User login
Official Newspaper of the American College of Surgeons
New blood test could identify early pancreatic cancer
An investigational serum biomarker panel accurately identified potentially resectable cases of pancreatic cancer, opening the possibility that a blood test could identify the cancer early and improve its dismal prognosis.
The panel measured four metabolites and had an overall sensitivity of 71% and a specificity of 78% for pancreatic cancer; the specificity for resectable tumors also approached 78%, reported Dr. Masaru Yoshida (Cancer Epidemiol. Biomarkers Prev. 2013 March 29 [doi: 10.1158/1055-9965.EPI-12-1033]).
The panel was more accurate than were any of the currently used biomarkers, including CA19-9 and CEA, said Dr. Yoshida, professor and chief of metabolomics research at Kobe University, Japan.
"This novel diagnostic approach, which is safe and easy to apply as a screening method, is expected to improve the prognosis of patients with pancreatic cancer by detecting their cancers early, when still in a resectable and curable state," Dr. Yoshida said in a press statement.
The researchers created the panel based on study of a cohort of 85 subjects: 43 with pancreatic cancer and 42 healthy controls. First, they pared down 113 potentially useful metabolites into a workable testing panel. Of the 45 candidate metabolites, four of them – xylitol, 1,5-anhydro-D-glucitol, histidine, and inositol – showed the highest variation between the healthy controls and the patients. In the training cohort, the panel of these four markers had a sensitivity of 86% and specificity of 88% for pancreatic cancer.
Next, the researchers evaluated a validation cohort of 42 cancer patients, 41 healthy controls, and 23 patients with chronic pancreatitis. In this cohort, with an area under the curve of 0.76, the panel’s sensitivity for pancreatic cancer was 71% and specificity, 78%. In contrast, the sensitivity of CA19-9 was 69% and specificity 86%; for CEA, those numbers were 36% and 80%, respectively.
In the subset of patients with resectable pancreatic cancer, the panel’s sensitivity was 78%, compared with 56% for CA19-9 and 44% for CEA.
The metabolic panel was also able to identify chronic pancreatitis, with a 17% rate of false positives, compared with a false positive rate of 30% for CA19-9 and 44% for CEA.
A blood panel could address three key problems in the field of pancreatic cancer, Dr. Yoshida and his colleagues said. "The first is the difficulty of detecting pancreatic cancer early in resectable stages. A sensitivity and specificity of about 80% for resectable disease ... should be acceptable for clinical use because most patients with resectable cancer have no symptoms, and blood examinations are useful tools for initial screening examinations."
The second problem is the difficulty in differentiating pancreatic cancer from chronic pancreatitis. "Many gastroenterologists follow up chronic pancreatitis with scheduled CT, magnetic resonance imaging (MRI), and endoscopic ultrasound scans (EUS); tumor marker tests; and endoscopic retrograde cholangiopancreatography (ERCP), but the initial malignant changes are frequently overlooked, and pancreatic tumors can rapidly become unresectable. In addition, unnecessary resections for benign inflammatory lesions are sometimes done because of false-positive results from CA19-9 and/or imaging examinations."
The third clinical problem is the risk of complications that result from pancreatic examinations. Serum samples are easy and safe to obtain, with a low risk of adverse events and, with this panel, a potentially good return of information. A blood test could also be a useful population screening tool, the researchers noted.
The metabolites probably reflect metabolic derangement that arises not only from focal tumorigenesis, but also from systemic reactions to pancreatic disease, Dr. Yoshida and his coinvestigators wrote. Pancreatic cancer causes significant decreases in some amino and fatty acids, probably because the tumor recruits these substances to aid its rapid cellular proliferation.
"Patients with pancreatic disease are also troubled by malnutrition because of pancreatic endocrine and exocrine insufficiency. Therefore, there is a possibility that the decreases in serum metabolite levels also reflect malnutrition."
Finally, they said, the decrease in 1,5-anhydro-D-glucitol indicates the presence of hyperglycemia and recent glycosuria. "These results suggest that glucose tolerance was impaired in these patients because of pancreatic insufficiency."
The authors reported no financial conflicts. The work was supported by grants administered by agencies of the Japanese government.
An investigational serum biomarker panel accurately identified potentially resectable cases of pancreatic cancer, opening the possibility that a blood test could identify the cancer early and improve its dismal prognosis.
The panel measured four metabolites and had an overall sensitivity of 71% and a specificity of 78% for pancreatic cancer; the specificity for resectable tumors also approached 78%, reported Dr. Masaru Yoshida (Cancer Epidemiol. Biomarkers Prev. 2013 March 29 [doi: 10.1158/1055-9965.EPI-12-1033]).
The panel was more accurate than were any of the currently used biomarkers, including CA19-9 and CEA, said Dr. Yoshida, professor and chief of metabolomics research at Kobe University, Japan.
"This novel diagnostic approach, which is safe and easy to apply as a screening method, is expected to improve the prognosis of patients with pancreatic cancer by detecting their cancers early, when still in a resectable and curable state," Dr. Yoshida said in a press statement.
The researchers created the panel based on study of a cohort of 85 subjects: 43 with pancreatic cancer and 42 healthy controls. First, they pared down 113 potentially useful metabolites into a workable testing panel. Of the 45 candidate metabolites, four of them – xylitol, 1,5-anhydro-D-glucitol, histidine, and inositol – showed the highest variation between the healthy controls and the patients. In the training cohort, the panel of these four markers had a sensitivity of 86% and specificity of 88% for pancreatic cancer.
Next, the researchers evaluated a validation cohort of 42 cancer patients, 41 healthy controls, and 23 patients with chronic pancreatitis. In this cohort, with an area under the curve of 0.76, the panel’s sensitivity for pancreatic cancer was 71% and specificity, 78%. In contrast, the sensitivity of CA19-9 was 69% and specificity 86%; for CEA, those numbers were 36% and 80%, respectively.
In the subset of patients with resectable pancreatic cancer, the panel’s sensitivity was 78%, compared with 56% for CA19-9 and 44% for CEA.
The metabolic panel was also able to identify chronic pancreatitis, with a 17% rate of false positives, compared with a false positive rate of 30% for CA19-9 and 44% for CEA.
A blood panel could address three key problems in the field of pancreatic cancer, Dr. Yoshida and his colleagues said. "The first is the difficulty of detecting pancreatic cancer early in resectable stages. A sensitivity and specificity of about 80% for resectable disease ... should be acceptable for clinical use because most patients with resectable cancer have no symptoms, and blood examinations are useful tools for initial screening examinations."
The second problem is the difficulty in differentiating pancreatic cancer from chronic pancreatitis. "Many gastroenterologists follow up chronic pancreatitis with scheduled CT, magnetic resonance imaging (MRI), and endoscopic ultrasound scans (EUS); tumor marker tests; and endoscopic retrograde cholangiopancreatography (ERCP), but the initial malignant changes are frequently overlooked, and pancreatic tumors can rapidly become unresectable. In addition, unnecessary resections for benign inflammatory lesions are sometimes done because of false-positive results from CA19-9 and/or imaging examinations."
The third clinical problem is the risk of complications that result from pancreatic examinations. Serum samples are easy and safe to obtain, with a low risk of adverse events and, with this panel, a potentially good return of information. A blood test could also be a useful population screening tool, the researchers noted.
The metabolites probably reflect metabolic derangement that arises not only from focal tumorigenesis, but also from systemic reactions to pancreatic disease, Dr. Yoshida and his coinvestigators wrote. Pancreatic cancer causes significant decreases in some amino and fatty acids, probably because the tumor recruits these substances to aid its rapid cellular proliferation.
"Patients with pancreatic disease are also troubled by malnutrition because of pancreatic endocrine and exocrine insufficiency. Therefore, there is a possibility that the decreases in serum metabolite levels also reflect malnutrition."
Finally, they said, the decrease in 1,5-anhydro-D-glucitol indicates the presence of hyperglycemia and recent glycosuria. "These results suggest that glucose tolerance was impaired in these patients because of pancreatic insufficiency."
The authors reported no financial conflicts. The work was supported by grants administered by agencies of the Japanese government.
An investigational serum biomarker panel accurately identified potentially resectable cases of pancreatic cancer, opening the possibility that a blood test could identify the cancer early and improve its dismal prognosis.
The panel measured four metabolites and had an overall sensitivity of 71% and a specificity of 78% for pancreatic cancer; the specificity for resectable tumors also approached 78%, reported Dr. Masaru Yoshida (Cancer Epidemiol. Biomarkers Prev. 2013 March 29 [doi: 10.1158/1055-9965.EPI-12-1033]).
The panel was more accurate than were any of the currently used biomarkers, including CA19-9 and CEA, said Dr. Yoshida, professor and chief of metabolomics research at Kobe University, Japan.
"This novel diagnostic approach, which is safe and easy to apply as a screening method, is expected to improve the prognosis of patients with pancreatic cancer by detecting their cancers early, when still in a resectable and curable state," Dr. Yoshida said in a press statement.
The researchers created the panel based on study of a cohort of 85 subjects: 43 with pancreatic cancer and 42 healthy controls. First, they pared down 113 potentially useful metabolites into a workable testing panel. Of the 45 candidate metabolites, four of them – xylitol, 1,5-anhydro-D-glucitol, histidine, and inositol – showed the highest variation between the healthy controls and the patients. In the training cohort, the panel of these four markers had a sensitivity of 86% and specificity of 88% for pancreatic cancer.
Next, the researchers evaluated a validation cohort of 42 cancer patients, 41 healthy controls, and 23 patients with chronic pancreatitis. In this cohort, with an area under the curve of 0.76, the panel’s sensitivity for pancreatic cancer was 71% and specificity, 78%. In contrast, the sensitivity of CA19-9 was 69% and specificity 86%; for CEA, those numbers were 36% and 80%, respectively.
In the subset of patients with resectable pancreatic cancer, the panel’s sensitivity was 78%, compared with 56% for CA19-9 and 44% for CEA.
The metabolic panel was also able to identify chronic pancreatitis, with a 17% rate of false positives, compared with a false positive rate of 30% for CA19-9 and 44% for CEA.
A blood panel could address three key problems in the field of pancreatic cancer, Dr. Yoshida and his colleagues said. "The first is the difficulty of detecting pancreatic cancer early in resectable stages. A sensitivity and specificity of about 80% for resectable disease ... should be acceptable for clinical use because most patients with resectable cancer have no symptoms, and blood examinations are useful tools for initial screening examinations."
The second problem is the difficulty in differentiating pancreatic cancer from chronic pancreatitis. "Many gastroenterologists follow up chronic pancreatitis with scheduled CT, magnetic resonance imaging (MRI), and endoscopic ultrasound scans (EUS); tumor marker tests; and endoscopic retrograde cholangiopancreatography (ERCP), but the initial malignant changes are frequently overlooked, and pancreatic tumors can rapidly become unresectable. In addition, unnecessary resections for benign inflammatory lesions are sometimes done because of false-positive results from CA19-9 and/or imaging examinations."
The third clinical problem is the risk of complications that result from pancreatic examinations. Serum samples are easy and safe to obtain, with a low risk of adverse events and, with this panel, a potentially good return of information. A blood test could also be a useful population screening tool, the researchers noted.
The metabolites probably reflect metabolic derangement that arises not only from focal tumorigenesis, but also from systemic reactions to pancreatic disease, Dr. Yoshida and his coinvestigators wrote. Pancreatic cancer causes significant decreases in some amino and fatty acids, probably because the tumor recruits these substances to aid its rapid cellular proliferation.
"Patients with pancreatic disease are also troubled by malnutrition because of pancreatic endocrine and exocrine insufficiency. Therefore, there is a possibility that the decreases in serum metabolite levels also reflect malnutrition."
Finally, they said, the decrease in 1,5-anhydro-D-glucitol indicates the presence of hyperglycemia and recent glycosuria. "These results suggest that glucose tolerance was impaired in these patients because of pancreatic insufficiency."
The authors reported no financial conflicts. The work was supported by grants administered by agencies of the Japanese government.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS, AND PREVENTION
Major finding: A serum panel of four metabolites had a 78% sensitivity for detecting resectable pancreatic cancers.
Data source: The panel was derived from a test cohort of 85, and a validation cohort of 42 cancer patients, 41 healthy controls, and 23 patients with chronic pancreatitis.
Disclosures: The authors had no financial disclosures. Japanese government agencies funded the study.
Bariatric surgery advancement spurs guideline update
Weight loss surgery patients should get routine copper supplements along with other vitamins and minerals, according to newly updated bariatric surgery guidelines from the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic and Bariatric Surgery.
The groups call for 2 mg/day to offset the potential for surgery to cause a deficiency. Although routine copper screening isn’t necessary after the procedure, copper levels should be assessed and treated as needed in patients with anemia, neutropenia, myeloneuropathy, and impaired wound healing.
The copper recommendations are new since the guidelines were last published in 2008. Other recommendations – there are 74 in all – have been revised to incorporate new advances in weight loss surgery and an improved evidence base. Changes are pointed out where they’ve been made, and the level of evidence cited for each assertion. Pre- and postoperative bariatric surgery checklists have been added as well, to help avoid errors.
"This is actually a very unique collaboration among the internists represented by the endocrinologists and the obesity people and the surgeons. We actually agreed on all these things. The main intent is to assist with clinical decision making," including selecting patients and procedures and perioperative management, said lead author Dr. Jeffrey Mechanick, president-elect of the American Association of Clinical Endocrinologists and director of metabolic support at the Mt. Sinai School of Medicine in New York.
"We scrutinized every recommendation one by one in the context of the new data. In many cases the recommendations changed," he said in an interview.
Another new recommendation is for patients to be followed by their primary care physicians and screened for cancer prior to surgery, as appropriate for age and risk. Dr. Mechanick and his colleagues have also given more attention to consent, behavioral, and psychiatric issues as well as weight loss surgery in patients with type 2 diabetes.
There’s more information on sleeve gastrectomy, as well. Considered experimental in 2008, it’s now "approved and being done more widely. There are some very nice data about its metabolic effects, independent from just the weight loss effect, effects on glycemic control, and cardiovascular risk. It was very important to devote a fair amount of time" to the procedure, he said.
The guidelines note that "sleeve gastrectomy has demonstrated benefits comparable to other bariatric procedures. ... A national risk-adjusted database positions [it] between the laparoscopic adjustable gastric band and laparoscopic Roux-en-Y gastric bypass in terms of weight loss, co-morbidity resolution, and complications."
"We [also] addressed two issues which were quite controversial, and are still rather unsettled. The first is the use of the lap band for mild obesity. The second is the use of these weight loss procedures specifically for patients with type 2 diabetes for glycemic control. Since 2008, there’ve been a lot more data" about the issues, he said, just as there’ve been more data about the need for copper supplementation.
As in 2008, the guidelines do not recommend bariatric surgery solely for glycemic control. "We still don’t have an absolute indication for ‘diabetes surgery,’ but we do recognize the existence of the salutary effects on glycemic control when these procedures are done for weight loss. It was important for the reader to be exposed to this information," Dr. Mechanick said.
Regarding surgery in the mildly obese, the guidelines note that patients with a body mass index of 30-34.9 kg/m2 with diabetes or metabolic syndrome "may also be offered a bariatric procedure, although current evidence is limited by the number of subjects studied and lack of long-term data demonstrating net benefit."
The guidelines will be published in the March/April 2013 issue of Endocrine Practice and March 2013 issue of Surgery for Obesity and Related Diseases.
Dr. Mechanick disclosed compensation from Abbott Nutrition for lectures and program development.
From preoperative evaluation through bariatric
surgery and onward through long-term postoperative health management, weight
loss surgery and the medical care associated with it is, obligatorily, a
thoroughly interdisciplinary effort. Endocrinologists and internists on the
bariatrics team spearhead lifestyle management, medical weight loss, and
long-term postoperative care and efforts to maintain durable weight loss.
Surgeons, endocrinologists, and internists work together to select patients
appropriate for bariatric surgery, to choose the weight-loss surgery best
suited to each individual patient, and to provide the proper preoperative
evaluation. Surgeons perform the appropriate bariatric operation and oversee
immediate postoperative and short-term perioperative care, and, frequently in
concert with gastroenterologists, internists, and endocrinologists, manage
complications that can result from bariatric surgery. Finally, long-term
continuity of medical care and durable maintenance of weight loss is again
directed by the endocrinologist and internist.
Thus, given that the entire bariatric care schema is
such an interdisciplinary effort, clinical practice guidelines for the
management of bariatric surgical patients must also be the product of an
analogous interdisciplinary effort. It is with this aim and in this spirit that
the American Association of Clinical Endocrinologists (AACE), The Obesity
Society (TOS), and American Society for Metabolic and Bariatric Surgery (AAMBS)
published their initial Medical Guidelines for Clinical Practice for the Perioperative
Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery
Patient in 2008. The same cooperating societies have just published their
sequel with numerous substantive additions, changes, and refinements. The
Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and
Nonsurgical Support of the Bariatric Surgery Patient – 2013 Update: Cosponsored
by American Association of Clinical Endocrinologists, The Obesity Society, and
American Society for Metabolic & Bariatric Surgery was published jointly in
the March issue of Surgery for Obesity and Related Disease, and in the
March/April issue of Endocrine Practice.
Clearly, much has changed in the bariatric landscape
in the intervening half-decade. Laparoscopic gastric band surgery has declined,
while sleeve gastrectomy has gained traction as a restrictive bariatric
operation with more robust weight loss and glycemic effects. The
increasingly recognized impact of Roux-en-Y gastric bypass surgery not only on
weight loss, but also on glycemic control and other endocrinologic endpoints
has prompted studies to determine if such benefits might also result from
restrictive-only bariatric surgeries such as sleeve gastrectomy, and initial
results appear encouraging. The arrival of more and higher-quality data with
longer-term follow up of a greater variety of endpoints has led to the ability
of these updated guidelines to provide an increasing number of more specific,
data-driven recommendations related to the broader spectrum of bariatric
surgical procedures and anatomies managed by clinicians today. They cover every
aspect of the bariatric surgical patient, from preoperative evaluation through
surgery, to postoperative management, all with more solidly outcomes-based
recommendations from over 400 references, with user-friendly and more
error-proof preoperative and postoperative care checklists, while still
arriving at such expert guidelines through interdisciplinary study and
agreement in this timely update.
John A. Martin, M.D., is associate
professor of medicine and surgery and director of endoscopy, Northwestern
University Feinberg School of Medicine, Chicago.
From preoperative evaluation through bariatric
surgery and onward through long-term postoperative health management, weight
loss surgery and the medical care associated with it is, obligatorily, a
thoroughly interdisciplinary effort. Endocrinologists and internists on the
bariatrics team spearhead lifestyle management, medical weight loss, and
long-term postoperative care and efforts to maintain durable weight loss.
Surgeons, endocrinologists, and internists work together to select patients
appropriate for bariatric surgery, to choose the weight-loss surgery best
suited to each individual patient, and to provide the proper preoperative
evaluation. Surgeons perform the appropriate bariatric operation and oversee
immediate postoperative and short-term perioperative care, and, frequently in
concert with gastroenterologists, internists, and endocrinologists, manage
complications that can result from bariatric surgery. Finally, long-term
continuity of medical care and durable maintenance of weight loss is again
directed by the endocrinologist and internist.
Thus, given that the entire bariatric care schema is
such an interdisciplinary effort, clinical practice guidelines for the
management of bariatric surgical patients must also be the product of an
analogous interdisciplinary effort. It is with this aim and in this spirit that
the American Association of Clinical Endocrinologists (AACE), The Obesity
Society (TOS), and American Society for Metabolic and Bariatric Surgery (AAMBS)
published their initial Medical Guidelines for Clinical Practice for the Perioperative
Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery
Patient in 2008. The same cooperating societies have just published their
sequel with numerous substantive additions, changes, and refinements. The
Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and
Nonsurgical Support of the Bariatric Surgery Patient – 2013 Update: Cosponsored
by American Association of Clinical Endocrinologists, The Obesity Society, and
American Society for Metabolic & Bariatric Surgery was published jointly in
the March issue of Surgery for Obesity and Related Disease, and in the
March/April issue of Endocrine Practice.
Clearly, much has changed in the bariatric landscape
in the intervening half-decade. Laparoscopic gastric band surgery has declined,
while sleeve gastrectomy has gained traction as a restrictive bariatric
operation with more robust weight loss and glycemic effects. The
increasingly recognized impact of Roux-en-Y gastric bypass surgery not only on
weight loss, but also on glycemic control and other endocrinologic endpoints
has prompted studies to determine if such benefits might also result from
restrictive-only bariatric surgeries such as sleeve gastrectomy, and initial
results appear encouraging. The arrival of more and higher-quality data with
longer-term follow up of a greater variety of endpoints has led to the ability
of these updated guidelines to provide an increasing number of more specific,
data-driven recommendations related to the broader spectrum of bariatric
surgical procedures and anatomies managed by clinicians today. They cover every
aspect of the bariatric surgical patient, from preoperative evaluation through
surgery, to postoperative management, all with more solidly outcomes-based
recommendations from over 400 references, with user-friendly and more
error-proof preoperative and postoperative care checklists, while still
arriving at such expert guidelines through interdisciplinary study and
agreement in this timely update.
John A. Martin, M.D., is associate
professor of medicine and surgery and director of endoscopy, Northwestern
University Feinberg School of Medicine, Chicago.
From preoperative evaluation through bariatric
surgery and onward through long-term postoperative health management, weight
loss surgery and the medical care associated with it is, obligatorily, a
thoroughly interdisciplinary effort. Endocrinologists and internists on the
bariatrics team spearhead lifestyle management, medical weight loss, and
long-term postoperative care and efforts to maintain durable weight loss.
Surgeons, endocrinologists, and internists work together to select patients
appropriate for bariatric surgery, to choose the weight-loss surgery best
suited to each individual patient, and to provide the proper preoperative
evaluation. Surgeons perform the appropriate bariatric operation and oversee
immediate postoperative and short-term perioperative care, and, frequently in
concert with gastroenterologists, internists, and endocrinologists, manage
complications that can result from bariatric surgery. Finally, long-term
continuity of medical care and durable maintenance of weight loss is again
directed by the endocrinologist and internist.
Thus, given that the entire bariatric care schema is
such an interdisciplinary effort, clinical practice guidelines for the
management of bariatric surgical patients must also be the product of an
analogous interdisciplinary effort. It is with this aim and in this spirit that
the American Association of Clinical Endocrinologists (AACE), The Obesity
Society (TOS), and American Society for Metabolic and Bariatric Surgery (AAMBS)
published their initial Medical Guidelines for Clinical Practice for the Perioperative
Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery
Patient in 2008. The same cooperating societies have just published their
sequel with numerous substantive additions, changes, and refinements. The
Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and
Nonsurgical Support of the Bariatric Surgery Patient – 2013 Update: Cosponsored
by American Association of Clinical Endocrinologists, The Obesity Society, and
American Society for Metabolic & Bariatric Surgery was published jointly in
the March issue of Surgery for Obesity and Related Disease, and in the
March/April issue of Endocrine Practice.
Clearly, much has changed in the bariatric landscape
in the intervening half-decade. Laparoscopic gastric band surgery has declined,
while sleeve gastrectomy has gained traction as a restrictive bariatric
operation with more robust weight loss and glycemic effects. The
increasingly recognized impact of Roux-en-Y gastric bypass surgery not only on
weight loss, but also on glycemic control and other endocrinologic endpoints
has prompted studies to determine if such benefits might also result from
restrictive-only bariatric surgeries such as sleeve gastrectomy, and initial
results appear encouraging. The arrival of more and higher-quality data with
longer-term follow up of a greater variety of endpoints has led to the ability
of these updated guidelines to provide an increasing number of more specific,
data-driven recommendations related to the broader spectrum of bariatric
surgical procedures and anatomies managed by clinicians today. They cover every
aspect of the bariatric surgical patient, from preoperative evaluation through
surgery, to postoperative management, all with more solidly outcomes-based
recommendations from over 400 references, with user-friendly and more
error-proof preoperative and postoperative care checklists, while still
arriving at such expert guidelines through interdisciplinary study and
agreement in this timely update.
John A. Martin, M.D., is associate
professor of medicine and surgery and director of endoscopy, Northwestern
University Feinberg School of Medicine, Chicago.
Weight loss surgery patients should get routine copper supplements along with other vitamins and minerals, according to newly updated bariatric surgery guidelines from the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic and Bariatric Surgery.
The groups call for 2 mg/day to offset the potential for surgery to cause a deficiency. Although routine copper screening isn’t necessary after the procedure, copper levels should be assessed and treated as needed in patients with anemia, neutropenia, myeloneuropathy, and impaired wound healing.
The copper recommendations are new since the guidelines were last published in 2008. Other recommendations – there are 74 in all – have been revised to incorporate new advances in weight loss surgery and an improved evidence base. Changes are pointed out where they’ve been made, and the level of evidence cited for each assertion. Pre- and postoperative bariatric surgery checklists have been added as well, to help avoid errors.
"This is actually a very unique collaboration among the internists represented by the endocrinologists and the obesity people and the surgeons. We actually agreed on all these things. The main intent is to assist with clinical decision making," including selecting patients and procedures and perioperative management, said lead author Dr. Jeffrey Mechanick, president-elect of the American Association of Clinical Endocrinologists and director of metabolic support at the Mt. Sinai School of Medicine in New York.
"We scrutinized every recommendation one by one in the context of the new data. In many cases the recommendations changed," he said in an interview.
Another new recommendation is for patients to be followed by their primary care physicians and screened for cancer prior to surgery, as appropriate for age and risk. Dr. Mechanick and his colleagues have also given more attention to consent, behavioral, and psychiatric issues as well as weight loss surgery in patients with type 2 diabetes.
There’s more information on sleeve gastrectomy, as well. Considered experimental in 2008, it’s now "approved and being done more widely. There are some very nice data about its metabolic effects, independent from just the weight loss effect, effects on glycemic control, and cardiovascular risk. It was very important to devote a fair amount of time" to the procedure, he said.
The guidelines note that "sleeve gastrectomy has demonstrated benefits comparable to other bariatric procedures. ... A national risk-adjusted database positions [it] between the laparoscopic adjustable gastric band and laparoscopic Roux-en-Y gastric bypass in terms of weight loss, co-morbidity resolution, and complications."
"We [also] addressed two issues which were quite controversial, and are still rather unsettled. The first is the use of the lap band for mild obesity. The second is the use of these weight loss procedures specifically for patients with type 2 diabetes for glycemic control. Since 2008, there’ve been a lot more data" about the issues, he said, just as there’ve been more data about the need for copper supplementation.
As in 2008, the guidelines do not recommend bariatric surgery solely for glycemic control. "We still don’t have an absolute indication for ‘diabetes surgery,’ but we do recognize the existence of the salutary effects on glycemic control when these procedures are done for weight loss. It was important for the reader to be exposed to this information," Dr. Mechanick said.
Regarding surgery in the mildly obese, the guidelines note that patients with a body mass index of 30-34.9 kg/m2 with diabetes or metabolic syndrome "may also be offered a bariatric procedure, although current evidence is limited by the number of subjects studied and lack of long-term data demonstrating net benefit."
The guidelines will be published in the March/April 2013 issue of Endocrine Practice and March 2013 issue of Surgery for Obesity and Related Diseases.
Dr. Mechanick disclosed compensation from Abbott Nutrition for lectures and program development.
Weight loss surgery patients should get routine copper supplements along with other vitamins and minerals, according to newly updated bariatric surgery guidelines from the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic and Bariatric Surgery.
The groups call for 2 mg/day to offset the potential for surgery to cause a deficiency. Although routine copper screening isn’t necessary after the procedure, copper levels should be assessed and treated as needed in patients with anemia, neutropenia, myeloneuropathy, and impaired wound healing.
The copper recommendations are new since the guidelines were last published in 2008. Other recommendations – there are 74 in all – have been revised to incorporate new advances in weight loss surgery and an improved evidence base. Changes are pointed out where they’ve been made, and the level of evidence cited for each assertion. Pre- and postoperative bariatric surgery checklists have been added as well, to help avoid errors.
"This is actually a very unique collaboration among the internists represented by the endocrinologists and the obesity people and the surgeons. We actually agreed on all these things. The main intent is to assist with clinical decision making," including selecting patients and procedures and perioperative management, said lead author Dr. Jeffrey Mechanick, president-elect of the American Association of Clinical Endocrinologists and director of metabolic support at the Mt. Sinai School of Medicine in New York.
"We scrutinized every recommendation one by one in the context of the new data. In many cases the recommendations changed," he said in an interview.
Another new recommendation is for patients to be followed by their primary care physicians and screened for cancer prior to surgery, as appropriate for age and risk. Dr. Mechanick and his colleagues have also given more attention to consent, behavioral, and psychiatric issues as well as weight loss surgery in patients with type 2 diabetes.
There’s more information on sleeve gastrectomy, as well. Considered experimental in 2008, it’s now "approved and being done more widely. There are some very nice data about its metabolic effects, independent from just the weight loss effect, effects on glycemic control, and cardiovascular risk. It was very important to devote a fair amount of time" to the procedure, he said.
The guidelines note that "sleeve gastrectomy has demonstrated benefits comparable to other bariatric procedures. ... A national risk-adjusted database positions [it] between the laparoscopic adjustable gastric band and laparoscopic Roux-en-Y gastric bypass in terms of weight loss, co-morbidity resolution, and complications."
"We [also] addressed two issues which were quite controversial, and are still rather unsettled. The first is the use of the lap band for mild obesity. The second is the use of these weight loss procedures specifically for patients with type 2 diabetes for glycemic control. Since 2008, there’ve been a lot more data" about the issues, he said, just as there’ve been more data about the need for copper supplementation.
As in 2008, the guidelines do not recommend bariatric surgery solely for glycemic control. "We still don’t have an absolute indication for ‘diabetes surgery,’ but we do recognize the existence of the salutary effects on glycemic control when these procedures are done for weight loss. It was important for the reader to be exposed to this information," Dr. Mechanick said.
Regarding surgery in the mildly obese, the guidelines note that patients with a body mass index of 30-34.9 kg/m2 with diabetes or metabolic syndrome "may also be offered a bariatric procedure, although current evidence is limited by the number of subjects studied and lack of long-term data demonstrating net benefit."
The guidelines will be published in the March/April 2013 issue of Endocrine Practice and March 2013 issue of Surgery for Obesity and Related Diseases.
Dr. Mechanick disclosed compensation from Abbott Nutrition for lectures and program development.
Platelet-rich plasma improved tennis elbow pain
Platelet-rich plasma therapy improved both the pain scores and elbow tenderness for almost three-quarters of patients suffering from tennis elbow during a 6-month randomized, double-blind controlled trial.
This study is the third to show a treatment response with no significant complications in patients with lateral epicondylar tendinopathy, commonly known as tennis elbow, from platelet-rich plasma (PRP) injections.
Dr. Allan Mishra, of Stanford (Calif.) University Medical Center,* and his coinvestigators from eight other institutions presented their findings from the trial at the annual meeting of the American Academy of Orthopaedic Surgeons in Chicago.
The 230 study participants had symptoms for at least 3 months and reported tenderness at the lateral epicondyle and pain scored at a minimum of 50 out of 100 on a visual analog scale during a resisted wrist extension. All participants failed to respond to conventional therapy, including a combination of physical therapy, nonsteroidal anti-inflammatory medications, and/or steroid injections, the investigators reported.
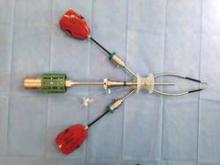
Dr. Mishra and his colleagues used a Biomet GPS centrifuge and canister system to prepare a formulation of 2-3 mL of PRP for 116 patients who received the intervention. The PRP contained concentrated platelets and concentrated white blood cells at a concentration five to six times greater than in plasma at baseline.
Both the patients who received PRP and the 114 active controls were given a local anesthesia block of 0.25% bupivacaine with epinephrine before investigators needled the origin of their extensor tendons, delivering the PRP only to the intervention group.
At 12 weeks’ follow-up, patients receiving the PRP injections reported 55.1% improvement in their pain scores, compared with their baseline pain before the procedure, whereas controls reported 47.4% improvement in pain compared with baseline. The findings were not statistically significant (P = .094). The 12-week secondary outcome measurement was statistically significant, with 37.4% of the intervention group reporting significant elbow tenderness, compared with 48.4% of controls reporting significant tenderness (P = .036).
At 24 weeks, the difference in pain scores between the two groups was statistically significant: PRP patients reported 71.5% improvement, whereas controls reported 56.1% improvement (P = .027). Similarly, significant elbow tenderness remained in 29.1% of PRP patients and 54% of the controls (P less than .001).
The two previous trials, one led by Dr. Mishra with a mean 25.6-month follow-up, and another 2-year study, used the same methodology and PRP system as this one and showed similar improvements, said Dr. Mishra. "Together these studies have treated 350 patients in a prospective, controlled fashion with all of the studies showing superiority when patients are treated with PRP," he said.
However, PRP treatment should not be used as a first-line therapy, he said. "Most patients will respond to conservative treatment such as exercise and rest," Dr. Mishra said. "PRP should, however, be used instead of cortisone for patients who have failed initial treatment."
The investigators noted that there are several potential mechanisms by which the PRP helps improve the pain in tennis elbow. Preclinical studies have shown that PRP can improve cell proliferation and others have shown it improves local blood flow, Dr. Mishra said. "Finally, it may be possible that PRP modifies neurogenic pain receptors and thereby improves clinical outcomes," he said. "More research is clearly needed in this area."
As with the other two studies, no significant complications were reported among the participants in this study, the investigators found. "Importantly, these studies were conducted over the course of a decade with an excellent safety profile for PRP," Dr. Mishra said. "Clinicians and patients can now be confident when using this specific form of PRP to treat chronic tennis elbow."
The study was funded by Biomet Biologics. All authors have received funding from a range of industry sources, including Biomet.
* Correction, 3/28/13: Dr. Mishra's affiliation has been corrected and not all of the investigators were from the same institution.
Platelet-rich plasma therapy improved both the pain scores and elbow tenderness for almost three-quarters of patients suffering from tennis elbow during a 6-month randomized, double-blind controlled trial.
This study is the third to show a treatment response with no significant complications in patients with lateral epicondylar tendinopathy, commonly known as tennis elbow, from platelet-rich plasma (PRP) injections.
Dr. Allan Mishra, of Stanford (Calif.) University Medical Center,* and his coinvestigators from eight other institutions presented their findings from the trial at the annual meeting of the American Academy of Orthopaedic Surgeons in Chicago.
The 230 study participants had symptoms for at least 3 months and reported tenderness at the lateral epicondyle and pain scored at a minimum of 50 out of 100 on a visual analog scale during a resisted wrist extension. All participants failed to respond to conventional therapy, including a combination of physical therapy, nonsteroidal anti-inflammatory medications, and/or steroid injections, the investigators reported.
Dr. Mishra and his colleagues used a Biomet GPS centrifuge and canister system to prepare a formulation of 2-3 mL of PRP for 116 patients who received the intervention. The PRP contained concentrated platelets and concentrated white blood cells at a concentration five to six times greater than in plasma at baseline.
Both the patients who received PRP and the 114 active controls were given a local anesthesia block of 0.25% bupivacaine with epinephrine before investigators needled the origin of their extensor tendons, delivering the PRP only to the intervention group.
At 12 weeks’ follow-up, patients receiving the PRP injections reported 55.1% improvement in their pain scores, compared with their baseline pain before the procedure, whereas controls reported 47.4% improvement in pain compared with baseline. The findings were not statistically significant (P = .094). The 12-week secondary outcome measurement was statistically significant, with 37.4% of the intervention group reporting significant elbow tenderness, compared with 48.4% of controls reporting significant tenderness (P = .036).
At 24 weeks, the difference in pain scores between the two groups was statistically significant: PRP patients reported 71.5% improvement, whereas controls reported 56.1% improvement (P = .027). Similarly, significant elbow tenderness remained in 29.1% of PRP patients and 54% of the controls (P less than .001).
The two previous trials, one led by Dr. Mishra with a mean 25.6-month follow-up, and another 2-year study, used the same methodology and PRP system as this one and showed similar improvements, said Dr. Mishra. "Together these studies have treated 350 patients in a prospective, controlled fashion with all of the studies showing superiority when patients are treated with PRP," he said.
However, PRP treatment should not be used as a first-line therapy, he said. "Most patients will respond to conservative treatment such as exercise and rest," Dr. Mishra said. "PRP should, however, be used instead of cortisone for patients who have failed initial treatment."
The investigators noted that there are several potential mechanisms by which the PRP helps improve the pain in tennis elbow. Preclinical studies have shown that PRP can improve cell proliferation and others have shown it improves local blood flow, Dr. Mishra said. "Finally, it may be possible that PRP modifies neurogenic pain receptors and thereby improves clinical outcomes," he said. "More research is clearly needed in this area."
As with the other two studies, no significant complications were reported among the participants in this study, the investigators found. "Importantly, these studies were conducted over the course of a decade with an excellent safety profile for PRP," Dr. Mishra said. "Clinicians and patients can now be confident when using this specific form of PRP to treat chronic tennis elbow."
The study was funded by Biomet Biologics. All authors have received funding from a range of industry sources, including Biomet.
* Correction, 3/28/13: Dr. Mishra's affiliation has been corrected and not all of the investigators were from the same institution.
Platelet-rich plasma therapy improved both the pain scores and elbow tenderness for almost three-quarters of patients suffering from tennis elbow during a 6-month randomized, double-blind controlled trial.
This study is the third to show a treatment response with no significant complications in patients with lateral epicondylar tendinopathy, commonly known as tennis elbow, from platelet-rich plasma (PRP) injections.
Dr. Allan Mishra, of Stanford (Calif.) University Medical Center,* and his coinvestigators from eight other institutions presented their findings from the trial at the annual meeting of the American Academy of Orthopaedic Surgeons in Chicago.
The 230 study participants had symptoms for at least 3 months and reported tenderness at the lateral epicondyle and pain scored at a minimum of 50 out of 100 on a visual analog scale during a resisted wrist extension. All participants failed to respond to conventional therapy, including a combination of physical therapy, nonsteroidal anti-inflammatory medications, and/or steroid injections, the investigators reported.
Dr. Mishra and his colleagues used a Biomet GPS centrifuge and canister system to prepare a formulation of 2-3 mL of PRP for 116 patients who received the intervention. The PRP contained concentrated platelets and concentrated white blood cells at a concentration five to six times greater than in plasma at baseline.
Both the patients who received PRP and the 114 active controls were given a local anesthesia block of 0.25% bupivacaine with epinephrine before investigators needled the origin of their extensor tendons, delivering the PRP only to the intervention group.
At 12 weeks’ follow-up, patients receiving the PRP injections reported 55.1% improvement in their pain scores, compared with their baseline pain before the procedure, whereas controls reported 47.4% improvement in pain compared with baseline. The findings were not statistically significant (P = .094). The 12-week secondary outcome measurement was statistically significant, with 37.4% of the intervention group reporting significant elbow tenderness, compared with 48.4% of controls reporting significant tenderness (P = .036).
At 24 weeks, the difference in pain scores between the two groups was statistically significant: PRP patients reported 71.5% improvement, whereas controls reported 56.1% improvement (P = .027). Similarly, significant elbow tenderness remained in 29.1% of PRP patients and 54% of the controls (P less than .001).
The two previous trials, one led by Dr. Mishra with a mean 25.6-month follow-up, and another 2-year study, used the same methodology and PRP system as this one and showed similar improvements, said Dr. Mishra. "Together these studies have treated 350 patients in a prospective, controlled fashion with all of the studies showing superiority when patients are treated with PRP," he said.
However, PRP treatment should not be used as a first-line therapy, he said. "Most patients will respond to conservative treatment such as exercise and rest," Dr. Mishra said. "PRP should, however, be used instead of cortisone for patients who have failed initial treatment."
The investigators noted that there are several potential mechanisms by which the PRP helps improve the pain in tennis elbow. Preclinical studies have shown that PRP can improve cell proliferation and others have shown it improves local blood flow, Dr. Mishra said. "Finally, it may be possible that PRP modifies neurogenic pain receptors and thereby improves clinical outcomes," he said. "More research is clearly needed in this area."
As with the other two studies, no significant complications were reported among the participants in this study, the investigators found. "Importantly, these studies were conducted over the course of a decade with an excellent safety profile for PRP," Dr. Mishra said. "Clinicians and patients can now be confident when using this specific form of PRP to treat chronic tennis elbow."
The study was funded by Biomet Biologics. All authors have received funding from a range of industry sources, including Biomet.
* Correction, 3/28/13: Dr. Mishra's affiliation has been corrected and not all of the investigators were from the same institution.
Major finding: Injections of platelet-rich plasma for tennis elbow sufferers produced a 71.5% improvement in pain scores, compared with the 56.1% improvement in an active control group at 24 weeks (P = .027).
Data source: A 24-week multicenter, randomized, controlled double-blind trial of 230 patients with lateral epicondylar tendinopathy who had failed to respond to a combination of physical therapy, nonsteroidal anti-inflammatory medications, and/or steroid injections.
Disclosures: The study was funded by Biomet Biologics. All authors have received funding from a range of industry sources, including Biomet.
Only 11% of health plan payments are value based
WASHINGTON – Only about 11% of health plan payments to physicians and hospitals are tied to performance or efficiency – meaning that almost 90% of payments are still fee for service, according to a report released March 26 by Catalyst for Payment Reform.
The San Francisco–based nonprofit is a collaborative of employers and health plans that advocates the overhaul of the nation’s health care payment infrastructure by encouraging more value-based payment.
Using data provided by commercial health plans, the group determined that 11% of hospital payments, 6% of outpatient specialist payments, and 6% of primary care physician payments are "value oriented."
Of those payment arrangements, 57% involve provider risk such as bundled payment, capitation, and shared risk payment. The remaining 43% provide incentives, such as shared savings or pay for performance.
The main goal of Catalyst for Payment Reform (CPR) is to raise the volume of value-based commercial payments to health care providers to 20% by 2020. Coalition members said that they saw reason for both pessimism and optimism in the report’s findings.
"Obviously, these results are pretty disappointing," said Dr. Robert Galvin, chief executive officer of Equity Healthcare, which buys health care coverage for private equity companies. Even so, the report itself represents "the triumph of transparency," he said at the press briefing. "It is just simply good to know."
Susan Delbanco, executive director of CPR, noted that in 2010, 1%-3% of provider payments were tied to performance. Given the latest information, "it looks to me like we are on a fast track and that we may get there before 2020,"she said.
The group's research also found that about 2% of health plan enrollees are enrolled in an accountable care organization or a patient-centered medical home.
Most health plan payments (about 75%) are still made to specialists, while 25% go to primary care physicians, according to their analysis. Non–fee-for-service payments are still not entirely rewarding or providing incentives to improve the quality of care. Only 35% of those value-based payments have quality of care as a factor.
Dr. Richard Gilfillan, director of the Center for Medicare and Medicaid Innovation at the Centers for Medicare and Medicaid Services, said that the agency was "thrilled" with the report, noting that it showed that private payers were helping encourage a transformation in payment.
"We’re not discouraged – we think that change is happening, it’s underway," Dr. Gilfillan said at the press briefing.
The growing number of physicians participating in new payment models reflects a cultural shift, said Dr. Mark Smith, president and chief executive officer of the California HealthCare Foundation. "I think we have turned the corner on providers recognizing the feasibility, the desirability, and in fact, the inevitability of the kinds of payment reforms that you’ve heard about."
The California HealthCare Foundation and the Commonwealth Fund provided the funding for the National Scorecard on Payment Reform, and a sister effort, the National Compendium on Payment Reform.
The scorecard tabulated data that 57 health plans provided to the National Business Coalition on Health. Participation is voluntary, and not all 57 plans answered all questions posed. The plans represent 104 million people in the commercial group market, or about two-thirds of the total commercially insured population in the United States. Respondents were primarily large health plans, which means the results may not necessarily reflect the entire group market.
On Twitter @aliciaault
WASHINGTON – Only about 11% of health plan payments to physicians and hospitals are tied to performance or efficiency – meaning that almost 90% of payments are still fee for service, according to a report released March 26 by Catalyst for Payment Reform.
The San Francisco–based nonprofit is a collaborative of employers and health plans that advocates the overhaul of the nation’s health care payment infrastructure by encouraging more value-based payment.
Using data provided by commercial health plans, the group determined that 11% of hospital payments, 6% of outpatient specialist payments, and 6% of primary care physician payments are "value oriented."
Of those payment arrangements, 57% involve provider risk such as bundled payment, capitation, and shared risk payment. The remaining 43% provide incentives, such as shared savings or pay for performance.
The main goal of Catalyst for Payment Reform (CPR) is to raise the volume of value-based commercial payments to health care providers to 20% by 2020. Coalition members said that they saw reason for both pessimism and optimism in the report’s findings.
"Obviously, these results are pretty disappointing," said Dr. Robert Galvin, chief executive officer of Equity Healthcare, which buys health care coverage for private equity companies. Even so, the report itself represents "the triumph of transparency," he said at the press briefing. "It is just simply good to know."
Susan Delbanco, executive director of CPR, noted that in 2010, 1%-3% of provider payments were tied to performance. Given the latest information, "it looks to me like we are on a fast track and that we may get there before 2020,"she said.
The group's research also found that about 2% of health plan enrollees are enrolled in an accountable care organization or a patient-centered medical home.
Most health plan payments (about 75%) are still made to specialists, while 25% go to primary care physicians, according to their analysis. Non–fee-for-service payments are still not entirely rewarding or providing incentives to improve the quality of care. Only 35% of those value-based payments have quality of care as a factor.
Dr. Richard Gilfillan, director of the Center for Medicare and Medicaid Innovation at the Centers for Medicare and Medicaid Services, said that the agency was "thrilled" with the report, noting that it showed that private payers were helping encourage a transformation in payment.
"We’re not discouraged – we think that change is happening, it’s underway," Dr. Gilfillan said at the press briefing.
The growing number of physicians participating in new payment models reflects a cultural shift, said Dr. Mark Smith, president and chief executive officer of the California HealthCare Foundation. "I think we have turned the corner on providers recognizing the feasibility, the desirability, and in fact, the inevitability of the kinds of payment reforms that you’ve heard about."
The California HealthCare Foundation and the Commonwealth Fund provided the funding for the National Scorecard on Payment Reform, and a sister effort, the National Compendium on Payment Reform.
The scorecard tabulated data that 57 health plans provided to the National Business Coalition on Health. Participation is voluntary, and not all 57 plans answered all questions posed. The plans represent 104 million people in the commercial group market, or about two-thirds of the total commercially insured population in the United States. Respondents were primarily large health plans, which means the results may not necessarily reflect the entire group market.
On Twitter @aliciaault
WASHINGTON – Only about 11% of health plan payments to physicians and hospitals are tied to performance or efficiency – meaning that almost 90% of payments are still fee for service, according to a report released March 26 by Catalyst for Payment Reform.
The San Francisco–based nonprofit is a collaborative of employers and health plans that advocates the overhaul of the nation’s health care payment infrastructure by encouraging more value-based payment.
Using data provided by commercial health plans, the group determined that 11% of hospital payments, 6% of outpatient specialist payments, and 6% of primary care physician payments are "value oriented."
Of those payment arrangements, 57% involve provider risk such as bundled payment, capitation, and shared risk payment. The remaining 43% provide incentives, such as shared savings or pay for performance.
The main goal of Catalyst for Payment Reform (CPR) is to raise the volume of value-based commercial payments to health care providers to 20% by 2020. Coalition members said that they saw reason for both pessimism and optimism in the report’s findings.
"Obviously, these results are pretty disappointing," said Dr. Robert Galvin, chief executive officer of Equity Healthcare, which buys health care coverage for private equity companies. Even so, the report itself represents "the triumph of transparency," he said at the press briefing. "It is just simply good to know."
Susan Delbanco, executive director of CPR, noted that in 2010, 1%-3% of provider payments were tied to performance. Given the latest information, "it looks to me like we are on a fast track and that we may get there before 2020,"she said.
The group's research also found that about 2% of health plan enrollees are enrolled in an accountable care organization or a patient-centered medical home.
Most health plan payments (about 75%) are still made to specialists, while 25% go to primary care physicians, according to their analysis. Non–fee-for-service payments are still not entirely rewarding or providing incentives to improve the quality of care. Only 35% of those value-based payments have quality of care as a factor.
Dr. Richard Gilfillan, director of the Center for Medicare and Medicaid Innovation at the Centers for Medicare and Medicaid Services, said that the agency was "thrilled" with the report, noting that it showed that private payers were helping encourage a transformation in payment.
"We’re not discouraged – we think that change is happening, it’s underway," Dr. Gilfillan said at the press briefing.
The growing number of physicians participating in new payment models reflects a cultural shift, said Dr. Mark Smith, president and chief executive officer of the California HealthCare Foundation. "I think we have turned the corner on providers recognizing the feasibility, the desirability, and in fact, the inevitability of the kinds of payment reforms that you’ve heard about."
The California HealthCare Foundation and the Commonwealth Fund provided the funding for the National Scorecard on Payment Reform, and a sister effort, the National Compendium on Payment Reform.
The scorecard tabulated data that 57 health plans provided to the National Business Coalition on Health. Participation is voluntary, and not all 57 plans answered all questions posed. The plans represent 104 million people in the commercial group market, or about two-thirds of the total commercially insured population in the United States. Respondents were primarily large health plans, which means the results may not necessarily reflect the entire group market.
On Twitter @aliciaault
'Liberation therapy' may make MS worse
SAN DIEGO – Percutaneous transluminal venous angioplasty – also known as "liberation therapy" – doesn’t help people with multiple sclerosis and may increase MS brain activity in the short term, according to a small, randomized, sham-controlled trial from the State University of New York at Buffalo, the first randomized trial to investigate the procedure.
It "was ineffective in correcting" chronic cerebrospinal venous insufficiency (CCSVI), the recently described condition it targets. "The results ... caution against widespread adoption of venous angioplasty in the management of patients with MS outside of rigorous clinical trials," the investigators concluded.
The findings follow a recent Food and Drug Administration warning that PTVA (percutaneous transluminal venous angioplasty) can cause deaths and injuries, including strokes, damage to the treated vein, blood clots, cranial nerve damage, abdominal bleeding, and detachment and migration of stents.
The idea is to use balloon angioplasty and stents to widen veins in the chests and necks that appear to be narrowed in some MS patients. Proponents of the procedure say that those narrowed veins impair blood flow and lead to disease progression. The researchers who discovered the problem dubbed it CCSVI. A cottage industry has since sprung up to offer PTVA to MS patients.
The FDA noted in its warning that there have been no "controlled ... rigorously conducted, properly targeted" studies of the issue; that may have changed when Dr. Robert Zivadinov, a professor in the department of neurology at SUNY-Buffalo, presented his team’s findings at the annual meeting of the American Academy of Neurology.
"When you reopened those veins in the neck, I think something happened in reperfusing the brain and re-exacerbating disease activity. The message of this is clear. The majority of patients who are relapsing-remitting should not undergo this treatment," he said in an interview.
Ten patients got PTVA in the first phase of the study. The second phase randomized 9 to PTVA and 10 to a sham intervention. Most had relapsing-remitting MS.
There were no MS relapses in the first phase, but PTVA patients had more relapses (4 vs. 1; P = .389) and more MRI disease activity (cumulative number of new contrast-enhancing lesions (19 vs. 3; P = .062) and new T2 lesions (17 vs. 3; P = .066) in the 6 months following treatment in phase II.
PTVA patients also didn’t fare any better on Expanded Disability Status Scale (EDSS) scores, Multiple Sclerosis Functional Composite scores, 6-minute walk tests, or measures of cognition and quality of life.
"We chose very active patients who had one relapse in the previous year or [gadolinium-] enhancing lesions in the 3 months before. The sample size is small, but [more than half] of patients in the treatment group showed increased activity," Dr. Zivadinov said.
The majority of the subjects were women. On average, they were about 45 years old, had been diagnosed with MS for 11 years, and were mildly to moderately disabled (mean EDSS score about 4). Most were on interferon, glatiramer acetate, or both.
Venous angioplasty didn’t cause any serious complications, and it restored venous outflow to at least 50% of normal in most patients. Phase I patients had a better than 75% improvement overall. Phase II patients had less benefit; there were no differences in venous hemodynamic insufficiency scores between treated and sham patients.
The treatment "failed to provide any sustained improvement in venous outflow as measured through duplex and/or clinical and MRI outcomes," and "more sizable changes in venous outflow [were] associated with increased disease activity primarily noted on MRI," Dr. Zivadinov and his colleagues concluded.
The work was funded primarily by SUNY-Buffalo’s Neuroimaging Analysis Center and Baird MS Research Center. Dr. Zivadinov receives personal compensation from Teva Pharmaceuticals, Biogen Idec, EMD Serono, Bayer, Genzyme-Sanofi, Novartis, Bracco Imaging, and Questcor Pharmaceuticals.
SAN DIEGO – Percutaneous transluminal venous angioplasty – also known as "liberation therapy" – doesn’t help people with multiple sclerosis and may increase MS brain activity in the short term, according to a small, randomized, sham-controlled trial from the State University of New York at Buffalo, the first randomized trial to investigate the procedure.
It "was ineffective in correcting" chronic cerebrospinal venous insufficiency (CCSVI), the recently described condition it targets. "The results ... caution against widespread adoption of venous angioplasty in the management of patients with MS outside of rigorous clinical trials," the investigators concluded.
The findings follow a recent Food and Drug Administration warning that PTVA (percutaneous transluminal venous angioplasty) can cause deaths and injuries, including strokes, damage to the treated vein, blood clots, cranial nerve damage, abdominal bleeding, and detachment and migration of stents.
The idea is to use balloon angioplasty and stents to widen veins in the chests and necks that appear to be narrowed in some MS patients. Proponents of the procedure say that those narrowed veins impair blood flow and lead to disease progression. The researchers who discovered the problem dubbed it CCSVI. A cottage industry has since sprung up to offer PTVA to MS patients.
The FDA noted in its warning that there have been no "controlled ... rigorously conducted, properly targeted" studies of the issue; that may have changed when Dr. Robert Zivadinov, a professor in the department of neurology at SUNY-Buffalo, presented his team’s findings at the annual meeting of the American Academy of Neurology.
"When you reopened those veins in the neck, I think something happened in reperfusing the brain and re-exacerbating disease activity. The message of this is clear. The majority of patients who are relapsing-remitting should not undergo this treatment," he said in an interview.
Ten patients got PTVA in the first phase of the study. The second phase randomized 9 to PTVA and 10 to a sham intervention. Most had relapsing-remitting MS.
There were no MS relapses in the first phase, but PTVA patients had more relapses (4 vs. 1; P = .389) and more MRI disease activity (cumulative number of new contrast-enhancing lesions (19 vs. 3; P = .062) and new T2 lesions (17 vs. 3; P = .066) in the 6 months following treatment in phase II.
PTVA patients also didn’t fare any better on Expanded Disability Status Scale (EDSS) scores, Multiple Sclerosis Functional Composite scores, 6-minute walk tests, or measures of cognition and quality of life.
"We chose very active patients who had one relapse in the previous year or [gadolinium-] enhancing lesions in the 3 months before. The sample size is small, but [more than half] of patients in the treatment group showed increased activity," Dr. Zivadinov said.
The majority of the subjects were women. On average, they were about 45 years old, had been diagnosed with MS for 11 years, and were mildly to moderately disabled (mean EDSS score about 4). Most were on interferon, glatiramer acetate, or both.
Venous angioplasty didn’t cause any serious complications, and it restored venous outflow to at least 50% of normal in most patients. Phase I patients had a better than 75% improvement overall. Phase II patients had less benefit; there were no differences in venous hemodynamic insufficiency scores between treated and sham patients.
The treatment "failed to provide any sustained improvement in venous outflow as measured through duplex and/or clinical and MRI outcomes," and "more sizable changes in venous outflow [were] associated with increased disease activity primarily noted on MRI," Dr. Zivadinov and his colleagues concluded.
The work was funded primarily by SUNY-Buffalo’s Neuroimaging Analysis Center and Baird MS Research Center. Dr. Zivadinov receives personal compensation from Teva Pharmaceuticals, Biogen Idec, EMD Serono, Bayer, Genzyme-Sanofi, Novartis, Bracco Imaging, and Questcor Pharmaceuticals.
SAN DIEGO – Percutaneous transluminal venous angioplasty – also known as "liberation therapy" – doesn’t help people with multiple sclerosis and may increase MS brain activity in the short term, according to a small, randomized, sham-controlled trial from the State University of New York at Buffalo, the first randomized trial to investigate the procedure.
It "was ineffective in correcting" chronic cerebrospinal venous insufficiency (CCSVI), the recently described condition it targets. "The results ... caution against widespread adoption of venous angioplasty in the management of patients with MS outside of rigorous clinical trials," the investigators concluded.
The findings follow a recent Food and Drug Administration warning that PTVA (percutaneous transluminal venous angioplasty) can cause deaths and injuries, including strokes, damage to the treated vein, blood clots, cranial nerve damage, abdominal bleeding, and detachment and migration of stents.
The idea is to use balloon angioplasty and stents to widen veins in the chests and necks that appear to be narrowed in some MS patients. Proponents of the procedure say that those narrowed veins impair blood flow and lead to disease progression. The researchers who discovered the problem dubbed it CCSVI. A cottage industry has since sprung up to offer PTVA to MS patients.
The FDA noted in its warning that there have been no "controlled ... rigorously conducted, properly targeted" studies of the issue; that may have changed when Dr. Robert Zivadinov, a professor in the department of neurology at SUNY-Buffalo, presented his team’s findings at the annual meeting of the American Academy of Neurology.
"When you reopened those veins in the neck, I think something happened in reperfusing the brain and re-exacerbating disease activity. The message of this is clear. The majority of patients who are relapsing-remitting should not undergo this treatment," he said in an interview.
Ten patients got PTVA in the first phase of the study. The second phase randomized 9 to PTVA and 10 to a sham intervention. Most had relapsing-remitting MS.
There were no MS relapses in the first phase, but PTVA patients had more relapses (4 vs. 1; P = .389) and more MRI disease activity (cumulative number of new contrast-enhancing lesions (19 vs. 3; P = .062) and new T2 lesions (17 vs. 3; P = .066) in the 6 months following treatment in phase II.
PTVA patients also didn’t fare any better on Expanded Disability Status Scale (EDSS) scores, Multiple Sclerosis Functional Composite scores, 6-minute walk tests, or measures of cognition and quality of life.
"We chose very active patients who had one relapse in the previous year or [gadolinium-] enhancing lesions in the 3 months before. The sample size is small, but [more than half] of patients in the treatment group showed increased activity," Dr. Zivadinov said.
The majority of the subjects were women. On average, they were about 45 years old, had been diagnosed with MS for 11 years, and were mildly to moderately disabled (mean EDSS score about 4). Most were on interferon, glatiramer acetate, or both.
Venous angioplasty didn’t cause any serious complications, and it restored venous outflow to at least 50% of normal in most patients. Phase I patients had a better than 75% improvement overall. Phase II patients had less benefit; there were no differences in venous hemodynamic insufficiency scores between treated and sham patients.
The treatment "failed to provide any sustained improvement in venous outflow as measured through duplex and/or clinical and MRI outcomes," and "more sizable changes in venous outflow [were] associated with increased disease activity primarily noted on MRI," Dr. Zivadinov and his colleagues concluded.
The work was funded primarily by SUNY-Buffalo’s Neuroimaging Analysis Center and Baird MS Research Center. Dr. Zivadinov receives personal compensation from Teva Pharmaceuticals, Biogen Idec, EMD Serono, Bayer, Genzyme-Sanofi, Novartis, Bracco Imaging, and Questcor Pharmaceuticals.
AT THE 2013 AAN ANNUAL MEETING
Major finding: A total of 19 new contrast-enhancing MRI lesions were observed in 9 "liberation therapy" MS patients within 6 months of treatment, compared with 3 lesions in 10 control patients.
Date Source: A randomized, sham-controlled trial with 29 MS patients
Disclosures: The work was funded primarily by SUNY–Buffalo’s Neuroimaging Analysis Center and Baird MS Research Center. Dr. Zivadinov receives personal compensation from Teva Pharmaceuticals, Biogen Idec, EMD Serono, Bayer, Genzyme-Sanofi, Novartis, Bracco Imaging, and Questcor Pharmaceuticals.
Surgery may be avoided in early rectal cancer
NATIONAL HARBOR, MD. – It may sound like heresy, but select patients with locally advanced rectal cancer may be spared surgery and its associated complications, a cancer surgeon suggested at the annual Society of Surgical Oncology Cancer Symposium.
Approximately 10%-25% of patients with locally advanced rectal cancer will have clinical complete responses (cCR) to neoadjuvant chemotherapy and radiation, said Dr. Philip B. Paty, an attending surgeon in the colorectal surgery service at Memorial Sloan-Kettering Cancer Center in New York City.
"The vast majority of these patients will avoid rectal resection, at least within the first 5 years," Dr. Paty added.
Although local failure occurs in 10%-25% of patients, most of the failures occur within the first 18 months, and most of these cases can be salvaged with R0 resections. Patients treated with nonoperative management appear to have rates of distant recurrence and survival similar to those of patients with pathologic complete responses (pCR) treated with total mesorectal resection, he said.
If surgery is required, local excision may be sufficient for some patients with stage T1 lesions and a select few with T2 lesions, said Dr. Heidi Nelson, professor of surgery in the department of colon and rectal surgery at the Mayo Clinic in Rochester, Minn.
If a patient has a favorable T1 lesion and would otherwise face a life-altering procedure such as abdominal perineal resection (APR) and colostomy, the surgeon should at least show the patient the data and discuss local excision as a safe and effective alternative with results comparable to more extensive resections, she said.
T2 lesions are more problematic, but a select few patients with this tumor type might be spared the morbidity of standard rectal resection, she added.
Hold the surgery?
Dr. Paty noted that, with standard management of stage T3 or T4 rectal cancers, the combination of neoadjuvant chemoradiotherapy, surgery, and adjuvant chemotherapy resulted in a 76% overall survival rate with less than 0.3% local recurrence after 5 years (Ann. Surg. 2005;241:829-36).
"What we have not dwelt on much is the morbidity of surgery, which is very significant. Having a rectal resection is a life-changing event for every patient that has one. Surgeons know that, and patients know that even better than surgeons," he said.
Rectal resections are associated with significant perioperative morbidity, colostomy, altered bowel function, sexual dysfunction, and infertility, he noted.
Pathologic complete responses to neoadjuvant therapy occur in 10%-44% of patients, and patients who have a pCR have markedly better oncologic outcomes than patients with less robust responses.
Of course, pCR can only be determined after surgery, raising the question of whether a clinical CR is sufficient for determining whether a patient might be spared rectal resection.
There are currently more data on pCR in rectal cancer than cCR, "probably because clinical CR criteria right now are quite stringent; we don’t want to not operate on patients who have disease," Dr. Paty said.
His criteria for clinical complete response include a flat mucosa with no nodularity or mass on digital rectal examination. Smooth induration or minor scarring without nodularity is acceptable, "but it has to have a benign feel to it," he said.
In addition, on proctoscopy the mucosa must appear normal and flat, and if a scar is present it should be pale or white in appearance. Alternatively, there can be telangiectasias, he said.
"What’s not clear is whether ulceration is an exclusion criterion [for nonoperative management]. For me it is. Any time I see ulceration I feel there is something ongoing in that tumor that is not resolved and I don’t feel comfortable calling it a complete response," Dr. Paty commented.
Take local route
When surgery is required, local excision rather than total mesorectal resection may suffice, Dr. Nelson said. Suitable patients may be those who are frail or elderly or have limited life expectancy or serious medical conditions that might preclude more extensive surgery.
Tumors that may be good candidates for local excision include smaller lesions (less than 2-3 cm) below the peritoneal reflection that are not amenable to lower anterior resection. The tumors should be subject to full thickness excision, and the team should be able to confirm negative margins, she noted.
Favorable pathologic findings include well-differentiated tumors with the absence of lymphovascular invasion, mucinous features, or signet ring features, she said.
"Local excision really just takes care of the primary, of course. It doesn’t deal with the lymphatics, which is always the hidden game," Dr. Nelson said.
She noted that a 1989 study showed that the likelihood of untreated lymph node disease in patients who had undergone local excision was 0% for patients with T1 tumors, 28% for those with T2 tumors, 36% for T3, and 53% for T4 lesions, showing a significant increase in risk associated with tumor depth (Cancer 1989;63:1421-9).
"If you start tackling anything above a T2 lesion, you’re probably going to be missing lymphatic disease. It’s of relevance because it will form the site of recurrent disease," she said.
For patients with T1 tumors, overall survival is the same, but disease-free survival and local recurrence rates favor standard resection over local excision. "Selection criteria must be much more restrictive when it comes to a T2 lesion," Dr. Nelson said. "I’m pretty reticent to use it in my own practice. I have to really choose the tumor well and choose the patient well to want to do that with some assurance that it’s the right decision."
She pointed to a study published in 2000 comparing patients who underwent either local excision or standard resection for rectal cancer (Dis. Colon Rectum 2000;43:1064-71). Over about 4.5 years of follow-up, local recurrence for patients with T2 lesions was 47% if they had received local excision, compared with 6% for those who had standard resections. Respective overall survival rates were 65% and 81%.
Dr. Paty and Dr. Nelson reported having no financial disclosures.
NATIONAL HARBOR, MD. – It may sound like heresy, but select patients with locally advanced rectal cancer may be spared surgery and its associated complications, a cancer surgeon suggested at the annual Society of Surgical Oncology Cancer Symposium.
Approximately 10%-25% of patients with locally advanced rectal cancer will have clinical complete responses (cCR) to neoadjuvant chemotherapy and radiation, said Dr. Philip B. Paty, an attending surgeon in the colorectal surgery service at Memorial Sloan-Kettering Cancer Center in New York City.
"The vast majority of these patients will avoid rectal resection, at least within the first 5 years," Dr. Paty added.
Although local failure occurs in 10%-25% of patients, most of the failures occur within the first 18 months, and most of these cases can be salvaged with R0 resections. Patients treated with nonoperative management appear to have rates of distant recurrence and survival similar to those of patients with pathologic complete responses (pCR) treated with total mesorectal resection, he said.
If surgery is required, local excision may be sufficient for some patients with stage T1 lesions and a select few with T2 lesions, said Dr. Heidi Nelson, professor of surgery in the department of colon and rectal surgery at the Mayo Clinic in Rochester, Minn.
If a patient has a favorable T1 lesion and would otherwise face a life-altering procedure such as abdominal perineal resection (APR) and colostomy, the surgeon should at least show the patient the data and discuss local excision as a safe and effective alternative with results comparable to more extensive resections, she said.
T2 lesions are more problematic, but a select few patients with this tumor type might be spared the morbidity of standard rectal resection, she added.
Hold the surgery?
Dr. Paty noted that, with standard management of stage T3 or T4 rectal cancers, the combination of neoadjuvant chemoradiotherapy, surgery, and adjuvant chemotherapy resulted in a 76% overall survival rate with less than 0.3% local recurrence after 5 years (Ann. Surg. 2005;241:829-36).
"What we have not dwelt on much is the morbidity of surgery, which is very significant. Having a rectal resection is a life-changing event for every patient that has one. Surgeons know that, and patients know that even better than surgeons," he said.
Rectal resections are associated with significant perioperative morbidity, colostomy, altered bowel function, sexual dysfunction, and infertility, he noted.
Pathologic complete responses to neoadjuvant therapy occur in 10%-44% of patients, and patients who have a pCR have markedly better oncologic outcomes than patients with less robust responses.
Of course, pCR can only be determined after surgery, raising the question of whether a clinical CR is sufficient for determining whether a patient might be spared rectal resection.
There are currently more data on pCR in rectal cancer than cCR, "probably because clinical CR criteria right now are quite stringent; we don’t want to not operate on patients who have disease," Dr. Paty said.
His criteria for clinical complete response include a flat mucosa with no nodularity or mass on digital rectal examination. Smooth induration or minor scarring without nodularity is acceptable, "but it has to have a benign feel to it," he said.
In addition, on proctoscopy the mucosa must appear normal and flat, and if a scar is present it should be pale or white in appearance. Alternatively, there can be telangiectasias, he said.
"What’s not clear is whether ulceration is an exclusion criterion [for nonoperative management]. For me it is. Any time I see ulceration I feel there is something ongoing in that tumor that is not resolved and I don’t feel comfortable calling it a complete response," Dr. Paty commented.
Take local route
When surgery is required, local excision rather than total mesorectal resection may suffice, Dr. Nelson said. Suitable patients may be those who are frail or elderly or have limited life expectancy or serious medical conditions that might preclude more extensive surgery.
Tumors that may be good candidates for local excision include smaller lesions (less than 2-3 cm) below the peritoneal reflection that are not amenable to lower anterior resection. The tumors should be subject to full thickness excision, and the team should be able to confirm negative margins, she noted.
Favorable pathologic findings include well-differentiated tumors with the absence of lymphovascular invasion, mucinous features, or signet ring features, she said.
"Local excision really just takes care of the primary, of course. It doesn’t deal with the lymphatics, which is always the hidden game," Dr. Nelson said.
She noted that a 1989 study showed that the likelihood of untreated lymph node disease in patients who had undergone local excision was 0% for patients with T1 tumors, 28% for those with T2 tumors, 36% for T3, and 53% for T4 lesions, showing a significant increase in risk associated with tumor depth (Cancer 1989;63:1421-9).
"If you start tackling anything above a T2 lesion, you’re probably going to be missing lymphatic disease. It’s of relevance because it will form the site of recurrent disease," she said.
For patients with T1 tumors, overall survival is the same, but disease-free survival and local recurrence rates favor standard resection over local excision. "Selection criteria must be much more restrictive when it comes to a T2 lesion," Dr. Nelson said. "I’m pretty reticent to use it in my own practice. I have to really choose the tumor well and choose the patient well to want to do that with some assurance that it’s the right decision."
She pointed to a study published in 2000 comparing patients who underwent either local excision or standard resection for rectal cancer (Dis. Colon Rectum 2000;43:1064-71). Over about 4.5 years of follow-up, local recurrence for patients with T2 lesions was 47% if they had received local excision, compared with 6% for those who had standard resections. Respective overall survival rates were 65% and 81%.
Dr. Paty and Dr. Nelson reported having no financial disclosures.
NATIONAL HARBOR, MD. – It may sound like heresy, but select patients with locally advanced rectal cancer may be spared surgery and its associated complications, a cancer surgeon suggested at the annual Society of Surgical Oncology Cancer Symposium.
Approximately 10%-25% of patients with locally advanced rectal cancer will have clinical complete responses (cCR) to neoadjuvant chemotherapy and radiation, said Dr. Philip B. Paty, an attending surgeon in the colorectal surgery service at Memorial Sloan-Kettering Cancer Center in New York City.
"The vast majority of these patients will avoid rectal resection, at least within the first 5 years," Dr. Paty added.
Although local failure occurs in 10%-25% of patients, most of the failures occur within the first 18 months, and most of these cases can be salvaged with R0 resections. Patients treated with nonoperative management appear to have rates of distant recurrence and survival similar to those of patients with pathologic complete responses (pCR) treated with total mesorectal resection, he said.
If surgery is required, local excision may be sufficient for some patients with stage T1 lesions and a select few with T2 lesions, said Dr. Heidi Nelson, professor of surgery in the department of colon and rectal surgery at the Mayo Clinic in Rochester, Minn.
If a patient has a favorable T1 lesion and would otherwise face a life-altering procedure such as abdominal perineal resection (APR) and colostomy, the surgeon should at least show the patient the data and discuss local excision as a safe and effective alternative with results comparable to more extensive resections, she said.
T2 lesions are more problematic, but a select few patients with this tumor type might be spared the morbidity of standard rectal resection, she added.
Hold the surgery?
Dr. Paty noted that, with standard management of stage T3 or T4 rectal cancers, the combination of neoadjuvant chemoradiotherapy, surgery, and adjuvant chemotherapy resulted in a 76% overall survival rate with less than 0.3% local recurrence after 5 years (Ann. Surg. 2005;241:829-36).
"What we have not dwelt on much is the morbidity of surgery, which is very significant. Having a rectal resection is a life-changing event for every patient that has one. Surgeons know that, and patients know that even better than surgeons," he said.
Rectal resections are associated with significant perioperative morbidity, colostomy, altered bowel function, sexual dysfunction, and infertility, he noted.
Pathologic complete responses to neoadjuvant therapy occur in 10%-44% of patients, and patients who have a pCR have markedly better oncologic outcomes than patients with less robust responses.
Of course, pCR can only be determined after surgery, raising the question of whether a clinical CR is sufficient for determining whether a patient might be spared rectal resection.
There are currently more data on pCR in rectal cancer than cCR, "probably because clinical CR criteria right now are quite stringent; we don’t want to not operate on patients who have disease," Dr. Paty said.
His criteria for clinical complete response include a flat mucosa with no nodularity or mass on digital rectal examination. Smooth induration or minor scarring without nodularity is acceptable, "but it has to have a benign feel to it," he said.
In addition, on proctoscopy the mucosa must appear normal and flat, and if a scar is present it should be pale or white in appearance. Alternatively, there can be telangiectasias, he said.
"What’s not clear is whether ulceration is an exclusion criterion [for nonoperative management]. For me it is. Any time I see ulceration I feel there is something ongoing in that tumor that is not resolved and I don’t feel comfortable calling it a complete response," Dr. Paty commented.
Take local route
When surgery is required, local excision rather than total mesorectal resection may suffice, Dr. Nelson said. Suitable patients may be those who are frail or elderly or have limited life expectancy or serious medical conditions that might preclude more extensive surgery.
Tumors that may be good candidates for local excision include smaller lesions (less than 2-3 cm) below the peritoneal reflection that are not amenable to lower anterior resection. The tumors should be subject to full thickness excision, and the team should be able to confirm negative margins, she noted.
Favorable pathologic findings include well-differentiated tumors with the absence of lymphovascular invasion, mucinous features, or signet ring features, she said.
"Local excision really just takes care of the primary, of course. It doesn’t deal with the lymphatics, which is always the hidden game," Dr. Nelson said.
She noted that a 1989 study showed that the likelihood of untreated lymph node disease in patients who had undergone local excision was 0% for patients with T1 tumors, 28% for those with T2 tumors, 36% for T3, and 53% for T4 lesions, showing a significant increase in risk associated with tumor depth (Cancer 1989;63:1421-9).
"If you start tackling anything above a T2 lesion, you’re probably going to be missing lymphatic disease. It’s of relevance because it will form the site of recurrent disease," she said.
For patients with T1 tumors, overall survival is the same, but disease-free survival and local recurrence rates favor standard resection over local excision. "Selection criteria must be much more restrictive when it comes to a T2 lesion," Dr. Nelson said. "I’m pretty reticent to use it in my own practice. I have to really choose the tumor well and choose the patient well to want to do that with some assurance that it’s the right decision."
She pointed to a study published in 2000 comparing patients who underwent either local excision or standard resection for rectal cancer (Dis. Colon Rectum 2000;43:1064-71). Over about 4.5 years of follow-up, local recurrence for patients with T2 lesions was 47% if they had received local excision, compared with 6% for those who had standard resections. Respective overall survival rates were 65% and 81%.
Dr. Paty and Dr. Nelson reported having no financial disclosures.
EXPERT ANALYSIS FROM SSO 2013
Advancements in robotic hysterectomy
Robotic-assisted surgery has been both celebrated as "revolutionary" and defamed as a "crutch." No matter where your loyalties lie in this debate, what is not debatable is the dramatic increase in minimally invasive surgery (MIS) rates for hysterectomy since robotic-assisted surgery was approved for gynecology in 2005. Rates vary across samples and sources, but according to 2011 data from Solucient and 2010 data from the Agency for Healthcare Research and Quality, approximately 27% of hysterectomies are performed with the robot, 26% with standard laparoscopy, and 12% vaginally.
It should be clear to all in 2013 that a total abdominal hysterectomy approach (TAH) is the least favored route for hysterectomy in terms of global cost, invasiveness, and overall complication rate. Therefore, as the AAGL has stated, we should all strive to improve our MIS skill-set – whether it is by the vaginal, laparoscopic, or robotic-assisted approach (J. Minim. Invasive Gynecol. 2011;18:1-3).
Personally, I prefer robotic-assisted techniques. As a community gynecologist, I believe that the marriage of high-tech computerization with the surgical sciences allows for more reproducibility than the traditional vaginal or laparoscopic approaches (J. Minim. Invasive Gynecol. 2008;15:286-91; Obstet. Gynecol. 2010;115:535-42).
In my experience, there are now three reproducible techniques for performing robotic-assisted hysterectomy. The first is a robotic total laparoscopic hysterectomy (TLH) technique involving 4-5 ports, which incorporates some of the steps familiar to surgeons performing TAH. This approach was initially described by Dr. Charles Koh after the advent of the Koh colpotomizer (J. Am. Assoc. Gynecol. Laparosc. 1998;5:187-92) and was then modified and adapted to the robotic platform with my colleagues at the Ochsner Clinic in Louisiana.
The second is a reduced two-port technique that was developed last year with my colleagues at the Texas Institute for Robotic Surgery in Austin.
Last, clearance by the Food and Drug Administration in February 2013 for a da Vinci single-site instrumentation package for use in benign hysterectomy and salpingo-oophorectomy makes the single-site technique a third reproducible approach for performing hysterectomy with the robotic platform. Use of the instrumentation package is currently being launched at Celebration Health Florida Hospital, the Cleveland Clinic, Newark (N.J.) Beth Israel Medical Center, and the Texas Institute for Robotic Surgery.
In addition to being more reproducible, the robotic route to hysterectomy now affords a "see-and-treat" approach, by which we can insert an endoscopic camera, assess the difficulty of the operation (pathology, uterine size, adhesions, etc.), and then select the robotic technique that is best for the patient.
Multisite technique
In positioning the patient, precautions are taken to prevent patient slippage on the operating table during steep Trendelenburg. Most commonly, we place a gel pad or egg crate mattress directly onto the operating table, secure it with tape, and follow with direct placement of the patient onto the gel pad or egg crate. The patient’s arms are then padded and tucked by the sides and the legs are placed in Allen stirrups.
The actual procedure is begun by placing the uterine manipulator of choice. I prefer the RUMI II System with articulating tip or the Advincula Arch with the Koh colpotomizer ring (CooperSurgical, Trumball, Conn.). Other popular options are the VCare manipulator with cup (ConMed Endosurgery, Utica, N.Y.) and the McCarus-Volker Fornisee (LSI Solutions, Victor, N.Y.).
The vaginal pneumo-occlusion balloon can be placed on all three manipulators and is critical for maintaining the pneumoperitoneum that allows for the success of this technique. The importance of properly placing the uterine manipulator of your choice cannot be overemphasized.
For insufflation, I use a Veress needle placed intraumbilically or in the left upper quadrant (LUQ), depending on the patient’s surgical history. The LUQ is preferred if the patient has a history of a prior midline incision. (The stomach must be desufflated first.) The intraumbilical approach is preferred if the patient has a history of LUQ or bariatric surgery.
For port placement, the 8-mm camera port can be placed 8-10 cm above the fundus of the uterus when pushed cephalad on examination under anesthesia (EUA). The robotic camera or a separate camera with a 5-mm laparoscope is introduced (hand-held), and a four-quadrant inspection is undertaken. Direct visualization is used to place two or three additional 8-mm ports in an arch configuration. An 8-mm assistant port is placed on the patient’s side opposite the surgeon’s dominant hand. All ports are spaced 8-10 cm away from each other.
The patient is placed in sufficiently steep Trendelenburg to allow the small bowel to be displaced from the pelvis. The surgical cart is straight docked between the patient’s legs or side docked on the surgeon’s dominant hand side. The 8-mm camera is placed into the camera arm, and then two or three (per the surgeon’s preference) 8-mm robotic instruments are placed under direct visualization.
I prefer to use three instruments during the procedure: the fenestrated bipolar grasper, the monopolar scissors, and the mega suture-cut needle driver.
The ureters are identified. Retroperitoneal dissection is utilized to confirm the ureteral path if needed. Depending on the patient’s desires and history, salpingectomy may be performed.
Isolation and transection of the infundibulopelvic ligaments or the utero-ovarian ligaments are then undertaken. The dissection is carried to the middle of the round ligament, well away from the uterus (where you would place suture when performing TAH). The round ligament is transected, allowing the anterior and posterior leaves of the broad ligament to separate and be visualized. These initial steps will secure two of the four main blood supplies, avoid early uterine artery bleeding, and maximize uterine mobility with larger uteri.
To outline the bladder flap, the location of the Koh ring, VCare cup, or McCarus-Volker Fornisee at the cervicovaginal junction should be noted and used as a general target. The bladder is then filled through the Foley to confirm its location and is then emptied. The anterior leaf of the broad ligament is then picked up and tented with the fenestrated bipolar grasper.
The monopolar scissors are employed to incise the anterior leaf from where the round ligament was transected to the area just cephalad of the cervicovaginal ring and the border of the bladder, in a fashion similar to TAH. Each of these steps is performed bilaterally.
Next, in preparation for the anterior colpotomy, further development of the bladder flap is necessary. Aggressive and continuous cephalad pressure of the uterine manipulator with the ring/cup is critical to create a clear delineation of the cervicovaginal junction. Creation of the bladder flap is then completed in the caudad direction approximately 1-2 cm over the ring/cup (see image 2).
The anterior colpotomy is initiated with the posterior displacement of the uterine fundus using the RUMI II articulating tip (CooperSurgical) by rotating the handle counterclockwise. This movement simultaneously allows for pressure and emphasis to be placed on the anterior portion of the Koh ring.
Using a clockface as the reference, the anterior colpotomy is initiated at the 12 o’clock position with the monopolar scissors (settings: 30 watts). Once the ring/cup is successfully identified, the colpotomy is extended from the 12 o’clock position to the 2 o’clock and 10 o’clock positions, stopping to avoid the uterine arteries bilaterally.
To begin the posterior colpotomy, the uterine fundus is repositioned anteriorly while maintaining aggressive, continuous cephalad pressure. Again, the RUMI II allows for anterior displacement of the uterine fundus with posterior pressure and emphasis on the Koh ring by turning its handle – this time in the clockwise direction. The posterior colpotomy is initiated at the 6 o’clock position and extended upward to the 4 o’clock and 8 o’clock positions, stopping to avoid the uterine arteries bilaterally.
For taking down the uterine arteries, the optimal placement of the uterus is a midplane position. A clear view of the uterine sidewall is created with retraction using a grasper on the remnant of the round ligament. While maintaining this view, the uterine artery is grasped, cauterized, and transected high up on the uterine sidewall.
The initial pedicle is created well away from the ring/cup in a fashion similar to the placement of a curved Heaney clamp when performing a TAH (see image 3).
Subsequently, each pedicle is then cauterized and transected close to the uterine sidewall, allowing it to fall away from the uterus as progress toward the vaginal ring/cup is made. This portion of the procedure is similar to creating pedicles with straight Heaney clamps during a TAH. Aggressive cephalad pressure is placed on the uterine manipulator and cup throughout the process, further allowing the ureters to fall away with the formation of each pedicle. Upon reaching the vaginal ring/cup, the circumferential colpotomy is completed at the 3 o’clock and 9 o’clock positions.
The specimen is then removed intact transvaginally or is morcellated. Large uteri may be morcellated endoscopically or may be removed by traditional vaginal morcellation techniques to avoid additional costs.
To decrease the chances of vaginal cuff dehiscence, it is critical to use low monopolar energy settings, create appropriate tension to allow efficient and quick colpotomies, and create an adequate bladder flap to allow incorporation of 1-2 cm of vaginal cuff tissue in the closure.
Common techniques for cuff closure include tying the suture with figure-of-eight stitches, running the suture with Lapra-Ty anchors (Ethicon Endosurgery, Nokesville, Va.), or completing the closure with barbed suture.
Dual-site technique
Patient positioning, placement of the uterine manipulator, and insufflation are all performed as previously described. However, with the two-port technique we strongly recommend using the RUMI II, which provides an added degree of manipulation as a result of its articulating tip.
The 8-mm camera port is placed midline 8-10 cm above the uterine fundus when pushed cephalad during EUA. Following the arched port arrangement described above, one additional 8-mm port is placed on the surgeon’s dominant hand side 8-10 cm lateral to the camera port in the mediolateral position. A 2-mm portless alligator grasper is placed 8-10 cm from the camera port on the opposite side (the surgeon’s nondominant side) in the mediolateral position after the robotic surgical system is docked.
The surgical cart is side docked on the surgeon’s dominant hand side, which is the same side as the working port for the robotic instrument. The 8-mm camera is then placed into the camera port and the endowrist one vessel sealer is placed under direct visualization into the robotic working port. Next, the 2-mm alligator grasper is punched through the dermis in needlelike fashion under direct visualization in the location as just described.
(For the system to correctly count instrument lives in the active robotic instrument arm, a "dummy" trocar [locked into the robotic arm but not inserted into the patient’s abdomen] must be placed into an inactive robotic arm opposite the vessel sealer.)
We use the camera arm and one robotic arm for this technique and employ three robotic instruments and a portless 2-mm grasper. Currently, we have successfully performed the two-port technique on uteri up to 16 weeks without the use of additional arms or open conversion.
The order of steps to complete the dual-site hysterectomy generally resembles that of the multisite approach, with several nuances.
The technique for lateral attachments is generally the same, except that the surgeon employs an articulating endowrist one vessel sealer for sealing and cutting tissue, while the first assist uses the 2-mm alligator grasper to proactively present and retract the adnexa for the surgeon (see image 4).
Once the round ligaments are transected, the vessel sealer is replaced with the monopolar scissors. The first assist uses the 2-mm grasper to tent the anterior leaf of the broad ligament, and the surgeon utilizes the scissors to outline and develop the bladder flap as described above. An advanced uterine manipulation skill-set is highly recommended.
After the development of the bladder flap is completed, the anterior and posterior colpotomies are completed as described above (see image 5).
Following completion of the colpotomies, the monopolar scissors are removed and the endowrist one vessel sealer is reinserted. The first assist grasps the round ligament remnant and retracts it to provide a clear view of the uterine sidewall and vessels while cephalad pressure is maintained on the manipulator. The surgeon uses the articulating vessel sealer to create pedicles as described above. Once progress is made to the level of the Koh ring, the vessel sealer is replaced with the scissor and the scissors are used to complete the circumferential colpotomy.
The vast majority of two-port hysterectomy specimens will be removed transvaginally and intact. For the supracervical approach, endoscopic morcellation is applied. With TLH and large uteri, endoscopic or traditional transvaginal morcellation may be applied. If morcellation is performed endoscopically, the robotic patient cart is undocked, the camera is moved to the mediolateral 8-mm port, and the morcellator of choice is placed midline through an expanded umbilical incision.
Following removal of the uterus, the mega suture-cut needle driver and barbed suture are used to close the vaginal cuff. Successful vaginal cuff closure with the two-port technique requires coordinated teamwork between the surgeon and an experienced first assistant. Closure is facilitated with the first assistant grasping the anterior and then the posterior cuff close to the point of needle entry that is chosen by the surgeon.
Throughout the case, suction-irrigation and passing of suture are carried out by temporarily removing the robotic instrument in the 8-mm mediolateral port.
Single-site technique
Patient positioning, placement of the uterine manipulator, and insufflation are again all performed as described for the multisite technique.
The single-site port is placed via an approximately 2-cm incision (Omega, Arch or Z type) through the umbilicus with the arrow displayed on the port pointed toward the target organ. The single-site port accommodates insufflation tubing, an 8-mm camera, two 5-mm operative instruments, and an assistant instrument; all are placed through preordained, standardized lumens (see image 6).
The surgical cart is straight or side docked on the patient’s right side. The cannulas labeled "1" and "2" are docked to robotic arms "1" and "2."
The new single-site tool set differs from instrumentation used in multisite and dual-site procedures in that the operative instruments do not have articulating wrists. Instead, they are flexible and semirigid, allowing them to fit through the curved cannulas to facilitate operative triangulation.
The aesthetic umbilical port placement used in the single-site platform should allow the completion of hysterectomy in uteri with straightforward pathology up to approximately a 14-week size.
The lateral attachments are isolated, secured, and transected as previously described utilizing the 5-mm bipolar Maryland forceps and the 5-mm monopolar hook. Additional presentation and retraction of tissue are performed by the first assistant.
Development of the bladder flap and the anterior and posterior colpotomy are performed just as they are in the multisite and dual-site techniques. If needed, internal swapping of the bipolar and the hook may facilitate more precision during right- and left-side dissections.
Uterine arteries are also dissected in an identical fashion, with internal swapping of instruments facilitating a more precise right and left dissection if needed.
The vast majority of single-site hysterectomy specimens will be removed transvaginally intact. In the supracervical approach or with larger uteri, a transumbilical approach using traditional morcellation can be used. The robotic patient side cart is undocked, the single-site port is removed, and a retractor (the Mini Mobius retractor by CooperSurgical or the extra small Alexis retractor by Applied Medical in Rancho Santa Margarita, Calif.) is inserted.
The specimen is then removed utilizing traditional instruments (i.e., knife, tenaculum, Mayo scissors). Visual "in-line" endoscopic morcellation is not recommended.
The absence of articulating wrists does add some difficulty to the vaginal cuff closure when compared to the multisite platform. We found use of the 5-mm curved needle driver combined with a Keith needle to be highly effective and time efficient (see image 7). Throughout the procedure, suction and irrigation are performed with a 5-mm instrument and suture passage is carried out via the assistant port.
The new robotic single-site instrumentation maintains advantages compared with traditional laparoscopic instrumentation. High-definition three-dimensional visualization, tremor-free instrument movement and surgeon ergonomics are distinct advantages. Other benefits include curved cannulas that restore triangulation and software that reassigns the instruments visualized on the right and left sides to the right and left hands, making hand-eye orientation fluid and intuitive.
Dr. Payne reported that he is a member of the speakers’ bureau for both Intuitive Surgical and CooperSurgical. He would like to acknowledge Dr. Devin Garza, Dr. Sherry Neyman, and Dr. Christopher Seeker for their collaboration and contributions to development of the dual-site approach, and Dr. Garza, Dr. Neyman, and Dr. Lisa Jukes for their contributions to the single-site technique.
Robotic-assisted surgery has been both celebrated as "revolutionary" and defamed as a "crutch." No matter where your loyalties lie in this debate, what is not debatable is the dramatic increase in minimally invasive surgery (MIS) rates for hysterectomy since robotic-assisted surgery was approved for gynecology in 2005. Rates vary across samples and sources, but according to 2011 data from Solucient and 2010 data from the Agency for Healthcare Research and Quality, approximately 27% of hysterectomies are performed with the robot, 26% with standard laparoscopy, and 12% vaginally.
It should be clear to all in 2013 that a total abdominal hysterectomy approach (TAH) is the least favored route for hysterectomy in terms of global cost, invasiveness, and overall complication rate. Therefore, as the AAGL has stated, we should all strive to improve our MIS skill-set – whether it is by the vaginal, laparoscopic, or robotic-assisted approach (J. Minim. Invasive Gynecol. 2011;18:1-3).
Personally, I prefer robotic-assisted techniques. As a community gynecologist, I believe that the marriage of high-tech computerization with the surgical sciences allows for more reproducibility than the traditional vaginal or laparoscopic approaches (J. Minim. Invasive Gynecol. 2008;15:286-91; Obstet. Gynecol. 2010;115:535-42).
In my experience, there are now three reproducible techniques for performing robotic-assisted hysterectomy. The first is a robotic total laparoscopic hysterectomy (TLH) technique involving 4-5 ports, which incorporates some of the steps familiar to surgeons performing TAH. This approach was initially described by Dr. Charles Koh after the advent of the Koh colpotomizer (J. Am. Assoc. Gynecol. Laparosc. 1998;5:187-92) and was then modified and adapted to the robotic platform with my colleagues at the Ochsner Clinic in Louisiana.
The second is a reduced two-port technique that was developed last year with my colleagues at the Texas Institute for Robotic Surgery in Austin.
Last, clearance by the Food and Drug Administration in February 2013 for a da Vinci single-site instrumentation package for use in benign hysterectomy and salpingo-oophorectomy makes the single-site technique a third reproducible approach for performing hysterectomy with the robotic platform. Use of the instrumentation package is currently being launched at Celebration Health Florida Hospital, the Cleveland Clinic, Newark (N.J.) Beth Israel Medical Center, and the Texas Institute for Robotic Surgery.
In addition to being more reproducible, the robotic route to hysterectomy now affords a "see-and-treat" approach, by which we can insert an endoscopic camera, assess the difficulty of the operation (pathology, uterine size, adhesions, etc.), and then select the robotic technique that is best for the patient.
Multisite technique
In positioning the patient, precautions are taken to prevent patient slippage on the operating table during steep Trendelenburg. Most commonly, we place a gel pad or egg crate mattress directly onto the operating table, secure it with tape, and follow with direct placement of the patient onto the gel pad or egg crate. The patient’s arms are then padded and tucked by the sides and the legs are placed in Allen stirrups.
The actual procedure is begun by placing the uterine manipulator of choice. I prefer the RUMI II System with articulating tip or the Advincula Arch with the Koh colpotomizer ring (CooperSurgical, Trumball, Conn.). Other popular options are the VCare manipulator with cup (ConMed Endosurgery, Utica, N.Y.) and the McCarus-Volker Fornisee (LSI Solutions, Victor, N.Y.).
The vaginal pneumo-occlusion balloon can be placed on all three manipulators and is critical for maintaining the pneumoperitoneum that allows for the success of this technique. The importance of properly placing the uterine manipulator of your choice cannot be overemphasized.
For insufflation, I use a Veress needle placed intraumbilically or in the left upper quadrant (LUQ), depending on the patient’s surgical history. The LUQ is preferred if the patient has a history of a prior midline incision. (The stomach must be desufflated first.) The intraumbilical approach is preferred if the patient has a history of LUQ or bariatric surgery.
For port placement, the 8-mm camera port can be placed 8-10 cm above the fundus of the uterus when pushed cephalad on examination under anesthesia (EUA). The robotic camera or a separate camera with a 5-mm laparoscope is introduced (hand-held), and a four-quadrant inspection is undertaken. Direct visualization is used to place two or three additional 8-mm ports in an arch configuration. An 8-mm assistant port is placed on the patient’s side opposite the surgeon’s dominant hand. All ports are spaced 8-10 cm away from each other.
The patient is placed in sufficiently steep Trendelenburg to allow the small bowel to be displaced from the pelvis. The surgical cart is straight docked between the patient’s legs or side docked on the surgeon’s dominant hand side. The 8-mm camera is placed into the camera arm, and then two or three (per the surgeon’s preference) 8-mm robotic instruments are placed under direct visualization.
I prefer to use three instruments during the procedure: the fenestrated bipolar grasper, the monopolar scissors, and the mega suture-cut needle driver.
The ureters are identified. Retroperitoneal dissection is utilized to confirm the ureteral path if needed. Depending on the patient’s desires and history, salpingectomy may be performed.
Isolation and transection of the infundibulopelvic ligaments or the utero-ovarian ligaments are then undertaken. The dissection is carried to the middle of the round ligament, well away from the uterus (where you would place suture when performing TAH). The round ligament is transected, allowing the anterior and posterior leaves of the broad ligament to separate and be visualized. These initial steps will secure two of the four main blood supplies, avoid early uterine artery bleeding, and maximize uterine mobility with larger uteri.
To outline the bladder flap, the location of the Koh ring, VCare cup, or McCarus-Volker Fornisee at the cervicovaginal junction should be noted and used as a general target. The bladder is then filled through the Foley to confirm its location and is then emptied. The anterior leaf of the broad ligament is then picked up and tented with the fenestrated bipolar grasper.
The monopolar scissors are employed to incise the anterior leaf from where the round ligament was transected to the area just cephalad of the cervicovaginal ring and the border of the bladder, in a fashion similar to TAH. Each of these steps is performed bilaterally.
Next, in preparation for the anterior colpotomy, further development of the bladder flap is necessary. Aggressive and continuous cephalad pressure of the uterine manipulator with the ring/cup is critical to create a clear delineation of the cervicovaginal junction. Creation of the bladder flap is then completed in the caudad direction approximately 1-2 cm over the ring/cup (see image 2).
The anterior colpotomy is initiated with the posterior displacement of the uterine fundus using the RUMI II articulating tip (CooperSurgical) by rotating the handle counterclockwise. This movement simultaneously allows for pressure and emphasis to be placed on the anterior portion of the Koh ring.
Using a clockface as the reference, the anterior colpotomy is initiated at the 12 o’clock position with the monopolar scissors (settings: 30 watts). Once the ring/cup is successfully identified, the colpotomy is extended from the 12 o’clock position to the 2 o’clock and 10 o’clock positions, stopping to avoid the uterine arteries bilaterally.
To begin the posterior colpotomy, the uterine fundus is repositioned anteriorly while maintaining aggressive, continuous cephalad pressure. Again, the RUMI II allows for anterior displacement of the uterine fundus with posterior pressure and emphasis on the Koh ring by turning its handle – this time in the clockwise direction. The posterior colpotomy is initiated at the 6 o’clock position and extended upward to the 4 o’clock and 8 o’clock positions, stopping to avoid the uterine arteries bilaterally.
For taking down the uterine arteries, the optimal placement of the uterus is a midplane position. A clear view of the uterine sidewall is created with retraction using a grasper on the remnant of the round ligament. While maintaining this view, the uterine artery is grasped, cauterized, and transected high up on the uterine sidewall.
The initial pedicle is created well away from the ring/cup in a fashion similar to the placement of a curved Heaney clamp when performing a TAH (see image 3).
Subsequently, each pedicle is then cauterized and transected close to the uterine sidewall, allowing it to fall away from the uterus as progress toward the vaginal ring/cup is made. This portion of the procedure is similar to creating pedicles with straight Heaney clamps during a TAH. Aggressive cephalad pressure is placed on the uterine manipulator and cup throughout the process, further allowing the ureters to fall away with the formation of each pedicle. Upon reaching the vaginal ring/cup, the circumferential colpotomy is completed at the 3 o’clock and 9 o’clock positions.
The specimen is then removed intact transvaginally or is morcellated. Large uteri may be morcellated endoscopically or may be removed by traditional vaginal morcellation techniques to avoid additional costs.
To decrease the chances of vaginal cuff dehiscence, it is critical to use low monopolar energy settings, create appropriate tension to allow efficient and quick colpotomies, and create an adequate bladder flap to allow incorporation of 1-2 cm of vaginal cuff tissue in the closure.
Common techniques for cuff closure include tying the suture with figure-of-eight stitches, running the suture with Lapra-Ty anchors (Ethicon Endosurgery, Nokesville, Va.), or completing the closure with barbed suture.
Dual-site technique
Patient positioning, placement of the uterine manipulator, and insufflation are all performed as previously described. However, with the two-port technique we strongly recommend using the RUMI II, which provides an added degree of manipulation as a result of its articulating tip.
The 8-mm camera port is placed midline 8-10 cm above the uterine fundus when pushed cephalad during EUA. Following the arched port arrangement described above, one additional 8-mm port is placed on the surgeon’s dominant hand side 8-10 cm lateral to the camera port in the mediolateral position. A 2-mm portless alligator grasper is placed 8-10 cm from the camera port on the opposite side (the surgeon’s nondominant side) in the mediolateral position after the robotic surgical system is docked.
The surgical cart is side docked on the surgeon’s dominant hand side, which is the same side as the working port for the robotic instrument. The 8-mm camera is then placed into the camera port and the endowrist one vessel sealer is placed under direct visualization into the robotic working port. Next, the 2-mm alligator grasper is punched through the dermis in needlelike fashion under direct visualization in the location as just described.
(For the system to correctly count instrument lives in the active robotic instrument arm, a "dummy" trocar [locked into the robotic arm but not inserted into the patient’s abdomen] must be placed into an inactive robotic arm opposite the vessel sealer.)
We use the camera arm and one robotic arm for this technique and employ three robotic instruments and a portless 2-mm grasper. Currently, we have successfully performed the two-port technique on uteri up to 16 weeks without the use of additional arms or open conversion.
The order of steps to complete the dual-site hysterectomy generally resembles that of the multisite approach, with several nuances.
The technique for lateral attachments is generally the same, except that the surgeon employs an articulating endowrist one vessel sealer for sealing and cutting tissue, while the first assist uses the 2-mm alligator grasper to proactively present and retract the adnexa for the surgeon (see image 4).
Once the round ligaments are transected, the vessel sealer is replaced with the monopolar scissors. The first assist uses the 2-mm grasper to tent the anterior leaf of the broad ligament, and the surgeon utilizes the scissors to outline and develop the bladder flap as described above. An advanced uterine manipulation skill-set is highly recommended.
After the development of the bladder flap is completed, the anterior and posterior colpotomies are completed as described above (see image 5).
Following completion of the colpotomies, the monopolar scissors are removed and the endowrist one vessel sealer is reinserted. The first assist grasps the round ligament remnant and retracts it to provide a clear view of the uterine sidewall and vessels while cephalad pressure is maintained on the manipulator. The surgeon uses the articulating vessel sealer to create pedicles as described above. Once progress is made to the level of the Koh ring, the vessel sealer is replaced with the scissor and the scissors are used to complete the circumferential colpotomy.
The vast majority of two-port hysterectomy specimens will be removed transvaginally and intact. For the supracervical approach, endoscopic morcellation is applied. With TLH and large uteri, endoscopic or traditional transvaginal morcellation may be applied. If morcellation is performed endoscopically, the robotic patient cart is undocked, the camera is moved to the mediolateral 8-mm port, and the morcellator of choice is placed midline through an expanded umbilical incision.
Following removal of the uterus, the mega suture-cut needle driver and barbed suture are used to close the vaginal cuff. Successful vaginal cuff closure with the two-port technique requires coordinated teamwork between the surgeon and an experienced first assistant. Closure is facilitated with the first assistant grasping the anterior and then the posterior cuff close to the point of needle entry that is chosen by the surgeon.
Throughout the case, suction-irrigation and passing of suture are carried out by temporarily removing the robotic instrument in the 8-mm mediolateral port.
Single-site technique
Patient positioning, placement of the uterine manipulator, and insufflation are again all performed as described for the multisite technique.
The single-site port is placed via an approximately 2-cm incision (Omega, Arch or Z type) through the umbilicus with the arrow displayed on the port pointed toward the target organ. The single-site port accommodates insufflation tubing, an 8-mm camera, two 5-mm operative instruments, and an assistant instrument; all are placed through preordained, standardized lumens (see image 6).
The surgical cart is straight or side docked on the patient’s right side. The cannulas labeled "1" and "2" are docked to robotic arms "1" and "2."
The new single-site tool set differs from instrumentation used in multisite and dual-site procedures in that the operative instruments do not have articulating wrists. Instead, they are flexible and semirigid, allowing them to fit through the curved cannulas to facilitate operative triangulation.
The aesthetic umbilical port placement used in the single-site platform should allow the completion of hysterectomy in uteri with straightforward pathology up to approximately a 14-week size.
The lateral attachments are isolated, secured, and transected as previously described utilizing the 5-mm bipolar Maryland forceps and the 5-mm monopolar hook. Additional presentation and retraction of tissue are performed by the first assistant.
Development of the bladder flap and the anterior and posterior colpotomy are performed just as they are in the multisite and dual-site techniques. If needed, internal swapping of the bipolar and the hook may facilitate more precision during right- and left-side dissections.
Uterine arteries are also dissected in an identical fashion, with internal swapping of instruments facilitating a more precise right and left dissection if needed.
The vast majority of single-site hysterectomy specimens will be removed transvaginally intact. In the supracervical approach or with larger uteri, a transumbilical approach using traditional morcellation can be used. The robotic patient side cart is undocked, the single-site port is removed, and a retractor (the Mini Mobius retractor by CooperSurgical or the extra small Alexis retractor by Applied Medical in Rancho Santa Margarita, Calif.) is inserted.
The specimen is then removed utilizing traditional instruments (i.e., knife, tenaculum, Mayo scissors). Visual "in-line" endoscopic morcellation is not recommended.
The absence of articulating wrists does add some difficulty to the vaginal cuff closure when compared to the multisite platform. We found use of the 5-mm curved needle driver combined with a Keith needle to be highly effective and time efficient (see image 7). Throughout the procedure, suction and irrigation are performed with a 5-mm instrument and suture passage is carried out via the assistant port.
The new robotic single-site instrumentation maintains advantages compared with traditional laparoscopic instrumentation. High-definition three-dimensional visualization, tremor-free instrument movement and surgeon ergonomics are distinct advantages. Other benefits include curved cannulas that restore triangulation and software that reassigns the instruments visualized on the right and left sides to the right and left hands, making hand-eye orientation fluid and intuitive.
Dr. Payne reported that he is a member of the speakers’ bureau for both Intuitive Surgical and CooperSurgical. He would like to acknowledge Dr. Devin Garza, Dr. Sherry Neyman, and Dr. Christopher Seeker for their collaboration and contributions to development of the dual-site approach, and Dr. Garza, Dr. Neyman, and Dr. Lisa Jukes for their contributions to the single-site technique.
Robotic-assisted surgery has been both celebrated as "revolutionary" and defamed as a "crutch." No matter where your loyalties lie in this debate, what is not debatable is the dramatic increase in minimally invasive surgery (MIS) rates for hysterectomy since robotic-assisted surgery was approved for gynecology in 2005. Rates vary across samples and sources, but according to 2011 data from Solucient and 2010 data from the Agency for Healthcare Research and Quality, approximately 27% of hysterectomies are performed with the robot, 26% with standard laparoscopy, and 12% vaginally.
It should be clear to all in 2013 that a total abdominal hysterectomy approach (TAH) is the least favored route for hysterectomy in terms of global cost, invasiveness, and overall complication rate. Therefore, as the AAGL has stated, we should all strive to improve our MIS skill-set – whether it is by the vaginal, laparoscopic, or robotic-assisted approach (J. Minim. Invasive Gynecol. 2011;18:1-3).
Personally, I prefer robotic-assisted techniques. As a community gynecologist, I believe that the marriage of high-tech computerization with the surgical sciences allows for more reproducibility than the traditional vaginal or laparoscopic approaches (J. Minim. Invasive Gynecol. 2008;15:286-91; Obstet. Gynecol. 2010;115:535-42).
In my experience, there are now three reproducible techniques for performing robotic-assisted hysterectomy. The first is a robotic total laparoscopic hysterectomy (TLH) technique involving 4-5 ports, which incorporates some of the steps familiar to surgeons performing TAH. This approach was initially described by Dr. Charles Koh after the advent of the Koh colpotomizer (J. Am. Assoc. Gynecol. Laparosc. 1998;5:187-92) and was then modified and adapted to the robotic platform with my colleagues at the Ochsner Clinic in Louisiana.
The second is a reduced two-port technique that was developed last year with my colleagues at the Texas Institute for Robotic Surgery in Austin.
Last, clearance by the Food and Drug Administration in February 2013 for a da Vinci single-site instrumentation package for use in benign hysterectomy and salpingo-oophorectomy makes the single-site technique a third reproducible approach for performing hysterectomy with the robotic platform. Use of the instrumentation package is currently being launched at Celebration Health Florida Hospital, the Cleveland Clinic, Newark (N.J.) Beth Israel Medical Center, and the Texas Institute for Robotic Surgery.
In addition to being more reproducible, the robotic route to hysterectomy now affords a "see-and-treat" approach, by which we can insert an endoscopic camera, assess the difficulty of the operation (pathology, uterine size, adhesions, etc.), and then select the robotic technique that is best for the patient.
Multisite technique
In positioning the patient, precautions are taken to prevent patient slippage on the operating table during steep Trendelenburg. Most commonly, we place a gel pad or egg crate mattress directly onto the operating table, secure it with tape, and follow with direct placement of the patient onto the gel pad or egg crate. The patient’s arms are then padded and tucked by the sides and the legs are placed in Allen stirrups.
The actual procedure is begun by placing the uterine manipulator of choice. I prefer the RUMI II System with articulating tip or the Advincula Arch with the Koh colpotomizer ring (CooperSurgical, Trumball, Conn.). Other popular options are the VCare manipulator with cup (ConMed Endosurgery, Utica, N.Y.) and the McCarus-Volker Fornisee (LSI Solutions, Victor, N.Y.).
The vaginal pneumo-occlusion balloon can be placed on all three manipulators and is critical for maintaining the pneumoperitoneum that allows for the success of this technique. The importance of properly placing the uterine manipulator of your choice cannot be overemphasized.
For insufflation, I use a Veress needle placed intraumbilically or in the left upper quadrant (LUQ), depending on the patient’s surgical history. The LUQ is preferred if the patient has a history of a prior midline incision. (The stomach must be desufflated first.) The intraumbilical approach is preferred if the patient has a history of LUQ or bariatric surgery.
For port placement, the 8-mm camera port can be placed 8-10 cm above the fundus of the uterus when pushed cephalad on examination under anesthesia (EUA). The robotic camera or a separate camera with a 5-mm laparoscope is introduced (hand-held), and a four-quadrant inspection is undertaken. Direct visualization is used to place two or three additional 8-mm ports in an arch configuration. An 8-mm assistant port is placed on the patient’s side opposite the surgeon’s dominant hand. All ports are spaced 8-10 cm away from each other.
The patient is placed in sufficiently steep Trendelenburg to allow the small bowel to be displaced from the pelvis. The surgical cart is straight docked between the patient’s legs or side docked on the surgeon’s dominant hand side. The 8-mm camera is placed into the camera arm, and then two or three (per the surgeon’s preference) 8-mm robotic instruments are placed under direct visualization.
I prefer to use three instruments during the procedure: the fenestrated bipolar grasper, the monopolar scissors, and the mega suture-cut needle driver.
The ureters are identified. Retroperitoneal dissection is utilized to confirm the ureteral path if needed. Depending on the patient’s desires and history, salpingectomy may be performed.
Isolation and transection of the infundibulopelvic ligaments or the utero-ovarian ligaments are then undertaken. The dissection is carried to the middle of the round ligament, well away from the uterus (where you would place suture when performing TAH). The round ligament is transected, allowing the anterior and posterior leaves of the broad ligament to separate and be visualized. These initial steps will secure two of the four main blood supplies, avoid early uterine artery bleeding, and maximize uterine mobility with larger uteri.
To outline the bladder flap, the location of the Koh ring, VCare cup, or McCarus-Volker Fornisee at the cervicovaginal junction should be noted and used as a general target. The bladder is then filled through the Foley to confirm its location and is then emptied. The anterior leaf of the broad ligament is then picked up and tented with the fenestrated bipolar grasper.
The monopolar scissors are employed to incise the anterior leaf from where the round ligament was transected to the area just cephalad of the cervicovaginal ring and the border of the bladder, in a fashion similar to TAH. Each of these steps is performed bilaterally.
Next, in preparation for the anterior colpotomy, further development of the bladder flap is necessary. Aggressive and continuous cephalad pressure of the uterine manipulator with the ring/cup is critical to create a clear delineation of the cervicovaginal junction. Creation of the bladder flap is then completed in the caudad direction approximately 1-2 cm over the ring/cup (see image 2).
The anterior colpotomy is initiated with the posterior displacement of the uterine fundus using the RUMI II articulating tip (CooperSurgical) by rotating the handle counterclockwise. This movement simultaneously allows for pressure and emphasis to be placed on the anterior portion of the Koh ring.
Using a clockface as the reference, the anterior colpotomy is initiated at the 12 o’clock position with the monopolar scissors (settings: 30 watts). Once the ring/cup is successfully identified, the colpotomy is extended from the 12 o’clock position to the 2 o’clock and 10 o’clock positions, stopping to avoid the uterine arteries bilaterally.
To begin the posterior colpotomy, the uterine fundus is repositioned anteriorly while maintaining aggressive, continuous cephalad pressure. Again, the RUMI II allows for anterior displacement of the uterine fundus with posterior pressure and emphasis on the Koh ring by turning its handle – this time in the clockwise direction. The posterior colpotomy is initiated at the 6 o’clock position and extended upward to the 4 o’clock and 8 o’clock positions, stopping to avoid the uterine arteries bilaterally.
For taking down the uterine arteries, the optimal placement of the uterus is a midplane position. A clear view of the uterine sidewall is created with retraction using a grasper on the remnant of the round ligament. While maintaining this view, the uterine artery is grasped, cauterized, and transected high up on the uterine sidewall.
The initial pedicle is created well away from the ring/cup in a fashion similar to the placement of a curved Heaney clamp when performing a TAH (see image 3).
Subsequently, each pedicle is then cauterized and transected close to the uterine sidewall, allowing it to fall away from the uterus as progress toward the vaginal ring/cup is made. This portion of the procedure is similar to creating pedicles with straight Heaney clamps during a TAH. Aggressive cephalad pressure is placed on the uterine manipulator and cup throughout the process, further allowing the ureters to fall away with the formation of each pedicle. Upon reaching the vaginal ring/cup, the circumferential colpotomy is completed at the 3 o’clock and 9 o’clock positions.
The specimen is then removed intact transvaginally or is morcellated. Large uteri may be morcellated endoscopically or may be removed by traditional vaginal morcellation techniques to avoid additional costs.
To decrease the chances of vaginal cuff dehiscence, it is critical to use low monopolar energy settings, create appropriate tension to allow efficient and quick colpotomies, and create an adequate bladder flap to allow incorporation of 1-2 cm of vaginal cuff tissue in the closure.
Common techniques for cuff closure include tying the suture with figure-of-eight stitches, running the suture with Lapra-Ty anchors (Ethicon Endosurgery, Nokesville, Va.), or completing the closure with barbed suture.
Dual-site technique
Patient positioning, placement of the uterine manipulator, and insufflation are all performed as previously described. However, with the two-port technique we strongly recommend using the RUMI II, which provides an added degree of manipulation as a result of its articulating tip.
The 8-mm camera port is placed midline 8-10 cm above the uterine fundus when pushed cephalad during EUA. Following the arched port arrangement described above, one additional 8-mm port is placed on the surgeon’s dominant hand side 8-10 cm lateral to the camera port in the mediolateral position. A 2-mm portless alligator grasper is placed 8-10 cm from the camera port on the opposite side (the surgeon’s nondominant side) in the mediolateral position after the robotic surgical system is docked.
The surgical cart is side docked on the surgeon’s dominant hand side, which is the same side as the working port for the robotic instrument. The 8-mm camera is then placed into the camera port and the endowrist one vessel sealer is placed under direct visualization into the robotic working port. Next, the 2-mm alligator grasper is punched through the dermis in needlelike fashion under direct visualization in the location as just described.
(For the system to correctly count instrument lives in the active robotic instrument arm, a "dummy" trocar [locked into the robotic arm but not inserted into the patient’s abdomen] must be placed into an inactive robotic arm opposite the vessel sealer.)
We use the camera arm and one robotic arm for this technique and employ three robotic instruments and a portless 2-mm grasper. Currently, we have successfully performed the two-port technique on uteri up to 16 weeks without the use of additional arms or open conversion.
The order of steps to complete the dual-site hysterectomy generally resembles that of the multisite approach, with several nuances.
The technique for lateral attachments is generally the same, except that the surgeon employs an articulating endowrist one vessel sealer for sealing and cutting tissue, while the first assist uses the 2-mm alligator grasper to proactively present and retract the adnexa for the surgeon (see image 4).
Once the round ligaments are transected, the vessel sealer is replaced with the monopolar scissors. The first assist uses the 2-mm grasper to tent the anterior leaf of the broad ligament, and the surgeon utilizes the scissors to outline and develop the bladder flap as described above. An advanced uterine manipulation skill-set is highly recommended.
After the development of the bladder flap is completed, the anterior and posterior colpotomies are completed as described above (see image 5).
Following completion of the colpotomies, the monopolar scissors are removed and the endowrist one vessel sealer is reinserted. The first assist grasps the round ligament remnant and retracts it to provide a clear view of the uterine sidewall and vessels while cephalad pressure is maintained on the manipulator. The surgeon uses the articulating vessel sealer to create pedicles as described above. Once progress is made to the level of the Koh ring, the vessel sealer is replaced with the scissor and the scissors are used to complete the circumferential colpotomy.
The vast majority of two-port hysterectomy specimens will be removed transvaginally and intact. For the supracervical approach, endoscopic morcellation is applied. With TLH and large uteri, endoscopic or traditional transvaginal morcellation may be applied. If morcellation is performed endoscopically, the robotic patient cart is undocked, the camera is moved to the mediolateral 8-mm port, and the morcellator of choice is placed midline through an expanded umbilical incision.
Following removal of the uterus, the mega suture-cut needle driver and barbed suture are used to close the vaginal cuff. Successful vaginal cuff closure with the two-port technique requires coordinated teamwork between the surgeon and an experienced first assistant. Closure is facilitated with the first assistant grasping the anterior and then the posterior cuff close to the point of needle entry that is chosen by the surgeon.
Throughout the case, suction-irrigation and passing of suture are carried out by temporarily removing the robotic instrument in the 8-mm mediolateral port.
Single-site technique
Patient positioning, placement of the uterine manipulator, and insufflation are again all performed as described for the multisite technique.
The single-site port is placed via an approximately 2-cm incision (Omega, Arch or Z type) through the umbilicus with the arrow displayed on the port pointed toward the target organ. The single-site port accommodates insufflation tubing, an 8-mm camera, two 5-mm operative instruments, and an assistant instrument; all are placed through preordained, standardized lumens (see image 6).
The surgical cart is straight or side docked on the patient’s right side. The cannulas labeled "1" and "2" are docked to robotic arms "1" and "2."
The new single-site tool set differs from instrumentation used in multisite and dual-site procedures in that the operative instruments do not have articulating wrists. Instead, they are flexible and semirigid, allowing them to fit through the curved cannulas to facilitate operative triangulation.
The aesthetic umbilical port placement used in the single-site platform should allow the completion of hysterectomy in uteri with straightforward pathology up to approximately a 14-week size.
The lateral attachments are isolated, secured, and transected as previously described utilizing the 5-mm bipolar Maryland forceps and the 5-mm monopolar hook. Additional presentation and retraction of tissue are performed by the first assistant.
Development of the bladder flap and the anterior and posterior colpotomy are performed just as they are in the multisite and dual-site techniques. If needed, internal swapping of the bipolar and the hook may facilitate more precision during right- and left-side dissections.
Uterine arteries are also dissected in an identical fashion, with internal swapping of instruments facilitating a more precise right and left dissection if needed.
The vast majority of single-site hysterectomy specimens will be removed transvaginally intact. In the supracervical approach or with larger uteri, a transumbilical approach using traditional morcellation can be used. The robotic patient side cart is undocked, the single-site port is removed, and a retractor (the Mini Mobius retractor by CooperSurgical or the extra small Alexis retractor by Applied Medical in Rancho Santa Margarita, Calif.) is inserted.
The specimen is then removed utilizing traditional instruments (i.e., knife, tenaculum, Mayo scissors). Visual "in-line" endoscopic morcellation is not recommended.
The absence of articulating wrists does add some difficulty to the vaginal cuff closure when compared to the multisite platform. We found use of the 5-mm curved needle driver combined with a Keith needle to be highly effective and time efficient (see image 7). Throughout the procedure, suction and irrigation are performed with a 5-mm instrument and suture passage is carried out via the assistant port.
The new robotic single-site instrumentation maintains advantages compared with traditional laparoscopic instrumentation. High-definition three-dimensional visualization, tremor-free instrument movement and surgeon ergonomics are distinct advantages. Other benefits include curved cannulas that restore triangulation and software that reassigns the instruments visualized on the right and left sides to the right and left hands, making hand-eye orientation fluid and intuitive.
Dr. Payne reported that he is a member of the speakers’ bureau for both Intuitive Surgical and CooperSurgical. He would like to acknowledge Dr. Devin Garza, Dr. Sherry Neyman, and Dr. Christopher Seeker for their collaboration and contributions to development of the dual-site approach, and Dr. Garza, Dr. Neyman, and Dr. Lisa Jukes for their contributions to the single-site technique.
ACA Turns 3: The Policy & Practice Podcast
The Affordable Care Act withstood another repeal attempt last week – even as it celebrated its third anniversary. The health reform law was signed on March 23, 2010, but Republicans still seek to roll back the ACA or at least eliminate some of what they consider to be its less desirable parts.
A budget plan by Rep. Paul Ryan (R-Wisc.) that would have repealed the law got a floor vote last week and was handily approved by Republicans in the House. Senate Democrats nixed it just as quickly.
Surprisingly, though, in a separate vote, 33 Senate Democrats joined Republicans to support repeal of a medical device tax that was established by the ACA.
That tax may be one of the few areas of bipartisan agreement when it comes to the reform law. For more, take a listen to this week’s Policy and Practice podcast.
On Twitter @aliciaault
The Affordable Care Act withstood another repeal attempt last week – even as it celebrated its third anniversary. The health reform law was signed on March 23, 2010, but Republicans still seek to roll back the ACA or at least eliminate some of what they consider to be its less desirable parts.
A budget plan by Rep. Paul Ryan (R-Wisc.) that would have repealed the law got a floor vote last week and was handily approved by Republicans in the House. Senate Democrats nixed it just as quickly.
Surprisingly, though, in a separate vote, 33 Senate Democrats joined Republicans to support repeal of a medical device tax that was established by the ACA.
That tax may be one of the few areas of bipartisan agreement when it comes to the reform law. For more, take a listen to this week’s Policy and Practice podcast.
On Twitter @aliciaault
The Affordable Care Act withstood another repeal attempt last week – even as it celebrated its third anniversary. The health reform law was signed on March 23, 2010, but Republicans still seek to roll back the ACA or at least eliminate some of what they consider to be its less desirable parts.
A budget plan by Rep. Paul Ryan (R-Wisc.) that would have repealed the law got a floor vote last week and was handily approved by Republicans in the House. Senate Democrats nixed it just as quickly.
Surprisingly, though, in a separate vote, 33 Senate Democrats joined Republicans to support repeal of a medical device tax that was established by the ACA.
That tax may be one of the few areas of bipartisan agreement when it comes to the reform law. For more, take a listen to this week’s Policy and Practice podcast.
On Twitter @aliciaault
Match Day- Surgery remains most popular, primary care rising
Surgery residencies are still the top choice for U.S. medical students, but the number choosing primary care continues to rise.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
Surgery residencies are still the top choice for U.S. medical students, but the number choosing primary care continues to rise.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
Surgery residencies are still the top choice for U.S. medical students, but the number choosing primary care continues to rise.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
Green glow the tumors during surgery
NATIONAL HARBOR, MD – Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the U.S. and the Netherlands reported in oral and poster sessions.
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors – including noncontiguous pockets of malignancy – during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within two centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the near-infrared portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam," which consists of a light source and near-infrared (NIR) camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5 cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
"This is another patient who would have gone home [with a diagnosis of] stage 1A. I would have walked down to the recovery room, say ‘I cured you,’ and he would come back 1 year later with metastatic disease and die. This patient, who had minimal disease when we discovered it, got chemotherapy and is still alive at the 1-year mark," Dr. Singhal said.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal’s studies were supported by the Society of Surgical Oncology and the University of Pennsylvania. He reported having no financial disclosures. Dr. Brouwer’s study was supported by the Netherlands Cancer Institute. He reported having no financial disclosures.
NATIONAL HARBOR, MD – Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the U.S. and the Netherlands reported in oral and poster sessions.
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors – including noncontiguous pockets of malignancy – during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within two centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the near-infrared portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam," which consists of a light source and near-infrared (NIR) camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5 cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
"This is another patient who would have gone home [with a diagnosis of] stage 1A. I would have walked down to the recovery room, say ‘I cured you,’ and he would come back 1 year later with metastatic disease and die. This patient, who had minimal disease when we discovered it, got chemotherapy and is still alive at the 1-year mark," Dr. Singhal said.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal’s studies were supported by the Society of Surgical Oncology and the University of Pennsylvania. He reported having no financial disclosures. Dr. Brouwer’s study was supported by the Netherlands Cancer Institute. He reported having no financial disclosures.
NATIONAL HARBOR, MD – Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the U.S. and the Netherlands reported in oral and poster sessions.
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors – including noncontiguous pockets of malignancy – during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within two centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the near-infrared portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam," which consists of a light source and near-infrared (NIR) camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5 cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
"This is another patient who would have gone home [with a diagnosis of] stage 1A. I would have walked down to the recovery room, say ‘I cured you,’ and he would come back 1 year later with metastatic disease and die. This patient, who had minimal disease when we discovered it, got chemotherapy and is still alive at the 1-year mark," Dr. Singhal said.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal’s studies were supported by the Society of Surgical Oncology and the University of Pennsylvania. He reported having no financial disclosures. Dr. Brouwer’s study was supported by the Netherlands Cancer Institute. He reported having no financial disclosures.
AT SSO 2013
Major finding: Indocyanine green dye highlights tumors for intraoperative visualization and more complete resection with the aid of a portable near-infrared camera.
Data source: Review of research and early clinical studies in patients with lung tumors; case series investigating the use of a hybrid radio-labeled and fluorescent tracer for evaluating lymph nodes in patients with melanomas.
Disclosures: Dr. Singhal’s studies were supported by the Society of Surgical Oncology and the University of Pennsylvania. He reported having no financial disclosures. Dr. Brouwer's study was supported by the Netherlands Cancer Institute. He reported having no financial disclosures.