User login
How to identify inducible urticaria
CHAMPIONSGATE, FLA. – Physical urticarias, also known as inducible urticarias, comprise 20%-30% of all chronic urticaria cases, and these patients are rarely responsive to corticosteroids, according to Dr. Adam Friedman.
Physical urticarias are often episodic, and spontaneous resolution is less likely in this subset of patients, compared with chronic urticaria patients overall (33% vs. 20%), said Dr. Friedman, director of dermatologic research at Albert Einstein College of Medicine in New York.
Identifying the unique source of a patient’s inducible urticarias is important because it paves the way for more successful treatment, he said at the Orlando Dermatology Aesthetic and Clinical Conference.
Causes of physical urticaria include dermatographism, cholinergic factors, heat, cold, water, sun, and vibration.
To diagnose physical urticaria, ask patients about family history and whether they have pictures documenting the urticaria episodes, Dr. Friedman said. The reaction in patients with physical urticaria is reproducible in response to environmental factors, he noted.
Dr. Friedman described several provocative tests for the most common physical urticarias.
If cold-induced urticaria is suspected, place an ice cube on the forearm to see whether hives occur after it is removed. If patients report hives after sweating or exposure to heat, the heat may be the cause; test by using localized heat (a test tube of water at 44 degrees Celsius).
Less obvious, but genuine, causes of physical urticaria include delayed pressure-induced urticaria and angioedema, which may be the culprit in patients who report swelling in the shoulder within 4-6 hours after carrying a heavy purse or other shoulder bag. To test for this trigger in the office, use a 15-pound sandbag on the target area. In cases of aquagenic urticaria, patients develop hives with exposure to water, which can be reproduced with a wet compress. And, believe it or not, individuals can develop vibratory-induced urticaria on the hands after mowing the lawn (this one is harder to reproduce in the office).
For physical urticaria, as with any type, "Make sure you have the right diagnosis," Dr. Friedman said. The patient may come in without anything on the skin, complaining of episodes of hives. The urticarial differential diagnosis is quite extensive, so a good history is important to clinching the diagnosis.
Biopsies and lab tests aren’t usually helpful for physical urticarias, Dr. Friedman said, "but if something suggests a workup, go after it."
The treatment of physical urticaria can be complicated, and includes both avoiding triggers (if possible) and managing the inflammatory response. The first-line preference is high-dose, second-generation H1 antihistamines. "You can go as high as fourfold the recommended daily dose," Dr. Friedman said.
"Don’t be afraid to try some off-label uses for recalcitrant physical urticarias," advised Dr. Friedman. Options for cold urticarias, for example, include zafirlukast, montelukast, and omalizumab. Although omalizumab is currently used off label for these patients, its approval by the FDA is expected later this year, Dr. Friedman said. "This is a very exciting time, with this new therapy at our fingertips," he added.
For patients with aquagenic urticaria, stanozolol has shown some efficacy, as well as narrow-band UVB or PUVA photochemotherapy. Potential treatments for patients with delayed-pressure urticaria include NSAIDs, dapsone, sulfasalazine, antimalarials, and even intravenous immunoglobulin. Systemic steroids should be avoided as a go-to solution, but can help bridge a patient onto a nonsteroidal immunosuppressant that has a slow onset of action.
In managing physical urticarias, as with urticarias in general, "climb the therapeutic ladder, and remember that combination therapy is king," Dr. Friedman said.
He disclosed ties with Onset, Valeant, and other companies.
CHAMPIONSGATE, FLA. – Physical urticarias, also known as inducible urticarias, comprise 20%-30% of all chronic urticaria cases, and these patients are rarely responsive to corticosteroids, according to Dr. Adam Friedman.
Physical urticarias are often episodic, and spontaneous resolution is less likely in this subset of patients, compared with chronic urticaria patients overall (33% vs. 20%), said Dr. Friedman, director of dermatologic research at Albert Einstein College of Medicine in New York.
Identifying the unique source of a patient’s inducible urticarias is important because it paves the way for more successful treatment, he said at the Orlando Dermatology Aesthetic and Clinical Conference.
Causes of physical urticaria include dermatographism, cholinergic factors, heat, cold, water, sun, and vibration.
To diagnose physical urticaria, ask patients about family history and whether they have pictures documenting the urticaria episodes, Dr. Friedman said. The reaction in patients with physical urticaria is reproducible in response to environmental factors, he noted.
Dr. Friedman described several provocative tests for the most common physical urticarias.
If cold-induced urticaria is suspected, place an ice cube on the forearm to see whether hives occur after it is removed. If patients report hives after sweating or exposure to heat, the heat may be the cause; test by using localized heat (a test tube of water at 44 degrees Celsius).
Less obvious, but genuine, causes of physical urticaria include delayed pressure-induced urticaria and angioedema, which may be the culprit in patients who report swelling in the shoulder within 4-6 hours after carrying a heavy purse or other shoulder bag. To test for this trigger in the office, use a 15-pound sandbag on the target area. In cases of aquagenic urticaria, patients develop hives with exposure to water, which can be reproduced with a wet compress. And, believe it or not, individuals can develop vibratory-induced urticaria on the hands after mowing the lawn (this one is harder to reproduce in the office).
For physical urticaria, as with any type, "Make sure you have the right diagnosis," Dr. Friedman said. The patient may come in without anything on the skin, complaining of episodes of hives. The urticarial differential diagnosis is quite extensive, so a good history is important to clinching the diagnosis.
Biopsies and lab tests aren’t usually helpful for physical urticarias, Dr. Friedman said, "but if something suggests a workup, go after it."
The treatment of physical urticaria can be complicated, and includes both avoiding triggers (if possible) and managing the inflammatory response. The first-line preference is high-dose, second-generation H1 antihistamines. "You can go as high as fourfold the recommended daily dose," Dr. Friedman said.
"Don’t be afraid to try some off-label uses for recalcitrant physical urticarias," advised Dr. Friedman. Options for cold urticarias, for example, include zafirlukast, montelukast, and omalizumab. Although omalizumab is currently used off label for these patients, its approval by the FDA is expected later this year, Dr. Friedman said. "This is a very exciting time, with this new therapy at our fingertips," he added.
For patients with aquagenic urticaria, stanozolol has shown some efficacy, as well as narrow-band UVB or PUVA photochemotherapy. Potential treatments for patients with delayed-pressure urticaria include NSAIDs, dapsone, sulfasalazine, antimalarials, and even intravenous immunoglobulin. Systemic steroids should be avoided as a go-to solution, but can help bridge a patient onto a nonsteroidal immunosuppressant that has a slow onset of action.
In managing physical urticarias, as with urticarias in general, "climb the therapeutic ladder, and remember that combination therapy is king," Dr. Friedman said.
He disclosed ties with Onset, Valeant, and other companies.
CHAMPIONSGATE, FLA. – Physical urticarias, also known as inducible urticarias, comprise 20%-30% of all chronic urticaria cases, and these patients are rarely responsive to corticosteroids, according to Dr. Adam Friedman.
Physical urticarias are often episodic, and spontaneous resolution is less likely in this subset of patients, compared with chronic urticaria patients overall (33% vs. 20%), said Dr. Friedman, director of dermatologic research at Albert Einstein College of Medicine in New York.
Identifying the unique source of a patient’s inducible urticarias is important because it paves the way for more successful treatment, he said at the Orlando Dermatology Aesthetic and Clinical Conference.
Causes of physical urticaria include dermatographism, cholinergic factors, heat, cold, water, sun, and vibration.
To diagnose physical urticaria, ask patients about family history and whether they have pictures documenting the urticaria episodes, Dr. Friedman said. The reaction in patients with physical urticaria is reproducible in response to environmental factors, he noted.
Dr. Friedman described several provocative tests for the most common physical urticarias.
If cold-induced urticaria is suspected, place an ice cube on the forearm to see whether hives occur after it is removed. If patients report hives after sweating or exposure to heat, the heat may be the cause; test by using localized heat (a test tube of water at 44 degrees Celsius).
Less obvious, but genuine, causes of physical urticaria include delayed pressure-induced urticaria and angioedema, which may be the culprit in patients who report swelling in the shoulder within 4-6 hours after carrying a heavy purse or other shoulder bag. To test for this trigger in the office, use a 15-pound sandbag on the target area. In cases of aquagenic urticaria, patients develop hives with exposure to water, which can be reproduced with a wet compress. And, believe it or not, individuals can develop vibratory-induced urticaria on the hands after mowing the lawn (this one is harder to reproduce in the office).
For physical urticaria, as with any type, "Make sure you have the right diagnosis," Dr. Friedman said. The patient may come in without anything on the skin, complaining of episodes of hives. The urticarial differential diagnosis is quite extensive, so a good history is important to clinching the diagnosis.
Biopsies and lab tests aren’t usually helpful for physical urticarias, Dr. Friedman said, "but if something suggests a workup, go after it."
The treatment of physical urticaria can be complicated, and includes both avoiding triggers (if possible) and managing the inflammatory response. The first-line preference is high-dose, second-generation H1 antihistamines. "You can go as high as fourfold the recommended daily dose," Dr. Friedman said.
"Don’t be afraid to try some off-label uses for recalcitrant physical urticarias," advised Dr. Friedman. Options for cold urticarias, for example, include zafirlukast, montelukast, and omalizumab. Although omalizumab is currently used off label for these patients, its approval by the FDA is expected later this year, Dr. Friedman said. "This is a very exciting time, with this new therapy at our fingertips," he added.
For patients with aquagenic urticaria, stanozolol has shown some efficacy, as well as narrow-band UVB or PUVA photochemotherapy. Potential treatments for patients with delayed-pressure urticaria include NSAIDs, dapsone, sulfasalazine, antimalarials, and even intravenous immunoglobulin. Systemic steroids should be avoided as a go-to solution, but can help bridge a patient onto a nonsteroidal immunosuppressant that has a slow onset of action.
In managing physical urticarias, as with urticarias in general, "climb the therapeutic ladder, and remember that combination therapy is king," Dr. Friedman said.
He disclosed ties with Onset, Valeant, and other companies.
AT THE ODAC CONFERENCE
Survey: Anti-MRSA drugs routinely prescribed for simple abscesses
Nearly 90% of more than 500 dermatologists surveyed said they would initially prescribe an antibiotic to cover possible methicillin-resistant Staphylococcus aureus when incising and draining an uncomplicated cutaneous abscess. Further, 24% reported prescribing antibiotics that are not active against the pathogen, and 82% said they cultured simple abscesses in 50% of cases.
The survey findings, while limited by their self-reporting nature, point to the need for clearer guidelines on the best approaches to simple abscesses.
"A comprehensive clinical guideline based on local antimicrobial rates, and increased knowledge of local resistance patterns and microbiologic data could not only improve abscess management and antibacterial stewardship, but could also combat the rising health care costs associated with SSTIs [skin and soft tissue infections] and their complications," wrote Dr. Adam Friedman and his colleagues in the February issue of the Journal of Drugs in Dermatology.
Simple excision and drainage (I&D) is the standard treatment for an uncomplicated skin abscess. With the increase in community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) as the culprit behind SSTIs in the United States, the Centers for Disease Control and Prevention recommends that health professionals consider CA-MRSA in all cases of skin abscesses, perform I&D, and use culture results to guide treatment, the researchers noted.
Guidelines from the Infectious Diseases Society of America recommend antibiotics for abscesses after I&D in certain circumstances, and coverage in the outpatient setting if needed. IDSA and other organizations currently recommend empiric coverage of CA-MRSA for acute bacterial skin and skin structure infections if and when antibiotics are incorporated into the therapeutic regimen (Clin. Infect. Dis. 2011;52: e18-e55).
The IDSA guidelines do not recommend culture for simple abscesses; however, 82% of the survey respondents said they cultured simple abscesses more than 50% of the time.
Overall, 459 respondents said that, for an uncomplicated abscess, they would initially prescribe an antibiotic that would cover methicillin-resistant Staphylococcus aureus (MRSA). Tetracycline class antibiotics were the top choice (35%), while 27% of respondents said they would use trimethoprim sulfamethoxazole. Interestingly, 24% said they would use a beta-lactam or cephalosporin, which do not cover MRSA, noted Dr. Friedman, of Montefiore–Albert Einstein College of Medicine, New York, and his colleagues.
To assess dermatologists’ perceptions about the treatment of cutaneous abscesses, the researchers used data from 510 board-certified dermatologists who responded to a 28-question survey via e-mail during May-June 2012. Approximately half (49%) of the respondents practiced primarily in urban settings, 42% in suburban settings, and 9% in rural settings; 53% were in private practice, and 32% worked in an academic setting. Surveys from physicians in training and incomplete surveys were excluded (J. Drugs Dermatol. 2014;13:611-16).
The survey involved a clinical scenario of a 2-cm nondraining abscess in a previously healthy patient, and respondents were asked to consider management strategies depending on the location of the abscess (face, trunk, and fronts and backs of hands and feet) and the age of the patient (6 months, 3 years, 15 years, 50 years, and 82 years).
"As the age of the patient in the clinical scenario rose, the respondents reported an increased likelihood of incorporating I&D into treatment," the researchers wrote.
"Respondents were significantly less likely to do I&D on a 6-month-old than a 3-year-old, a 3-year-old than a 15-year-old, a 15-year-old than a 50-year-old, and a 50-year-old than an 82-year-old," they noted. These differences were statistically significant between each jump in age.
The likelihood of incorporating I&D into treatment for truncal and distal lower extremities increased between each age group, with a trend toward significance, but the differences were not significant.
Of note, data from a recent study by Kemper et al. (Clin. Pediatr. [Phila.] 2011;50:525-8) showed that dermatologists were more likely than pediatricians to perform I&D on children, the researchers said.
Dr. Friedman disclosed relationships with Onset, Valeant, and other companies.
On Twitter @hsplete
Nearly 90% of more than 500 dermatologists surveyed said they would initially prescribe an antibiotic to cover possible methicillin-resistant Staphylococcus aureus when incising and draining an uncomplicated cutaneous abscess. Further, 24% reported prescribing antibiotics that are not active against the pathogen, and 82% said they cultured simple abscesses in 50% of cases.
The survey findings, while limited by their self-reporting nature, point to the need for clearer guidelines on the best approaches to simple abscesses.
"A comprehensive clinical guideline based on local antimicrobial rates, and increased knowledge of local resistance patterns and microbiologic data could not only improve abscess management and antibacterial stewardship, but could also combat the rising health care costs associated with SSTIs [skin and soft tissue infections] and their complications," wrote Dr. Adam Friedman and his colleagues in the February issue of the Journal of Drugs in Dermatology.
Simple excision and drainage (I&D) is the standard treatment for an uncomplicated skin abscess. With the increase in community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) as the culprit behind SSTIs in the United States, the Centers for Disease Control and Prevention recommends that health professionals consider CA-MRSA in all cases of skin abscesses, perform I&D, and use culture results to guide treatment, the researchers noted.
Guidelines from the Infectious Diseases Society of America recommend antibiotics for abscesses after I&D in certain circumstances, and coverage in the outpatient setting if needed. IDSA and other organizations currently recommend empiric coverage of CA-MRSA for acute bacterial skin and skin structure infections if and when antibiotics are incorporated into the therapeutic regimen (Clin. Infect. Dis. 2011;52: e18-e55).
The IDSA guidelines do not recommend culture for simple abscesses; however, 82% of the survey respondents said they cultured simple abscesses more than 50% of the time.
Overall, 459 respondents said that, for an uncomplicated abscess, they would initially prescribe an antibiotic that would cover methicillin-resistant Staphylococcus aureus (MRSA). Tetracycline class antibiotics were the top choice (35%), while 27% of respondents said they would use trimethoprim sulfamethoxazole. Interestingly, 24% said they would use a beta-lactam or cephalosporin, which do not cover MRSA, noted Dr. Friedman, of Montefiore–Albert Einstein College of Medicine, New York, and his colleagues.
To assess dermatologists’ perceptions about the treatment of cutaneous abscesses, the researchers used data from 510 board-certified dermatologists who responded to a 28-question survey via e-mail during May-June 2012. Approximately half (49%) of the respondents practiced primarily in urban settings, 42% in suburban settings, and 9% in rural settings; 53% were in private practice, and 32% worked in an academic setting. Surveys from physicians in training and incomplete surveys were excluded (J. Drugs Dermatol. 2014;13:611-16).
The survey involved a clinical scenario of a 2-cm nondraining abscess in a previously healthy patient, and respondents were asked to consider management strategies depending on the location of the abscess (face, trunk, and fronts and backs of hands and feet) and the age of the patient (6 months, 3 years, 15 years, 50 years, and 82 years).
"As the age of the patient in the clinical scenario rose, the respondents reported an increased likelihood of incorporating I&D into treatment," the researchers wrote.
"Respondents were significantly less likely to do I&D on a 6-month-old than a 3-year-old, a 3-year-old than a 15-year-old, a 15-year-old than a 50-year-old, and a 50-year-old than an 82-year-old," they noted. These differences were statistically significant between each jump in age.
The likelihood of incorporating I&D into treatment for truncal and distal lower extremities increased between each age group, with a trend toward significance, but the differences were not significant.
Of note, data from a recent study by Kemper et al. (Clin. Pediatr. [Phila.] 2011;50:525-8) showed that dermatologists were more likely than pediatricians to perform I&D on children, the researchers said.
Dr. Friedman disclosed relationships with Onset, Valeant, and other companies.
On Twitter @hsplete
Nearly 90% of more than 500 dermatologists surveyed said they would initially prescribe an antibiotic to cover possible methicillin-resistant Staphylococcus aureus when incising and draining an uncomplicated cutaneous abscess. Further, 24% reported prescribing antibiotics that are not active against the pathogen, and 82% said they cultured simple abscesses in 50% of cases.
The survey findings, while limited by their self-reporting nature, point to the need for clearer guidelines on the best approaches to simple abscesses.
"A comprehensive clinical guideline based on local antimicrobial rates, and increased knowledge of local resistance patterns and microbiologic data could not only improve abscess management and antibacterial stewardship, but could also combat the rising health care costs associated with SSTIs [skin and soft tissue infections] and their complications," wrote Dr. Adam Friedman and his colleagues in the February issue of the Journal of Drugs in Dermatology.
Simple excision and drainage (I&D) is the standard treatment for an uncomplicated skin abscess. With the increase in community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) as the culprit behind SSTIs in the United States, the Centers for Disease Control and Prevention recommends that health professionals consider CA-MRSA in all cases of skin abscesses, perform I&D, and use culture results to guide treatment, the researchers noted.
Guidelines from the Infectious Diseases Society of America recommend antibiotics for abscesses after I&D in certain circumstances, and coverage in the outpatient setting if needed. IDSA and other organizations currently recommend empiric coverage of CA-MRSA for acute bacterial skin and skin structure infections if and when antibiotics are incorporated into the therapeutic regimen (Clin. Infect. Dis. 2011;52: e18-e55).
The IDSA guidelines do not recommend culture for simple abscesses; however, 82% of the survey respondents said they cultured simple abscesses more than 50% of the time.
Overall, 459 respondents said that, for an uncomplicated abscess, they would initially prescribe an antibiotic that would cover methicillin-resistant Staphylococcus aureus (MRSA). Tetracycline class antibiotics were the top choice (35%), while 27% of respondents said they would use trimethoprim sulfamethoxazole. Interestingly, 24% said they would use a beta-lactam or cephalosporin, which do not cover MRSA, noted Dr. Friedman, of Montefiore–Albert Einstein College of Medicine, New York, and his colleagues.
To assess dermatologists’ perceptions about the treatment of cutaneous abscesses, the researchers used data from 510 board-certified dermatologists who responded to a 28-question survey via e-mail during May-June 2012. Approximately half (49%) of the respondents practiced primarily in urban settings, 42% in suburban settings, and 9% in rural settings; 53% were in private practice, and 32% worked in an academic setting. Surveys from physicians in training and incomplete surveys were excluded (J. Drugs Dermatol. 2014;13:611-16).
The survey involved a clinical scenario of a 2-cm nondraining abscess in a previously healthy patient, and respondents were asked to consider management strategies depending on the location of the abscess (face, trunk, and fronts and backs of hands and feet) and the age of the patient (6 months, 3 years, 15 years, 50 years, and 82 years).
"As the age of the patient in the clinical scenario rose, the respondents reported an increased likelihood of incorporating I&D into treatment," the researchers wrote.
"Respondents were significantly less likely to do I&D on a 6-month-old than a 3-year-old, a 3-year-old than a 15-year-old, a 15-year-old than a 50-year-old, and a 50-year-old than an 82-year-old," they noted. These differences were statistically significant between each jump in age.
The likelihood of incorporating I&D into treatment for truncal and distal lower extremities increased between each age group, with a trend toward significance, but the differences were not significant.
Of note, data from a recent study by Kemper et al. (Clin. Pediatr. [Phila.] 2011;50:525-8) showed that dermatologists were more likely than pediatricians to perform I&D on children, the researchers said.
Dr. Friedman disclosed relationships with Onset, Valeant, and other companies.
On Twitter @hsplete
FROM THE JOURNAL OF DRUGS IN DERMATOLOGY
Major finding: Ninety percent of dermatologists surveyed said they would prescribe an antibiotic that would cover MRSA when faced with an uncomplicated cutaneous abscess.
Data source: E-mail survey responses from 510 board-certified dermatologists
Disclosures: Dr. Friedman disclosed relationships with Onset, Valeant, and other companies.
Botulinum toxin tantalizes as a rosacea tamer
CHAMPIONSGATE, FLA. – Injections of botulinum neurotoxin type A on the nose, cheeks, and chin can significantly improve the appearance of some rosacea patients, in part by reducing overactivity of the sebaceous gland, according to Dr. Erin Gilbert of SUNY Downstate Medical Center, New York.
"I have had remarkably consistent results" using neuromodulators to treat patients with papulopustular and erythematotelangiectatic rosacea, Dr. Gilbert said in a presentation at the Orlando Dermatology Aesthetic and Clinical Conference.
Current therapies for rosacea include topical antibiotics, azelaic acid, metronidazole, sodium sulfacetamide, and the recently approved brimonidine, Dr. Gilbert said. Subantimicrobially dosed doxycycline remains the first and only oral therapy currently approved by the Food and Drug Administration, she noted.
Botulinum toxin represents a cutting-edge treatment option for rosacea that capitalizes on the skin’s biochemistry: Specific neuropeptide genes are up- or downregulated in rosacea patients, explained Dr. Gilbert, who also holds a Ph.D. in neural and behavioral sciences.
In addition, the expression of non-neuronal transient receptor potential (TRPV2, 3, and 4) ion channels is differentially upregulated in phymatous, erythematotelangiectatic, and papulopustular rosacea subtypes, she said.
When botulinum toxin type A is injected in the nose, cheeks, and chin of rosacea patients, the sebaceous gland activity and vasodilatory responses decrease. This translates to clinical findings, including reduced flushing and oil production, decreased inflammatory lesion counts, and reduced pore size, said Dr. Gilbert.
"The question is, what’s the mechanism?" she said. The answer: "Rosacea is likely improving when nerves stop talking to blood vessels and to the immune system."
For what it is worth, histology on patients with papulopustular and erythematotelangiectatic rosacea shows significant fibrosis, she noted.
Additional research is needed, but Dr. Steven H. Dayan of the University of Illinois, Chicago, and his colleagues published data on a short series of 13 patients in the Journal of Drugs in Dermatology. Their data showed substantial reduction of flushing, redness, and inflammation within a week of treatment, with effects lasting up to 3 months. No adverse events were reported (J. Drugs Dermatol. 2012;11:e76-e79).
To treat rosacea patients with botulinum toxin type A, "you have to map out the treatment area," Dr. Gilbert said. She uses 0.5-2 units in intradermal blebs spaced 1 cm apart.
She has observed improvements at 7-14 days after a single treatment, with a maximum effect evident in 2-8 weeks, but with effects persisting for an average of 4-6 months and sometimes as long as 7 months.
Her additional treatment pearls include reconstituting each of the three FDA-approved neurotoxins with 1 cc of saline, and using small syringes. She generally injects 7-10 units per cheek. "Don’t forget to treat the nose," she said.
Botulinum toxin type A (onabotulinumtoxinA) is not approved by the FDA to treat rosacea, but a randomized, double-blind, placebo-controlled pilot study comparing incobotulinumtoxinA to placebo for the treatment of rosacea is underway, conducted by Dr. Dayan and sponsored by Merz Pharmaceuticals.
Dr. Gilbert has served as a consultant for Merz Aesthetics, Allergan, and Medicis Aesthetics, and as a consultant and speaker for Johnson & Johnston and Glytone.
On Twitter @hsplete
CHAMPIONSGATE, FLA. – Injections of botulinum neurotoxin type A on the nose, cheeks, and chin can significantly improve the appearance of some rosacea patients, in part by reducing overactivity of the sebaceous gland, according to Dr. Erin Gilbert of SUNY Downstate Medical Center, New York.
"I have had remarkably consistent results" using neuromodulators to treat patients with papulopustular and erythematotelangiectatic rosacea, Dr. Gilbert said in a presentation at the Orlando Dermatology Aesthetic and Clinical Conference.
Current therapies for rosacea include topical antibiotics, azelaic acid, metronidazole, sodium sulfacetamide, and the recently approved brimonidine, Dr. Gilbert said. Subantimicrobially dosed doxycycline remains the first and only oral therapy currently approved by the Food and Drug Administration, she noted.
Botulinum toxin represents a cutting-edge treatment option for rosacea that capitalizes on the skin’s biochemistry: Specific neuropeptide genes are up- or downregulated in rosacea patients, explained Dr. Gilbert, who also holds a Ph.D. in neural and behavioral sciences.
In addition, the expression of non-neuronal transient receptor potential (TRPV2, 3, and 4) ion channels is differentially upregulated in phymatous, erythematotelangiectatic, and papulopustular rosacea subtypes, she said.
When botulinum toxin type A is injected in the nose, cheeks, and chin of rosacea patients, the sebaceous gland activity and vasodilatory responses decrease. This translates to clinical findings, including reduced flushing and oil production, decreased inflammatory lesion counts, and reduced pore size, said Dr. Gilbert.
"The question is, what’s the mechanism?" she said. The answer: "Rosacea is likely improving when nerves stop talking to blood vessels and to the immune system."
For what it is worth, histology on patients with papulopustular and erythematotelangiectatic rosacea shows significant fibrosis, she noted.
Additional research is needed, but Dr. Steven H. Dayan of the University of Illinois, Chicago, and his colleagues published data on a short series of 13 patients in the Journal of Drugs in Dermatology. Their data showed substantial reduction of flushing, redness, and inflammation within a week of treatment, with effects lasting up to 3 months. No adverse events were reported (J. Drugs Dermatol. 2012;11:e76-e79).
To treat rosacea patients with botulinum toxin type A, "you have to map out the treatment area," Dr. Gilbert said. She uses 0.5-2 units in intradermal blebs spaced 1 cm apart.
She has observed improvements at 7-14 days after a single treatment, with a maximum effect evident in 2-8 weeks, but with effects persisting for an average of 4-6 months and sometimes as long as 7 months.
Her additional treatment pearls include reconstituting each of the three FDA-approved neurotoxins with 1 cc of saline, and using small syringes. She generally injects 7-10 units per cheek. "Don’t forget to treat the nose," she said.
Botulinum toxin type A (onabotulinumtoxinA) is not approved by the FDA to treat rosacea, but a randomized, double-blind, placebo-controlled pilot study comparing incobotulinumtoxinA to placebo for the treatment of rosacea is underway, conducted by Dr. Dayan and sponsored by Merz Pharmaceuticals.
Dr. Gilbert has served as a consultant for Merz Aesthetics, Allergan, and Medicis Aesthetics, and as a consultant and speaker for Johnson & Johnston and Glytone.
On Twitter @hsplete
CHAMPIONSGATE, FLA. – Injections of botulinum neurotoxin type A on the nose, cheeks, and chin can significantly improve the appearance of some rosacea patients, in part by reducing overactivity of the sebaceous gland, according to Dr. Erin Gilbert of SUNY Downstate Medical Center, New York.
"I have had remarkably consistent results" using neuromodulators to treat patients with papulopustular and erythematotelangiectatic rosacea, Dr. Gilbert said in a presentation at the Orlando Dermatology Aesthetic and Clinical Conference.
Current therapies for rosacea include topical antibiotics, azelaic acid, metronidazole, sodium sulfacetamide, and the recently approved brimonidine, Dr. Gilbert said. Subantimicrobially dosed doxycycline remains the first and only oral therapy currently approved by the Food and Drug Administration, she noted.
Botulinum toxin represents a cutting-edge treatment option for rosacea that capitalizes on the skin’s biochemistry: Specific neuropeptide genes are up- or downregulated in rosacea patients, explained Dr. Gilbert, who also holds a Ph.D. in neural and behavioral sciences.
In addition, the expression of non-neuronal transient receptor potential (TRPV2, 3, and 4) ion channels is differentially upregulated in phymatous, erythematotelangiectatic, and papulopustular rosacea subtypes, she said.
When botulinum toxin type A is injected in the nose, cheeks, and chin of rosacea patients, the sebaceous gland activity and vasodilatory responses decrease. This translates to clinical findings, including reduced flushing and oil production, decreased inflammatory lesion counts, and reduced pore size, said Dr. Gilbert.
"The question is, what’s the mechanism?" she said. The answer: "Rosacea is likely improving when nerves stop talking to blood vessels and to the immune system."
For what it is worth, histology on patients with papulopustular and erythematotelangiectatic rosacea shows significant fibrosis, she noted.
Additional research is needed, but Dr. Steven H. Dayan of the University of Illinois, Chicago, and his colleagues published data on a short series of 13 patients in the Journal of Drugs in Dermatology. Their data showed substantial reduction of flushing, redness, and inflammation within a week of treatment, with effects lasting up to 3 months. No adverse events were reported (J. Drugs Dermatol. 2012;11:e76-e79).
To treat rosacea patients with botulinum toxin type A, "you have to map out the treatment area," Dr. Gilbert said. She uses 0.5-2 units in intradermal blebs spaced 1 cm apart.
She has observed improvements at 7-14 days after a single treatment, with a maximum effect evident in 2-8 weeks, but with effects persisting for an average of 4-6 months and sometimes as long as 7 months.
Her additional treatment pearls include reconstituting each of the three FDA-approved neurotoxins with 1 cc of saline, and using small syringes. She generally injects 7-10 units per cheek. "Don’t forget to treat the nose," she said.
Botulinum toxin type A (onabotulinumtoxinA) is not approved by the FDA to treat rosacea, but a randomized, double-blind, placebo-controlled pilot study comparing incobotulinumtoxinA to placebo for the treatment of rosacea is underway, conducted by Dr. Dayan and sponsored by Merz Pharmaceuticals.
Dr. Gilbert has served as a consultant for Merz Aesthetics, Allergan, and Medicis Aesthetics, and as a consultant and speaker for Johnson & Johnston and Glytone.
On Twitter @hsplete
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
Desoximetasone spray succeeds in psoriasis studies
Significantly more psoriasis patients randomized to a 0.25% desoximetasone spray showed clinical success and treatment success, compared with those who used a placebo vehicle, based on data from a pair of phase III studies. The findings were published in the December issue of Journal of Drugs in Dermatology by Dr. Leon Kircik of Indiana University School of Medicine, Indianapolis, and his colleagues.
The study population included adults with moderate to severe plaque psoriasis. The patients used the spray twice daily for 28 days, and they were assessed at baseline and during the study using the Physician Global Assessment score and the Total Lesion Severity Score. No significant differences in adverse events were reported between the treatment and placebo groups, and no patients reported stinging or burning from the spray formulation (J. Drugs Dermatol. 2013;12:1404-10).
Significantly more psoriasis patients randomized to a 0.25% desoximetasone spray showed clinical success and treatment success, compared with those who used a placebo vehicle, based on data from a pair of phase III studies. The findings were published in the December issue of Journal of Drugs in Dermatology by Dr. Leon Kircik of Indiana University School of Medicine, Indianapolis, and his colleagues.
The study population included adults with moderate to severe plaque psoriasis. The patients used the spray twice daily for 28 days, and they were assessed at baseline and during the study using the Physician Global Assessment score and the Total Lesion Severity Score. No significant differences in adverse events were reported between the treatment and placebo groups, and no patients reported stinging or burning from the spray formulation (J. Drugs Dermatol. 2013;12:1404-10).
Significantly more psoriasis patients randomized to a 0.25% desoximetasone spray showed clinical success and treatment success, compared with those who used a placebo vehicle, based on data from a pair of phase III studies. The findings were published in the December issue of Journal of Drugs in Dermatology by Dr. Leon Kircik of Indiana University School of Medicine, Indianapolis, and his colleagues.
The study population included adults with moderate to severe plaque psoriasis. The patients used the spray twice daily for 28 days, and they were assessed at baseline and during the study using the Physician Global Assessment score and the Total Lesion Severity Score. No significant differences in adverse events were reported between the treatment and placebo groups, and no patients reported stinging or burning from the spray formulation (J. Drugs Dermatol. 2013;12:1404-10).
FROM JOURNAL OF DRUGS IN DERMATOLOGY
FDA updates clobazam label to reflect risk of severe skin reactions
The antiseizure medication clobazam can cause potentially severe skin reactions that may lead to injury and death, and the drug label has been changed to reflect this information, according to a statement issued by the Food and Drug Administration on Dec. 3.
The FDA has approved changes to the Warnings and Precautions section of the medication label and the patient Medication Guide to describe the possible reactions: Stevens-Johnson syndrome and toxic epidermal necrolysis. These reactions can occur at any time while a patient is taking clobazam (Onfi), but the risk is greatest during the first 8 weeks of treatment or when the patient has discontinued and then resumed use of the drug, the FDA said.
The label change is based in part on the results of an FDA case series of 20 patients (6 U.S. patients, including 5 children, and 14 foreign patients), in which all cases of Stevens-Johnson syndrome and toxic epidermal necrolysis associated with clobazam resulted in hospitalization; in addition, one case resulted in blindness, and another resulted in death.
"Patients should not stop taking Onfi without first talking to their health care professionals," according to the agency’s statement. "Stopping Onfi suddenly can cause serious withdrawal problems, such as seizures that will not stop, hallucinations (hearing or seeing things that are not real), shaking, nervousness, and stomach or muscle cramps."
The FDA advised health professionals to consider clobazam as a cause in patients with possible drug-induced skin reactions, and to discontinue the drug at the first sign of rash, "unless it is clearly not drug related."
Health professionals should inform patients taking clobazam, a benzodiazepine used to manage seizures in children with severe epilepsy (Lennox-Gastaut syndrome) in combination with other antiepileptic medications, to seek medical attention immediately if they develop a rash, skin blistering or peeling, hives, or sores in the mouth.
"Serious skin reactions have not generally been associated with other benzodiazepines," the FDA noted.
Since clobazam was approved in October 2011 and through September 2013, the FDA says that approximately 31,000 patients received a dispensed prescription for the drug from U.S. outpatient retail pharmacies, which account for the majority of all clobazam bottle sales. The agency also noted that clobazam has been marketed outside the United States for about 40 years under various brand names for the treatment of anxiety and seizures.
To view the complete safety announcement online, visit the FDA's website.
The antiseizure medication clobazam can cause potentially severe skin reactions that may lead to injury and death, and the drug label has been changed to reflect this information, according to a statement issued by the Food and Drug Administration on Dec. 3.
The FDA has approved changes to the Warnings and Precautions section of the medication label and the patient Medication Guide to describe the possible reactions: Stevens-Johnson syndrome and toxic epidermal necrolysis. These reactions can occur at any time while a patient is taking clobazam (Onfi), but the risk is greatest during the first 8 weeks of treatment or when the patient has discontinued and then resumed use of the drug, the FDA said.
The label change is based in part on the results of an FDA case series of 20 patients (6 U.S. patients, including 5 children, and 14 foreign patients), in which all cases of Stevens-Johnson syndrome and toxic epidermal necrolysis associated with clobazam resulted in hospitalization; in addition, one case resulted in blindness, and another resulted in death.
"Patients should not stop taking Onfi without first talking to their health care professionals," according to the agency’s statement. "Stopping Onfi suddenly can cause serious withdrawal problems, such as seizures that will not stop, hallucinations (hearing or seeing things that are not real), shaking, nervousness, and stomach or muscle cramps."
The FDA advised health professionals to consider clobazam as a cause in patients with possible drug-induced skin reactions, and to discontinue the drug at the first sign of rash, "unless it is clearly not drug related."
Health professionals should inform patients taking clobazam, a benzodiazepine used to manage seizures in children with severe epilepsy (Lennox-Gastaut syndrome) in combination with other antiepileptic medications, to seek medical attention immediately if they develop a rash, skin blistering or peeling, hives, or sores in the mouth.
"Serious skin reactions have not generally been associated with other benzodiazepines," the FDA noted.
Since clobazam was approved in October 2011 and through September 2013, the FDA says that approximately 31,000 patients received a dispensed prescription for the drug from U.S. outpatient retail pharmacies, which account for the majority of all clobazam bottle sales. The agency also noted that clobazam has been marketed outside the United States for about 40 years under various brand names for the treatment of anxiety and seizures.
To view the complete safety announcement online, visit the FDA's website.
The antiseizure medication clobazam can cause potentially severe skin reactions that may lead to injury and death, and the drug label has been changed to reflect this information, according to a statement issued by the Food and Drug Administration on Dec. 3.
The FDA has approved changes to the Warnings and Precautions section of the medication label and the patient Medication Guide to describe the possible reactions: Stevens-Johnson syndrome and toxic epidermal necrolysis. These reactions can occur at any time while a patient is taking clobazam (Onfi), but the risk is greatest during the first 8 weeks of treatment or when the patient has discontinued and then resumed use of the drug, the FDA said.
The label change is based in part on the results of an FDA case series of 20 patients (6 U.S. patients, including 5 children, and 14 foreign patients), in which all cases of Stevens-Johnson syndrome and toxic epidermal necrolysis associated with clobazam resulted in hospitalization; in addition, one case resulted in blindness, and another resulted in death.
"Patients should not stop taking Onfi without first talking to their health care professionals," according to the agency’s statement. "Stopping Onfi suddenly can cause serious withdrawal problems, such as seizures that will not stop, hallucinations (hearing or seeing things that are not real), shaking, nervousness, and stomach or muscle cramps."
The FDA advised health professionals to consider clobazam as a cause in patients with possible drug-induced skin reactions, and to discontinue the drug at the first sign of rash, "unless it is clearly not drug related."
Health professionals should inform patients taking clobazam, a benzodiazepine used to manage seizures in children with severe epilepsy (Lennox-Gastaut syndrome) in combination with other antiepileptic medications, to seek medical attention immediately if they develop a rash, skin blistering or peeling, hives, or sores in the mouth.
"Serious skin reactions have not generally been associated with other benzodiazepines," the FDA noted.
Since clobazam was approved in October 2011 and through September 2013, the FDA says that approximately 31,000 patients received a dispensed prescription for the drug from U.S. outpatient retail pharmacies, which account for the majority of all clobazam bottle sales. The agency also noted that clobazam has been marketed outside the United States for about 40 years under various brand names for the treatment of anxiety and seizures.
To view the complete safety announcement online, visit the FDA's website.
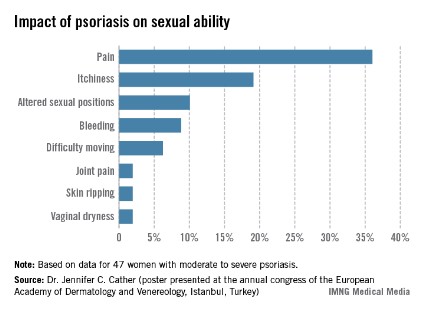
Impact of psoriasis on sexual activity
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
One third of a group of women with psoriasis reported that the pain associated with their condition interfered with their sexual activity, according to findings from a survey presented by Dr. Jennifer C. Cather.
Based on responses from a survey of 60 women with moderate to severe psoriasis, the specific complaints that were the most common ways in which psoriasis interfered with sexual activity were itchiness (19%), the need to adjust sexual position (10%), and bleeding (9%), Dr. Cather reported at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. The survey was part of an effort to determine the impact of psoriasis on women’s sexual activity, desires, and relationships.
The data were previously presented in a poster at the annual congress of the European Academy of Dermatology and Venereology (Istanbul.
SDEF and this news organization are owned by Frontline Medical Communications. Dr. Cather disclosed that she is a consultant, speaker, or researcher for AbbVie, Novartis, Leo, Janssen, Amgen, Celgene, Merck, and Pfizer.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Patient Education on Heart Failure Risk is Crucial in Psoriasis
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Patient education on heart failure risk is crucial in psoriasis
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
As evidence supporting an association between psoriasis and cardiovascular disease continues to mount, dermatologists may be the first line of defense in lowering heart failure risk.
"The increased risk of cardiovascular disease for patients with psoriasis may be of a similar magnitude as other well-described CV risk factors, such as uncontrolled hypertension," said Dr. Bruce E. Strober of the University of Connecticut, Farmington. "Further, epidemiological studies show that psoriasis patients have a shortened life expectancy, likely as a result of their experience with CV comorbitidies."
Patient education is essential, he noted at the Skin Disease Education Foundation’s annual Las Vegas dermatology seminar. "At the very least, dermatologists should alert patients of the link between psoriasis and CV disease, and remind these patients of the necessity of having a primary care physician who monitors conventional risk factors of CV disease. Patients should be reminded that psoriasis is ‘systemic disease of inflammation’ that creates risks beyond the skin and may shorten life expectancy."
"Dermatologists who care for moderate to severe psoriasis patients should measure blood pressure and draw baseline blood tests assessing for abnormalities of cholesterol, triglycerides, kidney function, liver function, and blood glucose. Abnormalities should prompt an appropriate referral to a primary care physician," he noted.
In a population-based Dutch study presented at the annual congress of the European Society of Cardiology in September, adults with mild psoriasis developed 4.02 cases of new-onset heart failure per 1,000 person-years of follow-up, compared with 4.50/1,000 person-years in patients with severe psoriasis; both of which were significantly higher than the rate of 2.27/1,000 person-years in the general population.
Data from a 2006 study found that diabetes, hypertension, hyperlipidemia, and obesity were more prevalent in psoriasis patients, when compared with controls (J. Am. Acad. Dermatol. 2006;55:829-35). Diabetes and obesity were significantly more prevalent in patients with severe psoriasis, compared with patients with mild psoriasis.
Although the reasons for the increased cardiovascular risk in psoriasis patients remain unknown, possible causes include the use of dyslipidemic therapies, including corticosteroids, acitretin, and cyclosporine, as well as uncontrolled inflammation that could lead to endothelial dysfunction and dyslipidemia, said Dr. Strober. The prevalence of other associated and/or independent risk factors including obesity, hypertension, smoking, and alcohol misuse in psoriasis patients, also could play a role.
Dr. Strober disclosed relationships with multiple pharmaceutical companies including Abbott, Amgen, Janssen, Pfizer, Novartis, and Celgene. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Don't Brush Off Topical Therapies for Psoriasis
Biologics and systemic therapies command much of the spotlight for treating psoriasis, but topical therapy remains an effective option for many psoriasis patients, according to Dr. Linda Stein Gold.
In fact, up to 80% of psoriasis patients can be adequately treated with topical therapy (N. Engl. J. Med. 2005;352:1899-912), said Dr. Stein Gold at the Skin Disease Education Foundation’s (SDEF’s) annual Las Vegas dermatology seminar.
She offered several principles to help clinicians make the most of topical therapies by troubleshooting potential problems.
• Check the amount. One gram of most topical psoriasis products covers 4% of body surface area per application, so a 60-gram tube should treat 4% of body surface area for a month, said Dr. Stein Gold, citing guidelines developed by Dr. Alan Menter and his colleagues and approved by the American Academy of Dermatology in 2009.
• Don’t miss corticosteroid allergies. "We are missing this," said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital in Detroit. Suspect a possible allergy if a patient returns with a worsening rash after using hydrocortisone, for example. Data have shown that between 0.2% and 5% of all dermatitis patients have a steroid allergy. "Allergy to the active molecule or to the vehicle should be suspected in all patients who don’t respond as expected to topical steroids," she noted.
• Visit (or revisit) vitamin D. Another plus for topical therapy is the usefulness of topical vitamin D for tricky areas, such as the forehead, armpit, groin, and the area behind the ears. Data from a randomized trial of 75 patients found calcitriol ointment to be significantly more effective against target lesions and better tolerated by patients than calcipotriene ointment (Br. J. Dermatol. 2003;148:326-33).
• Don’t forget coal tar. Simple, but effective, coal tar is a proven safe topical psoriasis treatment and is available in several vehicles, including solution and foam. Data from a study of more than 13,000 patients with psoriasis and eczema found that coal tar was safe, and that it did not increase the risk for skin cancer (J. Invest. Dermatol. 2010;130:953-61).
The future of topical psoriasis therapy is not static, said Dr. Stein Gold. New molecules – notably topical Janus kinase inhibitors and phosphodiesterase-4 inhibitors – are currently being explored in clinical trials.
Dr. Stein Gold disclosed relationships with Leo, Medicis, and other companies. SDEF and this news organization are owned by Frontline Medical Communications.
Biologics and systemic therapies command much of the spotlight for treating psoriasis, but topical therapy remains an effective option for many psoriasis patients, according to Dr. Linda Stein Gold.
In fact, up to 80% of psoriasis patients can be adequately treated with topical therapy (N. Engl. J. Med. 2005;352:1899-912), said Dr. Stein Gold at the Skin Disease Education Foundation’s (SDEF’s) annual Las Vegas dermatology seminar.
She offered several principles to help clinicians make the most of topical therapies by troubleshooting potential problems.
• Check the amount. One gram of most topical psoriasis products covers 4% of body surface area per application, so a 60-gram tube should treat 4% of body surface area for a month, said Dr. Stein Gold, citing guidelines developed by Dr. Alan Menter and his colleagues and approved by the American Academy of Dermatology in 2009.
• Don’t miss corticosteroid allergies. "We are missing this," said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital in Detroit. Suspect a possible allergy if a patient returns with a worsening rash after using hydrocortisone, for example. Data have shown that between 0.2% and 5% of all dermatitis patients have a steroid allergy. "Allergy to the active molecule or to the vehicle should be suspected in all patients who don’t respond as expected to topical steroids," she noted.
• Visit (or revisit) vitamin D. Another plus for topical therapy is the usefulness of topical vitamin D for tricky areas, such as the forehead, armpit, groin, and the area behind the ears. Data from a randomized trial of 75 patients found calcitriol ointment to be significantly more effective against target lesions and better tolerated by patients than calcipotriene ointment (Br. J. Dermatol. 2003;148:326-33).
• Don’t forget coal tar. Simple, but effective, coal tar is a proven safe topical psoriasis treatment and is available in several vehicles, including solution and foam. Data from a study of more than 13,000 patients with psoriasis and eczema found that coal tar was safe, and that it did not increase the risk for skin cancer (J. Invest. Dermatol. 2010;130:953-61).
The future of topical psoriasis therapy is not static, said Dr. Stein Gold. New molecules – notably topical Janus kinase inhibitors and phosphodiesterase-4 inhibitors – are currently being explored in clinical trials.
Dr. Stein Gold disclosed relationships with Leo, Medicis, and other companies. SDEF and this news organization are owned by Frontline Medical Communications.
Biologics and systemic therapies command much of the spotlight for treating psoriasis, but topical therapy remains an effective option for many psoriasis patients, according to Dr. Linda Stein Gold.
In fact, up to 80% of psoriasis patients can be adequately treated with topical therapy (N. Engl. J. Med. 2005;352:1899-912), said Dr. Stein Gold at the Skin Disease Education Foundation’s (SDEF’s) annual Las Vegas dermatology seminar.
She offered several principles to help clinicians make the most of topical therapies by troubleshooting potential problems.
• Check the amount. One gram of most topical psoriasis products covers 4% of body surface area per application, so a 60-gram tube should treat 4% of body surface area for a month, said Dr. Stein Gold, citing guidelines developed by Dr. Alan Menter and his colleagues and approved by the American Academy of Dermatology in 2009.
• Don’t miss corticosteroid allergies. "We are missing this," said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital in Detroit. Suspect a possible allergy if a patient returns with a worsening rash after using hydrocortisone, for example. Data have shown that between 0.2% and 5% of all dermatitis patients have a steroid allergy. "Allergy to the active molecule or to the vehicle should be suspected in all patients who don’t respond as expected to topical steroids," she noted.
• Visit (or revisit) vitamin D. Another plus for topical therapy is the usefulness of topical vitamin D for tricky areas, such as the forehead, armpit, groin, and the area behind the ears. Data from a randomized trial of 75 patients found calcitriol ointment to be significantly more effective against target lesions and better tolerated by patients than calcipotriene ointment (Br. J. Dermatol. 2003;148:326-33).
• Don’t forget coal tar. Simple, but effective, coal tar is a proven safe topical psoriasis treatment and is available in several vehicles, including solution and foam. Data from a study of more than 13,000 patients with psoriasis and eczema found that coal tar was safe, and that it did not increase the risk for skin cancer (J. Invest. Dermatol. 2010;130:953-61).
The future of topical psoriasis therapy is not static, said Dr. Stein Gold. New molecules – notably topical Janus kinase inhibitors and phosphodiesterase-4 inhibitors – are currently being explored in clinical trials.
Dr. Stein Gold disclosed relationships with Leo, Medicis, and other companies. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Don’t brush off topical therapies for psoriasis
Biologics and systemic therapies command much of the spotlight for treating psoriasis, but topical therapy remains an effective option for many psoriasis patients, according to Dr. Linda Stein Gold.
In fact, up to 80% of psoriasis patients can be adequately treated with topical therapy (N. Engl. J. Med. 2005;352:1899-912), said Dr. Stein Gold at the Skin Disease Education Foundation’s (SDEF’s) annual Las Vegas dermatology seminar.
She offered several principles to help clinicians make the most of topical therapies by troubleshooting potential problems.
• Check the amount. One gram of most topical psoriasis products covers 4% of body surface area per application, so a 60-gram tube should treat 4% of body surface area for a month, said Dr. Stein Gold, citing guidelines developed by Dr. Alan Menter and his colleagues and approved by the American Academy of Dermatology in 2009.
• Don’t miss corticosteroid allergies. "We are missing this," said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital in Detroit. Suspect a possible allergy if a patient returns with a worsening rash after using hydrocortisone, for example. Data have shown that between 0.2% and 5% of all dermatitis patients have a steroid allergy. "Allergy to the active molecule or to the vehicle should be suspected in all patients who don’t respond as expected to topical steroids," she noted.
• Visit (or revisit) vitamin D. Another plus for topical therapy is the usefulness of topical vitamin D for tricky areas, such as the forehead, armpit, groin, and the area behind the ears. Data from a randomized trial of 75 patients found calcitriol ointment to be significantly more effective against target lesions and better tolerated by patients than calcipotriene ointment (Br. J. Dermatol. 2003;148:326-33).
• Don’t forget coal tar. Simple, but effective, coal tar is a proven safe topical psoriasis treatment and is available in several vehicles, including solution and foam. Data from a study of more than 13,000 patients with psoriasis and eczema found that coal tar was safe, and that it did not increase the risk for skin cancer (J. Invest. Dermatol. 2010;130:953-61).
The future of topical psoriasis therapy is not static, said Dr. Stein Gold. New molecules – notably topical Janus kinase inhibitors and phosphodiesterase-4 inhibitors – are currently being explored in clinical trials.
Dr. Stein Gold disclosed relationships with Leo, Medicis, and other companies. SDEF and this news organization are owned by Frontline Medical Communications.
Biologics and systemic therapies command much of the spotlight for treating psoriasis, but topical therapy remains an effective option for many psoriasis patients, according to Dr. Linda Stein Gold.
In fact, up to 80% of psoriasis patients can be adequately treated with topical therapy (N. Engl. J. Med. 2005;352:1899-912), said Dr. Stein Gold at the Skin Disease Education Foundation’s (SDEF’s) annual Las Vegas dermatology seminar.
She offered several principles to help clinicians make the most of topical therapies by troubleshooting potential problems.
• Check the amount. One gram of most topical psoriasis products covers 4% of body surface area per application, so a 60-gram tube should treat 4% of body surface area for a month, said Dr. Stein Gold, citing guidelines developed by Dr. Alan Menter and his colleagues and approved by the American Academy of Dermatology in 2009.
• Don’t miss corticosteroid allergies. "We are missing this," said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital in Detroit. Suspect a possible allergy if a patient returns with a worsening rash after using hydrocortisone, for example. Data have shown that between 0.2% and 5% of all dermatitis patients have a steroid allergy. "Allergy to the active molecule or to the vehicle should be suspected in all patients who don’t respond as expected to topical steroids," she noted.
• Visit (or revisit) vitamin D. Another plus for topical therapy is the usefulness of topical vitamin D for tricky areas, such as the forehead, armpit, groin, and the area behind the ears. Data from a randomized trial of 75 patients found calcitriol ointment to be significantly more effective against target lesions and better tolerated by patients than calcipotriene ointment (Br. J. Dermatol. 2003;148:326-33).
• Don’t forget coal tar. Simple, but effective, coal tar is a proven safe topical psoriasis treatment and is available in several vehicles, including solution and foam. Data from a study of more than 13,000 patients with psoriasis and eczema found that coal tar was safe, and that it did not increase the risk for skin cancer (J. Invest. Dermatol. 2010;130:953-61).
The future of topical psoriasis therapy is not static, said Dr. Stein Gold. New molecules – notably topical Janus kinase inhibitors and phosphodiesterase-4 inhibitors – are currently being explored in clinical trials.
Dr. Stein Gold disclosed relationships with Leo, Medicis, and other companies. SDEF and this news organization are owned by Frontline Medical Communications.
Biologics and systemic therapies command much of the spotlight for treating psoriasis, but topical therapy remains an effective option for many psoriasis patients, according to Dr. Linda Stein Gold.
In fact, up to 80% of psoriasis patients can be adequately treated with topical therapy (N. Engl. J. Med. 2005;352:1899-912), said Dr. Stein Gold at the Skin Disease Education Foundation’s (SDEF’s) annual Las Vegas dermatology seminar.
She offered several principles to help clinicians make the most of topical therapies by troubleshooting potential problems.
• Check the amount. One gram of most topical psoriasis products covers 4% of body surface area per application, so a 60-gram tube should treat 4% of body surface area for a month, said Dr. Stein Gold, citing guidelines developed by Dr. Alan Menter and his colleagues and approved by the American Academy of Dermatology in 2009.
• Don’t miss corticosteroid allergies. "We are missing this," said Dr. Stein Gold, director of dermatology research at Henry Ford Hospital in Detroit. Suspect a possible allergy if a patient returns with a worsening rash after using hydrocortisone, for example. Data have shown that between 0.2% and 5% of all dermatitis patients have a steroid allergy. "Allergy to the active molecule or to the vehicle should be suspected in all patients who don’t respond as expected to topical steroids," she noted.
• Visit (or revisit) vitamin D. Another plus for topical therapy is the usefulness of topical vitamin D for tricky areas, such as the forehead, armpit, groin, and the area behind the ears. Data from a randomized trial of 75 patients found calcitriol ointment to be significantly more effective against target lesions and better tolerated by patients than calcipotriene ointment (Br. J. Dermatol. 2003;148:326-33).
• Don’t forget coal tar. Simple, but effective, coal tar is a proven safe topical psoriasis treatment and is available in several vehicles, including solution and foam. Data from a study of more than 13,000 patients with psoriasis and eczema found that coal tar was safe, and that it did not increase the risk for skin cancer (J. Invest. Dermatol. 2010;130:953-61).
The future of topical psoriasis therapy is not static, said Dr. Stein Gold. New molecules – notably topical Janus kinase inhibitors and phosphodiesterase-4 inhibitors – are currently being explored in clinical trials.
Dr. Stein Gold disclosed relationships with Leo, Medicis, and other companies. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR