User login
Medication-Nonadherent Hypothyroidism Requiring Frequent Primary Care Visits to Achieve Euthyroidism
Nonadherence to medications is an issue across health care. In endocrinology, hypothyroidism, a deficiency of thyroid hormones, is most often treated with levothyroxine and if left untreated can lead to myxedema coma, which can lead to death due to multiorgan dysfunction.1 Therefore, adherence to levothyroxine is very important in preventing fatal complications.
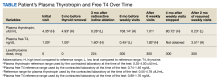
We present the case of a patient with persistent primary hypothyroidism who was suspected to be nonadherent to levothyroxine, although the patient consistently claimed adherence. The patient’s plasma thyrotropin (TSH) level improved to reference range after 6 weeks of weekly primary care clinic visits. After stopping the visits, his plasma TSH level increased again, so 9 more weeks of visits resumed, which again helped bring down his plasma TSH levels.
Case Presentation
A male patient aged 67 years presented to the Dayton Veterans Affairs Medical Center (VAMC) endocrinology clinic for evaluation of thyroid nodules. The patient reported no history of neck irradiation and a physical examination was unremarkable. At that time, laboratory results showed a slightly elevated plasma TSH level of 4.35 uIU/mL (reference range, 0.35-4.00 uIU/mL) and normal free thyroxine (T4) of 1.00 ng/dL (reference range, 0.74-1.46 ng/dL). Later that year, the patient underwent a total thyroidectomy at the Cincinnati VAMC for Hurthle cell variant papillary thyroid carcinoma that was noted on biopsy at the Dayton VAMC. After surgical pathology results were available, the patient started levothyroxine 200 mcg daily, although 224 mcg would have been more appropriate based on his 142 kg weight. Due to a history of arrhythmia, the goal plasma TSH level was 0.10 to 0.50 uIU/mL. The patient subsequently underwent radioactive iodine ablation. After levothyroxine dose adjustments, the patient’s plasma TSH level was noted to be within his target range at 0.28 uIU/mL 3 months postablation.
Over the next 5 years the patient had regular laboratory tests during which his plasma TSH level rose and were typically high despite adjusting levothyroxine doses between 200 mcg and 325 mcg. The patient received counseling on taking the medication in the morning on an empty stomach and waiting at least 1 hour before consuming anything, and he went to many follow-up visits at the Dayton VAMC endocrinology clinic. He reported no vomiting or diarrhea but endorsed weight gain once. The patient also had high free T4 at times and did not take extra levothyroxine before undergoing laboratory tests.
Nonadherence to levothyroxine was suspected, but the patient insisted he was adherent. He received the medication in the mail regularly, generally had 90-day refills unless a dose change was made, used a pill box, and had social support from his son, but he did not use a phone alarm to remind him to take it. A home care nurse made weekly visits to make sure the remaining levothyroxine pill counts were correct; however, the patient continued to have difficulty maintaining daily adherence at home as indicated by the nurse’s pill counts not aligning with the number of pills which should have been left if the patient was talking the pills daily.
The patient was asked to visit a local community-based outpatient clinic (CBOC) weekly (to avoid patient travel time to Dayton VAMC > 1 hour) to check pill counts and assess adherence. The patient went to the CBOC clinic for these visits, during which pill counts indicated much better but not 100% adherence. After 6 weeks of clinic visits, his plasma TSH decreased to 1.01 uIU/mL, which was within the reference range, and the patient stopped coming to the weekly clinic visits (Table). Four months later, the patient's plasma TSH levels increased to 80.72 uIU/mL. Nonadherence to levothyroxine was suspected again. He was asked to resume weekly clinic visits, and the life-threatening effects of hypothyroidism and not taking levothyroxine were discussed with the patient and his son. The patient made CBOC clinic visits for 9 weeks, after which his plasma TSH level was low at 0.23 uIU/mL.
Discussion
There are multiple important causes to consider in patients with persistent hypothyroidism. One is medication nonadherence, which was most likely seen in the patient in this case. Missing even 1 day of levothyroxine can affect TSH and thyroid hormone levels for several days due to the long half-life of the medication.2 Hepp and colleagues found that patients with hypothyroidism were significantly more likely to be nonadherent to levothyroxine if they had comorbid conditions such as type 2 diabetes or were obese.3 Another study of levothyroxine adherence found that the most common reason for missing doses was forgetfulness.4 However, memory and cognition impairments can also be symptoms of hypothyroidism itself; Haskard-Zolnierek and colleagues found a significant association between nonadherence to levothyroxine and self-reported brain fog in patients with hypothyroidism.5
Another cause of persistent hypothyroidism is malabsorption. Absorption of levothyroxine can be affected by intestinal malabsorption due to inflammatory bowel disease, lactose intolerance, or gastrointestinal infection, as well as several foods, drinks (eg, coffee), medications, vitamins, and supplements (eg, proton-pump inhibitors and calcium).2,6 Levothyroxine is absorbed mainly at the jejunum and upper ileum, so any pathologies or ingested items that would directly or indirectly affect absorption at those sites can affect levothyroxine absorption.2
A liquid levothyroxine formulation can help with malabsorption.2 Alternatively, weight gain may lead to a need for increasing the dosage of levothyroxine.2,6 Other factors that can affect TSH levels include Addison disease, dysregulation of the hypothalamic-pituitary-thyroid axis, and TSH heterophile antibodies.2
Research describes methods that have effectively treated hypothyroidism in patients struggling with levothyroxine adherence. Two case reports describe weekly visits for levothyroxine administration successfully treating uncontrolled hypothyroidism.7,8 A meta-analysis found that while weekly levothyroxine tablets led to a higher mean TSH level than daily use, weekly use still led to reference-range TSH levels, suggesting that weekly levothyroxine may be a helpful alternative for nonadherent patients.9 Alternatively, patients taking levothyroxine tablets have been shown to forget to take their medication more frequently compared to those taking the liquid formulation.10,11 Additionally, a study by El Helou and colleagues found that adherence to levothyroxine was significantly improved when patients had endocrinology visits once a month and when the endocrinologist provided information about hypothyroidism.12
Another method that may improve adherence to levothyroxine is telehealth visits. This would be especially helpful for patients who live far from the clinic or do not have the time, transportation, or financial means to visit the clinic for weekly visits to assess medication adherence. Additionally, patients may be afraid of admitting to a health care professional that they are nonadherent. Clinicians must be tactful when asking about adherence to make the patient feel comfortable with admitting to nonadherence if their cognition is not impaired. Then, a patient-led conversation can occur regarding realistic ways the patient feels they can work toward adherence.
To our knowledge, the patient in this case report had no symptoms of intestinal malabsorption, and weight gain was not thought to be the issue, as levothyroxine dosage was adjusted multiple times. His plasma TSH levels returned to reference range after weekly pill count visits for 6 weeks and after weekly pill count visits for 9 weeks. Therefore, nonadherence to levothyroxine was suspected to be the cause of frequently elevated plasma TSH levels despite the patient’s insistence on adherence. While the patient did not report memory issues, cognitive impairments due to hypothyroidism may have been contributing to his probable nonadherence. Additionally, he had comorbidities, such as type 2 diabetes mellitus and obesity, which may have made adherence more difficult.
Levothyroxine was also only prescribed in daily tablet form, so the frequency and formulation may have also contributed to nonadherence. While the home nurse was originally sent to assess the patient’s adherence, the care team could have had the nurse start giving the patient weekly levothyroxine once nonadherence was determined to be a likely issue. The patient’s adherence only improved when he went to the clinic for pill counts but not when the home nurse came to his house weekly; this could be because the patient knew he had to invest the time to physically go to clinic visits for pill checks, motivating him to increase adherence.
Conclusions
This case reports a patient with frequently high plasma TSH levels achieving normalization of plasma TSH levels after weekly medication adherence checks at a primary care clinic. Weekly visits to a clinic seem impractical compared to weekly dosing with a visiting nurse; however, after review of the literature, this may be an approach to consider in the future. This strategy may especially help in cases of persistent abnormal plasma TSH levels in which no etiology can be found other than suspected medication nonadherence. Knowing their medication use will be checked at weekly clinic visits may motivate patients to be adherent.
1. Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390(10101):1550-1562. doi:10.1016/S0140-6736(17)30703-1
2. Centanni M, Benvenga S, Sachmechi I. Diagnosis and management of treatment-refractory hypothyroidism: an expert consensus report. J Endocrinol Invest. 2017;40(12):1289-1301. doi:10.1007/s40618-017-0706-y
3. Hepp Z, Lage MJ, Espaillat R, Gossain VV. The association between adherence to levothyroxine and economic and clinical outcomes in patients with hypothyroidism in the US. J Med Econ. 2018;21(9):912-919. doi:10.1080/13696998.2018.1484749
4. Shakya Shrestha S, Risal K, Shrestha R, Bhatta RD. Medication Adherence to Levothyroxine Therapy among Hypothyroid Patients and their Clinical Outcomes with Special Reference to Thyroid Function Parameters. Kathmandu Univ Med J (KUMJ). 2018;16(62):129-137.
5. Haskard-Zolnierek K, Wilson C, Pruin J, Deason R, Howard K. The Relationship Between Brain Fog and Medication Adherence for Individuals With Hypothyroidism. Clin Nurs Res. 2022;31(3):445-452. doi:10.1177/10547738211038127
6. McNally LJ, Ofiaeli CI, Oyibo SO. Treatment-refractory hypothyroidism. BMJ. 2019;364:l579. Published 2019 Feb 25. doi:10.1136/bmj.l579
7. Nakano Y, Hashimoto K, Ohkiba N, et al. A Case of Refractory Hypothyroidism due to Poor Compliance Treated with the Weekly Intravenous and Oral Levothyroxine Administration. Case Rep Endocrinol. 2019;2019:5986014. Published 2019 Feb 5. doi:10.1155/2019/5986014
8. Kiran Z, Shaikh KS, Fatima N, Tariq N, Baloch AA. Levothyroxine absorption test followed by directly observed treatment on an outpatient basis to address long-term high TSH levels in a hypothyroid patient: a case report. J Med Case Rep. 2023;17(1):24. Published 2023 Jan 25. doi:10.1186/s13256-023-03760-0
9. Chiu HH, Larrazabal R Jr, Uy AB, Jimeno C. Weekly Versus Daily Levothyroxine Tablet Replacement in Adults with Hypothyroidism: A Meta-Analysis. J ASEAN Fed Endocr Soc. 2021;36(2):156-160. doi:10.15605/jafes.036.02.07
10. Cappelli C, Castello R, Marini F, et al. Adherence to Levothyroxine Treatment Among Patients With Hypothyroidism: A Northeastern Italian Survey. Front Endocrinol (Lausanne). 2018;9:699. Published 2018 Nov 23. doi:10.3389/fendo.2018.00699
11. Bocale R, Desideri G, Barini A, et al. Long-Term Adherence to Levothyroxine Replacement Therapy in Thyroidectomized Patients. J Clin Med. 2022;11(15):4296. Published 2022 Jul 24. doi:10.3390/jcm11154296
12. El Helou S, Hallit S, Awada S, et al. Adherence to levothyroxine among patients with hypothyroidism in Lebanon. East Mediterr Health J. 2019;25(3):149-159. Published 2019 Apr 25. doi:10.26719/emhj.18.022
Nonadherence to medications is an issue across health care. In endocrinology, hypothyroidism, a deficiency of thyroid hormones, is most often treated with levothyroxine and if left untreated can lead to myxedema coma, which can lead to death due to multiorgan dysfunction.1 Therefore, adherence to levothyroxine is very important in preventing fatal complications.
We present the case of a patient with persistent primary hypothyroidism who was suspected to be nonadherent to levothyroxine, although the patient consistently claimed adherence. The patient’s plasma thyrotropin (TSH) level improved to reference range after 6 weeks of weekly primary care clinic visits. After stopping the visits, his plasma TSH level increased again, so 9 more weeks of visits resumed, which again helped bring down his plasma TSH levels.
Case Presentation
A male patient aged 67 years presented to the Dayton Veterans Affairs Medical Center (VAMC) endocrinology clinic for evaluation of thyroid nodules. The patient reported no history of neck irradiation and a physical examination was unremarkable. At that time, laboratory results showed a slightly elevated plasma TSH level of 4.35 uIU/mL (reference range, 0.35-4.00 uIU/mL) and normal free thyroxine (T4) of 1.00 ng/dL (reference range, 0.74-1.46 ng/dL). Later that year, the patient underwent a total thyroidectomy at the Cincinnati VAMC for Hurthle cell variant papillary thyroid carcinoma that was noted on biopsy at the Dayton VAMC. After surgical pathology results were available, the patient started levothyroxine 200 mcg daily, although 224 mcg would have been more appropriate based on his 142 kg weight. Due to a history of arrhythmia, the goal plasma TSH level was 0.10 to 0.50 uIU/mL. The patient subsequently underwent radioactive iodine ablation. After levothyroxine dose adjustments, the patient’s plasma TSH level was noted to be within his target range at 0.28 uIU/mL 3 months postablation.
Over the next 5 years the patient had regular laboratory tests during which his plasma TSH level rose and were typically high despite adjusting levothyroxine doses between 200 mcg and 325 mcg. The patient received counseling on taking the medication in the morning on an empty stomach and waiting at least 1 hour before consuming anything, and he went to many follow-up visits at the Dayton VAMC endocrinology clinic. He reported no vomiting or diarrhea but endorsed weight gain once. The patient also had high free T4 at times and did not take extra levothyroxine before undergoing laboratory tests.
Nonadherence to levothyroxine was suspected, but the patient insisted he was adherent. He received the medication in the mail regularly, generally had 90-day refills unless a dose change was made, used a pill box, and had social support from his son, but he did not use a phone alarm to remind him to take it. A home care nurse made weekly visits to make sure the remaining levothyroxine pill counts were correct; however, the patient continued to have difficulty maintaining daily adherence at home as indicated by the nurse’s pill counts not aligning with the number of pills which should have been left if the patient was talking the pills daily.
The patient was asked to visit a local community-based outpatient clinic (CBOC) weekly (to avoid patient travel time to Dayton VAMC > 1 hour) to check pill counts and assess adherence. The patient went to the CBOC clinic for these visits, during which pill counts indicated much better but not 100% adherence. After 6 weeks of clinic visits, his plasma TSH decreased to 1.01 uIU/mL, which was within the reference range, and the patient stopped coming to the weekly clinic visits (Table). Four months later, the patient's plasma TSH levels increased to 80.72 uIU/mL. Nonadherence to levothyroxine was suspected again. He was asked to resume weekly clinic visits, and the life-threatening effects of hypothyroidism and not taking levothyroxine were discussed with the patient and his son. The patient made CBOC clinic visits for 9 weeks, after which his plasma TSH level was low at 0.23 uIU/mL.
Discussion
There are multiple important causes to consider in patients with persistent hypothyroidism. One is medication nonadherence, which was most likely seen in the patient in this case. Missing even 1 day of levothyroxine can affect TSH and thyroid hormone levels for several days due to the long half-life of the medication.2 Hepp and colleagues found that patients with hypothyroidism were significantly more likely to be nonadherent to levothyroxine if they had comorbid conditions such as type 2 diabetes or were obese.3 Another study of levothyroxine adherence found that the most common reason for missing doses was forgetfulness.4 However, memory and cognition impairments can also be symptoms of hypothyroidism itself; Haskard-Zolnierek and colleagues found a significant association between nonadherence to levothyroxine and self-reported brain fog in patients with hypothyroidism.5
Another cause of persistent hypothyroidism is malabsorption. Absorption of levothyroxine can be affected by intestinal malabsorption due to inflammatory bowel disease, lactose intolerance, or gastrointestinal infection, as well as several foods, drinks (eg, coffee), medications, vitamins, and supplements (eg, proton-pump inhibitors and calcium).2,6 Levothyroxine is absorbed mainly at the jejunum and upper ileum, so any pathologies or ingested items that would directly or indirectly affect absorption at those sites can affect levothyroxine absorption.2
A liquid levothyroxine formulation can help with malabsorption.2 Alternatively, weight gain may lead to a need for increasing the dosage of levothyroxine.2,6 Other factors that can affect TSH levels include Addison disease, dysregulation of the hypothalamic-pituitary-thyroid axis, and TSH heterophile antibodies.2
Research describes methods that have effectively treated hypothyroidism in patients struggling with levothyroxine adherence. Two case reports describe weekly visits for levothyroxine administration successfully treating uncontrolled hypothyroidism.7,8 A meta-analysis found that while weekly levothyroxine tablets led to a higher mean TSH level than daily use, weekly use still led to reference-range TSH levels, suggesting that weekly levothyroxine may be a helpful alternative for nonadherent patients.9 Alternatively, patients taking levothyroxine tablets have been shown to forget to take their medication more frequently compared to those taking the liquid formulation.10,11 Additionally, a study by El Helou and colleagues found that adherence to levothyroxine was significantly improved when patients had endocrinology visits once a month and when the endocrinologist provided information about hypothyroidism.12
Another method that may improve adherence to levothyroxine is telehealth visits. This would be especially helpful for patients who live far from the clinic or do not have the time, transportation, or financial means to visit the clinic for weekly visits to assess medication adherence. Additionally, patients may be afraid of admitting to a health care professional that they are nonadherent. Clinicians must be tactful when asking about adherence to make the patient feel comfortable with admitting to nonadherence if their cognition is not impaired. Then, a patient-led conversation can occur regarding realistic ways the patient feels they can work toward adherence.
To our knowledge, the patient in this case report had no symptoms of intestinal malabsorption, and weight gain was not thought to be the issue, as levothyroxine dosage was adjusted multiple times. His plasma TSH levels returned to reference range after weekly pill count visits for 6 weeks and after weekly pill count visits for 9 weeks. Therefore, nonadherence to levothyroxine was suspected to be the cause of frequently elevated plasma TSH levels despite the patient’s insistence on adherence. While the patient did not report memory issues, cognitive impairments due to hypothyroidism may have been contributing to his probable nonadherence. Additionally, he had comorbidities, such as type 2 diabetes mellitus and obesity, which may have made adherence more difficult.
Levothyroxine was also only prescribed in daily tablet form, so the frequency and formulation may have also contributed to nonadherence. While the home nurse was originally sent to assess the patient’s adherence, the care team could have had the nurse start giving the patient weekly levothyroxine once nonadherence was determined to be a likely issue. The patient’s adherence only improved when he went to the clinic for pill counts but not when the home nurse came to his house weekly; this could be because the patient knew he had to invest the time to physically go to clinic visits for pill checks, motivating him to increase adherence.
Conclusions
This case reports a patient with frequently high plasma TSH levels achieving normalization of plasma TSH levels after weekly medication adherence checks at a primary care clinic. Weekly visits to a clinic seem impractical compared to weekly dosing with a visiting nurse; however, after review of the literature, this may be an approach to consider in the future. This strategy may especially help in cases of persistent abnormal plasma TSH levels in which no etiology can be found other than suspected medication nonadherence. Knowing their medication use will be checked at weekly clinic visits may motivate patients to be adherent.
Nonadherence to medications is an issue across health care. In endocrinology, hypothyroidism, a deficiency of thyroid hormones, is most often treated with levothyroxine and if left untreated can lead to myxedema coma, which can lead to death due to multiorgan dysfunction.1 Therefore, adherence to levothyroxine is very important in preventing fatal complications.
We present the case of a patient with persistent primary hypothyroidism who was suspected to be nonadherent to levothyroxine, although the patient consistently claimed adherence. The patient’s plasma thyrotropin (TSH) level improved to reference range after 6 weeks of weekly primary care clinic visits. After stopping the visits, his plasma TSH level increased again, so 9 more weeks of visits resumed, which again helped bring down his plasma TSH levels.
Case Presentation
A male patient aged 67 years presented to the Dayton Veterans Affairs Medical Center (VAMC) endocrinology clinic for evaluation of thyroid nodules. The patient reported no history of neck irradiation and a physical examination was unremarkable. At that time, laboratory results showed a slightly elevated plasma TSH level of 4.35 uIU/mL (reference range, 0.35-4.00 uIU/mL) and normal free thyroxine (T4) of 1.00 ng/dL (reference range, 0.74-1.46 ng/dL). Later that year, the patient underwent a total thyroidectomy at the Cincinnati VAMC for Hurthle cell variant papillary thyroid carcinoma that was noted on biopsy at the Dayton VAMC. After surgical pathology results were available, the patient started levothyroxine 200 mcg daily, although 224 mcg would have been more appropriate based on his 142 kg weight. Due to a history of arrhythmia, the goal plasma TSH level was 0.10 to 0.50 uIU/mL. The patient subsequently underwent radioactive iodine ablation. After levothyroxine dose adjustments, the patient’s plasma TSH level was noted to be within his target range at 0.28 uIU/mL 3 months postablation.
Over the next 5 years the patient had regular laboratory tests during which his plasma TSH level rose and were typically high despite adjusting levothyroxine doses between 200 mcg and 325 mcg. The patient received counseling on taking the medication in the morning on an empty stomach and waiting at least 1 hour before consuming anything, and he went to many follow-up visits at the Dayton VAMC endocrinology clinic. He reported no vomiting or diarrhea but endorsed weight gain once. The patient also had high free T4 at times and did not take extra levothyroxine before undergoing laboratory tests.
Nonadherence to levothyroxine was suspected, but the patient insisted he was adherent. He received the medication in the mail regularly, generally had 90-day refills unless a dose change was made, used a pill box, and had social support from his son, but he did not use a phone alarm to remind him to take it. A home care nurse made weekly visits to make sure the remaining levothyroxine pill counts were correct; however, the patient continued to have difficulty maintaining daily adherence at home as indicated by the nurse’s pill counts not aligning with the number of pills which should have been left if the patient was talking the pills daily.
The patient was asked to visit a local community-based outpatient clinic (CBOC) weekly (to avoid patient travel time to Dayton VAMC > 1 hour) to check pill counts and assess adherence. The patient went to the CBOC clinic for these visits, during which pill counts indicated much better but not 100% adherence. After 6 weeks of clinic visits, his plasma TSH decreased to 1.01 uIU/mL, which was within the reference range, and the patient stopped coming to the weekly clinic visits (Table). Four months later, the patient's plasma TSH levels increased to 80.72 uIU/mL. Nonadherence to levothyroxine was suspected again. He was asked to resume weekly clinic visits, and the life-threatening effects of hypothyroidism and not taking levothyroxine were discussed with the patient and his son. The patient made CBOC clinic visits for 9 weeks, after which his plasma TSH level was low at 0.23 uIU/mL.
Discussion
There are multiple important causes to consider in patients with persistent hypothyroidism. One is medication nonadherence, which was most likely seen in the patient in this case. Missing even 1 day of levothyroxine can affect TSH and thyroid hormone levels for several days due to the long half-life of the medication.2 Hepp and colleagues found that patients with hypothyroidism were significantly more likely to be nonadherent to levothyroxine if they had comorbid conditions such as type 2 diabetes or were obese.3 Another study of levothyroxine adherence found that the most common reason for missing doses was forgetfulness.4 However, memory and cognition impairments can also be symptoms of hypothyroidism itself; Haskard-Zolnierek and colleagues found a significant association between nonadherence to levothyroxine and self-reported brain fog in patients with hypothyroidism.5
Another cause of persistent hypothyroidism is malabsorption. Absorption of levothyroxine can be affected by intestinal malabsorption due to inflammatory bowel disease, lactose intolerance, or gastrointestinal infection, as well as several foods, drinks (eg, coffee), medications, vitamins, and supplements (eg, proton-pump inhibitors and calcium).2,6 Levothyroxine is absorbed mainly at the jejunum and upper ileum, so any pathologies or ingested items that would directly or indirectly affect absorption at those sites can affect levothyroxine absorption.2
A liquid levothyroxine formulation can help with malabsorption.2 Alternatively, weight gain may lead to a need for increasing the dosage of levothyroxine.2,6 Other factors that can affect TSH levels include Addison disease, dysregulation of the hypothalamic-pituitary-thyroid axis, and TSH heterophile antibodies.2
Research describes methods that have effectively treated hypothyroidism in patients struggling with levothyroxine adherence. Two case reports describe weekly visits for levothyroxine administration successfully treating uncontrolled hypothyroidism.7,8 A meta-analysis found that while weekly levothyroxine tablets led to a higher mean TSH level than daily use, weekly use still led to reference-range TSH levels, suggesting that weekly levothyroxine may be a helpful alternative for nonadherent patients.9 Alternatively, patients taking levothyroxine tablets have been shown to forget to take their medication more frequently compared to those taking the liquid formulation.10,11 Additionally, a study by El Helou and colleagues found that adherence to levothyroxine was significantly improved when patients had endocrinology visits once a month and when the endocrinologist provided information about hypothyroidism.12
Another method that may improve adherence to levothyroxine is telehealth visits. This would be especially helpful for patients who live far from the clinic or do not have the time, transportation, or financial means to visit the clinic for weekly visits to assess medication adherence. Additionally, patients may be afraid of admitting to a health care professional that they are nonadherent. Clinicians must be tactful when asking about adherence to make the patient feel comfortable with admitting to nonadherence if their cognition is not impaired. Then, a patient-led conversation can occur regarding realistic ways the patient feels they can work toward adherence.
To our knowledge, the patient in this case report had no symptoms of intestinal malabsorption, and weight gain was not thought to be the issue, as levothyroxine dosage was adjusted multiple times. His plasma TSH levels returned to reference range after weekly pill count visits for 6 weeks and after weekly pill count visits for 9 weeks. Therefore, nonadherence to levothyroxine was suspected to be the cause of frequently elevated plasma TSH levels despite the patient’s insistence on adherence. While the patient did not report memory issues, cognitive impairments due to hypothyroidism may have been contributing to his probable nonadherence. Additionally, he had comorbidities, such as type 2 diabetes mellitus and obesity, which may have made adherence more difficult.
Levothyroxine was also only prescribed in daily tablet form, so the frequency and formulation may have also contributed to nonadherence. While the home nurse was originally sent to assess the patient’s adherence, the care team could have had the nurse start giving the patient weekly levothyroxine once nonadherence was determined to be a likely issue. The patient’s adherence only improved when he went to the clinic for pill counts but not when the home nurse came to his house weekly; this could be because the patient knew he had to invest the time to physically go to clinic visits for pill checks, motivating him to increase adherence.
Conclusions
This case reports a patient with frequently high plasma TSH levels achieving normalization of plasma TSH levels after weekly medication adherence checks at a primary care clinic. Weekly visits to a clinic seem impractical compared to weekly dosing with a visiting nurse; however, after review of the literature, this may be an approach to consider in the future. This strategy may especially help in cases of persistent abnormal plasma TSH levels in which no etiology can be found other than suspected medication nonadherence. Knowing their medication use will be checked at weekly clinic visits may motivate patients to be adherent.
1. Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390(10101):1550-1562. doi:10.1016/S0140-6736(17)30703-1
2. Centanni M, Benvenga S, Sachmechi I. Diagnosis and management of treatment-refractory hypothyroidism: an expert consensus report. J Endocrinol Invest. 2017;40(12):1289-1301. doi:10.1007/s40618-017-0706-y
3. Hepp Z, Lage MJ, Espaillat R, Gossain VV. The association between adherence to levothyroxine and economic and clinical outcomes in patients with hypothyroidism in the US. J Med Econ. 2018;21(9):912-919. doi:10.1080/13696998.2018.1484749
4. Shakya Shrestha S, Risal K, Shrestha R, Bhatta RD. Medication Adherence to Levothyroxine Therapy among Hypothyroid Patients and their Clinical Outcomes with Special Reference to Thyroid Function Parameters. Kathmandu Univ Med J (KUMJ). 2018;16(62):129-137.
5. Haskard-Zolnierek K, Wilson C, Pruin J, Deason R, Howard K. The Relationship Between Brain Fog and Medication Adherence for Individuals With Hypothyroidism. Clin Nurs Res. 2022;31(3):445-452. doi:10.1177/10547738211038127
6. McNally LJ, Ofiaeli CI, Oyibo SO. Treatment-refractory hypothyroidism. BMJ. 2019;364:l579. Published 2019 Feb 25. doi:10.1136/bmj.l579
7. Nakano Y, Hashimoto K, Ohkiba N, et al. A Case of Refractory Hypothyroidism due to Poor Compliance Treated with the Weekly Intravenous and Oral Levothyroxine Administration. Case Rep Endocrinol. 2019;2019:5986014. Published 2019 Feb 5. doi:10.1155/2019/5986014
8. Kiran Z, Shaikh KS, Fatima N, Tariq N, Baloch AA. Levothyroxine absorption test followed by directly observed treatment on an outpatient basis to address long-term high TSH levels in a hypothyroid patient: a case report. J Med Case Rep. 2023;17(1):24. Published 2023 Jan 25. doi:10.1186/s13256-023-03760-0
9. Chiu HH, Larrazabal R Jr, Uy AB, Jimeno C. Weekly Versus Daily Levothyroxine Tablet Replacement in Adults with Hypothyroidism: A Meta-Analysis. J ASEAN Fed Endocr Soc. 2021;36(2):156-160. doi:10.15605/jafes.036.02.07
10. Cappelli C, Castello R, Marini F, et al. Adherence to Levothyroxine Treatment Among Patients With Hypothyroidism: A Northeastern Italian Survey. Front Endocrinol (Lausanne). 2018;9:699. Published 2018 Nov 23. doi:10.3389/fendo.2018.00699
11. Bocale R, Desideri G, Barini A, et al. Long-Term Adherence to Levothyroxine Replacement Therapy in Thyroidectomized Patients. J Clin Med. 2022;11(15):4296. Published 2022 Jul 24. doi:10.3390/jcm11154296
12. El Helou S, Hallit S, Awada S, et al. Adherence to levothyroxine among patients with hypothyroidism in Lebanon. East Mediterr Health J. 2019;25(3):149-159. Published 2019 Apr 25. doi:10.26719/emhj.18.022
1. Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390(10101):1550-1562. doi:10.1016/S0140-6736(17)30703-1
2. Centanni M, Benvenga S, Sachmechi I. Diagnosis and management of treatment-refractory hypothyroidism: an expert consensus report. J Endocrinol Invest. 2017;40(12):1289-1301. doi:10.1007/s40618-017-0706-y
3. Hepp Z, Lage MJ, Espaillat R, Gossain VV. The association between adherence to levothyroxine and economic and clinical outcomes in patients with hypothyroidism in the US. J Med Econ. 2018;21(9):912-919. doi:10.1080/13696998.2018.1484749
4. Shakya Shrestha S, Risal K, Shrestha R, Bhatta RD. Medication Adherence to Levothyroxine Therapy among Hypothyroid Patients and their Clinical Outcomes with Special Reference to Thyroid Function Parameters. Kathmandu Univ Med J (KUMJ). 2018;16(62):129-137.
5. Haskard-Zolnierek K, Wilson C, Pruin J, Deason R, Howard K. The Relationship Between Brain Fog and Medication Adherence for Individuals With Hypothyroidism. Clin Nurs Res. 2022;31(3):445-452. doi:10.1177/10547738211038127
6. McNally LJ, Ofiaeli CI, Oyibo SO. Treatment-refractory hypothyroidism. BMJ. 2019;364:l579. Published 2019 Feb 25. doi:10.1136/bmj.l579
7. Nakano Y, Hashimoto K, Ohkiba N, et al. A Case of Refractory Hypothyroidism due to Poor Compliance Treated with the Weekly Intravenous and Oral Levothyroxine Administration. Case Rep Endocrinol. 2019;2019:5986014. Published 2019 Feb 5. doi:10.1155/2019/5986014
8. Kiran Z, Shaikh KS, Fatima N, Tariq N, Baloch AA. Levothyroxine absorption test followed by directly observed treatment on an outpatient basis to address long-term high TSH levels in a hypothyroid patient: a case report. J Med Case Rep. 2023;17(1):24. Published 2023 Jan 25. doi:10.1186/s13256-023-03760-0
9. Chiu HH, Larrazabal R Jr, Uy AB, Jimeno C. Weekly Versus Daily Levothyroxine Tablet Replacement in Adults with Hypothyroidism: A Meta-Analysis. J ASEAN Fed Endocr Soc. 2021;36(2):156-160. doi:10.15605/jafes.036.02.07
10. Cappelli C, Castello R, Marini F, et al. Adherence to Levothyroxine Treatment Among Patients With Hypothyroidism: A Northeastern Italian Survey. Front Endocrinol (Lausanne). 2018;9:699. Published 2018 Nov 23. doi:10.3389/fendo.2018.00699
11. Bocale R, Desideri G, Barini A, et al. Long-Term Adherence to Levothyroxine Replacement Therapy in Thyroidectomized Patients. J Clin Med. 2022;11(15):4296. Published 2022 Jul 24. doi:10.3390/jcm11154296
12. El Helou S, Hallit S, Awada S, et al. Adherence to levothyroxine among patients with hypothyroidism in Lebanon. East Mediterr Health J. 2019;25(3):149-159. Published 2019 Apr 25. doi:10.26719/emhj.18.022
Clinical Implications of a Formulary Conversion From Budesonide/formoterol to Fluticasone/salmeterol at a VA Medical Center
Chronic obstructive pulmonary disease (COPD) is a respiratory disorder associated with slowly progressive systemic inflammation. It includes emphysema, chronic bronchitis, and small airway disease. Patients with COPD have an incomplete reversibility of airway obstruction, the key differentiating factor between it and asthma.1
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend a combination inhaler consisting of a long-acting β-2 agonist (LABA) and inhaled corticosteroid (ICS) for patients with a history of COPD exacerbations.2 Blood eosinophil count is another marker for the initiation of an ICS in patients with COPD. According to the 2023 GOLD Report, ICS therapy is appropriate for patients who experience frequent exacerbations and have a blood eosinophil count > 100 cells/μL, while on maximum tolerated inhaler therapy.3 A 2019 meta-analysis found an overall reduction in the risk of exacerbations in patients with blood eosinophil counts ≥ 100 cells/µL after initiating an ICS.4
Common ICS-LABA inhalers include the combination of budesonide/formoterol as well as fluticasone/salmeterol. Though these combinations are within the same therapeutic class, they have different delivery systems: budesonide/formoterol is a metered dose inhaler, while fluticasone/salmeterol is a dry powder inhaler. The PATHOS study compared the exacerbation rates for the 2 inhalers in primary care patients with COPD. Patients treated long-term with the budesonide/formoterol inhaler were significantly less likely to experience a COPD exacerbation than those treated with the fluticasone/salmeterol inhaler.5
In 2021, The Veteran Health Administration transitioned patients from budesonide/formoterol inhalers to fluticasone/salmeterol inhalers through a formulary conversion. The purpose of this study was to examine the outcomes for patients undergoing the transition.
Methods
A retrospective chart review was conducted on patients at the Hershel “Woody” Williams Veterans Affairs Medical Center in Huntington, West Virginia, with COPD and prescriptions for both budesonide/formoterol and fluticasone/salmeterol inhalers between February 1, 2021, and May 30, 2022. In 2018, the prevalence of COPD in West Virginia was 13.9%, highest in the US.6 Data was obtained through the US Department of Veteran Affairs (VA) Corporate Data Warehouse and stored on a VA Informatics and Computing Infrastructure server. Patients were randomly selected from this cohort and included if they were aged 18 to 89 years, prescribed both inhalers, and had a confirmed COPD diagnosis. Patients were excluded if they also had an asthma diagnosis, if they had an interstitial lung disease, or any tracheostomy tubes. The date of transition from a budesonide/formoterol inhaler to a fluticasone/salmeterol inhaler was collected to establish a timeline of 6 months before and 6 months after the transition.
The primary endpoint was to assess clinical outcomes such as the number of COPD exacerbations and hospitalizations within 6 months of the transition for patients affected by the formulary conversion. Secondary outcomes included the incidence of adverse effects (AEs), treatment failure, tobacco use, and systemic corticosteroid/antimicrobial utilization.
Statistical analyses were performed using STATA v.15. Numerical data was analyzed using a Wilcoxon signed rank test. Categorical data was analyzed by a logistic regression analysis.
Results
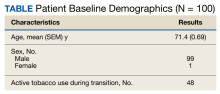
Of 1497 included patients who transitioned from budesonide/formoterol to fluticasone/salmeterol inhalers, 165 were randomly selected and 100 patients were included in this analysis. Of the 100 patients, 99 were male with a mean (SEM) age of 71 (0.69) years (range, 54-87) (Table).
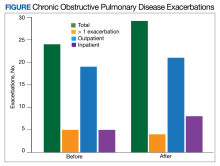
The transition from budesonide/formoterol to fluticasone/salmeterol inhalers did not have a statistically significant impact on exacerbations (P = .56). Thirty patients had ≥ 1 exacerbation: 12 had an exacerbation before the transition, 10 had an exacerbation after the transition, and 8 had exacerbations before and after the transition. In the 6 months prior to the transition while on a budesonide/formoterol inhaler, there were 24 exacerbations among 20 patients. Five patients had > 1 exacerbation, accounting for 11 of the 24 exacerbations. There were 29 exacerbations among 19 patients while on a fluticasone/salmeterol inhaler in the 6 months after the transition. Four of these patients had > 1 exacerbation, accounting for 14 of 29 exacerbations (Figure).
Secondary endpoints showed 3 patients experienced an AE related to fluticasone/salmeterol, including thrush, coughing and throat irritation, and dyspnea. Eighteen fluticasone/salmeterol therapeutic failures were indicated by related prior authorization medication requests in the electronic health record. Twelve of 18 patients experienced no difference in exacerbations before vs after the transition to budesonide/formoterol. Twenty-three patients transitioned from fluticasone/salmeterol to a different ICS-LABA therapy; 20 of those 23 patients transitioned back to a budesonide/formoterol inhaler.
There were 48 documented active tobacco users in the study. There was no statistically significant correlation (P = .52) when comparing tobacco use at time of conversion and exacerbation frequency, although the coefficient showed a negative correlation of -0.387. In the 6 months prior to the transition, there were 17 prescriptions for systemic corticosteroids and 24 for antibiotics to treat COPD exacerbations. Following the transition, there were only 12 prescriptions for systemic corticosteroids and 23 for antibiotics. Fifty-two patients had an active prescription for a fluticasone/salmeterol inhaler at the time of the data review (November to December 2022); of the 48 patients who did not, 10 were no longer active due to patient death between the study period and data retrieval.
Discussion
Patients who transitioned from budesonide/formoterol to fluticasone/salmeterol inhalers did not show a significant difference in clinical COPD outcomes. While the total number of exacerbations increased after switching to the fluticasone/salmeterol inhaler, fewer patients had exacerbations during fluticasone/salmeterol therapy when compared with budesonide/fluticasone therapy. The number of patients receiving systemic corticosteroids and antibiotics to treat exacerbations before and after the transition were similar.
The frequency of treatment failures and AEs to the fluticasone/salmeterol inhaler could be due to the change of the inhaler delivery systems. Budesonide/formoterol is a metered dose inhaler (MDI). It is equipped with a pressurized canister that allows a spacer to be used to maximize benefit. Spacers can assist in preventing oral candidiasis by reducing the amount of medication that touches the back of the throat. Spacers are an option for patients, but not all use them for their MDIs, which can result in a less effective administered dose. Fluticasone/salmeterol is a dry powder inhaler, which requires a deep, fast breath to maximize the benefit, and spacers cannot be used with them. MDIs have been shown to be responsible for a negative impact on climate change, which can be reduced by switching to a dry powder inhaler.7
Tobacco cessation is very important in limiting the progression of COPD. As shown with the negative coefficient correlation, not being an active tobacco user at the time of transition correlated (although not significantly) with less frequent exacerbations. When comparing this study to similar research, such as the PATHOS study, several differences are observed.5 The PATHOS study compared long term treatment (> 1 year) of budesonide/formoterol or fluticasone/salmeterol, a longer period than this study. It regarded similar outcomes for the definition of an exacerbation, such as antibiotic/steroid use or hospital admission. While the current study showed no significant difference between the 2 inhalers and their effect on exacerbations, the PATHOS study found that those treated with a budesonide/formoterol inhaler were less likely to experience COPD-related exacerbations than those treated with the fluticasone/salmeterol inhaler. The PATHOS study had a larger mainly Scandinavian sample (N = 5500). This population could exhibit baseline differences from a study of US veterans.5 A similar Canadian matched cohort study of 2262 patients compared the 2 inhalers to assess their relative effectiveness. It found that COPD exacerbations did not differ between the 2 groups, but the budesonide/formoterol group was significantly less likely to have an emergency department visit compared to the fluticasone salmeterol group.8 Like the PATHOS study, the Canadian study had a larger sample size and longer timeframe than did our study.
Limitations
There are various limitations to this study. It was a retrospective, single-center study and the patient population was relatively homogenous, with only 1 female and a mean age of 71 years. As a study conducted in a veteran population in West Virginia, the findings may not be representative of the general population with COPD, which includes more women and more racial diversity.9 The American Lung Association discusses how environmental exposures to hazardous conditions increase the risks of pulmonary diseases for veterans.10 It has been reported that the prevalence of COPD is higher among veterans compared to the general population, but it is not different in terms of disease manifestation.10
Another limitation is the short time frame. Clinical guidelines, including the GOLD Report, typically track the number of exacerbations for 1 year to escalate therapy.3 Six months was a relatively short time frame, and it is possible that more exacerbations may have occurred beyond the study time frame. Ten patients in the sample died between the end of the study period and data retrieval, which might have been caught by a longer study period. An additional limitation was the inability to measure adherence. As this was a formulary conversion, many patients had been mailed a 30- or 90-day prescription of the budesonide/formoterol inhaler when transitioned to the fluticasone/salmeterol inhaler. There was no way to accurately determine when the patient made the switch to the fluticasone/salmeterol inhaler. This study also had a small sample group (a pre-post analysis of the same group), a limitation when evaluating the impact of this formulary change on a small percentage of the population transitioned.
This formulary conversion occurred during the COVID-19 pandemic, and some exacerbations could have been the result of a misdiagnosed COVID-19 infection. Respiratory infections, including COVID-19, are common causes of exacerbations. It is also possible that some patients elected not to receive medical care for symptoms of an exacerbation during the pandemic.11
Conclusions
Switching from the budesonide/formoterol inhaler to the fluticasone/salmeterol inhaler through formulary conversion did not have a significant impact on the clinical outcomes in patients with COPD. This study found that although the inhalers contain different active ingredients, products within the same therapeutic class yielded nonsignificant changes. When conducting formulary conversions, intolerances and treatment failures should be expected when switching from different inhaler delivery systems. This study further justifies the ability to be cost effective by making formulary conversions within the same therapeutic class within a veterans population.
Acknowledgments
The authors would like to acknowledge James Brown, PharmD, PhD.
1. US Department of Veterans Affairs. VA/DOD Clinical Practice Guideline. Management of Outpatient Chronic Obstructive Pulmonary Disease. 2021. Accessed January 22, 2024. https://www.healthquality.va.gov/guidelines/cd/copd/
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD Report. 2022. Accessed January 22, 2024. https://goldcopd.org/2022-gold-reports/
3. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis management, and prevention of chronic obstructive pulmonary disease 2023 report. Accessed January 26, 2024. https://goldcopd.org/wp-content/uploads/2023/03/GOLD-2023-ver-1.3-17Feb2023_WMV.pdf
4. Oshagbemi OA, Odiba JO, Daniel A, Yunusa I. Absolute blood eosinophil counts to guide inhaled corticosteroids therapy among patients with COPD: systematic review and meta-analysis. Curr Drug Targets. 2019;20(16):1670-1679. doi:10.2174/1389450120666190808141625
5. Larsson K, Janson C, Lisspers K, et al. Combination of budesonide/formoterol more effective than fluticasone/salmeterol in preventing exacerbations in chronic obstructive pulmonary disease: the PATHOS study. J Intern Med. 2013;273(6):584-594. doi:10.1111/joim.12067
6. West Virginia Department of Health and Human Resources, Division of Health Promotion and Chronic Disease. Statistics about the population of West Virginia. 2018. Accessed January 22, 2024. https://dhhr.wv.gov/hpcd/data_reports/ Pages/Fast-Facts.aspx
7. Fidler L, Green S, Wintemute K. Pressurized metered-dose inhalers and their impact on climate change. CMAJ. 2022;194(12):E460. doi:10.1503/cmaj.211747
8. Blais L, Forget A, Ramachandran S. Relative effectiveness of budesonide/formoterol and fluticasone propionate/salmeterol in a 1-year, population-based, matched cohort study of patients with chronic obstructive pulmonary disease (COPD): Effect on COPD-related exacerbations, emergency department visits and hospitalizations, medication utilization, and treatment adherence. Clin Ther. 2010;32(7):1320-1328. doi:10.1016/j.clinthera.2010.06.022
9. Wheaton AG, Cunningham TJ, Ford ES, Croft JB; Centers for Disease Control and Prevention (CDC). Employment and activity limitations among adults with chronic obstructive pulmonary disease — United States, 2013. MMWR Morb Mortal Wkly Rep. 2015:64(11):289-295.
10. Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269-1283. doi:10.2147/COPD.S339323
11. Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250-1257. doi:10.15585/mmwr.mm6936a4
Chronic obstructive pulmonary disease (COPD) is a respiratory disorder associated with slowly progressive systemic inflammation. It includes emphysema, chronic bronchitis, and small airway disease. Patients with COPD have an incomplete reversibility of airway obstruction, the key differentiating factor between it and asthma.1
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend a combination inhaler consisting of a long-acting β-2 agonist (LABA) and inhaled corticosteroid (ICS) for patients with a history of COPD exacerbations.2 Blood eosinophil count is another marker for the initiation of an ICS in patients with COPD. According to the 2023 GOLD Report, ICS therapy is appropriate for patients who experience frequent exacerbations and have a blood eosinophil count > 100 cells/μL, while on maximum tolerated inhaler therapy.3 A 2019 meta-analysis found an overall reduction in the risk of exacerbations in patients with blood eosinophil counts ≥ 100 cells/µL after initiating an ICS.4
Common ICS-LABA inhalers include the combination of budesonide/formoterol as well as fluticasone/salmeterol. Though these combinations are within the same therapeutic class, they have different delivery systems: budesonide/formoterol is a metered dose inhaler, while fluticasone/salmeterol is a dry powder inhaler. The PATHOS study compared the exacerbation rates for the 2 inhalers in primary care patients with COPD. Patients treated long-term with the budesonide/formoterol inhaler were significantly less likely to experience a COPD exacerbation than those treated with the fluticasone/salmeterol inhaler.5
In 2021, The Veteran Health Administration transitioned patients from budesonide/formoterol inhalers to fluticasone/salmeterol inhalers through a formulary conversion. The purpose of this study was to examine the outcomes for patients undergoing the transition.
Methods
A retrospective chart review was conducted on patients at the Hershel “Woody” Williams Veterans Affairs Medical Center in Huntington, West Virginia, with COPD and prescriptions for both budesonide/formoterol and fluticasone/salmeterol inhalers between February 1, 2021, and May 30, 2022. In 2018, the prevalence of COPD in West Virginia was 13.9%, highest in the US.6 Data was obtained through the US Department of Veteran Affairs (VA) Corporate Data Warehouse and stored on a VA Informatics and Computing Infrastructure server. Patients were randomly selected from this cohort and included if they were aged 18 to 89 years, prescribed both inhalers, and had a confirmed COPD diagnosis. Patients were excluded if they also had an asthma diagnosis, if they had an interstitial lung disease, or any tracheostomy tubes. The date of transition from a budesonide/formoterol inhaler to a fluticasone/salmeterol inhaler was collected to establish a timeline of 6 months before and 6 months after the transition.
The primary endpoint was to assess clinical outcomes such as the number of COPD exacerbations and hospitalizations within 6 months of the transition for patients affected by the formulary conversion. Secondary outcomes included the incidence of adverse effects (AEs), treatment failure, tobacco use, and systemic corticosteroid/antimicrobial utilization.
Statistical analyses were performed using STATA v.15. Numerical data was analyzed using a Wilcoxon signed rank test. Categorical data was analyzed by a logistic regression analysis.
Results
Of 1497 included patients who transitioned from budesonide/formoterol to fluticasone/salmeterol inhalers, 165 were randomly selected and 100 patients were included in this analysis. Of the 100 patients, 99 were male with a mean (SEM) age of 71 (0.69) years (range, 54-87) (Table).
The transition from budesonide/formoterol to fluticasone/salmeterol inhalers did not have a statistically significant impact on exacerbations (P = .56). Thirty patients had ≥ 1 exacerbation: 12 had an exacerbation before the transition, 10 had an exacerbation after the transition, and 8 had exacerbations before and after the transition. In the 6 months prior to the transition while on a budesonide/formoterol inhaler, there were 24 exacerbations among 20 patients. Five patients had > 1 exacerbation, accounting for 11 of the 24 exacerbations. There were 29 exacerbations among 19 patients while on a fluticasone/salmeterol inhaler in the 6 months after the transition. Four of these patients had > 1 exacerbation, accounting for 14 of 29 exacerbations (Figure).
Secondary endpoints showed 3 patients experienced an AE related to fluticasone/salmeterol, including thrush, coughing and throat irritation, and dyspnea. Eighteen fluticasone/salmeterol therapeutic failures were indicated by related prior authorization medication requests in the electronic health record. Twelve of 18 patients experienced no difference in exacerbations before vs after the transition to budesonide/formoterol. Twenty-three patients transitioned from fluticasone/salmeterol to a different ICS-LABA therapy; 20 of those 23 patients transitioned back to a budesonide/formoterol inhaler.
There were 48 documented active tobacco users in the study. There was no statistically significant correlation (P = .52) when comparing tobacco use at time of conversion and exacerbation frequency, although the coefficient showed a negative correlation of -0.387. In the 6 months prior to the transition, there were 17 prescriptions for systemic corticosteroids and 24 for antibiotics to treat COPD exacerbations. Following the transition, there were only 12 prescriptions for systemic corticosteroids and 23 for antibiotics. Fifty-two patients had an active prescription for a fluticasone/salmeterol inhaler at the time of the data review (November to December 2022); of the 48 patients who did not, 10 were no longer active due to patient death between the study period and data retrieval.
Discussion
Patients who transitioned from budesonide/formoterol to fluticasone/salmeterol inhalers did not show a significant difference in clinical COPD outcomes. While the total number of exacerbations increased after switching to the fluticasone/salmeterol inhaler, fewer patients had exacerbations during fluticasone/salmeterol therapy when compared with budesonide/fluticasone therapy. The number of patients receiving systemic corticosteroids and antibiotics to treat exacerbations before and after the transition were similar.
The frequency of treatment failures and AEs to the fluticasone/salmeterol inhaler could be due to the change of the inhaler delivery systems. Budesonide/formoterol is a metered dose inhaler (MDI). It is equipped with a pressurized canister that allows a spacer to be used to maximize benefit. Spacers can assist in preventing oral candidiasis by reducing the amount of medication that touches the back of the throat. Spacers are an option for patients, but not all use them for their MDIs, which can result in a less effective administered dose. Fluticasone/salmeterol is a dry powder inhaler, which requires a deep, fast breath to maximize the benefit, and spacers cannot be used with them. MDIs have been shown to be responsible for a negative impact on climate change, which can be reduced by switching to a dry powder inhaler.7
Tobacco cessation is very important in limiting the progression of COPD. As shown with the negative coefficient correlation, not being an active tobacco user at the time of transition correlated (although not significantly) with less frequent exacerbations. When comparing this study to similar research, such as the PATHOS study, several differences are observed.5 The PATHOS study compared long term treatment (> 1 year) of budesonide/formoterol or fluticasone/salmeterol, a longer period than this study. It regarded similar outcomes for the definition of an exacerbation, such as antibiotic/steroid use or hospital admission. While the current study showed no significant difference between the 2 inhalers and their effect on exacerbations, the PATHOS study found that those treated with a budesonide/formoterol inhaler were less likely to experience COPD-related exacerbations than those treated with the fluticasone/salmeterol inhaler. The PATHOS study had a larger mainly Scandinavian sample (N = 5500). This population could exhibit baseline differences from a study of US veterans.5 A similar Canadian matched cohort study of 2262 patients compared the 2 inhalers to assess their relative effectiveness. It found that COPD exacerbations did not differ between the 2 groups, but the budesonide/formoterol group was significantly less likely to have an emergency department visit compared to the fluticasone salmeterol group.8 Like the PATHOS study, the Canadian study had a larger sample size and longer timeframe than did our study.
Limitations
There are various limitations to this study. It was a retrospective, single-center study and the patient population was relatively homogenous, with only 1 female and a mean age of 71 years. As a study conducted in a veteran population in West Virginia, the findings may not be representative of the general population with COPD, which includes more women and more racial diversity.9 The American Lung Association discusses how environmental exposures to hazardous conditions increase the risks of pulmonary diseases for veterans.10 It has been reported that the prevalence of COPD is higher among veterans compared to the general population, but it is not different in terms of disease manifestation.10
Another limitation is the short time frame. Clinical guidelines, including the GOLD Report, typically track the number of exacerbations for 1 year to escalate therapy.3 Six months was a relatively short time frame, and it is possible that more exacerbations may have occurred beyond the study time frame. Ten patients in the sample died between the end of the study period and data retrieval, which might have been caught by a longer study period. An additional limitation was the inability to measure adherence. As this was a formulary conversion, many patients had been mailed a 30- or 90-day prescription of the budesonide/formoterol inhaler when transitioned to the fluticasone/salmeterol inhaler. There was no way to accurately determine when the patient made the switch to the fluticasone/salmeterol inhaler. This study also had a small sample group (a pre-post analysis of the same group), a limitation when evaluating the impact of this formulary change on a small percentage of the population transitioned.
This formulary conversion occurred during the COVID-19 pandemic, and some exacerbations could have been the result of a misdiagnosed COVID-19 infection. Respiratory infections, including COVID-19, are common causes of exacerbations. It is also possible that some patients elected not to receive medical care for symptoms of an exacerbation during the pandemic.11
Conclusions
Switching from the budesonide/formoterol inhaler to the fluticasone/salmeterol inhaler through formulary conversion did not have a significant impact on the clinical outcomes in patients with COPD. This study found that although the inhalers contain different active ingredients, products within the same therapeutic class yielded nonsignificant changes. When conducting formulary conversions, intolerances and treatment failures should be expected when switching from different inhaler delivery systems. This study further justifies the ability to be cost effective by making formulary conversions within the same therapeutic class within a veterans population.
Acknowledgments
The authors would like to acknowledge James Brown, PharmD, PhD.
Chronic obstructive pulmonary disease (COPD) is a respiratory disorder associated with slowly progressive systemic inflammation. It includes emphysema, chronic bronchitis, and small airway disease. Patients with COPD have an incomplete reversibility of airway obstruction, the key differentiating factor between it and asthma.1
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend a combination inhaler consisting of a long-acting β-2 agonist (LABA) and inhaled corticosteroid (ICS) for patients with a history of COPD exacerbations.2 Blood eosinophil count is another marker for the initiation of an ICS in patients with COPD. According to the 2023 GOLD Report, ICS therapy is appropriate for patients who experience frequent exacerbations and have a blood eosinophil count > 100 cells/μL, while on maximum tolerated inhaler therapy.3 A 2019 meta-analysis found an overall reduction in the risk of exacerbations in patients with blood eosinophil counts ≥ 100 cells/µL after initiating an ICS.4
Common ICS-LABA inhalers include the combination of budesonide/formoterol as well as fluticasone/salmeterol. Though these combinations are within the same therapeutic class, they have different delivery systems: budesonide/formoterol is a metered dose inhaler, while fluticasone/salmeterol is a dry powder inhaler. The PATHOS study compared the exacerbation rates for the 2 inhalers in primary care patients with COPD. Patients treated long-term with the budesonide/formoterol inhaler were significantly less likely to experience a COPD exacerbation than those treated with the fluticasone/salmeterol inhaler.5
In 2021, The Veteran Health Administration transitioned patients from budesonide/formoterol inhalers to fluticasone/salmeterol inhalers through a formulary conversion. The purpose of this study was to examine the outcomes for patients undergoing the transition.
Methods
A retrospective chart review was conducted on patients at the Hershel “Woody” Williams Veterans Affairs Medical Center in Huntington, West Virginia, with COPD and prescriptions for both budesonide/formoterol and fluticasone/salmeterol inhalers between February 1, 2021, and May 30, 2022. In 2018, the prevalence of COPD in West Virginia was 13.9%, highest in the US.6 Data was obtained through the US Department of Veteran Affairs (VA) Corporate Data Warehouse and stored on a VA Informatics and Computing Infrastructure server. Patients were randomly selected from this cohort and included if they were aged 18 to 89 years, prescribed both inhalers, and had a confirmed COPD diagnosis. Patients were excluded if they also had an asthma diagnosis, if they had an interstitial lung disease, or any tracheostomy tubes. The date of transition from a budesonide/formoterol inhaler to a fluticasone/salmeterol inhaler was collected to establish a timeline of 6 months before and 6 months after the transition.
The primary endpoint was to assess clinical outcomes such as the number of COPD exacerbations and hospitalizations within 6 months of the transition for patients affected by the formulary conversion. Secondary outcomes included the incidence of adverse effects (AEs), treatment failure, tobacco use, and systemic corticosteroid/antimicrobial utilization.
Statistical analyses were performed using STATA v.15. Numerical data was analyzed using a Wilcoxon signed rank test. Categorical data was analyzed by a logistic regression analysis.
Results
Of 1497 included patients who transitioned from budesonide/formoterol to fluticasone/salmeterol inhalers, 165 were randomly selected and 100 patients were included in this analysis. Of the 100 patients, 99 were male with a mean (SEM) age of 71 (0.69) years (range, 54-87) (Table).
The transition from budesonide/formoterol to fluticasone/salmeterol inhalers did not have a statistically significant impact on exacerbations (P = .56). Thirty patients had ≥ 1 exacerbation: 12 had an exacerbation before the transition, 10 had an exacerbation after the transition, and 8 had exacerbations before and after the transition. In the 6 months prior to the transition while on a budesonide/formoterol inhaler, there were 24 exacerbations among 20 patients. Five patients had > 1 exacerbation, accounting for 11 of the 24 exacerbations. There were 29 exacerbations among 19 patients while on a fluticasone/salmeterol inhaler in the 6 months after the transition. Four of these patients had > 1 exacerbation, accounting for 14 of 29 exacerbations (Figure).
Secondary endpoints showed 3 patients experienced an AE related to fluticasone/salmeterol, including thrush, coughing and throat irritation, and dyspnea. Eighteen fluticasone/salmeterol therapeutic failures were indicated by related prior authorization medication requests in the electronic health record. Twelve of 18 patients experienced no difference in exacerbations before vs after the transition to budesonide/formoterol. Twenty-three patients transitioned from fluticasone/salmeterol to a different ICS-LABA therapy; 20 of those 23 patients transitioned back to a budesonide/formoterol inhaler.
There were 48 documented active tobacco users in the study. There was no statistically significant correlation (P = .52) when comparing tobacco use at time of conversion and exacerbation frequency, although the coefficient showed a negative correlation of -0.387. In the 6 months prior to the transition, there were 17 prescriptions for systemic corticosteroids and 24 for antibiotics to treat COPD exacerbations. Following the transition, there were only 12 prescriptions for systemic corticosteroids and 23 for antibiotics. Fifty-two patients had an active prescription for a fluticasone/salmeterol inhaler at the time of the data review (November to December 2022); of the 48 patients who did not, 10 were no longer active due to patient death between the study period and data retrieval.
Discussion
Patients who transitioned from budesonide/formoterol to fluticasone/salmeterol inhalers did not show a significant difference in clinical COPD outcomes. While the total number of exacerbations increased after switching to the fluticasone/salmeterol inhaler, fewer patients had exacerbations during fluticasone/salmeterol therapy when compared with budesonide/fluticasone therapy. The number of patients receiving systemic corticosteroids and antibiotics to treat exacerbations before and after the transition were similar.
The frequency of treatment failures and AEs to the fluticasone/salmeterol inhaler could be due to the change of the inhaler delivery systems. Budesonide/formoterol is a metered dose inhaler (MDI). It is equipped with a pressurized canister that allows a spacer to be used to maximize benefit. Spacers can assist in preventing oral candidiasis by reducing the amount of medication that touches the back of the throat. Spacers are an option for patients, but not all use them for their MDIs, which can result in a less effective administered dose. Fluticasone/salmeterol is a dry powder inhaler, which requires a deep, fast breath to maximize the benefit, and spacers cannot be used with them. MDIs have been shown to be responsible for a negative impact on climate change, which can be reduced by switching to a dry powder inhaler.7
Tobacco cessation is very important in limiting the progression of COPD. As shown with the negative coefficient correlation, not being an active tobacco user at the time of transition correlated (although not significantly) with less frequent exacerbations. When comparing this study to similar research, such as the PATHOS study, several differences are observed.5 The PATHOS study compared long term treatment (> 1 year) of budesonide/formoterol or fluticasone/salmeterol, a longer period than this study. It regarded similar outcomes for the definition of an exacerbation, such as antibiotic/steroid use or hospital admission. While the current study showed no significant difference between the 2 inhalers and their effect on exacerbations, the PATHOS study found that those treated with a budesonide/formoterol inhaler were less likely to experience COPD-related exacerbations than those treated with the fluticasone/salmeterol inhaler. The PATHOS study had a larger mainly Scandinavian sample (N = 5500). This population could exhibit baseline differences from a study of US veterans.5 A similar Canadian matched cohort study of 2262 patients compared the 2 inhalers to assess their relative effectiveness. It found that COPD exacerbations did not differ between the 2 groups, but the budesonide/formoterol group was significantly less likely to have an emergency department visit compared to the fluticasone salmeterol group.8 Like the PATHOS study, the Canadian study had a larger sample size and longer timeframe than did our study.
Limitations
There are various limitations to this study. It was a retrospective, single-center study and the patient population was relatively homogenous, with only 1 female and a mean age of 71 years. As a study conducted in a veteran population in West Virginia, the findings may not be representative of the general population with COPD, which includes more women and more racial diversity.9 The American Lung Association discusses how environmental exposures to hazardous conditions increase the risks of pulmonary diseases for veterans.10 It has been reported that the prevalence of COPD is higher among veterans compared to the general population, but it is not different in terms of disease manifestation.10
Another limitation is the short time frame. Clinical guidelines, including the GOLD Report, typically track the number of exacerbations for 1 year to escalate therapy.3 Six months was a relatively short time frame, and it is possible that more exacerbations may have occurred beyond the study time frame. Ten patients in the sample died between the end of the study period and data retrieval, which might have been caught by a longer study period. An additional limitation was the inability to measure adherence. As this was a formulary conversion, many patients had been mailed a 30- or 90-day prescription of the budesonide/formoterol inhaler when transitioned to the fluticasone/salmeterol inhaler. There was no way to accurately determine when the patient made the switch to the fluticasone/salmeterol inhaler. This study also had a small sample group (a pre-post analysis of the same group), a limitation when evaluating the impact of this formulary change on a small percentage of the population transitioned.
This formulary conversion occurred during the COVID-19 pandemic, and some exacerbations could have been the result of a misdiagnosed COVID-19 infection. Respiratory infections, including COVID-19, are common causes of exacerbations. It is also possible that some patients elected not to receive medical care for symptoms of an exacerbation during the pandemic.11
Conclusions
Switching from the budesonide/formoterol inhaler to the fluticasone/salmeterol inhaler through formulary conversion did not have a significant impact on the clinical outcomes in patients with COPD. This study found that although the inhalers contain different active ingredients, products within the same therapeutic class yielded nonsignificant changes. When conducting formulary conversions, intolerances and treatment failures should be expected when switching from different inhaler delivery systems. This study further justifies the ability to be cost effective by making formulary conversions within the same therapeutic class within a veterans population.
Acknowledgments
The authors would like to acknowledge James Brown, PharmD, PhD.
1. US Department of Veterans Affairs. VA/DOD Clinical Practice Guideline. Management of Outpatient Chronic Obstructive Pulmonary Disease. 2021. Accessed January 22, 2024. https://www.healthquality.va.gov/guidelines/cd/copd/
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD Report. 2022. Accessed January 22, 2024. https://goldcopd.org/2022-gold-reports/
3. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis management, and prevention of chronic obstructive pulmonary disease 2023 report. Accessed January 26, 2024. https://goldcopd.org/wp-content/uploads/2023/03/GOLD-2023-ver-1.3-17Feb2023_WMV.pdf
4. Oshagbemi OA, Odiba JO, Daniel A, Yunusa I. Absolute blood eosinophil counts to guide inhaled corticosteroids therapy among patients with COPD: systematic review and meta-analysis. Curr Drug Targets. 2019;20(16):1670-1679. doi:10.2174/1389450120666190808141625
5. Larsson K, Janson C, Lisspers K, et al. Combination of budesonide/formoterol more effective than fluticasone/salmeterol in preventing exacerbations in chronic obstructive pulmonary disease: the PATHOS study. J Intern Med. 2013;273(6):584-594. doi:10.1111/joim.12067
6. West Virginia Department of Health and Human Resources, Division of Health Promotion and Chronic Disease. Statistics about the population of West Virginia. 2018. Accessed January 22, 2024. https://dhhr.wv.gov/hpcd/data_reports/ Pages/Fast-Facts.aspx
7. Fidler L, Green S, Wintemute K. Pressurized metered-dose inhalers and their impact on climate change. CMAJ. 2022;194(12):E460. doi:10.1503/cmaj.211747
8. Blais L, Forget A, Ramachandran S. Relative effectiveness of budesonide/formoterol and fluticasone propionate/salmeterol in a 1-year, population-based, matched cohort study of patients with chronic obstructive pulmonary disease (COPD): Effect on COPD-related exacerbations, emergency department visits and hospitalizations, medication utilization, and treatment adherence. Clin Ther. 2010;32(7):1320-1328. doi:10.1016/j.clinthera.2010.06.022
9. Wheaton AG, Cunningham TJ, Ford ES, Croft JB; Centers for Disease Control and Prevention (CDC). Employment and activity limitations among adults with chronic obstructive pulmonary disease — United States, 2013. MMWR Morb Mortal Wkly Rep. 2015:64(11):289-295.
10. Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269-1283. doi:10.2147/COPD.S339323
11. Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250-1257. doi:10.15585/mmwr.mm6936a4
1. US Department of Veterans Affairs. VA/DOD Clinical Practice Guideline. Management of Outpatient Chronic Obstructive Pulmonary Disease. 2021. Accessed January 22, 2024. https://www.healthquality.va.gov/guidelines/cd/copd/
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD Report. 2022. Accessed January 22, 2024. https://goldcopd.org/2022-gold-reports/
3. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis management, and prevention of chronic obstructive pulmonary disease 2023 report. Accessed January 26, 2024. https://goldcopd.org/wp-content/uploads/2023/03/GOLD-2023-ver-1.3-17Feb2023_WMV.pdf
4. Oshagbemi OA, Odiba JO, Daniel A, Yunusa I. Absolute blood eosinophil counts to guide inhaled corticosteroids therapy among patients with COPD: systematic review and meta-analysis. Curr Drug Targets. 2019;20(16):1670-1679. doi:10.2174/1389450120666190808141625
5. Larsson K, Janson C, Lisspers K, et al. Combination of budesonide/formoterol more effective than fluticasone/salmeterol in preventing exacerbations in chronic obstructive pulmonary disease: the PATHOS study. J Intern Med. 2013;273(6):584-594. doi:10.1111/joim.12067
6. West Virginia Department of Health and Human Resources, Division of Health Promotion and Chronic Disease. Statistics about the population of West Virginia. 2018. Accessed January 22, 2024. https://dhhr.wv.gov/hpcd/data_reports/ Pages/Fast-Facts.aspx
7. Fidler L, Green S, Wintemute K. Pressurized metered-dose inhalers and their impact on climate change. CMAJ. 2022;194(12):E460. doi:10.1503/cmaj.211747
8. Blais L, Forget A, Ramachandran S. Relative effectiveness of budesonide/formoterol and fluticasone propionate/salmeterol in a 1-year, population-based, matched cohort study of patients with chronic obstructive pulmonary disease (COPD): Effect on COPD-related exacerbations, emergency department visits and hospitalizations, medication utilization, and treatment adherence. Clin Ther. 2010;32(7):1320-1328. doi:10.1016/j.clinthera.2010.06.022
9. Wheaton AG, Cunningham TJ, Ford ES, Croft JB; Centers for Disease Control and Prevention (CDC). Employment and activity limitations among adults with chronic obstructive pulmonary disease — United States, 2013. MMWR Morb Mortal Wkly Rep. 2015:64(11):289-295.
10. Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269-1283. doi:10.2147/COPD.S339323
11. Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250-1257. doi:10.15585/mmwr.mm6936a4
Diabetes Basic Training Program: Empowering Veterans for Wellness
More than 37 million Americans (11.3%) have diabetes mellitus (DM), and 90% to 95% are diagnosed with type 2 DM, including nearly 1 in 4 veterans receiving Veterans Health Administration (VHA) care.1,2 DM is associated with serious negative health outcomes, including cardiovascular disease and subsequent complications as well as significant health care system utilization and cost.1,3
Group interventions have been identified as a possible method of improving DM outcomes. For example, shared medical appointments (SMAs) have been identified by the VHA as holding promise for improving care and efficiency for DM and other common health conditions.4 Although the precise structure and SMA process for managing DM has been noted to be heterogeneous, the appointment is typically led by an interdisciplinary health care team and includes individualized assessment including medication review and adjustment, group education, and troubleshooting challenges with management in a group format.5 Research suggests that DM SMAs are a worthwhile treatment approach.5 Several studies have found that SMAs were associated with decreased hemoglobin A1c (Hb A1c) levels and improvement in overall disease complications and severity.6
The high degree of SMA heterogeneity and lack of detailed description of structure and process of SMAs studied has made meta-analysis and other synthesis of the literature difficult.5 Consequently, there is inadequate empirically supported guidance for clinicians and health care organizations on how to best implement SMAs and similar group-based treatments. Edelman and colleagues recommended that future research should focus on more consistent and standardized intervention structures and real-world patient- and staff-centered outcomes to address gaps in the literature.5 They noted that a mental health professional was utilized in only a minority of SMAs studied.5 Additionally, we noted a paucity of studies examining patient satisfaction with SMAs.
Another group-based intervention found to be effective in improving DM outcomes is the 6-session Stanford Diabetes Self-Management Program (DSMP), a workshop led in part by trained peers with DM. The sessions focus on educating patients on DM care and self-management tools. The workshop encourages active practice in building DM self-management skills and confidence. DSMP participation has been associated with improvement in DM-related outcomes, including Hb A1c levels, amount of exercise, and medication adherence.7
While SMAs and DSMP have been shown to enhance clinical outcomes, they provide differing types of patient support. SMAs allow for frequent interaction with a health care professional (HCP) and less emphasis on behavioral health interventions. DSMPs include behavioral health professionals and peer leaders and emphasize higher levels of psychosocial support, but do not offer access to clinicians. It is possible that combining these interventions could result in better outcomes than what either could provide on their own.
In 2018, the Cincinnati Veterans Affairs Medical Center (VAMC) in Ohio offered Diabetes Basic Training, a structured DM intervention. Patients enrolled in the program participated in a 9-week intervention that included 3 SMAs and 6 DSMP sessions. During the SMAs, a clinical psychologist or psychology postdoctoral fellow skilled in motivational interviewing facilitated the group to enhance patient engagement and empowerment for improved self-management. In addition, patients participated in structured DSMP groups with an emphasis on action-planning, often surrounding nutrition, physical activity, and other health behavior change information reviewed during the SMAs.
Design and Referral
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture
Observations
All measures were collected as part of traditional clinical care, and we present initial program evaluation data to demonstrate potential effectiveness of the clinic model. Paired samples t tests were used to examine differences between baseline and follow-up measures for the 24 veteran participants. The age of participants who completed the program ranged from 42 to 74 years (mean, 68 years); 29% of participants were Black veterans and 12% were female. Examination of clinical outcomes indicated that veterans reported significant increases in activation levels for managing their health increasing from a baseline mean (SD) 62.1 (12.3) to 68.4 (14.5) at follow up (t[23] = 2.15, P = .04). Hb A1c levels trended downward from a mean (SD) 8.6% (1.3) at baseline to 8.2% (1.2) at 90-day follow up (t[21] 1.05, P = .30). Similar nonsignificant trends in PAID scores were seen for pre- and postprogram reductions in emotional distress related to having DM from a mean (SD) 7.9 (5.0) at baseline to 6.3 (5.1) (t[18] = 11.51, P = .15), and enhanced self-management of glucose with a mean (SD) 6.5 (1.5) at baseline to 6.8 (1.3) at follow up (t[19] = 0.52, P = .61). The trends found in this study show promising outcomes for this pilot group-based DM treatment, though the small sample size (N = 24) limits statistical power. These findings support further exploration and expansion of interdisciplinary health programs supporting veteran self-management.
Discussion
DM is a condition of epidemic proportions that causes substantial negative health outcomes and costs at a national level. Current standards of DM care do not appear to be reversing these trends. Wider implementation of group-based treatment for DM could improve efficiency of care, increase access to quality care, and reduce burden on individual HCPs.
The VHA continues the transformation of its care system, which shifts toward a patient-centered, proactive focus on veteran well-being. This new whole health approach integrates conventional medical treatment with veteran self-empowerment in the pursuit of health goals based on individual veteran’s identified values.19 This approach emphasizes peer-led explorations of veterans’ aspirations, purpose, and individual mission, personalized health planning, and use of whole health coaches and well-being programs, with both allopathic and complementary and integrative clinical care centered around veterans’ identified goals and priorities.20
Including a program like Diabetes Basic Training as a part of whole health programming could offer several benefits. Diabetes Basic Training is unique in its integration of more traditional SMA structure with psychosocial interventions including values identification and motivational interviewing strategies to enhance patient engagement. Veterans can learn from each other’s experiences and concerns, leading to better DM management knowledge and skills. The group nature of the sessions enhances opportunities for emotional support and reduced isolation, as well as peer accountability for maintaining medication adherence.
By meeting with HCPs from multiple disciplines, veterans are exposed to different perspectives on self-management techniques, including behavioral approaches for overcoming barriers to behavior change. Clinicians have more time to engage with patients, building stronger relationships and trust. SMAs are cost-efficient and time efficient, allowing HCPs to see multiple patients at once, reducing wait times and increasing the number of patients treated in a given time frame.
The COVID-19 pandemic temporarily impacted the ongoing expansion of the program, when so many services were shifted from in-person to virtual classes. Due to staffing and other logistic issues, our pilot program was suspended during that time, but plans to resume the program by early 2024 are moving forward.
CONCLUSIONS
The Diabetes Basic Training program serves as a successful model for implementation within a VAMC. Although the number of veterans with complete data available for analysis was small, the trends exhibited in the preliminary outcome data are promising. We encourage other VAMCs to replicate this program with a larger participant base and evaluate its impact on veteran health outcomes. Next steps include comparing the clinical data from treatment as usual with outcomes from DM group participants. As the program resumes, we will reinitiate recruitment efforts to increase HCP referrals to this program.
1. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Statistics. Updated February 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics
2. US Department of Veterans Affairs, Office of Research and Development. VA research on diabetes. www.research.va.gov. Updated January 15, 2023. Accessed January 22, 2024. https://www.research.va.gov/topics/diabetes.cfm
3. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
4. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient and provider expertise to strengthen care management. Updated December 2010. Accessed January 22, 2024. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=1513366&FileName=VA244-14-R-0025-011.pdf
5. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW Jr. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med. 2015;30(1):99-106. doi:10.1007/s11606-014-2978-7
6. Watts SA, Strauss GJ, Pascuzzi K, et al. Shared medical appointments for patients with diabetes: glycemic reduction in high-risk patients. J Am Assoc Nurse Pract. 2015;27(8):450-456. doi:10.1002/2327-6924.12200
7. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. Published 2016 Jun 24. doi:10.2196/jmir.5568
8. Gilstrap LG, Chernew ME, Nguyen CA, et al. Association between clinical practice group adherence to quality measures and adverse outcomes among adult patients with diabetes. JAMA Netw Open. 2019;2(8):e199139. Published 2019 Aug 2. doi:10.1001/jamanetworkopen.2019.9139
9. Venkataraman K, Tan LS, Bautista DC, et al. Psychometric properties of the Problem Areas in Diabetes (PAID) instrument in Singapore. PLoS One. 2015;10(9):e0136759. Published 2015 Sep 3. doi:10.1371/journal.pone.0136759
10. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69-72. doi:10.1046/j.1464-5491.2003.00832.x
11. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. doi:10.1111/j.1475-6773.2005.00438.x
12. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005-1026. doi:10.1111/j.1475-6773.2004.00269.x
13. Ahn YH, Yi CH, Ham OK, Kim BJ. Psychometric properties of the Korean version of the “Patient Activation Measure 13” (PAM13-K) in patients with osteoarthritis. Eval Health Prof. 2015;38(2):255-264. doi:10.1177/0163278714540915
14. Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8(9):e74786. Published 2013 Sep 30. doi:10.1371/journal.pone.0074786
15. Zill JM, Dwinger S, Kriston L, Rohenkohl A, Härter M, Dirmaier J. Psychometric evaluation of the German version of the Patient Activation Measure (PAM13). BMC Public Health. 2013;13:1027. Published 2013 Oct 30. doi:10.1186/1471-2458-13-1027
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes. 2013;11:138. Published 2013 Aug 13. doi:10.1186/1477-7525-11-138
17. Schmitt A, Reimer A, Hermanns N, et al. assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. Published 2016 Mar 3. doi:10.1371/journal.pone.0150774
18. Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DSMQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. Published 2017 Oct 12. doi:10.1186/s12955-017-0776-8
19. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12 Suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
20. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans Affairs to a whole health system of care: time for action and research. Med Care. 2020;58(4):295-300. doi:10.1097/MLR.0000000000001316
More than 37 million Americans (11.3%) have diabetes mellitus (DM), and 90% to 95% are diagnosed with type 2 DM, including nearly 1 in 4 veterans receiving Veterans Health Administration (VHA) care.1,2 DM is associated with serious negative health outcomes, including cardiovascular disease and subsequent complications as well as significant health care system utilization and cost.1,3
Group interventions have been identified as a possible method of improving DM outcomes. For example, shared medical appointments (SMAs) have been identified by the VHA as holding promise for improving care and efficiency for DM and other common health conditions.4 Although the precise structure and SMA process for managing DM has been noted to be heterogeneous, the appointment is typically led by an interdisciplinary health care team and includes individualized assessment including medication review and adjustment, group education, and troubleshooting challenges with management in a group format.5 Research suggests that DM SMAs are a worthwhile treatment approach.5 Several studies have found that SMAs were associated with decreased hemoglobin A1c (Hb A1c) levels and improvement in overall disease complications and severity.6
The high degree of SMA heterogeneity and lack of detailed description of structure and process of SMAs studied has made meta-analysis and other synthesis of the literature difficult.5 Consequently, there is inadequate empirically supported guidance for clinicians and health care organizations on how to best implement SMAs and similar group-based treatments. Edelman and colleagues recommended that future research should focus on more consistent and standardized intervention structures and real-world patient- and staff-centered outcomes to address gaps in the literature.5 They noted that a mental health professional was utilized in only a minority of SMAs studied.5 Additionally, we noted a paucity of studies examining patient satisfaction with SMAs.
Another group-based intervention found to be effective in improving DM outcomes is the 6-session Stanford Diabetes Self-Management Program (DSMP), a workshop led in part by trained peers with DM. The sessions focus on educating patients on DM care and self-management tools. The workshop encourages active practice in building DM self-management skills and confidence. DSMP participation has been associated with improvement in DM-related outcomes, including Hb A1c levels, amount of exercise, and medication adherence.7
While SMAs and DSMP have been shown to enhance clinical outcomes, they provide differing types of patient support. SMAs allow for frequent interaction with a health care professional (HCP) and less emphasis on behavioral health interventions. DSMPs include behavioral health professionals and peer leaders and emphasize higher levels of psychosocial support, but do not offer access to clinicians. It is possible that combining these interventions could result in better outcomes than what either could provide on their own.
In 2018, the Cincinnati Veterans Affairs Medical Center (VAMC) in Ohio offered Diabetes Basic Training, a structured DM intervention. Patients enrolled in the program participated in a 9-week intervention that included 3 SMAs and 6 DSMP sessions. During the SMAs, a clinical psychologist or psychology postdoctoral fellow skilled in motivational interviewing facilitated the group to enhance patient engagement and empowerment for improved self-management. In addition, patients participated in structured DSMP groups with an emphasis on action-planning, often surrounding nutrition, physical activity, and other health behavior change information reviewed during the SMAs.
Design and Referral
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture
Observations
All measures were collected as part of traditional clinical care, and we present initial program evaluation data to demonstrate potential effectiveness of the clinic model. Paired samples t tests were used to examine differences between baseline and follow-up measures for the 24 veteran participants. The age of participants who completed the program ranged from 42 to 74 years (mean, 68 years); 29% of participants were Black veterans and 12% were female. Examination of clinical outcomes indicated that veterans reported significant increases in activation levels for managing their health increasing from a baseline mean (SD) 62.1 (12.3) to 68.4 (14.5) at follow up (t[23] = 2.15, P = .04). Hb A1c levels trended downward from a mean (SD) 8.6% (1.3) at baseline to 8.2% (1.2) at 90-day follow up (t[21] 1.05, P = .30). Similar nonsignificant trends in PAID scores were seen for pre- and postprogram reductions in emotional distress related to having DM from a mean (SD) 7.9 (5.0) at baseline to 6.3 (5.1) (t[18] = 11.51, P = .15), and enhanced self-management of glucose with a mean (SD) 6.5 (1.5) at baseline to 6.8 (1.3) at follow up (t[19] = 0.52, P = .61). The trends found in this study show promising outcomes for this pilot group-based DM treatment, though the small sample size (N = 24) limits statistical power. These findings support further exploration and expansion of interdisciplinary health programs supporting veteran self-management.
Discussion
DM is a condition of epidemic proportions that causes substantial negative health outcomes and costs at a national level. Current standards of DM care do not appear to be reversing these trends. Wider implementation of group-based treatment for DM could improve efficiency of care, increase access to quality care, and reduce burden on individual HCPs.
The VHA continues the transformation of its care system, which shifts toward a patient-centered, proactive focus on veteran well-being. This new whole health approach integrates conventional medical treatment with veteran self-empowerment in the pursuit of health goals based on individual veteran’s identified values.19 This approach emphasizes peer-led explorations of veterans’ aspirations, purpose, and individual mission, personalized health planning, and use of whole health coaches and well-being programs, with both allopathic and complementary and integrative clinical care centered around veterans’ identified goals and priorities.20
Including a program like Diabetes Basic Training as a part of whole health programming could offer several benefits. Diabetes Basic Training is unique in its integration of more traditional SMA structure with psychosocial interventions including values identification and motivational interviewing strategies to enhance patient engagement. Veterans can learn from each other’s experiences and concerns, leading to better DM management knowledge and skills. The group nature of the sessions enhances opportunities for emotional support and reduced isolation, as well as peer accountability for maintaining medication adherence.
By meeting with HCPs from multiple disciplines, veterans are exposed to different perspectives on self-management techniques, including behavioral approaches for overcoming barriers to behavior change. Clinicians have more time to engage with patients, building stronger relationships and trust. SMAs are cost-efficient and time efficient, allowing HCPs to see multiple patients at once, reducing wait times and increasing the number of patients treated in a given time frame.
The COVID-19 pandemic temporarily impacted the ongoing expansion of the program, when so many services were shifted from in-person to virtual classes. Due to staffing and other logistic issues, our pilot program was suspended during that time, but plans to resume the program by early 2024 are moving forward.
CONCLUSIONS
The Diabetes Basic Training program serves as a successful model for implementation within a VAMC. Although the number of veterans with complete data available for analysis was small, the trends exhibited in the preliminary outcome data are promising. We encourage other VAMCs to replicate this program with a larger participant base and evaluate its impact on veteran health outcomes. Next steps include comparing the clinical data from treatment as usual with outcomes from DM group participants. As the program resumes, we will reinitiate recruitment efforts to increase HCP referrals to this program.
More than 37 million Americans (11.3%) have diabetes mellitus (DM), and 90% to 95% are diagnosed with type 2 DM, including nearly 1 in 4 veterans receiving Veterans Health Administration (VHA) care.1,2 DM is associated with serious negative health outcomes, including cardiovascular disease and subsequent complications as well as significant health care system utilization and cost.1,3
Group interventions have been identified as a possible method of improving DM outcomes. For example, shared medical appointments (SMAs) have been identified by the VHA as holding promise for improving care and efficiency for DM and other common health conditions.4 Although the precise structure and SMA process for managing DM has been noted to be heterogeneous, the appointment is typically led by an interdisciplinary health care team and includes individualized assessment including medication review and adjustment, group education, and troubleshooting challenges with management in a group format.5 Research suggests that DM SMAs are a worthwhile treatment approach.5 Several studies have found that SMAs were associated with decreased hemoglobin A1c (Hb A1c) levels and improvement in overall disease complications and severity.6
The high degree of SMA heterogeneity and lack of detailed description of structure and process of SMAs studied has made meta-analysis and other synthesis of the literature difficult.5 Consequently, there is inadequate empirically supported guidance for clinicians and health care organizations on how to best implement SMAs and similar group-based treatments. Edelman and colleagues recommended that future research should focus on more consistent and standardized intervention structures and real-world patient- and staff-centered outcomes to address gaps in the literature.5 They noted that a mental health professional was utilized in only a minority of SMAs studied.5 Additionally, we noted a paucity of studies examining patient satisfaction with SMAs.
Another group-based intervention found to be effective in improving DM outcomes is the 6-session Stanford Diabetes Self-Management Program (DSMP), a workshop led in part by trained peers with DM. The sessions focus on educating patients on DM care and self-management tools. The workshop encourages active practice in building DM self-management skills and confidence. DSMP participation has been associated with improvement in DM-related outcomes, including Hb A1c levels, amount of exercise, and medication adherence.7
While SMAs and DSMP have been shown to enhance clinical outcomes, they provide differing types of patient support. SMAs allow for frequent interaction with a health care professional (HCP) and less emphasis on behavioral health interventions. DSMPs include behavioral health professionals and peer leaders and emphasize higher levels of psychosocial support, but do not offer access to clinicians. It is possible that combining these interventions could result in better outcomes than what either could provide on their own.
In 2018, the Cincinnati Veterans Affairs Medical Center (VAMC) in Ohio offered Diabetes Basic Training, a structured DM intervention. Patients enrolled in the program participated in a 9-week intervention that included 3 SMAs and 6 DSMP sessions. During the SMAs, a clinical psychologist or psychology postdoctoral fellow skilled in motivational interviewing facilitated the group to enhance patient engagement and empowerment for improved self-management. In addition, patients participated in structured DSMP groups with an emphasis on action-planning, often surrounding nutrition, physical activity, and other health behavior change information reviewed during the SMAs.
Design and Referral
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture
Observations
All measures were collected as part of traditional clinical care, and we present initial program evaluation data to demonstrate potential effectiveness of the clinic model. Paired samples t tests were used to examine differences between baseline and follow-up measures for the 24 veteran participants. The age of participants who completed the program ranged from 42 to 74 years (mean, 68 years); 29% of participants were Black veterans and 12% were female. Examination of clinical outcomes indicated that veterans reported significant increases in activation levels for managing their health increasing from a baseline mean (SD) 62.1 (12.3) to 68.4 (14.5) at follow up (t[23] = 2.15, P = .04). Hb A1c levels trended downward from a mean (SD) 8.6% (1.3) at baseline to 8.2% (1.2) at 90-day follow up (t[21] 1.05, P = .30). Similar nonsignificant trends in PAID scores were seen for pre- and postprogram reductions in emotional distress related to having DM from a mean (SD) 7.9 (5.0) at baseline to 6.3 (5.1) (t[18] = 11.51, P = .15), and enhanced self-management of glucose with a mean (SD) 6.5 (1.5) at baseline to 6.8 (1.3) at follow up (t[19] = 0.52, P = .61). The trends found in this study show promising outcomes for this pilot group-based DM treatment, though the small sample size (N = 24) limits statistical power. These findings support further exploration and expansion of interdisciplinary health programs supporting veteran self-management.
Discussion
DM is a condition of epidemic proportions that causes substantial negative health outcomes and costs at a national level. Current standards of DM care do not appear to be reversing these trends. Wider implementation of group-based treatment for DM could improve efficiency of care, increase access to quality care, and reduce burden on individual HCPs.
The VHA continues the transformation of its care system, which shifts toward a patient-centered, proactive focus on veteran well-being. This new whole health approach integrates conventional medical treatment with veteran self-empowerment in the pursuit of health goals based on individual veteran’s identified values.19 This approach emphasizes peer-led explorations of veterans’ aspirations, purpose, and individual mission, personalized health planning, and use of whole health coaches and well-being programs, with both allopathic and complementary and integrative clinical care centered around veterans’ identified goals and priorities.20
Including a program like Diabetes Basic Training as a part of whole health programming could offer several benefits. Diabetes Basic Training is unique in its integration of more traditional SMA structure with psychosocial interventions including values identification and motivational interviewing strategies to enhance patient engagement. Veterans can learn from each other’s experiences and concerns, leading to better DM management knowledge and skills. The group nature of the sessions enhances opportunities for emotional support and reduced isolation, as well as peer accountability for maintaining medication adherence.
By meeting with HCPs from multiple disciplines, veterans are exposed to different perspectives on self-management techniques, including behavioral approaches for overcoming barriers to behavior change. Clinicians have more time to engage with patients, building stronger relationships and trust. SMAs are cost-efficient and time efficient, allowing HCPs to see multiple patients at once, reducing wait times and increasing the number of patients treated in a given time frame.
The COVID-19 pandemic temporarily impacted the ongoing expansion of the program, when so many services were shifted from in-person to virtual classes. Due to staffing and other logistic issues, our pilot program was suspended during that time, but plans to resume the program by early 2024 are moving forward.
CONCLUSIONS
The Diabetes Basic Training program serves as a successful model for implementation within a VAMC. Although the number of veterans with complete data available for analysis was small, the trends exhibited in the preliminary outcome data are promising. We encourage other VAMCs to replicate this program with a larger participant base and evaluate its impact on veteran health outcomes. Next steps include comparing the clinical data from treatment as usual with outcomes from DM group participants. As the program resumes, we will reinitiate recruitment efforts to increase HCP referrals to this program.
1. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Statistics. Updated February 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics
2. US Department of Veterans Affairs, Office of Research and Development. VA research on diabetes. www.research.va.gov. Updated January 15, 2023. Accessed January 22, 2024. https://www.research.va.gov/topics/diabetes.cfm
3. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
4. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient and provider expertise to strengthen care management. Updated December 2010. Accessed January 22, 2024. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=1513366&FileName=VA244-14-R-0025-011.pdf
5. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW Jr. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med. 2015;30(1):99-106. doi:10.1007/s11606-014-2978-7
6. Watts SA, Strauss GJ, Pascuzzi K, et al. Shared medical appointments for patients with diabetes: glycemic reduction in high-risk patients. J Am Assoc Nurse Pract. 2015;27(8):450-456. doi:10.1002/2327-6924.12200
7. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. Published 2016 Jun 24. doi:10.2196/jmir.5568
8. Gilstrap LG, Chernew ME, Nguyen CA, et al. Association between clinical practice group adherence to quality measures and adverse outcomes among adult patients with diabetes. JAMA Netw Open. 2019;2(8):e199139. Published 2019 Aug 2. doi:10.1001/jamanetworkopen.2019.9139
9. Venkataraman K, Tan LS, Bautista DC, et al. Psychometric properties of the Problem Areas in Diabetes (PAID) instrument in Singapore. PLoS One. 2015;10(9):e0136759. Published 2015 Sep 3. doi:10.1371/journal.pone.0136759
10. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69-72. doi:10.1046/j.1464-5491.2003.00832.x
11. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. doi:10.1111/j.1475-6773.2005.00438.x
12. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005-1026. doi:10.1111/j.1475-6773.2004.00269.x
13. Ahn YH, Yi CH, Ham OK, Kim BJ. Psychometric properties of the Korean version of the “Patient Activation Measure 13” (PAM13-K) in patients with osteoarthritis. Eval Health Prof. 2015;38(2):255-264. doi:10.1177/0163278714540915
14. Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8(9):e74786. Published 2013 Sep 30. doi:10.1371/journal.pone.0074786
15. Zill JM, Dwinger S, Kriston L, Rohenkohl A, Härter M, Dirmaier J. Psychometric evaluation of the German version of the Patient Activation Measure (PAM13). BMC Public Health. 2013;13:1027. Published 2013 Oct 30. doi:10.1186/1471-2458-13-1027
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes. 2013;11:138. Published 2013 Aug 13. doi:10.1186/1477-7525-11-138
17. Schmitt A, Reimer A, Hermanns N, et al. assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. Published 2016 Mar 3. doi:10.1371/journal.pone.0150774
18. Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DSMQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. Published 2017 Oct 12. doi:10.1186/s12955-017-0776-8
19. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12 Suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
20. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans Affairs to a whole health system of care: time for action and research. Med Care. 2020;58(4):295-300. doi:10.1097/MLR.0000000000001316
1. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Statistics. Updated February 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics
2. US Department of Veterans Affairs, Office of Research and Development. VA research on diabetes. www.research.va.gov. Updated January 15, 2023. Accessed January 22, 2024. https://www.research.va.gov/topics/diabetes.cfm
3. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
4. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient and provider expertise to strengthen care management. Updated December 2010. Accessed January 22, 2024. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=1513366&FileName=VA244-14-R-0025-011.pdf
5. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW Jr. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med. 2015;30(1):99-106. doi:10.1007/s11606-014-2978-7
6. Watts SA, Strauss GJ, Pascuzzi K, et al. Shared medical appointments for patients with diabetes: glycemic reduction in high-risk patients. J Am Assoc Nurse Pract. 2015;27(8):450-456. doi:10.1002/2327-6924.12200
7. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. Published 2016 Jun 24. doi:10.2196/jmir.5568
8. Gilstrap LG, Chernew ME, Nguyen CA, et al. Association between clinical practice group adherence to quality measures and adverse outcomes among adult patients with diabetes. JAMA Netw Open. 2019;2(8):e199139. Published 2019 Aug 2. doi:10.1001/jamanetworkopen.2019.9139
9. Venkataraman K, Tan LS, Bautista DC, et al. Psychometric properties of the Problem Areas in Diabetes (PAID) instrument in Singapore. PLoS One. 2015;10(9):e0136759. Published 2015 Sep 3. doi:10.1371/journal.pone.0136759
10. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69-72. doi:10.1046/j.1464-5491.2003.00832.x
11. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. doi:10.1111/j.1475-6773.2005.00438.x
12. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005-1026. doi:10.1111/j.1475-6773.2004.00269.x
13. Ahn YH, Yi CH, Ham OK, Kim BJ. Psychometric properties of the Korean version of the “Patient Activation Measure 13” (PAM13-K) in patients with osteoarthritis. Eval Health Prof. 2015;38(2):255-264. doi:10.1177/0163278714540915
14. Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8(9):e74786. Published 2013 Sep 30. doi:10.1371/journal.pone.0074786
15. Zill JM, Dwinger S, Kriston L, Rohenkohl A, Härter M, Dirmaier J. Psychometric evaluation of the German version of the Patient Activation Measure (PAM13). BMC Public Health. 2013;13:1027. Published 2013 Oct 30. doi:10.1186/1471-2458-13-1027
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes. 2013;11:138. Published 2013 Aug 13. doi:10.1186/1477-7525-11-138
17. Schmitt A, Reimer A, Hermanns N, et al. assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. Published 2016 Mar 3. doi:10.1371/journal.pone.0150774
18. Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DSMQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. Published 2017 Oct 12. doi:10.1186/s12955-017-0776-8
19. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12 Suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
20. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans Affairs to a whole health system of care: time for action and research. Med Care. 2020;58(4):295-300. doi:10.1097/MLR.0000000000001316
Fighting to Serve: Women in Military Medicine
Let the generations know that women in uniform also guaranteed their freedom.
Mary Walker, MD
Hoping to make a career in nursing, my mother, a newly graduated registered nurse, enlisted in the US Army Nurse Corps shortly after the United States entered World War II. When she married my father, a US Army doctor, in 1942, she was summarily discharged (the Army Nurse Corp changed its policy and permitted married nurses to serve later that year), while my father went on to decades of distinguished service in military medicine.1 My mother always regretted being unable to advance through the ranks of the US Army as other woman nurses did in her training class.
March is Women’s History Month. My personal narrative of discrimination against women in military medicine is a footnote in a long volume of inequitable treatment. This column will examine a few of the most famous—or rather from a justice perspective, infamous—chapters in that story to illustrate how for centuries women heroically fought for the right to serve.
A theme of the early epochs of the American military is that women were forced to come to the difficult realization that the only way to serve was to conceal their identity. In 1776, Margaret Cochran Corbin felt called as her husband did to defend the new nation. She dressed as a man and joined him at the ramparts, helping load his cannon until he was killed, and took over firing at the enemy. Even after being shot, she remained in the ranks, entering the Invalid Regiment at West Point, New York, dedicated to caring for other injured soldiers. As recognition of her exemplary service and battlefield injury Corbin became the first US woman to receive a military pension. The Veterans Affairs New York Harbor Healthcare System Manhattan campus is named in her honor.2
The hypocrisy of the military’s gender politics was nowhere more evident than in the case of Mary Walker, MD, and the Congressional Medal of Honor. Walker graduated from Syracuse Medical College in 1855. At the beginning of the Civil War, Walker’s request to enlist as a surgeon was refused on the grounds of her gender. She declined to be a nurse, and instead volunteered for the Army where she cared for the wounded in various hospitals. Her medical degree was accepted in 1863, enabling her to become a paid surgical officer in the War Department, including 4 months as a prisoner of war.
An early and avid feminist, Walker wore men’s clothing and when she was arrested on the charge of impersonating a male, declared the government had given her permission to dress as a man to facilitate her surgical work. Walker separated from the military in 1865 and President Andrew Johnson awarded her the Congressional Medal of Honor that year. After Walker’s death in 1917, the Medal of Honor was rescinded on the grounds that she had never actually been commissioned and the medal could not be awarded to a civilian. It took 60 years of lobbying before President Jimmy Carter restored her award in 1977.3 That millions of women have served in the military since the Civil War, and Walker remains the only woman among the 3517 service members to have won the nation’s highest military honor, underscores the ongoing injustice.4
February commemorated Black History Month and a second theme that emerges from the study of the history of women in military medicine is intersectionality: How race, gender, sexual orientation, and other identities overlap and interact to generate distinctive forms of discrimination. Ethicists have applied the concept of intersectionality to health care and there are a plethora of examples in military medicine.5 Despite a dire need for nurses in the first and second world wars, and a track record of their exemplary service in prior conflicts, the government repeatedly set up arbitrary obstacles barring highly-qualified Black nurses from enlisting.6 Technically allowed to join the Army Nurse Corps in 1941, Black nurses confronted bureaucratic barriers that restricted them to only caring for Black servicemen and prisoners of war, and racial quotas that resulted in 500 Black nurses vs 59,000 White nurses that served during World War II. Black nurses and their supporters in government and society persisted, and once in uniform, broke through barriers to achieve administrative and clinical excellence.7
My mother’s experience mirrors that of thousands of women whose dreams for a career in military medicine were shattered or who enlisted only to find their aspirations for advancement in the service thwarted. Medical historians remind us that due to bias, much of the book of women healer’s accomplishments remains unwritten, itself a testimony to the pervasive and enduring marginalization of women in Western society. Yet, as this brief glimpse of women in military medicine shows, there is sufficient evidence for us to appreciate their impressive contributions.8
Reflecting on this sketch of women’s struggle for acceptance in military medicine in March 2024, we may presume that the fight for equity has been continuously trending upward.8 President Joseph R. Biden appointed, and even more surprisingly, the US Congress confirmed Rachel Levine, MD, as US Department of Health and Human Services Assistant Under Secretary for Health in 2021, making Levine the highest ranking openly transgender health official in the history of the US government.9 Levine also has the distinction of being the first 4-star admiral in the Commissioned Corps of the US Public Health Service and the only transgender person to achieve this rank in any branch of the US uniformed services.10
However, research suggests that the history of women in the military is far more like an undulating curve. A 2019 study of academic military surgery found evidence of gender disparity even greater than that of the civilian sector.11 True and lasting equity in federal health care practice will require all of us to follow the inspiring examples of so many women known and unknown who fought the military establishment within for the right to heal those wounded fighting the enemy without.
1. Treadwell ME. The Women’s Army Corps. US Army Center of Military History; 1991: Chap 25. Accessed February 20, 2024. https://history.army.mil/books/wwii/Wac/ch25.htm
2. Hayes P. Meet five inspiring women veterans. Published November 10, 2022. Accessed February 20, 2024. https://news.va.gov/110571/meet-five-inspiring-women-veterans/
3. Lange K. Meet Dr. Mary Walker: the only female recipient of the Medical of Honor recipient. Published March 7, 2017. Accessed February 20, 2024. https://www.army.mil/article/183800/meet_dr_mary_walker_the_only_female_medal_of_honor_recipient
4. The National Medal of Honor Museum. Accessed February 20, 2024. https://mohmuseum.org/the-medal
5. Wilson Y, White A, Jefferson A, Danis M. Intersectionality in Clinical Medicine: The Need for a Conceptual Framework. Am J Bioeth. 2019;19(2):8-19. doi:10.1080/15265161.2018.1557275
6. National Women’s History Museum. African American Nurses in World War II. Published July 8, 2019. Accessed February 20, 2024. https://www.womenshistory.org/articles/african-american-nurses-world-war-ii
7. O’Gan P. Smithsonian National Museum of African American History and Culture. Victory at Home and Abroad: African American Army Nurses in World War II. Published May 8, 2023. Accessed February 20, 2024. https://nmaahc.si.edu/explore/stories/nurses-WWII
8. Neve M. Conclusion. In Conrad LI, Neve M, Nutton V, Porter R, and Wear A, eds. The Western Medical Tradition 800 BC to AD 1800. Cambridge University Press; 1995:477-494.
9. Stolberg SG. ‘This is politics’: Dr. Rachel Levine’s rise as transgender issues gain prominence. The New York Times. Updated May 10, 2021. Accessed February 20, 2024. https://www.nytimes.com/2021/05/08/us/politics/rachel-levine-transgender.html
10. Franklin J. Dr. Rachel Levine is sworn in as the nation’s first transgender four-star officer. October 19, 2021. Accessed February 20, 2024. https://www.npr.org/2021/10/19/1047423156/rachel-levine-first-transgender-four-star-officer
11. Herrick-Reynolds K, Brooks D, Wind G, Jackson P, Latham K. Military medicine and the academic surgery gender gap. Mil Med. 2019;184(9-10):383-387. doi:10.1093/milmed/usz083
Let the generations know that women in uniform also guaranteed their freedom.
Mary Walker, MD
Hoping to make a career in nursing, my mother, a newly graduated registered nurse, enlisted in the US Army Nurse Corps shortly after the United States entered World War II. When she married my father, a US Army doctor, in 1942, she was summarily discharged (the Army Nurse Corp changed its policy and permitted married nurses to serve later that year), while my father went on to decades of distinguished service in military medicine.1 My mother always regretted being unable to advance through the ranks of the US Army as other woman nurses did in her training class.
March is Women’s History Month. My personal narrative of discrimination against women in military medicine is a footnote in a long volume of inequitable treatment. This column will examine a few of the most famous—or rather from a justice perspective, infamous—chapters in that story to illustrate how for centuries women heroically fought for the right to serve.
A theme of the early epochs of the American military is that women were forced to come to the difficult realization that the only way to serve was to conceal their identity. In 1776, Margaret Cochran Corbin felt called as her husband did to defend the new nation. She dressed as a man and joined him at the ramparts, helping load his cannon until he was killed, and took over firing at the enemy. Even after being shot, she remained in the ranks, entering the Invalid Regiment at West Point, New York, dedicated to caring for other injured soldiers. As recognition of her exemplary service and battlefield injury Corbin became the first US woman to receive a military pension. The Veterans Affairs New York Harbor Healthcare System Manhattan campus is named in her honor.2
The hypocrisy of the military’s gender politics was nowhere more evident than in the case of Mary Walker, MD, and the Congressional Medal of Honor. Walker graduated from Syracuse Medical College in 1855. At the beginning of the Civil War, Walker’s request to enlist as a surgeon was refused on the grounds of her gender. She declined to be a nurse, and instead volunteered for the Army where she cared for the wounded in various hospitals. Her medical degree was accepted in 1863, enabling her to become a paid surgical officer in the War Department, including 4 months as a prisoner of war.
An early and avid feminist, Walker wore men’s clothing and when she was arrested on the charge of impersonating a male, declared the government had given her permission to dress as a man to facilitate her surgical work. Walker separated from the military in 1865 and President Andrew Johnson awarded her the Congressional Medal of Honor that year. After Walker’s death in 1917, the Medal of Honor was rescinded on the grounds that she had never actually been commissioned and the medal could not be awarded to a civilian. It took 60 years of lobbying before President Jimmy Carter restored her award in 1977.3 That millions of women have served in the military since the Civil War, and Walker remains the only woman among the 3517 service members to have won the nation’s highest military honor, underscores the ongoing injustice.4
February commemorated Black History Month and a second theme that emerges from the study of the history of women in military medicine is intersectionality: How race, gender, sexual orientation, and other identities overlap and interact to generate distinctive forms of discrimination. Ethicists have applied the concept of intersectionality to health care and there are a plethora of examples in military medicine.5 Despite a dire need for nurses in the first and second world wars, and a track record of their exemplary service in prior conflicts, the government repeatedly set up arbitrary obstacles barring highly-qualified Black nurses from enlisting.6 Technically allowed to join the Army Nurse Corps in 1941, Black nurses confronted bureaucratic barriers that restricted them to only caring for Black servicemen and prisoners of war, and racial quotas that resulted in 500 Black nurses vs 59,000 White nurses that served during World War II. Black nurses and their supporters in government and society persisted, and once in uniform, broke through barriers to achieve administrative and clinical excellence.7
My mother’s experience mirrors that of thousands of women whose dreams for a career in military medicine were shattered or who enlisted only to find their aspirations for advancement in the service thwarted. Medical historians remind us that due to bias, much of the book of women healer’s accomplishments remains unwritten, itself a testimony to the pervasive and enduring marginalization of women in Western society. Yet, as this brief glimpse of women in military medicine shows, there is sufficient evidence for us to appreciate their impressive contributions.8
Reflecting on this sketch of women’s struggle for acceptance in military medicine in March 2024, we may presume that the fight for equity has been continuously trending upward.8 President Joseph R. Biden appointed, and even more surprisingly, the US Congress confirmed Rachel Levine, MD, as US Department of Health and Human Services Assistant Under Secretary for Health in 2021, making Levine the highest ranking openly transgender health official in the history of the US government.9 Levine also has the distinction of being the first 4-star admiral in the Commissioned Corps of the US Public Health Service and the only transgender person to achieve this rank in any branch of the US uniformed services.10
However, research suggests that the history of women in the military is far more like an undulating curve. A 2019 study of academic military surgery found evidence of gender disparity even greater than that of the civilian sector.11 True and lasting equity in federal health care practice will require all of us to follow the inspiring examples of so many women known and unknown who fought the military establishment within for the right to heal those wounded fighting the enemy without.
Let the generations know that women in uniform also guaranteed their freedom.
Mary Walker, MD
Hoping to make a career in nursing, my mother, a newly graduated registered nurse, enlisted in the US Army Nurse Corps shortly after the United States entered World War II. When she married my father, a US Army doctor, in 1942, she was summarily discharged (the Army Nurse Corp changed its policy and permitted married nurses to serve later that year), while my father went on to decades of distinguished service in military medicine.1 My mother always regretted being unable to advance through the ranks of the US Army as other woman nurses did in her training class.
March is Women’s History Month. My personal narrative of discrimination against women in military medicine is a footnote in a long volume of inequitable treatment. This column will examine a few of the most famous—or rather from a justice perspective, infamous—chapters in that story to illustrate how for centuries women heroically fought for the right to serve.
A theme of the early epochs of the American military is that women were forced to come to the difficult realization that the only way to serve was to conceal their identity. In 1776, Margaret Cochran Corbin felt called as her husband did to defend the new nation. She dressed as a man and joined him at the ramparts, helping load his cannon until he was killed, and took over firing at the enemy. Even after being shot, she remained in the ranks, entering the Invalid Regiment at West Point, New York, dedicated to caring for other injured soldiers. As recognition of her exemplary service and battlefield injury Corbin became the first US woman to receive a military pension. The Veterans Affairs New York Harbor Healthcare System Manhattan campus is named in her honor.2
The hypocrisy of the military’s gender politics was nowhere more evident than in the case of Mary Walker, MD, and the Congressional Medal of Honor. Walker graduated from Syracuse Medical College in 1855. At the beginning of the Civil War, Walker’s request to enlist as a surgeon was refused on the grounds of her gender. She declined to be a nurse, and instead volunteered for the Army where she cared for the wounded in various hospitals. Her medical degree was accepted in 1863, enabling her to become a paid surgical officer in the War Department, including 4 months as a prisoner of war.
An early and avid feminist, Walker wore men’s clothing and when she was arrested on the charge of impersonating a male, declared the government had given her permission to dress as a man to facilitate her surgical work. Walker separated from the military in 1865 and President Andrew Johnson awarded her the Congressional Medal of Honor that year. After Walker’s death in 1917, the Medal of Honor was rescinded on the grounds that she had never actually been commissioned and the medal could not be awarded to a civilian. It took 60 years of lobbying before President Jimmy Carter restored her award in 1977.3 That millions of women have served in the military since the Civil War, and Walker remains the only woman among the 3517 service members to have won the nation’s highest military honor, underscores the ongoing injustice.4
February commemorated Black History Month and a second theme that emerges from the study of the history of women in military medicine is intersectionality: How race, gender, sexual orientation, and other identities overlap and interact to generate distinctive forms of discrimination. Ethicists have applied the concept of intersectionality to health care and there are a plethora of examples in military medicine.5 Despite a dire need for nurses in the first and second world wars, and a track record of their exemplary service in prior conflicts, the government repeatedly set up arbitrary obstacles barring highly-qualified Black nurses from enlisting.6 Technically allowed to join the Army Nurse Corps in 1941, Black nurses confronted bureaucratic barriers that restricted them to only caring for Black servicemen and prisoners of war, and racial quotas that resulted in 500 Black nurses vs 59,000 White nurses that served during World War II. Black nurses and their supporters in government and society persisted, and once in uniform, broke through barriers to achieve administrative and clinical excellence.7
My mother’s experience mirrors that of thousands of women whose dreams for a career in military medicine were shattered or who enlisted only to find their aspirations for advancement in the service thwarted. Medical historians remind us that due to bias, much of the book of women healer’s accomplishments remains unwritten, itself a testimony to the pervasive and enduring marginalization of women in Western society. Yet, as this brief glimpse of women in military medicine shows, there is sufficient evidence for us to appreciate their impressive contributions.8
Reflecting on this sketch of women’s struggle for acceptance in military medicine in March 2024, we may presume that the fight for equity has been continuously trending upward.8 President Joseph R. Biden appointed, and even more surprisingly, the US Congress confirmed Rachel Levine, MD, as US Department of Health and Human Services Assistant Under Secretary for Health in 2021, making Levine the highest ranking openly transgender health official in the history of the US government.9 Levine also has the distinction of being the first 4-star admiral in the Commissioned Corps of the US Public Health Service and the only transgender person to achieve this rank in any branch of the US uniformed services.10
However, research suggests that the history of women in the military is far more like an undulating curve. A 2019 study of academic military surgery found evidence of gender disparity even greater than that of the civilian sector.11 True and lasting equity in federal health care practice will require all of us to follow the inspiring examples of so many women known and unknown who fought the military establishment within for the right to heal those wounded fighting the enemy without.
1. Treadwell ME. The Women’s Army Corps. US Army Center of Military History; 1991: Chap 25. Accessed February 20, 2024. https://history.army.mil/books/wwii/Wac/ch25.htm
2. Hayes P. Meet five inspiring women veterans. Published November 10, 2022. Accessed February 20, 2024. https://news.va.gov/110571/meet-five-inspiring-women-veterans/
3. Lange K. Meet Dr. Mary Walker: the only female recipient of the Medical of Honor recipient. Published March 7, 2017. Accessed February 20, 2024. https://www.army.mil/article/183800/meet_dr_mary_walker_the_only_female_medal_of_honor_recipient
4. The National Medal of Honor Museum. Accessed February 20, 2024. https://mohmuseum.org/the-medal
5. Wilson Y, White A, Jefferson A, Danis M. Intersectionality in Clinical Medicine: The Need for a Conceptual Framework. Am J Bioeth. 2019;19(2):8-19. doi:10.1080/15265161.2018.1557275
6. National Women’s History Museum. African American Nurses in World War II. Published July 8, 2019. Accessed February 20, 2024. https://www.womenshistory.org/articles/african-american-nurses-world-war-ii
7. O’Gan P. Smithsonian National Museum of African American History and Culture. Victory at Home and Abroad: African American Army Nurses in World War II. Published May 8, 2023. Accessed February 20, 2024. https://nmaahc.si.edu/explore/stories/nurses-WWII
8. Neve M. Conclusion. In Conrad LI, Neve M, Nutton V, Porter R, and Wear A, eds. The Western Medical Tradition 800 BC to AD 1800. Cambridge University Press; 1995:477-494.
9. Stolberg SG. ‘This is politics’: Dr. Rachel Levine’s rise as transgender issues gain prominence. The New York Times. Updated May 10, 2021. Accessed February 20, 2024. https://www.nytimes.com/2021/05/08/us/politics/rachel-levine-transgender.html
10. Franklin J. Dr. Rachel Levine is sworn in as the nation’s first transgender four-star officer. October 19, 2021. Accessed February 20, 2024. https://www.npr.org/2021/10/19/1047423156/rachel-levine-first-transgender-four-star-officer
11. Herrick-Reynolds K, Brooks D, Wind G, Jackson P, Latham K. Military medicine and the academic surgery gender gap. Mil Med. 2019;184(9-10):383-387. doi:10.1093/milmed/usz083
1. Treadwell ME. The Women’s Army Corps. US Army Center of Military History; 1991: Chap 25. Accessed February 20, 2024. https://history.army.mil/books/wwii/Wac/ch25.htm
2. Hayes P. Meet five inspiring women veterans. Published November 10, 2022. Accessed February 20, 2024. https://news.va.gov/110571/meet-five-inspiring-women-veterans/
3. Lange K. Meet Dr. Mary Walker: the only female recipient of the Medical of Honor recipient. Published March 7, 2017. Accessed February 20, 2024. https://www.army.mil/article/183800/meet_dr_mary_walker_the_only_female_medal_of_honor_recipient
4. The National Medal of Honor Museum. Accessed February 20, 2024. https://mohmuseum.org/the-medal
5. Wilson Y, White A, Jefferson A, Danis M. Intersectionality in Clinical Medicine: The Need for a Conceptual Framework. Am J Bioeth. 2019;19(2):8-19. doi:10.1080/15265161.2018.1557275
6. National Women’s History Museum. African American Nurses in World War II. Published July 8, 2019. Accessed February 20, 2024. https://www.womenshistory.org/articles/african-american-nurses-world-war-ii
7. O’Gan P. Smithsonian National Museum of African American History and Culture. Victory at Home and Abroad: African American Army Nurses in World War II. Published May 8, 2023. Accessed February 20, 2024. https://nmaahc.si.edu/explore/stories/nurses-WWII
8. Neve M. Conclusion. In Conrad LI, Neve M, Nutton V, Porter R, and Wear A, eds. The Western Medical Tradition 800 BC to AD 1800. Cambridge University Press; 1995:477-494.
9. Stolberg SG. ‘This is politics’: Dr. Rachel Levine’s rise as transgender issues gain prominence. The New York Times. Updated May 10, 2021. Accessed February 20, 2024. https://www.nytimes.com/2021/05/08/us/politics/rachel-levine-transgender.html
10. Franklin J. Dr. Rachel Levine is sworn in as the nation’s first transgender four-star officer. October 19, 2021. Accessed February 20, 2024. https://www.npr.org/2021/10/19/1047423156/rachel-levine-first-transgender-four-star-officer
11. Herrick-Reynolds K, Brooks D, Wind G, Jackson P, Latham K. Military medicine and the academic surgery gender gap. Mil Med. 2019;184(9-10):383-387. doi:10.1093/milmed/usz083
Myasthenia Gravis: Treating the Whole Patient
In the dynamic field of myasthenia gravis (MG) treatment, characterized by recent therapeutic advancements and a promising pipeline, Nicholas J. Silvestri, MD, advises early-career professionals to approach the whole patient, considering not only the disease manifestations but also its broader impact on their lives, including work and family.
Emphasizing the importance of tailoring therapies based on individual needs, Dr Silvestri encourages early and aggressive intervention, citing evidence supporting better long-term outcomes, and underscores the significance of treating the whole patient rather than just the disease.
In the dynamic field of myasthenia gravis (MG) treatment, characterized by recent therapeutic advancements and a promising pipeline, Nicholas J. Silvestri, MD, advises early-career professionals to approach the whole patient, considering not only the disease manifestations but also its broader impact on their lives, including work and family.
Emphasizing the importance of tailoring therapies based on individual needs, Dr Silvestri encourages early and aggressive intervention, citing evidence supporting better long-term outcomes, and underscores the significance of treating the whole patient rather than just the disease.
In the dynamic field of myasthenia gravis (MG) treatment, characterized by recent therapeutic advancements and a promising pipeline, Nicholas J. Silvestri, MD, advises early-career professionals to approach the whole patient, considering not only the disease manifestations but also its broader impact on their lives, including work and family.
Emphasizing the importance of tailoring therapies based on individual needs, Dr Silvestri encourages early and aggressive intervention, citing evidence supporting better long-term outcomes, and underscores the significance of treating the whole patient rather than just the disease.

Myasthenia Gravis: 3 Tips to Improve Patient-Centered Care
Kelly G. Gwathmey, MD, offers three key tips for clinicians early in their careers regarding myasthenia gravis (MG): First, prioritize listening to patients, as their experiences may not always align with clinical observations. Second, advocate for shared decision-making when starting or changing treatments, considering individual patient preferences and medical conditions. Third, understand the significance of ongoing monitoring using patient-reported outcome measures and MG scales to assess treatment response and optimize care for patients with MG.
Kelly G. Gwathmey, MD, offers three key tips for clinicians early in their careers regarding myasthenia gravis (MG): First, prioritize listening to patients, as their experiences may not always align with clinical observations. Second, advocate for shared decision-making when starting or changing treatments, considering individual patient preferences and medical conditions. Third, understand the significance of ongoing monitoring using patient-reported outcome measures and MG scales to assess treatment response and optimize care for patients with MG.
Kelly G. Gwathmey, MD, offers three key tips for clinicians early in their careers regarding myasthenia gravis (MG): First, prioritize listening to patients, as their experiences may not always align with clinical observations. Second, advocate for shared decision-making when starting or changing treatments, considering individual patient preferences and medical conditions. Third, understand the significance of ongoing monitoring using patient-reported outcome measures and MG scales to assess treatment response and optimize care for patients with MG.
Myasthenia Gravis: Reflections on Past Challenges and Evolving Strategies
Nicholas J. Silvestri, MD, recounts a memorable experience with a patient with myasthenia gravis (MG) during early neurology residency, detailing the diagnostic process and initial treatment with standard therapies. Despite the patient's positive response in terms of efficacy, tolerability issues and side effects posed challenges.
Dr Silvestri highlights the evolution in MG treatment, emphasizing the availability of newer, well-tolerated options with proven efficacy, suggesting a more balanced approach between effectiveness and patient safety in contemporary MG management.
Nicholas J. Silvestri, MD, recounts a memorable experience with a patient with myasthenia gravis (MG) during early neurology residency, detailing the diagnostic process and initial treatment with standard therapies. Despite the patient's positive response in terms of efficacy, tolerability issues and side effects posed challenges.
Dr Silvestri highlights the evolution in MG treatment, emphasizing the availability of newer, well-tolerated options with proven efficacy, suggesting a more balanced approach between effectiveness and patient safety in contemporary MG management.
Nicholas J. Silvestri, MD, recounts a memorable experience with a patient with myasthenia gravis (MG) during early neurology residency, detailing the diagnostic process and initial treatment with standard therapies. Despite the patient's positive response in terms of efficacy, tolerability issues and side effects posed challenges.
Dr Silvestri highlights the evolution in MG treatment, emphasizing the availability of newer, well-tolerated options with proven efficacy, suggesting a more balanced approach between effectiveness and patient safety in contemporary MG management.

Inspiring Encounters in the Treatment of Myasthenia Gravis
Kelly G. Gwathmey, MD, recounts shadowing a neurologist during an early phase of academic training and how witnessing examinations of patients with conditions like myasthenia gravis and amyotrophic lateral sclerosis inspired a career path in neuromuscular medicine.
Dr Gwathmey also reflects on the evolution of myasthenia gravis treatment over the past two decades, noting the introduction of new medications like eculizumab, complement inhibitors, and FcRn inhibitors — offering more targeted options and hope for patients with fewer side effects — and anticipates further advancements in treatment leading to improved disease control.
Kelly G. Gwathmey, MD, recounts shadowing a neurologist during an early phase of academic training and how witnessing examinations of patients with conditions like myasthenia gravis and amyotrophic lateral sclerosis inspired a career path in neuromuscular medicine.
Dr Gwathmey also reflects on the evolution of myasthenia gravis treatment over the past two decades, noting the introduction of new medications like eculizumab, complement inhibitors, and FcRn inhibitors — offering more targeted options and hope for patients with fewer side effects — and anticipates further advancements in treatment leading to improved disease control.
Kelly G. Gwathmey, MD, recounts shadowing a neurologist during an early phase of academic training and how witnessing examinations of patients with conditions like myasthenia gravis and amyotrophic lateral sclerosis inspired a career path in neuromuscular medicine.
Dr Gwathmey also reflects on the evolution of myasthenia gravis treatment over the past two decades, noting the introduction of new medications like eculizumab, complement inhibitors, and FcRn inhibitors — offering more targeted options and hope for patients with fewer side effects — and anticipates further advancements in treatment leading to improved disease control.
Myasthenia Gravis: Lessons on a Comprehensive Approach to Patient Care
Nicholas J. Silvestri, MD, expresses gratitude for the impactful relationships and mentorship in the field of myasthenia gravis. Dr Chip Howard at the University of North Carolina is distinguished as a humble and inclusive mentor, considered influential in the field.
Dr Howard's influence goes beyond the efficacy of medications, emphasizing the importance of considering patient care comprehensively, including side effects and overall safety. This perspective has significantly shaped Dr Silvestri’s treatment approach, leading to a more holistic and patient-centered care paradigm for individuals with myasthenia gravis.
Nicholas J. Silvestri, MD, expresses gratitude for the impactful relationships and mentorship in the field of myasthenia gravis. Dr Chip Howard at the University of North Carolina is distinguished as a humble and inclusive mentor, considered influential in the field.
Dr Howard's influence goes beyond the efficacy of medications, emphasizing the importance of considering patient care comprehensively, including side effects and overall safety. This perspective has significantly shaped Dr Silvestri’s treatment approach, leading to a more holistic and patient-centered care paradigm for individuals with myasthenia gravis.
Nicholas J. Silvestri, MD, expresses gratitude for the impactful relationships and mentorship in the field of myasthenia gravis. Dr Chip Howard at the University of North Carolina is distinguished as a humble and inclusive mentor, considered influential in the field.
Dr Howard's influence goes beyond the efficacy of medications, emphasizing the importance of considering patient care comprehensively, including side effects and overall safety. This perspective has significantly shaped Dr Silvestri’s treatment approach, leading to a more holistic and patient-centered care paradigm for individuals with myasthenia gravis.

Myasthenia Gravis: A Mentor's Emphasis on Patient-Centered Outcomes
During her time in training at the University of Virginia, Kelly G. Gwathmey, MD, gained invaluable insights into myasthenia gravis (MG) care and research from the late Dr Ted Burns and Dr Larry Phillips. Dr Burns, a renowned leader in MG research, emphasized patient-centric approaches, fostering the development of crucial outcome measures like the MG composite scale and MG-QOL-15.
Burns' dedication to listening to patients' experiences shaped the development of health-related quality-of-life instruments used in MG clinical trials. For Dr Gwathmey, learning under Dr Burns underscored the significance of patient experiences in treatment decisions and highlighted the importance of incorporating patient perspectives in clinical care and research endeavors.
During her time in training at the University of Virginia, Kelly G. Gwathmey, MD, gained invaluable insights into myasthenia gravis (MG) care and research from the late Dr Ted Burns and Dr Larry Phillips. Dr Burns, a renowned leader in MG research, emphasized patient-centric approaches, fostering the development of crucial outcome measures like the MG composite scale and MG-QOL-15.
Burns' dedication to listening to patients' experiences shaped the development of health-related quality-of-life instruments used in MG clinical trials. For Dr Gwathmey, learning under Dr Burns underscored the significance of patient experiences in treatment decisions and highlighted the importance of incorporating patient perspectives in clinical care and research endeavors.
During her time in training at the University of Virginia, Kelly G. Gwathmey, MD, gained invaluable insights into myasthenia gravis (MG) care and research from the late Dr Ted Burns and Dr Larry Phillips. Dr Burns, a renowned leader in MG research, emphasized patient-centric approaches, fostering the development of crucial outcome measures like the MG composite scale and MG-QOL-15.
Burns' dedication to listening to patients' experiences shaped the development of health-related quality-of-life instruments used in MG clinical trials. For Dr Gwathmey, learning under Dr Burns underscored the significance of patient experiences in treatment decisions and highlighted the importance of incorporating patient perspectives in clinical care and research endeavors.