User login
Risk factors outweigh benefits of opioids for chronic noncancer pain
The benefits of prescribing opioids to patients with some chronic noncancer pain conditions such as headache, fibromyalgia, and chronic low back pain are offset by the severity of the risks inherent to taking those drugs, according to new position paper published by the American Academy of Neurology.
Opioids such as morphine, codeine, oxycodone, methadone, fentanyl, and hydrocodone have become commonly associated with a high risk of addiction, overdosing, and sometimes death. These are key reasons why new protocols are urgently needed to help curb the growing problem, said Dr. Gary M. Franklin, a neurologist and research professor in the department of environmental and occupational health sciences at the University of Washington, Seattle.
“The language in these [opioid] laws implying no ceiling on dose, or placing no limits on dispensing controlled substances from prescriber offices, should be revisited in the context of the benefits, morbidity, and mortality,” Dr. Franklin wrote (Neurology 2014;83:1277-84).
Since the late 1990s, when policy changes allowed for more liberal long-term use, there have been more than 100,000 deaths related to prescription opioids. At Washington State Hospital alone, hospitalizations due to opioid overdoses skyrocketed between 1995 and 2008, growing from well under 100 per year to over 400.
Studies also indicate that about half of all patients who take opioids for 3 months to treat chronic pain continue to use the drugs as much as 5 years later. In fact, within the age group of 35-54 years, opioid-related mortality has exceeded deaths caused by both motor vehicle accidents and firearms since the late 1990s.
In an interview, Dr. Franklin advised physicians to be very careful about using opioid therapy as a first-line treatment for mild to moderate pain conditions. If it is used at all, it should be for only a few days. For patients who are already on high doses of opioids, Dr. Franklin recommended that physicians consult guidelines on tapering and help patients find a therapy without the risks of chronic opioid treatment.
“You should not abandon your patients,” he said. “You might decide not to keep using opioids, but don’t abandon the patient. Offer them some other things that might help them.”
The overprescribing of opioids has been slow to turn around, Dr. Franklin said, because physicians lack alternatives and in many cases it is easier to simply write a prescription. Potentially helpful alternative treatments such as cognitive behavior therapy or multidisciplinary pain care are not always covered by insurers, he said.
“I feel like there has been a tipping point, but that still doesn’t mean that it’s going to reverse soon,” he added. “There’s still going to be a lot of lives lost.”
In the position statement, Dr. Franklin proposed a regimen for doctors that could help limit the amount of opioids prescribed, the length of such treatments, and their misuse. This would include a patient-doctor opioid treatment agreement, prescreening for past drug abuse and depression, random urine testing, abiding by state Prescription Drug Monitoring Programs, and strict avoidance of sedative-hypnotics and benzodiazepines. The American Academy of Neurology recommends that all doctors consult with a pain management specialist before prescribing morphine-equivalent dosages of 80-120 mg/day.
Although measures have been taken by U.S. government agencies to crack down on long-term opioid prescriptions – such as the 2007 Risk Evaluation and Mitigation Strategies implemented by the Food and Drug Administration and the Drug Enforcement Agency’s 2010 decision to restrict e-prescribing of opioids – Dr. Franklin said that there is still much to be done.
“Ongoing research and data collection regarding opioid efficacy and management are needed, as well as revision in state and federal laws and policy” to ensure patient safety, Dr. Franklin wrote.
He reported no relevant financial disclosures.
The benefits of prescribing opioids to patients with some chronic noncancer pain conditions such as headache, fibromyalgia, and chronic low back pain are offset by the severity of the risks inherent to taking those drugs, according to new position paper published by the American Academy of Neurology.
Opioids such as morphine, codeine, oxycodone, methadone, fentanyl, and hydrocodone have become commonly associated with a high risk of addiction, overdosing, and sometimes death. These are key reasons why new protocols are urgently needed to help curb the growing problem, said Dr. Gary M. Franklin, a neurologist and research professor in the department of environmental and occupational health sciences at the University of Washington, Seattle.
“The language in these [opioid] laws implying no ceiling on dose, or placing no limits on dispensing controlled substances from prescriber offices, should be revisited in the context of the benefits, morbidity, and mortality,” Dr. Franklin wrote (Neurology 2014;83:1277-84).
Since the late 1990s, when policy changes allowed for more liberal long-term use, there have been more than 100,000 deaths related to prescription opioids. At Washington State Hospital alone, hospitalizations due to opioid overdoses skyrocketed between 1995 and 2008, growing from well under 100 per year to over 400.
Studies also indicate that about half of all patients who take opioids for 3 months to treat chronic pain continue to use the drugs as much as 5 years later. In fact, within the age group of 35-54 years, opioid-related mortality has exceeded deaths caused by both motor vehicle accidents and firearms since the late 1990s.
In an interview, Dr. Franklin advised physicians to be very careful about using opioid therapy as a first-line treatment for mild to moderate pain conditions. If it is used at all, it should be for only a few days. For patients who are already on high doses of opioids, Dr. Franklin recommended that physicians consult guidelines on tapering and help patients find a therapy without the risks of chronic opioid treatment.
“You should not abandon your patients,” he said. “You might decide not to keep using opioids, but don’t abandon the patient. Offer them some other things that might help them.”
The overprescribing of opioids has been slow to turn around, Dr. Franklin said, because physicians lack alternatives and in many cases it is easier to simply write a prescription. Potentially helpful alternative treatments such as cognitive behavior therapy or multidisciplinary pain care are not always covered by insurers, he said.
“I feel like there has been a tipping point, but that still doesn’t mean that it’s going to reverse soon,” he added. “There’s still going to be a lot of lives lost.”
In the position statement, Dr. Franklin proposed a regimen for doctors that could help limit the amount of opioids prescribed, the length of such treatments, and their misuse. This would include a patient-doctor opioid treatment agreement, prescreening for past drug abuse and depression, random urine testing, abiding by state Prescription Drug Monitoring Programs, and strict avoidance of sedative-hypnotics and benzodiazepines. The American Academy of Neurology recommends that all doctors consult with a pain management specialist before prescribing morphine-equivalent dosages of 80-120 mg/day.
Although measures have been taken by U.S. government agencies to crack down on long-term opioid prescriptions – such as the 2007 Risk Evaluation and Mitigation Strategies implemented by the Food and Drug Administration and the Drug Enforcement Agency’s 2010 decision to restrict e-prescribing of opioids – Dr. Franklin said that there is still much to be done.
“Ongoing research and data collection regarding opioid efficacy and management are needed, as well as revision in state and federal laws and policy” to ensure patient safety, Dr. Franklin wrote.
He reported no relevant financial disclosures.
The benefits of prescribing opioids to patients with some chronic noncancer pain conditions such as headache, fibromyalgia, and chronic low back pain are offset by the severity of the risks inherent to taking those drugs, according to new position paper published by the American Academy of Neurology.
Opioids such as morphine, codeine, oxycodone, methadone, fentanyl, and hydrocodone have become commonly associated with a high risk of addiction, overdosing, and sometimes death. These are key reasons why new protocols are urgently needed to help curb the growing problem, said Dr. Gary M. Franklin, a neurologist and research professor in the department of environmental and occupational health sciences at the University of Washington, Seattle.
“The language in these [opioid] laws implying no ceiling on dose, or placing no limits on dispensing controlled substances from prescriber offices, should be revisited in the context of the benefits, morbidity, and mortality,” Dr. Franklin wrote (Neurology 2014;83:1277-84).
Since the late 1990s, when policy changes allowed for more liberal long-term use, there have been more than 100,000 deaths related to prescription opioids. At Washington State Hospital alone, hospitalizations due to opioid overdoses skyrocketed between 1995 and 2008, growing from well under 100 per year to over 400.
Studies also indicate that about half of all patients who take opioids for 3 months to treat chronic pain continue to use the drugs as much as 5 years later. In fact, within the age group of 35-54 years, opioid-related mortality has exceeded deaths caused by both motor vehicle accidents and firearms since the late 1990s.
In an interview, Dr. Franklin advised physicians to be very careful about using opioid therapy as a first-line treatment for mild to moderate pain conditions. If it is used at all, it should be for only a few days. For patients who are already on high doses of opioids, Dr. Franklin recommended that physicians consult guidelines on tapering and help patients find a therapy without the risks of chronic opioid treatment.
“You should not abandon your patients,” he said. “You might decide not to keep using opioids, but don’t abandon the patient. Offer them some other things that might help them.”
The overprescribing of opioids has been slow to turn around, Dr. Franklin said, because physicians lack alternatives and in many cases it is easier to simply write a prescription. Potentially helpful alternative treatments such as cognitive behavior therapy or multidisciplinary pain care are not always covered by insurers, he said.
“I feel like there has been a tipping point, but that still doesn’t mean that it’s going to reverse soon,” he added. “There’s still going to be a lot of lives lost.”
In the position statement, Dr. Franklin proposed a regimen for doctors that could help limit the amount of opioids prescribed, the length of such treatments, and their misuse. This would include a patient-doctor opioid treatment agreement, prescreening for past drug abuse and depression, random urine testing, abiding by state Prescription Drug Monitoring Programs, and strict avoidance of sedative-hypnotics and benzodiazepines. The American Academy of Neurology recommends that all doctors consult with a pain management specialist before prescribing morphine-equivalent dosages of 80-120 mg/day.
Although measures have been taken by U.S. government agencies to crack down on long-term opioid prescriptions – such as the 2007 Risk Evaluation and Mitigation Strategies implemented by the Food and Drug Administration and the Drug Enforcement Agency’s 2010 decision to restrict e-prescribing of opioids – Dr. Franklin said that there is still much to be done.
“Ongoing research and data collection regarding opioid efficacy and management are needed, as well as revision in state and federal laws and policy” to ensure patient safety, Dr. Franklin wrote.
He reported no relevant financial disclosures.
FROM NEUROLOGY
VIDEO: Single-dose peramivir may simplify flu treatment
WASHINGTON – Peramivir, an investigational single-dose antiviral drug to treat influenza, could deliver multiple benefits for physicians and patients alike, Dr. Richard J. Whitley predicted.
At the 2014 Interscience Conference on Antimicrobial Agents and Chemotherapy meeting in Washington, Dr. Whitley co-presented an analysis of phase II and phase III clinical trials that show the safety and efficacy of peramivir, which is currently under review by the U.S. Food and Drug Administration. Dr. Whitley is distinguished professor of pediatrics and microbiology at the University of Alabama at Birmingham.
In a video interview, Dr. Whitley discusses what this new flu drug could mean for physicians and patients, when the drug might be approved by the FDA, and why a new flu pandemic could be coming sooner rather than later.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Peramivir, an investigational single-dose antiviral drug to treat influenza, could deliver multiple benefits for physicians and patients alike, Dr. Richard J. Whitley predicted.
At the 2014 Interscience Conference on Antimicrobial Agents and Chemotherapy meeting in Washington, Dr. Whitley co-presented an analysis of phase II and phase III clinical trials that show the safety and efficacy of peramivir, which is currently under review by the U.S. Food and Drug Administration. Dr. Whitley is distinguished professor of pediatrics and microbiology at the University of Alabama at Birmingham.
In a video interview, Dr. Whitley discusses what this new flu drug could mean for physicians and patients, when the drug might be approved by the FDA, and why a new flu pandemic could be coming sooner rather than later.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Peramivir, an investigational single-dose antiviral drug to treat influenza, could deliver multiple benefits for physicians and patients alike, Dr. Richard J. Whitley predicted.
At the 2014 Interscience Conference on Antimicrobial Agents and Chemotherapy meeting in Washington, Dr. Whitley co-presented an analysis of phase II and phase III clinical trials that show the safety and efficacy of peramivir, which is currently under review by the U.S. Food and Drug Administration. Dr. Whitley is distinguished professor of pediatrics and microbiology at the University of Alabama at Birmingham.
In a video interview, Dr. Whitley discusses what this new flu drug could mean for physicians and patients, when the drug might be approved by the FDA, and why a new flu pandemic could be coming sooner rather than later.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ICAAC 2014
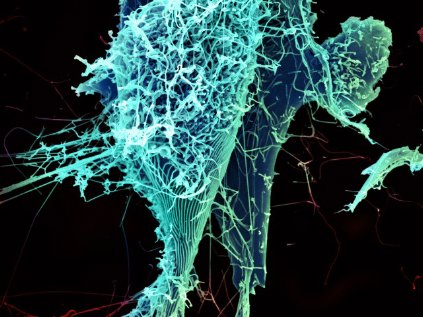
NIH set to begin human testing on experimental Ebola vaccine
The National Institute of Allergy and Infectious Diseases will begin human testing of a new vaccine developed to prevent contracting the deadly Ebola virus.
The vaccine is the first of several phase I treatments to go into clinical trials on humans. The hope is that the vaccine ultimately will be used to stem the tide of Ebola infections in western Africa, where the virus already has claimed more than 1,400 lives since the outbreak began in March.
"There is an urgent need for a protective Ebola vaccine, and it is important to establish that a vaccine is safe and spurs the immune system to react in a way necessary to protect against infection," Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, said in a statement. "The [National Institutes of Health] is playing a key role in accelerating the development and testing of investigational Ebola vaccines."
The testing will take place at the National Institutes of Health Clinical Center in Maryland, where the vaccine – developed jointly by the NIAID and GlaxoSmithKline – will be administered to 20 healthy adults who have not contracted the Ebola virus. Ten adults will receive an intramuscular injection, while the other ten will receive the same injection in a higher dosage. All participants in the trial, which has been dubbed VRC 207, are between the ages of 18 and 50.
Once phase I trials are complete, the next step will be to test the vaccine on a larger number of people in phase II studies. Phase III trials would determine whether the vaccine is effective. The VRC 207 trial is expected to begin in October.
"Today we know the best way to prevent the spread of Ebola infection is through public health measures, including good infection control practices, isolation, contact tracing, quarantine, and provision of personal protective equipment," Dr. Fauci said in the statement. "However, a vaccine will ultimately be an important tool in the prevention effort. The launch of phase I Ebola vaccine studies is the first step in a long process."
Additionally, the NIH has partnered with a British consortium to test the NIAID/GSK vaccine on healthy adults in the United Kingdom. Permission to test the vaccine in the western African nations of Gambia and Mali is still pending approval from authorities in those countries. The U.K. trial is scheduled to begin in September.
The NIAID anticipates that initial safety and immunogenicity data from the phase I trials should be available by late 2014.
The National Institute of Allergy and Infectious Diseases will begin human testing of a new vaccine developed to prevent contracting the deadly Ebola virus.
The vaccine is the first of several phase I treatments to go into clinical trials on humans. The hope is that the vaccine ultimately will be used to stem the tide of Ebola infections in western Africa, where the virus already has claimed more than 1,400 lives since the outbreak began in March.
"There is an urgent need for a protective Ebola vaccine, and it is important to establish that a vaccine is safe and spurs the immune system to react in a way necessary to protect against infection," Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, said in a statement. "The [National Institutes of Health] is playing a key role in accelerating the development and testing of investigational Ebola vaccines."
The testing will take place at the National Institutes of Health Clinical Center in Maryland, where the vaccine – developed jointly by the NIAID and GlaxoSmithKline – will be administered to 20 healthy adults who have not contracted the Ebola virus. Ten adults will receive an intramuscular injection, while the other ten will receive the same injection in a higher dosage. All participants in the trial, which has been dubbed VRC 207, are between the ages of 18 and 50.
Once phase I trials are complete, the next step will be to test the vaccine on a larger number of people in phase II studies. Phase III trials would determine whether the vaccine is effective. The VRC 207 trial is expected to begin in October.
"Today we know the best way to prevent the spread of Ebola infection is through public health measures, including good infection control practices, isolation, contact tracing, quarantine, and provision of personal protective equipment," Dr. Fauci said in the statement. "However, a vaccine will ultimately be an important tool in the prevention effort. The launch of phase I Ebola vaccine studies is the first step in a long process."
Additionally, the NIH has partnered with a British consortium to test the NIAID/GSK vaccine on healthy adults in the United Kingdom. Permission to test the vaccine in the western African nations of Gambia and Mali is still pending approval from authorities in those countries. The U.K. trial is scheduled to begin in September.
The NIAID anticipates that initial safety and immunogenicity data from the phase I trials should be available by late 2014.
The National Institute of Allergy and Infectious Diseases will begin human testing of a new vaccine developed to prevent contracting the deadly Ebola virus.
The vaccine is the first of several phase I treatments to go into clinical trials on humans. The hope is that the vaccine ultimately will be used to stem the tide of Ebola infections in western Africa, where the virus already has claimed more than 1,400 lives since the outbreak began in March.
"There is an urgent need for a protective Ebola vaccine, and it is important to establish that a vaccine is safe and spurs the immune system to react in a way necessary to protect against infection," Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, said in a statement. "The [National Institutes of Health] is playing a key role in accelerating the development and testing of investigational Ebola vaccines."
The testing will take place at the National Institutes of Health Clinical Center in Maryland, where the vaccine – developed jointly by the NIAID and GlaxoSmithKline – will be administered to 20 healthy adults who have not contracted the Ebola virus. Ten adults will receive an intramuscular injection, while the other ten will receive the same injection in a higher dosage. All participants in the trial, which has been dubbed VRC 207, are between the ages of 18 and 50.
Once phase I trials are complete, the next step will be to test the vaccine on a larger number of people in phase II studies. Phase III trials would determine whether the vaccine is effective. The VRC 207 trial is expected to begin in October.
"Today we know the best way to prevent the spread of Ebola infection is through public health measures, including good infection control practices, isolation, contact tracing, quarantine, and provision of personal protective equipment," Dr. Fauci said in the statement. "However, a vaccine will ultimately be an important tool in the prevention effort. The launch of phase I Ebola vaccine studies is the first step in a long process."
Additionally, the NIH has partnered with a British consortium to test the NIAID/GSK vaccine on healthy adults in the United Kingdom. Permission to test the vaccine in the western African nations of Gambia and Mali is still pending approval from authorities in those countries. The U.K. trial is scheduled to begin in September.
The NIAID anticipates that initial safety and immunogenicity data from the phase I trials should be available by late 2014.
AHA wants e-cigarettes regulated but notes they help some smokers quit
The American Heart Association has released its recommendations regarding the sale and usage of e-cigarettes, cautioning that the devices should be regulated to avoid enticing children to smoke while also saying that e-cigarettes could be used as a way to help some current smokers quit.
The guidelines, published online Aug. 24 in Circulation, state that clinicians "should not discourage" their patients from resorting to e-cigarettes if other approved forms of smoking cessation, such as the nicotine patch, have been exhausted. The AHA warned, however, that further studies are needed to fully understand the effects of e-cigarette usage, stressing that e-cigarettes have not been approved by the Food and Drug Administration as an acceptable smoking cessation device and could contain low amounts of toxic chemicals that would prove more harmful than helpful to patients in the long run.
"E-cigarettes have caused a major shift in the tobacco-control landscape," Aruni Bhatnagar, Ph.D., lead author of the guidelines and chair of cardiovascular medicine at the University of Louisville, Ky., said in a statement. "It’s critical that we rigorously examine the long-term impact of this new technology on public health, cardiovascular disease, and stroke, and pay careful attention to the effect of e-cigarettes on adolescents."
For now, the AHA says that clinicians should tell their patients who use e-cigarettes to set a firm quit date, warning that any device that delivers nicotine into the body is harmful and likely lethal.
"Nicotine is a dangerous and highly addictive chemical no matter what form it takes – conventional cigarettes or some other tobacco product," Dr. Elliott Antman, AHA president, said in the statement. "Every life that has been lost to tobacco addiction" could have been saved, he noted.
To that end, the AHA also called for strong regulations regarding the potential marketability of e-cigarettes to youngsters. The group recommended a federal ban on the sale of e-cigarettes to minors, warning that the devices could become a gateway to actual cigarettes for young people who see e-cigarettes as "high-tech, accessible, and convenient," according to a JAMA Pediatrics study of 40,000 middle and high school students. The AHA also recommended that all existing rules and regulations in place for tobacco-related products should apply to e-cigarettes.
"We must protect future generations from any potential smokescreens in the tobacco product landscape that will cause us to lose precious ground in the fight to make our nation 100% tobacco-free," Dr. Antman said.
According to the AHA, 20 million Americans have lost their lives to tobacco over the last 50 years.
The American Heart Association has released its recommendations regarding the sale and usage of e-cigarettes, cautioning that the devices should be regulated to avoid enticing children to smoke while also saying that e-cigarettes could be used as a way to help some current smokers quit.
The guidelines, published online Aug. 24 in Circulation, state that clinicians "should not discourage" their patients from resorting to e-cigarettes if other approved forms of smoking cessation, such as the nicotine patch, have been exhausted. The AHA warned, however, that further studies are needed to fully understand the effects of e-cigarette usage, stressing that e-cigarettes have not been approved by the Food and Drug Administration as an acceptable smoking cessation device and could contain low amounts of toxic chemicals that would prove more harmful than helpful to patients in the long run.
"E-cigarettes have caused a major shift in the tobacco-control landscape," Aruni Bhatnagar, Ph.D., lead author of the guidelines and chair of cardiovascular medicine at the University of Louisville, Ky., said in a statement. "It’s critical that we rigorously examine the long-term impact of this new technology on public health, cardiovascular disease, and stroke, and pay careful attention to the effect of e-cigarettes on adolescents."
For now, the AHA says that clinicians should tell their patients who use e-cigarettes to set a firm quit date, warning that any device that delivers nicotine into the body is harmful and likely lethal.
"Nicotine is a dangerous and highly addictive chemical no matter what form it takes – conventional cigarettes or some other tobacco product," Dr. Elliott Antman, AHA president, said in the statement. "Every life that has been lost to tobacco addiction" could have been saved, he noted.
To that end, the AHA also called for strong regulations regarding the potential marketability of e-cigarettes to youngsters. The group recommended a federal ban on the sale of e-cigarettes to minors, warning that the devices could become a gateway to actual cigarettes for young people who see e-cigarettes as "high-tech, accessible, and convenient," according to a JAMA Pediatrics study of 40,000 middle and high school students. The AHA also recommended that all existing rules and regulations in place for tobacco-related products should apply to e-cigarettes.
"We must protect future generations from any potential smokescreens in the tobacco product landscape that will cause us to lose precious ground in the fight to make our nation 100% tobacco-free," Dr. Antman said.
According to the AHA, 20 million Americans have lost their lives to tobacco over the last 50 years.
The American Heart Association has released its recommendations regarding the sale and usage of e-cigarettes, cautioning that the devices should be regulated to avoid enticing children to smoke while also saying that e-cigarettes could be used as a way to help some current smokers quit.
The guidelines, published online Aug. 24 in Circulation, state that clinicians "should not discourage" their patients from resorting to e-cigarettes if other approved forms of smoking cessation, such as the nicotine patch, have been exhausted. The AHA warned, however, that further studies are needed to fully understand the effects of e-cigarette usage, stressing that e-cigarettes have not been approved by the Food and Drug Administration as an acceptable smoking cessation device and could contain low amounts of toxic chemicals that would prove more harmful than helpful to patients in the long run.
"E-cigarettes have caused a major shift in the tobacco-control landscape," Aruni Bhatnagar, Ph.D., lead author of the guidelines and chair of cardiovascular medicine at the University of Louisville, Ky., said in a statement. "It’s critical that we rigorously examine the long-term impact of this new technology on public health, cardiovascular disease, and stroke, and pay careful attention to the effect of e-cigarettes on adolescents."
For now, the AHA says that clinicians should tell their patients who use e-cigarettes to set a firm quit date, warning that any device that delivers nicotine into the body is harmful and likely lethal.
"Nicotine is a dangerous and highly addictive chemical no matter what form it takes – conventional cigarettes or some other tobacco product," Dr. Elliott Antman, AHA president, said in the statement. "Every life that has been lost to tobacco addiction" could have been saved, he noted.
To that end, the AHA also called for strong regulations regarding the potential marketability of e-cigarettes to youngsters. The group recommended a federal ban on the sale of e-cigarettes to minors, warning that the devices could become a gateway to actual cigarettes for young people who see e-cigarettes as "high-tech, accessible, and convenient," according to a JAMA Pediatrics study of 40,000 middle and high school students. The AHA also recommended that all existing rules and regulations in place for tobacco-related products should apply to e-cigarettes.
"We must protect future generations from any potential smokescreens in the tobacco product landscape that will cause us to lose precious ground in the fight to make our nation 100% tobacco-free," Dr. Antman said.
According to the AHA, 20 million Americans have lost their lives to tobacco over the last 50 years.
FROM CIRCULATION