User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Abnormal Placenta Linked to Increased Postcesarean Hemorrhage Risk
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: A hemoglobin decrease of at least 30% from the preoperative value was significantly associated with abnormal placenta (OR, 5.38), incision extension or uterine rupture (OR, 2.81), and labor (OR, 2.78).
Data Source: This review involved 3,677 cesarean deliveries performed at a large hospital between Jan. 1, 2009 and Oct. 31, 2010.
Disclosures: Dr. Thompson said that he had no relevant financial conflicts to disclose.
Surgeons See Merit In Social Media
SAN DIEGO -- Facebook, Twitter, and other social media have their rightful place in surgeons' busy schedules, according to several surgeons who participated in a social media symposium at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
In fact, these media just might help you land your dream job, raise money, screen applicants to your fellowship program, enhance communication with your peers, or strengthen relationships with your patients.
Dr. Gretchen Purcell Jackson noted that 61% of adults in the United States look online for health information. In addition, 41% of patients have read a commentary or shared experiences about health or medical issues in an online news group, website, or blog; 24% of online patients have consulted rankings or reviews of physicians, providers, and hospitals; 60% of active online patients report that using the Web affected a medical decision; and more than 700 hospitals currently use social networking tools.
"People seek and give advice about their health care concerns, they seek and share information about medical problems, and they share stories about their health care experiences. Some people use social media to raise money for health-related causes. Patients are using social media in a wide variety of ways, and they might be talking about you," said Dr. Jackson, an ACS Fellow and assistant professor of surgery and biomedical informatics at Vanderbilt University, Nashville, Tenn.
Facebook has 845 million active users making more than 1 billion posts per day, while Twitter has more than 465 million accounts and grows by 11 accounts per second.
Facebook is used by 64% of surgeons, compared with 42% of the general population in the United States, according to Dr. Kiran K. Turaga. "As usual, we surgeons are ahead of the curve, but Facebook has unique characteristics that can affect every single aspect of our lives," said Dr. Turaga, assistant professor of surgery at the Medical College of Wisconsin, Milwaukee. "In terms of trainees, it can affect medical student and resident education, and it can affect recruitment. For patients, you can use this for fund-raising, marketing, forming support groups, increasing awareness [about an aspect of health], recruiting for clinical trials, and monitoring for diseases."
More than 95% of U.S. medical schools have a Facebook presence, Dr. Turaga said, and 71% of these have active student group accounts. In addition, 70% of medical students have active individual Facebook accounts. However, 60% of medical schools have reported incidents of students posting unprofessional content, including profanity (in 52% of cases), breach of patient confidentiality (in 13% of cases), or photos of themselves in a state of intoxication (in 39% of cases) (JAMA 2009;302:1309-15).
Through a sister organization known as Causes (www.causes.com), Facebook has 170 million users who have generated $40 million for 27,000 not-for-profit groups, including hospitals. This makes Facebook "a remarkable tool for fund-raising," Dr. Turaga said. "This could be as simple as raising $1,000 for a new east wing in your hospital."
Furthermore, he said, creating an ad on Facebook allows you to reach 19 million people with an interest in cancer, 600,000 people with an interest in surgery, and 5,000 people with an interest in laparoscopy. Facebook also offers physicians unique opportunities for peer-to-peer interaction by providing a platform for online consultations, virtual tumor boards, journals and summaries of medical news and blogs, and discussions of health care reform and other topics of interest. There are currently 757 Facebook health groups with 300,000 members, he said.
Dr. Turaga warned that posting recognizable patient information on Facebook or other social media channels can violate the Health Insurance Portability and Accountability Act, state criminal laws regarding patient health information, state licensure laws, state professional misconduct laws, and standards set by the Joint Commission.
"If you are considering posting any information that is patient specific, make sure you have exclusive consent of the patient," he said. "The other thing to consider is unnecessary patient-provider interaction, which would mean that you start engaging in a relationship with a patient in which you start giving advice. Then you become liable for that advice, so there can be medical-legal consequences."
Before you start using Facebook or another type of social media, Dr. Turaga recommends considering the acronym POST, which stands for people (whom do you want to target with your social media?), objectives (why do you want to target them?), strategy (how are you going to target them?), and technology (which social media will you use to do so?).
Twitter, a microblogging site that allows communication by posts of no more than 140 characters in length, is an open platform of communication rather than a closed platform, explained Dr. Niraj J. Gusani. "This adds a level of complexity – and possibly risk – that may make this medium less ideal for health care professional use. Anything that you post can be seen by anyone in the world at any time. There’s no filter. On the other hand, Twitter has a wide reach, and it’s easy for people to find you," said Dr. Gusani, an ACS Fellow and assistant professor of surgery, medicine, and public health sciences at Pennsylvania State University, Hershey.
A recent survey of 315 members of the American College of Surgeons found that 79% never use Twitter, while 6% use it daily and 3% use it weekly (Bull. Am. Coll. Surg. 2011;96:46-8). In Dr. Gusani’s opinion, surgeons can use Twitter to update the public about the latest news, events, and research highlights; respond to other tweets related to their field, area of research, or organization; participate in tweet chats or Q&A sessions; and tweet highlights from professional events and meetings.
While some clinicians use Twitter for patient contact and marketing, Dr. Gusani cautioned that it’s important to be wary of violating patient confidentiality. A review of 260 physician Twitter accounts revealed that 144 of 5,156 tweets (3%) were categorized as unprofessional (JAMA 2011;305:566-8). Of these, 38 (0.7%) represented potential patient privacy violations and 33 (0.6%) contained profanity.
Dr. Gusani said that he uses Twitter to "push information, studies, and observations related mainly to oncology and surgical oncology patient education. I post perspectives about medical news and occasional retweets." Twitter-based resources and chats that are recommended by Dr. Gusani include #twitJP, a journal club; #hcsm, a global health care chat that takes place at 9 p.m. ET every Sunday; #CMEchat, which takes place every Wednesday at 11 a.m. ET; and #Meded chat, which takes place every Thursday at 4 p.m. and 9 p.m. ET.
Dr. Seung S. Gwon spoke about the potential benefits of LinkedIn, a professional networking site that allows users to strengthen and expand their network of contacts. It currently has more than 15 million members in more than 200 countries and territories, including 44 million-plus members in the U. S. alone.
"The best part about LinkedIn is that it only takes a few minutes to set up your online profile, where you might list your experience, education, and accomplishments," said Dr. Gwon, an ACS Fellow with El Centro (Calif.) Regional Medical Center. The overall purpose is to connect to other users and build a network of trusted contacts, including personal e-mail contacts, professional colleagues, coworkers, and former classmates.
Dr. Gwon said that physicians have been slow to join LinkedIn because it doesn’t allow them to directly connect with their patients. "However, it does provide you with a digital footprint, so if patients want to look, they can," she said. "Also, a lot of people feel there is no value to networking if they’re already employed. If you like your job and you like where you are, there’s no reason to set up a big profile, primarily because most physicians work in a narrowly defined geography and we don’t really see the need to sell ourselves. We rely on word-of-mouth, the reputations that we create in our communities, [and] physicians who refer patients to us."
Even so, she advises physicians to consider joining LinkedIn because it improves Google search rankings, and it is a cost-effective and efficient means to share information and maintain professional relationships.
No speaker had relevant conflicts.
SAN DIEGO -- Facebook, Twitter, and other social media have their rightful place in surgeons' busy schedules, according to several surgeons who participated in a social media symposium at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
In fact, these media just might help you land your dream job, raise money, screen applicants to your fellowship program, enhance communication with your peers, or strengthen relationships with your patients.
Dr. Gretchen Purcell Jackson noted that 61% of adults in the United States look online for health information. In addition, 41% of patients have read a commentary or shared experiences about health or medical issues in an online news group, website, or blog; 24% of online patients have consulted rankings or reviews of physicians, providers, and hospitals; 60% of active online patients report that using the Web affected a medical decision; and more than 700 hospitals currently use social networking tools.
"People seek and give advice about their health care concerns, they seek and share information about medical problems, and they share stories about their health care experiences. Some people use social media to raise money for health-related causes. Patients are using social media in a wide variety of ways, and they might be talking about you," said Dr. Jackson, an ACS Fellow and assistant professor of surgery and biomedical informatics at Vanderbilt University, Nashville, Tenn.
Facebook has 845 million active users making more than 1 billion posts per day, while Twitter has more than 465 million accounts and grows by 11 accounts per second.
Facebook is used by 64% of surgeons, compared with 42% of the general population in the United States, according to Dr. Kiran K. Turaga. "As usual, we surgeons are ahead of the curve, but Facebook has unique characteristics that can affect every single aspect of our lives," said Dr. Turaga, assistant professor of surgery at the Medical College of Wisconsin, Milwaukee. "In terms of trainees, it can affect medical student and resident education, and it can affect recruitment. For patients, you can use this for fund-raising, marketing, forming support groups, increasing awareness [about an aspect of health], recruiting for clinical trials, and monitoring for diseases."
More than 95% of U.S. medical schools have a Facebook presence, Dr. Turaga said, and 71% of these have active student group accounts. In addition, 70% of medical students have active individual Facebook accounts. However, 60% of medical schools have reported incidents of students posting unprofessional content, including profanity (in 52% of cases), breach of patient confidentiality (in 13% of cases), or photos of themselves in a state of intoxication (in 39% of cases) (JAMA 2009;302:1309-15).
Through a sister organization known as Causes (www.causes.com), Facebook has 170 million users who have generated $40 million for 27,000 not-for-profit groups, including hospitals. This makes Facebook "a remarkable tool for fund-raising," Dr. Turaga said. "This could be as simple as raising $1,000 for a new east wing in your hospital."
Furthermore, he said, creating an ad on Facebook allows you to reach 19 million people with an interest in cancer, 600,000 people with an interest in surgery, and 5,000 people with an interest in laparoscopy. Facebook also offers physicians unique opportunities for peer-to-peer interaction by providing a platform for online consultations, virtual tumor boards, journals and summaries of medical news and blogs, and discussions of health care reform and other topics of interest. There are currently 757 Facebook health groups with 300,000 members, he said.
Dr. Turaga warned that posting recognizable patient information on Facebook or other social media channels can violate the Health Insurance Portability and Accountability Act, state criminal laws regarding patient health information, state licensure laws, state professional misconduct laws, and standards set by the Joint Commission.
"If you are considering posting any information that is patient specific, make sure you have exclusive consent of the patient," he said. "The other thing to consider is unnecessary patient-provider interaction, which would mean that you start engaging in a relationship with a patient in which you start giving advice. Then you become liable for that advice, so there can be medical-legal consequences."
Before you start using Facebook or another type of social media, Dr. Turaga recommends considering the acronym POST, which stands for people (whom do you want to target with your social media?), objectives (why do you want to target them?), strategy (how are you going to target them?), and technology (which social media will you use to do so?).
Twitter, a microblogging site that allows communication by posts of no more than 140 characters in length, is an open platform of communication rather than a closed platform, explained Dr. Niraj J. Gusani. "This adds a level of complexity – and possibly risk – that may make this medium less ideal for health care professional use. Anything that you post can be seen by anyone in the world at any time. There’s no filter. On the other hand, Twitter has a wide reach, and it’s easy for people to find you," said Dr. Gusani, an ACS Fellow and assistant professor of surgery, medicine, and public health sciences at Pennsylvania State University, Hershey.
A recent survey of 315 members of the American College of Surgeons found that 79% never use Twitter, while 6% use it daily and 3% use it weekly (Bull. Am. Coll. Surg. 2011;96:46-8). In Dr. Gusani’s opinion, surgeons can use Twitter to update the public about the latest news, events, and research highlights; respond to other tweets related to their field, area of research, or organization; participate in tweet chats or Q&A sessions; and tweet highlights from professional events and meetings.
While some clinicians use Twitter for patient contact and marketing, Dr. Gusani cautioned that it’s important to be wary of violating patient confidentiality. A review of 260 physician Twitter accounts revealed that 144 of 5,156 tweets (3%) were categorized as unprofessional (JAMA 2011;305:566-8). Of these, 38 (0.7%) represented potential patient privacy violations and 33 (0.6%) contained profanity.
Dr. Gusani said that he uses Twitter to "push information, studies, and observations related mainly to oncology and surgical oncology patient education. I post perspectives about medical news and occasional retweets." Twitter-based resources and chats that are recommended by Dr. Gusani include #twitJP, a journal club; #hcsm, a global health care chat that takes place at 9 p.m. ET every Sunday; #CMEchat, which takes place every Wednesday at 11 a.m. ET; and #Meded chat, which takes place every Thursday at 4 p.m. and 9 p.m. ET.
Dr. Seung S. Gwon spoke about the potential benefits of LinkedIn, a professional networking site that allows users to strengthen and expand their network of contacts. It currently has more than 15 million members in more than 200 countries and territories, including 44 million-plus members in the U. S. alone.
"The best part about LinkedIn is that it only takes a few minutes to set up your online profile, where you might list your experience, education, and accomplishments," said Dr. Gwon, an ACS Fellow with El Centro (Calif.) Regional Medical Center. The overall purpose is to connect to other users and build a network of trusted contacts, including personal e-mail contacts, professional colleagues, coworkers, and former classmates.
Dr. Gwon said that physicians have been slow to join LinkedIn because it doesn’t allow them to directly connect with their patients. "However, it does provide you with a digital footprint, so if patients want to look, they can," she said. "Also, a lot of people feel there is no value to networking if they’re already employed. If you like your job and you like where you are, there’s no reason to set up a big profile, primarily because most physicians work in a narrowly defined geography and we don’t really see the need to sell ourselves. We rely on word-of-mouth, the reputations that we create in our communities, [and] physicians who refer patients to us."
Even so, she advises physicians to consider joining LinkedIn because it improves Google search rankings, and it is a cost-effective and efficient means to share information and maintain professional relationships.
No speaker had relevant conflicts.
SAN DIEGO -- Facebook, Twitter, and other social media have their rightful place in surgeons' busy schedules, according to several surgeons who participated in a social media symposium at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
In fact, these media just might help you land your dream job, raise money, screen applicants to your fellowship program, enhance communication with your peers, or strengthen relationships with your patients.
Dr. Gretchen Purcell Jackson noted that 61% of adults in the United States look online for health information. In addition, 41% of patients have read a commentary or shared experiences about health or medical issues in an online news group, website, or blog; 24% of online patients have consulted rankings or reviews of physicians, providers, and hospitals; 60% of active online patients report that using the Web affected a medical decision; and more than 700 hospitals currently use social networking tools.
"People seek and give advice about their health care concerns, they seek and share information about medical problems, and they share stories about their health care experiences. Some people use social media to raise money for health-related causes. Patients are using social media in a wide variety of ways, and they might be talking about you," said Dr. Jackson, an ACS Fellow and assistant professor of surgery and biomedical informatics at Vanderbilt University, Nashville, Tenn.
Facebook has 845 million active users making more than 1 billion posts per day, while Twitter has more than 465 million accounts and grows by 11 accounts per second.
Facebook is used by 64% of surgeons, compared with 42% of the general population in the United States, according to Dr. Kiran K. Turaga. "As usual, we surgeons are ahead of the curve, but Facebook has unique characteristics that can affect every single aspect of our lives," said Dr. Turaga, assistant professor of surgery at the Medical College of Wisconsin, Milwaukee. "In terms of trainees, it can affect medical student and resident education, and it can affect recruitment. For patients, you can use this for fund-raising, marketing, forming support groups, increasing awareness [about an aspect of health], recruiting for clinical trials, and monitoring for diseases."
More than 95% of U.S. medical schools have a Facebook presence, Dr. Turaga said, and 71% of these have active student group accounts. In addition, 70% of medical students have active individual Facebook accounts. However, 60% of medical schools have reported incidents of students posting unprofessional content, including profanity (in 52% of cases), breach of patient confidentiality (in 13% of cases), or photos of themselves in a state of intoxication (in 39% of cases) (JAMA 2009;302:1309-15).
Through a sister organization known as Causes (www.causes.com), Facebook has 170 million users who have generated $40 million for 27,000 not-for-profit groups, including hospitals. This makes Facebook "a remarkable tool for fund-raising," Dr. Turaga said. "This could be as simple as raising $1,000 for a new east wing in your hospital."
Furthermore, he said, creating an ad on Facebook allows you to reach 19 million people with an interest in cancer, 600,000 people with an interest in surgery, and 5,000 people with an interest in laparoscopy. Facebook also offers physicians unique opportunities for peer-to-peer interaction by providing a platform for online consultations, virtual tumor boards, journals and summaries of medical news and blogs, and discussions of health care reform and other topics of interest. There are currently 757 Facebook health groups with 300,000 members, he said.
Dr. Turaga warned that posting recognizable patient information on Facebook or other social media channels can violate the Health Insurance Portability and Accountability Act, state criminal laws regarding patient health information, state licensure laws, state professional misconduct laws, and standards set by the Joint Commission.
"If you are considering posting any information that is patient specific, make sure you have exclusive consent of the patient," he said. "The other thing to consider is unnecessary patient-provider interaction, which would mean that you start engaging in a relationship with a patient in which you start giving advice. Then you become liable for that advice, so there can be medical-legal consequences."
Before you start using Facebook or another type of social media, Dr. Turaga recommends considering the acronym POST, which stands for people (whom do you want to target with your social media?), objectives (why do you want to target them?), strategy (how are you going to target them?), and technology (which social media will you use to do so?).
Twitter, a microblogging site that allows communication by posts of no more than 140 characters in length, is an open platform of communication rather than a closed platform, explained Dr. Niraj J. Gusani. "This adds a level of complexity – and possibly risk – that may make this medium less ideal for health care professional use. Anything that you post can be seen by anyone in the world at any time. There’s no filter. On the other hand, Twitter has a wide reach, and it’s easy for people to find you," said Dr. Gusani, an ACS Fellow and assistant professor of surgery, medicine, and public health sciences at Pennsylvania State University, Hershey.
A recent survey of 315 members of the American College of Surgeons found that 79% never use Twitter, while 6% use it daily and 3% use it weekly (Bull. Am. Coll. Surg. 2011;96:46-8). In Dr. Gusani’s opinion, surgeons can use Twitter to update the public about the latest news, events, and research highlights; respond to other tweets related to their field, area of research, or organization; participate in tweet chats or Q&A sessions; and tweet highlights from professional events and meetings.
While some clinicians use Twitter for patient contact and marketing, Dr. Gusani cautioned that it’s important to be wary of violating patient confidentiality. A review of 260 physician Twitter accounts revealed that 144 of 5,156 tweets (3%) were categorized as unprofessional (JAMA 2011;305:566-8). Of these, 38 (0.7%) represented potential patient privacy violations and 33 (0.6%) contained profanity.
Dr. Gusani said that he uses Twitter to "push information, studies, and observations related mainly to oncology and surgical oncology patient education. I post perspectives about medical news and occasional retweets." Twitter-based resources and chats that are recommended by Dr. Gusani include #twitJP, a journal club; #hcsm, a global health care chat that takes place at 9 p.m. ET every Sunday; #CMEchat, which takes place every Wednesday at 11 a.m. ET; and #Meded chat, which takes place every Thursday at 4 p.m. and 9 p.m. ET.
Dr. Seung S. Gwon spoke about the potential benefits of LinkedIn, a professional networking site that allows users to strengthen and expand their network of contacts. It currently has more than 15 million members in more than 200 countries and territories, including 44 million-plus members in the U. S. alone.
"The best part about LinkedIn is that it only takes a few minutes to set up your online profile, where you might list your experience, education, and accomplishments," said Dr. Gwon, an ACS Fellow with El Centro (Calif.) Regional Medical Center. The overall purpose is to connect to other users and build a network of trusted contacts, including personal e-mail contacts, professional colleagues, coworkers, and former classmates.
Dr. Gwon said that physicians have been slow to join LinkedIn because it doesn’t allow them to directly connect with their patients. "However, it does provide you with a digital footprint, so if patients want to look, they can," she said. "Also, a lot of people feel there is no value to networking if they’re already employed. If you like your job and you like where you are, there’s no reason to set up a big profile, primarily because most physicians work in a narrowly defined geography and we don’t really see the need to sell ourselves. We rely on word-of-mouth, the reputations that we create in our communities, [and] physicians who refer patients to us."
Even so, she advises physicians to consider joining LinkedIn because it improves Google search rankings, and it is a cost-effective and efficient means to share information and maintain professional relationships.
No speaker had relevant conflicts.
New Staples Add to Options for Cesarean Section
SAN DIEGO – Of 500 consecutive cesarean deliveries closed with subcuticular absorbable staples, only one hematoma occurred, and the overall surgical site infection rate was 1.2%, according to study findings.
"This study was surprising," lead investigator Dr. Kirk A. Shibley said in an interview before a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "I anticipated a low infection rate due to the interrupted and subcuticular nature of the technology, but I did not anticipate that the number of other wound complications would be so low. That is to say that the number of wound hematomas and seromas and separations is almost nonexistent."
Dr. Shibley, who practices obstetrics and gynecology in Edina, Minn., and his associates evaluated data from 500 consecutive cesarean procedures closed with Incisive Surgical’s INSORB absorbable staples. All the operations were performed by five clinicians in a single obstetrics practice during a 4-year period that ended in 2008. The investigators obtained the data from clinic medical records and from 30-day postdischarge infection surveillance programs at two community hospitals.
Dr. Shibley reported that there were only six surgical site infections, for a rate of 1.2%. There was one hematoma, no seromas, and no wound disruptions. In follow-up visits, he said, patients expressed a high level of satisfaction with the results. "The take-home message is that this skin closure technology is fast, and provides low-maintenance, cosmetic wounds with a very low infection and complication rate," he said.
In the poster, Dr. Shibley and his associates postulated that the improved outcomes may be due in part to the fact that the INSORB staples are made of a benign copolymer "of predominately polylactic acid, shown to elicit a very low inflammatory response in animal and human clinical studies, and may account for decreased pain, serous exudate, and other associated complications."
Also, they continued, "absorbable staples are placed entirely within the dermis without the percutaneous insult of metal staples. Absorbable staples avoid the associated patient discomfort and anxiety associated with metal staple removal. The absorbable staples precisely and effectively secure the dermis without tissue strangulation or compression that can occur with ... metal staples."
Dr. Shibley acknowledged that the study is limited as patients were not prospectively randomized to different closure types.
Dr. Shibley disclosed that he is a paid consultant to Incisive Surgical.
SAN DIEGO – Of 500 consecutive cesarean deliveries closed with subcuticular absorbable staples, only one hematoma occurred, and the overall surgical site infection rate was 1.2%, according to study findings.
"This study was surprising," lead investigator Dr. Kirk A. Shibley said in an interview before a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "I anticipated a low infection rate due to the interrupted and subcuticular nature of the technology, but I did not anticipate that the number of other wound complications would be so low. That is to say that the number of wound hematomas and seromas and separations is almost nonexistent."
Dr. Shibley, who practices obstetrics and gynecology in Edina, Minn., and his associates evaluated data from 500 consecutive cesarean procedures closed with Incisive Surgical’s INSORB absorbable staples. All the operations were performed by five clinicians in a single obstetrics practice during a 4-year period that ended in 2008. The investigators obtained the data from clinic medical records and from 30-day postdischarge infection surveillance programs at two community hospitals.
Dr. Shibley reported that there were only six surgical site infections, for a rate of 1.2%. There was one hematoma, no seromas, and no wound disruptions. In follow-up visits, he said, patients expressed a high level of satisfaction with the results. "The take-home message is that this skin closure technology is fast, and provides low-maintenance, cosmetic wounds with a very low infection and complication rate," he said.
In the poster, Dr. Shibley and his associates postulated that the improved outcomes may be due in part to the fact that the INSORB staples are made of a benign copolymer "of predominately polylactic acid, shown to elicit a very low inflammatory response in animal and human clinical studies, and may account for decreased pain, serous exudate, and other associated complications."
Also, they continued, "absorbable staples are placed entirely within the dermis without the percutaneous insult of metal staples. Absorbable staples avoid the associated patient discomfort and anxiety associated with metal staple removal. The absorbable staples precisely and effectively secure the dermis without tissue strangulation or compression that can occur with ... metal staples."
Dr. Shibley acknowledged that the study is limited as patients were not prospectively randomized to different closure types.
Dr. Shibley disclosed that he is a paid consultant to Incisive Surgical.
SAN DIEGO – Of 500 consecutive cesarean deliveries closed with subcuticular absorbable staples, only one hematoma occurred, and the overall surgical site infection rate was 1.2%, according to study findings.
"This study was surprising," lead investigator Dr. Kirk A. Shibley said in an interview before a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "I anticipated a low infection rate due to the interrupted and subcuticular nature of the technology, but I did not anticipate that the number of other wound complications would be so low. That is to say that the number of wound hematomas and seromas and separations is almost nonexistent."
Dr. Shibley, who practices obstetrics and gynecology in Edina, Minn., and his associates evaluated data from 500 consecutive cesarean procedures closed with Incisive Surgical’s INSORB absorbable staples. All the operations were performed by five clinicians in a single obstetrics practice during a 4-year period that ended in 2008. The investigators obtained the data from clinic medical records and from 30-day postdischarge infection surveillance programs at two community hospitals.
Dr. Shibley reported that there were only six surgical site infections, for a rate of 1.2%. There was one hematoma, no seromas, and no wound disruptions. In follow-up visits, he said, patients expressed a high level of satisfaction with the results. "The take-home message is that this skin closure technology is fast, and provides low-maintenance, cosmetic wounds with a very low infection and complication rate," he said.
In the poster, Dr. Shibley and his associates postulated that the improved outcomes may be due in part to the fact that the INSORB staples are made of a benign copolymer "of predominately polylactic acid, shown to elicit a very low inflammatory response in animal and human clinical studies, and may account for decreased pain, serous exudate, and other associated complications."
Also, they continued, "absorbable staples are placed entirely within the dermis without the percutaneous insult of metal staples. Absorbable staples avoid the associated patient discomfort and anxiety associated with metal staple removal. The absorbable staples precisely and effectively secure the dermis without tissue strangulation or compression that can occur with ... metal staples."
Dr. Shibley acknowledged that the study is limited as patients were not prospectively randomized to different closure types.
Dr. Shibley disclosed that he is a paid consultant to Incisive Surgical.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Investigational Contraceptive Patch Shows Promise
SAN DIEGO – Women who were randomized to an investigative low-dose ethinyl estradiol and levonorgestrel contraceptive patch had similar contraceptive efficacy, cycle control, and safety results, compared with those who were randomized to a standard oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel, results from a phase III trial demonstrated.
In addition, efficacy of the once-weekly patch, developed by Princeton, N.J.–based Agile Therapeutics and known as AG200-15, was comparable among obese and nonobese women, a finding that surprised investigators, who were led by Dr. Andrew M. Kaunitz, professor of the department of obstetrics and gynecology at the University of Florida, Jacksonville.
"There has been controversy and concern over the past decade that obese women might experience higher failure rates with some hormonal contraceptive methods, particularly transdermal contraception," Dr. Kaunitz said in an interview in advance of a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "We found that efficacy was comparable regardless of body mass index. That was an unexpected, but welcome, finding."
Pharmacokinetic studies of AG200-15 have shown that it delivers ethinyl estradiol (EE) and levonorgestrel equivalent to that seen with a 30-mg dose of EE and a 120-mg dose of levonorgestrel oral contraceptives. This is in contrast to Ortho Evra (norelgestromin/ethinyl estradiol transdermal system, Ortho-McNeil–Janssen Pharmaceuticals), the first-generation contraceptive patch that gained popularity upon release, but was found to deliver a dose of EE substantially higher than conventional oral contraceptives.
"At the same time, some well-publicized cases of vascular events, including fatal pulmonary emboli, occurred in women using the Ortho Evra patch," Dr. Kaunitz said. "These cases generated a fair amount of medical-legal attention. Ortho Evra went through this boom/bust phenomenon, where it was wildly popular, and now I think I only have one patient who is using it. I think it points out that if there were a lower-[dose] estrogen patch that provided effective contraception, but did not expose women to more estrogen than with current low-dose birth control pills, it could occupy an important contraceptive niche for U.S. women."
For the current study, which was conducted at 96 centers, 1,128 women were treated for 1 year (13 cycles) with AG200-15, and 375 were treated for six cycles with oral contraceptives followed by seven cycles of AG200-15. Blood draws were performed at cycles 2, 6, and 13, and complete physical and gynecologic exams were performed at baseline, cycle 7, and the final visit, which was 14 days after the removal of the last patch or intake of the last oral contraceptive.
The mean age of the study participants was 26 years, 55% were white/non-Hispanic, and their mean body mass index was 27.5 kg/m2. More than half (60%) were new users of hormonal contraceptives; 14% switched from another contraceptive prior to the study.
Dr. Kaunitz reported that there were no clinically meaningful differences in contraceptive efficacy among the intent-to-treat population between the oral contraceptive group and the AG200-15 group (a Pearl Index [PI] of 4.02 vs. 4.92). When the PI was stratified by BMI for the intent-to-treat population in the AG200-15 group, the PI for obese patients (defined as a BMI of 32 kg/m2 or greater) was similar to that of the nonobese patients (PI of 2.85 vs. 3.17).
When the researchers stratified the study participants by race/ethnicity, the PI for the AG200-15 and oral contraceptive groups was lowest in the white subgroup, followed by the Hispanic and the black subgroups. This likely reflects that women of lower socioeconomic status take oral contraceptives less consistently than other women, Dr. Kaunitz said, a phenomenon that has been observed by other investigators (Contraception 2012;85:465-9).
Cycle control was similar between the two treatment groups. In cycle 3, for example, the incidence of breakthrough bleeding and/or spotting episodes was 24.8% in the AG200-15 group, compared with 23.2% in the oral contraceptive group. In cycle 5, the incidence of these events was 22.3% and 21.9.
Nearly half of women (48%) chose to apply AG200-15 to their buttocks, while 40% chose the abdomen, and 12% chose the upper torso. "We found that there was good adhesiveness, as fewer than 3% of women experienced patch detachment," Dr. Kaunitz said. "Also, there was no suggestion that patches would come off with a lot of sweating or vigorous physical activity."
Overall, 80% of women reported no skin irritation. Only 0.1% of women reported severe irritation; 17%, mild skin irritation; and 2%-3%, moderate skin irritation.
The incidence of hormone-related adverse events was similar between the two groups: 1.3% in the AG200-15 group vs. 1.2% in the oral contraceptive group. Breast tenderness was uncommon, reported by fewer than 2% of women in both groups. "That was a reassuring safety signal," Dr. Kaunitz said.
The investigators reported one serious adverse event in the oral contraceptive group (one case with an unspecified liver problem) and three adverse events in the AG200-15 group (one case with a blood clot in the left subclavian vein, one case of uncontrollable nausea and vomiting, and one case of drug overdose with Benadryl) to be possibly or probably related to the study drug.
Going forward, Dr. Kaunitz said that he would like to see clinical trials of AG200-15 that involve shorter hormone intervals than the classic schedule of 21 active tablets followed by 7 hormone-free days as followed in this study. "Newer contraceptives tend to have shorter hormone-free intervals or be continuous," he said. "Going forward, I’d be interested in clinical trials of this patch using hormone-free intervals shorter than 7 days or cycles longer than 1 month."
Agile Therapeutics has submitted a New Drug Application for AG200-15 with the Food and Drug Administration.
The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
SAN DIEGO – Women who were randomized to an investigative low-dose ethinyl estradiol and levonorgestrel contraceptive patch had similar contraceptive efficacy, cycle control, and safety results, compared with those who were randomized to a standard oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel, results from a phase III trial demonstrated.
In addition, efficacy of the once-weekly patch, developed by Princeton, N.J.–based Agile Therapeutics and known as AG200-15, was comparable among obese and nonobese women, a finding that surprised investigators, who were led by Dr. Andrew M. Kaunitz, professor of the department of obstetrics and gynecology at the University of Florida, Jacksonville.
"There has been controversy and concern over the past decade that obese women might experience higher failure rates with some hormonal contraceptive methods, particularly transdermal contraception," Dr. Kaunitz said in an interview in advance of a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "We found that efficacy was comparable regardless of body mass index. That was an unexpected, but welcome, finding."
Pharmacokinetic studies of AG200-15 have shown that it delivers ethinyl estradiol (EE) and levonorgestrel equivalent to that seen with a 30-mg dose of EE and a 120-mg dose of levonorgestrel oral contraceptives. This is in contrast to Ortho Evra (norelgestromin/ethinyl estradiol transdermal system, Ortho-McNeil–Janssen Pharmaceuticals), the first-generation contraceptive patch that gained popularity upon release, but was found to deliver a dose of EE substantially higher than conventional oral contraceptives.
"At the same time, some well-publicized cases of vascular events, including fatal pulmonary emboli, occurred in women using the Ortho Evra patch," Dr. Kaunitz said. "These cases generated a fair amount of medical-legal attention. Ortho Evra went through this boom/bust phenomenon, where it was wildly popular, and now I think I only have one patient who is using it. I think it points out that if there were a lower-[dose] estrogen patch that provided effective contraception, but did not expose women to more estrogen than with current low-dose birth control pills, it could occupy an important contraceptive niche for U.S. women."
For the current study, which was conducted at 96 centers, 1,128 women were treated for 1 year (13 cycles) with AG200-15, and 375 were treated for six cycles with oral contraceptives followed by seven cycles of AG200-15. Blood draws were performed at cycles 2, 6, and 13, and complete physical and gynecologic exams were performed at baseline, cycle 7, and the final visit, which was 14 days after the removal of the last patch or intake of the last oral contraceptive.
The mean age of the study participants was 26 years, 55% were white/non-Hispanic, and their mean body mass index was 27.5 kg/m2. More than half (60%) were new users of hormonal contraceptives; 14% switched from another contraceptive prior to the study.
Dr. Kaunitz reported that there were no clinically meaningful differences in contraceptive efficacy among the intent-to-treat population between the oral contraceptive group and the AG200-15 group (a Pearl Index [PI] of 4.02 vs. 4.92). When the PI was stratified by BMI for the intent-to-treat population in the AG200-15 group, the PI for obese patients (defined as a BMI of 32 kg/m2 or greater) was similar to that of the nonobese patients (PI of 2.85 vs. 3.17).
When the researchers stratified the study participants by race/ethnicity, the PI for the AG200-15 and oral contraceptive groups was lowest in the white subgroup, followed by the Hispanic and the black subgroups. This likely reflects that women of lower socioeconomic status take oral contraceptives less consistently than other women, Dr. Kaunitz said, a phenomenon that has been observed by other investigators (Contraception 2012;85:465-9).
Cycle control was similar between the two treatment groups. In cycle 3, for example, the incidence of breakthrough bleeding and/or spotting episodes was 24.8% in the AG200-15 group, compared with 23.2% in the oral contraceptive group. In cycle 5, the incidence of these events was 22.3% and 21.9.
Nearly half of women (48%) chose to apply AG200-15 to their buttocks, while 40% chose the abdomen, and 12% chose the upper torso. "We found that there was good adhesiveness, as fewer than 3% of women experienced patch detachment," Dr. Kaunitz said. "Also, there was no suggestion that patches would come off with a lot of sweating or vigorous physical activity."
Overall, 80% of women reported no skin irritation. Only 0.1% of women reported severe irritation; 17%, mild skin irritation; and 2%-3%, moderate skin irritation.
The incidence of hormone-related adverse events was similar between the two groups: 1.3% in the AG200-15 group vs. 1.2% in the oral contraceptive group. Breast tenderness was uncommon, reported by fewer than 2% of women in both groups. "That was a reassuring safety signal," Dr. Kaunitz said.
The investigators reported one serious adverse event in the oral contraceptive group (one case with an unspecified liver problem) and three adverse events in the AG200-15 group (one case with a blood clot in the left subclavian vein, one case of uncontrollable nausea and vomiting, and one case of drug overdose with Benadryl) to be possibly or probably related to the study drug.
Going forward, Dr. Kaunitz said that he would like to see clinical trials of AG200-15 that involve shorter hormone intervals than the classic schedule of 21 active tablets followed by 7 hormone-free days as followed in this study. "Newer contraceptives tend to have shorter hormone-free intervals or be continuous," he said. "Going forward, I’d be interested in clinical trials of this patch using hormone-free intervals shorter than 7 days or cycles longer than 1 month."
Agile Therapeutics has submitted a New Drug Application for AG200-15 with the Food and Drug Administration.
The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
SAN DIEGO – Women who were randomized to an investigative low-dose ethinyl estradiol and levonorgestrel contraceptive patch had similar contraceptive efficacy, cycle control, and safety results, compared with those who were randomized to a standard oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel, results from a phase III trial demonstrated.
In addition, efficacy of the once-weekly patch, developed by Princeton, N.J.–based Agile Therapeutics and known as AG200-15, was comparable among obese and nonobese women, a finding that surprised investigators, who were led by Dr. Andrew M. Kaunitz, professor of the department of obstetrics and gynecology at the University of Florida, Jacksonville.
"There has been controversy and concern over the past decade that obese women might experience higher failure rates with some hormonal contraceptive methods, particularly transdermal contraception," Dr. Kaunitz said in an interview in advance of a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "We found that efficacy was comparable regardless of body mass index. That was an unexpected, but welcome, finding."
Pharmacokinetic studies of AG200-15 have shown that it delivers ethinyl estradiol (EE) and levonorgestrel equivalent to that seen with a 30-mg dose of EE and a 120-mg dose of levonorgestrel oral contraceptives. This is in contrast to Ortho Evra (norelgestromin/ethinyl estradiol transdermal system, Ortho-McNeil–Janssen Pharmaceuticals), the first-generation contraceptive patch that gained popularity upon release, but was found to deliver a dose of EE substantially higher than conventional oral contraceptives.
"At the same time, some well-publicized cases of vascular events, including fatal pulmonary emboli, occurred in women using the Ortho Evra patch," Dr. Kaunitz said. "These cases generated a fair amount of medical-legal attention. Ortho Evra went through this boom/bust phenomenon, where it was wildly popular, and now I think I only have one patient who is using it. I think it points out that if there were a lower-[dose] estrogen patch that provided effective contraception, but did not expose women to more estrogen than with current low-dose birth control pills, it could occupy an important contraceptive niche for U.S. women."
For the current study, which was conducted at 96 centers, 1,128 women were treated for 1 year (13 cycles) with AG200-15, and 375 were treated for six cycles with oral contraceptives followed by seven cycles of AG200-15. Blood draws were performed at cycles 2, 6, and 13, and complete physical and gynecologic exams were performed at baseline, cycle 7, and the final visit, which was 14 days after the removal of the last patch or intake of the last oral contraceptive.
The mean age of the study participants was 26 years, 55% were white/non-Hispanic, and their mean body mass index was 27.5 kg/m2. More than half (60%) were new users of hormonal contraceptives; 14% switched from another contraceptive prior to the study.
Dr. Kaunitz reported that there were no clinically meaningful differences in contraceptive efficacy among the intent-to-treat population between the oral contraceptive group and the AG200-15 group (a Pearl Index [PI] of 4.02 vs. 4.92). When the PI was stratified by BMI for the intent-to-treat population in the AG200-15 group, the PI for obese patients (defined as a BMI of 32 kg/m2 or greater) was similar to that of the nonobese patients (PI of 2.85 vs. 3.17).
When the researchers stratified the study participants by race/ethnicity, the PI for the AG200-15 and oral contraceptive groups was lowest in the white subgroup, followed by the Hispanic and the black subgroups. This likely reflects that women of lower socioeconomic status take oral contraceptives less consistently than other women, Dr. Kaunitz said, a phenomenon that has been observed by other investigators (Contraception 2012;85:465-9).
Cycle control was similar between the two treatment groups. In cycle 3, for example, the incidence of breakthrough bleeding and/or spotting episodes was 24.8% in the AG200-15 group, compared with 23.2% in the oral contraceptive group. In cycle 5, the incidence of these events was 22.3% and 21.9.
Nearly half of women (48%) chose to apply AG200-15 to their buttocks, while 40% chose the abdomen, and 12% chose the upper torso. "We found that there was good adhesiveness, as fewer than 3% of women experienced patch detachment," Dr. Kaunitz said. "Also, there was no suggestion that patches would come off with a lot of sweating or vigorous physical activity."
Overall, 80% of women reported no skin irritation. Only 0.1% of women reported severe irritation; 17%, mild skin irritation; and 2%-3%, moderate skin irritation.
The incidence of hormone-related adverse events was similar between the two groups: 1.3% in the AG200-15 group vs. 1.2% in the oral contraceptive group. Breast tenderness was uncommon, reported by fewer than 2% of women in both groups. "That was a reassuring safety signal," Dr. Kaunitz said.
The investigators reported one serious adverse event in the oral contraceptive group (one case with an unspecified liver problem) and three adverse events in the AG200-15 group (one case with a blood clot in the left subclavian vein, one case of uncontrollable nausea and vomiting, and one case of drug overdose with Benadryl) to be possibly or probably related to the study drug.
Going forward, Dr. Kaunitz said that he would like to see clinical trials of AG200-15 that involve shorter hormone intervals than the classic schedule of 21 active tablets followed by 7 hormone-free days as followed in this study. "Newer contraceptives tend to have shorter hormone-free intervals or be continuous," he said. "Going forward, I’d be interested in clinical trials of this patch using hormone-free intervals shorter than 7 days or cycles longer than 1 month."
Agile Therapeutics has submitted a New Drug Application for AG200-15 with the Food and Drug Administration.
The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: No clinically meaningful differences in contraceptive efficacy were observed between women who used an oral contraceptive and those who used a transdermal contraceptive patch (a Pearl Index of 4.02 vs. 4.92).
Data Source: A phase III, year-long study of 1,503 women who were randomized to receive either an oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel or a once-weekly transdermal patch containing a 30-mg dose of ethinyl estradiol and a 120-mg dose of levonorgestrel.
Disclosures: The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
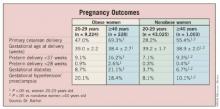
Maternal Age, Obesity Associated With Adverse Pregnancy Outcomes
SAN DIEGO – Although women who delay pregnancy to age 40 years and older face an increased risk for adverse outcomes, reducing prepregnancy body mass index may reduce their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery, results from a large study demonstrated.
"This is an important issue in the United States as more than 13% of pregnant women are now age 35 and older, and nearly 3% are age 40 and older at delivery," Dr. John R. Barton said in an interview prior to a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "These data underscore the impact of obesity on increasing adverse outcomes in otherwise healthy women."
To examine pregnancy outcomes of healthy nulliparous women aged 40 years or older at delivery, Dr. Barton, director of maternal-fetal medicine at Central Baptist Hospital, Lexington, Ky., and his associates evaluated 53,480 women who were voluntarily enrolled in a pregnancy risk assessment and education program operated by Alere Health between July 1, 2006, and Aug. 1, 2011.
The researchers excluded women who reported heart disease, chronic hypertension, pregestational diabetes, other medical disorders, tobacco use, and conception with assistive reproductive technology. Data were grouped by maternal age (20-29 years or 40 and older) and obesity. Those with a prepregnancy body mass index (PPBMI) of 30 kg/m2 or higher were defined as obese; those with lower BMIs were defined a nonobese.
Within each PPBMI group, nulliparous women 40 years of age and older delivered at a significantly lower gestational age, had a greater incidence of cesarean delivery, gestational diabetes, preterm birth, and both low and very-low birth weight infants, compared with controls aged 20-29 years. In addition, obesity was associated with higher rates of adverse pregnancy outcomes in the group of women aged 40 years and older.
"Throughout the reproductive years, health care providers to women should support and encourage them to maintain a healthy lifestyle and a healthy body habitus," Dr. Barton advised. "In healthy nulliparous women, both advanced maternal age and obesity influence pregnancy outcomes. Women choosing to delay pregnancy until age 40 years and older may modify their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery by reducing their body mass index to nonobese levels prior to conception."
Dr. Barton acknowledged certain limitations of the study, including the fact that while the population included both Medicaid and commercially insured women from across the United States, "we do not know for sure if the same results would be observed in the general population or for those with later prenatal care initiation. It is also important to stress that these women were healthy in that they did not have heart disease, chronic hypertension, diabetes, or other medical disorders such as kidney disease or autoimmune disorders. We also did not include women that reported smoking during pregnancy. The overall rate of obesity was 17.7%, which is not comparable with the general obstetrical population (about 35%) – yet reflects our inclusion/exclusion criteria."
Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
SAN DIEGO – Although women who delay pregnancy to age 40 years and older face an increased risk for adverse outcomes, reducing prepregnancy body mass index may reduce their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery, results from a large study demonstrated.
"This is an important issue in the United States as more than 13% of pregnant women are now age 35 and older, and nearly 3% are age 40 and older at delivery," Dr. John R. Barton said in an interview prior to a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "These data underscore the impact of obesity on increasing adverse outcomes in otherwise healthy women."
To examine pregnancy outcomes of healthy nulliparous women aged 40 years or older at delivery, Dr. Barton, director of maternal-fetal medicine at Central Baptist Hospital, Lexington, Ky., and his associates evaluated 53,480 women who were voluntarily enrolled in a pregnancy risk assessment and education program operated by Alere Health between July 1, 2006, and Aug. 1, 2011.
The researchers excluded women who reported heart disease, chronic hypertension, pregestational diabetes, other medical disorders, tobacco use, and conception with assistive reproductive technology. Data were grouped by maternal age (20-29 years or 40 and older) and obesity. Those with a prepregnancy body mass index (PPBMI) of 30 kg/m2 or higher were defined as obese; those with lower BMIs were defined a nonobese.
Within each PPBMI group, nulliparous women 40 years of age and older delivered at a significantly lower gestational age, had a greater incidence of cesarean delivery, gestational diabetes, preterm birth, and both low and very-low birth weight infants, compared with controls aged 20-29 years. In addition, obesity was associated with higher rates of adverse pregnancy outcomes in the group of women aged 40 years and older.
"Throughout the reproductive years, health care providers to women should support and encourage them to maintain a healthy lifestyle and a healthy body habitus," Dr. Barton advised. "In healthy nulliparous women, both advanced maternal age and obesity influence pregnancy outcomes. Women choosing to delay pregnancy until age 40 years and older may modify their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery by reducing their body mass index to nonobese levels prior to conception."
Dr. Barton acknowledged certain limitations of the study, including the fact that while the population included both Medicaid and commercially insured women from across the United States, "we do not know for sure if the same results would be observed in the general population or for those with later prenatal care initiation. It is also important to stress that these women were healthy in that they did not have heart disease, chronic hypertension, diabetes, or other medical disorders such as kidney disease or autoimmune disorders. We also did not include women that reported smoking during pregnancy. The overall rate of obesity was 17.7%, which is not comparable with the general obstetrical population (about 35%) – yet reflects our inclusion/exclusion criteria."
Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
SAN DIEGO – Although women who delay pregnancy to age 40 years and older face an increased risk for adverse outcomes, reducing prepregnancy body mass index may reduce their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery, results from a large study demonstrated.
"This is an important issue in the United States as more than 13% of pregnant women are now age 35 and older, and nearly 3% are age 40 and older at delivery," Dr. John R. Barton said in an interview prior to a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "These data underscore the impact of obesity on increasing adverse outcomes in otherwise healthy women."
To examine pregnancy outcomes of healthy nulliparous women aged 40 years or older at delivery, Dr. Barton, director of maternal-fetal medicine at Central Baptist Hospital, Lexington, Ky., and his associates evaluated 53,480 women who were voluntarily enrolled in a pregnancy risk assessment and education program operated by Alere Health between July 1, 2006, and Aug. 1, 2011.
The researchers excluded women who reported heart disease, chronic hypertension, pregestational diabetes, other medical disorders, tobacco use, and conception with assistive reproductive technology. Data were grouped by maternal age (20-29 years or 40 and older) and obesity. Those with a prepregnancy body mass index (PPBMI) of 30 kg/m2 or higher were defined as obese; those with lower BMIs were defined a nonobese.
Within each PPBMI group, nulliparous women 40 years of age and older delivered at a significantly lower gestational age, had a greater incidence of cesarean delivery, gestational diabetes, preterm birth, and both low and very-low birth weight infants, compared with controls aged 20-29 years. In addition, obesity was associated with higher rates of adverse pregnancy outcomes in the group of women aged 40 years and older.
"Throughout the reproductive years, health care providers to women should support and encourage them to maintain a healthy lifestyle and a healthy body habitus," Dr. Barton advised. "In healthy nulliparous women, both advanced maternal age and obesity influence pregnancy outcomes. Women choosing to delay pregnancy until age 40 years and older may modify their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery by reducing their body mass index to nonobese levels prior to conception."
Dr. Barton acknowledged certain limitations of the study, including the fact that while the population included both Medicaid and commercially insured women from across the United States, "we do not know for sure if the same results would be observed in the general population or for those with later prenatal care initiation. It is also important to stress that these women were healthy in that they did not have heart disease, chronic hypertension, diabetes, or other medical disorders such as kidney disease or autoimmune disorders. We also did not include women that reported smoking during pregnancy. The overall rate of obesity was 17.7%, which is not comparable with the general obstetrical population (about 35%) – yet reflects our inclusion/exclusion criteria."
Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: A significantly higher proportion of obese women aged 40 years or older underwent primary cesarean delivery, compared with obese women aged 20-29 years (69.3% vs. 47%, respectively). A similar age-related association was observed among nonobese women (55.4% vs. 28.2%).
Data Source: Data were from a study of 53,480 nulliparous women aged either 20-29 years or 40 years and older who were voluntarily enrolled in a pregnancy risk assessment and education program.
Disclosures: Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
Wide Disparity in Appendicitis Costs Observed
In California, the median cost of treating patients hospitalized for uncomplicated appendicitis ranged from $1,529 to a whopping $182,955, a finding that surprised investigators led by Dr. Renee Y. Hsia, of the emergency medicine department at the University of California, San Francisco.
"Given estimates that 60% of bankruptcies in the United States involve catastrophic medical expenses, these data should alarm those making decisions about our society’s ability to obtain medical care without financial catastrophe," Dr. Hsia and her associates wrote online April 23 in the Archives of Internal Medicine.
The investigators used demographic and financial data from the 2009 Discharge Database of California’s Office of Statewide Health Planning and Development to review 19,368 cases of routine appendicitis treated at 289 hospitals and medical centers throughout California. They limited the analysis to patients 18-59 years who were admitted for 3 or fewer days (Arch. Intern. Med. 2012 April 23 [doi:10.1001/archinternmed.2012.1173]). The main outcome of interest was total charges per visit.
"It has been well described that the actual cost of care and charges billed to the patient are not necessarily the same," the investigators wrote. "But for the uninsured or underinsured, these charges are what the patient ultimately sees and therefore represent the perceived cost of their care."
Dr. Hsia and her associates found that the median hospital charge among all patients was $33,611; the lowest observed charge was $1,529 and highest was $182,955. Factors associated with higher median charges included being on Medicaid, being insured, and being treated at a for-profit hospital.
"A patient with severe abdominal pain is in a poor position to determine whether his or her physician is ordering the appropriate blood work, imaging, or surgical procedure," the investigators commented. "Price shopping is improbable, if not impossible, because the services are complex, urgently needed, and no definitive diagnosis has yet been made. In our study, even if patients did have the luxury of time and clinical knowledge to ‘shop around,’ we found that California hospitals charge patients inconsistently for what should be similar services as defined by our relatively strict definition of uncomplicated appendicitis."
The study was funded by grant KL2 RR024130 and the Robert Wood Johnson Foundation Physician Faculty Scholars. The investigators stated that they had no relevant financial conflicts to disclose.
In California, the median cost of treating patients hospitalized for uncomplicated appendicitis ranged from $1,529 to a whopping $182,955, a finding that surprised investigators led by Dr. Renee Y. Hsia, of the emergency medicine department at the University of California, San Francisco.
"Given estimates that 60% of bankruptcies in the United States involve catastrophic medical expenses, these data should alarm those making decisions about our society’s ability to obtain medical care without financial catastrophe," Dr. Hsia and her associates wrote online April 23 in the Archives of Internal Medicine.
The investigators used demographic and financial data from the 2009 Discharge Database of California’s Office of Statewide Health Planning and Development to review 19,368 cases of routine appendicitis treated at 289 hospitals and medical centers throughout California. They limited the analysis to patients 18-59 years who were admitted for 3 or fewer days (Arch. Intern. Med. 2012 April 23 [doi:10.1001/archinternmed.2012.1173]). The main outcome of interest was total charges per visit.
"It has been well described that the actual cost of care and charges billed to the patient are not necessarily the same," the investigators wrote. "But for the uninsured or underinsured, these charges are what the patient ultimately sees and therefore represent the perceived cost of their care."
Dr. Hsia and her associates found that the median hospital charge among all patients was $33,611; the lowest observed charge was $1,529 and highest was $182,955. Factors associated with higher median charges included being on Medicaid, being insured, and being treated at a for-profit hospital.
"A patient with severe abdominal pain is in a poor position to determine whether his or her physician is ordering the appropriate blood work, imaging, or surgical procedure," the investigators commented. "Price shopping is improbable, if not impossible, because the services are complex, urgently needed, and no definitive diagnosis has yet been made. In our study, even if patients did have the luxury of time and clinical knowledge to ‘shop around,’ we found that California hospitals charge patients inconsistently for what should be similar services as defined by our relatively strict definition of uncomplicated appendicitis."
The study was funded by grant KL2 RR024130 and the Robert Wood Johnson Foundation Physician Faculty Scholars. The investigators stated that they had no relevant financial conflicts to disclose.
In California, the median cost of treating patients hospitalized for uncomplicated appendicitis ranged from $1,529 to a whopping $182,955, a finding that surprised investigators led by Dr. Renee Y. Hsia, of the emergency medicine department at the University of California, San Francisco.
"Given estimates that 60% of bankruptcies in the United States involve catastrophic medical expenses, these data should alarm those making decisions about our society’s ability to obtain medical care without financial catastrophe," Dr. Hsia and her associates wrote online April 23 in the Archives of Internal Medicine.
The investigators used demographic and financial data from the 2009 Discharge Database of California’s Office of Statewide Health Planning and Development to review 19,368 cases of routine appendicitis treated at 289 hospitals and medical centers throughout California. They limited the analysis to patients 18-59 years who were admitted for 3 or fewer days (Arch. Intern. Med. 2012 April 23 [doi:10.1001/archinternmed.2012.1173]). The main outcome of interest was total charges per visit.
"It has been well described that the actual cost of care and charges billed to the patient are not necessarily the same," the investigators wrote. "But for the uninsured or underinsured, these charges are what the patient ultimately sees and therefore represent the perceived cost of their care."
Dr. Hsia and her associates found that the median hospital charge among all patients was $33,611; the lowest observed charge was $1,529 and highest was $182,955. Factors associated with higher median charges included being on Medicaid, being insured, and being treated at a for-profit hospital.
"A patient with severe abdominal pain is in a poor position to determine whether his or her physician is ordering the appropriate blood work, imaging, or surgical procedure," the investigators commented. "Price shopping is improbable, if not impossible, because the services are complex, urgently needed, and no definitive diagnosis has yet been made. In our study, even if patients did have the luxury of time and clinical knowledge to ‘shop around,’ we found that California hospitals charge patients inconsistently for what should be similar services as defined by our relatively strict definition of uncomplicated appendicitis."
The study was funded by grant KL2 RR024130 and the Robert Wood Johnson Foundation Physician Faculty Scholars. The investigators stated that they had no relevant financial conflicts to disclose.
FROM THE ARCHIVES OF INTERNAL MEDICINE
Major Finding: The median hospital charge for a routine appendectomy was $33,611. The lowest observed charge was $1,529 and the highest was $182,955.
Data Source: Data came from a review of 19,368 cases of routine appendicitis treated at 289 hospitals and medical centers in California.
Disclosures: The study was funded by grant KL2 RR024130 and the Robert Wood Johnson Foundation Physician Faculty Scholars. Dr. Hsia reported having no financial disclosures.
Gender Disparity Seen Between PEFR, Vitamin D Deficiency
Low levels of serum 25-hydroxyvitamin D are associated with decreasing peak expiratory flow rate in older men but not in older women, according to results from a longitudinal Dutch study.
Although the mediating effects of muscle strength and physical performance were examined as part of the analysis, it remains unclear exactly how vitamin D impacts pulmonary function, according to Dr. N.M. van Schoor and her colleagues at VU University Medical Center, Amsterdam, the Netherlands. The report was published online in the Journal of Clinical Endocrinology and Metabolism.
"With the exception of men having serum 25-OHD levels below 10 ng/mL (in cross-sectional analyses), adding physical performance or grip strength to the model did not lead to major changes in the association between serum 25-OHD and PEFR," the researchers wrote. "Several other mechanisms have been proposed. First, in vitro studies revealed that vitamin D modulates the activity of various defense and immune cells. Second, in a mouse model, it was shown that vitamin D deficiency decreases pulmonary function. This was primarily explained by a deficit in lung volume and could not be explained by alterations in somatic growth."
For the current study, believed to be the first of its kind, Dr. van Schoor and colleagues assessed 1,509 men and women aged 65 or older as of Jan. 1, 1996, who participated in a medical interview during 1995/1996 for the Longitudinal Aging Study Amsterdam, which they described as "an ongoing multidisciplinary cohort study on predictors and consequences of changes in physical, cognitive, emotional, and social functioning in older persons" (J. Clin. Endocrinol. Metab. 2012 April 3 [doi:10.1210/jc.2011-3199]). Data on serum 25-hydroxyvitamin D (25-OHD), peak expiratory flow rate (PEFR), and covariables were available for 596 men and 611 women in the cross-sectional analysis (limited to those who underwent medical interviews during 1995/1996) and for 454 men and 496 women in the longitudinal analysis (limited to those who underwent subsequent measurements in 1998/1999).
At baseline, men had a mean serum 25-OHD of 23.5 ng/mL while the mean level for women was 19.7 ng/mL. In men, a strong correlation between vitamin D status and PEFR was seen for serum 25-OHD levels up to 20 ng/mL. "In the cross-sectional analyses, this association was no longer statistically significant for serum 25-OHD levels between 10 and 20 ng/mL in the fully adjusted model but remained statistically significant for serum 25-OHD levels below 10 ng/mL," the researchers wrote. "In the longitudinal analyses, the relationships remained statistically significant up to a serum 25-OHD level of 20 ng/mL."
Adjustment for physical performance or grip strength did not change these results in the longitudinal analyses. However, in the cross-sectional analyses, the relationship between serum 25-OHD and PEFR was no longer statistically significant after researchers added the potential mediator grip strength.
In women, significant associations between 25-OHD levels and PEFR were observed in the cross-sectional analyses, but only after adjustment for age and season of blood collection – not in the fully adjusted models or in the longitudinal analyses. "The reason for this is unclear," the researchers noted. "It may be more difficult to find a statistically significant result in women, because women showed less variation in PEFR than men. In addition, women had lower PEFR values than men, and fewer women reported obstructive airway diseases at baseline. When excluding women having obstructive airway diseases at baseline, a trend toward significance was observed after additional adjustment for physical performance and grip strength, respectively."
The investigators acknowledged certain limitations of the study, including the fact that causality "cannot be established within the setting of a cohort study, although the observed longitudinal relationship in men does support causality. Second, data on FEV1 and FVC were not available. However, we do think that PEFR is a valid outcome, because it is an effort-independent measure of expiratory flow limitation, which might play a role in the observed association between vitamin D status and respiratory tract infections. In addition, PEFR is related to physical functioning, cognitive functioning, and mortality. Third, we did not have data on fat mass, which may be a more important confounder than body weight."
The Longitudinal Aging Study Amsterdam is largely supported by a grant from The Netherlands Ministry of Health Welfare and Sports, Directorate of Long-Term Care. The authors stated that they had no relevant financial conflicts to disclose.
Low levels of serum 25-hydroxyvitamin D are associated with decreasing peak expiratory flow rate in older men but not in older women, according to results from a longitudinal Dutch study.
Although the mediating effects of muscle strength and physical performance were examined as part of the analysis, it remains unclear exactly how vitamin D impacts pulmonary function, according to Dr. N.M. van Schoor and her colleagues at VU University Medical Center, Amsterdam, the Netherlands. The report was published online in the Journal of Clinical Endocrinology and Metabolism.
"With the exception of men having serum 25-OHD levels below 10 ng/mL (in cross-sectional analyses), adding physical performance or grip strength to the model did not lead to major changes in the association between serum 25-OHD and PEFR," the researchers wrote. "Several other mechanisms have been proposed. First, in vitro studies revealed that vitamin D modulates the activity of various defense and immune cells. Second, in a mouse model, it was shown that vitamin D deficiency decreases pulmonary function. This was primarily explained by a deficit in lung volume and could not be explained by alterations in somatic growth."
For the current study, believed to be the first of its kind, Dr. van Schoor and colleagues assessed 1,509 men and women aged 65 or older as of Jan. 1, 1996, who participated in a medical interview during 1995/1996 for the Longitudinal Aging Study Amsterdam, which they described as "an ongoing multidisciplinary cohort study on predictors and consequences of changes in physical, cognitive, emotional, and social functioning in older persons" (J. Clin. Endocrinol. Metab. 2012 April 3 [doi:10.1210/jc.2011-3199]). Data on serum 25-hydroxyvitamin D (25-OHD), peak expiratory flow rate (PEFR), and covariables were available for 596 men and 611 women in the cross-sectional analysis (limited to those who underwent medical interviews during 1995/1996) and for 454 men and 496 women in the longitudinal analysis (limited to those who underwent subsequent measurements in 1998/1999).
At baseline, men had a mean serum 25-OHD of 23.5 ng/mL while the mean level for women was 19.7 ng/mL. In men, a strong correlation between vitamin D status and PEFR was seen for serum 25-OHD levels up to 20 ng/mL. "In the cross-sectional analyses, this association was no longer statistically significant for serum 25-OHD levels between 10 and 20 ng/mL in the fully adjusted model but remained statistically significant for serum 25-OHD levels below 10 ng/mL," the researchers wrote. "In the longitudinal analyses, the relationships remained statistically significant up to a serum 25-OHD level of 20 ng/mL."
Adjustment for physical performance or grip strength did not change these results in the longitudinal analyses. However, in the cross-sectional analyses, the relationship between serum 25-OHD and PEFR was no longer statistically significant after researchers added the potential mediator grip strength.
In women, significant associations between 25-OHD levels and PEFR were observed in the cross-sectional analyses, but only after adjustment for age and season of blood collection – not in the fully adjusted models or in the longitudinal analyses. "The reason for this is unclear," the researchers noted. "It may be more difficult to find a statistically significant result in women, because women showed less variation in PEFR than men. In addition, women had lower PEFR values than men, and fewer women reported obstructive airway diseases at baseline. When excluding women having obstructive airway diseases at baseline, a trend toward significance was observed after additional adjustment for physical performance and grip strength, respectively."
The investigators acknowledged certain limitations of the study, including the fact that causality "cannot be established within the setting of a cohort study, although the observed longitudinal relationship in men does support causality. Second, data on FEV1 and FVC were not available. However, we do think that PEFR is a valid outcome, because it is an effort-independent measure of expiratory flow limitation, which might play a role in the observed association between vitamin D status and respiratory tract infections. In addition, PEFR is related to physical functioning, cognitive functioning, and mortality. Third, we did not have data on fat mass, which may be a more important confounder than body weight."
The Longitudinal Aging Study Amsterdam is largely supported by a grant from The Netherlands Ministry of Health Welfare and Sports, Directorate of Long-Term Care. The authors stated that they had no relevant financial conflicts to disclose.
Low levels of serum 25-hydroxyvitamin D are associated with decreasing peak expiratory flow rate in older men but not in older women, according to results from a longitudinal Dutch study.
Although the mediating effects of muscle strength and physical performance were examined as part of the analysis, it remains unclear exactly how vitamin D impacts pulmonary function, according to Dr. N.M. van Schoor and her colleagues at VU University Medical Center, Amsterdam, the Netherlands. The report was published online in the Journal of Clinical Endocrinology and Metabolism.
"With the exception of men having serum 25-OHD levels below 10 ng/mL (in cross-sectional analyses), adding physical performance or grip strength to the model did not lead to major changes in the association between serum 25-OHD and PEFR," the researchers wrote. "Several other mechanisms have been proposed. First, in vitro studies revealed that vitamin D modulates the activity of various defense and immune cells. Second, in a mouse model, it was shown that vitamin D deficiency decreases pulmonary function. This was primarily explained by a deficit in lung volume and could not be explained by alterations in somatic growth."
For the current study, believed to be the first of its kind, Dr. van Schoor and colleagues assessed 1,509 men and women aged 65 or older as of Jan. 1, 1996, who participated in a medical interview during 1995/1996 for the Longitudinal Aging Study Amsterdam, which they described as "an ongoing multidisciplinary cohort study on predictors and consequences of changes in physical, cognitive, emotional, and social functioning in older persons" (J. Clin. Endocrinol. Metab. 2012 April 3 [doi:10.1210/jc.2011-3199]). Data on serum 25-hydroxyvitamin D (25-OHD), peak expiratory flow rate (PEFR), and covariables were available for 596 men and 611 women in the cross-sectional analysis (limited to those who underwent medical interviews during 1995/1996) and for 454 men and 496 women in the longitudinal analysis (limited to those who underwent subsequent measurements in 1998/1999).
At baseline, men had a mean serum 25-OHD of 23.5 ng/mL while the mean level for women was 19.7 ng/mL. In men, a strong correlation between vitamin D status and PEFR was seen for serum 25-OHD levels up to 20 ng/mL. "In the cross-sectional analyses, this association was no longer statistically significant for serum 25-OHD levels between 10 and 20 ng/mL in the fully adjusted model but remained statistically significant for serum 25-OHD levels below 10 ng/mL," the researchers wrote. "In the longitudinal analyses, the relationships remained statistically significant up to a serum 25-OHD level of 20 ng/mL."
Adjustment for physical performance or grip strength did not change these results in the longitudinal analyses. However, in the cross-sectional analyses, the relationship between serum 25-OHD and PEFR was no longer statistically significant after researchers added the potential mediator grip strength.
In women, significant associations between 25-OHD levels and PEFR were observed in the cross-sectional analyses, but only after adjustment for age and season of blood collection – not in the fully adjusted models or in the longitudinal analyses. "The reason for this is unclear," the researchers noted. "It may be more difficult to find a statistically significant result in women, because women showed less variation in PEFR than men. In addition, women had lower PEFR values than men, and fewer women reported obstructive airway diseases at baseline. When excluding women having obstructive airway diseases at baseline, a trend toward significance was observed after additional adjustment for physical performance and grip strength, respectively."
The investigators acknowledged certain limitations of the study, including the fact that causality "cannot be established within the setting of a cohort study, although the observed longitudinal relationship in men does support causality. Second, data on FEV1 and FVC were not available. However, we do think that PEFR is a valid outcome, because it is an effort-independent measure of expiratory flow limitation, which might play a role in the observed association between vitamin D status and respiratory tract infections. In addition, PEFR is related to physical functioning, cognitive functioning, and mortality. Third, we did not have data on fat mass, which may be a more important confounder than body weight."
The Longitudinal Aging Study Amsterdam is largely supported by a grant from The Netherlands Ministry of Health Welfare and Sports, Directorate of Long-Term Care. The authors stated that they had no relevant financial conflicts to disclose.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Major Finding: Older men who had levels of serum 25-hydroxyvitamin D (25-OHD) up to 20 ng/mL had significantly lower peak expiratory flow rates compared with their counterparts who had levels of 25-OHD above 20 ng/mL. This association was not observed in older women.
Data Source: This was a cohort of 1,509 elderly men and women in the Netherlands who participated in The Longitudinal Aging Study Amsterdam.
Disclosures: The Longitudinal Aging Study Amsterdam is largely supported by a grant from The Netherlands Ministry of Health Welfare and Sports, Directorate of Long-Term Care. The authors stated that they had no relevant financial conflicts to disclose.
Morning Stiffness in Psoriasis Patient? Think Arthritis
SAN DIEGO – When psoriasis patients present to Dr. Abrar A. Qureshi with concomitant pain or stiffness, he routinely asks, "What is your worst time of day?"
"If patients say they experience an hour or more of profound morning stiffness, think inflammatory arthritis," Dr. Qureshi said at the annual meeting of the American Academy of Dermatology. "Some patients will be stiff in the morning for 5-15 minutes. That’s more suggestive of osteoarthritis, though there is no hard and fast rule."
Dr. Qureshi of the department of dermatology at Brigham and Women’s Hospital, Boston, also asks patients about joint swelling and if they have trouble getting into a car. His recommended physical exam consists of vitals, weight, height, nail changes, inverse psoriasis, swollen joints, warm joints, "sausage" digits, and the Schober test. "We do see patients with fatigue and malaise, occasionally low grade fever, and we always ask about TB exposure," he said.
He emphasized that dermatologists "are on the front line in the care of these patients. It behooves us to think about psoriatic arthritis, because the numbers suggest that 20%-25% of patients with psoriasis may develop psoriatic arthritis. If the diagnosis is missed, this can lead to debilitating pain, permanent joint damage, and disability."
If a psoriasis patient presents with pain or stiffness, consider inflammatory arthritis, including dactylitis and spondyloarthropathy, Dr. Qureshi said. Other differential diagnoses to consider include noninflammatory arthritis (osteoarthritis) or soft tissue problems such as enthesitis. "Osteoarthritis is probably the biggest red herring for dermatologists," he said.
In a study of patients referred by rheumatologists to the department of dermatology at Brigham and Women’s Hospital, the three most common diagnoses made by the rheumatologists prior to referral were psoriatic arthritis (41%), osteoarthritis (27%), and psoriatic arthritis plus osteoarthritis (15%).
Dr. Qureshi said that he had no relevant financial conflicts to disclose.
SAN DIEGO – When psoriasis patients present to Dr. Abrar A. Qureshi with concomitant pain or stiffness, he routinely asks, "What is your worst time of day?"
"If patients say they experience an hour or more of profound morning stiffness, think inflammatory arthritis," Dr. Qureshi said at the annual meeting of the American Academy of Dermatology. "Some patients will be stiff in the morning for 5-15 minutes. That’s more suggestive of osteoarthritis, though there is no hard and fast rule."
Dr. Qureshi of the department of dermatology at Brigham and Women’s Hospital, Boston, also asks patients about joint swelling and if they have trouble getting into a car. His recommended physical exam consists of vitals, weight, height, nail changes, inverse psoriasis, swollen joints, warm joints, "sausage" digits, and the Schober test. "We do see patients with fatigue and malaise, occasionally low grade fever, and we always ask about TB exposure," he said.
He emphasized that dermatologists "are on the front line in the care of these patients. It behooves us to think about psoriatic arthritis, because the numbers suggest that 20%-25% of patients with psoriasis may develop psoriatic arthritis. If the diagnosis is missed, this can lead to debilitating pain, permanent joint damage, and disability."
If a psoriasis patient presents with pain or stiffness, consider inflammatory arthritis, including dactylitis and spondyloarthropathy, Dr. Qureshi said. Other differential diagnoses to consider include noninflammatory arthritis (osteoarthritis) or soft tissue problems such as enthesitis. "Osteoarthritis is probably the biggest red herring for dermatologists," he said.
In a study of patients referred by rheumatologists to the department of dermatology at Brigham and Women’s Hospital, the three most common diagnoses made by the rheumatologists prior to referral were psoriatic arthritis (41%), osteoarthritis (27%), and psoriatic arthritis plus osteoarthritis (15%).
Dr. Qureshi said that he had no relevant financial conflicts to disclose.
SAN DIEGO – When psoriasis patients present to Dr. Abrar A. Qureshi with concomitant pain or stiffness, he routinely asks, "What is your worst time of day?"
"If patients say they experience an hour or more of profound morning stiffness, think inflammatory arthritis," Dr. Qureshi said at the annual meeting of the American Academy of Dermatology. "Some patients will be stiff in the morning for 5-15 minutes. That’s more suggestive of osteoarthritis, though there is no hard and fast rule."
Dr. Qureshi of the department of dermatology at Brigham and Women’s Hospital, Boston, also asks patients about joint swelling and if they have trouble getting into a car. His recommended physical exam consists of vitals, weight, height, nail changes, inverse psoriasis, swollen joints, warm joints, "sausage" digits, and the Schober test. "We do see patients with fatigue and malaise, occasionally low grade fever, and we always ask about TB exposure," he said.
He emphasized that dermatologists "are on the front line in the care of these patients. It behooves us to think about psoriatic arthritis, because the numbers suggest that 20%-25% of patients with psoriasis may develop psoriatic arthritis. If the diagnosis is missed, this can lead to debilitating pain, permanent joint damage, and disability."
If a psoriasis patient presents with pain or stiffness, consider inflammatory arthritis, including dactylitis and spondyloarthropathy, Dr. Qureshi said. Other differential diagnoses to consider include noninflammatory arthritis (osteoarthritis) or soft tissue problems such as enthesitis. "Osteoarthritis is probably the biggest red herring for dermatologists," he said.
In a study of patients referred by rheumatologists to the department of dermatology at Brigham and Women’s Hospital, the three most common diagnoses made by the rheumatologists prior to referral were psoriatic arthritis (41%), osteoarthritis (27%), and psoriatic arthritis plus osteoarthritis (15%).
Dr. Qureshi said that he had no relevant financial conflicts to disclose.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF DERMATOLOGY
Botanicals on Par With Hydroquinone for Treating Melasma
SAN DIEGO – Expect botanicals to play an increasing role in the development of cosmeceuticals to treat melasma, Dr. Zoe D. Draelos said at the annual meeting of the American Academy of Dermatology.
"Combinations of kojic acid, emblica, and glycolic acid are now available in the cosmeceutical market," said Dr. Draelos, a clinical dermatologist and researcher in High Point, N.C. "This combination uses several mechanisms of pigment lightening, and clinical results are pretty much on par with hydroquinone."
Perhaps the most effective pigment-lightening agent in the over-the-counter market, she said, is kojic acid, a hydrophilic fungal derivative evolved from Acetobacter, Aspergillus, and Penicillium. Obtained from mushrooms, it inhibits tyrosinase by binding to copper. "Kojic acid is thought to be the most effective active [agent] behind hydroquinone," said Dr. Draelos, who is also a consulting professor of dermatology at Duke University in Durham, N.C.
Licorice extracts are also widely used for the treatment of melasma, particularly the licorice-derived flavonoids liquiritin and isoquercetin. "Glabridin is the most commonly used substance," Dr. Draelos said. "It is commonly combined with kojic acid and other active agents in order to create a sort of cocktail to multidimensionally inhibit pigment production."
Sometimes kojic acid and licorice extracts are combined with arbutin, which is obtained from the bearberry plant. "Interestingly enough, arbutin is very similar to glycosylated hydroquinone, and it has been used in Indian tribal medicine," she said. The most active form is deoxyarbutin, which is synthetic, inhibits tyrosinase, and has no cytotoxicity.
Soy, which interferes with melanosome transfer, is another natural substance that is being used to treat melasma. Fresh soy milk contains soybean trypsin inhibitor (STI), a polypeptide that decreases protease-activated receptor-2, a protein that is important in the regulation of pigmentation. STI reduces keratinocytes and decreases pigmentation.
The newcomer for the treatment of melasma is emblica, also known as Indian gooseberry. This substance is high in vitamin C and tannins, but also contains flavonoids, kaempferol, ellagic acid, and gallic acid. "It is thought that the tannins contained within emblica inhibit melanogenesis in human melanocyte cultures," Dr. Draelos said. "It is also a potent antioxidant."
She concluded her presentation by noting that although melasma is an important dermatologic need, "the depth of pigment is key to treatment success. Sunscreens, pharmaceuticals, cosmeceuticals, and surgical treatments may be used individually or in combination to treat melasma."
Dr. Draelos disclosed that she has received research consulting funds from Beiersdorf, L’Oréal, Neocutis, Neutrogena, Nu Skin, Procter & Gamble, and Syneron.
SAN DIEGO – Expect botanicals to play an increasing role in the development of cosmeceuticals to treat melasma, Dr. Zoe D. Draelos said at the annual meeting of the American Academy of Dermatology.
"Combinations of kojic acid, emblica, and glycolic acid are now available in the cosmeceutical market," said Dr. Draelos, a clinical dermatologist and researcher in High Point, N.C. "This combination uses several mechanisms of pigment lightening, and clinical results are pretty much on par with hydroquinone."
Perhaps the most effective pigment-lightening agent in the over-the-counter market, she said, is kojic acid, a hydrophilic fungal derivative evolved from Acetobacter, Aspergillus, and Penicillium. Obtained from mushrooms, it inhibits tyrosinase by binding to copper. "Kojic acid is thought to be the most effective active [agent] behind hydroquinone," said Dr. Draelos, who is also a consulting professor of dermatology at Duke University in Durham, N.C.
Licorice extracts are also widely used for the treatment of melasma, particularly the licorice-derived flavonoids liquiritin and isoquercetin. "Glabridin is the most commonly used substance," Dr. Draelos said. "It is commonly combined with kojic acid and other active agents in order to create a sort of cocktail to multidimensionally inhibit pigment production."
Sometimes kojic acid and licorice extracts are combined with arbutin, which is obtained from the bearberry plant. "Interestingly enough, arbutin is very similar to glycosylated hydroquinone, and it has been used in Indian tribal medicine," she said. The most active form is deoxyarbutin, which is synthetic, inhibits tyrosinase, and has no cytotoxicity.
Soy, which interferes with melanosome transfer, is another natural substance that is being used to treat melasma. Fresh soy milk contains soybean trypsin inhibitor (STI), a polypeptide that decreases protease-activated receptor-2, a protein that is important in the regulation of pigmentation. STI reduces keratinocytes and decreases pigmentation.
The newcomer for the treatment of melasma is emblica, also known as Indian gooseberry. This substance is high in vitamin C and tannins, but also contains flavonoids, kaempferol, ellagic acid, and gallic acid. "It is thought that the tannins contained within emblica inhibit melanogenesis in human melanocyte cultures," Dr. Draelos said. "It is also a potent antioxidant."
She concluded her presentation by noting that although melasma is an important dermatologic need, "the depth of pigment is key to treatment success. Sunscreens, pharmaceuticals, cosmeceuticals, and surgical treatments may be used individually or in combination to treat melasma."
Dr. Draelos disclosed that she has received research consulting funds from Beiersdorf, L’Oréal, Neocutis, Neutrogena, Nu Skin, Procter & Gamble, and Syneron.
SAN DIEGO – Expect botanicals to play an increasing role in the development of cosmeceuticals to treat melasma, Dr. Zoe D. Draelos said at the annual meeting of the American Academy of Dermatology.
"Combinations of kojic acid, emblica, and glycolic acid are now available in the cosmeceutical market," said Dr. Draelos, a clinical dermatologist and researcher in High Point, N.C. "This combination uses several mechanisms of pigment lightening, and clinical results are pretty much on par with hydroquinone."
Perhaps the most effective pigment-lightening agent in the over-the-counter market, she said, is kojic acid, a hydrophilic fungal derivative evolved from Acetobacter, Aspergillus, and Penicillium. Obtained from mushrooms, it inhibits tyrosinase by binding to copper. "Kojic acid is thought to be the most effective active [agent] behind hydroquinone," said Dr. Draelos, who is also a consulting professor of dermatology at Duke University in Durham, N.C.
Licorice extracts are also widely used for the treatment of melasma, particularly the licorice-derived flavonoids liquiritin and isoquercetin. "Glabridin is the most commonly used substance," Dr. Draelos said. "It is commonly combined with kojic acid and other active agents in order to create a sort of cocktail to multidimensionally inhibit pigment production."
Sometimes kojic acid and licorice extracts are combined with arbutin, which is obtained from the bearberry plant. "Interestingly enough, arbutin is very similar to glycosylated hydroquinone, and it has been used in Indian tribal medicine," she said. The most active form is deoxyarbutin, which is synthetic, inhibits tyrosinase, and has no cytotoxicity.
Soy, which interferes with melanosome transfer, is another natural substance that is being used to treat melasma. Fresh soy milk contains soybean trypsin inhibitor (STI), a polypeptide that decreases protease-activated receptor-2, a protein that is important in the regulation of pigmentation. STI reduces keratinocytes and decreases pigmentation.
The newcomer for the treatment of melasma is emblica, also known as Indian gooseberry. This substance is high in vitamin C and tannins, but also contains flavonoids, kaempferol, ellagic acid, and gallic acid. "It is thought that the tannins contained within emblica inhibit melanogenesis in human melanocyte cultures," Dr. Draelos said. "It is also a potent antioxidant."
She concluded her presentation by noting that although melasma is an important dermatologic need, "the depth of pigment is key to treatment success. Sunscreens, pharmaceuticals, cosmeceuticals, and surgical treatments may be used individually or in combination to treat melasma."
Dr. Draelos disclosed that she has received research consulting funds from Beiersdorf, L’Oréal, Neocutis, Neutrogena, Nu Skin, Procter & Gamble, and Syneron.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF DERMATOLOGY
Propranolol Considered Standard of Care for Infantile Hemangiomas
SAN DIEGO – There are currently no Food and Drug Administration–approved treatments for infantile hemangiomas, but propranolol appears to be the current standard of care, Dr. Alfie Krol said at the annual meeting of the American Academy of Dermatology.
Since 2008, more than 200 journal articles have been published regarding the use of propranolol for hemangiomas in children, and "initial results are excellent – not just stabilization but shrinkage of the hemangioma occurs, and overall it’s safe," said Dr. Krol, professor of dermatology and pediatrics at Oregon Health and Science University in Portland. "There are some reports of hypoglycemia, which is the most common significant side effect."
Other adverse reactions reported include disturbed sleep, cool extremities, somnolence, hyperkalemia, gastrointestinal esophageal reflux disease, and dental caries. "Overall it’s been well tolerated," Dr. Krol said. "One of the concerning potential side effects is bronchospasm in patients who have a family history of asthma. We haven’t seen that in our center, but it’s something to watch out for."
The dose range is 1-3 mg/kg per day divided b.i.d. or t.i.d. The usual target dose is 2 mg/kg per day. "We don’t know the exact length of time that you need to treat," Dr. Krol said. "In younger patients, it’s likely that 6 months is the minimum because there are reports of regrowth if you discontinue prior to 6 months of active treatment. We have seen that in our center."
Dr. Krol noted that there is currently no clear consensus as to whether to initiate propranolol on an inpatient or outpatient basis. "There are some pediatric dermatologists who admit all patients to start treatment, and they usually do a rapid escalation of the dose from 1-2 mg/kg per day over 48 hours," Dr. Krol said. "Also, some centers have cardiologists see every patient and do echocardiograms on every patient prior to starting therapy. What is clear is that all patients need vital sign monitoring, EKG, cardiac auscultation, and monitoring of vital signs after initial dosing and dose escalations for a minimum of 2 hours on initial visits until the target dose is achieved."
At Oregon Health and Science University, outpatient initiation is done in the pediatric dermatology clinic in the majority of cases, "unless it’s a life- or sight-threatening lesion," Dr. Krol said. "We start at 0.5 mg/kg per day and increase weekly to 1 mg/kg per day and then 2 mg/kg per day over 2 weeks, with appropriate monitoring at each visit."
Rebound can occur, "but certainly not in all patients," he continued. "When it does occur, it often is only partial regrowth. [Propranolol] can shrink fully grown lesions that are no longer proliferating, and there seem to be site-specific effects. Periocular and parotid lesions seem to respond exceedingly well, while nasal tip lesions seem to be less responsive. Overall this drug works very well. The initial safety seems quite good, and overall [propranolol] seems to have replaced oral steroids as the initial therapy. Our comfort level and the overall efficacy of the drug would indicate that most pediatric dermatologists are using this as first-line therapy for hemangiomas of infancy."
In the largest published study to date, researchers in Spain and Argentina conducted a multicenter trial of 71 patients who received a propranolol dose of 2 mg/kg per day for at least 12 weeks (Pediatr. Dermatol. 2011;28:108-14). They found that the effect of propranolol occurred rapidly, usually within 4 weeks. The main side effect in this study was agitated sleep, which occurred in 10 of the 71 patients (14%).
The drug also appears to work beyond the proliferation phase. In a multicenter, retrospective study, researchers from eight centers enrolled 49 patients with hemangiomas that had ceased growth or patients aged 12 months or older (Pediatr. Dermatol.2011;28:94-8). A visual analog scale (VAS) of photographs was used to determine improvement.
The duration of therapy ranged from 1 to 8 months, for a mean of 3.6 months. The VAS score was reduced from 6.8 to 2.6. No significant side effects were reported, and the researchers concluded that propranolol is effective in treating hemangiomas in the postproliferative phase and should be considered first-line therapy in that setting.
In another published study conducted at the University of Miami and Miami Children’s Hospital, researchers compared the use of propranolol with corticosteroids in 110 patients with infantile hemangiomas (Arch. Dermatol. 2011;147:1371-6). They found that 82% of patients in the propranolol group improved by 75% or more, compared with 29% of patients in the steroid group. "That’s a significant improvement over the use of steroids alone," Dr. Krol commented.
One patient on propranolol had hypoglycemia, but all patients in the steroid group had at least one adverse event. The researchers also found propranolol therapy was about half the cost of steroid therapy ($205 for 7.9 months vs. $416 for 5.2 months, respectively). They concluded that propranolol should be considered a first-line therapy for infantile hemangiomas.
He said that larger, long-term studies "are needed to identify any potentially serious as well as long-term safety questions."
Dr. Krol disclosed that he is a paid investigator for Pierre Fabre.
SAN DIEGO – There are currently no Food and Drug Administration–approved treatments for infantile hemangiomas, but propranolol appears to be the current standard of care, Dr. Alfie Krol said at the annual meeting of the American Academy of Dermatology.
Since 2008, more than 200 journal articles have been published regarding the use of propranolol for hemangiomas in children, and "initial results are excellent – not just stabilization but shrinkage of the hemangioma occurs, and overall it’s safe," said Dr. Krol, professor of dermatology and pediatrics at Oregon Health and Science University in Portland. "There are some reports of hypoglycemia, which is the most common significant side effect."
Other adverse reactions reported include disturbed sleep, cool extremities, somnolence, hyperkalemia, gastrointestinal esophageal reflux disease, and dental caries. "Overall it’s been well tolerated," Dr. Krol said. "One of the concerning potential side effects is bronchospasm in patients who have a family history of asthma. We haven’t seen that in our center, but it’s something to watch out for."
The dose range is 1-3 mg/kg per day divided b.i.d. or t.i.d. The usual target dose is 2 mg/kg per day. "We don’t know the exact length of time that you need to treat," Dr. Krol said. "In younger patients, it’s likely that 6 months is the minimum because there are reports of regrowth if you discontinue prior to 6 months of active treatment. We have seen that in our center."
Dr. Krol noted that there is currently no clear consensus as to whether to initiate propranolol on an inpatient or outpatient basis. "There are some pediatric dermatologists who admit all patients to start treatment, and they usually do a rapid escalation of the dose from 1-2 mg/kg per day over 48 hours," Dr. Krol said. "Also, some centers have cardiologists see every patient and do echocardiograms on every patient prior to starting therapy. What is clear is that all patients need vital sign monitoring, EKG, cardiac auscultation, and monitoring of vital signs after initial dosing and dose escalations for a minimum of 2 hours on initial visits until the target dose is achieved."
At Oregon Health and Science University, outpatient initiation is done in the pediatric dermatology clinic in the majority of cases, "unless it’s a life- or sight-threatening lesion," Dr. Krol said. "We start at 0.5 mg/kg per day and increase weekly to 1 mg/kg per day and then 2 mg/kg per day over 2 weeks, with appropriate monitoring at each visit."
Rebound can occur, "but certainly not in all patients," he continued. "When it does occur, it often is only partial regrowth. [Propranolol] can shrink fully grown lesions that are no longer proliferating, and there seem to be site-specific effects. Periocular and parotid lesions seem to respond exceedingly well, while nasal tip lesions seem to be less responsive. Overall this drug works very well. The initial safety seems quite good, and overall [propranolol] seems to have replaced oral steroids as the initial therapy. Our comfort level and the overall efficacy of the drug would indicate that most pediatric dermatologists are using this as first-line therapy for hemangiomas of infancy."
In the largest published study to date, researchers in Spain and Argentina conducted a multicenter trial of 71 patients who received a propranolol dose of 2 mg/kg per day for at least 12 weeks (Pediatr. Dermatol. 2011;28:108-14). They found that the effect of propranolol occurred rapidly, usually within 4 weeks. The main side effect in this study was agitated sleep, which occurred in 10 of the 71 patients (14%).
The drug also appears to work beyond the proliferation phase. In a multicenter, retrospective study, researchers from eight centers enrolled 49 patients with hemangiomas that had ceased growth or patients aged 12 months or older (Pediatr. Dermatol.2011;28:94-8). A visual analog scale (VAS) of photographs was used to determine improvement.
The duration of therapy ranged from 1 to 8 months, for a mean of 3.6 months. The VAS score was reduced from 6.8 to 2.6. No significant side effects were reported, and the researchers concluded that propranolol is effective in treating hemangiomas in the postproliferative phase and should be considered first-line therapy in that setting.
In another published study conducted at the University of Miami and Miami Children’s Hospital, researchers compared the use of propranolol with corticosteroids in 110 patients with infantile hemangiomas (Arch. Dermatol. 2011;147:1371-6). They found that 82% of patients in the propranolol group improved by 75% or more, compared with 29% of patients in the steroid group. "That’s a significant improvement over the use of steroids alone," Dr. Krol commented.
One patient on propranolol had hypoglycemia, but all patients in the steroid group had at least one adverse event. The researchers also found propranolol therapy was about half the cost of steroid therapy ($205 for 7.9 months vs. $416 for 5.2 months, respectively). They concluded that propranolol should be considered a first-line therapy for infantile hemangiomas.
He said that larger, long-term studies "are needed to identify any potentially serious as well as long-term safety questions."
Dr. Krol disclosed that he is a paid investigator for Pierre Fabre.
SAN DIEGO – There are currently no Food and Drug Administration–approved treatments for infantile hemangiomas, but propranolol appears to be the current standard of care, Dr. Alfie Krol said at the annual meeting of the American Academy of Dermatology.
Since 2008, more than 200 journal articles have been published regarding the use of propranolol for hemangiomas in children, and "initial results are excellent – not just stabilization but shrinkage of the hemangioma occurs, and overall it’s safe," said Dr. Krol, professor of dermatology and pediatrics at Oregon Health and Science University in Portland. "There are some reports of hypoglycemia, which is the most common significant side effect."
Other adverse reactions reported include disturbed sleep, cool extremities, somnolence, hyperkalemia, gastrointestinal esophageal reflux disease, and dental caries. "Overall it’s been well tolerated," Dr. Krol said. "One of the concerning potential side effects is bronchospasm in patients who have a family history of asthma. We haven’t seen that in our center, but it’s something to watch out for."
The dose range is 1-3 mg/kg per day divided b.i.d. or t.i.d. The usual target dose is 2 mg/kg per day. "We don’t know the exact length of time that you need to treat," Dr. Krol said. "In younger patients, it’s likely that 6 months is the minimum because there are reports of regrowth if you discontinue prior to 6 months of active treatment. We have seen that in our center."
Dr. Krol noted that there is currently no clear consensus as to whether to initiate propranolol on an inpatient or outpatient basis. "There are some pediatric dermatologists who admit all patients to start treatment, and they usually do a rapid escalation of the dose from 1-2 mg/kg per day over 48 hours," Dr. Krol said. "Also, some centers have cardiologists see every patient and do echocardiograms on every patient prior to starting therapy. What is clear is that all patients need vital sign monitoring, EKG, cardiac auscultation, and monitoring of vital signs after initial dosing and dose escalations for a minimum of 2 hours on initial visits until the target dose is achieved."
At Oregon Health and Science University, outpatient initiation is done in the pediatric dermatology clinic in the majority of cases, "unless it’s a life- or sight-threatening lesion," Dr. Krol said. "We start at 0.5 mg/kg per day and increase weekly to 1 mg/kg per day and then 2 mg/kg per day over 2 weeks, with appropriate monitoring at each visit."
Rebound can occur, "but certainly not in all patients," he continued. "When it does occur, it often is only partial regrowth. [Propranolol] can shrink fully grown lesions that are no longer proliferating, and there seem to be site-specific effects. Periocular and parotid lesions seem to respond exceedingly well, while nasal tip lesions seem to be less responsive. Overall this drug works very well. The initial safety seems quite good, and overall [propranolol] seems to have replaced oral steroids as the initial therapy. Our comfort level and the overall efficacy of the drug would indicate that most pediatric dermatologists are using this as first-line therapy for hemangiomas of infancy."
In the largest published study to date, researchers in Spain and Argentina conducted a multicenter trial of 71 patients who received a propranolol dose of 2 mg/kg per day for at least 12 weeks (Pediatr. Dermatol. 2011;28:108-14). They found that the effect of propranolol occurred rapidly, usually within 4 weeks. The main side effect in this study was agitated sleep, which occurred in 10 of the 71 patients (14%).
The drug also appears to work beyond the proliferation phase. In a multicenter, retrospective study, researchers from eight centers enrolled 49 patients with hemangiomas that had ceased growth or patients aged 12 months or older (Pediatr. Dermatol.2011;28:94-8). A visual analog scale (VAS) of photographs was used to determine improvement.
The duration of therapy ranged from 1 to 8 months, for a mean of 3.6 months. The VAS score was reduced from 6.8 to 2.6. No significant side effects were reported, and the researchers concluded that propranolol is effective in treating hemangiomas in the postproliferative phase and should be considered first-line therapy in that setting.
In another published study conducted at the University of Miami and Miami Children’s Hospital, researchers compared the use of propranolol with corticosteroids in 110 patients with infantile hemangiomas (Arch. Dermatol. 2011;147:1371-6). They found that 82% of patients in the propranolol group improved by 75% or more, compared with 29% of patients in the steroid group. "That’s a significant improvement over the use of steroids alone," Dr. Krol commented.
One patient on propranolol had hypoglycemia, but all patients in the steroid group had at least one adverse event. The researchers also found propranolol therapy was about half the cost of steroid therapy ($205 for 7.9 months vs. $416 for 5.2 months, respectively). They concluded that propranolol should be considered a first-line therapy for infantile hemangiomas.
He said that larger, long-term studies "are needed to identify any potentially serious as well as long-term safety questions."
Dr. Krol disclosed that he is a paid investigator for Pierre Fabre.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF DERMATOLOGY