User login
Official Newspaper of the American College of Surgeons
MAGELLAN trial results support rivaroxaban for DVT prophylaxis
Nearly 2 years after their presentation at a national meeting, the results of MAGELLAN, comparing rivaroxaban to enoxaparin for thromboprophylaxis in critically ill hospitalized patients, have been published online Feb. 6 in the New England Journal of Medicine.
In that large, multicenter trial, rivaroxaban was noninferior to enoxaparin when used for the standard 10-day duration, and superior when used for an extended 35-day duration, for thromboprophylaxis.
However, the rate of clinically relevant bleeding and the incidence of major bleeding events were significantly higher with rivaroxaban than with enoxaparin. This adverse effect apparently balanced out the reduction in venous thromboembolism, as a prespecified analysis of net clinical benefit and harm did not show either one at day 10 or day 35, reported Dr. Alexander T. Cohen and his associates in MAGELLAN (Multicenter, Randomized, Parallel Group Efficacy and Safety Study for the Prevention of Venous Thromboembolism in Hospitalized Acutely Ill Medical Patients Comparing Rivaroxaban with Enoxaparin). The results were first presented by Dr. Cohen, of King's College Hospital, London, at the annual meeting of the American College of Cardiology in spring 2011.
In the 2.5-year study, 8,101 patients at 556 sites in 52 countries were randomized to receive rivaroxaban (4,050 subjects) or enoxaparin (4,051 subjects). Hundreds of patients in both study groups were excluded from the final analyses for various reasons, usually because they could not be assessed for venous thromboembolism using ultrasonography and other imaging techniques in a timely fashion, as required by the study protocol.
At 10 days' follow-up, 2.7% of patients in both groups had a primary outcome event - asymptomatic proximal deep vein thrombosis (DVT), symptomatic nonfatal pulmonary embolism (PE), or thromboembolism-related death - so rivaroxaban met the criteria for noninferiority to enoxaparin.
At the 35-day follow-up, 4.4% of subjects who received extended-duration rivaroxaban and 5.7% of those who received enoxaparin plus placebo had a primary outcome event, so rivaroxaban met the criteria for superiority to enoxaparin, the investigators reported (N. Engl. J. Med. 2013 Feb. 6 [doi: 10.1056/NEJMoa1111096]).
Rivaroxaban (Xarelto)has several indications: for stroke prevention in nonvalvular atrial fibrillation, for the treatment of DVT and PE, for reducing the risk of recurrence of DVT and PE, and for the prophylaxis of DVT in patients undergoing knee or hip replacement surgery. It is not indicated for the condition studied in MAGELLAN, namely prevention of VTE in acutely medically ill patients.
This study was funded by Bayer HealthCare and Janssen, sponsors that also collected and analyzed the study data. Dr. Cohen and his associates reported numerous ties to industry sources.
Nearly 2 years after their presentation at a national meeting, the results of MAGELLAN, comparing rivaroxaban to enoxaparin for thromboprophylaxis in critically ill hospitalized patients, have been published online Feb. 6 in the New England Journal of Medicine.
In that large, multicenter trial, rivaroxaban was noninferior to enoxaparin when used for the standard 10-day duration, and superior when used for an extended 35-day duration, for thromboprophylaxis.
However, the rate of clinically relevant bleeding and the incidence of major bleeding events were significantly higher with rivaroxaban than with enoxaparin. This adverse effect apparently balanced out the reduction in venous thromboembolism, as a prespecified analysis of net clinical benefit and harm did not show either one at day 10 or day 35, reported Dr. Alexander T. Cohen and his associates in MAGELLAN (Multicenter, Randomized, Parallel Group Efficacy and Safety Study for the Prevention of Venous Thromboembolism in Hospitalized Acutely Ill Medical Patients Comparing Rivaroxaban with Enoxaparin). The results were first presented by Dr. Cohen, of King's College Hospital, London, at the annual meeting of the American College of Cardiology in spring 2011.
In the 2.5-year study, 8,101 patients at 556 sites in 52 countries were randomized to receive rivaroxaban (4,050 subjects) or enoxaparin (4,051 subjects). Hundreds of patients in both study groups were excluded from the final analyses for various reasons, usually because they could not be assessed for venous thromboembolism using ultrasonography and other imaging techniques in a timely fashion, as required by the study protocol.
At 10 days' follow-up, 2.7% of patients in both groups had a primary outcome event - asymptomatic proximal deep vein thrombosis (DVT), symptomatic nonfatal pulmonary embolism (PE), or thromboembolism-related death - so rivaroxaban met the criteria for noninferiority to enoxaparin.
At the 35-day follow-up, 4.4% of subjects who received extended-duration rivaroxaban and 5.7% of those who received enoxaparin plus placebo had a primary outcome event, so rivaroxaban met the criteria for superiority to enoxaparin, the investigators reported (N. Engl. J. Med. 2013 Feb. 6 [doi: 10.1056/NEJMoa1111096]).
Rivaroxaban (Xarelto)has several indications: for stroke prevention in nonvalvular atrial fibrillation, for the treatment of DVT and PE, for reducing the risk of recurrence of DVT and PE, and for the prophylaxis of DVT in patients undergoing knee or hip replacement surgery. It is not indicated for the condition studied in MAGELLAN, namely prevention of VTE in acutely medically ill patients.
This study was funded by Bayer HealthCare and Janssen, sponsors that also collected and analyzed the study data. Dr. Cohen and his associates reported numerous ties to industry sources.
Nearly 2 years after their presentation at a national meeting, the results of MAGELLAN, comparing rivaroxaban to enoxaparin for thromboprophylaxis in critically ill hospitalized patients, have been published online Feb. 6 in the New England Journal of Medicine.
In that large, multicenter trial, rivaroxaban was noninferior to enoxaparin when used for the standard 10-day duration, and superior when used for an extended 35-day duration, for thromboprophylaxis.
However, the rate of clinically relevant bleeding and the incidence of major bleeding events were significantly higher with rivaroxaban than with enoxaparin. This adverse effect apparently balanced out the reduction in venous thromboembolism, as a prespecified analysis of net clinical benefit and harm did not show either one at day 10 or day 35, reported Dr. Alexander T. Cohen and his associates in MAGELLAN (Multicenter, Randomized, Parallel Group Efficacy and Safety Study for the Prevention of Venous Thromboembolism in Hospitalized Acutely Ill Medical Patients Comparing Rivaroxaban with Enoxaparin). The results were first presented by Dr. Cohen, of King's College Hospital, London, at the annual meeting of the American College of Cardiology in spring 2011.
In the 2.5-year study, 8,101 patients at 556 sites in 52 countries were randomized to receive rivaroxaban (4,050 subjects) or enoxaparin (4,051 subjects). Hundreds of patients in both study groups were excluded from the final analyses for various reasons, usually because they could not be assessed for venous thromboembolism using ultrasonography and other imaging techniques in a timely fashion, as required by the study protocol.
At 10 days' follow-up, 2.7% of patients in both groups had a primary outcome event - asymptomatic proximal deep vein thrombosis (DVT), symptomatic nonfatal pulmonary embolism (PE), or thromboembolism-related death - so rivaroxaban met the criteria for noninferiority to enoxaparin.
At the 35-day follow-up, 4.4% of subjects who received extended-duration rivaroxaban and 5.7% of those who received enoxaparin plus placebo had a primary outcome event, so rivaroxaban met the criteria for superiority to enoxaparin, the investigators reported (N. Engl. J. Med. 2013 Feb. 6 [doi: 10.1056/NEJMoa1111096]).
Rivaroxaban (Xarelto)has several indications: for stroke prevention in nonvalvular atrial fibrillation, for the treatment of DVT and PE, for reducing the risk of recurrence of DVT and PE, and for the prophylaxis of DVT in patients undergoing knee or hip replacement surgery. It is not indicated for the condition studied in MAGELLAN, namely prevention of VTE in acutely medically ill patients.
This study was funded by Bayer HealthCare and Janssen, sponsors that also collected and analyzed the study data. Dr. Cohen and his associates reported numerous ties to industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: At 10-day follow-up, 2.7% of both study groups
had a thromboembolic event; at 35-day follow-up, 4.4% of subjects who received
rivaroxaban and 5.7% of those who received enoxaparin had a thromboembolic
event.
Data Source: A randomized, double-blind trial in 5,931 inpatients
with acute medical illness comparing rivaroxaban with enoxaparin for
thromboprophylaxis.
Disclosures: This study was funded by Bayer HealthCare and
Janssen, sponsors that also collected and analyzed the study data. Dr. Cohen
and his associates reported numerous ties to industry sources.
Doctors support bipartisan SGR repeal bill
A bill with bipartisan sponsors has been introduced in the U.S. House of Representatives to permanently repeal Medicare's Sustainable Growth Rate formula.
Rep. Joe Heck (R-Nev.) and Rep. Allyson Schwartz (D-Penn.) unveiled their proposal at a briefing with reporters on Feb. 6. They were surrounded by supporters, including representatives from the American College of Physicians, the American Academy of Family Physicians, the American College of Osteopathic Family Physicians, and the National Coalition on Health Care.
In addition to repealing the SGR, the bill also "stabilizes the current payment system for physicians, and it institutes measures to ensure access to primary care with increased updates for primary care physicians in the short term," said Rep. Schwartz, who added that it also "aggressively" tests new payment and delivery models and rewards high value, high quality health care.
Rep. Schwartz and Rep. Heck, an osteopathic physician trained in emergency medicine, also introduced the bill in the last Congress. But both said that they think that legislators are primed to act, in part because of the struggle to reduce health care spending and the deficit.
If the SGR is not replaced or repealed by the end of the year, physicians will see a 27% reduction in pay beginning in January 2014. Each year the cuts are delayed merely adds more on to the final tally for fixing the formula, noted Rep. Heck. The Congressional Budget Office estimated in its latest economic outlook released on Feb. 5 that it would cost about $138 billion to permanently repeal the SGR. That's less than the $245 billion in previous CBO estimates.
"The time right now is perfect to finally pass this legislation," said Rep. Heck.
"I think the imminent process of sequestration may add a little urgency to reform because across the board cuts are not going to get us where we need to go," said John Rother, president and CEO of the National Coalition on Health Care, an umbrella group representing medical societies, businesses, unions, health care providers, religious associations, insurers, and consumers. "And the alternative here is smarter and much more oriented toward value, and it provides a very practical and beneficial alternative to the kind of meat-axe approaches in sequestration," Mr. Rother said.
Physician groups said they are hopeful that the proposal has legs this year.
The constant uncertainty about whether SGR cuts will occur, "undermines the family doctor's ability to continue to keep doors open and to invest in their practices," said Dr. Jeffrey Cain, president of the AAFP. He praised the Heck-Schwartz bill, which had not been officially introduced in the House at press time, saying that it would put an end to "the annual question of whether physicians can continue to afford to practice in Medicare," and that it also "stabilizes the Medicare cost system and provides solutions that are based on successful and proven methods that can improve quality and incent value."
Dr. Chuck Cutler, chair-elect of the ACP Board of Regents, said that "the stability that this bill brings to the marketplace and to our practice is particularly encouraging." He also said that the ACP was happy that the bill would maintain 2013 payment levels through the end of 2014 and then provide "positive and predictable updates" through 2019.
That is especially important as physicians test out new delivery and payment models, said Dr. Cutler.
From 2015 to 2018, the bill calls for annual increases of 2.5% for primary care, preventive, and care-coordination services. All other physicians would get a 0.5% increase for the 4-year period.
By 2019, physicians who continue to use a volume-drive fee-for-service model would get a smaller increase than would those who have transitioned to new models.
In addition to the groups who participated in the briefing, the bill also is supported by the American College of Obstetricians and Gynecologists, the Society of Hospital Medicine, the American College of Rheumatology, the American College of Cardiology, the American Academy of Neurology, and the American Academy of Pediatrics.
On Twitter @aliciaault
A bill with bipartisan sponsors has been introduced in the U.S. House of Representatives to permanently repeal Medicare's Sustainable Growth Rate formula.
Rep. Joe Heck (R-Nev.) and Rep. Allyson Schwartz (D-Penn.) unveiled their proposal at a briefing with reporters on Feb. 6. They were surrounded by supporters, including representatives from the American College of Physicians, the American Academy of Family Physicians, the American College of Osteopathic Family Physicians, and the National Coalition on Health Care.
In addition to repealing the SGR, the bill also "stabilizes the current payment system for physicians, and it institutes measures to ensure access to primary care with increased updates for primary care physicians in the short term," said Rep. Schwartz, who added that it also "aggressively" tests new payment and delivery models and rewards high value, high quality health care.
Rep. Schwartz and Rep. Heck, an osteopathic physician trained in emergency medicine, also introduced the bill in the last Congress. But both said that they think that legislators are primed to act, in part because of the struggle to reduce health care spending and the deficit.
If the SGR is not replaced or repealed by the end of the year, physicians will see a 27% reduction in pay beginning in January 2014. Each year the cuts are delayed merely adds more on to the final tally for fixing the formula, noted Rep. Heck. The Congressional Budget Office estimated in its latest economic outlook released on Feb. 5 that it would cost about $138 billion to permanently repeal the SGR. That's less than the $245 billion in previous CBO estimates.
"The time right now is perfect to finally pass this legislation," said Rep. Heck.
"I think the imminent process of sequestration may add a little urgency to reform because across the board cuts are not going to get us where we need to go," said John Rother, president and CEO of the National Coalition on Health Care, an umbrella group representing medical societies, businesses, unions, health care providers, religious associations, insurers, and consumers. "And the alternative here is smarter and much more oriented toward value, and it provides a very practical and beneficial alternative to the kind of meat-axe approaches in sequestration," Mr. Rother said.
Physician groups said they are hopeful that the proposal has legs this year.
The constant uncertainty about whether SGR cuts will occur, "undermines the family doctor's ability to continue to keep doors open and to invest in their practices," said Dr. Jeffrey Cain, president of the AAFP. He praised the Heck-Schwartz bill, which had not been officially introduced in the House at press time, saying that it would put an end to "the annual question of whether physicians can continue to afford to practice in Medicare," and that it also "stabilizes the Medicare cost system and provides solutions that are based on successful and proven methods that can improve quality and incent value."
Dr. Chuck Cutler, chair-elect of the ACP Board of Regents, said that "the stability that this bill brings to the marketplace and to our practice is particularly encouraging." He also said that the ACP was happy that the bill would maintain 2013 payment levels through the end of 2014 and then provide "positive and predictable updates" through 2019.
That is especially important as physicians test out new delivery and payment models, said Dr. Cutler.
From 2015 to 2018, the bill calls for annual increases of 2.5% for primary care, preventive, and care-coordination services. All other physicians would get a 0.5% increase for the 4-year period.
By 2019, physicians who continue to use a volume-drive fee-for-service model would get a smaller increase than would those who have transitioned to new models.
In addition to the groups who participated in the briefing, the bill also is supported by the American College of Obstetricians and Gynecologists, the Society of Hospital Medicine, the American College of Rheumatology, the American College of Cardiology, the American Academy of Neurology, and the American Academy of Pediatrics.
On Twitter @aliciaault
A bill with bipartisan sponsors has been introduced in the U.S. House of Representatives to permanently repeal Medicare's Sustainable Growth Rate formula.
Rep. Joe Heck (R-Nev.) and Rep. Allyson Schwartz (D-Penn.) unveiled their proposal at a briefing with reporters on Feb. 6. They were surrounded by supporters, including representatives from the American College of Physicians, the American Academy of Family Physicians, the American College of Osteopathic Family Physicians, and the National Coalition on Health Care.
In addition to repealing the SGR, the bill also "stabilizes the current payment system for physicians, and it institutes measures to ensure access to primary care with increased updates for primary care physicians in the short term," said Rep. Schwartz, who added that it also "aggressively" tests new payment and delivery models and rewards high value, high quality health care.
Rep. Schwartz and Rep. Heck, an osteopathic physician trained in emergency medicine, also introduced the bill in the last Congress. But both said that they think that legislators are primed to act, in part because of the struggle to reduce health care spending and the deficit.
If the SGR is not replaced or repealed by the end of the year, physicians will see a 27% reduction in pay beginning in January 2014. Each year the cuts are delayed merely adds more on to the final tally for fixing the formula, noted Rep. Heck. The Congressional Budget Office estimated in its latest economic outlook released on Feb. 5 that it would cost about $138 billion to permanently repeal the SGR. That's less than the $245 billion in previous CBO estimates.
"The time right now is perfect to finally pass this legislation," said Rep. Heck.
"I think the imminent process of sequestration may add a little urgency to reform because across the board cuts are not going to get us where we need to go," said John Rother, president and CEO of the National Coalition on Health Care, an umbrella group representing medical societies, businesses, unions, health care providers, religious associations, insurers, and consumers. "And the alternative here is smarter and much more oriented toward value, and it provides a very practical and beneficial alternative to the kind of meat-axe approaches in sequestration," Mr. Rother said.
Physician groups said they are hopeful that the proposal has legs this year.
The constant uncertainty about whether SGR cuts will occur, "undermines the family doctor's ability to continue to keep doors open and to invest in their practices," said Dr. Jeffrey Cain, president of the AAFP. He praised the Heck-Schwartz bill, which had not been officially introduced in the House at press time, saying that it would put an end to "the annual question of whether physicians can continue to afford to practice in Medicare," and that it also "stabilizes the Medicare cost system and provides solutions that are based on successful and proven methods that can improve quality and incent value."
Dr. Chuck Cutler, chair-elect of the ACP Board of Regents, said that "the stability that this bill brings to the marketplace and to our practice is particularly encouraging." He also said that the ACP was happy that the bill would maintain 2013 payment levels through the end of 2014 and then provide "positive and predictable updates" through 2019.
That is especially important as physicians test out new delivery and payment models, said Dr. Cutler.
From 2015 to 2018, the bill calls for annual increases of 2.5% for primary care, preventive, and care-coordination services. All other physicians would get a 0.5% increase for the 4-year period.
By 2019, physicians who continue to use a volume-drive fee-for-service model would get a smaller increase than would those who have transitioned to new models.
In addition to the groups who participated in the briefing, the bill also is supported by the American College of Obstetricians and Gynecologists, the Society of Hospital Medicine, the American College of Rheumatology, the American College of Cardiology, the American Academy of Neurology, and the American Academy of Pediatrics.
On Twitter @aliciaault
Medicaid's share of state budgets nears 24%
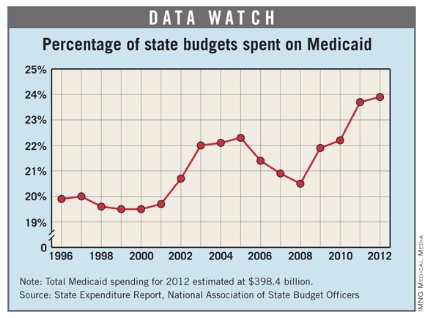
In fiscal 2012, total state spending on Medicaid rose to an estimated $398.4 billion, bringing the program’s average share of state budgets to 23.9%, according to a report from the National Association of State Budget Officers.
Medicaid has accounted for the single largest portion of states’ total spending each year since 2009, outpacing elementary/secondary education, the association’s data show.
The increase in total spending from 2011 to 2012 was 1.2%, which is considerably less than the 9.6% increase from 2010 to 2011 and "significantly below historical trends," the report noted.

In fiscal 2012, total state spending on Medicaid rose to an estimated $398.4 billion, bringing the program’s average share of state budgets to 23.9%, according to a report from the National Association of State Budget Officers.
Medicaid has accounted for the single largest portion of states’ total spending each year since 2009, outpacing elementary/secondary education, the association’s data show.
The increase in total spending from 2011 to 2012 was 1.2%, which is considerably less than the 9.6% increase from 2010 to 2011 and "significantly below historical trends," the report noted.

In fiscal 2012, total state spending on Medicaid rose to an estimated $398.4 billion, bringing the program’s average share of state budgets to 23.9%, according to a report from the National Association of State Budget Officers.
Medicaid has accounted for the single largest portion of states’ total spending each year since 2009, outpacing elementary/secondary education, the association’s data show.
The increase in total spending from 2011 to 2012 was 1.2%, which is considerably less than the 9.6% increase from 2010 to 2011 and "significantly below historical trends," the report noted.

Why should doctors die differently?
My attention was drawn to a recent headline in a local newspaper: "Doctors die differently than their patients." The article discussed the fact that physicians often do not request complicated treatment and life-sustaining therapies. It referenced a February 2012 piece in the Wall Street Journal by Dr. Ken Murray. Dr. Murray discussed some of the available evidence supporting the different decisions physicians reach regarding end-of-life care.
He quoted a 2003 article by Joseph Gallo and associates, who surveyed participants in the Johns Hopkins Precursors Study, which covered physicians graduating from Hopkins between 1948 and 1964. The investigators obtained responses from nearly 800 physicians regarding their end-of-life decisions. Compared with 20% of the general public, 64% of physician respondents had created an advanced directive. Additionally, nearly 90% of the physicians did not want CPR if they were in a chronic coma. This contrasts with about 25% of the general public not desiring "heroic measures." Clearly, physicians were taking the initiative and outlining the care that they did and did not want to receive in the setting of advanced medical illness.
Murray also mentioned a 1996 study that examined how CPR was portrayed in television shows and the potential impact it may have on patients’ decision making. In that paper, CPR was successful in 75% of the TV cases, with 67% of patients ultimately being discharged from the hospital (N. Engl. J. Med. 1996;334:1578-82).
Compare this with what we know to be true. CPR rarely works. A 2010 study that evaluated the impact of 95,000 cases of CPR in Japan demonstrated that clearly. Only 8% of patients who had received CPR survived for more than 1 month. Of those who survived, only 3% were able to lead "normal" lives.
Based upon our experiences, we are able to make objective assessments of the likelihood of success of various therapies in our patients. As hospitalists, we are often placed in the position of helping explain therapies provided by other specialists – cardiologists, oncologists, surgeons. I know that there have been times when I have seen patients receiving treatments I considered futile. I believe many of us have been in similar situations. Patients do not fully understand the risks and benefits of their therapy. Once the big picture is made clear to them, they often opt for more conservative therapy aimed at improving quality of life.
I believe we have an obligation to our patients to share with them the reality of the care they receive. We need to check in with our patients and understand what is important to them. Do they want to exhaust every medical option available? Are they looking to live long enough to attend a graduation or wedding? Do they value comfort and quality time above all else? We need to ask these questions and fully understand our patients and their desires.
I wrote previously about my former colleague Darlene. Had I not known her desires regarding continued therapy, she would have received care she did not want. I am certain of this because she was in the process of being transferred to the intensive care unit when I intervened at the behest of a mutual friend. She would have received several days of great, high-tech care in the ICU – and ultimately died despite that care, care that she did not want in the first place.
We, as hospitalists, must talk with our patients about their wishes. We must educate them about the likelihood of success of their therapies and of CPR. We must act as their advocates with subspecialists who too often focus on their specific portion of the patient, losing sight of the bigger picture. We need to do better. We need to ask the question: Should doctors die differently?
If advanced directives and dying in comfort are good enough for us, they should be good enough for our patients.
Dr. Pistoria is chief of hospital medicine at Coordinated Health in Bethlehem, Pa. He believes that the best care is always personal.
My attention was drawn to a recent headline in a local newspaper: "Doctors die differently than their patients." The article discussed the fact that physicians often do not request complicated treatment and life-sustaining therapies. It referenced a February 2012 piece in the Wall Street Journal by Dr. Ken Murray. Dr. Murray discussed some of the available evidence supporting the different decisions physicians reach regarding end-of-life care.
He quoted a 2003 article by Joseph Gallo and associates, who surveyed participants in the Johns Hopkins Precursors Study, which covered physicians graduating from Hopkins between 1948 and 1964. The investigators obtained responses from nearly 800 physicians regarding their end-of-life decisions. Compared with 20% of the general public, 64% of physician respondents had created an advanced directive. Additionally, nearly 90% of the physicians did not want CPR if they were in a chronic coma. This contrasts with about 25% of the general public not desiring "heroic measures." Clearly, physicians were taking the initiative and outlining the care that they did and did not want to receive in the setting of advanced medical illness.
Murray also mentioned a 1996 study that examined how CPR was portrayed in television shows and the potential impact it may have on patients’ decision making. In that paper, CPR was successful in 75% of the TV cases, with 67% of patients ultimately being discharged from the hospital (N. Engl. J. Med. 1996;334:1578-82).
Compare this with what we know to be true. CPR rarely works. A 2010 study that evaluated the impact of 95,000 cases of CPR in Japan demonstrated that clearly. Only 8% of patients who had received CPR survived for more than 1 month. Of those who survived, only 3% were able to lead "normal" lives.
Based upon our experiences, we are able to make objective assessments of the likelihood of success of various therapies in our patients. As hospitalists, we are often placed in the position of helping explain therapies provided by other specialists – cardiologists, oncologists, surgeons. I know that there have been times when I have seen patients receiving treatments I considered futile. I believe many of us have been in similar situations. Patients do not fully understand the risks and benefits of their therapy. Once the big picture is made clear to them, they often opt for more conservative therapy aimed at improving quality of life.
I believe we have an obligation to our patients to share with them the reality of the care they receive. We need to check in with our patients and understand what is important to them. Do they want to exhaust every medical option available? Are they looking to live long enough to attend a graduation or wedding? Do they value comfort and quality time above all else? We need to ask these questions and fully understand our patients and their desires.
I wrote previously about my former colleague Darlene. Had I not known her desires regarding continued therapy, she would have received care she did not want. I am certain of this because she was in the process of being transferred to the intensive care unit when I intervened at the behest of a mutual friend. She would have received several days of great, high-tech care in the ICU – and ultimately died despite that care, care that she did not want in the first place.
We, as hospitalists, must talk with our patients about their wishes. We must educate them about the likelihood of success of their therapies and of CPR. We must act as their advocates with subspecialists who too often focus on their specific portion of the patient, losing sight of the bigger picture. We need to do better. We need to ask the question: Should doctors die differently?
If advanced directives and dying in comfort are good enough for us, they should be good enough for our patients.
Dr. Pistoria is chief of hospital medicine at Coordinated Health in Bethlehem, Pa. He believes that the best care is always personal.
My attention was drawn to a recent headline in a local newspaper: "Doctors die differently than their patients." The article discussed the fact that physicians often do not request complicated treatment and life-sustaining therapies. It referenced a February 2012 piece in the Wall Street Journal by Dr. Ken Murray. Dr. Murray discussed some of the available evidence supporting the different decisions physicians reach regarding end-of-life care.
He quoted a 2003 article by Joseph Gallo and associates, who surveyed participants in the Johns Hopkins Precursors Study, which covered physicians graduating from Hopkins between 1948 and 1964. The investigators obtained responses from nearly 800 physicians regarding their end-of-life decisions. Compared with 20% of the general public, 64% of physician respondents had created an advanced directive. Additionally, nearly 90% of the physicians did not want CPR if they were in a chronic coma. This contrasts with about 25% of the general public not desiring "heroic measures." Clearly, physicians were taking the initiative and outlining the care that they did and did not want to receive in the setting of advanced medical illness.
Murray also mentioned a 1996 study that examined how CPR was portrayed in television shows and the potential impact it may have on patients’ decision making. In that paper, CPR was successful in 75% of the TV cases, with 67% of patients ultimately being discharged from the hospital (N. Engl. J. Med. 1996;334:1578-82).
Compare this with what we know to be true. CPR rarely works. A 2010 study that evaluated the impact of 95,000 cases of CPR in Japan demonstrated that clearly. Only 8% of patients who had received CPR survived for more than 1 month. Of those who survived, only 3% were able to lead "normal" lives.
Based upon our experiences, we are able to make objective assessments of the likelihood of success of various therapies in our patients. As hospitalists, we are often placed in the position of helping explain therapies provided by other specialists – cardiologists, oncologists, surgeons. I know that there have been times when I have seen patients receiving treatments I considered futile. I believe many of us have been in similar situations. Patients do not fully understand the risks and benefits of their therapy. Once the big picture is made clear to them, they often opt for more conservative therapy aimed at improving quality of life.
I believe we have an obligation to our patients to share with them the reality of the care they receive. We need to check in with our patients and understand what is important to them. Do they want to exhaust every medical option available? Are they looking to live long enough to attend a graduation or wedding? Do they value comfort and quality time above all else? We need to ask these questions and fully understand our patients and their desires.
I wrote previously about my former colleague Darlene. Had I not known her desires regarding continued therapy, she would have received care she did not want. I am certain of this because she was in the process of being transferred to the intensive care unit when I intervened at the behest of a mutual friend. She would have received several days of great, high-tech care in the ICU – and ultimately died despite that care, care that she did not want in the first place.
We, as hospitalists, must talk with our patients about their wishes. We must educate them about the likelihood of success of their therapies and of CPR. We must act as their advocates with subspecialists who too often focus on their specific portion of the patient, losing sight of the bigger picture. We need to do better. We need to ask the question: Should doctors die differently?
If advanced directives and dying in comfort are good enough for us, they should be good enough for our patients.
Dr. Pistoria is chief of hospital medicine at Coordinated Health in Bethlehem, Pa. He believes that the best care is always personal.
CMS finalizes rules for reporting physician-industry payments
Federal health officials have finally released the details on how online public reporting of industry payments to physicians will work.
Under the final rule released on Feb. 1 by the Centers for Medicare and Medicaid Services (CMS), drug, device, and medical supply manufacturers who participate in Medicare, Medicaid, or the Children’s Health Insurance Program will be required to submit annual reports to the federal government on any payments of $10 or more that they made to physicians and teaching hospitals. They also will be required to report on all payments if the payments and transfers of value to a single physician reach $100 in aggregate value for a year.
Manufacturers and group purchasing organizations (GPOs) must also report on physician ownership and investment interests each year. CMS will post the information on a public website. The requirements are mandated under the Affordable Care Act (ACA).
"You should know when your doctor has a financial relationship with the companies that manufacture or supply the medicines or medical devices you may need," Dr. Peter Budetti, CMS deputy administrator for Program Integrity, said in a statement. "Disclosure of these relationships allows patients to have more informed discussions with their doctors."
Manufacturers and GPOs have until Aug. 1 to begin collecting data. They must submit their reports on payments made in 2013 by March 31, 2014. CMS will post the data online by Sept. 30, 2014.
CMS did not meet the deadline set by law for issuing this final regulation: Under the ACA, data collection was supposed to begin in January 2012.
The final rule contains plenty of exceptions, however. For instance, reporting is not required for gifts between individuals with an existing personal relationship. Other exclusions include small payments of less than $10, educational materials that directly benefit patients or are intended for patient use, discounts for rebates for drugs and devices, in-kind items for charity care, and samples.
Indirect payments made to speakers at accredited or certified continuing medical education (CME) events also do not need to be reported as long as the manufacturer doesn’t suggest speakers.
The final rule also clarifies that companies sponsoring large-scale conferences do not need to track and report on small gifts and food items worth less than $10 such as pens and bottles of water. These items also won’t count toward the minimum yearly reporting threshold of $100, according to CMS.
"I think this will make life easier, because it will contribute toward a more relaxed atmosphere at meetings so that attendees won’t have to worry every time they pick up a bottle of water or a granola bar," said Dr. Daniel Carlat, project director for the Pew Prescription Project, which works for greater transparency in physician-industry relationships.
Dr. Carlat said the final rule strikes the right balance between increasing payment transparency and not overburdening physicians with the requirements.
Although the data collection and reporting requirements are on the drug and device industry, physicians are responsible for reviewing their information before publication. Under the final rule, physicians will have 45 days to review the reports and another 15 days to work with the manufacturers to correct any disputed reports. After that, if there are still disputes, the information will be posted publicly but will include a disclaimer that it is disputed, according to the final rule.
The new transparency initiative will likely enhance the public’s trust and confidence in their physicians, Dr. Carlat said. Consumers often hear about the worst-case scenarios, where physicians are taking millions of dollars that may cause conflicts of interest, but the new reporting is likely to show that is rare, he said.
"I think we’ll find with these transparency reports that the vast majority of payments and gifts are of very low value and are the equivalent of $50 to $100 or a few hundred dollars a year," Dr. Carlat said. "I think when patients see these figures, their concerns about relationships between doctors and companies will be to some extent allayed."
Federal health officials have finally released the details on how online public reporting of industry payments to physicians will work.
Under the final rule released on Feb. 1 by the Centers for Medicare and Medicaid Services (CMS), drug, device, and medical supply manufacturers who participate in Medicare, Medicaid, or the Children’s Health Insurance Program will be required to submit annual reports to the federal government on any payments of $10 or more that they made to physicians and teaching hospitals. They also will be required to report on all payments if the payments and transfers of value to a single physician reach $100 in aggregate value for a year.
Manufacturers and group purchasing organizations (GPOs) must also report on physician ownership and investment interests each year. CMS will post the information on a public website. The requirements are mandated under the Affordable Care Act (ACA).
"You should know when your doctor has a financial relationship with the companies that manufacture or supply the medicines or medical devices you may need," Dr. Peter Budetti, CMS deputy administrator for Program Integrity, said in a statement. "Disclosure of these relationships allows patients to have more informed discussions with their doctors."
Manufacturers and GPOs have until Aug. 1 to begin collecting data. They must submit their reports on payments made in 2013 by March 31, 2014. CMS will post the data online by Sept. 30, 2014.
CMS did not meet the deadline set by law for issuing this final regulation: Under the ACA, data collection was supposed to begin in January 2012.
The final rule contains plenty of exceptions, however. For instance, reporting is not required for gifts between individuals with an existing personal relationship. Other exclusions include small payments of less than $10, educational materials that directly benefit patients or are intended for patient use, discounts for rebates for drugs and devices, in-kind items for charity care, and samples.
Indirect payments made to speakers at accredited or certified continuing medical education (CME) events also do not need to be reported as long as the manufacturer doesn’t suggest speakers.
The final rule also clarifies that companies sponsoring large-scale conferences do not need to track and report on small gifts and food items worth less than $10 such as pens and bottles of water. These items also won’t count toward the minimum yearly reporting threshold of $100, according to CMS.
"I think this will make life easier, because it will contribute toward a more relaxed atmosphere at meetings so that attendees won’t have to worry every time they pick up a bottle of water or a granola bar," said Dr. Daniel Carlat, project director for the Pew Prescription Project, which works for greater transparency in physician-industry relationships.
Dr. Carlat said the final rule strikes the right balance between increasing payment transparency and not overburdening physicians with the requirements.
Although the data collection and reporting requirements are on the drug and device industry, physicians are responsible for reviewing their information before publication. Under the final rule, physicians will have 45 days to review the reports and another 15 days to work with the manufacturers to correct any disputed reports. After that, if there are still disputes, the information will be posted publicly but will include a disclaimer that it is disputed, according to the final rule.
The new transparency initiative will likely enhance the public’s trust and confidence in their physicians, Dr. Carlat said. Consumers often hear about the worst-case scenarios, where physicians are taking millions of dollars that may cause conflicts of interest, but the new reporting is likely to show that is rare, he said.
"I think we’ll find with these transparency reports that the vast majority of payments and gifts are of very low value and are the equivalent of $50 to $100 or a few hundred dollars a year," Dr. Carlat said. "I think when patients see these figures, their concerns about relationships between doctors and companies will be to some extent allayed."
Federal health officials have finally released the details on how online public reporting of industry payments to physicians will work.
Under the final rule released on Feb. 1 by the Centers for Medicare and Medicaid Services (CMS), drug, device, and medical supply manufacturers who participate in Medicare, Medicaid, or the Children’s Health Insurance Program will be required to submit annual reports to the federal government on any payments of $10 or more that they made to physicians and teaching hospitals. They also will be required to report on all payments if the payments and transfers of value to a single physician reach $100 in aggregate value for a year.
Manufacturers and group purchasing organizations (GPOs) must also report on physician ownership and investment interests each year. CMS will post the information on a public website. The requirements are mandated under the Affordable Care Act (ACA).
"You should know when your doctor has a financial relationship with the companies that manufacture or supply the medicines or medical devices you may need," Dr. Peter Budetti, CMS deputy administrator for Program Integrity, said in a statement. "Disclosure of these relationships allows patients to have more informed discussions with their doctors."
Manufacturers and GPOs have until Aug. 1 to begin collecting data. They must submit their reports on payments made in 2013 by March 31, 2014. CMS will post the data online by Sept. 30, 2014.
CMS did not meet the deadline set by law for issuing this final regulation: Under the ACA, data collection was supposed to begin in January 2012.
The final rule contains plenty of exceptions, however. For instance, reporting is not required for gifts between individuals with an existing personal relationship. Other exclusions include small payments of less than $10, educational materials that directly benefit patients or are intended for patient use, discounts for rebates for drugs and devices, in-kind items for charity care, and samples.
Indirect payments made to speakers at accredited or certified continuing medical education (CME) events also do not need to be reported as long as the manufacturer doesn’t suggest speakers.
The final rule also clarifies that companies sponsoring large-scale conferences do not need to track and report on small gifts and food items worth less than $10 such as pens and bottles of water. These items also won’t count toward the minimum yearly reporting threshold of $100, according to CMS.
"I think this will make life easier, because it will contribute toward a more relaxed atmosphere at meetings so that attendees won’t have to worry every time they pick up a bottle of water or a granola bar," said Dr. Daniel Carlat, project director for the Pew Prescription Project, which works for greater transparency in physician-industry relationships.
Dr. Carlat said the final rule strikes the right balance between increasing payment transparency and not overburdening physicians with the requirements.
Although the data collection and reporting requirements are on the drug and device industry, physicians are responsible for reviewing their information before publication. Under the final rule, physicians will have 45 days to review the reports and another 15 days to work with the manufacturers to correct any disputed reports. After that, if there are still disputes, the information will be posted publicly but will include a disclaimer that it is disputed, according to the final rule.
The new transparency initiative will likely enhance the public’s trust and confidence in their physicians, Dr. Carlat said. Consumers often hear about the worst-case scenarios, where physicians are taking millions of dollars that may cause conflicts of interest, but the new reporting is likely to show that is rare, he said.
"I think we’ll find with these transparency reports that the vast majority of payments and gifts are of very low value and are the equivalent of $50 to $100 or a few hundred dollars a year," Dr. Carlat said. "I think when patients see these figures, their concerns about relationships between doctors and companies will be to some extent allayed."
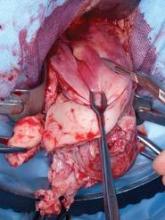
Hybrid CFV endovenectomy promising, but not for the faint at heart
CHICAGO – Common femoral endovenectomy with endoluminal iliac recanalization should be considered in patients with chronic post-thrombotic iliofemoral venous obstruction.
The procedure substantially reduces post-thrombotic syndrome morbidity and improves quality of life, although it "is not a procedure for the faint of heart," acknowledged Dr. Anthony Comerota, director of the Jobst Vascular Center at ProMedica Toledo (Ohio) Hospital.
Postthrombotic syndrome occurs in 30%-40% of all patients with a lower-extremity deep vein thrombosis (DVT) at 2 years, despite the use of anticoagulation. Postthrombotic syndrome can be particularly debilitating following an iliofemoral DVT if the common femoral vein (CFV) is badly obstructed or occluded, resulting in such poor quality of life that Dr. Comerota compared it with angina, cancer, and congestive heart failure.
Stenting and angioplasty are often successful in treating postthrombotic iliac vein occlusion, although the risk of stent occlusion is at least 3.8-fold higher in postthrombotic limbs if the stent is extended below the inguinal ligament, he noted.
Relative obstruction of the CFV also can persist after percutaneous intervention and compromise drainage from the profunda femoris vein. This mitigates the benefits of iliac vein recanalization and can actually worsen the patient’s post-thrombotic symptoms, Dr. Comerota said at a symposium on vascular surgery sponsored by Northwestern University.
"It is crucial to open up the orifice of the profunda," he said. "One of the problems we’ve seen in patients referred to us is that, when the common femoral was stented and the stent takes that fibrous tissue and plasters it up against the orifice of the profunda, if there was any minimal drainage from the profunda, it will obliterate it and those patients got worse."
Having previously detailed the technical aspects of the procedure (J. Vasc. Surg. 2012;55:129-35), Dr. Comerota highlighted outcomes of 14 patients and 16 limbs treated to date for severe post-thrombotic, iliofemoral/caval venous obstruction with CEAP (clinical severity, etiology, anatomy, pathophysiology) classification of C3-C6. The median duration of obstruction was nearly 7 years (range, 7 months to 25 years) and median follow-up 3 years (range, 5 months to 6 years). Two patients were lost to follow-up.
To date, one death occurred in a 52-year-old woman with multiple cardiovascular risk factors 9 days after discharge because of an acute myocardial infarction, Dr. Comerota said.
Three patients required surgical evacuation of wound hematomas and three developed early postoperative thrombosis treated with lysis in two cases and thrombectomy in one. All three patients were discharged with patency restored.
One segmental occlusion of the CFV has occurred, and a recent patient with longstanding sickle cell disease developed significant acute lymphedema "that we are still at a loss to explain," he said.
At 6 months, significant improvements were observed in preoperative scores on the Villalta scale (mean, 14 vs. 6; P = .002), Venous Clinical Severity Score (mean, 17 vs. 10; P = .02), CEAP (mean, 4.8 vs. 3.8; P less than .05) and Venous Insufficiency Epidemiological and Economic Study-Quality of Life/Sym questionnaire (data not provided; P = .01).
In some patients, the turnaround was quite dramatic, observed Dr. Comerota, who described a patient who suffered severe trauma and was unable to be anticoagulated. He subsequently had chronic iliofemoral and caval obstruction causing a swollen limb and a painful ulcer for 4 years. The day after surgery, there was remarkable change in the color of the ulcer and leg, and within 3 months the ulcer was completely healed, most of the edema was controlled, and his legs were no longer painful to compression, he said. The patient is back to full activity and has lost 30 pounds.
As a result of inactivity, many of the patients had gained a significant amount of weight, thereby requiring a large incision.
"It is a big procedure," said Dr. Comerota, adding that "it is certainly a procedure in evolution."
Some of the issues requiring further study include the risk/benefit of combined preoperative platelet inhibition and the optimal postoperative anticoagulation; location of an arteriovenous (AV) fistula; and size of the wound drain, currently a 7F closed suction drain.
Three days prior to the procedure, patients receive platelet inhibition with aspirin 81 mg/day and clopidogrel 75 mg/day and twice-daily chlorhexidine showers.
On the day of surgery, patients are fully anticoagulated with 100 IU/kg of unfractionated heparin. It is not reversed with protamine after the surgery is complete, but rather followed with a standard intravenous therapeutic heparin infusion, he said. To reduce the need for supratherapeutic systemic anticoagulation in some patients, a silastic intravenous catheter was placed in a dorsal foot vein to infuse the postoperative heparin.
A small AV fistula of 3.5-4 mm has been required in about half of procedures after continuous wave Doppler failed to identify robust venous velocity signals. The goal of the AV fistula is to increase velocity but not venous pressure, and it has typically been constructed with a wrap around the greater saphenous vein to ensure that it will not enlarge over time, Dr. Comerota said.
"I’ve never been sorry I did an AV fistula. I certainly have been sorry that I have not, so now it’s a routine part of the procedure," he added.
If an iliac venous stenosis or occlusion needs to be stented, Dr. Comerota said that he prefers Wallstents.
"I’m not sure if radial strength is the best term, but Wallstents have the best compression to pressure," he explained. "We’ve used Nitinol [stents] earlier on in our experience, but we had to go back in and reline 50% to 60% of them because they just didn’t hold up the vein properly."
Initially, the team also attempted to keep the stents above the inguinal ligament, but it now takes the approach that the iliac venous occlusion can be stented into the endovenectomized portion of the external iliac vein or CFV, with the caveat that the distal end of the stent must stay above the saphenofemoral junction to preserve profunda femoris venous drainage. Stenting avoids skip lesions that might lead to recurrent thrombosis or continued functional compromise, Dr. Comerota noted.
During a discussion of the procedure, he said that symptomatic presentation and degree of disability are used to determine whether patients should undergo the rigorous procedure.
Surgeons at the Mayo Clinic reported far less promising results in 12 patients who underwent CFV endovenectomy, patch angioplasty, and stenting for chronic iliofemoral venous obstruction, with a 30% 2-year patency and 50% of ulcers with patent grafts recurring (J. Vasc. Surg. 2011;53:383-93).
Dr. Comerata presents an aggressive approach to venous obstructive disease, with operative resection of the fibrotic tissue within the common femoral vein, coupled with endovascular stenting of the iliac segment. He reports relatively good results for these complex patients with a large operative procedure. Other groups have yet to replicate his results and the study population is still relatively small. Certainly, this technique is worth further prospective assessment, as this patient population does experience fairly debilitating symptoms. Whether open surgical treatment coupled with endovascular intervention is the best option remains to be seen.
Dr. Linda Harris is chief of the division of vascular surgery at the State University of New York, Buffalo. Dr. Harris stated that she had no disclosures.
Dr. Comerata presents an aggressive approach to venous obstructive disease, with operative resection of the fibrotic tissue within the common femoral vein, coupled with endovascular stenting of the iliac segment. He reports relatively good results for these complex patients with a large operative procedure. Other groups have yet to replicate his results and the study population is still relatively small. Certainly, this technique is worth further prospective assessment, as this patient population does experience fairly debilitating symptoms. Whether open surgical treatment coupled with endovascular intervention is the best option remains to be seen.
Dr. Linda Harris is chief of the division of vascular surgery at the State University of New York, Buffalo. Dr. Harris stated that she had no disclosures.
Dr. Comerata presents an aggressive approach to venous obstructive disease, with operative resection of the fibrotic tissue within the common femoral vein, coupled with endovascular stenting of the iliac segment. He reports relatively good results for these complex patients with a large operative procedure. Other groups have yet to replicate his results and the study population is still relatively small. Certainly, this technique is worth further prospective assessment, as this patient population does experience fairly debilitating symptoms. Whether open surgical treatment coupled with endovascular intervention is the best option remains to be seen.
Dr. Linda Harris is chief of the division of vascular surgery at the State University of New York, Buffalo. Dr. Harris stated that she had no disclosures.
CHICAGO – Common femoral endovenectomy with endoluminal iliac recanalization should be considered in patients with chronic post-thrombotic iliofemoral venous obstruction.
The procedure substantially reduces post-thrombotic syndrome morbidity and improves quality of life, although it "is not a procedure for the faint of heart," acknowledged Dr. Anthony Comerota, director of the Jobst Vascular Center at ProMedica Toledo (Ohio) Hospital.
Postthrombotic syndrome occurs in 30%-40% of all patients with a lower-extremity deep vein thrombosis (DVT) at 2 years, despite the use of anticoagulation. Postthrombotic syndrome can be particularly debilitating following an iliofemoral DVT if the common femoral vein (CFV) is badly obstructed or occluded, resulting in such poor quality of life that Dr. Comerota compared it with angina, cancer, and congestive heart failure.
Stenting and angioplasty are often successful in treating postthrombotic iliac vein occlusion, although the risk of stent occlusion is at least 3.8-fold higher in postthrombotic limbs if the stent is extended below the inguinal ligament, he noted.
Relative obstruction of the CFV also can persist after percutaneous intervention and compromise drainage from the profunda femoris vein. This mitigates the benefits of iliac vein recanalization and can actually worsen the patient’s post-thrombotic symptoms, Dr. Comerota said at a symposium on vascular surgery sponsored by Northwestern University.
"It is crucial to open up the orifice of the profunda," he said. "One of the problems we’ve seen in patients referred to us is that, when the common femoral was stented and the stent takes that fibrous tissue and plasters it up against the orifice of the profunda, if there was any minimal drainage from the profunda, it will obliterate it and those patients got worse."
Having previously detailed the technical aspects of the procedure (J. Vasc. Surg. 2012;55:129-35), Dr. Comerota highlighted outcomes of 14 patients and 16 limbs treated to date for severe post-thrombotic, iliofemoral/caval venous obstruction with CEAP (clinical severity, etiology, anatomy, pathophysiology) classification of C3-C6. The median duration of obstruction was nearly 7 years (range, 7 months to 25 years) and median follow-up 3 years (range, 5 months to 6 years). Two patients were lost to follow-up.
To date, one death occurred in a 52-year-old woman with multiple cardiovascular risk factors 9 days after discharge because of an acute myocardial infarction, Dr. Comerota said.
Three patients required surgical evacuation of wound hematomas and three developed early postoperative thrombosis treated with lysis in two cases and thrombectomy in one. All three patients were discharged with patency restored.
One segmental occlusion of the CFV has occurred, and a recent patient with longstanding sickle cell disease developed significant acute lymphedema "that we are still at a loss to explain," he said.
At 6 months, significant improvements were observed in preoperative scores on the Villalta scale (mean, 14 vs. 6; P = .002), Venous Clinical Severity Score (mean, 17 vs. 10; P = .02), CEAP (mean, 4.8 vs. 3.8; P less than .05) and Venous Insufficiency Epidemiological and Economic Study-Quality of Life/Sym questionnaire (data not provided; P = .01).
In some patients, the turnaround was quite dramatic, observed Dr. Comerota, who described a patient who suffered severe trauma and was unable to be anticoagulated. He subsequently had chronic iliofemoral and caval obstruction causing a swollen limb and a painful ulcer for 4 years. The day after surgery, there was remarkable change in the color of the ulcer and leg, and within 3 months the ulcer was completely healed, most of the edema was controlled, and his legs were no longer painful to compression, he said. The patient is back to full activity and has lost 30 pounds.
As a result of inactivity, many of the patients had gained a significant amount of weight, thereby requiring a large incision.
"It is a big procedure," said Dr. Comerota, adding that "it is certainly a procedure in evolution."
Some of the issues requiring further study include the risk/benefit of combined preoperative platelet inhibition and the optimal postoperative anticoagulation; location of an arteriovenous (AV) fistula; and size of the wound drain, currently a 7F closed suction drain.
Three days prior to the procedure, patients receive platelet inhibition with aspirin 81 mg/day and clopidogrel 75 mg/day and twice-daily chlorhexidine showers.
On the day of surgery, patients are fully anticoagulated with 100 IU/kg of unfractionated heparin. It is not reversed with protamine after the surgery is complete, but rather followed with a standard intravenous therapeutic heparin infusion, he said. To reduce the need for supratherapeutic systemic anticoagulation in some patients, a silastic intravenous catheter was placed in a dorsal foot vein to infuse the postoperative heparin.
A small AV fistula of 3.5-4 mm has been required in about half of procedures after continuous wave Doppler failed to identify robust venous velocity signals. The goal of the AV fistula is to increase velocity but not venous pressure, and it has typically been constructed with a wrap around the greater saphenous vein to ensure that it will not enlarge over time, Dr. Comerota said.
"I’ve never been sorry I did an AV fistula. I certainly have been sorry that I have not, so now it’s a routine part of the procedure," he added.
If an iliac venous stenosis or occlusion needs to be stented, Dr. Comerota said that he prefers Wallstents.
"I’m not sure if radial strength is the best term, but Wallstents have the best compression to pressure," he explained. "We’ve used Nitinol [stents] earlier on in our experience, but we had to go back in and reline 50% to 60% of them because they just didn’t hold up the vein properly."
Initially, the team also attempted to keep the stents above the inguinal ligament, but it now takes the approach that the iliac venous occlusion can be stented into the endovenectomized portion of the external iliac vein or CFV, with the caveat that the distal end of the stent must stay above the saphenofemoral junction to preserve profunda femoris venous drainage. Stenting avoids skip lesions that might lead to recurrent thrombosis or continued functional compromise, Dr. Comerota noted.
During a discussion of the procedure, he said that symptomatic presentation and degree of disability are used to determine whether patients should undergo the rigorous procedure.
Surgeons at the Mayo Clinic reported far less promising results in 12 patients who underwent CFV endovenectomy, patch angioplasty, and stenting for chronic iliofemoral venous obstruction, with a 30% 2-year patency and 50% of ulcers with patent grafts recurring (J. Vasc. Surg. 2011;53:383-93).
CHICAGO – Common femoral endovenectomy with endoluminal iliac recanalization should be considered in patients with chronic post-thrombotic iliofemoral venous obstruction.
The procedure substantially reduces post-thrombotic syndrome morbidity and improves quality of life, although it "is not a procedure for the faint of heart," acknowledged Dr. Anthony Comerota, director of the Jobst Vascular Center at ProMedica Toledo (Ohio) Hospital.
Postthrombotic syndrome occurs in 30%-40% of all patients with a lower-extremity deep vein thrombosis (DVT) at 2 years, despite the use of anticoagulation. Postthrombotic syndrome can be particularly debilitating following an iliofemoral DVT if the common femoral vein (CFV) is badly obstructed or occluded, resulting in such poor quality of life that Dr. Comerota compared it with angina, cancer, and congestive heart failure.
Stenting and angioplasty are often successful in treating postthrombotic iliac vein occlusion, although the risk of stent occlusion is at least 3.8-fold higher in postthrombotic limbs if the stent is extended below the inguinal ligament, he noted.
Relative obstruction of the CFV also can persist after percutaneous intervention and compromise drainage from the profunda femoris vein. This mitigates the benefits of iliac vein recanalization and can actually worsen the patient’s post-thrombotic symptoms, Dr. Comerota said at a symposium on vascular surgery sponsored by Northwestern University.
"It is crucial to open up the orifice of the profunda," he said. "One of the problems we’ve seen in patients referred to us is that, when the common femoral was stented and the stent takes that fibrous tissue and plasters it up against the orifice of the profunda, if there was any minimal drainage from the profunda, it will obliterate it and those patients got worse."
Having previously detailed the technical aspects of the procedure (J. Vasc. Surg. 2012;55:129-35), Dr. Comerota highlighted outcomes of 14 patients and 16 limbs treated to date for severe post-thrombotic, iliofemoral/caval venous obstruction with CEAP (clinical severity, etiology, anatomy, pathophysiology) classification of C3-C6. The median duration of obstruction was nearly 7 years (range, 7 months to 25 years) and median follow-up 3 years (range, 5 months to 6 years). Two patients were lost to follow-up.
To date, one death occurred in a 52-year-old woman with multiple cardiovascular risk factors 9 days after discharge because of an acute myocardial infarction, Dr. Comerota said.
Three patients required surgical evacuation of wound hematomas and three developed early postoperative thrombosis treated with lysis in two cases and thrombectomy in one. All three patients were discharged with patency restored.
One segmental occlusion of the CFV has occurred, and a recent patient with longstanding sickle cell disease developed significant acute lymphedema "that we are still at a loss to explain," he said.
At 6 months, significant improvements were observed in preoperative scores on the Villalta scale (mean, 14 vs. 6; P = .002), Venous Clinical Severity Score (mean, 17 vs. 10; P = .02), CEAP (mean, 4.8 vs. 3.8; P less than .05) and Venous Insufficiency Epidemiological and Economic Study-Quality of Life/Sym questionnaire (data not provided; P = .01).
In some patients, the turnaround was quite dramatic, observed Dr. Comerota, who described a patient who suffered severe trauma and was unable to be anticoagulated. He subsequently had chronic iliofemoral and caval obstruction causing a swollen limb and a painful ulcer for 4 years. The day after surgery, there was remarkable change in the color of the ulcer and leg, and within 3 months the ulcer was completely healed, most of the edema was controlled, and his legs were no longer painful to compression, he said. The patient is back to full activity and has lost 30 pounds.
As a result of inactivity, many of the patients had gained a significant amount of weight, thereby requiring a large incision.
"It is a big procedure," said Dr. Comerota, adding that "it is certainly a procedure in evolution."
Some of the issues requiring further study include the risk/benefit of combined preoperative platelet inhibition and the optimal postoperative anticoagulation; location of an arteriovenous (AV) fistula; and size of the wound drain, currently a 7F closed suction drain.
Three days prior to the procedure, patients receive platelet inhibition with aspirin 81 mg/day and clopidogrel 75 mg/day and twice-daily chlorhexidine showers.
On the day of surgery, patients are fully anticoagulated with 100 IU/kg of unfractionated heparin. It is not reversed with protamine after the surgery is complete, but rather followed with a standard intravenous therapeutic heparin infusion, he said. To reduce the need for supratherapeutic systemic anticoagulation in some patients, a silastic intravenous catheter was placed in a dorsal foot vein to infuse the postoperative heparin.
A small AV fistula of 3.5-4 mm has been required in about half of procedures after continuous wave Doppler failed to identify robust venous velocity signals. The goal of the AV fistula is to increase velocity but not venous pressure, and it has typically been constructed with a wrap around the greater saphenous vein to ensure that it will not enlarge over time, Dr. Comerota said.
"I’ve never been sorry I did an AV fistula. I certainly have been sorry that I have not, so now it’s a routine part of the procedure," he added.
If an iliac venous stenosis or occlusion needs to be stented, Dr. Comerota said that he prefers Wallstents.
"I’m not sure if radial strength is the best term, but Wallstents have the best compression to pressure," he explained. "We’ve used Nitinol [stents] earlier on in our experience, but we had to go back in and reline 50% to 60% of them because they just didn’t hold up the vein properly."
Initially, the team also attempted to keep the stents above the inguinal ligament, but it now takes the approach that the iliac venous occlusion can be stented into the endovenectomized portion of the external iliac vein or CFV, with the caveat that the distal end of the stent must stay above the saphenofemoral junction to preserve profunda femoris venous drainage. Stenting avoids skip lesions that might lead to recurrent thrombosis or continued functional compromise, Dr. Comerota noted.
During a discussion of the procedure, he said that symptomatic presentation and degree of disability are used to determine whether patients should undergo the rigorous procedure.
Surgeons at the Mayo Clinic reported far less promising results in 12 patients who underwent CFV endovenectomy, patch angioplasty, and stenting for chronic iliofemoral venous obstruction, with a 30% 2-year patency and 50% of ulcers with patent grafts recurring (J. Vasc. Surg. 2011;53:383-93).
AT A SYMPOSIUM ON VASCULAR SURGERY SPONSORED BY NORTHWESTERN UNIVERSITY
Major Finding: At 6 months, significant improvements were observed in preoperative scores on the Villalta scale (mean 14 vs. 6; P = .002), Venous Clinical Severity Score (mean 17 vs. 10; P = .02), and CEAP (mean 4.8 vs. 3.8; P less than .05).
Data Source: Outcomes of 14 patients and 16 limbs treated to date for severe post-thrombotic, iliofemoral/caval venous obstruction with CEAP classification of C3-C6.
Disclosures: Dr. Comerota reported no relevant conflicts of interest.
Preserving Medicaid at Medicare's expense?: The Policy & Practice podcast
As the White House prepares its fiscal roadmap to deficit reduction, it’s not clear what role the looming cuts under sequestration will play. However, one of President Obama’s top economists said the administration will fight to keep Medicaid off the chopping block. So, that leaves Medicare exposed to potential cuts.
Meanwhile, health economists are questioning the effectiveness of the individual insurance mandate, saying that exemptions included in the recently proposed rule highlight the mandate’s weakness.
Among the exempted are the incarcerated, American Indians, and the Medicaid-eligible living in states that aren’t expanding the program. Princeton policy expert Uwe Reinhardt said the mandate is anything but – and young people likely will find it cheaper to just pay the penalty.
To hear more, and for details about how the feds are testing bundled payments for doctors and hospitals, check out this week’s Policy & Practice podcast.
- Frances Correa (@FMCReporting)
As the White House prepares its fiscal roadmap to deficit reduction, it’s not clear what role the looming cuts under sequestration will play. However, one of President Obama’s top economists said the administration will fight to keep Medicaid off the chopping block. So, that leaves Medicare exposed to potential cuts.
Meanwhile, health economists are questioning the effectiveness of the individual insurance mandate, saying that exemptions included in the recently proposed rule highlight the mandate’s weakness.
Among the exempted are the incarcerated, American Indians, and the Medicaid-eligible living in states that aren’t expanding the program. Princeton policy expert Uwe Reinhardt said the mandate is anything but – and young people likely will find it cheaper to just pay the penalty.
To hear more, and for details about how the feds are testing bundled payments for doctors and hospitals, check out this week’s Policy & Practice podcast.
- Frances Correa (@FMCReporting)
As the White House prepares its fiscal roadmap to deficit reduction, it’s not clear what role the looming cuts under sequestration will play. However, one of President Obama’s top economists said the administration will fight to keep Medicaid off the chopping block. So, that leaves Medicare exposed to potential cuts.
Meanwhile, health economists are questioning the effectiveness of the individual insurance mandate, saying that exemptions included in the recently proposed rule highlight the mandate’s weakness.
Among the exempted are the incarcerated, American Indians, and the Medicaid-eligible living in states that aren’t expanding the program. Princeton policy expert Uwe Reinhardt said the mandate is anything but – and young people likely will find it cheaper to just pay the penalty.
To hear more, and for details about how the feds are testing bundled payments for doctors and hospitals, check out this week’s Policy & Practice podcast.
- Frances Correa (@FMCReporting)
Pregnancy and Marfan: New insight into risks
SNOWMASS, COLO–Pregnancy increases the long-term risk of aortic complications in women with Marfan syndrome, according to a recent prospective study causing a stir among adult congenital heart disease specialists.
"This is the first study that says, ‘Even if the aortic root size is okay before pregnancy, the aorta is going to get bigger during pregnancy and it’s not going to go back to baseline. And if your aorta is bigger at the outset, there is a risk for long-term adverse outcomes,’ " Dr. Carole A. Warnes explained at the annual cardiovascular conference at Snowmass sponsored by the American College of Cardiology (ACC).
This study on pregnancy’s impact on aortic growth rate and complications in patients with Marfan syndrome sheds much needed light on an area where there has been a paucity of data. The deficiency of data is reflected in discordant recommendations in the current U.S., European, and Canadian guidelines, said Dr. Warnes, professor of medicine at the Mayo Clinic, Rochester, Minn.
The U.S. guidelines put forth jointly by the ACC, American Heart Association, American Association for Thoracic Surgery, and other groups advocate that Marfan syndrome patients avoid pregnancy if their aortic root diameter exceeds 40 mm and recommend prophylactic aortic replacement in those interested in pregnancy (J. Am. Coll. Cardiol. 2010;55:e27-129).
In contrast, the European guidelines (Eur. Heart J. 2010;31:2915-57) consider an aortic root diameter of 45 mm or less to be generally safe, while strongly discouraging pregnancy in Marfan syndrome patients with a measurement above that threshold because of the associated increased dissection risk. The Canadian guidelines take a similar stance, albeit with a safety threshold of 44 mm rather than 45 mm (Can. J. Cardiol. 2010;26:e80-e97).
The Europeans qualify their position by noting that patients with a prepregnancy aortic root diameter of 40-45 mm who have a rapid aortic root growth rate or a family history of dissection ought to be considered high risk for pregnancy. The European and Canadian guidelines characterize dissection as a rare problem in patients with an aortic root diameter of less than 40 mm.
The recent Utah study included 98 women with Marfan syndrome, 69 of whom collectively had 199 pregnancies, with 170 live births, 26 spontaneous abortions, and 2 ectopic pregnancies.
Serial echocardiograms demonstrated that the aortic growth rate was significantly greater during pregnancy than beforehand, and after pregnancy it didn’t return to baseline. Obstetric complications occurred in 10% of pregnancies. Adverse fetal outcomes occurred in 13%.
Reassuringly, there were no catastrophic peripartum complications. No one required cardiac surgery or experienced aortic dissection during pregnancy. However, women with a prior pregnancy had a greater prevalence of both aortic dissection and elective aortic surgery during long-term follow-up, compared with matched childless women with Marfan syndrome. Thus, it’s important during prepregnancy counseling of women with Marfan syndrome to let them know they’ll need to have elective aortic root surgery at a younger age than if they remain childless, Dr. Warnes noted.
A larger initial root diameter and a faster increase in diameter were independent predictors of long-term adverse cardiovascular events in the Utah study.
Besides the recent Utah study, only two other prospective studies of pregnancy’s impact on aortic growth and complications have been done. Both were much smaller. In an editorial accompanying the Utah study, Dutch physicians combined the three studies to get a fuller picture. No type A dissections occurred during 145 pregnancies in 78 nonoperated women with Marfan syndrome. Of 25 women with an aortic root diameter of 40-51 mm during 29 pregnancies, one experienced a type B dissection, two had carotid artery dissections, and one developed accelerated aortic regurgitation, which went from mild to severe during pregnancy.
Five women underwent aortic root replacement (three electively), prior to six pregnancies. Two of them developed a type B dissection during pregnancy. Both women who underwent a valve-sparing elective aortic root replacement prior to pregnancy had pregnancies complicated by a worsening of aortic regurgitation, which went from trivial to moderate. These findings raise a red flag for Dr. Warnes.
"Even if they’ve had a successful root replacement, it doesn’t mean they’re out of the woods in terms of pregnancy. I think we have to question the role of prophylactic root replacement [as recommended in the U.S. guidelines] because these women will still have type B dissections, and trying to look for a type B dissection during pregnancy is a real difficult issue," the cardiologist observed.
The authors of the editorial concluded that Marfan syndrome patients without previous cardiac complications and who have a baseline aortic root diameter not in excess of 45 mm seem to tolerate pregnancy well as long as they receive good clinical care before, during, and after pregnancy. In contrast, pregnancy should be discouraged in patients with a history of aortic dissection because they are at elevated risk for aortic complications (J. Am. Coll. Cardiol. 2012;60:230-1).
Marfan syndrome is a genetic connective tissue disorder with an incidence of roughly 1 in 5,000 and autosomal dominant inheritance, so the fetus of an affected mom has a 50% chance of having the disorder. Dr. Warnes said that because the diagnostic criteria were overhauled in 2010, patients believed to have Marfan syndrome really ought to be referred to a specialized center in order to confirm or refute the diagnosis according to the contemporary Ghent criteria.
Dr. Warnes reported having no relevant financial interests.
SNOWMASS, COLO–Pregnancy increases the long-term risk of aortic complications in women with Marfan syndrome, according to a recent prospective study causing a stir among adult congenital heart disease specialists.
"This is the first study that says, ‘Even if the aortic root size is okay before pregnancy, the aorta is going to get bigger during pregnancy and it’s not going to go back to baseline. And if your aorta is bigger at the outset, there is a risk for long-term adverse outcomes,’ " Dr. Carole A. Warnes explained at the annual cardiovascular conference at Snowmass sponsored by the American College of Cardiology (ACC).
This study on pregnancy’s impact on aortic growth rate and complications in patients with Marfan syndrome sheds much needed light on an area where there has been a paucity of data. The deficiency of data is reflected in discordant recommendations in the current U.S., European, and Canadian guidelines, said Dr. Warnes, professor of medicine at the Mayo Clinic, Rochester, Minn.
The U.S. guidelines put forth jointly by the ACC, American Heart Association, American Association for Thoracic Surgery, and other groups advocate that Marfan syndrome patients avoid pregnancy if their aortic root diameter exceeds 40 mm and recommend prophylactic aortic replacement in those interested in pregnancy (J. Am. Coll. Cardiol. 2010;55:e27-129).
In contrast, the European guidelines (Eur. Heart J. 2010;31:2915-57) consider an aortic root diameter of 45 mm or less to be generally safe, while strongly discouraging pregnancy in Marfan syndrome patients with a measurement above that threshold because of the associated increased dissection risk. The Canadian guidelines take a similar stance, albeit with a safety threshold of 44 mm rather than 45 mm (Can. J. Cardiol. 2010;26:e80-e97).
The Europeans qualify their position by noting that patients with a prepregnancy aortic root diameter of 40-45 mm who have a rapid aortic root growth rate or a family history of dissection ought to be considered high risk for pregnancy. The European and Canadian guidelines characterize dissection as a rare problem in patients with an aortic root diameter of less than 40 mm.
The recent Utah study included 98 women with Marfan syndrome, 69 of whom collectively had 199 pregnancies, with 170 live births, 26 spontaneous abortions, and 2 ectopic pregnancies.
Serial echocardiograms demonstrated that the aortic growth rate was significantly greater during pregnancy than beforehand, and after pregnancy it didn’t return to baseline. Obstetric complications occurred in 10% of pregnancies. Adverse fetal outcomes occurred in 13%.
Reassuringly, there were no catastrophic peripartum complications. No one required cardiac surgery or experienced aortic dissection during pregnancy. However, women with a prior pregnancy had a greater prevalence of both aortic dissection and elective aortic surgery during long-term follow-up, compared with matched childless women with Marfan syndrome. Thus, it’s important during prepregnancy counseling of women with Marfan syndrome to let them know they’ll need to have elective aortic root surgery at a younger age than if they remain childless, Dr. Warnes noted.
A larger initial root diameter and a faster increase in diameter were independent predictors of long-term adverse cardiovascular events in the Utah study.
Besides the recent Utah study, only two other prospective studies of pregnancy’s impact on aortic growth and complications have been done. Both were much smaller. In an editorial accompanying the Utah study, Dutch physicians combined the three studies to get a fuller picture. No type A dissections occurred during 145 pregnancies in 78 nonoperated women with Marfan syndrome. Of 25 women with an aortic root diameter of 40-51 mm during 29 pregnancies, one experienced a type B dissection, two had carotid artery dissections, and one developed accelerated aortic regurgitation, which went from mild to severe during pregnancy.
Five women underwent aortic root replacement (three electively), prior to six pregnancies. Two of them developed a type B dissection during pregnancy. Both women who underwent a valve-sparing elective aortic root replacement prior to pregnancy had pregnancies complicated by a worsening of aortic regurgitation, which went from trivial to moderate. These findings raise a red flag for Dr. Warnes.
"Even if they’ve had a successful root replacement, it doesn’t mean they’re out of the woods in terms of pregnancy. I think we have to question the role of prophylactic root replacement [as recommended in the U.S. guidelines] because these women will still have type B dissections, and trying to look for a type B dissection during pregnancy is a real difficult issue," the cardiologist observed.
The authors of the editorial concluded that Marfan syndrome patients without previous cardiac complications and who have a baseline aortic root diameter not in excess of 45 mm seem to tolerate pregnancy well as long as they receive good clinical care before, during, and after pregnancy. In contrast, pregnancy should be discouraged in patients with a history of aortic dissection because they are at elevated risk for aortic complications (J. Am. Coll. Cardiol. 2012;60:230-1).
Marfan syndrome is a genetic connective tissue disorder with an incidence of roughly 1 in 5,000 and autosomal dominant inheritance, so the fetus of an affected mom has a 50% chance of having the disorder. Dr. Warnes said that because the diagnostic criteria were overhauled in 2010, patients believed to have Marfan syndrome really ought to be referred to a specialized center in order to confirm or refute the diagnosis according to the contemporary Ghent criteria.
Dr. Warnes reported having no relevant financial interests.
SNOWMASS, COLO–Pregnancy increases the long-term risk of aortic complications in women with Marfan syndrome, according to a recent prospective study causing a stir among adult congenital heart disease specialists.
"This is the first study that says, ‘Even if the aortic root size is okay before pregnancy, the aorta is going to get bigger during pregnancy and it’s not going to go back to baseline. And if your aorta is bigger at the outset, there is a risk for long-term adverse outcomes,’ " Dr. Carole A. Warnes explained at the annual cardiovascular conference at Snowmass sponsored by the American College of Cardiology (ACC).
This study on pregnancy’s impact on aortic growth rate and complications in patients with Marfan syndrome sheds much needed light on an area where there has been a paucity of data. The deficiency of data is reflected in discordant recommendations in the current U.S., European, and Canadian guidelines, said Dr. Warnes, professor of medicine at the Mayo Clinic, Rochester, Minn.
The U.S. guidelines put forth jointly by the ACC, American Heart Association, American Association for Thoracic Surgery, and other groups advocate that Marfan syndrome patients avoid pregnancy if their aortic root diameter exceeds 40 mm and recommend prophylactic aortic replacement in those interested in pregnancy (J. Am. Coll. Cardiol. 2010;55:e27-129).
In contrast, the European guidelines (Eur. Heart J. 2010;31:2915-57) consider an aortic root diameter of 45 mm or less to be generally safe, while strongly discouraging pregnancy in Marfan syndrome patients with a measurement above that threshold because of the associated increased dissection risk. The Canadian guidelines take a similar stance, albeit with a safety threshold of 44 mm rather than 45 mm (Can. J. Cardiol. 2010;26:e80-e97).
The Europeans qualify their position by noting that patients with a prepregnancy aortic root diameter of 40-45 mm who have a rapid aortic root growth rate or a family history of dissection ought to be considered high risk for pregnancy. The European and Canadian guidelines characterize dissection as a rare problem in patients with an aortic root diameter of less than 40 mm.
The recent Utah study included 98 women with Marfan syndrome, 69 of whom collectively had 199 pregnancies, with 170 live births, 26 spontaneous abortions, and 2 ectopic pregnancies.
Serial echocardiograms demonstrated that the aortic growth rate was significantly greater during pregnancy than beforehand, and after pregnancy it didn’t return to baseline. Obstetric complications occurred in 10% of pregnancies. Adverse fetal outcomes occurred in 13%.
Reassuringly, there were no catastrophic peripartum complications. No one required cardiac surgery or experienced aortic dissection during pregnancy. However, women with a prior pregnancy had a greater prevalence of both aortic dissection and elective aortic surgery during long-term follow-up, compared with matched childless women with Marfan syndrome. Thus, it’s important during prepregnancy counseling of women with Marfan syndrome to let them know they’ll need to have elective aortic root surgery at a younger age than if they remain childless, Dr. Warnes noted.
A larger initial root diameter and a faster increase in diameter were independent predictors of long-term adverse cardiovascular events in the Utah study.
Besides the recent Utah study, only two other prospective studies of pregnancy’s impact on aortic growth and complications have been done. Both were much smaller. In an editorial accompanying the Utah study, Dutch physicians combined the three studies to get a fuller picture. No type A dissections occurred during 145 pregnancies in 78 nonoperated women with Marfan syndrome. Of 25 women with an aortic root diameter of 40-51 mm during 29 pregnancies, one experienced a type B dissection, two had carotid artery dissections, and one developed accelerated aortic regurgitation, which went from mild to severe during pregnancy.
Five women underwent aortic root replacement (three electively), prior to six pregnancies. Two of them developed a type B dissection during pregnancy. Both women who underwent a valve-sparing elective aortic root replacement prior to pregnancy had pregnancies complicated by a worsening of aortic regurgitation, which went from trivial to moderate. These findings raise a red flag for Dr. Warnes.
"Even if they’ve had a successful root replacement, it doesn’t mean they’re out of the woods in terms of pregnancy. I think we have to question the role of prophylactic root replacement [as recommended in the U.S. guidelines] because these women will still have type B dissections, and trying to look for a type B dissection during pregnancy is a real difficult issue," the cardiologist observed.
The authors of the editorial concluded that Marfan syndrome patients without previous cardiac complications and who have a baseline aortic root diameter not in excess of 45 mm seem to tolerate pregnancy well as long as they receive good clinical care before, during, and after pregnancy. In contrast, pregnancy should be discouraged in patients with a history of aortic dissection because they are at elevated risk for aortic complications (J. Am. Coll. Cardiol. 2012;60:230-1).
Marfan syndrome is a genetic connective tissue disorder with an incidence of roughly 1 in 5,000 and autosomal dominant inheritance, so the fetus of an affected mom has a 50% chance of having the disorder. Dr. Warnes said that because the diagnostic criteria were overhauled in 2010, patients believed to have Marfan syndrome really ought to be referred to a specialized center in order to confirm or refute the diagnosis according to the contemporary Ghent criteria.
Dr. Warnes reported having no relevant financial interests.
EXPERT ANALYSIS FROM THE ANNUAL CARDIOVASCULAR CONFERENCE AT SNOWMASS
The vaginal approach to hysterectomy
The vaginal route is the preferred approach for benign hysterectomy. The most recent Cochrane review of surgical approaches to hysterectomy (abdominal, vaginal, and laparoscopic), which involved more than 3,000 women in 27 randomized controlled trials, shows that vaginal hysterectomy results in fewer complications, shorter hospital stay, and faster recovery and return to normal activity (Cochrane Database Syst. Rev. 2006 (2):CD003677). The vaginal approach also provides the best cosmetic result with its single and concealed incision.
Despite strong evidence for the greater advantage of the vaginal approach, there has not been any increase in the number of hysterectomies performed vaginally. In the United States, the rate appears to have declined in 15 years from 24% in 1990 to 22% in 2005, and this decline may be continuing (Obstet. Gynecol. 2002;99:229-34 and Obstet. Gynecol. 2009;114:1041-8). According to an analysis of a national database from more than 500 acute care hospitals, the majority of gynecologic surgeons in United States (more than 80%) perform fewer than five vaginal surgeries in a year (Obstet. Gynecol. 2010;116:1341-7).
Challenges with exposure, entry into the anterior cul-de-sac, hemostasis, avoidance of ureteral and bladder injury, and removal of the large uterus have been the main stumbling blocks for many surgeons in choosing the vaginal route. I provide, herein, simple techniques, instruments, and devices that can facilitate the performance of the procedure in a safe and efficient manner.
Obtaining exposure
The use of a self-retaining retractor, such as the Magrina-Bookwalter vaginal retractor system (Symmetry Surgical, Nashville, Tenn.) provides consistent and reliable exposure without requiring two surgical assistants at the bedside. Similar to the abdominal self-retractor system, it is attached to the operating table and is designed to fit the contour of the patient’s perineum while in a high lithotomy position. Self-retracting blades of multiple lengths are placed in the four quadrants to maximize room for surgery.
In cases where the introital opening is limited (i.e. = 2.5 cm), such as in nulliparous or menopausal women, a superficial 2- to 3-cm longitudinal incision is performed with bovie cautery in the midline and distal portion of the posterior vaginal wall. This provides additional width to allow placement of the lateral and posterior self-retracting blades.
Additional light from a flexible light source (such as the cystoscopy light) held with a Babcock and a lighted suction irrigator tip (such as Vital Vue, Covidien, Mansfield, Mass.) is extremely helpful in visualization of structures deep within the vagina.
Essential in a vaginal hysterectomy instrument tray are modified deep Deaver retractors that provide additional retraction and visualization particularly in cases of bleeding from pedicles that have retracted to the pelvic sidewall. . A long vaginal pack is also placed to keep loops of bowel out of the operating field. We avoid the use of multiple small sponges that can easily be lost in vaginal cases.
Entry into cul-de-sac
Entry into the anterior cul-de-sac in vaginal hysterectomy can and should be delayed until better descensus of the uterus is obtained. This is achieved with first entering the posterior cul-de-sac, which is often easier to accomplish. To then enter the anterior cul-de-sac, traction is applied posteriorly on the anterior lip of the cervix with the Jacobs tenaculum forceps. The posterior blade is removed to achieve better exposure with a more pronounced angulation of the lower uterine segment.
With ventral traction on the anterior vaginal wall, the bladder is separated from the anterior cervix via sharp dissection with the Mayo curved scissors. The scissor tips are pointed downwards, aimed parallel to the plane of the cervix to reveal the avascular vesicouterine space.
Knowing the anatomy and feel of the tissues is key to mastering entry into the anterior cul-de-sac. Cutting into the cervix will feel tough against the tips of the Metzenbaum scissors, while cutting into the softer beefy-appearing detrusor muscles will manifest with excessive bleeding. The vesicouterine fold is identified as a crescent-shaped peritoneal fold that can be lifted and divided for entry.
In cases where scarring between the bladder and uterus is encountered in patients with multiple previous caesarean sections, dissection is best performed lateral to the midline away from central dense adhesions.
An inability to enter either or both cul-de-sacs should not preclude continuation with the vaginal approach. Securing the uterine arteries can still be accomplished extraperitoneally until better descensus of the uterus is obtained.
Securing vascular pedicles
Achieving hemostasis in vaginal procedures is challenging where there is limited space for placing a suture around the clamp and for securing knots with fingers deep within the vaginal canal. The use of vessel-sealing devices in vaginal hysterectomy overcomes this limitation of tight vaginal access and has proved to be feasible and safe.
Multiple types of energy devices are available, such as PK devices (Gyrus ACMI, Southborough, Mass.), LigaSure instruments (Covidien, Mansfield, Mass.), the Enseal Super Jaw device (Ethicon Endo-Surgery, Nokesville, Va.) and Altrus devices (ConMed Electrosurgery, Centennial, Colo.). These devices can be particularly helpful in cases with narrowed introitus and large uterus. The choice of device is surgeon dependent and requires a learning curve.
Gentle traction is placed on the cervix while the device clamp is pushed up against the pedicle, taking care to avoid leaning against any adjacent tissues or retractor blades to avoid thermal injury. Bringing in a suction device quickly dissipates the hot steam that can be generated from the device.
Avoidance of bladder and ureteral injury
Once the vesicouterine space is entered, bladder pillars are gently pushed superiorly and laterally with the index finger to avoid injury during placement of the vessel-sealing clamp. It is imperative that the surgeon is aware of the location of the ureters, which are easily injured, particularly in cases with pelvic prolapse.
The ureters can be palpated with the index finger at 2 o’clock or at 10 o’clock (for the left and right ureter, respectively) against a curved Deaver retractor placed outside the peritoneal cavity on the lateral vaginal wall. Intraoperative cystoscopy should always be performed at the end of the procedure to diagnose inadvertent bladder and ureteral injury.
Removing the Large Uterus
Morcellation can be initiated after the uterine arteries have been sealed and divided on each side. Orientation of the uterus is maintained by placing two Jacobs tenaculi at the 3 o’clock and at 9 o’clock positions on the cervix. The cervix is bivalved to the level of the lower uterine segment.
If the anterior cul-de-sac has not been entered yet, the cervix should be bivalved to a centimeter below the vesicouterine peritoneal fold and morcellation started within the uterus.
Morcellation is performed with a Schroeder tenaculum (Aesculap Inc., Center Valley, Pa.) placed on the myometrium, and a wedge excision is accomplished with a 10 blade. Serial wedges are performed to decompress the uterus. Entry into the anterior cul-de-sac can now be performed easily with better uterine descensus and visualization of the peritoneal fold.
The surgeon should avoid forceful traction on the cervix during morcellation, which can cause the vascular pedicles to avulse.
Depending on the size of the uterus, morcellation can take over an hour. Use of an articulated long scalpel handle (such as the Precise CMK ergonomic knife by LaparoTools, in Metairie, La., which is rounded) can facilitate morcellation with less fatigue.
The surgeon must persist with morcellation as long as descensus of the uterus is continually achieved. An increase in bleeding is encountered when morcellation is near the fundus. At this point, the utero-ovarian pedicles can be identified and secured to finish the procedure.
Mastering the procedure
Simple techniques and new surgical devices are available to facilitate the difficult vaginal hysterectomy. Cases of narrowed introitus, multiple previous caesarean sections, and the large uteri requiring morcellation can be approached vaginally and achieved safely and efficiently with use of the above techniques.
In recognition of the vaginal approach as a minimally invasive procedure, AAGL has provided postgraduate courses in the recent past that incorporate hands-on workshops with the cadaveric model to master the procedure.
Similarly, AAGL has identified five large-volume vaginal centers throughout the country where observership programs are available to practitioners interested in learning the techniques (www.aagl.org). These opportunities allow the surgeon to advance their skills and reincorporate the vaginal hysterectomy into their armamentarium so that patients can benefit from its most minimally invasive approach.
Dr. Kho is associate professor and director of the minimally invasive gynecologic surgery (MIGS) fellowship program in the department of medical and surgical gynecology at the Mayo Clinic in Phoenix, Ariz. She reported that she has no relevant financial disclosures.
The vaginal route is the preferred approach for benign hysterectomy. The most recent Cochrane review of surgical approaches to hysterectomy (abdominal, vaginal, and laparoscopic), which involved more than 3,000 women in 27 randomized controlled trials, shows that vaginal hysterectomy results in fewer complications, shorter hospital stay, and faster recovery and return to normal activity (Cochrane Database Syst. Rev. 2006 (2):CD003677). The vaginal approach also provides the best cosmetic result with its single and concealed incision.
Despite strong evidence for the greater advantage of the vaginal approach, there has not been any increase in the number of hysterectomies performed vaginally. In the United States, the rate appears to have declined in 15 years from 24% in 1990 to 22% in 2005, and this decline may be continuing (Obstet. Gynecol. 2002;99:229-34 and Obstet. Gynecol. 2009;114:1041-8). According to an analysis of a national database from more than 500 acute care hospitals, the majority of gynecologic surgeons in United States (more than 80%) perform fewer than five vaginal surgeries in a year (Obstet. Gynecol. 2010;116:1341-7).
Challenges with exposure, entry into the anterior cul-de-sac, hemostasis, avoidance of ureteral and bladder injury, and removal of the large uterus have been the main stumbling blocks for many surgeons in choosing the vaginal route. I provide, herein, simple techniques, instruments, and devices that can facilitate the performance of the procedure in a safe and efficient manner.
Obtaining exposure
The use of a self-retaining retractor, such as the Magrina-Bookwalter vaginal retractor system (Symmetry Surgical, Nashville, Tenn.) provides consistent and reliable exposure without requiring two surgical assistants at the bedside. Similar to the abdominal self-retractor system, it is attached to the operating table and is designed to fit the contour of the patient’s perineum while in a high lithotomy position. Self-retracting blades of multiple lengths are placed in the four quadrants to maximize room for surgery.
In cases where the introital opening is limited (i.e. = 2.5 cm), such as in nulliparous or menopausal women, a superficial 2- to 3-cm longitudinal incision is performed with bovie cautery in the midline and distal portion of the posterior vaginal wall. This provides additional width to allow placement of the lateral and posterior self-retracting blades.
Additional light from a flexible light source (such as the cystoscopy light) held with a Babcock and a lighted suction irrigator tip (such as Vital Vue, Covidien, Mansfield, Mass.) is extremely helpful in visualization of structures deep within the vagina.
Essential in a vaginal hysterectomy instrument tray are modified deep Deaver retractors that provide additional retraction and visualization particularly in cases of bleeding from pedicles that have retracted to the pelvic sidewall. . A long vaginal pack is also placed to keep loops of bowel out of the operating field. We avoid the use of multiple small sponges that can easily be lost in vaginal cases.
Entry into cul-de-sac
Entry into the anterior cul-de-sac in vaginal hysterectomy can and should be delayed until better descensus of the uterus is obtained. This is achieved with first entering the posterior cul-de-sac, which is often easier to accomplish. To then enter the anterior cul-de-sac, traction is applied posteriorly on the anterior lip of the cervix with the Jacobs tenaculum forceps. The posterior blade is removed to achieve better exposure with a more pronounced angulation of the lower uterine segment.
With ventral traction on the anterior vaginal wall, the bladder is separated from the anterior cervix via sharp dissection with the Mayo curved scissors. The scissor tips are pointed downwards, aimed parallel to the plane of the cervix to reveal the avascular vesicouterine space.
Knowing the anatomy and feel of the tissues is key to mastering entry into the anterior cul-de-sac. Cutting into the cervix will feel tough against the tips of the Metzenbaum scissors, while cutting into the softer beefy-appearing detrusor muscles will manifest with excessive bleeding. The vesicouterine fold is identified as a crescent-shaped peritoneal fold that can be lifted and divided for entry.
In cases where scarring between the bladder and uterus is encountered in patients with multiple previous caesarean sections, dissection is best performed lateral to the midline away from central dense adhesions.
An inability to enter either or both cul-de-sacs should not preclude continuation with the vaginal approach. Securing the uterine arteries can still be accomplished extraperitoneally until better descensus of the uterus is obtained.
Securing vascular pedicles
Achieving hemostasis in vaginal procedures is challenging where there is limited space for placing a suture around the clamp and for securing knots with fingers deep within the vaginal canal. The use of vessel-sealing devices in vaginal hysterectomy overcomes this limitation of tight vaginal access and has proved to be feasible and safe.
Multiple types of energy devices are available, such as PK devices (Gyrus ACMI, Southborough, Mass.), LigaSure instruments (Covidien, Mansfield, Mass.), the Enseal Super Jaw device (Ethicon Endo-Surgery, Nokesville, Va.) and Altrus devices (ConMed Electrosurgery, Centennial, Colo.). These devices can be particularly helpful in cases with narrowed introitus and large uterus. The choice of device is surgeon dependent and requires a learning curve.
Gentle traction is placed on the cervix while the device clamp is pushed up against the pedicle, taking care to avoid leaning against any adjacent tissues or retractor blades to avoid thermal injury. Bringing in a suction device quickly dissipates the hot steam that can be generated from the device.
Avoidance of bladder and ureteral injury
Once the vesicouterine space is entered, bladder pillars are gently pushed superiorly and laterally with the index finger to avoid injury during placement of the vessel-sealing clamp. It is imperative that the surgeon is aware of the location of the ureters, which are easily injured, particularly in cases with pelvic prolapse.
The ureters can be palpated with the index finger at 2 o’clock or at 10 o’clock (for the left and right ureter, respectively) against a curved Deaver retractor placed outside the peritoneal cavity on the lateral vaginal wall. Intraoperative cystoscopy should always be performed at the end of the procedure to diagnose inadvertent bladder and ureteral injury.
Removing the Large Uterus
Morcellation can be initiated after the uterine arteries have been sealed and divided on each side. Orientation of the uterus is maintained by placing two Jacobs tenaculi at the 3 o’clock and at 9 o’clock positions on the cervix. The cervix is bivalved to the level of the lower uterine segment.
If the anterior cul-de-sac has not been entered yet, the cervix should be bivalved to a centimeter below the vesicouterine peritoneal fold and morcellation started within the uterus.
Morcellation is performed with a Schroeder tenaculum (Aesculap Inc., Center Valley, Pa.) placed on the myometrium, and a wedge excision is accomplished with a 10 blade. Serial wedges are performed to decompress the uterus. Entry into the anterior cul-de-sac can now be performed easily with better uterine descensus and visualization of the peritoneal fold.
The surgeon should avoid forceful traction on the cervix during morcellation, which can cause the vascular pedicles to avulse.
Depending on the size of the uterus, morcellation can take over an hour. Use of an articulated long scalpel handle (such as the Precise CMK ergonomic knife by LaparoTools, in Metairie, La., which is rounded) can facilitate morcellation with less fatigue.
The surgeon must persist with morcellation as long as descensus of the uterus is continually achieved. An increase in bleeding is encountered when morcellation is near the fundus. At this point, the utero-ovarian pedicles can be identified and secured to finish the procedure.
Mastering the procedure
Simple techniques and new surgical devices are available to facilitate the difficult vaginal hysterectomy. Cases of narrowed introitus, multiple previous caesarean sections, and the large uteri requiring morcellation can be approached vaginally and achieved safely and efficiently with use of the above techniques.
In recognition of the vaginal approach as a minimally invasive procedure, AAGL has provided postgraduate courses in the recent past that incorporate hands-on workshops with the cadaveric model to master the procedure.
Similarly, AAGL has identified five large-volume vaginal centers throughout the country where observership programs are available to practitioners interested in learning the techniques (www.aagl.org). These opportunities allow the surgeon to advance their skills and reincorporate the vaginal hysterectomy into their armamentarium so that patients can benefit from its most minimally invasive approach.
Dr. Kho is associate professor and director of the minimally invasive gynecologic surgery (MIGS) fellowship program in the department of medical and surgical gynecology at the Mayo Clinic in Phoenix, Ariz. She reported that she has no relevant financial disclosures.
The vaginal route is the preferred approach for benign hysterectomy. The most recent Cochrane review of surgical approaches to hysterectomy (abdominal, vaginal, and laparoscopic), which involved more than 3,000 women in 27 randomized controlled trials, shows that vaginal hysterectomy results in fewer complications, shorter hospital stay, and faster recovery and return to normal activity (Cochrane Database Syst. Rev. 2006 (2):CD003677). The vaginal approach also provides the best cosmetic result with its single and concealed incision.
Despite strong evidence for the greater advantage of the vaginal approach, there has not been any increase in the number of hysterectomies performed vaginally. In the United States, the rate appears to have declined in 15 years from 24% in 1990 to 22% in 2005, and this decline may be continuing (Obstet. Gynecol. 2002;99:229-34 and Obstet. Gynecol. 2009;114:1041-8). According to an analysis of a national database from more than 500 acute care hospitals, the majority of gynecologic surgeons in United States (more than 80%) perform fewer than five vaginal surgeries in a year (Obstet. Gynecol. 2010;116:1341-7).
Challenges with exposure, entry into the anterior cul-de-sac, hemostasis, avoidance of ureteral and bladder injury, and removal of the large uterus have been the main stumbling blocks for many surgeons in choosing the vaginal route. I provide, herein, simple techniques, instruments, and devices that can facilitate the performance of the procedure in a safe and efficient manner.
Obtaining exposure
The use of a self-retaining retractor, such as the Magrina-Bookwalter vaginal retractor system (Symmetry Surgical, Nashville, Tenn.) provides consistent and reliable exposure without requiring two surgical assistants at the bedside. Similar to the abdominal self-retractor system, it is attached to the operating table and is designed to fit the contour of the patient’s perineum while in a high lithotomy position. Self-retracting blades of multiple lengths are placed in the four quadrants to maximize room for surgery.
In cases where the introital opening is limited (i.e. = 2.5 cm), such as in nulliparous or menopausal women, a superficial 2- to 3-cm longitudinal incision is performed with bovie cautery in the midline and distal portion of the posterior vaginal wall. This provides additional width to allow placement of the lateral and posterior self-retracting blades.
Additional light from a flexible light source (such as the cystoscopy light) held with a Babcock and a lighted suction irrigator tip (such as Vital Vue, Covidien, Mansfield, Mass.) is extremely helpful in visualization of structures deep within the vagina.
Essential in a vaginal hysterectomy instrument tray are modified deep Deaver retractors that provide additional retraction and visualization particularly in cases of bleeding from pedicles that have retracted to the pelvic sidewall. . A long vaginal pack is also placed to keep loops of bowel out of the operating field. We avoid the use of multiple small sponges that can easily be lost in vaginal cases.
Entry into cul-de-sac
Entry into the anterior cul-de-sac in vaginal hysterectomy can and should be delayed until better descensus of the uterus is obtained. This is achieved with first entering the posterior cul-de-sac, which is often easier to accomplish. To then enter the anterior cul-de-sac, traction is applied posteriorly on the anterior lip of the cervix with the Jacobs tenaculum forceps. The posterior blade is removed to achieve better exposure with a more pronounced angulation of the lower uterine segment.
With ventral traction on the anterior vaginal wall, the bladder is separated from the anterior cervix via sharp dissection with the Mayo curved scissors. The scissor tips are pointed downwards, aimed parallel to the plane of the cervix to reveal the avascular vesicouterine space.
Knowing the anatomy and feel of the tissues is key to mastering entry into the anterior cul-de-sac. Cutting into the cervix will feel tough against the tips of the Metzenbaum scissors, while cutting into the softer beefy-appearing detrusor muscles will manifest with excessive bleeding. The vesicouterine fold is identified as a crescent-shaped peritoneal fold that can be lifted and divided for entry.
In cases where scarring between the bladder and uterus is encountered in patients with multiple previous caesarean sections, dissection is best performed lateral to the midline away from central dense adhesions.
An inability to enter either or both cul-de-sacs should not preclude continuation with the vaginal approach. Securing the uterine arteries can still be accomplished extraperitoneally until better descensus of the uterus is obtained.
Securing vascular pedicles
Achieving hemostasis in vaginal procedures is challenging where there is limited space for placing a suture around the clamp and for securing knots with fingers deep within the vaginal canal. The use of vessel-sealing devices in vaginal hysterectomy overcomes this limitation of tight vaginal access and has proved to be feasible and safe.
Multiple types of energy devices are available, such as PK devices (Gyrus ACMI, Southborough, Mass.), LigaSure instruments (Covidien, Mansfield, Mass.), the Enseal Super Jaw device (Ethicon Endo-Surgery, Nokesville, Va.) and Altrus devices (ConMed Electrosurgery, Centennial, Colo.). These devices can be particularly helpful in cases with narrowed introitus and large uterus. The choice of device is surgeon dependent and requires a learning curve.
Gentle traction is placed on the cervix while the device clamp is pushed up against the pedicle, taking care to avoid leaning against any adjacent tissues or retractor blades to avoid thermal injury. Bringing in a suction device quickly dissipates the hot steam that can be generated from the device.
Avoidance of bladder and ureteral injury
Once the vesicouterine space is entered, bladder pillars are gently pushed superiorly and laterally with the index finger to avoid injury during placement of the vessel-sealing clamp. It is imperative that the surgeon is aware of the location of the ureters, which are easily injured, particularly in cases with pelvic prolapse.
The ureters can be palpated with the index finger at 2 o’clock or at 10 o’clock (for the left and right ureter, respectively) against a curved Deaver retractor placed outside the peritoneal cavity on the lateral vaginal wall. Intraoperative cystoscopy should always be performed at the end of the procedure to diagnose inadvertent bladder and ureteral injury.
Removing the Large Uterus
Morcellation can be initiated after the uterine arteries have been sealed and divided on each side. Orientation of the uterus is maintained by placing two Jacobs tenaculi at the 3 o’clock and at 9 o’clock positions on the cervix. The cervix is bivalved to the level of the lower uterine segment.
If the anterior cul-de-sac has not been entered yet, the cervix should be bivalved to a centimeter below the vesicouterine peritoneal fold and morcellation started within the uterus.
Morcellation is performed with a Schroeder tenaculum (Aesculap Inc., Center Valley, Pa.) placed on the myometrium, and a wedge excision is accomplished with a 10 blade. Serial wedges are performed to decompress the uterus. Entry into the anterior cul-de-sac can now be performed easily with better uterine descensus and visualization of the peritoneal fold.
The surgeon should avoid forceful traction on the cervix during morcellation, which can cause the vascular pedicles to avulse.
Depending on the size of the uterus, morcellation can take over an hour. Use of an articulated long scalpel handle (such as the Precise CMK ergonomic knife by LaparoTools, in Metairie, La., which is rounded) can facilitate morcellation with less fatigue.
The surgeon must persist with morcellation as long as descensus of the uterus is continually achieved. An increase in bleeding is encountered when morcellation is near the fundus. At this point, the utero-ovarian pedicles can be identified and secured to finish the procedure.
Mastering the procedure
Simple techniques and new surgical devices are available to facilitate the difficult vaginal hysterectomy. Cases of narrowed introitus, multiple previous caesarean sections, and the large uteri requiring morcellation can be approached vaginally and achieved safely and efficiently with use of the above techniques.
In recognition of the vaginal approach as a minimally invasive procedure, AAGL has provided postgraduate courses in the recent past that incorporate hands-on workshops with the cadaveric model to master the procedure.
Similarly, AAGL has identified five large-volume vaginal centers throughout the country where observership programs are available to practitioners interested in learning the techniques (www.aagl.org). These opportunities allow the surgeon to advance their skills and reincorporate the vaginal hysterectomy into their armamentarium so that patients can benefit from its most minimally invasive approach.
Dr. Kho is associate professor and director of the minimally invasive gynecologic surgery (MIGS) fellowship program in the department of medical and surgical gynecology at the Mayo Clinic in Phoenix, Ariz. She reported that she has no relevant financial disclosures.
South Florida simulation center makes its mark
High-tech computer and robotic simulators are changing the way that obstetricians and gynecologists learn and maintain their skills. Now a new state-of-the-art simulation center in Tampa is changing the way academic medical centers offer this training.
With its modern architecture and gleaming glass exterior, the Center for Advanced Medical Learning and Simulation, located in downtown Tampa, looks like the type of building that houses cutting-edge technology.
The 90,000 square-foot-facility includes a surgical skills lab with more than 30 operating stations, an on-site tissue bank, a robotics suite with two da Vinci robots (S and Si), a synthetic cadaver, a 64-slice CT scanner, and a hybrid operating room. And those are just some of the offerings in the Surgical and Interventional Training Center.
The Center for Advanced Medical Learning and Simulation (CAMLS), which is affiliated with the University of South Florida, houses three other centers: the Virtual Patient Care Center, the Education Center, and the Tampa Bay Research and Innovation Center.
But it’s not the technology alone that sets CAMLS apart, said Dr. Stuart Hart, an ob.gyn. and urogynecologist who is the medical director for the Tampa Bay Research and Innovation Center.
"What makes it so unique is the tight integration among the various centers at CAMLS," he said.
The center, which opened in February 2012, has a lot of overlap among its education, training, and simulation programs. Anyone who comes to CAMLS for continuing medical education can get a sense of that integration, said Dr. Hart, who also oversees the minimally invasive gynecologic surgery courses.
For instance, ob.gyns. might have the chance to practice their skills on a synthetic cadaver in the Surgical and Interventional Training Center. Then they could take a trip upstairs to the Virtual Patient Care Center, where they could continue working on high-fidelity human patient simulators and laparoscopic surgical simulators.
"That’s what makes us so exciting," Dr. Hart said.
Dr. Robert W. Yelverton, an ob.gyn. in Tampa, first became involved with CAMLS while the center was still under construction. Dr. Yelverton, who at the time was the chief medical officer for a large ob.gyn. group in central Florida, was looking for a place where his physicians could get simulator training to improve the quality and safety of robotic and minimally invasive gynecological procedures.
For example, some of their physicians hadn’t received training during residency on how to examine the bladder with a cystoscope following a gynecologic procedure. In the past, urologists had typically been the ones performing cystoscopy, so many ob.gyns weren’t trained. But with those roles changing, Dr. Yelverton wanted his physicians to be able to learn and perfect the procedure on a simulator, rather than on real patients in the operating room. With the bladder simulator at CAMLS, physicians were able to perform cystoscopy hundreds of times and see virtually every abnormal legion in a realistic fashion, he said.
"This is a huge attraction for physicians who really are looking for improvement in ways that they can perfect their surgical skills, particularly those that were introduced after they were in training," Dr. Yelverton said.
Dr. Yelverton, who is the chairman for the American Congress of Obstetricians and Gynecologists District XII, is continuing to work with CAMLS to set up training for ACOG’s Florida fellows as part of their educational meetings.
He said he expects many local physicians, and even some from other parts of the country, will want to try out the center. One of the attractions, he said, is the ability to conduct team training. For instance, a team of obstetricians and nurses can simulate emergencies, from shoulder dystocia to postpartum hemorrhage, in a mock labor and delivery suite.
Practicing physicians aren’t the only ones who can hone their skills at CAMLS. The center is also available for medical students and residents, as well as pharmacy and nursing students. The certified registered nurse anesthetist program is permanently housed in the building.
Even graduate business and engineering students drop in at CAMLS as part of their work with the Tampa Bay Research and Innovation Center. Coming to CAMLS means that engineering and business students get the chance to sit down with physicians and learn about the clinical problems driving the need for new technologies and devices, Dr. Hart said.
As part of the innovation work, Dr. Hart often presents a problem to the engineering students and then brings them to the operating room to see a simulated surgery first hand. The students then come up ideas for different devices that could help solve the problem.
"We go in with problems," he said. "We don’t go in and say, ‘I have an idea for a medical device.’ That’s actually the last thing we want to do."
As part of that process, Dr. Hart and his colleagues also work closely with industry on device development and commercialization. And the device and pharmaceutical industry is also a presence in other parts of CAMLS. Medical device and pharmaceutical companies come to the center to train their sales forces and their clients, said Deborah Sutherland, Ph.D., the CEO of CAMLS.
One of the reasons that CAMLS is able to offer its services to groups and individuals who are not affiliated with the University of South Florida is that the center is part of a not-for-profit corporation that includes USF Health.
CAMLS is run on a business model, not a traditional academic model, Dr. Sutherland said. CAMLS does not receive any financial support from the University of South Florida. All of the revenue comes instead from user fees.
"That is very unique because most simulation centers that you see nationally are supported by a clinical department," she said.
That type of approach may make CAMLS the envy of other simulation centers around the country, said Dr. Carol A. Aschenbrener, the chief medical education officer at the Association of American Medical Colleges.
Running a simulation center is costly, with the annual price tag ranging anywhere between $50,000 and $2.5 million, depending on the scope of the center and the staffing levels, she said. A 2010 survey conducted by the AAMC shows that most of these centers are funded either by a medical school or a teaching hospital. With those organizations under significant financial pressure, many are looking carefully at other ways to pay the bills. A handful of centers are actively developing new business models, she said, but it’s early on in the process. "So people are watching the South Florida center very closely," Dr. Aschenbrener said.
High-tech computer and robotic simulators are changing the way that obstetricians and gynecologists learn and maintain their skills. Now a new state-of-the-art simulation center in Tampa is changing the way academic medical centers offer this training.
With its modern architecture and gleaming glass exterior, the Center for Advanced Medical Learning and Simulation, located in downtown Tampa, looks like the type of building that houses cutting-edge technology.
The 90,000 square-foot-facility includes a surgical skills lab with more than 30 operating stations, an on-site tissue bank, a robotics suite with two da Vinci robots (S and Si), a synthetic cadaver, a 64-slice CT scanner, and a hybrid operating room. And those are just some of the offerings in the Surgical and Interventional Training Center.
The Center for Advanced Medical Learning and Simulation (CAMLS), which is affiliated with the University of South Florida, houses three other centers: the Virtual Patient Care Center, the Education Center, and the Tampa Bay Research and Innovation Center.
But it’s not the technology alone that sets CAMLS apart, said Dr. Stuart Hart, an ob.gyn. and urogynecologist who is the medical director for the Tampa Bay Research and Innovation Center.
"What makes it so unique is the tight integration among the various centers at CAMLS," he said.
The center, which opened in February 2012, has a lot of overlap among its education, training, and simulation programs. Anyone who comes to CAMLS for continuing medical education can get a sense of that integration, said Dr. Hart, who also oversees the minimally invasive gynecologic surgery courses.
For instance, ob.gyns. might have the chance to practice their skills on a synthetic cadaver in the Surgical and Interventional Training Center. Then they could take a trip upstairs to the Virtual Patient Care Center, where they could continue working on high-fidelity human patient simulators and laparoscopic surgical simulators.
"That’s what makes us so exciting," Dr. Hart said.
Dr. Robert W. Yelverton, an ob.gyn. in Tampa, first became involved with CAMLS while the center was still under construction. Dr. Yelverton, who at the time was the chief medical officer for a large ob.gyn. group in central Florida, was looking for a place where his physicians could get simulator training to improve the quality and safety of robotic and minimally invasive gynecological procedures.
For example, some of their physicians hadn’t received training during residency on how to examine the bladder with a cystoscope following a gynecologic procedure. In the past, urologists had typically been the ones performing cystoscopy, so many ob.gyns weren’t trained. But with those roles changing, Dr. Yelverton wanted his physicians to be able to learn and perfect the procedure on a simulator, rather than on real patients in the operating room. With the bladder simulator at CAMLS, physicians were able to perform cystoscopy hundreds of times and see virtually every abnormal legion in a realistic fashion, he said.
"This is a huge attraction for physicians who really are looking for improvement in ways that they can perfect their surgical skills, particularly those that were introduced after they were in training," Dr. Yelverton said.
Dr. Yelverton, who is the chairman for the American Congress of Obstetricians and Gynecologists District XII, is continuing to work with CAMLS to set up training for ACOG’s Florida fellows as part of their educational meetings.
He said he expects many local physicians, and even some from other parts of the country, will want to try out the center. One of the attractions, he said, is the ability to conduct team training. For instance, a team of obstetricians and nurses can simulate emergencies, from shoulder dystocia to postpartum hemorrhage, in a mock labor and delivery suite.
Practicing physicians aren’t the only ones who can hone their skills at CAMLS. The center is also available for medical students and residents, as well as pharmacy and nursing students. The certified registered nurse anesthetist program is permanently housed in the building.
Even graduate business and engineering students drop in at CAMLS as part of their work with the Tampa Bay Research and Innovation Center. Coming to CAMLS means that engineering and business students get the chance to sit down with physicians and learn about the clinical problems driving the need for new technologies and devices, Dr. Hart said.
As part of the innovation work, Dr. Hart often presents a problem to the engineering students and then brings them to the operating room to see a simulated surgery first hand. The students then come up ideas for different devices that could help solve the problem.
"We go in with problems," he said. "We don’t go in and say, ‘I have an idea for a medical device.’ That’s actually the last thing we want to do."
As part of that process, Dr. Hart and his colleagues also work closely with industry on device development and commercialization. And the device and pharmaceutical industry is also a presence in other parts of CAMLS. Medical device and pharmaceutical companies come to the center to train their sales forces and their clients, said Deborah Sutherland, Ph.D., the CEO of CAMLS.
One of the reasons that CAMLS is able to offer its services to groups and individuals who are not affiliated with the University of South Florida is that the center is part of a not-for-profit corporation that includes USF Health.
CAMLS is run on a business model, not a traditional academic model, Dr. Sutherland said. CAMLS does not receive any financial support from the University of South Florida. All of the revenue comes instead from user fees.
"That is very unique because most simulation centers that you see nationally are supported by a clinical department," she said.
That type of approach may make CAMLS the envy of other simulation centers around the country, said Dr. Carol A. Aschenbrener, the chief medical education officer at the Association of American Medical Colleges.
Running a simulation center is costly, with the annual price tag ranging anywhere between $50,000 and $2.5 million, depending on the scope of the center and the staffing levels, she said. A 2010 survey conducted by the AAMC shows that most of these centers are funded either by a medical school or a teaching hospital. With those organizations under significant financial pressure, many are looking carefully at other ways to pay the bills. A handful of centers are actively developing new business models, she said, but it’s early on in the process. "So people are watching the South Florida center very closely," Dr. Aschenbrener said.
High-tech computer and robotic simulators are changing the way that obstetricians and gynecologists learn and maintain their skills. Now a new state-of-the-art simulation center in Tampa is changing the way academic medical centers offer this training.
With its modern architecture and gleaming glass exterior, the Center for Advanced Medical Learning and Simulation, located in downtown Tampa, looks like the type of building that houses cutting-edge technology.
The 90,000 square-foot-facility includes a surgical skills lab with more than 30 operating stations, an on-site tissue bank, a robotics suite with two da Vinci robots (S and Si), a synthetic cadaver, a 64-slice CT scanner, and a hybrid operating room. And those are just some of the offerings in the Surgical and Interventional Training Center.
The Center for Advanced Medical Learning and Simulation (CAMLS), which is affiliated with the University of South Florida, houses three other centers: the Virtual Patient Care Center, the Education Center, and the Tampa Bay Research and Innovation Center.
But it’s not the technology alone that sets CAMLS apart, said Dr. Stuart Hart, an ob.gyn. and urogynecologist who is the medical director for the Tampa Bay Research and Innovation Center.
"What makes it so unique is the tight integration among the various centers at CAMLS," he said.
The center, which opened in February 2012, has a lot of overlap among its education, training, and simulation programs. Anyone who comes to CAMLS for continuing medical education can get a sense of that integration, said Dr. Hart, who also oversees the minimally invasive gynecologic surgery courses.
For instance, ob.gyns. might have the chance to practice their skills on a synthetic cadaver in the Surgical and Interventional Training Center. Then they could take a trip upstairs to the Virtual Patient Care Center, where they could continue working on high-fidelity human patient simulators and laparoscopic surgical simulators.
"That’s what makes us so exciting," Dr. Hart said.
Dr. Robert W. Yelverton, an ob.gyn. in Tampa, first became involved with CAMLS while the center was still under construction. Dr. Yelverton, who at the time was the chief medical officer for a large ob.gyn. group in central Florida, was looking for a place where his physicians could get simulator training to improve the quality and safety of robotic and minimally invasive gynecological procedures.
For example, some of their physicians hadn’t received training during residency on how to examine the bladder with a cystoscope following a gynecologic procedure. In the past, urologists had typically been the ones performing cystoscopy, so many ob.gyns weren’t trained. But with those roles changing, Dr. Yelverton wanted his physicians to be able to learn and perfect the procedure on a simulator, rather than on real patients in the operating room. With the bladder simulator at CAMLS, physicians were able to perform cystoscopy hundreds of times and see virtually every abnormal legion in a realistic fashion, he said.
"This is a huge attraction for physicians who really are looking for improvement in ways that they can perfect their surgical skills, particularly those that were introduced after they were in training," Dr. Yelverton said.
Dr. Yelverton, who is the chairman for the American Congress of Obstetricians and Gynecologists District XII, is continuing to work with CAMLS to set up training for ACOG’s Florida fellows as part of their educational meetings.
He said he expects many local physicians, and even some from other parts of the country, will want to try out the center. One of the attractions, he said, is the ability to conduct team training. For instance, a team of obstetricians and nurses can simulate emergencies, from shoulder dystocia to postpartum hemorrhage, in a mock labor and delivery suite.
Practicing physicians aren’t the only ones who can hone their skills at CAMLS. The center is also available for medical students and residents, as well as pharmacy and nursing students. The certified registered nurse anesthetist program is permanently housed in the building.
Even graduate business and engineering students drop in at CAMLS as part of their work with the Tampa Bay Research and Innovation Center. Coming to CAMLS means that engineering and business students get the chance to sit down with physicians and learn about the clinical problems driving the need for new technologies and devices, Dr. Hart said.
As part of the innovation work, Dr. Hart often presents a problem to the engineering students and then brings them to the operating room to see a simulated surgery first hand. The students then come up ideas for different devices that could help solve the problem.
"We go in with problems," he said. "We don’t go in and say, ‘I have an idea for a medical device.’ That’s actually the last thing we want to do."
As part of that process, Dr. Hart and his colleagues also work closely with industry on device development and commercialization. And the device and pharmaceutical industry is also a presence in other parts of CAMLS. Medical device and pharmaceutical companies come to the center to train their sales forces and their clients, said Deborah Sutherland, Ph.D., the CEO of CAMLS.
One of the reasons that CAMLS is able to offer its services to groups and individuals who are not affiliated with the University of South Florida is that the center is part of a not-for-profit corporation that includes USF Health.
CAMLS is run on a business model, not a traditional academic model, Dr. Sutherland said. CAMLS does not receive any financial support from the University of South Florida. All of the revenue comes instead from user fees.
"That is very unique because most simulation centers that you see nationally are supported by a clinical department," she said.
That type of approach may make CAMLS the envy of other simulation centers around the country, said Dr. Carol A. Aschenbrener, the chief medical education officer at the Association of American Medical Colleges.
Running a simulation center is costly, with the annual price tag ranging anywhere between $50,000 and $2.5 million, depending on the scope of the center and the staffing levels, she said. A 2010 survey conducted by the AAMC shows that most of these centers are funded either by a medical school or a teaching hospital. With those organizations under significant financial pressure, many are looking carefully at other ways to pay the bills. A handful of centers are actively developing new business models, she said, but it’s early on in the process. "So people are watching the South Florida center very closely," Dr. Aschenbrener said.