User login
Jeff Evans has been editor of Rheumatology News/MDedge Rheumatology and the EULAR Congress News since 2013. He started at Frontline Medical Communications in 2001 and was a reporter for 8 years before serving as editor of Clinical Neurology News and World Neurology, and briefly as editor of GI & Hepatology News. He graduated cum laude from Cornell University (New York) with a BA in biological sciences, concentrating in neurobiology and behavior.
Neurologists weigh in on rising drug prices
Neurologists will tackle the issues surrounding rising prices for neurological drug treatments in a set of presentations during the annual meeting of the American Academy of Neurology in Boston.
During the Contemporary Clinical Issues Plenary Session on April 24, Dennis N. Bourdette, MD, of Oregon Health and Science University, Portland, will give his presentation, “High Drug Prices: The Elephant in the Clinic.”
Dr. Bourdette will also address the problem on April 26 in a session called “Section Topic Controversies,” in which he and Dennis W. Choi, MD, PhD, of the State University of New York at Stony Brook will offer their opinions on how “Neurologists Should Take a Position Regarding the Cost of Neurological Treatments.” Dr. Bourdette is set to illustrate how “Neurologists Should More Vocally Protest Some of the Marked Price Increases Involving Neurological Treatments,” while Dr. Choi will provide rationale for his argument on why “Neurologists Should Influence Policies that Allow Companies to Commit More Resources to R&D for Neurological Diseases While Not Allowing for Rapacious Pricing Practices.” Following the discussion, Dr. Bourdette, Dr. Choi, and session moderators will have a panel discussion on the ways in which AAN members can work most productively for the benefit of their patients.
Sure to be discussed in the series of talks is a recent AAN position paper on prescription drug prices released in March that identified three distinct drug pricing challenges:
- Massive increase in the pricing of previously low-cost generic drugs used to treat common disorders without obvious increases in cost of production or distribution.
- Massive increase in the pricing for high-priced generic and brand name drugs used to treat serious disorders that are not protected by the Orphan Drug Act.
- The high cost of new medications used to treat rare disorders as defined by the Orphan Drug Act.
Neurologists will tackle the issues surrounding rising prices for neurological drug treatments in a set of presentations during the annual meeting of the American Academy of Neurology in Boston.
During the Contemporary Clinical Issues Plenary Session on April 24, Dennis N. Bourdette, MD, of Oregon Health and Science University, Portland, will give his presentation, “High Drug Prices: The Elephant in the Clinic.”
Dr. Bourdette will also address the problem on April 26 in a session called “Section Topic Controversies,” in which he and Dennis W. Choi, MD, PhD, of the State University of New York at Stony Brook will offer their opinions on how “Neurologists Should Take a Position Regarding the Cost of Neurological Treatments.” Dr. Bourdette is set to illustrate how “Neurologists Should More Vocally Protest Some of the Marked Price Increases Involving Neurological Treatments,” while Dr. Choi will provide rationale for his argument on why “Neurologists Should Influence Policies that Allow Companies to Commit More Resources to R&D for Neurological Diseases While Not Allowing for Rapacious Pricing Practices.” Following the discussion, Dr. Bourdette, Dr. Choi, and session moderators will have a panel discussion on the ways in which AAN members can work most productively for the benefit of their patients.
Sure to be discussed in the series of talks is a recent AAN position paper on prescription drug prices released in March that identified three distinct drug pricing challenges:
- Massive increase in the pricing of previously low-cost generic drugs used to treat common disorders without obvious increases in cost of production or distribution.
- Massive increase in the pricing for high-priced generic and brand name drugs used to treat serious disorders that are not protected by the Orphan Drug Act.
- The high cost of new medications used to treat rare disorders as defined by the Orphan Drug Act.
Neurologists will tackle the issues surrounding rising prices for neurological drug treatments in a set of presentations during the annual meeting of the American Academy of Neurology in Boston.
During the Contemporary Clinical Issues Plenary Session on April 24, Dennis N. Bourdette, MD, of Oregon Health and Science University, Portland, will give his presentation, “High Drug Prices: The Elephant in the Clinic.”
Dr. Bourdette will also address the problem on April 26 in a session called “Section Topic Controversies,” in which he and Dennis W. Choi, MD, PhD, of the State University of New York at Stony Brook will offer their opinions on how “Neurologists Should Take a Position Regarding the Cost of Neurological Treatments.” Dr. Bourdette is set to illustrate how “Neurologists Should More Vocally Protest Some of the Marked Price Increases Involving Neurological Treatments,” while Dr. Choi will provide rationale for his argument on why “Neurologists Should Influence Policies that Allow Companies to Commit More Resources to R&D for Neurological Diseases While Not Allowing for Rapacious Pricing Practices.” Following the discussion, Dr. Bourdette, Dr. Choi, and session moderators will have a panel discussion on the ways in which AAN members can work most productively for the benefit of their patients.
Sure to be discussed in the series of talks is a recent AAN position paper on prescription drug prices released in March that identified three distinct drug pricing challenges:
- Massive increase in the pricing of previously low-cost generic drugs used to treat common disorders without obvious increases in cost of production or distribution.
- Massive increase in the pricing for high-priced generic and brand name drugs used to treat serious disorders that are not protected by the Orphan Drug Act.
- The high cost of new medications used to treat rare disorders as defined by the Orphan Drug Act.
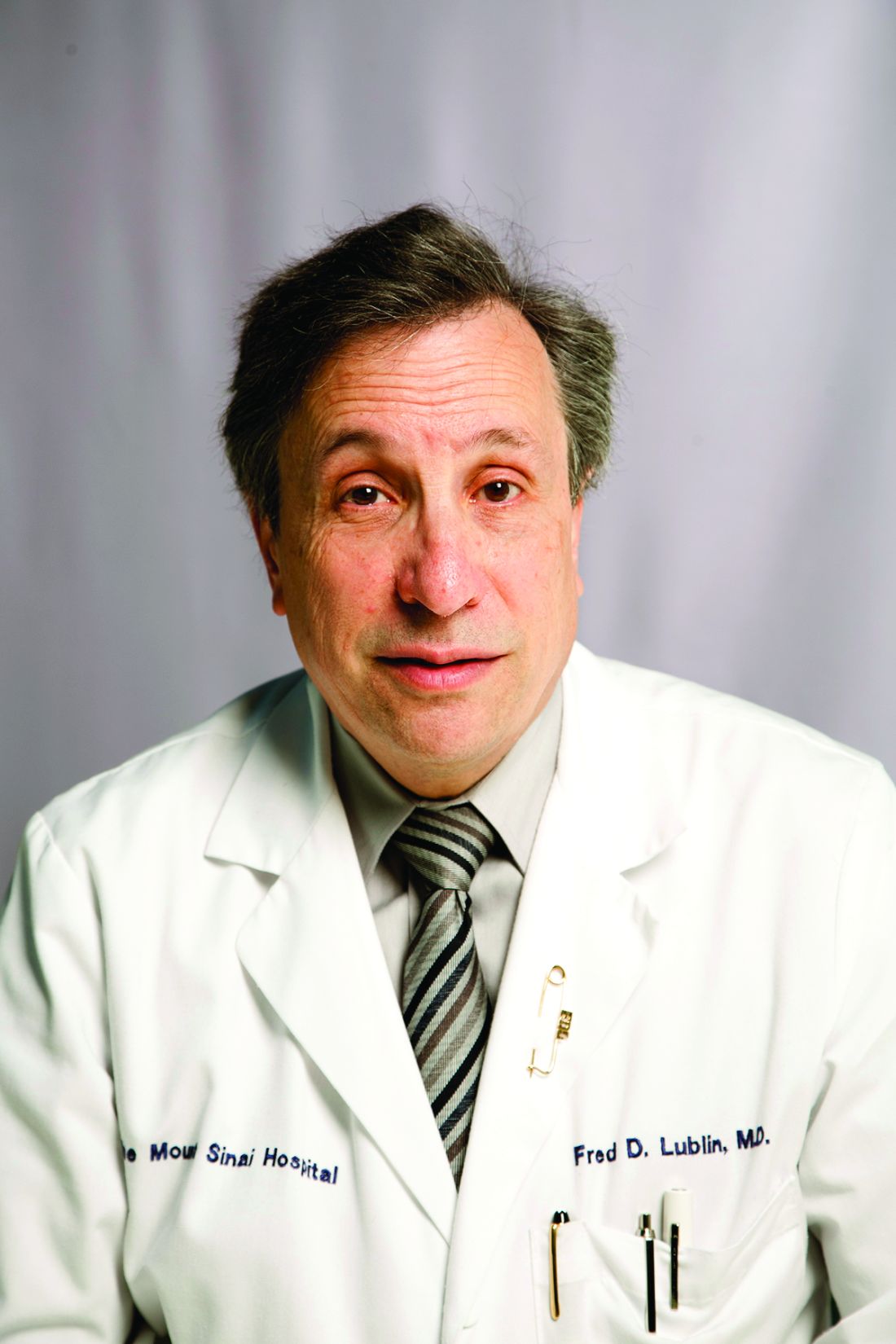
Ocrelizumab gets first-ever FDA approval for primary progressive MS
The humanized monoclonal antibody ocrelizumab became the first drug to receive approval from the Food and Drug Administration for the treatment of primary progressive multiple sclerosis in adults, according to a March 29 announcement from the agency that also said it is approved for relapsing-remitting disease in adults.
The drug has a mechanism of action similar to rituximab (Rituxan) through its selective targeting of CD20-positive B cells, which depletes them from circulation. CD20-positive B cells are thought to be a key contributor to myelin and axonal damage.
Although the effect of ocrelizumab on primary progressive MS patients was modest, its stature as the only drug approved for the indication represents “a start for being able to treat progressive MS,” Fred Lublin, MD, a member of the steering committee that designed and monitored the phase III ocrelizumab trials, said in an interview.
In the ORATORIO trial that randomized 732 patients with primary progressive MS in a 2:1 ratio to infusions of either 600 mg ocrelizumab or placebo every 24 weeks for 120 weeks, ocrelizumab reduced the risk of progression in clinical disability by 24% at 12 weeks (the primary end point), 25% at 24 weeks, and 24% at 120 weeks, compared with placebo (N Engl J Med. 2017 Jan 19;376[3]:209-20).
Over 120 weeks, the antibody also reduced the volume of hyperintense T2 lesions by 3.4%, whereas patients taking placebo experienced a 7.4% increase. The rate of whole brain volume loss was also significantly reduced from week 24 to 120 (–0.9% with ocrelizumab vs. –1.1% for placebo).
The group of patients who participated in ORATORIO was younger and had more activity on MRI, but it’s unclear if there is a progressive MS patient population who will respond best to the biologic, said Dr. Lublin, director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis at Mount Sinai Hospital in New York.
“The safety was acceptable, and so I think it will get a lot of use. There are always some who like to wait until a drug has been out for a while, but there is considerable experience with this type of drug based on off-label use of rituximab” in relapsing-remitting patients, including phase II trial data (but not phase III), he said. There’s potential for ocrelizumab to be used as a first-line treatment for relapsing-remitting disease to the same extent as natalizumab (Tysabri), he added.
In two identical phase III trials, OPERA I and OPERA II, investigators randomized 1,656 relapsing-remitting MS patients to intravenous ocrelizumab 600 mg every 24 weeks plus placebo subcutaneous injections three times weekly or to subcutaneous interferon beta-1a 44 mcg (Rebif) three times weekly plus placebo IV infusions every 24 weeks over 96 weeks (N Engl J Med. 2017 Jan 19;376[3]:221-34).
Compared with interferon beta-1a, ocrelizumab reduced the annualized relapse rate by 46% in OPERA 1 and 47% in OPERA 2. In a pooled analysis of both trials, the risk of confirmed disability progression was 40% lower for ocrelizumab at both 12 and 24 weeks. Ocrelizumab conferred a 94% and 95% reduction in the total number of T1 gadolinium-enhancing lesions and a 77% and 83% reduction in the total number of new and/or enlarging hyperintense T2 lesions. An exploratory analysis also suggested that the drug reduced the rate of whole brain volume loss, compared with interferon beta-1a.
At 96 weeks, 47.9% and 47.5% of ocrelizumab patients versus 29.2% and 25.1% of interferon patients had no evidence of disease activity (NEDA) in the two studies. NEDA is a composite score defined as no relapses, no confirmed disability progression, and no new or enlarging T2 or gadolinium-enhancing T1 lesions.
Across both studies, relapses occurred in about 20% of ocrelizumab patients versus about 35% of interferon patients. About 10% of ocrelizumab patients had clinical disease progression, compared with about 15% of interferon patients. Similarly, about 10% of ocrelizumab patients developed new gadolinium-enhancing lesions, compared with about 35% in the interferon groups. New or enlarging T2 lesions were found in about 40% in the ocrelizumab groups but in more than 60% in the interferon arms.
Safety results at 24 weeks in the OPERA trials showed that infusion reactions were significantly more common with ocrelizumab than with interferon beta-1a (34% vs. 9.7%), and most of these were mild to moderate in severity. Otherwise, there were similar rates of serious adverse events, including serious infections.
In ORATORIO, infusion reaction occurred in 40% of ocrelizumab patients and 26% of placebo patients. Most of the reactions were mild to moderate in severity. Among all patients in ORATORIO, 13 malignancies occurred over 3 years, and they occurred more than twice as often in the ocrelizumab arm than in the placebo arm (2.3% vs. 0.8%). These included four breast cancers in the active arm and none in the placebo arm.
No cases of progressive multifocal leukoencephalopathy (PML) have been reported in association with ocrelizumab, although the risk of PML with long-term use is unknown.
The FDA said in its announcement that ocrelizumab should not be used in patients with hepatitis B infection or a history of life-threatening infusion-related reactions to the drug. Ocrelizumab is required to be dispensed with a patient Medication Guide that describes important information about the drug’s uses and risks. The agency also advised that vaccination with live or live attenuated vaccines is not recommended in patients receiving the drug.
Genentech says it plans to offer patient assistance programs through Genentech Access Solutions.
Dr. Lublin reported receiving fees for serving on an advisory board from Genentech/Roche and from many other companies investigating or marketing drugs for MS.
The humanized monoclonal antibody ocrelizumab became the first drug to receive approval from the Food and Drug Administration for the treatment of primary progressive multiple sclerosis in adults, according to a March 29 announcement from the agency that also said it is approved for relapsing-remitting disease in adults.
The drug has a mechanism of action similar to rituximab (Rituxan) through its selective targeting of CD20-positive B cells, which depletes them from circulation. CD20-positive B cells are thought to be a key contributor to myelin and axonal damage.
Although the effect of ocrelizumab on primary progressive MS patients was modest, its stature as the only drug approved for the indication represents “a start for being able to treat progressive MS,” Fred Lublin, MD, a member of the steering committee that designed and monitored the phase III ocrelizumab trials, said in an interview.
In the ORATORIO trial that randomized 732 patients with primary progressive MS in a 2:1 ratio to infusions of either 600 mg ocrelizumab or placebo every 24 weeks for 120 weeks, ocrelizumab reduced the risk of progression in clinical disability by 24% at 12 weeks (the primary end point), 25% at 24 weeks, and 24% at 120 weeks, compared with placebo (N Engl J Med. 2017 Jan 19;376[3]:209-20).
Over 120 weeks, the antibody also reduced the volume of hyperintense T2 lesions by 3.4%, whereas patients taking placebo experienced a 7.4% increase. The rate of whole brain volume loss was also significantly reduced from week 24 to 120 (–0.9% with ocrelizumab vs. –1.1% for placebo).
The group of patients who participated in ORATORIO was younger and had more activity on MRI, but it’s unclear if there is a progressive MS patient population who will respond best to the biologic, said Dr. Lublin, director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis at Mount Sinai Hospital in New York.
“The safety was acceptable, and so I think it will get a lot of use. There are always some who like to wait until a drug has been out for a while, but there is considerable experience with this type of drug based on off-label use of rituximab” in relapsing-remitting patients, including phase II trial data (but not phase III), he said. There’s potential for ocrelizumab to be used as a first-line treatment for relapsing-remitting disease to the same extent as natalizumab (Tysabri), he added.
In two identical phase III trials, OPERA I and OPERA II, investigators randomized 1,656 relapsing-remitting MS patients to intravenous ocrelizumab 600 mg every 24 weeks plus placebo subcutaneous injections three times weekly or to subcutaneous interferon beta-1a 44 mcg (Rebif) three times weekly plus placebo IV infusions every 24 weeks over 96 weeks (N Engl J Med. 2017 Jan 19;376[3]:221-34).
Compared with interferon beta-1a, ocrelizumab reduced the annualized relapse rate by 46% in OPERA 1 and 47% in OPERA 2. In a pooled analysis of both trials, the risk of confirmed disability progression was 40% lower for ocrelizumab at both 12 and 24 weeks. Ocrelizumab conferred a 94% and 95% reduction in the total number of T1 gadolinium-enhancing lesions and a 77% and 83% reduction in the total number of new and/or enlarging hyperintense T2 lesions. An exploratory analysis also suggested that the drug reduced the rate of whole brain volume loss, compared with interferon beta-1a.
At 96 weeks, 47.9% and 47.5% of ocrelizumab patients versus 29.2% and 25.1% of interferon patients had no evidence of disease activity (NEDA) in the two studies. NEDA is a composite score defined as no relapses, no confirmed disability progression, and no new or enlarging T2 or gadolinium-enhancing T1 lesions.
Across both studies, relapses occurred in about 20% of ocrelizumab patients versus about 35% of interferon patients. About 10% of ocrelizumab patients had clinical disease progression, compared with about 15% of interferon patients. Similarly, about 10% of ocrelizumab patients developed new gadolinium-enhancing lesions, compared with about 35% in the interferon groups. New or enlarging T2 lesions were found in about 40% in the ocrelizumab groups but in more than 60% in the interferon arms.
Safety results at 24 weeks in the OPERA trials showed that infusion reactions were significantly more common with ocrelizumab than with interferon beta-1a (34% vs. 9.7%), and most of these were mild to moderate in severity. Otherwise, there were similar rates of serious adverse events, including serious infections.
In ORATORIO, infusion reaction occurred in 40% of ocrelizumab patients and 26% of placebo patients. Most of the reactions were mild to moderate in severity. Among all patients in ORATORIO, 13 malignancies occurred over 3 years, and they occurred more than twice as often in the ocrelizumab arm than in the placebo arm (2.3% vs. 0.8%). These included four breast cancers in the active arm and none in the placebo arm.
No cases of progressive multifocal leukoencephalopathy (PML) have been reported in association with ocrelizumab, although the risk of PML with long-term use is unknown.
The FDA said in its announcement that ocrelizumab should not be used in patients with hepatitis B infection or a history of life-threatening infusion-related reactions to the drug. Ocrelizumab is required to be dispensed with a patient Medication Guide that describes important information about the drug’s uses and risks. The agency also advised that vaccination with live or live attenuated vaccines is not recommended in patients receiving the drug.
Genentech says it plans to offer patient assistance programs through Genentech Access Solutions.
Dr. Lublin reported receiving fees for serving on an advisory board from Genentech/Roche and from many other companies investigating or marketing drugs for MS.
The humanized monoclonal antibody ocrelizumab became the first drug to receive approval from the Food and Drug Administration for the treatment of primary progressive multiple sclerosis in adults, according to a March 29 announcement from the agency that also said it is approved for relapsing-remitting disease in adults.
The drug has a mechanism of action similar to rituximab (Rituxan) through its selective targeting of CD20-positive B cells, which depletes them from circulation. CD20-positive B cells are thought to be a key contributor to myelin and axonal damage.
Although the effect of ocrelizumab on primary progressive MS patients was modest, its stature as the only drug approved for the indication represents “a start for being able to treat progressive MS,” Fred Lublin, MD, a member of the steering committee that designed and monitored the phase III ocrelizumab trials, said in an interview.
In the ORATORIO trial that randomized 732 patients with primary progressive MS in a 2:1 ratio to infusions of either 600 mg ocrelizumab or placebo every 24 weeks for 120 weeks, ocrelizumab reduced the risk of progression in clinical disability by 24% at 12 weeks (the primary end point), 25% at 24 weeks, and 24% at 120 weeks, compared with placebo (N Engl J Med. 2017 Jan 19;376[3]:209-20).
Over 120 weeks, the antibody also reduced the volume of hyperintense T2 lesions by 3.4%, whereas patients taking placebo experienced a 7.4% increase. The rate of whole brain volume loss was also significantly reduced from week 24 to 120 (–0.9% with ocrelizumab vs. –1.1% for placebo).
The group of patients who participated in ORATORIO was younger and had more activity on MRI, but it’s unclear if there is a progressive MS patient population who will respond best to the biologic, said Dr. Lublin, director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis at Mount Sinai Hospital in New York.
“The safety was acceptable, and so I think it will get a lot of use. There are always some who like to wait until a drug has been out for a while, but there is considerable experience with this type of drug based on off-label use of rituximab” in relapsing-remitting patients, including phase II trial data (but not phase III), he said. There’s potential for ocrelizumab to be used as a first-line treatment for relapsing-remitting disease to the same extent as natalizumab (Tysabri), he added.
In two identical phase III trials, OPERA I and OPERA II, investigators randomized 1,656 relapsing-remitting MS patients to intravenous ocrelizumab 600 mg every 24 weeks plus placebo subcutaneous injections three times weekly or to subcutaneous interferon beta-1a 44 mcg (Rebif) three times weekly plus placebo IV infusions every 24 weeks over 96 weeks (N Engl J Med. 2017 Jan 19;376[3]:221-34).
Compared with interferon beta-1a, ocrelizumab reduced the annualized relapse rate by 46% in OPERA 1 and 47% in OPERA 2. In a pooled analysis of both trials, the risk of confirmed disability progression was 40% lower for ocrelizumab at both 12 and 24 weeks. Ocrelizumab conferred a 94% and 95% reduction in the total number of T1 gadolinium-enhancing lesions and a 77% and 83% reduction in the total number of new and/or enlarging hyperintense T2 lesions. An exploratory analysis also suggested that the drug reduced the rate of whole brain volume loss, compared with interferon beta-1a.
At 96 weeks, 47.9% and 47.5% of ocrelizumab patients versus 29.2% and 25.1% of interferon patients had no evidence of disease activity (NEDA) in the two studies. NEDA is a composite score defined as no relapses, no confirmed disability progression, and no new or enlarging T2 or gadolinium-enhancing T1 lesions.
Across both studies, relapses occurred in about 20% of ocrelizumab patients versus about 35% of interferon patients. About 10% of ocrelizumab patients had clinical disease progression, compared with about 15% of interferon patients. Similarly, about 10% of ocrelizumab patients developed new gadolinium-enhancing lesions, compared with about 35% in the interferon groups. New or enlarging T2 lesions were found in about 40% in the ocrelizumab groups but in more than 60% in the interferon arms.
Safety results at 24 weeks in the OPERA trials showed that infusion reactions were significantly more common with ocrelizumab than with interferon beta-1a (34% vs. 9.7%), and most of these were mild to moderate in severity. Otherwise, there were similar rates of serious adverse events, including serious infections.
In ORATORIO, infusion reaction occurred in 40% of ocrelizumab patients and 26% of placebo patients. Most of the reactions were mild to moderate in severity. Among all patients in ORATORIO, 13 malignancies occurred over 3 years, and they occurred more than twice as often in the ocrelizumab arm than in the placebo arm (2.3% vs. 0.8%). These included four breast cancers in the active arm and none in the placebo arm.
No cases of progressive multifocal leukoencephalopathy (PML) have been reported in association with ocrelizumab, although the risk of PML with long-term use is unknown.
The FDA said in its announcement that ocrelizumab should not be used in patients with hepatitis B infection or a history of life-threatening infusion-related reactions to the drug. Ocrelizumab is required to be dispensed with a patient Medication Guide that describes important information about the drug’s uses and risks. The agency also advised that vaccination with live or live attenuated vaccines is not recommended in patients receiving the drug.
Genentech says it plans to offer patient assistance programs through Genentech Access Solutions.
Dr. Lublin reported receiving fees for serving on an advisory board from Genentech/Roche and from many other companies investigating or marketing drugs for MS.
Methotrexate use justified for early RA, disease prevention
Efforts to delay or prevent rheumatoid arthritis (RA) in individuals at high risk for the disease received a boost from the findings of a subgroup analysis of an older Dutch prevention trial involving methotrexate that were published recently in Arthritis & Rheumatology.
However, while the 22-patient subgroup analysis of the 2007 trial, called PROMPT (Probable RA: Methotrexate Versus Placebo Treatment), showed that 1 year of methotrexate prevented the development of rheumatoid arthritis in significantly more individuals at high risk for the disease than did placebo, hindsight has shown that most of these high-risk individuals actually had RA at baseline as defined by the 2010 American College or Rheumatology/European League Against Rheumatism classification criteria.
Even though the “landscape of RA has changed since this study was conceived, enrolled, and performed,” Dr. Sparks noted that the study provides evidence that today’s “standard of care really works” by making use of data that are unobtainable today.
“Nowadays, we wouldn’t be able to do a placebo-controlled trial in early RA because those patients need to be treated, but at the time, it was perfectly fine, based on the treatment landscape, to put these patients in a [placebo-controlled] trial,” he said in an interview.
“It also demonstrates that you really need to find high-risk individuals, because, if you recruit people who are never going to develop RA, you’re just diluting your effect, and you’re not going to find the difference in the groups based on that diluted effect when there could be a true effect in that special subgroup,” he added.
Senior study author Annette van der Helm-van Mil, MD, PhD, and her colleagues at Leiden (the Netherlands) University Medical Center performed the reanalysis after the initial finding that methotrexate had no preventative effect may have been falsely negative because the study included patients with a low risk of progressing to RA (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40062).
In the reanalysis, the investigators defined 22 out of the trial’s 110 participants as high risk based on their score of 8 or higher on the Leiden prediction rule at baseline. Of those 22, 18 also fulfilled the 2010 classification criteria for RA.
This “definition of high risk [in the trial] very much coincided with the new classification criteria and reinforces the standard of care that patients with new diagnosed RA should be treated with DMARDs [disease-modifying antirheumatic drugs] front line,” Dr. Sparks said.
The Leiden prediction rule score is based on ACPA statuses, as well as age, sex, distribution of involved joints, number of swollen and tender joints, severity of morning stiffness, C-reactive protein level, and rheumatoid factor. In previous studies of patients with undifferentiated arthritis, a score of 8 or higher with the prediction rule had a positive predictive value of 84% in patients with undifferentiated arthritis, according to the investigators.
Based on a primary outcome of fulfilling the 1987 classification criteria for RA after 5 years of follow-up, the investigators found that 6 of 11 (55%) in the methotrexate arm developed RA, compared with all 11 patients in the placebo arm (P = .011). “A 1-year course of methotrexate was associated with an absolute risk reduction of 45% on RA development, resulting in a number needed to treat of 2.2 (95% [confidence interval], 1.3-6.2),” the authors wrote.
Furthermore, the time to the development of RA based on the 1987 criteria was longer with methotrexate than with placebo (median of 22.5 months vs. 3 months; P less than .001).
Drug-free remission was also achieved by 4 of 11 (36%) patients taking methotrexate, compared with none of the patients taking placebo (P = .027).
The beneficial effects of methotrexate were seen in ACPA-positive and ACPA-negative high-risk patients but not in patients without a high risk of RA.
For the patients who did not fulfill the 2010 RA criteria at baseline, only one of four of those in the placebo arm did go on to develop RA based on 1987 criteria, whereas only one of three who received methotrexate did.
Overall, the reanalysis of PROMPT trial data illustrates how “noninformative inclusions can blur highly relevant study outcomes, such as prevention of RA,” the study authors concluded.
“As trials are now being conducted to evaluate the efficacy of treatment initiated in the phase of arthralgia, the development of adequate risk prediction models are of importance in order to prevent false-negative study results in the future,” they added.
The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
Small numbers not withstanding, the findings of this reanalysis of the PROMPT trial are exciting, and they address the importance of identifying the right individuals to include in any type of prevention study in RA.
Given the temporal limits of clinical trials, inclusion criteria will need to incorporate both the likelihood of an important outcome and the timing of that outcome – right individuals, right time, right drug/intervention.
It is hoped that investigators will be able to demonstrate conclusively that preventive interventions work for rheumatic disease once these issues are addressed.
Kevin D. Deane, MD, PhD, and his coauthors are with the division of rheumatology at the University of Colorado, Denver, and made these remarks in an editorial accompanying the PROMPT trial reanalysis (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40061).
Small numbers not withstanding, the findings of this reanalysis of the PROMPT trial are exciting, and they address the importance of identifying the right individuals to include in any type of prevention study in RA.
Given the temporal limits of clinical trials, inclusion criteria will need to incorporate both the likelihood of an important outcome and the timing of that outcome – right individuals, right time, right drug/intervention.
It is hoped that investigators will be able to demonstrate conclusively that preventive interventions work for rheumatic disease once these issues are addressed.
Kevin D. Deane, MD, PhD, and his coauthors are with the division of rheumatology at the University of Colorado, Denver, and made these remarks in an editorial accompanying the PROMPT trial reanalysis (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40061).
Small numbers not withstanding, the findings of this reanalysis of the PROMPT trial are exciting, and they address the importance of identifying the right individuals to include in any type of prevention study in RA.
Given the temporal limits of clinical trials, inclusion criteria will need to incorporate both the likelihood of an important outcome and the timing of that outcome – right individuals, right time, right drug/intervention.
It is hoped that investigators will be able to demonstrate conclusively that preventive interventions work for rheumatic disease once these issues are addressed.
Kevin D. Deane, MD, PhD, and his coauthors are with the division of rheumatology at the University of Colorado, Denver, and made these remarks in an editorial accompanying the PROMPT trial reanalysis (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40061).
Efforts to delay or prevent rheumatoid arthritis (RA) in individuals at high risk for the disease received a boost from the findings of a subgroup analysis of an older Dutch prevention trial involving methotrexate that were published recently in Arthritis & Rheumatology.
However, while the 22-patient subgroup analysis of the 2007 trial, called PROMPT (Probable RA: Methotrexate Versus Placebo Treatment), showed that 1 year of methotrexate prevented the development of rheumatoid arthritis in significantly more individuals at high risk for the disease than did placebo, hindsight has shown that most of these high-risk individuals actually had RA at baseline as defined by the 2010 American College or Rheumatology/European League Against Rheumatism classification criteria.
Even though the “landscape of RA has changed since this study was conceived, enrolled, and performed,” Dr. Sparks noted that the study provides evidence that today’s “standard of care really works” by making use of data that are unobtainable today.
“Nowadays, we wouldn’t be able to do a placebo-controlled trial in early RA because those patients need to be treated, but at the time, it was perfectly fine, based on the treatment landscape, to put these patients in a [placebo-controlled] trial,” he said in an interview.
“It also demonstrates that you really need to find high-risk individuals, because, if you recruit people who are never going to develop RA, you’re just diluting your effect, and you’re not going to find the difference in the groups based on that diluted effect when there could be a true effect in that special subgroup,” he added.
Senior study author Annette van der Helm-van Mil, MD, PhD, and her colleagues at Leiden (the Netherlands) University Medical Center performed the reanalysis after the initial finding that methotrexate had no preventative effect may have been falsely negative because the study included patients with a low risk of progressing to RA (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40062).
In the reanalysis, the investigators defined 22 out of the trial’s 110 participants as high risk based on their score of 8 or higher on the Leiden prediction rule at baseline. Of those 22, 18 also fulfilled the 2010 classification criteria for RA.
This “definition of high risk [in the trial] very much coincided with the new classification criteria and reinforces the standard of care that patients with new diagnosed RA should be treated with DMARDs [disease-modifying antirheumatic drugs] front line,” Dr. Sparks said.
The Leiden prediction rule score is based on ACPA statuses, as well as age, sex, distribution of involved joints, number of swollen and tender joints, severity of morning stiffness, C-reactive protein level, and rheumatoid factor. In previous studies of patients with undifferentiated arthritis, a score of 8 or higher with the prediction rule had a positive predictive value of 84% in patients with undifferentiated arthritis, according to the investigators.
Based on a primary outcome of fulfilling the 1987 classification criteria for RA after 5 years of follow-up, the investigators found that 6 of 11 (55%) in the methotrexate arm developed RA, compared with all 11 patients in the placebo arm (P = .011). “A 1-year course of methotrexate was associated with an absolute risk reduction of 45% on RA development, resulting in a number needed to treat of 2.2 (95% [confidence interval], 1.3-6.2),” the authors wrote.
Furthermore, the time to the development of RA based on the 1987 criteria was longer with methotrexate than with placebo (median of 22.5 months vs. 3 months; P less than .001).
Drug-free remission was also achieved by 4 of 11 (36%) patients taking methotrexate, compared with none of the patients taking placebo (P = .027).
The beneficial effects of methotrexate were seen in ACPA-positive and ACPA-negative high-risk patients but not in patients without a high risk of RA.
For the patients who did not fulfill the 2010 RA criteria at baseline, only one of four of those in the placebo arm did go on to develop RA based on 1987 criteria, whereas only one of three who received methotrexate did.
Overall, the reanalysis of PROMPT trial data illustrates how “noninformative inclusions can blur highly relevant study outcomes, such as prevention of RA,” the study authors concluded.
“As trials are now being conducted to evaluate the efficacy of treatment initiated in the phase of arthralgia, the development of adequate risk prediction models are of importance in order to prevent false-negative study results in the future,” they added.
The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
Efforts to delay or prevent rheumatoid arthritis (RA) in individuals at high risk for the disease received a boost from the findings of a subgroup analysis of an older Dutch prevention trial involving methotrexate that were published recently in Arthritis & Rheumatology.
However, while the 22-patient subgroup analysis of the 2007 trial, called PROMPT (Probable RA: Methotrexate Versus Placebo Treatment), showed that 1 year of methotrexate prevented the development of rheumatoid arthritis in significantly more individuals at high risk for the disease than did placebo, hindsight has shown that most of these high-risk individuals actually had RA at baseline as defined by the 2010 American College or Rheumatology/European League Against Rheumatism classification criteria.
Even though the “landscape of RA has changed since this study was conceived, enrolled, and performed,” Dr. Sparks noted that the study provides evidence that today’s “standard of care really works” by making use of data that are unobtainable today.
“Nowadays, we wouldn’t be able to do a placebo-controlled trial in early RA because those patients need to be treated, but at the time, it was perfectly fine, based on the treatment landscape, to put these patients in a [placebo-controlled] trial,” he said in an interview.
“It also demonstrates that you really need to find high-risk individuals, because, if you recruit people who are never going to develop RA, you’re just diluting your effect, and you’re not going to find the difference in the groups based on that diluted effect when there could be a true effect in that special subgroup,” he added.
Senior study author Annette van der Helm-van Mil, MD, PhD, and her colleagues at Leiden (the Netherlands) University Medical Center performed the reanalysis after the initial finding that methotrexate had no preventative effect may have been falsely negative because the study included patients with a low risk of progressing to RA (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40062).
In the reanalysis, the investigators defined 22 out of the trial’s 110 participants as high risk based on their score of 8 or higher on the Leiden prediction rule at baseline. Of those 22, 18 also fulfilled the 2010 classification criteria for RA.
This “definition of high risk [in the trial] very much coincided with the new classification criteria and reinforces the standard of care that patients with new diagnosed RA should be treated with DMARDs [disease-modifying antirheumatic drugs] front line,” Dr. Sparks said.
The Leiden prediction rule score is based on ACPA statuses, as well as age, sex, distribution of involved joints, number of swollen and tender joints, severity of morning stiffness, C-reactive protein level, and rheumatoid factor. In previous studies of patients with undifferentiated arthritis, a score of 8 or higher with the prediction rule had a positive predictive value of 84% in patients with undifferentiated arthritis, according to the investigators.
Based on a primary outcome of fulfilling the 1987 classification criteria for RA after 5 years of follow-up, the investigators found that 6 of 11 (55%) in the methotrexate arm developed RA, compared with all 11 patients in the placebo arm (P = .011). “A 1-year course of methotrexate was associated with an absolute risk reduction of 45% on RA development, resulting in a number needed to treat of 2.2 (95% [confidence interval], 1.3-6.2),” the authors wrote.
Furthermore, the time to the development of RA based on the 1987 criteria was longer with methotrexate than with placebo (median of 22.5 months vs. 3 months; P less than .001).
Drug-free remission was also achieved by 4 of 11 (36%) patients taking methotrexate, compared with none of the patients taking placebo (P = .027).
The beneficial effects of methotrexate were seen in ACPA-positive and ACPA-negative high-risk patients but not in patients without a high risk of RA.
For the patients who did not fulfill the 2010 RA criteria at baseline, only one of four of those in the placebo arm did go on to develop RA based on 1987 criteria, whereas only one of three who received methotrexate did.
Overall, the reanalysis of PROMPT trial data illustrates how “noninformative inclusions can blur highly relevant study outcomes, such as prevention of RA,” the study authors concluded.
“As trials are now being conducted to evaluate the efficacy of treatment initiated in the phase of arthralgia, the development of adequate risk prediction models are of importance in order to prevent false-negative study results in the future,” they added.
The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Main finding: In people deemed to be at high risk for RA, a 1-year course of methotrexate was associated with an absolute risk reduction of 45% of RA development, resulting in a number needed to treat of 2.2 (95% CI, 1.3-6.2).
Data source: A reanalysis of the PROMPT trial involving 110 patients with undifferentiated arthritis randomized to a 1-year course of methotrexate or placebo.
Disclosures: The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
Opinions vary considerably on withdrawing drugs in clinically inactive JIA
A wide range of attitudes and practices for the process of withdrawing medications in pediatric patients with clinically inactive juvenile idiopathic arthritis (JIA) exist among clinician members of the Childhood Arthritis and Rheumatology Research Alliance (CARRA), according to findings from an anonymous survey.
The cross-sectional, electronic survey found that respondents varied in the amount of time they thought was necessary to spend in clinically inactive disease before beginning withdrawal of medications and in the amount of time to spend during tapering or stopping medications, for both methotrexate and biologics.
To better understand how clinicians care for patients with clinically inactive disease, the investigators emailed the survey to 388 clinician members of the CARRA in the United States and Canada over a 4-week period during November-December 2015 (J Rheumatol. 2017 Feb 1. doi: 10.3899/jrheum.161078).
The survey, which the investigators thought to be “the first comprehensive evaluation of influential factors and approaches for the clinical management of children with clinically inactive JIA,” did not include questions about systemic JIA, inflammatory bowel disease, psoriasis, and uveitis in order “to simplify responses and encourage participation, because in practice, the manifestations and outcomes of these diseases could substantially influence treatment decisions for children with JIA.”
They received complete responses from 124 of the 132 clinicians who responded to the survey email. Of the 121 respondents who reported taking clinical care of patients with JIA, 87% were physicians, and the same number reported taking care of pediatric patients only. About three-quarters spent half of their professional time in clinical care, and about half had more than 10 years of post-training clinical experience.
When deciding about withdrawing JIA medications, more than one-half of respondents said that the time that a patient spent in clinically inactive disease and a history of drug toxicity are very important factors. Most participants ranked those two factors most highly and most often among their top five factors for decision making.
Respondents also commonly ranked these factors as important:
- JIA duration before attaining clinically inactive disease.
- Patient/family preferences.
- Presence of JIA-related damage.
- JIA category.
The factors that consistently appeared in responses fit into three clusters that included JIA features and time spent in clinically inactive disease (JIA category and total disease duration), JIA severity and resistance to treatment (disease duration before clinically inactive disease, number of drugs needed to attain inactivity, joint damage, and a history of sacroiliac or temporomandibular disease), and the patient’s experience (drug toxicity and family preference).
The respondents indicated that they would be least likely to stop medications for children with rheumatoid factor (RF)–positive polyarthritis (85%), which is “consistent with prior studies showing that RF-positive polyarthritis is associated with higher rates of flares than other JIA categories,” the investigators wrote. However, respondents said they would be most likely to stop medications for children with persistent oligoarthritis (87%) “even though rates of flares in this category appear similar to other JIA types. This method may reflect a belief that flares in children with persistent oligoarticular JIA will be less severe and easier to control.”
When patients met all criteria for clinically inactive disease for a “sufficient amount of time” and families were interested in stopping medications, some factors continued to make respondents reluctant to withdraw medications. These factors were most often a history of erosions (81%), asymptomatic joint abnormalities on ultrasound or MRI (72%), and failure of multiple prior disease-modifying antirheumatic drugs or biologics to control disease (64%). The definition of clinically inactive disease is a composite of no active arthritis, uveitis, or systemic JIA symptoms; the best possible clinical global assessment; inflammatory markers normal or elevated for reasons other than JIA; and no more than 15 minutes of joint stiffness.
A little over half of respondents said they would wait until clinically inactive disease had lasted 12 months before considering stopping or tapering methotrexate or biologic monotherapy, but a substantial minority said they would wait for only 6 months for methotrexate (31%) or biologic monotherapy (23%). A smaller number would wait for 18 months for methotrexate (13%) or biologics (18%), and another 3%-5% said they could not give a time frame.
The strategies varied for how actual withdrawing of medications occurred. Most methotrexate monotherapy withdrawals involved tapering over 2-6 months, one-third over longer periods, and the fewest reported tapering for less than 2 months (7%) or immediate withdrawal (17%).
Withdrawal of biologics was generally said to occur more gradually than with methotrexate, with one-third of respondents citing over 2-6 months, a quarter more slowly, and another 29% in less than 2 months or immediately. Some wrote that they preferred spacing out the interval between doses, but none decreased the dose. When children took combination therapy with methotrexate plus a biologic, 63% said that they began tapering or stopping methotrexate first, but a quarter said that the order was strongly context dependent, and the most commonly cited reason for deciding was history of toxicity or intolerance.
Imaging played a role in less than half of the decisions to withdraw medications, with it being used often by 9% and sometimes by 36%. And while it’s assumed that patients and family consideration played an important role in decision making, only 25% of respondents reported using specific patient-reported outcomes in deciding to withdraw medications.
The study was funded by grants from Rutgers Biomedical and Health Sciences and the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
A wide range of attitudes and practices for the process of withdrawing medications in pediatric patients with clinically inactive juvenile idiopathic arthritis (JIA) exist among clinician members of the Childhood Arthritis and Rheumatology Research Alliance (CARRA), according to findings from an anonymous survey.
The cross-sectional, electronic survey found that respondents varied in the amount of time they thought was necessary to spend in clinically inactive disease before beginning withdrawal of medications and in the amount of time to spend during tapering or stopping medications, for both methotrexate and biologics.
To better understand how clinicians care for patients with clinically inactive disease, the investigators emailed the survey to 388 clinician members of the CARRA in the United States and Canada over a 4-week period during November-December 2015 (J Rheumatol. 2017 Feb 1. doi: 10.3899/jrheum.161078).
The survey, which the investigators thought to be “the first comprehensive evaluation of influential factors and approaches for the clinical management of children with clinically inactive JIA,” did not include questions about systemic JIA, inflammatory bowel disease, psoriasis, and uveitis in order “to simplify responses and encourage participation, because in practice, the manifestations and outcomes of these diseases could substantially influence treatment decisions for children with JIA.”
They received complete responses from 124 of the 132 clinicians who responded to the survey email. Of the 121 respondents who reported taking clinical care of patients with JIA, 87% were physicians, and the same number reported taking care of pediatric patients only. About three-quarters spent half of their professional time in clinical care, and about half had more than 10 years of post-training clinical experience.
When deciding about withdrawing JIA medications, more than one-half of respondents said that the time that a patient spent in clinically inactive disease and a history of drug toxicity are very important factors. Most participants ranked those two factors most highly and most often among their top five factors for decision making.
Respondents also commonly ranked these factors as important:
- JIA duration before attaining clinically inactive disease.
- Patient/family preferences.
- Presence of JIA-related damage.
- JIA category.
The factors that consistently appeared in responses fit into three clusters that included JIA features and time spent in clinically inactive disease (JIA category and total disease duration), JIA severity and resistance to treatment (disease duration before clinically inactive disease, number of drugs needed to attain inactivity, joint damage, and a history of sacroiliac or temporomandibular disease), and the patient’s experience (drug toxicity and family preference).
The respondents indicated that they would be least likely to stop medications for children with rheumatoid factor (RF)–positive polyarthritis (85%), which is “consistent with prior studies showing that RF-positive polyarthritis is associated with higher rates of flares than other JIA categories,” the investigators wrote. However, respondents said they would be most likely to stop medications for children with persistent oligoarthritis (87%) “even though rates of flares in this category appear similar to other JIA types. This method may reflect a belief that flares in children with persistent oligoarticular JIA will be less severe and easier to control.”
When patients met all criteria for clinically inactive disease for a “sufficient amount of time” and families were interested in stopping medications, some factors continued to make respondents reluctant to withdraw medications. These factors were most often a history of erosions (81%), asymptomatic joint abnormalities on ultrasound or MRI (72%), and failure of multiple prior disease-modifying antirheumatic drugs or biologics to control disease (64%). The definition of clinically inactive disease is a composite of no active arthritis, uveitis, or systemic JIA symptoms; the best possible clinical global assessment; inflammatory markers normal or elevated for reasons other than JIA; and no more than 15 minutes of joint stiffness.
A little over half of respondents said they would wait until clinically inactive disease had lasted 12 months before considering stopping or tapering methotrexate or biologic monotherapy, but a substantial minority said they would wait for only 6 months for methotrexate (31%) or biologic monotherapy (23%). A smaller number would wait for 18 months for methotrexate (13%) or biologics (18%), and another 3%-5% said they could not give a time frame.
The strategies varied for how actual withdrawing of medications occurred. Most methotrexate monotherapy withdrawals involved tapering over 2-6 months, one-third over longer periods, and the fewest reported tapering for less than 2 months (7%) or immediate withdrawal (17%).
Withdrawal of biologics was generally said to occur more gradually than with methotrexate, with one-third of respondents citing over 2-6 months, a quarter more slowly, and another 29% in less than 2 months or immediately. Some wrote that they preferred spacing out the interval between doses, but none decreased the dose. When children took combination therapy with methotrexate plus a biologic, 63% said that they began tapering or stopping methotrexate first, but a quarter said that the order was strongly context dependent, and the most commonly cited reason for deciding was history of toxicity or intolerance.
Imaging played a role in less than half of the decisions to withdraw medications, with it being used often by 9% and sometimes by 36%. And while it’s assumed that patients and family consideration played an important role in decision making, only 25% of respondents reported using specific patient-reported outcomes in deciding to withdraw medications.
The study was funded by grants from Rutgers Biomedical and Health Sciences and the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
A wide range of attitudes and practices for the process of withdrawing medications in pediatric patients with clinically inactive juvenile idiopathic arthritis (JIA) exist among clinician members of the Childhood Arthritis and Rheumatology Research Alliance (CARRA), according to findings from an anonymous survey.
The cross-sectional, electronic survey found that respondents varied in the amount of time they thought was necessary to spend in clinically inactive disease before beginning withdrawal of medications and in the amount of time to spend during tapering or stopping medications, for both methotrexate and biologics.
To better understand how clinicians care for patients with clinically inactive disease, the investigators emailed the survey to 388 clinician members of the CARRA in the United States and Canada over a 4-week period during November-December 2015 (J Rheumatol. 2017 Feb 1. doi: 10.3899/jrheum.161078).
The survey, which the investigators thought to be “the first comprehensive evaluation of influential factors and approaches for the clinical management of children with clinically inactive JIA,” did not include questions about systemic JIA, inflammatory bowel disease, psoriasis, and uveitis in order “to simplify responses and encourage participation, because in practice, the manifestations and outcomes of these diseases could substantially influence treatment decisions for children with JIA.”
They received complete responses from 124 of the 132 clinicians who responded to the survey email. Of the 121 respondents who reported taking clinical care of patients with JIA, 87% were physicians, and the same number reported taking care of pediatric patients only. About three-quarters spent half of their professional time in clinical care, and about half had more than 10 years of post-training clinical experience.
When deciding about withdrawing JIA medications, more than one-half of respondents said that the time that a patient spent in clinically inactive disease and a history of drug toxicity are very important factors. Most participants ranked those two factors most highly and most often among their top five factors for decision making.
Respondents also commonly ranked these factors as important:
- JIA duration before attaining clinically inactive disease.
- Patient/family preferences.
- Presence of JIA-related damage.
- JIA category.
The factors that consistently appeared in responses fit into three clusters that included JIA features and time spent in clinically inactive disease (JIA category and total disease duration), JIA severity and resistance to treatment (disease duration before clinically inactive disease, number of drugs needed to attain inactivity, joint damage, and a history of sacroiliac or temporomandibular disease), and the patient’s experience (drug toxicity and family preference).
The respondents indicated that they would be least likely to stop medications for children with rheumatoid factor (RF)–positive polyarthritis (85%), which is “consistent with prior studies showing that RF-positive polyarthritis is associated with higher rates of flares than other JIA categories,” the investigators wrote. However, respondents said they would be most likely to stop medications for children with persistent oligoarthritis (87%) “even though rates of flares in this category appear similar to other JIA types. This method may reflect a belief that flares in children with persistent oligoarticular JIA will be less severe and easier to control.”
When patients met all criteria for clinically inactive disease for a “sufficient amount of time” and families were interested in stopping medications, some factors continued to make respondents reluctant to withdraw medications. These factors were most often a history of erosions (81%), asymptomatic joint abnormalities on ultrasound or MRI (72%), and failure of multiple prior disease-modifying antirheumatic drugs or biologics to control disease (64%). The definition of clinically inactive disease is a composite of no active arthritis, uveitis, or systemic JIA symptoms; the best possible clinical global assessment; inflammatory markers normal or elevated for reasons other than JIA; and no more than 15 minutes of joint stiffness.
A little over half of respondents said they would wait until clinically inactive disease had lasted 12 months before considering stopping or tapering methotrexate or biologic monotherapy, but a substantial minority said they would wait for only 6 months for methotrexate (31%) or biologic monotherapy (23%). A smaller number would wait for 18 months for methotrexate (13%) or biologics (18%), and another 3%-5% said they could not give a time frame.
The strategies varied for how actual withdrawing of medications occurred. Most methotrexate monotherapy withdrawals involved tapering over 2-6 months, one-third over longer periods, and the fewest reported tapering for less than 2 months (7%) or immediate withdrawal (17%).
Withdrawal of biologics was generally said to occur more gradually than with methotrexate, with one-third of respondents citing over 2-6 months, a quarter more slowly, and another 29% in less than 2 months or immediately. Some wrote that they preferred spacing out the interval between doses, but none decreased the dose. When children took combination therapy with methotrexate plus a biologic, 63% said that they began tapering or stopping methotrexate first, but a quarter said that the order was strongly context dependent, and the most commonly cited reason for deciding was history of toxicity or intolerance.
Imaging played a role in less than half of the decisions to withdraw medications, with it being used often by 9% and sometimes by 36%. And while it’s assumed that patients and family consideration played an important role in decision making, only 25% of respondents reported using specific patient-reported outcomes in deciding to withdraw medications.
The study was funded by grants from Rutgers Biomedical and Health Sciences and the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Key clinical point:
Major finding: A little over half of respondents said they would wait until clinically inactive disease had lasted 12 months before considering stopping or tapering methotrexate or biologic monotherapy.
Data source: A survey of 121 of 388 CARRA members involved in clinical care of JIA patients.
Disclosures: The study was funded by grants from Rutgers Biomedical and Health Sciences and the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Lyme arthritis changes its immune response profile if it persists after antibiotics
The persistence of Lyme arthritis after treatment with antibiotics comes with a shift from an immune response expected for bacterial infection to one characterized by chronic inflammation, synovial proliferation, and breakdown of wound repair processes, according to an analysis of microRNA expression in patients before, during, and after infection.
Based on the findings, investigators led by Robert B. Lochhead, PhD, of Massachusetts General Hospital, Boston, said that they “suspect that, in humans, genetic variables determine whether the response to B. burgdorferi infection elicits an appropriate wound repair response … or a maladaptive inflammatory cellular response and arrest of wound repair processes.”
The investigators studied synovial fluid or tissue from 32 patients with LA who were representative of the spectrum of disease severity and treatment responses seen in this disease. In 18 patients for whom synovial fluid samples were available, 5 illustrated the differences in miRNA expression that occur from the time before any antibiotic treatment to the time after antibiotic treatment that successfully resolves arthritis symptoms, and 13 showed how an incomplete response to antibiotic treatment can affect miRNA expression. The expression profile of miRNA in synovial tissue samples from another 14 patients who underwent arthroscopic synovectomies 4-48 months after oral and intravenous antibiotics demonstrated the change in immune response seen in postinfectious LA.
The group of five patients with synovial fluid samples who were referred prior to antibiotic therapy when they had active B. burgdorferi infection (group 1) had a history of mild to severe knee swelling and pain for a median duration of 1 month prior to evaluation and the start of antibiotic treatment. A 1-month course of oral doxycycline resolved arthritis in three of the patients, and the other two continued to have marked knee swelling that later resolved after 1 month of IV ceftriaxone. Of six different miRNAs that the investigators measured, five were at low levels in these patients. The lone exception was a hematopoietic-specific miRNA, miR-223, which is abundantly expressed in polymorphonuclear lymphocytes (PMNs) and is associated with downregulation of acute inflammation and tissue remodeling.
In the group of 13 who still had joint swelling despite oral or IV antibiotics (group 2), only 2 had resolution of their swelling after IV antibiotics. Most of the remaining 11 had successful treatment with methotrexate. The synovial fluid samples for seven patients were collected after oral antibiotics but before IV antibiotics, and in the other six the samples were collected after both therapies. These 13 patients had significantly lower white blood cell counts in synovial fluid, fewer PMNs, and greater percentages of lymphocytes and monocytes than did group 1 patients. The five miRNAs that were found at low levels among the patients in group 1 were higher in these patients, which “suggested that the nature of the arthritis had changed after spirochetal killing.” The higher miR-223 levels seen in group 1 also occurred in group 2.
A separate analysis of synovial fluid samples from four patients with osteoarthritis and six patients with RA showed that levels of the six miRNAs from RA patients were similar to those of patients from group 2, and the low levels that were observed for most of the miRNAs in group 1 were similar to those seen in OA patients.
The investigators found that the five miRNAs with elevated levels in group 2 patients, but not miR-223, were positively correlated with arthritis duration after start of oral antibiotic therapy. B. burgdorferi IgG antibody titers negatively correlated with some of the elevated miRNAs in group 2.
The investigators analyzed a larger set of miRNAs in the synovial tissue samples obtained from 14 patients who underwent synovectomies for treatment of persistent synovitis a median of 15.5 months after they had undergone 2-3 months of antibiotic therapy (group 3). Some of the miRNAs overexpressed in these postinfectious LA samples, relative to samples from five OA patients, were associated with proliferative, tumor-associated responses and regulation of inflammatory processes. However, miRNAs overexpressed in tissues from OA patients relative to postinfectious LA patients were thought to affect genes that control tissue remodeling and cell proliferation, but not inflammation. The “distinct oncogenic miRNA profile” exhibited by postinfectious synovial tissue, according to the investigators, showed that “in these patients, the transition to the postinfectious phase was blocked by chronic inflammation, which stalled the wound repair process.”
The investigators concluded that “miRNAs hold promise as potential biomarkers to identify LA patients who are developing maladaptive immune responses during the period of infection. In such patients, it will be important to learn whether simultaneous treatment with antibiotics and DMARDs, rather than sequential treatment with these medications, will reduce the period of therapy and improve outcome, creating a new paradigm in treatment of this form of chronic inflammatory arthritis.”
The study was supported by grants from the National Institutes of Health, the Lucius N. Littauer Foundation, the Roland Foundation, the Lyme Disease and Arthritis Research Fund at Massachusetts General Hospital, the Rheumatology Research Foundation, and the English, Bonter, Mitchell Foundation.
The persistence of Lyme arthritis after treatment with antibiotics comes with a shift from an immune response expected for bacterial infection to one characterized by chronic inflammation, synovial proliferation, and breakdown of wound repair processes, according to an analysis of microRNA expression in patients before, during, and after infection.
Based on the findings, investigators led by Robert B. Lochhead, PhD, of Massachusetts General Hospital, Boston, said that they “suspect that, in humans, genetic variables determine whether the response to B. burgdorferi infection elicits an appropriate wound repair response … or a maladaptive inflammatory cellular response and arrest of wound repair processes.”
The investigators studied synovial fluid or tissue from 32 patients with LA who were representative of the spectrum of disease severity and treatment responses seen in this disease. In 18 patients for whom synovial fluid samples were available, 5 illustrated the differences in miRNA expression that occur from the time before any antibiotic treatment to the time after antibiotic treatment that successfully resolves arthritis symptoms, and 13 showed how an incomplete response to antibiotic treatment can affect miRNA expression. The expression profile of miRNA in synovial tissue samples from another 14 patients who underwent arthroscopic synovectomies 4-48 months after oral and intravenous antibiotics demonstrated the change in immune response seen in postinfectious LA.
The group of five patients with synovial fluid samples who were referred prior to antibiotic therapy when they had active B. burgdorferi infection (group 1) had a history of mild to severe knee swelling and pain for a median duration of 1 month prior to evaluation and the start of antibiotic treatment. A 1-month course of oral doxycycline resolved arthritis in three of the patients, and the other two continued to have marked knee swelling that later resolved after 1 month of IV ceftriaxone. Of six different miRNAs that the investigators measured, five were at low levels in these patients. The lone exception was a hematopoietic-specific miRNA, miR-223, which is abundantly expressed in polymorphonuclear lymphocytes (PMNs) and is associated with downregulation of acute inflammation and tissue remodeling.
In the group of 13 who still had joint swelling despite oral or IV antibiotics (group 2), only 2 had resolution of their swelling after IV antibiotics. Most of the remaining 11 had successful treatment with methotrexate. The synovial fluid samples for seven patients were collected after oral antibiotics but before IV antibiotics, and in the other six the samples were collected after both therapies. These 13 patients had significantly lower white blood cell counts in synovial fluid, fewer PMNs, and greater percentages of lymphocytes and monocytes than did group 1 patients. The five miRNAs that were found at low levels among the patients in group 1 were higher in these patients, which “suggested that the nature of the arthritis had changed after spirochetal killing.” The higher miR-223 levels seen in group 1 also occurred in group 2.
A separate analysis of synovial fluid samples from four patients with osteoarthritis and six patients with RA showed that levels of the six miRNAs from RA patients were similar to those of patients from group 2, and the low levels that were observed for most of the miRNAs in group 1 were similar to those seen in OA patients.
The investigators found that the five miRNAs with elevated levels in group 2 patients, but not miR-223, were positively correlated with arthritis duration after start of oral antibiotic therapy. B. burgdorferi IgG antibody titers negatively correlated with some of the elevated miRNAs in group 2.
The investigators analyzed a larger set of miRNAs in the synovial tissue samples obtained from 14 patients who underwent synovectomies for treatment of persistent synovitis a median of 15.5 months after they had undergone 2-3 months of antibiotic therapy (group 3). Some of the miRNAs overexpressed in these postinfectious LA samples, relative to samples from five OA patients, were associated with proliferative, tumor-associated responses and regulation of inflammatory processes. However, miRNAs overexpressed in tissues from OA patients relative to postinfectious LA patients were thought to affect genes that control tissue remodeling and cell proliferation, but not inflammation. The “distinct oncogenic miRNA profile” exhibited by postinfectious synovial tissue, according to the investigators, showed that “in these patients, the transition to the postinfectious phase was blocked by chronic inflammation, which stalled the wound repair process.”
The investigators concluded that “miRNAs hold promise as potential biomarkers to identify LA patients who are developing maladaptive immune responses during the period of infection. In such patients, it will be important to learn whether simultaneous treatment with antibiotics and DMARDs, rather than sequential treatment with these medications, will reduce the period of therapy and improve outcome, creating a new paradigm in treatment of this form of chronic inflammatory arthritis.”
The study was supported by grants from the National Institutes of Health, the Lucius N. Littauer Foundation, the Roland Foundation, the Lyme Disease and Arthritis Research Fund at Massachusetts General Hospital, the Rheumatology Research Foundation, and the English, Bonter, Mitchell Foundation.
The persistence of Lyme arthritis after treatment with antibiotics comes with a shift from an immune response expected for bacterial infection to one characterized by chronic inflammation, synovial proliferation, and breakdown of wound repair processes, according to an analysis of microRNA expression in patients before, during, and after infection.
Based on the findings, investigators led by Robert B. Lochhead, PhD, of Massachusetts General Hospital, Boston, said that they “suspect that, in humans, genetic variables determine whether the response to B. burgdorferi infection elicits an appropriate wound repair response … or a maladaptive inflammatory cellular response and arrest of wound repair processes.”
The investigators studied synovial fluid or tissue from 32 patients with LA who were representative of the spectrum of disease severity and treatment responses seen in this disease. In 18 patients for whom synovial fluid samples were available, 5 illustrated the differences in miRNA expression that occur from the time before any antibiotic treatment to the time after antibiotic treatment that successfully resolves arthritis symptoms, and 13 showed how an incomplete response to antibiotic treatment can affect miRNA expression. The expression profile of miRNA in synovial tissue samples from another 14 patients who underwent arthroscopic synovectomies 4-48 months after oral and intravenous antibiotics demonstrated the change in immune response seen in postinfectious LA.
The group of five patients with synovial fluid samples who were referred prior to antibiotic therapy when they had active B. burgdorferi infection (group 1) had a history of mild to severe knee swelling and pain for a median duration of 1 month prior to evaluation and the start of antibiotic treatment. A 1-month course of oral doxycycline resolved arthritis in three of the patients, and the other two continued to have marked knee swelling that later resolved after 1 month of IV ceftriaxone. Of six different miRNAs that the investigators measured, five were at low levels in these patients. The lone exception was a hematopoietic-specific miRNA, miR-223, which is abundantly expressed in polymorphonuclear lymphocytes (PMNs) and is associated with downregulation of acute inflammation and tissue remodeling.
In the group of 13 who still had joint swelling despite oral or IV antibiotics (group 2), only 2 had resolution of their swelling after IV antibiotics. Most of the remaining 11 had successful treatment with methotrexate. The synovial fluid samples for seven patients were collected after oral antibiotics but before IV antibiotics, and in the other six the samples were collected after both therapies. These 13 patients had significantly lower white blood cell counts in synovial fluid, fewer PMNs, and greater percentages of lymphocytes and monocytes than did group 1 patients. The five miRNAs that were found at low levels among the patients in group 1 were higher in these patients, which “suggested that the nature of the arthritis had changed after spirochetal killing.” The higher miR-223 levels seen in group 1 also occurred in group 2.
A separate analysis of synovial fluid samples from four patients with osteoarthritis and six patients with RA showed that levels of the six miRNAs from RA patients were similar to those of patients from group 2, and the low levels that were observed for most of the miRNAs in group 1 were similar to those seen in OA patients.
The investigators found that the five miRNAs with elevated levels in group 2 patients, but not miR-223, were positively correlated with arthritis duration after start of oral antibiotic therapy. B. burgdorferi IgG antibody titers negatively correlated with some of the elevated miRNAs in group 2.
The investigators analyzed a larger set of miRNAs in the synovial tissue samples obtained from 14 patients who underwent synovectomies for treatment of persistent synovitis a median of 15.5 months after they had undergone 2-3 months of antibiotic therapy (group 3). Some of the miRNAs overexpressed in these postinfectious LA samples, relative to samples from five OA patients, were associated with proliferative, tumor-associated responses and regulation of inflammatory processes. However, miRNAs overexpressed in tissues from OA patients relative to postinfectious LA patients were thought to affect genes that control tissue remodeling and cell proliferation, but not inflammation. The “distinct oncogenic miRNA profile” exhibited by postinfectious synovial tissue, according to the investigators, showed that “in these patients, the transition to the postinfectious phase was blocked by chronic inflammation, which stalled the wound repair process.”
The investigators concluded that “miRNAs hold promise as potential biomarkers to identify LA patients who are developing maladaptive immune responses during the period of infection. In such patients, it will be important to learn whether simultaneous treatment with antibiotics and DMARDs, rather than sequential treatment with these medications, will reduce the period of therapy and improve outcome, creating a new paradigm in treatment of this form of chronic inflammatory arthritis.”
The study was supported by grants from the National Institutes of Health, the Lucius N. Littauer Foundation, the Roland Foundation, the Lyme Disease and Arthritis Research Fund at Massachusetts General Hospital, the Rheumatology Research Foundation, and the English, Bonter, Mitchell Foundation.
Key clinical point:
Major finding: miRNAs overexpressed in synovial tissue samples from 14 patients with postinfectious Lyme arthritis, relative to samples from five OA patients, were associated with proliferative, tumor-associated responses and regulation of inflammatory processes.
Data source: A retrospective study of synovial fluid or tissue samples from 32 patients with Lyme arthritis.
Disclosures: The study was supported by grants from the National Institutes of Health, the Lucius N. Littauer Foundation, the Roland Foundation, the Lyme Disease and Arthritis Research Fund at Massachusetts General Hospital, the Rheumatology Research Foundation, and the English, Bonter, Mitchell Foundation.
New histopathologic marker may aid dermatomyositis diagnosis
The detection of sarcoplasmic myxovirus resistance A expression in immunohistochemical analysis of muscle biopsy in patients suspected of having dermatomyositis may add greater sensitivity for the diagnosis when compared with conventional pathologic hallmarks of the disease, according to findings from a retrospective cohort study.
Myxovirus resistance A (MxA) is one of the type 1 interferon–inducible proteins whose overexpression is believed to play a role in the pathogenesis of dermatomyositis, and MxA expression has rarely been observed in other idiopathic inflammatory myopathies, said first author Akinori Uruha, MD, PhD, of the National Center of Neurology and Psychiatry, Tokyo, and his colleagues. They compared MxA expression in muscle biopsy samples from definite, probable, and possible dermatomyositis cases as well as other idiopathic inflammatory myopathies and other control conditions to assess its value against other muscle pathologic markers of dermatomyositis, such as the presence of perifascicular atrophy (PFA) and capillary membrane attack complex (MAC) deposition (Neurology. 2016 Dec 30. doi: 10.1212/WNL.0000000000003568).
The investigators studied muscle biopsy samples collected from 154 consecutive patients with idiopathic inflammatory myopathies seen from all over Japan, including 34 with dermatomyositis (10 juvenile cases), 8 with polymyositis (1 juvenile), 16 with anti–tRNA-synthetase antibody–associated myopathy (ASM); 46 with immune-mediated necrotizing myopathy (IMNM), and 50 with inclusion body myositis. The IMNM cases involved included 24 with anti–signal recognition particle (SRP) antibodies, 6 with anti–3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) antibodies, and 16 without anti-SRP, anti-HMGCR, or anti–tRNA-synthetase antibodies (3 juvenile patients). They used 51 patients with muscular dystrophy and 26 with neuropathies as controls.
Sarcoplasmic MxA expression proved to be more sensitive for a diagnosis of dermatomyositis than PFA and capillary MAC deposition (71% vs. 47% and 35%, respectively) but still had comparable specificity to those two markers (98% vs. 98% and 93%, respectively).
Of 18 cases with probable dermatomyositis, defined as typical skin rash but a lack of PFA, 8 (44%) showed sarcoplasmic MxA expression, and its sensitivity was 90% in juvenile cases overall and 63% in adult patients. Only 3 (17%) of the 18 showed capillary MAC deposition. Sarcoplasmic MxA expression occurred in all 12 patients with definite dermatomyositis, defined by the typical skin rash plus presence of PFA, whereas only 7 (58%) showed capillary MAC deposition. Among the four patients with possible dermatomyositis (PFA present but lacking typical skin rash), all showed sarcoplasmic MxA expression, compared with just two showing capillary MAC deposition.
In all other patients without definite, probable, or possible dermatomyositis, only two were positive for sarcoplasmic MxA expression (one with ASM and one with IMNM).
Dr. Uruha and his associates said that the results are “clearly demonstrating that sarcoplasmic MxA expression should be an excellent diagnostic marker of [dermatomyositis].”
The authors noted that the study was limited by the fact that they could not obtain full information about dermatomyositis-associated antibodies, and because other proteins of type 1 interferon signature are known to be upregulated in dermatomyositis, additional studies will need to determine which of the proteins is a better diagnostic marker.
The study was supported partly by an Intramural Research Grant of the National Center of Neurology and Psychiatry and grants from the Japanese Ministry of Education, Science, Sports and Culture and the Ministry of Health, Labor and Welfare of Japan. The investigators had no relevant disclosures.
The detection of sarcoplasmic myxovirus resistance A expression in immunohistochemical analysis of muscle biopsy in patients suspected of having dermatomyositis may add greater sensitivity for the diagnosis when compared with conventional pathologic hallmarks of the disease, according to findings from a retrospective cohort study.
Myxovirus resistance A (MxA) is one of the type 1 interferon–inducible proteins whose overexpression is believed to play a role in the pathogenesis of dermatomyositis, and MxA expression has rarely been observed in other idiopathic inflammatory myopathies, said first author Akinori Uruha, MD, PhD, of the National Center of Neurology and Psychiatry, Tokyo, and his colleagues. They compared MxA expression in muscle biopsy samples from definite, probable, and possible dermatomyositis cases as well as other idiopathic inflammatory myopathies and other control conditions to assess its value against other muscle pathologic markers of dermatomyositis, such as the presence of perifascicular atrophy (PFA) and capillary membrane attack complex (MAC) deposition (Neurology. 2016 Dec 30. doi: 10.1212/WNL.0000000000003568).
The investigators studied muscle biopsy samples collected from 154 consecutive patients with idiopathic inflammatory myopathies seen from all over Japan, including 34 with dermatomyositis (10 juvenile cases), 8 with polymyositis (1 juvenile), 16 with anti–tRNA-synthetase antibody–associated myopathy (ASM); 46 with immune-mediated necrotizing myopathy (IMNM), and 50 with inclusion body myositis. The IMNM cases involved included 24 with anti–signal recognition particle (SRP) antibodies, 6 with anti–3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) antibodies, and 16 without anti-SRP, anti-HMGCR, or anti–tRNA-synthetase antibodies (3 juvenile patients). They used 51 patients with muscular dystrophy and 26 with neuropathies as controls.
Sarcoplasmic MxA expression proved to be more sensitive for a diagnosis of dermatomyositis than PFA and capillary MAC deposition (71% vs. 47% and 35%, respectively) but still had comparable specificity to those two markers (98% vs. 98% and 93%, respectively).
Of 18 cases with probable dermatomyositis, defined as typical skin rash but a lack of PFA, 8 (44%) showed sarcoplasmic MxA expression, and its sensitivity was 90% in juvenile cases overall and 63% in adult patients. Only 3 (17%) of the 18 showed capillary MAC deposition. Sarcoplasmic MxA expression occurred in all 12 patients with definite dermatomyositis, defined by the typical skin rash plus presence of PFA, whereas only 7 (58%) showed capillary MAC deposition. Among the four patients with possible dermatomyositis (PFA present but lacking typical skin rash), all showed sarcoplasmic MxA expression, compared with just two showing capillary MAC deposition.
In all other patients without definite, probable, or possible dermatomyositis, only two were positive for sarcoplasmic MxA expression (one with ASM and one with IMNM).
Dr. Uruha and his associates said that the results are “clearly demonstrating that sarcoplasmic MxA expression should be an excellent diagnostic marker of [dermatomyositis].”
The authors noted that the study was limited by the fact that they could not obtain full information about dermatomyositis-associated antibodies, and because other proteins of type 1 interferon signature are known to be upregulated in dermatomyositis, additional studies will need to determine which of the proteins is a better diagnostic marker.
The study was supported partly by an Intramural Research Grant of the National Center of Neurology and Psychiatry and grants from the Japanese Ministry of Education, Science, Sports and Culture and the Ministry of Health, Labor and Welfare of Japan. The investigators had no relevant disclosures.
The detection of sarcoplasmic myxovirus resistance A expression in immunohistochemical analysis of muscle biopsy in patients suspected of having dermatomyositis may add greater sensitivity for the diagnosis when compared with conventional pathologic hallmarks of the disease, according to findings from a retrospective cohort study.
Myxovirus resistance A (MxA) is one of the type 1 interferon–inducible proteins whose overexpression is believed to play a role in the pathogenesis of dermatomyositis, and MxA expression has rarely been observed in other idiopathic inflammatory myopathies, said first author Akinori Uruha, MD, PhD, of the National Center of Neurology and Psychiatry, Tokyo, and his colleagues. They compared MxA expression in muscle biopsy samples from definite, probable, and possible dermatomyositis cases as well as other idiopathic inflammatory myopathies and other control conditions to assess its value against other muscle pathologic markers of dermatomyositis, such as the presence of perifascicular atrophy (PFA) and capillary membrane attack complex (MAC) deposition (Neurology. 2016 Dec 30. doi: 10.1212/WNL.0000000000003568).
The investigators studied muscle biopsy samples collected from 154 consecutive patients with idiopathic inflammatory myopathies seen from all over Japan, including 34 with dermatomyositis (10 juvenile cases), 8 with polymyositis (1 juvenile), 16 with anti–tRNA-synthetase antibody–associated myopathy (ASM); 46 with immune-mediated necrotizing myopathy (IMNM), and 50 with inclusion body myositis. The IMNM cases involved included 24 with anti–signal recognition particle (SRP) antibodies, 6 with anti–3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) antibodies, and 16 without anti-SRP, anti-HMGCR, or anti–tRNA-synthetase antibodies (3 juvenile patients). They used 51 patients with muscular dystrophy and 26 with neuropathies as controls.
Sarcoplasmic MxA expression proved to be more sensitive for a diagnosis of dermatomyositis than PFA and capillary MAC deposition (71% vs. 47% and 35%, respectively) but still had comparable specificity to those two markers (98% vs. 98% and 93%, respectively).
Of 18 cases with probable dermatomyositis, defined as typical skin rash but a lack of PFA, 8 (44%) showed sarcoplasmic MxA expression, and its sensitivity was 90% in juvenile cases overall and 63% in adult patients. Only 3 (17%) of the 18 showed capillary MAC deposition. Sarcoplasmic MxA expression occurred in all 12 patients with definite dermatomyositis, defined by the typical skin rash plus presence of PFA, whereas only 7 (58%) showed capillary MAC deposition. Among the four patients with possible dermatomyositis (PFA present but lacking typical skin rash), all showed sarcoplasmic MxA expression, compared with just two showing capillary MAC deposition.
In all other patients without definite, probable, or possible dermatomyositis, only two were positive for sarcoplasmic MxA expression (one with ASM and one with IMNM).
Dr. Uruha and his associates said that the results are “clearly demonstrating that sarcoplasmic MxA expression should be an excellent diagnostic marker of [dermatomyositis].”
The authors noted that the study was limited by the fact that they could not obtain full information about dermatomyositis-associated antibodies, and because other proteins of type 1 interferon signature are known to be upregulated in dermatomyositis, additional studies will need to determine which of the proteins is a better diagnostic marker.
The study was supported partly by an Intramural Research Grant of the National Center of Neurology and Psychiatry and grants from the Japanese Ministry of Education, Science, Sports and Culture and the Ministry of Health, Labor and Welfare of Japan. The investigators had no relevant disclosures.
FROM NEUROLOGY
Key clinical point:
Major finding: Sarcoplasmic MxA expression proved to be more sensitive for a diagnosis of dermatomyositis than PFA and capillary MAC deposition (71% vs. 47% and 35%, respectively) but still had comparable specificity to those two markers (98% vs. 98% and 93%, respectively).
Data source: A retrospective cohort study of 154 patients with idiopathic inflammatory myopathies, 51 with muscular dystrophy, and 26 with neuropathies.
Disclosures: The study was supported partly by an Intramural Research Grant of the National Center of Neurology and Psychiatry and grants from the Japanese Ministry of Education, Science, Sports and Culture and the Ministry of Health, Labor and Welfare of Japan. The investigators had no relevant disclosures.
When primary anti-TNF fails in axial spondyloarthritis, consider comorbidities or second anti-TNF
Most of the minority of axial spondyloarthritis patients who do not respond to their first tumor necrosis factor inhibitor still meet classification criteria for the condition 5-10 years later, but more than half respond to a second TNFi and most also have comorbidities that could affect the spondyloarthritis evaluation, according to findings from a single-center cohort study.
The study’s finding of TNFi primary inefficacy in 27 (12%) of 222 patients with axial spondyloarthritis (axSpA) who were given their first TNFi during 2004-2009 is in line with previous results of about 5%-15% primary inefficacy for a first TNFi in axSpA. However, the French investigators, led by Sandra Kossi of Cochin Hospital in Paris, noted that the difficulty of making an axSpA diagnosis and the presence of certain comorbidities “could interfere either with the activity of SpA (falsely heightened disease activity) or with the response to TNFi (falsely heightened inefficacy).” They sought to report the characteristics of axSpA patients with primary inefficacy after their first TNFi in the 5- to 10-year period after their prescription (Rheumatology [Oxford]. 2017 Jan 9. doi: 10.1093/rheumatology/kew456).
A total of 25 of the patients with primary inefficacy underwent re-evaluation 5-10 years (mean of 6 years) later. The investigators defined primary inefficacy as “treatment interruption 3-4 months after treatment onset, with a rheumatologist assessment in the medical file citing lack of efficacy as primary reason for drug interruption.”
The patients with primary TNFi inefficacy had a mean age of 53 years at the time of follow-up, and about half were female. All the patients still had symptoms and back pain, but symptoms were moderate based on a mean Bath Ankylosing Spondylitis Disease Activity Index score of 42. Overall, nine were taking a TNFi and nine were taking nonsteroidal anti-inflammatory drugs, while others used analgesics or nonpharmacologic measures.
Primary TNFi inefficacy occurred significantly more often occurred among females (48% vs. 27%; P = .04), older aged patients at first TNFi use (45 vs. 39 years; P = .04), patients with higher mean Bath Ankylosing Spondylitis Functional Index scores (68 vs. 42; P = .03), and in those who did not have an abnormally elevated C-reactive protein level (33% vs. 63%; P = .02). Patients with primary TNFi inefficacy had lower rates of HLAB27 positivity (56% vs. 72%) or radiographic sacroiliitis (67% vs. 81%), but the differences were not statistically significant.
At follow-up, 21 (84%) patients met Assessment of Spondyloarthritis International Society classification criteria for axSpA, and 20 (80%) met the axSpA diagnosis according to the rheumatologists’ opinion, with 17 (68%) fulfilling both.
A total of 18 (72%) had at least one of the following comorbidities: widespread pain syndrome, osteoarthritis, or depression. Five patients – all females – had widespread pain syndrome according to the Fibromyalgia Rapid Screening Tool questionnaire. Another 10 patients had osteoarthritis of lower-limb peripheral joints or of the spine, while an additional 8 had self-declared depression, for which 3 were taking antidepressants.
By the time of follow-up, 16 (64%) had switched to another TNFi, including 9 who had received two TNFi drugs and 7 who had received three or more. The second TNFi was considered efficacious in nine patients. The retention rate of the second TNFi at 1 year among those with primary inefficacy was 50%, and overall, nine patients were still prescribed a TNFi at the time of follow-up.
The fact that most of the patients with primary inefficacy to their first TNFi had confirmed axSpA but also had comorbidities that could affect axSpA evaluation “is important because practitioners might consider that primary inefficacy to TNFi leads to reconsidering the diagnosis of SpA (i.e. the notion of a TNFi prescription being used as the diagnostic test). We suggest here that primary inefficacy should not be considered as equivalent to a diagnostic error, and that a second prescription of TNFi may be of use in such patients, although painful comorbidities should certainly be screened for and taken into account.”
The study was funded by the Assistance Publique des Hôpitaux de Paris. The investigators had no conflicts of interest to declare.
Most of the minority of axial spondyloarthritis patients who do not respond to their first tumor necrosis factor inhibitor still meet classification criteria for the condition 5-10 years later, but more than half respond to a second TNFi and most also have comorbidities that could affect the spondyloarthritis evaluation, according to findings from a single-center cohort study.
The study’s finding of TNFi primary inefficacy in 27 (12%) of 222 patients with axial spondyloarthritis (axSpA) who were given their first TNFi during 2004-2009 is in line with previous results of about 5%-15% primary inefficacy for a first TNFi in axSpA. However, the French investigators, led by Sandra Kossi of Cochin Hospital in Paris, noted that the difficulty of making an axSpA diagnosis and the presence of certain comorbidities “could interfere either with the activity of SpA (falsely heightened disease activity) or with the response to TNFi (falsely heightened inefficacy).” They sought to report the characteristics of axSpA patients with primary inefficacy after their first TNFi in the 5- to 10-year period after their prescription (Rheumatology [Oxford]. 2017 Jan 9. doi: 10.1093/rheumatology/kew456).
A total of 25 of the patients with primary inefficacy underwent re-evaluation 5-10 years (mean of 6 years) later. The investigators defined primary inefficacy as “treatment interruption 3-4 months after treatment onset, with a rheumatologist assessment in the medical file citing lack of efficacy as primary reason for drug interruption.”
The patients with primary TNFi inefficacy had a mean age of 53 years at the time of follow-up, and about half were female. All the patients still had symptoms and back pain, but symptoms were moderate based on a mean Bath Ankylosing Spondylitis Disease Activity Index score of 42. Overall, nine were taking a TNFi and nine were taking nonsteroidal anti-inflammatory drugs, while others used analgesics or nonpharmacologic measures.
Primary TNFi inefficacy occurred significantly more often occurred among females (48% vs. 27%; P = .04), older aged patients at first TNFi use (45 vs. 39 years; P = .04), patients with higher mean Bath Ankylosing Spondylitis Functional Index scores (68 vs. 42; P = .03), and in those who did not have an abnormally elevated C-reactive protein level (33% vs. 63%; P = .02). Patients with primary TNFi inefficacy had lower rates of HLAB27 positivity (56% vs. 72%) or radiographic sacroiliitis (67% vs. 81%), but the differences were not statistically significant.
At follow-up, 21 (84%) patients met Assessment of Spondyloarthritis International Society classification criteria for axSpA, and 20 (80%) met the axSpA diagnosis according to the rheumatologists’ opinion, with 17 (68%) fulfilling both.
A total of 18 (72%) had at least one of the following comorbidities: widespread pain syndrome, osteoarthritis, or depression. Five patients – all females – had widespread pain syndrome according to the Fibromyalgia Rapid Screening Tool questionnaire. Another 10 patients had osteoarthritis of lower-limb peripheral joints or of the spine, while an additional 8 had self-declared depression, for which 3 were taking antidepressants.
By the time of follow-up, 16 (64%) had switched to another TNFi, including 9 who had received two TNFi drugs and 7 who had received three or more. The second TNFi was considered efficacious in nine patients. The retention rate of the second TNFi at 1 year among those with primary inefficacy was 50%, and overall, nine patients were still prescribed a TNFi at the time of follow-up.
The fact that most of the patients with primary inefficacy to their first TNFi had confirmed axSpA but also had comorbidities that could affect axSpA evaluation “is important because practitioners might consider that primary inefficacy to TNFi leads to reconsidering the diagnosis of SpA (i.e. the notion of a TNFi prescription being used as the diagnostic test). We suggest here that primary inefficacy should not be considered as equivalent to a diagnostic error, and that a second prescription of TNFi may be of use in such patients, although painful comorbidities should certainly be screened for and taken into account.”
The study was funded by the Assistance Publique des Hôpitaux de Paris. The investigators had no conflicts of interest to declare.
Most of the minority of axial spondyloarthritis patients who do not respond to their first tumor necrosis factor inhibitor still meet classification criteria for the condition 5-10 years later, but more than half respond to a second TNFi and most also have comorbidities that could affect the spondyloarthritis evaluation, according to findings from a single-center cohort study.
The study’s finding of TNFi primary inefficacy in 27 (12%) of 222 patients with axial spondyloarthritis (axSpA) who were given their first TNFi during 2004-2009 is in line with previous results of about 5%-15% primary inefficacy for a first TNFi in axSpA. However, the French investigators, led by Sandra Kossi of Cochin Hospital in Paris, noted that the difficulty of making an axSpA diagnosis and the presence of certain comorbidities “could interfere either with the activity of SpA (falsely heightened disease activity) or with the response to TNFi (falsely heightened inefficacy).” They sought to report the characteristics of axSpA patients with primary inefficacy after their first TNFi in the 5- to 10-year period after their prescription (Rheumatology [Oxford]. 2017 Jan 9. doi: 10.1093/rheumatology/kew456).
A total of 25 of the patients with primary inefficacy underwent re-evaluation 5-10 years (mean of 6 years) later. The investigators defined primary inefficacy as “treatment interruption 3-4 months after treatment onset, with a rheumatologist assessment in the medical file citing lack of efficacy as primary reason for drug interruption.”
The patients with primary TNFi inefficacy had a mean age of 53 years at the time of follow-up, and about half were female. All the patients still had symptoms and back pain, but symptoms were moderate based on a mean Bath Ankylosing Spondylitis Disease Activity Index score of 42. Overall, nine were taking a TNFi and nine were taking nonsteroidal anti-inflammatory drugs, while others used analgesics or nonpharmacologic measures.
Primary TNFi inefficacy occurred significantly more often occurred among females (48% vs. 27%; P = .04), older aged patients at first TNFi use (45 vs. 39 years; P = .04), patients with higher mean Bath Ankylosing Spondylitis Functional Index scores (68 vs. 42; P = .03), and in those who did not have an abnormally elevated C-reactive protein level (33% vs. 63%; P = .02). Patients with primary TNFi inefficacy had lower rates of HLAB27 positivity (56% vs. 72%) or radiographic sacroiliitis (67% vs. 81%), but the differences were not statistically significant.
At follow-up, 21 (84%) patients met Assessment of Spondyloarthritis International Society classification criteria for axSpA, and 20 (80%) met the axSpA diagnosis according to the rheumatologists’ opinion, with 17 (68%) fulfilling both.
A total of 18 (72%) had at least one of the following comorbidities: widespread pain syndrome, osteoarthritis, or depression. Five patients – all females – had widespread pain syndrome according to the Fibromyalgia Rapid Screening Tool questionnaire. Another 10 patients had osteoarthritis of lower-limb peripheral joints or of the spine, while an additional 8 had self-declared depression, for which 3 were taking antidepressants.
By the time of follow-up, 16 (64%) had switched to another TNFi, including 9 who had received two TNFi drugs and 7 who had received three or more. The second TNFi was considered efficacious in nine patients. The retention rate of the second TNFi at 1 year among those with primary inefficacy was 50%, and overall, nine patients were still prescribed a TNFi at the time of follow-up.
The fact that most of the patients with primary inefficacy to their first TNFi had confirmed axSpA but also had comorbidities that could affect axSpA evaluation “is important because practitioners might consider that primary inefficacy to TNFi leads to reconsidering the diagnosis of SpA (i.e. the notion of a TNFi prescription being used as the diagnostic test). We suggest here that primary inefficacy should not be considered as equivalent to a diagnostic error, and that a second prescription of TNFi may be of use in such patients, although painful comorbidities should certainly be screened for and taken into account.”
The study was funded by the Assistance Publique des Hôpitaux de Paris. The investigators had no conflicts of interest to declare.
Key clinical point:
Major finding: A total of 18 (72%) of 25 patients with primary TNFi inefficacy had at least one of the following comorbidities: widespread pain syndrome, osteoarthritis, or depression.
Data source: A retrospective and prospective cohort study of 222 patients who received a first TNFi after being diagnosed with axial spondyloarthritis during 2004-2009.
Disclosures: The study was funded by the Assistance Publique des Hôpitaux de Paris. The investigators had no conflicts of interest to declare.
Medicare payments set for infliximab biosimilar Inflectra
Payment for the infliximab biosimilar drug Inflectra will now be covered by Medicare, the drug’s manufacturer, Pfizer, said in an announcement.
The Centers for Medicare & Medicaid Services (CMS) included Inflectra (infliximab-dyyb) in its January 2017 Average Sales Price pricing file, which went into effect Jan. 1, 2017. Pfizer said that Inflectra is priced at a 15% discount to the current wholesale acquisition cost for the infliximab originator Remicade, but this price does not include discounts to payers, providers, distributors, and other purchasing organizations.
For the first quarter of 2017, the payment limit set by the CMS for Inflectra is $100.306 per 10-mg unit and $82.218 for Remicade.
Various national and regional wholesalers across the country began receiving shipments of Inflectra in November 2016, according to Pfizer.
In conjunction with the availability of Inflectra, Pfizer announced its enCompass program, “a comprehensive reimbursement service and patient support program offering coding and reimbursement support for providers, copay assistance to eligible patients who have commercial insurance that covers Inflectra, and financial assistance for eligible uninsured and underinsured patients.”
The FDA approved Inflectra in April 2016 for all of the same indications as Remicade: rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, plaque psoriasis, and ulcerative colitis.
Payment for the infliximab biosimilar drug Inflectra will now be covered by Medicare, the drug’s manufacturer, Pfizer, said in an announcement.
The Centers for Medicare & Medicaid Services (CMS) included Inflectra (infliximab-dyyb) in its January 2017 Average Sales Price pricing file, which went into effect Jan. 1, 2017. Pfizer said that Inflectra is priced at a 15% discount to the current wholesale acquisition cost for the infliximab originator Remicade, but this price does not include discounts to payers, providers, distributors, and other purchasing organizations.
For the first quarter of 2017, the payment limit set by the CMS for Inflectra is $100.306 per 10-mg unit and $82.218 for Remicade.
Various national and regional wholesalers across the country began receiving shipments of Inflectra in November 2016, according to Pfizer.
In conjunction with the availability of Inflectra, Pfizer announced its enCompass program, “a comprehensive reimbursement service and patient support program offering coding and reimbursement support for providers, copay assistance to eligible patients who have commercial insurance that covers Inflectra, and financial assistance for eligible uninsured and underinsured patients.”
The FDA approved Inflectra in April 2016 for all of the same indications as Remicade: rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, plaque psoriasis, and ulcerative colitis.
Payment for the infliximab biosimilar drug Inflectra will now be covered by Medicare, the drug’s manufacturer, Pfizer, said in an announcement.
The Centers for Medicare & Medicaid Services (CMS) included Inflectra (infliximab-dyyb) in its January 2017 Average Sales Price pricing file, which went into effect Jan. 1, 2017. Pfizer said that Inflectra is priced at a 15% discount to the current wholesale acquisition cost for the infliximab originator Remicade, but this price does not include discounts to payers, providers, distributors, and other purchasing organizations.
For the first quarter of 2017, the payment limit set by the CMS for Inflectra is $100.306 per 10-mg unit and $82.218 for Remicade.
Various national and regional wholesalers across the country began receiving shipments of Inflectra in November 2016, according to Pfizer.
In conjunction with the availability of Inflectra, Pfizer announced its enCompass program, “a comprehensive reimbursement service and patient support program offering coding and reimbursement support for providers, copay assistance to eligible patients who have commercial insurance that covers Inflectra, and financial assistance for eligible uninsured and underinsured patients.”
The FDA approved Inflectra in April 2016 for all of the same indications as Remicade: rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, plaque psoriasis, and ulcerative colitis.
MACRA’s near and potential long-term future outlined for rheumatology
WASHINGTON – Now that implementation of the Medicare Access and CHIP Reauthorization Act is on rheumatologists’ doorsteps, figuring out what is required in 2017 is imperative to avoid future penalties and maximize the chance of earning a bonus.
Recent announcements from the Centers for Medicare & Medicaid Services (CMS) on performance thresholds and how to meet them in 2017 give rheumatologists a great shot at not getting penalized when payment adjustments begin in 2019.
However, efforts by the ACR to create new rheumatology-focused APMs could play a major role in changing that, said Dr. Harvey, clinical director of the Arthritis Treatment Center at Tufts Medical Center, Boston, and former chair of the ACR’s Committee on Government Affairs.
The MIPS option in MACRA is “a repackaging” of old programs, including Meaningful Use (which is now called Advancing Care Information), value-based modifiers, and the Physician Quality Reporting System (PQRS). “One silver lining to this massive piece of legislation is that it’s actually less downside risk than if you had continued with Meaningful Use, PQRS, and value-based modifier,” Dr. Harvey said.
MIPS is onerous by design, in Dr. Harvey’s opinion. “CMS does not want to continue the fee-for-service arrangement and MIPS is basically fee-for-service with a bit of pay-for-performance bolted on top of it. They’ve already stated that they want to push every provider into alternative payment model–type reimbursements going forward.”
Rheumatologists aren’t eligible for MIPS if they see fewer than 100 Medicare patients per year or if they bill less than $30,000 in Medicare fees. For MIPS-eligible physicians, adjustments to Medicare payments begin in 2019 based on 2017 quality reporting data. Physicians will still receive yearly 0.5% increases in Medicare pay in 2017-2019 and 0% each year through 2025 before any adjustments are made based on the MIPS score. Participation in the MIPS pathway gives the potential for payment adjustments starting at plus or minus 4% in 2019, plus or minus 5% in 2020, plus or minus 7% in 2021, and plus or minus 9% in 2022 and beyond, based on how rheumatologists compare against their peers.
Targets for 2017 and adjustments beyond 2017
Each year in November, CMS will announce the base performance threshold goal that physicians will need to reach in the following year in order to avoid negative Medicare payment adjustments 2 years later.
Each year’s threshold will be based on the data collected from the prior year. For the year starting Jan. 1, 2017, in order to avoid a 4% cut in their Medicare Part B base rate payment in 2019, rheumatologists will need to meet a base performance threshold score of just 3 out of 100.
“Basically, if you participate in a program in any way whatsoever, you can hit this target,” Dr. Harvey said.
In 2017, getting a score of 70 or more out of 100 puts rheumatologists into a high performance category that makes them eligible for a piece of the $500 million pool of positive payment adjustments that will be available in each of the first 6 years of MIPS.
Providers who score less than 3 out of 100 will get the maximum penalty – a 4% cut in their 2019 Medicare payment rate. Further, in 2017, only 90 days of reporting is required to qualify for positive adjustments in 2019.
The base performance threshold will certainly go up for 2018 to “probably 30, 40, 50; something like that,” Dr. Harvey said.
Knowing the threshold in advance should help rheumatologists to predict by the middle of each year whether they are going to make it, but how much of any increase (or decrease) in payment adjustment they will have 2 years hence will be very difficult to know, he said, because each year the adjustment must be budget neutral and is dependent on how many physicians are above and below the threshold.
The MIPS score is based on four categories that total up to 100 points:
Quality (60% of 2017 score)
The quality category is determined by six measures that are worth 10 points each. All of the quality domains from PQRS are gone, and out of those six measures providers must have one cross-cutting measure and one outcome measure, or just one high-priority measure. Since rheumatology does not yet have any designated outcome measures, rheumatologists will need to report other designated measures. For each of these six required measures, a provider would earn 3 points for reaching the benchmark, and then the score could be increased to 4-10 points per measure based on a decile system that determines the provider’s performance against others who have met the benchmark for that measure.
Of the 13 quality metrics that are in the rheumatology quality measure set, 7 are not specific to rheumatology (advanced directive documentation, body mass index screening and follow-up, taking a comprehensive medication list, tobacco screening in adolescents, tobacco screening in adults, hypertension screening and follow-up, and sending consult note to referring doctor), whereas 6 are (TB screening within 6 months of starting a biologic, yearly TB screening on biologics, measuring rheumatoid arthritis [RA] disease activity, measuring RA functional assessment, documenting RA prognosis, and RA steroid management).
The quality category will account for 50% of the MIPS score in 2018.
Resource use (0% of 2017 score)
“The fact that the resource use part of the equation has been set to 0% for the 2017 performance year is a really good thing for rheumatologists because we use some of the most expensive drugs around,” Dr. Harvey said. “Part of the reason that CMS did this is that they are having trouble accounting for the fact that they have easy access to Part B cost data – infusion cost data – but they don’t have very good access to Part D self-injectable drug cost data.”
“We are going to make it a key advocacy point that they appropriately take into account cost in future years,” he added.
While the resource use category of MIPS contributes nothing to the 2017 MIPS score, it will increase to 10% in 2018 and by 2021 it’s anticipated to be 30% of the MIPS score, while the quality category is anticipated to drop to 30%.
Clinical practice improvement activities (15% of 2017 score)
This part includes more than 90 proposed activities to count toward the category’s score, including patient engagement activities, care coordination, extended office hours, and participation in a qualified clinical data registry (QCDR), such as the ACR’s RISE Registry, which is already a certified QCDR. A total of 40 points in this category gives full credit for the 15 percentage point value given to it for 2017.
All of the proposed activities for 2017 are weighted as medium (10 points) or high weight (20 points). For example, 40 points could be earned by meeting two medium-weight measures and one high-weight measure.
The clinical practice improvement activities category will stay at 15% of the MIPS score in 2018.
Advancing care information (25% of 2017 score)
“This is another one that gets complicated, but there’s one key take-home message: This is way easier than Meaningful Use has ever been,” Dr. Harvey said. There are 100 points needed in the advancing care information category in order to get the full 25 percentage points that it accounts for in the 2017 MIPS score.
For reporting on five required measures (electronic health record [EHR] security analysis, e-prescribing, patient access to an EHR, and being able to send and accept summary of care documents), a provider will earn 50 points.
Another 90 performance points are available for reporting certain information, and this is based on a decile system just like the quality category in which a rheumatologist’s performance is measured against other rheumatologists who have met the benchmark for each particular measure. These optional measures include providing patient-specific educational information; patients being able to view, download, and transmit their own medical records; secure messaging; acceptance of patient-generated health data; medication reconciliation; and submitting data to a state immunization registry.
Another 15 bonus points are available for additional public health reporting and reporting to CMS using a certified EHR or QCDR.
All these measures together give providers the potential to earn 155 points toward the 100-point threshold.
“If you’re already doing Meaningful Use, chances are you’re going to do really well in this area,” he said.
The advancing care information category will stay at 25% of the MIPS score in 2018.
Problems with current APMs
Under MACRA, participation in an APM means that the physician is exempt from MIPS and will receive a 5% lump sum bonus per year in 2019-2024, a higher annual increase in fee-for-service revenues, and the general benefits of participating in an APM. However, few rheumatologists will qualify for the APM pathway, and there are no rheumatology-specific APMs in existence.
Most current APMs are “shared savings” programs where if the physician or health system can reduce spending below the expected levels, then the provider receives a share of the payer’s savings. However, these shared-savings APMs all still use a fee-for-service structure, which makes them just a different form of pay for performance, according to Mr. Miller.
Physicians still don’t get paid for unfunded or underfunded services, and physicians who are already efficient receive little or no additional revenue and may be forced out of business, while physicians who have been practicing inefficiently or inappropriately are paid more than conservative physicians. There’s also the potential for rewarding the denial of needed care. Physicians in shared-savings APMs are also placed at risk for costs they cannot control and for random variations in spending. And most of all, the shared savings bonuses are temporary and when there are no more savings to be generated, physicians are underpaid, Mr. Miller said.
During 2013-2015, 46%-48% of Medicare shared-savings accountable care organizations (ACOs) increased their Medicare spending rather than reduced it, and only 24%-30% of the ACOs received shared-savings payments. In each year, Medicare spent more than it saved, with net losses ranging from $50 million to $216 million. This happened because physicians in the programs still got paid with fee-for-service payments, Mr. Miller said.
Creating rheumatology-focused APMs
MACRA designated the development of the Physician-Focused Payment Model Technical Advisory Committee, of which Mr. Miller is a member, to solicit and review physician-focused payment models and make recommendations to CMS about which ones to implement.
Physician-focused payment models got their start through pioneering work by physicians who obtained data from insurers to find ways to reach out proactively to patients to address problems before patients are hospitalized. Through these efforts, they have reduced cost and increased patient satisfaction while also increasing payment to physicians by supporting “medical home” services, according to Dr. Miller.
These efforts to create APMs that support high-quality, physician-directed care begin by identifying avoidable spending that varies from specialty to specialty and from condition to condition. Then they address barriers in the current fee-for-service system – such as no payment for many high-value services and insufficient revenue to cover costs when using fewer or low-cost services – by providing flexible, adequate payment while requiring physicians to take responsibility for the things they said could be avoidable when paid in that way. However, this responsibility must be focused on what a particular physician can influence, Mr. Miller noted.
Rheumatologists could be helped by these physician-focused payment models because they receive less than 10% of the total Medicare health care spending per patient whose care was directed by a rheumatologist. In that case, finding ways to drop total spending per patient by 5% could at the same time give rheumatologists a 25% increase in payment while also saving Medicare 3% overall, he said.
Rheumatologists are best set up to take condition-based payments that are geared to keep patients out of the hospital, rather than the hospital episode–based payments that have dominated APMs in existence so far. Central to this condition-based model is getting the right diagnosis at the start, so payment for getting the correct diagnosis would be critical.
APMs designed for rheumatologists could take into account the diseases often seen by a rheumatologist, such as RA, and then identify opportunities to improve care and reduce costs while identifying barriers in the current payment system for achieving those goals, Mr. Miller said. These opportunities and barriers would vary from condition to condition. In some cases, particularly for low-frequency conditions, there may not need to be a new payment model established and it could be done through fee-for-service.
Ideally, these condition-based payment models for specialists such as rheumatologists would exist within the “medical neighborhood” of primary care physicians who could refer to them when necessary. Specialists would be accountable for the aspects of care that they can control, such as avoiding unnecessary tests and procedures and avoiding infections and complications.
“That’s building the ACO from the bottom up, rather than what Medicare is trying to do, which is to create it from the top down,” Mr. Miller said.
Mr. Miller noted that it will be important for specialties such as rheumatology to define the cost data it needs in order to develop condition-based payment models.
Dr. Harvey had no relevant disclosures. Mr. Miller has no financial relationships with any commercial interests.
WASHINGTON – Now that implementation of the Medicare Access and CHIP Reauthorization Act is on rheumatologists’ doorsteps, figuring out what is required in 2017 is imperative to avoid future penalties and maximize the chance of earning a bonus.
Recent announcements from the Centers for Medicare & Medicaid Services (CMS) on performance thresholds and how to meet them in 2017 give rheumatologists a great shot at not getting penalized when payment adjustments begin in 2019.
However, efforts by the ACR to create new rheumatology-focused APMs could play a major role in changing that, said Dr. Harvey, clinical director of the Arthritis Treatment Center at Tufts Medical Center, Boston, and former chair of the ACR’s Committee on Government Affairs.
The MIPS option in MACRA is “a repackaging” of old programs, including Meaningful Use (which is now called Advancing Care Information), value-based modifiers, and the Physician Quality Reporting System (PQRS). “One silver lining to this massive piece of legislation is that it’s actually less downside risk than if you had continued with Meaningful Use, PQRS, and value-based modifier,” Dr. Harvey said.
MIPS is onerous by design, in Dr. Harvey’s opinion. “CMS does not want to continue the fee-for-service arrangement and MIPS is basically fee-for-service with a bit of pay-for-performance bolted on top of it. They’ve already stated that they want to push every provider into alternative payment model–type reimbursements going forward.”
Rheumatologists aren’t eligible for MIPS if they see fewer than 100 Medicare patients per year or if they bill less than $30,000 in Medicare fees. For MIPS-eligible physicians, adjustments to Medicare payments begin in 2019 based on 2017 quality reporting data. Physicians will still receive yearly 0.5% increases in Medicare pay in 2017-2019 and 0% each year through 2025 before any adjustments are made based on the MIPS score. Participation in the MIPS pathway gives the potential for payment adjustments starting at plus or minus 4% in 2019, plus or minus 5% in 2020, plus or minus 7% in 2021, and plus or minus 9% in 2022 and beyond, based on how rheumatologists compare against their peers.
Targets for 2017 and adjustments beyond 2017
Each year in November, CMS will announce the base performance threshold goal that physicians will need to reach in the following year in order to avoid negative Medicare payment adjustments 2 years later.
Each year’s threshold will be based on the data collected from the prior year. For the year starting Jan. 1, 2017, in order to avoid a 4% cut in their Medicare Part B base rate payment in 2019, rheumatologists will need to meet a base performance threshold score of just 3 out of 100.
“Basically, if you participate in a program in any way whatsoever, you can hit this target,” Dr. Harvey said.
In 2017, getting a score of 70 or more out of 100 puts rheumatologists into a high performance category that makes them eligible for a piece of the $500 million pool of positive payment adjustments that will be available in each of the first 6 years of MIPS.
Providers who score less than 3 out of 100 will get the maximum penalty – a 4% cut in their 2019 Medicare payment rate. Further, in 2017, only 90 days of reporting is required to qualify for positive adjustments in 2019.
The base performance threshold will certainly go up for 2018 to “probably 30, 40, 50; something like that,” Dr. Harvey said.
Knowing the threshold in advance should help rheumatologists to predict by the middle of each year whether they are going to make it, but how much of any increase (or decrease) in payment adjustment they will have 2 years hence will be very difficult to know, he said, because each year the adjustment must be budget neutral and is dependent on how many physicians are above and below the threshold.
The MIPS score is based on four categories that total up to 100 points:
Quality (60% of 2017 score)
The quality category is determined by six measures that are worth 10 points each. All of the quality domains from PQRS are gone, and out of those six measures providers must have one cross-cutting measure and one outcome measure, or just one high-priority measure. Since rheumatology does not yet have any designated outcome measures, rheumatologists will need to report other designated measures. For each of these six required measures, a provider would earn 3 points for reaching the benchmark, and then the score could be increased to 4-10 points per measure based on a decile system that determines the provider’s performance against others who have met the benchmark for that measure.
Of the 13 quality metrics that are in the rheumatology quality measure set, 7 are not specific to rheumatology (advanced directive documentation, body mass index screening and follow-up, taking a comprehensive medication list, tobacco screening in adolescents, tobacco screening in adults, hypertension screening and follow-up, and sending consult note to referring doctor), whereas 6 are (TB screening within 6 months of starting a biologic, yearly TB screening on biologics, measuring rheumatoid arthritis [RA] disease activity, measuring RA functional assessment, documenting RA prognosis, and RA steroid management).
The quality category will account for 50% of the MIPS score in 2018.
Resource use (0% of 2017 score)
“The fact that the resource use part of the equation has been set to 0% for the 2017 performance year is a really good thing for rheumatologists because we use some of the most expensive drugs around,” Dr. Harvey said. “Part of the reason that CMS did this is that they are having trouble accounting for the fact that they have easy access to Part B cost data – infusion cost data – but they don’t have very good access to Part D self-injectable drug cost data.”
“We are going to make it a key advocacy point that they appropriately take into account cost in future years,” he added.
While the resource use category of MIPS contributes nothing to the 2017 MIPS score, it will increase to 10% in 2018 and by 2021 it’s anticipated to be 30% of the MIPS score, while the quality category is anticipated to drop to 30%.
Clinical practice improvement activities (15% of 2017 score)
This part includes more than 90 proposed activities to count toward the category’s score, including patient engagement activities, care coordination, extended office hours, and participation in a qualified clinical data registry (QCDR), such as the ACR’s RISE Registry, which is already a certified QCDR. A total of 40 points in this category gives full credit for the 15 percentage point value given to it for 2017.
All of the proposed activities for 2017 are weighted as medium (10 points) or high weight (20 points). For example, 40 points could be earned by meeting two medium-weight measures and one high-weight measure.
The clinical practice improvement activities category will stay at 15% of the MIPS score in 2018.
Advancing care information (25% of 2017 score)
“This is another one that gets complicated, but there’s one key take-home message: This is way easier than Meaningful Use has ever been,” Dr. Harvey said. There are 100 points needed in the advancing care information category in order to get the full 25 percentage points that it accounts for in the 2017 MIPS score.
For reporting on five required measures (electronic health record [EHR] security analysis, e-prescribing, patient access to an EHR, and being able to send and accept summary of care documents), a provider will earn 50 points.
Another 90 performance points are available for reporting certain information, and this is based on a decile system just like the quality category in which a rheumatologist’s performance is measured against other rheumatologists who have met the benchmark for each particular measure. These optional measures include providing patient-specific educational information; patients being able to view, download, and transmit their own medical records; secure messaging; acceptance of patient-generated health data; medication reconciliation; and submitting data to a state immunization registry.
Another 15 bonus points are available for additional public health reporting and reporting to CMS using a certified EHR or QCDR.
All these measures together give providers the potential to earn 155 points toward the 100-point threshold.
“If you’re already doing Meaningful Use, chances are you’re going to do really well in this area,” he said.
The advancing care information category will stay at 25% of the MIPS score in 2018.
Problems with current APMs
Under MACRA, participation in an APM means that the physician is exempt from MIPS and will receive a 5% lump sum bonus per year in 2019-2024, a higher annual increase in fee-for-service revenues, and the general benefits of participating in an APM. However, few rheumatologists will qualify for the APM pathway, and there are no rheumatology-specific APMs in existence.
Most current APMs are “shared savings” programs where if the physician or health system can reduce spending below the expected levels, then the provider receives a share of the payer’s savings. However, these shared-savings APMs all still use a fee-for-service structure, which makes them just a different form of pay for performance, according to Mr. Miller.
Physicians still don’t get paid for unfunded or underfunded services, and physicians who are already efficient receive little or no additional revenue and may be forced out of business, while physicians who have been practicing inefficiently or inappropriately are paid more than conservative physicians. There’s also the potential for rewarding the denial of needed care. Physicians in shared-savings APMs are also placed at risk for costs they cannot control and for random variations in spending. And most of all, the shared savings bonuses are temporary and when there are no more savings to be generated, physicians are underpaid, Mr. Miller said.
During 2013-2015, 46%-48% of Medicare shared-savings accountable care organizations (ACOs) increased their Medicare spending rather than reduced it, and only 24%-30% of the ACOs received shared-savings payments. In each year, Medicare spent more than it saved, with net losses ranging from $50 million to $216 million. This happened because physicians in the programs still got paid with fee-for-service payments, Mr. Miller said.
Creating rheumatology-focused APMs
MACRA designated the development of the Physician-Focused Payment Model Technical Advisory Committee, of which Mr. Miller is a member, to solicit and review physician-focused payment models and make recommendations to CMS about which ones to implement.
Physician-focused payment models got their start through pioneering work by physicians who obtained data from insurers to find ways to reach out proactively to patients to address problems before patients are hospitalized. Through these efforts, they have reduced cost and increased patient satisfaction while also increasing payment to physicians by supporting “medical home” services, according to Dr. Miller.
These efforts to create APMs that support high-quality, physician-directed care begin by identifying avoidable spending that varies from specialty to specialty and from condition to condition. Then they address barriers in the current fee-for-service system – such as no payment for many high-value services and insufficient revenue to cover costs when using fewer or low-cost services – by providing flexible, adequate payment while requiring physicians to take responsibility for the things they said could be avoidable when paid in that way. However, this responsibility must be focused on what a particular physician can influence, Mr. Miller noted.
Rheumatologists could be helped by these physician-focused payment models because they receive less than 10% of the total Medicare health care spending per patient whose care was directed by a rheumatologist. In that case, finding ways to drop total spending per patient by 5% could at the same time give rheumatologists a 25% increase in payment while also saving Medicare 3% overall, he said.
Rheumatologists are best set up to take condition-based payments that are geared to keep patients out of the hospital, rather than the hospital episode–based payments that have dominated APMs in existence so far. Central to this condition-based model is getting the right diagnosis at the start, so payment for getting the correct diagnosis would be critical.
APMs designed for rheumatologists could take into account the diseases often seen by a rheumatologist, such as RA, and then identify opportunities to improve care and reduce costs while identifying barriers in the current payment system for achieving those goals, Mr. Miller said. These opportunities and barriers would vary from condition to condition. In some cases, particularly for low-frequency conditions, there may not need to be a new payment model established and it could be done through fee-for-service.
Ideally, these condition-based payment models for specialists such as rheumatologists would exist within the “medical neighborhood” of primary care physicians who could refer to them when necessary. Specialists would be accountable for the aspects of care that they can control, such as avoiding unnecessary tests and procedures and avoiding infections and complications.
“That’s building the ACO from the bottom up, rather than what Medicare is trying to do, which is to create it from the top down,” Mr. Miller said.
Mr. Miller noted that it will be important for specialties such as rheumatology to define the cost data it needs in order to develop condition-based payment models.
Dr. Harvey had no relevant disclosures. Mr. Miller has no financial relationships with any commercial interests.
WASHINGTON – Now that implementation of the Medicare Access and CHIP Reauthorization Act is on rheumatologists’ doorsteps, figuring out what is required in 2017 is imperative to avoid future penalties and maximize the chance of earning a bonus.
Recent announcements from the Centers for Medicare & Medicaid Services (CMS) on performance thresholds and how to meet them in 2017 give rheumatologists a great shot at not getting penalized when payment adjustments begin in 2019.
However, efforts by the ACR to create new rheumatology-focused APMs could play a major role in changing that, said Dr. Harvey, clinical director of the Arthritis Treatment Center at Tufts Medical Center, Boston, and former chair of the ACR’s Committee on Government Affairs.
The MIPS option in MACRA is “a repackaging” of old programs, including Meaningful Use (which is now called Advancing Care Information), value-based modifiers, and the Physician Quality Reporting System (PQRS). “One silver lining to this massive piece of legislation is that it’s actually less downside risk than if you had continued with Meaningful Use, PQRS, and value-based modifier,” Dr. Harvey said.
MIPS is onerous by design, in Dr. Harvey’s opinion. “CMS does not want to continue the fee-for-service arrangement and MIPS is basically fee-for-service with a bit of pay-for-performance bolted on top of it. They’ve already stated that they want to push every provider into alternative payment model–type reimbursements going forward.”
Rheumatologists aren’t eligible for MIPS if they see fewer than 100 Medicare patients per year or if they bill less than $30,000 in Medicare fees. For MIPS-eligible physicians, adjustments to Medicare payments begin in 2019 based on 2017 quality reporting data. Physicians will still receive yearly 0.5% increases in Medicare pay in 2017-2019 and 0% each year through 2025 before any adjustments are made based on the MIPS score. Participation in the MIPS pathway gives the potential for payment adjustments starting at plus or minus 4% in 2019, plus or minus 5% in 2020, plus or minus 7% in 2021, and plus or minus 9% in 2022 and beyond, based on how rheumatologists compare against their peers.
Targets for 2017 and adjustments beyond 2017
Each year in November, CMS will announce the base performance threshold goal that physicians will need to reach in the following year in order to avoid negative Medicare payment adjustments 2 years later.
Each year’s threshold will be based on the data collected from the prior year. For the year starting Jan. 1, 2017, in order to avoid a 4% cut in their Medicare Part B base rate payment in 2019, rheumatologists will need to meet a base performance threshold score of just 3 out of 100.
“Basically, if you participate in a program in any way whatsoever, you can hit this target,” Dr. Harvey said.
In 2017, getting a score of 70 or more out of 100 puts rheumatologists into a high performance category that makes them eligible for a piece of the $500 million pool of positive payment adjustments that will be available in each of the first 6 years of MIPS.
Providers who score less than 3 out of 100 will get the maximum penalty – a 4% cut in their 2019 Medicare payment rate. Further, in 2017, only 90 days of reporting is required to qualify for positive adjustments in 2019.
The base performance threshold will certainly go up for 2018 to “probably 30, 40, 50; something like that,” Dr. Harvey said.
Knowing the threshold in advance should help rheumatologists to predict by the middle of each year whether they are going to make it, but how much of any increase (or decrease) in payment adjustment they will have 2 years hence will be very difficult to know, he said, because each year the adjustment must be budget neutral and is dependent on how many physicians are above and below the threshold.
The MIPS score is based on four categories that total up to 100 points:
Quality (60% of 2017 score)
The quality category is determined by six measures that are worth 10 points each. All of the quality domains from PQRS are gone, and out of those six measures providers must have one cross-cutting measure and one outcome measure, or just one high-priority measure. Since rheumatology does not yet have any designated outcome measures, rheumatologists will need to report other designated measures. For each of these six required measures, a provider would earn 3 points for reaching the benchmark, and then the score could be increased to 4-10 points per measure based on a decile system that determines the provider’s performance against others who have met the benchmark for that measure.
Of the 13 quality metrics that are in the rheumatology quality measure set, 7 are not specific to rheumatology (advanced directive documentation, body mass index screening and follow-up, taking a comprehensive medication list, tobacco screening in adolescents, tobacco screening in adults, hypertension screening and follow-up, and sending consult note to referring doctor), whereas 6 are (TB screening within 6 months of starting a biologic, yearly TB screening on biologics, measuring rheumatoid arthritis [RA] disease activity, measuring RA functional assessment, documenting RA prognosis, and RA steroid management).
The quality category will account for 50% of the MIPS score in 2018.
Resource use (0% of 2017 score)
“The fact that the resource use part of the equation has been set to 0% for the 2017 performance year is a really good thing for rheumatologists because we use some of the most expensive drugs around,” Dr. Harvey said. “Part of the reason that CMS did this is that they are having trouble accounting for the fact that they have easy access to Part B cost data – infusion cost data – but they don’t have very good access to Part D self-injectable drug cost data.”
“We are going to make it a key advocacy point that they appropriately take into account cost in future years,” he added.
While the resource use category of MIPS contributes nothing to the 2017 MIPS score, it will increase to 10% in 2018 and by 2021 it’s anticipated to be 30% of the MIPS score, while the quality category is anticipated to drop to 30%.
Clinical practice improvement activities (15% of 2017 score)
This part includes more than 90 proposed activities to count toward the category’s score, including patient engagement activities, care coordination, extended office hours, and participation in a qualified clinical data registry (QCDR), such as the ACR’s RISE Registry, which is already a certified QCDR. A total of 40 points in this category gives full credit for the 15 percentage point value given to it for 2017.
All of the proposed activities for 2017 are weighted as medium (10 points) or high weight (20 points). For example, 40 points could be earned by meeting two medium-weight measures and one high-weight measure.
The clinical practice improvement activities category will stay at 15% of the MIPS score in 2018.
Advancing care information (25% of 2017 score)
“This is another one that gets complicated, but there’s one key take-home message: This is way easier than Meaningful Use has ever been,” Dr. Harvey said. There are 100 points needed in the advancing care information category in order to get the full 25 percentage points that it accounts for in the 2017 MIPS score.
For reporting on five required measures (electronic health record [EHR] security analysis, e-prescribing, patient access to an EHR, and being able to send and accept summary of care documents), a provider will earn 50 points.
Another 90 performance points are available for reporting certain information, and this is based on a decile system just like the quality category in which a rheumatologist’s performance is measured against other rheumatologists who have met the benchmark for each particular measure. These optional measures include providing patient-specific educational information; patients being able to view, download, and transmit their own medical records; secure messaging; acceptance of patient-generated health data; medication reconciliation; and submitting data to a state immunization registry.
Another 15 bonus points are available for additional public health reporting and reporting to CMS using a certified EHR or QCDR.
All these measures together give providers the potential to earn 155 points toward the 100-point threshold.
“If you’re already doing Meaningful Use, chances are you’re going to do really well in this area,” he said.
The advancing care information category will stay at 25% of the MIPS score in 2018.
Problems with current APMs
Under MACRA, participation in an APM means that the physician is exempt from MIPS and will receive a 5% lump sum bonus per year in 2019-2024, a higher annual increase in fee-for-service revenues, and the general benefits of participating in an APM. However, few rheumatologists will qualify for the APM pathway, and there are no rheumatology-specific APMs in existence.
Most current APMs are “shared savings” programs where if the physician or health system can reduce spending below the expected levels, then the provider receives a share of the payer’s savings. However, these shared-savings APMs all still use a fee-for-service structure, which makes them just a different form of pay for performance, according to Mr. Miller.
Physicians still don’t get paid for unfunded or underfunded services, and physicians who are already efficient receive little or no additional revenue and may be forced out of business, while physicians who have been practicing inefficiently or inappropriately are paid more than conservative physicians. There’s also the potential for rewarding the denial of needed care. Physicians in shared-savings APMs are also placed at risk for costs they cannot control and for random variations in spending. And most of all, the shared savings bonuses are temporary and when there are no more savings to be generated, physicians are underpaid, Mr. Miller said.
During 2013-2015, 46%-48% of Medicare shared-savings accountable care organizations (ACOs) increased their Medicare spending rather than reduced it, and only 24%-30% of the ACOs received shared-savings payments. In each year, Medicare spent more than it saved, with net losses ranging from $50 million to $216 million. This happened because physicians in the programs still got paid with fee-for-service payments, Mr. Miller said.
Creating rheumatology-focused APMs
MACRA designated the development of the Physician-Focused Payment Model Technical Advisory Committee, of which Mr. Miller is a member, to solicit and review physician-focused payment models and make recommendations to CMS about which ones to implement.
Physician-focused payment models got their start through pioneering work by physicians who obtained data from insurers to find ways to reach out proactively to patients to address problems before patients are hospitalized. Through these efforts, they have reduced cost and increased patient satisfaction while also increasing payment to physicians by supporting “medical home” services, according to Dr. Miller.
These efforts to create APMs that support high-quality, physician-directed care begin by identifying avoidable spending that varies from specialty to specialty and from condition to condition. Then they address barriers in the current fee-for-service system – such as no payment for many high-value services and insufficient revenue to cover costs when using fewer or low-cost services – by providing flexible, adequate payment while requiring physicians to take responsibility for the things they said could be avoidable when paid in that way. However, this responsibility must be focused on what a particular physician can influence, Mr. Miller noted.
Rheumatologists could be helped by these physician-focused payment models because they receive less than 10% of the total Medicare health care spending per patient whose care was directed by a rheumatologist. In that case, finding ways to drop total spending per patient by 5% could at the same time give rheumatologists a 25% increase in payment while also saving Medicare 3% overall, he said.
Rheumatologists are best set up to take condition-based payments that are geared to keep patients out of the hospital, rather than the hospital episode–based payments that have dominated APMs in existence so far. Central to this condition-based model is getting the right diagnosis at the start, so payment for getting the correct diagnosis would be critical.
APMs designed for rheumatologists could take into account the diseases often seen by a rheumatologist, such as RA, and then identify opportunities to improve care and reduce costs while identifying barriers in the current payment system for achieving those goals, Mr. Miller said. These opportunities and barriers would vary from condition to condition. In some cases, particularly for low-frequency conditions, there may not need to be a new payment model established and it could be done through fee-for-service.
Ideally, these condition-based payment models for specialists such as rheumatologists would exist within the “medical neighborhood” of primary care physicians who could refer to them when necessary. Specialists would be accountable for the aspects of care that they can control, such as avoiding unnecessary tests and procedures and avoiding infections and complications.
“That’s building the ACO from the bottom up, rather than what Medicare is trying to do, which is to create it from the top down,” Mr. Miller said.
Mr. Miller noted that it will be important for specialties such as rheumatology to define the cost data it needs in order to develop condition-based payment models.
Dr. Harvey had no relevant disclosures. Mr. Miller has no financial relationships with any commercial interests.
EXPERT ANALYSIS FROM THE ACR ANNUAL MEETING
Lack of natalizumab concentration increase before PML argues against extending dosing interval
Serum concentrations of natalizumab do not appear to rise before patients with relapsing-remitting multiple sclerosis are diagnosed with progressive multifocal leukoencephalopathy, contradicting the hypothesis that exposure to elevated concentrations of the drug is a risk factor for the disease, according to findings from a prospective, observational cohort study.
Zoé L.E. van Kempen, MD, and her colleagues at VU Medical Center Amsterdam noted that a small but increasing number of “neurologists are extending dose intervals of natalizumab [Tysabri] with the primary aim of reducing the risk of PML [progressive multifocal leukoencephalopathy] by lowering the natalizumab exposure per patient,” which also potentially has the benefit of decreasing drug costs, as well as clinic or hospital visits. However, there have been no prospective studies that confirm that extending natalizumab dose intervals does not affect efficacy.
Dr. van Kempen and her coinvestigators investigated this hypothesis by comparing serum concentrations of natalizumab in 5 patients with PML and 10 age- and sex-matched controls from a cohort of 219 relapsing-remitting multiple sclerosis patients taking natalizumab who had blood samples routinely drawn every 12 weeks before the infusion of natalizumab (Mult Scler. 2016 Dec 13. doi: 10.1177/1352458516684023). These 10 controls had a mean concentration of 23.8 mcg/mL, which was in the same range as the 18.9 mcg/mL level observed before the diagnosis of PML in the 5 cases from the cohort. The five cases also did not show a rise in concentration before the diagnosis of PML and did not have concentrations fluctuate more than 11 mcg/mL during treatment. The patients with PML received a mean of 43 infusions, whereas controls received an average of 106 infusions. A median number of 5 pre-PML samples underwent testing, compared with yearly concentration measurements in the 10 controls who had at least 7 years’ treatment duration.
The increased risk of PML that has been documented in other studies with more than 24 months of natalizumab treatment also was not explained in this study by a rise in serum concentration over long-term follow-up.
“Although this cohort is too small to draw definite conclusions, our results do not support the hypothesis of high serum concentrations as a risk factor for developing PML,” the investigators wrote.
“With our small cohort in mind and insufficient data on this subject so far, neurologists should be careful in extending dose intervals and not overstate a possible decrease in the risk of developing PML. Obviously, if neurologists choose to extend dosing intervals of natalizumab in [John Cunningham virus]–positive patients, these patients should still receive stringent PML monitoring according to current recommendations,” they advised.
The study received support from the Brain Foundation Netherlands. Five of the authors reported financial ties to various pharmaceutical companies that market MS drugs, including Biogen, which markets natalizumab.
Serum concentrations of natalizumab do not appear to rise before patients with relapsing-remitting multiple sclerosis are diagnosed with progressive multifocal leukoencephalopathy, contradicting the hypothesis that exposure to elevated concentrations of the drug is a risk factor for the disease, according to findings from a prospective, observational cohort study.
Zoé L.E. van Kempen, MD, and her colleagues at VU Medical Center Amsterdam noted that a small but increasing number of “neurologists are extending dose intervals of natalizumab [Tysabri] with the primary aim of reducing the risk of PML [progressive multifocal leukoencephalopathy] by lowering the natalizumab exposure per patient,” which also potentially has the benefit of decreasing drug costs, as well as clinic or hospital visits. However, there have been no prospective studies that confirm that extending natalizumab dose intervals does not affect efficacy.
Dr. van Kempen and her coinvestigators investigated this hypothesis by comparing serum concentrations of natalizumab in 5 patients with PML and 10 age- and sex-matched controls from a cohort of 219 relapsing-remitting multiple sclerosis patients taking natalizumab who had blood samples routinely drawn every 12 weeks before the infusion of natalizumab (Mult Scler. 2016 Dec 13. doi: 10.1177/1352458516684023). These 10 controls had a mean concentration of 23.8 mcg/mL, which was in the same range as the 18.9 mcg/mL level observed before the diagnosis of PML in the 5 cases from the cohort. The five cases also did not show a rise in concentration before the diagnosis of PML and did not have concentrations fluctuate more than 11 mcg/mL during treatment. The patients with PML received a mean of 43 infusions, whereas controls received an average of 106 infusions. A median number of 5 pre-PML samples underwent testing, compared with yearly concentration measurements in the 10 controls who had at least 7 years’ treatment duration.
The increased risk of PML that has been documented in other studies with more than 24 months of natalizumab treatment also was not explained in this study by a rise in serum concentration over long-term follow-up.
“Although this cohort is too small to draw definite conclusions, our results do not support the hypothesis of high serum concentrations as a risk factor for developing PML,” the investigators wrote.
“With our small cohort in mind and insufficient data on this subject so far, neurologists should be careful in extending dose intervals and not overstate a possible decrease in the risk of developing PML. Obviously, if neurologists choose to extend dosing intervals of natalizumab in [John Cunningham virus]–positive patients, these patients should still receive stringent PML monitoring according to current recommendations,” they advised.
The study received support from the Brain Foundation Netherlands. Five of the authors reported financial ties to various pharmaceutical companies that market MS drugs, including Biogen, which markets natalizumab.
Serum concentrations of natalizumab do not appear to rise before patients with relapsing-remitting multiple sclerosis are diagnosed with progressive multifocal leukoencephalopathy, contradicting the hypothesis that exposure to elevated concentrations of the drug is a risk factor for the disease, according to findings from a prospective, observational cohort study.
Zoé L.E. van Kempen, MD, and her colleagues at VU Medical Center Amsterdam noted that a small but increasing number of “neurologists are extending dose intervals of natalizumab [Tysabri] with the primary aim of reducing the risk of PML [progressive multifocal leukoencephalopathy] by lowering the natalizumab exposure per patient,” which also potentially has the benefit of decreasing drug costs, as well as clinic or hospital visits. However, there have been no prospective studies that confirm that extending natalizumab dose intervals does not affect efficacy.
Dr. van Kempen and her coinvestigators investigated this hypothesis by comparing serum concentrations of natalizumab in 5 patients with PML and 10 age- and sex-matched controls from a cohort of 219 relapsing-remitting multiple sclerosis patients taking natalizumab who had blood samples routinely drawn every 12 weeks before the infusion of natalizumab (Mult Scler. 2016 Dec 13. doi: 10.1177/1352458516684023). These 10 controls had a mean concentration of 23.8 mcg/mL, which was in the same range as the 18.9 mcg/mL level observed before the diagnosis of PML in the 5 cases from the cohort. The five cases also did not show a rise in concentration before the diagnosis of PML and did not have concentrations fluctuate more than 11 mcg/mL during treatment. The patients with PML received a mean of 43 infusions, whereas controls received an average of 106 infusions. A median number of 5 pre-PML samples underwent testing, compared with yearly concentration measurements in the 10 controls who had at least 7 years’ treatment duration.
The increased risk of PML that has been documented in other studies with more than 24 months of natalizumab treatment also was not explained in this study by a rise in serum concentration over long-term follow-up.
“Although this cohort is too small to draw definite conclusions, our results do not support the hypothesis of high serum concentrations as a risk factor for developing PML,” the investigators wrote.
“With our small cohort in mind and insufficient data on this subject so far, neurologists should be careful in extending dose intervals and not overstate a possible decrease in the risk of developing PML. Obviously, if neurologists choose to extend dosing intervals of natalizumab in [John Cunningham virus]–positive patients, these patients should still receive stringent PML monitoring according to current recommendations,” they advised.
The study received support from the Brain Foundation Netherlands. Five of the authors reported financial ties to various pharmaceutical companies that market MS drugs, including Biogen, which markets natalizumab.
FROM MULTIPLE SCLEROSIS JOURNAL
Key clinical point:
Major finding: A total of 10 control patients had a mean natalizumab serum concentration of 23.8 mcg/mL, which was in the same range as the 18.9 mcg/mL level observed in 5 patients before a diagnosis of PML.
Data source: A comparison of 5 patients with PML and 10 age- and sex-matched controls from a prospective cohort of 219 patients with relapsing-remitting MS who were treated with natalizumab at one center.
Disclosures: The study received support from the Brain Foundation Netherlands. Five of the authors reported financial ties to various pharmaceutical companies that market MS drugs, including Biogen, which markets natalizumab.