User login
Ribociclib plus endocrine therapy boosts survival of HR+/HER2- breast cancer
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis performed at 42 months of follow-up showed that the overall survival (OS) rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib (Kisqali) was 70%, compared with 46% for women randomized to endocrine therapy plus placebo.
The trial is the first study to evaluate a CDK4/6 inhibitor exclusively in premenopausal women, and the first to show a statistically significant improvement in overall survival with a CDK4/6 inhibitor in combination with endocrine therapy in patients with HR-positive, HER2-negative advanced breast cancer.
In a video interview at the American Society of Clinical Oncology annual meeting, Sara A. Hurvitz, MD, from the University of California Los Angeles Jonsson Comprehensive Cancer Center, describes the significance of the MONALEESA-7 findings and the potential for improving on the study results with other agents or combinations.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis.
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis performed at 42 months of follow-up showed that the overall survival (OS) rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib (Kisqali) was 70%, compared with 46% for women randomized to endocrine therapy plus placebo.
The trial is the first study to evaluate a CDK4/6 inhibitor exclusively in premenopausal women, and the first to show a statistically significant improvement in overall survival with a CDK4/6 inhibitor in combination with endocrine therapy in patients with HR-positive, HER2-negative advanced breast cancer.
In a video interview at the American Society of Clinical Oncology annual meeting, Sara A. Hurvitz, MD, from the University of California Los Angeles Jonsson Comprehensive Cancer Center, describes the significance of the MONALEESA-7 findings and the potential for improving on the study results with other agents or combinations.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis.
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis performed at 42 months of follow-up showed that the overall survival (OS) rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib (Kisqali) was 70%, compared with 46% for women randomized to endocrine therapy plus placebo.
The trial is the first study to evaluate a CDK4/6 inhibitor exclusively in premenopausal women, and the first to show a statistically significant improvement in overall survival with a CDK4/6 inhibitor in combination with endocrine therapy in patients with HR-positive, HER2-negative advanced breast cancer.
In a video interview at the American Society of Clinical Oncology annual meeting, Sara A. Hurvitz, MD, from the University of California Los Angeles Jonsson Comprehensive Cancer Center, describes the significance of the MONALEESA-7 findings and the potential for improving on the study results with other agents or combinations.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis.
REPORTING FROM ASCO 2019
Artificial intelligence advances optical biopsy
SAN DIEGO – Artificial intelligence is improving the accuracy of optical biopsies, a development that may ultimately avoid the need for tissue biopsies of many low-risk colonic polyps, Michael Byrne, MD, said at the annual Digestive Disease Week.

Dr. Byrne, chief executive officer of Satisfai Health, founder of ai4gi, and gastroenterologist at Vancouver General Hospital; Nicolas Guizard, medical imaging researcher at Imagia; and their colleagues at ai4gi developed a “full clinical workflow” for detecting colonic polyps and performing optical biopsies of the polyps.”
Using narrow band imaging (NBI) enhanced with artificial intelligence, the system was used to review 21,804 colonoscopy frames and it achieved a “near-perfect” diagnostic accuracy of 99.9%. In an assessment of colonoscopy videos that included 125 polyps, the system had 95.9% sensitivity, with a specificity of 91.6% and a negative predictive value of 93.6%, Dr. Byrne said.
The speed of the system’s decision-making is rapid, with a typical reaction time of 360 milliseconds. The system was able to make diagnostic inferences at a rate of 26 milliseconds per frame.
With exposure to more learning experiences, the artificial intelligence system improved and committed to a prediction for 97.6% of the polyps it visualized. Dr. Byrne said this result represented a 12.8% improvement from previously published data on the model’s performance.
Dr. Byrne and his colleagues found the system had a tracking accuracy of 92.8%, meaning that this percentage of polyps was both correctly detected and assigned to a unique identifier for follow-up of the site of each excised polyp over time. The interface worked even when multiple polyps were seen on the same screen.
In a video interview, Dr. Byrne discussed the implications for gastroenterology and plans for a clinical trial for rigorous testing of the model.
ai4gi is developing the AI colonoscopy technology. Dr. Byrne is founder of the ai4gi joint venture, which holds a technology codevelopment agreement with Olympus US.
SAN DIEGO – Artificial intelligence is improving the accuracy of optical biopsies, a development that may ultimately avoid the need for tissue biopsies of many low-risk colonic polyps, Michael Byrne, MD, said at the annual Digestive Disease Week.

Dr. Byrne, chief executive officer of Satisfai Health, founder of ai4gi, and gastroenterologist at Vancouver General Hospital; Nicolas Guizard, medical imaging researcher at Imagia; and their colleagues at ai4gi developed a “full clinical workflow” for detecting colonic polyps and performing optical biopsies of the polyps.”
Using narrow band imaging (NBI) enhanced with artificial intelligence, the system was used to review 21,804 colonoscopy frames and it achieved a “near-perfect” diagnostic accuracy of 99.9%. In an assessment of colonoscopy videos that included 125 polyps, the system had 95.9% sensitivity, with a specificity of 91.6% and a negative predictive value of 93.6%, Dr. Byrne said.
The speed of the system’s decision-making is rapid, with a typical reaction time of 360 milliseconds. The system was able to make diagnostic inferences at a rate of 26 milliseconds per frame.
With exposure to more learning experiences, the artificial intelligence system improved and committed to a prediction for 97.6% of the polyps it visualized. Dr. Byrne said this result represented a 12.8% improvement from previously published data on the model’s performance.
Dr. Byrne and his colleagues found the system had a tracking accuracy of 92.8%, meaning that this percentage of polyps was both correctly detected and assigned to a unique identifier for follow-up of the site of each excised polyp over time. The interface worked even when multiple polyps were seen on the same screen.
In a video interview, Dr. Byrne discussed the implications for gastroenterology and plans for a clinical trial for rigorous testing of the model.
ai4gi is developing the AI colonoscopy technology. Dr. Byrne is founder of the ai4gi joint venture, which holds a technology codevelopment agreement with Olympus US.
SAN DIEGO – Artificial intelligence is improving the accuracy of optical biopsies, a development that may ultimately avoid the need for tissue biopsies of many low-risk colonic polyps, Michael Byrne, MD, said at the annual Digestive Disease Week.

Dr. Byrne, chief executive officer of Satisfai Health, founder of ai4gi, and gastroenterologist at Vancouver General Hospital; Nicolas Guizard, medical imaging researcher at Imagia; and their colleagues at ai4gi developed a “full clinical workflow” for detecting colonic polyps and performing optical biopsies of the polyps.”
Using narrow band imaging (NBI) enhanced with artificial intelligence, the system was used to review 21,804 colonoscopy frames and it achieved a “near-perfect” diagnostic accuracy of 99.9%. In an assessment of colonoscopy videos that included 125 polyps, the system had 95.9% sensitivity, with a specificity of 91.6% and a negative predictive value of 93.6%, Dr. Byrne said.
The speed of the system’s decision-making is rapid, with a typical reaction time of 360 milliseconds. The system was able to make diagnostic inferences at a rate of 26 milliseconds per frame.
With exposure to more learning experiences, the artificial intelligence system improved and committed to a prediction for 97.6% of the polyps it visualized. Dr. Byrne said this result represented a 12.8% improvement from previously published data on the model’s performance.
Dr. Byrne and his colleagues found the system had a tracking accuracy of 92.8%, meaning that this percentage of polyps was both correctly detected and assigned to a unique identifier for follow-up of the site of each excised polyp over time. The interface worked even when multiple polyps were seen on the same screen.
In a video interview, Dr. Byrne discussed the implications for gastroenterology and plans for a clinical trial for rigorous testing of the model.
ai4gi is developing the AI colonoscopy technology. Dr. Byrne is founder of the ai4gi joint venture, which holds a technology codevelopment agreement with Olympus US.
REPORTING FROM DDW 2019
Major increase in hidradenitis suppurativa cases anticipated
CHICAGO – Once thought to be a rare disease and largely neglected as a focus of research, and increase the number of patients seeking care, according to an expert interview conducted at the annual meeting of the Society for Investigational Dermatology.
“For decades ... we’ve really not understood how prevalent it is,” said Haley B. Naik, MD, of the department of dermatology at University of California, San Francisco, in a video interview. “Now, thanks to great population-based studies and new data, we know that HS is common and hugely impacts the lives of the people who suffer with this condition.”
Recapping some of the highlights of an update on this chronic inflammatory skin condition that she presented at the meeting, Dr. Naik said that HS has been mischaracterized as rare. Many patients, embarrassed by the symptoms or failing to receive adequate relief from previous health care encounters, are not currently seeking care.
This will change as treatments improve, according to Dr. Naik, who asserted that HS has become a hot topic. Progress in understanding the underlying pathophysiology has been driving new management strategies. She counted more than 15 clinical trials being conducted with new agents for this disease in a clinicaltrials.gov survey.
In the interview, Dr. Naik calls on dermatologists to increase their awareness of the signs and symptoms of HS so that they can diagnose and intervene earlier, a step that will be made easier as new therapies become available.
CHICAGO – Once thought to be a rare disease and largely neglected as a focus of research, and increase the number of patients seeking care, according to an expert interview conducted at the annual meeting of the Society for Investigational Dermatology.
“For decades ... we’ve really not understood how prevalent it is,” said Haley B. Naik, MD, of the department of dermatology at University of California, San Francisco, in a video interview. “Now, thanks to great population-based studies and new data, we know that HS is common and hugely impacts the lives of the people who suffer with this condition.”
Recapping some of the highlights of an update on this chronic inflammatory skin condition that she presented at the meeting, Dr. Naik said that HS has been mischaracterized as rare. Many patients, embarrassed by the symptoms or failing to receive adequate relief from previous health care encounters, are not currently seeking care.
This will change as treatments improve, according to Dr. Naik, who asserted that HS has become a hot topic. Progress in understanding the underlying pathophysiology has been driving new management strategies. She counted more than 15 clinical trials being conducted with new agents for this disease in a clinicaltrials.gov survey.
In the interview, Dr. Naik calls on dermatologists to increase their awareness of the signs and symptoms of HS so that they can diagnose and intervene earlier, a step that will be made easier as new therapies become available.
CHICAGO – Once thought to be a rare disease and largely neglected as a focus of research, and increase the number of patients seeking care, according to an expert interview conducted at the annual meeting of the Society for Investigational Dermatology.
“For decades ... we’ve really not understood how prevalent it is,” said Haley B. Naik, MD, of the department of dermatology at University of California, San Francisco, in a video interview. “Now, thanks to great population-based studies and new data, we know that HS is common and hugely impacts the lives of the people who suffer with this condition.”
Recapping some of the highlights of an update on this chronic inflammatory skin condition that she presented at the meeting, Dr. Naik said that HS has been mischaracterized as rare. Many patients, embarrassed by the symptoms or failing to receive adequate relief from previous health care encounters, are not currently seeking care.
This will change as treatments improve, according to Dr. Naik, who asserted that HS has become a hot topic. Progress in understanding the underlying pathophysiology has been driving new management strategies. She counted more than 15 clinical trials being conducted with new agents for this disease in a clinicaltrials.gov survey.
In the interview, Dr. Naik calls on dermatologists to increase their awareness of the signs and symptoms of HS so that they can diagnose and intervene earlier, a step that will be made easier as new therapies become available.
REPORTING FROM SID 2019
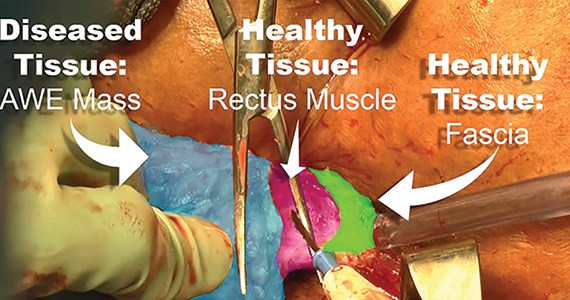
Excision of abdominal wall endometriosis
Endometriosis, defined by the ectopic growth of functioning endometrial glands and stroma,1,2 usually affects the peritoneal cavity. However, endometriosis has been identified in the pneumothorax, brain, and within the extraperitoneum, such as the abdominal wall.1-3 Incidence of abdominal wall endometriosis can be up to 12%.3-5 If patients report symptoms, they can include abdominal pain, a palpable mass, pelvic pain consistent with endometriosis, and bleeding from involvement of the overlying skin. Abdominal wall endometriosis can be surgically resected, with complete resolution and a low rate of recurrence.
In the following video, we review the diagnosis of abdominal wall endometriosis, including our imaging of choice, and treatment options. In addition, we illustrate a surgical technique for the excision of abdominal wall endometriosis in a 38-year-old patient with symptomatic disease. We conclude with a review of key surgical steps.
We hope that you find this video useful to your clinical practice.
>> Dr. Arnold P. Advincula, and colleagues

- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98:511-519.
- Ecker AM, Donnellan NM, Shepherd JP, et al. Abdominal wall endometriosis: 12 years of experience at a large academic institution. Am J Obstet Gynecol. 2014;211:363.e1-e5.
- Horton JD, Dezee KJ, Ahnfeldt EP, et al. Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg. 2008;196:207-212.
- Ding Y, Zhu J. A retrospective review of abdominal wall endometriosis in Shanghai, China. Int J Gynaecol Obstet. 2013;121:41-44.
- Chang Y, Tsai EM, Long CY, et al. Abdominal wall endometriosis. J Reproductive Med. 2009;54:155-159.
Endometriosis, defined by the ectopic growth of functioning endometrial glands and stroma,1,2 usually affects the peritoneal cavity. However, endometriosis has been identified in the pneumothorax, brain, and within the extraperitoneum, such as the abdominal wall.1-3 Incidence of abdominal wall endometriosis can be up to 12%.3-5 If patients report symptoms, they can include abdominal pain, a palpable mass, pelvic pain consistent with endometriosis, and bleeding from involvement of the overlying skin. Abdominal wall endometriosis can be surgically resected, with complete resolution and a low rate of recurrence.
In the following video, we review the diagnosis of abdominal wall endometriosis, including our imaging of choice, and treatment options. In addition, we illustrate a surgical technique for the excision of abdominal wall endometriosis in a 38-year-old patient with symptomatic disease. We conclude with a review of key surgical steps.
We hope that you find this video useful to your clinical practice.
>> Dr. Arnold P. Advincula, and colleagues

Endometriosis, defined by the ectopic growth of functioning endometrial glands and stroma,1,2 usually affects the peritoneal cavity. However, endometriosis has been identified in the pneumothorax, brain, and within the extraperitoneum, such as the abdominal wall.1-3 Incidence of abdominal wall endometriosis can be up to 12%.3-5 If patients report symptoms, they can include abdominal pain, a palpable mass, pelvic pain consistent with endometriosis, and bleeding from involvement of the overlying skin. Abdominal wall endometriosis can be surgically resected, with complete resolution and a low rate of recurrence.
In the following video, we review the diagnosis of abdominal wall endometriosis, including our imaging of choice, and treatment options. In addition, we illustrate a surgical technique for the excision of abdominal wall endometriosis in a 38-year-old patient with symptomatic disease. We conclude with a review of key surgical steps.
We hope that you find this video useful to your clinical practice.
>> Dr. Arnold P. Advincula, and colleagues

- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98:511-519.
- Ecker AM, Donnellan NM, Shepherd JP, et al. Abdominal wall endometriosis: 12 years of experience at a large academic institution. Am J Obstet Gynecol. 2014;211:363.e1-e5.
- Horton JD, Dezee KJ, Ahnfeldt EP, et al. Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg. 2008;196:207-212.
- Ding Y, Zhu J. A retrospective review of abdominal wall endometriosis in Shanghai, China. Int J Gynaecol Obstet. 2013;121:41-44.
- Chang Y, Tsai EM, Long CY, et al. Abdominal wall endometriosis. J Reproductive Med. 2009;54:155-159.
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98:511-519.
- Ecker AM, Donnellan NM, Shepherd JP, et al. Abdominal wall endometriosis: 12 years of experience at a large academic institution. Am J Obstet Gynecol. 2014;211:363.e1-e5.
- Horton JD, Dezee KJ, Ahnfeldt EP, et al. Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg. 2008;196:207-212.
- Ding Y, Zhu J. A retrospective review of abdominal wall endometriosis in Shanghai, China. Int J Gynaecol Obstet. 2013;121:41-44.
- Chang Y, Tsai EM, Long CY, et al. Abdominal wall endometriosis. J Reproductive Med. 2009;54:155-159.
Adding drugs to gastric balloons increases weight loss
SAN DIEGO – In a multicenter study involving four academic medical centers, the addition of weight loss drugs to intragastric balloons resulted in better weight loss 12 months after balloon placement.
In a video interview at the annual Digestive Disease Week, study investigator Reem Sharaiha, MD, explained that one of the drawbacks of intragastric balloons is that, although they produce weight loss for the 6 or 12 months that they are in place, patients tend to regain that weight after they are removed. The study, involving 111 patients, was designed to determine whether the addition of weight loss drugs could mitigate this effect and improve weight loss, said Dr. Sharaiha of Weill Cornell Medical Center, New York.
Adding drugs such as metformin or weight loss drugs tailored to patients’ particular weight issues (cravings, anxiety, or fast gastric emptying) at the 3- or 6-month mark while the intragastric balloon was in place helped patients continue losing weight after balloon removal. At 12 months, the percentage of total body weight lost was significantly greater in the intragastric balloon group with concurrent pharmacotherapy (21.4% vs. 13.1%).
SOURCE: Shah SL et al. DDW 2019, Abstract 1105.
SAN DIEGO – In a multicenter study involving four academic medical centers, the addition of weight loss drugs to intragastric balloons resulted in better weight loss 12 months after balloon placement.
In a video interview at the annual Digestive Disease Week, study investigator Reem Sharaiha, MD, explained that one of the drawbacks of intragastric balloons is that, although they produce weight loss for the 6 or 12 months that they are in place, patients tend to regain that weight after they are removed. The study, involving 111 patients, was designed to determine whether the addition of weight loss drugs could mitigate this effect and improve weight loss, said Dr. Sharaiha of Weill Cornell Medical Center, New York.
Adding drugs such as metformin or weight loss drugs tailored to patients’ particular weight issues (cravings, anxiety, or fast gastric emptying) at the 3- or 6-month mark while the intragastric balloon was in place helped patients continue losing weight after balloon removal. At 12 months, the percentage of total body weight lost was significantly greater in the intragastric balloon group with concurrent pharmacotherapy (21.4% vs. 13.1%).
SOURCE: Shah SL et al. DDW 2019, Abstract 1105.
SAN DIEGO – In a multicenter study involving four academic medical centers, the addition of weight loss drugs to intragastric balloons resulted in better weight loss 12 months after balloon placement.
In a video interview at the annual Digestive Disease Week, study investigator Reem Sharaiha, MD, explained that one of the drawbacks of intragastric balloons is that, although they produce weight loss for the 6 or 12 months that they are in place, patients tend to regain that weight after they are removed. The study, involving 111 patients, was designed to determine whether the addition of weight loss drugs could mitigate this effect and improve weight loss, said Dr. Sharaiha of Weill Cornell Medical Center, New York.
Adding drugs such as metformin or weight loss drugs tailored to patients’ particular weight issues (cravings, anxiety, or fast gastric emptying) at the 3- or 6-month mark while the intragastric balloon was in place helped patients continue losing weight after balloon removal. At 12 months, the percentage of total body weight lost was significantly greater in the intragastric balloon group with concurrent pharmacotherapy (21.4% vs. 13.1%).
SOURCE: Shah SL et al. DDW 2019, Abstract 1105.
REPORTING FROM DDW 2019
Patients with intellectual disability require nuanced care
SAN FRANCISCO – Some physicians are uncomfortable providing mental health care to patients with intellectual disability (ID) because many of the patients’ communications skills are limited. But many resources are available that can help.
In this video, Nita V. Bhatt, MD, MPH, interviews Julie P. Gentile, MD, about some of those resources and discusses how to approach psychiatric treatment interventions for patients with ID.
In addition to the DSM-5, Dr. Gentile said the National Association for the Dually Diagnosed has published the Diagnostic Manual – Intellectual Disability. Another resource is a practical reference manual originally proposed by one of Dr. Gentile’s residents.
“He came into my office for supervision one day and said, ‘You know, there’s all these nuances for psychiatric treatment in this patient population. So we should write a practice, quick reference manual to help clinicians who aren’t able to spend as much time concentrate on this patient population.’ ”
As a result, several residents and faculty members formed a team to produce an 18-chapter book published this year by Springer called the Guide to Intellectual Disabilities: A Clinical Handbook.
Dr. Bhatt is a staff psychiatrist at Twin Valley Behavioral Healthcare, the state psychiatric hospital in Columbus, Ohio. Dr. Gentile is professor and chair of the department of psychiatry at Wright State in Dayton. She is also serves as project director of Ohio’s Telepsychiatry Project for Intellectual Disability and has been awarded more than $7 million in grant funding to support her projects in the field of ID.
Dr. Gentile’s work has been funded by the Ohio Department of Developmental Disabilities and the Ohio Department of Mental Health and Addiction Services.
SAN FRANCISCO – Some physicians are uncomfortable providing mental health care to patients with intellectual disability (ID) because many of the patients’ communications skills are limited. But many resources are available that can help.
In this video, Nita V. Bhatt, MD, MPH, interviews Julie P. Gentile, MD, about some of those resources and discusses how to approach psychiatric treatment interventions for patients with ID.
In addition to the DSM-5, Dr. Gentile said the National Association for the Dually Diagnosed has published the Diagnostic Manual – Intellectual Disability. Another resource is a practical reference manual originally proposed by one of Dr. Gentile’s residents.
“He came into my office for supervision one day and said, ‘You know, there’s all these nuances for psychiatric treatment in this patient population. So we should write a practice, quick reference manual to help clinicians who aren’t able to spend as much time concentrate on this patient population.’ ”
As a result, several residents and faculty members formed a team to produce an 18-chapter book published this year by Springer called the Guide to Intellectual Disabilities: A Clinical Handbook.
Dr. Bhatt is a staff psychiatrist at Twin Valley Behavioral Healthcare, the state psychiatric hospital in Columbus, Ohio. Dr. Gentile is professor and chair of the department of psychiatry at Wright State in Dayton. She is also serves as project director of Ohio’s Telepsychiatry Project for Intellectual Disability and has been awarded more than $7 million in grant funding to support her projects in the field of ID.
Dr. Gentile’s work has been funded by the Ohio Department of Developmental Disabilities and the Ohio Department of Mental Health and Addiction Services.
SAN FRANCISCO – Some physicians are uncomfortable providing mental health care to patients with intellectual disability (ID) because many of the patients’ communications skills are limited. But many resources are available that can help.
In this video, Nita V. Bhatt, MD, MPH, interviews Julie P. Gentile, MD, about some of those resources and discusses how to approach psychiatric treatment interventions for patients with ID.
In addition to the DSM-5, Dr. Gentile said the National Association for the Dually Diagnosed has published the Diagnostic Manual – Intellectual Disability. Another resource is a practical reference manual originally proposed by one of Dr. Gentile’s residents.
“He came into my office for supervision one day and said, ‘You know, there’s all these nuances for psychiatric treatment in this patient population. So we should write a practice, quick reference manual to help clinicians who aren’t able to spend as much time concentrate on this patient population.’ ”
As a result, several residents and faculty members formed a team to produce an 18-chapter book published this year by Springer called the Guide to Intellectual Disabilities: A Clinical Handbook.
Dr. Bhatt is a staff psychiatrist at Twin Valley Behavioral Healthcare, the state psychiatric hospital in Columbus, Ohio. Dr. Gentile is professor and chair of the department of psychiatry at Wright State in Dayton. She is also serves as project director of Ohio’s Telepsychiatry Project for Intellectual Disability and has been awarded more than $7 million in grant funding to support her projects in the field of ID.
Dr. Gentile’s work has been funded by the Ohio Department of Developmental Disabilities and the Ohio Department of Mental Health and Addiction Services.
REPORTING FROM APA 2019
How to counsel patients interested in trying marijuana
SAN FRANCISCO – It’s a common scenario, and it’s going to become more common: Psychiatric patients will be coming into the office not quite satisfied with their current treatment and wanting to try cannabis.
With laws varying from state to state and a limited but growing body of evidence, the situation “presents a complicated, often difficult clinical situation,” said David A. Gorelick, MD, PhD, professor of psychiatry at the University of Maryland, Baltimore.
There is some evidence supporting cannabis for chronic pain, neuropathic pain, spasticity in multiple sclerosis, and chemotherapy-induced nausea and vomiting. Cannabidiol is also Food and Drug Administration approved for two severe forms of pediatric epilepsy.
When it comes to psychiatric disorders, however, evidence is largely lacking. On the other hand, some patients swear by marijuana for psychiatric symptom relief.
So what to do? Dr. Gorelick, editor of the Journal of Cannabis Research, had some advice in a video interview at the annual meeting of the American Psychiatric Association.
Where it’s legal, a cannabis recommendation for pain and sleep problems is reasonable, but it’s important to figure out what’s lacking in the patients’ treatment regimen that makes them want to try cannabis, and to first try to maximize treatment with approved, evidence-based options. As with any medication, a talk about risks and benefits is also essential. There’s an increased risk of motor vehicle accidents, acute panic attacks, and other issues with cannabis. Also, keep in mind that cannabinoids, particularly tetrahydrocannabinol, are metabolized in the liver and can interfere with concentrations of other liver-metabolized drugs, including some antidepressants and anticonvulsants. It’s not clear how significant the clinical interactions are, “but if patients are on warfarin, I would be very careful,” he said.
Dr. Gorelick disclosed speaking fees from hospitals and organizations for presentations on medical cannabis and royalties from Up-to-Date for cannabis topics. He also disclosed receiving honoraria from Colorado State University, Pueblo, and from Springer for his work on the Journal of Cannabis Research.
SAN FRANCISCO – It’s a common scenario, and it’s going to become more common: Psychiatric patients will be coming into the office not quite satisfied with their current treatment and wanting to try cannabis.
With laws varying from state to state and a limited but growing body of evidence, the situation “presents a complicated, often difficult clinical situation,” said David A. Gorelick, MD, PhD, professor of psychiatry at the University of Maryland, Baltimore.
There is some evidence supporting cannabis for chronic pain, neuropathic pain, spasticity in multiple sclerosis, and chemotherapy-induced nausea and vomiting. Cannabidiol is also Food and Drug Administration approved for two severe forms of pediatric epilepsy.
When it comes to psychiatric disorders, however, evidence is largely lacking. On the other hand, some patients swear by marijuana for psychiatric symptom relief.
So what to do? Dr. Gorelick, editor of the Journal of Cannabis Research, had some advice in a video interview at the annual meeting of the American Psychiatric Association.
Where it’s legal, a cannabis recommendation for pain and sleep problems is reasonable, but it’s important to figure out what’s lacking in the patients’ treatment regimen that makes them want to try cannabis, and to first try to maximize treatment with approved, evidence-based options. As with any medication, a talk about risks and benefits is also essential. There’s an increased risk of motor vehicle accidents, acute panic attacks, and other issues with cannabis. Also, keep in mind that cannabinoids, particularly tetrahydrocannabinol, are metabolized in the liver and can interfere with concentrations of other liver-metabolized drugs, including some antidepressants and anticonvulsants. It’s not clear how significant the clinical interactions are, “but if patients are on warfarin, I would be very careful,” he said.
Dr. Gorelick disclosed speaking fees from hospitals and organizations for presentations on medical cannabis and royalties from Up-to-Date for cannabis topics. He also disclosed receiving honoraria from Colorado State University, Pueblo, and from Springer for his work on the Journal of Cannabis Research.
SAN FRANCISCO – It’s a common scenario, and it’s going to become more common: Psychiatric patients will be coming into the office not quite satisfied with their current treatment and wanting to try cannabis.
With laws varying from state to state and a limited but growing body of evidence, the situation “presents a complicated, often difficult clinical situation,” said David A. Gorelick, MD, PhD, professor of psychiatry at the University of Maryland, Baltimore.
There is some evidence supporting cannabis for chronic pain, neuropathic pain, spasticity in multiple sclerosis, and chemotherapy-induced nausea and vomiting. Cannabidiol is also Food and Drug Administration approved for two severe forms of pediatric epilepsy.
When it comes to psychiatric disorders, however, evidence is largely lacking. On the other hand, some patients swear by marijuana for psychiatric symptom relief.
So what to do? Dr. Gorelick, editor of the Journal of Cannabis Research, had some advice in a video interview at the annual meeting of the American Psychiatric Association.
Where it’s legal, a cannabis recommendation for pain and sleep problems is reasonable, but it’s important to figure out what’s lacking in the patients’ treatment regimen that makes them want to try cannabis, and to first try to maximize treatment with approved, evidence-based options. As with any medication, a talk about risks and benefits is also essential. There’s an increased risk of motor vehicle accidents, acute panic attacks, and other issues with cannabis. Also, keep in mind that cannabinoids, particularly tetrahydrocannabinol, are metabolized in the liver and can interfere with concentrations of other liver-metabolized drugs, including some antidepressants and anticonvulsants. It’s not clear how significant the clinical interactions are, “but if patients are on warfarin, I would be very careful,” he said.
Dr. Gorelick disclosed speaking fees from hospitals and organizations for presentations on medical cannabis and royalties from Up-to-Date for cannabis topics. He also disclosed receiving honoraria from Colorado State University, Pueblo, and from Springer for his work on the Journal of Cannabis Research.
REPORTING FROM APA 2019
Navigating racism while in medical training
SAN FRANCISCO – When Jessica Isom, MD, MPH, and her colleagues noticed the absence of good role modeling about how to address race and racism in interactions with supervisors at their long-term care clinic, they conducted a research study.

“Now, we’re working on rolling out what those solutions might be for addressing this gap in the education,” said Dr. Isom, a PGY-4 resident at Yale University, New Haven, Conn. Many of the issues Dr. Isom and her colleagues found are reminiscent of those identified almost 50 years ago by Billy E. Jones, MD, and his colleagues. Their article (1970 Dec; 127[6]:798-803) focusing on the problems of black residents in predominantly white institutions was published in the American Journal of Psychiatry, Constance E. Dunlap, MD, said at the annual meeting of the American Psychiatric Association.
In this video, Dr. Dunlap interviews Dr. Isom about her experiences with both supervisors and patients on issues tied to race and racism – and examines possible solutions.
In one case, Dr. Isom said she created an opening for discussion with a supervisor by advising him to read the book White Fragility (Beacon Press, 2018). “He read the book,” Dr. Isom said. “And And he’s thinking about these things now as a white man and his relationship to racism. So that’s sort of a positive outcome from having that conversation in the first place.”
In another case involving a patient who declined treatment from Dr. Isom and an Asian male medical student, Dr. Isom said she respected the patient’s wishes and walked out of the room. When she shared the experience with her team, the incident was not addressed.
Dr. Isom’s experiences reflects that of African Americans and other ethnic minorities in the United States, Dr. Dunlap said. “I think about being in junior high school and reading ... and doing my own study outside of school and that has carried through college, medical school, and even in residency – and definitely psychoanalytic training – where psychoanalysts like Frantz Fanon, Frances Cress Welsing, even Dorothy Holmes ... were not included in the mainstream curriculum.” However, those thinkers are included in some curricula now.
“This is an example of how medicine and psychoanalysis have been functioning in parallel with the way the country functions,” Dr. Dunlap said. “This is a huge blind spot.”
Dr. Isom worked on the research study with fellow residents* Myra Mathis, MD; Flavia DeSouza, MHS, MD; and Natalie Lastra, MD. Dr. Isom is member of the American Psychiatric Association Assembly as the area 1 representative for resident fellow members. She also is one of the chief residents of diversity and inclusion, and a codirector of the social justice and health equity curriculum at the department of psychiatry at Yale. Dr. Dunlap is a psychiatrist and psychoanalyst with more than 25 years’ experience in clinical care, psychiatric education, patient advocacy, and community outreach. She is a member of the APA assembly representing the Washington Psychiatric Society. Dr. Isom and Dr. Dunlap had no disclosures.
*CLARIFICATION, 5/22/2019
SAN FRANCISCO – When Jessica Isom, MD, MPH, and her colleagues noticed the absence of good role modeling about how to address race and racism in interactions with supervisors at their long-term care clinic, they conducted a research study.

“Now, we’re working on rolling out what those solutions might be for addressing this gap in the education,” said Dr. Isom, a PGY-4 resident at Yale University, New Haven, Conn. Many of the issues Dr. Isom and her colleagues found are reminiscent of those identified almost 50 years ago by Billy E. Jones, MD, and his colleagues. Their article (1970 Dec; 127[6]:798-803) focusing on the problems of black residents in predominantly white institutions was published in the American Journal of Psychiatry, Constance E. Dunlap, MD, said at the annual meeting of the American Psychiatric Association.
In this video, Dr. Dunlap interviews Dr. Isom about her experiences with both supervisors and patients on issues tied to race and racism – and examines possible solutions.
In one case, Dr. Isom said she created an opening for discussion with a supervisor by advising him to read the book White Fragility (Beacon Press, 2018). “He read the book,” Dr. Isom said. “And And he’s thinking about these things now as a white man and his relationship to racism. So that’s sort of a positive outcome from having that conversation in the first place.”
In another case involving a patient who declined treatment from Dr. Isom and an Asian male medical student, Dr. Isom said she respected the patient’s wishes and walked out of the room. When she shared the experience with her team, the incident was not addressed.
Dr. Isom’s experiences reflects that of African Americans and other ethnic minorities in the United States, Dr. Dunlap said. “I think about being in junior high school and reading ... and doing my own study outside of school and that has carried through college, medical school, and even in residency – and definitely psychoanalytic training – where psychoanalysts like Frantz Fanon, Frances Cress Welsing, even Dorothy Holmes ... were not included in the mainstream curriculum.” However, those thinkers are included in some curricula now.
“This is an example of how medicine and psychoanalysis have been functioning in parallel with the way the country functions,” Dr. Dunlap said. “This is a huge blind spot.”
Dr. Isom worked on the research study with fellow residents* Myra Mathis, MD; Flavia DeSouza, MHS, MD; and Natalie Lastra, MD. Dr. Isom is member of the American Psychiatric Association Assembly as the area 1 representative for resident fellow members. She also is one of the chief residents of diversity and inclusion, and a codirector of the social justice and health equity curriculum at the department of psychiatry at Yale. Dr. Dunlap is a psychiatrist and psychoanalyst with more than 25 years’ experience in clinical care, psychiatric education, patient advocacy, and community outreach. She is a member of the APA assembly representing the Washington Psychiatric Society. Dr. Isom and Dr. Dunlap had no disclosures.
*CLARIFICATION, 5/22/2019
SAN FRANCISCO – When Jessica Isom, MD, MPH, and her colleagues noticed the absence of good role modeling about how to address race and racism in interactions with supervisors at their long-term care clinic, they conducted a research study.

“Now, we’re working on rolling out what those solutions might be for addressing this gap in the education,” said Dr. Isom, a PGY-4 resident at Yale University, New Haven, Conn. Many of the issues Dr. Isom and her colleagues found are reminiscent of those identified almost 50 years ago by Billy E. Jones, MD, and his colleagues. Their article (1970 Dec; 127[6]:798-803) focusing on the problems of black residents in predominantly white institutions was published in the American Journal of Psychiatry, Constance E. Dunlap, MD, said at the annual meeting of the American Psychiatric Association.
In this video, Dr. Dunlap interviews Dr. Isom about her experiences with both supervisors and patients on issues tied to race and racism – and examines possible solutions.
In one case, Dr. Isom said she created an opening for discussion with a supervisor by advising him to read the book White Fragility (Beacon Press, 2018). “He read the book,” Dr. Isom said. “And And he’s thinking about these things now as a white man and his relationship to racism. So that’s sort of a positive outcome from having that conversation in the first place.”
In another case involving a patient who declined treatment from Dr. Isom and an Asian male medical student, Dr. Isom said she respected the patient’s wishes and walked out of the room. When she shared the experience with her team, the incident was not addressed.
Dr. Isom’s experiences reflects that of African Americans and other ethnic minorities in the United States, Dr. Dunlap said. “I think about being in junior high school and reading ... and doing my own study outside of school and that has carried through college, medical school, and even in residency – and definitely psychoanalytic training – where psychoanalysts like Frantz Fanon, Frances Cress Welsing, even Dorothy Holmes ... were not included in the mainstream curriculum.” However, those thinkers are included in some curricula now.
“This is an example of how medicine and psychoanalysis have been functioning in parallel with the way the country functions,” Dr. Dunlap said. “This is a huge blind spot.”
Dr. Isom worked on the research study with fellow residents* Myra Mathis, MD; Flavia DeSouza, MHS, MD; and Natalie Lastra, MD. Dr. Isom is member of the American Psychiatric Association Assembly as the area 1 representative for resident fellow members. She also is one of the chief residents of diversity and inclusion, and a codirector of the social justice and health equity curriculum at the department of psychiatry at Yale. Dr. Dunlap is a psychiatrist and psychoanalyst with more than 25 years’ experience in clinical care, psychiatric education, patient advocacy, and community outreach. She is a member of the APA assembly representing the Washington Psychiatric Society. Dr. Isom and Dr. Dunlap had no disclosures.
*CLARIFICATION, 5/22/2019
REPORTING FROM APA 2019
Treatment-resistant GERD reported by more than half of patients
SAN DIEGO – Gastroesophageal reflux disease refractory to proton pump inhibitors may affect nearly half of those treated, according to the findings of a population-based sample of more than 70,000 Americans.
As part of the National Institutes of Health GI Patient Reported Outcomes Measurement Information System (NIH GI-PROMIS) questionnaire, respondents could download a free app called “My GI Health,” which led them through a series of questions about GI diseases. Sean Delshad, MD, MBA, of Cedars-Sinai Medical Center Los Angeles, and his colleagues examined data on symptom responses about GERD and heartburn.
Their somewhat surprising findings were that 44% of respondents had ever had GERD and that 70% of those respondents had symptoms in the past week. GERD seemed to be more common in women than in men, and in non-Hispanic whites more than other demographic groups. The rate of proton pump inhibitor–refractory GERD was reported at 54%.
Dr. Delshad discussed the implications of the study results for treatment and research in a video interview at the annual Digestive Disease Week.
SAN DIEGO – Gastroesophageal reflux disease refractory to proton pump inhibitors may affect nearly half of those treated, according to the findings of a population-based sample of more than 70,000 Americans.
As part of the National Institutes of Health GI Patient Reported Outcomes Measurement Information System (NIH GI-PROMIS) questionnaire, respondents could download a free app called “My GI Health,” which led them through a series of questions about GI diseases. Sean Delshad, MD, MBA, of Cedars-Sinai Medical Center Los Angeles, and his colleagues examined data on symptom responses about GERD and heartburn.
Their somewhat surprising findings were that 44% of respondents had ever had GERD and that 70% of those respondents had symptoms in the past week. GERD seemed to be more common in women than in men, and in non-Hispanic whites more than other demographic groups. The rate of proton pump inhibitor–refractory GERD was reported at 54%.
Dr. Delshad discussed the implications of the study results for treatment and research in a video interview at the annual Digestive Disease Week.
SAN DIEGO – Gastroesophageal reflux disease refractory to proton pump inhibitors may affect nearly half of those treated, according to the findings of a population-based sample of more than 70,000 Americans.
As part of the National Institutes of Health GI Patient Reported Outcomes Measurement Information System (NIH GI-PROMIS) questionnaire, respondents could download a free app called “My GI Health,” which led them through a series of questions about GI diseases. Sean Delshad, MD, MBA, of Cedars-Sinai Medical Center Los Angeles, and his colleagues examined data on symptom responses about GERD and heartburn.
Their somewhat surprising findings were that 44% of respondents had ever had GERD and that 70% of those respondents had symptoms in the past week. GERD seemed to be more common in women than in men, and in non-Hispanic whites more than other demographic groups. The rate of proton pump inhibitor–refractory GERD was reported at 54%.
Dr. Delshad discussed the implications of the study results for treatment and research in a video interview at the annual Digestive Disease Week.
REPORTING FROM DDW 2019
Bariatric surgery found to be effective in IBD patients
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019