User login
TORS: Postop bleeding risk rises with antithrombotic use
The risk of postoperative hemorrhage after transoral robotic-assisted surgery was significantly higher in patients taking antithrombotic medication than in those not taking it, based on data from 147 consecutive patients.
"Even with this small sample size, we were able to identify that increased risk was associated with antithrombotic medication use," said Dr. Scott Asher of the University of Alabama at Birmingham.
Transoral robotic-assisted surgery (TORS) is gaining in popularity among head and neck surgeons, but the potential for postop bleeding in patients taking antithrombotic medication remains a problem, Dr. Asher said at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
To assess the postop bleeding complications in TORS patients, Dr. Asher and his colleagues reviewed data from patients seen at a single tertiary academic medical center between March 2007 and September 2011.
Overall, 11 patients (8%) experienced some postop hemorrhage, but 8 of these hemorrhages (72%) occurred in patients taking antithrombotics, Dr. Asher said. Nine patients who hemorrhaged returned to the operating room for further examination and bleeding control, he noted. All postop hemorrhage events were controlled with standard techniques.
The incidence of postop hemorrhage was significantly higher among patients on antithrombotics (17%) compared with those not on antithrombotics (3%). However, no significant difference in the incidence of bleeding occurred between patients undergoing primary surgery and those undergoing salvage surgery (7% vs. 10%). Bleeding occurred an average of 11 days after surgery.
The bleeding events occurred past the time points when most patients would resume their antithrombotic medications, Dr. Asher noted.
"Our recommendation is that patients taking these meds should receive additional preop counseling when considering a TORS procedure," he said.
"A second recommendation is to collaborate preoperatively with the physicians who are prescribing," as well as the anesthesia team, to closely analyze the indications for use of antithrombotics, Dr. Asher added. "If you can safely discontinue them, you can potentially improve your TORS outcomes," he said.
Additional long-term safety and outcomes data are needed for TORS procedures, said Dr. Asher. "We are constantly reflecting on our own experience," he said. "We would encourage other institutions to collect and publish their complications-related data to continue to improve TORS outcomes."
Dr. Asher said he had no relevant financial conflicts.
The risk of postoperative hemorrhage after transoral robotic-assisted surgery was significantly higher in patients taking antithrombotic medication than in those not taking it, based on data from 147 consecutive patients.
"Even with this small sample size, we were able to identify that increased risk was associated with antithrombotic medication use," said Dr. Scott Asher of the University of Alabama at Birmingham.
Transoral robotic-assisted surgery (TORS) is gaining in popularity among head and neck surgeons, but the potential for postop bleeding in patients taking antithrombotic medication remains a problem, Dr. Asher said at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
To assess the postop bleeding complications in TORS patients, Dr. Asher and his colleagues reviewed data from patients seen at a single tertiary academic medical center between March 2007 and September 2011.
Overall, 11 patients (8%) experienced some postop hemorrhage, but 8 of these hemorrhages (72%) occurred in patients taking antithrombotics, Dr. Asher said. Nine patients who hemorrhaged returned to the operating room for further examination and bleeding control, he noted. All postop hemorrhage events were controlled with standard techniques.
The incidence of postop hemorrhage was significantly higher among patients on antithrombotics (17%) compared with those not on antithrombotics (3%). However, no significant difference in the incidence of bleeding occurred between patients undergoing primary surgery and those undergoing salvage surgery (7% vs. 10%). Bleeding occurred an average of 11 days after surgery.
The bleeding events occurred past the time points when most patients would resume their antithrombotic medications, Dr. Asher noted.
"Our recommendation is that patients taking these meds should receive additional preop counseling when considering a TORS procedure," he said.
"A second recommendation is to collaborate preoperatively with the physicians who are prescribing," as well as the anesthesia team, to closely analyze the indications for use of antithrombotics, Dr. Asher added. "If you can safely discontinue them, you can potentially improve your TORS outcomes," he said.
Additional long-term safety and outcomes data are needed for TORS procedures, said Dr. Asher. "We are constantly reflecting on our own experience," he said. "We would encourage other institutions to collect and publish their complications-related data to continue to improve TORS outcomes."
Dr. Asher said he had no relevant financial conflicts.
The risk of postoperative hemorrhage after transoral robotic-assisted surgery was significantly higher in patients taking antithrombotic medication than in those not taking it, based on data from 147 consecutive patients.
"Even with this small sample size, we were able to identify that increased risk was associated with antithrombotic medication use," said Dr. Scott Asher of the University of Alabama at Birmingham.
Transoral robotic-assisted surgery (TORS) is gaining in popularity among head and neck surgeons, but the potential for postop bleeding in patients taking antithrombotic medication remains a problem, Dr. Asher said at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
To assess the postop bleeding complications in TORS patients, Dr. Asher and his colleagues reviewed data from patients seen at a single tertiary academic medical center between March 2007 and September 2011.
Overall, 11 patients (8%) experienced some postop hemorrhage, but 8 of these hemorrhages (72%) occurred in patients taking antithrombotics, Dr. Asher said. Nine patients who hemorrhaged returned to the operating room for further examination and bleeding control, he noted. All postop hemorrhage events were controlled with standard techniques.
The incidence of postop hemorrhage was significantly higher among patients on antithrombotics (17%) compared with those not on antithrombotics (3%). However, no significant difference in the incidence of bleeding occurred between patients undergoing primary surgery and those undergoing salvage surgery (7% vs. 10%). Bleeding occurred an average of 11 days after surgery.
The bleeding events occurred past the time points when most patients would resume their antithrombotic medications, Dr. Asher noted.
"Our recommendation is that patients taking these meds should receive additional preop counseling when considering a TORS procedure," he said.
"A second recommendation is to collaborate preoperatively with the physicians who are prescribing," as well as the anesthesia team, to closely analyze the indications for use of antithrombotics, Dr. Asher added. "If you can safely discontinue them, you can potentially improve your TORS outcomes," he said.
Additional long-term safety and outcomes data are needed for TORS procedures, said Dr. Asher. "We are constantly reflecting on our own experience," he said. "We would encourage other institutions to collect and publish their complications-related data to continue to improve TORS outcomes."
Dr. Asher said he had no relevant financial conflicts.
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF OTOLARYNGOLOGY; HEAD AND NECK SURGERY FOUNDATION
Major Finding: Approximately three-quarters of patients (8 of 11) who underwent TORS and experienced some postop bleeding were on an antithrombotic medication.
Data Source: A review of 147 consecutive patients at a single surgery center.
Disclosures: Dr. Asher said he had no relevant financial conflicts.
COPD varies by state, peaks above 9%
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012;61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012;61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012;61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Major Finding: The overall prevalence of chronic obstructive pulmonary disease in the United States is approximately 6%.
Data Source: The data come from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey.
Disclosures: The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Seropositivity predicts progressive joint damage in established RA
WASHINGTON – Seropositivity for either rheumatoid factor or anti-cyclic citrullinated peptide was significantly associated with progressive joint damage in adults with established rheumatoid arthritis, based on a single-center, observational cohort study of 390 patients.
Most rheumatoid arthritis (RA) patients in clinical practice have established disease, but the predictors and proportion of disease progression in these patients has not been well studied, Dr. Siri Lillegraven of Diakonhjemmet Hospital in Oslo said at the annual meeting of the American College of Rheumatology.
Dr. Lillegraven and her colleagues reviewed data from BRASS (the Brigham and Women’s Hospital Rheumatoid Arthritis Sequential Study). Joint damage was assessed using baseline and 2-year radiographic data for patients with disease duration of at least 5 years. The average age of the patients was 60 years, 84% were women, and 44% received biologic treatment in the form of disease-modifying antirheumatic drugs (DMARDs). The median disease duration was 17 years. Disease progression was defined as a change in Sharp/van der Heijde score of 1 or more units per year.
Overall, 44% of the patients showed disease progression after 2 years. A total of 68% of the patients were positive for both rheumatoid factor (RF) and anticyclic citrullinated peptide (anti-CCP), 16% were positive for either RF or anti-CCP, and 16% were negative for both.
Seropositivity was the only significant independent predictor of disease progression after controlling for factors including age, gender, body-mass index, smoking status, treatment, DMARD use, disease duration, and presence of subcutaneous nodules, Dr. Lillegraven said.
Patients who were seropositive for either RF or anti-CCP were five times more likely than were seronegative patients to have disease progression (odds ratio 5.0), while seropositivity for both was associated with four times greater odds for disease progression (odds ratio 4.1).
"Although the odds ratios for progressive joint damage were similar if patients were positive for one or both of RF and anti-CCP, patients who were positive for both RF and anti-CCP tended to experience more joint damage," Dr. Lillegraven said. Rapid progression of joint damage (defined as a change in van der Heijde-Sharp score of 5 or more units per year) was noted in 16% patients who were seropositive for both RF and anti-CCP, compared with 9% of those who were positive for either RF or anti-CCP, although this difference was not statistically significant.
The results were limited by the use of data from a single center and by the challenge of fully adjusting for treatment in patients with established RA, Dr. Lillegraven noted. However, the findings suggest that seropositivity could be used to inform treatment decisions for these patients, she said.
Dr. Lillegraven had no financial conflicts to disclose. Several of the study coauthors disclosed relationships with multiple pharmaceutical companies, including Amgen, Abbott, Merck, and MedImmune.
WASHINGTON – Seropositivity for either rheumatoid factor or anti-cyclic citrullinated peptide was significantly associated with progressive joint damage in adults with established rheumatoid arthritis, based on a single-center, observational cohort study of 390 patients.
Most rheumatoid arthritis (RA) patients in clinical practice have established disease, but the predictors and proportion of disease progression in these patients has not been well studied, Dr. Siri Lillegraven of Diakonhjemmet Hospital in Oslo said at the annual meeting of the American College of Rheumatology.
Dr. Lillegraven and her colleagues reviewed data from BRASS (the Brigham and Women’s Hospital Rheumatoid Arthritis Sequential Study). Joint damage was assessed using baseline and 2-year radiographic data for patients with disease duration of at least 5 years. The average age of the patients was 60 years, 84% were women, and 44% received biologic treatment in the form of disease-modifying antirheumatic drugs (DMARDs). The median disease duration was 17 years. Disease progression was defined as a change in Sharp/van der Heijde score of 1 or more units per year.
Overall, 44% of the patients showed disease progression after 2 years. A total of 68% of the patients were positive for both rheumatoid factor (RF) and anticyclic citrullinated peptide (anti-CCP), 16% were positive for either RF or anti-CCP, and 16% were negative for both.
Seropositivity was the only significant independent predictor of disease progression after controlling for factors including age, gender, body-mass index, smoking status, treatment, DMARD use, disease duration, and presence of subcutaneous nodules, Dr. Lillegraven said.
Patients who were seropositive for either RF or anti-CCP were five times more likely than were seronegative patients to have disease progression (odds ratio 5.0), while seropositivity for both was associated with four times greater odds for disease progression (odds ratio 4.1).
"Although the odds ratios for progressive joint damage were similar if patients were positive for one or both of RF and anti-CCP, patients who were positive for both RF and anti-CCP tended to experience more joint damage," Dr. Lillegraven said. Rapid progression of joint damage (defined as a change in van der Heijde-Sharp score of 5 or more units per year) was noted in 16% patients who were seropositive for both RF and anti-CCP, compared with 9% of those who were positive for either RF or anti-CCP, although this difference was not statistically significant.
The results were limited by the use of data from a single center and by the challenge of fully adjusting for treatment in patients with established RA, Dr. Lillegraven noted. However, the findings suggest that seropositivity could be used to inform treatment decisions for these patients, she said.
Dr. Lillegraven had no financial conflicts to disclose. Several of the study coauthors disclosed relationships with multiple pharmaceutical companies, including Amgen, Abbott, Merck, and MedImmune.
WASHINGTON – Seropositivity for either rheumatoid factor or anti-cyclic citrullinated peptide was significantly associated with progressive joint damage in adults with established rheumatoid arthritis, based on a single-center, observational cohort study of 390 patients.
Most rheumatoid arthritis (RA) patients in clinical practice have established disease, but the predictors and proportion of disease progression in these patients has not been well studied, Dr. Siri Lillegraven of Diakonhjemmet Hospital in Oslo said at the annual meeting of the American College of Rheumatology.
Dr. Lillegraven and her colleagues reviewed data from BRASS (the Brigham and Women’s Hospital Rheumatoid Arthritis Sequential Study). Joint damage was assessed using baseline and 2-year radiographic data for patients with disease duration of at least 5 years. The average age of the patients was 60 years, 84% were women, and 44% received biologic treatment in the form of disease-modifying antirheumatic drugs (DMARDs). The median disease duration was 17 years. Disease progression was defined as a change in Sharp/van der Heijde score of 1 or more units per year.
Overall, 44% of the patients showed disease progression after 2 years. A total of 68% of the patients were positive for both rheumatoid factor (RF) and anticyclic citrullinated peptide (anti-CCP), 16% were positive for either RF or anti-CCP, and 16% were negative for both.
Seropositivity was the only significant independent predictor of disease progression after controlling for factors including age, gender, body-mass index, smoking status, treatment, DMARD use, disease duration, and presence of subcutaneous nodules, Dr. Lillegraven said.
Patients who were seropositive for either RF or anti-CCP were five times more likely than were seronegative patients to have disease progression (odds ratio 5.0), while seropositivity for both was associated with four times greater odds for disease progression (odds ratio 4.1).
"Although the odds ratios for progressive joint damage were similar if patients were positive for one or both of RF and anti-CCP, patients who were positive for both RF and anti-CCP tended to experience more joint damage," Dr. Lillegraven said. Rapid progression of joint damage (defined as a change in van der Heijde-Sharp score of 5 or more units per year) was noted in 16% patients who were seropositive for both RF and anti-CCP, compared with 9% of those who were positive for either RF or anti-CCP, although this difference was not statistically significant.
The results were limited by the use of data from a single center and by the challenge of fully adjusting for treatment in patients with established RA, Dr. Lillegraven noted. However, the findings suggest that seropositivity could be used to inform treatment decisions for these patients, she said.
Dr. Lillegraven had no financial conflicts to disclose. Several of the study coauthors disclosed relationships with multiple pharmaceutical companies, including Amgen, Abbott, Merck, and MedImmune.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: Patients with established rheumatoid arthritis and seropositivity for either RF or anti-CCP were five times more likely to have disease progression after 2 years than were seronegative patients.
Data Source: The Brigham and Women’s Hospital Rheumatoid Arthritis Sequential Study (BRASS), a single-center, observational cohort study of 390 patients.
Disclosures: Dr. Lillegraven had no financial conflicts to disclose. Several of the study coauthors disclosed relationships with multiple pharmaceutical companies including Amgen, Abbott, Merck, and MedImmune.
SurgiSIS myringoplasty shortens operative time
WASHINGTON – SurgiSIS, a material derived from porcine small intestinal mucosa, can be safely and effectively used for myringoplasty in children, based on data from a prospective, blinded study of 404 patients.
Patients’ tissue is not always available for tympanic membrane repair, and harvesting the graft may increase intraoperative time, said Dr. Riccardo D’Eredita of Vincenza (Italy) Civil Hospital. SurgiSIS (SIS) "promotes early vessel growth, provides scaffolding for remodeling tissues, and is inexpensive and ready to use." He presented the findings at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
The material has been used widely in children, and data from previous studies show that SurgiSIS is gradually replaced by host cells, said Dr. D’Eredita. After 30 days, host cells invade SurgiSIS. After 1 year, SurgiSIS is no longer evident, and has been replaced by the patients’ collagen.
In this study, 404 children underwent tympanic membrane repair in 432 ears; 217 were randomized to myringoplasty with SurgiSIS and 215 were randomized to repair using the patients’ own temporalis fascia.
Overall, the group without SurgiSIS had a 97% rate of stable closures and the group with SurgiSIS had a 95% rate. Surgical time was approximately 15 minutes less for SurgiSIS-treated patients, Dr. D’Eredita said.
The researchers assessed the healing of the tympanic membranes over a 10-year period and found comparable reduction of inflammation in the two groups. There were no adverse reactions in the SIS group.
Dr. D’Eredita had no financial conflicts to disclose.
WASHINGTON – SurgiSIS, a material derived from porcine small intestinal mucosa, can be safely and effectively used for myringoplasty in children, based on data from a prospective, blinded study of 404 patients.
Patients’ tissue is not always available for tympanic membrane repair, and harvesting the graft may increase intraoperative time, said Dr. Riccardo D’Eredita of Vincenza (Italy) Civil Hospital. SurgiSIS (SIS) "promotes early vessel growth, provides scaffolding for remodeling tissues, and is inexpensive and ready to use." He presented the findings at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
The material has been used widely in children, and data from previous studies show that SurgiSIS is gradually replaced by host cells, said Dr. D’Eredita. After 30 days, host cells invade SurgiSIS. After 1 year, SurgiSIS is no longer evident, and has been replaced by the patients’ collagen.
In this study, 404 children underwent tympanic membrane repair in 432 ears; 217 were randomized to myringoplasty with SurgiSIS and 215 were randomized to repair using the patients’ own temporalis fascia.
Overall, the group without SurgiSIS had a 97% rate of stable closures and the group with SurgiSIS had a 95% rate. Surgical time was approximately 15 minutes less for SurgiSIS-treated patients, Dr. D’Eredita said.
The researchers assessed the healing of the tympanic membranes over a 10-year period and found comparable reduction of inflammation in the two groups. There were no adverse reactions in the SIS group.
Dr. D’Eredita had no financial conflicts to disclose.
WASHINGTON – SurgiSIS, a material derived from porcine small intestinal mucosa, can be safely and effectively used for myringoplasty in children, based on data from a prospective, blinded study of 404 patients.
Patients’ tissue is not always available for tympanic membrane repair, and harvesting the graft may increase intraoperative time, said Dr. Riccardo D’Eredita of Vincenza (Italy) Civil Hospital. SurgiSIS (SIS) "promotes early vessel growth, provides scaffolding for remodeling tissues, and is inexpensive and ready to use." He presented the findings at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
The material has been used widely in children, and data from previous studies show that SurgiSIS is gradually replaced by host cells, said Dr. D’Eredita. After 30 days, host cells invade SurgiSIS. After 1 year, SurgiSIS is no longer evident, and has been replaced by the patients’ collagen.
In this study, 404 children underwent tympanic membrane repair in 432 ears; 217 were randomized to myringoplasty with SurgiSIS and 215 were randomized to repair using the patients’ own temporalis fascia.
Overall, the group without SurgiSIS had a 97% rate of stable closures and the group with SurgiSIS had a 95% rate. Surgical time was approximately 15 minutes less for SurgiSIS-treated patients, Dr. D’Eredita said.
The researchers assessed the healing of the tympanic membranes over a 10-year period and found comparable reduction of inflammation in the two groups. There were no adverse reactions in the SIS group.
Dr. D’Eredita had no financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF OTOLARYNGOLOGY - HEAD AND NECK SURGERY FOUNDATION
Major Finding: The number of stable surgical closures was similar in children who had tympanic membrane repair with porcine small intestinal mucosa (212) compared with use of their own tissue (204).
Data Source: The data comprise 432 ears in 404 children.
Disclosures: Dr. D’Eredita had no financial conflicts to disclose.
Facial Nerve Dysfunction Seen in 25% of Pediatric Parotidectomy Patients
WASHINGTON – Facial nerve dysfunction affected 23% of 43 children who had parotidectomies in a single-center study presented at the annual meeting of the American Academy of Otolaryngology–Head and Neck Surgery Foundation.
The findings suggest that facial nerve dysfunction after parotidectomy is common enough in children to merit preoperative counseling, said Dr. James A. Owusu of the University of Minnesota, Minneapolis.
Facial nerve dysfunction rates reported in the literature range from 9% to 60% in adults after parotidectomy, but the condition has not been well studied in children.
Dr. Owusu and his colleagues reviewed the charts of 43 patients younger than age 18 years who underwent parotidectomies at a single tertiary care center between 1999 and 2011. Patients who only had parotid biopsies and those without follow-up data were excluded from the study. The average age of the patients was 4 years, and 58% were girls.
Postoperatively, 33 children (77%) had normal nerve function and 10 (23%) had abnormal nerve function. One patient experienced immediate facial nerve paralysis and nine experienced immediate facial nerve paresis. The marginal mandibular branch was affected in seven patients, the frontal branch in one patient, the buccal branch in one, and both marginal mandibular and frontal branches in one.
The most common diagnosis that led to a parotidectomy was atypical mycobacterium infection (37%), followed by branchial cleft abnormality (19%) and lymphangioma (16%). Nearly all (41) of the children underwent superficial parotidectomy; 2 underwent total parotidectomy.
"Age, gender, and pathologic diagnosis were not predictive of postoperative nerve dysfunction," Dr. Owusu said.
In patients with paresis, full nerve recovery occurred within 1 month for 2 patients, within 2 months for 1 patient, within 6 months for 3 patients, and within 10 months for 2 patients. Final nerve status was not available for 1 patient.
The study was limited by its small size and focus on a single center, Dr. Owusu said.
Dr. Owusu had no financial conflicts to disclose.
WASHINGTON – Facial nerve dysfunction affected 23% of 43 children who had parotidectomies in a single-center study presented at the annual meeting of the American Academy of Otolaryngology–Head and Neck Surgery Foundation.
The findings suggest that facial nerve dysfunction after parotidectomy is common enough in children to merit preoperative counseling, said Dr. James A. Owusu of the University of Minnesota, Minneapolis.
Facial nerve dysfunction rates reported in the literature range from 9% to 60% in adults after parotidectomy, but the condition has not been well studied in children.
Dr. Owusu and his colleagues reviewed the charts of 43 patients younger than age 18 years who underwent parotidectomies at a single tertiary care center between 1999 and 2011. Patients who only had parotid biopsies and those without follow-up data were excluded from the study. The average age of the patients was 4 years, and 58% were girls.
Postoperatively, 33 children (77%) had normal nerve function and 10 (23%) had abnormal nerve function. One patient experienced immediate facial nerve paralysis and nine experienced immediate facial nerve paresis. The marginal mandibular branch was affected in seven patients, the frontal branch in one patient, the buccal branch in one, and both marginal mandibular and frontal branches in one.
The most common diagnosis that led to a parotidectomy was atypical mycobacterium infection (37%), followed by branchial cleft abnormality (19%) and lymphangioma (16%). Nearly all (41) of the children underwent superficial parotidectomy; 2 underwent total parotidectomy.
"Age, gender, and pathologic diagnosis were not predictive of postoperative nerve dysfunction," Dr. Owusu said.
In patients with paresis, full nerve recovery occurred within 1 month for 2 patients, within 2 months for 1 patient, within 6 months for 3 patients, and within 10 months for 2 patients. Final nerve status was not available for 1 patient.
The study was limited by its small size and focus on a single center, Dr. Owusu said.
Dr. Owusu had no financial conflicts to disclose.
WASHINGTON – Facial nerve dysfunction affected 23% of 43 children who had parotidectomies in a single-center study presented at the annual meeting of the American Academy of Otolaryngology–Head and Neck Surgery Foundation.
The findings suggest that facial nerve dysfunction after parotidectomy is common enough in children to merit preoperative counseling, said Dr. James A. Owusu of the University of Minnesota, Minneapolis.
Facial nerve dysfunction rates reported in the literature range from 9% to 60% in adults after parotidectomy, but the condition has not been well studied in children.
Dr. Owusu and his colleagues reviewed the charts of 43 patients younger than age 18 years who underwent parotidectomies at a single tertiary care center between 1999 and 2011. Patients who only had parotid biopsies and those without follow-up data were excluded from the study. The average age of the patients was 4 years, and 58% were girls.
Postoperatively, 33 children (77%) had normal nerve function and 10 (23%) had abnormal nerve function. One patient experienced immediate facial nerve paralysis and nine experienced immediate facial nerve paresis. The marginal mandibular branch was affected in seven patients, the frontal branch in one patient, the buccal branch in one, and both marginal mandibular and frontal branches in one.
The most common diagnosis that led to a parotidectomy was atypical mycobacterium infection (37%), followed by branchial cleft abnormality (19%) and lymphangioma (16%). Nearly all (41) of the children underwent superficial parotidectomy; 2 underwent total parotidectomy.
"Age, gender, and pathologic diagnosis were not predictive of postoperative nerve dysfunction," Dr. Owusu said.
In patients with paresis, full nerve recovery occurred within 1 month for 2 patients, within 2 months for 1 patient, within 6 months for 3 patients, and within 10 months for 2 patients. Final nerve status was not available for 1 patient.
The study was limited by its small size and focus on a single center, Dr. Owusu said.
Dr. Owusu had no financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF OTOLARYNGOLOGY - HEAD AND NECK SURGERY FOUNDATION
Major Finding: After parotidectomies, 23% of children experienced facial nerve dysfunction, but most were fully recovered within 6 months.
Data Source: Investigators reviewed the charts of 43 children who underwent parotidectomies at a single center between 1999 and 2011.
Disclosures: Dr. Owusu had no financial conflicts to disclose.
Antibodies May Link to Lung Disease in RA
WASHINGTON – Specific anticitrullinated peptide antibody levels were significantly higher in rheumatoid arthritis patients with interstitial lung disease than in those without lung disease, based on data from 177 patients.
Complications and death are common in rheumatoid arthritis (RA) patients with interstitial lung disease (ILD), and the findings "may implicate the lung as a site in which protein citrullination initiates epitope spreading and propagation of RA," said Dr. Jon T. Giles of Columbia University in New York.
To determine the association of anticitrullinated peptide antibodies (ACPA) with ILD, Dr. Giles and his colleagues reviewed data from multidetector computed tomography images and concurrent serum samples for 177 RA patients. The mean age of the patients was 59 years, 60% were women, and 11% were smokers.
A total of 57 patients (32%) showed some evidence of ILD on imaging, and 32 (18%) had ILD scores of 3 U or higher, Dr. Giles said at the meeting. Overall, levels of anticyclic citrullinated peptide (anti-CCP) and 17 specific ACPAs ranged from 46% to 273% higher in patients with ILD than in those without ILD. Patients with ILD were more likely to be male, to smoke, and to have a history of prednisone and leflunomide use as well as rheumatoid factor and anti-CCP seropositivity compared with patients without ILD, said Dr. Giles.
Anti-CCP seropositivity was significantly more common among patients with any ILD vs. those without ILD (89% vs. 69%), and the seropositivity was even more common (94%) in patients with ILD scores of 3 U or higher.
Higher levels of seven or more ACPAs were significantly more common in patients with reticulation, honeycombing, or traction bronchiectasis than in those with no ILD (40% vs. 18%).
In addition, higher levels of seven or more ACPAs were significantly more common in patients with evidence of restriction on a pulmonary function test and/or decreased results on a diffusing capacity of the lungs for carbon monoxide test compared with those without ILD (39% vs. 20%). The differences were significant after adjustment for age, sex, smoking status, disease activity score (using DAS28), and current prednisone and leflunomide use.
Levels of antibodies targeting noncitrullinated proteins were not significantly higher in patients with ILD, which "suggests a specificity for ACPA in the association," Dr. Giles said.
"Another mechanistic possibility is that ACPA[s] targeting citrullinated synovial antigens are generated and mediate remote pathogenic effects upon circulating to the lungs, where their cognate citrullinated proteins may also be present," he said.
The findings were limited in part by the use of multidetector computed tomography, which differs in slice thickness from high-resolution CT, Dr. Giles noted. But the strengths of the research include the multiple measures of pulmonary disease, he said.
Dr. Giles said he had no financial conflicts to disclose. The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the American College of Rheumatology’s Within Our Reach Campaign.
WASHINGTON – Specific anticitrullinated peptide antibody levels were significantly higher in rheumatoid arthritis patients with interstitial lung disease than in those without lung disease, based on data from 177 patients.
Complications and death are common in rheumatoid arthritis (RA) patients with interstitial lung disease (ILD), and the findings "may implicate the lung as a site in which protein citrullination initiates epitope spreading and propagation of RA," said Dr. Jon T. Giles of Columbia University in New York.
To determine the association of anticitrullinated peptide antibodies (ACPA) with ILD, Dr. Giles and his colleagues reviewed data from multidetector computed tomography images and concurrent serum samples for 177 RA patients. The mean age of the patients was 59 years, 60% were women, and 11% were smokers.
A total of 57 patients (32%) showed some evidence of ILD on imaging, and 32 (18%) had ILD scores of 3 U or higher, Dr. Giles said at the meeting. Overall, levels of anticyclic citrullinated peptide (anti-CCP) and 17 specific ACPAs ranged from 46% to 273% higher in patients with ILD than in those without ILD. Patients with ILD were more likely to be male, to smoke, and to have a history of prednisone and leflunomide use as well as rheumatoid factor and anti-CCP seropositivity compared with patients without ILD, said Dr. Giles.
Anti-CCP seropositivity was significantly more common among patients with any ILD vs. those without ILD (89% vs. 69%), and the seropositivity was even more common (94%) in patients with ILD scores of 3 U or higher.
Higher levels of seven or more ACPAs were significantly more common in patients with reticulation, honeycombing, or traction bronchiectasis than in those with no ILD (40% vs. 18%).
In addition, higher levels of seven or more ACPAs were significantly more common in patients with evidence of restriction on a pulmonary function test and/or decreased results on a diffusing capacity of the lungs for carbon monoxide test compared with those without ILD (39% vs. 20%). The differences were significant after adjustment for age, sex, smoking status, disease activity score (using DAS28), and current prednisone and leflunomide use.
Levels of antibodies targeting noncitrullinated proteins were not significantly higher in patients with ILD, which "suggests a specificity for ACPA in the association," Dr. Giles said.
"Another mechanistic possibility is that ACPA[s] targeting citrullinated synovial antigens are generated and mediate remote pathogenic effects upon circulating to the lungs, where their cognate citrullinated proteins may also be present," he said.
The findings were limited in part by the use of multidetector computed tomography, which differs in slice thickness from high-resolution CT, Dr. Giles noted. But the strengths of the research include the multiple measures of pulmonary disease, he said.
Dr. Giles said he had no financial conflicts to disclose. The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the American College of Rheumatology’s Within Our Reach Campaign.
WASHINGTON – Specific anticitrullinated peptide antibody levels were significantly higher in rheumatoid arthritis patients with interstitial lung disease than in those without lung disease, based on data from 177 patients.
Complications and death are common in rheumatoid arthritis (RA) patients with interstitial lung disease (ILD), and the findings "may implicate the lung as a site in which protein citrullination initiates epitope spreading and propagation of RA," said Dr. Jon T. Giles of Columbia University in New York.
To determine the association of anticitrullinated peptide antibodies (ACPA) with ILD, Dr. Giles and his colleagues reviewed data from multidetector computed tomography images and concurrent serum samples for 177 RA patients. The mean age of the patients was 59 years, 60% were women, and 11% were smokers.
A total of 57 patients (32%) showed some evidence of ILD on imaging, and 32 (18%) had ILD scores of 3 U or higher, Dr. Giles said at the meeting. Overall, levels of anticyclic citrullinated peptide (anti-CCP) and 17 specific ACPAs ranged from 46% to 273% higher in patients with ILD than in those without ILD. Patients with ILD were more likely to be male, to smoke, and to have a history of prednisone and leflunomide use as well as rheumatoid factor and anti-CCP seropositivity compared with patients without ILD, said Dr. Giles.
Anti-CCP seropositivity was significantly more common among patients with any ILD vs. those without ILD (89% vs. 69%), and the seropositivity was even more common (94%) in patients with ILD scores of 3 U or higher.
Higher levels of seven or more ACPAs were significantly more common in patients with reticulation, honeycombing, or traction bronchiectasis than in those with no ILD (40% vs. 18%).
In addition, higher levels of seven or more ACPAs were significantly more common in patients with evidence of restriction on a pulmonary function test and/or decreased results on a diffusing capacity of the lungs for carbon monoxide test compared with those without ILD (39% vs. 20%). The differences were significant after adjustment for age, sex, smoking status, disease activity score (using DAS28), and current prednisone and leflunomide use.
Levels of antibodies targeting noncitrullinated proteins were not significantly higher in patients with ILD, which "suggests a specificity for ACPA in the association," Dr. Giles said.
"Another mechanistic possibility is that ACPA[s] targeting citrullinated synovial antigens are generated and mediate remote pathogenic effects upon circulating to the lungs, where their cognate citrullinated proteins may also be present," he said.
The findings were limited in part by the use of multidetector computed tomography, which differs in slice thickness from high-resolution CT, Dr. Giles noted. But the strengths of the research include the multiple measures of pulmonary disease, he said.
Dr. Giles said he had no financial conflicts to disclose. The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the American College of Rheumatology’s Within Our Reach Campaign.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: Levels of anticyclic citrullinated peptide and 17 specific anticitrullinated peptide antibodies ranged from 46% to 273% higher in rheumatoid arthritis patients with interstitial lung disease than in those without.
Data Source: The data come from chest imaging and serum samples from 177 adults with RA.
Disclosures: Dr. Giles said he had no relevant financial conflicts to disclose. The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the American College of Rheumatology’s Within Our Reach Campaign.
AACR Launches Immunology Journal
The American Association for Cancer Research has announced the launch of Cancer Immunology Research, a peer-reviewed journal for original articles on advances in cancer immunology.
The new journal is receiving manuscripts for consideration for publication through its website, according to a press release. The journal is scheduled to launch online at the 2013 AACR annual meeting, and in print with monthly issues starting in June 2013.
The journal will highlight research from all areas of cancer immunology. Potential topics include: tumor-promoting inflammation, cancer antigens, vaccines, antibodies, cellular therapy, cytokines, endogenous antitumor immunity, immune regulation, immune suppression, immunomodulatory effects of cancer treatment, emerging technologies, and clinical investigations.
Plans for regular features include Masters of Immunology – primers on immunology topics from leaders in the field – and Cancer Immunology at the Crossroads – perspectives on the relationship between immunology and other areas of cancer research and allied disciplines.
Dr. Glenn Dranoff, professor of medicine at Dana-Farber Cancer Institute and Harvard Medical School, Boston, is slated to serve as the founding editor-in-chief of Cancer Immunology Research. Dr. Dranoff also leads the Dana-Farber/Harvard Cancer Center Program in Cancer Immunology.
The American Association for Cancer Research has announced the launch of Cancer Immunology Research, a peer-reviewed journal for original articles on advances in cancer immunology.
The new journal is receiving manuscripts for consideration for publication through its website, according to a press release. The journal is scheduled to launch online at the 2013 AACR annual meeting, and in print with monthly issues starting in June 2013.
The journal will highlight research from all areas of cancer immunology. Potential topics include: tumor-promoting inflammation, cancer antigens, vaccines, antibodies, cellular therapy, cytokines, endogenous antitumor immunity, immune regulation, immune suppression, immunomodulatory effects of cancer treatment, emerging technologies, and clinical investigations.
Plans for regular features include Masters of Immunology – primers on immunology topics from leaders in the field – and Cancer Immunology at the Crossroads – perspectives on the relationship between immunology and other areas of cancer research and allied disciplines.
Dr. Glenn Dranoff, professor of medicine at Dana-Farber Cancer Institute and Harvard Medical School, Boston, is slated to serve as the founding editor-in-chief of Cancer Immunology Research. Dr. Dranoff also leads the Dana-Farber/Harvard Cancer Center Program in Cancer Immunology.
The American Association for Cancer Research has announced the launch of Cancer Immunology Research, a peer-reviewed journal for original articles on advances in cancer immunology.
The new journal is receiving manuscripts for consideration for publication through its website, according to a press release. The journal is scheduled to launch online at the 2013 AACR annual meeting, and in print with monthly issues starting in June 2013.
The journal will highlight research from all areas of cancer immunology. Potential topics include: tumor-promoting inflammation, cancer antigens, vaccines, antibodies, cellular therapy, cytokines, endogenous antitumor immunity, immune regulation, immune suppression, immunomodulatory effects of cancer treatment, emerging technologies, and clinical investigations.
Plans for regular features include Masters of Immunology – primers on immunology topics from leaders in the field – and Cancer Immunology at the Crossroads – perspectives on the relationship between immunology and other areas of cancer research and allied disciplines.
Dr. Glenn Dranoff, professor of medicine at Dana-Farber Cancer Institute and Harvard Medical School, Boston, is slated to serve as the founding editor-in-chief of Cancer Immunology Research. Dr. Dranoff also leads the Dana-Farber/Harvard Cancer Center Program in Cancer Immunology.
Teduglutide Trims Parenteral Support in Short Bowel Syndrome
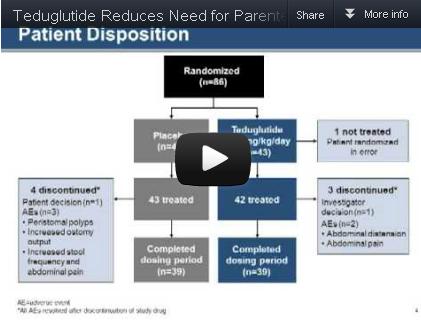
Teduglutide significantly reduced the need for parenteral support in patients with short bowel syndrome and intestinal failure, based on data from 85 adults in a randomized, controlled multicenter trial. The findings were published in the December issue of Gastroenterology.
Patients with short bowel syndrome and intestinal failure (SBS-IF) have inadequate intestinal absorption and require parenteral support (PS) to maintain fluids, electrolytes, trace elements, vitamins, and nutrient balances, said Dr. Palle Bekker Jeppesen of Rigshospitalet in Copenhagen and colleagues.
Source: American Gastroenterological Association
Data from previous open-label studies suggest an association between teduglutide and clinically meaningful reductions in wet weight and energy, which may reduce the need for PS in these patients, the investigators noted.
The researchers randomized 86 adults with SBS-IF to either 0.05 mg/kg per day of teduglutide or a placebo. One patient was randomized in error; complete data were available for 42 teduglutide patients and 43 placebo patients.
Significantly more patients in the teduglutide group responded to treatment, compared with the placebo group (63% vs. 30%). This response was defined as sustaining a 20%-100% reduction from baseline in weekly PS volume during weeks 20-24. "Small bowel length did not appear to be a predictor of response," the researchers noted.
The high placebo response may be explained by examining the fluid composite effect, a measure of the combined effects of teduglutide on PS volume reduction as well as the ability to reduce oral fluid intake and increase urine output volume, the researchers noted.
"In the current study, where protocol modifications encouraged earlier and more aggressive PS reductions, significantly larger PS reductions were also achieved in patients receiving placebo, but subsequently these patients had to increase their oral fluid intake significantly to maintain urine production and hydration constant," they said.
After 24 weeks, overall PS volume was reduced by 32% from baseline in teduglutide patients, compared with 21% in placebo patients. Although no patients in either group were completely weaned from parenteral support at 24 weeks, the difference in PS volume reduction was significantly greater in the teduglutide group.
The average weekly PS volume in teduglutide patients decreased significantly from 12.5 L/wk at baseline to 8.1 L/wk at week 24. The placebo patients also had a significant decrease in average weekly PS volume, from 13.4 L/wk at baseline to 11.1 L/wk at week 24.
Treatment-ending adverse events were similar between the two groups; 5% of teduglutide patients and 7% of placebo patients discontinued treatment because of such events during the study period. The most frequently reported treatment-emergent adverse events included abdominal pain, abdominal distension, nausea, and gastrointestinal stoma complications.
Although the study did not specifically assess quality of life measures, significantly more teduglutide patients had at least 1 day off PS, compared with placebo patients, which could help to "liberate considerable time for unhindered daytime activities or undisturbed sleep," the researchers said.
The study did not address the possible benefit of teduglutide therapy earlier in the course of SBS, or the duration of effect after patients discontinued teduglutide, the researchers added.
However, the findings indicate that teduglutide was safe and well tolerated, and "could positively add to the limited treatment armamentarium" for patients with SBS-IF.
Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
Patients with short bowel syndrome whose absorption is insufficient to maintain nutritional or fluid autonomy have intestinal failure. These patients, particularly those with proximal jejunostomies, who may actually secrete more fluid than they ingest, are among the most complex and challenging to manage of patients with any gastrointestinal disease. Patients with short bowel syndrome and intestinal failure are dependent on parenteral nutrition and/or fluid support (PS) to maintain life. This therapy has substantial implications for employment, activities, sleep, and finances. Numerous, often life-threatening, complications develop.

|
|
A myriad of growth factors may be involved in the process of postresection intestinal adaptation, including glucagonlike peptide-2 (GLP-2), wherein intestinal epithelial growth is promoted. Teduglutide is a long-acting analog of native GLP-2 and is somewhat more resistant to enzymatic degradation in the enterocyte than is the native enzyme. Dr. Jeppesen and colleagues reported a sustained 20%-100% decrease in PS volume requirements during weeks 20-24 of treatment in 63% of patients who received teduglutide, compared with 30% of placebo-treated patients. The mean drop in weekly PS volume from baseline to week 24 totaled 4.4 L in patients who received teduglutide, which equates to a decrease of 1-2 nights of infusion weekly, a very profound improvement for individual patients. The PS weaning protocol used was similar to that used in most centers experienced in the care of these patients.
As would be expected in the SBS-IF patient population, there were many adverse events, although these were equally distributed across teduglutide and placebo groups. Stomal changes, primarily related to enlargement, were evident in a significant minority of patients in the teduglutide group, as would be expected given the hyperplastic effect of the medication on intestinal epithelial tissue.Concern has been raised about GLP-2’s potential to stimulate the development of colonic adenomas in rodent models. Although the risk for malignancy is hypothetical in humans, colonoscopy should be considered at baseline for those patients with residual colons and perhaps as frequently as annually while the patients are on therapy until more long-term safety data are available.
Is teduglutide a "game changer"? The only patients who will be able to discontinue PS completely will be those who are on the borderline between nutritional autonomy and PS dependence. It is important to realize that teduglutide should be used to augment, not replace conventional management. What happens when teduglutide is stopped? Preliminary evidence suggests the effects on adaptation may be persistent, although earlier study noted that histologic changes trended toward baseline within 4 weeks of discontinuation. Perhaps longer treatment or maintenance will be required. The real future is an artificially grown and harvested intestine; even intestinal transplantation represents a bridge at best.
Dr. Alan L. Buchman is a former professor of medicine and surgery at the Feinberg School of Medicine at Northwestern University, Chicago. Within the past 12 months he has consulted for Takeda Pharmaceuticals and NPS Pharmaceuticals.
Patients with short bowel syndrome whose absorption is insufficient to maintain nutritional or fluid autonomy have intestinal failure. These patients, particularly those with proximal jejunostomies, who may actually secrete more fluid than they ingest, are among the most complex and challenging to manage of patients with any gastrointestinal disease. Patients with short bowel syndrome and intestinal failure are dependent on parenteral nutrition and/or fluid support (PS) to maintain life. This therapy has substantial implications for employment, activities, sleep, and finances. Numerous, often life-threatening, complications develop.

|
|
A myriad of growth factors may be involved in the process of postresection intestinal adaptation, including glucagonlike peptide-2 (GLP-2), wherein intestinal epithelial growth is promoted. Teduglutide is a long-acting analog of native GLP-2 and is somewhat more resistant to enzymatic degradation in the enterocyte than is the native enzyme. Dr. Jeppesen and colleagues reported a sustained 20%-100% decrease in PS volume requirements during weeks 20-24 of treatment in 63% of patients who received teduglutide, compared with 30% of placebo-treated patients. The mean drop in weekly PS volume from baseline to week 24 totaled 4.4 L in patients who received teduglutide, which equates to a decrease of 1-2 nights of infusion weekly, a very profound improvement for individual patients. The PS weaning protocol used was similar to that used in most centers experienced in the care of these patients.
As would be expected in the SBS-IF patient population, there were many adverse events, although these were equally distributed across teduglutide and placebo groups. Stomal changes, primarily related to enlargement, were evident in a significant minority of patients in the teduglutide group, as would be expected given the hyperplastic effect of the medication on intestinal epithelial tissue.Concern has been raised about GLP-2’s potential to stimulate the development of colonic adenomas in rodent models. Although the risk for malignancy is hypothetical in humans, colonoscopy should be considered at baseline for those patients with residual colons and perhaps as frequently as annually while the patients are on therapy until more long-term safety data are available.
Is teduglutide a "game changer"? The only patients who will be able to discontinue PS completely will be those who are on the borderline between nutritional autonomy and PS dependence. It is important to realize that teduglutide should be used to augment, not replace conventional management. What happens when teduglutide is stopped? Preliminary evidence suggests the effects on adaptation may be persistent, although earlier study noted that histologic changes trended toward baseline within 4 weeks of discontinuation. Perhaps longer treatment or maintenance will be required. The real future is an artificially grown and harvested intestine; even intestinal transplantation represents a bridge at best.
Dr. Alan L. Buchman is a former professor of medicine and surgery at the Feinberg School of Medicine at Northwestern University, Chicago. Within the past 12 months he has consulted for Takeda Pharmaceuticals and NPS Pharmaceuticals.
Patients with short bowel syndrome whose absorption is insufficient to maintain nutritional or fluid autonomy have intestinal failure. These patients, particularly those with proximal jejunostomies, who may actually secrete more fluid than they ingest, are among the most complex and challenging to manage of patients with any gastrointestinal disease. Patients with short bowel syndrome and intestinal failure are dependent on parenteral nutrition and/or fluid support (PS) to maintain life. This therapy has substantial implications for employment, activities, sleep, and finances. Numerous, often life-threatening, complications develop.

|
|
A myriad of growth factors may be involved in the process of postresection intestinal adaptation, including glucagonlike peptide-2 (GLP-2), wherein intestinal epithelial growth is promoted. Teduglutide is a long-acting analog of native GLP-2 and is somewhat more resistant to enzymatic degradation in the enterocyte than is the native enzyme. Dr. Jeppesen and colleagues reported a sustained 20%-100% decrease in PS volume requirements during weeks 20-24 of treatment in 63% of patients who received teduglutide, compared with 30% of placebo-treated patients. The mean drop in weekly PS volume from baseline to week 24 totaled 4.4 L in patients who received teduglutide, which equates to a decrease of 1-2 nights of infusion weekly, a very profound improvement for individual patients. The PS weaning protocol used was similar to that used in most centers experienced in the care of these patients.
As would be expected in the SBS-IF patient population, there were many adverse events, although these were equally distributed across teduglutide and placebo groups. Stomal changes, primarily related to enlargement, were evident in a significant minority of patients in the teduglutide group, as would be expected given the hyperplastic effect of the medication on intestinal epithelial tissue.Concern has been raised about GLP-2’s potential to stimulate the development of colonic adenomas in rodent models. Although the risk for malignancy is hypothetical in humans, colonoscopy should be considered at baseline for those patients with residual colons and perhaps as frequently as annually while the patients are on therapy until more long-term safety data are available.
Is teduglutide a "game changer"? The only patients who will be able to discontinue PS completely will be those who are on the borderline between nutritional autonomy and PS dependence. It is important to realize that teduglutide should be used to augment, not replace conventional management. What happens when teduglutide is stopped? Preliminary evidence suggests the effects on adaptation may be persistent, although earlier study noted that histologic changes trended toward baseline within 4 weeks of discontinuation. Perhaps longer treatment or maintenance will be required. The real future is an artificially grown and harvested intestine; even intestinal transplantation represents a bridge at best.
Dr. Alan L. Buchman is a former professor of medicine and surgery at the Feinberg School of Medicine at Northwestern University, Chicago. Within the past 12 months he has consulted for Takeda Pharmaceuticals and NPS Pharmaceuticals.
Teduglutide significantly reduced the need for parenteral support in patients with short bowel syndrome and intestinal failure, based on data from 85 adults in a randomized, controlled multicenter trial. The findings were published in the December issue of Gastroenterology.
Patients with short bowel syndrome and intestinal failure (SBS-IF) have inadequate intestinal absorption and require parenteral support (PS) to maintain fluids, electrolytes, trace elements, vitamins, and nutrient balances, said Dr. Palle Bekker Jeppesen of Rigshospitalet in Copenhagen and colleagues.
Source: American Gastroenterological Association
Data from previous open-label studies suggest an association between teduglutide and clinically meaningful reductions in wet weight and energy, which may reduce the need for PS in these patients, the investigators noted.
The researchers randomized 86 adults with SBS-IF to either 0.05 mg/kg per day of teduglutide or a placebo. One patient was randomized in error; complete data were available for 42 teduglutide patients and 43 placebo patients.
Significantly more patients in the teduglutide group responded to treatment, compared with the placebo group (63% vs. 30%). This response was defined as sustaining a 20%-100% reduction from baseline in weekly PS volume during weeks 20-24. "Small bowel length did not appear to be a predictor of response," the researchers noted.
The high placebo response may be explained by examining the fluid composite effect, a measure of the combined effects of teduglutide on PS volume reduction as well as the ability to reduce oral fluid intake and increase urine output volume, the researchers noted.
"In the current study, where protocol modifications encouraged earlier and more aggressive PS reductions, significantly larger PS reductions were also achieved in patients receiving placebo, but subsequently these patients had to increase their oral fluid intake significantly to maintain urine production and hydration constant," they said.
After 24 weeks, overall PS volume was reduced by 32% from baseline in teduglutide patients, compared with 21% in placebo patients. Although no patients in either group were completely weaned from parenteral support at 24 weeks, the difference in PS volume reduction was significantly greater in the teduglutide group.
The average weekly PS volume in teduglutide patients decreased significantly from 12.5 L/wk at baseline to 8.1 L/wk at week 24. The placebo patients also had a significant decrease in average weekly PS volume, from 13.4 L/wk at baseline to 11.1 L/wk at week 24.
Treatment-ending adverse events were similar between the two groups; 5% of teduglutide patients and 7% of placebo patients discontinued treatment because of such events during the study period. The most frequently reported treatment-emergent adverse events included abdominal pain, abdominal distension, nausea, and gastrointestinal stoma complications.
Although the study did not specifically assess quality of life measures, significantly more teduglutide patients had at least 1 day off PS, compared with placebo patients, which could help to "liberate considerable time for unhindered daytime activities or undisturbed sleep," the researchers said.
The study did not address the possible benefit of teduglutide therapy earlier in the course of SBS, or the duration of effect after patients discontinued teduglutide, the researchers added.
However, the findings indicate that teduglutide was safe and well tolerated, and "could positively add to the limited treatment armamentarium" for patients with SBS-IF.
Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
Teduglutide significantly reduced the need for parenteral support in patients with short bowel syndrome and intestinal failure, based on data from 85 adults in a randomized, controlled multicenter trial. The findings were published in the December issue of Gastroenterology.
Patients with short bowel syndrome and intestinal failure (SBS-IF) have inadequate intestinal absorption and require parenteral support (PS) to maintain fluids, electrolytes, trace elements, vitamins, and nutrient balances, said Dr. Palle Bekker Jeppesen of Rigshospitalet in Copenhagen and colleagues.
Source: American Gastroenterological Association
Data from previous open-label studies suggest an association between teduglutide and clinically meaningful reductions in wet weight and energy, which may reduce the need for PS in these patients, the investigators noted.
The researchers randomized 86 adults with SBS-IF to either 0.05 mg/kg per day of teduglutide or a placebo. One patient was randomized in error; complete data were available for 42 teduglutide patients and 43 placebo patients.
Significantly more patients in the teduglutide group responded to treatment, compared with the placebo group (63% vs. 30%). This response was defined as sustaining a 20%-100% reduction from baseline in weekly PS volume during weeks 20-24. "Small bowel length did not appear to be a predictor of response," the researchers noted.
The high placebo response may be explained by examining the fluid composite effect, a measure of the combined effects of teduglutide on PS volume reduction as well as the ability to reduce oral fluid intake and increase urine output volume, the researchers noted.
"In the current study, where protocol modifications encouraged earlier and more aggressive PS reductions, significantly larger PS reductions were also achieved in patients receiving placebo, but subsequently these patients had to increase their oral fluid intake significantly to maintain urine production and hydration constant," they said.
After 24 weeks, overall PS volume was reduced by 32% from baseline in teduglutide patients, compared with 21% in placebo patients. Although no patients in either group were completely weaned from parenteral support at 24 weeks, the difference in PS volume reduction was significantly greater in the teduglutide group.
The average weekly PS volume in teduglutide patients decreased significantly from 12.5 L/wk at baseline to 8.1 L/wk at week 24. The placebo patients also had a significant decrease in average weekly PS volume, from 13.4 L/wk at baseline to 11.1 L/wk at week 24.
Treatment-ending adverse events were similar between the two groups; 5% of teduglutide patients and 7% of placebo patients discontinued treatment because of such events during the study period. The most frequently reported treatment-emergent adverse events included abdominal pain, abdominal distension, nausea, and gastrointestinal stoma complications.
Although the study did not specifically assess quality of life measures, significantly more teduglutide patients had at least 1 day off PS, compared with placebo patients, which could help to "liberate considerable time for unhindered daytime activities or undisturbed sleep," the researchers said.
The study did not address the possible benefit of teduglutide therapy earlier in the course of SBS, or the duration of effect after patients discontinued teduglutide, the researchers added.
However, the findings indicate that teduglutide was safe and well tolerated, and "could positively add to the limited treatment armamentarium" for patients with SBS-IF.
Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
FROM GASTROENTEROLOGY
Major Finding: Significantly more patients who received 0.05 mg/kg per day of teduglutide had a sustained response to treatment during weeks 20-24, compared with the placebo group (63% vs. 30%).
Data Source: The data come from a randomized, controlled multicenter trial of 85 adults with short bowel syndrome and intestinal failure.
Disclosures: Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
Recurrent Acute Pancreatitis No Better After Dual Sphincterotomy
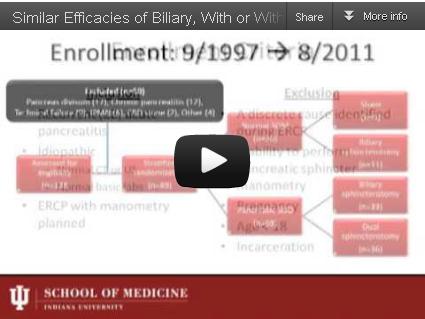
Performance of either biliary endoscopic sphincterotomy alone or dual biliary and pancreatic sphincterotomy similarly prevented approximately half of idiopathic recurrent acute pancreatitis cases in a trial in which 89 patients were randomized to treatments based on the presence or absence of sphincter of Oddi dysfunction.
The study is "the largest randomized clinical trial studying ERCP [endoscopic retrograde cholangiopancreatography] with SOM [sphincter of Oddi manometry] in this population" with long-term follow-up data, Dr. Gregory A. Coté of Indiana University in Indianapolis and his colleagues reported in the December issue of Gastroenterology (2012 [doi: 10.1053/j.gastro.2012.09.006]).
Source: American Gastroenterological Institute
Finding therapeutic equivalence between biliary endoscopic sphincterotomy (BES) and dual endoscopic sphincterotomy (DES) in preventing at least one episode of acute pancreatitis during follow-up is important, because the addition of pancreatic sphincterotomy to ERCP carries the risk of post-ERCP pancreatitis, bleeding, perforation, and sphincter restenosis, according to Dr. Coté and his associates.
To assess the therapeutic value of two types of sphincterotomy and the prognostic value of pancreatic SOD for patients with idiopathic recurrent acute pancreatitis (RAP), the researchers randomized 69 adults with SOD to BES or DES. The other 20 patients who did not have SOD were randomized to BES or a sham therapy. SOD was defined as basal pressure of 40 mm Hg or greater, "sustained for at least 30 seconds across two transducers," the researchers noted.
The patients were aged 18 years and older, and those with chronic pancreatitis or an identified cause of RAP were excluded from the study.
Of the 69 patients with SOD, RAP occurred in 49% of patients who underwent BES and 47% who underwent DES. There was no significant difference in rates of RAP between non-SOD patients who had BES and those who had a sham procedure (27% vs. 11%, respectively).
The risk of RAP was approximately four times higher in patients with SOD than in those without SOD, they added.
"Most RAP events occurred within 30 months of randomization in all subgroups," the researchers said.
Overall, chronic pancreatitis developed in 17% of all patients over a median of 78 months, and there was no difference in the probability of developing chronic pancreatitis in patients with and without SOD.
The study was limited by several factors, including its small sample size for the non-SOD population and the impact of environmental and genetic risk factors on idiopathic RAP, the researchers noted.
The small sample of patients with normal SOM meant that the researchers could draw no conclusions about the benefit of BES in these patients, but the results "represent preliminary data for estimating the sample size of a future definitive trial of ERCP with empiric biliary sphincterotomy," they noted.
In addition, the findings suggest that SOD "may be a secondary marker of more significant inflammation related to previous acute pancreatitis," and that pancreatic sphincterotomy "cannot be recommended as a curative treatment of unexplained RAP alone," they wrote.
None of the study authors had any financial conflicts to disclose.
Performance of either biliary endoscopic sphincterotomy alone or dual biliary and pancreatic sphincterotomy similarly prevented approximately half of idiopathic recurrent acute pancreatitis cases in a trial in which 89 patients were randomized to treatments based on the presence or absence of sphincter of Oddi dysfunction.
The study is "the largest randomized clinical trial studying ERCP [endoscopic retrograde cholangiopancreatography] with SOM [sphincter of Oddi manometry] in this population" with long-term follow-up data, Dr. Gregory A. Coté of Indiana University in Indianapolis and his colleagues reported in the December issue of Gastroenterology (2012 [doi: 10.1053/j.gastro.2012.09.006]).
Source: American Gastroenterological Institute
Finding therapeutic equivalence between biliary endoscopic sphincterotomy (BES) and dual endoscopic sphincterotomy (DES) in preventing at least one episode of acute pancreatitis during follow-up is important, because the addition of pancreatic sphincterotomy to ERCP carries the risk of post-ERCP pancreatitis, bleeding, perforation, and sphincter restenosis, according to Dr. Coté and his associates.
To assess the therapeutic value of two types of sphincterotomy and the prognostic value of pancreatic SOD for patients with idiopathic recurrent acute pancreatitis (RAP), the researchers randomized 69 adults with SOD to BES or DES. The other 20 patients who did not have SOD were randomized to BES or a sham therapy. SOD was defined as basal pressure of 40 mm Hg or greater, "sustained for at least 30 seconds across two transducers," the researchers noted.
The patients were aged 18 years and older, and those with chronic pancreatitis or an identified cause of RAP were excluded from the study.
Of the 69 patients with SOD, RAP occurred in 49% of patients who underwent BES and 47% who underwent DES. There was no significant difference in rates of RAP between non-SOD patients who had BES and those who had a sham procedure (27% vs. 11%, respectively).
The risk of RAP was approximately four times higher in patients with SOD than in those without SOD, they added.
"Most RAP events occurred within 30 months of randomization in all subgroups," the researchers said.
Overall, chronic pancreatitis developed in 17% of all patients over a median of 78 months, and there was no difference in the probability of developing chronic pancreatitis in patients with and without SOD.
The study was limited by several factors, including its small sample size for the non-SOD population and the impact of environmental and genetic risk factors on idiopathic RAP, the researchers noted.
The small sample of patients with normal SOM meant that the researchers could draw no conclusions about the benefit of BES in these patients, but the results "represent preliminary data for estimating the sample size of a future definitive trial of ERCP with empiric biliary sphincterotomy," they noted.
In addition, the findings suggest that SOD "may be a secondary marker of more significant inflammation related to previous acute pancreatitis," and that pancreatic sphincterotomy "cannot be recommended as a curative treatment of unexplained RAP alone," they wrote.
None of the study authors had any financial conflicts to disclose.
Performance of either biliary endoscopic sphincterotomy alone or dual biliary and pancreatic sphincterotomy similarly prevented approximately half of idiopathic recurrent acute pancreatitis cases in a trial in which 89 patients were randomized to treatments based on the presence or absence of sphincter of Oddi dysfunction.
The study is "the largest randomized clinical trial studying ERCP [endoscopic retrograde cholangiopancreatography] with SOM [sphincter of Oddi manometry] in this population" with long-term follow-up data, Dr. Gregory A. Coté of Indiana University in Indianapolis and his colleagues reported in the December issue of Gastroenterology (2012 [doi: 10.1053/j.gastro.2012.09.006]).
Source: American Gastroenterological Institute
Finding therapeutic equivalence between biliary endoscopic sphincterotomy (BES) and dual endoscopic sphincterotomy (DES) in preventing at least one episode of acute pancreatitis during follow-up is important, because the addition of pancreatic sphincterotomy to ERCP carries the risk of post-ERCP pancreatitis, bleeding, perforation, and sphincter restenosis, according to Dr. Coté and his associates.
To assess the therapeutic value of two types of sphincterotomy and the prognostic value of pancreatic SOD for patients with idiopathic recurrent acute pancreatitis (RAP), the researchers randomized 69 adults with SOD to BES or DES. The other 20 patients who did not have SOD were randomized to BES or a sham therapy. SOD was defined as basal pressure of 40 mm Hg or greater, "sustained for at least 30 seconds across two transducers," the researchers noted.
The patients were aged 18 years and older, and those with chronic pancreatitis or an identified cause of RAP were excluded from the study.
Of the 69 patients with SOD, RAP occurred in 49% of patients who underwent BES and 47% who underwent DES. There was no significant difference in rates of RAP between non-SOD patients who had BES and those who had a sham procedure (27% vs. 11%, respectively).
The risk of RAP was approximately four times higher in patients with SOD than in those without SOD, they added.
"Most RAP events occurred within 30 months of randomization in all subgroups," the researchers said.
Overall, chronic pancreatitis developed in 17% of all patients over a median of 78 months, and there was no difference in the probability of developing chronic pancreatitis in patients with and without SOD.
The study was limited by several factors, including its small sample size for the non-SOD population and the impact of environmental and genetic risk factors on idiopathic RAP, the researchers noted.
The small sample of patients with normal SOM meant that the researchers could draw no conclusions about the benefit of BES in these patients, but the results "represent preliminary data for estimating the sample size of a future definitive trial of ERCP with empiric biliary sphincterotomy," they noted.
In addition, the findings suggest that SOD "may be a secondary marker of more significant inflammation related to previous acute pancreatitis," and that pancreatic sphincterotomy "cannot be recommended as a curative treatment of unexplained RAP alone," they wrote.
None of the study authors had any financial conflicts to disclose.
FROM GASTROENTEROLOGY
Major Finding: Of 69 patients with sphincter of Oddi dysfunction, recurrent acute pancreatitis occurred in 49% of patients who underwent biliary endoscopic sphincterectomy and 47% who had dual biliary and pancreatic endoscopic sphincterectomy.
Data Source: The data come from a randomized trial of 89 adults with idiopathic recurrent acute pancreatitis.
Disclosures: None of the study authors had any financial conflicts to disclose.
COPD Varies By State, Peaks Above 9%
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report on Nov. 23.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012; 61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report on Nov. 23.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012; 61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report on Nov. 23.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012; 61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION'S MORBIDITY AND MORTALITY WEEKLY REPORT
Major Finding: The overall prevalence of chronic obstructive pulmonary disease in the United States is approximately 6%.
Data Source: The data come from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey.
Disclosures: The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.