User login
Obesity is diverticula risk factor in women, not men
SAN DIEGO – Obesity is a risk factor for colonic diverticulosis among women but not men, while a low-fiber diet was not found to be a risk factor in a recent study reported at the annual Digestive Disease Week.
“The classic teaching in medical school is that a low-fiber diet increases constipation, which in turn increases the risk of diverticula,” explained lead author Dr. Anne Peery, assistant professor of medicine at the University of North Carolina, Chapel Hill. “This is in textbooks and on your boards. But there is no association between low-fiber dietary intake and diverticula.
“There is, however, evidence from other studies that a high-fiber diet and increased physical activity decrease the risk of developing complications from diverticula,” Dr. Peery added. She noted that the study was designed to look at risk factors for developing diverticula, not at complications.
“The provocative findings from our study are twofold: We found that the prevalence of diverticula is higher in men and lower in women younger than age 50, and that obesity is a risk factor for diverticula in women but not in men,” Dr Peery said.
“The age-related gender differences we identified were quite surprising, and suggest that something is going on in women under the age of 50 that may be estrogen-related. This opens up an avenue of research,” she noted.
Colonic diverticula are common, and they are important because of complications such as hemorrhage, perforation, and inflammation. They also pose a substantial health burden, accounting for 2.5 million office visits and 4,500 deaths each year in the United States.
“Despite this, we know very little about risk factors for colonic diverticula,” Dr. Peery noted.
The prospective study recruited 624 patients between the ages of 30 years and 80 years undergoing a first screening colonoscopy between 2013 and 2015 at the University of North Carolina in Chapel Hill. Prior to undergoing the procedure, each participant was interviewed using validated instruments to assess diet and physical activity. Each participant had a detailed examination for colonic diverticula, with a research assistant present during the entire colonoscopy.
“The presence or absence of diverticula reported in previous studies were extracted from colonoscopy reports. Our study assessed risk factors prior to undergoing colonoscopy,” she emphasized. “This is one of the study strengths.”
Not surprisingly, the study showed that the prevalence of diverticula (or “tics”) increased with age. Younger than age 50, the prevalence was higher in men than in women, after which prevalence equalized with age.
In the study population, 124 men had diverticula and 150 did not; 136 women had diverticula and 214 did not. Women with diverticula were more likely to be older, white, and have a higher body mass index (BMI).
The investigators looked at several measures of obesity, including BMI, waist circumference, and waist-to-height ratio. Women with greater BMI were at increased risk for diverticula, a risk relationship that was not seen in men. The risk of developing six or more diverticula was more than twofold greater in obese women.
Men with a greater waist circumference (more than 102 cm) had no increased risk for diverticula, while women with a greater waist circumference (more than 88 cm) were at increased risk of any diverticula, as well as having six or more diverticula.
A similar pattern was observed for waist-to-height ratio, which some experts believe is related to obesity, according to Dr. Peery. No association was found in men. But for women, a high-risk waist-to-height ratio increased the risk of diverticula, and the risk of having six or more diverticula was almost twice as great in these women, compared with men.
The investigators then measured the association between dietary fiber and physical activity with diverticula. No associations with diverticula were found in any quartile (lowest to highest) for both physical activity and dietary fiber intake.
In an interview, Dr. Peery speculated on why women have a lower prevalence of “tics,” compared with men younger than age 50. She said there are gender-related differences in the way fat is stored and metabolized.
“Obese women have more visceral adiposity that men, and they tend to eat more carbohydrates, while obese men have higher alcohol and meat intake. These differences will be studied in greater depth as they relate to diverticula and complications,” she noted.
SAN DIEGO – Obesity is a risk factor for colonic diverticulosis among women but not men, while a low-fiber diet was not found to be a risk factor in a recent study reported at the annual Digestive Disease Week.
“The classic teaching in medical school is that a low-fiber diet increases constipation, which in turn increases the risk of diverticula,” explained lead author Dr. Anne Peery, assistant professor of medicine at the University of North Carolina, Chapel Hill. “This is in textbooks and on your boards. But there is no association between low-fiber dietary intake and diverticula.
“There is, however, evidence from other studies that a high-fiber diet and increased physical activity decrease the risk of developing complications from diverticula,” Dr. Peery added. She noted that the study was designed to look at risk factors for developing diverticula, not at complications.
“The provocative findings from our study are twofold: We found that the prevalence of diverticula is higher in men and lower in women younger than age 50, and that obesity is a risk factor for diverticula in women but not in men,” Dr Peery said.
“The age-related gender differences we identified were quite surprising, and suggest that something is going on in women under the age of 50 that may be estrogen-related. This opens up an avenue of research,” she noted.
Colonic diverticula are common, and they are important because of complications such as hemorrhage, perforation, and inflammation. They also pose a substantial health burden, accounting for 2.5 million office visits and 4,500 deaths each year in the United States.
“Despite this, we know very little about risk factors for colonic diverticula,” Dr. Peery noted.
The prospective study recruited 624 patients between the ages of 30 years and 80 years undergoing a first screening colonoscopy between 2013 and 2015 at the University of North Carolina in Chapel Hill. Prior to undergoing the procedure, each participant was interviewed using validated instruments to assess diet and physical activity. Each participant had a detailed examination for colonic diverticula, with a research assistant present during the entire colonoscopy.
“The presence or absence of diverticula reported in previous studies were extracted from colonoscopy reports. Our study assessed risk factors prior to undergoing colonoscopy,” she emphasized. “This is one of the study strengths.”
Not surprisingly, the study showed that the prevalence of diverticula (or “tics”) increased with age. Younger than age 50, the prevalence was higher in men than in women, after which prevalence equalized with age.
In the study population, 124 men had diverticula and 150 did not; 136 women had diverticula and 214 did not. Women with diverticula were more likely to be older, white, and have a higher body mass index (BMI).
The investigators looked at several measures of obesity, including BMI, waist circumference, and waist-to-height ratio. Women with greater BMI were at increased risk for diverticula, a risk relationship that was not seen in men. The risk of developing six or more diverticula was more than twofold greater in obese women.
Men with a greater waist circumference (more than 102 cm) had no increased risk for diverticula, while women with a greater waist circumference (more than 88 cm) were at increased risk of any diverticula, as well as having six or more diverticula.
A similar pattern was observed for waist-to-height ratio, which some experts believe is related to obesity, according to Dr. Peery. No association was found in men. But for women, a high-risk waist-to-height ratio increased the risk of diverticula, and the risk of having six or more diverticula was almost twice as great in these women, compared with men.
The investigators then measured the association between dietary fiber and physical activity with diverticula. No associations with diverticula were found in any quartile (lowest to highest) for both physical activity and dietary fiber intake.
In an interview, Dr. Peery speculated on why women have a lower prevalence of “tics,” compared with men younger than age 50. She said there are gender-related differences in the way fat is stored and metabolized.
“Obese women have more visceral adiposity that men, and they tend to eat more carbohydrates, while obese men have higher alcohol and meat intake. These differences will be studied in greater depth as they relate to diverticula and complications,” she noted.
SAN DIEGO – Obesity is a risk factor for colonic diverticulosis among women but not men, while a low-fiber diet was not found to be a risk factor in a recent study reported at the annual Digestive Disease Week.
“The classic teaching in medical school is that a low-fiber diet increases constipation, which in turn increases the risk of diverticula,” explained lead author Dr. Anne Peery, assistant professor of medicine at the University of North Carolina, Chapel Hill. “This is in textbooks and on your boards. But there is no association between low-fiber dietary intake and diverticula.
“There is, however, evidence from other studies that a high-fiber diet and increased physical activity decrease the risk of developing complications from diverticula,” Dr. Peery added. She noted that the study was designed to look at risk factors for developing diverticula, not at complications.
“The provocative findings from our study are twofold: We found that the prevalence of diverticula is higher in men and lower in women younger than age 50, and that obesity is a risk factor for diverticula in women but not in men,” Dr Peery said.
“The age-related gender differences we identified were quite surprising, and suggest that something is going on in women under the age of 50 that may be estrogen-related. This opens up an avenue of research,” she noted.
Colonic diverticula are common, and they are important because of complications such as hemorrhage, perforation, and inflammation. They also pose a substantial health burden, accounting for 2.5 million office visits and 4,500 deaths each year in the United States.
“Despite this, we know very little about risk factors for colonic diverticula,” Dr. Peery noted.
The prospective study recruited 624 patients between the ages of 30 years and 80 years undergoing a first screening colonoscopy between 2013 and 2015 at the University of North Carolina in Chapel Hill. Prior to undergoing the procedure, each participant was interviewed using validated instruments to assess diet and physical activity. Each participant had a detailed examination for colonic diverticula, with a research assistant present during the entire colonoscopy.
“The presence or absence of diverticula reported in previous studies were extracted from colonoscopy reports. Our study assessed risk factors prior to undergoing colonoscopy,” she emphasized. “This is one of the study strengths.”
Not surprisingly, the study showed that the prevalence of diverticula (or “tics”) increased with age. Younger than age 50, the prevalence was higher in men than in women, after which prevalence equalized with age.
In the study population, 124 men had diverticula and 150 did not; 136 women had diverticula and 214 did not. Women with diverticula were more likely to be older, white, and have a higher body mass index (BMI).
The investigators looked at several measures of obesity, including BMI, waist circumference, and waist-to-height ratio. Women with greater BMI were at increased risk for diverticula, a risk relationship that was not seen in men. The risk of developing six or more diverticula was more than twofold greater in obese women.
Men with a greater waist circumference (more than 102 cm) had no increased risk for diverticula, while women with a greater waist circumference (more than 88 cm) were at increased risk of any diverticula, as well as having six or more diverticula.
A similar pattern was observed for waist-to-height ratio, which some experts believe is related to obesity, according to Dr. Peery. No association was found in men. But for women, a high-risk waist-to-height ratio increased the risk of diverticula, and the risk of having six or more diverticula was almost twice as great in these women, compared with men.
The investigators then measured the association between dietary fiber and physical activity with diverticula. No associations with diverticula were found in any quartile (lowest to highest) for both physical activity and dietary fiber intake.
In an interview, Dr. Peery speculated on why women have a lower prevalence of “tics,” compared with men younger than age 50. She said there are gender-related differences in the way fat is stored and metabolized.
“Obese women have more visceral adiposity that men, and they tend to eat more carbohydrates, while obese men have higher alcohol and meat intake. These differences will be studied in greater depth as they relate to diverticula and complications,” she noted.
AT DDW® 2016
Key clinical point: Obesity is associated with diverticula in women, not men, and a low-fiber diet is not a risk factor.
Major finding: Younger than age 50 years, men were more likely to have diverticula, and obese women were twice as likely as men to have six or more diverticula.
Data source: A prospective, cross-sectional study.
Disclosures: The National Institutes of Health sponsored the study.
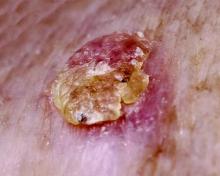
SCCA2: Potential biomarker for psoriasis severity and treatment efficacy
The level of serum squamous cell carcinoma antigen 2 – an isoform of SCCA that is widely used as a tumor marker for SCC – was significantly higher in both skin and serum of patients with psoriasis, compared with healthy volunteers in a recent study, correlating with psoriasis severity score and reflecting treatment efficacy.
The intensity of skin and serum levels of SCCA2 was correlated in patients with psoriasis, and the study results also suggest that Th17 cytokines (IL-17 and IL-22) induce SCCA 2 elevation in serum and skin. “Significant elevation of SCCA2 is associated with disease severity and reflects treatment efficacy. SCCA2 may be a useful biomarker in psoriasis, reflecting Th17-type inflammation – the main determinant of the severity of psoriasis,” wrote Dr. Yuko Watanabe of Yokohama (Japan) City University and associates (Br J Derm. 2016 Jan 29. doi: 10.1111/bjd.14426).
According to the investigators, the commonly used psoriasis area severity index (PASI) is suboptimal because it is not truly quantitative and varies among clinicians. Since there are several new treatment options for psoriasis, including biologics, the authors believe that a new serum marker for psoriasis is needed to evaluate disease activity and manage treatment.
The prospective, cross-sectional study included 123 patients with psoriasis and 25 healthy controls. Serum SCCA2 levels were significantly higher in patients with psoriasis, compared with controls: a median of 2.7 ng/mL versus 0.70 ng/mL, respectively (P <.0001). Serum SCCA2 levels were positively correlated with PASI for all patients with psoriasis, regardless of subtype. In 38 patients on monotherapy or combination therapy with drugs to treat psoriasis, SCCA2 levels decreased in the 35 patients whose PASI improved on treatment (P <.0001) and increased in the three cases of clinical deterioration.
The study was supported by a grant from Japan’s Ministry of Education, Culture, Sports, Science and Technology. The investigators declared that they had no conflicts of interest.
The level of serum squamous cell carcinoma antigen 2 – an isoform of SCCA that is widely used as a tumor marker for SCC – was significantly higher in both skin and serum of patients with psoriasis, compared with healthy volunteers in a recent study, correlating with psoriasis severity score and reflecting treatment efficacy.
The intensity of skin and serum levels of SCCA2 was correlated in patients with psoriasis, and the study results also suggest that Th17 cytokines (IL-17 and IL-22) induce SCCA 2 elevation in serum and skin. “Significant elevation of SCCA2 is associated with disease severity and reflects treatment efficacy. SCCA2 may be a useful biomarker in psoriasis, reflecting Th17-type inflammation – the main determinant of the severity of psoriasis,” wrote Dr. Yuko Watanabe of Yokohama (Japan) City University and associates (Br J Derm. 2016 Jan 29. doi: 10.1111/bjd.14426).
According to the investigators, the commonly used psoriasis area severity index (PASI) is suboptimal because it is not truly quantitative and varies among clinicians. Since there are several new treatment options for psoriasis, including biologics, the authors believe that a new serum marker for psoriasis is needed to evaluate disease activity and manage treatment.
The prospective, cross-sectional study included 123 patients with psoriasis and 25 healthy controls. Serum SCCA2 levels were significantly higher in patients with psoriasis, compared with controls: a median of 2.7 ng/mL versus 0.70 ng/mL, respectively (P <.0001). Serum SCCA2 levels were positively correlated with PASI for all patients with psoriasis, regardless of subtype. In 38 patients on monotherapy or combination therapy with drugs to treat psoriasis, SCCA2 levels decreased in the 35 patients whose PASI improved on treatment (P <.0001) and increased in the three cases of clinical deterioration.
The study was supported by a grant from Japan’s Ministry of Education, Culture, Sports, Science and Technology. The investigators declared that they had no conflicts of interest.
The level of serum squamous cell carcinoma antigen 2 – an isoform of SCCA that is widely used as a tumor marker for SCC – was significantly higher in both skin and serum of patients with psoriasis, compared with healthy volunteers in a recent study, correlating with psoriasis severity score and reflecting treatment efficacy.
The intensity of skin and serum levels of SCCA2 was correlated in patients with psoriasis, and the study results also suggest that Th17 cytokines (IL-17 and IL-22) induce SCCA 2 elevation in serum and skin. “Significant elevation of SCCA2 is associated with disease severity and reflects treatment efficacy. SCCA2 may be a useful biomarker in psoriasis, reflecting Th17-type inflammation – the main determinant of the severity of psoriasis,” wrote Dr. Yuko Watanabe of Yokohama (Japan) City University and associates (Br J Derm. 2016 Jan 29. doi: 10.1111/bjd.14426).
According to the investigators, the commonly used psoriasis area severity index (PASI) is suboptimal because it is not truly quantitative and varies among clinicians. Since there are several new treatment options for psoriasis, including biologics, the authors believe that a new serum marker for psoriasis is needed to evaluate disease activity and manage treatment.
The prospective, cross-sectional study included 123 patients with psoriasis and 25 healthy controls. Serum SCCA2 levels were significantly higher in patients with psoriasis, compared with controls: a median of 2.7 ng/mL versus 0.70 ng/mL, respectively (P <.0001). Serum SCCA2 levels were positively correlated with PASI for all patients with psoriasis, regardless of subtype. In 38 patients on monotherapy or combination therapy with drugs to treat psoriasis, SCCA2 levels decreased in the 35 patients whose PASI improved on treatment (P <.0001) and increased in the three cases of clinical deterioration.
The study was supported by a grant from Japan’s Ministry of Education, Culture, Sports, Science and Technology. The investigators declared that they had no conflicts of interest.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Average person with atopic dermatitis has no increased risk of actinic keratosis or nonmelanoma skin cancer
People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer, according to a recent population-based, cross-sectional study.
“This is the first study to examine the association between atopic dermatitis and actinic keratosis [AK]. Our findings suggest that within a population-based sample, atopic dermatitis patients do not have more AKs than the rest of the population. Patients with atopic dermatitis were not found to have more AKs or keratotic cancers [basal or squamous cell cancers]. Moreover, individuals with atopic dermatitis seem to be less likely to develop multiple AKs,” said Dr. Enes Hajdarbegovic and his associates of the Erasmus Medical Centre, Rotterdam, the Netherlands.
The study is part of an ongoing, prospective, Dutch population-based cohort study that follows people in a district of Rotterdam since 1990. There are now 14,926 participants in the database. The current study included 4,375 participants who had undergone full body skin examinations; 56% of patients were female, and the mean age was 68 years (Br J Dermatol. 2016 Jan 29. doi: 10.1111/bjd.14423).
Twenty-four percent had 1 or more AKs; 57% had 1-3 of these lesions; 23% had 4-9, and 20% had more than 10. The mean age of participants with AK was significantly higher, compared with those without AK (73 years vs. 66 years; P less than .01).
Of the 4,375 participants screened, 6.3% met the diagnostic criteria for atopic dermatitis. A lower proportion of those with atopic dermatitis had AK: 16% vs. 24%, respectively (P = .002). In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more AKs than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted odds ratio, 0.71) and squamous cell cancer (adjusted OR, 1.54).
The authors explained that it is already known that patients with severe atopic dermatitis exposed to ultraviolet light and immunosuppressants are at increased risk of keratinocyte malignancies. This study shows that a community-dwelling person with moderate atopic dermatitis does not develop more AKs or keratinocyte cancers.
The investigators said they had no relevant financial disclosures.
People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer, according to a recent population-based, cross-sectional study.
“This is the first study to examine the association between atopic dermatitis and actinic keratosis [AK]. Our findings suggest that within a population-based sample, atopic dermatitis patients do not have more AKs than the rest of the population. Patients with atopic dermatitis were not found to have more AKs or keratotic cancers [basal or squamous cell cancers]. Moreover, individuals with atopic dermatitis seem to be less likely to develop multiple AKs,” said Dr. Enes Hajdarbegovic and his associates of the Erasmus Medical Centre, Rotterdam, the Netherlands.
The study is part of an ongoing, prospective, Dutch population-based cohort study that follows people in a district of Rotterdam since 1990. There are now 14,926 participants in the database. The current study included 4,375 participants who had undergone full body skin examinations; 56% of patients were female, and the mean age was 68 years (Br J Dermatol. 2016 Jan 29. doi: 10.1111/bjd.14423).
Twenty-four percent had 1 or more AKs; 57% had 1-3 of these lesions; 23% had 4-9, and 20% had more than 10. The mean age of participants with AK was significantly higher, compared with those without AK (73 years vs. 66 years; P less than .01).
Of the 4,375 participants screened, 6.3% met the diagnostic criteria for atopic dermatitis. A lower proportion of those with atopic dermatitis had AK: 16% vs. 24%, respectively (P = .002). In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more AKs than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted odds ratio, 0.71) and squamous cell cancer (adjusted OR, 1.54).
The authors explained that it is already known that patients with severe atopic dermatitis exposed to ultraviolet light and immunosuppressants are at increased risk of keratinocyte malignancies. This study shows that a community-dwelling person with moderate atopic dermatitis does not develop more AKs or keratinocyte cancers.
The investigators said they had no relevant financial disclosures.
People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer, according to a recent population-based, cross-sectional study.
“This is the first study to examine the association between atopic dermatitis and actinic keratosis [AK]. Our findings suggest that within a population-based sample, atopic dermatitis patients do not have more AKs than the rest of the population. Patients with atopic dermatitis were not found to have more AKs or keratotic cancers [basal or squamous cell cancers]. Moreover, individuals with atopic dermatitis seem to be less likely to develop multiple AKs,” said Dr. Enes Hajdarbegovic and his associates of the Erasmus Medical Centre, Rotterdam, the Netherlands.
The study is part of an ongoing, prospective, Dutch population-based cohort study that follows people in a district of Rotterdam since 1990. There are now 14,926 participants in the database. The current study included 4,375 participants who had undergone full body skin examinations; 56% of patients were female, and the mean age was 68 years (Br J Dermatol. 2016 Jan 29. doi: 10.1111/bjd.14423).
Twenty-four percent had 1 or more AKs; 57% had 1-3 of these lesions; 23% had 4-9, and 20% had more than 10. The mean age of participants with AK was significantly higher, compared with those without AK (73 years vs. 66 years; P less than .01).
Of the 4,375 participants screened, 6.3% met the diagnostic criteria for atopic dermatitis. A lower proportion of those with atopic dermatitis had AK: 16% vs. 24%, respectively (P = .002). In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more AKs than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted odds ratio, 0.71) and squamous cell cancer (adjusted OR, 1.54).
The authors explained that it is already known that patients with severe atopic dermatitis exposed to ultraviolet light and immunosuppressants are at increased risk of keratinocyte malignancies. This study shows that a community-dwelling person with moderate atopic dermatitis does not develop more AKs or keratinocyte cancers.
The investigators said they had no relevant financial disclosures.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer.
Major finding: In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more actinic keratoses than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted OR, 0.71) and squamous cell cancer (adjusted OR, 1.54).
Data source: A prospective, Dutch population-based cohort study of 4,375 participants who had undergone full body skin examinations.
Disclosures: The investigators said they had no relevant financial disclosures.
Early-wheezing Patterns Prefigure Adolescent Respiratory Outcomes and Asthma
Wheezing patterns in early childhood can predict pulmonary function and the development of asthma in adolescence in a high-risk population, a study finds.
The study validates four clinically distinct early-life wheezing phenotypes identified by the landmark Tucson Children’s Respiratory Study in a high-risk population:
• Never.
• Transient early – wheezing before age 3 years but not at age 6 years.
• Late onset – wheezing at age 6 years but not before age 3 years.
• Persistent – wheezing before age 3 years and at age 6 years.
Previously, these phenotypes were shown to be associated with respiratory outcomes in adolescence but not with diagnosed asthma or in genetically predisposed children. The present study extends the associations with these early phenotypes to a high-risk adolescent population, said Meghan B. Azad, Ph.D., of the University of Manitoba, Winnipeg, and her associates.
The study findings were based on findings in 459 children previously enrolled in the Canadian Asthma Primary Prevention Study cohort; this was a prenatally randomized prevention trial in children at high genetic risk for asthma. The distribution of early-wheeze phenotypes was 51% never, 28% transient early, 9% late onset, and 13% persistent (JAMA Pediatrics. 2016 Feb 8. doi: 10.1001/jamapediatrics.2015.4127).
Across all four phenotypes, the authors found a strong gradient of decreasing lung function and increasing asthma risk by age 15 years. Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: the prevalence of asthma was 5% among never, 19% among transient early, 27% among late onset, and 42% among persistent phenotypes.
At age 15, early-wheezing phenotypes were not associated with atopic dermatitis or allergic rhinitis. Atopy before 2 years of age was associated with persistent wheeze, which was in turn associated with a 12-fold increased risk of diagnosed asthma by age 15.
“Our results are consistent with other cohorts” and the study “extends these findings through adolescence in a high-risk cohort and demonstrates that asthma-associated deficits are already present at a young age. Collectively, these data show that early wheezing patterns provide clinically meaningful information and suggest that strategies to reduce early-life wheezing and atopic sensitization could have long-term health benefits,” Dr. Azad and her colleagues concluded.
Proven strategies to prevent wheezing include avoiding dust, pets, and tobacco smoke; encouragement of breastfeeding; and delayed introduction of solid foods.
The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
Wheezing patterns in early childhood can predict pulmonary function and the development of asthma in adolescence in a high-risk population, a study finds.
The study validates four clinically distinct early-life wheezing phenotypes identified by the landmark Tucson Children’s Respiratory Study in a high-risk population:
• Never.
• Transient early – wheezing before age 3 years but not at age 6 years.
• Late onset – wheezing at age 6 years but not before age 3 years.
• Persistent – wheezing before age 3 years and at age 6 years.
Previously, these phenotypes were shown to be associated with respiratory outcomes in adolescence but not with diagnosed asthma or in genetically predisposed children. The present study extends the associations with these early phenotypes to a high-risk adolescent population, said Meghan B. Azad, Ph.D., of the University of Manitoba, Winnipeg, and her associates.
The study findings were based on findings in 459 children previously enrolled in the Canadian Asthma Primary Prevention Study cohort; this was a prenatally randomized prevention trial in children at high genetic risk for asthma. The distribution of early-wheeze phenotypes was 51% never, 28% transient early, 9% late onset, and 13% persistent (JAMA Pediatrics. 2016 Feb 8. doi: 10.1001/jamapediatrics.2015.4127).
Across all four phenotypes, the authors found a strong gradient of decreasing lung function and increasing asthma risk by age 15 years. Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: the prevalence of asthma was 5% among never, 19% among transient early, 27% among late onset, and 42% among persistent phenotypes.
At age 15, early-wheezing phenotypes were not associated with atopic dermatitis or allergic rhinitis. Atopy before 2 years of age was associated with persistent wheeze, which was in turn associated with a 12-fold increased risk of diagnosed asthma by age 15.
“Our results are consistent with other cohorts” and the study “extends these findings through adolescence in a high-risk cohort and demonstrates that asthma-associated deficits are already present at a young age. Collectively, these data show that early wheezing patterns provide clinically meaningful information and suggest that strategies to reduce early-life wheezing and atopic sensitization could have long-term health benefits,” Dr. Azad and her colleagues concluded.
Proven strategies to prevent wheezing include avoiding dust, pets, and tobacco smoke; encouragement of breastfeeding; and delayed introduction of solid foods.
The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
Wheezing patterns in early childhood can predict pulmonary function and the development of asthma in adolescence in a high-risk population, a study finds.
The study validates four clinically distinct early-life wheezing phenotypes identified by the landmark Tucson Children’s Respiratory Study in a high-risk population:
• Never.
• Transient early – wheezing before age 3 years but not at age 6 years.
• Late onset – wheezing at age 6 years but not before age 3 years.
• Persistent – wheezing before age 3 years and at age 6 years.
Previously, these phenotypes were shown to be associated with respiratory outcomes in adolescence but not with diagnosed asthma or in genetically predisposed children. The present study extends the associations with these early phenotypes to a high-risk adolescent population, said Meghan B. Azad, Ph.D., of the University of Manitoba, Winnipeg, and her associates.
The study findings were based on findings in 459 children previously enrolled in the Canadian Asthma Primary Prevention Study cohort; this was a prenatally randomized prevention trial in children at high genetic risk for asthma. The distribution of early-wheeze phenotypes was 51% never, 28% transient early, 9% late onset, and 13% persistent (JAMA Pediatrics. 2016 Feb 8. doi: 10.1001/jamapediatrics.2015.4127).
Across all four phenotypes, the authors found a strong gradient of decreasing lung function and increasing asthma risk by age 15 years. Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: the prevalence of asthma was 5% among never, 19% among transient early, 27% among late onset, and 42% among persistent phenotypes.
At age 15, early-wheezing phenotypes were not associated with atopic dermatitis or allergic rhinitis. Atopy before 2 years of age was associated with persistent wheeze, which was in turn associated with a 12-fold increased risk of diagnosed asthma by age 15.
“Our results are consistent with other cohorts” and the study “extends these findings through adolescence in a high-risk cohort and demonstrates that asthma-associated deficits are already present at a young age. Collectively, these data show that early wheezing patterns provide clinically meaningful information and suggest that strategies to reduce early-life wheezing and atopic sensitization could have long-term health benefits,” Dr. Azad and her colleagues concluded.
Proven strategies to prevent wheezing include avoiding dust, pets, and tobacco smoke; encouragement of breastfeeding; and delayed introduction of solid foods.
The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
FROM JAMA PEDIATRICS
Early-wheezing patterns prefigure adolescent respiratory outcomes and asthma
Wheezing patterns in early childhood can predict pulmonary function and the development of asthma in adolescence in a high-risk population, a study finds.
The study validates four clinically distinct early-life wheezing phenotypes identified by the landmark Tucson Children’s Respiratory Study in a high-risk population:
• Never.
• Transient early – wheezing before age 3 years but not at age 6 years.
• Late onset – wheezing at age 6 years but not before age 3 years.
• Persistent – wheezing before age 3 years and at age 6 years.
Previously, these phenotypes were shown to be associated with respiratory outcomes in adolescence but not with diagnosed asthma or in genetically predisposed children. The present study extends the associations with these early phenotypes to a high-risk adolescent population, said Meghan B. Azad, Ph.D., of the University of Manitoba, Winnipeg, and her associates.
The study findings were based on findings in 459 children previously enrolled in the Canadian Asthma Primary Prevention Study cohort; this was a prenatally randomized prevention trial in children at high genetic risk for asthma. The distribution of early-wheeze phenotypes was 51% never, 28% transient early, 9% late onset, and 13% persistent (JAMA Pediatrics. 2016 Feb 8. doi: 10.1001/jamapediatrics.2015.4127).
Across all four phenotypes, the authors found a strong gradient of decreasing lung function and increasing asthma risk by age 15 years. Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: the prevalence of asthma was 5% among never, 19% among transient early, 27% among late onset, and 42% among persistent phenotypes.
At age 15, early-wheezing phenotypes were not associated with atopic dermatitis or allergic rhinitis. Atopy before 2 years of age was associated with persistent wheeze, which was in turn associated with a 12-fold increased risk of diagnosed asthma by age 15.
“Our results are consistent with other cohorts” and the study “extends these findings through adolescence in a high-risk cohort and demonstrates that asthma-associated deficits are already present at a young age. Collectively, these data show that early wheezing patterns provide clinically meaningful information and suggest that strategies to reduce early-life wheezing and atopic sensitization could have long-term health benefits,” Dr. Azad and her colleagues concluded.
Proven strategies to prevent wheezing include avoiding dust, pets, and tobacco smoke; encouragement of breastfeeding; and delayed introduction of solid foods.
The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
Wheezing patterns in early childhood can predict pulmonary function and the development of asthma in adolescence in a high-risk population, a study finds.
The study validates four clinically distinct early-life wheezing phenotypes identified by the landmark Tucson Children’s Respiratory Study in a high-risk population:
• Never.
• Transient early – wheezing before age 3 years but not at age 6 years.
• Late onset – wheezing at age 6 years but not before age 3 years.
• Persistent – wheezing before age 3 years and at age 6 years.
Previously, these phenotypes were shown to be associated with respiratory outcomes in adolescence but not with diagnosed asthma or in genetically predisposed children. The present study extends the associations with these early phenotypes to a high-risk adolescent population, said Meghan B. Azad, Ph.D., of the University of Manitoba, Winnipeg, and her associates.
The study findings were based on findings in 459 children previously enrolled in the Canadian Asthma Primary Prevention Study cohort; this was a prenatally randomized prevention trial in children at high genetic risk for asthma. The distribution of early-wheeze phenotypes was 51% never, 28% transient early, 9% late onset, and 13% persistent (JAMA Pediatrics. 2016 Feb 8. doi: 10.1001/jamapediatrics.2015.4127).
Across all four phenotypes, the authors found a strong gradient of decreasing lung function and increasing asthma risk by age 15 years. Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: the prevalence of asthma was 5% among never, 19% among transient early, 27% among late onset, and 42% among persistent phenotypes.
At age 15, early-wheezing phenotypes were not associated with atopic dermatitis or allergic rhinitis. Atopy before 2 years of age was associated with persistent wheeze, which was in turn associated with a 12-fold increased risk of diagnosed asthma by age 15.
“Our results are consistent with other cohorts” and the study “extends these findings through adolescence in a high-risk cohort and demonstrates that asthma-associated deficits are already present at a young age. Collectively, these data show that early wheezing patterns provide clinically meaningful information and suggest that strategies to reduce early-life wheezing and atopic sensitization could have long-term health benefits,” Dr. Azad and her colleagues concluded.
Proven strategies to prevent wheezing include avoiding dust, pets, and tobacco smoke; encouragement of breastfeeding; and delayed introduction of solid foods.
The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
Wheezing patterns in early childhood can predict pulmonary function and the development of asthma in adolescence in a high-risk population, a study finds.
The study validates four clinically distinct early-life wheezing phenotypes identified by the landmark Tucson Children’s Respiratory Study in a high-risk population:
• Never.
• Transient early – wheezing before age 3 years but not at age 6 years.
• Late onset – wheezing at age 6 years but not before age 3 years.
• Persistent – wheezing before age 3 years and at age 6 years.
Previously, these phenotypes were shown to be associated with respiratory outcomes in adolescence but not with diagnosed asthma or in genetically predisposed children. The present study extends the associations with these early phenotypes to a high-risk adolescent population, said Meghan B. Azad, Ph.D., of the University of Manitoba, Winnipeg, and her associates.
The study findings were based on findings in 459 children previously enrolled in the Canadian Asthma Primary Prevention Study cohort; this was a prenatally randomized prevention trial in children at high genetic risk for asthma. The distribution of early-wheeze phenotypes was 51% never, 28% transient early, 9% late onset, and 13% persistent (JAMA Pediatrics. 2016 Feb 8. doi: 10.1001/jamapediatrics.2015.4127).
Across all four phenotypes, the authors found a strong gradient of decreasing lung function and increasing asthma risk by age 15 years. Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: the prevalence of asthma was 5% among never, 19% among transient early, 27% among late onset, and 42% among persistent phenotypes.
At age 15, early-wheezing phenotypes were not associated with atopic dermatitis or allergic rhinitis. Atopy before 2 years of age was associated with persistent wheeze, which was in turn associated with a 12-fold increased risk of diagnosed asthma by age 15.
“Our results are consistent with other cohorts” and the study “extends these findings through adolescence in a high-risk cohort and demonstrates that asthma-associated deficits are already present at a young age. Collectively, these data show that early wheezing patterns provide clinically meaningful information and suggest that strategies to reduce early-life wheezing and atopic sensitization could have long-term health benefits,” Dr. Azad and her colleagues concluded.
Proven strategies to prevent wheezing include avoiding dust, pets, and tobacco smoke; encouragement of breastfeeding; and delayed introduction of solid foods.
The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
FROM JAMA PEDIATRICS
Key clinical point: Persistent early-life wheezing was associated with an 12-fold increased risk of diagnosed asthma by age 15 years.
Major finding: Asthma, assessed at 15 years in 320 adolescents, was associated with early-wheeze phenotypes: prevalence of asthma was 5% among never, 19% among early transient, 27% among late onset, and 42% among persistent phenotypes.
Data source: A study of 459 children.
Disclosures: The research was supported by the Canadian Institutes of Health Research. The investigators reported no relevant financial disclosures.
ACR: Infection risk with DMARDs doesn’t change with age of RA onset
SAN FRANCISCO – Biologics do not pose an increased risk of infection in patients with elderly-onset rheumatoid arthritis over the age of 60 years because their time to first infection and time to multiple infections were not different from people of the same age who developed the disease at a younger age in a large, prospective, longitudinal, observational study .
The data also suggest that noncytotoxic disease-modifying antirheumatic drugs (DMARDs) and non-TNF biologics may have a protective effect against infection in elderly patients with RA regardless of time of disease onset when compared with methotrexate monotherapy.
“Elderly-onset RA [EORA] patients are less likely to be treated with biologics than [are] patients with younger-onset RA [YORA]. This difference may be related to concerns about the risk of serious infections in elderly patients versus younger ones. There are only two papers on this subject in the literature, and now our study shows no increased risk. These findings support providing similar treatment for elderly versus younger-onset RA patients,” lead author Sofia Pedro of the National Data Bank for Rheumatic Diseases, Wichita, Kan., said at the annual meeting of the American College of Rheumatology.
The study was based on people with RA included in the National Data Bank for Rheumatic Diseases followed from 1998 through 2014. Patients filled out questionnaires on demographics, clinical factors, medications, and infections. A total of 1,865 EORA patients (onset older than 60 years) were matched 1:3 with 5,595 YORA patients (onset younger than 60 years) based on age, sex, and year of study entry.
At baseline, all patients were older than 60 years. The median age was between 65 and 70 years.
Serious infections were those that required hospitalization or intravenous antibiotics or caused death. Serious infectious were validated from hospital, physician, and death records. Overall, a total of 1,196 serious infections were reported during the study: 204 (11%) in the EORA group and 992 (18%) in YORA patients. Pneumonia, skin, and sepsis were the most common infections in both groups. Pneumonia was reported in 55% of EORA patients and 66% of the YORA group; skin infections, in 22% vs. 14%, respectively; and sepsis in 16% vs. 17%, respectively. The rate of self-reported prior infections was 4% in EORA patients and 7% in YORA patients (P less than .01). Overall, EORA patients were no quicker to have a first infection or multiple infections than were YORA patients after adjustments for Comorbidity Index, Health Assessment Questionnaire (HAQ), headache, pain, education, ethnicity, prednisone use, and urban versus rural setting.
Treatments were grouped according to noncytotoxic DMARDS; cytotoxic DMARDs; anti-TNF biologics; and non-TNF biologics. Methotrexate monotherapy was the referent. The hazard ratios for time to first infection and time to multiple infections were 0.72 and 0.82, respectively, for non-cytotoxic DMARDs and 0.43 and 0.48, respectively, for non-TNF biologics, all of which were statistically significant after adjustment for confounders.
EORA patients, compared with YORA patients, had greater exposure to prednisone and fewer prior serious infections, shorter disease duration (4.4 years vs. 20.9 years, respectively), lower Comorbidity Index, and more favorable disease markers. YORA patients had greater exposure to TNF biologics.
YORA patients had slightly higher incidence rates across all age groups, except between the ages of 60-70 years, when more infections were reported in EORA patients. The risk for multiple infections was greater in patients aged 80 years and older, but Ms. Pedro noted that covariates, such as HAQ, Comorbidity Index, prior serious infection, and exposure to prednisone, were associated with increased risk.
Ms. Pedro had no financial disclosures.
SAN FRANCISCO – Biologics do not pose an increased risk of infection in patients with elderly-onset rheumatoid arthritis over the age of 60 years because their time to first infection and time to multiple infections were not different from people of the same age who developed the disease at a younger age in a large, prospective, longitudinal, observational study .
The data also suggest that noncytotoxic disease-modifying antirheumatic drugs (DMARDs) and non-TNF biologics may have a protective effect against infection in elderly patients with RA regardless of time of disease onset when compared with methotrexate monotherapy.
“Elderly-onset RA [EORA] patients are less likely to be treated with biologics than [are] patients with younger-onset RA [YORA]. This difference may be related to concerns about the risk of serious infections in elderly patients versus younger ones. There are only two papers on this subject in the literature, and now our study shows no increased risk. These findings support providing similar treatment for elderly versus younger-onset RA patients,” lead author Sofia Pedro of the National Data Bank for Rheumatic Diseases, Wichita, Kan., said at the annual meeting of the American College of Rheumatology.
The study was based on people with RA included in the National Data Bank for Rheumatic Diseases followed from 1998 through 2014. Patients filled out questionnaires on demographics, clinical factors, medications, and infections. A total of 1,865 EORA patients (onset older than 60 years) were matched 1:3 with 5,595 YORA patients (onset younger than 60 years) based on age, sex, and year of study entry.
At baseline, all patients were older than 60 years. The median age was between 65 and 70 years.
Serious infections were those that required hospitalization or intravenous antibiotics or caused death. Serious infectious were validated from hospital, physician, and death records. Overall, a total of 1,196 serious infections were reported during the study: 204 (11%) in the EORA group and 992 (18%) in YORA patients. Pneumonia, skin, and sepsis were the most common infections in both groups. Pneumonia was reported in 55% of EORA patients and 66% of the YORA group; skin infections, in 22% vs. 14%, respectively; and sepsis in 16% vs. 17%, respectively. The rate of self-reported prior infections was 4% in EORA patients and 7% in YORA patients (P less than .01). Overall, EORA patients were no quicker to have a first infection or multiple infections than were YORA patients after adjustments for Comorbidity Index, Health Assessment Questionnaire (HAQ), headache, pain, education, ethnicity, prednisone use, and urban versus rural setting.
Treatments were grouped according to noncytotoxic DMARDS; cytotoxic DMARDs; anti-TNF biologics; and non-TNF biologics. Methotrexate monotherapy was the referent. The hazard ratios for time to first infection and time to multiple infections were 0.72 and 0.82, respectively, for non-cytotoxic DMARDs and 0.43 and 0.48, respectively, for non-TNF biologics, all of which were statistically significant after adjustment for confounders.
EORA patients, compared with YORA patients, had greater exposure to prednisone and fewer prior serious infections, shorter disease duration (4.4 years vs. 20.9 years, respectively), lower Comorbidity Index, and more favorable disease markers. YORA patients had greater exposure to TNF biologics.
YORA patients had slightly higher incidence rates across all age groups, except between the ages of 60-70 years, when more infections were reported in EORA patients. The risk for multiple infections was greater in patients aged 80 years and older, but Ms. Pedro noted that covariates, such as HAQ, Comorbidity Index, prior serious infection, and exposure to prednisone, were associated with increased risk.
Ms. Pedro had no financial disclosures.
SAN FRANCISCO – Biologics do not pose an increased risk of infection in patients with elderly-onset rheumatoid arthritis over the age of 60 years because their time to first infection and time to multiple infections were not different from people of the same age who developed the disease at a younger age in a large, prospective, longitudinal, observational study .
The data also suggest that noncytotoxic disease-modifying antirheumatic drugs (DMARDs) and non-TNF biologics may have a protective effect against infection in elderly patients with RA regardless of time of disease onset when compared with methotrexate monotherapy.
“Elderly-onset RA [EORA] patients are less likely to be treated with biologics than [are] patients with younger-onset RA [YORA]. This difference may be related to concerns about the risk of serious infections in elderly patients versus younger ones. There are only two papers on this subject in the literature, and now our study shows no increased risk. These findings support providing similar treatment for elderly versus younger-onset RA patients,” lead author Sofia Pedro of the National Data Bank for Rheumatic Diseases, Wichita, Kan., said at the annual meeting of the American College of Rheumatology.
The study was based on people with RA included in the National Data Bank for Rheumatic Diseases followed from 1998 through 2014. Patients filled out questionnaires on demographics, clinical factors, medications, and infections. A total of 1,865 EORA patients (onset older than 60 years) were matched 1:3 with 5,595 YORA patients (onset younger than 60 years) based on age, sex, and year of study entry.
At baseline, all patients were older than 60 years. The median age was between 65 and 70 years.
Serious infections were those that required hospitalization or intravenous antibiotics or caused death. Serious infectious were validated from hospital, physician, and death records. Overall, a total of 1,196 serious infections were reported during the study: 204 (11%) in the EORA group and 992 (18%) in YORA patients. Pneumonia, skin, and sepsis were the most common infections in both groups. Pneumonia was reported in 55% of EORA patients and 66% of the YORA group; skin infections, in 22% vs. 14%, respectively; and sepsis in 16% vs. 17%, respectively. The rate of self-reported prior infections was 4% in EORA patients and 7% in YORA patients (P less than .01). Overall, EORA patients were no quicker to have a first infection or multiple infections than were YORA patients after adjustments for Comorbidity Index, Health Assessment Questionnaire (HAQ), headache, pain, education, ethnicity, prednisone use, and urban versus rural setting.
Treatments were grouped according to noncytotoxic DMARDS; cytotoxic DMARDs; anti-TNF biologics; and non-TNF biologics. Methotrexate monotherapy was the referent. The hazard ratios for time to first infection and time to multiple infections were 0.72 and 0.82, respectively, for non-cytotoxic DMARDs and 0.43 and 0.48, respectively, for non-TNF biologics, all of which were statistically significant after adjustment for confounders.
EORA patients, compared with YORA patients, had greater exposure to prednisone and fewer prior serious infections, shorter disease duration (4.4 years vs. 20.9 years, respectively), lower Comorbidity Index, and more favorable disease markers. YORA patients had greater exposure to TNF biologics.
YORA patients had slightly higher incidence rates across all age groups, except between the ages of 60-70 years, when more infections were reported in EORA patients. The risk for multiple infections was greater in patients aged 80 years and older, but Ms. Pedro noted that covariates, such as HAQ, Comorbidity Index, prior serious infection, and exposure to prednisone, were associated with increased risk.
Ms. Pedro had no financial disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Patients with older onset RA can be safely treated with biologics.
Major finding: There was no significant difference in serious infections between older onset and younger onset RA patients.
Data source: A prospective, longitudinal observational study of 7,460 patients with RA followed during 1998-2014 in the National Data Bank for Rheumatic Diseases.
Disclosures: The presenter had no financial disclosures.
ACR: Criteria enable prompt diagnosis and treatment of CAPS
SAN FRANCISCO – Valid diagnostic criteria for cryopyrin-associated periodic syndromes are sorely needed, and a new model of CAPS diagnostic criteria enables rapid diagnosis of this rare, heterogeneous, inflammatory disease that can have devastating consequences if left undiagnosed and untreated.
“Our novel, unique approach integrated traditional methods of evidence synthesis with expert consensus, web-based decision tools, and innovative statistical methods. We hope this model can be of benefit in the diagnosis of other rare diseases,” said Dr. Jasmin B. Kümmerle-Deschner of the department of pediatrics at the University of Tübingen (Germany). She noted that the panel wanted to develop diagnostic criteria that could be used prior to genetic testing or in cases where no genetic mutation is identified.
Dr. Kümmerle-Deschner, who was on the multinational panel that developed the new diagnostic criteria, reviewed the process and presented the new criteria at the annual meeting of the American College of Rheumatology.
Cryopyrin-associated periodic syndromes (CAPS) comprise a rare, clinically heterogeneous group of devastating inflammatory diseases characterized by variable, severe system and organ inflammation resulting in permanent organ damage. The disease can manifest right after birth or later in life, and it can be associated with a mutation in the NLRP3 gene. Because the pathogenesis involves continually increased IL-1 secretion, early diagnosis and rapid initiation of IL-1 inhibition can control inflammation and prevent organ damage in children and adults with CAPS.
The lengthy process for developing the diagnostic criteria involved building an 18-member team of pediatric and adult subspecialists and experts in methods for rare disease. They generated 32 CAPS-typical items from a systematic literature review of 33 papers that described symptoms of CAPS and then reviewed the items in CAPS registries, weighting them via decision analysis software. Next, the panel refined these to 14 items plus the NLRP3 mutation. 1000Minds decision-making software ranked these 14 variables based on importance for the diagnosis of CAPS, with excellent correlation among experts.
Then a correspondence analysis determined variables consistently associated with the diagnosis of CAPS based on 284 cases and 873 controls; this process removed infrequently observed variables, such as “amyloidosis.” The remaining seven variables were found to be significantly associated with a diagnosis of CAPS (P less than .001 for all).
The final CAPS diagnosis model includes raised inflammatory markers (C-reactive protein/serum amyloid A) as a mandatory criterion, plus at least two of six different typical signs and symptoms of CAPS: urticaria-like rash, cold-stress triggered episodes, sensorineural hearing loss, musculoskeletal symptoms such as arthralgia, arthritis, and myalgia, chronic aseptic meningitis, and skeletal abnormalities such as epiphyseal overgrowth/frontal bossing. This model had a sensitivity of 81% and a specificity of 94%, performing well in all CAPS subtypes as well as in subgroups with or without evidence of germline NLRP3 mutations.
Dr. Kümmerle-Deschner opened her talk with a case description of an 81-year-old man who presented with a baffling disease. It turned out that his granddaughter was diagnosed with CAPS and 16 other family members were affected. She closed the talk by showing how this man could have been rapidly diagnosed by the new CAPS criteria. He presented with urticaria-like rash, arthralgia, arthritis, and cold-triggered episodes in the context of raised inflammatory markers.
“Early diagnosis enabling rapid treatment is possible,” she stated.
Dr. Kümmerle-Deschner disclosed financial ties with Novartis.
SAN FRANCISCO – Valid diagnostic criteria for cryopyrin-associated periodic syndromes are sorely needed, and a new model of CAPS diagnostic criteria enables rapid diagnosis of this rare, heterogeneous, inflammatory disease that can have devastating consequences if left undiagnosed and untreated.
“Our novel, unique approach integrated traditional methods of evidence synthesis with expert consensus, web-based decision tools, and innovative statistical methods. We hope this model can be of benefit in the diagnosis of other rare diseases,” said Dr. Jasmin B. Kümmerle-Deschner of the department of pediatrics at the University of Tübingen (Germany). She noted that the panel wanted to develop diagnostic criteria that could be used prior to genetic testing or in cases where no genetic mutation is identified.
Dr. Kümmerle-Deschner, who was on the multinational panel that developed the new diagnostic criteria, reviewed the process and presented the new criteria at the annual meeting of the American College of Rheumatology.
Cryopyrin-associated periodic syndromes (CAPS) comprise a rare, clinically heterogeneous group of devastating inflammatory diseases characterized by variable, severe system and organ inflammation resulting in permanent organ damage. The disease can manifest right after birth or later in life, and it can be associated with a mutation in the NLRP3 gene. Because the pathogenesis involves continually increased IL-1 secretion, early diagnosis and rapid initiation of IL-1 inhibition can control inflammation and prevent organ damage in children and adults with CAPS.
The lengthy process for developing the diagnostic criteria involved building an 18-member team of pediatric and adult subspecialists and experts in methods for rare disease. They generated 32 CAPS-typical items from a systematic literature review of 33 papers that described symptoms of CAPS and then reviewed the items in CAPS registries, weighting them via decision analysis software. Next, the panel refined these to 14 items plus the NLRP3 mutation. 1000Minds decision-making software ranked these 14 variables based on importance for the diagnosis of CAPS, with excellent correlation among experts.
Then a correspondence analysis determined variables consistently associated with the diagnosis of CAPS based on 284 cases and 873 controls; this process removed infrequently observed variables, such as “amyloidosis.” The remaining seven variables were found to be significantly associated with a diagnosis of CAPS (P less than .001 for all).
The final CAPS diagnosis model includes raised inflammatory markers (C-reactive protein/serum amyloid A) as a mandatory criterion, plus at least two of six different typical signs and symptoms of CAPS: urticaria-like rash, cold-stress triggered episodes, sensorineural hearing loss, musculoskeletal symptoms such as arthralgia, arthritis, and myalgia, chronic aseptic meningitis, and skeletal abnormalities such as epiphyseal overgrowth/frontal bossing. This model had a sensitivity of 81% and a specificity of 94%, performing well in all CAPS subtypes as well as in subgroups with or without evidence of germline NLRP3 mutations.
Dr. Kümmerle-Deschner opened her talk with a case description of an 81-year-old man who presented with a baffling disease. It turned out that his granddaughter was diagnosed with CAPS and 16 other family members were affected. She closed the talk by showing how this man could have been rapidly diagnosed by the new CAPS criteria. He presented with urticaria-like rash, arthralgia, arthritis, and cold-triggered episodes in the context of raised inflammatory markers.
“Early diagnosis enabling rapid treatment is possible,” she stated.
Dr. Kümmerle-Deschner disclosed financial ties with Novartis.
SAN FRANCISCO – Valid diagnostic criteria for cryopyrin-associated periodic syndromes are sorely needed, and a new model of CAPS diagnostic criteria enables rapid diagnosis of this rare, heterogeneous, inflammatory disease that can have devastating consequences if left undiagnosed and untreated.
“Our novel, unique approach integrated traditional methods of evidence synthesis with expert consensus, web-based decision tools, and innovative statistical methods. We hope this model can be of benefit in the diagnosis of other rare diseases,” said Dr. Jasmin B. Kümmerle-Deschner of the department of pediatrics at the University of Tübingen (Germany). She noted that the panel wanted to develop diagnostic criteria that could be used prior to genetic testing or in cases where no genetic mutation is identified.
Dr. Kümmerle-Deschner, who was on the multinational panel that developed the new diagnostic criteria, reviewed the process and presented the new criteria at the annual meeting of the American College of Rheumatology.
Cryopyrin-associated periodic syndromes (CAPS) comprise a rare, clinically heterogeneous group of devastating inflammatory diseases characterized by variable, severe system and organ inflammation resulting in permanent organ damage. The disease can manifest right after birth or later in life, and it can be associated with a mutation in the NLRP3 gene. Because the pathogenesis involves continually increased IL-1 secretion, early diagnosis and rapid initiation of IL-1 inhibition can control inflammation and prevent organ damage in children and adults with CAPS.
The lengthy process for developing the diagnostic criteria involved building an 18-member team of pediatric and adult subspecialists and experts in methods for rare disease. They generated 32 CAPS-typical items from a systematic literature review of 33 papers that described symptoms of CAPS and then reviewed the items in CAPS registries, weighting them via decision analysis software. Next, the panel refined these to 14 items plus the NLRP3 mutation. 1000Minds decision-making software ranked these 14 variables based on importance for the diagnosis of CAPS, with excellent correlation among experts.
Then a correspondence analysis determined variables consistently associated with the diagnosis of CAPS based on 284 cases and 873 controls; this process removed infrequently observed variables, such as “amyloidosis.” The remaining seven variables were found to be significantly associated with a diagnosis of CAPS (P less than .001 for all).
The final CAPS diagnosis model includes raised inflammatory markers (C-reactive protein/serum amyloid A) as a mandatory criterion, plus at least two of six different typical signs and symptoms of CAPS: urticaria-like rash, cold-stress triggered episodes, sensorineural hearing loss, musculoskeletal symptoms such as arthralgia, arthritis, and myalgia, chronic aseptic meningitis, and skeletal abnormalities such as epiphyseal overgrowth/frontal bossing. This model had a sensitivity of 81% and a specificity of 94%, performing well in all CAPS subtypes as well as in subgroups with or without evidence of germline NLRP3 mutations.
Dr. Kümmerle-Deschner opened her talk with a case description of an 81-year-old man who presented with a baffling disease. It turned out that his granddaughter was diagnosed with CAPS and 16 other family members were affected. She closed the talk by showing how this man could have been rapidly diagnosed by the new CAPS criteria. He presented with urticaria-like rash, arthralgia, arthritis, and cold-triggered episodes in the context of raised inflammatory markers.
“Early diagnosis enabling rapid treatment is possible,” she stated.
Dr. Kümmerle-Deschner disclosed financial ties with Novartis.
AT THE ACR ANNUAL MEETING
Targeting IL-6 effective in RA poor responders to anti-TNF inhibitors
SAN FRANCISCO – Sarilumab, an investigational monoclonal antibody directed against the IL-6 receptor, demonstrated efficacy at two different dose levels, compared with placebo, in patients with active rheumatoid arthritis (RA) who were intolerant to or had inadequate response to anti–tumor necrosis factor (anti-TNF) inhibitors in the pivotal phase III TARGET study.
On all measures of disease activity and physical function, sarilumab was significantly superior to placebo in these very sick patients. Results were presented at the annual meeting of the American College of Rheumatology.
“New treatments are needed to address unmet patient needs, including the failure to respond to therapy. Sarilumab, if approved, may be a potential option for RA patients with moderate to severe RA,” said Dr. Roy Fleischmann of University of Texas in Dallas.
“Both the 150-mg and 200-mg doses of sarilumab demonstrate improvement and clinical efficacy versus placebo in these patients. The higher dose appears to have slightly better efficacy but also had a higher incidence of treatment-emergent adverse events leading to discontinuations. The 150-mg dose may be a little safer. I would start with 200 mg and methotrexate and if an adverse event occurred, lower the dose to 150 mg,” Dr. Fleischmann told the audience.
TARGET enrolled 546 patients with active RA for at least 6 months who were intolerant to or failed prior anti-TNF therapy. Active disease was defined as at least six swollen and eight tender joints. All patients had high C-reactive protein (CRP) levels at screening (more than 8 mg/L).
The patients’ median age was 52 years, and 80% were female. Median duration of RA was 12 years. Twenty-five percent had been treated with more than one prior anti-TNF agent. About 74% were rheumatoid factor positive.
“These were recalcitrant and sick RA patients,” Dr. Fleischmann said.
Patients were randomized to sarilumab 150 mg, 200 mg, or placebo in addition to background conventional DMARD therapy. Study drugs and placebo were self-administered subcutaneously every other week. Patients who did not respond adequately to therapy at week 12 were rescued with sarilumab 200 mg every 2 weeks.
“Both doses of sarilumab had significantly improved ACR 20/50/70 response, compared with placebo,” he said.
Mean change from baseline to week 12 in Health Assessment Questionnaire–Disease Index (HAQ-DI), which assesses daily physical function, was –0.49, –0.50, and –0.29 in the 200-mg, 150-mg, and placebo groups, respectively (P = .0004 and P = .0007, respectively, for each dose of sarilumab).
The percentage of patients with an ACR 20 response at week 24 was 61%, 56%, and 34%, for the 200-mg, 150-mg, and placebo groups, respectively (P less than .0001, for both comparisons).
Sarilumab was also superior to placebo for all secondary endpoints, including the percentage of patients achieving an ACR 50 and ACR 70 response, change from baseline in Disease Activity Score (DAS) 28-CRP, achieving DAS28-CRP less than 2.6, change from baseline in clinical disease activity index (CDAI), and change in HAQ-DI at week 24.
Looking at safety, treatment-emergent adverse events were more frequent in the sarilumab-treated patients, compared with placebo: 65% for the 200-mg dose, 66% for the 150-mg dose, versus 50% for placebo. Serious adverse events were more frequent in the sarilumab 200-mg group, compared with placebo (5% versus 3%), and were similar to placebo in the sarilumab 150-mg group (3%)
Serious infections occurred in two patients in the sarilumab 200-mg group, one patient in the sarilumab 150-mg group, and two patients on placebo. Neutropenia and infection were the most frequent adverse events leading to treatment discontinuations (17 in the 200-mg group, 14 in the 150-mg group).
Regeneron Pharmaceuticals and Sanofi funded the study. Dr. Fleischmann disclosed financial ties with Abbvie, Akros, Amgen, Ardea, AstraZeneca, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, Janssen Pharmaceutica Products, Eli Lilly & Co., Merck Pharmaceuticals, Pfizer, Resolve, Roche Pharmaceuticals, Sanofi-Aventis Pharmaceuticals, and UCB.
SAN FRANCISCO – Sarilumab, an investigational monoclonal antibody directed against the IL-6 receptor, demonstrated efficacy at two different dose levels, compared with placebo, in patients with active rheumatoid arthritis (RA) who were intolerant to or had inadequate response to anti–tumor necrosis factor (anti-TNF) inhibitors in the pivotal phase III TARGET study.
On all measures of disease activity and physical function, sarilumab was significantly superior to placebo in these very sick patients. Results were presented at the annual meeting of the American College of Rheumatology.
“New treatments are needed to address unmet patient needs, including the failure to respond to therapy. Sarilumab, if approved, may be a potential option for RA patients with moderate to severe RA,” said Dr. Roy Fleischmann of University of Texas in Dallas.
“Both the 150-mg and 200-mg doses of sarilumab demonstrate improvement and clinical efficacy versus placebo in these patients. The higher dose appears to have slightly better efficacy but also had a higher incidence of treatment-emergent adverse events leading to discontinuations. The 150-mg dose may be a little safer. I would start with 200 mg and methotrexate and if an adverse event occurred, lower the dose to 150 mg,” Dr. Fleischmann told the audience.
TARGET enrolled 546 patients with active RA for at least 6 months who were intolerant to or failed prior anti-TNF therapy. Active disease was defined as at least six swollen and eight tender joints. All patients had high C-reactive protein (CRP) levels at screening (more than 8 mg/L).
The patients’ median age was 52 years, and 80% were female. Median duration of RA was 12 years. Twenty-five percent had been treated with more than one prior anti-TNF agent. About 74% were rheumatoid factor positive.
“These were recalcitrant and sick RA patients,” Dr. Fleischmann said.
Patients were randomized to sarilumab 150 mg, 200 mg, or placebo in addition to background conventional DMARD therapy. Study drugs and placebo were self-administered subcutaneously every other week. Patients who did not respond adequately to therapy at week 12 were rescued with sarilumab 200 mg every 2 weeks.
“Both doses of sarilumab had significantly improved ACR 20/50/70 response, compared with placebo,” he said.
Mean change from baseline to week 12 in Health Assessment Questionnaire–Disease Index (HAQ-DI), which assesses daily physical function, was –0.49, –0.50, and –0.29 in the 200-mg, 150-mg, and placebo groups, respectively (P = .0004 and P = .0007, respectively, for each dose of sarilumab).
The percentage of patients with an ACR 20 response at week 24 was 61%, 56%, and 34%, for the 200-mg, 150-mg, and placebo groups, respectively (P less than .0001, for both comparisons).
Sarilumab was also superior to placebo for all secondary endpoints, including the percentage of patients achieving an ACR 50 and ACR 70 response, change from baseline in Disease Activity Score (DAS) 28-CRP, achieving DAS28-CRP less than 2.6, change from baseline in clinical disease activity index (CDAI), and change in HAQ-DI at week 24.
Looking at safety, treatment-emergent adverse events were more frequent in the sarilumab-treated patients, compared with placebo: 65% for the 200-mg dose, 66% for the 150-mg dose, versus 50% for placebo. Serious adverse events were more frequent in the sarilumab 200-mg group, compared with placebo (5% versus 3%), and were similar to placebo in the sarilumab 150-mg group (3%)
Serious infections occurred in two patients in the sarilumab 200-mg group, one patient in the sarilumab 150-mg group, and two patients on placebo. Neutropenia and infection were the most frequent adverse events leading to treatment discontinuations (17 in the 200-mg group, 14 in the 150-mg group).
Regeneron Pharmaceuticals and Sanofi funded the study. Dr. Fleischmann disclosed financial ties with Abbvie, Akros, Amgen, Ardea, AstraZeneca, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, Janssen Pharmaceutica Products, Eli Lilly & Co., Merck Pharmaceuticals, Pfizer, Resolve, Roche Pharmaceuticals, Sanofi-Aventis Pharmaceuticals, and UCB.
SAN FRANCISCO – Sarilumab, an investigational monoclonal antibody directed against the IL-6 receptor, demonstrated efficacy at two different dose levels, compared with placebo, in patients with active rheumatoid arthritis (RA) who were intolerant to or had inadequate response to anti–tumor necrosis factor (anti-TNF) inhibitors in the pivotal phase III TARGET study.
On all measures of disease activity and physical function, sarilumab was significantly superior to placebo in these very sick patients. Results were presented at the annual meeting of the American College of Rheumatology.
“New treatments are needed to address unmet patient needs, including the failure to respond to therapy. Sarilumab, if approved, may be a potential option for RA patients with moderate to severe RA,” said Dr. Roy Fleischmann of University of Texas in Dallas.
“Both the 150-mg and 200-mg doses of sarilumab demonstrate improvement and clinical efficacy versus placebo in these patients. The higher dose appears to have slightly better efficacy but also had a higher incidence of treatment-emergent adverse events leading to discontinuations. The 150-mg dose may be a little safer. I would start with 200 mg and methotrexate and if an adverse event occurred, lower the dose to 150 mg,” Dr. Fleischmann told the audience.
TARGET enrolled 546 patients with active RA for at least 6 months who were intolerant to or failed prior anti-TNF therapy. Active disease was defined as at least six swollen and eight tender joints. All patients had high C-reactive protein (CRP) levels at screening (more than 8 mg/L).
The patients’ median age was 52 years, and 80% were female. Median duration of RA was 12 years. Twenty-five percent had been treated with more than one prior anti-TNF agent. About 74% were rheumatoid factor positive.
“These were recalcitrant and sick RA patients,” Dr. Fleischmann said.
Patients were randomized to sarilumab 150 mg, 200 mg, or placebo in addition to background conventional DMARD therapy. Study drugs and placebo were self-administered subcutaneously every other week. Patients who did not respond adequately to therapy at week 12 were rescued with sarilumab 200 mg every 2 weeks.
“Both doses of sarilumab had significantly improved ACR 20/50/70 response, compared with placebo,” he said.
Mean change from baseline to week 12 in Health Assessment Questionnaire–Disease Index (HAQ-DI), which assesses daily physical function, was –0.49, –0.50, and –0.29 in the 200-mg, 150-mg, and placebo groups, respectively (P = .0004 and P = .0007, respectively, for each dose of sarilumab).
The percentage of patients with an ACR 20 response at week 24 was 61%, 56%, and 34%, for the 200-mg, 150-mg, and placebo groups, respectively (P less than .0001, for both comparisons).
Sarilumab was also superior to placebo for all secondary endpoints, including the percentage of patients achieving an ACR 50 and ACR 70 response, change from baseline in Disease Activity Score (DAS) 28-CRP, achieving DAS28-CRP less than 2.6, change from baseline in clinical disease activity index (CDAI), and change in HAQ-DI at week 24.
Looking at safety, treatment-emergent adverse events were more frequent in the sarilumab-treated patients, compared with placebo: 65% for the 200-mg dose, 66% for the 150-mg dose, versus 50% for placebo. Serious adverse events were more frequent in the sarilumab 200-mg group, compared with placebo (5% versus 3%), and were similar to placebo in the sarilumab 150-mg group (3%)
Serious infections occurred in two patients in the sarilumab 200-mg group, one patient in the sarilumab 150-mg group, and two patients on placebo. Neutropenia and infection were the most frequent adverse events leading to treatment discontinuations (17 in the 200-mg group, 14 in the 150-mg group).
Regeneron Pharmaceuticals and Sanofi funded the study. Dr. Fleischmann disclosed financial ties with Abbvie, Akros, Amgen, Ardea, AstraZeneca, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, Janssen Pharmaceutica Products, Eli Lilly & Co., Merck Pharmaceuticals, Pfizer, Resolve, Roche Pharmaceuticals, Sanofi-Aventis Pharmaceuticals, and UCB.
AT THE ACR ANNUAL MEETING
Key clinical point: Sarilumab is effective in patients with active RA who have suboptimal response to anti-TNF inhibitors.
Major finding: Patients on both doses of sarilumab had significantly improved responses, compared with placebo, on all measures of disease and disability.
Data source: A double-blind, randomized, pivotal phase III trial.
Disclosures: Regeneron Pharmaceuticals and Sanofi funded the study. Dr. Fleischmann disclosed financial ties with many other pharmaceutical companies.
Baricitinib shows encouraging phase III results in RA
SAN FRANCISCO – Baricitinib, an investigational oral investigational JAK 1/2 inhibitor, was significantly superior to adalimumab and to placebo in the treatment of patients with active rheumatoid arthritis despite background methotrexate in the phase III RA-BEAM study.
Patients taking baricitinib had significant improvements in signs and symptoms of rheumatoid arthritis (RA), physical function, and patient-reported outcomes. These encouraging results, reported at a late-breaking abstract session during the annual meeting of the American College of Rheumatology, come on the heels of other positive phase III studies of this drug in treatment-naive patients and those with an inadequate response to anti-TNF agents plus methotrexate.
“I feel that this is a real clinical benefit we see with baricitinib, but we will need further studies. The safety and tolerability of baricitinib are satisfactory and consistent with other phase II and III studies reported at this meeting,” said Dr. Peter Taylor of the Kennedy Institute of Rheumatology at University of Oxford (England).
“The most important finding is that baricitinib administered with methotrexate is a superior treatment to methotrexate alone, but another interesting finding is that the baricitinib/methotrexate combination was superior to adalimumab [Humira] plus methotrexate,” Dr. Taylor added.
“Baricitinib is an oral, highly selective inhibitor of JAK 2, and the drug improves disease activity with acceptable safety in patients with an inadequate response to conventional therapy and also in disease-modifying antirheumatic drug [DMARD]-naive patients with rheumatoid arthritis,” Dr. Taylor told the audience.
The RA-BEAM study enrolled 1,307 RA patients who had an inadequate response to methotrexate. Patients were randomized 3:3:2 to placebo, baricitinib 4 mg/day or adalimumab 40 mg biweekly. From week 16 on, nonresponders were rescued with 4 mg baricitinib. All patients continued on stable doses of background methotrexate.
Median age of the patients was 50 years, and a majority were seropositive for rheumatoid factor. The mean methotrexate dose was 15 mg/once weekly, and 60% of patients were taking concomitant oral glucocorticoids.
At baseline, groups were well balanced for disease activity, disease duration, and demographic characteristics. The mean number of swollen joints was 16 and mean number of tender joints 23.
“These patients had marked disability and high baseline disease activity,” Dr. Taylor said.
At week 24, about 84%-90% of patients remained on study, and at week 52, more than 80% were still on study.
Rescue rates were 26% for placebo patients, 7% for baricitinib-treated patients, and 12% for those randomized to adalimumab.
For the primary endpoint of at least a 20% response at 12 weeks according to ACR criteria (i.e., ACR20), baricitinib was superior to both adalimumab and placebo (plus methotrexate in all three arms). ACR20 was achieved in 40% of patients in the placebo arm, 61% of those in the adalimumab arm, and by 70% of those taking baricitinib (P less than .001 for both comparisons versus placebo).
At week 24, the same pattern was observed for ACR20, ACR50, and ACR70. An ACR20 response was achieved by 37% with placebo, 66% with adalimumab, and 74% with baricitinib. For ACR50, response rates were 19%, 46%, and 50%, respectively. For ACR70, response rates were 9%, 22%, and 30%, respectively. (The P value was less than .001 for all comparisons versus placebo.)
Significantly more patients in the baricitinib-plus-methotrexate arm achieved low disease activity or remission, compared with placebo and with adalimumab plus methotrexate. Over time, the benefits increased in the baricitinib arm.
“A rapid reduction was observed in the number of swollen joints and tender joints with baricitinib and adalimumab, but the reduction was deeper with baricitinib,” said Dr. Taylor. “Patient-reported outcomes, such as joint stiffness and pain and fatigue, were improved on baricitinib as early as week 1, compared with placebo.
Both baricitinib and adalimumab achieved a greater inhibition on structural damage, compared with placebo, and this difference was maintained at week 52.
The percentage of patients with no change in Sharp van der Heijde Score was 70% for placebo, 79% for baricitinib, and 81% for adalimumab.
Rates of treatment-emergent adverse events were higher for the active treatment groups versus placebo: during weeks 0-12, 47.3% for placebo, 52.8% for baricitinib, and 50.9% for adalimumab. Infection rates during weeks 0-12 were 17.8%, 21.8%, and 20%, respectively.
The rates of serious adverse events during weeks 0-12 were 2.7% for placebo, 2.3% for baricitinib, and 1.2% for adalimumab, respectively. During an additional 12 weeks they rose further to 4.3%, 4.5%, and 1.8%, respectively.
There were four cases of malignancy reported in the baricitinib group and none in the adalimumab group in weeks 0-24. Two deaths were reported in the baricitinib group and none in the other two groups.
If baricitinib gains Food and Drug Administration approval for the treatment of RA, Dr. Taylor predicted that as experience is gained, it will be used “relatively early” in the course of treatment, but he acknowledged that cost will enter into the discussion.
Eli Lilly & Co. and Incyte Corporation sponsored the study. All investigators reported ties with Lilly, and some had ties with other companies marketing RA drugs.
SAN FRANCISCO – Baricitinib, an investigational oral investigational JAK 1/2 inhibitor, was significantly superior to adalimumab and to placebo in the treatment of patients with active rheumatoid arthritis despite background methotrexate in the phase III RA-BEAM study.
Patients taking baricitinib had significant improvements in signs and symptoms of rheumatoid arthritis (RA), physical function, and patient-reported outcomes. These encouraging results, reported at a late-breaking abstract session during the annual meeting of the American College of Rheumatology, come on the heels of other positive phase III studies of this drug in treatment-naive patients and those with an inadequate response to anti-TNF agents plus methotrexate.
“I feel that this is a real clinical benefit we see with baricitinib, but we will need further studies. The safety and tolerability of baricitinib are satisfactory and consistent with other phase II and III studies reported at this meeting,” said Dr. Peter Taylor of the Kennedy Institute of Rheumatology at University of Oxford (England).
“The most important finding is that baricitinib administered with methotrexate is a superior treatment to methotrexate alone, but another interesting finding is that the baricitinib/methotrexate combination was superior to adalimumab [Humira] plus methotrexate,” Dr. Taylor added.
“Baricitinib is an oral, highly selective inhibitor of JAK 2, and the drug improves disease activity with acceptable safety in patients with an inadequate response to conventional therapy and also in disease-modifying antirheumatic drug [DMARD]-naive patients with rheumatoid arthritis,” Dr. Taylor told the audience.
The RA-BEAM study enrolled 1,307 RA patients who had an inadequate response to methotrexate. Patients were randomized 3:3:2 to placebo, baricitinib 4 mg/day or adalimumab 40 mg biweekly. From week 16 on, nonresponders were rescued with 4 mg baricitinib. All patients continued on stable doses of background methotrexate.
Median age of the patients was 50 years, and a majority were seropositive for rheumatoid factor. The mean methotrexate dose was 15 mg/once weekly, and 60% of patients were taking concomitant oral glucocorticoids.
At baseline, groups were well balanced for disease activity, disease duration, and demographic characteristics. The mean number of swollen joints was 16 and mean number of tender joints 23.
“These patients had marked disability and high baseline disease activity,” Dr. Taylor said.
At week 24, about 84%-90% of patients remained on study, and at week 52, more than 80% were still on study.
Rescue rates were 26% for placebo patients, 7% for baricitinib-treated patients, and 12% for those randomized to adalimumab.
For the primary endpoint of at least a 20% response at 12 weeks according to ACR criteria (i.e., ACR20), baricitinib was superior to both adalimumab and placebo (plus methotrexate in all three arms). ACR20 was achieved in 40% of patients in the placebo arm, 61% of those in the adalimumab arm, and by 70% of those taking baricitinib (P less than .001 for both comparisons versus placebo).
At week 24, the same pattern was observed for ACR20, ACR50, and ACR70. An ACR20 response was achieved by 37% with placebo, 66% with adalimumab, and 74% with baricitinib. For ACR50, response rates were 19%, 46%, and 50%, respectively. For ACR70, response rates were 9%, 22%, and 30%, respectively. (The P value was less than .001 for all comparisons versus placebo.)
Significantly more patients in the baricitinib-plus-methotrexate arm achieved low disease activity or remission, compared with placebo and with adalimumab plus methotrexate. Over time, the benefits increased in the baricitinib arm.
“A rapid reduction was observed in the number of swollen joints and tender joints with baricitinib and adalimumab, but the reduction was deeper with baricitinib,” said Dr. Taylor. “Patient-reported outcomes, such as joint stiffness and pain and fatigue, were improved on baricitinib as early as week 1, compared with placebo.
Both baricitinib and adalimumab achieved a greater inhibition on structural damage, compared with placebo, and this difference was maintained at week 52.
The percentage of patients with no change in Sharp van der Heijde Score was 70% for placebo, 79% for baricitinib, and 81% for adalimumab.
Rates of treatment-emergent adverse events were higher for the active treatment groups versus placebo: during weeks 0-12, 47.3% for placebo, 52.8% for baricitinib, and 50.9% for adalimumab. Infection rates during weeks 0-12 were 17.8%, 21.8%, and 20%, respectively.
The rates of serious adverse events during weeks 0-12 were 2.7% for placebo, 2.3% for baricitinib, and 1.2% for adalimumab, respectively. During an additional 12 weeks they rose further to 4.3%, 4.5%, and 1.8%, respectively.
There were four cases of malignancy reported in the baricitinib group and none in the adalimumab group in weeks 0-24. Two deaths were reported in the baricitinib group and none in the other two groups.
If baricitinib gains Food and Drug Administration approval for the treatment of RA, Dr. Taylor predicted that as experience is gained, it will be used “relatively early” in the course of treatment, but he acknowledged that cost will enter into the discussion.
Eli Lilly & Co. and Incyte Corporation sponsored the study. All investigators reported ties with Lilly, and some had ties with other companies marketing RA drugs.
SAN FRANCISCO – Baricitinib, an investigational oral investigational JAK 1/2 inhibitor, was significantly superior to adalimumab and to placebo in the treatment of patients with active rheumatoid arthritis despite background methotrexate in the phase III RA-BEAM study.
Patients taking baricitinib had significant improvements in signs and symptoms of rheumatoid arthritis (RA), physical function, and patient-reported outcomes. These encouraging results, reported at a late-breaking abstract session during the annual meeting of the American College of Rheumatology, come on the heels of other positive phase III studies of this drug in treatment-naive patients and those with an inadequate response to anti-TNF agents plus methotrexate.
“I feel that this is a real clinical benefit we see with baricitinib, but we will need further studies. The safety and tolerability of baricitinib are satisfactory and consistent with other phase II and III studies reported at this meeting,” said Dr. Peter Taylor of the Kennedy Institute of Rheumatology at University of Oxford (England).
“The most important finding is that baricitinib administered with methotrexate is a superior treatment to methotrexate alone, but another interesting finding is that the baricitinib/methotrexate combination was superior to adalimumab [Humira] plus methotrexate,” Dr. Taylor added.
“Baricitinib is an oral, highly selective inhibitor of JAK 2, and the drug improves disease activity with acceptable safety in patients with an inadequate response to conventional therapy and also in disease-modifying antirheumatic drug [DMARD]-naive patients with rheumatoid arthritis,” Dr. Taylor told the audience.
The RA-BEAM study enrolled 1,307 RA patients who had an inadequate response to methotrexate. Patients were randomized 3:3:2 to placebo, baricitinib 4 mg/day or adalimumab 40 mg biweekly. From week 16 on, nonresponders were rescued with 4 mg baricitinib. All patients continued on stable doses of background methotrexate.
Median age of the patients was 50 years, and a majority were seropositive for rheumatoid factor. The mean methotrexate dose was 15 mg/once weekly, and 60% of patients were taking concomitant oral glucocorticoids.
At baseline, groups were well balanced for disease activity, disease duration, and demographic characteristics. The mean number of swollen joints was 16 and mean number of tender joints 23.
“These patients had marked disability and high baseline disease activity,” Dr. Taylor said.
At week 24, about 84%-90% of patients remained on study, and at week 52, more than 80% were still on study.
Rescue rates were 26% for placebo patients, 7% for baricitinib-treated patients, and 12% for those randomized to adalimumab.
For the primary endpoint of at least a 20% response at 12 weeks according to ACR criteria (i.e., ACR20), baricitinib was superior to both adalimumab and placebo (plus methotrexate in all three arms). ACR20 was achieved in 40% of patients in the placebo arm, 61% of those in the adalimumab arm, and by 70% of those taking baricitinib (P less than .001 for both comparisons versus placebo).
At week 24, the same pattern was observed for ACR20, ACR50, and ACR70. An ACR20 response was achieved by 37% with placebo, 66% with adalimumab, and 74% with baricitinib. For ACR50, response rates were 19%, 46%, and 50%, respectively. For ACR70, response rates were 9%, 22%, and 30%, respectively. (The P value was less than .001 for all comparisons versus placebo.)
Significantly more patients in the baricitinib-plus-methotrexate arm achieved low disease activity or remission, compared with placebo and with adalimumab plus methotrexate. Over time, the benefits increased in the baricitinib arm.
“A rapid reduction was observed in the number of swollen joints and tender joints with baricitinib and adalimumab, but the reduction was deeper with baricitinib,” said Dr. Taylor. “Patient-reported outcomes, such as joint stiffness and pain and fatigue, were improved on baricitinib as early as week 1, compared with placebo.
Both baricitinib and adalimumab achieved a greater inhibition on structural damage, compared with placebo, and this difference was maintained at week 52.
The percentage of patients with no change in Sharp van der Heijde Score was 70% for placebo, 79% for baricitinib, and 81% for adalimumab.
Rates of treatment-emergent adverse events were higher for the active treatment groups versus placebo: during weeks 0-12, 47.3% for placebo, 52.8% for baricitinib, and 50.9% for adalimumab. Infection rates during weeks 0-12 were 17.8%, 21.8%, and 20%, respectively.
The rates of serious adverse events during weeks 0-12 were 2.7% for placebo, 2.3% for baricitinib, and 1.2% for adalimumab, respectively. During an additional 12 weeks they rose further to 4.3%, 4.5%, and 1.8%, respectively.
There were four cases of malignancy reported in the baricitinib group and none in the adalimumab group in weeks 0-24. Two deaths were reported in the baricitinib group and none in the other two groups.
If baricitinib gains Food and Drug Administration approval for the treatment of RA, Dr. Taylor predicted that as experience is gained, it will be used “relatively early” in the course of treatment, but he acknowledged that cost will enter into the discussion.
Eli Lilly & Co. and Incyte Corporation sponsored the study. All investigators reported ties with Lilly, and some had ties with other companies marketing RA drugs.
AT THE ACR ANNUAL MEETING
Key clinical point: Baricitinib plus methotrexate was superior to placebo and to adalimumab plus methotrexate in achieving responses and remission in RA patients with an inadequate response to methotrexate.
Major finding: An ACR20 response was achieved at 12 weeks by 40% of patients in the placebo arm, 61% of those in the adalimumab arm, and by 70% of those taking baricitinib (P less than .001 for both comparisons versus placebo).
Data source: Randomized, double-blind, phase III comparison in 1,307 patients who had active RA despite background methotrexate.
Disclosures: Eli Lilly & Co. and Incyte Corporation sponsored the study. All investigators reported ties with Lilly, and some had ties with other companies marketing RA drugs.
Multibiomarker blood test could aid treatment decisions in RA
SAN FRANCISCO – Vectra DA, a multibiomarker blood test, can predict response to therapy for patients with rheumatoid arthritis, and it can also identify patients who can safely taper and discontinue disease-modifying antirheumatic drug (DMARD) therapy, according to two separate poster presentations at the annual meeting of the American College of Rheumatology.
Management of patients with RA is typically based on clinical criteria and lab test results. Vectra DA is the only multibiomarker panel available for assessing therapeutic response in RA. The test is Medicare-approved, and Medicare allows about $580 per test, according to a spokesperson for Crescendo Bioscience, the company providing the test. Currently, Vectra DA is used in about 20% of RA patients who are actively managed by a rheumatologist in the United States, and about 40% of U.S. rheumatologists use the test at least once per month, the spokesperson said.
“Vectra DA can assess the risk of radiographic changes and track therapeutic response. Patients with low to moderate Vectra DA scores have a reduced risk of radiographic progression over the next year,” said a coauthor of the first study, Rebecca J. Bolce, an employee of Crescendo.
Response to subsequent therapy
This retrospective study analyzed multibiomarker disease activity score (that is, Vectra DA) in incomplete responders to 3 months of methotrexate monotherapy to predict response to subsequent triple therapy versus biologic therapies. The patient sample came from the SWEFOT (Swedish Farmacotherapy) study of patients with early RA.
After 3 months of methotrexate therapy, 157 nonresponders were randomized to triple therapy or methotrexate plus infliximab (biologic therapy). At the time of randomization, nonresponders were assessed with Vectra DA. Patients with low Vectra DA scores (that is, less than 30) were successfully treated with triple therapy; at 1 year, 88% of these patients achieved low disease activity (a 28-joint Disease Activity Score [DAS28] less than 3.2), compared with 18% assigned to biologic therapy (P = .006).
Patients with a high score on Vectra DA were more likely to respond to biologics. In this group, at 1 year, low disease activity was achieved in 58% of patients randomized to biologics versus 35% randomized to triple therapy (P = .04).
“At 1 year, the Vectra DA score at 3 months was a superior predictor of response to both conventional triple therapy and biologic therapy, compared with C-reactive protein, erythrocyte sedimentation rate, and DAS28,” Ms. Bolce said.
“These findings may help facilitate and improve the development of individualized and cost-effective treatment plans for individuals with RA,” Ms. Bolce said.
Tapering therapy
A second study analyzed the role of multibiomarker disease activity (Vectra DA score) in predicting relapses in RA patients in sustained remission when tapering disease-modifying antirheumatic drug therapy in the context of the RETRO randomized clinical trial.
On a scale from 0-100, Vectra DA scores of less than 30 are categorized as low, scores 30-44 are called moderate, and those greater than 44 are considered high. Scores were calculated and compared between 94 patients who were relapsing or in sustained remission while tapering DMARD therapy.
Patients were randomized to one of three arms: continuation of DMARD; reduction of DMARD by 50%; or reduction of DMARD by 50% for 6 months and then stopping therapy.
Moderate to high scores were found in one-third of RA patients in remission. Scores were twice as high in relapsing patients (58.3%), compared with those in stable remission (25%). Baseline scores were significantly higher in relapsing patients than in those in stable remission in the entire population, in tapering patients, and in those who stopped DMARDs.
A multivariate analysis found that Vectra DA scores were independent predictors of relapse next to anticitrullinated protein antibody (ACPA) status. Relapse rates were as follows: 13% in VECTRA-low/ACPA-low patients; about one-third in patients positive on one or the other test; and 76.4% in those with high VECTRA DA scores and high ACPA level.
“Vectra DA score improved the prediction of relapses in RA patients in stable remission undergoing DMARD tapering. Combined with ACPA testing, the score allowed a correct identification of relapse in more than 80% of patients,” stated lead author Dr. Juergen Rech of the University of Erlangen-Nuremberg, Germany.
SAN FRANCISCO – Vectra DA, a multibiomarker blood test, can predict response to therapy for patients with rheumatoid arthritis, and it can also identify patients who can safely taper and discontinue disease-modifying antirheumatic drug (DMARD) therapy, according to two separate poster presentations at the annual meeting of the American College of Rheumatology.
Management of patients with RA is typically based on clinical criteria and lab test results. Vectra DA is the only multibiomarker panel available for assessing therapeutic response in RA. The test is Medicare-approved, and Medicare allows about $580 per test, according to a spokesperson for Crescendo Bioscience, the company providing the test. Currently, Vectra DA is used in about 20% of RA patients who are actively managed by a rheumatologist in the United States, and about 40% of U.S. rheumatologists use the test at least once per month, the spokesperson said.
“Vectra DA can assess the risk of radiographic changes and track therapeutic response. Patients with low to moderate Vectra DA scores have a reduced risk of radiographic progression over the next year,” said a coauthor of the first study, Rebecca J. Bolce, an employee of Crescendo.
Response to subsequent therapy
This retrospective study analyzed multibiomarker disease activity score (that is, Vectra DA) in incomplete responders to 3 months of methotrexate monotherapy to predict response to subsequent triple therapy versus biologic therapies. The patient sample came from the SWEFOT (Swedish Farmacotherapy) study of patients with early RA.
After 3 months of methotrexate therapy, 157 nonresponders were randomized to triple therapy or methotrexate plus infliximab (biologic therapy). At the time of randomization, nonresponders were assessed with Vectra DA. Patients with low Vectra DA scores (that is, less than 30) were successfully treated with triple therapy; at 1 year, 88% of these patients achieved low disease activity (a 28-joint Disease Activity Score [DAS28] less than 3.2), compared with 18% assigned to biologic therapy (P = .006).
Patients with a high score on Vectra DA were more likely to respond to biologics. In this group, at 1 year, low disease activity was achieved in 58% of patients randomized to biologics versus 35% randomized to triple therapy (P = .04).
“At 1 year, the Vectra DA score at 3 months was a superior predictor of response to both conventional triple therapy and biologic therapy, compared with C-reactive protein, erythrocyte sedimentation rate, and DAS28,” Ms. Bolce said.
“These findings may help facilitate and improve the development of individualized and cost-effective treatment plans for individuals with RA,” Ms. Bolce said.
Tapering therapy
A second study analyzed the role of multibiomarker disease activity (Vectra DA score) in predicting relapses in RA patients in sustained remission when tapering disease-modifying antirheumatic drug therapy in the context of the RETRO randomized clinical trial.
On a scale from 0-100, Vectra DA scores of less than 30 are categorized as low, scores 30-44 are called moderate, and those greater than 44 are considered high. Scores were calculated and compared between 94 patients who were relapsing or in sustained remission while tapering DMARD therapy.
Patients were randomized to one of three arms: continuation of DMARD; reduction of DMARD by 50%; or reduction of DMARD by 50% for 6 months and then stopping therapy.
Moderate to high scores were found in one-third of RA patients in remission. Scores were twice as high in relapsing patients (58.3%), compared with those in stable remission (25%). Baseline scores were significantly higher in relapsing patients than in those in stable remission in the entire population, in tapering patients, and in those who stopped DMARDs.
A multivariate analysis found that Vectra DA scores were independent predictors of relapse next to anticitrullinated protein antibody (ACPA) status. Relapse rates were as follows: 13% in VECTRA-low/ACPA-low patients; about one-third in patients positive on one or the other test; and 76.4% in those with high VECTRA DA scores and high ACPA level.
“Vectra DA score improved the prediction of relapses in RA patients in stable remission undergoing DMARD tapering. Combined with ACPA testing, the score allowed a correct identification of relapse in more than 80% of patients,” stated lead author Dr. Juergen Rech of the University of Erlangen-Nuremberg, Germany.
SAN FRANCISCO – Vectra DA, a multibiomarker blood test, can predict response to therapy for patients with rheumatoid arthritis, and it can also identify patients who can safely taper and discontinue disease-modifying antirheumatic drug (DMARD) therapy, according to two separate poster presentations at the annual meeting of the American College of Rheumatology.
Management of patients with RA is typically based on clinical criteria and lab test results. Vectra DA is the only multibiomarker panel available for assessing therapeutic response in RA. The test is Medicare-approved, and Medicare allows about $580 per test, according to a spokesperson for Crescendo Bioscience, the company providing the test. Currently, Vectra DA is used in about 20% of RA patients who are actively managed by a rheumatologist in the United States, and about 40% of U.S. rheumatologists use the test at least once per month, the spokesperson said.
“Vectra DA can assess the risk of radiographic changes and track therapeutic response. Patients with low to moderate Vectra DA scores have a reduced risk of radiographic progression over the next year,” said a coauthor of the first study, Rebecca J. Bolce, an employee of Crescendo.
Response to subsequent therapy
This retrospective study analyzed multibiomarker disease activity score (that is, Vectra DA) in incomplete responders to 3 months of methotrexate monotherapy to predict response to subsequent triple therapy versus biologic therapies. The patient sample came from the SWEFOT (Swedish Farmacotherapy) study of patients with early RA.
After 3 months of methotrexate therapy, 157 nonresponders were randomized to triple therapy or methotrexate plus infliximab (biologic therapy). At the time of randomization, nonresponders were assessed with Vectra DA. Patients with low Vectra DA scores (that is, less than 30) were successfully treated with triple therapy; at 1 year, 88% of these patients achieved low disease activity (a 28-joint Disease Activity Score [DAS28] less than 3.2), compared with 18% assigned to biologic therapy (P = .006).
Patients with a high score on Vectra DA were more likely to respond to biologics. In this group, at 1 year, low disease activity was achieved in 58% of patients randomized to biologics versus 35% randomized to triple therapy (P = .04).
“At 1 year, the Vectra DA score at 3 months was a superior predictor of response to both conventional triple therapy and biologic therapy, compared with C-reactive protein, erythrocyte sedimentation rate, and DAS28,” Ms. Bolce said.
“These findings may help facilitate and improve the development of individualized and cost-effective treatment plans for individuals with RA,” Ms. Bolce said.
Tapering therapy
A second study analyzed the role of multibiomarker disease activity (Vectra DA score) in predicting relapses in RA patients in sustained remission when tapering disease-modifying antirheumatic drug therapy in the context of the RETRO randomized clinical trial.
On a scale from 0-100, Vectra DA scores of less than 30 are categorized as low, scores 30-44 are called moderate, and those greater than 44 are considered high. Scores were calculated and compared between 94 patients who were relapsing or in sustained remission while tapering DMARD therapy.
Patients were randomized to one of three arms: continuation of DMARD; reduction of DMARD by 50%; or reduction of DMARD by 50% for 6 months and then stopping therapy.
Moderate to high scores were found in one-third of RA patients in remission. Scores were twice as high in relapsing patients (58.3%), compared with those in stable remission (25%). Baseline scores were significantly higher in relapsing patients than in those in stable remission in the entire population, in tapering patients, and in those who stopped DMARDs.
A multivariate analysis found that Vectra DA scores were independent predictors of relapse next to anticitrullinated protein antibody (ACPA) status. Relapse rates were as follows: 13% in VECTRA-low/ACPA-low patients; about one-third in patients positive on one or the other test; and 76.4% in those with high VECTRA DA scores and high ACPA level.
“Vectra DA score improved the prediction of relapses in RA patients in stable remission undergoing DMARD tapering. Combined with ACPA testing, the score allowed a correct identification of relapse in more than 80% of patients,” stated lead author Dr. Juergen Rech of the University of Erlangen-Nuremberg, Germany.
AT THE ACR ANNUAL MEETING
Key clinical point: A multibiomarker-based blood test identifies specific therapies for RA patients and helps to decide who can safely taper or discontinue their RA medications.
Major finding: At 1 year, 88% of patients with low Vectra DA scores achieved low disease activity, compared with 18% on biologics; those with a high Vectra DA score were more likely to respond to biologics; at 1 year, 58% of patients treated with biologics achieved low disease activity, compared with 35% for patients treated with triple therapy.
Data source: Retrospective analyses of two prospective studies.
Disclosures: The studies were sponsored by Crescendo Bioscience. Rebecca J. Bolce is an employee of Crescendo Bioscience. Juergen Rech had no financial disclosures.