User login
Abilify Maintena OK’d by FDA for adults with bipolar I disorder
The Food and Drug Administration has approved a monthly injectable formulation of aripiprazole, (Abilify Maintena) , for a maintenance monotherapy treatment of bipolar I disorder for adults, Otsuka and Lundbeck have announced.
Patients treated with the injectable formulation of the atypical antipsychotic must continue to take a daily oral antipsychotic for the first 14 days. After that, however, the long-acting injectable (LAI) – which must be administered by a health care professional – can replace the daily medication.
Joseph R. Calabrese, MD, director of the mood disorders program at University Hospitals Cleveland Medical Center, said in the July 28 announcement that the LAI is a new treatment option for bipolar I patients “who have established tolerability with oral aripiprazole.”
The drug label includes a warning that elderly patients with dementia-related psychosis who are treated with antipsychotics are at a higher mortality risk. Adverse reactions that have been associated with treatment with aripiprazole include weight gain, akathisia, injection site pain, sedation, and certain compulsive behaviors.
Created by Otsuka, and marketed by Otsuka and Lundbeck, the LAI was approved in the United States for treating adults with schizophrenia in 2013.
The Food and Drug Administration has approved a monthly injectable formulation of aripiprazole, (Abilify Maintena) , for a maintenance monotherapy treatment of bipolar I disorder for adults, Otsuka and Lundbeck have announced.
Patients treated with the injectable formulation of the atypical antipsychotic must continue to take a daily oral antipsychotic for the first 14 days. After that, however, the long-acting injectable (LAI) – which must be administered by a health care professional – can replace the daily medication.
Joseph R. Calabrese, MD, director of the mood disorders program at University Hospitals Cleveland Medical Center, said in the July 28 announcement that the LAI is a new treatment option for bipolar I patients “who have established tolerability with oral aripiprazole.”
The drug label includes a warning that elderly patients with dementia-related psychosis who are treated with antipsychotics are at a higher mortality risk. Adverse reactions that have been associated with treatment with aripiprazole include weight gain, akathisia, injection site pain, sedation, and certain compulsive behaviors.
Created by Otsuka, and marketed by Otsuka and Lundbeck, the LAI was approved in the United States for treating adults with schizophrenia in 2013.
The Food and Drug Administration has approved a monthly injectable formulation of aripiprazole, (Abilify Maintena) , for a maintenance monotherapy treatment of bipolar I disorder for adults, Otsuka and Lundbeck have announced.
Patients treated with the injectable formulation of the atypical antipsychotic must continue to take a daily oral antipsychotic for the first 14 days. After that, however, the long-acting injectable (LAI) – which must be administered by a health care professional – can replace the daily medication.
Joseph R. Calabrese, MD, director of the mood disorders program at University Hospitals Cleveland Medical Center, said in the July 28 announcement that the LAI is a new treatment option for bipolar I patients “who have established tolerability with oral aripiprazole.”
The drug label includes a warning that elderly patients with dementia-related psychosis who are treated with antipsychotics are at a higher mortality risk. Adverse reactions that have been associated with treatment with aripiprazole include weight gain, akathisia, injection site pain, sedation, and certain compulsive behaviors.
Created by Otsuka, and marketed by Otsuka and Lundbeck, the LAI was approved in the United States for treating adults with schizophrenia in 2013.
First interchangeability study for an adalimumab biosimilar has begun
The VOLTAIRE-X study of a biosimilar candidate for adalimumab (Humira) for chronic plaque psoriasis has enrolled its first patient, announced Boehringer Ingelheim, the biosimilar’s developer, on July 27.
This is the first study in the United States to investigate whether a biosimilar candidate should be granted an interchangeability designation with adalimumab. The candidate, BI 695501, is up against adalimumab’s 40-mg injection.
In VOLTAIRE-X, some patients will alternate between adalimumab and BI 695501, and others will take adalimumab continuously. The study will compare the pharmacokinetics, clinical outcomes, safety, immunogenicity, and efficacy between the two groups of patients. The estimated enrollment of adult patients with moderate to severe chronic plaque psoriasis is 240, and the study is expected to conclude in July 2019.
A phase 3 study of BI 695501’s performance for rheumatoid arthritis patients, completed in 2016, demonstrated similar efficacy, safety, and immunogenicity.
The VOLTAIRE-X study of a biosimilar candidate for adalimumab (Humira) for chronic plaque psoriasis has enrolled its first patient, announced Boehringer Ingelheim, the biosimilar’s developer, on July 27.
This is the first study in the United States to investigate whether a biosimilar candidate should be granted an interchangeability designation with adalimumab. The candidate, BI 695501, is up against adalimumab’s 40-mg injection.
In VOLTAIRE-X, some patients will alternate between adalimumab and BI 695501, and others will take adalimumab continuously. The study will compare the pharmacokinetics, clinical outcomes, safety, immunogenicity, and efficacy between the two groups of patients. The estimated enrollment of adult patients with moderate to severe chronic plaque psoriasis is 240, and the study is expected to conclude in July 2019.
A phase 3 study of BI 695501’s performance for rheumatoid arthritis patients, completed in 2016, demonstrated similar efficacy, safety, and immunogenicity.
The VOLTAIRE-X study of a biosimilar candidate for adalimumab (Humira) for chronic plaque psoriasis has enrolled its first patient, announced Boehringer Ingelheim, the biosimilar’s developer, on July 27.
This is the first study in the United States to investigate whether a biosimilar candidate should be granted an interchangeability designation with adalimumab. The candidate, BI 695501, is up against adalimumab’s 40-mg injection.
In VOLTAIRE-X, some patients will alternate between adalimumab and BI 695501, and others will take adalimumab continuously. The study will compare the pharmacokinetics, clinical outcomes, safety, immunogenicity, and efficacy between the two groups of patients. The estimated enrollment of adult patients with moderate to severe chronic plaque psoriasis is 240, and the study is expected to conclude in July 2019.
A phase 3 study of BI 695501’s performance for rheumatoid arthritis patients, completed in 2016, demonstrated similar efficacy, safety, and immunogenicity.
New monotherapy approved for partial-onset seizures
The U.S. Food and Drug Administration has approved perampanel (Fycompa) for monotherapy treatment of partial-onset seizures (POS) in patients aged 12 years or older as of July 27. It was approved in 2012 for adjunctive use for POS and primary, generalized tonic-clonic seizures in patients aged 12 years or older.
Three clinical trials showed improvement in seizure control for the patients with POS taking perampanel, compared with placebo.
The drug is available in tablets from 2 mg to 12 mg and as an oral suspension formulation. It is taken once daily.
“Approximately one-third of people living with epilepsy have seizures that are not adequately controlled,” said Robert T. Wechsler, MD, PhD, medical director of the Idaho Comprehensive Epilepsy Center, in Eisai’s press release. “Having a new monotherapy option for partial-onset seizures that is once a day gives physicians and patients an effective treatment option that has the potential to make a difference in patients’ lives.”
The U.S. Food and Drug Administration has approved perampanel (Fycompa) for monotherapy treatment of partial-onset seizures (POS) in patients aged 12 years or older as of July 27. It was approved in 2012 for adjunctive use for POS and primary, generalized tonic-clonic seizures in patients aged 12 years or older.
Three clinical trials showed improvement in seizure control for the patients with POS taking perampanel, compared with placebo.
The drug is available in tablets from 2 mg to 12 mg and as an oral suspension formulation. It is taken once daily.
“Approximately one-third of people living with epilepsy have seizures that are not adequately controlled,” said Robert T. Wechsler, MD, PhD, medical director of the Idaho Comprehensive Epilepsy Center, in Eisai’s press release. “Having a new monotherapy option for partial-onset seizures that is once a day gives physicians and patients an effective treatment option that has the potential to make a difference in patients’ lives.”
The U.S. Food and Drug Administration has approved perampanel (Fycompa) for monotherapy treatment of partial-onset seizures (POS) in patients aged 12 years or older as of July 27. It was approved in 2012 for adjunctive use for POS and primary, generalized tonic-clonic seizures in patients aged 12 years or older.
Three clinical trials showed improvement in seizure control for the patients with POS taking perampanel, compared with placebo.
The drug is available in tablets from 2 mg to 12 mg and as an oral suspension formulation. It is taken once daily.
“Approximately one-third of people living with epilepsy have seizures that are not adequately controlled,” said Robert T. Wechsler, MD, PhD, medical director of the Idaho Comprehensive Epilepsy Center, in Eisai’s press release. “Having a new monotherapy option for partial-onset seizures that is once a day gives physicians and patients an effective treatment option that has the potential to make a difference in patients’ lives.”
Self-injectable belimumab receives FDA approval for systemic lupus erythematosus
GlaxoSmithKline announced on July 21 that it had received approval from the U.S. Food and Drug Administration for a new, self-injectable form of belimumab (Benlysta) for adult patients with systemic lupus erythematosus (SLE). Belimumab has previously been approved for SLE, in 2011, in an intravenous formulation.
The new formulation is the first self-injectable subcutaneous treatment available for patients with SLE. The previous treatment required 1 hour of intravenous infusion every 4 weeks, while the new treatment is 1 weekly injection.
Two of the 280 patients receiving placebo (0.7%) died during the study, as did 3 of the 556 patients receiving belimumab (0.5%). Serious infections occurred in 4.1% and 5.4% of patients receiving belimumab and placebo, respectively.
“The safety profile observed for Benlysta administered subcutaneously was consistent with the known safety profile of Benlysta administered intravenously, with the exception of local injection site reactions,” noted GlaxoSmithKline in its announcement. Each form of the drug has a risk of a reaction, whether an infusion reaction for IV administration or a hypersensitivity reaction for self-injection. A patient who reacted to the intravenous formulation with anaphylaxis is contraindicated for the self-injectable version.
It is not known what effect belimumab has on the risk of birth defects or miscarriage, so birth control is recommended for patients on the drug. Likewise, the effects of the drug on breast milk are not known. As belimumab may interfere with immunizations, a patient should not be vaccinated 30 days before or after taking the drug.
GlaxoSmithKline announced on July 21 that it had received approval from the U.S. Food and Drug Administration for a new, self-injectable form of belimumab (Benlysta) for adult patients with systemic lupus erythematosus (SLE). Belimumab has previously been approved for SLE, in 2011, in an intravenous formulation.
The new formulation is the first self-injectable subcutaneous treatment available for patients with SLE. The previous treatment required 1 hour of intravenous infusion every 4 weeks, while the new treatment is 1 weekly injection.
Two of the 280 patients receiving placebo (0.7%) died during the study, as did 3 of the 556 patients receiving belimumab (0.5%). Serious infections occurred in 4.1% and 5.4% of patients receiving belimumab and placebo, respectively.
“The safety profile observed for Benlysta administered subcutaneously was consistent with the known safety profile of Benlysta administered intravenously, with the exception of local injection site reactions,” noted GlaxoSmithKline in its announcement. Each form of the drug has a risk of a reaction, whether an infusion reaction for IV administration or a hypersensitivity reaction for self-injection. A patient who reacted to the intravenous formulation with anaphylaxis is contraindicated for the self-injectable version.
It is not known what effect belimumab has on the risk of birth defects or miscarriage, so birth control is recommended for patients on the drug. Likewise, the effects of the drug on breast milk are not known. As belimumab may interfere with immunizations, a patient should not be vaccinated 30 days before or after taking the drug.
GlaxoSmithKline announced on July 21 that it had received approval from the U.S. Food and Drug Administration for a new, self-injectable form of belimumab (Benlysta) for adult patients with systemic lupus erythematosus (SLE). Belimumab has previously been approved for SLE, in 2011, in an intravenous formulation.
The new formulation is the first self-injectable subcutaneous treatment available for patients with SLE. The previous treatment required 1 hour of intravenous infusion every 4 weeks, while the new treatment is 1 weekly injection.
Two of the 280 patients receiving placebo (0.7%) died during the study, as did 3 of the 556 patients receiving belimumab (0.5%). Serious infections occurred in 4.1% and 5.4% of patients receiving belimumab and placebo, respectively.
“The safety profile observed for Benlysta administered subcutaneously was consistent with the known safety profile of Benlysta administered intravenously, with the exception of local injection site reactions,” noted GlaxoSmithKline in its announcement. Each form of the drug has a risk of a reaction, whether an infusion reaction for IV administration or a hypersensitivity reaction for self-injection. A patient who reacted to the intravenous formulation with anaphylaxis is contraindicated for the self-injectable version.
It is not known what effect belimumab has on the risk of birth defects or miscarriage, so birth control is recommended for patients on the drug. Likewise, the effects of the drug on breast milk are not known. As belimumab may interfere with immunizations, a patient should not be vaccinated 30 days before or after taking the drug.
FDA okays ClearLLab test for hematologic cancer detection
Beckman Coulter has been authorized to market its ClearLLab Reagents (T1, T2, B1, B2, M) tests for use with flow cytometry to detect leukemias, lymphomas, and myeloproliferative disorders in blood, bone marrow, and lymph nodes, according to the U.S. Food and Drug Administration.
A study evaluating the efficacy of the test compared the test results (n = 279) with clinical evaluations at four independent clinical sites. The results matched the diagnoses 93.4% of the time and correctly detected cancer 84.2% of the time.
“This represents a major step forward for the hematology-oncology community,” Alberto Gutierrez, PhD, of the FDA’s Center for Devices and Radiological Health said in the FDA’s release. “Laboratories and health care professionals now have access to an FDA-validated test that provides consistent results to aid in the diagnoses of these serious cancers.”
The approval coincides with criteria for ongoing evaluation of the ClearLLab tests and approval of future tests. The release notes that the ClearLLab test results must be reviewed by a trained professional.
Beckman Coulter has been authorized to market its ClearLLab Reagents (T1, T2, B1, B2, M) tests for use with flow cytometry to detect leukemias, lymphomas, and myeloproliferative disorders in blood, bone marrow, and lymph nodes, according to the U.S. Food and Drug Administration.
A study evaluating the efficacy of the test compared the test results (n = 279) with clinical evaluations at four independent clinical sites. The results matched the diagnoses 93.4% of the time and correctly detected cancer 84.2% of the time.
“This represents a major step forward for the hematology-oncology community,” Alberto Gutierrez, PhD, of the FDA’s Center for Devices and Radiological Health said in the FDA’s release. “Laboratories and health care professionals now have access to an FDA-validated test that provides consistent results to aid in the diagnoses of these serious cancers.”
The approval coincides with criteria for ongoing evaluation of the ClearLLab tests and approval of future tests. The release notes that the ClearLLab test results must be reviewed by a trained professional.
Beckman Coulter has been authorized to market its ClearLLab Reagents (T1, T2, B1, B2, M) tests for use with flow cytometry to detect leukemias, lymphomas, and myeloproliferative disorders in blood, bone marrow, and lymph nodes, according to the U.S. Food and Drug Administration.
A study evaluating the efficacy of the test compared the test results (n = 279) with clinical evaluations at four independent clinical sites. The results matched the diagnoses 93.4% of the time and correctly detected cancer 84.2% of the time.
“This represents a major step forward for the hematology-oncology community,” Alberto Gutierrez, PhD, of the FDA’s Center for Devices and Radiological Health said in the FDA’s release. “Laboratories and health care professionals now have access to an FDA-validated test that provides consistent results to aid in the diagnoses of these serious cancers.”
The approval coincides with criteria for ongoing evaluation of the ClearLLab tests and approval of future tests. The release notes that the ClearLLab test results must be reviewed by a trained professional.
Multiply recurrent C. difficile infection is on the rise
A retrospective cohort study of Clostridium difficile infection (CDI), the most common health care–associated infection, found that multiply recurrent CDI (mrCDI) is increasing in incidence, disproportionately to the overall increase in CDI.
Researchers from the University of Pennsylvania, Philadelphia, worked with a database of more than 38 million individuals with private health insurance between January 2001 and December 2012.
Cases of CDI and mrCDI in the study population were determined through ICD-9 diagnosis codes, and prescriptions for treatment. To meet the definition of mrCDI, there had to be at least three courses of treatment lasting at least 14 days each.
In the study population, 45,341 persons developed CDI, of whom 1,669 had mrCDI. The median age was 46 years, and 58.9% were female. Between 2001 and 2012, CDI incidence increased by 42.7% (P = .004), while mrCDI incidence increased by 188.8% (P less than .001).
With increases in CDI and mrCDI incidence, and with the effectiveness of standard antibiotic treatment decreasing with each recurrence, “demand for new antimicrobial therapies and FMT [fecal microbiota transplantation] can be expected to increase considerably in the coming years,” wrote Gene K. Ma, MD, and his coauthors.
As for FMT, the researchers noted that its likely greater demand in the future (as suggested by their study results) highlights the importance of establishing the long-term safety of the procedure (Ann Intern Med. 2017 Jul. doi: 10.7326/M16-2733).
The retrospective cohort study was based on administrative data rather than laboratory data, Sameer D. Saini, MD, MS, and Akbar K. Waljee, MD, noted in an editorial accompanying the study. Further, with Medicare patients excluded from the study (because Medicare data were not available for the full time period studied for private insurance data), the data may not be of relevance to patients older than age 65 years.
But the general conclusion that both CDI and mrCDI are on the rise is a crucial matter. “We must first have a better understanding of mrCDI, its scope and epidemiology, and its associated risk factors. The study by Ma and colleagues begins this important work. A better understanding of the epidemiology of mrCDI is a critical first step toward developing a sound strategy to address this growing public health challenge.”
Dr. Saini and Dr. Waljee are with the VA Ann Arbor (Michigan) Center for Clinical Management. Their editorial accompanied the study in Annals of Internal Medicine (2017 Jul. doi: 10.7326/M17-1565).
The retrospective cohort study was based on administrative data rather than laboratory data, Sameer D. Saini, MD, MS, and Akbar K. Waljee, MD, noted in an editorial accompanying the study. Further, with Medicare patients excluded from the study (because Medicare data were not available for the full time period studied for private insurance data), the data may not be of relevance to patients older than age 65 years.
But the general conclusion that both CDI and mrCDI are on the rise is a crucial matter. “We must first have a better understanding of mrCDI, its scope and epidemiology, and its associated risk factors. The study by Ma and colleagues begins this important work. A better understanding of the epidemiology of mrCDI is a critical first step toward developing a sound strategy to address this growing public health challenge.”
Dr. Saini and Dr. Waljee are with the VA Ann Arbor (Michigan) Center for Clinical Management. Their editorial accompanied the study in Annals of Internal Medicine (2017 Jul. doi: 10.7326/M17-1565).
The retrospective cohort study was based on administrative data rather than laboratory data, Sameer D. Saini, MD, MS, and Akbar K. Waljee, MD, noted in an editorial accompanying the study. Further, with Medicare patients excluded from the study (because Medicare data were not available for the full time period studied for private insurance data), the data may not be of relevance to patients older than age 65 years.
But the general conclusion that both CDI and mrCDI are on the rise is a crucial matter. “We must first have a better understanding of mrCDI, its scope and epidemiology, and its associated risk factors. The study by Ma and colleagues begins this important work. A better understanding of the epidemiology of mrCDI is a critical first step toward developing a sound strategy to address this growing public health challenge.”
Dr. Saini and Dr. Waljee are with the VA Ann Arbor (Michigan) Center for Clinical Management. Their editorial accompanied the study in Annals of Internal Medicine (2017 Jul. doi: 10.7326/M17-1565).
A retrospective cohort study of Clostridium difficile infection (CDI), the most common health care–associated infection, found that multiply recurrent CDI (mrCDI) is increasing in incidence, disproportionately to the overall increase in CDI.
Researchers from the University of Pennsylvania, Philadelphia, worked with a database of more than 38 million individuals with private health insurance between January 2001 and December 2012.
Cases of CDI and mrCDI in the study population were determined through ICD-9 diagnosis codes, and prescriptions for treatment. To meet the definition of mrCDI, there had to be at least three courses of treatment lasting at least 14 days each.
In the study population, 45,341 persons developed CDI, of whom 1,669 had mrCDI. The median age was 46 years, and 58.9% were female. Between 2001 and 2012, CDI incidence increased by 42.7% (P = .004), while mrCDI incidence increased by 188.8% (P less than .001).
With increases in CDI and mrCDI incidence, and with the effectiveness of standard antibiotic treatment decreasing with each recurrence, “demand for new antimicrobial therapies and FMT [fecal microbiota transplantation] can be expected to increase considerably in the coming years,” wrote Gene K. Ma, MD, and his coauthors.
As for FMT, the researchers noted that its likely greater demand in the future (as suggested by their study results) highlights the importance of establishing the long-term safety of the procedure (Ann Intern Med. 2017 Jul. doi: 10.7326/M16-2733).
A retrospective cohort study of Clostridium difficile infection (CDI), the most common health care–associated infection, found that multiply recurrent CDI (mrCDI) is increasing in incidence, disproportionately to the overall increase in CDI.
Researchers from the University of Pennsylvania, Philadelphia, worked with a database of more than 38 million individuals with private health insurance between January 2001 and December 2012.
Cases of CDI and mrCDI in the study population were determined through ICD-9 diagnosis codes, and prescriptions for treatment. To meet the definition of mrCDI, there had to be at least three courses of treatment lasting at least 14 days each.
In the study population, 45,341 persons developed CDI, of whom 1,669 had mrCDI. The median age was 46 years, and 58.9% were female. Between 2001 and 2012, CDI incidence increased by 42.7% (P = .004), while mrCDI incidence increased by 188.8% (P less than .001).
With increases in CDI and mrCDI incidence, and with the effectiveness of standard antibiotic treatment decreasing with each recurrence, “demand for new antimicrobial therapies and FMT [fecal microbiota transplantation] can be expected to increase considerably in the coming years,” wrote Gene K. Ma, MD, and his coauthors.
As for FMT, the researchers noted that its likely greater demand in the future (as suggested by their study results) highlights the importance of establishing the long-term safety of the procedure (Ann Intern Med. 2017 Jul. doi: 10.7326/M16-2733).
FROM ANNALS OF INTERNAL MEDICINE
Dietary carbohydrate and glycemic load linked to acne
A cross-sectional study of 64 adults in New York City with and without moderate/severe acne found a significant association between dietary carbohydrate consumption and acne, which the authors said merited further study.
“Epidemiologic studies typically report a low incidence of acne in non-developed nations, suggesting that environmental factors, such as diet, can play a role in acne pathogenesis,” wrote Jennifer Burris, PhD, of the department of nutrition and food studies, at Steinhardt School of Culture, Education, and Human Development, New York University, and her coauthors.
The study participants either had no acne (32) or had moderate or severe acne (32); those with mild or shorter-term acne (less than 6 months) were excluded. They made a 5-day food record and took a questionnaire, and had blood drawn and anthropometric measurements taken during two visits.
Moderate and severe acne was associated with significantly greater total carbohydrate consumption (P = .003), available carbohydrate (total carbohydrate minus dietary fiber), percent energy from carbohydrate, and glycemic load (all P less than .001), compared with those who did not have acne.
The patients with moderate or severe acne also had greater insulin and insulin growth factor–1 concentrations, and lower sex hormone–binding globulin concentrations, (P = .002, .009, and .015, respectively); and greater insulin resistance (P = .001), compared with those who did not have acne.
“Although the results from our study cannot determine causation, these preliminary results suggest a relationship between dietary [glycemic load] and acne,” Dr. Burris and her coauthors wrote. “In addition to replicating our findings, future research is necessary to elucidate the mechanisms linking diet and acne and to evaluate the effectiveness of [medical nutrition therapy] on biological factors associated with acne and conceivably acne-specific quality of life,” they added (J Acad Nutr Diet. 2017 Jun 9. doi: 10.1016/j.jand.2017.03.024).
[email protected]
A cross-sectional study of 64 adults in New York City with and without moderate/severe acne found a significant association between dietary carbohydrate consumption and acne, which the authors said merited further study.
“Epidemiologic studies typically report a low incidence of acne in non-developed nations, suggesting that environmental factors, such as diet, can play a role in acne pathogenesis,” wrote Jennifer Burris, PhD, of the department of nutrition and food studies, at Steinhardt School of Culture, Education, and Human Development, New York University, and her coauthors.
The study participants either had no acne (32) or had moderate or severe acne (32); those with mild or shorter-term acne (less than 6 months) were excluded. They made a 5-day food record and took a questionnaire, and had blood drawn and anthropometric measurements taken during two visits.
Moderate and severe acne was associated with significantly greater total carbohydrate consumption (P = .003), available carbohydrate (total carbohydrate minus dietary fiber), percent energy from carbohydrate, and glycemic load (all P less than .001), compared with those who did not have acne.
The patients with moderate or severe acne also had greater insulin and insulin growth factor–1 concentrations, and lower sex hormone–binding globulin concentrations, (P = .002, .009, and .015, respectively); and greater insulin resistance (P = .001), compared with those who did not have acne.
“Although the results from our study cannot determine causation, these preliminary results suggest a relationship between dietary [glycemic load] and acne,” Dr. Burris and her coauthors wrote. “In addition to replicating our findings, future research is necessary to elucidate the mechanisms linking diet and acne and to evaluate the effectiveness of [medical nutrition therapy] on biological factors associated with acne and conceivably acne-specific quality of life,” they added (J Acad Nutr Diet. 2017 Jun 9. doi: 10.1016/j.jand.2017.03.024).
[email protected]
A cross-sectional study of 64 adults in New York City with and without moderate/severe acne found a significant association between dietary carbohydrate consumption and acne, which the authors said merited further study.
“Epidemiologic studies typically report a low incidence of acne in non-developed nations, suggesting that environmental factors, such as diet, can play a role in acne pathogenesis,” wrote Jennifer Burris, PhD, of the department of nutrition and food studies, at Steinhardt School of Culture, Education, and Human Development, New York University, and her coauthors.
The study participants either had no acne (32) or had moderate or severe acne (32); those with mild or shorter-term acne (less than 6 months) were excluded. They made a 5-day food record and took a questionnaire, and had blood drawn and anthropometric measurements taken during two visits.
Moderate and severe acne was associated with significantly greater total carbohydrate consumption (P = .003), available carbohydrate (total carbohydrate minus dietary fiber), percent energy from carbohydrate, and glycemic load (all P less than .001), compared with those who did not have acne.
The patients with moderate or severe acne also had greater insulin and insulin growth factor–1 concentrations, and lower sex hormone–binding globulin concentrations, (P = .002, .009, and .015, respectively); and greater insulin resistance (P = .001), compared with those who did not have acne.
“Although the results from our study cannot determine causation, these preliminary results suggest a relationship between dietary [glycemic load] and acne,” Dr. Burris and her coauthors wrote. “In addition to replicating our findings, future research is necessary to elucidate the mechanisms linking diet and acne and to evaluate the effectiveness of [medical nutrition therapy] on biological factors associated with acne and conceivably acne-specific quality of life,” they added (J Acad Nutr Diet. 2017 Jun 9. doi: 10.1016/j.jand.2017.03.024).
[email protected]
FROM THE JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICS
Isotretinoin not associated with increased depression risk, in meta-analysis
A meta-analysis of 31 studies examining the relationship between isotretinoin treatment for acne and depression found no significant association. Rather, the treatment of acne was associated with improved symptoms of depression.
Researchers have been evaluating isotretinoin’s possible association with depression since 1983. Many studies have failed to find an association or have been inconclusive. One study found a statistically significant association between isotretinoin treatment and depression, but there are also depression risks associated with not treating a patient with severe acne.
Gathering the existing literature into a meta-analysis allowed the researchers to assess possible confounding factors in the individual studies, such as sex, length of treatment, and cumulative isotretinoin dose.
“In our meta-analysis, we pooled the results of 1,411 patients who received depression evaluations at baseline and after treatment, which revealed a significant improvement in the depression scores,” wrote Yu-Chen Huang, MD, of the department of dermatology, Taipei Medical University, Taiwan, and Ying-Chih Cheng, MD, of National Taiwan University. The 31 studies included 3 population-based studies, 8 controlled studies, and 20 prospective, open-label studies, and were published through September 2016.
Prevalence of depression also significantly dropped after treatment (relative risk, .588), they wrote, but they pointed out that “some studies described newly developed depression during treatment.” They referred to one controlled study in which “new onset of depression was noted in both the isotretinoin and antibiotic groups, implying that depression is associated with acne, independently of isotretinoin” (World J Psychiatr. 2016 Mar 22;6[1]:136-42). “Thus, physicians should consider the possibility of depression among all acne patients regardless of the treatment method,” they added.
They also concluded that some patients “might be more prone to depression regardless of acne or other conditions. Thus, closely monitoring acne patients for depression is essential to identify patients at a high risk.”
The full study can be found at: J Am Acad Dermatol. 2017 Jun;76[6]:1068-76.
A meta-analysis of 31 studies examining the relationship between isotretinoin treatment for acne and depression found no significant association. Rather, the treatment of acne was associated with improved symptoms of depression.
Researchers have been evaluating isotretinoin’s possible association with depression since 1983. Many studies have failed to find an association or have been inconclusive. One study found a statistically significant association between isotretinoin treatment and depression, but there are also depression risks associated with not treating a patient with severe acne.
Gathering the existing literature into a meta-analysis allowed the researchers to assess possible confounding factors in the individual studies, such as sex, length of treatment, and cumulative isotretinoin dose.
“In our meta-analysis, we pooled the results of 1,411 patients who received depression evaluations at baseline and after treatment, which revealed a significant improvement in the depression scores,” wrote Yu-Chen Huang, MD, of the department of dermatology, Taipei Medical University, Taiwan, and Ying-Chih Cheng, MD, of National Taiwan University. The 31 studies included 3 population-based studies, 8 controlled studies, and 20 prospective, open-label studies, and were published through September 2016.
Prevalence of depression also significantly dropped after treatment (relative risk, .588), they wrote, but they pointed out that “some studies described newly developed depression during treatment.” They referred to one controlled study in which “new onset of depression was noted in both the isotretinoin and antibiotic groups, implying that depression is associated with acne, independently of isotretinoin” (World J Psychiatr. 2016 Mar 22;6[1]:136-42). “Thus, physicians should consider the possibility of depression among all acne patients regardless of the treatment method,” they added.
They also concluded that some patients “might be more prone to depression regardless of acne or other conditions. Thus, closely monitoring acne patients for depression is essential to identify patients at a high risk.”
The full study can be found at: J Am Acad Dermatol. 2017 Jun;76[6]:1068-76.
A meta-analysis of 31 studies examining the relationship between isotretinoin treatment for acne and depression found no significant association. Rather, the treatment of acne was associated with improved symptoms of depression.
Researchers have been evaluating isotretinoin’s possible association with depression since 1983. Many studies have failed to find an association or have been inconclusive. One study found a statistically significant association between isotretinoin treatment and depression, but there are also depression risks associated with not treating a patient with severe acne.
Gathering the existing literature into a meta-analysis allowed the researchers to assess possible confounding factors in the individual studies, such as sex, length of treatment, and cumulative isotretinoin dose.
“In our meta-analysis, we pooled the results of 1,411 patients who received depression evaluations at baseline and after treatment, which revealed a significant improvement in the depression scores,” wrote Yu-Chen Huang, MD, of the department of dermatology, Taipei Medical University, Taiwan, and Ying-Chih Cheng, MD, of National Taiwan University. The 31 studies included 3 population-based studies, 8 controlled studies, and 20 prospective, open-label studies, and were published through September 2016.
Prevalence of depression also significantly dropped after treatment (relative risk, .588), they wrote, but they pointed out that “some studies described newly developed depression during treatment.” They referred to one controlled study in which “new onset of depression was noted in both the isotretinoin and antibiotic groups, implying that depression is associated with acne, independently of isotretinoin” (World J Psychiatr. 2016 Mar 22;6[1]:136-42). “Thus, physicians should consider the possibility of depression among all acne patients regardless of the treatment method,” they added.
They also concluded that some patients “might be more prone to depression regardless of acne or other conditions. Thus, closely monitoring acne patients for depression is essential to identify patients at a high risk.”
The full study can be found at: J Am Acad Dermatol. 2017 Jun;76[6]:1068-76.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
U.S. malaria cases dipped slightly in 2014
The number of confirmed malaria cases reported in the United States in 2014 is the fourth highest annual total since 1973, according to the Centers for Disease Control and Prevention, but the 2014 number of 1,724 cases is down slightly from 1,741 – the previous year’s number of confirmed cases.
The CDC monitors malaria cases in part to identify any instances of local, rather than imported, transmission. For 2014, no cases of local transmission were reported.
Of the imported transmission cases for which the region of acquisition was known, 1,383 (82.1%) came from Africa and 160 (9.5%) from Asia, making up all but 62 of the imported cases. The four leading countries of origin in Africa were Nigeria, Ghana, Sierra Leone, and Liberia (346, 153, 133, and 125 cases, respectively). Most of the cases from Asia came from India, which accounted for 100 of the 160 cases.
Sierra Leone, Liberia, and Guinea were the countries primarily affected by the Ebola virus disease outbreak in 2014 and into 2015. The study authors, Kimberly E. Mace, PhD, and Paul M. Arguin, MD, noted in the May 26 Morbidity and Mortality Weekly Report that “Ebola negatively impacted the delivery of malaria care and prevention services in the Ebola-affected countries, which could have increased malaria morbidity and mortality” (MMWR Surveill Summ. 2017;66[12]:1-24).
“Despite progress in reducing global prevalence of malaria, the disease remains endemic in many regions and use of appropriate prevention measures by travelers is still inadequate,” they added.
Among all cases, 17% were classified as severe illness, including five deaths (a decrease from 10 deaths in 2013). All five patients who died reported not taking chemoprophylaxis during their travel. More than half (57.5%) of the patients reported that the purpose of their travel was to visit friends and relatives.
“Health care providers should talk to their patients, especially those who would travel to countries where malaria is endemic to visit friends and relatives, about upcoming travel plans and offer education and medicines to prevent malaria,” the authors wrote.
The number of confirmed malaria cases reported in the United States in 2014 is the fourth highest annual total since 1973, according to the Centers for Disease Control and Prevention, but the 2014 number of 1,724 cases is down slightly from 1,741 – the previous year’s number of confirmed cases.
The CDC monitors malaria cases in part to identify any instances of local, rather than imported, transmission. For 2014, no cases of local transmission were reported.
Of the imported transmission cases for which the region of acquisition was known, 1,383 (82.1%) came from Africa and 160 (9.5%) from Asia, making up all but 62 of the imported cases. The four leading countries of origin in Africa were Nigeria, Ghana, Sierra Leone, and Liberia (346, 153, 133, and 125 cases, respectively). Most of the cases from Asia came from India, which accounted for 100 of the 160 cases.
Sierra Leone, Liberia, and Guinea were the countries primarily affected by the Ebola virus disease outbreak in 2014 and into 2015. The study authors, Kimberly E. Mace, PhD, and Paul M. Arguin, MD, noted in the May 26 Morbidity and Mortality Weekly Report that “Ebola negatively impacted the delivery of malaria care and prevention services in the Ebola-affected countries, which could have increased malaria morbidity and mortality” (MMWR Surveill Summ. 2017;66[12]:1-24).
“Despite progress in reducing global prevalence of malaria, the disease remains endemic in many regions and use of appropriate prevention measures by travelers is still inadequate,” they added.
Among all cases, 17% were classified as severe illness, including five deaths (a decrease from 10 deaths in 2013). All five patients who died reported not taking chemoprophylaxis during their travel. More than half (57.5%) of the patients reported that the purpose of their travel was to visit friends and relatives.
“Health care providers should talk to their patients, especially those who would travel to countries where malaria is endemic to visit friends and relatives, about upcoming travel plans and offer education and medicines to prevent malaria,” the authors wrote.
The number of confirmed malaria cases reported in the United States in 2014 is the fourth highest annual total since 1973, according to the Centers for Disease Control and Prevention, but the 2014 number of 1,724 cases is down slightly from 1,741 – the previous year’s number of confirmed cases.
The CDC monitors malaria cases in part to identify any instances of local, rather than imported, transmission. For 2014, no cases of local transmission were reported.
Of the imported transmission cases for which the region of acquisition was known, 1,383 (82.1%) came from Africa and 160 (9.5%) from Asia, making up all but 62 of the imported cases. The four leading countries of origin in Africa were Nigeria, Ghana, Sierra Leone, and Liberia (346, 153, 133, and 125 cases, respectively). Most of the cases from Asia came from India, which accounted for 100 of the 160 cases.
Sierra Leone, Liberia, and Guinea were the countries primarily affected by the Ebola virus disease outbreak in 2014 and into 2015. The study authors, Kimberly E. Mace, PhD, and Paul M. Arguin, MD, noted in the May 26 Morbidity and Mortality Weekly Report that “Ebola negatively impacted the delivery of malaria care and prevention services in the Ebola-affected countries, which could have increased malaria morbidity and mortality” (MMWR Surveill Summ. 2017;66[12]:1-24).
“Despite progress in reducing global prevalence of malaria, the disease remains endemic in many regions and use of appropriate prevention measures by travelers is still inadequate,” they added.
Among all cases, 17% were classified as severe illness, including five deaths (a decrease from 10 deaths in 2013). All five patients who died reported not taking chemoprophylaxis during their travel. More than half (57.5%) of the patients reported that the purpose of their travel was to visit friends and relatives.
“Health care providers should talk to their patients, especially those who would travel to countries where malaria is endemic to visit friends and relatives, about upcoming travel plans and offer education and medicines to prevent malaria,” the authors wrote.
FROM MMWR
Survival in the first 3 years of ART continues to improve
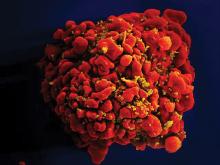
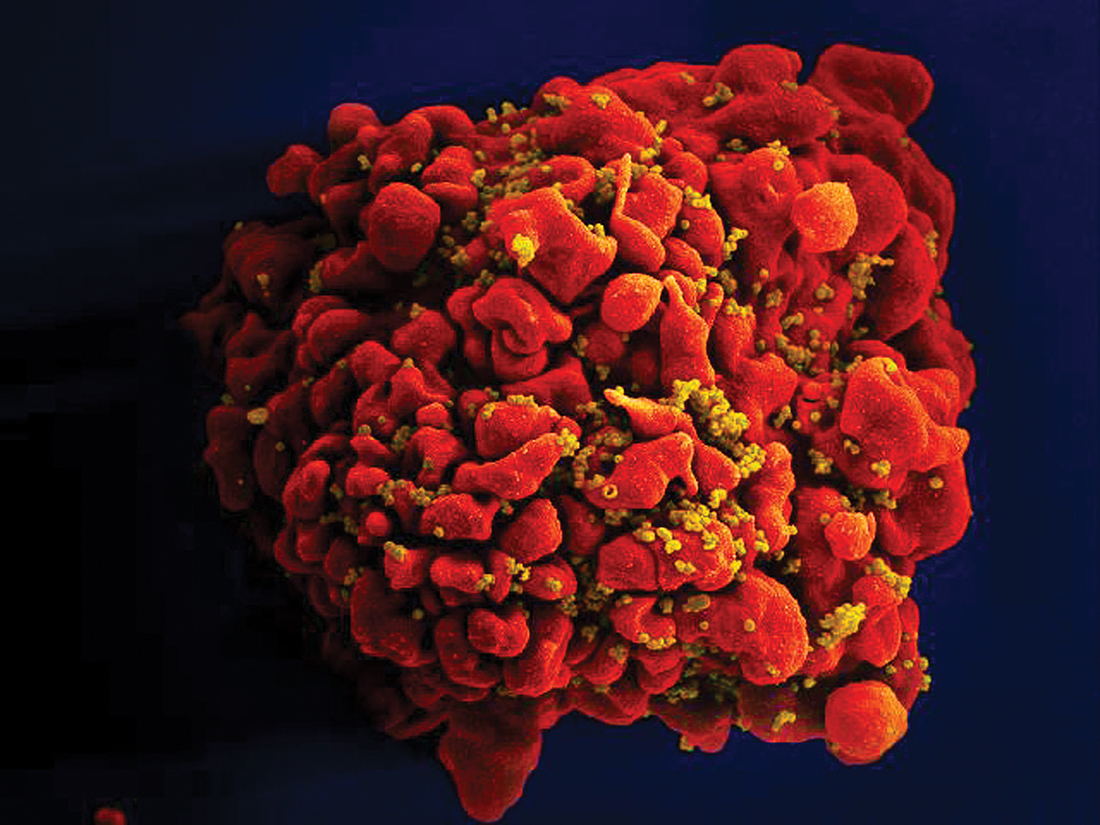
Mortality continues to decline for patients in the first 3 years of combination antiretroviral therapy (ART) for HIV-1 infection, according to an analysis of 18 different cohorts from 1996 to 2013.
The Antiretroviral Therapy Cohort Collaboration (ART-CC) combined data from participating cohorts from Europe and North America. Patients were at least 16 years of age, naive to ART, and starting treatment with three or more antiretroviral drugs between 1996 and 2010. Of 88,504 patients, 2% died in the first year of ART, and 3% died in the second or third year of ART.
Where the ART-CC previously reported that mortality within 1 year of starting ART had not improved from 1998 to 2003, the current analysis found lower mortality in the first year for patients starting ART in the years 2008 to 2010, compared with patients starting ART in the years 2000 to 2003 (hazard ratio, 0.71; 95% confidence interval, 0.61-0.83).
All-cause mortality also was decreased in the second and third years of ART for those respective calendar periods (HR, 0.57; 95% CI, 0.49-0.67).
“Patients who started ART during 2008-2010 whose CD4 counts exceeded 350 cells per microL 1 year after ART initiation have estimated life expectancy approaching that of the general population,” Dr. Trickey and his colleagues said.
The authors speculate that the improvements in mortality may result from better ART regimens and improved adherence. Declines in all-cause mortality may reflect better management of comorbidities.
Given the high effectiveness of ART today, for further improvement “lifestyle issues that affect adherence to ART and non-AIDS mortality, and diagnosis and treatment of comorbidities in people living with HIV will need to be addressed,” Dr. Trickey and his coauthors concluded.
The study received funding from the United Kingdom Medical Research Council, the United Kingdom Department for International Development, and the European Union European & Developing Countries Clinical Trials Partnership (EDCTP2) program. Dr. Trickey reported no conflicts of interest. Some members of the writing committee received fees from various drug companies for work unrelated to this study.
This article was updated on 5/18/17.
Mortality continues to decline for patients in the first 3 years of combination antiretroviral therapy (ART) for HIV-1 infection, according to an analysis of 18 different cohorts from 1996 to 2013.
The Antiretroviral Therapy Cohort Collaboration (ART-CC) combined data from participating cohorts from Europe and North America. Patients were at least 16 years of age, naive to ART, and starting treatment with three or more antiretroviral drugs between 1996 and 2010. Of 88,504 patients, 2% died in the first year of ART, and 3% died in the second or third year of ART.
Where the ART-CC previously reported that mortality within 1 year of starting ART had not improved from 1998 to 2003, the current analysis found lower mortality in the first year for patients starting ART in the years 2008 to 2010, compared with patients starting ART in the years 2000 to 2003 (hazard ratio, 0.71; 95% confidence interval, 0.61-0.83).
All-cause mortality also was decreased in the second and third years of ART for those respective calendar periods (HR, 0.57; 95% CI, 0.49-0.67).
“Patients who started ART during 2008-2010 whose CD4 counts exceeded 350 cells per microL 1 year after ART initiation have estimated life expectancy approaching that of the general population,” Dr. Trickey and his colleagues said.
The authors speculate that the improvements in mortality may result from better ART regimens and improved adherence. Declines in all-cause mortality may reflect better management of comorbidities.
Given the high effectiveness of ART today, for further improvement “lifestyle issues that affect adherence to ART and non-AIDS mortality, and diagnosis and treatment of comorbidities in people living with HIV will need to be addressed,” Dr. Trickey and his coauthors concluded.
The study received funding from the United Kingdom Medical Research Council, the United Kingdom Department for International Development, and the European Union European & Developing Countries Clinical Trials Partnership (EDCTP2) program. Dr. Trickey reported no conflicts of interest. Some members of the writing committee received fees from various drug companies for work unrelated to this study.
This article was updated on 5/18/17.
Mortality continues to decline for patients in the first 3 years of combination antiretroviral therapy (ART) for HIV-1 infection, according to an analysis of 18 different cohorts from 1996 to 2013.
The Antiretroviral Therapy Cohort Collaboration (ART-CC) combined data from participating cohorts from Europe and North America. Patients were at least 16 years of age, naive to ART, and starting treatment with three or more antiretroviral drugs between 1996 and 2010. Of 88,504 patients, 2% died in the first year of ART, and 3% died in the second or third year of ART.
Where the ART-CC previously reported that mortality within 1 year of starting ART had not improved from 1998 to 2003, the current analysis found lower mortality in the first year for patients starting ART in the years 2008 to 2010, compared with patients starting ART in the years 2000 to 2003 (hazard ratio, 0.71; 95% confidence interval, 0.61-0.83).
All-cause mortality also was decreased in the second and third years of ART for those respective calendar periods (HR, 0.57; 95% CI, 0.49-0.67).
“Patients who started ART during 2008-2010 whose CD4 counts exceeded 350 cells per microL 1 year after ART initiation have estimated life expectancy approaching that of the general population,” Dr. Trickey and his colleagues said.
The authors speculate that the improvements in mortality may result from better ART regimens and improved adherence. Declines in all-cause mortality may reflect better management of comorbidities.
Given the high effectiveness of ART today, for further improvement “lifestyle issues that affect adherence to ART and non-AIDS mortality, and diagnosis and treatment of comorbidities in people living with HIV will need to be addressed,” Dr. Trickey and his coauthors concluded.
The study received funding from the United Kingdom Medical Research Council, the United Kingdom Department for International Development, and the European Union European & Developing Countries Clinical Trials Partnership (EDCTP2) program. Dr. Trickey reported no conflicts of interest. Some members of the writing committee received fees from various drug companies for work unrelated to this study.
This article was updated on 5/18/17.
FROM THE LANCET HIV
Key clinical point: Mortality continues to decline for patients in the first 3 years of taking ART for HIV-1 infection.
Major finding: The current analysis found lower mortality in the first year for patients starting ART in the years 2008 to 2010, compared with patients starting ART in the years 2000 to 2003 (HR, 0.71; 95% CI, 0.61-0.83).
Data source: An analysis of 18 different cohorts in Europe and North America from 1996 to 2013.
Disclosures: The study received funding from the United Kingdom Medical Research Council, the United Kingdom Department for International Development, and the European Union European & Developing Countries Clinical Trials Partnership (EDCTP2) program. Some members of the writing committee received fees from various drug companies for work unrelated to this study.