket surveillance, according to Dr. Kasirajan.
Within the study population, the out-of-hospital and in-hospital groups had similar rates of major bleeding (1.1 vs. 1.4 events per patient-year). The former had a lower rate of major infection (0 vs. 2.8 events per patient-year) but higher rates of device malfunction (4.6 vs. 0 events per patient-year) and hemolysis (2.3 vs. 0 events per patient-year).
The five device malfunctions in the out-of-hospital group were due to a Valsalva maneuver, a faulty sensor, hypertension, a kink in the driveline while a patient was getting into a car, and dropping of the driver while showering.
"All these patients remained stable and had no changes in cardiac output," Dr. Kasirajan pointed out. "They were able to switch to the backup driver as educated, and returned to the hospital."
Valsalva maneuvers can cause a sudden transient rise in intrathoracic pressure that a device sensor interprets as outside the set parameters, he explained; the software has since been modified to allow for these changes.
"The importance of hypertension management is critical," he commented. "The pump tolerates blood pressures at high levels for brief periods of time; however, prolonged hypertension leads to a decrease in left heart cardiac output and pulmonary edema."
The cases of hemolysis were due to transient rises in plasma free hemoglobin as a result of hemothorax and hydralazine-induced hemolytic anemia.
Only a single patient, in the out-of-hospital group, died before transplantation. This patient was stable on the driver for 437 days, but experienced a fall with a spinal cord hematoma, and developed fatal complications.
Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
LOS ANGELES – Some patients with a total artificial heart can safely go home with the use of a small portable driver while awaiting heart transplantation, according to data from the first U.S. patient cohort in whom this was attempted.
Investigators assessed outcomes in 13 total artificial heart recipients who were stable enough clinically to be transitioned from the usual driver to SynCardia Systems’ investigational portable driver, the Freedom Driver System. The driver weighs 14 pounds and allows several hours of untethered activity.
Eight of the patients were able to go home for an average of 5.5 months, lead investigator Dr. Vigneshwar Kasirajan reported at the annual meeting of the Society of Thoracic Surgeons.
They had a low rate of major bleeding and no major infections. There were roughly five device malfunctions per patient-year, but in all cases, patients were able to switch to a backup driver uneventfully.
Twelve of the 13 total patients ultimately underwent transplantation, for a transplantation rate of 92%.
"The Freedom driver is effective in supporting circulation with a total artificial heart. Discharge home is safe and feasible," commented Dr. Kasirajan, who is director of heart transplantation, heart-lung transplantation, and mechanical circulatory support at Virginia Commonwealth University in Richmond.
"Further data on the completion of this study will help to demonstrate the efficacy and safety of the driver. In addition, important data on exercise capacity and quality of life will be valuable in finally moving the artificial heart technology to more widespread use," he said.
Session comoderator Dr. Todd M. Dewey, a cardiothoracic surgeon with Medical City Specialists in Dallas, noted, "The majority of patients on axial-flow left ventricular assist devices are discharged home. What percentage of total artificial heart patients do you think will ultimately leave the hospital?"
"We are close to 80% of our patients going home right now, at least in high-volume institutions," Dr. Kasirajan replied. Two patients have been at home for more than 2 years without readmissions related to the device, he added.
A pivotal study previously showed that the total artificial heart can be used as a bridge to transplantation in patients with irreversible biventricular failure (N. Engl. J. Med. 2004;351:859-67).
"Unfortunately, ... the widespread use of this technology is limited because of the inability to discharge these patients home, and that relates to the fact that the circulatory support system console has to be powered by compressed air either from the hospital or via a cylinder," Dr. Kasirajan explained.
However, once patients are stable, the driver settings need little adjustment, which spurred development of the portable driver. "The driver has two batteries that allow up to 3 hours of untethered activity. These can be charged in place using an alternating current output or car charger," he said.
The ongoing study of the driver will enroll up to 60 patients from 30 international sites. Patients are required to be wait-listed for heart transplantation and receive a total artificial heart, and to be clinically stable on the circulatory support system, with a cardiac index of at least 2.2 L/min/m2. They are then switched to the portable driver with the intent of discharge from the hospital.
Dr. Kasirajan reported results for the first 13 patients enrolled from four U.S. sites. Overall, 5 of the patients remained in the hospital (because of medical reasons, discharge logistics, or personal preference), whereas 8 went home with the driver. The median duration out of the hospital in the latter group was 162 days (range, 39-437 days).
The 13 patients had maintenance of cardiac function, with a cardiac index averaging 3.3 L/min/m2, and their laboratory values remained stable between baseline and 90 days. "Particularly, there was no evidence of hemolysis that was worse than at the beginning," he noted. "Increasing albumin levels reflect the increasing nutritional status in these patients."
The in-hospital group had a very similar rate of adverse events relative to an earlier comparison cohort of stable patients with a total artificial heart followed as part of postmarket surveillance, according to Dr. Kasirajan.
Within the study population, the out-of-hospital and in-hospital groups had similar rates of major bleeding (1.1 vs. 1.4 events per patient-year). The former had a lower rate of major infection (0 vs. 2.8 events per patient-year) but higher rates of device malfunction (4.6 vs. 0 events per patient-year) and hemolysis (2.3 vs. 0 events per patient-year).
The five device malfunctions in the out-of-hospital group were due to a Valsalva maneuver, a faulty sensor, hypertension, a kink in the driveline while a patient was getting into a car, and dropping of the driver while showering.
"All these patients remained stable and had no changes in cardiac output," Dr. Kasirajan pointed out. "They were able to switch to the backup driver as educated, and returned to the hospital."
Valsalva maneuvers can cause a sudden transient rise in intrathoracic pressure that a device sensor interprets as outside the set parameters, he explained; the software has since been modified to allow for these changes.
"The importance of hypertension management is critical," he commented. "The pump tolerates blood pressures at high levels for brief periods of time; however, prolonged hypertension leads to a decrease in left heart cardiac output and pulmonary edema."
The cases of hemolysis were due to transient rises in plasma free hemoglobin as a result of hemothorax and hydralazine-induced hemolytic anemia.
Only a single patient, in the out-of-hospital group, died before transplantation. This patient was stable on the driver for 437 days, but experienced a fall with a spinal cord hematoma, and developed fatal complications.
Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
LOS ANGELES – Some patients with a total artificial heart can safely go home with the use of a small portable driver while awaiting heart transplantation, according to data from the first U.S. patient cohort in whom this was attempted.
Investigators assessed outcomes in 13 total artificial heart recipients who were stable enough clinically to be transitioned from the usual driver to SynCardia Systems’ investigational portable driver, the Freedom Driver System. The driver weighs 14 pounds and allows several hours of untethered activity.
Eight of the patients were able to go home for an average of 5.5 months, lead investigator Dr. Vigneshwar Kasirajan reported at the annual meeting of the Society of Thoracic Surgeons.
They had a low rate of major bleeding and no major infections. There were roughly five device malfunctions per patient-year, but in all cases, patients were able to switch to a backup driver uneventfully.
Twelve of the 13 total patients ultimately underwent transplantation, for a transplantation rate of 92%.
"The Freedom driver is effective in supporting circulation with a total artificial heart. Discharge home is safe and feasible," commented Dr. Kasirajan, who is director of heart transplantation, heart-lung transplantation, and mechanical circulatory support at Virginia Commonwealth University in Richmond.
"Further data on the completion of this study will help to demonstrate the efficacy and safety of the driver. In addition, important data on exercise capacity and quality of life will be valuable in finally moving the artificial heart technology to more widespread use," he said.
Session comoderator Dr. Todd M. Dewey, a cardiothoracic surgeon with Medical City Specialists in Dallas, noted, "The majority of patients on axial-flow left ventricular assist devices are discharged home. What percentage of total artificial heart patients do you think will ultimately leave the hospital?"
"We are close to 80% of our patients going home right now, at least in high-volume institutions," Dr. Kasirajan replied. Two patients have been at home for more than 2 years without readmissions related to the device, he added.
A pivotal study previously showed that the total artificial heart can be used as a bridge to transplantation in patients with irreversible biventricular failure (N. Engl. J. Med. 2004;351:859-67).
"Unfortunately, ... the widespread use of this technology is limited because of the inability to discharge these patients home, and that relates to the fact that the circulatory support system console has to be powered by compressed air either from the hospital or via a cylinder," Dr. Kasirajan explained.
However, once patients are stable, the driver settings need little adjustment, which spurred development of the portable driver. "The driver has two batteries that allow up to 3 hours of untethered activity. These can be charged in place using an alternating current output or car charger," he said.
The ongoing study of the driver will enroll up to 60 patients from 30 international sites. Patients are required to be wait-listed for heart transplantation and receive a total artificial heart, and to be clinically stable on the circulatory support system, with a cardiac index of at least 2.2 L/min/m2. They are then switched to the portable driver with the intent of discharge from the hospital.
Dr. Kasirajan reported results for the first 13 patients enrolled from four U.S. sites. Overall, 5 of the patients remained in the hospital (because of medical reasons, discharge logistics, or personal preference), whereas 8 went home with the driver. The median duration out of the hospital in the latter group was 162 days (range, 39-437 days).
The 13 patients had maintenance of cardiac function, with a cardiac index averaging 3.3 L/min/m2, and their laboratory values remained stable between baseline and 90 days. "Particularly, there was no evidence of hemolysis that was worse than at the beginning," he noted. "Increasing albumin levels reflect the increasing nutritional status in these patients."
The in-hospital group had a very similar rate of adverse events relative to an earlier comparison cohort of stable patients with a total artificial heart followed as part of postmarket surveillance, according to Dr. Kasirajan.
Within the study population, the out-of-hospital and in-hospital groups had similar rates of major bleeding (1.1 vs. 1.4 events per patient-year). The former had a lower rate of major infection (0 vs. 2.8 events per patient-year) but higher rates of device malfunction (4.6 vs. 0 events per patient-year) and hemolysis (2.3 vs. 0 events per patient-year).
The five device malfunctions in the out-of-hospital group were due to a Valsalva maneuver, a faulty sensor, hypertension, a kink in the driveline while a patient was getting into a car, and dropping of the driver while showering.
"All these patients remained stable and had no changes in cardiac output," Dr. Kasirajan pointed out. "They were able to switch to the backup driver as educated, and returned to the hospital."
Valsalva maneuvers can cause a sudden transient rise in intrathoracic pressure that a device sensor interprets as outside the set parameters, he explained; the software has since been modified to allow for these changes.
"The importance of hypertension management is critical," he commented. "The pump tolerates blood pressures at high levels for brief periods of time; however, prolonged hypertension leads to a decrease in left heart cardiac output and pulmonary edema."
The cases of hemolysis were due to transient rises in plasma free hemoglobin as a result of hemothorax and hydralazine-induced hemolytic anemia.
Only a single patient, in the out-of-hospital group, died before transplantation. This patient was stable on the driver for 437 days, but experienced a fall with a spinal cord hematoma, and developed fatal complications.
Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
AT THE STS ANNUAL MEETING
Major finding: The eight patients who were able to go home had a low rate of major bleeding and no major infections. The rate of device malfunctions was 4.6 events per patient-year, but none of these patients experienced a change in cardiac output.
Data source: An interim analysis of a cohort study among 13 clinically stable patients with a total artificial heart powered by a portable driver.
Disclosures: Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
Mold again found in compounded product
A compounding pharmacy has issued a nationwide voluntary recall of all of its products after mold was discovered in one of its intravenous solutions. To date, no injuries or illnesses have been reported in association with the contaminated product: magnesium sulfate 2 g in dextrose 5% in water, 50 mL for injection.
The compounding pharmacy, Med Prep Consulting Inc., announced in a statement that it has voluntarily recalled all lots of all products compounded at its facility after clinicians at a Connecticut hospital notified the company that visible particulate contaminants were observed in five 50-mL bags of the product. These were unique and distinct lots compounded and dispensed by the pharmacy to the Connecticut hospital, according to the company.
The contaminants were subsequently confirmed to be mold; the pharmacy then decided to voluntarily recall all of its compounded products because of lack of sterility assurance.
Injectable steroids contaminated with mold and produced by a different compounding pharmacy were discovered last October and resulted in numerous infections and deaths nationwide. The issue also was part of a recent Institute of Medicine report on drug quality concerns.
Products produced by Med Prep Consulting are used for a wide range of therapeutic purposes in hospitals, outpatient facilities, and physicians’ offices. None are dispensed directly to patients for either self-administration or nursing administration. All products are packaged in plastic infusion bags, plastic infusion devices, plastic syringes, or glass vials.
Recalled products packaged in plastic infusion bags, plastic infusion devices, plastic syringes, and glass vials were distributed directly to regional hospital pharmacies in New Jersey, Pennsylvania, Connecticut, and Delaware.
Recalled products packaged in plastic syringes were distributed nationwide to physician office practice facilities and clinics. All of these products were distributed through March 17, 2013, from Tinton Falls, N.J., to both regional and nationwide locations.
All recipients of products compounded by Med Prep Consulting have been notified by telephone, fax, e-mail, and regular mail of the recall and have been instructed to remove and return the product to the pharmacy. Facilities with questions may contact the company at 732-493-3390. The company has asked that product complaints related to this recall be reported to the same number.
Adverse events that may be related to the use of these products should be reported to FDA’s MedWatch Adverse Event Reporting Program.
A compounding pharmacy has issued a nationwide voluntary recall of all of its products after mold was discovered in one of its intravenous solutions. To date, no injuries or illnesses have been reported in association with the contaminated product: magnesium sulfate 2 g in dextrose 5% in water, 50 mL for injection.
The compounding pharmacy, Med Prep Consulting Inc., announced in a statement that it has voluntarily recalled all lots of all products compounded at its facility after clinicians at a Connecticut hospital notified the company that visible particulate contaminants were observed in five 50-mL bags of the product. These were unique and distinct lots compounded and dispensed by the pharmacy to the Connecticut hospital, according to the company.
The contaminants were subsequently confirmed to be mold; the pharmacy then decided to voluntarily recall all of its compounded products because of lack of sterility assurance.
Injectable steroids contaminated with mold and produced by a different compounding pharmacy were discovered last October and resulted in numerous infections and deaths nationwide. The issue also was part of a recent Institute of Medicine report on drug quality concerns.
Products produced by Med Prep Consulting are used for a wide range of therapeutic purposes in hospitals, outpatient facilities, and physicians’ offices. None are dispensed directly to patients for either self-administration or nursing administration. All products are packaged in plastic infusion bags, plastic infusion devices, plastic syringes, or glass vials.
Recalled products packaged in plastic infusion bags, plastic infusion devices, plastic syringes, and glass vials were distributed directly to regional hospital pharmacies in New Jersey, Pennsylvania, Connecticut, and Delaware.
Recalled products packaged in plastic syringes were distributed nationwide to physician office practice facilities and clinics. All of these products were distributed through March 17, 2013, from Tinton Falls, N.J., to both regional and nationwide locations.
All recipients of products compounded by Med Prep Consulting have been notified by telephone, fax, e-mail, and regular mail of the recall and have been instructed to remove and return the product to the pharmacy. Facilities with questions may contact the company at 732-493-3390. The company has asked that product complaints related to this recall be reported to the same number.
Adverse events that may be related to the use of these products should be reported to FDA’s MedWatch Adverse Event Reporting Program.
A compounding pharmacy has issued a nationwide voluntary recall of all of its products after mold was discovered in one of its intravenous solutions. To date, no injuries or illnesses have been reported in association with the contaminated product: magnesium sulfate 2 g in dextrose 5% in water, 50 mL for injection.
The compounding pharmacy, Med Prep Consulting Inc., announced in a statement that it has voluntarily recalled all lots of all products compounded at its facility after clinicians at a Connecticut hospital notified the company that visible particulate contaminants were observed in five 50-mL bags of the product. These were unique and distinct lots compounded and dispensed by the pharmacy to the Connecticut hospital, according to the company.
The contaminants were subsequently confirmed to be mold; the pharmacy then decided to voluntarily recall all of its compounded products because of lack of sterility assurance.
Injectable steroids contaminated with mold and produced by a different compounding pharmacy were discovered last October and resulted in numerous infections and deaths nationwide. The issue also was part of a recent Institute of Medicine report on drug quality concerns.
Products produced by Med Prep Consulting are used for a wide range of therapeutic purposes in hospitals, outpatient facilities, and physicians’ offices. None are dispensed directly to patients for either self-administration or nursing administration. All products are packaged in plastic infusion bags, plastic infusion devices, plastic syringes, or glass vials.
Recalled products packaged in plastic infusion bags, plastic infusion devices, plastic syringes, and glass vials were distributed directly to regional hospital pharmacies in New Jersey, Pennsylvania, Connecticut, and Delaware.
Recalled products packaged in plastic syringes were distributed nationwide to physician office practice facilities and clinics. All of these products were distributed through March 17, 2013, from Tinton Falls, N.J., to both regional and nationwide locations.
All recipients of products compounded by Med Prep Consulting have been notified by telephone, fax, e-mail, and regular mail of the recall and have been instructed to remove and return the product to the pharmacy. Facilities with questions may contact the company at 732-493-3390. The company has asked that product complaints related to this recall be reported to the same number.
Adverse events that may be related to the use of these products should be reported to FDA’s MedWatch Adverse Event Reporting Program.
Contralateral prophylactic mastectomy adds complications
NATIONAL HARBOR, MD. – The rate of contralateral prophylactic mastectomies is rising, even though there is no evidence for a survival benefit.
From 1998 through 2007, contralateral prophylactic mastectomies (CPM) were performed within 1 year of unilateral mastectomies in 21% of those with ductal carcinoma in situ (DCIS) and in 17% of those with stage I-III breast cancer who were treated at one of 10 National Comprehensive Cancer Network (NCCN) centers.
But in an analysis of overall survival for patients with stages I-III invasive breast cancer, there was so significant difference in overall survival for patients who underwent a CPM, compared with those who underwent only unilateral mastectomy, regardless of whether they had received neoadjuvant chemotherapy, reported Dr. William E. Carson III, professor of surgery at the Ohio State University Comprehensive Cancer Center in Columbus.
In addition, CPMs are associated with a significantly greater risk of complications than unilateral mastectomies, including increased risk for major complications requiring reoperation and rehospitalization, said Dr. Megan Miller, a surgery resident at the University of Chicago, Illinois.
"CPM patients are 1.5 times more likely to have any complication, and 2.6 times more likely to have a major complication than unilateral mastectomy patients," she said at the annual Society of Surgical Oncology Cancer Symposium.
Among patients who underwent CPM, almost 40% of the complications occurred on the side of the body without cancer, she noted.
SSO position statement
A 2007 position statement from the Society of Surgical Oncology (SSO) states that in patients with a current or prior diagnosis, CPM may be indicated for risk reduction in cases where surveillance is difficult or for reconstructive issues such as symmetry and balance, Dr. Carson noted.
Two studies using Surveillance, Epidemiology, and End Results (SEER) data (Tuttle et al. [J. Clin. Oncology 2009;27:1362-7]); Bedrosian et al. [J. Natl. Cancer Inst. 2010;102:401-9]) and one from his own center (Jones et al. [Ann. Surg. Oncol. 2009;16:2691-6]) showed about a 10% increase in the rate of CPM over a decade. Younger women with higher levels of education were more likely to seek CPM.
To see whether this trend extended to NCCN centers, Dr. Carson and his colleagues reviewed data on 1,309 women with DCIS, and 7,044 with stage I-III breast cancer who underwent unilateral mastectomy from 1998 through 2007 at one of 10 designated centers.
In all, 273 of the women diagnosed with DCIS (21%) had a contralateral prophylactic mastectomy, as did 1,199 (17%) of the women with a diagnosis of stage I-III invasive disease. Median follow-up was more than 4 years for both groups.
In a multivariate analysis, factors that significantly predicted the likelihood of CPM included age younger than 50 years, Caucasian race, MRI as the method of detection, and tumor size of 1 cm or smaller. In women with invasive disease, years of education, node-negative status, and no immediate reconstruction were also significant predictors of CPM (P less than .0001 for all variables).
Use of CPM varied widely by institution from 8.2%-34.7% of women with DCIS, and from 3.6%-30.8% of patients with stage I-III disease. As other studies have shown, the use of CPM increased over time, from 15% for DCIS in 1998 to 27% in 2007. For patients with invasive breast cancer, the respective increase was from 8% to 26%. The most pronounced increases were among patients younger than 50 years, Dr. Carson noted.
When they looked at overall survival in a multivariate Cox regression model adjusted for age, race, tumor size, nodal status, tumor grade, histology, and treatment, they found that there was no significant survival advantage for unilateral mastectomy plus CPM, compared with unilateral mastectomy alone.
Complications, complications
Dr. Miller and her colleagues retrospectively reviewed 600 patients who underwent either unilateral mastectomy (391) or CPM (209) at their center from January 2009 through March 2012. They looked at major complications such as seroma or hematoma requiring reoperations, infections requiring hospital admission, total nipple or flap necrosis, and bleeding requiring transfusion; and minor complications such as seromas and hematomas requiring aspiration, infections requiring oral antibiotics, partial nipple or flap necrosis, minor bleeding, and delayed wound healing.
The percentage of patients experiencing any complications was 29% for patients who had a unilateral mastectomy, compared with 42% of those who underwent CPM (P less than .001). Major complications occurred in 4.1% and 14%, respectively (P less than .001). Rates of minor complications were identical between the groups, at 15% each.
Multiple major complications were seen in 4.9% of unilateral patients, compared with 9.1% of CPM patients (P = .043).
Among the CPM patients, 40% of complications occurred on the CPM side.
In a multivariate analysis controlling for age, body mass index, diabetes, previous radiation, smoking history and reconstruction type, CPM was associated with an odds ratio for any complication of 1.5 (P = .029) and 2.6 for major complications (P = .007).
"We believe that patients considering CPM should be made aware of these risks, and certainly more research is needed on patient decision pathways and shared decision making," Dr. Miller said.
Both Dr. Carson’s and Dr. Miller’s studies were internally funded. Dr. Carson disclosed serving on the NCCN Board of Directors. Dr. Miller reported having no financial disclosures.
NATIONAL HARBOR, MD. – The rate of contralateral prophylactic mastectomies is rising, even though there is no evidence for a survival benefit.
From 1998 through 2007, contralateral prophylactic mastectomies (CPM) were performed within 1 year of unilateral mastectomies in 21% of those with ductal carcinoma in situ (DCIS) and in 17% of those with stage I-III breast cancer who were treated at one of 10 National Comprehensive Cancer Network (NCCN) centers.
But in an analysis of overall survival for patients with stages I-III invasive breast cancer, there was so significant difference in overall survival for patients who underwent a CPM, compared with those who underwent only unilateral mastectomy, regardless of whether they had received neoadjuvant chemotherapy, reported Dr. William E. Carson III, professor of surgery at the Ohio State University Comprehensive Cancer Center in Columbus.
In addition, CPMs are associated with a significantly greater risk of complications than unilateral mastectomies, including increased risk for major complications requiring reoperation and rehospitalization, said Dr. Megan Miller, a surgery resident at the University of Chicago, Illinois.
"CPM patients are 1.5 times more likely to have any complication, and 2.6 times more likely to have a major complication than unilateral mastectomy patients," she said at the annual Society of Surgical Oncology Cancer Symposium.
Among patients who underwent CPM, almost 40% of the complications occurred on the side of the body without cancer, she noted.
SSO position statement
A 2007 position statement from the Society of Surgical Oncology (SSO) states that in patients with a current or prior diagnosis, CPM may be indicated for risk reduction in cases where surveillance is difficult or for reconstructive issues such as symmetry and balance, Dr. Carson noted.
Two studies using Surveillance, Epidemiology, and End Results (SEER) data (Tuttle et al. [J. Clin. Oncology 2009;27:1362-7]); Bedrosian et al. [J. Natl. Cancer Inst. 2010;102:401-9]) and one from his own center (Jones et al. [Ann. Surg. Oncol. 2009;16:2691-6]) showed about a 10% increase in the rate of CPM over a decade. Younger women with higher levels of education were more likely to seek CPM.
To see whether this trend extended to NCCN centers, Dr. Carson and his colleagues reviewed data on 1,309 women with DCIS, and 7,044 with stage I-III breast cancer who underwent unilateral mastectomy from 1998 through 2007 at one of 10 designated centers.
In all, 273 of the women diagnosed with DCIS (21%) had a contralateral prophylactic mastectomy, as did 1,199 (17%) of the women with a diagnosis of stage I-III invasive disease. Median follow-up was more than 4 years for both groups.
In a multivariate analysis, factors that significantly predicted the likelihood of CPM included age younger than 50 years, Caucasian race, MRI as the method of detection, and tumor size of 1 cm or smaller. In women with invasive disease, years of education, node-negative status, and no immediate reconstruction were also significant predictors of CPM (P less than .0001 for all variables).
Use of CPM varied widely by institution from 8.2%-34.7% of women with DCIS, and from 3.6%-30.8% of patients with stage I-III disease. As other studies have shown, the use of CPM increased over time, from 15% for DCIS in 1998 to 27% in 2007. For patients with invasive breast cancer, the respective increase was from 8% to 26%. The most pronounced increases were among patients younger than 50 years, Dr. Carson noted.
When they looked at overall survival in a multivariate Cox regression model adjusted for age, race, tumor size, nodal status, tumor grade, histology, and treatment, they found that there was no significant survival advantage for unilateral mastectomy plus CPM, compared with unilateral mastectomy alone.
Complications, complications
Dr. Miller and her colleagues retrospectively reviewed 600 patients who underwent either unilateral mastectomy (391) or CPM (209) at their center from January 2009 through March 2012. They looked at major complications such as seroma or hematoma requiring reoperations, infections requiring hospital admission, total nipple or flap necrosis, and bleeding requiring transfusion; and minor complications such as seromas and hematomas requiring aspiration, infections requiring oral antibiotics, partial nipple or flap necrosis, minor bleeding, and delayed wound healing.
The percentage of patients experiencing any complications was 29% for patients who had a unilateral mastectomy, compared with 42% of those who underwent CPM (P less than .001). Major complications occurred in 4.1% and 14%, respectively (P less than .001). Rates of minor complications were identical between the groups, at 15% each.
Multiple major complications were seen in 4.9% of unilateral patients, compared with 9.1% of CPM patients (P = .043).
Among the CPM patients, 40% of complications occurred on the CPM side.
In a multivariate analysis controlling for age, body mass index, diabetes, previous radiation, smoking history and reconstruction type, CPM was associated with an odds ratio for any complication of 1.5 (P = .029) and 2.6 for major complications (P = .007).
"We believe that patients considering CPM should be made aware of these risks, and certainly more research is needed on patient decision pathways and shared decision making," Dr. Miller said.
Both Dr. Carson’s and Dr. Miller’s studies were internally funded. Dr. Carson disclosed serving on the NCCN Board of Directors. Dr. Miller reported having no financial disclosures.
NATIONAL HARBOR, MD. – The rate of contralateral prophylactic mastectomies is rising, even though there is no evidence for a survival benefit.
From 1998 through 2007, contralateral prophylactic mastectomies (CPM) were performed within 1 year of unilateral mastectomies in 21% of those with ductal carcinoma in situ (DCIS) and in 17% of those with stage I-III breast cancer who were treated at one of 10 National Comprehensive Cancer Network (NCCN) centers.
But in an analysis of overall survival for patients with stages I-III invasive breast cancer, there was so significant difference in overall survival for patients who underwent a CPM, compared with those who underwent only unilateral mastectomy, regardless of whether they had received neoadjuvant chemotherapy, reported Dr. William E. Carson III, professor of surgery at the Ohio State University Comprehensive Cancer Center in Columbus.
In addition, CPMs are associated with a significantly greater risk of complications than unilateral mastectomies, including increased risk for major complications requiring reoperation and rehospitalization, said Dr. Megan Miller, a surgery resident at the University of Chicago, Illinois.
"CPM patients are 1.5 times more likely to have any complication, and 2.6 times more likely to have a major complication than unilateral mastectomy patients," she said at the annual Society of Surgical Oncology Cancer Symposium.
Among patients who underwent CPM, almost 40% of the complications occurred on the side of the body without cancer, she noted.
SSO position statement
A 2007 position statement from the Society of Surgical Oncology (SSO) states that in patients with a current or prior diagnosis, CPM may be indicated for risk reduction in cases where surveillance is difficult or for reconstructive issues such as symmetry and balance, Dr. Carson noted.
Two studies using Surveillance, Epidemiology, and End Results (SEER) data (Tuttle et al. [J. Clin. Oncology 2009;27:1362-7]); Bedrosian et al. [J. Natl. Cancer Inst. 2010;102:401-9]) and one from his own center (Jones et al. [Ann. Surg. Oncol. 2009;16:2691-6]) showed about a 10% increase in the rate of CPM over a decade. Younger women with higher levels of education were more likely to seek CPM.
To see whether this trend extended to NCCN centers, Dr. Carson and his colleagues reviewed data on 1,309 women with DCIS, and 7,044 with stage I-III breast cancer who underwent unilateral mastectomy from 1998 through 2007 at one of 10 designated centers.
In all, 273 of the women diagnosed with DCIS (21%) had a contralateral prophylactic mastectomy, as did 1,199 (17%) of the women with a diagnosis of stage I-III invasive disease. Median follow-up was more than 4 years for both groups.
In a multivariate analysis, factors that significantly predicted the likelihood of CPM included age younger than 50 years, Caucasian race, MRI as the method of detection, and tumor size of 1 cm or smaller. In women with invasive disease, years of education, node-negative status, and no immediate reconstruction were also significant predictors of CPM (P less than .0001 for all variables).
Use of CPM varied widely by institution from 8.2%-34.7% of women with DCIS, and from 3.6%-30.8% of patients with stage I-III disease. As other studies have shown, the use of CPM increased over time, from 15% for DCIS in 1998 to 27% in 2007. For patients with invasive breast cancer, the respective increase was from 8% to 26%. The most pronounced increases were among patients younger than 50 years, Dr. Carson noted.
When they looked at overall survival in a multivariate Cox regression model adjusted for age, race, tumor size, nodal status, tumor grade, histology, and treatment, they found that there was no significant survival advantage for unilateral mastectomy plus CPM, compared with unilateral mastectomy alone.
Complications, complications
Dr. Miller and her colleagues retrospectively reviewed 600 patients who underwent either unilateral mastectomy (391) or CPM (209) at their center from January 2009 through March 2012. They looked at major complications such as seroma or hematoma requiring reoperations, infections requiring hospital admission, total nipple or flap necrosis, and bleeding requiring transfusion; and minor complications such as seromas and hematomas requiring aspiration, infections requiring oral antibiotics, partial nipple or flap necrosis, minor bleeding, and delayed wound healing.
The percentage of patients experiencing any complications was 29% for patients who had a unilateral mastectomy, compared with 42% of those who underwent CPM (P less than .001). Major complications occurred in 4.1% and 14%, respectively (P less than .001). Rates of minor complications were identical between the groups, at 15% each.
Multiple major complications were seen in 4.9% of unilateral patients, compared with 9.1% of CPM patients (P = .043).
Among the CPM patients, 40% of complications occurred on the CPM side.
In a multivariate analysis controlling for age, body mass index, diabetes, previous radiation, smoking history and reconstruction type, CPM was associated with an odds ratio for any complication of 1.5 (P = .029) and 2.6 for major complications (P = .007).
"We believe that patients considering CPM should be made aware of these risks, and certainly more research is needed on patient decision pathways and shared decision making," Dr. Miller said.
Both Dr. Carson’s and Dr. Miller’s studies were internally funded. Dr. Carson disclosed serving on the NCCN Board of Directors. Dr. Miller reported having no financial disclosures.
AT SSO 2013
Major finding: The percentage of patients experiencing any complications was 29% for patients who had a unilateral mastectomy, compared with 42% of those who also underwent a contralateral prophylactic mastectomy (P less than .001).
Data source: Retrospective studies of data on patients with breast cancer treated at 10 NCI-designated comprehensive cancer centers and at a single institution.
Disclosures: Both Dr. Carson’s and Dr. Milller’s studies were internally funded. Dr. Carson disclosed serving on the NCCN Board of Directors. Dr. Miller reported having no financial disclosures.
Guideline nonadherence linked to increased ovarian cancer deaths
LOS ANGELES – Guideline-adherent treatment can make the difference between life and death in patients with ovarian cancer, and it often hinges on where and from whom patients receive care, new data suggest.
In a retrospective, population-based study of more than 13,000 patients with epithelial ovarian cancer, only about 40% of patients received treatment adhering to that recommended by the National Comprehensive Cancer Network (NCCN).
Patients were more likely to receive guideline-adherent treatment if they went to high-volume hospitals (those treating at least 20 such patients each year) and high-volume physicians (those treating at least 10 such patients each year), according to results reported at the annual meeting of the Society of Gynecologic Oncology*. Still, in absolute terms, only about half of patients treated in high-volume hospitals or by high-volume surgeons received adherent treatment.
Compared with their counterparts who received guideline-adherent treatment, patients who received nonadherent treatment had a 33% higher risk of dying from their disease in the subsequent 5 years.
"NCCN guideline adherence predicts improved survival," lead investigator Dr. Robert E. Bristow commented in an interview. "A minority of patients is getting access to guideline care, and increased efforts to direct ovarian cancer patients to high-volume providers are warranted."
From a population-based perspective, much greater gains in survival can be achieved by centralizing ovarian cancer care to gynecologic oncologists and high-volume hospitals than through new chemotherapy drugs or experimental treatments, according to Dr. Bristow, who is director of the division of gynecologic oncology at the University of California, Irvine, medical center. The success of this model "has been demonstrated in Norway, where nonaccredited providers are not paid for any ovarian cancer care they deliver."
That said, the data cannot be used to discern the reasons for the overall poor rate of guideline adherence.
"In population-based data sets, you don’t have the granularity of data to tease out the nuances that might contribute to risk, like an infirm 85-year-old woman who can’t tolerate major surgery and aggressive surgery. We were not able to control for that," Dr. Bristow noted. Yet "only about 20% of patients had access to high-volume providers, and since high-volume providers are more likely to deliver appropriate care, the lack of access to these physicians and hospitals is probably the biggest reason (for nonadherence). By ensuring that we do everything possible to get ovarian cancer patients to the physicians and centers that are best equipped to take care of them, we will maximize each patient’s chance for the best possible outcome."
Analyses were based on 13,321 patients with epithelial ovarian cancer having data in the California Cancer Registry for the years 1999 through 2006. They had a median age of 61 years; 70% had stage III or IV disease, and 42% had serous tumor histology.
Among patients having data on these measures, 81% were treated at low-volume hospitals and 79% by low-volume surgeons. In multivariate analyses, patients were significantly more likely to receive nonadherent treatment if they were treated in low-volume hospitals (odds ratio, 1.83) or by low-volume physicians (OR, 1.19).
Overall, 37% of the patients received treatment recommended by NCCN guidelines. The 5-year disease-specific survival rate was 45% for the cohort overall. In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
"We are in the infancy of defining quality care for ovarian cancer," concluded Dr. Bristow. "We need to develop risk-adjusted models for comparison, to make sure we are comparing apples to apples, so to speak. We need to become more sophisticated in our measurement and reporting. Ideally, one day, everyone’s quality performance measures will be publicly available and patients and payers can choose for themselves where to go for care."
The investigators plan future research on such models and on universal reporting requirements. "There are also critical issues of racial and socioeconomic disparities in ovarian cancer care and outcomes that we are investigating," he said.
Dr. Bristow disclosed no relevant conflicts of interest.
Correction, 3/28/2013: An earlier version of this story misstated the name of the Society of Gynecologic Oncology.

|
|
Dr. Maurie Markman comments:
The report from Bristow, et al., is provocative and raises reasonable
questions regarding the quality of care provided to patients with
ovarian cancer. However, it is critical to acknowledge that while this
report suggests an association between "guideline adherence" and
clinical outcome, it does not in any way demonstrate the inferior
outcome actually resulted from the lack of guideline adherence. For
example, it is highly likely that patients with more advanced disease or
with clinically relevant co-morbidity were less likely to
undergo primary cytoreductive surgery, and these factors are known to be
independently associated with inferior survival. Large databases, as
employed in this analysis, will almost certainly be unable to capture
these clinical factors (for example, performance status, presence of
massive ascites, or large-volume pleural effusion) that will influence
both the decision to perform surgery and the survival outcome.
Therefore, while this study requires follow-up evaluation, it would be
premature to believe outcomes would improve simply because of physician
adherence to a declared "guideline." In fact, inappropriate adherence
that goes against a physician’s clinical judgment may result in a worse
outcome for an individual patient.
Dr. Markman is the senior
vice president of clinical affairs and national director of medical
oncology for the Cancer Treatment Centers of America.

|
|
Dr. Maurie Markman comments:
The report from Bristow, et al., is provocative and raises reasonable
questions regarding the quality of care provided to patients with
ovarian cancer. However, it is critical to acknowledge that while this
report suggests an association between "guideline adherence" and
clinical outcome, it does not in any way demonstrate the inferior
outcome actually resulted from the lack of guideline adherence. For
example, it is highly likely that patients with more advanced disease or
with clinically relevant co-morbidity were less likely to
undergo primary cytoreductive surgery, and these factors are known to be
independently associated with inferior survival. Large databases, as
employed in this analysis, will almost certainly be unable to capture
these clinical factors (for example, performance status, presence of
massive ascites, or large-volume pleural effusion) that will influence
both the decision to perform surgery and the survival outcome.
Therefore, while this study requires follow-up evaluation, it would be
premature to believe outcomes would improve simply because of physician
adherence to a declared "guideline." In fact, inappropriate adherence
that goes against a physician’s clinical judgment may result in a worse
outcome for an individual patient.
Dr. Markman is the senior
vice president of clinical affairs and national director of medical
oncology for the Cancer Treatment Centers of America.

|
|
Dr. Maurie Markman comments:
The report from Bristow, et al., is provocative and raises reasonable
questions regarding the quality of care provided to patients with
ovarian cancer. However, it is critical to acknowledge that while this
report suggests an association between "guideline adherence" and
clinical outcome, it does not in any way demonstrate the inferior
outcome actually resulted from the lack of guideline adherence. For
example, it is highly likely that patients with more advanced disease or
with clinically relevant co-morbidity were less likely to
undergo primary cytoreductive surgery, and these factors are known to be
independently associated with inferior survival. Large databases, as
employed in this analysis, will almost certainly be unable to capture
these clinical factors (for example, performance status, presence of
massive ascites, or large-volume pleural effusion) that will influence
both the decision to perform surgery and the survival outcome.
Therefore, while this study requires follow-up evaluation, it would be
premature to believe outcomes would improve simply because of physician
adherence to a declared "guideline." In fact, inappropriate adherence
that goes against a physician’s clinical judgment may result in a worse
outcome for an individual patient.
Dr. Markman is the senior
vice president of clinical affairs and national director of medical
oncology for the Cancer Treatment Centers of America.
LOS ANGELES – Guideline-adherent treatment can make the difference between life and death in patients with ovarian cancer, and it often hinges on where and from whom patients receive care, new data suggest.
In a retrospective, population-based study of more than 13,000 patients with epithelial ovarian cancer, only about 40% of patients received treatment adhering to that recommended by the National Comprehensive Cancer Network (NCCN).
Patients were more likely to receive guideline-adherent treatment if they went to high-volume hospitals (those treating at least 20 such patients each year) and high-volume physicians (those treating at least 10 such patients each year), according to results reported at the annual meeting of the Society of Gynecologic Oncology*. Still, in absolute terms, only about half of patients treated in high-volume hospitals or by high-volume surgeons received adherent treatment.
Compared with their counterparts who received guideline-adherent treatment, patients who received nonadherent treatment had a 33% higher risk of dying from their disease in the subsequent 5 years.
"NCCN guideline adherence predicts improved survival," lead investigator Dr. Robert E. Bristow commented in an interview. "A minority of patients is getting access to guideline care, and increased efforts to direct ovarian cancer patients to high-volume providers are warranted."
From a population-based perspective, much greater gains in survival can be achieved by centralizing ovarian cancer care to gynecologic oncologists and high-volume hospitals than through new chemotherapy drugs or experimental treatments, according to Dr. Bristow, who is director of the division of gynecologic oncology at the University of California, Irvine, medical center. The success of this model "has been demonstrated in Norway, where nonaccredited providers are not paid for any ovarian cancer care they deliver."
That said, the data cannot be used to discern the reasons for the overall poor rate of guideline adherence.
"In population-based data sets, you don’t have the granularity of data to tease out the nuances that might contribute to risk, like an infirm 85-year-old woman who can’t tolerate major surgery and aggressive surgery. We were not able to control for that," Dr. Bristow noted. Yet "only about 20% of patients had access to high-volume providers, and since high-volume providers are more likely to deliver appropriate care, the lack of access to these physicians and hospitals is probably the biggest reason (for nonadherence). By ensuring that we do everything possible to get ovarian cancer patients to the physicians and centers that are best equipped to take care of them, we will maximize each patient’s chance for the best possible outcome."
Analyses were based on 13,321 patients with epithelial ovarian cancer having data in the California Cancer Registry for the years 1999 through 2006. They had a median age of 61 years; 70% had stage III or IV disease, and 42% had serous tumor histology.
Among patients having data on these measures, 81% were treated at low-volume hospitals and 79% by low-volume surgeons. In multivariate analyses, patients were significantly more likely to receive nonadherent treatment if they were treated in low-volume hospitals (odds ratio, 1.83) or by low-volume physicians (OR, 1.19).
Overall, 37% of the patients received treatment recommended by NCCN guidelines. The 5-year disease-specific survival rate was 45% for the cohort overall. In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
"We are in the infancy of defining quality care for ovarian cancer," concluded Dr. Bristow. "We need to develop risk-adjusted models for comparison, to make sure we are comparing apples to apples, so to speak. We need to become more sophisticated in our measurement and reporting. Ideally, one day, everyone’s quality performance measures will be publicly available and patients and payers can choose for themselves where to go for care."
The investigators plan future research on such models and on universal reporting requirements. "There are also critical issues of racial and socioeconomic disparities in ovarian cancer care and outcomes that we are investigating," he said.
Dr. Bristow disclosed no relevant conflicts of interest.
Correction, 3/28/2013: An earlier version of this story misstated the name of the Society of Gynecologic Oncology.
LOS ANGELES – Guideline-adherent treatment can make the difference between life and death in patients with ovarian cancer, and it often hinges on where and from whom patients receive care, new data suggest.
In a retrospective, population-based study of more than 13,000 patients with epithelial ovarian cancer, only about 40% of patients received treatment adhering to that recommended by the National Comprehensive Cancer Network (NCCN).
Patients were more likely to receive guideline-adherent treatment if they went to high-volume hospitals (those treating at least 20 such patients each year) and high-volume physicians (those treating at least 10 such patients each year), according to results reported at the annual meeting of the Society of Gynecologic Oncology*. Still, in absolute terms, only about half of patients treated in high-volume hospitals or by high-volume surgeons received adherent treatment.
Compared with their counterparts who received guideline-adherent treatment, patients who received nonadherent treatment had a 33% higher risk of dying from their disease in the subsequent 5 years.
"NCCN guideline adherence predicts improved survival," lead investigator Dr. Robert E. Bristow commented in an interview. "A minority of patients is getting access to guideline care, and increased efforts to direct ovarian cancer patients to high-volume providers are warranted."
From a population-based perspective, much greater gains in survival can be achieved by centralizing ovarian cancer care to gynecologic oncologists and high-volume hospitals than through new chemotherapy drugs or experimental treatments, according to Dr. Bristow, who is director of the division of gynecologic oncology at the University of California, Irvine, medical center. The success of this model "has been demonstrated in Norway, where nonaccredited providers are not paid for any ovarian cancer care they deliver."
That said, the data cannot be used to discern the reasons for the overall poor rate of guideline adherence.
"In population-based data sets, you don’t have the granularity of data to tease out the nuances that might contribute to risk, like an infirm 85-year-old woman who can’t tolerate major surgery and aggressive surgery. We were not able to control for that," Dr. Bristow noted. Yet "only about 20% of patients had access to high-volume providers, and since high-volume providers are more likely to deliver appropriate care, the lack of access to these physicians and hospitals is probably the biggest reason (for nonadherence). By ensuring that we do everything possible to get ovarian cancer patients to the physicians and centers that are best equipped to take care of them, we will maximize each patient’s chance for the best possible outcome."
Analyses were based on 13,321 patients with epithelial ovarian cancer having data in the California Cancer Registry for the years 1999 through 2006. They had a median age of 61 years; 70% had stage III or IV disease, and 42% had serous tumor histology.
Among patients having data on these measures, 81% were treated at low-volume hospitals and 79% by low-volume surgeons. In multivariate analyses, patients were significantly more likely to receive nonadherent treatment if they were treated in low-volume hospitals (odds ratio, 1.83) or by low-volume physicians (OR, 1.19).
Overall, 37% of the patients received treatment recommended by NCCN guidelines. The 5-year disease-specific survival rate was 45% for the cohort overall. In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
"We are in the infancy of defining quality care for ovarian cancer," concluded Dr. Bristow. "We need to develop risk-adjusted models for comparison, to make sure we are comparing apples to apples, so to speak. We need to become more sophisticated in our measurement and reporting. Ideally, one day, everyone’s quality performance measures will be publicly available and patients and payers can choose for themselves where to go for care."
The investigators plan future research on such models and on universal reporting requirements. "There are also critical issues of racial and socioeconomic disparities in ovarian cancer care and outcomes that we are investigating," he said.
Dr. Bristow disclosed no relevant conflicts of interest.
Correction, 3/28/2013: An earlier version of this story misstated the name of the Society of Gynecologic Oncology.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
Data source: A retrospective population-based cohort study of 13,321 patients with epithelial ovarian cancer from the California Cancer Registry
Disclosures: Dr. Bristow disclosed no relevant conflicts of interest.
Breast cancer: Cardiac risk increases with radiation dose to heart
The risk of major ischemic coronary events was significantly and proportionately associated with the estimated mean radiation dose to the heart in a study of women in Sweden and Denmark who received radiotherapy for breast cancer over a 43-year period.
"The risk of a major coronary event increased linearly with the mean dose to the heart," reported Sarah Darby, Ph.D., of the University of Oxford (England), and her associates. The risk began to increase within the first 5 years of treatment and continued to increase for at least 20 years.
The findings make it possible for a woman to estimate her absolute risk of radiation-related ischemic heart disease, the authors wrote. "This absolute risk can be weighed against the probable absolute reduction in her risk of recurrence or death from breast cancer that would be achieved without radiotherapy" (N. Engl. J. Med. 2013;368:987-98 [doi: 10.1056/NEJMoa1209825]).
The population-based study included 2,168 women who had been treated with external-beam radiation for invasive breast cancer between 1958 and 2001, and were enrolled in the Swedish National Cancer Register or the Danish Breast Cancer Cooperative Group. The 963 women who were subsequently diagnosed with a major coronary event (myocardial infarction, coronary revascularization, or death from ischemic heart disease, but not angina) were compared with 1,205 controls.
The major coronary events were diagnosed in the first decade after breast cancer diagnosis in 44% of patients; 33% of events were diagnosed 10-19 years after breast cancer diagnosis; and 23% occurred 20 or more years later. Of the cases, 54% died of ischemic heart disease.
The estimated mean radiation dose to the heart overall was 4.9 Gy (range, 0.03-27.72 Gy). For those with cancer in their left breast, the mean dose exposure to the heart was 6.6 Gy; for those with right-breast tumors, it was 2.9 Gy. Major coronary events were significantly higher among the women with radiation to the left breast.
The estimated dose to the heart of women who are currently treated with radiotherapy ranges from 1 to 5 Gy, the authors said.
For each 1-Gy increase in the mean dose of radiation to the heart, the rate of major coronary events increased by 7.4%, which was a highly statistically significant finding. Compared with controls who had no cardiac dose, the rate of major coronary events increased by 10% among those exposed to a mean radiation dose of less than 2 Gy, by 30% among those exposed to 2-4 Gy, by 40% among those exposed to 5-9 Gy, and by 116% in those exposed to 10 Gy or more.
Among women with a history of ischemic heart disease, the risk of major coronary events was almost sevenfold higher than it was in women with no history of ischemic heart disease. This risk was increased by about 13-fold during the first 10 years after treatment and was about twofold higher in later years.
"Absolute increases in risk for a given dose to the heart were larger for women with preexisting risk factors," they wrote, so "clinicians may wish to consider cardiac dose and cardiac risk factors as well as tumor control when making decisions about the use of radiotherapy for breast cancer."
Among the strengths of the study was that the analysis included all women who were documented as having received radiotherapy for breast cancer in the two countries during the time period studied. The authors cautioned against applying the results to breast cancer patients who are treated before age 30 because few women in this age group were included in the study.
The study was supported by the Oxford University Clinical Trial Service Unit from Cancer Research UK, the British Heart Foundation, and the UK Medical Research Council.
While the results of the study are interesting, they likely overestimate the risk of coronary events associated with contemporary radiation therapy. Of greater concern, the findings could be misinterpreted and could deter women from having potentially lifesaving treatment.
Increases in the rate of major coronary events – about 20% higher per 1 Gy – were far greater among the women diagnosed in the 1980s, who drive much of the increase in risk. There was barely an increase in the rate of events – 0.85% per 1 Gy – among those diagnosed in the 1990s, for example.
Most of the data are taken from a time when radiation was administered by techniques that differ from those used today, which are associated with a lot less scatter to the heart. Three-dimensional, CT-based planning was not used for the women in the study, which the authors acknowledged was a limitation. Also, the dose was estimated using radiotherapy charts, which are notoriously inaccurate.
Further, there is now a better understanding of which patients are likely to have a survival benefit from radiation. Correctly targeted radiation therapy plays an incredibly important role in the excellent results we see today, with the majority of breast cancer patients surviving their disease.
Dr. Hope Rugo is professor of medicine at the University of California, San Francisco, and director of breast oncology and clinical trials education at the UCSF Helen Diller Family Comprehensive Cancer Center. She had no relevant financial disclosures.
While the results of the study are interesting, they likely overestimate the risk of coronary events associated with contemporary radiation therapy. Of greater concern, the findings could be misinterpreted and could deter women from having potentially lifesaving treatment.
Increases in the rate of major coronary events – about 20% higher per 1 Gy – were far greater among the women diagnosed in the 1980s, who drive much of the increase in risk. There was barely an increase in the rate of events – 0.85% per 1 Gy – among those diagnosed in the 1990s, for example.
Most of the data are taken from a time when radiation was administered by techniques that differ from those used today, which are associated with a lot less scatter to the heart. Three-dimensional, CT-based planning was not used for the women in the study, which the authors acknowledged was a limitation. Also, the dose was estimated using radiotherapy charts, which are notoriously inaccurate.
Further, there is now a better understanding of which patients are likely to have a survival benefit from radiation. Correctly targeted radiation therapy plays an incredibly important role in the excellent results we see today, with the majority of breast cancer patients surviving their disease.
Dr. Hope Rugo is professor of medicine at the University of California, San Francisco, and director of breast oncology and clinical trials education at the UCSF Helen Diller Family Comprehensive Cancer Center. She had no relevant financial disclosures.
While the results of the study are interesting, they likely overestimate the risk of coronary events associated with contemporary radiation therapy. Of greater concern, the findings could be misinterpreted and could deter women from having potentially lifesaving treatment.
Increases in the rate of major coronary events – about 20% higher per 1 Gy – were far greater among the women diagnosed in the 1980s, who drive much of the increase in risk. There was barely an increase in the rate of events – 0.85% per 1 Gy – among those diagnosed in the 1990s, for example.
Most of the data are taken from a time when radiation was administered by techniques that differ from those used today, which are associated with a lot less scatter to the heart. Three-dimensional, CT-based planning was not used for the women in the study, which the authors acknowledged was a limitation. Also, the dose was estimated using radiotherapy charts, which are notoriously inaccurate.
Further, there is now a better understanding of which patients are likely to have a survival benefit from radiation. Correctly targeted radiation therapy plays an incredibly important role in the excellent results we see today, with the majority of breast cancer patients surviving their disease.
Dr. Hope Rugo is professor of medicine at the University of California, San Francisco, and director of breast oncology and clinical trials education at the UCSF Helen Diller Family Comprehensive Cancer Center. She had no relevant financial disclosures.
The risk of major ischemic coronary events was significantly and proportionately associated with the estimated mean radiation dose to the heart in a study of women in Sweden and Denmark who received radiotherapy for breast cancer over a 43-year period.
"The risk of a major coronary event increased linearly with the mean dose to the heart," reported Sarah Darby, Ph.D., of the University of Oxford (England), and her associates. The risk began to increase within the first 5 years of treatment and continued to increase for at least 20 years.
The findings make it possible for a woman to estimate her absolute risk of radiation-related ischemic heart disease, the authors wrote. "This absolute risk can be weighed against the probable absolute reduction in her risk of recurrence or death from breast cancer that would be achieved without radiotherapy" (N. Engl. J. Med. 2013;368:987-98 [doi: 10.1056/NEJMoa1209825]).
The population-based study included 2,168 women who had been treated with external-beam radiation for invasive breast cancer between 1958 and 2001, and were enrolled in the Swedish National Cancer Register or the Danish Breast Cancer Cooperative Group. The 963 women who were subsequently diagnosed with a major coronary event (myocardial infarction, coronary revascularization, or death from ischemic heart disease, but not angina) were compared with 1,205 controls.
The major coronary events were diagnosed in the first decade after breast cancer diagnosis in 44% of patients; 33% of events were diagnosed 10-19 years after breast cancer diagnosis; and 23% occurred 20 or more years later. Of the cases, 54% died of ischemic heart disease.
The estimated mean radiation dose to the heart overall was 4.9 Gy (range, 0.03-27.72 Gy). For those with cancer in their left breast, the mean dose exposure to the heart was 6.6 Gy; for those with right-breast tumors, it was 2.9 Gy. Major coronary events were significantly higher among the women with radiation to the left breast.
The estimated dose to the heart of women who are currently treated with radiotherapy ranges from 1 to 5 Gy, the authors said.
For each 1-Gy increase in the mean dose of radiation to the heart, the rate of major coronary events increased by 7.4%, which was a highly statistically significant finding. Compared with controls who had no cardiac dose, the rate of major coronary events increased by 10% among those exposed to a mean radiation dose of less than 2 Gy, by 30% among those exposed to 2-4 Gy, by 40% among those exposed to 5-9 Gy, and by 116% in those exposed to 10 Gy or more.
Among women with a history of ischemic heart disease, the risk of major coronary events was almost sevenfold higher than it was in women with no history of ischemic heart disease. This risk was increased by about 13-fold during the first 10 years after treatment and was about twofold higher in later years.
"Absolute increases in risk for a given dose to the heart were larger for women with preexisting risk factors," they wrote, so "clinicians may wish to consider cardiac dose and cardiac risk factors as well as tumor control when making decisions about the use of radiotherapy for breast cancer."
Among the strengths of the study was that the analysis included all women who were documented as having received radiotherapy for breast cancer in the two countries during the time period studied. The authors cautioned against applying the results to breast cancer patients who are treated before age 30 because few women in this age group were included in the study.
The study was supported by the Oxford University Clinical Trial Service Unit from Cancer Research UK, the British Heart Foundation, and the UK Medical Research Council.
The risk of major ischemic coronary events was significantly and proportionately associated with the estimated mean radiation dose to the heart in a study of women in Sweden and Denmark who received radiotherapy for breast cancer over a 43-year period.
"The risk of a major coronary event increased linearly with the mean dose to the heart," reported Sarah Darby, Ph.D., of the University of Oxford (England), and her associates. The risk began to increase within the first 5 years of treatment and continued to increase for at least 20 years.
The findings make it possible for a woman to estimate her absolute risk of radiation-related ischemic heart disease, the authors wrote. "This absolute risk can be weighed against the probable absolute reduction in her risk of recurrence or death from breast cancer that would be achieved without radiotherapy" (N. Engl. J. Med. 2013;368:987-98 [doi: 10.1056/NEJMoa1209825]).
The population-based study included 2,168 women who had been treated with external-beam radiation for invasive breast cancer between 1958 and 2001, and were enrolled in the Swedish National Cancer Register or the Danish Breast Cancer Cooperative Group. The 963 women who were subsequently diagnosed with a major coronary event (myocardial infarction, coronary revascularization, or death from ischemic heart disease, but not angina) were compared with 1,205 controls.
The major coronary events were diagnosed in the first decade after breast cancer diagnosis in 44% of patients; 33% of events were diagnosed 10-19 years after breast cancer diagnosis; and 23% occurred 20 or more years later. Of the cases, 54% died of ischemic heart disease.
The estimated mean radiation dose to the heart overall was 4.9 Gy (range, 0.03-27.72 Gy). For those with cancer in their left breast, the mean dose exposure to the heart was 6.6 Gy; for those with right-breast tumors, it was 2.9 Gy. Major coronary events were significantly higher among the women with radiation to the left breast.
The estimated dose to the heart of women who are currently treated with radiotherapy ranges from 1 to 5 Gy, the authors said.
For each 1-Gy increase in the mean dose of radiation to the heart, the rate of major coronary events increased by 7.4%, which was a highly statistically significant finding. Compared with controls who had no cardiac dose, the rate of major coronary events increased by 10% among those exposed to a mean radiation dose of less than 2 Gy, by 30% among those exposed to 2-4 Gy, by 40% among those exposed to 5-9 Gy, and by 116% in those exposed to 10 Gy or more.
Among women with a history of ischemic heart disease, the risk of major coronary events was almost sevenfold higher than it was in women with no history of ischemic heart disease. This risk was increased by about 13-fold during the first 10 years after treatment and was about twofold higher in later years.
"Absolute increases in risk for a given dose to the heart were larger for women with preexisting risk factors," they wrote, so "clinicians may wish to consider cardiac dose and cardiac risk factors as well as tumor control when making decisions about the use of radiotherapy for breast cancer."
Among the strengths of the study was that the analysis included all women who were documented as having received radiotherapy for breast cancer in the two countries during the time period studied. The authors cautioned against applying the results to breast cancer patients who are treated before age 30 because few women in this age group were included in the study.
The study was supported by the Oxford University Clinical Trial Service Unit from Cancer Research UK, the British Heart Foundation, and the UK Medical Research Council.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: The risk of major coronary events increased by 7.4% per 1 Gy of radiation received as treatment for breast cancer.
Data source: A population-based, case-control study in 2,168 women treated with external-beam radiation therapy for invasive breast cancer in Sweden and Denmark between 1958 and 2001.
Disclosures: The study was supported by the Oxford University Clinical Trial Service Unit from Cancer Research UK, the British Heart Foundation, and the UK Medical Research Council.
Lipid metabolism genes linked to breast cancer subtype
Fine-needle aspirant samples taken from the healthy contralateral breast of patients undergoing surgery for breast cancer contained newly identified genetic markers that were expressed differently in estrogen receptor–negative and estrogen receptor–positive tumors.
The findings suggest that a metabolic derangement in lipid processing may precede the development of a breast tumor.
All of these genes are involved in lipid metabolism, an unexpected finding that speaks to the long-observed relationship between weight and breast cancer risk, Dr. Seema Khan and her colleagues wrote in the March issue of Cancer Prevention Research (2013 [doi:10.1158/1940-6207.CAPR-12-0304]).
"This was interesting because obesity is a breast cancer risk factor for postmenopausal women, but obese women are generally thought to be at increased risk for hormone-sensitive cancer," Khan said in a press statement. "We were surprised to see that some of these genes that are associated with lipid metabolism, or the metabolism of fats, are actually more highly expressed in the unaffected breasts of women with estrogen receptor–negative breast cancer."
The investigators, all from Northwestern University in Chicago, conducted their initial analysis on a set of 30 breast cancer patients – 15 with ER-negative tumors and 15 with ER-positive tumors. They then validated their results on 36-subjects, 12 with ER-negative cancers, 12 with ER-positive cancers, and 12 controls. All of the women in the study were matched for age, menopausal status, weight, and, in the patients, HER2 status. All subjects were followed for a minimum of 3 years.
Based on RNA extracted from fine-needle aspirations of the subjects’ contralateral breasts, eight unique genes were identified. There was significant differential expression of the genes between the groups. All of the genes were directly involved in lipid metabolism, and seven of them were significantly more common in ER-negative tumors.
Similar results were observed in the validation group, with all eight genes observed to be significantly more common in the ER-negative group than in the ER-positive group.
When the ER-negative cases were compared with the controls, four genes were significantly overexpressed and were observed to be up to six times more common in cases. The genetic markers were similarly expressed in ER-positive cases and in controls, however.
Two of the remaining four genes were significantly underexpressed in ER-positive cases, compared with controls (three and six times less likely to occur, respectively), indicating that both genes may protect against the development of ER-negative tumors. Of the remaining two genes, one was significantly under-expressed in both ER-negative and ER-positive groups, compared with controls (15 and 11 times less common, respectively). This, the authors said, indicates that the gene may protect against both types of cancer.
There were no significant associations between the final gene and either cancer subtype.
A clustering analysis of the eight genes separated the cases into low- mid- and high-expression groups, and also successfully separated the controls from the cases. In this analysis, 70% of the cases in the low-expression group were ER-positive; 67% of the cases in the mid-expression group were ER-positive; and 88% of the cases in the high-expression group were ER-negative.
The analysis also identified a high- and a low-expression group among the 12 controls. Four of these control cases had high-expression profiles, similar to those of the high-expression cases. The cytology of these four samples was atypical in two, borderline in one, and benign in one. The other eight samples had low gene expression and all had benign cytology.
"The potential involvement of lipid metabolism–related genes to ER-negative breast cancer is unexpected, though evidence pointing to a link of lipid/steroid metabolism with ER-negative breast cancer risk and outcomes exists," the authors said. "ER-negative/PR (progesterone receptor)-negative tumors are more common in obese premenopausal women, and large hip circumference has a particularly strong association with premenopausal ER-negative/PR-negative breast cancer. The functions of these genes in relation to lipid modification and elimination, and to transportation and detoxification of distinct lipid compounds, suggest that their expression results in a specific microenvironment of steroid hormone metabolites, which may determine whether initiated cells progress to ER-positive or ER-negative tumors."
None of the authors declared any financial relationships. The study was funded by the Lynn Sage Cancer Research Foundation, the Avon Foundation, and a private contribution.
Fine-needle aspirant samples taken from the healthy contralateral breast of patients undergoing surgery for breast cancer contained newly identified genetic markers that were expressed differently in estrogen receptor–negative and estrogen receptor–positive tumors.
The findings suggest that a metabolic derangement in lipid processing may precede the development of a breast tumor.
All of these genes are involved in lipid metabolism, an unexpected finding that speaks to the long-observed relationship between weight and breast cancer risk, Dr. Seema Khan and her colleagues wrote in the March issue of Cancer Prevention Research (2013 [doi:10.1158/1940-6207.CAPR-12-0304]).
"This was interesting because obesity is a breast cancer risk factor for postmenopausal women, but obese women are generally thought to be at increased risk for hormone-sensitive cancer," Khan said in a press statement. "We were surprised to see that some of these genes that are associated with lipid metabolism, or the metabolism of fats, are actually more highly expressed in the unaffected breasts of women with estrogen receptor–negative breast cancer."
The investigators, all from Northwestern University in Chicago, conducted their initial analysis on a set of 30 breast cancer patients – 15 with ER-negative tumors and 15 with ER-positive tumors. They then validated their results on 36-subjects, 12 with ER-negative cancers, 12 with ER-positive cancers, and 12 controls. All of the women in the study were matched for age, menopausal status, weight, and, in the patients, HER2 status. All subjects were followed for a minimum of 3 years.
Based on RNA extracted from fine-needle aspirations of the subjects’ contralateral breasts, eight unique genes were identified. There was significant differential expression of the genes between the groups. All of the genes were directly involved in lipid metabolism, and seven of them were significantly more common in ER-negative tumors.
Similar results were observed in the validation group, with all eight genes observed to be significantly more common in the ER-negative group than in the ER-positive group.
When the ER-negative cases were compared with the controls, four genes were significantly overexpressed and were observed to be up to six times more common in cases. The genetic markers were similarly expressed in ER-positive cases and in controls, however.
Two of the remaining four genes were significantly underexpressed in ER-positive cases, compared with controls (three and six times less likely to occur, respectively), indicating that both genes may protect against the development of ER-negative tumors. Of the remaining two genes, one was significantly under-expressed in both ER-negative and ER-positive groups, compared with controls (15 and 11 times less common, respectively). This, the authors said, indicates that the gene may protect against both types of cancer.
There were no significant associations between the final gene and either cancer subtype.
A clustering analysis of the eight genes separated the cases into low- mid- and high-expression groups, and also successfully separated the controls from the cases. In this analysis, 70% of the cases in the low-expression group were ER-positive; 67% of the cases in the mid-expression group were ER-positive; and 88% of the cases in the high-expression group were ER-negative.
The analysis also identified a high- and a low-expression group among the 12 controls. Four of these control cases had high-expression profiles, similar to those of the high-expression cases. The cytology of these four samples was atypical in two, borderline in one, and benign in one. The other eight samples had low gene expression and all had benign cytology.
"The potential involvement of lipid metabolism–related genes to ER-negative breast cancer is unexpected, though evidence pointing to a link of lipid/steroid metabolism with ER-negative breast cancer risk and outcomes exists," the authors said. "ER-negative/PR (progesterone receptor)-negative tumors are more common in obese premenopausal women, and large hip circumference has a particularly strong association with premenopausal ER-negative/PR-negative breast cancer. The functions of these genes in relation to lipid modification and elimination, and to transportation and detoxification of distinct lipid compounds, suggest that their expression results in a specific microenvironment of steroid hormone metabolites, which may determine whether initiated cells progress to ER-positive or ER-negative tumors."
None of the authors declared any financial relationships. The study was funded by the Lynn Sage Cancer Research Foundation, the Avon Foundation, and a private contribution.
Fine-needle aspirant samples taken from the healthy contralateral breast of patients undergoing surgery for breast cancer contained newly identified genetic markers that were expressed differently in estrogen receptor–negative and estrogen receptor–positive tumors.
The findings suggest that a metabolic derangement in lipid processing may precede the development of a breast tumor.
All of these genes are involved in lipid metabolism, an unexpected finding that speaks to the long-observed relationship between weight and breast cancer risk, Dr. Seema Khan and her colleagues wrote in the March issue of Cancer Prevention Research (2013 [doi:10.1158/1940-6207.CAPR-12-0304]).
"This was interesting because obesity is a breast cancer risk factor for postmenopausal women, but obese women are generally thought to be at increased risk for hormone-sensitive cancer," Khan said in a press statement. "We were surprised to see that some of these genes that are associated with lipid metabolism, or the metabolism of fats, are actually more highly expressed in the unaffected breasts of women with estrogen receptor–negative breast cancer."
The investigators, all from Northwestern University in Chicago, conducted their initial analysis on a set of 30 breast cancer patients – 15 with ER-negative tumors and 15 with ER-positive tumors. They then validated their results on 36-subjects, 12 with ER-negative cancers, 12 with ER-positive cancers, and 12 controls. All of the women in the study were matched for age, menopausal status, weight, and, in the patients, HER2 status. All subjects were followed for a minimum of 3 years.
Based on RNA extracted from fine-needle aspirations of the subjects’ contralateral breasts, eight unique genes were identified. There was significant differential expression of the genes between the groups. All of the genes were directly involved in lipid metabolism, and seven of them were significantly more common in ER-negative tumors.
Similar results were observed in the validation group, with all eight genes observed to be significantly more common in the ER-negative group than in the ER-positive group.
When the ER-negative cases were compared with the controls, four genes were significantly overexpressed and were observed to be up to six times more common in cases. The genetic markers were similarly expressed in ER-positive cases and in controls, however.
Two of the remaining four genes were significantly underexpressed in ER-positive cases, compared with controls (three and six times less likely to occur, respectively), indicating that both genes may protect against the development of ER-negative tumors. Of the remaining two genes, one was significantly under-expressed in both ER-negative and ER-positive groups, compared with controls (15 and 11 times less common, respectively). This, the authors said, indicates that the gene may protect against both types of cancer.
There were no significant associations between the final gene and either cancer subtype.
A clustering analysis of the eight genes separated the cases into low- mid- and high-expression groups, and also successfully separated the controls from the cases. In this analysis, 70% of the cases in the low-expression group were ER-positive; 67% of the cases in the mid-expression group were ER-positive; and 88% of the cases in the high-expression group were ER-negative.
The analysis also identified a high- and a low-expression group among the 12 controls. Four of these control cases had high-expression profiles, similar to those of the high-expression cases. The cytology of these four samples was atypical in two, borderline in one, and benign in one. The other eight samples had low gene expression and all had benign cytology.
"The potential involvement of lipid metabolism–related genes to ER-negative breast cancer is unexpected, though evidence pointing to a link of lipid/steroid metabolism with ER-negative breast cancer risk and outcomes exists," the authors said. "ER-negative/PR (progesterone receptor)-negative tumors are more common in obese premenopausal women, and large hip circumference has a particularly strong association with premenopausal ER-negative/PR-negative breast cancer. The functions of these genes in relation to lipid modification and elimination, and to transportation and detoxification of distinct lipid compounds, suggest that their expression results in a specific microenvironment of steroid hormone metabolites, which may determine whether initiated cells progress to ER-positive or ER-negative tumors."
None of the authors declared any financial relationships. The study was funded by the Lynn Sage Cancer Research Foundation, the Avon Foundation, and a private contribution.
FROM CANCER PREVENTION RESEARCH
Major finding: A clustering analysis of eight genes separated cases into expression groups; 70% of the low-expression cases had ER-positive tumors, 67% of the mid-expression cases had ER-positive tumors; and 88% of the high-expression group had ER-negative tumors.
Data source: The findings are from investigation and validation groups that comprised a total of 24 cases and 12 controls.
Disclosures: None of the authors declared any financial relationships. The study was funded by the Lynn Sage Cancer Research Foundation, the Avon Foundation, and a private contribution.
MVAC plus cystectomy boosts bladder cancer survival
ORLANDO – Cisplatin-based neoadjuvant chemotherapy plus cystectomy improved the overall survival of patients with muscle-invasive bladder cancer beyond that achieved with cystectomy alone; however, the results did not reach statistical significance in the Japan Clinical Oncology Group Study, JCOG0209.
In a randomized trial of 130 patients accrued over a 6-year period, overall survival at 5 years was 72.3% for patients who had two cycles of chemotherapy followed by radical cystectomy and 62.4% for patients who had radical cystectomy alone. The overall survival results were not significant because of insufficient sample size, according to Dr. Hiroshi Kitamura of Sapporo (Japan) Medical University.
Median progression-free survival time, however, was significantly longer at 99 months in the group who received neoadjuvant chemotherapy plus cystectomy compared with 78 months in those who had radical cystectomy alone (HR = 0.61, P = .04). Progression-free survival at 5 years was 69.1% and 56.4%, respectively.
The Japan Clinical Oncology Group Study, JCOG0209, examined the MVAC regimen of methotrexate, vinblastine, doxorubicin (Adriamycin), and cisplatin followed by radical cystectomy. MVAC comprised methotrexate (30 mg/m2) on days 1, 15, and 22; vinblastine (3 mg/m2) on days 2, 15, and 22; Adriamycin (30 mg/m2) on day 2; and cisplatin (70 mg/m2) on day 2.
Because neoadjuvant therapy with gemcitabine and cisplatin is now widely used to treat invasive bladder cancer, and considered to provide a 5%-8% overall survival advantage, the Data and Safety Monitoring Committee recommended early publication of the results, Dr. Kitamura said at the annual Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology. The findings indicate that the MVAC regimen can still be considered promising.
"Although (the chemotherapy regimen) was two cycles, and the study was underpowered," chemotherapy plus radical cystectomy were confirmed as the standard of care for muscle-invasive bladder cancer, commented Dr. Dean Bajorin of Memorial Sloan-Kettering Cancer Center, New York, who was not involved in the study. "I do not think we need to include nontreatment arms in these trials anymore."
Between March 2003 and March 2009, researchers randomized 130 patients to receive two cycles of MVAC neoadjuvant chemotherapy followed by radical cystectomy (64 patients) or to radical cystectomy alone (66 patients). Patient registration was terminated early because of slow accrual.
The primary endpoint was overall survival. Secondary endpoints were progression-free survival, surgery-related complication rate, adverse events during neoadjuvant chemotherapy, the rate of no residual tumor in radical cystectomy specimens (pT0), and quality of life.
Results at the second interim analysis showed that overall survival was better with MVAC plus surgery (median, 102 months) than with radical cystectomy alone (median, 81 months), but the difference did not achieve statistical significance because the sample size was small (HR = 0.65, P = .07).
At the time of radical cystectomy, clinical stage was pT0 in 37% of the MVAC arm and 9% in the radical cystectomy arm (P less than .01).
Dr. Kitamura said he had no relationships to disclose. Dr. Bajorin disclosed that he has been a consultant or adviser for Bristol-Myers Squibb, Dendreon, Lilly, and Novartis. He has received honoraria from Lilly, and research funding from Amgen, Dendreon, Genentech, Genta, GlaxoSmithKline, and Novartis.
On Twitter @naseemsmiller
ORLANDO – Cisplatin-based neoadjuvant chemotherapy plus cystectomy improved the overall survival of patients with muscle-invasive bladder cancer beyond that achieved with cystectomy alone; however, the results did not reach statistical significance in the Japan Clinical Oncology Group Study, JCOG0209.
In a randomized trial of 130 patients accrued over a 6-year period, overall survival at 5 years was 72.3% for patients who had two cycles of chemotherapy followed by radical cystectomy and 62.4% for patients who had radical cystectomy alone. The overall survival results were not significant because of insufficient sample size, according to Dr. Hiroshi Kitamura of Sapporo (Japan) Medical University.
Median progression-free survival time, however, was significantly longer at 99 months in the group who received neoadjuvant chemotherapy plus cystectomy compared with 78 months in those who had radical cystectomy alone (HR = 0.61, P = .04). Progression-free survival at 5 years was 69.1% and 56.4%, respectively.
The Japan Clinical Oncology Group Study, JCOG0209, examined the MVAC regimen of methotrexate, vinblastine, doxorubicin (Adriamycin), and cisplatin followed by radical cystectomy. MVAC comprised methotrexate (30 mg/m2) on days 1, 15, and 22; vinblastine (3 mg/m2) on days 2, 15, and 22; Adriamycin (30 mg/m2) on day 2; and cisplatin (70 mg/m2) on day 2.
Because neoadjuvant therapy with gemcitabine and cisplatin is now widely used to treat invasive bladder cancer, and considered to provide a 5%-8% overall survival advantage, the Data and Safety Monitoring Committee recommended early publication of the results, Dr. Kitamura said at the annual Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology. The findings indicate that the MVAC regimen can still be considered promising.
"Although (the chemotherapy regimen) was two cycles, and the study was underpowered," chemotherapy plus radical cystectomy were confirmed as the standard of care for muscle-invasive bladder cancer, commented Dr. Dean Bajorin of Memorial Sloan-Kettering Cancer Center, New York, who was not involved in the study. "I do not think we need to include nontreatment arms in these trials anymore."
Between March 2003 and March 2009, researchers randomized 130 patients to receive two cycles of MVAC neoadjuvant chemotherapy followed by radical cystectomy (64 patients) or to radical cystectomy alone (66 patients). Patient registration was terminated early because of slow accrual.
The primary endpoint was overall survival. Secondary endpoints were progression-free survival, surgery-related complication rate, adverse events during neoadjuvant chemotherapy, the rate of no residual tumor in radical cystectomy specimens (pT0), and quality of life.
Results at the second interim analysis showed that overall survival was better with MVAC plus surgery (median, 102 months) than with radical cystectomy alone (median, 81 months), but the difference did not achieve statistical significance because the sample size was small (HR = 0.65, P = .07).
At the time of radical cystectomy, clinical stage was pT0 in 37% of the MVAC arm and 9% in the radical cystectomy arm (P less than .01).
Dr. Kitamura said he had no relationships to disclose. Dr. Bajorin disclosed that he has been a consultant or adviser for Bristol-Myers Squibb, Dendreon, Lilly, and Novartis. He has received honoraria from Lilly, and research funding from Amgen, Dendreon, Genentech, Genta, GlaxoSmithKline, and Novartis.
On Twitter @naseemsmiller
ORLANDO – Cisplatin-based neoadjuvant chemotherapy plus cystectomy improved the overall survival of patients with muscle-invasive bladder cancer beyond that achieved with cystectomy alone; however, the results did not reach statistical significance in the Japan Clinical Oncology Group Study, JCOG0209.
In a randomized trial of 130 patients accrued over a 6-year period, overall survival at 5 years was 72.3% for patients who had two cycles of chemotherapy followed by radical cystectomy and 62.4% for patients who had radical cystectomy alone. The overall survival results were not significant because of insufficient sample size, according to Dr. Hiroshi Kitamura of Sapporo (Japan) Medical University.
Median progression-free survival time, however, was significantly longer at 99 months in the group who received neoadjuvant chemotherapy plus cystectomy compared with 78 months in those who had radical cystectomy alone (HR = 0.61, P = .04). Progression-free survival at 5 years was 69.1% and 56.4%, respectively.
The Japan Clinical Oncology Group Study, JCOG0209, examined the MVAC regimen of methotrexate, vinblastine, doxorubicin (Adriamycin), and cisplatin followed by radical cystectomy. MVAC comprised methotrexate (30 mg/m2) on days 1, 15, and 22; vinblastine (3 mg/m2) on days 2, 15, and 22; Adriamycin (30 mg/m2) on day 2; and cisplatin (70 mg/m2) on day 2.
Because neoadjuvant therapy with gemcitabine and cisplatin is now widely used to treat invasive bladder cancer, and considered to provide a 5%-8% overall survival advantage, the Data and Safety Monitoring Committee recommended early publication of the results, Dr. Kitamura said at the annual Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology. The findings indicate that the MVAC regimen can still be considered promising.
"Although (the chemotherapy regimen) was two cycles, and the study was underpowered," chemotherapy plus radical cystectomy were confirmed as the standard of care for muscle-invasive bladder cancer, commented Dr. Dean Bajorin of Memorial Sloan-Kettering Cancer Center, New York, who was not involved in the study. "I do not think we need to include nontreatment arms in these trials anymore."
Between March 2003 and March 2009, researchers randomized 130 patients to receive two cycles of MVAC neoadjuvant chemotherapy followed by radical cystectomy (64 patients) or to radical cystectomy alone (66 patients). Patient registration was terminated early because of slow accrual.
The primary endpoint was overall survival. Secondary endpoints were progression-free survival, surgery-related complication rate, adverse events during neoadjuvant chemotherapy, the rate of no residual tumor in radical cystectomy specimens (pT0), and quality of life.
Results at the second interim analysis showed that overall survival was better with MVAC plus surgery (median, 102 months) than with radical cystectomy alone (median, 81 months), but the difference did not achieve statistical significance because the sample size was small (HR = 0.65, P = .07).
At the time of radical cystectomy, clinical stage was pT0 in 37% of the MVAC arm and 9% in the radical cystectomy arm (P less than .01).
Dr. Kitamura said he had no relationships to disclose. Dr. Bajorin disclosed that he has been a consultant or adviser for Bristol-Myers Squibb, Dendreon, Lilly, and Novartis. He has received honoraria from Lilly, and research funding from Amgen, Dendreon, Genentech, Genta, GlaxoSmithKline, and Novartis.
On Twitter @naseemsmiller
AT ASCO GENITOURINARY CANCERS SYMPOSIUM
Major finding: Overall survival was better with MVAC plus radical cystectomy (median, 102 months) than with radical cystectomy alone, (median, 81 months), but the difference did not achieve statistical significance because the sample size was small (HR = 0.65, P = .07).
Data source: A study of 130 patients randomized to receive two cycles of MVAC neoadjuvant chemotherapy followed by radical cystectomy (64 patients), or radical cystectomy alone (66).
Disclosures: Dr. Kitamura said he had no relationships to disclose. Dr. Bajorin disclosed that he has been a consultant or adviser for Bristol-Myers Squibb, Dendreon, Lilly, and Novartis. He has received honoraria from Lilly, and research funding from Amgen, Dendreon, Genentech, Genta, GlaxoSmithKline, and Novartis.
Survey exposes physician frustrations with EHRs
NEW ORLEANS – Frustrated with your electronic medical record system? Getting increasingly irritated? You most definitely are not alone.
A survey of thousands of physicians across multiple specialties shows that user satisfaction with electronic health records fell 12% from 2010 to 2012.
The survey was conducted by the American College of Physicians and AmericanEHR Partners, an online agent that helps physicians select and evaluate health information technology. It is supported by 16 medical societies and five health IT organizations.
"Dissatisfaction is increasing regardless of practice type or EHR system," said Dr. Michael S. Barr, who leads ACP\'s Medical Practice, Professionalism & Quality division. "These findings highlight the need for the Meaningful Use program and EHR manufacturers to focus on improving EHR features and usability to help reduce inefficient work flows, improve error rates and patient care, and for practices to recognize the importance of ongoing training at all stages of EHR adoption," said Dr. Barr, in a statement issued along with the survey results.
The survey was released at the Healthcare Information and Management Systems Society Annual Conference and exhibition.
Dr. Alan Brookstone, a cofounder of AmericanEHR Partners, said at the meeting that satisfaction rates may be dropping in part because there had been so much adoption of technology so quickly. Also, it’s not just the early adopters anymore, he said.
The largest number of respondents – almost 1,900 – was from primary care. Specialists, surgeons, hospital-based physicians, and psychiatrists were also represented.
The vast majority of respondents – 70% – were from practices with fewer than 10 physicians.
The number who said they intended to participate in meaningful use has grown over the past few years, with a full 82% saying they would apply for incentives paid by Medicare and Medicaid.
Satisfaction rates with current EHR systems were low across a spectrum of parameters. While 45% said they would recommend the product they use to a colleague, 39% said they would not. In 2010, more physicians said they’d recommend that system, while only 24% said they would urge against use.
Of those surveyed, 36% said that they had encountered unexpected events, problems, or costs after signing the initial contract for the system.
Physicians were especially frustrated with the systems’ promise to decrease their workload. Thirty-four percent said they were dissatisfied with that promised ability, up from only 19% in 2010. Some respondents said that the EHR had decreased productivity and increased the amount of time needed to complete documentation. Fully a third of respondents said they had not returned to the productivity they had before they began to use the system.
About half of respondents were satisfied with functionality and ease of use, but a third were dissatisfied with those measures. That level of dissatisfaction was higher than it had been in 2010.
For instance, thirty-six percent said that it was difficult to reconcile an imported medication list with medications listed in a patient record.
Overall, when compared with other specialties, primary care physicians were the most satisfied with their system’s ability to improve patient care. Surgeons, representing about 660 respondents, were the least satisfied.
Good customer support and training for the EHR systems was rated as crucial to satisfaction. There was an 11% increase in dissatisfaction with customer support from 2010 to 2012. Thirty-three percent of respondents said they weren’t happy with the customer support they received.
The number of practices using a patient portal increased by 20% from 2010 to 2012, rising to 40%. This is probably driven by the stage 2 meaningful use rules, which require physicians to be able to securely communicate with patients and for patients to be able to download and share their health information. Still, 50% of respondents did not have a portal.
Dr. Brookstone said they survey showed that vendors needed to better integrate functionality, improve training, and find ways to help physicians rebalance their workload.
If physicians’ concerns aren’t addressed, it will lead to a decline in willingness to use the systems, he said.
NEW ORLEANS – Frustrated with your electronic medical record system? Getting increasingly irritated? You most definitely are not alone.
A survey of thousands of physicians across multiple specialties shows that user satisfaction with electronic health records fell 12% from 2010 to 2012.
The survey was conducted by the American College of Physicians and AmericanEHR Partners, an online agent that helps physicians select and evaluate health information technology. It is supported by 16 medical societies and five health IT organizations.
"Dissatisfaction is increasing regardless of practice type or EHR system," said Dr. Michael S. Barr, who leads ACP\'s Medical Practice, Professionalism & Quality division. "These findings highlight the need for the Meaningful Use program and EHR manufacturers to focus on improving EHR features and usability to help reduce inefficient work flows, improve error rates and patient care, and for practices to recognize the importance of ongoing training at all stages of EHR adoption," said Dr. Barr, in a statement issued along with the survey results.
The survey was released at the Healthcare Information and Management Systems Society Annual Conference and exhibition.
Dr. Alan Brookstone, a cofounder of AmericanEHR Partners, said at the meeting that satisfaction rates may be dropping in part because there had been so much adoption of technology so quickly. Also, it’s not just the early adopters anymore, he said.
The largest number of respondents – almost 1,900 – was from primary care. Specialists, surgeons, hospital-based physicians, and psychiatrists were also represented.
The vast majority of respondents – 70% – were from practices with fewer than 10 physicians.
The number who said they intended to participate in meaningful use has grown over the past few years, with a full 82% saying they would apply for incentives paid by Medicare and Medicaid.
Satisfaction rates with current EHR systems were low across a spectrum of parameters. While 45% said they would recommend the product they use to a colleague, 39% said they would not. In 2010, more physicians said they’d recommend that system, while only 24% said they would urge against use.
Of those surveyed, 36% said that they had encountered unexpected events, problems, or costs after signing the initial contract for the system.
Physicians were especially frustrated with the systems’ promise to decrease their workload. Thirty-four percent said they were dissatisfied with that promised ability, up from only 19% in 2010. Some respondents said that the EHR had decreased productivity and increased the amount of time needed to complete documentation. Fully a third of respondents said they had not returned to the productivity they had before they began to use the system.
About half of respondents were satisfied with functionality and ease of use, but a third were dissatisfied with those measures. That level of dissatisfaction was higher than it had been in 2010.
For instance, thirty-six percent said that it was difficult to reconcile an imported medication list with medications listed in a patient record.
Overall, when compared with other specialties, primary care physicians were the most satisfied with their system’s ability to improve patient care. Surgeons, representing about 660 respondents, were the least satisfied.
Good customer support and training for the EHR systems was rated as crucial to satisfaction. There was an 11% increase in dissatisfaction with customer support from 2010 to 2012. Thirty-three percent of respondents said they weren’t happy with the customer support they received.
The number of practices using a patient portal increased by 20% from 2010 to 2012, rising to 40%. This is probably driven by the stage 2 meaningful use rules, which require physicians to be able to securely communicate with patients and for patients to be able to download and share their health information. Still, 50% of respondents did not have a portal.
Dr. Brookstone said they survey showed that vendors needed to better integrate functionality, improve training, and find ways to help physicians rebalance their workload.
If physicians’ concerns aren’t addressed, it will lead to a decline in willingness to use the systems, he said.
NEW ORLEANS – Frustrated with your electronic medical record system? Getting increasingly irritated? You most definitely are not alone.
A survey of thousands of physicians across multiple specialties shows that user satisfaction with electronic health records fell 12% from 2010 to 2012.
The survey was conducted by the American College of Physicians and AmericanEHR Partners, an online agent that helps physicians select and evaluate health information technology. It is supported by 16 medical societies and five health IT organizations.
"Dissatisfaction is increasing regardless of practice type or EHR system," said Dr. Michael S. Barr, who leads ACP\'s Medical Practice, Professionalism & Quality division. "These findings highlight the need for the Meaningful Use program and EHR manufacturers to focus on improving EHR features and usability to help reduce inefficient work flows, improve error rates and patient care, and for practices to recognize the importance of ongoing training at all stages of EHR adoption," said Dr. Barr, in a statement issued along with the survey results.
The survey was released at the Healthcare Information and Management Systems Society Annual Conference and exhibition.
Dr. Alan Brookstone, a cofounder of AmericanEHR Partners, said at the meeting that satisfaction rates may be dropping in part because there had been so much adoption of technology so quickly. Also, it’s not just the early adopters anymore, he said.
The largest number of respondents – almost 1,900 – was from primary care. Specialists, surgeons, hospital-based physicians, and psychiatrists were also represented.
The vast majority of respondents – 70% – were from practices with fewer than 10 physicians.
The number who said they intended to participate in meaningful use has grown over the past few years, with a full 82% saying they would apply for incentives paid by Medicare and Medicaid.
Satisfaction rates with current EHR systems were low across a spectrum of parameters. While 45% said they would recommend the product they use to a colleague, 39% said they would not. In 2010, more physicians said they’d recommend that system, while only 24% said they would urge against use.
Of those surveyed, 36% said that they had encountered unexpected events, problems, or costs after signing the initial contract for the system.
Physicians were especially frustrated with the systems’ promise to decrease their workload. Thirty-four percent said they were dissatisfied with that promised ability, up from only 19% in 2010. Some respondents said that the EHR had decreased productivity and increased the amount of time needed to complete documentation. Fully a third of respondents said they had not returned to the productivity they had before they began to use the system.
About half of respondents were satisfied with functionality and ease of use, but a third were dissatisfied with those measures. That level of dissatisfaction was higher than it had been in 2010.
For instance, thirty-six percent said that it was difficult to reconcile an imported medication list with medications listed in a patient record.
Overall, when compared with other specialties, primary care physicians were the most satisfied with their system’s ability to improve patient care. Surgeons, representing about 660 respondents, were the least satisfied.
Good customer support and training for the EHR systems was rated as crucial to satisfaction. There was an 11% increase in dissatisfaction with customer support from 2010 to 2012. Thirty-three percent of respondents said they weren’t happy with the customer support they received.
The number of practices using a patient portal increased by 20% from 2010 to 2012, rising to 40%. This is probably driven by the stage 2 meaningful use rules, which require physicians to be able to securely communicate with patients and for patients to be able to download and share their health information. Still, 50% of respondents did not have a portal.
Dr. Brookstone said they survey showed that vendors needed to better integrate functionality, improve training, and find ways to help physicians rebalance their workload.
If physicians’ concerns aren’t addressed, it will lead to a decline in willingness to use the systems, he said.
AT THE HIMSS13 ANNUAL CONFERENCE
Survey: How appearance counts in ICU
An easy-to-read name tag and neat grooming are the most important individual appearance factors for physicians working in intensive care units, according to a survey of patients’ family members in JAMA Internal Medicine.
Among the 337 respondents, 77% considered an easy-to-read name tag the most important characteristic, followed by neat grooming (65%) and professional dress (59%). Respondents rated nine different factors on a five-point scale, with 5 being very important. The least important factors are physician sex (3%) and race (3%), reported Dr. Selena Au of the University of Calgary, Alta., and her associates (JAMA Intern. Med. 2013 Feb. 18 [doi:10.1001/jamainternmed.2013.2732]).
Respondents also viewed a series of 32 photographs of 8 physician models dressed in four types of attire – traditional white coat, scrubs, suit, and casual – and were asked to select the best physician overall. Physicians wearing a white coat received 52% of the vote, compared with 24% for scrubs, 13% for a suit, and 11% for casual attire, Dr. Au and her associates wrote.
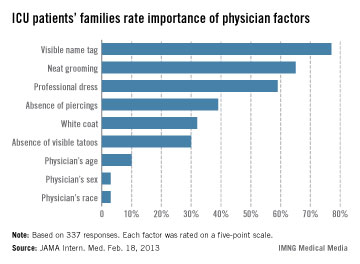
An easy-to-read name tag and neat grooming are the most important individual appearance factors for physicians working in intensive care units, according to a survey of patients’ family members in JAMA Internal Medicine.
Among the 337 respondents, 77% considered an easy-to-read name tag the most important characteristic, followed by neat grooming (65%) and professional dress (59%). Respondents rated nine different factors on a five-point scale, with 5 being very important. The least important factors are physician sex (3%) and race (3%), reported Dr. Selena Au of the University of Calgary, Alta., and her associates (JAMA Intern. Med. 2013 Feb. 18 [doi:10.1001/jamainternmed.2013.2732]).
Respondents also viewed a series of 32 photographs of 8 physician models dressed in four types of attire – traditional white coat, scrubs, suit, and casual – and were asked to select the best physician overall. Physicians wearing a white coat received 52% of the vote, compared with 24% for scrubs, 13% for a suit, and 11% for casual attire, Dr. Au and her associates wrote.
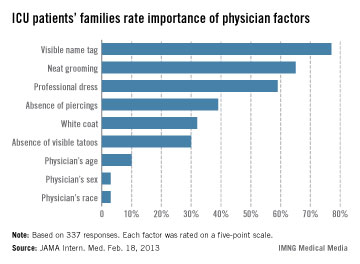
An easy-to-read name tag and neat grooming are the most important individual appearance factors for physicians working in intensive care units, according to a survey of patients’ family members in JAMA Internal Medicine.
Among the 337 respondents, 77% considered an easy-to-read name tag the most important characteristic, followed by neat grooming (65%) and professional dress (59%). Respondents rated nine different factors on a five-point scale, with 5 being very important. The least important factors are physician sex (3%) and race (3%), reported Dr. Selena Au of the University of Calgary, Alta., and her associates (JAMA Intern. Med. 2013 Feb. 18 [doi:10.1001/jamainternmed.2013.2732]).
Respondents also viewed a series of 32 photographs of 8 physician models dressed in four types of attire – traditional white coat, scrubs, suit, and casual – and were asked to select the best physician overall. Physicians wearing a white coat received 52% of the vote, compared with 24% for scrubs, 13% for a suit, and 11% for casual attire, Dr. Au and her associates wrote.
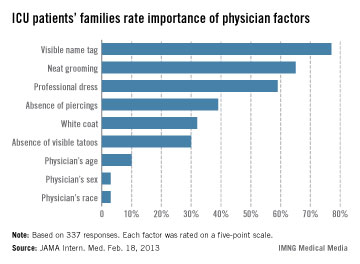
FROM JAMA INTERNAL MEDICINE
Rabies death follows infected organ transplant
A Maryland man recently died of rabies more than a year after receiving an infected organ in a transplant, according to the Centers for Disease Control and Prevention.
Officials at the CDC and the Maryland Department of Health and Mental Hygiene confirmed that the man died from rabies contracted through an organ transplant performed in 2011. After an investigation found that the Maryland man had no reported animal exposures, health officials began looking into the possibility that the infection was transmitted during his transplant.
Tissue testing of the organ donor and recipient revealed that they both had a raccoon type of rabies virus, which can infect raccoons as well as other wild and domestic animals. Only one other person is reported to have died from a raccoon-type rabies virus in the United States, according to the CDC.
Three other people who received organs from the infected donor have been identified and are receiving immune globulin and antirabies vaccination. In addition, the CDC is working with health officials in Florida, Georgia, Illinois, Maryland, and North Carolina to identify anyone who was in close contact with either the initial organ donor or the four recipients since they may also need postexposure rabies treatment.
At the time of the organ donor’s death in 2011, rabies was not suspected as the cause. Investigators are still trying to piece together how the donor first contracted rabies.
Although all potential organ donors in the United States are screened for infectious diseases such as HIV and hepatitis, rabies is not part of the standard screening process. The CDC estimates that there are only one to three cases of human rabies diagnosed each year in the United States. Because cases are so rare, screening for rabies is not routinely performed unless it is suspected based on interviews with family and friends or a physical examination, according to the CDC.
Maryland Department of Health and Mental Hygiene, infection
A Maryland man recently died of rabies more than a year after receiving an infected organ in a transplant, according to the Centers for Disease Control and Prevention.
Officials at the CDC and the Maryland Department of Health and Mental Hygiene confirmed that the man died from rabies contracted through an organ transplant performed in 2011. After an investigation found that the Maryland man had no reported animal exposures, health officials began looking into the possibility that the infection was transmitted during his transplant.
Tissue testing of the organ donor and recipient revealed that they both had a raccoon type of rabies virus, which can infect raccoons as well as other wild and domestic animals. Only one other person is reported to have died from a raccoon-type rabies virus in the United States, according to the CDC.
Three other people who received organs from the infected donor have been identified and are receiving immune globulin and antirabies vaccination. In addition, the CDC is working with health officials in Florida, Georgia, Illinois, Maryland, and North Carolina to identify anyone who was in close contact with either the initial organ donor or the four recipients since they may also need postexposure rabies treatment.
At the time of the organ donor’s death in 2011, rabies was not suspected as the cause. Investigators are still trying to piece together how the donor first contracted rabies.
Although all potential organ donors in the United States are screened for infectious diseases such as HIV and hepatitis, rabies is not part of the standard screening process. The CDC estimates that there are only one to three cases of human rabies diagnosed each year in the United States. Because cases are so rare, screening for rabies is not routinely performed unless it is suspected based on interviews with family and friends or a physical examination, according to the CDC.
A Maryland man recently died of rabies more than a year after receiving an infected organ in a transplant, according to the Centers for Disease Control and Prevention.
Officials at the CDC and the Maryland Department of Health and Mental Hygiene confirmed that the man died from rabies contracted through an organ transplant performed in 2011. After an investigation found that the Maryland man had no reported animal exposures, health officials began looking into the possibility that the infection was transmitted during his transplant.
Tissue testing of the organ donor and recipient revealed that they both had a raccoon type of rabies virus, which can infect raccoons as well as other wild and domestic animals. Only one other person is reported to have died from a raccoon-type rabies virus in the United States, according to the CDC.
Three other people who received organs from the infected donor have been identified and are receiving immune globulin and antirabies vaccination. In addition, the CDC is working with health officials in Florida, Georgia, Illinois, Maryland, and North Carolina to identify anyone who was in close contact with either the initial organ donor or the four recipients since they may also need postexposure rabies treatment.
At the time of the organ donor’s death in 2011, rabies was not suspected as the cause. Investigators are still trying to piece together how the donor first contracted rabies.
Although all potential organ donors in the United States are screened for infectious diseases such as HIV and hepatitis, rabies is not part of the standard screening process. The CDC estimates that there are only one to three cases of human rabies diagnosed each year in the United States. Because cases are so rare, screening for rabies is not routinely performed unless it is suspected based on interviews with family and friends or a physical examination, according to the CDC.
Maryland Department of Health and Mental Hygiene, infection
Maryland Department of Health and Mental Hygiene, infection