User login
Efinaconazole shows effectiveness against toenail fungus
A topical 10% efinaconazole solution was significantly more effective than was placebo against mild to moderate onychomycosis in a pair of randomized, controlled phase III studies comprising more than 1,000 patients.
Current topical therapies for distal lateral subungual onychomycosis (DLSO) are lacquer based, and require nail debridement and the removal of lacquer residue, said Dr. Boni Elewski of the University of Alabama, Birmingham, and her colleagues.
"Oral treatment is limited by drug interactions and risk of acute liver injury (requiring laboratory monitoring)," the researchers noted.
To test the efficacy of topical efinaconazole 10%, 1,655 adults with onychomycosis were randomized in two studies (study 1: 870 patients, study 2: 785 patients) at 118 sites in the United States, Canada, and Japan. In both studies, the mean area of target toenail involvement was approximately 36%, with an average of 2.8 affected nontarget toenails per patient. Demographic characteristics were not significantly different between the treatment and placebo groups in either study.
Overall, 18% and 15% of efinaconazole patients in study 1 and study 2, respectively, met the primary endpoint of complete cure at 52 weeks, compared with 3% and 6% of placebo patients, respectively. In addition, 55% and 53% of treatment patients in the two studies met the secondary endpoint of mycologic cure, compared with 7% of placebo patients in each study. Both complete cure and mycologic cure rates were in the range of cure rates achieved with oral therapies, the researchers noted.
The average age of the patients in studies 1 and 2 was 52 years and 51 years, respectively, and approximately 75% of the participants in both studies were men. Patients in each study were randomized to a topical solution of 10% efinaconazole or a placebo vehicle, self-applied at home once daily for 48 weeks. Patients were assessed at 12-week intervals during the study period, and reexamined at 52 weeks after a 4-week treatment-free period. The findings were published in the Journal of the American Academy of Dermatology (2013;68:600-8).
Overall, the rate of adverse events was similar between the drug and placebo groups. Efinaconazole was not associated with adverse events including redness, swelling, burning, itching, or vesiculation, and localized skin reactions were similar between the groups. A total of 235 patients discontinued the study early; the main reasons were patient request (98), lost to follow-up (78), and adverse events (33).
The study was limited by its specific patient population, which did not include children or those with severe disease, the researchers noted. Efinaconazole has not yet been studied in combination with oral antifungal treatment. But the findings suggest that topical efinaconazole is safe and effective, and "may be the first topical treatment for DLSO that can be considered a viable alternative to oral treatments," the researchers wrote.
Dr. Elewski has served as an adviser to Valeant Dermatology, a division of Valeant Pharmaceuticals, which funded the study and manufactures efinaconazole. Her coauthors disclosed that they were employees and stockholders of, and/or advisers and consultants to, several pharmaceutical companies, including Valeant.
On Twitter @hsplete
A topical 10% efinaconazole solution was significantly more effective than was placebo against mild to moderate onychomycosis in a pair of randomized, controlled phase III studies comprising more than 1,000 patients.
Current topical therapies for distal lateral subungual onychomycosis (DLSO) are lacquer based, and require nail debridement and the removal of lacquer residue, said Dr. Boni Elewski of the University of Alabama, Birmingham, and her colleagues.
"Oral treatment is limited by drug interactions and risk of acute liver injury (requiring laboratory monitoring)," the researchers noted.
To test the efficacy of topical efinaconazole 10%, 1,655 adults with onychomycosis were randomized in two studies (study 1: 870 patients, study 2: 785 patients) at 118 sites in the United States, Canada, and Japan. In both studies, the mean area of target toenail involvement was approximately 36%, with an average of 2.8 affected nontarget toenails per patient. Demographic characteristics were not significantly different between the treatment and placebo groups in either study.
Overall, 18% and 15% of efinaconazole patients in study 1 and study 2, respectively, met the primary endpoint of complete cure at 52 weeks, compared with 3% and 6% of placebo patients, respectively. In addition, 55% and 53% of treatment patients in the two studies met the secondary endpoint of mycologic cure, compared with 7% of placebo patients in each study. Both complete cure and mycologic cure rates were in the range of cure rates achieved with oral therapies, the researchers noted.
The average age of the patients in studies 1 and 2 was 52 years and 51 years, respectively, and approximately 75% of the participants in both studies were men. Patients in each study were randomized to a topical solution of 10% efinaconazole or a placebo vehicle, self-applied at home once daily for 48 weeks. Patients were assessed at 12-week intervals during the study period, and reexamined at 52 weeks after a 4-week treatment-free period. The findings were published in the Journal of the American Academy of Dermatology (2013;68:600-8).
Overall, the rate of adverse events was similar between the drug and placebo groups. Efinaconazole was not associated with adverse events including redness, swelling, burning, itching, or vesiculation, and localized skin reactions were similar between the groups. A total of 235 patients discontinued the study early; the main reasons were patient request (98), lost to follow-up (78), and adverse events (33).
The study was limited by its specific patient population, which did not include children or those with severe disease, the researchers noted. Efinaconazole has not yet been studied in combination with oral antifungal treatment. But the findings suggest that topical efinaconazole is safe and effective, and "may be the first topical treatment for DLSO that can be considered a viable alternative to oral treatments," the researchers wrote.
Dr. Elewski has served as an adviser to Valeant Dermatology, a division of Valeant Pharmaceuticals, which funded the study and manufactures efinaconazole. Her coauthors disclosed that they were employees and stockholders of, and/or advisers and consultants to, several pharmaceutical companies, including Valeant.
On Twitter @hsplete
A topical 10% efinaconazole solution was significantly more effective than was placebo against mild to moderate onychomycosis in a pair of randomized, controlled phase III studies comprising more than 1,000 patients.
Current topical therapies for distal lateral subungual onychomycosis (DLSO) are lacquer based, and require nail debridement and the removal of lacquer residue, said Dr. Boni Elewski of the University of Alabama, Birmingham, and her colleagues.
"Oral treatment is limited by drug interactions and risk of acute liver injury (requiring laboratory monitoring)," the researchers noted.
To test the efficacy of topical efinaconazole 10%, 1,655 adults with onychomycosis were randomized in two studies (study 1: 870 patients, study 2: 785 patients) at 118 sites in the United States, Canada, and Japan. In both studies, the mean area of target toenail involvement was approximately 36%, with an average of 2.8 affected nontarget toenails per patient. Demographic characteristics were not significantly different between the treatment and placebo groups in either study.
Overall, 18% and 15% of efinaconazole patients in study 1 and study 2, respectively, met the primary endpoint of complete cure at 52 weeks, compared with 3% and 6% of placebo patients, respectively. In addition, 55% and 53% of treatment patients in the two studies met the secondary endpoint of mycologic cure, compared with 7% of placebo patients in each study. Both complete cure and mycologic cure rates were in the range of cure rates achieved with oral therapies, the researchers noted.
The average age of the patients in studies 1 and 2 was 52 years and 51 years, respectively, and approximately 75% of the participants in both studies were men. Patients in each study were randomized to a topical solution of 10% efinaconazole or a placebo vehicle, self-applied at home once daily for 48 weeks. Patients were assessed at 12-week intervals during the study period, and reexamined at 52 weeks after a 4-week treatment-free period. The findings were published in the Journal of the American Academy of Dermatology (2013;68:600-8).
Overall, the rate of adverse events was similar between the drug and placebo groups. Efinaconazole was not associated with adverse events including redness, swelling, burning, itching, or vesiculation, and localized skin reactions were similar between the groups. A total of 235 patients discontinued the study early; the main reasons were patient request (98), lost to follow-up (78), and adverse events (33).
The study was limited by its specific patient population, which did not include children or those with severe disease, the researchers noted. Efinaconazole has not yet been studied in combination with oral antifungal treatment. But the findings suggest that topical efinaconazole is safe and effective, and "may be the first topical treatment for DLSO that can be considered a viable alternative to oral treatments," the researchers wrote.
Dr. Elewski has served as an adviser to Valeant Dermatology, a division of Valeant Pharmaceuticals, which funded the study and manufactures efinaconazole. Her coauthors disclosed that they were employees and stockholders of, and/or advisers and consultants to, several pharmaceutical companies, including Valeant.
On Twitter @hsplete
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Major finding: Topical efinaconazole 10% was significantly more effective against onychomycosis than was placebo in a pair of studies involving more than 1,000 patients.
Data source: Two multicenter, randomized, double-blind, placebo-controlled phase III studies of adults with onychomycosis.
Disclosures: Dr. Elewski has served as an adviser to Valeant Dermatology, a division of Valeant Pharmaceuticals, which funded the study and manufactures efinaconazole. Her coauthors disclosed that they were employees and stockholders of, or advisers and consultants to, several pharmaceutical companies, including Valeant.
Feet first for fungal diversity
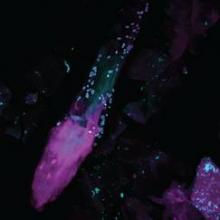
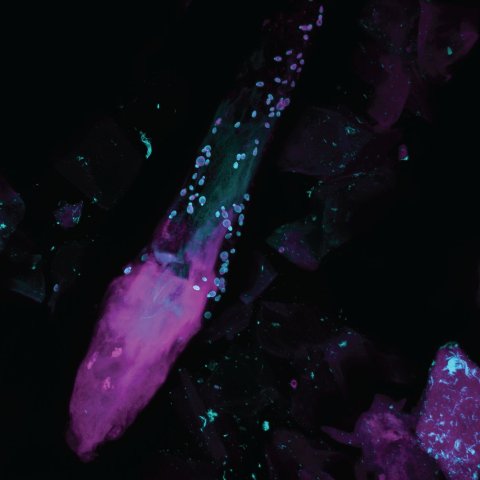
DNA sequencing is helping researchers to get better acquainted with the fungi that inhabit the skin.
"By gaining a more complete awareness of the fungal and bacterial ecosystems, we can better address associated skin diseases, including skin conditions which can be related to cancer treatments," Dr. Heidi Kong, a dermatologist at the National Cancer Institute center for cancer research, said in a statement.
To provide a foundation for investigating fungal skin conditions, a research team from the NCI and the National Human Genome Research Institute examined fungi from 14 skin sites on 10 healthy adults.
"Fungal communities occupy complex niches, even on the human body," said Dr. Kong.
In fact, the feet are first when it comes to fungal diversity. Heels harbor approximately 80 genus-level types of fungi; researchers also identified 60 types in toenail swab samples and 40 types in samples from between the toes.
By contrast, the area inside the bend of the arms, the inside of the forearms, and the palms hosted 18-32 fungal genera each, while areas of the head and trunk, including the back, the back of the neck, inside and behind the ears, and between the eyebrows, contained just 2-10 types of fungi. Overall, Malassezia was the most popular genus, identified in 11 of the 14 body sites sampled.
"DNA sequence–based methods of identification enabled us to differentiate among species of fungi and to conclude that the diversity of fungi is highly dependent on the body site rather than the person," Dr. Kong said.
"Our study [Nature 2013 May 22 (doi:10.1038/nature12171)] focused on areas of the skin where we commonly find skin diseases that have been associated with fungi," she noted.
The researchers identified problems consistent with fungal infections, including heel scaling, toe web scaling, and toenail changes, in 20% of study participants.
Although individuals with heel site infections had common fungal communities at that site, those with toenail infections hosted a wide range of different fungal communities, the researchers noted.
In addition, they found "greater similarity in the fungal community structure on the left and right sides of the same person’s body compared to the same body parts on any two individuals," according to the press release. "Fungal communities also appear to be quite stable over time, with little change when tested on two separate occasions, up to 3 months apart."
On Twitter @hsplete
DNA sequencing is helping researchers to get better acquainted with the fungi that inhabit the skin.
"By gaining a more complete awareness of the fungal and bacterial ecosystems, we can better address associated skin diseases, including skin conditions which can be related to cancer treatments," Dr. Heidi Kong, a dermatologist at the National Cancer Institute center for cancer research, said in a statement.
To provide a foundation for investigating fungal skin conditions, a research team from the NCI and the National Human Genome Research Institute examined fungi from 14 skin sites on 10 healthy adults.
"Fungal communities occupy complex niches, even on the human body," said Dr. Kong.
In fact, the feet are first when it comes to fungal diversity. Heels harbor approximately 80 genus-level types of fungi; researchers also identified 60 types in toenail swab samples and 40 types in samples from between the toes.
By contrast, the area inside the bend of the arms, the inside of the forearms, and the palms hosted 18-32 fungal genera each, while areas of the head and trunk, including the back, the back of the neck, inside and behind the ears, and between the eyebrows, contained just 2-10 types of fungi. Overall, Malassezia was the most popular genus, identified in 11 of the 14 body sites sampled.
"DNA sequence–based methods of identification enabled us to differentiate among species of fungi and to conclude that the diversity of fungi is highly dependent on the body site rather than the person," Dr. Kong said.
"Our study [Nature 2013 May 22 (doi:10.1038/nature12171)] focused on areas of the skin where we commonly find skin diseases that have been associated with fungi," she noted.
The researchers identified problems consistent with fungal infections, including heel scaling, toe web scaling, and toenail changes, in 20% of study participants.
Although individuals with heel site infections had common fungal communities at that site, those with toenail infections hosted a wide range of different fungal communities, the researchers noted.
In addition, they found "greater similarity in the fungal community structure on the left and right sides of the same person’s body compared to the same body parts on any two individuals," according to the press release. "Fungal communities also appear to be quite stable over time, with little change when tested on two separate occasions, up to 3 months apart."
On Twitter @hsplete
DNA sequencing is helping researchers to get better acquainted with the fungi that inhabit the skin.
"By gaining a more complete awareness of the fungal and bacterial ecosystems, we can better address associated skin diseases, including skin conditions which can be related to cancer treatments," Dr. Heidi Kong, a dermatologist at the National Cancer Institute center for cancer research, said in a statement.
To provide a foundation for investigating fungal skin conditions, a research team from the NCI and the National Human Genome Research Institute examined fungi from 14 skin sites on 10 healthy adults.
"Fungal communities occupy complex niches, even on the human body," said Dr. Kong.
In fact, the feet are first when it comes to fungal diversity. Heels harbor approximately 80 genus-level types of fungi; researchers also identified 60 types in toenail swab samples and 40 types in samples from between the toes.
By contrast, the area inside the bend of the arms, the inside of the forearms, and the palms hosted 18-32 fungal genera each, while areas of the head and trunk, including the back, the back of the neck, inside and behind the ears, and between the eyebrows, contained just 2-10 types of fungi. Overall, Malassezia was the most popular genus, identified in 11 of the 14 body sites sampled.
"DNA sequence–based methods of identification enabled us to differentiate among species of fungi and to conclude that the diversity of fungi is highly dependent on the body site rather than the person," Dr. Kong said.
"Our study [Nature 2013 May 22 (doi:10.1038/nature12171)] focused on areas of the skin where we commonly find skin diseases that have been associated with fungi," she noted.
The researchers identified problems consistent with fungal infections, including heel scaling, toe web scaling, and toenail changes, in 20% of study participants.
Although individuals with heel site infections had common fungal communities at that site, those with toenail infections hosted a wide range of different fungal communities, the researchers noted.
In addition, they found "greater similarity in the fungal community structure on the left and right sides of the same person’s body compared to the same body parts on any two individuals," according to the press release. "Fungal communities also appear to be quite stable over time, with little change when tested on two separate occasions, up to 3 months apart."
On Twitter @hsplete
Daily sunscreen slowed skin aging in middle-aged adults
Daily sunscreen users were significantly less likely than discretionary sunscreen users to show signs of skin aging after 4.5 years, according to a study of young and middle-aged adults.
However, beta-carotene supplements appeared to have no effect on skin aging.
The findings from the randomized controlled trial were published online June 3 in Annals of Internal Medicine (2013;158:781-90).
"No known randomized studies in humans have evaluated the effect of sunscreen on surface changes associated with skin aging," wrote Maria Celia B. Hughes, MMedSci., of the Queensland Institute of Medical Research, Australia, and her colleagues.
The investigators used data from the Nambour (Australia) Skin Cancer Prevention Trial, in which 1,621 adults were studied from 1992 to 1996 to test the effect of sunscreen use or dietary supplements on skin cancer risk, photoaging, and actinic keratosis development.
To determine whether consistent, daily sunscreen use could prevent progression of skin aging, researchers randomized Nambour study participants under age 55 into four groups: daily use of broad-spectrum sunscreen plus 30 mg of beta-carotene; daily sunscreen use plus a placebo supplement; discretionary sunscreen use plus 30 mg of beta-carotene; and discretionary sunscreen use plus a placebo supplement.
The investigators focused on 903 adults younger than 55 to exclude the potential effects of growing old on participants’ skin aging.
Skin aging was assessed by comparing skin microtopography based on impressions taken of the backs of participants’ hands at baseline in 1992 and 4.5 years later in 1996. Assessors were blinded to the treatment groups.
"Most of the study participants were fair skinned, and more than 90% burned on acute sun exposure," the researchers noted. The groups were similar in terms of phenotype, sun exposure, and pretrial sunscreen use. All groups reported similar amounts of sun exposure during the study period; 78% of daily sunscreen users and 76% of discretionary sunscreen users reported being outdoors for less than 50% of their weekend time. In addition, the use of other sun protection measures, including seeking shade and wearing a hat, was similar among the groups.
By the end of the study, 77% of the daily sunscreen users applied sunscreen at least 3-4 days per week, vs. 33% of the discretionary users.
Overall, 58% of the participants in the current study met criteria for moderate photoaging at baseline in 1992, and 49% met those criteria in 1996. However, at the end of the 4.5-year period, daily sunscreen users were 24% less likely to show signs of skin aging than were discretionary users, a statistically significant difference.
When the odds of having a higher microtopography grade in 1996 than in 1992 were adjusted for sunburns and photoaging of the neck, the researchers noted, "only the daily sunscreen intervention group showed no detectable increase in microtopography grade."
No significant differences in skin aging were seen in participants randomized to beta-carotene vs. placebo.
The study was limited by several factors, including limited outcome data, which reduced the power to detect moderate treatment effects. In addition, the data were insufficient to rule out an effect of beta carotene on skin aging, the researchers noted.
However, "these results have important clinical implications," the researchers said. "A unit increase in microtopography significantly correlates with risk for actinic keratoses and skin cancer." Thus, the cosmetic benefits of reducing skin changes in middle age also may reduce cancer risk.
The National Health and Medical Research Council of Australia funded the study.
Daily sunscreen users were significantly less likely than discretionary sunscreen users to show signs of skin aging after 4.5 years, according to a study of young and middle-aged adults.
However, beta-carotene supplements appeared to have no effect on skin aging.
The findings from the randomized controlled trial were published online June 3 in Annals of Internal Medicine (2013;158:781-90).
"No known randomized studies in humans have evaluated the effect of sunscreen on surface changes associated with skin aging," wrote Maria Celia B. Hughes, MMedSci., of the Queensland Institute of Medical Research, Australia, and her colleagues.
The investigators used data from the Nambour (Australia) Skin Cancer Prevention Trial, in which 1,621 adults were studied from 1992 to 1996 to test the effect of sunscreen use or dietary supplements on skin cancer risk, photoaging, and actinic keratosis development.
To determine whether consistent, daily sunscreen use could prevent progression of skin aging, researchers randomized Nambour study participants under age 55 into four groups: daily use of broad-spectrum sunscreen plus 30 mg of beta-carotene; daily sunscreen use plus a placebo supplement; discretionary sunscreen use plus 30 mg of beta-carotene; and discretionary sunscreen use plus a placebo supplement.
The investigators focused on 903 adults younger than 55 to exclude the potential effects of growing old on participants’ skin aging.
Skin aging was assessed by comparing skin microtopography based on impressions taken of the backs of participants’ hands at baseline in 1992 and 4.5 years later in 1996. Assessors were blinded to the treatment groups.
"Most of the study participants were fair skinned, and more than 90% burned on acute sun exposure," the researchers noted. The groups were similar in terms of phenotype, sun exposure, and pretrial sunscreen use. All groups reported similar amounts of sun exposure during the study period; 78% of daily sunscreen users and 76% of discretionary sunscreen users reported being outdoors for less than 50% of their weekend time. In addition, the use of other sun protection measures, including seeking shade and wearing a hat, was similar among the groups.
By the end of the study, 77% of the daily sunscreen users applied sunscreen at least 3-4 days per week, vs. 33% of the discretionary users.
Overall, 58% of the participants in the current study met criteria for moderate photoaging at baseline in 1992, and 49% met those criteria in 1996. However, at the end of the 4.5-year period, daily sunscreen users were 24% less likely to show signs of skin aging than were discretionary users, a statistically significant difference.
When the odds of having a higher microtopography grade in 1996 than in 1992 were adjusted for sunburns and photoaging of the neck, the researchers noted, "only the daily sunscreen intervention group showed no detectable increase in microtopography grade."
No significant differences in skin aging were seen in participants randomized to beta-carotene vs. placebo.
The study was limited by several factors, including limited outcome data, which reduced the power to detect moderate treatment effects. In addition, the data were insufficient to rule out an effect of beta carotene on skin aging, the researchers noted.
However, "these results have important clinical implications," the researchers said. "A unit increase in microtopography significantly correlates with risk for actinic keratoses and skin cancer." Thus, the cosmetic benefits of reducing skin changes in middle age also may reduce cancer risk.
The National Health and Medical Research Council of Australia funded the study.
Daily sunscreen users were significantly less likely than discretionary sunscreen users to show signs of skin aging after 4.5 years, according to a study of young and middle-aged adults.
However, beta-carotene supplements appeared to have no effect on skin aging.
The findings from the randomized controlled trial were published online June 3 in Annals of Internal Medicine (2013;158:781-90).
"No known randomized studies in humans have evaluated the effect of sunscreen on surface changes associated with skin aging," wrote Maria Celia B. Hughes, MMedSci., of the Queensland Institute of Medical Research, Australia, and her colleagues.
The investigators used data from the Nambour (Australia) Skin Cancer Prevention Trial, in which 1,621 adults were studied from 1992 to 1996 to test the effect of sunscreen use or dietary supplements on skin cancer risk, photoaging, and actinic keratosis development.
To determine whether consistent, daily sunscreen use could prevent progression of skin aging, researchers randomized Nambour study participants under age 55 into four groups: daily use of broad-spectrum sunscreen plus 30 mg of beta-carotene; daily sunscreen use plus a placebo supplement; discretionary sunscreen use plus 30 mg of beta-carotene; and discretionary sunscreen use plus a placebo supplement.
The investigators focused on 903 adults younger than 55 to exclude the potential effects of growing old on participants’ skin aging.
Skin aging was assessed by comparing skin microtopography based on impressions taken of the backs of participants’ hands at baseline in 1992 and 4.5 years later in 1996. Assessors were blinded to the treatment groups.
"Most of the study participants were fair skinned, and more than 90% burned on acute sun exposure," the researchers noted. The groups were similar in terms of phenotype, sun exposure, and pretrial sunscreen use. All groups reported similar amounts of sun exposure during the study period; 78% of daily sunscreen users and 76% of discretionary sunscreen users reported being outdoors for less than 50% of their weekend time. In addition, the use of other sun protection measures, including seeking shade and wearing a hat, was similar among the groups.
By the end of the study, 77% of the daily sunscreen users applied sunscreen at least 3-4 days per week, vs. 33% of the discretionary users.
Overall, 58% of the participants in the current study met criteria for moderate photoaging at baseline in 1992, and 49% met those criteria in 1996. However, at the end of the 4.5-year period, daily sunscreen users were 24% less likely to show signs of skin aging than were discretionary users, a statistically significant difference.
When the odds of having a higher microtopography grade in 1996 than in 1992 were adjusted for sunburns and photoaging of the neck, the researchers noted, "only the daily sunscreen intervention group showed no detectable increase in microtopography grade."
No significant differences in skin aging were seen in participants randomized to beta-carotene vs. placebo.
The study was limited by several factors, including limited outcome data, which reduced the power to detect moderate treatment effects. In addition, the data were insufficient to rule out an effect of beta carotene on skin aging, the researchers noted.
However, "these results have important clinical implications," the researchers said. "A unit increase in microtopography significantly correlates with risk for actinic keratoses and skin cancer." Thus, the cosmetic benefits of reducing skin changes in middle age also may reduce cancer risk.
The National Health and Medical Research Council of Australia funded the study.
FROM ANNALS OF INTERNAL MEDICINE
Major finding: After 4.5 years, daily sunscreen users were 24% less likely to show signs of skin aging than were discretionary sunscreen users.
Data source: A randomized, controlled, community-based trial of 903 adults younger than 55 years.
Disclosures: The National Health and Medical Research Council of Australia funded the study.
Pulley stitch: A go-to for defects under tension
EDITOR'S NOTE: August 26, 2013: This article has been amended since it was first published to make it clear that Dr. Kelley Pagliai Redbord's description of the pulley stitch procedure was taken directly from an article published by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg.2011;37:1503-5). In her presentation, Dr. Redbord credited Dr. Yag-Howard and her article. However, this credit and attribution to Dr. Yag-Howard was not included in the article published.
WASHINGTON – The pulley stitch "is my go-to stitch for defects under tension," said Dr. Kelley Pagliai Redbord.
The pulley stitch allows for considerable reduction in the surface area of a large defect that can’t be closed by side-to-side stitches alone, making it an excellent choice for use on the scalp and legs, Dr. Redbord said at the Atlantic Dermatological Conference.
"When the tension across the wound is decreased, buried dermal sutures can be placed more easily and accurately," she said. "I use it a lot as an intraoperative tissue expander."
Dr. Redbord said that her description of the pulley stitch was taken from an article by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg. 2011; 37:1503-5).*
The pulley stitch can serve as a temporary suture that can be left in place or removed, said Dr. Redbord, a dermatologist in group practice in Rockville, Md.
The technique follows a far-near-near-far pattern, starting the stitch 8 mm from the wound edge (far), then bringing it to the opposite side just 4 mm from the wound edge (near). Dr. Redbord then reenters the stitch 4 mm from the wound edge on the initial side (near), and makes another pass to the opposite side 8 mm from the wound edge (far).
Multiple passes through the tissue create resistance that keeps the suture from slipping. "The loops of the stitch are placed at an oblique angle so that the inner and outer loops are offset and do not override each other," she noted. This technique minimizes potential skin damage from pressure necrosis caused by overriding loop sutures. The pulley stitch has a 2:1 mechanical advantage over an interrupted suture, and the additional friction of a second loop prevents the knot from slipping.
A modification of the pulley stitch is to loop the suture through an external loop on the opposite side of the incision, and pull across. "This new loop functions as a pulley and directs the tension away from the other strands," she said.
Another stitch with excellent eversion, in which the pulley stitch plays a key role, is the subcutaneous inverted cross mattress stitch (SICM). The SCIM is entirely subcutaneous, and combines the buried vertical mattress stitch and the buried pulley stitch.
The SCIM "uses the buried vertical mattress’s ability to evert wound edges and combines it with the pulley stitch’s ability to decrease tension at the wound edge," she said.
The four-step process is as follows:
• 1. Insert the needle into the dermis 3-5 mm lateral to the wound edge. Advance the needle into the upper reticular dermis, and then curve down to exit through the lower reticular dermis.
• 2. Insert the needle into the opposite edge of the wound at the lower reticular dermis and advance into the upper reticular dermis, then curve down and exit intradermally.
• 3. Insert the needle across the defect using an intradermal approach 1-2 mm lateral to the initial needle insertion point. Then, create a second buried vertical mattress stitch.
• 4. Pull the two stitches to close, which "creates a pulley effect with minimal recoil, and tie off," Dr. Redbord said.
"The pulley system locks the wound edges so that a knot can be tied without slipping," she added.
Dr. Redbord said she had no relevant financial disclosures.
EDITOR'S NOTE: August 26, 2013: This article has been amended since it was first published to make it clear that Dr. Kelley Pagliai Redbord's description of the pulley stitch procedure was taken directly from an article published by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg.2011;37:1503-5). In her presentation, Dr. Redbord credited Dr. Yag-Howard and her article. However, this credit and attribution to Dr. Yag-Howard was not included in the article published.
WASHINGTON – The pulley stitch "is my go-to stitch for defects under tension," said Dr. Kelley Pagliai Redbord.
The pulley stitch allows for considerable reduction in the surface area of a large defect that can’t be closed by side-to-side stitches alone, making it an excellent choice for use on the scalp and legs, Dr. Redbord said at the Atlantic Dermatological Conference.
"When the tension across the wound is decreased, buried dermal sutures can be placed more easily and accurately," she said. "I use it a lot as an intraoperative tissue expander."
Dr. Redbord said that her description of the pulley stitch was taken from an article by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg. 2011; 37:1503-5).*
The pulley stitch can serve as a temporary suture that can be left in place or removed, said Dr. Redbord, a dermatologist in group practice in Rockville, Md.
The technique follows a far-near-near-far pattern, starting the stitch 8 mm from the wound edge (far), then bringing it to the opposite side just 4 mm from the wound edge (near). Dr. Redbord then reenters the stitch 4 mm from the wound edge on the initial side (near), and makes another pass to the opposite side 8 mm from the wound edge (far).
Multiple passes through the tissue create resistance that keeps the suture from slipping. "The loops of the stitch are placed at an oblique angle so that the inner and outer loops are offset and do not override each other," she noted. This technique minimizes potential skin damage from pressure necrosis caused by overriding loop sutures. The pulley stitch has a 2:1 mechanical advantage over an interrupted suture, and the additional friction of a second loop prevents the knot from slipping.
A modification of the pulley stitch is to loop the suture through an external loop on the opposite side of the incision, and pull across. "This new loop functions as a pulley and directs the tension away from the other strands," she said.
Another stitch with excellent eversion, in which the pulley stitch plays a key role, is the subcutaneous inverted cross mattress stitch (SICM). The SCIM is entirely subcutaneous, and combines the buried vertical mattress stitch and the buried pulley stitch.
The SCIM "uses the buried vertical mattress’s ability to evert wound edges and combines it with the pulley stitch’s ability to decrease tension at the wound edge," she said.
The four-step process is as follows:
• 1. Insert the needle into the dermis 3-5 mm lateral to the wound edge. Advance the needle into the upper reticular dermis, and then curve down to exit through the lower reticular dermis.
• 2. Insert the needle into the opposite edge of the wound at the lower reticular dermis and advance into the upper reticular dermis, then curve down and exit intradermally.
• 3. Insert the needle across the defect using an intradermal approach 1-2 mm lateral to the initial needle insertion point. Then, create a second buried vertical mattress stitch.
• 4. Pull the two stitches to close, which "creates a pulley effect with minimal recoil, and tie off," Dr. Redbord said.
"The pulley system locks the wound edges so that a knot can be tied without slipping," she added.
Dr. Redbord said she had no relevant financial disclosures.
EDITOR'S NOTE: August 26, 2013: This article has been amended since it was first published to make it clear that Dr. Kelley Pagliai Redbord's description of the pulley stitch procedure was taken directly from an article published by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg.2011;37:1503-5). In her presentation, Dr. Redbord credited Dr. Yag-Howard and her article. However, this credit and attribution to Dr. Yag-Howard was not included in the article published.
WASHINGTON – The pulley stitch "is my go-to stitch for defects under tension," said Dr. Kelley Pagliai Redbord.
The pulley stitch allows for considerable reduction in the surface area of a large defect that can’t be closed by side-to-side stitches alone, making it an excellent choice for use on the scalp and legs, Dr. Redbord said at the Atlantic Dermatological Conference.
"When the tension across the wound is decreased, buried dermal sutures can be placed more easily and accurately," she said. "I use it a lot as an intraoperative tissue expander."
Dr. Redbord said that her description of the pulley stitch was taken from an article by Dr. Cyndi Yag-Howard in Dermatologic Surgery (Dermatol. Surg. 2011; 37:1503-5).*
The pulley stitch can serve as a temporary suture that can be left in place or removed, said Dr. Redbord, a dermatologist in group practice in Rockville, Md.
The technique follows a far-near-near-far pattern, starting the stitch 8 mm from the wound edge (far), then bringing it to the opposite side just 4 mm from the wound edge (near). Dr. Redbord then reenters the stitch 4 mm from the wound edge on the initial side (near), and makes another pass to the opposite side 8 mm from the wound edge (far).
Multiple passes through the tissue create resistance that keeps the suture from slipping. "The loops of the stitch are placed at an oblique angle so that the inner and outer loops are offset and do not override each other," she noted. This technique minimizes potential skin damage from pressure necrosis caused by overriding loop sutures. The pulley stitch has a 2:1 mechanical advantage over an interrupted suture, and the additional friction of a second loop prevents the knot from slipping.
A modification of the pulley stitch is to loop the suture through an external loop on the opposite side of the incision, and pull across. "This new loop functions as a pulley and directs the tension away from the other strands," she said.
Another stitch with excellent eversion, in which the pulley stitch plays a key role, is the subcutaneous inverted cross mattress stitch (SICM). The SCIM is entirely subcutaneous, and combines the buried vertical mattress stitch and the buried pulley stitch.
The SCIM "uses the buried vertical mattress’s ability to evert wound edges and combines it with the pulley stitch’s ability to decrease tension at the wound edge," she said.
The four-step process is as follows:
• 1. Insert the needle into the dermis 3-5 mm lateral to the wound edge. Advance the needle into the upper reticular dermis, and then curve down to exit through the lower reticular dermis.
• 2. Insert the needle into the opposite edge of the wound at the lower reticular dermis and advance into the upper reticular dermis, then curve down and exit intradermally.
• 3. Insert the needle across the defect using an intradermal approach 1-2 mm lateral to the initial needle insertion point. Then, create a second buried vertical mattress stitch.
• 4. Pull the two stitches to close, which "creates a pulley effect with minimal recoil, and tie off," Dr. Redbord said.
"The pulley system locks the wound edges so that a knot can be tied without slipping," she added.
Dr. Redbord said she had no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ATLANTIC DERMATOLOGICAL CONFERENCE
Major finding: Key numerical finding (e.g., number needed to treat to prevent one death/event; number lived or died as result of intervention). Maximum 10 words/1 sentence.
Data source: Include type of study (e.g., randomized, placebo controlled trial; retrospective case-control study). Include number in the study.
Disclosures: Sponsor of study, funding source, relevant disclosures. If author has no relevant disclosures, "Dr. X reported having no financial disclosures." If necessary, "Meeting Y did not require reports of financial disclosures." Check meeting website because many list disclosures. Written in sentence form.
Tweeting the truth about acne
The truth about acne is out there, but it isn’t always on Twitter.
As the popular social-networking platform continues to grow as a forum for health information, clinicians should be aware of the acne myths, misinformation, and miscellaneous home remedies being shared, and take the opportunity to tweak their patient-education strategies in the clinic setting and online, according to information published in a research letter in JAMA Dermatology.
Health care providers who are comfortable with Twitter can use it to follow acne-related tweets and share reliable medical information and resources, Dr. Kamal Jethwani of the Center for Connected Health, Boston, and his colleagues suggested.
During a 2-week period in June 2012, Dr. Jethwani and his colleagues identified more than 8,000 "high-impact" tweets related to acne. High-impact tweets were defined as those with one or more retweets during the study period, and contained at least one of five keywords: acne, pimple, pimples, zit, or zits.
They used the Twitter Streaming Application Programming Interface to determine how Twitter users share information (and misinformation) about acne.
The researchers sorted the tweets into four categories: personal, celebrity (because stars like Jessica Simpson get acne, too), education, and irrelevant/excluded.
Overall, the researchers examined 8,192 English-language high-impact tweets. Of these, 43% were personal, 20% were about celebrities (the researchers didn’t mention any names), 27% were educational, and 9% were excluded or irrelevant. Of the education tweets, 17% were related to disease information and 9% were treatment-related.
Approximately two-thirds of the disease tweets were variations on the theme of "Why does acne exist?" Not surprisingly, the most often tweeted treatment-related question was a variation of "How do I get rid of my acne?"
"There were a large variety of acne home remedies suggested, including topical food-based remedies ranging from eggs to herbs to fruit," the researchers noted. In addition, 3% of tweeters recommended the topical use of over-the-counter products including baking soda, aloe vera gel, and crushed aspirin (for salicylic acid).
The researchers then compared the word frequency of the selected tweets to the word choices on the American Academy of Dermatology website. Tweeters were more likely to use nonmedical terms such as pimple or pimples vs. terms like pores, skin, or cells used on the AAD website.
"In addition, the AAD website did not address topics that are commonly discussed on Twitter, like makeup, stress, and the efficacy of diet, toothpaste, or other home remedies on acne," the researchers noted.
So, doctors who tweet, you have 140 characters to say whether toothpaste works on zits.
One of the study coauthors, Dr. Joseph Kvedar, reported serving as a consultant for and holding stock in Healthrageous. The other researchers had no financial conflicts to disclose.
The truth about acne is out there, but it isn’t always on Twitter.
As the popular social-networking platform continues to grow as a forum for health information, clinicians should be aware of the acne myths, misinformation, and miscellaneous home remedies being shared, and take the opportunity to tweak their patient-education strategies in the clinic setting and online, according to information published in a research letter in JAMA Dermatology.
Health care providers who are comfortable with Twitter can use it to follow acne-related tweets and share reliable medical information and resources, Dr. Kamal Jethwani of the Center for Connected Health, Boston, and his colleagues suggested.
During a 2-week period in June 2012, Dr. Jethwani and his colleagues identified more than 8,000 "high-impact" tweets related to acne. High-impact tweets were defined as those with one or more retweets during the study period, and contained at least one of five keywords: acne, pimple, pimples, zit, or zits.
They used the Twitter Streaming Application Programming Interface to determine how Twitter users share information (and misinformation) about acne.
The researchers sorted the tweets into four categories: personal, celebrity (because stars like Jessica Simpson get acne, too), education, and irrelevant/excluded.
Overall, the researchers examined 8,192 English-language high-impact tweets. Of these, 43% were personal, 20% were about celebrities (the researchers didn’t mention any names), 27% were educational, and 9% were excluded or irrelevant. Of the education tweets, 17% were related to disease information and 9% were treatment-related.
Approximately two-thirds of the disease tweets were variations on the theme of "Why does acne exist?" Not surprisingly, the most often tweeted treatment-related question was a variation of "How do I get rid of my acne?"
"There were a large variety of acne home remedies suggested, including topical food-based remedies ranging from eggs to herbs to fruit," the researchers noted. In addition, 3% of tweeters recommended the topical use of over-the-counter products including baking soda, aloe vera gel, and crushed aspirin (for salicylic acid).
The researchers then compared the word frequency of the selected tweets to the word choices on the American Academy of Dermatology website. Tweeters were more likely to use nonmedical terms such as pimple or pimples vs. terms like pores, skin, or cells used on the AAD website.
"In addition, the AAD website did not address topics that are commonly discussed on Twitter, like makeup, stress, and the efficacy of diet, toothpaste, or other home remedies on acne," the researchers noted.
So, doctors who tweet, you have 140 characters to say whether toothpaste works on zits.
One of the study coauthors, Dr. Joseph Kvedar, reported serving as a consultant for and holding stock in Healthrageous. The other researchers had no financial conflicts to disclose.
The truth about acne is out there, but it isn’t always on Twitter.
As the popular social-networking platform continues to grow as a forum for health information, clinicians should be aware of the acne myths, misinformation, and miscellaneous home remedies being shared, and take the opportunity to tweak their patient-education strategies in the clinic setting and online, according to information published in a research letter in JAMA Dermatology.
Health care providers who are comfortable with Twitter can use it to follow acne-related tweets and share reliable medical information and resources, Dr. Kamal Jethwani of the Center for Connected Health, Boston, and his colleagues suggested.
During a 2-week period in June 2012, Dr. Jethwani and his colleagues identified more than 8,000 "high-impact" tweets related to acne. High-impact tweets were defined as those with one or more retweets during the study period, and contained at least one of five keywords: acne, pimple, pimples, zit, or zits.
They used the Twitter Streaming Application Programming Interface to determine how Twitter users share information (and misinformation) about acne.
The researchers sorted the tweets into four categories: personal, celebrity (because stars like Jessica Simpson get acne, too), education, and irrelevant/excluded.
Overall, the researchers examined 8,192 English-language high-impact tweets. Of these, 43% were personal, 20% were about celebrities (the researchers didn’t mention any names), 27% were educational, and 9% were excluded or irrelevant. Of the education tweets, 17% were related to disease information and 9% were treatment-related.
Approximately two-thirds of the disease tweets were variations on the theme of "Why does acne exist?" Not surprisingly, the most often tweeted treatment-related question was a variation of "How do I get rid of my acne?"
"There were a large variety of acne home remedies suggested, including topical food-based remedies ranging from eggs to herbs to fruit," the researchers noted. In addition, 3% of tweeters recommended the topical use of over-the-counter products including baking soda, aloe vera gel, and crushed aspirin (for salicylic acid).
The researchers then compared the word frequency of the selected tweets to the word choices on the American Academy of Dermatology website. Tweeters were more likely to use nonmedical terms such as pimple or pimples vs. terms like pores, skin, or cells used on the AAD website.
"In addition, the AAD website did not address topics that are commonly discussed on Twitter, like makeup, stress, and the efficacy of diet, toothpaste, or other home remedies on acne," the researchers noted.
So, doctors who tweet, you have 140 characters to say whether toothpaste works on zits.
One of the study coauthors, Dr. Joseph Kvedar, reported serving as a consultant for and holding stock in Healthrageous. The other researchers had no financial conflicts to disclose.
Monitor for bone toxicity with prolonged retinoid use
WASHINGTON – In patients using continued or high doses of retinoids for indications other than acne, monitoring for bone side effects makes sense, Dr. John DiGiovanna said at the Atlantic Dermatological Conference.
The standard courses of isotretinoin used to treat acne have not been shown to be associated with decreased bone mineral density. In addition, recent data from a large, population-based Danish study of fractures including patients taking isotretinoin, acitretin, and topical retinoids showed that none of the retinoids was associated with a change in the risk of fracture at any skeletal site (Arch. Dermatol. 2010;146:478-82).
With prolonged use, however, patients with risk factors such as a family history of osteopenia or osteoporosis and those taking other medications that might contribute to decreased bone density need to be monitored, said Dr. DiGiovanna of the National Cancer Institute, Bethesda, Md.
There are no set rules for such monitoring. Lab tests every 3-6 months are a good starting point, Dr. DiGiovanna said. Also, consider obtaining a radiographic series every 3 years or more frequently if the patient is symptomatic. Imaging should include the cervical and thoracic spine, heels, knees, pelvis, shoulders, and any symptomatic areas.
Retinoid bone toxicity comes in three types: premature epiphyseal closure, diffuse idiopathic skeletal hyperostosis (DISH), and osteopenia/osteoporosis.
Data on the effects of isotretinoin on growth plates are limited, and have generally been associated with high doses, extended treatment duration, and underlying bone demineralization, Dr. DiGiovanna said.
Rare cases of premature closure of epiphyses have been reported in early studies in patients given high doses of retinoids, Dr. DiGiovanna said. He cited the case of a 6-year-old boy whose isotretinoin dose ranged from 0.5 to 4.5 mg/kg per day. At age 9, he reported periodic pain in his right knee, and a radiograph showed diffuse demineralization. At age 10, the pain recurred and imaging showed partial fusion of the proximal tibial growth plate (J. Amer. Acad. Derm. 1982;7:663-6).
In a second case, a 9-year-old boy with a history of high-dose isotretinoin (up to 5 mg/kg per day) for the rare disorder known as fibrodysplasia ossificans progressiva reported leg pain and showed evidence of arrested growth in the form of dense metaphyseal bands on imaging. Normal growth resumed after he discontinued isotretinoin (Am. J. Dis. Child. 1988;142:316-8).
For young children who need continued use of retinoids, a lower dose can be considered until the child achieves full height. Remind parents that the child may need to be re-treated once the epiphyses have fully closed.
DISH has been reported in patients taking retinoids for extended periods of 2 or more years, Dr. DiGiovanna said. In fact, DISH is common in the general population, and most of the time it is asymptomatic.
Some patients weather the bone effects, as in the case of a 52-year-old man with a history of frequent blistering due to generalized epidermolytic hyperkeratosis. Despite developing osteophytes related to stenosis of a neural foramen in the spine, the patient had no neurological symptoms, and wanted to continue retinoids for relief of his skin symptoms. He continues on his therapy and receives yearly MRIs and neurologic evaluations, Dr. DiGiovanna reported.
Regarding the association between retinoid therapy and bone demineralization or osteopenia, "the evidence is really very weak" and there are many risk factors to consider, said Dr. DiGiovanna. "But if you have a patient with a history of osteopenia, for example, a DEXA [dual-energy x-ray absorptiometry] scan is easy to obtain, and there is minimal exposure to radiation."
Remind potentially high-risk patients to stay active, maintain normal vitamin D levels with oral supplementation, and follow a healthy lifestyle, Dr. DiGiovanna said.
The bone density at Ward’s triangle also can be a confounding factor and lead to a misdiagnosis of osteoporosis, said Dr. DiGiovanna.
"Ward’s triangle is not an anatomic area; it is an area of lowest density in the femoral neck," and it is imprecise and positional, he emphasized. In fact, the consensus from osteoporosis experts is that osteoporosis should be measured using the total hip and spine, and not Ward’s triangle.
A randomized trial of acne patients on 1 mg/kg per day of isotretinoin vs. controls showed no significant difference in bone density after 6 months except at Ward’s triangle, he said (Arch. Dermatol. 1999;135:961-5).
Dr. DiGiovanna had no financial conflicts to disclose.
WASHINGTON – In patients using continued or high doses of retinoids for indications other than acne, monitoring for bone side effects makes sense, Dr. John DiGiovanna said at the Atlantic Dermatological Conference.
The standard courses of isotretinoin used to treat acne have not been shown to be associated with decreased bone mineral density. In addition, recent data from a large, population-based Danish study of fractures including patients taking isotretinoin, acitretin, and topical retinoids showed that none of the retinoids was associated with a change in the risk of fracture at any skeletal site (Arch. Dermatol. 2010;146:478-82).
With prolonged use, however, patients with risk factors such as a family history of osteopenia or osteoporosis and those taking other medications that might contribute to decreased bone density need to be monitored, said Dr. DiGiovanna of the National Cancer Institute, Bethesda, Md.
There are no set rules for such monitoring. Lab tests every 3-6 months are a good starting point, Dr. DiGiovanna said. Also, consider obtaining a radiographic series every 3 years or more frequently if the patient is symptomatic. Imaging should include the cervical and thoracic spine, heels, knees, pelvis, shoulders, and any symptomatic areas.
Retinoid bone toxicity comes in three types: premature epiphyseal closure, diffuse idiopathic skeletal hyperostosis (DISH), and osteopenia/osteoporosis.
Data on the effects of isotretinoin on growth plates are limited, and have generally been associated with high doses, extended treatment duration, and underlying bone demineralization, Dr. DiGiovanna said.
Rare cases of premature closure of epiphyses have been reported in early studies in patients given high doses of retinoids, Dr. DiGiovanna said. He cited the case of a 6-year-old boy whose isotretinoin dose ranged from 0.5 to 4.5 mg/kg per day. At age 9, he reported periodic pain in his right knee, and a radiograph showed diffuse demineralization. At age 10, the pain recurred and imaging showed partial fusion of the proximal tibial growth plate (J. Amer. Acad. Derm. 1982;7:663-6).
In a second case, a 9-year-old boy with a history of high-dose isotretinoin (up to 5 mg/kg per day) for the rare disorder known as fibrodysplasia ossificans progressiva reported leg pain and showed evidence of arrested growth in the form of dense metaphyseal bands on imaging. Normal growth resumed after he discontinued isotretinoin (Am. J. Dis. Child. 1988;142:316-8).
For young children who need continued use of retinoids, a lower dose can be considered until the child achieves full height. Remind parents that the child may need to be re-treated once the epiphyses have fully closed.
DISH has been reported in patients taking retinoids for extended periods of 2 or more years, Dr. DiGiovanna said. In fact, DISH is common in the general population, and most of the time it is asymptomatic.
Some patients weather the bone effects, as in the case of a 52-year-old man with a history of frequent blistering due to generalized epidermolytic hyperkeratosis. Despite developing osteophytes related to stenosis of a neural foramen in the spine, the patient had no neurological symptoms, and wanted to continue retinoids for relief of his skin symptoms. He continues on his therapy and receives yearly MRIs and neurologic evaluations, Dr. DiGiovanna reported.
Regarding the association between retinoid therapy and bone demineralization or osteopenia, "the evidence is really very weak" and there are many risk factors to consider, said Dr. DiGiovanna. "But if you have a patient with a history of osteopenia, for example, a DEXA [dual-energy x-ray absorptiometry] scan is easy to obtain, and there is minimal exposure to radiation."
Remind potentially high-risk patients to stay active, maintain normal vitamin D levels with oral supplementation, and follow a healthy lifestyle, Dr. DiGiovanna said.
The bone density at Ward’s triangle also can be a confounding factor and lead to a misdiagnosis of osteoporosis, said Dr. DiGiovanna.
"Ward’s triangle is not an anatomic area; it is an area of lowest density in the femoral neck," and it is imprecise and positional, he emphasized. In fact, the consensus from osteoporosis experts is that osteoporosis should be measured using the total hip and spine, and not Ward’s triangle.
A randomized trial of acne patients on 1 mg/kg per day of isotretinoin vs. controls showed no significant difference in bone density after 6 months except at Ward’s triangle, he said (Arch. Dermatol. 1999;135:961-5).
Dr. DiGiovanna had no financial conflicts to disclose.
WASHINGTON – In patients using continued or high doses of retinoids for indications other than acne, monitoring for bone side effects makes sense, Dr. John DiGiovanna said at the Atlantic Dermatological Conference.
The standard courses of isotretinoin used to treat acne have not been shown to be associated with decreased bone mineral density. In addition, recent data from a large, population-based Danish study of fractures including patients taking isotretinoin, acitretin, and topical retinoids showed that none of the retinoids was associated with a change in the risk of fracture at any skeletal site (Arch. Dermatol. 2010;146:478-82).
With prolonged use, however, patients with risk factors such as a family history of osteopenia or osteoporosis and those taking other medications that might contribute to decreased bone density need to be monitored, said Dr. DiGiovanna of the National Cancer Institute, Bethesda, Md.
There are no set rules for such monitoring. Lab tests every 3-6 months are a good starting point, Dr. DiGiovanna said. Also, consider obtaining a radiographic series every 3 years or more frequently if the patient is symptomatic. Imaging should include the cervical and thoracic spine, heels, knees, pelvis, shoulders, and any symptomatic areas.
Retinoid bone toxicity comes in three types: premature epiphyseal closure, diffuse idiopathic skeletal hyperostosis (DISH), and osteopenia/osteoporosis.
Data on the effects of isotretinoin on growth plates are limited, and have generally been associated with high doses, extended treatment duration, and underlying bone demineralization, Dr. DiGiovanna said.
Rare cases of premature closure of epiphyses have been reported in early studies in patients given high doses of retinoids, Dr. DiGiovanna said. He cited the case of a 6-year-old boy whose isotretinoin dose ranged from 0.5 to 4.5 mg/kg per day. At age 9, he reported periodic pain in his right knee, and a radiograph showed diffuse demineralization. At age 10, the pain recurred and imaging showed partial fusion of the proximal tibial growth plate (J. Amer. Acad. Derm. 1982;7:663-6).
In a second case, a 9-year-old boy with a history of high-dose isotretinoin (up to 5 mg/kg per day) for the rare disorder known as fibrodysplasia ossificans progressiva reported leg pain and showed evidence of arrested growth in the form of dense metaphyseal bands on imaging. Normal growth resumed after he discontinued isotretinoin (Am. J. Dis. Child. 1988;142:316-8).
For young children who need continued use of retinoids, a lower dose can be considered until the child achieves full height. Remind parents that the child may need to be re-treated once the epiphyses have fully closed.
DISH has been reported in patients taking retinoids for extended periods of 2 or more years, Dr. DiGiovanna said. In fact, DISH is common in the general population, and most of the time it is asymptomatic.
Some patients weather the bone effects, as in the case of a 52-year-old man with a history of frequent blistering due to generalized epidermolytic hyperkeratosis. Despite developing osteophytes related to stenosis of a neural foramen in the spine, the patient had no neurological symptoms, and wanted to continue retinoids for relief of his skin symptoms. He continues on his therapy and receives yearly MRIs and neurologic evaluations, Dr. DiGiovanna reported.
Regarding the association between retinoid therapy and bone demineralization or osteopenia, "the evidence is really very weak" and there are many risk factors to consider, said Dr. DiGiovanna. "But if you have a patient with a history of osteopenia, for example, a DEXA [dual-energy x-ray absorptiometry] scan is easy to obtain, and there is minimal exposure to radiation."
Remind potentially high-risk patients to stay active, maintain normal vitamin D levels with oral supplementation, and follow a healthy lifestyle, Dr. DiGiovanna said.
The bone density at Ward’s triangle also can be a confounding factor and lead to a misdiagnosis of osteoporosis, said Dr. DiGiovanna.
"Ward’s triangle is not an anatomic area; it is an area of lowest density in the femoral neck," and it is imprecise and positional, he emphasized. In fact, the consensus from osteoporosis experts is that osteoporosis should be measured using the total hip and spine, and not Ward’s triangle.
A randomized trial of acne patients on 1 mg/kg per day of isotretinoin vs. controls showed no significant difference in bone density after 6 months except at Ward’s triangle, he said (Arch. Dermatol. 1999;135:961-5).
Dr. DiGiovanna had no financial conflicts to disclose.
EXPERT ANALYSIS FROM THE ATLANTIC DERMATOLOGICAL CONFERENCE
FDA panel supports injectable midface filler
GAITHERSBURG, MD. – A Food and Drug Administration advisory panel unanimously recommended approval of an injectable filler specifically for use in the midface.
At a May 2 meeting, the members of the FDA’s General and Plastic Surgery Devices Panel supported approval of Allergan’s Juvéderm Voluma XC (Voluma) for the correction of age-related volume loss in the midface. The FDA usually follows the recommendations of its advisory panels, which are not binding.
The meeting was held for the panel to discuss, make recommendations, and vote on information related to the premarket approval application for Voluma. Voluma is a biodegradable dermal filler that combines low- and high-molecular-weight hyaluronic acid (20 mg/mL) and 0.3% lidocaine in phosphate-buffered saline.
This new formulation distinguishes Voluma from other injectable products, noted Joseph Nielsen, Ph.D., a biologist with the FDA’s Center for Drug Evaluation and Research.
Voluma’s combination of high- and low-molecular-weight hyaluronic acid creates a thicker product with a jamlike consistency that is designed for deeper injections, said Dr. Rui Avelar, chief medical officer for Allergan. Voluma is indicated specifically for deep injections (subcutaneous and/or supraperiosteal) to correct age-related volume loss in the midface. No products are currently approved in the United States for this indication, although Voluma is approved in 65 countries, including Canada and Australia.
The approval was based on data from a randomized clinical trial. The study population included adults aged 35-65 years (mean age, 55 years). Approximately 80% of the patients were women, more than half were white, and 44% were Fitzpatrick skin types IV, V, and VI. A total of 235 patients were randomized to immediate treatment with Voluma, and 47 served as nontreatment controls to receive injections 6 months later; 208 treatment patients and 36 nontreatment controls had complete data for evaluation at 6 months.
Primary effectiveness was based on the blinded live evaluation of two investigators using the Mid-Face Volume Deficit Scale (MFVDS), a 0-5 point scale approved and validated for the study. Significant response was defined as at least a 1-point change in the MFVDS. In addition, three-dimensional imaging was used to assess changes in volume. Imaging data were not collected from nonresponders.
At 6 months, 86% of the treatment patients and 35% of the untreated controls met the response criteria. In addition, the evaluators rated 82% of treatment patients and 22% of controls as "improved" or "much improved," compared with pretreatment photos using the Global Aesthetic Improvement Scale, and 93% of treated patients rated themselves as improved or much improved, compared with pretreatment photos.
The average initial treatment was 5.2 mL, and 82% of treated patients received an optional touch-up injection of an average of 2 mL 30 days after the first treatment. The injection techniques were consistent with the methods used for other currently available fillers.
Individuals were excluded from the study if they had permanent or semipermanent facial aesthetic procedures, temporary facial aesthetic procedures within the washout period, midface volume loss unrelated to age, or very thin skin in the midface.
Greater baseline volume deficit was a stronger predictor than age of the volume of filler injected, although both factors were associated with a greater volume injected, said Todd Gross, Ph.D., a biostatistician for Allergan.
However, age, volume of product injected, and tunneling technique were associated with an increased risk of adverse events, said Dr. Janette Alexander, an FDA medical officer.
A total of 33% of the participants reported treatment-related adverse events. Five patients had late-onset adverse events; three of these were deemed severe and device related. The three severe treatment-related events involved lumps at the injection sites, all of which were treated with hyaluronidase, Dr. Alexander said.
The other two serious events included a death caused by stroke 1 year after treatment, and an ischemic optic neuropathy that the FDA could not definitely deem device related.
Approximately 78% of subjects reported an injection site response, but the majority of these resolved within 30 days. Injection site responses included firmness, lumps or bumps, tenderness, swelling, pain, bruising, redness, and discoloration. Approximately 20% of treated patients reported firmness or lumps/bumps persisting longer than 30 days.
The safety profile appears similar to that of other hyaluronic acid fillers except for the duration of firmness and lumps/bumps, and the occurrence of late adverse events, Dr. Alexander said.
No increase in risk of adverse events was observed in darker skin types, said Alvin Van Orden, of the FDA’s division of biostatistics.
The panel agreed that the postapproval study of 12 months’ follow-up proposed by Allergan is adequate, but extra attention should be paid to the subset of patients with darker skin, who might respond differently to the treatment, said panel chair Dr. Joseph LoCicero III, of the State University of New York, Brooklyn.
The panelists’ comments in support of their votes included acknowledgment of the safety profile and the reversibility of the product if needed, and the benefits of having an FDA-approved product for volume enhancement.
During their discussion, the panel members also agreed that setting upper limits on filler volume, age, and relative skin thickness should be left to clinical judgment, and not contraindicated.
Members of FDA advisory panels have been cleared of potential conflicts of interest related to the products under discussion prior to the meeting.
GAITHERSBURG, MD. – A Food and Drug Administration advisory panel unanimously recommended approval of an injectable filler specifically for use in the midface.
At a May 2 meeting, the members of the FDA’s General and Plastic Surgery Devices Panel supported approval of Allergan’s Juvéderm Voluma XC (Voluma) for the correction of age-related volume loss in the midface. The FDA usually follows the recommendations of its advisory panels, which are not binding.
The meeting was held for the panel to discuss, make recommendations, and vote on information related to the premarket approval application for Voluma. Voluma is a biodegradable dermal filler that combines low- and high-molecular-weight hyaluronic acid (20 mg/mL) and 0.3% lidocaine in phosphate-buffered saline.
This new formulation distinguishes Voluma from other injectable products, noted Joseph Nielsen, Ph.D., a biologist with the FDA’s Center for Drug Evaluation and Research.
Voluma’s combination of high- and low-molecular-weight hyaluronic acid creates a thicker product with a jamlike consistency that is designed for deeper injections, said Dr. Rui Avelar, chief medical officer for Allergan. Voluma is indicated specifically for deep injections (subcutaneous and/or supraperiosteal) to correct age-related volume loss in the midface. No products are currently approved in the United States for this indication, although Voluma is approved in 65 countries, including Canada and Australia.
The approval was based on data from a randomized clinical trial. The study population included adults aged 35-65 years (mean age, 55 years). Approximately 80% of the patients were women, more than half were white, and 44% were Fitzpatrick skin types IV, V, and VI. A total of 235 patients were randomized to immediate treatment with Voluma, and 47 served as nontreatment controls to receive injections 6 months later; 208 treatment patients and 36 nontreatment controls had complete data for evaluation at 6 months.
Primary effectiveness was based on the blinded live evaluation of two investigators using the Mid-Face Volume Deficit Scale (MFVDS), a 0-5 point scale approved and validated for the study. Significant response was defined as at least a 1-point change in the MFVDS. In addition, three-dimensional imaging was used to assess changes in volume. Imaging data were not collected from nonresponders.
At 6 months, 86% of the treatment patients and 35% of the untreated controls met the response criteria. In addition, the evaluators rated 82% of treatment patients and 22% of controls as "improved" or "much improved," compared with pretreatment photos using the Global Aesthetic Improvement Scale, and 93% of treated patients rated themselves as improved or much improved, compared with pretreatment photos.
The average initial treatment was 5.2 mL, and 82% of treated patients received an optional touch-up injection of an average of 2 mL 30 days after the first treatment. The injection techniques were consistent with the methods used for other currently available fillers.
Individuals were excluded from the study if they had permanent or semipermanent facial aesthetic procedures, temporary facial aesthetic procedures within the washout period, midface volume loss unrelated to age, or very thin skin in the midface.
Greater baseline volume deficit was a stronger predictor than age of the volume of filler injected, although both factors were associated with a greater volume injected, said Todd Gross, Ph.D., a biostatistician for Allergan.
However, age, volume of product injected, and tunneling technique were associated with an increased risk of adverse events, said Dr. Janette Alexander, an FDA medical officer.
A total of 33% of the participants reported treatment-related adverse events. Five patients had late-onset adverse events; three of these were deemed severe and device related. The three severe treatment-related events involved lumps at the injection sites, all of which were treated with hyaluronidase, Dr. Alexander said.
The other two serious events included a death caused by stroke 1 year after treatment, and an ischemic optic neuropathy that the FDA could not definitely deem device related.
Approximately 78% of subjects reported an injection site response, but the majority of these resolved within 30 days. Injection site responses included firmness, lumps or bumps, tenderness, swelling, pain, bruising, redness, and discoloration. Approximately 20% of treated patients reported firmness or lumps/bumps persisting longer than 30 days.
The safety profile appears similar to that of other hyaluronic acid fillers except for the duration of firmness and lumps/bumps, and the occurrence of late adverse events, Dr. Alexander said.
No increase in risk of adverse events was observed in darker skin types, said Alvin Van Orden, of the FDA’s division of biostatistics.
The panel agreed that the postapproval study of 12 months’ follow-up proposed by Allergan is adequate, but extra attention should be paid to the subset of patients with darker skin, who might respond differently to the treatment, said panel chair Dr. Joseph LoCicero III, of the State University of New York, Brooklyn.
The panelists’ comments in support of their votes included acknowledgment of the safety profile and the reversibility of the product if needed, and the benefits of having an FDA-approved product for volume enhancement.
During their discussion, the panel members also agreed that setting upper limits on filler volume, age, and relative skin thickness should be left to clinical judgment, and not contraindicated.
Members of FDA advisory panels have been cleared of potential conflicts of interest related to the products under discussion prior to the meeting.
GAITHERSBURG, MD. – A Food and Drug Administration advisory panel unanimously recommended approval of an injectable filler specifically for use in the midface.
At a May 2 meeting, the members of the FDA’s General and Plastic Surgery Devices Panel supported approval of Allergan’s Juvéderm Voluma XC (Voluma) for the correction of age-related volume loss in the midface. The FDA usually follows the recommendations of its advisory panels, which are not binding.
The meeting was held for the panel to discuss, make recommendations, and vote on information related to the premarket approval application for Voluma. Voluma is a biodegradable dermal filler that combines low- and high-molecular-weight hyaluronic acid (20 mg/mL) and 0.3% lidocaine in phosphate-buffered saline.
This new formulation distinguishes Voluma from other injectable products, noted Joseph Nielsen, Ph.D., a biologist with the FDA’s Center for Drug Evaluation and Research.
Voluma’s combination of high- and low-molecular-weight hyaluronic acid creates a thicker product with a jamlike consistency that is designed for deeper injections, said Dr. Rui Avelar, chief medical officer for Allergan. Voluma is indicated specifically for deep injections (subcutaneous and/or supraperiosteal) to correct age-related volume loss in the midface. No products are currently approved in the United States for this indication, although Voluma is approved in 65 countries, including Canada and Australia.
The approval was based on data from a randomized clinical trial. The study population included adults aged 35-65 years (mean age, 55 years). Approximately 80% of the patients were women, more than half were white, and 44% were Fitzpatrick skin types IV, V, and VI. A total of 235 patients were randomized to immediate treatment with Voluma, and 47 served as nontreatment controls to receive injections 6 months later; 208 treatment patients and 36 nontreatment controls had complete data for evaluation at 6 months.
Primary effectiveness was based on the blinded live evaluation of two investigators using the Mid-Face Volume Deficit Scale (MFVDS), a 0-5 point scale approved and validated for the study. Significant response was defined as at least a 1-point change in the MFVDS. In addition, three-dimensional imaging was used to assess changes in volume. Imaging data were not collected from nonresponders.
At 6 months, 86% of the treatment patients and 35% of the untreated controls met the response criteria. In addition, the evaluators rated 82% of treatment patients and 22% of controls as "improved" or "much improved," compared with pretreatment photos using the Global Aesthetic Improvement Scale, and 93% of treated patients rated themselves as improved or much improved, compared with pretreatment photos.
The average initial treatment was 5.2 mL, and 82% of treated patients received an optional touch-up injection of an average of 2 mL 30 days after the first treatment. The injection techniques were consistent with the methods used for other currently available fillers.
Individuals were excluded from the study if they had permanent or semipermanent facial aesthetic procedures, temporary facial aesthetic procedures within the washout period, midface volume loss unrelated to age, or very thin skin in the midface.
Greater baseline volume deficit was a stronger predictor than age of the volume of filler injected, although both factors were associated with a greater volume injected, said Todd Gross, Ph.D., a biostatistician for Allergan.
However, age, volume of product injected, and tunneling technique were associated with an increased risk of adverse events, said Dr. Janette Alexander, an FDA medical officer.
A total of 33% of the participants reported treatment-related adverse events. Five patients had late-onset adverse events; three of these were deemed severe and device related. The three severe treatment-related events involved lumps at the injection sites, all of which were treated with hyaluronidase, Dr. Alexander said.
The other two serious events included a death caused by stroke 1 year after treatment, and an ischemic optic neuropathy that the FDA could not definitely deem device related.
Approximately 78% of subjects reported an injection site response, but the majority of these resolved within 30 days. Injection site responses included firmness, lumps or bumps, tenderness, swelling, pain, bruising, redness, and discoloration. Approximately 20% of treated patients reported firmness or lumps/bumps persisting longer than 30 days.
The safety profile appears similar to that of other hyaluronic acid fillers except for the duration of firmness and lumps/bumps, and the occurrence of late adverse events, Dr. Alexander said.
No increase in risk of adverse events was observed in darker skin types, said Alvin Van Orden, of the FDA’s division of biostatistics.
The panel agreed that the postapproval study of 12 months’ follow-up proposed by Allergan is adequate, but extra attention should be paid to the subset of patients with darker skin, who might respond differently to the treatment, said panel chair Dr. Joseph LoCicero III, of the State University of New York, Brooklyn.
The panelists’ comments in support of their votes included acknowledgment of the safety profile and the reversibility of the product if needed, and the benefits of having an FDA-approved product for volume enhancement.
During their discussion, the panel members also agreed that setting upper limits on filler volume, age, and relative skin thickness should be left to clinical judgment, and not contraindicated.
Members of FDA advisory panels have been cleared of potential conflicts of interest related to the products under discussion prior to the meeting.
AT AN FDA ADVISORY COMMITTEE MEETING
Don't miss these emerging hair diseases
WASHINGTON – Potentially puzzling hair diseases might be one of three emerging types of alopecia: psoriatic, frontal fibrosing, and permanent chemotherapy induced, according to Dr. Leonard Sperling.
"You have a good chance of seeing these in the coming year," he said.
Psoriatic alopecia claims features of both cicatricial and noncicatricial alopecia, said Dr. Sperling of the Uniformed Services University of the Health Sciences, Bethesda, Md. "It is a histological mimic of alopecia areata," he noted.
However, sebaceous gland atrophy is evident on histology and is a dependable diagnostic feature. "That’s what sets this disease apart," Dr. Sperling said.
A clinical differential diagnosis of psoriatic alopecia may include tinea capitis, chronic cutaneous systemic lupus erythematosus, seborrheic dermatitis, syphilitic alopecia, and psoriasis plus alopecia areata, he said.
Psoriatic alopecia is not new; a case was reported in 1972 (Br. J. Dermatol. 1972;87:73-7).
Clinical studies of treatment outcomes are limited, but one review of data from 47 cases of psoriatic alopecia showed that most patients had complete hair regrowth, although five patients developed residual scarring, Dr. Sperling noted (Dermatology 1992;185:82-7).
"The prognosis for hair regrowth seems to be favorable, but we have more to learn about this condition," he said.
Another emerging hair disease, psoriatic alopecialike reaction to tumor necrosis factor–inhibitor therapy is becoming increasingly common, Dr. Sperling said.
"If you haven’t seen this yet, I predict that you will, as the biologics are more utilized," he said. All the TNF-alpha inhibitors have been associated with this.
It is psoriasis from hell.
"The follicular findings resemble those seen in alopecia areata, in that there is a lot of hair miniaturization" and inflammation, Dr. Sperling said. Numerous different plasma cells and eosinophils are evident on histology, which would be unusual in alopecia areata, he noted. Atrophy of the sebaceous glands also is evident. Recognizing the role of the underlying drug is important to make the diagnosis, he added.
The reason for the atrophy of the sebaceous glands in these cases, as in patients with psoriatic alopecia, remains unknown, Dr. Sperling said.
Frontal fibrosing alopecia is becoming more common, "It’s like an epidemic," said Dr. Sperling. It is becoming more common, especially in the black community, although it was historically described in postmenopausal white women, he said. Frontal fibrosing alopecia can be mistaken for traction alopecia in black women in particular, he noted. However, it can be distinguished from traction alopecia by the loss of eyebrow hair, which might be a clue to consider a biopsy. "The histology is what you would expect in lichen planopilaris," he noted.
Fibrosing alopecia in a pattern distribution is another condition that might be mistaken for lichen planopilaris, Dr. Sperling said. The pattern of hair loss resembles common balding, "but there is inflammation in the zone of thinning," he said. If a biopsy also shows lichenoid changes and obliteration of follicles, consider a diagnosis of fibrosing alopecia in a pattern distribution. "A lot of the inflammation is concentrated around miniaturized hair follicles," he said, but terminal hair follicles are involved as well.
Permanent chemotherapy-induced alopecia occurs in some chemotherapy patients.
"A sizable number of chemotherapy patients develop some type of permanent hair loss after treatment," Dr. Sperling said. Data from biopsies have shown areas of permanent hair loss, but also telogenlike structures, with a curious, amoeboid shape, he said. However, similar structures have been identified in patients with linear morphea, suggesting that these features are not uniquely characteristic of postchemotherapy permanent alopecia, he said.
Instead, they seem to be some sort of end-stage marker for a follicle that isn’t going to grow back, he said.
Dr. Sperling said he had no relevant financial conflicts.
On Twitter @hsplete
WASHINGTON – Potentially puzzling hair diseases might be one of three emerging types of alopecia: psoriatic, frontal fibrosing, and permanent chemotherapy induced, according to Dr. Leonard Sperling.
"You have a good chance of seeing these in the coming year," he said.
Psoriatic alopecia claims features of both cicatricial and noncicatricial alopecia, said Dr. Sperling of the Uniformed Services University of the Health Sciences, Bethesda, Md. "It is a histological mimic of alopecia areata," he noted.
However, sebaceous gland atrophy is evident on histology and is a dependable diagnostic feature. "That’s what sets this disease apart," Dr. Sperling said.
A clinical differential diagnosis of psoriatic alopecia may include tinea capitis, chronic cutaneous systemic lupus erythematosus, seborrheic dermatitis, syphilitic alopecia, and psoriasis plus alopecia areata, he said.
Psoriatic alopecia is not new; a case was reported in 1972 (Br. J. Dermatol. 1972;87:73-7).
Clinical studies of treatment outcomes are limited, but one review of data from 47 cases of psoriatic alopecia showed that most patients had complete hair regrowth, although five patients developed residual scarring, Dr. Sperling noted (Dermatology 1992;185:82-7).
"The prognosis for hair regrowth seems to be favorable, but we have more to learn about this condition," he said.
Another emerging hair disease, psoriatic alopecialike reaction to tumor necrosis factor–inhibitor therapy is becoming increasingly common, Dr. Sperling said.
"If you haven’t seen this yet, I predict that you will, as the biologics are more utilized," he said. All the TNF-alpha inhibitors have been associated with this.
It is psoriasis from hell.
"The follicular findings resemble those seen in alopecia areata, in that there is a lot of hair miniaturization" and inflammation, Dr. Sperling said. Numerous different plasma cells and eosinophils are evident on histology, which would be unusual in alopecia areata, he noted. Atrophy of the sebaceous glands also is evident. Recognizing the role of the underlying drug is important to make the diagnosis, he added.
The reason for the atrophy of the sebaceous glands in these cases, as in patients with psoriatic alopecia, remains unknown, Dr. Sperling said.
Frontal fibrosing alopecia is becoming more common, "It’s like an epidemic," said Dr. Sperling. It is becoming more common, especially in the black community, although it was historically described in postmenopausal white women, he said. Frontal fibrosing alopecia can be mistaken for traction alopecia in black women in particular, he noted. However, it can be distinguished from traction alopecia by the loss of eyebrow hair, which might be a clue to consider a biopsy. "The histology is what you would expect in lichen planopilaris," he noted.
Fibrosing alopecia in a pattern distribution is another condition that might be mistaken for lichen planopilaris, Dr. Sperling said. The pattern of hair loss resembles common balding, "but there is inflammation in the zone of thinning," he said. If a biopsy also shows lichenoid changes and obliteration of follicles, consider a diagnosis of fibrosing alopecia in a pattern distribution. "A lot of the inflammation is concentrated around miniaturized hair follicles," he said, but terminal hair follicles are involved as well.
Permanent chemotherapy-induced alopecia occurs in some chemotherapy patients.
"A sizable number of chemotherapy patients develop some type of permanent hair loss after treatment," Dr. Sperling said. Data from biopsies have shown areas of permanent hair loss, but also telogenlike structures, with a curious, amoeboid shape, he said. However, similar structures have been identified in patients with linear morphea, suggesting that these features are not uniquely characteristic of postchemotherapy permanent alopecia, he said.
Instead, they seem to be some sort of end-stage marker for a follicle that isn’t going to grow back, he said.
Dr. Sperling said he had no relevant financial conflicts.
On Twitter @hsplete
WASHINGTON – Potentially puzzling hair diseases might be one of three emerging types of alopecia: psoriatic, frontal fibrosing, and permanent chemotherapy induced, according to Dr. Leonard Sperling.
"You have a good chance of seeing these in the coming year," he said.
Psoriatic alopecia claims features of both cicatricial and noncicatricial alopecia, said Dr. Sperling of the Uniformed Services University of the Health Sciences, Bethesda, Md. "It is a histological mimic of alopecia areata," he noted.
However, sebaceous gland atrophy is evident on histology and is a dependable diagnostic feature. "That’s what sets this disease apart," Dr. Sperling said.
A clinical differential diagnosis of psoriatic alopecia may include tinea capitis, chronic cutaneous systemic lupus erythematosus, seborrheic dermatitis, syphilitic alopecia, and psoriasis plus alopecia areata, he said.
Psoriatic alopecia is not new; a case was reported in 1972 (Br. J. Dermatol. 1972;87:73-7).
Clinical studies of treatment outcomes are limited, but one review of data from 47 cases of psoriatic alopecia showed that most patients had complete hair regrowth, although five patients developed residual scarring, Dr. Sperling noted (Dermatology 1992;185:82-7).
"The prognosis for hair regrowth seems to be favorable, but we have more to learn about this condition," he said.
Another emerging hair disease, psoriatic alopecialike reaction to tumor necrosis factor–inhibitor therapy is becoming increasingly common, Dr. Sperling said.
"If you haven’t seen this yet, I predict that you will, as the biologics are more utilized," he said. All the TNF-alpha inhibitors have been associated with this.
It is psoriasis from hell.
"The follicular findings resemble those seen in alopecia areata, in that there is a lot of hair miniaturization" and inflammation, Dr. Sperling said. Numerous different plasma cells and eosinophils are evident on histology, which would be unusual in alopecia areata, he noted. Atrophy of the sebaceous glands also is evident. Recognizing the role of the underlying drug is important to make the diagnosis, he added.
The reason for the atrophy of the sebaceous glands in these cases, as in patients with psoriatic alopecia, remains unknown, Dr. Sperling said.
Frontal fibrosing alopecia is becoming more common, "It’s like an epidemic," said Dr. Sperling. It is becoming more common, especially in the black community, although it was historically described in postmenopausal white women, he said. Frontal fibrosing alopecia can be mistaken for traction alopecia in black women in particular, he noted. However, it can be distinguished from traction alopecia by the loss of eyebrow hair, which might be a clue to consider a biopsy. "The histology is what you would expect in lichen planopilaris," he noted.
Fibrosing alopecia in a pattern distribution is another condition that might be mistaken for lichen planopilaris, Dr. Sperling said. The pattern of hair loss resembles common balding, "but there is inflammation in the zone of thinning," he said. If a biopsy also shows lichenoid changes and obliteration of follicles, consider a diagnosis of fibrosing alopecia in a pattern distribution. "A lot of the inflammation is concentrated around miniaturized hair follicles," he said, but terminal hair follicles are involved as well.
Permanent chemotherapy-induced alopecia occurs in some chemotherapy patients.
"A sizable number of chemotherapy patients develop some type of permanent hair loss after treatment," Dr. Sperling said. Data from biopsies have shown areas of permanent hair loss, but also telogenlike structures, with a curious, amoeboid shape, he said. However, similar structures have been identified in patients with linear morphea, suggesting that these features are not uniquely characteristic of postchemotherapy permanent alopecia, he said.
Instead, they seem to be some sort of end-stage marker for a follicle that isn’t going to grow back, he said.
Dr. Sperling said he had no relevant financial conflicts.
On Twitter @hsplete
EXPERT ANALYSIS FROM THE ATLANTIC DERMATOLOGICAL CONFERENCE
Hold your hoarseness: Tips for tackling challenging cases
WASHINGTON – If your patient complains of hoarseness, how do you handle it? Although the causes of hoarseness are often obvious, many patients with hoarseness have vocal folds that appear normal, which can create a diagnostic challenge, said Dr. Seth M. Cohen of Duke University Medical Center in Durham, N.C., and Dr. J. Pieter Noordzij of Boston Medical Center.
Some of the most common causes of hoarseness in patients with normal-looking vocal folds are muscle tension/functional dysphonia, spasmodic dysphonia, vocal fold tremor, Parkinson’s disease, presbylaryngis (vocal fold atrophy), and amyotrophic lateral sclerosis. Dr. Cohen and Dr. Noordzij reviewed these conditions and shared cases at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
The Work-Up
When evaluating a patient’s hoarseness, start with a history and physical exam. The history should include the duration of hoarseness, how it started, family history of hoarseness, and the patient’s vocal demands that could contribute to overuse of the voice, Dr. Cohen said. Fluid intake (or lack of) can play a role, as can certain medical conditions such as gastroesophageal reflux disease (GERD) and allergies involving postnasal drip, he said.
The complete evaluation of a hoarse patient should include a full head and neck exam and a full cranial nerve exam, as well as an assessment of general appearance, facial expression, and endolaryngeal findings, Dr. Cohen said.
In addition, clinicians can use a perceptual voice analysis to try to characterize the general voice quality in terms of roughness (raspy), breathiness, strain (voice breaking), pitch (may be lower than normal), articulation, and speed, Dr. Cohen said. Techniques to evaluate patients include asking them to whisper, sing, make sustained vowel sounds (aaah, eee, ooo), and count from 60 to 69 and from 80 to 89.
Although some patients with hoarseness may benefit from surgical procedures, voice therapy is usually the first choice for treatment, he noted.
"Listen to the patient, listen to what they tell you, and listen to what they sound like," Dr. Cohen said.
Muscle Tension/Functional Dysphonia
Patients with muscle tension and functional dysphonia have excessive tension or poor coordination of the muscles in and near the voice box. The hoarseness in these patients often occurs after a cold and may be worse at the end of the day, said Dr. Noordzij.
On physical exam, this patient’s voice may be raspy and lower in pitch than normal. Someone who puts heavy demands on their voice might be susceptible to this condition, Dr. Noordzij said. They perceive their voice as strained and lower pitched, and they feel that are talking at the end of a breath. An endolaryngeal exam may show a gap between the vocal folds and squeezing of the larynx above the vocal folds (called a supraglottic constriction).
Spasmodic Dysphonia
Spasmodic dysphonia (SD) most often occurs in adulthood and can be triggered by a major life stress, Dr. Noordzij said. SD is a neurologic problem, not a functional one, he noted. SD is a movement disorder that involves involuntary, repetitive contractions of the laryngeal muscles. SD may be one of two types: adductor (a spasm that pushes the vocal folds together) or abductor (a spasm that causes the vocal cords to pull apart). Adductor spasmodic dysphonia is the most common form. Vocal characteristics include a strained or strangled voice that breaks on voiced syllables. However, voice breaks do not occur when the patient whispers, sings, or speaks in a falsetto, Dr. Noordzij said.
Vocal Fold Tremor
Vocal tremor is a central nervous system disorder that can be associated with other tremor conditions such as Parkinson’s disease, cerebellar ataxia, and spasmodic dysphonia, Dr. Cohen said.
"The hallmark of the condition is a rhythmic alteration in both the pitch and the loudness," he said. Vocal tremor may be exacerbated by stress or fatigue, and there may be a family history of tremor, he added.
On physical exam, patients with vocal tremor also may have tremor of the hands, head, jaw, voice, pharynx, tongue, or palate. Oscillations of pitch and amplitude are most noticeable during sustained vowels.
Parkinson’s Disease
Patients with Parkinson’s disease can present with voice complaints before they have a Parkinson’s diagnosis, although they also may exhibit Parkinson’s symptoms including hand tremor, rigidity, drooling, or a shuffling gait, Dr. Cohen said.
Hoarseness in these patients is characterized by breathy, flat voice, in a monotone, with breaths at inappropriate times. Patients also may have decreased blinking and a lack of facial expression.
Parkinson’s patients may have a history of not realizing the low volume of their voices, and they may take breaths at inappropriate times, Dr. Cohen noted. An endolaryngeal exam may show evidence of vocal fold bowing and a pooling of secretions, he said.
Presbylaryngis
Presbylaryngis, also known as vocal fold atrophy, is caused by age-related changes in the vocal folds, including ossification of laryngeal cartilage, decreased muscle bulk, decreased mucus production, and thickening or thinning of the epithelium.
"This is one of the hardest problems to treat surgically," Dr. Cohen said. Therefore, voice therapy is the first line treatment, he said.
In general, the pitch of men’s voices rises in cases of presbylaryngis, while the pitch of women’s voices decreases, Dr. Cohen noted. Patients perceive their voices as breathy and weak, with vocal fatigue and decreased ability to project their voices.
Amyotrophic Lateral Sclerosis
Approximately 25% of patients with amyotrophic lateral sclerosis (ALS) present with speech and swallowing problems. ALS is a progressive degeneration of the upper and lower motor neurons. Speech in these patients is typically slow, weak, and hypernasal, said Dr. Cohen. ALS patients may have dysarthria (disturbance of articulation) as well as dysphonia, and involuntary twitches of the tongue, he added.
Neither Dr. Cohen nor Dr. Noordzij had any financial conflicts to disclose.
WASHINGTON – If your patient complains of hoarseness, how do you handle it? Although the causes of hoarseness are often obvious, many patients with hoarseness have vocal folds that appear normal, which can create a diagnostic challenge, said Dr. Seth M. Cohen of Duke University Medical Center in Durham, N.C., and Dr. J. Pieter Noordzij of Boston Medical Center.
Some of the most common causes of hoarseness in patients with normal-looking vocal folds are muscle tension/functional dysphonia, spasmodic dysphonia, vocal fold tremor, Parkinson’s disease, presbylaryngis (vocal fold atrophy), and amyotrophic lateral sclerosis. Dr. Cohen and Dr. Noordzij reviewed these conditions and shared cases at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
The Work-Up
When evaluating a patient’s hoarseness, start with a history and physical exam. The history should include the duration of hoarseness, how it started, family history of hoarseness, and the patient’s vocal demands that could contribute to overuse of the voice, Dr. Cohen said. Fluid intake (or lack of) can play a role, as can certain medical conditions such as gastroesophageal reflux disease (GERD) and allergies involving postnasal drip, he said.
The complete evaluation of a hoarse patient should include a full head and neck exam and a full cranial nerve exam, as well as an assessment of general appearance, facial expression, and endolaryngeal findings, Dr. Cohen said.
In addition, clinicians can use a perceptual voice analysis to try to characterize the general voice quality in terms of roughness (raspy), breathiness, strain (voice breaking), pitch (may be lower than normal), articulation, and speed, Dr. Cohen said. Techniques to evaluate patients include asking them to whisper, sing, make sustained vowel sounds (aaah, eee, ooo), and count from 60 to 69 and from 80 to 89.
Although some patients with hoarseness may benefit from surgical procedures, voice therapy is usually the first choice for treatment, he noted.
"Listen to the patient, listen to what they tell you, and listen to what they sound like," Dr. Cohen said.
Muscle Tension/Functional Dysphonia
Patients with muscle tension and functional dysphonia have excessive tension or poor coordination of the muscles in and near the voice box. The hoarseness in these patients often occurs after a cold and may be worse at the end of the day, said Dr. Noordzij.
On physical exam, this patient’s voice may be raspy and lower in pitch than normal. Someone who puts heavy demands on their voice might be susceptible to this condition, Dr. Noordzij said. They perceive their voice as strained and lower pitched, and they feel that are talking at the end of a breath. An endolaryngeal exam may show a gap between the vocal folds and squeezing of the larynx above the vocal folds (called a supraglottic constriction).
Spasmodic Dysphonia
Spasmodic dysphonia (SD) most often occurs in adulthood and can be triggered by a major life stress, Dr. Noordzij said. SD is a neurologic problem, not a functional one, he noted. SD is a movement disorder that involves involuntary, repetitive contractions of the laryngeal muscles. SD may be one of two types: adductor (a spasm that pushes the vocal folds together) or abductor (a spasm that causes the vocal cords to pull apart). Adductor spasmodic dysphonia is the most common form. Vocal characteristics include a strained or strangled voice that breaks on voiced syllables. However, voice breaks do not occur when the patient whispers, sings, or speaks in a falsetto, Dr. Noordzij said.
Vocal Fold Tremor
Vocal tremor is a central nervous system disorder that can be associated with other tremor conditions such as Parkinson’s disease, cerebellar ataxia, and spasmodic dysphonia, Dr. Cohen said.
"The hallmark of the condition is a rhythmic alteration in both the pitch and the loudness," he said. Vocal tremor may be exacerbated by stress or fatigue, and there may be a family history of tremor, he added.
On physical exam, patients with vocal tremor also may have tremor of the hands, head, jaw, voice, pharynx, tongue, or palate. Oscillations of pitch and amplitude are most noticeable during sustained vowels.
Parkinson’s Disease
Patients with Parkinson’s disease can present with voice complaints before they have a Parkinson’s diagnosis, although they also may exhibit Parkinson’s symptoms including hand tremor, rigidity, drooling, or a shuffling gait, Dr. Cohen said.
Hoarseness in these patients is characterized by breathy, flat voice, in a monotone, with breaths at inappropriate times. Patients also may have decreased blinking and a lack of facial expression.
Parkinson’s patients may have a history of not realizing the low volume of their voices, and they may take breaths at inappropriate times, Dr. Cohen noted. An endolaryngeal exam may show evidence of vocal fold bowing and a pooling of secretions, he said.
Presbylaryngis
Presbylaryngis, also known as vocal fold atrophy, is caused by age-related changes in the vocal folds, including ossification of laryngeal cartilage, decreased muscle bulk, decreased mucus production, and thickening or thinning of the epithelium.
"This is one of the hardest problems to treat surgically," Dr. Cohen said. Therefore, voice therapy is the first line treatment, he said.
In general, the pitch of men’s voices rises in cases of presbylaryngis, while the pitch of women’s voices decreases, Dr. Cohen noted. Patients perceive their voices as breathy and weak, with vocal fatigue and decreased ability to project their voices.
Amyotrophic Lateral Sclerosis
Approximately 25% of patients with amyotrophic lateral sclerosis (ALS) present with speech and swallowing problems. ALS is a progressive degeneration of the upper and lower motor neurons. Speech in these patients is typically slow, weak, and hypernasal, said Dr. Cohen. ALS patients may have dysarthria (disturbance of articulation) as well as dysphonia, and involuntary twitches of the tongue, he added.
Neither Dr. Cohen nor Dr. Noordzij had any financial conflicts to disclose.
WASHINGTON – If your patient complains of hoarseness, how do you handle it? Although the causes of hoarseness are often obvious, many patients with hoarseness have vocal folds that appear normal, which can create a diagnostic challenge, said Dr. Seth M. Cohen of Duke University Medical Center in Durham, N.C., and Dr. J. Pieter Noordzij of Boston Medical Center.
Some of the most common causes of hoarseness in patients with normal-looking vocal folds are muscle tension/functional dysphonia, spasmodic dysphonia, vocal fold tremor, Parkinson’s disease, presbylaryngis (vocal fold atrophy), and amyotrophic lateral sclerosis. Dr. Cohen and Dr. Noordzij reviewed these conditions and shared cases at the annual meeting of the American Academy of Otolaryngology – Head and Neck Surgery Foundation.
The Work-Up
When evaluating a patient’s hoarseness, start with a history and physical exam. The history should include the duration of hoarseness, how it started, family history of hoarseness, and the patient’s vocal demands that could contribute to overuse of the voice, Dr. Cohen said. Fluid intake (or lack of) can play a role, as can certain medical conditions such as gastroesophageal reflux disease (GERD) and allergies involving postnasal drip, he said.
The complete evaluation of a hoarse patient should include a full head and neck exam and a full cranial nerve exam, as well as an assessment of general appearance, facial expression, and endolaryngeal findings, Dr. Cohen said.
In addition, clinicians can use a perceptual voice analysis to try to characterize the general voice quality in terms of roughness (raspy), breathiness, strain (voice breaking), pitch (may be lower than normal), articulation, and speed, Dr. Cohen said. Techniques to evaluate patients include asking them to whisper, sing, make sustained vowel sounds (aaah, eee, ooo), and count from 60 to 69 and from 80 to 89.
Although some patients with hoarseness may benefit from surgical procedures, voice therapy is usually the first choice for treatment, he noted.
"Listen to the patient, listen to what they tell you, and listen to what they sound like," Dr. Cohen said.
Muscle Tension/Functional Dysphonia
Patients with muscle tension and functional dysphonia have excessive tension or poor coordination of the muscles in and near the voice box. The hoarseness in these patients often occurs after a cold and may be worse at the end of the day, said Dr. Noordzij.
On physical exam, this patient’s voice may be raspy and lower in pitch than normal. Someone who puts heavy demands on their voice might be susceptible to this condition, Dr. Noordzij said. They perceive their voice as strained and lower pitched, and they feel that are talking at the end of a breath. An endolaryngeal exam may show a gap between the vocal folds and squeezing of the larynx above the vocal folds (called a supraglottic constriction).
Spasmodic Dysphonia
Spasmodic dysphonia (SD) most often occurs in adulthood and can be triggered by a major life stress, Dr. Noordzij said. SD is a neurologic problem, not a functional one, he noted. SD is a movement disorder that involves involuntary, repetitive contractions of the laryngeal muscles. SD may be one of two types: adductor (a spasm that pushes the vocal folds together) or abductor (a spasm that causes the vocal cords to pull apart). Adductor spasmodic dysphonia is the most common form. Vocal characteristics include a strained or strangled voice that breaks on voiced syllables. However, voice breaks do not occur when the patient whispers, sings, or speaks in a falsetto, Dr. Noordzij said.
Vocal Fold Tremor
Vocal tremor is a central nervous system disorder that can be associated with other tremor conditions such as Parkinson’s disease, cerebellar ataxia, and spasmodic dysphonia, Dr. Cohen said.
"The hallmark of the condition is a rhythmic alteration in both the pitch and the loudness," he said. Vocal tremor may be exacerbated by stress or fatigue, and there may be a family history of tremor, he added.
On physical exam, patients with vocal tremor also may have tremor of the hands, head, jaw, voice, pharynx, tongue, or palate. Oscillations of pitch and amplitude are most noticeable during sustained vowels.
Parkinson’s Disease
Patients with Parkinson’s disease can present with voice complaints before they have a Parkinson’s diagnosis, although they also may exhibit Parkinson’s symptoms including hand tremor, rigidity, drooling, or a shuffling gait, Dr. Cohen said.
Hoarseness in these patients is characterized by breathy, flat voice, in a monotone, with breaths at inappropriate times. Patients also may have decreased blinking and a lack of facial expression.
Parkinson’s patients may have a history of not realizing the low volume of their voices, and they may take breaths at inappropriate times, Dr. Cohen noted. An endolaryngeal exam may show evidence of vocal fold bowing and a pooling of secretions, he said.
Presbylaryngis
Presbylaryngis, also known as vocal fold atrophy, is caused by age-related changes in the vocal folds, including ossification of laryngeal cartilage, decreased muscle bulk, decreased mucus production, and thickening or thinning of the epithelium.
"This is one of the hardest problems to treat surgically," Dr. Cohen said. Therefore, voice therapy is the first line treatment, he said.
In general, the pitch of men’s voices rises in cases of presbylaryngis, while the pitch of women’s voices decreases, Dr. Cohen noted. Patients perceive their voices as breathy and weak, with vocal fatigue and decreased ability to project their voices.
Amyotrophic Lateral Sclerosis
Approximately 25% of patients with amyotrophic lateral sclerosis (ALS) present with speech and swallowing problems. ALS is a progressive degeneration of the upper and lower motor neurons. Speech in these patients is typically slow, weak, and hypernasal, said Dr. Cohen. ALS patients may have dysarthria (disturbance of articulation) as well as dysphonia, and involuntary twitches of the tongue, he added.
Neither Dr. Cohen nor Dr. Noordzij had any financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF OTOLARYNGOLOGY HEAD AND NECK SURGERY FOUNDATION
Nanoparticles take aim at acne
Nanotechnology stands to make a big difference in the way acne is treated.
A 0.1% concentration of benzoyl peroxide encapsulated in chitosan-alginate nanoparticles showed more antimicrobial activity against acne bacteria than typical benzoyl peroxide or the nanoparticles alone in a recently published in vitro study (J. Invest. Dermatol. 2012 Nov. 29 [doi:10.1038/jid.2012.399]).
Chitosan-alginate has both antimicrobial and anti-inflammatory impact on Propionibacterium acnes, wrote Dr. Adam Friedman of Albert Einstein College of Medicine, New York, and his colleagues. The nanoparticle structure preserves the antimicrobial and immunological properties of chitosan while alginate lends stability.
Benzoyl peroxide is, of course, already a first-line therapy for acne, but encapsulating benzoyl peroxide in the nanoparticles stands to reduce the irritating side effects common with topical benzoyl peroxide use, the researchers noted. Less irritation could greatly improve patient compliance.
In the study, scanning electron microscopy and transmission electron microscopy showed "severe disruption, destruction, and ‘peeling’ of the cell wall," the researchers wrote. "These images suggest that the cell damage is due to an osmotic disturbance" created by the encapsulated benzoyl peroxide.
Nanoparticle encapsulation "provides previously undescribed therapeutic opportunities, including delivery of multidrug regimens to combat resistant microbes and inflammatory disease states," the researchers said.
Nanotechnology stands to make a big difference in the way acne is treated.
A 0.1% concentration of benzoyl peroxide encapsulated in chitosan-alginate nanoparticles showed more antimicrobial activity against acne bacteria than typical benzoyl peroxide or the nanoparticles alone in a recently published in vitro study (J. Invest. Dermatol. 2012 Nov. 29 [doi:10.1038/jid.2012.399]).
Chitosan-alginate has both antimicrobial and anti-inflammatory impact on Propionibacterium acnes, wrote Dr. Adam Friedman of Albert Einstein College of Medicine, New York, and his colleagues. The nanoparticle structure preserves the antimicrobial and immunological properties of chitosan while alginate lends stability.
Benzoyl peroxide is, of course, already a first-line therapy for acne, but encapsulating benzoyl peroxide in the nanoparticles stands to reduce the irritating side effects common with topical benzoyl peroxide use, the researchers noted. Less irritation could greatly improve patient compliance.
In the study, scanning electron microscopy and transmission electron microscopy showed "severe disruption, destruction, and ‘peeling’ of the cell wall," the researchers wrote. "These images suggest that the cell damage is due to an osmotic disturbance" created by the encapsulated benzoyl peroxide.
Nanoparticle encapsulation "provides previously undescribed therapeutic opportunities, including delivery of multidrug regimens to combat resistant microbes and inflammatory disease states," the researchers said.
Nanotechnology stands to make a big difference in the way acne is treated.
A 0.1% concentration of benzoyl peroxide encapsulated in chitosan-alginate nanoparticles showed more antimicrobial activity against acne bacteria than typical benzoyl peroxide or the nanoparticles alone in a recently published in vitro study (J. Invest. Dermatol. 2012 Nov. 29 [doi:10.1038/jid.2012.399]).
Chitosan-alginate has both antimicrobial and anti-inflammatory impact on Propionibacterium acnes, wrote Dr. Adam Friedman of Albert Einstein College of Medicine, New York, and his colleagues. The nanoparticle structure preserves the antimicrobial and immunological properties of chitosan while alginate lends stability.
Benzoyl peroxide is, of course, already a first-line therapy for acne, but encapsulating benzoyl peroxide in the nanoparticles stands to reduce the irritating side effects common with topical benzoyl peroxide use, the researchers noted. Less irritation could greatly improve patient compliance.
In the study, scanning electron microscopy and transmission electron microscopy showed "severe disruption, destruction, and ‘peeling’ of the cell wall," the researchers wrote. "These images suggest that the cell damage is due to an osmotic disturbance" created by the encapsulated benzoyl peroxide.
Nanoparticle encapsulation "provides previously undescribed therapeutic opportunities, including delivery of multidrug regimens to combat resistant microbes and inflammatory disease states," the researchers said.