User login
Official Newspaper of the American College of Surgeons
Enhanced recovery led to fewer complications for major oncologic procedures
CHICAGO – Use of an enhanced recovery protocol for oncology patients has been shown to improve outcomes in colorectal surgery but has been largely unproven in other types of major oncology operations. That prompted researchers at the University of Texas MD Anderson Cancer Center in Houston to investigate They found that the enhanced recovery protocol led to a reduction in complication rates and a decrease in hospital stay with no increase in readmissions, according to an analysis of more than 3,000 oncologic operations presented at the Society of Surgical Oncology Annual Cancer Symposium here.
“Patients treated with enhanced recovery did better,” Rebecca Marcus, MD, said in reporting the results. “There were decreased rates of perioperative transfusions, decreased rates of surgical site infections, decreased rates of complications, including severe complications such as wound dehiscence, pneumonia, renal failure, and unintended returns to the operating room.” She noted that the shorter hospital stays – 4 days for patients on the enhanced recovery protocol versus 5 days for those on the traditional postoperative protocol – did not result in increased readmissions.
The study reviewed 3,256 operations performed during 2011-2016 in the MD Anderson institutional American College of Surgeons National Surgical Quality Improvement Program database. The operations were colorectal (20.4%), gynecologic (19.5%), hepatobiliary (8.9%), thoracic (41.9%) and urologic (9.3%). Most employed the traditional postoperative protocol (53.4%). Colorectal and thoracic/vascular surgery were early adopters of the enhanced recovery protocol at MD Anderson.
Dr. Marcus noted that the overall complication rates were 21.9% for those treated with enhanced recovery–protocol versus 33.9% for those treated with traditional postoperative protocol (P less than .0001). The group treated with enhanced recovery protocol also had lower rates of severe complications: 8.7% vs. 11.7% (P =.0048). The study also noted a trend toward reduced National Surgical Quality Improvement Program 30-day mortality with the enhanced recover protocol (0.4% vs. 0.86%; P = .097). Readmission rates were similar between the two groups: 8.3% for enhanced recovery protocol versus 8.9% for traditional postoperative protocol.
The researchers performed a subanalysis of high-magnitude cases that had a relative value unit of 30 or more and involved operations of greater complexity, which constituted 38% of the study population. “In this group, we still saw the benefit of having treatment with an enhanced recovery protocol with decreased rates of preoperative transfusions, complications, and shorter length of stay without any recent readmission,” Dr. Marcus said. Complication rates in the high-magnitude group were 19% for the enhanced recovery protocol versus 26% for the traditional postoperative protocol in colorectal cases, 21% vs. 40% in gynecology, and 19% vs. 28% in thoracic/vascular.
“The beneficial impact of enhanced recovery appears to be maintained across all specialties and to be independent of case magnitude,” Dr. Marcus said.
She said future research of enhanced recovery in surgical oncology should focus on more long-term outcomes, “such as oncologic benefits of these protocols, especially given the known detrimental effect of the delayed return to adjuvant therapy for this patient population.”
Dr. Marcus and her coauthors reported having no financial disclosures.
SOURCE: Marcus RK et al. SSO 2018, Abstract 21.
CHICAGO – Use of an enhanced recovery protocol for oncology patients has been shown to improve outcomes in colorectal surgery but has been largely unproven in other types of major oncology operations. That prompted researchers at the University of Texas MD Anderson Cancer Center in Houston to investigate They found that the enhanced recovery protocol led to a reduction in complication rates and a decrease in hospital stay with no increase in readmissions, according to an analysis of more than 3,000 oncologic operations presented at the Society of Surgical Oncology Annual Cancer Symposium here.
“Patients treated with enhanced recovery did better,” Rebecca Marcus, MD, said in reporting the results. “There were decreased rates of perioperative transfusions, decreased rates of surgical site infections, decreased rates of complications, including severe complications such as wound dehiscence, pneumonia, renal failure, and unintended returns to the operating room.” She noted that the shorter hospital stays – 4 days for patients on the enhanced recovery protocol versus 5 days for those on the traditional postoperative protocol – did not result in increased readmissions.
The study reviewed 3,256 operations performed during 2011-2016 in the MD Anderson institutional American College of Surgeons National Surgical Quality Improvement Program database. The operations were colorectal (20.4%), gynecologic (19.5%), hepatobiliary (8.9%), thoracic (41.9%) and urologic (9.3%). Most employed the traditional postoperative protocol (53.4%). Colorectal and thoracic/vascular surgery were early adopters of the enhanced recovery protocol at MD Anderson.
Dr. Marcus noted that the overall complication rates were 21.9% for those treated with enhanced recovery–protocol versus 33.9% for those treated with traditional postoperative protocol (P less than .0001). The group treated with enhanced recovery protocol also had lower rates of severe complications: 8.7% vs. 11.7% (P =.0048). The study also noted a trend toward reduced National Surgical Quality Improvement Program 30-day mortality with the enhanced recover protocol (0.4% vs. 0.86%; P = .097). Readmission rates were similar between the two groups: 8.3% for enhanced recovery protocol versus 8.9% for traditional postoperative protocol.
The researchers performed a subanalysis of high-magnitude cases that had a relative value unit of 30 or more and involved operations of greater complexity, which constituted 38% of the study population. “In this group, we still saw the benefit of having treatment with an enhanced recovery protocol with decreased rates of preoperative transfusions, complications, and shorter length of stay without any recent readmission,” Dr. Marcus said. Complication rates in the high-magnitude group were 19% for the enhanced recovery protocol versus 26% for the traditional postoperative protocol in colorectal cases, 21% vs. 40% in gynecology, and 19% vs. 28% in thoracic/vascular.
“The beneficial impact of enhanced recovery appears to be maintained across all specialties and to be independent of case magnitude,” Dr. Marcus said.
She said future research of enhanced recovery in surgical oncology should focus on more long-term outcomes, “such as oncologic benefits of these protocols, especially given the known detrimental effect of the delayed return to adjuvant therapy for this patient population.”
Dr. Marcus and her coauthors reported having no financial disclosures.
SOURCE: Marcus RK et al. SSO 2018, Abstract 21.
CHICAGO – Use of an enhanced recovery protocol for oncology patients has been shown to improve outcomes in colorectal surgery but has been largely unproven in other types of major oncology operations. That prompted researchers at the University of Texas MD Anderson Cancer Center in Houston to investigate They found that the enhanced recovery protocol led to a reduction in complication rates and a decrease in hospital stay with no increase in readmissions, according to an analysis of more than 3,000 oncologic operations presented at the Society of Surgical Oncology Annual Cancer Symposium here.
“Patients treated with enhanced recovery did better,” Rebecca Marcus, MD, said in reporting the results. “There were decreased rates of perioperative transfusions, decreased rates of surgical site infections, decreased rates of complications, including severe complications such as wound dehiscence, pneumonia, renal failure, and unintended returns to the operating room.” She noted that the shorter hospital stays – 4 days for patients on the enhanced recovery protocol versus 5 days for those on the traditional postoperative protocol – did not result in increased readmissions.
The study reviewed 3,256 operations performed during 2011-2016 in the MD Anderson institutional American College of Surgeons National Surgical Quality Improvement Program database. The operations were colorectal (20.4%), gynecologic (19.5%), hepatobiliary (8.9%), thoracic (41.9%) and urologic (9.3%). Most employed the traditional postoperative protocol (53.4%). Colorectal and thoracic/vascular surgery were early adopters of the enhanced recovery protocol at MD Anderson.
Dr. Marcus noted that the overall complication rates were 21.9% for those treated with enhanced recovery–protocol versus 33.9% for those treated with traditional postoperative protocol (P less than .0001). The group treated with enhanced recovery protocol also had lower rates of severe complications: 8.7% vs. 11.7% (P =.0048). The study also noted a trend toward reduced National Surgical Quality Improvement Program 30-day mortality with the enhanced recover protocol (0.4% vs. 0.86%; P = .097). Readmission rates were similar between the two groups: 8.3% for enhanced recovery protocol versus 8.9% for traditional postoperative protocol.
The researchers performed a subanalysis of high-magnitude cases that had a relative value unit of 30 or more and involved operations of greater complexity, which constituted 38% of the study population. “In this group, we still saw the benefit of having treatment with an enhanced recovery protocol with decreased rates of preoperative transfusions, complications, and shorter length of stay without any recent readmission,” Dr. Marcus said. Complication rates in the high-magnitude group were 19% for the enhanced recovery protocol versus 26% for the traditional postoperative protocol in colorectal cases, 21% vs. 40% in gynecology, and 19% vs. 28% in thoracic/vascular.
“The beneficial impact of enhanced recovery appears to be maintained across all specialties and to be independent of case magnitude,” Dr. Marcus said.
She said future research of enhanced recovery in surgical oncology should focus on more long-term outcomes, “such as oncologic benefits of these protocols, especially given the known detrimental effect of the delayed return to adjuvant therapy for this patient population.”
Dr. Marcus and her coauthors reported having no financial disclosures.
SOURCE: Marcus RK et al. SSO 2018, Abstract 21.
REPORTING FROM SSO 2018
Key clinical point: Enhanced recovery protocol implementation is feasible in major oncologic surgery.
Major finding: Complication rates were 21.9% for enhanced recovery protocol versus 33.9% for traditional postoperative protocol.
Study details: Analysis of 3,256 oncology operations in an institutional ACS NSQIP database performed from 2011 to 2016.
Disclosures: Dr. Marcus and her coauthors reported having no financial disclosures.
Source: Marcus RK et al. SSO 2018, Abstract 21
Study: Preop EKGs have little utility for benign hysterectomy
ORLANDO – Preoperative electrocardiograms (EKGs) had no effect on management or perioperative complications in women undergoing benign hysterectomy over a 12-month period at a single medical center, according to a review of records.
Of 587 patients included in the review, 182 (31%) underwent EKG as part of their preoperative evaluation, and the majority of those were indicated according to institutional criteria (166; 28%) or National Institute for Health Care Excellence (NICE) guidelines (177; 30%), Nemi M. Shah, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“EKG was indicated in 91% of these patients according to institutional criteria, and in 97% of patients per NICE criteria,” said Dr. Shah, a third-year resident at the University of Texas Southwestern Medical Center, Dallas.
By institutional criteria, hypertension was the most common indication (68% of cases), and by NICE criteria, American Society of Anesthesia class 2 physical status was the most common indication (80% of cases), she noted, adding that obesity, which was present in 70% of patients, was the most common comorbidity classifying patients with American Society of Anesthesia class 2 or above.
Of the 182 EKGs performed, findings were abnormal in 89, but further workup was pursued in only 16 patients, and included repeat EKG, echocardiogram, and/or stress testing and cardiology consultation. Surgical delays of 1 and 4 months occurred in 2 patients as a result of the additional workup, and ultimately, all planned hysterectomies were completed by the primary surgical team without changes in management, she said.
Perioperative complications occurred in two patients, and included nonspecific postinduction EKG changes that led to surgery being aborted in one patient who had left ventricular hypertrophy on the preoperative EKG, and failed extubation in a patient with airway edema whose preoperative EKG showed a nonacute inferior infarct.
For the first, cardiology was consulted and determined the findings to be benign; the patient underwent hysterectomy at a later date without complications. The second patient was taken to the surgical intensive care unit for management, Dr. Shah said.
“Preoperative testing for benign hysterectomy is variable as there is no single standard of care,” she explained. “Though tests such as EKG are commonly ordered, there are no data linking study results to surgical outcomes.”
The current study was conducted to evaluate the rate of preoperative EKG performed in concordance with institutional and NICE guidelines, and to assess implications for management and perioperative complications.
Patients included in the review were adult women who underwent scheduled benign hysterectomy during 2016. Women who underwent emergency surgery or whose surgery was performed by gynecologic oncologists were excluded.
Subjects were primarily Hispanic, and had a mean age of 45 years, Dr. Shah noted.
Though limited by the single-center design and retrospective nature of the study, the findings suggest that preoperative EKG has little clinical utility.
“We found that practice patterns were highly concordant with institutional and NICE guidelines. However, EKG resulted in minimal impact on perioperative management, and no association between abnormal EKG and perioperative complications was found,” she said. “EKG may not accurately stratify perioperative cardiopulmonary risk, and alternative methods for preoperative evaluation should be considered.”
Dr. Shah reported having no disclosures.
SOURCE: Shah N et al. SGS 2018 Oral Poster 3.
ORLANDO – Preoperative electrocardiograms (EKGs) had no effect on management or perioperative complications in women undergoing benign hysterectomy over a 12-month period at a single medical center, according to a review of records.
Of 587 patients included in the review, 182 (31%) underwent EKG as part of their preoperative evaluation, and the majority of those were indicated according to institutional criteria (166; 28%) or National Institute for Health Care Excellence (NICE) guidelines (177; 30%), Nemi M. Shah, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“EKG was indicated in 91% of these patients according to institutional criteria, and in 97% of patients per NICE criteria,” said Dr. Shah, a third-year resident at the University of Texas Southwestern Medical Center, Dallas.
By institutional criteria, hypertension was the most common indication (68% of cases), and by NICE criteria, American Society of Anesthesia class 2 physical status was the most common indication (80% of cases), she noted, adding that obesity, which was present in 70% of patients, was the most common comorbidity classifying patients with American Society of Anesthesia class 2 or above.
Of the 182 EKGs performed, findings were abnormal in 89, but further workup was pursued in only 16 patients, and included repeat EKG, echocardiogram, and/or stress testing and cardiology consultation. Surgical delays of 1 and 4 months occurred in 2 patients as a result of the additional workup, and ultimately, all planned hysterectomies were completed by the primary surgical team without changes in management, she said.
Perioperative complications occurred in two patients, and included nonspecific postinduction EKG changes that led to surgery being aborted in one patient who had left ventricular hypertrophy on the preoperative EKG, and failed extubation in a patient with airway edema whose preoperative EKG showed a nonacute inferior infarct.
For the first, cardiology was consulted and determined the findings to be benign; the patient underwent hysterectomy at a later date without complications. The second patient was taken to the surgical intensive care unit for management, Dr. Shah said.
“Preoperative testing for benign hysterectomy is variable as there is no single standard of care,” she explained. “Though tests such as EKG are commonly ordered, there are no data linking study results to surgical outcomes.”
The current study was conducted to evaluate the rate of preoperative EKG performed in concordance with institutional and NICE guidelines, and to assess implications for management and perioperative complications.
Patients included in the review were adult women who underwent scheduled benign hysterectomy during 2016. Women who underwent emergency surgery or whose surgery was performed by gynecologic oncologists were excluded.
Subjects were primarily Hispanic, and had a mean age of 45 years, Dr. Shah noted.
Though limited by the single-center design and retrospective nature of the study, the findings suggest that preoperative EKG has little clinical utility.
“We found that practice patterns were highly concordant with institutional and NICE guidelines. However, EKG resulted in minimal impact on perioperative management, and no association between abnormal EKG and perioperative complications was found,” she said. “EKG may not accurately stratify perioperative cardiopulmonary risk, and alternative methods for preoperative evaluation should be considered.”
Dr. Shah reported having no disclosures.
SOURCE: Shah N et al. SGS 2018 Oral Poster 3.
ORLANDO – Preoperative electrocardiograms (EKGs) had no effect on management or perioperative complications in women undergoing benign hysterectomy over a 12-month period at a single medical center, according to a review of records.
Of 587 patients included in the review, 182 (31%) underwent EKG as part of their preoperative evaluation, and the majority of those were indicated according to institutional criteria (166; 28%) or National Institute for Health Care Excellence (NICE) guidelines (177; 30%), Nemi M. Shah, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“EKG was indicated in 91% of these patients according to institutional criteria, and in 97% of patients per NICE criteria,” said Dr. Shah, a third-year resident at the University of Texas Southwestern Medical Center, Dallas.
By institutional criteria, hypertension was the most common indication (68% of cases), and by NICE criteria, American Society of Anesthesia class 2 physical status was the most common indication (80% of cases), she noted, adding that obesity, which was present in 70% of patients, was the most common comorbidity classifying patients with American Society of Anesthesia class 2 or above.
Of the 182 EKGs performed, findings were abnormal in 89, but further workup was pursued in only 16 patients, and included repeat EKG, echocardiogram, and/or stress testing and cardiology consultation. Surgical delays of 1 and 4 months occurred in 2 patients as a result of the additional workup, and ultimately, all planned hysterectomies were completed by the primary surgical team without changes in management, she said.
Perioperative complications occurred in two patients, and included nonspecific postinduction EKG changes that led to surgery being aborted in one patient who had left ventricular hypertrophy on the preoperative EKG, and failed extubation in a patient with airway edema whose preoperative EKG showed a nonacute inferior infarct.
For the first, cardiology was consulted and determined the findings to be benign; the patient underwent hysterectomy at a later date without complications. The second patient was taken to the surgical intensive care unit for management, Dr. Shah said.
“Preoperative testing for benign hysterectomy is variable as there is no single standard of care,” she explained. “Though tests such as EKG are commonly ordered, there are no data linking study results to surgical outcomes.”
The current study was conducted to evaluate the rate of preoperative EKG performed in concordance with institutional and NICE guidelines, and to assess implications for management and perioperative complications.
Patients included in the review were adult women who underwent scheduled benign hysterectomy during 2016. Women who underwent emergency surgery or whose surgery was performed by gynecologic oncologists were excluded.
Subjects were primarily Hispanic, and had a mean age of 45 years, Dr. Shah noted.
Though limited by the single-center design and retrospective nature of the study, the findings suggest that preoperative EKG has little clinical utility.
“We found that practice patterns were highly concordant with institutional and NICE guidelines. However, EKG resulted in minimal impact on perioperative management, and no association between abnormal EKG and perioperative complications was found,” she said. “EKG may not accurately stratify perioperative cardiopulmonary risk, and alternative methods for preoperative evaluation should be considered.”
Dr. Shah reported having no disclosures.
SOURCE: Shah N et al. SGS 2018 Oral Poster 3.
REPORTING FROM SGS 2018
Key clinical point: Preoperative EKG appears to have little utility in patients undergoing benign hysterectomy.
Major finding: Only 16 of 89 patients with abnormal preoperative EKG underwent further workup, and surgery was delayed in only two cases.
Study details: A retrospective review of 587 cases.
Disclosures: Dr. Shah reported having no disclosures.
Source: Shah N et al. SGS 2018 Oral Poster 3.
Complication rates rise after decline in uterine fibroid morcellation
The rate of major and minor 30-day complications from the treatment of uterine fibroids has increased significantly since the Food and Drug Administration’s black-box warning against the use of power morcellation, data suggest.
Researchers examined the incidence of 30-day posthysterectomy complications in 75,487 women who underwent treatment for benign gynecologic indications before and after November 2014, when the FDA’s edict was issued over concerns about the risk of disseminating benign or malignant disease. Of these women, 25,571 had uterine fibroids as the indication for hysterectomy.
The retrospective cohort study, published online April 11 in JAMA Surgery, showed that while the overall rate of complications in the cohort was relatively unchanged before and after the FDA’s warning, complication rates increased significantly in women undergoing treatment for uterine fibroids.
Before the FDA’s announcement, the 30-day major complication rate in women undergoing hysterectomy for uterine fibroids was 1.9%, which increased to 2.4% after the FDA’s warning (odds ratio, 1.23; 95% confidence interval, 1.04-1.47; P = .02). Similarly, the rate of minor 30-day complications increased from 2.7% before the warning to 3.3% after the warning (OR, 1.21; 95% CI, 1.04-1.40; P = .01), after adjustment for factors such as age, body mass index, comorbidities, and other associated procedures.
“This 20% increase in the odds of major and minor complications could translate into a large number of additional complications among the 200,000 hysterectomies performed annually for uterine fibroids in the United States,” wrote Francesco Multinu, MD, of the department of obstetrics and gynecology at the Mayo Clinic, Rochester, Minn., and his coauthors.
Overall, the researchers saw a much higher rate of major complications in women undergoing open abdominal surgery, compared with women who underwent minimally invasive surgery or vaginal hysterectomy (3.5% vs. 1.7% vs. 1.7%). A similar pattern was seen in the subgroup of women who underwent hysterectomy for uterine fibroids (2.8% vs. 1.8% vs. 1.8%).
However, minor 30-day complication rates were higher in women who underwent vaginal hysterectomy (4.5%), compared with open abdominal surgery (4.1%) and minimally invasive surgery (3.2%). In women with uterine fibroids, the minor complication rates were slightly higher in those who underwent open hysterectomy or vaginal hysterectomy than in those who had minimally invasive surgery, but this was not statistically significant.
The type of surgery in women with uterine fibroids changed significantly after the FDA announcement. Before the black-box warning against power morcellation was issued, 37.2% of hysterectomy procedures for uterine fibroids were open, 56.1% were minimally invasive, and 6.7% were vaginal. After the announcement, the percentage that were open procedures increased to 43%, minimally invasive procedures decreased to 49.7%, and vaginal hysterectomies increased to 7.3% (P less than .001).
A similar but less pronounced trend was seen across all hysterectomies for benign gynecological indications.
The authors noted that the study analyzed data on 30-day complications, so they weren’t able to draw conclusions about longer-term outcomes.
“Although caution is required to avoid morcellation of unexpected uterine malignant neoplasms, our results should be considered by women and clinicians during the process of shared decision making and by medical societies and regulatory bodies when issuing safety communications,” the authors wrote.
The study was supported by a grant from the National Center for Advancing Translational Sciences, and one author was supported by the University of Insubria, and by Fondo Miglierina, Varese, Italy. No conflicts of interest were declared.
SOURCE: Multinu F et al. JAMA Surg. 2018 Apr 11. doi: 10.1001/jamasurg.2018.0141.
The rate of major and minor 30-day complications from the treatment of uterine fibroids has increased significantly since the Food and Drug Administration’s black-box warning against the use of power morcellation, data suggest.
Researchers examined the incidence of 30-day posthysterectomy complications in 75,487 women who underwent treatment for benign gynecologic indications before and after November 2014, when the FDA’s edict was issued over concerns about the risk of disseminating benign or malignant disease. Of these women, 25,571 had uterine fibroids as the indication for hysterectomy.
The retrospective cohort study, published online April 11 in JAMA Surgery, showed that while the overall rate of complications in the cohort was relatively unchanged before and after the FDA’s warning, complication rates increased significantly in women undergoing treatment for uterine fibroids.
Before the FDA’s announcement, the 30-day major complication rate in women undergoing hysterectomy for uterine fibroids was 1.9%, which increased to 2.4% after the FDA’s warning (odds ratio, 1.23; 95% confidence interval, 1.04-1.47; P = .02). Similarly, the rate of minor 30-day complications increased from 2.7% before the warning to 3.3% after the warning (OR, 1.21; 95% CI, 1.04-1.40; P = .01), after adjustment for factors such as age, body mass index, comorbidities, and other associated procedures.
“This 20% increase in the odds of major and minor complications could translate into a large number of additional complications among the 200,000 hysterectomies performed annually for uterine fibroids in the United States,” wrote Francesco Multinu, MD, of the department of obstetrics and gynecology at the Mayo Clinic, Rochester, Minn., and his coauthors.
Overall, the researchers saw a much higher rate of major complications in women undergoing open abdominal surgery, compared with women who underwent minimally invasive surgery or vaginal hysterectomy (3.5% vs. 1.7% vs. 1.7%). A similar pattern was seen in the subgroup of women who underwent hysterectomy for uterine fibroids (2.8% vs. 1.8% vs. 1.8%).
However, minor 30-day complication rates were higher in women who underwent vaginal hysterectomy (4.5%), compared with open abdominal surgery (4.1%) and minimally invasive surgery (3.2%). In women with uterine fibroids, the minor complication rates were slightly higher in those who underwent open hysterectomy or vaginal hysterectomy than in those who had minimally invasive surgery, but this was not statistically significant.
The type of surgery in women with uterine fibroids changed significantly after the FDA announcement. Before the black-box warning against power morcellation was issued, 37.2% of hysterectomy procedures for uterine fibroids were open, 56.1% were minimally invasive, and 6.7% were vaginal. After the announcement, the percentage that were open procedures increased to 43%, minimally invasive procedures decreased to 49.7%, and vaginal hysterectomies increased to 7.3% (P less than .001).
A similar but less pronounced trend was seen across all hysterectomies for benign gynecological indications.
The authors noted that the study analyzed data on 30-day complications, so they weren’t able to draw conclusions about longer-term outcomes.
“Although caution is required to avoid morcellation of unexpected uterine malignant neoplasms, our results should be considered by women and clinicians during the process of shared decision making and by medical societies and regulatory bodies when issuing safety communications,” the authors wrote.
The study was supported by a grant from the National Center for Advancing Translational Sciences, and one author was supported by the University of Insubria, and by Fondo Miglierina, Varese, Italy. No conflicts of interest were declared.
SOURCE: Multinu F et al. JAMA Surg. 2018 Apr 11. doi: 10.1001/jamasurg.2018.0141.
The rate of major and minor 30-day complications from the treatment of uterine fibroids has increased significantly since the Food and Drug Administration’s black-box warning against the use of power morcellation, data suggest.
Researchers examined the incidence of 30-day posthysterectomy complications in 75,487 women who underwent treatment for benign gynecologic indications before and after November 2014, when the FDA’s edict was issued over concerns about the risk of disseminating benign or malignant disease. Of these women, 25,571 had uterine fibroids as the indication for hysterectomy.
The retrospective cohort study, published online April 11 in JAMA Surgery, showed that while the overall rate of complications in the cohort was relatively unchanged before and after the FDA’s warning, complication rates increased significantly in women undergoing treatment for uterine fibroids.
Before the FDA’s announcement, the 30-day major complication rate in women undergoing hysterectomy for uterine fibroids was 1.9%, which increased to 2.4% after the FDA’s warning (odds ratio, 1.23; 95% confidence interval, 1.04-1.47; P = .02). Similarly, the rate of minor 30-day complications increased from 2.7% before the warning to 3.3% after the warning (OR, 1.21; 95% CI, 1.04-1.40; P = .01), after adjustment for factors such as age, body mass index, comorbidities, and other associated procedures.
“This 20% increase in the odds of major and minor complications could translate into a large number of additional complications among the 200,000 hysterectomies performed annually for uterine fibroids in the United States,” wrote Francesco Multinu, MD, of the department of obstetrics and gynecology at the Mayo Clinic, Rochester, Minn., and his coauthors.
Overall, the researchers saw a much higher rate of major complications in women undergoing open abdominal surgery, compared with women who underwent minimally invasive surgery or vaginal hysterectomy (3.5% vs. 1.7% vs. 1.7%). A similar pattern was seen in the subgroup of women who underwent hysterectomy for uterine fibroids (2.8% vs. 1.8% vs. 1.8%).
However, minor 30-day complication rates were higher in women who underwent vaginal hysterectomy (4.5%), compared with open abdominal surgery (4.1%) and minimally invasive surgery (3.2%). In women with uterine fibroids, the minor complication rates were slightly higher in those who underwent open hysterectomy or vaginal hysterectomy than in those who had minimally invasive surgery, but this was not statistically significant.
The type of surgery in women with uterine fibroids changed significantly after the FDA announcement. Before the black-box warning against power morcellation was issued, 37.2% of hysterectomy procedures for uterine fibroids were open, 56.1% were minimally invasive, and 6.7% were vaginal. After the announcement, the percentage that were open procedures increased to 43%, minimally invasive procedures decreased to 49.7%, and vaginal hysterectomies increased to 7.3% (P less than .001).
A similar but less pronounced trend was seen across all hysterectomies for benign gynecological indications.
The authors noted that the study analyzed data on 30-day complications, so they weren’t able to draw conclusions about longer-term outcomes.
“Although caution is required to avoid morcellation of unexpected uterine malignant neoplasms, our results should be considered by women and clinicians during the process of shared decision making and by medical societies and regulatory bodies when issuing safety communications,” the authors wrote.
The study was supported by a grant from the National Center for Advancing Translational Sciences, and one author was supported by the University of Insubria, and by Fondo Miglierina, Varese, Italy. No conflicts of interest were declared.
SOURCE: Multinu F et al. JAMA Surg. 2018 Apr 11. doi: 10.1001/jamasurg.2018.0141.
FROM JAMA SURGERY
Key clinical point: Major complications from uterine fibroid hysterectomies have increased with more open surgeries.
Major finding: The rate of 30-day complications after uterine fibroid hysterectomy has increased by 20%.
Study details: A retrospective cohort study of 75,487 women.
Disclosures: The study was supported by a grant from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health, and one author was supported by the University of Insubria, and by Fondo Miglierina, Varese, Italy. No conflicts of interest were declared.
Source: Multinu F et al. JAMA Surg. 2018 Apr 11. doi: 10.1001/jamasurg.2018.0141.
Can adhesive small bowel obstructions be addressed laparoscopically?
LAS VEGAS – whether they are open or laparoscopic. Small bowel obstructions can result, and management decisions can be complex. What if the patient resolves? Should you offer elective adhesiolysis? If it doesn’t resolve, can the surgery be done laparoscopically or should the procedure be open?
Bradley R. Davis, MD, FACS, discussed some of these options, and the case circumstances that inform the surgeon’s choices at the Annual Minimally Invasive Surgery Symposium by -Global Academy for Medical Education. Dr. Davis is chief of general surgery and of rectal surgery at Carolinas Medical Center, Charlotte, N.C.
Laparoscopic surgeries are associated with significantly lower rates of small bowel obstruction, but it can still happen. More often, patients will have had a previous open surgery, and this should be a selling point for doing first-time surgeries using minimally invasive techniques. “That’s one thing I tell my patients when I see them in the office. There’s a real reduction in adhesive small bowel obstruction and certainly in hernia formation, so there are long-term benefits that I don’t think we talk enough about,” said Dr. Davis.
Although the majority of obstructions are caused by adhesions, some are the result of malignancies or hernias, and Dr. Davis encourages his residents to do exams to determine if a hernia is to blame. “That’s harder and harder to do now that everyone does a CT scan, but that’s always an interesting question to ask a resident,” he said. Inflammatory bowel disease is sometimes also a cause, but that’s rare.
CT scans are the diagnostic mode of choice for small bowel obstructions. Some believe that oral contrast agents may help resolve obstructions, but Dr. Davis mentioned evidence from a study showing that contrast agents don’t change the course of obstructions or reduce laparotomy rates. However, contrast agents can help predict the clinical course of an obstruction. If the contrast agent is present in the colon at 24 hours, then that predicts that the patient will resolve with conservative treatment. “You have a pretty good idea that the patient is going to get better,” said Dr. Davis.
The American Association for the Surgery of Trauma severity grade is helpful for adhesive small bowel obstructions. Grade 2 cases involve intestinal distension and possibly a transition zone, some passage of contrast on follow-up films, and no evidence of intestinal compromise. Grade 3 cases have no distal contrast flow and evidence of complete obstruction or impending bowel compromise. In the latter cases, “we’re scratching our heads wondering whether to take the patient to the operating room. Certainly most of these cases we’ll manage initially nonoperatively, but those patients will end up getting an earlier operation,” said Dr. Davis.
The majority of surgeries are adhesiolysis, sometimes with a bowel resection. Whether or not the surgery can be performed laparoscopically or as an open surgery depends on several factors. If the index operation was done laparoscopically, chances are good that the adhesiolysis can be performed the same way. On the other hand, “if a patient has a known hostile abdomen, I wouldn’t even try. I would basically go straight to an open procedure,” said Dr. Davis.
Generally speaking, though, reoperative surgeries can be attempted laparoscopically and then converted to open procedures if needed, he added. The most common reasons for conversion are dense adhesions and ischemia-related resection.
However, iatrogenic injuries can also occur as a result of trocar access. “Just keep in mind that if you put the trocar into the bowel, the worst thing you can do is take it out because you won’t always find that hole. Just leave the trocar in the bowel, convert to an open procedure, and find the hole and fix it,” said Dr. Davis.
Cases are particularly challenging when the transition zone is in the pelvis. Those procedures are difficult to do laparoscopically because of a difficult angle, and they are more likely to convert to open surgery. “To be honest, that’s not an easy operation to open either, so beware that transition zone in the pelvis can be a difficult case.
“I don’t try to do anything heroic laparoscopically. If you put a camera in and you find it’s going to be a massive adhesiolysis laparoscopically, you might just be better off to open,” said Dr. Davis. In cases like that it can be hard to find the transition zone, which must be identified in order to ensure that the underlying problem is fixed.
An aggressive option in difficult cases is to use a PEEK Port, which starts with a 6-8 cm incision. The surgeon can open up a minimum of disposables and put a hand in to assist the laparoscopic view and determine if the procedure can be completed laparoscopically. “If you encounter extensive adhesions, you just convert to a laparotomy and you haven’t lost any time or spent any money in terms of disposables,” he said.
Dr. Davis had no disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – whether they are open or laparoscopic. Small bowel obstructions can result, and management decisions can be complex. What if the patient resolves? Should you offer elective adhesiolysis? If it doesn’t resolve, can the surgery be done laparoscopically or should the procedure be open?
Bradley R. Davis, MD, FACS, discussed some of these options, and the case circumstances that inform the surgeon’s choices at the Annual Minimally Invasive Surgery Symposium by -Global Academy for Medical Education. Dr. Davis is chief of general surgery and of rectal surgery at Carolinas Medical Center, Charlotte, N.C.
Laparoscopic surgeries are associated with significantly lower rates of small bowel obstruction, but it can still happen. More often, patients will have had a previous open surgery, and this should be a selling point for doing first-time surgeries using minimally invasive techniques. “That’s one thing I tell my patients when I see them in the office. There’s a real reduction in adhesive small bowel obstruction and certainly in hernia formation, so there are long-term benefits that I don’t think we talk enough about,” said Dr. Davis.
Although the majority of obstructions are caused by adhesions, some are the result of malignancies or hernias, and Dr. Davis encourages his residents to do exams to determine if a hernia is to blame. “That’s harder and harder to do now that everyone does a CT scan, but that’s always an interesting question to ask a resident,” he said. Inflammatory bowel disease is sometimes also a cause, but that’s rare.
CT scans are the diagnostic mode of choice for small bowel obstructions. Some believe that oral contrast agents may help resolve obstructions, but Dr. Davis mentioned evidence from a study showing that contrast agents don’t change the course of obstructions or reduce laparotomy rates. However, contrast agents can help predict the clinical course of an obstruction. If the contrast agent is present in the colon at 24 hours, then that predicts that the patient will resolve with conservative treatment. “You have a pretty good idea that the patient is going to get better,” said Dr. Davis.
The American Association for the Surgery of Trauma severity grade is helpful for adhesive small bowel obstructions. Grade 2 cases involve intestinal distension and possibly a transition zone, some passage of contrast on follow-up films, and no evidence of intestinal compromise. Grade 3 cases have no distal contrast flow and evidence of complete obstruction or impending bowel compromise. In the latter cases, “we’re scratching our heads wondering whether to take the patient to the operating room. Certainly most of these cases we’ll manage initially nonoperatively, but those patients will end up getting an earlier operation,” said Dr. Davis.
The majority of surgeries are adhesiolysis, sometimes with a bowel resection. Whether or not the surgery can be performed laparoscopically or as an open surgery depends on several factors. If the index operation was done laparoscopically, chances are good that the adhesiolysis can be performed the same way. On the other hand, “if a patient has a known hostile abdomen, I wouldn’t even try. I would basically go straight to an open procedure,” said Dr. Davis.
Generally speaking, though, reoperative surgeries can be attempted laparoscopically and then converted to open procedures if needed, he added. The most common reasons for conversion are dense adhesions and ischemia-related resection.
However, iatrogenic injuries can also occur as a result of trocar access. “Just keep in mind that if you put the trocar into the bowel, the worst thing you can do is take it out because you won’t always find that hole. Just leave the trocar in the bowel, convert to an open procedure, and find the hole and fix it,” said Dr. Davis.
Cases are particularly challenging when the transition zone is in the pelvis. Those procedures are difficult to do laparoscopically because of a difficult angle, and they are more likely to convert to open surgery. “To be honest, that’s not an easy operation to open either, so beware that transition zone in the pelvis can be a difficult case.
“I don’t try to do anything heroic laparoscopically. If you put a camera in and you find it’s going to be a massive adhesiolysis laparoscopically, you might just be better off to open,” said Dr. Davis. In cases like that it can be hard to find the transition zone, which must be identified in order to ensure that the underlying problem is fixed.
An aggressive option in difficult cases is to use a PEEK Port, which starts with a 6-8 cm incision. The surgeon can open up a minimum of disposables and put a hand in to assist the laparoscopic view and determine if the procedure can be completed laparoscopically. “If you encounter extensive adhesions, you just convert to a laparotomy and you haven’t lost any time or spent any money in terms of disposables,” he said.
Dr. Davis had no disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – whether they are open or laparoscopic. Small bowel obstructions can result, and management decisions can be complex. What if the patient resolves? Should you offer elective adhesiolysis? If it doesn’t resolve, can the surgery be done laparoscopically or should the procedure be open?
Bradley R. Davis, MD, FACS, discussed some of these options, and the case circumstances that inform the surgeon’s choices at the Annual Minimally Invasive Surgery Symposium by -Global Academy for Medical Education. Dr. Davis is chief of general surgery and of rectal surgery at Carolinas Medical Center, Charlotte, N.C.
Laparoscopic surgeries are associated with significantly lower rates of small bowel obstruction, but it can still happen. More often, patients will have had a previous open surgery, and this should be a selling point for doing first-time surgeries using minimally invasive techniques. “That’s one thing I tell my patients when I see them in the office. There’s a real reduction in adhesive small bowel obstruction and certainly in hernia formation, so there are long-term benefits that I don’t think we talk enough about,” said Dr. Davis.
Although the majority of obstructions are caused by adhesions, some are the result of malignancies or hernias, and Dr. Davis encourages his residents to do exams to determine if a hernia is to blame. “That’s harder and harder to do now that everyone does a CT scan, but that’s always an interesting question to ask a resident,” he said. Inflammatory bowel disease is sometimes also a cause, but that’s rare.
CT scans are the diagnostic mode of choice for small bowel obstructions. Some believe that oral contrast agents may help resolve obstructions, but Dr. Davis mentioned evidence from a study showing that contrast agents don’t change the course of obstructions or reduce laparotomy rates. However, contrast agents can help predict the clinical course of an obstruction. If the contrast agent is present in the colon at 24 hours, then that predicts that the patient will resolve with conservative treatment. “You have a pretty good idea that the patient is going to get better,” said Dr. Davis.
The American Association for the Surgery of Trauma severity grade is helpful for adhesive small bowel obstructions. Grade 2 cases involve intestinal distension and possibly a transition zone, some passage of contrast on follow-up films, and no evidence of intestinal compromise. Grade 3 cases have no distal contrast flow and evidence of complete obstruction or impending bowel compromise. In the latter cases, “we’re scratching our heads wondering whether to take the patient to the operating room. Certainly most of these cases we’ll manage initially nonoperatively, but those patients will end up getting an earlier operation,” said Dr. Davis.
The majority of surgeries are adhesiolysis, sometimes with a bowel resection. Whether or not the surgery can be performed laparoscopically or as an open surgery depends on several factors. If the index operation was done laparoscopically, chances are good that the adhesiolysis can be performed the same way. On the other hand, “if a patient has a known hostile abdomen, I wouldn’t even try. I would basically go straight to an open procedure,” said Dr. Davis.
Generally speaking, though, reoperative surgeries can be attempted laparoscopically and then converted to open procedures if needed, he added. The most common reasons for conversion are dense adhesions and ischemia-related resection.
However, iatrogenic injuries can also occur as a result of trocar access. “Just keep in mind that if you put the trocar into the bowel, the worst thing you can do is take it out because you won’t always find that hole. Just leave the trocar in the bowel, convert to an open procedure, and find the hole and fix it,” said Dr. Davis.
Cases are particularly challenging when the transition zone is in the pelvis. Those procedures are difficult to do laparoscopically because of a difficult angle, and they are more likely to convert to open surgery. “To be honest, that’s not an easy operation to open either, so beware that transition zone in the pelvis can be a difficult case.
“I don’t try to do anything heroic laparoscopically. If you put a camera in and you find it’s going to be a massive adhesiolysis laparoscopically, you might just be better off to open,” said Dr. Davis. In cases like that it can be hard to find the transition zone, which must be identified in order to ensure that the underlying problem is fixed.
An aggressive option in difficult cases is to use a PEEK Port, which starts with a 6-8 cm incision. The surgeon can open up a minimum of disposables and put a hand in to assist the laparoscopic view and determine if the procedure can be completed laparoscopically. “If you encounter extensive adhesions, you just convert to a laparotomy and you haven’t lost any time or spent any money in terms of disposables,” he said.
Dr. Davis had no disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM MISS
Residual single-site ovarian cancer surpasses multisite outcomes
NEW ORLEANS – When complete resection of advanced-stage, epithelial ovarian cancer is not possible, surgical resection that leaves a small volume of residual tumor at a single site produces significantly better outcomes than leaving minimal residual cancer at multiple sites, according to a review of 510 patients at two U.S. centers.
“In the past, we separated these patients based on whether they had a complete resection, R0 disease, or had 1 cm or less of residual disease” regardless of the number of sites with this small amount of residual tumor. The third category was patients with more than 1 cm of residual tumor at one or more sites, explained Dr. Manning-Geist in an interview. “What we did was break down the patients with 1 cm or less of residual tumor into those with one site or multiple sites. This is the first reported study to use number of sites” as a clinical characteristic for analysis in this context.
The message from the findings is that, while the goal of debulking surgery in patients with advanced epithelial ovarian cancer is complete tumor resection, if that can’t be achieved, the next goal is to leave residual tumor at just a single site, she concluded. A question that remains is whether primary debulking surgery is preferable to neoadjuvant treatment followed by interval debulking surgery. In the results Dr. Manning-Geist presented, patients who underwent primary debulking had better outcomes than those with neoadjuvant therapy followed by interval debulking, but these two subgroups also had different clinical characteristics.
The study used data from 510 patients with stage IIIC or IV epithelial ovarian cancer treated at either Brigham and Women’s or Massachusetts General Hospital during 2010-2015. The study cohort included 240 patients who underwent primary debulking surgery and 270 who first received neoadjuvant chemotherapy and then underwent interval debulking surgery. The patients who received neoadjuvant therapy were, on average, older (65 years vs. 63 years), had a higher prevalence of stage IV disease (44% vs. 16%), and had a higher prevalence of tumors with serous histology (93% vs. 77%), compared with patients who underwent primary debulking.
Complete tumor resections occurred in 39% of the primary debulking patients and in 64% of those who received neoadjuvant therapy; residual disease of 1 cm or less at one site occurred in 17% and 13%, respectively; minimal residual disease at multiple sites remained in 28% and 17% respectively; and the remaining patients had residual disease of more than 1 cm in at least one site, 16% and 6% respectively.
For this analysis, Dr. Manning-Geist and her associates considered residual disease at any of seven possible sites: diaphragm, upper abdomen, bowel mesentary, bowel serosa, abdominal peritoneum, pelvis, and nodal. Even if multiple individual metastases remained within one of these sites after surgery, it was categorized as a single site of residual disease.
Among patients who underwent primary debulking surgery, progression-free survival persisted for a median of 23 months among patients with full resection, 19 months in patients with a single site with minimal residual disease, 13 months among those with multiple sites of residual disease, and 10 months in patients with more than 1 cm of residual tumor. Median overall survival in these four subgroups was not yet reached, 64 months, 50 months, and 49 months, respectively.
Among patients who received neoadjuvant chemotherapy and then underwent interval debulking surgery, median durations of progression-free survival were 14 months, 12 months, 10 months, and 6 months, respectively. Median overall survival rates were 58 months, 37 months, 26 months, and 33 months, respectively. Within each of these four analyses, the differences in both survival and progression-free survival across the four subgroups was statistically significant, with a P less than .001 for each analysis.
In multivariate analyses, among patients who underwent primary debulking surgery, the significant linkages with worsening progression-free and overall survival were age, cancer stage, and amount and site number of residual disease. Among patients who received neoadjuvant chemotherapy followed by interval debulking residual disease diameter and site number of residual tumor was the only significant determinant for both progression-free and overall survival, Dr. Manning-Geist reported.
Dr. Manning-Geist had no disclosures.
SOURCE: Manning-Geist B et al. SGO 2018, Abstract 43.
NEW ORLEANS – When complete resection of advanced-stage, epithelial ovarian cancer is not possible, surgical resection that leaves a small volume of residual tumor at a single site produces significantly better outcomes than leaving minimal residual cancer at multiple sites, according to a review of 510 patients at two U.S. centers.
“In the past, we separated these patients based on whether they had a complete resection, R0 disease, or had 1 cm or less of residual disease” regardless of the number of sites with this small amount of residual tumor. The third category was patients with more than 1 cm of residual tumor at one or more sites, explained Dr. Manning-Geist in an interview. “What we did was break down the patients with 1 cm or less of residual tumor into those with one site or multiple sites. This is the first reported study to use number of sites” as a clinical characteristic for analysis in this context.
The message from the findings is that, while the goal of debulking surgery in patients with advanced epithelial ovarian cancer is complete tumor resection, if that can’t be achieved, the next goal is to leave residual tumor at just a single site, she concluded. A question that remains is whether primary debulking surgery is preferable to neoadjuvant treatment followed by interval debulking surgery. In the results Dr. Manning-Geist presented, patients who underwent primary debulking had better outcomes than those with neoadjuvant therapy followed by interval debulking, but these two subgroups also had different clinical characteristics.
The study used data from 510 patients with stage IIIC or IV epithelial ovarian cancer treated at either Brigham and Women’s or Massachusetts General Hospital during 2010-2015. The study cohort included 240 patients who underwent primary debulking surgery and 270 who first received neoadjuvant chemotherapy and then underwent interval debulking surgery. The patients who received neoadjuvant therapy were, on average, older (65 years vs. 63 years), had a higher prevalence of stage IV disease (44% vs. 16%), and had a higher prevalence of tumors with serous histology (93% vs. 77%), compared with patients who underwent primary debulking.
Complete tumor resections occurred in 39% of the primary debulking patients and in 64% of those who received neoadjuvant therapy; residual disease of 1 cm or less at one site occurred in 17% and 13%, respectively; minimal residual disease at multiple sites remained in 28% and 17% respectively; and the remaining patients had residual disease of more than 1 cm in at least one site, 16% and 6% respectively.
For this analysis, Dr. Manning-Geist and her associates considered residual disease at any of seven possible sites: diaphragm, upper abdomen, bowel mesentary, bowel serosa, abdominal peritoneum, pelvis, and nodal. Even if multiple individual metastases remained within one of these sites after surgery, it was categorized as a single site of residual disease.
Among patients who underwent primary debulking surgery, progression-free survival persisted for a median of 23 months among patients with full resection, 19 months in patients with a single site with minimal residual disease, 13 months among those with multiple sites of residual disease, and 10 months in patients with more than 1 cm of residual tumor. Median overall survival in these four subgroups was not yet reached, 64 months, 50 months, and 49 months, respectively.
Among patients who received neoadjuvant chemotherapy and then underwent interval debulking surgery, median durations of progression-free survival were 14 months, 12 months, 10 months, and 6 months, respectively. Median overall survival rates were 58 months, 37 months, 26 months, and 33 months, respectively. Within each of these four analyses, the differences in both survival and progression-free survival across the four subgroups was statistically significant, with a P less than .001 for each analysis.
In multivariate analyses, among patients who underwent primary debulking surgery, the significant linkages with worsening progression-free and overall survival were age, cancer stage, and amount and site number of residual disease. Among patients who received neoadjuvant chemotherapy followed by interval debulking residual disease diameter and site number of residual tumor was the only significant determinant for both progression-free and overall survival, Dr. Manning-Geist reported.
Dr. Manning-Geist had no disclosures.
SOURCE: Manning-Geist B et al. SGO 2018, Abstract 43.
NEW ORLEANS – When complete resection of advanced-stage, epithelial ovarian cancer is not possible, surgical resection that leaves a small volume of residual tumor at a single site produces significantly better outcomes than leaving minimal residual cancer at multiple sites, according to a review of 510 patients at two U.S. centers.
“In the past, we separated these patients based on whether they had a complete resection, R0 disease, or had 1 cm or less of residual disease” regardless of the number of sites with this small amount of residual tumor. The third category was patients with more than 1 cm of residual tumor at one or more sites, explained Dr. Manning-Geist in an interview. “What we did was break down the patients with 1 cm or less of residual tumor into those with one site or multiple sites. This is the first reported study to use number of sites” as a clinical characteristic for analysis in this context.
The message from the findings is that, while the goal of debulking surgery in patients with advanced epithelial ovarian cancer is complete tumor resection, if that can’t be achieved, the next goal is to leave residual tumor at just a single site, she concluded. A question that remains is whether primary debulking surgery is preferable to neoadjuvant treatment followed by interval debulking surgery. In the results Dr. Manning-Geist presented, patients who underwent primary debulking had better outcomes than those with neoadjuvant therapy followed by interval debulking, but these two subgroups also had different clinical characteristics.
The study used data from 510 patients with stage IIIC or IV epithelial ovarian cancer treated at either Brigham and Women’s or Massachusetts General Hospital during 2010-2015. The study cohort included 240 patients who underwent primary debulking surgery and 270 who first received neoadjuvant chemotherapy and then underwent interval debulking surgery. The patients who received neoadjuvant therapy were, on average, older (65 years vs. 63 years), had a higher prevalence of stage IV disease (44% vs. 16%), and had a higher prevalence of tumors with serous histology (93% vs. 77%), compared with patients who underwent primary debulking.
Complete tumor resections occurred in 39% of the primary debulking patients and in 64% of those who received neoadjuvant therapy; residual disease of 1 cm or less at one site occurred in 17% and 13%, respectively; minimal residual disease at multiple sites remained in 28% and 17% respectively; and the remaining patients had residual disease of more than 1 cm in at least one site, 16% and 6% respectively.
For this analysis, Dr. Manning-Geist and her associates considered residual disease at any of seven possible sites: diaphragm, upper abdomen, bowel mesentary, bowel serosa, abdominal peritoneum, pelvis, and nodal. Even if multiple individual metastases remained within one of these sites after surgery, it was categorized as a single site of residual disease.
Among patients who underwent primary debulking surgery, progression-free survival persisted for a median of 23 months among patients with full resection, 19 months in patients with a single site with minimal residual disease, 13 months among those with multiple sites of residual disease, and 10 months in patients with more than 1 cm of residual tumor. Median overall survival in these four subgroups was not yet reached, 64 months, 50 months, and 49 months, respectively.
Among patients who received neoadjuvant chemotherapy and then underwent interval debulking surgery, median durations of progression-free survival were 14 months, 12 months, 10 months, and 6 months, respectively. Median overall survival rates were 58 months, 37 months, 26 months, and 33 months, respectively. Within each of these four analyses, the differences in both survival and progression-free survival across the four subgroups was statistically significant, with a P less than .001 for each analysis.
In multivariate analyses, among patients who underwent primary debulking surgery, the significant linkages with worsening progression-free and overall survival were age, cancer stage, and amount and site number of residual disease. Among patients who received neoadjuvant chemotherapy followed by interval debulking residual disease diameter and site number of residual tumor was the only significant determinant for both progression-free and overall survival, Dr. Manning-Geist reported.
Dr. Manning-Geist had no disclosures.
SOURCE: Manning-Geist B et al. SGO 2018, Abstract 43.
REPORTING FROM SGO 2018
Key clinical point:
Major finding: Median overall survival after primary debulking was 64 months with single-site residual disease and 50 months with multisite disease.
Study details: Retrospective review of 510 patients from two U.S. centers.
Disclosures: Dr. Manning-Geist had no disclosures.
Source: Manning-Geist BL et al. SGO 2018, Abstract 43.
Most physicians support Medicaid work requirements
Almost 75% of physicians support the new federal policy that permits states to attach work requirements to Medicaid participation, according to a survey by physician recruitment firm Merritt Hawkins.
Physicians have to limit the number of Medicaid patients they treat for that reason and want to focus on those who need care the most,” Travis Singleton, executive vice president of Merritt Hawkins, said in a statement.
Kentucky, Indiana, and Arkansas currently are in the process of putting the work requirements into place. Kentucky’s policy will require able-bodied Medicaid applicants aged 19-64 years to do 80 hours of community engagement a month by working, going to school, training for a job, or volunteering, the company said.
The survey, which was conducted by email in early March, had a margin of error of less than 1%.
Almost 75% of physicians support the new federal policy that permits states to attach work requirements to Medicaid participation, according to a survey by physician recruitment firm Merritt Hawkins.
Physicians have to limit the number of Medicaid patients they treat for that reason and want to focus on those who need care the most,” Travis Singleton, executive vice president of Merritt Hawkins, said in a statement.
Kentucky, Indiana, and Arkansas currently are in the process of putting the work requirements into place. Kentucky’s policy will require able-bodied Medicaid applicants aged 19-64 years to do 80 hours of community engagement a month by working, going to school, training for a job, or volunteering, the company said.
The survey, which was conducted by email in early March, had a margin of error of less than 1%.
Almost 75% of physicians support the new federal policy that permits states to attach work requirements to Medicaid participation, according to a survey by physician recruitment firm Merritt Hawkins.
Physicians have to limit the number of Medicaid patients they treat for that reason and want to focus on those who need care the most,” Travis Singleton, executive vice president of Merritt Hawkins, said in a statement.
Kentucky, Indiana, and Arkansas currently are in the process of putting the work requirements into place. Kentucky’s policy will require able-bodied Medicaid applicants aged 19-64 years to do 80 hours of community engagement a month by working, going to school, training for a job, or volunteering, the company said.
The survey, which was conducted by email in early March, had a margin of error of less than 1%.
VIDEO: Interventions target opioid overprescribing after gynecologic surgery
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – U.S. clinicians prescribe opioid tablets to postsurgical patients too often and at too high a pill count, according to results from two independent studies that examined prescribing patterns and opioid use in patients following gynecologic surgery.
In addition, “setting preoperative expectations about pain management led to increased compliance at discharge,” said Dr. Mark, a gynecologic oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
Findings from the second study, of 122 women who underwent gynecologic surgery at Women and Infants Hospital in Providence, R.I., showed that 32% did not use any opioids for pain following hospital discharge, and that opioid use during hospitalization was a significant predictor of postdischarge opioid needs. This finding provided a way to devise a new prescribing guide for postsurgical patients based on their opioid use while hospitalized, said Erica Weston, MD, a gynecologic oncologist at Johns Hopkins University, Baltimore.
“No question, we are overprescribing,” Dr. Dowdy said, and described a program he and his colleagues at Mayo recently put in place that capped routine opioid pill prescriptions following various surgeries based on historic patient needs. For example, most laparotomy patients receive a prescription for 10 opioid doses on discharge. Based on the first 6 months of this program, it’s on track to cut the annual number of opioid tablets prescribed to postsurgical patients at Mayo by 35,000 for all gynecologic surgeries and by 1.5 million tablets for all Mayo surgical subspecialties, he said.
The study reported by Dr. Mark ran after the Roswell Park gynecologic oncology department implemented new guidelines for dispensing pain control medications following surgery. The guidelines called for comprehensive teaching for patients about pain expectations and pain management both before and after surgery and also established four dispensing categories:
- Patients undergoing minimally invasive or outpatient surgery and with no history of chronic pain and low opioid need while hospitalized received the default dispense of 600 mg ibuprofen every 6 hours as needed for 7 days and 500 mg acetaminophen every 6 hours as needed for 7 days.
- Patients who underwent this surgery but required 5 or more opioid tablets while hospitalized or those with a history of chronic pain and opioid use received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply with 1 tablet taken every 6 hours as needed.
- Patients who underwent laparotomy and had no chronic pain and opioid history and low opioid use while hospitalized received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply.
- Patients who underwent laparotomy and showed a higher opioid need based on their use during the 24 hours before discharge received the ibuprofen and acetaminophen regimen plus 24 opioid tablets for 3 days so they could take 2 tablets every 6 hours as needed.
Dr. Mark and his associates collected data from 337 patients managed with these guidelines during June 2017–January 2018 and compared them with 626 patients who underwent gynecologic surgery at Roswell Park during July 2016–June 2017. The data showed the average number of opioid tablets dispensed per patient for all discharges fell from 31.7 before the new guideline to 3.5, an 89% reduction. For the subgroup of patients who had undergone a laparotomy, the average pill number fell from 43.6 to 11.6, a 72% drop. Among patients treated with minimally invasive or outpatient surgery, average tablets dispensed fell from 28.1 before to 0.9 after, a 97% reduction. The reduction among opioid-naive patients was 90%, and it was 83% among patients who used opioids prior to their surgery.
Under the new program, patients requested an opioid refill 14% of the time after laparotomy and 8% of the time after minimally invasive surgery, rates that did not significantly differ from the prior era. Average postoperative pain scores were identical among patients treated under the new dispensing guidelines and those treated during the prior years, and 96% of patients said they were satisfied with the care they received during the new, restricted dispensing period, Dr. Mark reported.
The single-center experience reviewed by Dr. Weston tracked opioid use by 122 women who underwent a minimally invasive hysterectomy at Women and Infants both as inpatients and out to both 1-2 weeks and 4-6 weeks following discharge. The patients were an average age of 61 years, and included 16% who reported chronic pain and 5% with a history of chronic opioid use.
During the inpatient phase, median opioid use was three doses, with 25% of the patients using no opioids. During the first 1-2 weeks following discharge, median opioid use was nine tablets, with 37% of the patients using no opioids. By the 4- to 6-week follow-up (which collected data from 114 of the patients), median opioid use was a cumulative 11 tablets with 67% of the patients reporting no opioid use during the time between their first and second follow-up visit. During the total postdischarge period, 90% of the patients used 30 or fewer opioid tablets.
A multivariate analysis of the findings showed that opioid use while in hospital was the only significant predictor of opioid use after discharge. Age of 65 years or older showed a nonsignificant trend toward less postdischarge opioid use.
Based on these data Dr. Weston and her associates proposed a formula for estimating a patient’s opioid needs at discharge: Gynecologic surgery patients who needed no opioid medication as inpatients could receive 1-5 opioid tablets at discharge, patients who used opioids at or below the median level should receive 10-15 tablets at discharge, and those who used more than the median number of opioid tablets as inpatients should receive 25-30 tablets at discharge. For patients who undergo surgery as outpatients and have no record of pain medication needs, Dr. Weston recommended discharging them with a prescription for 25-30 tablets, possibly reducing this to 10-15 tablets for patients aged 65 years or older.
Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
SOURCE: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
The important and thought provoking reports by Dr. Mark and by Dr. Weston and their associates present innovative ways for clinicians to address the opioid crisis by prescribing fewer narcotics to postsurgical patients when they leave the hospital. Their work suggests that doing this can have little or no negative impact on patient satisfaction with their care. Their findings give us important documentation for prescribing fewer opioid tablets, while still giving patients adequate pain relief.

Their findings also provide clear documentation that, in current practice, without guidance like this opioids are often overprescribed, not out of negligence but because clinicians are simply not sure what a patient will need once they go home following gynecologic surgery. By reviewing the pain medication a patient needed in hospital we can better estimate what patients will need when they go home, and we can better avoid giving patients more opioid tablets than they will really need.
Brent Smith, MD , is a gynecologic oncologist at Ohio State University, Columbus. He had no disclosures. Dr. Smith made these comments in a video interview.
The important and thought provoking reports by Dr. Mark and by Dr. Weston and their associates present innovative ways for clinicians to address the opioid crisis by prescribing fewer narcotics to postsurgical patients when they leave the hospital. Their work suggests that doing this can have little or no negative impact on patient satisfaction with their care. Their findings give us important documentation for prescribing fewer opioid tablets, while still giving patients adequate pain relief.

Their findings also provide clear documentation that, in current practice, without guidance like this opioids are often overprescribed, not out of negligence but because clinicians are simply not sure what a patient will need once they go home following gynecologic surgery. By reviewing the pain medication a patient needed in hospital we can better estimate what patients will need when they go home, and we can better avoid giving patients more opioid tablets than they will really need.
Brent Smith, MD , is a gynecologic oncologist at Ohio State University, Columbus. He had no disclosures. Dr. Smith made these comments in a video interview.
The important and thought provoking reports by Dr. Mark and by Dr. Weston and their associates present innovative ways for clinicians to address the opioid crisis by prescribing fewer narcotics to postsurgical patients when they leave the hospital. Their work suggests that doing this can have little or no negative impact on patient satisfaction with their care. Their findings give us important documentation for prescribing fewer opioid tablets, while still giving patients adequate pain relief.

Their findings also provide clear documentation that, in current practice, without guidance like this opioids are often overprescribed, not out of negligence but because clinicians are simply not sure what a patient will need once they go home following gynecologic surgery. By reviewing the pain medication a patient needed in hospital we can better estimate what patients will need when they go home, and we can better avoid giving patients more opioid tablets than they will really need.
Brent Smith, MD , is a gynecologic oncologist at Ohio State University, Columbus. He had no disclosures. Dr. Smith made these comments in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – U.S. clinicians prescribe opioid tablets to postsurgical patients too often and at too high a pill count, according to results from two independent studies that examined prescribing patterns and opioid use in patients following gynecologic surgery.
In addition, “setting preoperative expectations about pain management led to increased compliance at discharge,” said Dr. Mark, a gynecologic oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
Findings from the second study, of 122 women who underwent gynecologic surgery at Women and Infants Hospital in Providence, R.I., showed that 32% did not use any opioids for pain following hospital discharge, and that opioid use during hospitalization was a significant predictor of postdischarge opioid needs. This finding provided a way to devise a new prescribing guide for postsurgical patients based on their opioid use while hospitalized, said Erica Weston, MD, a gynecologic oncologist at Johns Hopkins University, Baltimore.
“No question, we are overprescribing,” Dr. Dowdy said, and described a program he and his colleagues at Mayo recently put in place that capped routine opioid pill prescriptions following various surgeries based on historic patient needs. For example, most laparotomy patients receive a prescription for 10 opioid doses on discharge. Based on the first 6 months of this program, it’s on track to cut the annual number of opioid tablets prescribed to postsurgical patients at Mayo by 35,000 for all gynecologic surgeries and by 1.5 million tablets for all Mayo surgical subspecialties, he said.
The study reported by Dr. Mark ran after the Roswell Park gynecologic oncology department implemented new guidelines for dispensing pain control medications following surgery. The guidelines called for comprehensive teaching for patients about pain expectations and pain management both before and after surgery and also established four dispensing categories:
- Patients undergoing minimally invasive or outpatient surgery and with no history of chronic pain and low opioid need while hospitalized received the default dispense of 600 mg ibuprofen every 6 hours as needed for 7 days and 500 mg acetaminophen every 6 hours as needed for 7 days.
- Patients who underwent this surgery but required 5 or more opioid tablets while hospitalized or those with a history of chronic pain and opioid use received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply with 1 tablet taken every 6 hours as needed.
- Patients who underwent laparotomy and had no chronic pain and opioid history and low opioid use while hospitalized received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply.
- Patients who underwent laparotomy and showed a higher opioid need based on their use during the 24 hours before discharge received the ibuprofen and acetaminophen regimen plus 24 opioid tablets for 3 days so they could take 2 tablets every 6 hours as needed.
Dr. Mark and his associates collected data from 337 patients managed with these guidelines during June 2017–January 2018 and compared them with 626 patients who underwent gynecologic surgery at Roswell Park during July 2016–June 2017. The data showed the average number of opioid tablets dispensed per patient for all discharges fell from 31.7 before the new guideline to 3.5, an 89% reduction. For the subgroup of patients who had undergone a laparotomy, the average pill number fell from 43.6 to 11.6, a 72% drop. Among patients treated with minimally invasive or outpatient surgery, average tablets dispensed fell from 28.1 before to 0.9 after, a 97% reduction. The reduction among opioid-naive patients was 90%, and it was 83% among patients who used opioids prior to their surgery.
Under the new program, patients requested an opioid refill 14% of the time after laparotomy and 8% of the time after minimally invasive surgery, rates that did not significantly differ from the prior era. Average postoperative pain scores were identical among patients treated under the new dispensing guidelines and those treated during the prior years, and 96% of patients said they were satisfied with the care they received during the new, restricted dispensing period, Dr. Mark reported.
The single-center experience reviewed by Dr. Weston tracked opioid use by 122 women who underwent a minimally invasive hysterectomy at Women and Infants both as inpatients and out to both 1-2 weeks and 4-6 weeks following discharge. The patients were an average age of 61 years, and included 16% who reported chronic pain and 5% with a history of chronic opioid use.
During the inpatient phase, median opioid use was three doses, with 25% of the patients using no opioids. During the first 1-2 weeks following discharge, median opioid use was nine tablets, with 37% of the patients using no opioids. By the 4- to 6-week follow-up (which collected data from 114 of the patients), median opioid use was a cumulative 11 tablets with 67% of the patients reporting no opioid use during the time between their first and second follow-up visit. During the total postdischarge period, 90% of the patients used 30 or fewer opioid tablets.
A multivariate analysis of the findings showed that opioid use while in hospital was the only significant predictor of opioid use after discharge. Age of 65 years or older showed a nonsignificant trend toward less postdischarge opioid use.
Based on these data Dr. Weston and her associates proposed a formula for estimating a patient’s opioid needs at discharge: Gynecologic surgery patients who needed no opioid medication as inpatients could receive 1-5 opioid tablets at discharge, patients who used opioids at or below the median level should receive 10-15 tablets at discharge, and those who used more than the median number of opioid tablets as inpatients should receive 25-30 tablets at discharge. For patients who undergo surgery as outpatients and have no record of pain medication needs, Dr. Weston recommended discharging them with a prescription for 25-30 tablets, possibly reducing this to 10-15 tablets for patients aged 65 years or older.
Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
SOURCE: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – U.S. clinicians prescribe opioid tablets to postsurgical patients too often and at too high a pill count, according to results from two independent studies that examined prescribing patterns and opioid use in patients following gynecologic surgery.
In addition, “setting preoperative expectations about pain management led to increased compliance at discharge,” said Dr. Mark, a gynecologic oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
Findings from the second study, of 122 women who underwent gynecologic surgery at Women and Infants Hospital in Providence, R.I., showed that 32% did not use any opioids for pain following hospital discharge, and that opioid use during hospitalization was a significant predictor of postdischarge opioid needs. This finding provided a way to devise a new prescribing guide for postsurgical patients based on their opioid use while hospitalized, said Erica Weston, MD, a gynecologic oncologist at Johns Hopkins University, Baltimore.
“No question, we are overprescribing,” Dr. Dowdy said, and described a program he and his colleagues at Mayo recently put in place that capped routine opioid pill prescriptions following various surgeries based on historic patient needs. For example, most laparotomy patients receive a prescription for 10 opioid doses on discharge. Based on the first 6 months of this program, it’s on track to cut the annual number of opioid tablets prescribed to postsurgical patients at Mayo by 35,000 for all gynecologic surgeries and by 1.5 million tablets for all Mayo surgical subspecialties, he said.
The study reported by Dr. Mark ran after the Roswell Park gynecologic oncology department implemented new guidelines for dispensing pain control medications following surgery. The guidelines called for comprehensive teaching for patients about pain expectations and pain management both before and after surgery and also established four dispensing categories:
- Patients undergoing minimally invasive or outpatient surgery and with no history of chronic pain and low opioid need while hospitalized received the default dispense of 600 mg ibuprofen every 6 hours as needed for 7 days and 500 mg acetaminophen every 6 hours as needed for 7 days.
- Patients who underwent this surgery but required 5 or more opioid tablets while hospitalized or those with a history of chronic pain and opioid use received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply with 1 tablet taken every 6 hours as needed.
- Patients who underwent laparotomy and had no chronic pain and opioid history and low opioid use while hospitalized received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply.
- Patients who underwent laparotomy and showed a higher opioid need based on their use during the 24 hours before discharge received the ibuprofen and acetaminophen regimen plus 24 opioid tablets for 3 days so they could take 2 tablets every 6 hours as needed.
Dr. Mark and his associates collected data from 337 patients managed with these guidelines during June 2017–January 2018 and compared them with 626 patients who underwent gynecologic surgery at Roswell Park during July 2016–June 2017. The data showed the average number of opioid tablets dispensed per patient for all discharges fell from 31.7 before the new guideline to 3.5, an 89% reduction. For the subgroup of patients who had undergone a laparotomy, the average pill number fell from 43.6 to 11.6, a 72% drop. Among patients treated with minimally invasive or outpatient surgery, average tablets dispensed fell from 28.1 before to 0.9 after, a 97% reduction. The reduction among opioid-naive patients was 90%, and it was 83% among patients who used opioids prior to their surgery.
Under the new program, patients requested an opioid refill 14% of the time after laparotomy and 8% of the time after minimally invasive surgery, rates that did not significantly differ from the prior era. Average postoperative pain scores were identical among patients treated under the new dispensing guidelines and those treated during the prior years, and 96% of patients said they were satisfied with the care they received during the new, restricted dispensing period, Dr. Mark reported.
The single-center experience reviewed by Dr. Weston tracked opioid use by 122 women who underwent a minimally invasive hysterectomy at Women and Infants both as inpatients and out to both 1-2 weeks and 4-6 weeks following discharge. The patients were an average age of 61 years, and included 16% who reported chronic pain and 5% with a history of chronic opioid use.
During the inpatient phase, median opioid use was three doses, with 25% of the patients using no opioids. During the first 1-2 weeks following discharge, median opioid use was nine tablets, with 37% of the patients using no opioids. By the 4- to 6-week follow-up (which collected data from 114 of the patients), median opioid use was a cumulative 11 tablets with 67% of the patients reporting no opioid use during the time between their first and second follow-up visit. During the total postdischarge period, 90% of the patients used 30 or fewer opioid tablets.
A multivariate analysis of the findings showed that opioid use while in hospital was the only significant predictor of opioid use after discharge. Age of 65 years or older showed a nonsignificant trend toward less postdischarge opioid use.
Based on these data Dr. Weston and her associates proposed a formula for estimating a patient’s opioid needs at discharge: Gynecologic surgery patients who needed no opioid medication as inpatients could receive 1-5 opioid tablets at discharge, patients who used opioids at or below the median level should receive 10-15 tablets at discharge, and those who used more than the median number of opioid tablets as inpatients should receive 25-30 tablets at discharge. For patients who undergo surgery as outpatients and have no record of pain medication needs, Dr. Weston recommended discharging them with a prescription for 25-30 tablets, possibly reducing this to 10-15 tablets for patients aged 65 years or older.
Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
SOURCE: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
REPORTING FROM SGO 2018
Key clinical point: Patients who underwent gynecologic surgery received adequate pain relief when receiving fewer opioid tablets.
Major finding: A protocol that restricted opioid dispensing successfully cut the discharge allotment of opioid tablets by 89%.
Study details: A single-center review of 337 patients, and a second single-center experience with 122 patients.
Disclosures: Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
Source: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
Life and health are not even across the U.S.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.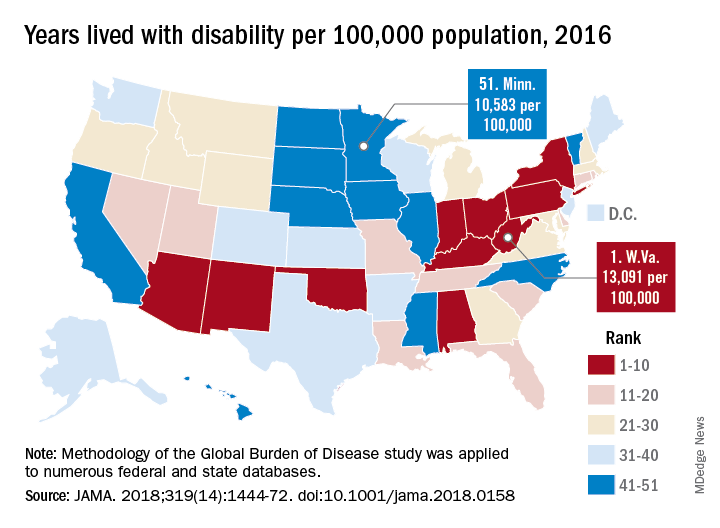
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
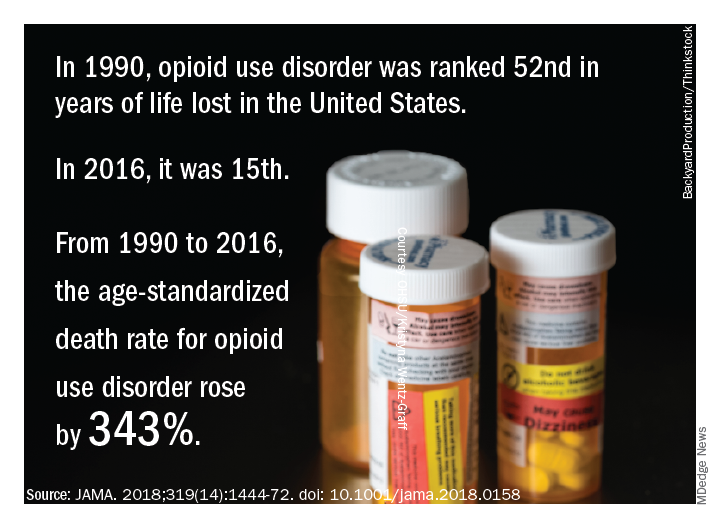
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.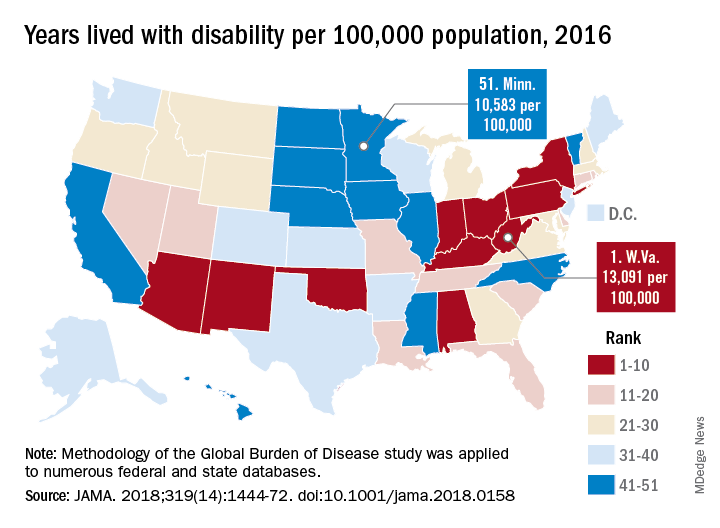
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
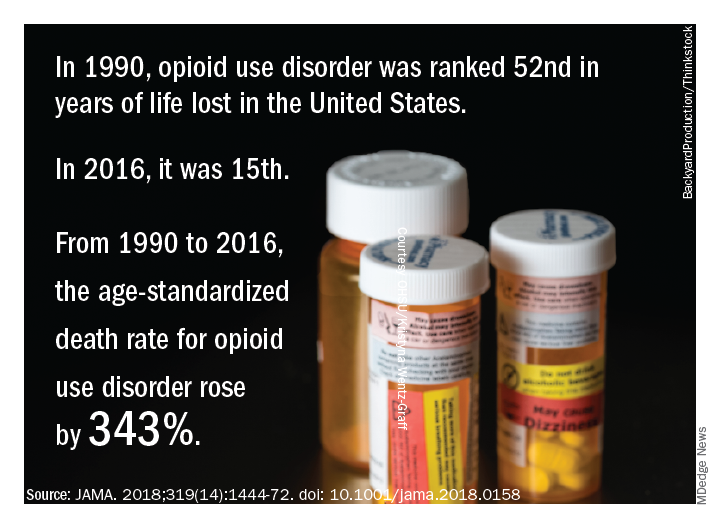
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.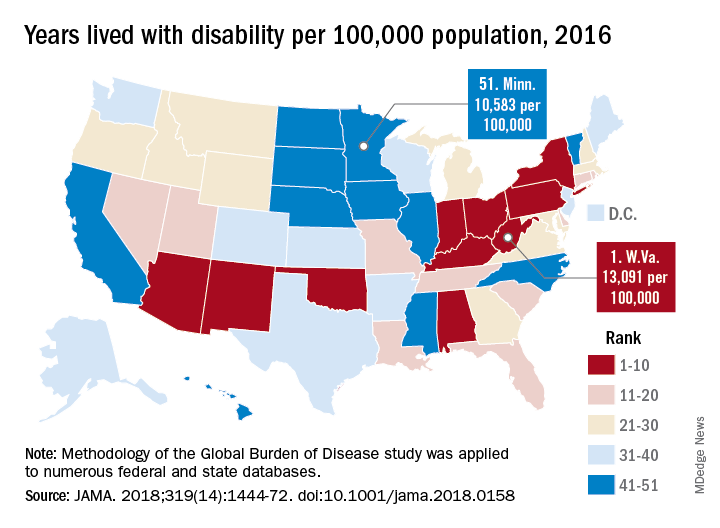
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
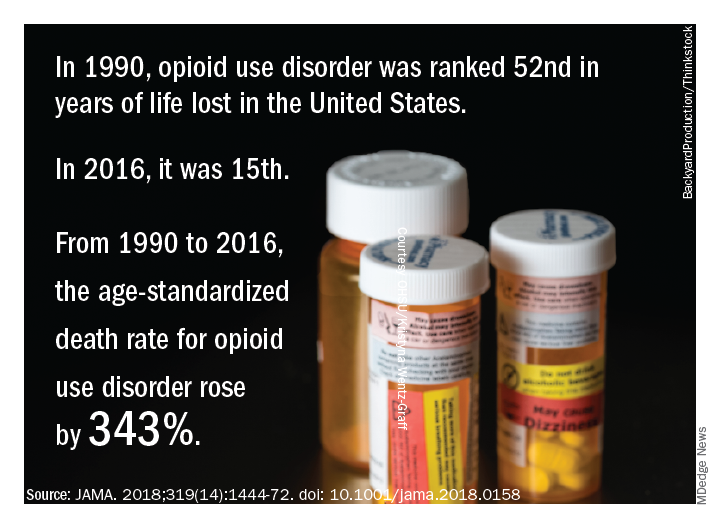
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
FROM JAMA
Key clinical point: While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors.
Major finding: Life expectancy ranged from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, and previously decreasing death rates for adults have reversed in 19 states.
Study details: A U.S. state-level analysis of results from the Global Burden of Disease (GBD) study illustrating trends in diseases, injuries, risk factors, and deaths from 1990 to 2016.
Disclosures: The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Study authors reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
Source: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-1472.
How complications drive post-surgery spending upward
JACKSONVILLE, FLA. – Post-hospital care after major surgery is a significant driver of overall surgery-related spending, and hospitals are focused on reducing this spending as payers move away from the fee-for-service model.
with a trend toward utilizing more expensive inpatient post-acute care and less outpatient care, according to an analysis of more than 700,000 Medicare procedures presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
This cross-sectional cohort study involved 707,943 cases in the Medicare database of coronary artery bypass grafting (CABG), colectomy, and total hip replacement (THR) from January 2009 to June 2012. The study found postoperative complication rates of 32% for CABG, 31% for colectomy, and 5% for THR. Postoperative complications resulted in an additional $4,083 spent on post-acute care following a CABG, an additional $4,049 after a colectomy, and an additional $1,742 after a THR.
This spending followed an increasing utilization of inpatient post-acute care and decreasing use of outpatient settings. “Relative to clinically similar patients with an uncomplicated course, patients who experienced a postoperative complication were more likely to utilize inpatient post-acute care than outpatient care,” Dr. Kanters said. For CABG, utilization rates of inpatient post-acute care increased 9.6% versus a decrease of 10.4% for outpatient post-acute care; for colectomy, inpatient post-acute care utilization increased 7.3% versus a drop of 6.2% for outpatient care; and for THR, inpatient post-acute care utilization rose 5.3% versus a drop of 2.4% for outpatient post-acute care. “The greatest impact is seen in the higher-risk procedures,” Dr. Kanters said.
The complications included cardiopulmonary complications, venous thromboembolism, renal failure, surgical site infections, and postoperative hemorrhage.
“Reductions in post-acute care spending will be central to hospitals’ efforts to reduce episode costs around major surgery,” Dr. Kanters said. “It is understood that complications are associated with increased cost, and this study helps quantify to what degree complications drive differences in spending on post-acute care.”
Hospitals’ efforts to reduce post-acute care spending must focus on preventing complications. “Thus, quality improvement efforts that reduce postoperative complications will be a key component of success in emerging payment reform,” Dr. Kanters noted
Session moderator Courtney Balentine, MD, of the University of Alabama at Birmingham, asked Dr. Kanters whether the research considered the incentives hospital systems have for referring patients to their own post-acute care facilities. “Post-acute care association with a single hospital has been documented as a likely incentive for discharge to a non-home destination,” Dr. Kanters replied, which leads to higher utilization of “certain” post-acute care facilities and higher costs. However, she said, this study’s dataset could not parse out that trend. “That’s certainly something that needs to be investigated,” she said.
Dr. Kanters and her coauthors had no financial relationships to disclose.
Source: Kanters AE. Annual Academic Surgical Congress 2018.
JACKSONVILLE, FLA. – Post-hospital care after major surgery is a significant driver of overall surgery-related spending, and hospitals are focused on reducing this spending as payers move away from the fee-for-service model.
with a trend toward utilizing more expensive inpatient post-acute care and less outpatient care, according to an analysis of more than 700,000 Medicare procedures presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
This cross-sectional cohort study involved 707,943 cases in the Medicare database of coronary artery bypass grafting (CABG), colectomy, and total hip replacement (THR) from January 2009 to June 2012. The study found postoperative complication rates of 32% for CABG, 31% for colectomy, and 5% for THR. Postoperative complications resulted in an additional $4,083 spent on post-acute care following a CABG, an additional $4,049 after a colectomy, and an additional $1,742 after a THR.
This spending followed an increasing utilization of inpatient post-acute care and decreasing use of outpatient settings. “Relative to clinically similar patients with an uncomplicated course, patients who experienced a postoperative complication were more likely to utilize inpatient post-acute care than outpatient care,” Dr. Kanters said. For CABG, utilization rates of inpatient post-acute care increased 9.6% versus a decrease of 10.4% for outpatient post-acute care; for colectomy, inpatient post-acute care utilization increased 7.3% versus a drop of 6.2% for outpatient care; and for THR, inpatient post-acute care utilization rose 5.3% versus a drop of 2.4% for outpatient post-acute care. “The greatest impact is seen in the higher-risk procedures,” Dr. Kanters said.
The complications included cardiopulmonary complications, venous thromboembolism, renal failure, surgical site infections, and postoperative hemorrhage.
“Reductions in post-acute care spending will be central to hospitals’ efforts to reduce episode costs around major surgery,” Dr. Kanters said. “It is understood that complications are associated with increased cost, and this study helps quantify to what degree complications drive differences in spending on post-acute care.”
Hospitals’ efforts to reduce post-acute care spending must focus on preventing complications. “Thus, quality improvement efforts that reduce postoperative complications will be a key component of success in emerging payment reform,” Dr. Kanters noted
Session moderator Courtney Balentine, MD, of the University of Alabama at Birmingham, asked Dr. Kanters whether the research considered the incentives hospital systems have for referring patients to their own post-acute care facilities. “Post-acute care association with a single hospital has been documented as a likely incentive for discharge to a non-home destination,” Dr. Kanters replied, which leads to higher utilization of “certain” post-acute care facilities and higher costs. However, she said, this study’s dataset could not parse out that trend. “That’s certainly something that needs to be investigated,” she said.
Dr. Kanters and her coauthors had no financial relationships to disclose.
Source: Kanters AE. Annual Academic Surgical Congress 2018.
JACKSONVILLE, FLA. – Post-hospital care after major surgery is a significant driver of overall surgery-related spending, and hospitals are focused on reducing this spending as payers move away from the fee-for-service model.
with a trend toward utilizing more expensive inpatient post-acute care and less outpatient care, according to an analysis of more than 700,000 Medicare procedures presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
This cross-sectional cohort study involved 707,943 cases in the Medicare database of coronary artery bypass grafting (CABG), colectomy, and total hip replacement (THR) from January 2009 to June 2012. The study found postoperative complication rates of 32% for CABG, 31% for colectomy, and 5% for THR. Postoperative complications resulted in an additional $4,083 spent on post-acute care following a CABG, an additional $4,049 after a colectomy, and an additional $1,742 after a THR.
This spending followed an increasing utilization of inpatient post-acute care and decreasing use of outpatient settings. “Relative to clinically similar patients with an uncomplicated course, patients who experienced a postoperative complication were more likely to utilize inpatient post-acute care than outpatient care,” Dr. Kanters said. For CABG, utilization rates of inpatient post-acute care increased 9.6% versus a decrease of 10.4% for outpatient post-acute care; for colectomy, inpatient post-acute care utilization increased 7.3% versus a drop of 6.2% for outpatient care; and for THR, inpatient post-acute care utilization rose 5.3% versus a drop of 2.4% for outpatient post-acute care. “The greatest impact is seen in the higher-risk procedures,” Dr. Kanters said.
The complications included cardiopulmonary complications, venous thromboembolism, renal failure, surgical site infections, and postoperative hemorrhage.
“Reductions in post-acute care spending will be central to hospitals’ efforts to reduce episode costs around major surgery,” Dr. Kanters said. “It is understood that complications are associated with increased cost, and this study helps quantify to what degree complications drive differences in spending on post-acute care.”
Hospitals’ efforts to reduce post-acute care spending must focus on preventing complications. “Thus, quality improvement efforts that reduce postoperative complications will be a key component of success in emerging payment reform,” Dr. Kanters noted
Session moderator Courtney Balentine, MD, of the University of Alabama at Birmingham, asked Dr. Kanters whether the research considered the incentives hospital systems have for referring patients to their own post-acute care facilities. “Post-acute care association with a single hospital has been documented as a likely incentive for discharge to a non-home destination,” Dr. Kanters replied, which leads to higher utilization of “certain” post-acute care facilities and higher costs. However, she said, this study’s dataset could not parse out that trend. “That’s certainly something that needs to be investigated,” she said.
Dr. Kanters and her coauthors had no financial relationships to disclose.
Source: Kanters AE. Annual Academic Surgical Congress 2018.
AT THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Complications after major surgery are a huge driver of increasing post-acute care spending.
Major finding: Complications after major surgery that led to post-acute care increased costs by $4,083 for coronary artery bypass grafting, $4,049 for colectomy, and $1,742 for total hip replacement.
Data source: Cross-sectional cohort study of all Medicare beneficiaries who had coronary artery bypass graft (n = 281,940), colectomy (n = 189,229) and total hip replacement (n = 231,773) between January 2009 and June 2012.
Disclosures: Dr. Kanters and her coauthors reported having no financial disclosures.
Source: Kanters AE. Annual Academic Surgical Congress 2018.
Study finds gaps in bundled colectomy payments
CHICAGO – As Medicare transitions to a value-based model that uses bundled payments, oncologic surgeons and medical institutions may want to take a close look at enhanced recovery pathways and more minimally invasive surgery for colectomy in both benign and malignant disease to close potential gaps in reimbursement and outcomes, according to a retrospective study of 4-year Medicare data presented at the Society of Surgical Oncology Annual Cancer Symposium here.
The study evaluated reimbursement rates of three Medicare Severity–Diagnosis Related Groups (MS-DRG) assigned to the study cohort of 10,928 cases in the Medicare database from 2011-2015: 331 (benign disease), 330 (colon cancer/no metastases), and 329 (metastatic colon cancer). “There is little data comparing the relative impact of MS-DRG on cost and reimbursement for oncologic versus benign colon resection as it relates to the index admission, post-acute care costs, and Centers for Medicare & Medicaid Services total costs,” Dr. Hughes said.
With descriptive statistics, the study showed that benign resection resulted in higher average total charges than malignant disease ($66,033 vs. $60,581, respectively; P less than .001) and longer hospital stays (7.25 days vs. 6.92; P less than .002), Dr. Hughes said. However, Medicare reimbursements were similar for both pathology groups: $10,358 for benign disease versus $10,483 for oncologic pathology (P = .434). Cancer patients were about 25% more likely to be discharged to a rehabilitation facility than were those in the benign group (16.6% vs. 12.4%, respectively; P less than .001).
“What we know from other data is that, compared to fee-for-service for surgical colectomies, a value-based payment model resulted in lower payments for the index admission,” Dr. Hughes said. “A greater proportion of these patients also contributed to a negative margin for hospitals when compared to the fee-for-service model, as well as a higher risk across acute care services.”
Of patients in the study cohort, 67% had surgery for malignant disease. Both benign and malignant groups had more open colectomies than minimally invasive colectomies: 60% and 36.8%, respectively, of procedures in the benign group and 63% and 40% in the cancer group (P less than .001).
The goal of the study was to identify potential gaps in adopting MS-DRG for the bundled payment model in benign versus malignant colectomy, Dr. Hughes said. The study identified three gaps:
- DRG poorly differentiates between benign and malignant disease. This problem is evidenced by the higher cost for the index admission in benign disease. “Whereas in malignant disease, there is a greater unrecognized cost-shifting to post-acute care services which are not addressed by the DRG system,” he said.
- The dominance of open colectomy where MIS could reduce episode costs. The study cited research that reported the advantages of MIS include lower episode costs in both younger and older patients, by $1,466 and $632, respectively; shorter hospital stays by 1.46 days; 20% lower 30-day readmissions rates; and lower rates of post-acute care services (J Laparoendosc Adv Surg Tech A. 2017 Dec 13. doi: 10.1089/lap.2017.0521)
- Potential for DRG migration from code 331 (benign disease) to 330 (colon cancer but not with metastasis). Dr. Hughes and his coauthors published a study that reported a 14.2% rate of DRG migration in this same Medicare cohort, that is, classified as 331 on admission but migrated to 330. So, compared with other patients, this group ended up with longer LOS (7.6 vs. 4.8 days); higher total charges ($63,149 vs. $46,339); and higher CMS payment ($11,159 vs. $7,210) (Am J Surg. 2018;215:493-6). “We also identified a potential role for enhanced-recovery pathways to mitigate these factors,” he said.
He noted that the different stakeholders – hospitals, surgeons, anesthesiologists, hospitalists, other physicians, nurses, and extenders – will have to resolve how to divide bundled payments. “The biggest thing is communication between these groups, because moving forward CMS is trying to step away from the role of determining who gets paid what,” Dr. Hughes said. He noted this finding is consistent with his own previously published findings, along with those from senior study coauthor Anthony J. Senagore, MD, FACS, on resource consumption in value-based care.
Dr. Hughes and coauthors reported having no financial disclosures. Dr. Hughes is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health.
SOURCE: Huges BD. SSO 2018.
CHICAGO – As Medicare transitions to a value-based model that uses bundled payments, oncologic surgeons and medical institutions may want to take a close look at enhanced recovery pathways and more minimally invasive surgery for colectomy in both benign and malignant disease to close potential gaps in reimbursement and outcomes, according to a retrospective study of 4-year Medicare data presented at the Society of Surgical Oncology Annual Cancer Symposium here.
The study evaluated reimbursement rates of three Medicare Severity–Diagnosis Related Groups (MS-DRG) assigned to the study cohort of 10,928 cases in the Medicare database from 2011-2015: 331 (benign disease), 330 (colon cancer/no metastases), and 329 (metastatic colon cancer). “There is little data comparing the relative impact of MS-DRG on cost and reimbursement for oncologic versus benign colon resection as it relates to the index admission, post-acute care costs, and Centers for Medicare & Medicaid Services total costs,” Dr. Hughes said.
With descriptive statistics, the study showed that benign resection resulted in higher average total charges than malignant disease ($66,033 vs. $60,581, respectively; P less than .001) and longer hospital stays (7.25 days vs. 6.92; P less than .002), Dr. Hughes said. However, Medicare reimbursements were similar for both pathology groups: $10,358 for benign disease versus $10,483 for oncologic pathology (P = .434). Cancer patients were about 25% more likely to be discharged to a rehabilitation facility than were those in the benign group (16.6% vs. 12.4%, respectively; P less than .001).
“What we know from other data is that, compared to fee-for-service for surgical colectomies, a value-based payment model resulted in lower payments for the index admission,” Dr. Hughes said. “A greater proportion of these patients also contributed to a negative margin for hospitals when compared to the fee-for-service model, as well as a higher risk across acute care services.”
Of patients in the study cohort, 67% had surgery for malignant disease. Both benign and malignant groups had more open colectomies than minimally invasive colectomies: 60% and 36.8%, respectively, of procedures in the benign group and 63% and 40% in the cancer group (P less than .001).
The goal of the study was to identify potential gaps in adopting MS-DRG for the bundled payment model in benign versus malignant colectomy, Dr. Hughes said. The study identified three gaps:
- DRG poorly differentiates between benign and malignant disease. This problem is evidenced by the higher cost for the index admission in benign disease. “Whereas in malignant disease, there is a greater unrecognized cost-shifting to post-acute care services which are not addressed by the DRG system,” he said.
- The dominance of open colectomy where MIS could reduce episode costs. The study cited research that reported the advantages of MIS include lower episode costs in both younger and older patients, by $1,466 and $632, respectively; shorter hospital stays by 1.46 days; 20% lower 30-day readmissions rates; and lower rates of post-acute care services (J Laparoendosc Adv Surg Tech A. 2017 Dec 13. doi: 10.1089/lap.2017.0521)
- Potential for DRG migration from code 331 (benign disease) to 330 (colon cancer but not with metastasis). Dr. Hughes and his coauthors published a study that reported a 14.2% rate of DRG migration in this same Medicare cohort, that is, classified as 331 on admission but migrated to 330. So, compared with other patients, this group ended up with longer LOS (7.6 vs. 4.8 days); higher total charges ($63,149 vs. $46,339); and higher CMS payment ($11,159 vs. $7,210) (Am J Surg. 2018;215:493-6). “We also identified a potential role for enhanced-recovery pathways to mitigate these factors,” he said.
He noted that the different stakeholders – hospitals, surgeons, anesthesiologists, hospitalists, other physicians, nurses, and extenders – will have to resolve how to divide bundled payments. “The biggest thing is communication between these groups, because moving forward CMS is trying to step away from the role of determining who gets paid what,” Dr. Hughes said. He noted this finding is consistent with his own previously published findings, along with those from senior study coauthor Anthony J. Senagore, MD, FACS, on resource consumption in value-based care.
Dr. Hughes and coauthors reported having no financial disclosures. Dr. Hughes is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health.
SOURCE: Huges BD. SSO 2018.
CHICAGO – As Medicare transitions to a value-based model that uses bundled payments, oncologic surgeons and medical institutions may want to take a close look at enhanced recovery pathways and more minimally invasive surgery for colectomy in both benign and malignant disease to close potential gaps in reimbursement and outcomes, according to a retrospective study of 4-year Medicare data presented at the Society of Surgical Oncology Annual Cancer Symposium here.
The study evaluated reimbursement rates of three Medicare Severity–Diagnosis Related Groups (MS-DRG) assigned to the study cohort of 10,928 cases in the Medicare database from 2011-2015: 331 (benign disease), 330 (colon cancer/no metastases), and 329 (metastatic colon cancer). “There is little data comparing the relative impact of MS-DRG on cost and reimbursement for oncologic versus benign colon resection as it relates to the index admission, post-acute care costs, and Centers for Medicare & Medicaid Services total costs,” Dr. Hughes said.
With descriptive statistics, the study showed that benign resection resulted in higher average total charges than malignant disease ($66,033 vs. $60,581, respectively; P less than .001) and longer hospital stays (7.25 days vs. 6.92; P less than .002), Dr. Hughes said. However, Medicare reimbursements were similar for both pathology groups: $10,358 for benign disease versus $10,483 for oncologic pathology (P = .434). Cancer patients were about 25% more likely to be discharged to a rehabilitation facility than were those in the benign group (16.6% vs. 12.4%, respectively; P less than .001).
“What we know from other data is that, compared to fee-for-service for surgical colectomies, a value-based payment model resulted in lower payments for the index admission,” Dr. Hughes said. “A greater proportion of these patients also contributed to a negative margin for hospitals when compared to the fee-for-service model, as well as a higher risk across acute care services.”
Of patients in the study cohort, 67% had surgery for malignant disease. Both benign and malignant groups had more open colectomies than minimally invasive colectomies: 60% and 36.8%, respectively, of procedures in the benign group and 63% and 40% in the cancer group (P less than .001).
The goal of the study was to identify potential gaps in adopting MS-DRG for the bundled payment model in benign versus malignant colectomy, Dr. Hughes said. The study identified three gaps:
- DRG poorly differentiates between benign and malignant disease. This problem is evidenced by the higher cost for the index admission in benign disease. “Whereas in malignant disease, there is a greater unrecognized cost-shifting to post-acute care services which are not addressed by the DRG system,” he said.
- The dominance of open colectomy where MIS could reduce episode costs. The study cited research that reported the advantages of MIS include lower episode costs in both younger and older patients, by $1,466 and $632, respectively; shorter hospital stays by 1.46 days; 20% lower 30-day readmissions rates; and lower rates of post-acute care services (J Laparoendosc Adv Surg Tech A. 2017 Dec 13. doi: 10.1089/lap.2017.0521)
- Potential for DRG migration from code 331 (benign disease) to 330 (colon cancer but not with metastasis). Dr. Hughes and his coauthors published a study that reported a 14.2% rate of DRG migration in this same Medicare cohort, that is, classified as 331 on admission but migrated to 330. So, compared with other patients, this group ended up with longer LOS (7.6 vs. 4.8 days); higher total charges ($63,149 vs. $46,339); and higher CMS payment ($11,159 vs. $7,210) (Am J Surg. 2018;215:493-6). “We also identified a potential role for enhanced-recovery pathways to mitigate these factors,” he said.
He noted that the different stakeholders – hospitals, surgeons, anesthesiologists, hospitalists, other physicians, nurses, and extenders – will have to resolve how to divide bundled payments. “The biggest thing is communication between these groups, because moving forward CMS is trying to step away from the role of determining who gets paid what,” Dr. Hughes said. He noted this finding is consistent with his own previously published findings, along with those from senior study coauthor Anthony J. Senagore, MD, FACS, on resource consumption in value-based care.
Dr. Hughes and coauthors reported having no financial disclosures. Dr. Hughes is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health.
SOURCE: Huges BD. SSO 2018.
REPORTING FROM SSO 2018
Key clinical point: Medicare payment methodology does not truly reflect episode costs for colectomy.
Major finding: Colectomy charges were higher for benign disease than for cancer.
Study details: Retrospective cohort study of 10,928 patients in a national Medicare database who had colon surgery during 2011-2014.
Disclosures: The investigators had no financial relationships to disclose. Dr. Hughes is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health.
Source: Huges BD. SSO 2018.