User login
PIONEER-HF secures place for sacubitril/valsartan in this heart failure doc’s practice
CHICAGO – Dr. Larry A. Allen will now have an easier time of treating hospitalized patients with acute decompensated heart failure because of the results of the PIONEER-HF trial.
That study examined whether in-hospital initiation of sacubitril/valsartan compared to enalapril is safe and effective in ADHF, a treatment that hasn’t been studied well or taken up in clinical practice.
, showed comparable safety, and reduced composite endpoint of death, rehospitalization for heart failure, implantation of a left-ventricular implant device, and need for a transplant by 46%.
Dr. Allen, of the University of Colorado, Denver, was the designated discussant for the PIONEER-HF presentation at the American Heart Association scientific sessions. In an interview, he explained how these results will change his practice as a heart failure specialist. “It simplifies things: I don’t have to start on an old therapy in the hospital, get the patients back in clinic, and switch the over to this newer therapy. I can just start from the beginning with the therapy that I think will be most effective.”
To find out why, watch the complete interview.
CHICAGO – Dr. Larry A. Allen will now have an easier time of treating hospitalized patients with acute decompensated heart failure because of the results of the PIONEER-HF trial.
That study examined whether in-hospital initiation of sacubitril/valsartan compared to enalapril is safe and effective in ADHF, a treatment that hasn’t been studied well or taken up in clinical practice.
, showed comparable safety, and reduced composite endpoint of death, rehospitalization for heart failure, implantation of a left-ventricular implant device, and need for a transplant by 46%.
Dr. Allen, of the University of Colorado, Denver, was the designated discussant for the PIONEER-HF presentation at the American Heart Association scientific sessions. In an interview, he explained how these results will change his practice as a heart failure specialist. “It simplifies things: I don’t have to start on an old therapy in the hospital, get the patients back in clinic, and switch the over to this newer therapy. I can just start from the beginning with the therapy that I think will be most effective.”
To find out why, watch the complete interview.
CHICAGO – Dr. Larry A. Allen will now have an easier time of treating hospitalized patients with acute decompensated heart failure because of the results of the PIONEER-HF trial.
That study examined whether in-hospital initiation of sacubitril/valsartan compared to enalapril is safe and effective in ADHF, a treatment that hasn’t been studied well or taken up in clinical practice.
, showed comparable safety, and reduced composite endpoint of death, rehospitalization for heart failure, implantation of a left-ventricular implant device, and need for a transplant by 46%.
Dr. Allen, of the University of Colorado, Denver, was the designated discussant for the PIONEER-HF presentation at the American Heart Association scientific sessions. In an interview, he explained how these results will change his practice as a heart failure specialist. “It simplifies things: I don’t have to start on an old therapy in the hospital, get the patients back in clinic, and switch the over to this newer therapy. I can just start from the beginning with the therapy that I think will be most effective.”
To find out why, watch the complete interview.
REPORTING FROM AHA 2018
United States must join with world to protect refugee children
ORLANDO – The United States is one of the wealthiest nations on the planet, yet it does not always stand with the rest of the global community in promoting universally accepted principles on the health and well-being of children across the world, particularly refugee children, according to Francis E. Rushton Jr., MD.
In an interview at the annual meeting of the American Academy of Pediatrics, Dr. Rushton discussed the importance of seeing American exceptionalism for what it is – a flaw rather than a virtue – and joining with the rest of the world in upholding the tenets of the Budapest Declaration On the Rights, Health and Well-being of Children and Youth on the Move.
In the three-page Budapest document, created by the International Society for Social Pediatrics and Child Health (ISSOP) in October 2017 and endorsed by the AAP, pediatricians from across the world acknowledge the realities of worldwide refugee crises and accept their detailed responsibilities in meeting and advocating for those children’s needs.
Although the current administration’s decision earlier this year to split children from their families at the border caught everyone attention, . He particularly stressed the “importance of working with the global community on clinical services, programs and policy.”
Dr. Rushton, clinical professor of pediatrics at the University of South Carolina, Columbia, and medical director of the Quality Through Innovation in Pediatrics network, also discussed the need to commit to the United Nations Convention on the Rights of the Child and to join the global community in following the UN’s Sustainable Development Goals and the principles in the World Health Organization’s publication, “Nurturing care for early childhood development.”
The former is a “blueprint” to overcoming challenges related to “poverty, inequality, climate, environmental degradation, prosperity and peace and justice” by achieving targets by 2030, and the latter is “a framework for helping children survive and thrive to transform health and human potential.”
“This is our issue as child health professionals. We need to continue applying pressure on our political leaders,” Dr. Rushton told his colleagues. He advocated taking the long view: “Let’s build a system that respects the human rights of all children.”
ORLANDO – The United States is one of the wealthiest nations on the planet, yet it does not always stand with the rest of the global community in promoting universally accepted principles on the health and well-being of children across the world, particularly refugee children, according to Francis E. Rushton Jr., MD.
In an interview at the annual meeting of the American Academy of Pediatrics, Dr. Rushton discussed the importance of seeing American exceptionalism for what it is – a flaw rather than a virtue – and joining with the rest of the world in upholding the tenets of the Budapest Declaration On the Rights, Health and Well-being of Children and Youth on the Move.
In the three-page Budapest document, created by the International Society for Social Pediatrics and Child Health (ISSOP) in October 2017 and endorsed by the AAP, pediatricians from across the world acknowledge the realities of worldwide refugee crises and accept their detailed responsibilities in meeting and advocating for those children’s needs.
Although the current administration’s decision earlier this year to split children from their families at the border caught everyone attention, . He particularly stressed the “importance of working with the global community on clinical services, programs and policy.”
Dr. Rushton, clinical professor of pediatrics at the University of South Carolina, Columbia, and medical director of the Quality Through Innovation in Pediatrics network, also discussed the need to commit to the United Nations Convention on the Rights of the Child and to join the global community in following the UN’s Sustainable Development Goals and the principles in the World Health Organization’s publication, “Nurturing care for early childhood development.”
The former is a “blueprint” to overcoming challenges related to “poverty, inequality, climate, environmental degradation, prosperity and peace and justice” by achieving targets by 2030, and the latter is “a framework for helping children survive and thrive to transform health and human potential.”
“This is our issue as child health professionals. We need to continue applying pressure on our political leaders,” Dr. Rushton told his colleagues. He advocated taking the long view: “Let’s build a system that respects the human rights of all children.”
ORLANDO – The United States is one of the wealthiest nations on the planet, yet it does not always stand with the rest of the global community in promoting universally accepted principles on the health and well-being of children across the world, particularly refugee children, according to Francis E. Rushton Jr., MD.
In an interview at the annual meeting of the American Academy of Pediatrics, Dr. Rushton discussed the importance of seeing American exceptionalism for what it is – a flaw rather than a virtue – and joining with the rest of the world in upholding the tenets of the Budapest Declaration On the Rights, Health and Well-being of Children and Youth on the Move.
In the three-page Budapest document, created by the International Society for Social Pediatrics and Child Health (ISSOP) in October 2017 and endorsed by the AAP, pediatricians from across the world acknowledge the realities of worldwide refugee crises and accept their detailed responsibilities in meeting and advocating for those children’s needs.
Although the current administration’s decision earlier this year to split children from their families at the border caught everyone attention, . He particularly stressed the “importance of working with the global community on clinical services, programs and policy.”
Dr. Rushton, clinical professor of pediatrics at the University of South Carolina, Columbia, and medical director of the Quality Through Innovation in Pediatrics network, also discussed the need to commit to the United Nations Convention on the Rights of the Child and to join the global community in following the UN’s Sustainable Development Goals and the principles in the World Health Organization’s publication, “Nurturing care for early childhood development.”
The former is a “blueprint” to overcoming challenges related to “poverty, inequality, climate, environmental degradation, prosperity and peace and justice” by achieving targets by 2030, and the latter is “a framework for helping children survive and thrive to transform health and human potential.”
“This is our issue as child health professionals. We need to continue applying pressure on our political leaders,” Dr. Rushton told his colleagues. He advocated taking the long view: “Let’s build a system that respects the human rights of all children.”
REPORTING FROM AAP 2018
Google Search Results for Diet and Psoriasis: Advice Patients Get on the Internet
Innovations in Dermatology: Sarecycline Approved for Acne



Communicate with Millennials using their preferred methods
ORLANDO – Pediatricians can learn from how Millennials use services and purchase products from popular companies, such as Amazon Alexa, Warby Parker, Instagram, and Snapchat, and use that information to connect with Millennial parents and children in their practice, Kristopher Jones, JD, MS, said.
In a video interview, Mr. Jones explained how Amazon Alexa uses structured data as recommendations when users make queries of the service; for example, a Millennial might make a choice to book an appointment with a pediatrician based on the results Amazon Alexa displays, such as an office’s available hours. An office that is not optimized to appear in those results would be missed by those potential patients.
Warby Parker has a digital-first strategy focused on convenience, ease of use, and an emphasis on mission; one opportunity for pediatricians in this area is to be more overt about which causes they are supporting, Mr. Jones said. In the case of Instagram and Snapchat, pediatricians should consider creating a presence on these platforms and focusing on less text-heavy content to appeal to Millennials.
“It’s a really, really important opportunity to be able to meet the Millennials where they want to be met, and that means developing strategies to leveraging pictures and videos and other forms of Millennial content to communicate with them,” he said.
Mr. Jones reported no relevant conflicts of interest.
ORLANDO – Pediatricians can learn from how Millennials use services and purchase products from popular companies, such as Amazon Alexa, Warby Parker, Instagram, and Snapchat, and use that information to connect with Millennial parents and children in their practice, Kristopher Jones, JD, MS, said.
In a video interview, Mr. Jones explained how Amazon Alexa uses structured data as recommendations when users make queries of the service; for example, a Millennial might make a choice to book an appointment with a pediatrician based on the results Amazon Alexa displays, such as an office’s available hours. An office that is not optimized to appear in those results would be missed by those potential patients.
Warby Parker has a digital-first strategy focused on convenience, ease of use, and an emphasis on mission; one opportunity for pediatricians in this area is to be more overt about which causes they are supporting, Mr. Jones said. In the case of Instagram and Snapchat, pediatricians should consider creating a presence on these platforms and focusing on less text-heavy content to appeal to Millennials.
“It’s a really, really important opportunity to be able to meet the Millennials where they want to be met, and that means developing strategies to leveraging pictures and videos and other forms of Millennial content to communicate with them,” he said.
Mr. Jones reported no relevant conflicts of interest.
ORLANDO – Pediatricians can learn from how Millennials use services and purchase products from popular companies, such as Amazon Alexa, Warby Parker, Instagram, and Snapchat, and use that information to connect with Millennial parents and children in their practice, Kristopher Jones, JD, MS, said.
In a video interview, Mr. Jones explained how Amazon Alexa uses structured data as recommendations when users make queries of the service; for example, a Millennial might make a choice to book an appointment with a pediatrician based on the results Amazon Alexa displays, such as an office’s available hours. An office that is not optimized to appear in those results would be missed by those potential patients.
Warby Parker has a digital-first strategy focused on convenience, ease of use, and an emphasis on mission; one opportunity for pediatricians in this area is to be more overt about which causes they are supporting, Mr. Jones said. In the case of Instagram and Snapchat, pediatricians should consider creating a presence on these platforms and focusing on less text-heavy content to appeal to Millennials.
“It’s a really, really important opportunity to be able to meet the Millennials where they want to be met, and that means developing strategies to leveraging pictures and videos and other forms of Millennial content to communicate with them,” he said.
Mr. Jones reported no relevant conflicts of interest.
REPORTING FROM AAP 2018
Emergency physician describes how to prepare for disasters
, according to Dr. Toree McGowan, an emergency physician who works in a critical care facility in rural Oregon.

In our video interview at the annual meeting of the American College of Emergency Physicians, she outlined key strategies for obtaining resources and delegating care when managing mass casualties from disasters.
Dr. McGowan of the St. Charles Medical Group, Culver, Ore., said that, although she is the only physician at her rural critical care center about 70% of the time, she has established plans in place for obtaining additional staff and resources in the event of disasters. During her time in the military, she was among a team that implemented a disaster plan after a toxic chemical release at a nearby factory. The response was effective because the threat had been anticipated and a plan was in place. To develop the skills and strategies she describes in this interview, Dr. McGowan recommends free training that is available from the nonprofit National Disaster Life Support Foundation.
, according to Dr. Toree McGowan, an emergency physician who works in a critical care facility in rural Oregon.

In our video interview at the annual meeting of the American College of Emergency Physicians, she outlined key strategies for obtaining resources and delegating care when managing mass casualties from disasters.
Dr. McGowan of the St. Charles Medical Group, Culver, Ore., said that, although she is the only physician at her rural critical care center about 70% of the time, she has established plans in place for obtaining additional staff and resources in the event of disasters. During her time in the military, she was among a team that implemented a disaster plan after a toxic chemical release at a nearby factory. The response was effective because the threat had been anticipated and a plan was in place. To develop the skills and strategies she describes in this interview, Dr. McGowan recommends free training that is available from the nonprofit National Disaster Life Support Foundation.
, according to Dr. Toree McGowan, an emergency physician who works in a critical care facility in rural Oregon.

In our video interview at the annual meeting of the American College of Emergency Physicians, she outlined key strategies for obtaining resources and delegating care when managing mass casualties from disasters.
Dr. McGowan of the St. Charles Medical Group, Culver, Ore., said that, although she is the only physician at her rural critical care center about 70% of the time, she has established plans in place for obtaining additional staff and resources in the event of disasters. During her time in the military, she was among a team that implemented a disaster plan after a toxic chemical release at a nearby factory. The response was effective because the threat had been anticipated and a plan was in place. To develop the skills and strategies she describes in this interview, Dr. McGowan recommends free training that is available from the nonprofit National Disaster Life Support Foundation.
REPORTING FROM ACEP18
AAP renews public health approach to gun injury prevention
ORLANDO – The American Academy of Pediatrics created the Gun Safety and Injury Prevention Research Initiative to study and implement gun safety interventions to prevent homicide, suicide and unintentional injuries caused by firearms.
In an interview at the annual meeting of the American Academy of Pediatrics, Colleen A. Kraft, MD, FAAP, current AAP president, explained how AAP has renewed its efforts to protect children from firearm injuries. Black children are more likely to die in a homicide, while white children are more likely to die in a suicide through use of a firearm, Dr. Kraft said. The AAP seeks to find a nonpolitical way to discuss gun safety “with a lens on children and a lens on safety,” she said.
“What we are looking to do is to bring together partners who have the research expertise in gun safety and injury prevention, find out what we know, decide what we don’t know yet, and begin to bring together focus groups of parents and families and legislators and doctors, and people to talk about … gun safety in a way that resonates with everyone,” Dr. Kraft said.
Visit AAP’s website for more information on the Gun Safety and Injury Prevention Research Initiative.
Dr. Kraft reports no relevant conflicts of interest.
ORLANDO – The American Academy of Pediatrics created the Gun Safety and Injury Prevention Research Initiative to study and implement gun safety interventions to prevent homicide, suicide and unintentional injuries caused by firearms.
In an interview at the annual meeting of the American Academy of Pediatrics, Colleen A. Kraft, MD, FAAP, current AAP president, explained how AAP has renewed its efforts to protect children from firearm injuries. Black children are more likely to die in a homicide, while white children are more likely to die in a suicide through use of a firearm, Dr. Kraft said. The AAP seeks to find a nonpolitical way to discuss gun safety “with a lens on children and a lens on safety,” she said.
“What we are looking to do is to bring together partners who have the research expertise in gun safety and injury prevention, find out what we know, decide what we don’t know yet, and begin to bring together focus groups of parents and families and legislators and doctors, and people to talk about … gun safety in a way that resonates with everyone,” Dr. Kraft said.
Visit AAP’s website for more information on the Gun Safety and Injury Prevention Research Initiative.
Dr. Kraft reports no relevant conflicts of interest.
ORLANDO – The American Academy of Pediatrics created the Gun Safety and Injury Prevention Research Initiative to study and implement gun safety interventions to prevent homicide, suicide and unintentional injuries caused by firearms.
In an interview at the annual meeting of the American Academy of Pediatrics, Colleen A. Kraft, MD, FAAP, current AAP president, explained how AAP has renewed its efforts to protect children from firearm injuries. Black children are more likely to die in a homicide, while white children are more likely to die in a suicide through use of a firearm, Dr. Kraft said. The AAP seeks to find a nonpolitical way to discuss gun safety “with a lens on children and a lens on safety,” she said.
“What we are looking to do is to bring together partners who have the research expertise in gun safety and injury prevention, find out what we know, decide what we don’t know yet, and begin to bring together focus groups of parents and families and legislators and doctors, and people to talk about … gun safety in a way that resonates with everyone,” Dr. Kraft said.
Visit AAP’s website for more information on the Gun Safety and Injury Prevention Research Initiative.
Dr. Kraft reports no relevant conflicts of interest.
REPORTING FROM AAP 2018
AAP president affirms academy’s support for transgender children
ORLANDO – Many Colleen A. Kraft, MD, president of the American Academy of Pediatrics, said in an interview.
The AAP’s policy on caring and supporting these patients is evidence-based, and includes recommendations on providing appropriate health care services for transgender individuals, as well as respect and understanding for families. In the interview, Dr. Kraft, discussed the role pediatricians have in providing a safe and supportive environment for transgender and gender-diverse individuals and their families.
“[These children] need to be listened to, they need to be respected for who they are, and they need access to the appropriate health services,” Dr. Kraft said.
The AAP’s policy statement on ensuring care and support for transgender children and adolescents is available here.
Dr. Kraft reported no relevant conflicts of interest.
ORLANDO – Many Colleen A. Kraft, MD, president of the American Academy of Pediatrics, said in an interview.
The AAP’s policy on caring and supporting these patients is evidence-based, and includes recommendations on providing appropriate health care services for transgender individuals, as well as respect and understanding for families. In the interview, Dr. Kraft, discussed the role pediatricians have in providing a safe and supportive environment for transgender and gender-diverse individuals and their families.
“[These children] need to be listened to, they need to be respected for who they are, and they need access to the appropriate health services,” Dr. Kraft said.
The AAP’s policy statement on ensuring care and support for transgender children and adolescents is available here.
Dr. Kraft reported no relevant conflicts of interest.
ORLANDO – Many Colleen A. Kraft, MD, president of the American Academy of Pediatrics, said in an interview.
The AAP’s policy on caring and supporting these patients is evidence-based, and includes recommendations on providing appropriate health care services for transgender individuals, as well as respect and understanding for families. In the interview, Dr. Kraft, discussed the role pediatricians have in providing a safe and supportive environment for transgender and gender-diverse individuals and their families.
“[These children] need to be listened to, they need to be respected for who they are, and they need access to the appropriate health services,” Dr. Kraft said.
The AAP’s policy statement on ensuring care and support for transgender children and adolescents is available here.
Dr. Kraft reported no relevant conflicts of interest.
REPORTING FROM AAP 2018
Childhood abuse linked with tripled adult SLE incidence
CHICAGO – , in a study of more than 67,000 American nurses.
The results also suggested that development of depression and post-traumatic stress disorder (PTSD) may have been intermediary steps between episodes of childhood abuse and later development of systemic lupus erythematosus (SLE), Candace H. Feldman, MD, said at the annual meeting of the American College of Rheumatology.
These findings suggest the “importance of screening for childhood abuse exposures as well as for depression and PTSD in routine practice,” although Dr. Feldman acknowledged that interventions aimed at treating depression and PTSD have as of now no proven role for mitigating SLE.
The analysis Dr. Feldman and her associates ran on data collected in the Nurses Health Study II also documented a “striking” number of the enrolled women who completed the survey in 2001 and reported a history of abuse when they were 11 years old or younger: 30% of the 67,516 respondents reported a moderate level of abuse, and 24% reported a high level of abuse. An additional 22% reported either no or a very low level of abuse. These numbers suggest that abuse of girls “is very common and probably underreported,” she said in a video interview.
The Nurses Health Study II enrolled more than 116,429 U.S. women in 1989 who were 25-42 years old and had no history of SLE. Recording of incident SLE cases began in 1991 and for this analysis continued for 24 years, through 2015, during which time 94 women developed SLE that was confirmed in a review by two rheumatologists applying the 1997 SLE classification criteria (Arthritis Rheum. 1997 Sept;40[9]:1725. The incidence of SLE was 2.57-fold more common among women who reported a high level of abuse, compared with those who had no or very low abuse, after adjustment for several demographic and clinical confounders, reported Dr. Feldman, a rheumatologist at Brigham and Women’s Hospital in Boston.
“To our knowledge this is the first study to prospectively look at exposure to different forms of childhood abuse and SLE incidence in a general population of women,” she said.
To make the analysis more prospective the researchers also ran a calculation that considered only SLE cases that appeared after completion of the 2001 abuse survey. Using this criterion the incidence was 3.11-fold higher among women who reported a high level of childhood abuse. Further analyses showed that statistically a diagnosis of PTSD accounted for about 23% of the risk for developing SLE, and depression appeared responsible for about 17% of the risk. The analysis also showed no statistically significant link between sexual abuse in childhood or as a teenager and later onset of SLE.
The findings are consistent with prior reports that linked stress to development of various autoimmune diseases, Dr. Feldman noted. She speculated that high childhood stress could cause changes in inflammation, immune function, epigenetics, the autonomic nervous system, and endocrine pathways that could play a role in triggering depression or PTSD, and eventually SLE.
[email protected]
On Twitter @mitchelzoler
SOURCE:Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
CHICAGO – , in a study of more than 67,000 American nurses.
The results also suggested that development of depression and post-traumatic stress disorder (PTSD) may have been intermediary steps between episodes of childhood abuse and later development of systemic lupus erythematosus (SLE), Candace H. Feldman, MD, said at the annual meeting of the American College of Rheumatology.
These findings suggest the “importance of screening for childhood abuse exposures as well as for depression and PTSD in routine practice,” although Dr. Feldman acknowledged that interventions aimed at treating depression and PTSD have as of now no proven role for mitigating SLE.
The analysis Dr. Feldman and her associates ran on data collected in the Nurses Health Study II also documented a “striking” number of the enrolled women who completed the survey in 2001 and reported a history of abuse when they were 11 years old or younger: 30% of the 67,516 respondents reported a moderate level of abuse, and 24% reported a high level of abuse. An additional 22% reported either no or a very low level of abuse. These numbers suggest that abuse of girls “is very common and probably underreported,” she said in a video interview.
The Nurses Health Study II enrolled more than 116,429 U.S. women in 1989 who were 25-42 years old and had no history of SLE. Recording of incident SLE cases began in 1991 and for this analysis continued for 24 years, through 2015, during which time 94 women developed SLE that was confirmed in a review by two rheumatologists applying the 1997 SLE classification criteria (Arthritis Rheum. 1997 Sept;40[9]:1725. The incidence of SLE was 2.57-fold more common among women who reported a high level of abuse, compared with those who had no or very low abuse, after adjustment for several demographic and clinical confounders, reported Dr. Feldman, a rheumatologist at Brigham and Women’s Hospital in Boston.
“To our knowledge this is the first study to prospectively look at exposure to different forms of childhood abuse and SLE incidence in a general population of women,” she said.
To make the analysis more prospective the researchers also ran a calculation that considered only SLE cases that appeared after completion of the 2001 abuse survey. Using this criterion the incidence was 3.11-fold higher among women who reported a high level of childhood abuse. Further analyses showed that statistically a diagnosis of PTSD accounted for about 23% of the risk for developing SLE, and depression appeared responsible for about 17% of the risk. The analysis also showed no statistically significant link between sexual abuse in childhood or as a teenager and later onset of SLE.
The findings are consistent with prior reports that linked stress to development of various autoimmune diseases, Dr. Feldman noted. She speculated that high childhood stress could cause changes in inflammation, immune function, epigenetics, the autonomic nervous system, and endocrine pathways that could play a role in triggering depression or PTSD, and eventually SLE.
[email protected]
On Twitter @mitchelzoler
SOURCE:Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
CHICAGO – , in a study of more than 67,000 American nurses.
The results also suggested that development of depression and post-traumatic stress disorder (PTSD) may have been intermediary steps between episodes of childhood abuse and later development of systemic lupus erythematosus (SLE), Candace H. Feldman, MD, said at the annual meeting of the American College of Rheumatology.
These findings suggest the “importance of screening for childhood abuse exposures as well as for depression and PTSD in routine practice,” although Dr. Feldman acknowledged that interventions aimed at treating depression and PTSD have as of now no proven role for mitigating SLE.
The analysis Dr. Feldman and her associates ran on data collected in the Nurses Health Study II also documented a “striking” number of the enrolled women who completed the survey in 2001 and reported a history of abuse when they were 11 years old or younger: 30% of the 67,516 respondents reported a moderate level of abuse, and 24% reported a high level of abuse. An additional 22% reported either no or a very low level of abuse. These numbers suggest that abuse of girls “is very common and probably underreported,” she said in a video interview.
The Nurses Health Study II enrolled more than 116,429 U.S. women in 1989 who were 25-42 years old and had no history of SLE. Recording of incident SLE cases began in 1991 and for this analysis continued for 24 years, through 2015, during which time 94 women developed SLE that was confirmed in a review by two rheumatologists applying the 1997 SLE classification criteria (Arthritis Rheum. 1997 Sept;40[9]:1725. The incidence of SLE was 2.57-fold more common among women who reported a high level of abuse, compared with those who had no or very low abuse, after adjustment for several demographic and clinical confounders, reported Dr. Feldman, a rheumatologist at Brigham and Women’s Hospital in Boston.
“To our knowledge this is the first study to prospectively look at exposure to different forms of childhood abuse and SLE incidence in a general population of women,” she said.
To make the analysis more prospective the researchers also ran a calculation that considered only SLE cases that appeared after completion of the 2001 abuse survey. Using this criterion the incidence was 3.11-fold higher among women who reported a high level of childhood abuse. Further analyses showed that statistically a diagnosis of PTSD accounted for about 23% of the risk for developing SLE, and depression appeared responsible for about 17% of the risk. The analysis also showed no statistically significant link between sexual abuse in childhood or as a teenager and later onset of SLE.
The findings are consistent with prior reports that linked stress to development of various autoimmune diseases, Dr. Feldman noted. She speculated that high childhood stress could cause changes in inflammation, immune function, epigenetics, the autonomic nervous system, and endocrine pathways that could play a role in triggering depression or PTSD, and eventually SLE.
[email protected]
On Twitter @mitchelzoler
SOURCE:Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: A history of high childhood abuse linked with a nearly three-fold higher incidence of systemic lupus erythematosus during adulthood.
Major finding: The incidence of systemic lupus erythematosus was 2.57-fold higher among women with high childhood abuse compared with unabused women.
Study details: Data from 67,516 women enrolled in the Nurses Health Study II.
Disclosures: Dr. Feldman had no disclosures.
Source: Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
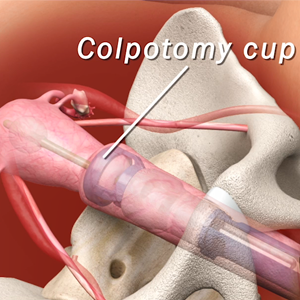
The art of manipulation: Simplifying hysterectomy by preparing the learner
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
- Vaginal and bilateral thigh removal of a transobturator sling
- Morcellation at the time of vaginal hysterectomy
- Surgical management of non-tubal ectopic pregnancies
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
- Vaginal and bilateral thigh removal of a transobturator sling
- Morcellation at the time of vaginal hysterectomy
- Surgical management of non-tubal ectopic pregnancies
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
- Vaginal and bilateral thigh removal of a transobturator sling
- Morcellation at the time of vaginal hysterectomy
- Surgical management of non-tubal ectopic pregnancies
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This video is brought to you by