User login
Novel text-messaging program boosts ADHD treatment adherence
An innovative text-messaging program that reminds patients with attention-deficit/hyperactivity disorder to take their medication and warns them about the hazards of noncompliance significantly increases treatment adherence in children and adults, new research suggests.
In a pediatric study, 85% of participants who received a text message had their prescriptions refilled in a timely manner, compared with 62% of those who received treatment as usual and no text messaging. In a second study of adults, 81% of the group that received a text message refilled their prescriptions, versus 36% of those in the usual-treatment group.
“Patients are not going to be fully compliant if they do not understand what the implications are if they do not take their pills,” lead author Joseph Biederman, MD, chief of clinical and research programs in pediatric psychopharmacology and adult ADHD at the Massachusetts General Hospital and professor of psychiatry at Harvard Medical School, Boston, told this news organization.
He noted that the text-messaging program also provides information, support, encouragement, and guidance.
“We remind them to get in touch with their prescriber as renewals come due, and if they tell us no, we tell them how important it is” to do so, Dr. Biederman said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 annual meeting.
Poor adherence
“Adherence to medications for ADHD is extremely poor, among the worst in medicine, despite the fact that ADHD is very morbid and we have excellent treatments people can take,” Dr. Biederman noted. “That’s the first tragedy, and it is totally unappreciated.”
He added that when patients require multiple prescriptions, he said.
Another contributor to medication nonadherence is the ongoing prejudice or stigma associated with ADHD, said Dr. Biederman.
“There is bad press about ADHD. There are no good comments, only disaster, doom and gloom, catastrophe, and so on. All people read in the available media are bad things about ADHD, and that only adds to stigma and misinformation,” he noted.
To combat these factors, Dr. Biederman and his team conducted two studies on the effectiveness of a novel ADHD-centric intervention based on text messaging.
One study included 87 children aged 6-12 years, and the other included 117 adults aged 18-55 years. Both groups were from primary care settings and were prescribed a stimulant medication for the treatment of ADHD.
As comparators, the researchers used age- and sex-matched pediatric patients and age-, race-, and sex-matched adult patients from the same primary care settings. They had also been prescribed stimulants but had not received the text messaging intervention.
Timely reminders
Results showed that 85% of the children who received text messages refilled their prescriptions vs. 65% of those who did not get the intervention (odds ratio, 3.46; 95% confidence interval, 1.82-6.58; P < .001).
Among adults, 81% of the intervention group refilled their prescriptions vs. 36% of the comparator group (OR, 7.54; 95% CI, 4.46-12.77; P < .001).
“In the number-needed-to-treat analysis, for every five pediatric patients who receive text messaging, we can keep one adherent with stimulant medication. In adults, that is one in every three who receive the text-messaging intervention,” Dr. Biederman said.
Text messaging reminds patients with ADHD to take their medications as prescribed, and it also reminds them of the consequences of not taking their medications, he added.
In another study presented at the ASCP meeting, Dr. Biederman introduced a new tool to help clinicians determine whether a patient with ADHD also has deficient emotional self-regulation (DESR).
ADHD has been associated with low frustration tolerance, impatience, and quickness to anger, he noted.
Emotional dysregulation, however, “is not a mood disorder,” said Dr. Biederman. “Some people use the term ‘hot tempered.’ These are people who overreact to things, and this is associated with a wide range of difficulties.”
Clinical guidance
The investigators operationalized DESR using the eight-item Emotional Dysregulation (ED) subscale of the Barkley Current Behavior Scale. They then used receiver operating characteristic curves to identify the optimal cutoff on the Barkley ED Scale that would categorize patients as having high- vs. low-level DESR.
“We wanted to give some guidance to clinicians, using a very simple rating scale that was developed by Dr. Barkley. It is one we think configures this syndrome of emotional dysregulation and emotional impulsivity,” Dr. Biederman said.
The study included 441 newly referred 18- to 55-year-old men and women who met DSM-5 diagnostic criteria for ADHD.
Using a cutoff score of 8 to represent high levels of DESR, the researchers identified 191 adults as having high-level DESR and the rest as having low-level DESR.
Those with high-level DESR had significantly more severe symptoms of ADHD, executive dysfunction, autistic traits, levels of psychopathology, and worse quality of life, compared with those with low-level DESR.
The problem of emotional dysregulation in ADHD is widespread and affects many people, Dr. Biederman noted.
“If you take 5% of adults at a minimum and 10% of children with ADHD [and] if 50% of those have emotional dysregulation, we’re talking about millions of people. And it is very morbid,” he said. “Having emotional dysregulation problems will get you in hot water.”
Promising results
Commenting on the findings for this news organization, Ira D. Glick, MD, professor emeritus of psychiatry and behavioral sciences, Stanford (Calif.) University, said the new studies are important.
He noted that, although ADHD has become more accepted as a “disease of the brain” over the past 20 years, patients with the disorder and their families often are not accepting of the diagnosis.
“Instead, they try to downplay it. They say this is just a ploy by psychiatrists to get business or this is just normal boys’ behavior, [and] they don’t need medicines,” said Dr. Glick, who was not involved in the current research.
“Biederman is trying to make clear that ADHD is a brain disease, and DESR symptoms are cardinal signs of a brain illness,” he said.
Dr. Glick also agreed that text messaging could be very useful for these patients.
“Text messaging might be helpful, especially in this population which can often be disorganized or forgetful. The results of that study were very promising,” he said.
Dr. Biederman is in the process of commercializing the text program used in the study. Dr. Glick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An innovative text-messaging program that reminds patients with attention-deficit/hyperactivity disorder to take their medication and warns them about the hazards of noncompliance significantly increases treatment adherence in children and adults, new research suggests.
In a pediatric study, 85% of participants who received a text message had their prescriptions refilled in a timely manner, compared with 62% of those who received treatment as usual and no text messaging. In a second study of adults, 81% of the group that received a text message refilled their prescriptions, versus 36% of those in the usual-treatment group.
“Patients are not going to be fully compliant if they do not understand what the implications are if they do not take their pills,” lead author Joseph Biederman, MD, chief of clinical and research programs in pediatric psychopharmacology and adult ADHD at the Massachusetts General Hospital and professor of psychiatry at Harvard Medical School, Boston, told this news organization.
He noted that the text-messaging program also provides information, support, encouragement, and guidance.
“We remind them to get in touch with their prescriber as renewals come due, and if they tell us no, we tell them how important it is” to do so, Dr. Biederman said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 annual meeting.
Poor adherence
“Adherence to medications for ADHD is extremely poor, among the worst in medicine, despite the fact that ADHD is very morbid and we have excellent treatments people can take,” Dr. Biederman noted. “That’s the first tragedy, and it is totally unappreciated.”
He added that when patients require multiple prescriptions, he said.
Another contributor to medication nonadherence is the ongoing prejudice or stigma associated with ADHD, said Dr. Biederman.
“There is bad press about ADHD. There are no good comments, only disaster, doom and gloom, catastrophe, and so on. All people read in the available media are bad things about ADHD, and that only adds to stigma and misinformation,” he noted.
To combat these factors, Dr. Biederman and his team conducted two studies on the effectiveness of a novel ADHD-centric intervention based on text messaging.
One study included 87 children aged 6-12 years, and the other included 117 adults aged 18-55 years. Both groups were from primary care settings and were prescribed a stimulant medication for the treatment of ADHD.
As comparators, the researchers used age- and sex-matched pediatric patients and age-, race-, and sex-matched adult patients from the same primary care settings. They had also been prescribed stimulants but had not received the text messaging intervention.
Timely reminders
Results showed that 85% of the children who received text messages refilled their prescriptions vs. 65% of those who did not get the intervention (odds ratio, 3.46; 95% confidence interval, 1.82-6.58; P < .001).
Among adults, 81% of the intervention group refilled their prescriptions vs. 36% of the comparator group (OR, 7.54; 95% CI, 4.46-12.77; P < .001).
“In the number-needed-to-treat analysis, for every five pediatric patients who receive text messaging, we can keep one adherent with stimulant medication. In adults, that is one in every three who receive the text-messaging intervention,” Dr. Biederman said.
Text messaging reminds patients with ADHD to take their medications as prescribed, and it also reminds them of the consequences of not taking their medications, he added.
In another study presented at the ASCP meeting, Dr. Biederman introduced a new tool to help clinicians determine whether a patient with ADHD also has deficient emotional self-regulation (DESR).
ADHD has been associated with low frustration tolerance, impatience, and quickness to anger, he noted.
Emotional dysregulation, however, “is not a mood disorder,” said Dr. Biederman. “Some people use the term ‘hot tempered.’ These are people who overreact to things, and this is associated with a wide range of difficulties.”
Clinical guidance
The investigators operationalized DESR using the eight-item Emotional Dysregulation (ED) subscale of the Barkley Current Behavior Scale. They then used receiver operating characteristic curves to identify the optimal cutoff on the Barkley ED Scale that would categorize patients as having high- vs. low-level DESR.
“We wanted to give some guidance to clinicians, using a very simple rating scale that was developed by Dr. Barkley. It is one we think configures this syndrome of emotional dysregulation and emotional impulsivity,” Dr. Biederman said.
The study included 441 newly referred 18- to 55-year-old men and women who met DSM-5 diagnostic criteria for ADHD.
Using a cutoff score of 8 to represent high levels of DESR, the researchers identified 191 adults as having high-level DESR and the rest as having low-level DESR.
Those with high-level DESR had significantly more severe symptoms of ADHD, executive dysfunction, autistic traits, levels of psychopathology, and worse quality of life, compared with those with low-level DESR.
The problem of emotional dysregulation in ADHD is widespread and affects many people, Dr. Biederman noted.
“If you take 5% of adults at a minimum and 10% of children with ADHD [and] if 50% of those have emotional dysregulation, we’re talking about millions of people. And it is very morbid,” he said. “Having emotional dysregulation problems will get you in hot water.”
Promising results
Commenting on the findings for this news organization, Ira D. Glick, MD, professor emeritus of psychiatry and behavioral sciences, Stanford (Calif.) University, said the new studies are important.
He noted that, although ADHD has become more accepted as a “disease of the brain” over the past 20 years, patients with the disorder and their families often are not accepting of the diagnosis.
“Instead, they try to downplay it. They say this is just a ploy by psychiatrists to get business or this is just normal boys’ behavior, [and] they don’t need medicines,” said Dr. Glick, who was not involved in the current research.
“Biederman is trying to make clear that ADHD is a brain disease, and DESR symptoms are cardinal signs of a brain illness,” he said.
Dr. Glick also agreed that text messaging could be very useful for these patients.
“Text messaging might be helpful, especially in this population which can often be disorganized or forgetful. The results of that study were very promising,” he said.
Dr. Biederman is in the process of commercializing the text program used in the study. Dr. Glick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An innovative text-messaging program that reminds patients with attention-deficit/hyperactivity disorder to take their medication and warns them about the hazards of noncompliance significantly increases treatment adherence in children and adults, new research suggests.
In a pediatric study, 85% of participants who received a text message had their prescriptions refilled in a timely manner, compared with 62% of those who received treatment as usual and no text messaging. In a second study of adults, 81% of the group that received a text message refilled their prescriptions, versus 36% of those in the usual-treatment group.
“Patients are not going to be fully compliant if they do not understand what the implications are if they do not take their pills,” lead author Joseph Biederman, MD, chief of clinical and research programs in pediatric psychopharmacology and adult ADHD at the Massachusetts General Hospital and professor of psychiatry at Harvard Medical School, Boston, told this news organization.
He noted that the text-messaging program also provides information, support, encouragement, and guidance.
“We remind them to get in touch with their prescriber as renewals come due, and if they tell us no, we tell them how important it is” to do so, Dr. Biederman said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 annual meeting.
Poor adherence
“Adherence to medications for ADHD is extremely poor, among the worst in medicine, despite the fact that ADHD is very morbid and we have excellent treatments people can take,” Dr. Biederman noted. “That’s the first tragedy, and it is totally unappreciated.”
He added that when patients require multiple prescriptions, he said.
Another contributor to medication nonadherence is the ongoing prejudice or stigma associated with ADHD, said Dr. Biederman.
“There is bad press about ADHD. There are no good comments, only disaster, doom and gloom, catastrophe, and so on. All people read in the available media are bad things about ADHD, and that only adds to stigma and misinformation,” he noted.
To combat these factors, Dr. Biederman and his team conducted two studies on the effectiveness of a novel ADHD-centric intervention based on text messaging.
One study included 87 children aged 6-12 years, and the other included 117 adults aged 18-55 years. Both groups were from primary care settings and were prescribed a stimulant medication for the treatment of ADHD.
As comparators, the researchers used age- and sex-matched pediatric patients and age-, race-, and sex-matched adult patients from the same primary care settings. They had also been prescribed stimulants but had not received the text messaging intervention.
Timely reminders
Results showed that 85% of the children who received text messages refilled their prescriptions vs. 65% of those who did not get the intervention (odds ratio, 3.46; 95% confidence interval, 1.82-6.58; P < .001).
Among adults, 81% of the intervention group refilled their prescriptions vs. 36% of the comparator group (OR, 7.54; 95% CI, 4.46-12.77; P < .001).
“In the number-needed-to-treat analysis, for every five pediatric patients who receive text messaging, we can keep one adherent with stimulant medication. In adults, that is one in every three who receive the text-messaging intervention,” Dr. Biederman said.
Text messaging reminds patients with ADHD to take their medications as prescribed, and it also reminds them of the consequences of not taking their medications, he added.
In another study presented at the ASCP meeting, Dr. Biederman introduced a new tool to help clinicians determine whether a patient with ADHD also has deficient emotional self-regulation (DESR).
ADHD has been associated with low frustration tolerance, impatience, and quickness to anger, he noted.
Emotional dysregulation, however, “is not a mood disorder,” said Dr. Biederman. “Some people use the term ‘hot tempered.’ These are people who overreact to things, and this is associated with a wide range of difficulties.”
Clinical guidance
The investigators operationalized DESR using the eight-item Emotional Dysregulation (ED) subscale of the Barkley Current Behavior Scale. They then used receiver operating characteristic curves to identify the optimal cutoff on the Barkley ED Scale that would categorize patients as having high- vs. low-level DESR.
“We wanted to give some guidance to clinicians, using a very simple rating scale that was developed by Dr. Barkley. It is one we think configures this syndrome of emotional dysregulation and emotional impulsivity,” Dr. Biederman said.
The study included 441 newly referred 18- to 55-year-old men and women who met DSM-5 diagnostic criteria for ADHD.
Using a cutoff score of 8 to represent high levels of DESR, the researchers identified 191 adults as having high-level DESR and the rest as having low-level DESR.
Those with high-level DESR had significantly more severe symptoms of ADHD, executive dysfunction, autistic traits, levels of psychopathology, and worse quality of life, compared with those with low-level DESR.
The problem of emotional dysregulation in ADHD is widespread and affects many people, Dr. Biederman noted.
“If you take 5% of adults at a minimum and 10% of children with ADHD [and] if 50% of those have emotional dysregulation, we’re talking about millions of people. And it is very morbid,” he said. “Having emotional dysregulation problems will get you in hot water.”
Promising results
Commenting on the findings for this news organization, Ira D. Glick, MD, professor emeritus of psychiatry and behavioral sciences, Stanford (Calif.) University, said the new studies are important.
He noted that, although ADHD has become more accepted as a “disease of the brain” over the past 20 years, patients with the disorder and their families often are not accepting of the diagnosis.
“Instead, they try to downplay it. They say this is just a ploy by psychiatrists to get business or this is just normal boys’ behavior, [and] they don’t need medicines,” said Dr. Glick, who was not involved in the current research.
“Biederman is trying to make clear that ADHD is a brain disease, and DESR symptoms are cardinal signs of a brain illness,” he said.
Dr. Glick also agreed that text messaging could be very useful for these patients.
“Text messaging might be helpful, especially in this population which can often be disorganized or forgetful. The results of that study were very promising,” he said.
Dr. Biederman is in the process of commercializing the text program used in the study. Dr. Glick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Subclinical myocarditis found in some athletes post COVID
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Pericardial fat an independent risk factor for heart failure
Pericardial fat is associated with a heightened risk for heart failure, particularly in women, new research suggests.
In a prospective cohort study of nearly 7,000 individuals, excess pericardial fat was linked to a higher risk for heart failure, even after adjustment for established risk factors for heart failure.
Women with high pericardial fat volume (PFV), defined as more than 70 cm3 or 2.4 fluid ounces, had double the risk of developing heart failure. For men, high PFV, defined as more than 120 cm3 or 4.0 fluid ounces, was associated with a 50% increase in the risk for heart failure.
The findings were published in the Journal of the American College of Cardiology.
“People will ask why should they measure fat around the heart. Why can’t they just take the waist circumference or body mass index as a measure for increased risk?” lead author Satish Kenchaiah, MD, MPH, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“Yet, when we adjusted for waist circumference, hip circumference, waist to hip ratio, and other known variables, pericardial fat was still associated with an increased risk of heart failure. This tells me that it is not just overall fat in the body but something about its location around the heart that is playing a role,” Dr. Kenchaiah said.
“Now that we have found an association between any amount of fat around the pericardium and heart failure, it gives us an impetus to build future research on identifying how exactly these fat deposits influence the development of cardiomyopathy,” he said.
Dr. Kenchaiah and colleagues investigated the association of pericardial fat with incident heart failure by examining chest CT scans from 6,785 participants (3,584 women and 3,201 men aged 45-84 years) in the Multi-Ethnic Study of Atherosclerosis.
The participants were from four different ethnic groups: 38% were White; 28% were Black, 22% were Hispanic, and 12% were Chinese American. They were recruited between July 17, 2000, and Aug. 31, 2002, from six communities in the United States: Baltimore and Baltimore County; Chicago; Forsyth County, N.C.; Los Angeles County northern Manhattan and the Bronx, New York; and St. Paul, Minn.
All participants were free of cardiovascular disease at baseline.
The researchers followed participants for more than 17 years. During this time, 385 (5.7%; 164 women and 221 men) developed newly diagnosed heart failure.
In women, the hazard ratio for every 42 cm3 increase in PFV was 1.44 (95% confidence interval, 1.21-1.71; P < .001). In men, the HR was 1.13 (95% CI, 1.01-1.27; P = .03).
High PVF conferred a twofold greater risk for heart failure in women (HR, 2.06; 95% CI, 1.48-2.87; P < .001) and a 53% higher risk in men (HR, 1.53; 95% CI, 1.13-2.07; P = .006).
These associations remained significant after further adjustment for circulating markers of systemic inflammation (that is, C-reactive protein and interleukin-6), and abdominal subcutaneous or visceral fat.
They also found that the heightened risk persisted, even after adjustment for established risk factors for heart failure, such as age, cigarette smoking, alcohol consumption, sedentary lifestyle, high blood pressure, high blood sugar, high cholesterol, and myocardial infarction.
Results were similar among all of the ethnic groups studied.
A surprise finding
“The most surprising part of this study was that the risk for heart failure with increased pericardial fat does not seem to be explained by obesity and systemic inflammation alone,” Andreas P. Kalogeropoulos, MD, MPH, PhD, Stony Brook (N.Y.) University, said in an interview.
“If pericardial fat was merely a proxy for increased visceral fat, one would expect the association of pericardial fat with heart failure risk to go away after factoring in abdominal CT findings, which was not the case here. Also, accounting for inflammatory markers did not change things dramatically. However, we need to be careful here, as abdominal CT scans have not been done simultaneously with the pericardial fat scans in the study,” said Dr. Kalogeropoulos, who coauthored an accompanying editorial with Michael E. Hall, MD, University of Mississippi Medical Center, Jackson.
The other striking finding, although not entirely surprising, was the stronger association of pericardial fat with heart failure risk in women, he noted.
“Although several clues have been reported pointing to women being more sensitive to the adverse cardiac effects of pericardial fat, this is the first large prospective study to connect the dots and show much higher risk in women in a convincing way. For the record, this is the first prospective study to show the connection between pericardial fat and heart failure risk altogether,” Dr. Kalogeropoulos said.
“Obviously, we need to do more work to see how we can use the important findings of Kenchaiah and colleagues to reduce risk for heart failure among patients with increased pericardial fat, especially women. For starters, we would need a way to identify these patients,” he said. “In this aspect, it is encouraging that pericardial fat can be measured in low-radiation CT scans, similar to those used for coronary calcium, and that automation technology to speed up pericardial fat measurements is already in the pipeline.
“The next step would be to see what kind of interventions would reduce risk for heart failure in these patients,” he added. “Weight loss would be an obvious thing, but novel agents with favorable cardiometabolic effects, like newer antidiabetic medications, are intriguing options, too.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr. Kenchaiah and Dr. Kalogeropoulos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pericardial fat is associated with a heightened risk for heart failure, particularly in women, new research suggests.
In a prospective cohort study of nearly 7,000 individuals, excess pericardial fat was linked to a higher risk for heart failure, even after adjustment for established risk factors for heart failure.
Women with high pericardial fat volume (PFV), defined as more than 70 cm3 or 2.4 fluid ounces, had double the risk of developing heart failure. For men, high PFV, defined as more than 120 cm3 or 4.0 fluid ounces, was associated with a 50% increase in the risk for heart failure.
The findings were published in the Journal of the American College of Cardiology.
“People will ask why should they measure fat around the heart. Why can’t they just take the waist circumference or body mass index as a measure for increased risk?” lead author Satish Kenchaiah, MD, MPH, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“Yet, when we adjusted for waist circumference, hip circumference, waist to hip ratio, and other known variables, pericardial fat was still associated with an increased risk of heart failure. This tells me that it is not just overall fat in the body but something about its location around the heart that is playing a role,” Dr. Kenchaiah said.
“Now that we have found an association between any amount of fat around the pericardium and heart failure, it gives us an impetus to build future research on identifying how exactly these fat deposits influence the development of cardiomyopathy,” he said.
Dr. Kenchaiah and colleagues investigated the association of pericardial fat with incident heart failure by examining chest CT scans from 6,785 participants (3,584 women and 3,201 men aged 45-84 years) in the Multi-Ethnic Study of Atherosclerosis.
The participants were from four different ethnic groups: 38% were White; 28% were Black, 22% were Hispanic, and 12% were Chinese American. They were recruited between July 17, 2000, and Aug. 31, 2002, from six communities in the United States: Baltimore and Baltimore County; Chicago; Forsyth County, N.C.; Los Angeles County northern Manhattan and the Bronx, New York; and St. Paul, Minn.
All participants were free of cardiovascular disease at baseline.
The researchers followed participants for more than 17 years. During this time, 385 (5.7%; 164 women and 221 men) developed newly diagnosed heart failure.
In women, the hazard ratio for every 42 cm3 increase in PFV was 1.44 (95% confidence interval, 1.21-1.71; P < .001). In men, the HR was 1.13 (95% CI, 1.01-1.27; P = .03).
High PVF conferred a twofold greater risk for heart failure in women (HR, 2.06; 95% CI, 1.48-2.87; P < .001) and a 53% higher risk in men (HR, 1.53; 95% CI, 1.13-2.07; P = .006).
These associations remained significant after further adjustment for circulating markers of systemic inflammation (that is, C-reactive protein and interleukin-6), and abdominal subcutaneous or visceral fat.
They also found that the heightened risk persisted, even after adjustment for established risk factors for heart failure, such as age, cigarette smoking, alcohol consumption, sedentary lifestyle, high blood pressure, high blood sugar, high cholesterol, and myocardial infarction.
Results were similar among all of the ethnic groups studied.
A surprise finding
“The most surprising part of this study was that the risk for heart failure with increased pericardial fat does not seem to be explained by obesity and systemic inflammation alone,” Andreas P. Kalogeropoulos, MD, MPH, PhD, Stony Brook (N.Y.) University, said in an interview.
“If pericardial fat was merely a proxy for increased visceral fat, one would expect the association of pericardial fat with heart failure risk to go away after factoring in abdominal CT findings, which was not the case here. Also, accounting for inflammatory markers did not change things dramatically. However, we need to be careful here, as abdominal CT scans have not been done simultaneously with the pericardial fat scans in the study,” said Dr. Kalogeropoulos, who coauthored an accompanying editorial with Michael E. Hall, MD, University of Mississippi Medical Center, Jackson.
The other striking finding, although not entirely surprising, was the stronger association of pericardial fat with heart failure risk in women, he noted.
“Although several clues have been reported pointing to women being more sensitive to the adverse cardiac effects of pericardial fat, this is the first large prospective study to connect the dots and show much higher risk in women in a convincing way. For the record, this is the first prospective study to show the connection between pericardial fat and heart failure risk altogether,” Dr. Kalogeropoulos said.
“Obviously, we need to do more work to see how we can use the important findings of Kenchaiah and colleagues to reduce risk for heart failure among patients with increased pericardial fat, especially women. For starters, we would need a way to identify these patients,” he said. “In this aspect, it is encouraging that pericardial fat can be measured in low-radiation CT scans, similar to those used for coronary calcium, and that automation technology to speed up pericardial fat measurements is already in the pipeline.
“The next step would be to see what kind of interventions would reduce risk for heart failure in these patients,” he added. “Weight loss would be an obvious thing, but novel agents with favorable cardiometabolic effects, like newer antidiabetic medications, are intriguing options, too.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr. Kenchaiah and Dr. Kalogeropoulos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pericardial fat is associated with a heightened risk for heart failure, particularly in women, new research suggests.
In a prospective cohort study of nearly 7,000 individuals, excess pericardial fat was linked to a higher risk for heart failure, even after adjustment for established risk factors for heart failure.
Women with high pericardial fat volume (PFV), defined as more than 70 cm3 or 2.4 fluid ounces, had double the risk of developing heart failure. For men, high PFV, defined as more than 120 cm3 or 4.0 fluid ounces, was associated with a 50% increase in the risk for heart failure.
The findings were published in the Journal of the American College of Cardiology.
“People will ask why should they measure fat around the heart. Why can’t they just take the waist circumference or body mass index as a measure for increased risk?” lead author Satish Kenchaiah, MD, MPH, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“Yet, when we adjusted for waist circumference, hip circumference, waist to hip ratio, and other known variables, pericardial fat was still associated with an increased risk of heart failure. This tells me that it is not just overall fat in the body but something about its location around the heart that is playing a role,” Dr. Kenchaiah said.
“Now that we have found an association between any amount of fat around the pericardium and heart failure, it gives us an impetus to build future research on identifying how exactly these fat deposits influence the development of cardiomyopathy,” he said.
Dr. Kenchaiah and colleagues investigated the association of pericardial fat with incident heart failure by examining chest CT scans from 6,785 participants (3,584 women and 3,201 men aged 45-84 years) in the Multi-Ethnic Study of Atherosclerosis.
The participants were from four different ethnic groups: 38% were White; 28% were Black, 22% were Hispanic, and 12% were Chinese American. They were recruited between July 17, 2000, and Aug. 31, 2002, from six communities in the United States: Baltimore and Baltimore County; Chicago; Forsyth County, N.C.; Los Angeles County northern Manhattan and the Bronx, New York; and St. Paul, Minn.
All participants were free of cardiovascular disease at baseline.
The researchers followed participants for more than 17 years. During this time, 385 (5.7%; 164 women and 221 men) developed newly diagnosed heart failure.
In women, the hazard ratio for every 42 cm3 increase in PFV was 1.44 (95% confidence interval, 1.21-1.71; P < .001). In men, the HR was 1.13 (95% CI, 1.01-1.27; P = .03).
High PVF conferred a twofold greater risk for heart failure in women (HR, 2.06; 95% CI, 1.48-2.87; P < .001) and a 53% higher risk in men (HR, 1.53; 95% CI, 1.13-2.07; P = .006).
These associations remained significant after further adjustment for circulating markers of systemic inflammation (that is, C-reactive protein and interleukin-6), and abdominal subcutaneous or visceral fat.
They also found that the heightened risk persisted, even after adjustment for established risk factors for heart failure, such as age, cigarette smoking, alcohol consumption, sedentary lifestyle, high blood pressure, high blood sugar, high cholesterol, and myocardial infarction.
Results were similar among all of the ethnic groups studied.
A surprise finding
“The most surprising part of this study was that the risk for heart failure with increased pericardial fat does not seem to be explained by obesity and systemic inflammation alone,” Andreas P. Kalogeropoulos, MD, MPH, PhD, Stony Brook (N.Y.) University, said in an interview.
“If pericardial fat was merely a proxy for increased visceral fat, one would expect the association of pericardial fat with heart failure risk to go away after factoring in abdominal CT findings, which was not the case here. Also, accounting for inflammatory markers did not change things dramatically. However, we need to be careful here, as abdominal CT scans have not been done simultaneously with the pericardial fat scans in the study,” said Dr. Kalogeropoulos, who coauthored an accompanying editorial with Michael E. Hall, MD, University of Mississippi Medical Center, Jackson.
The other striking finding, although not entirely surprising, was the stronger association of pericardial fat with heart failure risk in women, he noted.
“Although several clues have been reported pointing to women being more sensitive to the adverse cardiac effects of pericardial fat, this is the first large prospective study to connect the dots and show much higher risk in women in a convincing way. For the record, this is the first prospective study to show the connection between pericardial fat and heart failure risk altogether,” Dr. Kalogeropoulos said.
“Obviously, we need to do more work to see how we can use the important findings of Kenchaiah and colleagues to reduce risk for heart failure among patients with increased pericardial fat, especially women. For starters, we would need a way to identify these patients,” he said. “In this aspect, it is encouraging that pericardial fat can be measured in low-radiation CT scans, similar to those used for coronary calcium, and that automation technology to speed up pericardial fat measurements is already in the pipeline.
“The next step would be to see what kind of interventions would reduce risk for heart failure in these patients,” he added. “Weight loss would be an obvious thing, but novel agents with favorable cardiometabolic effects, like newer antidiabetic medications, are intriguing options, too.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr. Kenchaiah and Dr. Kalogeropoulos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Underlying heart rhythm, not ICD shocks, drives mortality
Combined data from five implantable cardioverter-defibrillator (ICD) trials suggest that it is the underlying arrhythmic disorder, rather than the ICD therapy itself, that affects mortality in these patients.
Analysis of the MADIT II, MADIT-RISK, MADIT-CRT, MADIT-RIT, and RAID trials showed that the major determinant of mortality in patients receiving a primary prevention ICD was the arrhythmic substrate that leads to occurrence of fast ventricular tachycardia (VT), defined as ≥ 200 bpm, or ventricular fibrillation (VF), not adverse effects of the ICD shock therapy itself.
Patients experiencing an episode of VT had more than a twofold increased risk for death during a follow-up of 2½ years; however, ICD therapies for VT less than 200 bpm and inappropriate ICD shocks were not associated with a higher risk for death.
The findings were published online in the Journal of the American College of Cardiology.
“We know that patients receiving an ICD shock have increased mortality during subsequent follow-up,” first author Mehmet K. Aktas, MD, MBA, University of Rochester (N.Y.), said in an interview.
“There are conflicting data on the impact of ICD shocks on subsequent mortality, and in this study, we aimed to determine whether shocks per se increase subsequent mortality risk or whether the arrhythmic substrate that leads to ICD therapy results in subsequent risk of death,” Dr. Aktas said.
He and his team evaluated the association of ICD therapy with subsequent mortality according to the type of ICD therapy (model I), type of arrhythmia for which ICD therapy was delivered (model II), combined assessment of all arrhythmia and therapy types during follow-up (model III), and incremental risk associated with repeated ICD shocks (model IV).
The study cohort included 5,516 patients. Of these, 1,001 patients (18%) received appropriate ICD therapy and 561 (10%) received inappropriate ICD therapy during an average of 2.4 years.
Patients receiving an appropriate ICD therapy were more likely to be male and to have prior atrial arrhythmia and nonsustained VT compared with those without ICD therapy.
Patients receiving an inappropriate shock were more likely to be younger, to be African American, and to be less likely to have prior nonsustained VT, compared with those without ICD therapy.
Most patients (90%) were receiving beta-blockers and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers regardless of device therapy during follow-up, and 10% of patients were treated with amiodarone.
In model I, at 3 years, the cumulative probability of death following an appropriate ICD shock was 38% compared with no appropriate ICD shock (P < .001). Inappropriate shock alone was not associated with mortality risk.
In model II, which looked at the type of arrhythmia for which ICD therapy was delivered, the cumulative death rate at 3 years following the first occurrence of ICD therapy for VT ≥ 200 beats/min or VF was 27%, compared with 10% in patients not experiencing VT ≥ 200 beats/min or VF (P < .001).
In model III, the highest risk for death was observed following shocks delivered after a failed antitachycardia pacing (ATP) for fast VT (hazard ratio [HR], 3.05), followed by ICD shock for VF (HR, 2.86), ICD shock for fast VT without a prior ATP (HR, 2.83), and ICD shock for slower VT (< 200 beats/min) without a prior ATP (HR, 2.39).
In contrast, other types of appropriate and inappropriate shock or ATP therapies were not associated with a significant risk increase.
In model IV, which assessed the association of shock therapy counts with the risk for death, two or more ICD appropriate shocks were not associated with increased risk after the first appropriate ICD shock.
“Our findings shed light on the mechanisms associated with increased mortality risk in primary prevention ICD recipients,” Dr. Aktas said.
“Studies that evaluate interventions focused on treating and stabilizing the myocardial substrate, which promotes ventricular tachyarrhythmias, such as catheter ablation, are needed to improve survival in heart failure patients,” he added.
Thoughtful study design
In an accompanying editorial, Rajat Deo, MD, and Naga Venkata K. Pothineni, MD, both from the University of Pennsylvania, Philadelphia, praised the researchers for their “thoughtful study design.”
“The take-home message that is most relevant to our clinical practice is clear: Sustained ventricular arrhythmias are a prognostic marker of death and heart failure hospitalization,” they wrote.
The editorialists also commented on the higher rate of inappropriate ICD therapies in African Americans.
“It is concerning to observe that Black patients had a markedly higher rate of inappropriate ICD therapies compared with White patients – and this was in the setting of some of the most respectable, established, and well-funded clinical trials,” they wrote.
Reasons for disparities in outcomes include access to appropriate and affordable medical therapies, access to specialty clinics and caregivers, remote ICD monitoring, and compliance issues.
“Future work will need to understand how the social determinants of health including race affect the treatment and outcomes of our primary prevention ICD population,” they wrote.
Identifying and characterizing the arrhythmic substrate will become a key component of sudden cardiac death risk stratification, the editorialists predicted.
“Concurrently, we must continue to partner with industry colleagues and work with our professional societies to ensure health equity across our patient population,” they concluded.
Dr. Aktas has received research grants from Boston Scientific and Medtronic. Dr. Deo and his coeditorialists report no relevant financial relationships. The MADIT trials were funded by an unrestricted research grant from Boston Scientific to the University of Rochester Medical Center. The RAID trial was funded by the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Combined data from five implantable cardioverter-defibrillator (ICD) trials suggest that it is the underlying arrhythmic disorder, rather than the ICD therapy itself, that affects mortality in these patients.
Analysis of the MADIT II, MADIT-RISK, MADIT-CRT, MADIT-RIT, and RAID trials showed that the major determinant of mortality in patients receiving a primary prevention ICD was the arrhythmic substrate that leads to occurrence of fast ventricular tachycardia (VT), defined as ≥ 200 bpm, or ventricular fibrillation (VF), not adverse effects of the ICD shock therapy itself.
Patients experiencing an episode of VT had more than a twofold increased risk for death during a follow-up of 2½ years; however, ICD therapies for VT less than 200 bpm and inappropriate ICD shocks were not associated with a higher risk for death.
The findings were published online in the Journal of the American College of Cardiology.
“We know that patients receiving an ICD shock have increased mortality during subsequent follow-up,” first author Mehmet K. Aktas, MD, MBA, University of Rochester (N.Y.), said in an interview.
“There are conflicting data on the impact of ICD shocks on subsequent mortality, and in this study, we aimed to determine whether shocks per se increase subsequent mortality risk or whether the arrhythmic substrate that leads to ICD therapy results in subsequent risk of death,” Dr. Aktas said.
He and his team evaluated the association of ICD therapy with subsequent mortality according to the type of ICD therapy (model I), type of arrhythmia for which ICD therapy was delivered (model II), combined assessment of all arrhythmia and therapy types during follow-up (model III), and incremental risk associated with repeated ICD shocks (model IV).
The study cohort included 5,516 patients. Of these, 1,001 patients (18%) received appropriate ICD therapy and 561 (10%) received inappropriate ICD therapy during an average of 2.4 years.
Patients receiving an appropriate ICD therapy were more likely to be male and to have prior atrial arrhythmia and nonsustained VT compared with those without ICD therapy.
Patients receiving an inappropriate shock were more likely to be younger, to be African American, and to be less likely to have prior nonsustained VT, compared with those without ICD therapy.
Most patients (90%) were receiving beta-blockers and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers regardless of device therapy during follow-up, and 10% of patients were treated with amiodarone.
In model I, at 3 years, the cumulative probability of death following an appropriate ICD shock was 38% compared with no appropriate ICD shock (P < .001). Inappropriate shock alone was not associated with mortality risk.
In model II, which looked at the type of arrhythmia for which ICD therapy was delivered, the cumulative death rate at 3 years following the first occurrence of ICD therapy for VT ≥ 200 beats/min or VF was 27%, compared with 10% in patients not experiencing VT ≥ 200 beats/min or VF (P < .001).
In model III, the highest risk for death was observed following shocks delivered after a failed antitachycardia pacing (ATP) for fast VT (hazard ratio [HR], 3.05), followed by ICD shock for VF (HR, 2.86), ICD shock for fast VT without a prior ATP (HR, 2.83), and ICD shock for slower VT (< 200 beats/min) without a prior ATP (HR, 2.39).
In contrast, other types of appropriate and inappropriate shock or ATP therapies were not associated with a significant risk increase.
In model IV, which assessed the association of shock therapy counts with the risk for death, two or more ICD appropriate shocks were not associated with increased risk after the first appropriate ICD shock.
“Our findings shed light on the mechanisms associated with increased mortality risk in primary prevention ICD recipients,” Dr. Aktas said.
“Studies that evaluate interventions focused on treating and stabilizing the myocardial substrate, which promotes ventricular tachyarrhythmias, such as catheter ablation, are needed to improve survival in heart failure patients,” he added.
Thoughtful study design
In an accompanying editorial, Rajat Deo, MD, and Naga Venkata K. Pothineni, MD, both from the University of Pennsylvania, Philadelphia, praised the researchers for their “thoughtful study design.”
“The take-home message that is most relevant to our clinical practice is clear: Sustained ventricular arrhythmias are a prognostic marker of death and heart failure hospitalization,” they wrote.
The editorialists also commented on the higher rate of inappropriate ICD therapies in African Americans.
“It is concerning to observe that Black patients had a markedly higher rate of inappropriate ICD therapies compared with White patients – and this was in the setting of some of the most respectable, established, and well-funded clinical trials,” they wrote.
Reasons for disparities in outcomes include access to appropriate and affordable medical therapies, access to specialty clinics and caregivers, remote ICD monitoring, and compliance issues.
“Future work will need to understand how the social determinants of health including race affect the treatment and outcomes of our primary prevention ICD population,” they wrote.
Identifying and characterizing the arrhythmic substrate will become a key component of sudden cardiac death risk stratification, the editorialists predicted.
“Concurrently, we must continue to partner with industry colleagues and work with our professional societies to ensure health equity across our patient population,” they concluded.
Dr. Aktas has received research grants from Boston Scientific and Medtronic. Dr. Deo and his coeditorialists report no relevant financial relationships. The MADIT trials were funded by an unrestricted research grant from Boston Scientific to the University of Rochester Medical Center. The RAID trial was funded by the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Combined data from five implantable cardioverter-defibrillator (ICD) trials suggest that it is the underlying arrhythmic disorder, rather than the ICD therapy itself, that affects mortality in these patients.
Analysis of the MADIT II, MADIT-RISK, MADIT-CRT, MADIT-RIT, and RAID trials showed that the major determinant of mortality in patients receiving a primary prevention ICD was the arrhythmic substrate that leads to occurrence of fast ventricular tachycardia (VT), defined as ≥ 200 bpm, or ventricular fibrillation (VF), not adverse effects of the ICD shock therapy itself.
Patients experiencing an episode of VT had more than a twofold increased risk for death during a follow-up of 2½ years; however, ICD therapies for VT less than 200 bpm and inappropriate ICD shocks were not associated with a higher risk for death.
The findings were published online in the Journal of the American College of Cardiology.
“We know that patients receiving an ICD shock have increased mortality during subsequent follow-up,” first author Mehmet K. Aktas, MD, MBA, University of Rochester (N.Y.), said in an interview.
“There are conflicting data on the impact of ICD shocks on subsequent mortality, and in this study, we aimed to determine whether shocks per se increase subsequent mortality risk or whether the arrhythmic substrate that leads to ICD therapy results in subsequent risk of death,” Dr. Aktas said.
He and his team evaluated the association of ICD therapy with subsequent mortality according to the type of ICD therapy (model I), type of arrhythmia for which ICD therapy was delivered (model II), combined assessment of all arrhythmia and therapy types during follow-up (model III), and incremental risk associated with repeated ICD shocks (model IV).
The study cohort included 5,516 patients. Of these, 1,001 patients (18%) received appropriate ICD therapy and 561 (10%) received inappropriate ICD therapy during an average of 2.4 years.
Patients receiving an appropriate ICD therapy were more likely to be male and to have prior atrial arrhythmia and nonsustained VT compared with those without ICD therapy.
Patients receiving an inappropriate shock were more likely to be younger, to be African American, and to be less likely to have prior nonsustained VT, compared with those without ICD therapy.
Most patients (90%) were receiving beta-blockers and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers regardless of device therapy during follow-up, and 10% of patients were treated with amiodarone.
In model I, at 3 years, the cumulative probability of death following an appropriate ICD shock was 38% compared with no appropriate ICD shock (P < .001). Inappropriate shock alone was not associated with mortality risk.
In model II, which looked at the type of arrhythmia for which ICD therapy was delivered, the cumulative death rate at 3 years following the first occurrence of ICD therapy for VT ≥ 200 beats/min or VF was 27%, compared with 10% in patients not experiencing VT ≥ 200 beats/min or VF (P < .001).
In model III, the highest risk for death was observed following shocks delivered after a failed antitachycardia pacing (ATP) for fast VT (hazard ratio [HR], 3.05), followed by ICD shock for VF (HR, 2.86), ICD shock for fast VT without a prior ATP (HR, 2.83), and ICD shock for slower VT (< 200 beats/min) without a prior ATP (HR, 2.39).
In contrast, other types of appropriate and inappropriate shock or ATP therapies were not associated with a significant risk increase.
In model IV, which assessed the association of shock therapy counts with the risk for death, two or more ICD appropriate shocks were not associated with increased risk after the first appropriate ICD shock.
“Our findings shed light on the mechanisms associated with increased mortality risk in primary prevention ICD recipients,” Dr. Aktas said.
“Studies that evaluate interventions focused on treating and stabilizing the myocardial substrate, which promotes ventricular tachyarrhythmias, such as catheter ablation, are needed to improve survival in heart failure patients,” he added.
Thoughtful study design
In an accompanying editorial, Rajat Deo, MD, and Naga Venkata K. Pothineni, MD, both from the University of Pennsylvania, Philadelphia, praised the researchers for their “thoughtful study design.”
“The take-home message that is most relevant to our clinical practice is clear: Sustained ventricular arrhythmias are a prognostic marker of death and heart failure hospitalization,” they wrote.
The editorialists also commented on the higher rate of inappropriate ICD therapies in African Americans.
“It is concerning to observe that Black patients had a markedly higher rate of inappropriate ICD therapies compared with White patients – and this was in the setting of some of the most respectable, established, and well-funded clinical trials,” they wrote.
Reasons for disparities in outcomes include access to appropriate and affordable medical therapies, access to specialty clinics and caregivers, remote ICD monitoring, and compliance issues.
“Future work will need to understand how the social determinants of health including race affect the treatment and outcomes of our primary prevention ICD population,” they wrote.
Identifying and characterizing the arrhythmic substrate will become a key component of sudden cardiac death risk stratification, the editorialists predicted.
“Concurrently, we must continue to partner with industry colleagues and work with our professional societies to ensure health equity across our patient population,” they concluded.
Dr. Aktas has received research grants from Boston Scientific and Medtronic. Dr. Deo and his coeditorialists report no relevant financial relationships. The MADIT trials were funded by an unrestricted research grant from Boston Scientific to the University of Rochester Medical Center. The RAID trial was funded by the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Doctors prescribe fewer statins in the afternoon
Primary care physicians are more likely to write a prescription for statins for their patients at risk for cardiovascular adverse events in the morning than in the afternoon, new research suggests.
In an observational cohort study, researchers from the nudge unit, University of Pennsylvania, Philadelphia, found that patients who had the first appointments of the day were most likely to have statins prescribed for them, and that this likelihood decreased as the day went on.
The study was published online May 11, 2021, in JAMA Network Open.
“Physicians are faced with decision fatigue, where they are seeing 20 patients in a day and may not have the mental bandwidth or cognitive bandwidth to fully think through every decision for every patient and to make all the appropriate decisions all of the time,” lead author Allison J. Hare, medical student and clinical informatics fellow in the nudge unit, said in an interview.
The Penn Medicine nudge unit attempts to better align clinician decision-making with current standards in best practices for the provision of various therapies, Ms. Hare explained.
“As we see more and more best-practice guidelines come out, we also see that there is a gap in the intention to treat and actual provision of these therapies,” she said. “There are also increasing expectations for clinicians to provide all of these different evidence-backed therapies. It can be hard to keep up with all these guidelines, especially when you are expected to take care of more and more patients, more and more efficiently.”
Guideline-directed statin therapy has been demonstrated to reduce the risk for major adverse cardiovascular events, yet 50% of statin-eligible patients have not been prescribed one.
“In our prior work at the nudge unit, we observed that rates of preventive care, including flu vaccination and cancer screening, declined as the clinic day progressed. We wanted to see if this occurred with statin scripts,” Ms. Hare said.
The researchers obtained data from 28 Penn Medicine primary care practices that included 10,757 patients at risk for heart disease for the period from March 2019 to February 2020.
Their mean age was 66.0 years (standard deviation, 10.5 years), 5,072 (47.2%) were female, and 7,071 (65.7%) were White. Patient characteristics were similar between morning and afternoon appointments.
All patients had clinical atherosclerotic cardiovascular disease, familial hypercholesterolemia, or LDL cholesterol of at least 190 mg/dL, conditions which qualified them for statins based on the U.S. Preventive Services Task Force guidelines.
The appointment times for each patient were broken down into hour blocks, ranging from the 8:00 a.m. hour to the 4:00 p.m. hour, which bookend open times in most practices.
Overall, statins were prescribed in 36% (n = 3,864) of visits.
The data showed a clear decline in statin prescribing as the day went on. For example, compared with patients who came in at 8:00 a.m. (the reference group), patients who came in at 9:00 a.m. were 12% less likely to get a prescription.
Patients coming in for noon appointments were 37% less likely to get a statin prescription, which made them the least likely to get a script. After the noon visits, there was a slight increase, but the likelihood of a statin prescription remained 27% less likely or worse for the rest of the day.
“In the context of the myriad tasks that clinicians are faced with doing for a single patient, and then also within the context of seeing 20 patients in 15-minute increments, it is easy to see how certain things fall through the cracks,” Ms. Hare said. “It’s impossible for any clinician to remember every single little thing for their patient every single time, so if we can augment the clinician’s ability to make those appropriate decisions with electronic tools, we can narrow that gap a little bit.”
Why the variability?
“The nudge unit uses prompts to ask the physician about prescribing statins. The question is, what is causing the variability in statin prescriptions?” Nieca Goldberg, MD, medical director of the New York University women’s heart program, said in an interview.
“Is it fatigue, lack of familiarity of guidelines, or is this due to the volume of patients and lack of time to discuss the therapy and make a shared decision with their patient? The answer to these questions was not part of the study,” said Dr. Goldberg, who is also an American Heart Association volunteer expert. “It would be interesting to know the thoughts of the physicians who were studied after they were informed of the results. Also, having a nudge to write the prescription will increase the prescriptions of statins, but will patients take the medication?”
The study was funded in part by a grant from the National Institute on Aging. Ms. Hare and Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians are more likely to write a prescription for statins for their patients at risk for cardiovascular adverse events in the morning than in the afternoon, new research suggests.
In an observational cohort study, researchers from the nudge unit, University of Pennsylvania, Philadelphia, found that patients who had the first appointments of the day were most likely to have statins prescribed for them, and that this likelihood decreased as the day went on.
The study was published online May 11, 2021, in JAMA Network Open.
“Physicians are faced with decision fatigue, where they are seeing 20 patients in a day and may not have the mental bandwidth or cognitive bandwidth to fully think through every decision for every patient and to make all the appropriate decisions all of the time,” lead author Allison J. Hare, medical student and clinical informatics fellow in the nudge unit, said in an interview.
The Penn Medicine nudge unit attempts to better align clinician decision-making with current standards in best practices for the provision of various therapies, Ms. Hare explained.
“As we see more and more best-practice guidelines come out, we also see that there is a gap in the intention to treat and actual provision of these therapies,” she said. “There are also increasing expectations for clinicians to provide all of these different evidence-backed therapies. It can be hard to keep up with all these guidelines, especially when you are expected to take care of more and more patients, more and more efficiently.”
Guideline-directed statin therapy has been demonstrated to reduce the risk for major adverse cardiovascular events, yet 50% of statin-eligible patients have not been prescribed one.
“In our prior work at the nudge unit, we observed that rates of preventive care, including flu vaccination and cancer screening, declined as the clinic day progressed. We wanted to see if this occurred with statin scripts,” Ms. Hare said.
The researchers obtained data from 28 Penn Medicine primary care practices that included 10,757 patients at risk for heart disease for the period from March 2019 to February 2020.
Their mean age was 66.0 years (standard deviation, 10.5 years), 5,072 (47.2%) were female, and 7,071 (65.7%) were White. Patient characteristics were similar between morning and afternoon appointments.
All patients had clinical atherosclerotic cardiovascular disease, familial hypercholesterolemia, or LDL cholesterol of at least 190 mg/dL, conditions which qualified them for statins based on the U.S. Preventive Services Task Force guidelines.
The appointment times for each patient were broken down into hour blocks, ranging from the 8:00 a.m. hour to the 4:00 p.m. hour, which bookend open times in most practices.
Overall, statins were prescribed in 36% (n = 3,864) of visits.
The data showed a clear decline in statin prescribing as the day went on. For example, compared with patients who came in at 8:00 a.m. (the reference group), patients who came in at 9:00 a.m. were 12% less likely to get a prescription.
Patients coming in for noon appointments were 37% less likely to get a statin prescription, which made them the least likely to get a script. After the noon visits, there was a slight increase, but the likelihood of a statin prescription remained 27% less likely or worse for the rest of the day.
“In the context of the myriad tasks that clinicians are faced with doing for a single patient, and then also within the context of seeing 20 patients in 15-minute increments, it is easy to see how certain things fall through the cracks,” Ms. Hare said. “It’s impossible for any clinician to remember every single little thing for their patient every single time, so if we can augment the clinician’s ability to make those appropriate decisions with electronic tools, we can narrow that gap a little bit.”
Why the variability?
“The nudge unit uses prompts to ask the physician about prescribing statins. The question is, what is causing the variability in statin prescriptions?” Nieca Goldberg, MD, medical director of the New York University women’s heart program, said in an interview.
“Is it fatigue, lack of familiarity of guidelines, or is this due to the volume of patients and lack of time to discuss the therapy and make a shared decision with their patient? The answer to these questions was not part of the study,” said Dr. Goldberg, who is also an American Heart Association volunteer expert. “It would be interesting to know the thoughts of the physicians who were studied after they were informed of the results. Also, having a nudge to write the prescription will increase the prescriptions of statins, but will patients take the medication?”
The study was funded in part by a grant from the National Institute on Aging. Ms. Hare and Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians are more likely to write a prescription for statins for their patients at risk for cardiovascular adverse events in the morning than in the afternoon, new research suggests.
In an observational cohort study, researchers from the nudge unit, University of Pennsylvania, Philadelphia, found that patients who had the first appointments of the day were most likely to have statins prescribed for them, and that this likelihood decreased as the day went on.
The study was published online May 11, 2021, in JAMA Network Open.
“Physicians are faced with decision fatigue, where they are seeing 20 patients in a day and may not have the mental bandwidth or cognitive bandwidth to fully think through every decision for every patient and to make all the appropriate decisions all of the time,” lead author Allison J. Hare, medical student and clinical informatics fellow in the nudge unit, said in an interview.
The Penn Medicine nudge unit attempts to better align clinician decision-making with current standards in best practices for the provision of various therapies, Ms. Hare explained.
“As we see more and more best-practice guidelines come out, we also see that there is a gap in the intention to treat and actual provision of these therapies,” she said. “There are also increasing expectations for clinicians to provide all of these different evidence-backed therapies. It can be hard to keep up with all these guidelines, especially when you are expected to take care of more and more patients, more and more efficiently.”
Guideline-directed statin therapy has been demonstrated to reduce the risk for major adverse cardiovascular events, yet 50% of statin-eligible patients have not been prescribed one.
“In our prior work at the nudge unit, we observed that rates of preventive care, including flu vaccination and cancer screening, declined as the clinic day progressed. We wanted to see if this occurred with statin scripts,” Ms. Hare said.
The researchers obtained data from 28 Penn Medicine primary care practices that included 10,757 patients at risk for heart disease for the period from March 2019 to February 2020.
Their mean age was 66.0 years (standard deviation, 10.5 years), 5,072 (47.2%) were female, and 7,071 (65.7%) were White. Patient characteristics were similar between morning and afternoon appointments.
All patients had clinical atherosclerotic cardiovascular disease, familial hypercholesterolemia, or LDL cholesterol of at least 190 mg/dL, conditions which qualified them for statins based on the U.S. Preventive Services Task Force guidelines.
The appointment times for each patient were broken down into hour blocks, ranging from the 8:00 a.m. hour to the 4:00 p.m. hour, which bookend open times in most practices.
Overall, statins were prescribed in 36% (n = 3,864) of visits.
The data showed a clear decline in statin prescribing as the day went on. For example, compared with patients who came in at 8:00 a.m. (the reference group), patients who came in at 9:00 a.m. were 12% less likely to get a prescription.
Patients coming in for noon appointments were 37% less likely to get a statin prescription, which made them the least likely to get a script. After the noon visits, there was a slight increase, but the likelihood of a statin prescription remained 27% less likely or worse for the rest of the day.
“In the context of the myriad tasks that clinicians are faced with doing for a single patient, and then also within the context of seeing 20 patients in 15-minute increments, it is easy to see how certain things fall through the cracks,” Ms. Hare said. “It’s impossible for any clinician to remember every single little thing for their patient every single time, so if we can augment the clinician’s ability to make those appropriate decisions with electronic tools, we can narrow that gap a little bit.”
Why the variability?
“The nudge unit uses prompts to ask the physician about prescribing statins. The question is, what is causing the variability in statin prescriptions?” Nieca Goldberg, MD, medical director of the New York University women’s heart program, said in an interview.
“Is it fatigue, lack of familiarity of guidelines, or is this due to the volume of patients and lack of time to discuss the therapy and make a shared decision with their patient? The answer to these questions was not part of the study,” said Dr. Goldberg, who is also an American Heart Association volunteer expert. “It would be interesting to know the thoughts of the physicians who were studied after they were informed of the results. Also, having a nudge to write the prescription will increase the prescriptions of statins, but will patients take the medication?”
The study was funded in part by a grant from the National Institute on Aging. Ms. Hare and Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Coffee intake may be driven by cardiovascular symptoms
An examination of coffee consumption habits of almost 400,000 people suggests that those habits are largely driven by a person’s cardiovascular health.
Data from a large population database showed that people with essential hypertension, angina, or cardiac arrhythmias drank less coffee than people who had none of these conditions. When they did drink coffee, it tended to be decaffeinated.
The investigators, led by Elina Hyppönen, PhD, director of the Australian Centre for Precision Health at the University of South Australia, Adelaide, say that this predilection for avoiding coffee, which is known to produce jitteriness and heart palpitations, is based on genetics.
“If your body is telling you not to drink that extra cup of coffee, there’s likely a reason why,” Dr. Hyppönen said in an interview.
The study was published online in the American Journal of Clinical Nutrition.
“People drink coffee as a pick-me-up when they’re feeling tired, or because it tastes good, or simply because it’s part of their daily routine, but what we don’t recognize is that people subconsciously self-regulate safe levels of caffeine based on how high their blood pressure is, and this is likely a result of a protective genetic mechanism, [meaning] that someone who drinks a lot of coffee is likely more genetically tolerant of caffeine, as compared to someone who drinks very little,” Dr. Hyppönen said.
“In addition, we’ve known from past research that when people feel unwell, they tend to drink less coffee. This type of phenomenon, where disease drives behavior, is called reverse causality,” Dr. Hyppönen said.
For this analysis, she and her team used information on 390,435 individuals of European ancestry from the UK Biobank, a large epidemiologic database. Habitual coffee consumption was self-reported, and systolic and diastolic blood pressure and heart rate were measured at baseline. Cardiovascular symptoms at baseline were gleaned from hospital diagnoses, primary care records, and/or self report, the authors note.
To look at the relationship of systolic BP, diastolic BP, and heart rate with coffee consumption, they used a strategy called Mendelian randomization, which allows genetic information such as variants reflecting higher blood pressures and heart rate to be used to provide evidence for a causal association.
Results showed that participants with essential hypertension, angina, or arrhythmia were “all more likely to drink less caffeinated coffee and to be nonhabitual or decaffeinated coffee drinkers compared with those who did not report related symptoms,” the authors write.
Those with higher systolic and diastolic BP based on their genetics tended to drink less caffeinated coffee at baseline, “with consistent genetic evidence to support a causal explanation across all methods,” they noted.
They also found that those people who have a higher resting heart rate due to their genes were more likely to choose decaffeinated coffee.
“These results have two major implications,” Dr. Hyppönen said. “Firstly, they show that our bodies can regulate behavior in ways that we may not realize, and that if something does not feel good to us, there is a likely to be a reason why.”
“Second, our results show that our health status in part regulates the amount of coffee we drink. This is important, because when disease drives behavior, it can lead to misleading health associations in observational studies, and indeed, create a false impression for health benefits if the group of people who do not drink coffee also includes more people who are unwell,” she said.
For now, doctors can tell their patients that this study provides an explanation as to why research on the health effects of habitual coffee consumption has been conflicting, Dr. Hyppönen said.
“Our study also highlights the uncertainty that underlies the claimed health benefits of coffee, but at the same time, it gives a positive message about the ability of our body to regulate our level of coffee consumption in a way that helps us avoid adverse effects.”
“The most common symptoms of excessive coffee consumption are palpitations and rapid heartbeat, also known as tachycardia,” Nieca Goldberg, MD, medical director of the NYU Women’s Heart Program at NYU Langone Health, said in an interview.
“This study was designed to see if cardiac symptoms affect coffee consumption, and it showed that people with hypertension, angina, history of arrhythmias, and poor health tend to be decaffeinated coffee drinkers or no coffee drinkers,” Dr. Goldberg said.
“People naturally alter their coffee intake base on their blood pressure and symptoms of palpitations and/or rapid heart rate,” she said.
The results also suggest that, “we cannot infer health benefit or harm based on the available coffee studies,” Dr. Goldberg added.
The study was funded by the National Health and Medical Research Council, Australia. Dr. Hyppönen and Dr. Goldberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An examination of coffee consumption habits of almost 400,000 people suggests that those habits are largely driven by a person’s cardiovascular health.
Data from a large population database showed that people with essential hypertension, angina, or cardiac arrhythmias drank less coffee than people who had none of these conditions. When they did drink coffee, it tended to be decaffeinated.
The investigators, led by Elina Hyppönen, PhD, director of the Australian Centre for Precision Health at the University of South Australia, Adelaide, say that this predilection for avoiding coffee, which is known to produce jitteriness and heart palpitations, is based on genetics.
“If your body is telling you not to drink that extra cup of coffee, there’s likely a reason why,” Dr. Hyppönen said in an interview.
The study was published online in the American Journal of Clinical Nutrition.
“People drink coffee as a pick-me-up when they’re feeling tired, or because it tastes good, or simply because it’s part of their daily routine, but what we don’t recognize is that people subconsciously self-regulate safe levels of caffeine based on how high their blood pressure is, and this is likely a result of a protective genetic mechanism, [meaning] that someone who drinks a lot of coffee is likely more genetically tolerant of caffeine, as compared to someone who drinks very little,” Dr. Hyppönen said.
“In addition, we’ve known from past research that when people feel unwell, they tend to drink less coffee. This type of phenomenon, where disease drives behavior, is called reverse causality,” Dr. Hyppönen said.
For this analysis, she and her team used information on 390,435 individuals of European ancestry from the UK Biobank, a large epidemiologic database. Habitual coffee consumption was self-reported, and systolic and diastolic blood pressure and heart rate were measured at baseline. Cardiovascular symptoms at baseline were gleaned from hospital diagnoses, primary care records, and/or self report, the authors note.
To look at the relationship of systolic BP, diastolic BP, and heart rate with coffee consumption, they used a strategy called Mendelian randomization, which allows genetic information such as variants reflecting higher blood pressures and heart rate to be used to provide evidence for a causal association.
Results showed that participants with essential hypertension, angina, or arrhythmia were “all more likely to drink less caffeinated coffee and to be nonhabitual or decaffeinated coffee drinkers compared with those who did not report related symptoms,” the authors write.
Those with higher systolic and diastolic BP based on their genetics tended to drink less caffeinated coffee at baseline, “with consistent genetic evidence to support a causal explanation across all methods,” they noted.
They also found that those people who have a higher resting heart rate due to their genes were more likely to choose decaffeinated coffee.
“These results have two major implications,” Dr. Hyppönen said. “Firstly, they show that our bodies can regulate behavior in ways that we may not realize, and that if something does not feel good to us, there is a likely to be a reason why.”
“Second, our results show that our health status in part regulates the amount of coffee we drink. This is important, because when disease drives behavior, it can lead to misleading health associations in observational studies, and indeed, create a false impression for health benefits if the group of people who do not drink coffee also includes more people who are unwell,” she said.
For now, doctors can tell their patients that this study provides an explanation as to why research on the health effects of habitual coffee consumption has been conflicting, Dr. Hyppönen said.
“Our study also highlights the uncertainty that underlies the claimed health benefits of coffee, but at the same time, it gives a positive message about the ability of our body to regulate our level of coffee consumption in a way that helps us avoid adverse effects.”
“The most common symptoms of excessive coffee consumption are palpitations and rapid heartbeat, also known as tachycardia,” Nieca Goldberg, MD, medical director of the NYU Women’s Heart Program at NYU Langone Health, said in an interview.
“This study was designed to see if cardiac symptoms affect coffee consumption, and it showed that people with hypertension, angina, history of arrhythmias, and poor health tend to be decaffeinated coffee drinkers or no coffee drinkers,” Dr. Goldberg said.
“People naturally alter their coffee intake base on their blood pressure and symptoms of palpitations and/or rapid heart rate,” she said.
The results also suggest that, “we cannot infer health benefit or harm based on the available coffee studies,” Dr. Goldberg added.
The study was funded by the National Health and Medical Research Council, Australia. Dr. Hyppönen and Dr. Goldberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An examination of coffee consumption habits of almost 400,000 people suggests that those habits are largely driven by a person’s cardiovascular health.
Data from a large population database showed that people with essential hypertension, angina, or cardiac arrhythmias drank less coffee than people who had none of these conditions. When they did drink coffee, it tended to be decaffeinated.
The investigators, led by Elina Hyppönen, PhD, director of the Australian Centre for Precision Health at the University of South Australia, Adelaide, say that this predilection for avoiding coffee, which is known to produce jitteriness and heart palpitations, is based on genetics.
“If your body is telling you not to drink that extra cup of coffee, there’s likely a reason why,” Dr. Hyppönen said in an interview.
The study was published online in the American Journal of Clinical Nutrition.
“People drink coffee as a pick-me-up when they’re feeling tired, or because it tastes good, or simply because it’s part of their daily routine, but what we don’t recognize is that people subconsciously self-regulate safe levels of caffeine based on how high their blood pressure is, and this is likely a result of a protective genetic mechanism, [meaning] that someone who drinks a lot of coffee is likely more genetically tolerant of caffeine, as compared to someone who drinks very little,” Dr. Hyppönen said.
“In addition, we’ve known from past research that when people feel unwell, they tend to drink less coffee. This type of phenomenon, where disease drives behavior, is called reverse causality,” Dr. Hyppönen said.
For this analysis, she and her team used information on 390,435 individuals of European ancestry from the UK Biobank, a large epidemiologic database. Habitual coffee consumption was self-reported, and systolic and diastolic blood pressure and heart rate were measured at baseline. Cardiovascular symptoms at baseline were gleaned from hospital diagnoses, primary care records, and/or self report, the authors note.
To look at the relationship of systolic BP, diastolic BP, and heart rate with coffee consumption, they used a strategy called Mendelian randomization, which allows genetic information such as variants reflecting higher blood pressures and heart rate to be used to provide evidence for a causal association.
Results showed that participants with essential hypertension, angina, or arrhythmia were “all more likely to drink less caffeinated coffee and to be nonhabitual or decaffeinated coffee drinkers compared with those who did not report related symptoms,” the authors write.
Those with higher systolic and diastolic BP based on their genetics tended to drink less caffeinated coffee at baseline, “with consistent genetic evidence to support a causal explanation across all methods,” they noted.
They also found that those people who have a higher resting heart rate due to their genes were more likely to choose decaffeinated coffee.
“These results have two major implications,” Dr. Hyppönen said. “Firstly, they show that our bodies can regulate behavior in ways that we may not realize, and that if something does not feel good to us, there is a likely to be a reason why.”
“Second, our results show that our health status in part regulates the amount of coffee we drink. This is important, because when disease drives behavior, it can lead to misleading health associations in observational studies, and indeed, create a false impression for health benefits if the group of people who do not drink coffee also includes more people who are unwell,” she said.
For now, doctors can tell their patients that this study provides an explanation as to why research on the health effects of habitual coffee consumption has been conflicting, Dr. Hyppönen said.
“Our study also highlights the uncertainty that underlies the claimed health benefits of coffee, but at the same time, it gives a positive message about the ability of our body to regulate our level of coffee consumption in a way that helps us avoid adverse effects.”
“The most common symptoms of excessive coffee consumption are palpitations and rapid heartbeat, also known as tachycardia,” Nieca Goldberg, MD, medical director of the NYU Women’s Heart Program at NYU Langone Health, said in an interview.
“This study was designed to see if cardiac symptoms affect coffee consumption, and it showed that people with hypertension, angina, history of arrhythmias, and poor health tend to be decaffeinated coffee drinkers or no coffee drinkers,” Dr. Goldberg said.
“People naturally alter their coffee intake base on their blood pressure and symptoms of palpitations and/or rapid heart rate,” she said.
The results also suggest that, “we cannot infer health benefit or harm based on the available coffee studies,” Dr. Goldberg added.
The study was funded by the National Health and Medical Research Council, Australia. Dr. Hyppönen and Dr. Goldberg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 outcomes similar with ECMO or mechanical ventilation
Severely ill COVID-19 patients treated with extracorporeal membrane oxygenation (ECMO) had similar survival to hospital discharge and long-term outcomes as survivors treated with mechanical ventilation alone, results of a new, multicenter study suggest.
Importantly, the study also showed that survivors, regardless of the treatment they received, experienced significant deficits following their stay in the ICU and were suffering problems with physical, psychological, and cognitive functioning for months afterward.
At 3 months after discharge, 50% of the survivors reported cognitive dysfunction, ICU-acquired weakness and depression, anxiety, or PTSD; over 25% still required supplemental oxygen; and only one in six survivors were back at work.
The findings were presented April 30 at the American Association for Thoracic Surgery annual meeting.
The study represents the efforts of a multidisciplinary team that included cardiothoracic surgeons, critical care doctors, medical staff at long-term care facilities, and physical therapists in addition to other specialists. The research followed patients at five academic centers: the University of Colorado, the University of Virginia, the University of Kentucky, Johns Hopkins University, and Vanderbilt University.
“We were a multidisciplinary team, a whole variety of people to really track the long-term outcomes for patients who have been critically ill from COVID-19 and survived to hospital discharge,” presenting author Lauren J. Taylor, MD, fellow at the University of Colorado at Denver, Aurora, said in an interview.
It’s unclear currently what happens to these patients once they leave the hospital, she noted. “This is information we have not had, but when we followed these patients in these multidisciplinary clinics, there was a high level of either physical, emotional, or cognitive dysfunction, even for patients who were well enough to be living at home at the time of follow-up.
“So, if you have somebody living at home and they come into the clinic, you assume they are functioning pretty well, but when you actually provide them with cognitive and psychological testing and check their physical capabilities, you find a high degree of deficits throughout the entire cohort of this study,” she said.
The study was prompted by discussion with patients’ family members about the rationale, risks, and benefits of ECMO cannulation in patients with COVID-19 failing mechanical ventilation, senior author Jessica V. Rove, MD, also from the University of Colorado, said in an interview.
“We wanted to find out what their hospital course would be like and what cognitive, physical, or emotional deficits might they experience if they survive,” Dr. Rove said.
The investigators compared 262 mechanically ventilated patients with 46 patients cannulated for ECMO who were hospitalized between March and May 2020.
ECMO patients were younger and traveled farther but there were no significant differences in gender, race, or body mass index.
ECMO patients were mechanically ventilated for longer durations (median, 26 days vs. 13 days) and were more likely to receive inhaled pulmonary vasodilators, neuromuscular blockade, investigational COVID-19 therapies, blood transfusions, and inotropes.
They also experienced greater bleeding and clotting events (P < .01).
Despite a more complex critical illness course, patients treated with ECMO had similar survival at discharge and long-term outcomes, compared with those who were treated with mechanical ventilation alone.
The survival rate for ECMO patients was 69.9%, and for mechanically ventilated patients it was 69.6%.
Of the 215 survivors, 66.5% had documented follow-up within 3 months of discharge from hospital. Most survivors (93.9%) were living at home; a small percentage (16.1%) had returned to work or their usual activities, and 26.2% were still using supplemental oxygen.
These rates did not differ significantly based on ECMO status and rates of physical, psychological, and cognitive deficits did not differ significantly.
“The cognitive, emotional, and physical deficits seen in survivors of critical illness from COVID-19 can only be treated if diagnosed,” Dr. Rove said.
“Detrimental effects can potentially be ameliorated with use of best practices in the ICU, maximizing acute rehabilitation services where indicated, and follow-up with providers in multidisciplinary post-ICU clinics who can assess and treat these patients to optimize survivorship,” she said.
A version of this article first appeared on Medscape.com.
Severely ill COVID-19 patients treated with extracorporeal membrane oxygenation (ECMO) had similar survival to hospital discharge and long-term outcomes as survivors treated with mechanical ventilation alone, results of a new, multicenter study suggest.
Importantly, the study also showed that survivors, regardless of the treatment they received, experienced significant deficits following their stay in the ICU and were suffering problems with physical, psychological, and cognitive functioning for months afterward.
At 3 months after discharge, 50% of the survivors reported cognitive dysfunction, ICU-acquired weakness and depression, anxiety, or PTSD; over 25% still required supplemental oxygen; and only one in six survivors were back at work.
The findings were presented April 30 at the American Association for Thoracic Surgery annual meeting.
The study represents the efforts of a multidisciplinary team that included cardiothoracic surgeons, critical care doctors, medical staff at long-term care facilities, and physical therapists in addition to other specialists. The research followed patients at five academic centers: the University of Colorado, the University of Virginia, the University of Kentucky, Johns Hopkins University, and Vanderbilt University.
“We were a multidisciplinary team, a whole variety of people to really track the long-term outcomes for patients who have been critically ill from COVID-19 and survived to hospital discharge,” presenting author Lauren J. Taylor, MD, fellow at the University of Colorado at Denver, Aurora, said in an interview.
It’s unclear currently what happens to these patients once they leave the hospital, she noted. “This is information we have not had, but when we followed these patients in these multidisciplinary clinics, there was a high level of either physical, emotional, or cognitive dysfunction, even for patients who were well enough to be living at home at the time of follow-up.
“So, if you have somebody living at home and they come into the clinic, you assume they are functioning pretty well, but when you actually provide them with cognitive and psychological testing and check their physical capabilities, you find a high degree of deficits throughout the entire cohort of this study,” she said.
The study was prompted by discussion with patients’ family members about the rationale, risks, and benefits of ECMO cannulation in patients with COVID-19 failing mechanical ventilation, senior author Jessica V. Rove, MD, also from the University of Colorado, said in an interview.
“We wanted to find out what their hospital course would be like and what cognitive, physical, or emotional deficits might they experience if they survive,” Dr. Rove said.
The investigators compared 262 mechanically ventilated patients with 46 patients cannulated for ECMO who were hospitalized between March and May 2020.
ECMO patients were younger and traveled farther but there were no significant differences in gender, race, or body mass index.
ECMO patients were mechanically ventilated for longer durations (median, 26 days vs. 13 days) and were more likely to receive inhaled pulmonary vasodilators, neuromuscular blockade, investigational COVID-19 therapies, blood transfusions, and inotropes.
They also experienced greater bleeding and clotting events (P < .01).
Despite a more complex critical illness course, patients treated with ECMO had similar survival at discharge and long-term outcomes, compared with those who were treated with mechanical ventilation alone.
The survival rate for ECMO patients was 69.9%, and for mechanically ventilated patients it was 69.6%.
Of the 215 survivors, 66.5% had documented follow-up within 3 months of discharge from hospital. Most survivors (93.9%) were living at home; a small percentage (16.1%) had returned to work or their usual activities, and 26.2% were still using supplemental oxygen.
These rates did not differ significantly based on ECMO status and rates of physical, psychological, and cognitive deficits did not differ significantly.
“The cognitive, emotional, and physical deficits seen in survivors of critical illness from COVID-19 can only be treated if diagnosed,” Dr. Rove said.
“Detrimental effects can potentially be ameliorated with use of best practices in the ICU, maximizing acute rehabilitation services where indicated, and follow-up with providers in multidisciplinary post-ICU clinics who can assess and treat these patients to optimize survivorship,” she said.
A version of this article first appeared on Medscape.com.
Severely ill COVID-19 patients treated with extracorporeal membrane oxygenation (ECMO) had similar survival to hospital discharge and long-term outcomes as survivors treated with mechanical ventilation alone, results of a new, multicenter study suggest.
Importantly, the study also showed that survivors, regardless of the treatment they received, experienced significant deficits following their stay in the ICU and were suffering problems with physical, psychological, and cognitive functioning for months afterward.
At 3 months after discharge, 50% of the survivors reported cognitive dysfunction, ICU-acquired weakness and depression, anxiety, or PTSD; over 25% still required supplemental oxygen; and only one in six survivors were back at work.
The findings were presented April 30 at the American Association for Thoracic Surgery annual meeting.
The study represents the efforts of a multidisciplinary team that included cardiothoracic surgeons, critical care doctors, medical staff at long-term care facilities, and physical therapists in addition to other specialists. The research followed patients at five academic centers: the University of Colorado, the University of Virginia, the University of Kentucky, Johns Hopkins University, and Vanderbilt University.
“We were a multidisciplinary team, a whole variety of people to really track the long-term outcomes for patients who have been critically ill from COVID-19 and survived to hospital discharge,” presenting author Lauren J. Taylor, MD, fellow at the University of Colorado at Denver, Aurora, said in an interview.
It’s unclear currently what happens to these patients once they leave the hospital, she noted. “This is information we have not had, but when we followed these patients in these multidisciplinary clinics, there was a high level of either physical, emotional, or cognitive dysfunction, even for patients who were well enough to be living at home at the time of follow-up.
“So, if you have somebody living at home and they come into the clinic, you assume they are functioning pretty well, but when you actually provide them with cognitive and psychological testing and check their physical capabilities, you find a high degree of deficits throughout the entire cohort of this study,” she said.
The study was prompted by discussion with patients’ family members about the rationale, risks, and benefits of ECMO cannulation in patients with COVID-19 failing mechanical ventilation, senior author Jessica V. Rove, MD, also from the University of Colorado, said in an interview.
“We wanted to find out what their hospital course would be like and what cognitive, physical, or emotional deficits might they experience if they survive,” Dr. Rove said.
The investigators compared 262 mechanically ventilated patients with 46 patients cannulated for ECMO who were hospitalized between March and May 2020.
ECMO patients were younger and traveled farther but there were no significant differences in gender, race, or body mass index.
ECMO patients were mechanically ventilated for longer durations (median, 26 days vs. 13 days) and were more likely to receive inhaled pulmonary vasodilators, neuromuscular blockade, investigational COVID-19 therapies, blood transfusions, and inotropes.
They also experienced greater bleeding and clotting events (P < .01).
Despite a more complex critical illness course, patients treated with ECMO had similar survival at discharge and long-term outcomes, compared with those who were treated with mechanical ventilation alone.
The survival rate for ECMO patients was 69.9%, and for mechanically ventilated patients it was 69.6%.
Of the 215 survivors, 66.5% had documented follow-up within 3 months of discharge from hospital. Most survivors (93.9%) were living at home; a small percentage (16.1%) had returned to work or their usual activities, and 26.2% were still using supplemental oxygen.
These rates did not differ significantly based on ECMO status and rates of physical, psychological, and cognitive deficits did not differ significantly.
“The cognitive, emotional, and physical deficits seen in survivors of critical illness from COVID-19 can only be treated if diagnosed,” Dr. Rove said.
“Detrimental effects can potentially be ameliorated with use of best practices in the ICU, maximizing acute rehabilitation services where indicated, and follow-up with providers in multidisciplinary post-ICU clinics who can assess and treat these patients to optimize survivorship,” she said.
A version of this article first appeared on Medscape.com.
Remote cardio visits expand access for underserved during COVID
Remote cardiology clinic visits during COVID-19 were used more often by certain traditionally underserved patient groups, but were also associated with less frequent testing and prescribing, new research shows.
“The COVID-19 pandemic has led to an unprecedented shift in ambulatory cardiovascular care from in-person to remote visits,” lead author Neal Yuan, MD, a cardiology fellow at the Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
Their findings were published online April 5 in JAMA Network Open.
“We wanted to explore whether the transition to remote visits was associated with disparities in how patients accessed care, and also how this transition affected diagnostic test ordering and medication prescribing,” Dr. Yuan said.
The researchers used electronic health records data for all ambulatory cardiology visits at an urban, multisite health system in Los Angeles County during two periods: April 1 to Dec. 31, 2019, the pre-COVID era; and April 1 to Dec. 31, 2020, the COVID era.
The investigators compared patient characteristics and frequencies of medication ordering and cardiology-specific testing across four visit types: pre-COVID in person, used as reference; COVID-era in person; COVID-era video; and COVID-era telephone.
The study looked at 176,781 ambulatory cardiology visits. Of these visits, 87,182 were conducted in person in the pre-COVID period; 74,498 were conducted in person in the COVID era; 4,720 were COVID-era video visits; and 10,381 were COVID-era telephone visits.
In the study cohort, 79,572 patients (45.0%) were female, 127,080 patients (71.9%) were non-Hispanic White, and the mean age was 68.1 years (standard deviation, 17.0).
Patients accessing COVID-era remote visits were more likely to be Asian, Black, or Hispanic, to have private insurance, and to have cardiovascular comorbidities, such as hypertension and heart failure.
Also, patients whose visits were conducted by video were significantly younger than patients whose visits were conducted in person or by telephone (P < .001).
In addition, the study found that clinicians ordered fewer diagnostic tests, such as electrocardiograms and echocardiograms, and were less likely to order any medication, in the pre-COVID era than during the COVID era.
“If you don’t have a patient in front of you, it’s much more difficult to get a physical exam or obtain reliable vital signs,” said Dr. Yuan. Communication can sometimes be difficult, often because of technical issues, like a bad connection. “You might be more reticent to get testing or to prescribe medications if you don’t feel confident knowing what the patient’s vital signs are.”
In addition, he added, “a lot of medications used in the cardiology setting require monitoring patients’ kidney function and electrolytes, and if you can’t do that reliably, you might be more cautious about prescribing those types of medications.”
An eye-opening study
Cardiologist Nieca Goldberg, MD, medical director of the New York University Langone womens’ heart program and spokesperson for the American Heart Association, recounted her experience with telemedicine at the height of the pandemic in New York, when everything, including medical outpatient offices, had to close.
“We were experienced with telemedicine because we had started a virtual urgent care program well ahead of the pandemic,” she said. “We started using that to screen people with potential COVID symptoms so that they wouldn’t have to come into the hospital, the medical center, or to the offices and expose people. We learned that it was great to have the telemedicine option from the infectious disease standpoint, and I did visits like that for my own patient population.”
An equally if not more important finding from the study is the fact that telemedicine increased access to care among traditionally underserved demographics, she said.
“This is eye-opening, that you can actually improve access to care by doing telemedicine visits. It was really important to see that telemedicine has added benefit to the way we can see people in the health care system.”
Telemedicine visits had a positive impact at a time when people were isolated at home, Dr. Goldberg said.
“It was a way for them to connect with their doctor and in some ways it was more personal,” she added. “I actually got to meet some of my patients’ family members. It was like making a remote house call.”
Stable cardiology patients can take their blood pressure at home, weigh themselves, and take their own pulse to give an excellent set of vital signs that will indicate how they are doing, said Dr. Goldberg.
“During a remote visit, we can talk to the patient and notice whether or not they are short of breath or coughing, but we can’t listen to their heart or do an EKG or any of the traditional cardiac testing. Still, for someone who is not having symptoms and is able to reliably monitor their blood pressure and weight, a remote visit is sufficient to give you a good sense of how that patient is doing,” she said. “We can talk to them about their medications, any potential side effects, and we can use their blood pressure information to adjust their medications.”
Many patients are becoming more savvy about using tech gadgets and devices to monitor their health.
“Some of my patients were using Apple watches and the Kardia app to address their heart rate. Many had purchased inexpensive pulse oximeters to check their oxygen during the pandemic, and that also reads the pulse,” Dr. Goldberg said.
In-person visits were reserved for symptomatic cardiac patients, she explained.
“Initially during the pandemic, we did mostly telemedicine visits and we organized the office so that each cardiologist would come in 1 day a week to take care of symptomatic cardiac patients. In that way, we were able to socially distance – they provided us with [personal protective equipment]; at NYU there was no problem with that – and nobody waited in the waiting room. To this day, office issues are more efficient and people are not waiting in the waiting room,” she added. “Telemedicine improves access to health care in populations where such access is limited.”
Dr. Yuan’s research is supported by a grant from the National Institutes of Health. Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Remote cardiology clinic visits during COVID-19 were used more often by certain traditionally underserved patient groups, but were also associated with less frequent testing and prescribing, new research shows.
“The COVID-19 pandemic has led to an unprecedented shift in ambulatory cardiovascular care from in-person to remote visits,” lead author Neal Yuan, MD, a cardiology fellow at the Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
Their findings were published online April 5 in JAMA Network Open.
“We wanted to explore whether the transition to remote visits was associated with disparities in how patients accessed care, and also how this transition affected diagnostic test ordering and medication prescribing,” Dr. Yuan said.
The researchers used electronic health records data for all ambulatory cardiology visits at an urban, multisite health system in Los Angeles County during two periods: April 1 to Dec. 31, 2019, the pre-COVID era; and April 1 to Dec. 31, 2020, the COVID era.
The investigators compared patient characteristics and frequencies of medication ordering and cardiology-specific testing across four visit types: pre-COVID in person, used as reference; COVID-era in person; COVID-era video; and COVID-era telephone.
The study looked at 176,781 ambulatory cardiology visits. Of these visits, 87,182 were conducted in person in the pre-COVID period; 74,498 were conducted in person in the COVID era; 4,720 were COVID-era video visits; and 10,381 were COVID-era telephone visits.
In the study cohort, 79,572 patients (45.0%) were female, 127,080 patients (71.9%) were non-Hispanic White, and the mean age was 68.1 years (standard deviation, 17.0).
Patients accessing COVID-era remote visits were more likely to be Asian, Black, or Hispanic, to have private insurance, and to have cardiovascular comorbidities, such as hypertension and heart failure.
Also, patients whose visits were conducted by video were significantly younger than patients whose visits were conducted in person or by telephone (P < .001).
In addition, the study found that clinicians ordered fewer diagnostic tests, such as electrocardiograms and echocardiograms, and were less likely to order any medication, in the pre-COVID era than during the COVID era.
“If you don’t have a patient in front of you, it’s much more difficult to get a physical exam or obtain reliable vital signs,” said Dr. Yuan. Communication can sometimes be difficult, often because of technical issues, like a bad connection. “You might be more reticent to get testing or to prescribe medications if you don’t feel confident knowing what the patient’s vital signs are.”
In addition, he added, “a lot of medications used in the cardiology setting require monitoring patients’ kidney function and electrolytes, and if you can’t do that reliably, you might be more cautious about prescribing those types of medications.”
An eye-opening study
Cardiologist Nieca Goldberg, MD, medical director of the New York University Langone womens’ heart program and spokesperson for the American Heart Association, recounted her experience with telemedicine at the height of the pandemic in New York, when everything, including medical outpatient offices, had to close.
“We were experienced with telemedicine because we had started a virtual urgent care program well ahead of the pandemic,” she said. “We started using that to screen people with potential COVID symptoms so that they wouldn’t have to come into the hospital, the medical center, or to the offices and expose people. We learned that it was great to have the telemedicine option from the infectious disease standpoint, and I did visits like that for my own patient population.”
An equally if not more important finding from the study is the fact that telemedicine increased access to care among traditionally underserved demographics, she said.
“This is eye-opening, that you can actually improve access to care by doing telemedicine visits. It was really important to see that telemedicine has added benefit to the way we can see people in the health care system.”
Telemedicine visits had a positive impact at a time when people were isolated at home, Dr. Goldberg said.
“It was a way for them to connect with their doctor and in some ways it was more personal,” she added. “I actually got to meet some of my patients’ family members. It was like making a remote house call.”
Stable cardiology patients can take their blood pressure at home, weigh themselves, and take their own pulse to give an excellent set of vital signs that will indicate how they are doing, said Dr. Goldberg.
“During a remote visit, we can talk to the patient and notice whether or not they are short of breath or coughing, but we can’t listen to their heart or do an EKG or any of the traditional cardiac testing. Still, for someone who is not having symptoms and is able to reliably monitor their blood pressure and weight, a remote visit is sufficient to give you a good sense of how that patient is doing,” she said. “We can talk to them about their medications, any potential side effects, and we can use their blood pressure information to adjust their medications.”
Many patients are becoming more savvy about using tech gadgets and devices to monitor their health.
“Some of my patients were using Apple watches and the Kardia app to address their heart rate. Many had purchased inexpensive pulse oximeters to check their oxygen during the pandemic, and that also reads the pulse,” Dr. Goldberg said.
In-person visits were reserved for symptomatic cardiac patients, she explained.
“Initially during the pandemic, we did mostly telemedicine visits and we organized the office so that each cardiologist would come in 1 day a week to take care of symptomatic cardiac patients. In that way, we were able to socially distance – they provided us with [personal protective equipment]; at NYU there was no problem with that – and nobody waited in the waiting room. To this day, office issues are more efficient and people are not waiting in the waiting room,” she added. “Telemedicine improves access to health care in populations where such access is limited.”
Dr. Yuan’s research is supported by a grant from the National Institutes of Health. Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Remote cardiology clinic visits during COVID-19 were used more often by certain traditionally underserved patient groups, but were also associated with less frequent testing and prescribing, new research shows.
“The COVID-19 pandemic has led to an unprecedented shift in ambulatory cardiovascular care from in-person to remote visits,” lead author Neal Yuan, MD, a cardiology fellow at the Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
Their findings were published online April 5 in JAMA Network Open.
“We wanted to explore whether the transition to remote visits was associated with disparities in how patients accessed care, and also how this transition affected diagnostic test ordering and medication prescribing,” Dr. Yuan said.
The researchers used electronic health records data for all ambulatory cardiology visits at an urban, multisite health system in Los Angeles County during two periods: April 1 to Dec. 31, 2019, the pre-COVID era; and April 1 to Dec. 31, 2020, the COVID era.
The investigators compared patient characteristics and frequencies of medication ordering and cardiology-specific testing across four visit types: pre-COVID in person, used as reference; COVID-era in person; COVID-era video; and COVID-era telephone.
The study looked at 176,781 ambulatory cardiology visits. Of these visits, 87,182 were conducted in person in the pre-COVID period; 74,498 were conducted in person in the COVID era; 4,720 were COVID-era video visits; and 10,381 were COVID-era telephone visits.
In the study cohort, 79,572 patients (45.0%) were female, 127,080 patients (71.9%) were non-Hispanic White, and the mean age was 68.1 years (standard deviation, 17.0).
Patients accessing COVID-era remote visits were more likely to be Asian, Black, or Hispanic, to have private insurance, and to have cardiovascular comorbidities, such as hypertension and heart failure.
Also, patients whose visits were conducted by video were significantly younger than patients whose visits were conducted in person or by telephone (P < .001).
In addition, the study found that clinicians ordered fewer diagnostic tests, such as electrocardiograms and echocardiograms, and were less likely to order any medication, in the pre-COVID era than during the COVID era.
“If you don’t have a patient in front of you, it’s much more difficult to get a physical exam or obtain reliable vital signs,” said Dr. Yuan. Communication can sometimes be difficult, often because of technical issues, like a bad connection. “You might be more reticent to get testing or to prescribe medications if you don’t feel confident knowing what the patient’s vital signs are.”
In addition, he added, “a lot of medications used in the cardiology setting require monitoring patients’ kidney function and electrolytes, and if you can’t do that reliably, you might be more cautious about prescribing those types of medications.”
An eye-opening study
Cardiologist Nieca Goldberg, MD, medical director of the New York University Langone womens’ heart program and spokesperson for the American Heart Association, recounted her experience with telemedicine at the height of the pandemic in New York, when everything, including medical outpatient offices, had to close.
“We were experienced with telemedicine because we had started a virtual urgent care program well ahead of the pandemic,” she said. “We started using that to screen people with potential COVID symptoms so that they wouldn’t have to come into the hospital, the medical center, or to the offices and expose people. We learned that it was great to have the telemedicine option from the infectious disease standpoint, and I did visits like that for my own patient population.”
An equally if not more important finding from the study is the fact that telemedicine increased access to care among traditionally underserved demographics, she said.
“This is eye-opening, that you can actually improve access to care by doing telemedicine visits. It was really important to see that telemedicine has added benefit to the way we can see people in the health care system.”
Telemedicine visits had a positive impact at a time when people were isolated at home, Dr. Goldberg said.
“It was a way for them to connect with their doctor and in some ways it was more personal,” she added. “I actually got to meet some of my patients’ family members. It was like making a remote house call.”
Stable cardiology patients can take their blood pressure at home, weigh themselves, and take their own pulse to give an excellent set of vital signs that will indicate how they are doing, said Dr. Goldberg.
“During a remote visit, we can talk to the patient and notice whether or not they are short of breath or coughing, but we can’t listen to their heart or do an EKG or any of the traditional cardiac testing. Still, for someone who is not having symptoms and is able to reliably monitor their blood pressure and weight, a remote visit is sufficient to give you a good sense of how that patient is doing,” she said. “We can talk to them about their medications, any potential side effects, and we can use their blood pressure information to adjust their medications.”
Many patients are becoming more savvy about using tech gadgets and devices to monitor their health.
“Some of my patients were using Apple watches and the Kardia app to address their heart rate. Many had purchased inexpensive pulse oximeters to check their oxygen during the pandemic, and that also reads the pulse,” Dr. Goldberg said.
In-person visits were reserved for symptomatic cardiac patients, she explained.
“Initially during the pandemic, we did mostly telemedicine visits and we organized the office so that each cardiologist would come in 1 day a week to take care of symptomatic cardiac patients. In that way, we were able to socially distance – they provided us with [personal protective equipment]; at NYU there was no problem with that – and nobody waited in the waiting room. To this day, office issues are more efficient and people are not waiting in the waiting room,” she added. “Telemedicine improves access to health care in populations where such access is limited.”
Dr. Yuan’s research is supported by a grant from the National Institutes of Health. Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Child abuse tied to persistent inflammation in later life
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Novel oral agent effective in teens with atopic dermatitis
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.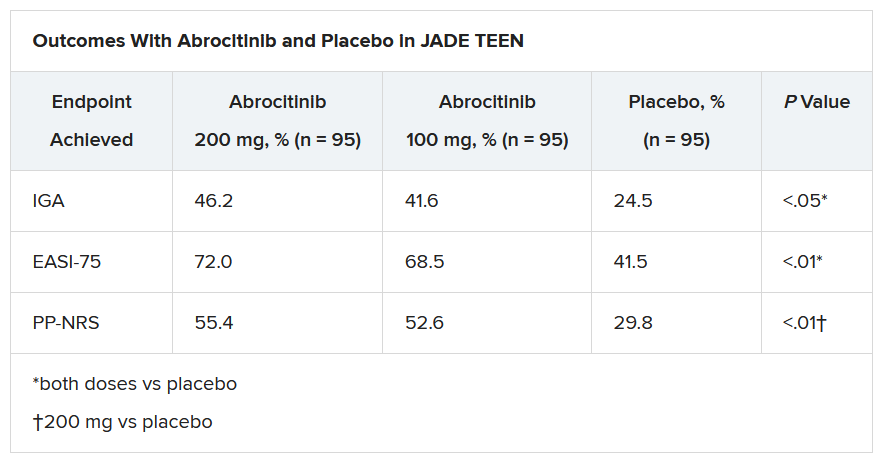
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.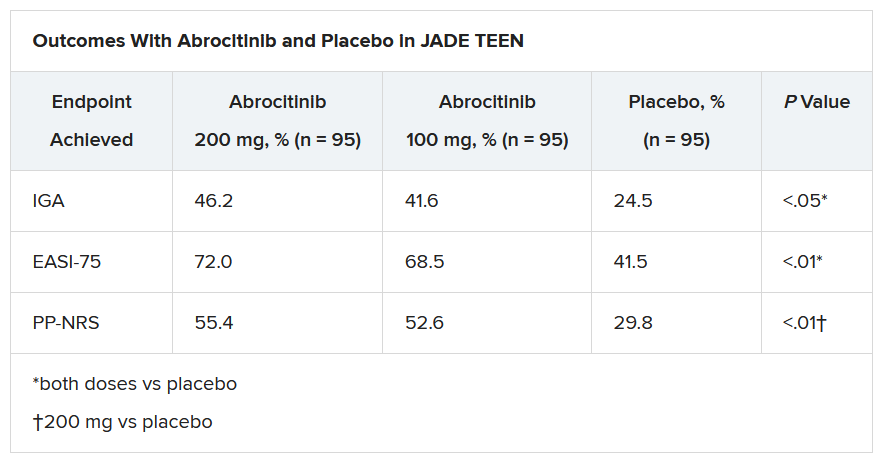
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.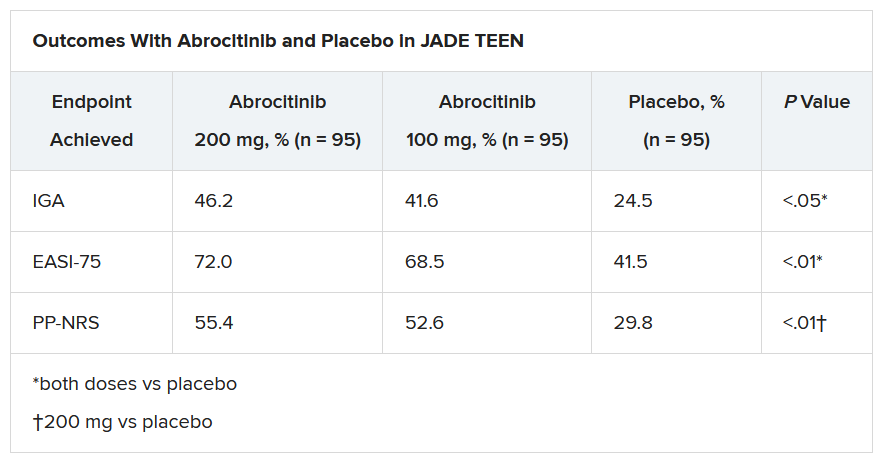
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.