User login
Official Newspaper of the American College of Surgeons
Empiric fluid restriction cuts transsphenoidal surgery readmissions
CHICAGO – A 70% drop in 30-day was achieved at the University of Colorado, Aurora, after endocrinologists there restricted fluid for the first 2 weeks postop, according to a report at the Endocrine Society annual meeting.
The antidiuretic hormone (ADH) rebound following pituitary adenoma resection often leads to fluid retention, and potentially dangerous hyponatremia, in about 25% of patients. It’s the leading cause of readmission for this procedure, occurring in up to 15% of patients.
To counter the problem, endocrinology fellow Kelsi Deaver, MD, and her colleagues limited patients to 1.5 L of fluid for 2 weeks after discharge, with a serum sodium check at day 7. If the sodium level was normal, patients remained on 1.5 L until the 2-week postop visit. If levels trended upward – a sign of dehydration – restrictions were eased to 2 or even 3 L, which is about the normal daily intake. If sodium levels trended downward, fluids were tightened to 1-1.2 L, or patients were brought in for further workup. The discharge packet included a 1.5-L cup so patients could track their intake.
Among 118 patients studied before the protocol was implemented in September 2015, 9 (7.6%) were readmitted for symptomatic hyponatremia within 30 days. Among 169 studied after the implementation of the fluid restriction protocol, just 4 (2.4%) were readmitted for hyponatremia (P = .044).
At present, there are no widely accepted postop fluid management guidelines for transsphenoidal surgery, but some hospitals have taken similar steps, she said.
It was the fluid restriction, not the 7-day sodium check, that drove the results. Among the four readmissions after the protocol took effect, two patients had their sodium checked, and two did not because their sodium drop was so precipitous that they were back in the hospital before the week was out. Overall, only about 70% of patients got their sodium checked as instructed.
Fluid restriction isn’t easy for patients. “The last day before discharge, we try to coach them through it,” with tips about sucking on ice chips and other strategies; “anything really to help them through it,” Dr. Deaver said.
Readmitted patients were no different from others in terms of pituitary tumor subtype, tumor size, gender, and other factors. “We couldn’t find any predictors,” she said. There were a higher percentage of macroadenomas in the preimplementation patients (91.5% versus 81.7%), but they were otherwise similar to postimplementation patients.
Those with evidence of diabetes insipidus at discharge were excluded from the study.
The National Institutes of Health funded the study. The investigators did not have any disclosures.
SOURCE: Deaver KE et al. Endocrine Society 2018 annual meeting abstract SUN-572.
CHICAGO – A 70% drop in 30-day was achieved at the University of Colorado, Aurora, after endocrinologists there restricted fluid for the first 2 weeks postop, according to a report at the Endocrine Society annual meeting.
The antidiuretic hormone (ADH) rebound following pituitary adenoma resection often leads to fluid retention, and potentially dangerous hyponatremia, in about 25% of patients. It’s the leading cause of readmission for this procedure, occurring in up to 15% of patients.
To counter the problem, endocrinology fellow Kelsi Deaver, MD, and her colleagues limited patients to 1.5 L of fluid for 2 weeks after discharge, with a serum sodium check at day 7. If the sodium level was normal, patients remained on 1.5 L until the 2-week postop visit. If levels trended upward – a sign of dehydration – restrictions were eased to 2 or even 3 L, which is about the normal daily intake. If sodium levels trended downward, fluids were tightened to 1-1.2 L, or patients were brought in for further workup. The discharge packet included a 1.5-L cup so patients could track their intake.
Among 118 patients studied before the protocol was implemented in September 2015, 9 (7.6%) were readmitted for symptomatic hyponatremia within 30 days. Among 169 studied after the implementation of the fluid restriction protocol, just 4 (2.4%) were readmitted for hyponatremia (P = .044).
At present, there are no widely accepted postop fluid management guidelines for transsphenoidal surgery, but some hospitals have taken similar steps, she said.
It was the fluid restriction, not the 7-day sodium check, that drove the results. Among the four readmissions after the protocol took effect, two patients had their sodium checked, and two did not because their sodium drop was so precipitous that they were back in the hospital before the week was out. Overall, only about 70% of patients got their sodium checked as instructed.
Fluid restriction isn’t easy for patients. “The last day before discharge, we try to coach them through it,” with tips about sucking on ice chips and other strategies; “anything really to help them through it,” Dr. Deaver said.
Readmitted patients were no different from others in terms of pituitary tumor subtype, tumor size, gender, and other factors. “We couldn’t find any predictors,” she said. There were a higher percentage of macroadenomas in the preimplementation patients (91.5% versus 81.7%), but they were otherwise similar to postimplementation patients.
Those with evidence of diabetes insipidus at discharge were excluded from the study.
The National Institutes of Health funded the study. The investigators did not have any disclosures.
SOURCE: Deaver KE et al. Endocrine Society 2018 annual meeting abstract SUN-572.
CHICAGO – A 70% drop in 30-day was achieved at the University of Colorado, Aurora, after endocrinologists there restricted fluid for the first 2 weeks postop, according to a report at the Endocrine Society annual meeting.
The antidiuretic hormone (ADH) rebound following pituitary adenoma resection often leads to fluid retention, and potentially dangerous hyponatremia, in about 25% of patients. It’s the leading cause of readmission for this procedure, occurring in up to 15% of patients.
To counter the problem, endocrinology fellow Kelsi Deaver, MD, and her colleagues limited patients to 1.5 L of fluid for 2 weeks after discharge, with a serum sodium check at day 7. If the sodium level was normal, patients remained on 1.5 L until the 2-week postop visit. If levels trended upward – a sign of dehydration – restrictions were eased to 2 or even 3 L, which is about the normal daily intake. If sodium levels trended downward, fluids were tightened to 1-1.2 L, or patients were brought in for further workup. The discharge packet included a 1.5-L cup so patients could track their intake.
Among 118 patients studied before the protocol was implemented in September 2015, 9 (7.6%) were readmitted for symptomatic hyponatremia within 30 days. Among 169 studied after the implementation of the fluid restriction protocol, just 4 (2.4%) were readmitted for hyponatremia (P = .044).
At present, there are no widely accepted postop fluid management guidelines for transsphenoidal surgery, but some hospitals have taken similar steps, she said.
It was the fluid restriction, not the 7-day sodium check, that drove the results. Among the four readmissions after the protocol took effect, two patients had their sodium checked, and two did not because their sodium drop was so precipitous that they were back in the hospital before the week was out. Overall, only about 70% of patients got their sodium checked as instructed.
Fluid restriction isn’t easy for patients. “The last day before discharge, we try to coach them through it,” with tips about sucking on ice chips and other strategies; “anything really to help them through it,” Dr. Deaver said.
Readmitted patients were no different from others in terms of pituitary tumor subtype, tumor size, gender, and other factors. “We couldn’t find any predictors,” she said. There were a higher percentage of macroadenomas in the preimplementation patients (91.5% versus 81.7%), but they were otherwise similar to postimplementation patients.
Those with evidence of diabetes insipidus at discharge were excluded from the study.
The National Institutes of Health funded the study. The investigators did not have any disclosures.
SOURCE: Deaver KE et al. Endocrine Society 2018 annual meeting abstract SUN-572.
REPORTING FROM ENDO 2018
Key clinical point: A simple fluid restriction protocol cuts readmissions 70% following transsphenoidal surgery.
Major finding: The readmission rate among the transsphenoidal surgery patients was 7.6% before the fluid restriction protocol was implemented, compared with 2.4% (P = .044) afterward.
Study details: Review of 287 transsphenoidal surgery patients.
Disclosures: The National Institutes of Health supported the work. The investigators did not have any disclosures.
Source: Deaver KE et al. Abstract SUN-572
Surgery after immunotherapy effective in advanced melanoma
CHICAGO – Surgical resection is an effective treatment in selected patients with advanced melanoma treated with checkpoint blockade immunotherapy, according to a study of an institutional database at Memorial Sloan Kettering Cancer Center in New York presented at the Society of Surgical Oncology Annual Cancer Symposium.
“In the era of improved systemic therapy, checkpoint blockade for metastatic melanoma and the ability to surgically resect all disease after treatment is associated with an estimated survival of 75%, better than what’s been previously reported,” said Danielle M. Bello, MD, of Memorial Sloan Kettering.
The study analyzed a cohort of 237 patients who had unresectable stage III and IV melanoma and were treated with checkpoint blockade, including CTLA-4, programmed cell death protein 1 (PD-1), and programmed death-ligand 1 inhibitors, and then had surgical resection during 2003-2017.
Dr. Bello noted two previous studies that had reported encouraging outcomes in advanced melanoma. The first highlighted the role for surgery in stage IV melanoma. In that phase 3 clinical trial, patients had resection of up to five sites of metastatic disease and were then randomized to one of two treatment arms: bacillus Calmette-Guérin and allogeneic whole-cell vaccine (Canvaxin) or bacillus Calmette-Guérin and placebo. While this trial found no difference in overall survival between groups, it did report a 5-year overall survival exceeding 40% in both treatment arms, which highlighted that Stage IV patients who underwent resection of all their disease had survival outcomes superior to outcomes previously reported (Ann Surg Onc. 2017 Dec;24[13]:3991-4000). The second trial, the recent Checkmate 067 trial, emphasized the role of effective systemic checkpoint blockade in advanced stage III and IV melanoma. It reported that patients treated with combined nivolumab/ipilimumab therapy had not reached median overall survival at minimum 36 months of follow-up (N Engl J Med. 2017 Oct 5;377[14]:1345-56).
“We know that checkpoint inhibitor therapy has revolutionized the landscape of unresectable stage III and IV melanoma,” Dr. Bello said. However, despite encouraging trial readouts of overall survival, progression-free survival is a different story. “We know that the median progression-free survival even in our best combination therapy is 11.5 months, meaning that 50% of patients will go on to progress in a year and many will go on to surgical resection of their disease and do quite well,” she said.
Dr. Bello and her coauthors set out to describe outcomes of a “highly selective group” of patients who had surgical resection after checkpoint inhibitor therapy. “The majority of patients in our study had a cutaneous primary melanoma,” she said. Median age was 63 years, and 88% had stage IV disease. Regarding checkpoint blockade regimen, 62% received anti–CTLA-4, and 29% received combination anti–PD-1 and anti–CLTA-4 either sequentially or concomitantly prior to resection.
The median time from the start of immunotherapy to the first operation was 7 months. Forty-six percent had no further postoperative treatment after resection. In those, who did require further treatment, the majority received anti–PD-1 followed by targeted BRAF/MEK therapy, she said.
The analysis stratified patients into the following three categories based on radiological response to immunotherapy:
- Overall response to checkpoint blockade and the index lesion was either smaller since initiation of therapy or stabilized (12; 5.1%). Half of this group had a pathological complete response.
- Isolated site of progressive disease with residual stable disease elsewhere or as the only site of progressive disease (106; 44.7%).
- Multiple sites of progressive and palliative operations (119; 50.2%).
Median overall survival was 21 months in the entire study cohort with a median follow-up of 23 months, Dr. Bello said. “Those resected to no evidence of disease (NED) – 87 patients – had an estimated 5-year overall survival of 75%.” The NED group did not reach median OS.
The analysis also stratified overall survival by response to immunotherapy. “Patients with responding or stable disease had an estimated 90% 5-year overall survival,” Dr. Bellow said. “Those with one isolated progressive lesion that was resected had a 60% 5-year overall survival.” A more detailed analysis of the latter group found that those who had a resection to NED had an improved overall survival of 75% at 5 years. Resected patients who had residual remaining disease had a 30% 5-year overall survival.
“Further follow-up is needed to assess the durability and contributions of surgery, and further studies are underway to identify biomarkers associated with improved survival after immunotherapy and surgery,” Dr. Bello said.
SOURCE: Bello DM et al. SSO 2018, Abstract 5.
CHICAGO – Surgical resection is an effective treatment in selected patients with advanced melanoma treated with checkpoint blockade immunotherapy, according to a study of an institutional database at Memorial Sloan Kettering Cancer Center in New York presented at the Society of Surgical Oncology Annual Cancer Symposium.
“In the era of improved systemic therapy, checkpoint blockade for metastatic melanoma and the ability to surgically resect all disease after treatment is associated with an estimated survival of 75%, better than what’s been previously reported,” said Danielle M. Bello, MD, of Memorial Sloan Kettering.
The study analyzed a cohort of 237 patients who had unresectable stage III and IV melanoma and were treated with checkpoint blockade, including CTLA-4, programmed cell death protein 1 (PD-1), and programmed death-ligand 1 inhibitors, and then had surgical resection during 2003-2017.
Dr. Bello noted two previous studies that had reported encouraging outcomes in advanced melanoma. The first highlighted the role for surgery in stage IV melanoma. In that phase 3 clinical trial, patients had resection of up to five sites of metastatic disease and were then randomized to one of two treatment arms: bacillus Calmette-Guérin and allogeneic whole-cell vaccine (Canvaxin) or bacillus Calmette-Guérin and placebo. While this trial found no difference in overall survival between groups, it did report a 5-year overall survival exceeding 40% in both treatment arms, which highlighted that Stage IV patients who underwent resection of all their disease had survival outcomes superior to outcomes previously reported (Ann Surg Onc. 2017 Dec;24[13]:3991-4000). The second trial, the recent Checkmate 067 trial, emphasized the role of effective systemic checkpoint blockade in advanced stage III and IV melanoma. It reported that patients treated with combined nivolumab/ipilimumab therapy had not reached median overall survival at minimum 36 months of follow-up (N Engl J Med. 2017 Oct 5;377[14]:1345-56).
“We know that checkpoint inhibitor therapy has revolutionized the landscape of unresectable stage III and IV melanoma,” Dr. Bello said. However, despite encouraging trial readouts of overall survival, progression-free survival is a different story. “We know that the median progression-free survival even in our best combination therapy is 11.5 months, meaning that 50% of patients will go on to progress in a year and many will go on to surgical resection of their disease and do quite well,” she said.
Dr. Bello and her coauthors set out to describe outcomes of a “highly selective group” of patients who had surgical resection after checkpoint inhibitor therapy. “The majority of patients in our study had a cutaneous primary melanoma,” she said. Median age was 63 years, and 88% had stage IV disease. Regarding checkpoint blockade regimen, 62% received anti–CTLA-4, and 29% received combination anti–PD-1 and anti–CLTA-4 either sequentially or concomitantly prior to resection.
The median time from the start of immunotherapy to the first operation was 7 months. Forty-six percent had no further postoperative treatment after resection. In those, who did require further treatment, the majority received anti–PD-1 followed by targeted BRAF/MEK therapy, she said.
The analysis stratified patients into the following three categories based on radiological response to immunotherapy:
- Overall response to checkpoint blockade and the index lesion was either smaller since initiation of therapy or stabilized (12; 5.1%). Half of this group had a pathological complete response.
- Isolated site of progressive disease with residual stable disease elsewhere or as the only site of progressive disease (106; 44.7%).
- Multiple sites of progressive and palliative operations (119; 50.2%).
Median overall survival was 21 months in the entire study cohort with a median follow-up of 23 months, Dr. Bello said. “Those resected to no evidence of disease (NED) – 87 patients – had an estimated 5-year overall survival of 75%.” The NED group did not reach median OS.
The analysis also stratified overall survival by response to immunotherapy. “Patients with responding or stable disease had an estimated 90% 5-year overall survival,” Dr. Bellow said. “Those with one isolated progressive lesion that was resected had a 60% 5-year overall survival.” A more detailed analysis of the latter group found that those who had a resection to NED had an improved overall survival of 75% at 5 years. Resected patients who had residual remaining disease had a 30% 5-year overall survival.
“Further follow-up is needed to assess the durability and contributions of surgery, and further studies are underway to identify biomarkers associated with improved survival after immunotherapy and surgery,” Dr. Bello said.
SOURCE: Bello DM et al. SSO 2018, Abstract 5.
CHICAGO – Surgical resection is an effective treatment in selected patients with advanced melanoma treated with checkpoint blockade immunotherapy, according to a study of an institutional database at Memorial Sloan Kettering Cancer Center in New York presented at the Society of Surgical Oncology Annual Cancer Symposium.
“In the era of improved systemic therapy, checkpoint blockade for metastatic melanoma and the ability to surgically resect all disease after treatment is associated with an estimated survival of 75%, better than what’s been previously reported,” said Danielle M. Bello, MD, of Memorial Sloan Kettering.
The study analyzed a cohort of 237 patients who had unresectable stage III and IV melanoma and were treated with checkpoint blockade, including CTLA-4, programmed cell death protein 1 (PD-1), and programmed death-ligand 1 inhibitors, and then had surgical resection during 2003-2017.
Dr. Bello noted two previous studies that had reported encouraging outcomes in advanced melanoma. The first highlighted the role for surgery in stage IV melanoma. In that phase 3 clinical trial, patients had resection of up to five sites of metastatic disease and were then randomized to one of two treatment arms: bacillus Calmette-Guérin and allogeneic whole-cell vaccine (Canvaxin) or bacillus Calmette-Guérin and placebo. While this trial found no difference in overall survival between groups, it did report a 5-year overall survival exceeding 40% in both treatment arms, which highlighted that Stage IV patients who underwent resection of all their disease had survival outcomes superior to outcomes previously reported (Ann Surg Onc. 2017 Dec;24[13]:3991-4000). The second trial, the recent Checkmate 067 trial, emphasized the role of effective systemic checkpoint blockade in advanced stage III and IV melanoma. It reported that patients treated with combined nivolumab/ipilimumab therapy had not reached median overall survival at minimum 36 months of follow-up (N Engl J Med. 2017 Oct 5;377[14]:1345-56).
“We know that checkpoint inhibitor therapy has revolutionized the landscape of unresectable stage III and IV melanoma,” Dr. Bello said. However, despite encouraging trial readouts of overall survival, progression-free survival is a different story. “We know that the median progression-free survival even in our best combination therapy is 11.5 months, meaning that 50% of patients will go on to progress in a year and many will go on to surgical resection of their disease and do quite well,” she said.
Dr. Bello and her coauthors set out to describe outcomes of a “highly selective group” of patients who had surgical resection after checkpoint inhibitor therapy. “The majority of patients in our study had a cutaneous primary melanoma,” she said. Median age was 63 years, and 88% had stage IV disease. Regarding checkpoint blockade regimen, 62% received anti–CTLA-4, and 29% received combination anti–PD-1 and anti–CLTA-4 either sequentially or concomitantly prior to resection.
The median time from the start of immunotherapy to the first operation was 7 months. Forty-six percent had no further postoperative treatment after resection. In those, who did require further treatment, the majority received anti–PD-1 followed by targeted BRAF/MEK therapy, she said.
The analysis stratified patients into the following three categories based on radiological response to immunotherapy:
- Overall response to checkpoint blockade and the index lesion was either smaller since initiation of therapy or stabilized (12; 5.1%). Half of this group had a pathological complete response.
- Isolated site of progressive disease with residual stable disease elsewhere or as the only site of progressive disease (106; 44.7%).
- Multiple sites of progressive and palliative operations (119; 50.2%).
Median overall survival was 21 months in the entire study cohort with a median follow-up of 23 months, Dr. Bello said. “Those resected to no evidence of disease (NED) – 87 patients – had an estimated 5-year overall survival of 75%.” The NED group did not reach median OS.
The analysis also stratified overall survival by response to immunotherapy. “Patients with responding or stable disease had an estimated 90% 5-year overall survival,” Dr. Bellow said. “Those with one isolated progressive lesion that was resected had a 60% 5-year overall survival.” A more detailed analysis of the latter group found that those who had a resection to NED had an improved overall survival of 75% at 5 years. Resected patients who had residual remaining disease had a 30% 5-year overall survival.
“Further follow-up is needed to assess the durability and contributions of surgery, and further studies are underway to identify biomarkers associated with improved survival after immunotherapy and surgery,” Dr. Bello said.
SOURCE: Bello DM et al. SSO 2018, Abstract 5.
REPORTING FROM SSO 2018
Key clinical point: Surgery after immunotherapy can achieve good outcomes in advanced melanoma.
Major findings: Complete resection achieved an estimated 5-year overall survival of 75%.
Study details: Analysis of a cohort of 237 patients from a prospectively maintained institutional melanoma database who had surgery after immunotherapy for unresectable stage III and IV melanoma during 2003-2017.
Disclosures: Dr. Bello reported having no financial disclosures. Some coauthors reported financial relationships with various pharmaceutical companies.
Source: Bello DM et al. SSO 2018, Abstract 5.
PVT after sleeve gastrectomy treatable with anticoagulants
can be effectively treated with extended postoperative anticoagulation therapy, findings from a large-scale, retrospective study indicate.
The research was conducted using data from medical records of created by physicians from five Australian bariatric centers, reported Stephanie Bee Ming Tan, MBBS, of the Gold Coast University Hospital, Queensland, Australia, and her associates in the journal Surgery for Obesity and Related Diseases. Following elective laparoscopic sleeve gastrectomy (LSG), a total of 18 (0.3%) of the 5,951 obese patients were diagnosed with portomesenteric vein thrombosis (PVT). The PVT-affected population was a mean age of 44 years and 61% were women. All of these patients had at least one venous thrombosis systematic predisposition factor such as morbid obesity (50%), smoking (50%), or a personal or family history of a clotting disorder (39%).
All study patients were given thromboprophylaxis of low-molecular-weight heparin (LMWH) or unfractionated heparin plus mechanical thromboprophylaxis during admission for LSG and at discharge when surgeons identified them as high risk.
PVT following LSG can be difficult to diagnose because presenting symptoms tend to be nonspecific. Within an average of 13 days following surgery, 77% of patients diagnosed with PVT reported abdominal pain, 33% reported nausea and vomiting, and also reported less common symptoms that included shoulder tip pain, problems in tolerating fluids, constipation, and diarrhea. Final diagnosis of PVT was determined with independent or a combination of CT and duplex ultrasound.
Complications from PVT can have serious consequences, including abdominal swelling from fluid accumulation, enlarged esophageal veins, terminal esophageal bleeding, and bowel infarction. As with admission thromboprophylaxis treatments, patients diagnosed with PVT received varied anticoagulation treatments with most, in equal numbers, receiving either LMWH or a heparin infusion, and the remaining 12% receiving anticoagulation with rivaroxaban and warfarin. Adjustments were made following initial treatments such that 37% and 66% of patients continued with longer-term therapy on LMWH or warfarin, respectively. Treatments generally lasted 3-6 months with only 11% continuing on warfarin because of a history of clotting disorder. The anticoagulation treatments were successful with the majority (94%) of patients with only one patient requiring surgical intervention.
Follow-up with the patients who had a PVT diagnosis of more than 6 months (with an average of 10 months) showed the overall success of the post-LSG anticoagulation and surgical therapies, without any mortalities.
The authors summarized earlier theories about confounding health conditions that may contribute to the development of PVT and the risks for PVT linked to laparoscopic surgery. In this retrospective study, they noted that PVT incidence following LSG was low at 0.3% but was still higher than with two other bariatric operative methods and suggested intraoperative and postoperative factors that could contribute to this difference. Because of the nonspecific early symptoms and the difficulty of diagnosing PVT, the investigators recommended that physicians be vigilant for this postoperative complication in LSG patients, and use “cross-sectional imagining with CT of the abdomen” for diagnosis. Furthermore, with diagnosed PVT “anticoagulation for 3 to 6 months with a target international normalized ratio of 2:3 is recommended unless the patient has additional risk factors and [is] therefore indicated for longer treatment.”
The authors reported that they had no conflicts of interest.
SOURCE: Tan SBM et al. Surg Obes Relat Dis. 2018 Mar;14:271-6.
can be effectively treated with extended postoperative anticoagulation therapy, findings from a large-scale, retrospective study indicate.
The research was conducted using data from medical records of created by physicians from five Australian bariatric centers, reported Stephanie Bee Ming Tan, MBBS, of the Gold Coast University Hospital, Queensland, Australia, and her associates in the journal Surgery for Obesity and Related Diseases. Following elective laparoscopic sleeve gastrectomy (LSG), a total of 18 (0.3%) of the 5,951 obese patients were diagnosed with portomesenteric vein thrombosis (PVT). The PVT-affected population was a mean age of 44 years and 61% were women. All of these patients had at least one venous thrombosis systematic predisposition factor such as morbid obesity (50%), smoking (50%), or a personal or family history of a clotting disorder (39%).
All study patients were given thromboprophylaxis of low-molecular-weight heparin (LMWH) or unfractionated heparin plus mechanical thromboprophylaxis during admission for LSG and at discharge when surgeons identified them as high risk.
PVT following LSG can be difficult to diagnose because presenting symptoms tend to be nonspecific. Within an average of 13 days following surgery, 77% of patients diagnosed with PVT reported abdominal pain, 33% reported nausea and vomiting, and also reported less common symptoms that included shoulder tip pain, problems in tolerating fluids, constipation, and diarrhea. Final diagnosis of PVT was determined with independent or a combination of CT and duplex ultrasound.
Complications from PVT can have serious consequences, including abdominal swelling from fluid accumulation, enlarged esophageal veins, terminal esophageal bleeding, and bowel infarction. As with admission thromboprophylaxis treatments, patients diagnosed with PVT received varied anticoagulation treatments with most, in equal numbers, receiving either LMWH or a heparin infusion, and the remaining 12% receiving anticoagulation with rivaroxaban and warfarin. Adjustments were made following initial treatments such that 37% and 66% of patients continued with longer-term therapy on LMWH or warfarin, respectively. Treatments generally lasted 3-6 months with only 11% continuing on warfarin because of a history of clotting disorder. The anticoagulation treatments were successful with the majority (94%) of patients with only one patient requiring surgical intervention.
Follow-up with the patients who had a PVT diagnosis of more than 6 months (with an average of 10 months) showed the overall success of the post-LSG anticoagulation and surgical therapies, without any mortalities.
The authors summarized earlier theories about confounding health conditions that may contribute to the development of PVT and the risks for PVT linked to laparoscopic surgery. In this retrospective study, they noted that PVT incidence following LSG was low at 0.3% but was still higher than with two other bariatric operative methods and suggested intraoperative and postoperative factors that could contribute to this difference. Because of the nonspecific early symptoms and the difficulty of diagnosing PVT, the investigators recommended that physicians be vigilant for this postoperative complication in LSG patients, and use “cross-sectional imagining with CT of the abdomen” for diagnosis. Furthermore, with diagnosed PVT “anticoagulation for 3 to 6 months with a target international normalized ratio of 2:3 is recommended unless the patient has additional risk factors and [is] therefore indicated for longer treatment.”
The authors reported that they had no conflicts of interest.
SOURCE: Tan SBM et al. Surg Obes Relat Dis. 2018 Mar;14:271-6.
can be effectively treated with extended postoperative anticoagulation therapy, findings from a large-scale, retrospective study indicate.
The research was conducted using data from medical records of created by physicians from five Australian bariatric centers, reported Stephanie Bee Ming Tan, MBBS, of the Gold Coast University Hospital, Queensland, Australia, and her associates in the journal Surgery for Obesity and Related Diseases. Following elective laparoscopic sleeve gastrectomy (LSG), a total of 18 (0.3%) of the 5,951 obese patients were diagnosed with portomesenteric vein thrombosis (PVT). The PVT-affected population was a mean age of 44 years and 61% were women. All of these patients had at least one venous thrombosis systematic predisposition factor such as morbid obesity (50%), smoking (50%), or a personal or family history of a clotting disorder (39%).
All study patients were given thromboprophylaxis of low-molecular-weight heparin (LMWH) or unfractionated heparin plus mechanical thromboprophylaxis during admission for LSG and at discharge when surgeons identified them as high risk.
PVT following LSG can be difficult to diagnose because presenting symptoms tend to be nonspecific. Within an average of 13 days following surgery, 77% of patients diagnosed with PVT reported abdominal pain, 33% reported nausea and vomiting, and also reported less common symptoms that included shoulder tip pain, problems in tolerating fluids, constipation, and diarrhea. Final diagnosis of PVT was determined with independent or a combination of CT and duplex ultrasound.
Complications from PVT can have serious consequences, including abdominal swelling from fluid accumulation, enlarged esophageal veins, terminal esophageal bleeding, and bowel infarction. As with admission thromboprophylaxis treatments, patients diagnosed with PVT received varied anticoagulation treatments with most, in equal numbers, receiving either LMWH or a heparin infusion, and the remaining 12% receiving anticoagulation with rivaroxaban and warfarin. Adjustments were made following initial treatments such that 37% and 66% of patients continued with longer-term therapy on LMWH or warfarin, respectively. Treatments generally lasted 3-6 months with only 11% continuing on warfarin because of a history of clotting disorder. The anticoagulation treatments were successful with the majority (94%) of patients with only one patient requiring surgical intervention.
Follow-up with the patients who had a PVT diagnosis of more than 6 months (with an average of 10 months) showed the overall success of the post-LSG anticoagulation and surgical therapies, without any mortalities.
The authors summarized earlier theories about confounding health conditions that may contribute to the development of PVT and the risks for PVT linked to laparoscopic surgery. In this retrospective study, they noted that PVT incidence following LSG was low at 0.3% but was still higher than with two other bariatric operative methods and suggested intraoperative and postoperative factors that could contribute to this difference. Because of the nonspecific early symptoms and the difficulty of diagnosing PVT, the investigators recommended that physicians be vigilant for this postoperative complication in LSG patients, and use “cross-sectional imagining with CT of the abdomen” for diagnosis. Furthermore, with diagnosed PVT “anticoagulation for 3 to 6 months with a target international normalized ratio of 2:3 is recommended unless the patient has additional risk factors and [is] therefore indicated for longer treatment.”
The authors reported that they had no conflicts of interest.
SOURCE: Tan SBM et al. Surg Obes Relat Dis. 2018 Mar;14:271-6.
FROM SURGERY FOR OBESITY AND RELATED DISEASES
Key clinical point: Anticoagulation treatments effectively managed most portomesenteric vein thrombosis cases following laparoscopic sleeve gastrectomy.
Major finding: PVT is rare (0.3%) but occurs more frequently with laparoscopic sleeve gastrectomy, compared with other bariatric surgery procedures.
Study details: A multicenter, retrospective study conducted in Australia from 2007 to 2016 with 5,951 adult obese patients who received elective laparoscopic sleeve gastrectomy.
Disclosures: The authors reported no conflicts of interest.
Source: Tan SBM et al. Surg Obes Relat Dis. Mar 2018;14:271-6.
Can cN0 and pCR limit axillary surgery in some breast cancer patients?
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
REPORTING FROM SSO 2018
Key clinical point: Neoadjuvant chemotherapy for certain breast cancers achieves low rates of nodal positivity.
Major finding: In clinically node-negative HER2+ and triple-negative disease, nodal positivity after NAC in patients that had breast pathological complete response was less than 2%.
Study details: Review of 22,695 patients in NCDB with clinical T1 or T2 disease from 2010 to 2014.
Disclosure: Dr. Barron and coauthors reported having no financial disclosures.
Source: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
No increased complication risk with delaying resection for LARC
CHICAGO – Delaying surgery after neoadjuvant therapy for locally advanced rectal cancer for up to 12 weeks does not seem to impact complication rates compared to surgery at 8 weeks or earlier, findings that run counter to results from a major European clinical trial reported in 2016, investigators reported at the Society of Surgical Oncology Annual Cancer Symposium.
“There’s an increasing trend toward delayed surgery beyond eight to 12 weeks after neoadjuvant therapy (NT) for locally advanced rectal cancer (LARC),” said Campbell Roxburgh, FRCS, PhD, of the University of Glasgow in Scotland. “Although we saw an increase in all complications in patients who had surgery beyond 12 weeks, there were no increases in surgical site complications, grade 3-5 complications, or anastomotic leaks. Before 12 weeks we did not observe increases in any type of complication where surgery was performed prior to or after 8 weeks.”
The study involved 798 patients who had received NT for LARC from June 2009 to March 2014 at Memorial Sloan Kettering Cancer Center in New York. The vast majority – 76% (607) – had rectal resection within 16 weeks of completing NT. Among them, 52% (317) had surgery 5-8 weeks after NT, 38% (229) had surgery at 8-12 weeks post-NT, and 10% (61) had surgery 12-16 weeks after completing NT. Those who had surgery beyond 16 weeks mostly had it deferred because they were undergoing nonoperative management in the case of complete clinical response to treatment or had a comorbidity that prevented earlier surgery, Dr. Roxburgh said.
The complication rate was 42.3% among the patients who had surgery up to 16 weeks after NT, Dr. Roxburgh said. The most common complication was surgical site infection (SSI) in 16.6% (101), followed by a grade 3-5 complication in 10.5% (64) and anastomotic leak in 6.4% (39). Overall complication rates among the two groups that had surgery within 12 weeks were not statistically different from the overall complication rate, Dr. Roxburgh said: 42.5% (138) in the 5- to 8-week group; and 36.7% (84) in the 8- to 12-week group. The 12- to16-week group had a complication rate of 56% (34, P = .022).
Dr. Roxburgh noted that the idea of delaying surgery beyond 8 weeks after NT has been a subject of debate, and that these findings run counter to those reported in the GRECCAR-6 trial (J Clin Oncol. 2016;34:3773-80). That study compared groups that had surgery for rectal cancer at 7 and 11 weeks after neoadjuvant radiochemotherapy and found that those in the 11-week group had higher rates of complications.
Dr. Roxburgh also reported on an analysis of the 12- to 16-week subgroup that found the highest complication rates were among those who had low anterior resection (53% vs. 41% in the 5- to 8-week group and 31% in the 8- to 12-week population), and patients who had a poor treatment response (no T-downstaging, 66% vs. 44% and 33%, respectively). Age, pretreatment and posttreatment TNM stages, surgical approach (open or minimally invasive), and year of treatment did not factor in complication rates in the subgroup analysis, Dr. Roxburgh noted.
The univariate regression analysis determined a trend toward increased rates of all complications in the 12- to 16-week group (P = .081). But the multivariate analysis did not find timing of surgery to be an independent risk factor for all complications, Dr. Roxburgh said. “We believe other factors, including tumor location, the type of NT, operative approach, and treatment response, however, were more important on multivariate analysis,” he said. For example, open surgery had an odds ratio of 1.7 (P = .004).
During the discussion, Dr. Roxburgh was asked what would be the optimal timing for resection after NT in LARC. “I would recommend posttreatment assessment with MRI and proctoscopy between 8 to 12 weeks and in the case of residual tumor or incomplete response to treatment, scheduling surgery at that time,” he said.
Dr. Roxburgh and coauthors reported having no financial disclosures.
SOURCE: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
CHICAGO – Delaying surgery after neoadjuvant therapy for locally advanced rectal cancer for up to 12 weeks does not seem to impact complication rates compared to surgery at 8 weeks or earlier, findings that run counter to results from a major European clinical trial reported in 2016, investigators reported at the Society of Surgical Oncology Annual Cancer Symposium.
“There’s an increasing trend toward delayed surgery beyond eight to 12 weeks after neoadjuvant therapy (NT) for locally advanced rectal cancer (LARC),” said Campbell Roxburgh, FRCS, PhD, of the University of Glasgow in Scotland. “Although we saw an increase in all complications in patients who had surgery beyond 12 weeks, there were no increases in surgical site complications, grade 3-5 complications, or anastomotic leaks. Before 12 weeks we did not observe increases in any type of complication where surgery was performed prior to or after 8 weeks.”
The study involved 798 patients who had received NT for LARC from June 2009 to March 2014 at Memorial Sloan Kettering Cancer Center in New York. The vast majority – 76% (607) – had rectal resection within 16 weeks of completing NT. Among them, 52% (317) had surgery 5-8 weeks after NT, 38% (229) had surgery at 8-12 weeks post-NT, and 10% (61) had surgery 12-16 weeks after completing NT. Those who had surgery beyond 16 weeks mostly had it deferred because they were undergoing nonoperative management in the case of complete clinical response to treatment or had a comorbidity that prevented earlier surgery, Dr. Roxburgh said.
The complication rate was 42.3% among the patients who had surgery up to 16 weeks after NT, Dr. Roxburgh said. The most common complication was surgical site infection (SSI) in 16.6% (101), followed by a grade 3-5 complication in 10.5% (64) and anastomotic leak in 6.4% (39). Overall complication rates among the two groups that had surgery within 12 weeks were not statistically different from the overall complication rate, Dr. Roxburgh said: 42.5% (138) in the 5- to 8-week group; and 36.7% (84) in the 8- to 12-week group. The 12- to16-week group had a complication rate of 56% (34, P = .022).
Dr. Roxburgh noted that the idea of delaying surgery beyond 8 weeks after NT has been a subject of debate, and that these findings run counter to those reported in the GRECCAR-6 trial (J Clin Oncol. 2016;34:3773-80). That study compared groups that had surgery for rectal cancer at 7 and 11 weeks after neoadjuvant radiochemotherapy and found that those in the 11-week group had higher rates of complications.
Dr. Roxburgh also reported on an analysis of the 12- to 16-week subgroup that found the highest complication rates were among those who had low anterior resection (53% vs. 41% in the 5- to 8-week group and 31% in the 8- to 12-week population), and patients who had a poor treatment response (no T-downstaging, 66% vs. 44% and 33%, respectively). Age, pretreatment and posttreatment TNM stages, surgical approach (open or minimally invasive), and year of treatment did not factor in complication rates in the subgroup analysis, Dr. Roxburgh noted.
The univariate regression analysis determined a trend toward increased rates of all complications in the 12- to 16-week group (P = .081). But the multivariate analysis did not find timing of surgery to be an independent risk factor for all complications, Dr. Roxburgh said. “We believe other factors, including tumor location, the type of NT, operative approach, and treatment response, however, were more important on multivariate analysis,” he said. For example, open surgery had an odds ratio of 1.7 (P = .004).
During the discussion, Dr. Roxburgh was asked what would be the optimal timing for resection after NT in LARC. “I would recommend posttreatment assessment with MRI and proctoscopy between 8 to 12 weeks and in the case of residual tumor or incomplete response to treatment, scheduling surgery at that time,” he said.
Dr. Roxburgh and coauthors reported having no financial disclosures.
SOURCE: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
CHICAGO – Delaying surgery after neoadjuvant therapy for locally advanced rectal cancer for up to 12 weeks does not seem to impact complication rates compared to surgery at 8 weeks or earlier, findings that run counter to results from a major European clinical trial reported in 2016, investigators reported at the Society of Surgical Oncology Annual Cancer Symposium.
“There’s an increasing trend toward delayed surgery beyond eight to 12 weeks after neoadjuvant therapy (NT) for locally advanced rectal cancer (LARC),” said Campbell Roxburgh, FRCS, PhD, of the University of Glasgow in Scotland. “Although we saw an increase in all complications in patients who had surgery beyond 12 weeks, there were no increases in surgical site complications, grade 3-5 complications, or anastomotic leaks. Before 12 weeks we did not observe increases in any type of complication where surgery was performed prior to or after 8 weeks.”
The study involved 798 patients who had received NT for LARC from June 2009 to March 2014 at Memorial Sloan Kettering Cancer Center in New York. The vast majority – 76% (607) – had rectal resection within 16 weeks of completing NT. Among them, 52% (317) had surgery 5-8 weeks after NT, 38% (229) had surgery at 8-12 weeks post-NT, and 10% (61) had surgery 12-16 weeks after completing NT. Those who had surgery beyond 16 weeks mostly had it deferred because they were undergoing nonoperative management in the case of complete clinical response to treatment or had a comorbidity that prevented earlier surgery, Dr. Roxburgh said.
The complication rate was 42.3% among the patients who had surgery up to 16 weeks after NT, Dr. Roxburgh said. The most common complication was surgical site infection (SSI) in 16.6% (101), followed by a grade 3-5 complication in 10.5% (64) and anastomotic leak in 6.4% (39). Overall complication rates among the two groups that had surgery within 12 weeks were not statistically different from the overall complication rate, Dr. Roxburgh said: 42.5% (138) in the 5- to 8-week group; and 36.7% (84) in the 8- to 12-week group. The 12- to16-week group had a complication rate of 56% (34, P = .022).
Dr. Roxburgh noted that the idea of delaying surgery beyond 8 weeks after NT has been a subject of debate, and that these findings run counter to those reported in the GRECCAR-6 trial (J Clin Oncol. 2016;34:3773-80). That study compared groups that had surgery for rectal cancer at 7 and 11 weeks after neoadjuvant radiochemotherapy and found that those in the 11-week group had higher rates of complications.
Dr. Roxburgh also reported on an analysis of the 12- to 16-week subgroup that found the highest complication rates were among those who had low anterior resection (53% vs. 41% in the 5- to 8-week group and 31% in the 8- to 12-week population), and patients who had a poor treatment response (no T-downstaging, 66% vs. 44% and 33%, respectively). Age, pretreatment and posttreatment TNM stages, surgical approach (open or minimally invasive), and year of treatment did not factor in complication rates in the subgroup analysis, Dr. Roxburgh noted.
The univariate regression analysis determined a trend toward increased rates of all complications in the 12- to 16-week group (P = .081). But the multivariate analysis did not find timing of surgery to be an independent risk factor for all complications, Dr. Roxburgh said. “We believe other factors, including tumor location, the type of NT, operative approach, and treatment response, however, were more important on multivariate analysis,” he said. For example, open surgery had an odds ratio of 1.7 (P = .004).
During the discussion, Dr. Roxburgh was asked what would be the optimal timing for resection after NT in LARC. “I would recommend posttreatment assessment with MRI and proctoscopy between 8 to 12 weeks and in the case of residual tumor or incomplete response to treatment, scheduling surgery at that time,” he said.
Dr. Roxburgh and coauthors reported having no financial disclosures.
SOURCE: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
REPORTING FROM SSO 2018
Key clinical point: Timing of surgery for rectal cancer within 12 weeks of neoadjuvant therapy does not influence complications.
Major finding: Complication rates in early and later surgery groups were 44% and 38%.
Study details: Institutional cohort of 607 patients who had rectal resection within 16 weeks of completing NT between June 2009 and March 2015.
Disclosure: Dr. Roxburgh and coauthors reported having no financial disclosures.
Source: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
VIDEO: Cervical cancer laparotomy outperforms minimally invasive surgery
NEW ORLEANS – Use of minimally invasive radical hysterectomy to treat early-stage cervical cancer has grown over the past decade, and in current U.S. practice, roughly half of these cases are done with a minimally-invasive approach, with the rest done by conventional laparotomy. But the first data ever reported from a large, prospective trial that compared the efficacy of both methods for cervical cancer had the unexpected finding that disease-free survival following minimally invasive procedures significantly lagged behind radical hysterectomies done by open laparotomy, Pedro T. Ramirez, MD, said at the annual meeting of the Society of Gynecologic Oncology.
Just after this report came results from a second study that used propensity score–adjusted observational data from the National Cancer Database and found significantly worse overall survival following minimally invasive radical hysterectomy for early-stage cervical cancer, compared with laparotomy, said J. Alejandro Rauh-Hain, MD, a gynecologic oncologist at the University of Texas MD Anderson Cancer Center in Houston.
Both findings were “very surprising,” said Dr. Rauh-Hain in a video interview. “I was pretty sure we’d see no difference” in outcomes between minimally invasive radical hysterectomies and the same surgery either done by laparoscope or robotically assisted.
Prior prospective comparisons of minimally invasive and open surgical methods for other cancer types, including endometrial, gastric, and ovarian, showed no differences in cancer recurrences and survival, which led to widening use of minimally invasive surgery (MIS) for cervical cancer despite no direct evidence supporting equivalence, Dr. Rauh-Hain noted. “We adopted it with no data. It made sense that cervical cancer would be the same as endometrial cancer,” he explained.
The Laparoscopic Approach to Cervical Cancer (LACC) trial ran at 33 centers in 12 countries, including six U.S. centers. The study randomized women during 2008-2017 who had stage 1A1, 1A2, or 1B1 cervical cancer to either MIS or open surgery for a radical hysterectomy. Each participating center had to submit to a trial review committee full case records for 10 patients and unedited surgical videos of two patients who had previously undergone a minimally invasive radical hysterectomy at the center to document local prowess with MIS.
Dr. Ramirez and his colleagues designed LACC to prove the noninferiority of MIS and calculated an expected enrollment of 740 patients based on statistical expectations, but the study stopped early after enrolling 631 patients because of the adverse outcomes identified in the MIS patients, with a median follow-up of 2.5 years instead of the planned follow-up of 4.5 years. The study reached the 4.5-year follow-up in about 39% of patients. Of the 312 patients randomized to undergo laparotomy, 88% actually underwent the surgery; of the 319 patients randomized to MIS, 91% received this surgery, with 16% of the MIS procedures done using robotic assistance.
The study’s primary endpoint was disease-free survival at 4.5 years, which occurred in 86% of the MIS patients and in 96.5% of the laparotomy patients, a difference that failed to meet the study’s prespecified definition of noninferiority for MIS, reported Dr. Ramirez, a professor of gynecologic oncology and director of Minimally Invasive Surgery Research and Education at the MD Anderson Cancer Center. In addition, several secondary analyses of the data all showed starkly superior outcomes in the laparotomy subgroup.
Disease-free survival among all patients regardless of follow-up duration occurred in 98% of laparotomy patients and 92% of MIS patients, which translated into a 3.74 hazard ratio (P = .002) for disease recurrence or death among the MIS patients when compared with laparotomy patients. The all-cause mortality rates were 1% in the laparotomy patients and 6% among the MIS patients, a hazard ratio of 6.00 (P = .004). The risk of local or regional recurrences was more than fourfold higher in the MIS patients. A blinded, central panel adjudicated all recurrences identified during the study.
The LACC results “should be discussed with patients scheduled to undergo radical hysterectomy” for cervical cancer, Dr. Ramirez concluded.
The observational data from the National Cancer Database used in the analysis led by Dr. Rauh-Hain came from 2,221 patients hospitalized and treated with radical hysterectomy and pelvic lymph node dissection at a U.S. center during 2010-2012 for either stage 1A2 or 1B1 cervical cancer. Among these patients, 47.5% underwent MIS, with 79% of those procedures done with robotic assistance, while the other 52.5% underwent open laparotomy, Dr. Rauh-Hain reported. Additional analysis of data from this database by the researchers showed that, although the first report of MIS for radical hysterectomy appeared in 1992, the approach remained largely unused in U.S. practice until 2007, when use of MIS began to sharply rise. By 2010, about a third of radical hysterectomies for cervical cancer involved MIS, and usage increased still further during 2011 and 2012 to produce a nearly 48% rate during the 3-year study period.
The primary endpoint of Dr. Rauh-Hain’s analysis was overall survival following propensity-score matching of the MIS and laparotomy patients using 13 demographic and clinical criteria. The analysis showed 4-year mortality rates of 5.8% among the laparotomy patients and 8.4% among the MIS patients, which calculated to a relatively increased mortality hazard from MIS of 48% (P = .02).
Dr. Rauh-Hain also reported results from an interrupted time series analysis using data from the Surveillance, Epidemiology, and End Results database of the National Cancer Institute. This analysis compared annual 4-year relative survival rates among women undergoing radical hysterectomy for cervical cancer and found that, after survival rates showed a gradual, steady rise during the years culminating in 2006, once MIS began being more widely used in 2007 survival rates began to drop, with a statistically significant annualized decline of 1% through 2010.
Based on the results from both studies, “at MD Anderson we discuss the results with patients,” with the consequence that the percentage of patients treated with laparotomy is now increasing, Dr. Rauh-Hain said. The results from both studies “are concerning,” he explained.
SOURCE: Ramirez PT and Rauh-Hain JA. SGO 2018, Late-Breaking Abstracts 1 and 2.
The findings from these studies appear valid and should be discussed with patients.
The findings raise a major question: Why has minimally invasive surgery (MIS) led to worse survival rates than laparotomy? Several possible explanations can be hypothesized: The uterine manipulator used in MIS led to local spread of cancer cells; MIS involves a learning curve and initial attempts at MIS did not remove enough of the tumor; and MIS led to increased exposure of the peritoneal cavity to the cancer. The findings also raise another question: Why has MIS for cervical cancer performed less well than MIS for cancers from other organs, such as endometrial and prostate?
The overall survival results from the LACC trial calculate out to 4.75 added deaths per year for every 1,000 patients treated with MIS, compared with laparoscopy. But the National Inpatient Sample data suggest that MIS cuts mortality by about two deaths per year per 1,000 patients, compared with laparotomy, and mortality data from a different analysis (Gynecol Oncol. 2012 Oct;127[1]:11-7) suggest that MIS might prevent six deaths annually for every 1,000 patients, compared with laparotomy. Overall, these three sets of findings suggest roughly comparable mortality outcomes from MIS and laparotomy, but with MIS having the bonus of fewer complications and less need for transfusions.
The cautions and concerns raised by the LACC trial and Dr. Rauh-Hain’s analysis of observational data cannot be easily dismissed. We need to figure out why the results from both studies show worse survival and recurrence rates with MIS, and we need to identify whether subgroups of patients exist who might clearly benefit from either the MIS or open-surgery approach.
Shitanshu Uppal, MD , is a gynecologic oncologist at the University of Michigan in Ann Arbor. He made these comments as designated discussant for the two studies. He had no disclosures.
The findings from these studies appear valid and should be discussed with patients.
The findings raise a major question: Why has minimally invasive surgery (MIS) led to worse survival rates than laparotomy? Several possible explanations can be hypothesized: The uterine manipulator used in MIS led to local spread of cancer cells; MIS involves a learning curve and initial attempts at MIS did not remove enough of the tumor; and MIS led to increased exposure of the peritoneal cavity to the cancer. The findings also raise another question: Why has MIS for cervical cancer performed less well than MIS for cancers from other organs, such as endometrial and prostate?
The overall survival results from the LACC trial calculate out to 4.75 added deaths per year for every 1,000 patients treated with MIS, compared with laparoscopy. But the National Inpatient Sample data suggest that MIS cuts mortality by about two deaths per year per 1,000 patients, compared with laparotomy, and mortality data from a different analysis (Gynecol Oncol. 2012 Oct;127[1]:11-7) suggest that MIS might prevent six deaths annually for every 1,000 patients, compared with laparotomy. Overall, these three sets of findings suggest roughly comparable mortality outcomes from MIS and laparotomy, but with MIS having the bonus of fewer complications and less need for transfusions.
The cautions and concerns raised by the LACC trial and Dr. Rauh-Hain’s analysis of observational data cannot be easily dismissed. We need to figure out why the results from both studies show worse survival and recurrence rates with MIS, and we need to identify whether subgroups of patients exist who might clearly benefit from either the MIS or open-surgery approach.
Shitanshu Uppal, MD , is a gynecologic oncologist at the University of Michigan in Ann Arbor. He made these comments as designated discussant for the two studies. He had no disclosures.
The findings from these studies appear valid and should be discussed with patients.
The findings raise a major question: Why has minimally invasive surgery (MIS) led to worse survival rates than laparotomy? Several possible explanations can be hypothesized: The uterine manipulator used in MIS led to local spread of cancer cells; MIS involves a learning curve and initial attempts at MIS did not remove enough of the tumor; and MIS led to increased exposure of the peritoneal cavity to the cancer. The findings also raise another question: Why has MIS for cervical cancer performed less well than MIS for cancers from other organs, such as endometrial and prostate?
The overall survival results from the LACC trial calculate out to 4.75 added deaths per year for every 1,000 patients treated with MIS, compared with laparoscopy. But the National Inpatient Sample data suggest that MIS cuts mortality by about two deaths per year per 1,000 patients, compared with laparotomy, and mortality data from a different analysis (Gynecol Oncol. 2012 Oct;127[1]:11-7) suggest that MIS might prevent six deaths annually for every 1,000 patients, compared with laparotomy. Overall, these three sets of findings suggest roughly comparable mortality outcomes from MIS and laparotomy, but with MIS having the bonus of fewer complications and less need for transfusions.
The cautions and concerns raised by the LACC trial and Dr. Rauh-Hain’s analysis of observational data cannot be easily dismissed. We need to figure out why the results from both studies show worse survival and recurrence rates with MIS, and we need to identify whether subgroups of patients exist who might clearly benefit from either the MIS or open-surgery approach.
Shitanshu Uppal, MD , is a gynecologic oncologist at the University of Michigan in Ann Arbor. He made these comments as designated discussant for the two studies. He had no disclosures.
NEW ORLEANS – Use of minimally invasive radical hysterectomy to treat early-stage cervical cancer has grown over the past decade, and in current U.S. practice, roughly half of these cases are done with a minimally-invasive approach, with the rest done by conventional laparotomy. But the first data ever reported from a large, prospective trial that compared the efficacy of both methods for cervical cancer had the unexpected finding that disease-free survival following minimally invasive procedures significantly lagged behind radical hysterectomies done by open laparotomy, Pedro T. Ramirez, MD, said at the annual meeting of the Society of Gynecologic Oncology.
Just after this report came results from a second study that used propensity score–adjusted observational data from the National Cancer Database and found significantly worse overall survival following minimally invasive radical hysterectomy for early-stage cervical cancer, compared with laparotomy, said J. Alejandro Rauh-Hain, MD, a gynecologic oncologist at the University of Texas MD Anderson Cancer Center in Houston.
Both findings were “very surprising,” said Dr. Rauh-Hain in a video interview. “I was pretty sure we’d see no difference” in outcomes between minimally invasive radical hysterectomies and the same surgery either done by laparoscope or robotically assisted.
Prior prospective comparisons of minimally invasive and open surgical methods for other cancer types, including endometrial, gastric, and ovarian, showed no differences in cancer recurrences and survival, which led to widening use of minimally invasive surgery (MIS) for cervical cancer despite no direct evidence supporting equivalence, Dr. Rauh-Hain noted. “We adopted it with no data. It made sense that cervical cancer would be the same as endometrial cancer,” he explained.
The Laparoscopic Approach to Cervical Cancer (LACC) trial ran at 33 centers in 12 countries, including six U.S. centers. The study randomized women during 2008-2017 who had stage 1A1, 1A2, or 1B1 cervical cancer to either MIS or open surgery for a radical hysterectomy. Each participating center had to submit to a trial review committee full case records for 10 patients and unedited surgical videos of two patients who had previously undergone a minimally invasive radical hysterectomy at the center to document local prowess with MIS.
Dr. Ramirez and his colleagues designed LACC to prove the noninferiority of MIS and calculated an expected enrollment of 740 patients based on statistical expectations, but the study stopped early after enrolling 631 patients because of the adverse outcomes identified in the MIS patients, with a median follow-up of 2.5 years instead of the planned follow-up of 4.5 years. The study reached the 4.5-year follow-up in about 39% of patients. Of the 312 patients randomized to undergo laparotomy, 88% actually underwent the surgery; of the 319 patients randomized to MIS, 91% received this surgery, with 16% of the MIS procedures done using robotic assistance.
The study’s primary endpoint was disease-free survival at 4.5 years, which occurred in 86% of the MIS patients and in 96.5% of the laparotomy patients, a difference that failed to meet the study’s prespecified definition of noninferiority for MIS, reported Dr. Ramirez, a professor of gynecologic oncology and director of Minimally Invasive Surgery Research and Education at the MD Anderson Cancer Center. In addition, several secondary analyses of the data all showed starkly superior outcomes in the laparotomy subgroup.
Disease-free survival among all patients regardless of follow-up duration occurred in 98% of laparotomy patients and 92% of MIS patients, which translated into a 3.74 hazard ratio (P = .002) for disease recurrence or death among the MIS patients when compared with laparotomy patients. The all-cause mortality rates were 1% in the laparotomy patients and 6% among the MIS patients, a hazard ratio of 6.00 (P = .004). The risk of local or regional recurrences was more than fourfold higher in the MIS patients. A blinded, central panel adjudicated all recurrences identified during the study.
The LACC results “should be discussed with patients scheduled to undergo radical hysterectomy” for cervical cancer, Dr. Ramirez concluded.
The observational data from the National Cancer Database used in the analysis led by Dr. Rauh-Hain came from 2,221 patients hospitalized and treated with radical hysterectomy and pelvic lymph node dissection at a U.S. center during 2010-2012 for either stage 1A2 or 1B1 cervical cancer. Among these patients, 47.5% underwent MIS, with 79% of those procedures done with robotic assistance, while the other 52.5% underwent open laparotomy, Dr. Rauh-Hain reported. Additional analysis of data from this database by the researchers showed that, although the first report of MIS for radical hysterectomy appeared in 1992, the approach remained largely unused in U.S. practice until 2007, when use of MIS began to sharply rise. By 2010, about a third of radical hysterectomies for cervical cancer involved MIS, and usage increased still further during 2011 and 2012 to produce a nearly 48% rate during the 3-year study period.
The primary endpoint of Dr. Rauh-Hain’s analysis was overall survival following propensity-score matching of the MIS and laparotomy patients using 13 demographic and clinical criteria. The analysis showed 4-year mortality rates of 5.8% among the laparotomy patients and 8.4% among the MIS patients, which calculated to a relatively increased mortality hazard from MIS of 48% (P = .02).
Dr. Rauh-Hain also reported results from an interrupted time series analysis using data from the Surveillance, Epidemiology, and End Results database of the National Cancer Institute. This analysis compared annual 4-year relative survival rates among women undergoing radical hysterectomy for cervical cancer and found that, after survival rates showed a gradual, steady rise during the years culminating in 2006, once MIS began being more widely used in 2007 survival rates began to drop, with a statistically significant annualized decline of 1% through 2010.
Based on the results from both studies, “at MD Anderson we discuss the results with patients,” with the consequence that the percentage of patients treated with laparotomy is now increasing, Dr. Rauh-Hain said. The results from both studies “are concerning,” he explained.
SOURCE: Ramirez PT and Rauh-Hain JA. SGO 2018, Late-Breaking Abstracts 1 and 2.
NEW ORLEANS – Use of minimally invasive radical hysterectomy to treat early-stage cervical cancer has grown over the past decade, and in current U.S. practice, roughly half of these cases are done with a minimally-invasive approach, with the rest done by conventional laparotomy. But the first data ever reported from a large, prospective trial that compared the efficacy of both methods for cervical cancer had the unexpected finding that disease-free survival following minimally invasive procedures significantly lagged behind radical hysterectomies done by open laparotomy, Pedro T. Ramirez, MD, said at the annual meeting of the Society of Gynecologic Oncology.
Just after this report came results from a second study that used propensity score–adjusted observational data from the National Cancer Database and found significantly worse overall survival following minimally invasive radical hysterectomy for early-stage cervical cancer, compared with laparotomy, said J. Alejandro Rauh-Hain, MD, a gynecologic oncologist at the University of Texas MD Anderson Cancer Center in Houston.
Both findings were “very surprising,” said Dr. Rauh-Hain in a video interview. “I was pretty sure we’d see no difference” in outcomes between minimally invasive radical hysterectomies and the same surgery either done by laparoscope or robotically assisted.
Prior prospective comparisons of minimally invasive and open surgical methods for other cancer types, including endometrial, gastric, and ovarian, showed no differences in cancer recurrences and survival, which led to widening use of minimally invasive surgery (MIS) for cervical cancer despite no direct evidence supporting equivalence, Dr. Rauh-Hain noted. “We adopted it with no data. It made sense that cervical cancer would be the same as endometrial cancer,” he explained.
The Laparoscopic Approach to Cervical Cancer (LACC) trial ran at 33 centers in 12 countries, including six U.S. centers. The study randomized women during 2008-2017 who had stage 1A1, 1A2, or 1B1 cervical cancer to either MIS or open surgery for a radical hysterectomy. Each participating center had to submit to a trial review committee full case records for 10 patients and unedited surgical videos of two patients who had previously undergone a minimally invasive radical hysterectomy at the center to document local prowess with MIS.
Dr. Ramirez and his colleagues designed LACC to prove the noninferiority of MIS and calculated an expected enrollment of 740 patients based on statistical expectations, but the study stopped early after enrolling 631 patients because of the adverse outcomes identified in the MIS patients, with a median follow-up of 2.5 years instead of the planned follow-up of 4.5 years. The study reached the 4.5-year follow-up in about 39% of patients. Of the 312 patients randomized to undergo laparotomy, 88% actually underwent the surgery; of the 319 patients randomized to MIS, 91% received this surgery, with 16% of the MIS procedures done using robotic assistance.
The study’s primary endpoint was disease-free survival at 4.5 years, which occurred in 86% of the MIS patients and in 96.5% of the laparotomy patients, a difference that failed to meet the study’s prespecified definition of noninferiority for MIS, reported Dr. Ramirez, a professor of gynecologic oncology and director of Minimally Invasive Surgery Research and Education at the MD Anderson Cancer Center. In addition, several secondary analyses of the data all showed starkly superior outcomes in the laparotomy subgroup.
Disease-free survival among all patients regardless of follow-up duration occurred in 98% of laparotomy patients and 92% of MIS patients, which translated into a 3.74 hazard ratio (P = .002) for disease recurrence or death among the MIS patients when compared with laparotomy patients. The all-cause mortality rates were 1% in the laparotomy patients and 6% among the MIS patients, a hazard ratio of 6.00 (P = .004). The risk of local or regional recurrences was more than fourfold higher in the MIS patients. A blinded, central panel adjudicated all recurrences identified during the study.
The LACC results “should be discussed with patients scheduled to undergo radical hysterectomy” for cervical cancer, Dr. Ramirez concluded.
The observational data from the National Cancer Database used in the analysis led by Dr. Rauh-Hain came from 2,221 patients hospitalized and treated with radical hysterectomy and pelvic lymph node dissection at a U.S. center during 2010-2012 for either stage 1A2 or 1B1 cervical cancer. Among these patients, 47.5% underwent MIS, with 79% of those procedures done with robotic assistance, while the other 52.5% underwent open laparotomy, Dr. Rauh-Hain reported. Additional analysis of data from this database by the researchers showed that, although the first report of MIS for radical hysterectomy appeared in 1992, the approach remained largely unused in U.S. practice until 2007, when use of MIS began to sharply rise. By 2010, about a third of radical hysterectomies for cervical cancer involved MIS, and usage increased still further during 2011 and 2012 to produce a nearly 48% rate during the 3-year study period.
The primary endpoint of Dr. Rauh-Hain’s analysis was overall survival following propensity-score matching of the MIS and laparotomy patients using 13 demographic and clinical criteria. The analysis showed 4-year mortality rates of 5.8% among the laparotomy patients and 8.4% among the MIS patients, which calculated to a relatively increased mortality hazard from MIS of 48% (P = .02).
Dr. Rauh-Hain also reported results from an interrupted time series analysis using data from the Surveillance, Epidemiology, and End Results database of the National Cancer Institute. This analysis compared annual 4-year relative survival rates among women undergoing radical hysterectomy for cervical cancer and found that, after survival rates showed a gradual, steady rise during the years culminating in 2006, once MIS began being more widely used in 2007 survival rates began to drop, with a statistically significant annualized decline of 1% through 2010.
Based on the results from both studies, “at MD Anderson we discuss the results with patients,” with the consequence that the percentage of patients treated with laparotomy is now increasing, Dr. Rauh-Hain said. The results from both studies “are concerning,” he explained.
SOURCE: Ramirez PT and Rauh-Hain JA. SGO 2018, Late-Breaking Abstracts 1 and 2.
REPORTING FROM SGO 2018
Key clinical point: Laparotomy produced better survival than did minimally invasive surgery for cervical cancer.
Major finding: Disease-free survival after 4.5 years was 96.5% with laparotomy and 86.0% with minimally invasive surgery.
Study details: LACC was a multicenter, randomized trial with 631 patients. The observational study included 2,221 patients from the National Cancer Database during 2010-2012.
Disclosures: Dr. Ramirez and Dr. Rauh-Hain had no disclosures.
Source: Ramirez PT and Rauh-Hain JA. SGO 2018, Late-Breaking Abstracts 1 and 2.
Health IT ‘under-users’ outnumber ‘super-users’
Almost 27% of medical practices are “super-users” of health information technology, but another 39% are “under-users” that may be affecting “the ability of the health system as a whole to provide coordinated and efficient care,” investigators said in the American Journal of Managed Care.
To put it another way, wrote Juliet Rumball-Smith, MBChB, PhD, and her associates, who analyzed data for 30,123 practices from the 2014 Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice survey.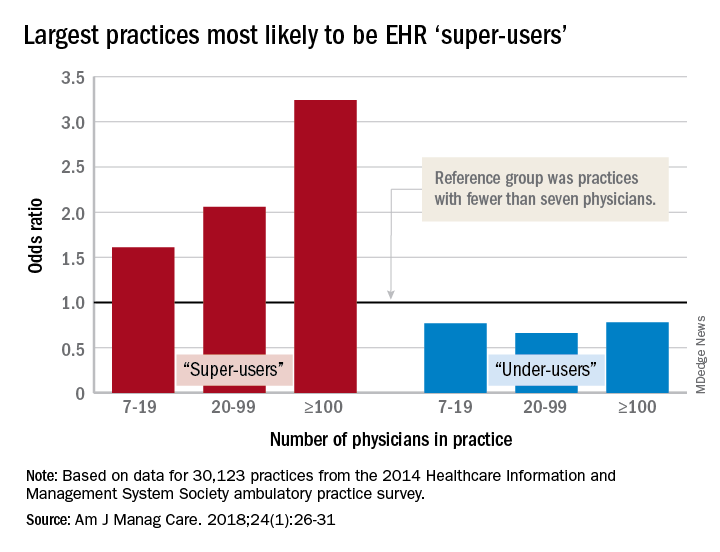
After all the scores were calculated, 8,003 practices (27%) were classified as super-users and 11,706 (39%) as under-users. More specific analysis showed that the smallest practices were least likely to be super-users, and that the likelihood rose with increasing practice size. With practices of fewer than seven physicians as the reference group, odds ratios of being a super-user were 1.61 for practices of 7-19 physicians, 2.06 for those with 20-99 physicians, and 3.24 for those of 100 or more associated physicians, reported Dr. Rumball-Smith and her associates at Rand Health in Santa Monica, Calif.
The situation was not as clear-cut among the technology avoiders, as the odds ratios made practices of 20-99 physicians less likely (0.66) than those of 7-19 (0.77) and 100 or more (0.78) physicians to be under-users, they said.
The super-users also were more likely to located in metropolitan areas (OR, 2.45, compared with rural practices) and in the Midwest (OR, 2.05, compared with the Northeast) or the South (OR, 1.32) and to be primary care/family medicine clinics, which were the reference group for the practice-type comparison (OR, 0.89, for single- or multiple-specialty; 0.64, for specialist services or urgent care), the investigators said.
“It is important that policy makers and health care providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners,” they wrote.
The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
SOURCE: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
Almost 27% of medical practices are “super-users” of health information technology, but another 39% are “under-users” that may be affecting “the ability of the health system as a whole to provide coordinated and efficient care,” investigators said in the American Journal of Managed Care.
To put it another way, wrote Juliet Rumball-Smith, MBChB, PhD, and her associates, who analyzed data for 30,123 practices from the 2014 Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice survey.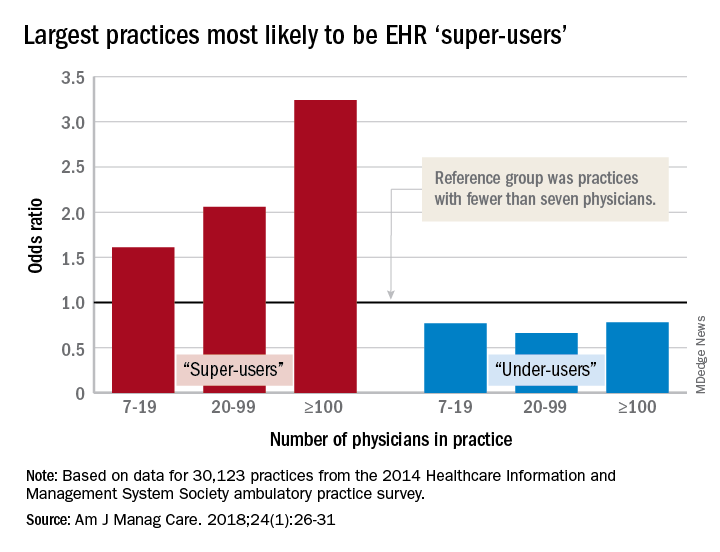
After all the scores were calculated, 8,003 practices (27%) were classified as super-users and 11,706 (39%) as under-users. More specific analysis showed that the smallest practices were least likely to be super-users, and that the likelihood rose with increasing practice size. With practices of fewer than seven physicians as the reference group, odds ratios of being a super-user were 1.61 for practices of 7-19 physicians, 2.06 for those with 20-99 physicians, and 3.24 for those of 100 or more associated physicians, reported Dr. Rumball-Smith and her associates at Rand Health in Santa Monica, Calif.
The situation was not as clear-cut among the technology avoiders, as the odds ratios made practices of 20-99 physicians less likely (0.66) than those of 7-19 (0.77) and 100 or more (0.78) physicians to be under-users, they said.
The super-users also were more likely to located in metropolitan areas (OR, 2.45, compared with rural practices) and in the Midwest (OR, 2.05, compared with the Northeast) or the South (OR, 1.32) and to be primary care/family medicine clinics, which were the reference group for the practice-type comparison (OR, 0.89, for single- or multiple-specialty; 0.64, for specialist services or urgent care), the investigators said.
“It is important that policy makers and health care providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners,” they wrote.
The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
SOURCE: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
Almost 27% of medical practices are “super-users” of health information technology, but another 39% are “under-users” that may be affecting “the ability of the health system as a whole to provide coordinated and efficient care,” investigators said in the American Journal of Managed Care.
To put it another way, wrote Juliet Rumball-Smith, MBChB, PhD, and her associates, who analyzed data for 30,123 practices from the 2014 Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice survey.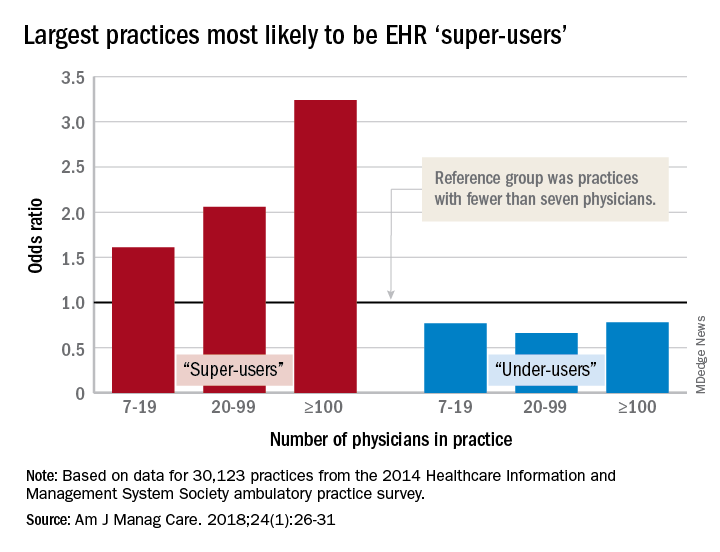
After all the scores were calculated, 8,003 practices (27%) were classified as super-users and 11,706 (39%) as under-users. More specific analysis showed that the smallest practices were least likely to be super-users, and that the likelihood rose with increasing practice size. With practices of fewer than seven physicians as the reference group, odds ratios of being a super-user were 1.61 for practices of 7-19 physicians, 2.06 for those with 20-99 physicians, and 3.24 for those of 100 or more associated physicians, reported Dr. Rumball-Smith and her associates at Rand Health in Santa Monica, Calif.
The situation was not as clear-cut among the technology avoiders, as the odds ratios made practices of 20-99 physicians less likely (0.66) than those of 7-19 (0.77) and 100 or more (0.78) physicians to be under-users, they said.
The super-users also were more likely to located in metropolitan areas (OR, 2.45, compared with rural practices) and in the Midwest (OR, 2.05, compared with the Northeast) or the South (OR, 1.32) and to be primary care/family medicine clinics, which were the reference group for the practice-type comparison (OR, 0.89, for single- or multiple-specialty; 0.64, for specialist services or urgent care), the investigators said.
“It is important that policy makers and health care providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners,” they wrote.
The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
SOURCE: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
FROM AMERICAN JOURNAL OF MANAGED CARE
Key clinical point: Many medical practices are not prepared to take advantage of EHR-based initiatives.
Major finding: 73% of ambulatory practices are not using EHRs “to their full benefit.”
Study details: HIMSS Analytics 2014 ambulatory practice survey for 30,123 practices.
Disclosures: The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
Source: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
Open enrollment 2018: Plan selections down slightly
the Centers for Medicare & Medicaid Services reported.
That’s a drop of 3.3%, compared with the 12.2 million enrollees for 2017, and a drop of 7.1% from the peak year of 2016, according to the 2018 open enrollment final report.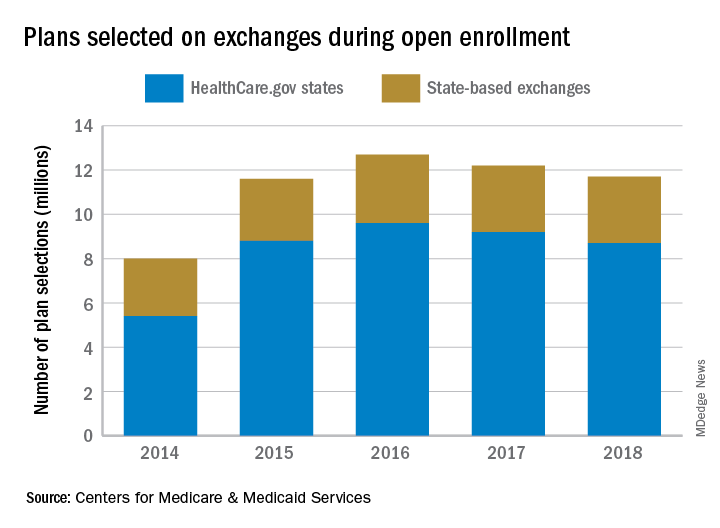
For 2018, the average premium before application of the premium tax credit was $621 in the HealthCare.gov states, which is an increase of 30% from the $476 average for 2017. After the tax credit, the average premium for 2018 was $153.
“Our primary goal this year was to ensure that Americans who wanted coverage through the exchange had a seamless experience,” CMS Administrator Seema Verma said in a statement. “We are pleased that consumer satisfaction was the highest it’s ever been during the 2018 open enrollment period.”
the Centers for Medicare & Medicaid Services reported.
That’s a drop of 3.3%, compared with the 12.2 million enrollees for 2017, and a drop of 7.1% from the peak year of 2016, according to the 2018 open enrollment final report.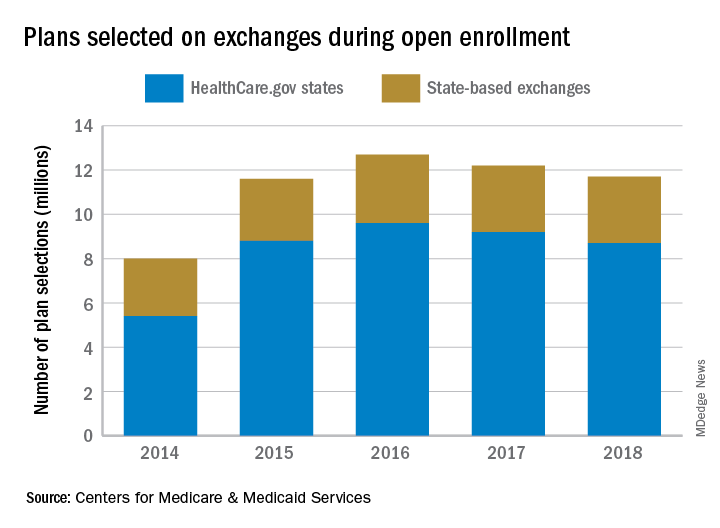
For 2018, the average premium before application of the premium tax credit was $621 in the HealthCare.gov states, which is an increase of 30% from the $476 average for 2017. After the tax credit, the average premium for 2018 was $153.
“Our primary goal this year was to ensure that Americans who wanted coverage through the exchange had a seamless experience,” CMS Administrator Seema Verma said in a statement. “We are pleased that consumer satisfaction was the highest it’s ever been during the 2018 open enrollment period.”
the Centers for Medicare & Medicaid Services reported.
That’s a drop of 3.3%, compared with the 12.2 million enrollees for 2017, and a drop of 7.1% from the peak year of 2016, according to the 2018 open enrollment final report.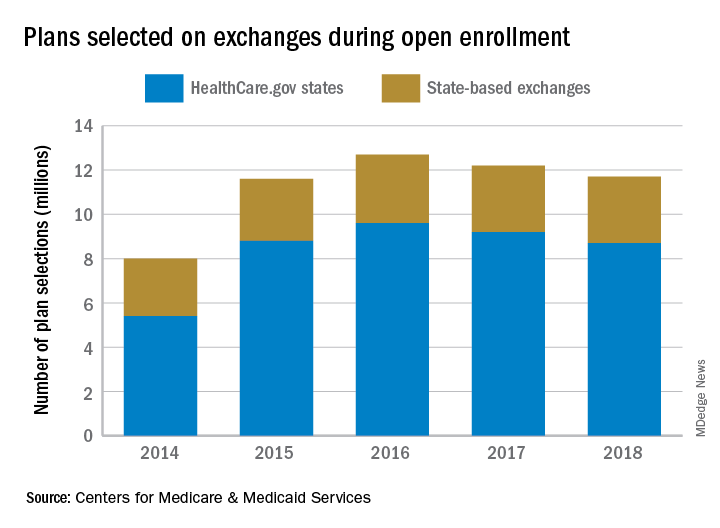
For 2018, the average premium before application of the premium tax credit was $621 in the HealthCare.gov states, which is an increase of 30% from the $476 average for 2017. After the tax credit, the average premium for 2018 was $153.
“Our primary goal this year was to ensure that Americans who wanted coverage through the exchange had a seamless experience,” CMS Administrator Seema Verma said in a statement. “We are pleased that consumer satisfaction was the highest it’s ever been during the 2018 open enrollment period.”
Fast-track catheter management offers little benefit after benign hysterectomy
ORLANDO – A fast-track approach to urinary catheter management after benign gynecologic surgery reduced catheter dwell time, but did not significantly improve outcomes or patient satisfaction in a prospective, randomized trial.
Catheter dwell times in 200 women randomized 1:1 to receive either fast-track catheter management with planned catheter removal at 4 hours after surgery, or conventional catheter management with planned catheter removal 1 day after surgery, were 650 minutes versus 1,196 minutes in the groups, respectively, Patrick Lang, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Overall, 93% of patients had a successful voiding trial for catheter removal, but failures occurred more often in the fast-track management group than in the conventional management group (12% vs. 2%), said Dr. Lang, a fellow at the Christ Hospital Health Network, Cincinnati.
Furthermore, the reduction in Urogenital Distress Inventory short form scores after surgery was significant overall but did not differ significantly in the fast-track and conventional management groups, and there was a trend toward less of a reduction in Urogenital Distress Inventory scores among those who failed the voiding trial versus those who passed, he noted.
Follow-up patient surveys at 2-3 weeks after surgery showed no significant difference between the groups in the rates of reported urinary tract infections (13% and 19% with fast-track and conventional management, respectively) and antibiotic exposure, or in lower urinary tract symptoms (P = .24 and .92), he said.
Patients also had a positive overall impression of their catheter management, with no significant difference between the groups in the percentage of patients who strongly agreed that their catheter was well managed (80% and 87%, respectively).
In women undergoing gynecologic surgery, indwelling urinary catheters often are used for an extended period as postoperative voiding dysfunction is presumed, Dr. Lang noted.
For the current single-center study, women undergoing any benign gynecologic surgery with an anticipated hospital stay of at least 1 night were enrolled and randomized to fast-track or conventional catheter management. All underwent hysterectomy, and the approaches, including robotic in 42%, traditional laparoscopic in 33%, vaginal in 14.3%, and abdominal in 10.3%, did not differ among the groups. Neither the rates of voiding trial success nor catheter dwell time differed, based on hysterectomy approach, he said.
“Catheter dwell time is reduced with a fast-track approach, but dwell time does not appear to influence patient satisfaction or urinary tract symptomatology, urinary tract infection, or antibiotic exposure in the 2-3 weeks following benign gynecologic surgery,” he concluded.
Dr. Lang reported having no disclosures.
SOURCE: Lang P et al. SGS 2018, Oral Poster 20.
ORLANDO – A fast-track approach to urinary catheter management after benign gynecologic surgery reduced catheter dwell time, but did not significantly improve outcomes or patient satisfaction in a prospective, randomized trial.
Catheter dwell times in 200 women randomized 1:1 to receive either fast-track catheter management with planned catheter removal at 4 hours after surgery, or conventional catheter management with planned catheter removal 1 day after surgery, were 650 minutes versus 1,196 minutes in the groups, respectively, Patrick Lang, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Overall, 93% of patients had a successful voiding trial for catheter removal, but failures occurred more often in the fast-track management group than in the conventional management group (12% vs. 2%), said Dr. Lang, a fellow at the Christ Hospital Health Network, Cincinnati.
Furthermore, the reduction in Urogenital Distress Inventory short form scores after surgery was significant overall but did not differ significantly in the fast-track and conventional management groups, and there was a trend toward less of a reduction in Urogenital Distress Inventory scores among those who failed the voiding trial versus those who passed, he noted.
Follow-up patient surveys at 2-3 weeks after surgery showed no significant difference between the groups in the rates of reported urinary tract infections (13% and 19% with fast-track and conventional management, respectively) and antibiotic exposure, or in lower urinary tract symptoms (P = .24 and .92), he said.
Patients also had a positive overall impression of their catheter management, with no significant difference between the groups in the percentage of patients who strongly agreed that their catheter was well managed (80% and 87%, respectively).
In women undergoing gynecologic surgery, indwelling urinary catheters often are used for an extended period as postoperative voiding dysfunction is presumed, Dr. Lang noted.
For the current single-center study, women undergoing any benign gynecologic surgery with an anticipated hospital stay of at least 1 night were enrolled and randomized to fast-track or conventional catheter management. All underwent hysterectomy, and the approaches, including robotic in 42%, traditional laparoscopic in 33%, vaginal in 14.3%, and abdominal in 10.3%, did not differ among the groups. Neither the rates of voiding trial success nor catheter dwell time differed, based on hysterectomy approach, he said.
“Catheter dwell time is reduced with a fast-track approach, but dwell time does not appear to influence patient satisfaction or urinary tract symptomatology, urinary tract infection, or antibiotic exposure in the 2-3 weeks following benign gynecologic surgery,” he concluded.
Dr. Lang reported having no disclosures.
SOURCE: Lang P et al. SGS 2018, Oral Poster 20.
ORLANDO – A fast-track approach to urinary catheter management after benign gynecologic surgery reduced catheter dwell time, but did not significantly improve outcomes or patient satisfaction in a prospective, randomized trial.
Catheter dwell times in 200 women randomized 1:1 to receive either fast-track catheter management with planned catheter removal at 4 hours after surgery, or conventional catheter management with planned catheter removal 1 day after surgery, were 650 minutes versus 1,196 minutes in the groups, respectively, Patrick Lang, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Overall, 93% of patients had a successful voiding trial for catheter removal, but failures occurred more often in the fast-track management group than in the conventional management group (12% vs. 2%), said Dr. Lang, a fellow at the Christ Hospital Health Network, Cincinnati.
Furthermore, the reduction in Urogenital Distress Inventory short form scores after surgery was significant overall but did not differ significantly in the fast-track and conventional management groups, and there was a trend toward less of a reduction in Urogenital Distress Inventory scores among those who failed the voiding trial versus those who passed, he noted.
Follow-up patient surveys at 2-3 weeks after surgery showed no significant difference between the groups in the rates of reported urinary tract infections (13% and 19% with fast-track and conventional management, respectively) and antibiotic exposure, or in lower urinary tract symptoms (P = .24 and .92), he said.
Patients also had a positive overall impression of their catheter management, with no significant difference between the groups in the percentage of patients who strongly agreed that their catheter was well managed (80% and 87%, respectively).
In women undergoing gynecologic surgery, indwelling urinary catheters often are used for an extended period as postoperative voiding dysfunction is presumed, Dr. Lang noted.
For the current single-center study, women undergoing any benign gynecologic surgery with an anticipated hospital stay of at least 1 night were enrolled and randomized to fast-track or conventional catheter management. All underwent hysterectomy, and the approaches, including robotic in 42%, traditional laparoscopic in 33%, vaginal in 14.3%, and abdominal in 10.3%, did not differ among the groups. Neither the rates of voiding trial success nor catheter dwell time differed, based on hysterectomy approach, he said.
“Catheter dwell time is reduced with a fast-track approach, but dwell time does not appear to influence patient satisfaction or urinary tract symptomatology, urinary tract infection, or antibiotic exposure in the 2-3 weeks following benign gynecologic surgery,” he concluded.
Dr. Lang reported having no disclosures.
SOURCE: Lang P et al. SGS 2018, Oral Poster 20.
REPORTING FROM SGS 2018
Key clinical point: Fast-track catheter management after surgery improves dwell time, but not other outcomes.
Major finding: Catheter dwell times were 650 versus 1,196 minutes with fast-track and conventional management, respectively.
Study details: A prospective, randomized study of 200 women.
Disclosures: Dr. Lang reported having no disclosures.
Source: Lang P et al. SGS 2018, Oral Poster 20.
Study: No increased risk of serious AEs with combined urogyn/gyn onc surgery
ORLANDO – Intraoperative and serious postoperative adverse events do not occur more frequently with concurrent urogynecologic and gynecologic oncology procedures versus the latter alone, but minor adverse events are more common, according to findings from a retrospective matched cohort study.
The study also showed that 10% of planned urogynecologic procedures are modified or abandoned at the time of gynecologic oncology surgery, Emily R. Davidson, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“Concurrent cases were longer by 76 minutes, which is not surprising given that additional procedures were performed, and on univariate analysis there were differences in the frequency of multiple postoperative adverse events between the cohorts, including estimated blood loss, discharge with a Foley catheter, perioperative transfusion, postoperative pulmonary complications, ileus, renal failure, and urinary tract infection,” she said.
However, on multivariate analysis controlling for preoperative cardiovascular and pulmonary comorbidities, only urinary tract infection and discharge with a Foley catheter related to postoperative voiding dysfunction, which were significantly more common in the combined surgery group (26% vs. 7% and 35% vs. 1%, respectively), remained significantly different between the groups, she noted.
No differences were seen between the groups in length of hospital stay, reoperation, readmission within 1 month, surgical site infection, or death within 1 year of surgery, but patients undergoing concurrent procedures had more Clavien-Dindo grade 2 complications (44% vs. 19%), and this was primarily related to the prescription of antibiotics for urinary tract infections, she said.
As for the 11 cases (10%) with planned urogynecologic surgeries that were significantly changed or aborted at the time of gynecologic oncology surgery, 5 were because of intraoperative complications, 3 because of technical limitations, and 3 because of a change in oncologic care plan, including the need for postoperative radiation, she noted.
Case patients were women who underwent planned concurrent procedures at a large tertiary care center from January 2004 to June 2017. Of these women, 77% had stress urinary incontinence, 74% had pelvic organ prolapse (with 55% having stage 3 or 4 prolapse), 71% had prolapse repair – most commonly a native-tissue transvaginal colpopexy – as part of their procedure, and 74% had an anti-incontinence procedure – most commonly a transobturator sling.
The most common final histologic diagnosis was benign disease (in 51% of patients), and uterine cancer was the most common malignancy encountered (36% of patients), Dr. Davidson said, noting that other diagnoses included ovarian and vulvar cancer, in 12% and 1% of cases, respectively.
Most surgeries were minimally invasive abdominal hysterectomies (56%), followed by laparotomies in 32%, minor vaginal surgeries in 6%, laparoscopy without hysterectomy in 5%, and vaginal hysterectomy in 1%.
Controls were matched 2:1 based on surgeon, surgery date and invasiveness (surgical route), and final pathological diagnosis.
The median age of all patients was 59 years. Case patients undergoing concurrent procedures were more likely to be older (median of 64 vs. 57 years) and postmenopausal.
“Other statistically significant differences were that women undergoing combined surgery had higher vaginal parity, and were more likely to have undergone preoperative chemotherapy. They were also more likely to have a prior diagnosis of cardiovascular or pulmonary disease,” Dr. Davidson said.
“Women undergoing treatment for suspected gynecologic malignancy have the same or higher prevalence of pelvic floor disorders, compared with the general population, and they may choose to have combined surgery if both subspecialists are available,” she continued. “However, there are limited data regarding the incidence of adverse events in these concurrent procedures, or how often the planned urogynecology portion of the procedure is modified intraoperatively.”
Though limited by factors inherent in retrospective chart review, such as information bias at the time of data collection (which was mitigated by cross-checking data and having only two data collectors), the findings of the current study suggest that “concurrent urogynecologic and gynecologic oncology surgery should be offered to appropriate patients, as adding urogynecology surgery does not increase the risk of serious adverse events,” she concluded, adding that the study “highlights the importance of preoperative counseling, including discussion of the increased risk of minor postoperative adverse events, such as postoperative voiding symptoms and urinary tract infection, as well as discussion of the 10% risk of a change in intraoperative plan in the urogynecologic procedure.”
“This study certainly helps us know that we’re doing no harm [in offering concurrent surgery],” he said.
Dr. Davidson and Dr. Noone each reported having no relevant disclosures.
SOURCE: Davidson ER et al. SGS 2018, Oral Presentation 13.
ORLANDO – Intraoperative and serious postoperative adverse events do not occur more frequently with concurrent urogynecologic and gynecologic oncology procedures versus the latter alone, but minor adverse events are more common, according to findings from a retrospective matched cohort study.
The study also showed that 10% of planned urogynecologic procedures are modified or abandoned at the time of gynecologic oncology surgery, Emily R. Davidson, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“Concurrent cases were longer by 76 minutes, which is not surprising given that additional procedures were performed, and on univariate analysis there were differences in the frequency of multiple postoperative adverse events between the cohorts, including estimated blood loss, discharge with a Foley catheter, perioperative transfusion, postoperative pulmonary complications, ileus, renal failure, and urinary tract infection,” she said.
However, on multivariate analysis controlling for preoperative cardiovascular and pulmonary comorbidities, only urinary tract infection and discharge with a Foley catheter related to postoperative voiding dysfunction, which were significantly more common in the combined surgery group (26% vs. 7% and 35% vs. 1%, respectively), remained significantly different between the groups, she noted.
No differences were seen between the groups in length of hospital stay, reoperation, readmission within 1 month, surgical site infection, or death within 1 year of surgery, but patients undergoing concurrent procedures had more Clavien-Dindo grade 2 complications (44% vs. 19%), and this was primarily related to the prescription of antibiotics for urinary tract infections, she said.
As for the 11 cases (10%) with planned urogynecologic surgeries that were significantly changed or aborted at the time of gynecologic oncology surgery, 5 were because of intraoperative complications, 3 because of technical limitations, and 3 because of a change in oncologic care plan, including the need for postoperative radiation, she noted.
Case patients were women who underwent planned concurrent procedures at a large tertiary care center from January 2004 to June 2017. Of these women, 77% had stress urinary incontinence, 74% had pelvic organ prolapse (with 55% having stage 3 or 4 prolapse), 71% had prolapse repair – most commonly a native-tissue transvaginal colpopexy – as part of their procedure, and 74% had an anti-incontinence procedure – most commonly a transobturator sling.
The most common final histologic diagnosis was benign disease (in 51% of patients), and uterine cancer was the most common malignancy encountered (36% of patients), Dr. Davidson said, noting that other diagnoses included ovarian and vulvar cancer, in 12% and 1% of cases, respectively.
Most surgeries were minimally invasive abdominal hysterectomies (56%), followed by laparotomies in 32%, minor vaginal surgeries in 6%, laparoscopy without hysterectomy in 5%, and vaginal hysterectomy in 1%.
Controls were matched 2:1 based on surgeon, surgery date and invasiveness (surgical route), and final pathological diagnosis.
The median age of all patients was 59 years. Case patients undergoing concurrent procedures were more likely to be older (median of 64 vs. 57 years) and postmenopausal.
“Other statistically significant differences were that women undergoing combined surgery had higher vaginal parity, and were more likely to have undergone preoperative chemotherapy. They were also more likely to have a prior diagnosis of cardiovascular or pulmonary disease,” Dr. Davidson said.
“Women undergoing treatment for suspected gynecologic malignancy have the same or higher prevalence of pelvic floor disorders, compared with the general population, and they may choose to have combined surgery if both subspecialists are available,” she continued. “However, there are limited data regarding the incidence of adverse events in these concurrent procedures, or how often the planned urogynecology portion of the procedure is modified intraoperatively.”
Though limited by factors inherent in retrospective chart review, such as information bias at the time of data collection (which was mitigated by cross-checking data and having only two data collectors), the findings of the current study suggest that “concurrent urogynecologic and gynecologic oncology surgery should be offered to appropriate patients, as adding urogynecology surgery does not increase the risk of serious adverse events,” she concluded, adding that the study “highlights the importance of preoperative counseling, including discussion of the increased risk of minor postoperative adverse events, such as postoperative voiding symptoms and urinary tract infection, as well as discussion of the 10% risk of a change in intraoperative plan in the urogynecologic procedure.”
“This study certainly helps us know that we’re doing no harm [in offering concurrent surgery],” he said.
Dr. Davidson and Dr. Noone each reported having no relevant disclosures.
SOURCE: Davidson ER et al. SGS 2018, Oral Presentation 13.
ORLANDO – Intraoperative and serious postoperative adverse events do not occur more frequently with concurrent urogynecologic and gynecologic oncology procedures versus the latter alone, but minor adverse events are more common, according to findings from a retrospective matched cohort study.
The study also showed that 10% of planned urogynecologic procedures are modified or abandoned at the time of gynecologic oncology surgery, Emily R. Davidson, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“Concurrent cases were longer by 76 minutes, which is not surprising given that additional procedures were performed, and on univariate analysis there were differences in the frequency of multiple postoperative adverse events between the cohorts, including estimated blood loss, discharge with a Foley catheter, perioperative transfusion, postoperative pulmonary complications, ileus, renal failure, and urinary tract infection,” she said.
However, on multivariate analysis controlling for preoperative cardiovascular and pulmonary comorbidities, only urinary tract infection and discharge with a Foley catheter related to postoperative voiding dysfunction, which were significantly more common in the combined surgery group (26% vs. 7% and 35% vs. 1%, respectively), remained significantly different between the groups, she noted.
No differences were seen between the groups in length of hospital stay, reoperation, readmission within 1 month, surgical site infection, or death within 1 year of surgery, but patients undergoing concurrent procedures had more Clavien-Dindo grade 2 complications (44% vs. 19%), and this was primarily related to the prescription of antibiotics for urinary tract infections, she said.
As for the 11 cases (10%) with planned urogynecologic surgeries that were significantly changed or aborted at the time of gynecologic oncology surgery, 5 were because of intraoperative complications, 3 because of technical limitations, and 3 because of a change in oncologic care plan, including the need for postoperative radiation, she noted.
Case patients were women who underwent planned concurrent procedures at a large tertiary care center from January 2004 to June 2017. Of these women, 77% had stress urinary incontinence, 74% had pelvic organ prolapse (with 55% having stage 3 or 4 prolapse), 71% had prolapse repair – most commonly a native-tissue transvaginal colpopexy – as part of their procedure, and 74% had an anti-incontinence procedure – most commonly a transobturator sling.
The most common final histologic diagnosis was benign disease (in 51% of patients), and uterine cancer was the most common malignancy encountered (36% of patients), Dr. Davidson said, noting that other diagnoses included ovarian and vulvar cancer, in 12% and 1% of cases, respectively.
Most surgeries were minimally invasive abdominal hysterectomies (56%), followed by laparotomies in 32%, minor vaginal surgeries in 6%, laparoscopy without hysterectomy in 5%, and vaginal hysterectomy in 1%.
Controls were matched 2:1 based on surgeon, surgery date and invasiveness (surgical route), and final pathological diagnosis.
The median age of all patients was 59 years. Case patients undergoing concurrent procedures were more likely to be older (median of 64 vs. 57 years) and postmenopausal.
“Other statistically significant differences were that women undergoing combined surgery had higher vaginal parity, and were more likely to have undergone preoperative chemotherapy. They were also more likely to have a prior diagnosis of cardiovascular or pulmonary disease,” Dr. Davidson said.
“Women undergoing treatment for suspected gynecologic malignancy have the same or higher prevalence of pelvic floor disorders, compared with the general population, and they may choose to have combined surgery if both subspecialists are available,” she continued. “However, there are limited data regarding the incidence of adverse events in these concurrent procedures, or how often the planned urogynecology portion of the procedure is modified intraoperatively.”
Though limited by factors inherent in retrospective chart review, such as information bias at the time of data collection (which was mitigated by cross-checking data and having only two data collectors), the findings of the current study suggest that “concurrent urogynecologic and gynecologic oncology surgery should be offered to appropriate patients, as adding urogynecology surgery does not increase the risk of serious adverse events,” she concluded, adding that the study “highlights the importance of preoperative counseling, including discussion of the increased risk of minor postoperative adverse events, such as postoperative voiding symptoms and urinary tract infection, as well as discussion of the 10% risk of a change in intraoperative plan in the urogynecologic procedure.”
“This study certainly helps us know that we’re doing no harm [in offering concurrent surgery],” he said.
Dr. Davidson and Dr. Noone each reported having no relevant disclosures.
SOURCE: Davidson ER et al. SGS 2018, Oral Presentation 13.
REPORTING FROM SGS 2018
Key clinical point: Concurrent urogynecologic/gynecologic oncology surgery does not increase the risk of serious adverse events.
Major finding: Concurrent surgery patients had more grade 2 complications (44% vs. 19%).
Study details: A retrospective study of 108 cases and 216 matched controls.
Disclosures: Dr. Davidson and Dr. Noone each reported having no disclosures.
Source: Davidson ER et al. SGS 2018, Oral Presentation 13.









