User login
Transient epileptic amnesia: Rare, treatable, and easy to miss
LOS ANGELES – Transient epileptic amnesia is a rare but a treatable memory condition that usually occurs in late life and can be mistaken for neurodegenerative disease among patients presenting to a neurology or memory clinic.
Transient epileptic amnesia (TEA) is thought to be a focal epilepsy whose major clinical feature is the presence of recurrent spells of anterograde or retrograde amnesia lasting under an hour. The spells tend to occur on waking from sleep.
At the annual meeting of the American Academy of Neurology, Vijay Ramanan, MD, PhD, of the Mayo Clinic in Rochester, Minn., presented a retrospective series of 31 TEA cases from a study attempting to characterize the disorder in more demographic, clinical, and neuroimaging detail than has been done in the literature to date.
The cases were seen over a 20-year period (1998-2017) at the Mayo Clinic. All had at least one EEG and at least one MRI result reviewed by a neuroradiologist. Half also underwent fluorodeoxyglucose (FDG)-positron emission tomography (PET). All cases were classed as TEA if they included recurrent amnesia and an epileptic trait (lip smacking, for example), recurrent amnesiac spells and memory complaints between spells, or memory complaints and an epileptic trait.
Of the 31 cases, two-thirds were male, and the mean age was 70. Neuropsychological testing found mild nonspecific abnormalities in 10 individuals and mild cognitive impairment in 2.
The investigators found 20 patients had abnormalities on EEG, usually in the temporal epileptogenic region. On MRI, abnormalities were found in only 6 patients.
FDG-PET, however, revealed focal abnormalities in 11 of the 16 cases that underwent scanning. “Most of them had focal areas of hypometabolism; none of those metabolic patterns fit those of known neurodegenerative disorders, and more rarely they were entirely normal,” Dr. Ramanan said during a presentation of his findings.
The results suggest that FDG-PET “may be a more useful tool than EEG” in distinguishing TEA from other disorders, he said. “I think the fascinating question going forward is whether TEA has an underlying biomarker and if there’s a neuroimaging biomarker for this. From these data, I think FDG-PET could be a very promising avenue for that,” he said.
In most of these cases where there was an abnormality detected on EEG, he noted that the patient “had multiple or prolonged EEGs, so it’s not always an easy thing to catch.”
Dr. Ramanan stressed that it’s important for clinicians “to have your antennae up for this diagnosis, particularly as these patients will come in with chronic memory trouble, because this is something we can fix.” In his study, all of the 22 individuals followed up after treatment with antiepileptic drugs, most commonly lamotrigine or levetiracetam, improved on follow-up.
Dr. Ramanan and his colleagues disclosed no conflicts of interest related to their findings.
SOURCE: Ramanan V et al. Neurology. 2018 Apr 90(15 Suppl.):P3.035.
LOS ANGELES – Transient epileptic amnesia is a rare but a treatable memory condition that usually occurs in late life and can be mistaken for neurodegenerative disease among patients presenting to a neurology or memory clinic.
Transient epileptic amnesia (TEA) is thought to be a focal epilepsy whose major clinical feature is the presence of recurrent spells of anterograde or retrograde amnesia lasting under an hour. The spells tend to occur on waking from sleep.
At the annual meeting of the American Academy of Neurology, Vijay Ramanan, MD, PhD, of the Mayo Clinic in Rochester, Minn., presented a retrospective series of 31 TEA cases from a study attempting to characterize the disorder in more demographic, clinical, and neuroimaging detail than has been done in the literature to date.
The cases were seen over a 20-year period (1998-2017) at the Mayo Clinic. All had at least one EEG and at least one MRI result reviewed by a neuroradiologist. Half also underwent fluorodeoxyglucose (FDG)-positron emission tomography (PET). All cases were classed as TEA if they included recurrent amnesia and an epileptic trait (lip smacking, for example), recurrent amnesiac spells and memory complaints between spells, or memory complaints and an epileptic trait.
Of the 31 cases, two-thirds were male, and the mean age was 70. Neuropsychological testing found mild nonspecific abnormalities in 10 individuals and mild cognitive impairment in 2.
The investigators found 20 patients had abnormalities on EEG, usually in the temporal epileptogenic region. On MRI, abnormalities were found in only 6 patients.
FDG-PET, however, revealed focal abnormalities in 11 of the 16 cases that underwent scanning. “Most of them had focal areas of hypometabolism; none of those metabolic patterns fit those of known neurodegenerative disorders, and more rarely they were entirely normal,” Dr. Ramanan said during a presentation of his findings.
The results suggest that FDG-PET “may be a more useful tool than EEG” in distinguishing TEA from other disorders, he said. “I think the fascinating question going forward is whether TEA has an underlying biomarker and if there’s a neuroimaging biomarker for this. From these data, I think FDG-PET could be a very promising avenue for that,” he said.
In most of these cases where there was an abnormality detected on EEG, he noted that the patient “had multiple or prolonged EEGs, so it’s not always an easy thing to catch.”
Dr. Ramanan stressed that it’s important for clinicians “to have your antennae up for this diagnosis, particularly as these patients will come in with chronic memory trouble, because this is something we can fix.” In his study, all of the 22 individuals followed up after treatment with antiepileptic drugs, most commonly lamotrigine or levetiracetam, improved on follow-up.
Dr. Ramanan and his colleagues disclosed no conflicts of interest related to their findings.
SOURCE: Ramanan V et al. Neurology. 2018 Apr 90(15 Suppl.):P3.035.
LOS ANGELES – Transient epileptic amnesia is a rare but a treatable memory condition that usually occurs in late life and can be mistaken for neurodegenerative disease among patients presenting to a neurology or memory clinic.
Transient epileptic amnesia (TEA) is thought to be a focal epilepsy whose major clinical feature is the presence of recurrent spells of anterograde or retrograde amnesia lasting under an hour. The spells tend to occur on waking from sleep.
At the annual meeting of the American Academy of Neurology, Vijay Ramanan, MD, PhD, of the Mayo Clinic in Rochester, Minn., presented a retrospective series of 31 TEA cases from a study attempting to characterize the disorder in more demographic, clinical, and neuroimaging detail than has been done in the literature to date.
The cases were seen over a 20-year period (1998-2017) at the Mayo Clinic. All had at least one EEG and at least one MRI result reviewed by a neuroradiologist. Half also underwent fluorodeoxyglucose (FDG)-positron emission tomography (PET). All cases were classed as TEA if they included recurrent amnesia and an epileptic trait (lip smacking, for example), recurrent amnesiac spells and memory complaints between spells, or memory complaints and an epileptic trait.
Of the 31 cases, two-thirds were male, and the mean age was 70. Neuropsychological testing found mild nonspecific abnormalities in 10 individuals and mild cognitive impairment in 2.
The investigators found 20 patients had abnormalities on EEG, usually in the temporal epileptogenic region. On MRI, abnormalities were found in only 6 patients.
FDG-PET, however, revealed focal abnormalities in 11 of the 16 cases that underwent scanning. “Most of them had focal areas of hypometabolism; none of those metabolic patterns fit those of known neurodegenerative disorders, and more rarely they were entirely normal,” Dr. Ramanan said during a presentation of his findings.
The results suggest that FDG-PET “may be a more useful tool than EEG” in distinguishing TEA from other disorders, he said. “I think the fascinating question going forward is whether TEA has an underlying biomarker and if there’s a neuroimaging biomarker for this. From these data, I think FDG-PET could be a very promising avenue for that,” he said.
In most of these cases where there was an abnormality detected on EEG, he noted that the patient “had multiple or prolonged EEGs, so it’s not always an easy thing to catch.”
Dr. Ramanan stressed that it’s important for clinicians “to have your antennae up for this diagnosis, particularly as these patients will come in with chronic memory trouble, because this is something we can fix.” In his study, all of the 22 individuals followed up after treatment with antiepileptic drugs, most commonly lamotrigine or levetiracetam, improved on follow-up.
Dr. Ramanan and his colleagues disclosed no conflicts of interest related to their findings.
SOURCE: Ramanan V et al. Neurology. 2018 Apr 90(15 Suppl.):P3.035.
Key clinical point:
Major finding: Brain FDG-PET revealed focal abnormalities in 69% of subjects with suspected TEA.
Study details: A retrospective analysis of 31 suspected TEA cases treated from 1998-2017 at one clinic.
Disclosures: Dr. Ramanan and his colleagues disclosed no conflicts of interest.
Source: Ramanan V et al. Neurology. 2018 Apr 90(15 Suppl.):P3.035.
Peripheral nerve stimulation can reduce tremor symptoms
LOS ANGELES – A noninvasive peripheral nerve stimulation device has been shown to reduce symptoms of hand tremor among people with essential tremor, offering a possible alternative to invasive treatments such as deep-brain stimulation.
The neuromodulation device is worn on the wrist and uses electrodes to stimulate the radial and median nerves at a frequency that interrupts tremor. It contains sensors that measure tremor and adjust stimulation accordingly.
In two small, randomized, controlled studies presented at the annual meeting of the at the American Academy of Neurology, investigator Rajesh Pahwa, MD, of the University of Kansas in Kansas City, said that treatment with the device significantly reduced tremor symptoms, compared with sham treatment.
On April 26, the device’s manufacturer, Cala Health, announced in a news release that the U.S. Food and Drug Administration had granted marketing clearance for the device, based on this evidence.
For the first study, conducted in-clinic, 77 patients were randomized to either treatment (n = 40) or sham stimulation (n = 37) of the tremor-dominant hand. Tremor was measured before and immediately after a single 40-minute session of stimulation, and patients were asked to perform tasks in accordance with the Essential Tremor Rating Assessment Scale or TETRAS, a severity measure.
Subjects in the intervention group had about a 65% improvement in their upper-limb TETRAS scores, compared with those receiving sham treatment (P less than .01) and in total TETRAS performance (P less than .05).
Subjects also were tested in-clinic with props simulating common daily tasks such as unlocking a door with a key, holding a cup of tea, picking up loose change, or dialing a phone. Patients in the treatment group self-reported greater ease with all of these tasks after treatment, compared with the sham-treated group. Differences for some tasks reached statistical significance.
For the second study, conducted for 4 weeks, 61 patients were randomized to at-home treatment sessions with the neuromodulator or sham treatment for 40 minutes at least twice daily. Those receiving treatment (n = 31) saw greater reduction in tremor measured by the devices’ built-in sensors, compared with those assigned sham treatment (n = 15) or no treatment (n = 15). Nearly all sessions completed resulted in a measurable reduction of tremor.
In an interview at AAN, Manish Gupta of Cala Health, the device manufacturer, said that further studies are underway to assess the durability of the treatment.
“What we seem to be looking at is an on-demand therapy that delivers a transient relief,” Mr. Gupta said, adding that the devices could be used by patients at times when their tremor is most bothersome, or in anticipation of a task – such as dressing oneself or eating – that a tremor would affect the ability to perform.
“One thing we’re learning from clinicians is that tremor is variable within the patient, and it’s variable across patients,” Mr. Gupta said. “The same patient may find that they have less tremor a certain day or at certain times of the day. We don’t think this would replace deep-brain stimulation, which is a constant treatment effect, but it could serve for some patients as a step before it.”
Cala Health, the manufacturer, sponsored the study. One coauthor is an employee of Cala Health.
SOURCE: Pahwa R et al. AAN 2018, Abstract P4.474.
LOS ANGELES – A noninvasive peripheral nerve stimulation device has been shown to reduce symptoms of hand tremor among people with essential tremor, offering a possible alternative to invasive treatments such as deep-brain stimulation.
The neuromodulation device is worn on the wrist and uses electrodes to stimulate the radial and median nerves at a frequency that interrupts tremor. It contains sensors that measure tremor and adjust stimulation accordingly.
In two small, randomized, controlled studies presented at the annual meeting of the at the American Academy of Neurology, investigator Rajesh Pahwa, MD, of the University of Kansas in Kansas City, said that treatment with the device significantly reduced tremor symptoms, compared with sham treatment.
On April 26, the device’s manufacturer, Cala Health, announced in a news release that the U.S. Food and Drug Administration had granted marketing clearance for the device, based on this evidence.
For the first study, conducted in-clinic, 77 patients were randomized to either treatment (n = 40) or sham stimulation (n = 37) of the tremor-dominant hand. Tremor was measured before and immediately after a single 40-minute session of stimulation, and patients were asked to perform tasks in accordance with the Essential Tremor Rating Assessment Scale or TETRAS, a severity measure.
Subjects in the intervention group had about a 65% improvement in their upper-limb TETRAS scores, compared with those receiving sham treatment (P less than .01) and in total TETRAS performance (P less than .05).
Subjects also were tested in-clinic with props simulating common daily tasks such as unlocking a door with a key, holding a cup of tea, picking up loose change, or dialing a phone. Patients in the treatment group self-reported greater ease with all of these tasks after treatment, compared with the sham-treated group. Differences for some tasks reached statistical significance.
For the second study, conducted for 4 weeks, 61 patients were randomized to at-home treatment sessions with the neuromodulator or sham treatment for 40 minutes at least twice daily. Those receiving treatment (n = 31) saw greater reduction in tremor measured by the devices’ built-in sensors, compared with those assigned sham treatment (n = 15) or no treatment (n = 15). Nearly all sessions completed resulted in a measurable reduction of tremor.
In an interview at AAN, Manish Gupta of Cala Health, the device manufacturer, said that further studies are underway to assess the durability of the treatment.
“What we seem to be looking at is an on-demand therapy that delivers a transient relief,” Mr. Gupta said, adding that the devices could be used by patients at times when their tremor is most bothersome, or in anticipation of a task – such as dressing oneself or eating – that a tremor would affect the ability to perform.
“One thing we’re learning from clinicians is that tremor is variable within the patient, and it’s variable across patients,” Mr. Gupta said. “The same patient may find that they have less tremor a certain day or at certain times of the day. We don’t think this would replace deep-brain stimulation, which is a constant treatment effect, but it could serve for some patients as a step before it.”
Cala Health, the manufacturer, sponsored the study. One coauthor is an employee of Cala Health.
SOURCE: Pahwa R et al. AAN 2018, Abstract P4.474.
LOS ANGELES – A noninvasive peripheral nerve stimulation device has been shown to reduce symptoms of hand tremor among people with essential tremor, offering a possible alternative to invasive treatments such as deep-brain stimulation.
The neuromodulation device is worn on the wrist and uses electrodes to stimulate the radial and median nerves at a frequency that interrupts tremor. It contains sensors that measure tremor and adjust stimulation accordingly.
In two small, randomized, controlled studies presented at the annual meeting of the at the American Academy of Neurology, investigator Rajesh Pahwa, MD, of the University of Kansas in Kansas City, said that treatment with the device significantly reduced tremor symptoms, compared with sham treatment.
On April 26, the device’s manufacturer, Cala Health, announced in a news release that the U.S. Food and Drug Administration had granted marketing clearance for the device, based on this evidence.
For the first study, conducted in-clinic, 77 patients were randomized to either treatment (n = 40) or sham stimulation (n = 37) of the tremor-dominant hand. Tremor was measured before and immediately after a single 40-minute session of stimulation, and patients were asked to perform tasks in accordance with the Essential Tremor Rating Assessment Scale or TETRAS, a severity measure.
Subjects in the intervention group had about a 65% improvement in their upper-limb TETRAS scores, compared with those receiving sham treatment (P less than .01) and in total TETRAS performance (P less than .05).
Subjects also were tested in-clinic with props simulating common daily tasks such as unlocking a door with a key, holding a cup of tea, picking up loose change, or dialing a phone. Patients in the treatment group self-reported greater ease with all of these tasks after treatment, compared with the sham-treated group. Differences for some tasks reached statistical significance.
For the second study, conducted for 4 weeks, 61 patients were randomized to at-home treatment sessions with the neuromodulator or sham treatment for 40 minutes at least twice daily. Those receiving treatment (n = 31) saw greater reduction in tremor measured by the devices’ built-in sensors, compared with those assigned sham treatment (n = 15) or no treatment (n = 15). Nearly all sessions completed resulted in a measurable reduction of tremor.
In an interview at AAN, Manish Gupta of Cala Health, the device manufacturer, said that further studies are underway to assess the durability of the treatment.
“What we seem to be looking at is an on-demand therapy that delivers a transient relief,” Mr. Gupta said, adding that the devices could be used by patients at times when their tremor is most bothersome, or in anticipation of a task – such as dressing oneself or eating – that a tremor would affect the ability to perform.
“One thing we’re learning from clinicians is that tremor is variable within the patient, and it’s variable across patients,” Mr. Gupta said. “The same patient may find that they have less tremor a certain day or at certain times of the day. We don’t think this would replace deep-brain stimulation, which is a constant treatment effect, but it could serve for some patients as a step before it.”
Cala Health, the manufacturer, sponsored the study. One coauthor is an employee of Cala Health.
SOURCE: Pahwa R et al. AAN 2018, Abstract P4.474.
REPORTING FROM AAN 2018
Key clinical point:
Major finding: Subjects using the devices saw improvement in their upper-limb tremor scores, compared with those receiving sham treatment (P less than .01)
Study details: Two randomized studies (n = 77 and n = 61) comparing in-home or in-office treatment with stimulation or sham treatment.
Disclosures: The device manufacturer sponsored the study. One employee is a coauthor.
Source: Pahwa R et al. AAN 2018, Abstract P4.474.
Cluster headache presents differently in never-smokers, survey finds
Los Angeles – Cluster headache, a severe, one-sided headache that occurs in cyclical patterns or clusters, is highly associated with smoking, but when it presents in people without any lifetime tobacco exposure, there are key differences – possibly due to a different underlying pathology.
At the American Academy of Neurology annual meeting, Todd D. Rozen, MD, of the Mayo Clinic in Jacksonville, Fla., presented a new analysis from the United States Cluster Headache Survey, an online survey of 1,134 patients with cluster headache, of whom only 12% reported neither personal tobacco use nor a parent who smoked. Dr. Rozen is a coauthor on the original survey, which collected data for a two-month period in late 2008, and has published several analyses using the survey’s data (Headache. 2012 Jan;52[1]:99-113).
Patients not exposed to tobacco developed cluster headache at a younger age than exposed subjects, with a significantly higher percentage reporting onset in their 20s and 30s, while tobacco-exposed people were more likely to see onset at aged 40 years or older.
And there were other important differences. The tobacco-naïve were more likely to have a family history of migraine (65% vs. 50%, P equal to .002). They were significantly more likely to have headache cycles that varied throughout the year rather than being concentrated during specific months or seasons (52% vs. 40%, P equal to .02), which is a hallmark of cluster headache.
Tobacco-exposed patients were more likely to transition from episodic to chronic cluster headaches (23% vs. 14%, P equal to .02) and to have cycles lasting 7 weeks or more (54% vs. 35%, P equal to .0003) compared with those who were tobacco-naïve. They also reported significantly more frequent attacks per day, and were more likely to develop cluster headache during the night (12 pm to 6 am).
“With cluster headache, the majority of patients smoke, and started smoking before they ever developed cluster headache,” Dr. Rozen said. Among the tobacco-exposed patients in the survey, 85% had what he described as a “double hit” – a parent who smoked and a personal history of smoking. “And that may be what’s necessary to develop cluster headache of this classic type,” he said.
Dr. Rozen said he suspects that tobacco-exposed people with cluster headache may have abnormal hypothalamic entrainment related to injury from toxins, though the exact mechanisms are unknown.
“So in times of hypothalamic stress – whether clock change or solstice, the hypothalamus has to work more, it doesn’t work correctly, and headache develops,” he said, noting the highly cyclical nature of the classic cluster phenotype.
As to what causes cluster headache in the non-exposed, Dr. Rozen said it’s possible that genetic factors may be more relevant – a possibility underscored by the higher rate of familial migraine reported among the tobacco-naïve in the cohort.
Dr. Rozen reported no financial conflicts of interest related to his findings.
SOURCE: Rozen TD, et al. AAN2018, P3 122.
Los Angeles – Cluster headache, a severe, one-sided headache that occurs in cyclical patterns or clusters, is highly associated with smoking, but when it presents in people without any lifetime tobacco exposure, there are key differences – possibly due to a different underlying pathology.
At the American Academy of Neurology annual meeting, Todd D. Rozen, MD, of the Mayo Clinic in Jacksonville, Fla., presented a new analysis from the United States Cluster Headache Survey, an online survey of 1,134 patients with cluster headache, of whom only 12% reported neither personal tobacco use nor a parent who smoked. Dr. Rozen is a coauthor on the original survey, which collected data for a two-month period in late 2008, and has published several analyses using the survey’s data (Headache. 2012 Jan;52[1]:99-113).
Patients not exposed to tobacco developed cluster headache at a younger age than exposed subjects, with a significantly higher percentage reporting onset in their 20s and 30s, while tobacco-exposed people were more likely to see onset at aged 40 years or older.
And there were other important differences. The tobacco-naïve were more likely to have a family history of migraine (65% vs. 50%, P equal to .002). They were significantly more likely to have headache cycles that varied throughout the year rather than being concentrated during specific months or seasons (52% vs. 40%, P equal to .02), which is a hallmark of cluster headache.
Tobacco-exposed patients were more likely to transition from episodic to chronic cluster headaches (23% vs. 14%, P equal to .02) and to have cycles lasting 7 weeks or more (54% vs. 35%, P equal to .0003) compared with those who were tobacco-naïve. They also reported significantly more frequent attacks per day, and were more likely to develop cluster headache during the night (12 pm to 6 am).
“With cluster headache, the majority of patients smoke, and started smoking before they ever developed cluster headache,” Dr. Rozen said. Among the tobacco-exposed patients in the survey, 85% had what he described as a “double hit” – a parent who smoked and a personal history of smoking. “And that may be what’s necessary to develop cluster headache of this classic type,” he said.
Dr. Rozen said he suspects that tobacco-exposed people with cluster headache may have abnormal hypothalamic entrainment related to injury from toxins, though the exact mechanisms are unknown.
“So in times of hypothalamic stress – whether clock change or solstice, the hypothalamus has to work more, it doesn’t work correctly, and headache develops,” he said, noting the highly cyclical nature of the classic cluster phenotype.
As to what causes cluster headache in the non-exposed, Dr. Rozen said it’s possible that genetic factors may be more relevant – a possibility underscored by the higher rate of familial migraine reported among the tobacco-naïve in the cohort.
Dr. Rozen reported no financial conflicts of interest related to his findings.
SOURCE: Rozen TD, et al. AAN2018, P3 122.
Los Angeles – Cluster headache, a severe, one-sided headache that occurs in cyclical patterns or clusters, is highly associated with smoking, but when it presents in people without any lifetime tobacco exposure, there are key differences – possibly due to a different underlying pathology.
At the American Academy of Neurology annual meeting, Todd D. Rozen, MD, of the Mayo Clinic in Jacksonville, Fla., presented a new analysis from the United States Cluster Headache Survey, an online survey of 1,134 patients with cluster headache, of whom only 12% reported neither personal tobacco use nor a parent who smoked. Dr. Rozen is a coauthor on the original survey, which collected data for a two-month period in late 2008, and has published several analyses using the survey’s data (Headache. 2012 Jan;52[1]:99-113).
Patients not exposed to tobacco developed cluster headache at a younger age than exposed subjects, with a significantly higher percentage reporting onset in their 20s and 30s, while tobacco-exposed people were more likely to see onset at aged 40 years or older.
And there were other important differences. The tobacco-naïve were more likely to have a family history of migraine (65% vs. 50%, P equal to .002). They were significantly more likely to have headache cycles that varied throughout the year rather than being concentrated during specific months or seasons (52% vs. 40%, P equal to .02), which is a hallmark of cluster headache.
Tobacco-exposed patients were more likely to transition from episodic to chronic cluster headaches (23% vs. 14%, P equal to .02) and to have cycles lasting 7 weeks or more (54% vs. 35%, P equal to .0003) compared with those who were tobacco-naïve. They also reported significantly more frequent attacks per day, and were more likely to develop cluster headache during the night (12 pm to 6 am).
“With cluster headache, the majority of patients smoke, and started smoking before they ever developed cluster headache,” Dr. Rozen said. Among the tobacco-exposed patients in the survey, 85% had what he described as a “double hit” – a parent who smoked and a personal history of smoking. “And that may be what’s necessary to develop cluster headache of this classic type,” he said.
Dr. Rozen said he suspects that tobacco-exposed people with cluster headache may have abnormal hypothalamic entrainment related to injury from toxins, though the exact mechanisms are unknown.
“So in times of hypothalamic stress – whether clock change or solstice, the hypothalamus has to work more, it doesn’t work correctly, and headache develops,” he said, noting the highly cyclical nature of the classic cluster phenotype.
As to what causes cluster headache in the non-exposed, Dr. Rozen said it’s possible that genetic factors may be more relevant – a possibility underscored by the higher rate of familial migraine reported among the tobacco-naïve in the cohort.
Dr. Rozen reported no financial conflicts of interest related to his findings.
SOURCE: Rozen TD, et al. AAN2018, P3 122.
REPORTING FROM AAN 2018
Key clinical point: Tobacco-naïve people with cluster headache have significant differences in symptomology compared with the tobacco-exposed
Major finding: Family history of migraine, earlier age of onset and episodic pattern were seen in non-tobacco exposed patients vs. smokers
Study details: Data came from more than 1,000 cluster headache patients surveyed in the U.S. Cluster Headache Survey.
Disclosures: The authors had no disclosures.
Source: Rozen TD, et al. AAN2018, P3 122.
VIDEO: Eptinezumab shows efficacy in episodic and chronic migraine trials
LOS ANGELES – New results from phase 3 randomized trials of the prophylactic migraine treatment eptinezumab show significant reductions in the number of monthly migraine headache days experienced by patients with chronic or frequent episodic migraines.
Eptinezumab, an experimental monoclonal antibody delivered by intravenous infusion, is one of several antimigraine agents in development that targets calcitonin gene-related peptide (CGRP), a key mediator of migraine.
At the annual meeting of the American Academy of Neurology, Richard Lipton, MD, of Albert Einstein College of Medicine in New York, presented results from PROMISE 2, a phase 3 randomized, placebo-controlled trial of eptinezumab in patients with chronic migraine, or 15 or more days with migraine per month.
The investigators randomized 1,072 patients to quarterly IV infusions of eptinezumab 100 or 300 mg or placebo.
The vast majority of patients in the study were women, (86%-90% across groups) with a mean age of about 40 years. Patients reported 11-12 years of chronic migraine and about 16 migraine days per month at baseline, Dr. Lipton told the conference, reflecting a high level of disability in the cohort.
The primary endpoint of the study was mean change in monthly migraine days from baseline through week 12. Dr. Lipton reported that the placebo group saw a 5.6-day reduction in migraine, while the 100-mg group saw a 7.7-day reduction, and patients receiving the 300-mg dose saw an 8.2-day reduction during the first 12 weeks after injection (P less than .0001 for both).
One-third of patients receiving the highest dose saw a 75% or greater reduction in monthly migraine days by week 12, “a relatively high bar” to meet, Dr. Lipton said. Some 61% of patients on the high dose saw a reduction of 50% or more in the same time period.
A unique secondary endpoint of the study was the proportion of patients who experienced migraine on day 1 after the initial dose. The treatment groups saw a 52% reduction 1 day after receiving the study drug, while the placebo group saw a 27% reduction in the expected prevalence of migraine in the cohort for any single day, and the decrease was sustained through day 28. The results suggest a rapid onset of action for eptinezumab, followed by a sustained benefit, Dr. Lipton said.
Also at AAN, Stephen D. Silberstein, MD, of Thomas Jefferson University in Philadelphia, presented new 12-month results from the PROMISE 1 trial, a randomized clinical trial to evaluate quarterly IV infusions of eptinezumab 30 mg, 100 mg, 300 mg, or placebo, in 888 patients with episodic migraines, defined as 14 or fewer days per month with migraine.
The researchers, who last year published 6-month results showing significant reductions in monthly migraine days associated with eptinezumab treatment over placebo, described further reductions from patients’ baseline frequency of migraines with longer duration of treatment.
After their third and fourth quarterly injections, 70.7% of eptinezumab-treated patients achieved a 50% reduction of monthly migraine days from baseline, compared with 58.7% for placebo, the investigators reported. These findings represent an 8.9% improvement over the reductions experienced during the first two quarterly doses of eptinezumab in this cohort.
More than half of patients in the treatment arms achieved on average a 75% reduction or greater of monthly migraine days from baseline, compared with 38.7% for placebo, a 12.8% improvement from the reductions experienced with the first two doses of eptinezumab.
Adverse effects seen in the trials were upper respiratory infection, nasopharyngitis, sinusitis, and nausea.
Both trials were sponsored by eptinezumab’s manufacturer, Alder. Dr. Lipton, Dr. Silberstein, and several of their coauthors disclosed support from Alder and other manufacturers, while some coauthors on the studies are employees of Alder.
SOURCE: Saper J et al. AAN 2018, Abstract S20.001 and Lipton R et al. AAN 2018, Clinical Trials Plenary Session Abstract.
LOS ANGELES – New results from phase 3 randomized trials of the prophylactic migraine treatment eptinezumab show significant reductions in the number of monthly migraine headache days experienced by patients with chronic or frequent episodic migraines.
Eptinezumab, an experimental monoclonal antibody delivered by intravenous infusion, is one of several antimigraine agents in development that targets calcitonin gene-related peptide (CGRP), a key mediator of migraine.
At the annual meeting of the American Academy of Neurology, Richard Lipton, MD, of Albert Einstein College of Medicine in New York, presented results from PROMISE 2, a phase 3 randomized, placebo-controlled trial of eptinezumab in patients with chronic migraine, or 15 or more days with migraine per month.
The investigators randomized 1,072 patients to quarterly IV infusions of eptinezumab 100 or 300 mg or placebo.
The vast majority of patients in the study were women, (86%-90% across groups) with a mean age of about 40 years. Patients reported 11-12 years of chronic migraine and about 16 migraine days per month at baseline, Dr. Lipton told the conference, reflecting a high level of disability in the cohort.
The primary endpoint of the study was mean change in monthly migraine days from baseline through week 12. Dr. Lipton reported that the placebo group saw a 5.6-day reduction in migraine, while the 100-mg group saw a 7.7-day reduction, and patients receiving the 300-mg dose saw an 8.2-day reduction during the first 12 weeks after injection (P less than .0001 for both).
One-third of patients receiving the highest dose saw a 75% or greater reduction in monthly migraine days by week 12, “a relatively high bar” to meet, Dr. Lipton said. Some 61% of patients on the high dose saw a reduction of 50% or more in the same time period.
A unique secondary endpoint of the study was the proportion of patients who experienced migraine on day 1 after the initial dose. The treatment groups saw a 52% reduction 1 day after receiving the study drug, while the placebo group saw a 27% reduction in the expected prevalence of migraine in the cohort for any single day, and the decrease was sustained through day 28. The results suggest a rapid onset of action for eptinezumab, followed by a sustained benefit, Dr. Lipton said.
Also at AAN, Stephen D. Silberstein, MD, of Thomas Jefferson University in Philadelphia, presented new 12-month results from the PROMISE 1 trial, a randomized clinical trial to evaluate quarterly IV infusions of eptinezumab 30 mg, 100 mg, 300 mg, or placebo, in 888 patients with episodic migraines, defined as 14 or fewer days per month with migraine.
The researchers, who last year published 6-month results showing significant reductions in monthly migraine days associated with eptinezumab treatment over placebo, described further reductions from patients’ baseline frequency of migraines with longer duration of treatment.
After their third and fourth quarterly injections, 70.7% of eptinezumab-treated patients achieved a 50% reduction of monthly migraine days from baseline, compared with 58.7% for placebo, the investigators reported. These findings represent an 8.9% improvement over the reductions experienced during the first two quarterly doses of eptinezumab in this cohort.
More than half of patients in the treatment arms achieved on average a 75% reduction or greater of monthly migraine days from baseline, compared with 38.7% for placebo, a 12.8% improvement from the reductions experienced with the first two doses of eptinezumab.
Adverse effects seen in the trials were upper respiratory infection, nasopharyngitis, sinusitis, and nausea.
Both trials were sponsored by eptinezumab’s manufacturer, Alder. Dr. Lipton, Dr. Silberstein, and several of their coauthors disclosed support from Alder and other manufacturers, while some coauthors on the studies are employees of Alder.
SOURCE: Saper J et al. AAN 2018, Abstract S20.001 and Lipton R et al. AAN 2018, Clinical Trials Plenary Session Abstract.
LOS ANGELES – New results from phase 3 randomized trials of the prophylactic migraine treatment eptinezumab show significant reductions in the number of monthly migraine headache days experienced by patients with chronic or frequent episodic migraines.
Eptinezumab, an experimental monoclonal antibody delivered by intravenous infusion, is one of several antimigraine agents in development that targets calcitonin gene-related peptide (CGRP), a key mediator of migraine.
At the annual meeting of the American Academy of Neurology, Richard Lipton, MD, of Albert Einstein College of Medicine in New York, presented results from PROMISE 2, a phase 3 randomized, placebo-controlled trial of eptinezumab in patients with chronic migraine, or 15 or more days with migraine per month.
The investigators randomized 1,072 patients to quarterly IV infusions of eptinezumab 100 or 300 mg or placebo.
The vast majority of patients in the study were women, (86%-90% across groups) with a mean age of about 40 years. Patients reported 11-12 years of chronic migraine and about 16 migraine days per month at baseline, Dr. Lipton told the conference, reflecting a high level of disability in the cohort.
The primary endpoint of the study was mean change in monthly migraine days from baseline through week 12. Dr. Lipton reported that the placebo group saw a 5.6-day reduction in migraine, while the 100-mg group saw a 7.7-day reduction, and patients receiving the 300-mg dose saw an 8.2-day reduction during the first 12 weeks after injection (P less than .0001 for both).
One-third of patients receiving the highest dose saw a 75% or greater reduction in monthly migraine days by week 12, “a relatively high bar” to meet, Dr. Lipton said. Some 61% of patients on the high dose saw a reduction of 50% or more in the same time period.
A unique secondary endpoint of the study was the proportion of patients who experienced migraine on day 1 after the initial dose. The treatment groups saw a 52% reduction 1 day after receiving the study drug, while the placebo group saw a 27% reduction in the expected prevalence of migraine in the cohort for any single day, and the decrease was sustained through day 28. The results suggest a rapid onset of action for eptinezumab, followed by a sustained benefit, Dr. Lipton said.
Also at AAN, Stephen D. Silberstein, MD, of Thomas Jefferson University in Philadelphia, presented new 12-month results from the PROMISE 1 trial, a randomized clinical trial to evaluate quarterly IV infusions of eptinezumab 30 mg, 100 mg, 300 mg, or placebo, in 888 patients with episodic migraines, defined as 14 or fewer days per month with migraine.
The researchers, who last year published 6-month results showing significant reductions in monthly migraine days associated with eptinezumab treatment over placebo, described further reductions from patients’ baseline frequency of migraines with longer duration of treatment.
After their third and fourth quarterly injections, 70.7% of eptinezumab-treated patients achieved a 50% reduction of monthly migraine days from baseline, compared with 58.7% for placebo, the investigators reported. These findings represent an 8.9% improvement over the reductions experienced during the first two quarterly doses of eptinezumab in this cohort.
More than half of patients in the treatment arms achieved on average a 75% reduction or greater of monthly migraine days from baseline, compared with 38.7% for placebo, a 12.8% improvement from the reductions experienced with the first two doses of eptinezumab.
Adverse effects seen in the trials were upper respiratory infection, nasopharyngitis, sinusitis, and nausea.
Both trials were sponsored by eptinezumab’s manufacturer, Alder. Dr. Lipton, Dr. Silberstein, and several of their coauthors disclosed support from Alder and other manufacturers, while some coauthors on the studies are employees of Alder.
SOURCE: Saper J et al. AAN 2018, Abstract S20.001 and Lipton R et al. AAN 2018, Clinical Trials Plenary Session Abstract.
REPORTING FROM AAN 2018
Endometriosis pain stemming from pelvic spasms improved with botulinum toxin
LOS ANGELES – Women treated surgically and with hormones for endometriosis may continue to experience pain, say investigators, and that pain frequently extends beyond the pelvis.
At the annual meeting of the American Academy of Neurology, Barbara Karp, MD, of the National Institute of Neurological Disorders and Stroke, presented results from an ongoing randomized trial of women with endometriosis receiving botulinum toxin to treat endometriosis-related chronic pelvic pain and pelvic spasm.
All 28 women currently enrolled in the trial (median age, 29 years) were evaluated by a gynecologist to confirm pelvic muscle spasm as their primary source of pain. Each also underwent a neuromuscular examination to identify pain points beyond the pelvis.
All subjects had myofascial dysfunction. Most reported headaches and half reported orofacial pain, while 13 subjects reported myofascial trigger points in all the 26 spots assessed, which included head and facial muscles, shoulder and back muscles, and muscles in the buttocks, abdomen, and upper legs.
Dr. Karp said her group hypothesized that for patients with endometriosis, the widespread pain seen in the study “probably has some origin in sensitization initiated by pain associated with the endometriosis lesions, and that gives us a mechanism to think about peripheral and central sensitization.” But she noted that such sensitization can be easily missed in the clinic.
“One of the things that’s really underappreciated is how much women with chronic pelvic pain have pain elsewhere. So the neurologist or pain specialist may say, ‘that’s not my body territory, there’s something going on with your pelvis.’ And the gynecologist may be focused on the endometriosis and the endometriosis lesions. So you have these women with really widespread pain problems whose care is being fractionated.”
In another aspect of the study she also presented at the meeting, Dr. Karp, a neurologist who has studied the therapeutic use of neurotoxins such as botulinum for 30 years, showed results from an open-label extension of a randomized trial of botulinum toxin injections to treat pelvic spasm in the same cohort of women with confirmed endometriosis and confirmed pelvic muscle spasm.
A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001), Dr. Karp and her colleagues reported. Between 5 and 11 months post injection, five women requested a repeat of the treatment.
Besides the data on pain and disability collected as part of the trial, Dr. Karp and her colleagues are also looking at biomarkers for pain and inflammation, and changes in medication and hormone use. They are preparing a separate literature review on injection techniques and dosages of toxin to the pelvic floor muscles.
“It’s an area of the body neurologists don’t feel comfortable injecting, and I don’t necessarily feel comfortable doing it myself,” Dr. Karp said.
The researchers had to develop their own procedure because at the time they started the research there was almost nothing in the literature on how to inject botulinum toxin for pelvic pain in women. “People in different specialties have been doing it [to relieve pelvic pain] and it’s really widespread, but they’re doing it all different ways,” Dr. Karp said. “We’re hoping to find a best approach.”
Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
SOURCE: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
LOS ANGELES – Women treated surgically and with hormones for endometriosis may continue to experience pain, say investigators, and that pain frequently extends beyond the pelvis.
At the annual meeting of the American Academy of Neurology, Barbara Karp, MD, of the National Institute of Neurological Disorders and Stroke, presented results from an ongoing randomized trial of women with endometriosis receiving botulinum toxin to treat endometriosis-related chronic pelvic pain and pelvic spasm.
All 28 women currently enrolled in the trial (median age, 29 years) were evaluated by a gynecologist to confirm pelvic muscle spasm as their primary source of pain. Each also underwent a neuromuscular examination to identify pain points beyond the pelvis.
All subjects had myofascial dysfunction. Most reported headaches and half reported orofacial pain, while 13 subjects reported myofascial trigger points in all the 26 spots assessed, which included head and facial muscles, shoulder and back muscles, and muscles in the buttocks, abdomen, and upper legs.
Dr. Karp said her group hypothesized that for patients with endometriosis, the widespread pain seen in the study “probably has some origin in sensitization initiated by pain associated with the endometriosis lesions, and that gives us a mechanism to think about peripheral and central sensitization.” But she noted that such sensitization can be easily missed in the clinic.
“One of the things that’s really underappreciated is how much women with chronic pelvic pain have pain elsewhere. So the neurologist or pain specialist may say, ‘that’s not my body territory, there’s something going on with your pelvis.’ And the gynecologist may be focused on the endometriosis and the endometriosis lesions. So you have these women with really widespread pain problems whose care is being fractionated.”
In another aspect of the study she also presented at the meeting, Dr. Karp, a neurologist who has studied the therapeutic use of neurotoxins such as botulinum for 30 years, showed results from an open-label extension of a randomized trial of botulinum toxin injections to treat pelvic spasm in the same cohort of women with confirmed endometriosis and confirmed pelvic muscle spasm.
A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001), Dr. Karp and her colleagues reported. Between 5 and 11 months post injection, five women requested a repeat of the treatment.
Besides the data on pain and disability collected as part of the trial, Dr. Karp and her colleagues are also looking at biomarkers for pain and inflammation, and changes in medication and hormone use. They are preparing a separate literature review on injection techniques and dosages of toxin to the pelvic floor muscles.
“It’s an area of the body neurologists don’t feel comfortable injecting, and I don’t necessarily feel comfortable doing it myself,” Dr. Karp said.
The researchers had to develop their own procedure because at the time they started the research there was almost nothing in the literature on how to inject botulinum toxin for pelvic pain in women. “People in different specialties have been doing it [to relieve pelvic pain] and it’s really widespread, but they’re doing it all different ways,” Dr. Karp said. “We’re hoping to find a best approach.”
Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
SOURCE: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
LOS ANGELES – Women treated surgically and with hormones for endometriosis may continue to experience pain, say investigators, and that pain frequently extends beyond the pelvis.
At the annual meeting of the American Academy of Neurology, Barbara Karp, MD, of the National Institute of Neurological Disorders and Stroke, presented results from an ongoing randomized trial of women with endometriosis receiving botulinum toxin to treat endometriosis-related chronic pelvic pain and pelvic spasm.
All 28 women currently enrolled in the trial (median age, 29 years) were evaluated by a gynecologist to confirm pelvic muscle spasm as their primary source of pain. Each also underwent a neuromuscular examination to identify pain points beyond the pelvis.
All subjects had myofascial dysfunction. Most reported headaches and half reported orofacial pain, while 13 subjects reported myofascial trigger points in all the 26 spots assessed, which included head and facial muscles, shoulder and back muscles, and muscles in the buttocks, abdomen, and upper legs.
Dr. Karp said her group hypothesized that for patients with endometriosis, the widespread pain seen in the study “probably has some origin in sensitization initiated by pain associated with the endometriosis lesions, and that gives us a mechanism to think about peripheral and central sensitization.” But she noted that such sensitization can be easily missed in the clinic.
“One of the things that’s really underappreciated is how much women with chronic pelvic pain have pain elsewhere. So the neurologist or pain specialist may say, ‘that’s not my body territory, there’s something going on with your pelvis.’ And the gynecologist may be focused on the endometriosis and the endometriosis lesions. So you have these women with really widespread pain problems whose care is being fractionated.”
In another aspect of the study she also presented at the meeting, Dr. Karp, a neurologist who has studied the therapeutic use of neurotoxins such as botulinum for 30 years, showed results from an open-label extension of a randomized trial of botulinum toxin injections to treat pelvic spasm in the same cohort of women with confirmed endometriosis and confirmed pelvic muscle spasm.
A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001), Dr. Karp and her colleagues reported. Between 5 and 11 months post injection, five women requested a repeat of the treatment.
Besides the data on pain and disability collected as part of the trial, Dr. Karp and her colleagues are also looking at biomarkers for pain and inflammation, and changes in medication and hormone use. They are preparing a separate literature review on injection techniques and dosages of toxin to the pelvic floor muscles.
“It’s an area of the body neurologists don’t feel comfortable injecting, and I don’t necessarily feel comfortable doing it myself,” Dr. Karp said.
The researchers had to develop their own procedure because at the time they started the research there was almost nothing in the literature on how to inject botulinum toxin for pelvic pain in women. “People in different specialties have been doing it [to relieve pelvic pain] and it’s really widespread, but they’re doing it all different ways,” Dr. Karp said. “We’re hoping to find a best approach.”
Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
SOURCE: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
REPORTING FROM AAN 2018
Key clinical point:
Major finding: A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001).
Study details: An open-label extension in 13 of 28 patients enrolled in a randomized trial.
Disclosures: Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
Source: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
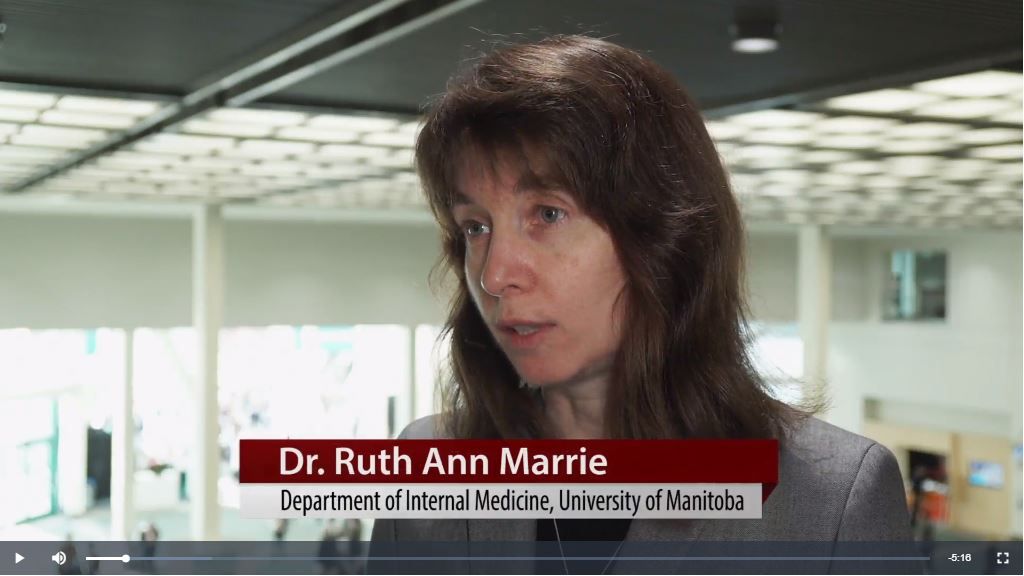
VIDEO: AAN MS guidelines aim to help clinicians weigh expanding drug choices
LOS ANGELES – A new clinical guideline for adults with multiple sclerosis is designed to help clinicians navigate an increasingly complex landscape of treatment options, its authors say.
The new American Academy of Neurology (AAN) guideline includes some 30 recommendations related to starting a disease-modifying therapy (DMT), switching therapies, or stopping treatment. The guideline, presented April 23 at the AAN annual meeting and published online simultaneously in Neurology, is the first full MS practice guideline issued by AAN since 2002, when only a handful of medications were licensed for use in MS.
The new guideline does not present a hierarchy of DMTs to start but instead weighs evidence for 21 medications or formulations, including 8 used off label, with the idea that clinicians will tailor their choices by considering patient needs, preferences, potential adverse affects, cost of medicines, comorbidities (including depression), and likelihood of adherence, among other factors addressed.
“It’s a dramatically different landscape of the choices clinicians have,” guideline lead author Alexander Rae-Grant, MD, of the Cleveland Clinic, said at a press conference announcing the guideline.
The guideline encourages clinicians and patients “to have a detailed discussion of the risks and benefits of different therapies,” guideline coauthor Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, said at the press conference. “You need to have that informed ... discussion to share decision making – the guideline provides information for each provider-patient dyad to make decisions specific to that patient.”
The guideline incorporates findings from nearly 50 randomized trials, although few of these were head-to-head comparisons of therapies. The authors graded evidence for each DMT as compared with placebo or other DMTs in lowering relapse rate, taking into consideration study design and size. The guideline reflects changes to diagnostic criteria made in 2010, and a classification scheme issued in 2014 for MS subtypes, both of which have complicated the extension of clinical trial findings to some patient groups. It stresses early treatment, recommending that clinicians start DMTs in people with a single clinical demyelinating event and two or more brain lesions characteristic of MS.
Several drugs used off label in MS, including azathioprine and cladribine, were included in the evidence review, with cladribine described as a cost-effective option for patients without the resources to obtain approved agents.
Patients with a new diagnosis of MS should be counseled on starting DMTs not at the time of diagnosis but in a dedicated follow-up visit, the guideline says. Dr. Rae-Grant said that there’s a reasonable amount of “literature to suggest that at the time of diagnosis, what people hear after diagnosis is zero – and that deciding what medication to use is such a weighty decision, we did feel it was important to do that at a different time.”
Dr. Marrie said the AAN guideline “shares some strong similarities” with guidelines released in 2017 by the European Academy of Neurology, including recommendations for early initiation of therapy, for maintaining therapies, and for switching DMTs in individuals not responding or who have breakthrough relapses or changes on MRI.
Dr. Marrie disclosed no conflicts of interest related to her work on the guidelines. Dr. Rae-Grant disclosed income from textbooks on neurology and MS, and no other financial conflicts of interest.
SOURCE: Rae-Grant A et al. Neurology. 2018;90:777-88.
LOS ANGELES – A new clinical guideline for adults with multiple sclerosis is designed to help clinicians navigate an increasingly complex landscape of treatment options, its authors say.
The new American Academy of Neurology (AAN) guideline includes some 30 recommendations related to starting a disease-modifying therapy (DMT), switching therapies, or stopping treatment. The guideline, presented April 23 at the AAN annual meeting and published online simultaneously in Neurology, is the first full MS practice guideline issued by AAN since 2002, when only a handful of medications were licensed for use in MS.
The new guideline does not present a hierarchy of DMTs to start but instead weighs evidence for 21 medications or formulations, including 8 used off label, with the idea that clinicians will tailor their choices by considering patient needs, preferences, potential adverse affects, cost of medicines, comorbidities (including depression), and likelihood of adherence, among other factors addressed.
“It’s a dramatically different landscape of the choices clinicians have,” guideline lead author Alexander Rae-Grant, MD, of the Cleveland Clinic, said at a press conference announcing the guideline.
The guideline encourages clinicians and patients “to have a detailed discussion of the risks and benefits of different therapies,” guideline coauthor Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, said at the press conference. “You need to have that informed ... discussion to share decision making – the guideline provides information for each provider-patient dyad to make decisions specific to that patient.”
The guideline incorporates findings from nearly 50 randomized trials, although few of these were head-to-head comparisons of therapies. The authors graded evidence for each DMT as compared with placebo or other DMTs in lowering relapse rate, taking into consideration study design and size. The guideline reflects changes to diagnostic criteria made in 2010, and a classification scheme issued in 2014 for MS subtypes, both of which have complicated the extension of clinical trial findings to some patient groups. It stresses early treatment, recommending that clinicians start DMTs in people with a single clinical demyelinating event and two or more brain lesions characteristic of MS.
Several drugs used off label in MS, including azathioprine and cladribine, were included in the evidence review, with cladribine described as a cost-effective option for patients without the resources to obtain approved agents.
Patients with a new diagnosis of MS should be counseled on starting DMTs not at the time of diagnosis but in a dedicated follow-up visit, the guideline says. Dr. Rae-Grant said that there’s a reasonable amount of “literature to suggest that at the time of diagnosis, what people hear after diagnosis is zero – and that deciding what medication to use is such a weighty decision, we did feel it was important to do that at a different time.”
Dr. Marrie said the AAN guideline “shares some strong similarities” with guidelines released in 2017 by the European Academy of Neurology, including recommendations for early initiation of therapy, for maintaining therapies, and for switching DMTs in individuals not responding or who have breakthrough relapses or changes on MRI.
Dr. Marrie disclosed no conflicts of interest related to her work on the guidelines. Dr. Rae-Grant disclosed income from textbooks on neurology and MS, and no other financial conflicts of interest.
SOURCE: Rae-Grant A et al. Neurology. 2018;90:777-88.
LOS ANGELES – A new clinical guideline for adults with multiple sclerosis is designed to help clinicians navigate an increasingly complex landscape of treatment options, its authors say.
The new American Academy of Neurology (AAN) guideline includes some 30 recommendations related to starting a disease-modifying therapy (DMT), switching therapies, or stopping treatment. The guideline, presented April 23 at the AAN annual meeting and published online simultaneously in Neurology, is the first full MS practice guideline issued by AAN since 2002, when only a handful of medications were licensed for use in MS.
The new guideline does not present a hierarchy of DMTs to start but instead weighs evidence for 21 medications or formulations, including 8 used off label, with the idea that clinicians will tailor their choices by considering patient needs, preferences, potential adverse affects, cost of medicines, comorbidities (including depression), and likelihood of adherence, among other factors addressed.
“It’s a dramatically different landscape of the choices clinicians have,” guideline lead author Alexander Rae-Grant, MD, of the Cleveland Clinic, said at a press conference announcing the guideline.
The guideline encourages clinicians and patients “to have a detailed discussion of the risks and benefits of different therapies,” guideline coauthor Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, said at the press conference. “You need to have that informed ... discussion to share decision making – the guideline provides information for each provider-patient dyad to make decisions specific to that patient.”
The guideline incorporates findings from nearly 50 randomized trials, although few of these were head-to-head comparisons of therapies. The authors graded evidence for each DMT as compared with placebo or other DMTs in lowering relapse rate, taking into consideration study design and size. The guideline reflects changes to diagnostic criteria made in 2010, and a classification scheme issued in 2014 for MS subtypes, both of which have complicated the extension of clinical trial findings to some patient groups. It stresses early treatment, recommending that clinicians start DMTs in people with a single clinical demyelinating event and two or more brain lesions characteristic of MS.
Several drugs used off label in MS, including azathioprine and cladribine, were included in the evidence review, with cladribine described as a cost-effective option for patients without the resources to obtain approved agents.
Patients with a new diagnosis of MS should be counseled on starting DMTs not at the time of diagnosis but in a dedicated follow-up visit, the guideline says. Dr. Rae-Grant said that there’s a reasonable amount of “literature to suggest that at the time of diagnosis, what people hear after diagnosis is zero – and that deciding what medication to use is such a weighty decision, we did feel it was important to do that at a different time.”
Dr. Marrie said the AAN guideline “shares some strong similarities” with guidelines released in 2017 by the European Academy of Neurology, including recommendations for early initiation of therapy, for maintaining therapies, and for switching DMTs in individuals not responding or who have breakthrough relapses or changes on MRI.
Dr. Marrie disclosed no conflicts of interest related to her work on the guidelines. Dr. Rae-Grant disclosed income from textbooks on neurology and MS, and no other financial conflicts of interest.
SOURCE: Rae-Grant A et al. Neurology. 2018;90:777-88.
REPORTING FROM AAN 2018
VIDEO: Encouraging results reported for novel Huntington’s disease therapy
LOS ANGELES – Results from the first-in-human trial of the investigational antisense oligonucleotide therapy IONIS-HTTRx showed strong dose-dependent reductions in the toxic huntingtin protein in Huntington’s disease patients’ cerebrospinal fluid when compared with placebo.
An exploratory analysis also showed signals of clinical improvement among patients receiving the therapy, the study’s lead author, Sarah Tabrizi, MD, PhD, of University College London, reported at the annual meeting of the American Academy of Neurology.
The findings represent a potential breakthrough in the way Huntington’s – and possibly other neurodegenerative diseases – are treated, said Dr. Tabrizi of University College London. The intrathecally-delivered drug binds to mutant huntingtin protein mRNA to reduce the level of the toxic protein being made.
In the phase 1/2a trial, Dr. Tabrizi and her colleagues enrolled 46 patients with early-stage Huntington’s disease and randomized them to four doses of IONIS-HTTRx or placebo. Patients received four monthly injections of the study drug into the cerebrospinal fluid followed by a 4-month untreated follow-up period. IONIS-HTTRx was delivered in five ascending-dose cohorts.
IONIS-HTTRx was safe and well tolerated and all patients completed the study, Dr. Tabrizi reported. “Our results show that we had significant lowering of the toxic mutant huntingtin protein in the spinal fluid of the patients,” she said, noting that patients receiving the highest doses saw 40%-60% lowering of the protein, which preclinical work suggests correlates to reductions of the protein in the brain.
Dr. Tabrizi stressed that the main outcome measures in the study were reduction of the mutant protein in the CSF and safety and tolerance of the study drug. The investigators did not expect to see clinical measures to change in such a short, small study, she said.
“But then when we looked more carefully at the data with exploratory analysis we found a link between lowering of CSF mutant huntingtin and improvement in total motor score, which is a measure of neurological function, and also, improvement in the Symbol Digit Modalities Test.”
The clinical results are exploratory and require confirmation in larger studies, Dr. Tabrizi stressed.
The study was supported by Ionis Pharmaceuticals. Roche will develop the drug in further clinical trials.
SOURCE: Tabrizi S et al. AAN 2018 abstract CT.002.
LOS ANGELES – Results from the first-in-human trial of the investigational antisense oligonucleotide therapy IONIS-HTTRx showed strong dose-dependent reductions in the toxic huntingtin protein in Huntington’s disease patients’ cerebrospinal fluid when compared with placebo.
An exploratory analysis also showed signals of clinical improvement among patients receiving the therapy, the study’s lead author, Sarah Tabrizi, MD, PhD, of University College London, reported at the annual meeting of the American Academy of Neurology.
The findings represent a potential breakthrough in the way Huntington’s – and possibly other neurodegenerative diseases – are treated, said Dr. Tabrizi of University College London. The intrathecally-delivered drug binds to mutant huntingtin protein mRNA to reduce the level of the toxic protein being made.
In the phase 1/2a trial, Dr. Tabrizi and her colleagues enrolled 46 patients with early-stage Huntington’s disease and randomized them to four doses of IONIS-HTTRx or placebo. Patients received four monthly injections of the study drug into the cerebrospinal fluid followed by a 4-month untreated follow-up period. IONIS-HTTRx was delivered in five ascending-dose cohorts.
IONIS-HTTRx was safe and well tolerated and all patients completed the study, Dr. Tabrizi reported. “Our results show that we had significant lowering of the toxic mutant huntingtin protein in the spinal fluid of the patients,” she said, noting that patients receiving the highest doses saw 40%-60% lowering of the protein, which preclinical work suggests correlates to reductions of the protein in the brain.
Dr. Tabrizi stressed that the main outcome measures in the study were reduction of the mutant protein in the CSF and safety and tolerance of the study drug. The investigators did not expect to see clinical measures to change in such a short, small study, she said.
“But then when we looked more carefully at the data with exploratory analysis we found a link between lowering of CSF mutant huntingtin and improvement in total motor score, which is a measure of neurological function, and also, improvement in the Symbol Digit Modalities Test.”
The clinical results are exploratory and require confirmation in larger studies, Dr. Tabrizi stressed.
The study was supported by Ionis Pharmaceuticals. Roche will develop the drug in further clinical trials.
SOURCE: Tabrizi S et al. AAN 2018 abstract CT.002.
LOS ANGELES – Results from the first-in-human trial of the investigational antisense oligonucleotide therapy IONIS-HTTRx showed strong dose-dependent reductions in the toxic huntingtin protein in Huntington’s disease patients’ cerebrospinal fluid when compared with placebo.
An exploratory analysis also showed signals of clinical improvement among patients receiving the therapy, the study’s lead author, Sarah Tabrizi, MD, PhD, of University College London, reported at the annual meeting of the American Academy of Neurology.
The findings represent a potential breakthrough in the way Huntington’s – and possibly other neurodegenerative diseases – are treated, said Dr. Tabrizi of University College London. The intrathecally-delivered drug binds to mutant huntingtin protein mRNA to reduce the level of the toxic protein being made.
In the phase 1/2a trial, Dr. Tabrizi and her colleagues enrolled 46 patients with early-stage Huntington’s disease and randomized them to four doses of IONIS-HTTRx or placebo. Patients received four monthly injections of the study drug into the cerebrospinal fluid followed by a 4-month untreated follow-up period. IONIS-HTTRx was delivered in five ascending-dose cohorts.
IONIS-HTTRx was safe and well tolerated and all patients completed the study, Dr. Tabrizi reported. “Our results show that we had significant lowering of the toxic mutant huntingtin protein in the spinal fluid of the patients,” she said, noting that patients receiving the highest doses saw 40%-60% lowering of the protein, which preclinical work suggests correlates to reductions of the protein in the brain.
Dr. Tabrizi stressed that the main outcome measures in the study were reduction of the mutant protein in the CSF and safety and tolerance of the study drug. The investigators did not expect to see clinical measures to change in such a short, small study, she said.
“But then when we looked more carefully at the data with exploratory analysis we found a link between lowering of CSF mutant huntingtin and improvement in total motor score, which is a measure of neurological function, and also, improvement in the Symbol Digit Modalities Test.”
The clinical results are exploratory and require confirmation in larger studies, Dr. Tabrizi stressed.
The study was supported by Ionis Pharmaceuticals. Roche will develop the drug in further clinical trials.
SOURCE: Tabrizi S et al. AAN 2018 abstract CT.002.
REPORTING FROM AAN 2018
VIDEO: Ubrogepant reduced pain, related symptoms of a migraine attack
LOS ANGELES – The investigational oral calcitonin gene-related peptide (CGRP) blocker ubrogepant proved superior to placebo in treating a single, acute, moderate to severe migraine attack in the phase 3 ACHIEVE I trial.
Blocking the function of CGRP when it is pathologically released during a migraine attack is the mechanism of a bevy of antagonists under development for treating migraine, and the ACHIEVE I trial results are the first to be reported from a phase 3 trial of an oral small molecule to treat single migraine attacks rather than prevent attacks with monoclonal antibodies targeting CGRP or its receptor, according to the lead author of ACHIEVE I, Joel M. Trugman, MD, director of clinical development for Allergan.
Dr. Trugman and his colleagues recruited 1,672 adult patients (88% female, mean age 41) with a history of migraine with or without aura, and randomized them to placebo, ubrogepant 50 mg, or ubrogepant 100 mg. Patients were instructed to treat a single migraine attack of moderate to severe pain intensity and record symptoms, such as pain, light sensitivity, and sound sensitivity, before and after taking the medication.
“The paradigm for this type of trial is to treat a single, well characterized migraine attack in a large population of patients,” Dr. Trugman said in a press conference at the annual meeting of the American Academy of Neurology.
At 2 hours after dosing, the percentage of ubrogepant-treated patients achieving freedom from pain was significantly greater than the percentage of those treated with placebo (50 mg: 19.2%, P = .0023; 100 mg: 21.2%, P = .0003; placebo: 11.8%).
The percentage of ubrogepant-treated patients achieving absence of their most bothersome symptom was also significantly greater than that of placebo (50 mg: 38.6%, P = .0023; 100 mg: 37.7%, P = .0023; placebo: 27.8%).
Adverse events in the ubrogepant groups were similar to those of placebo, the most reported to be nausea, somnolence, and dry mouth.
Several authors are employees of Allergan, which sponsored the study.
SOURCE: Trugman J et al. AAN 2018 emerging science abstract 008.
LOS ANGELES – The investigational oral calcitonin gene-related peptide (CGRP) blocker ubrogepant proved superior to placebo in treating a single, acute, moderate to severe migraine attack in the phase 3 ACHIEVE I trial.
Blocking the function of CGRP when it is pathologically released during a migraine attack is the mechanism of a bevy of antagonists under development for treating migraine, and the ACHIEVE I trial results are the first to be reported from a phase 3 trial of an oral small molecule to treat single migraine attacks rather than prevent attacks with monoclonal antibodies targeting CGRP or its receptor, according to the lead author of ACHIEVE I, Joel M. Trugman, MD, director of clinical development for Allergan.
Dr. Trugman and his colleagues recruited 1,672 adult patients (88% female, mean age 41) with a history of migraine with or without aura, and randomized them to placebo, ubrogepant 50 mg, or ubrogepant 100 mg. Patients were instructed to treat a single migraine attack of moderate to severe pain intensity and record symptoms, such as pain, light sensitivity, and sound sensitivity, before and after taking the medication.
“The paradigm for this type of trial is to treat a single, well characterized migraine attack in a large population of patients,” Dr. Trugman said in a press conference at the annual meeting of the American Academy of Neurology.
At 2 hours after dosing, the percentage of ubrogepant-treated patients achieving freedom from pain was significantly greater than the percentage of those treated with placebo (50 mg: 19.2%, P = .0023; 100 mg: 21.2%, P = .0003; placebo: 11.8%).
The percentage of ubrogepant-treated patients achieving absence of their most bothersome symptom was also significantly greater than that of placebo (50 mg: 38.6%, P = .0023; 100 mg: 37.7%, P = .0023; placebo: 27.8%).
Adverse events in the ubrogepant groups were similar to those of placebo, the most reported to be nausea, somnolence, and dry mouth.
Several authors are employees of Allergan, which sponsored the study.
SOURCE: Trugman J et al. AAN 2018 emerging science abstract 008.
LOS ANGELES – The investigational oral calcitonin gene-related peptide (CGRP) blocker ubrogepant proved superior to placebo in treating a single, acute, moderate to severe migraine attack in the phase 3 ACHIEVE I trial.
Blocking the function of CGRP when it is pathologically released during a migraine attack is the mechanism of a bevy of antagonists under development for treating migraine, and the ACHIEVE I trial results are the first to be reported from a phase 3 trial of an oral small molecule to treat single migraine attacks rather than prevent attacks with monoclonal antibodies targeting CGRP or its receptor, according to the lead author of ACHIEVE I, Joel M. Trugman, MD, director of clinical development for Allergan.
Dr. Trugman and his colleagues recruited 1,672 adult patients (88% female, mean age 41) with a history of migraine with or without aura, and randomized them to placebo, ubrogepant 50 mg, or ubrogepant 100 mg. Patients were instructed to treat a single migraine attack of moderate to severe pain intensity and record symptoms, such as pain, light sensitivity, and sound sensitivity, before and after taking the medication.
“The paradigm for this type of trial is to treat a single, well characterized migraine attack in a large population of patients,” Dr. Trugman said in a press conference at the annual meeting of the American Academy of Neurology.
At 2 hours after dosing, the percentage of ubrogepant-treated patients achieving freedom from pain was significantly greater than the percentage of those treated with placebo (50 mg: 19.2%, P = .0023; 100 mg: 21.2%, P = .0003; placebo: 11.8%).
The percentage of ubrogepant-treated patients achieving absence of their most bothersome symptom was also significantly greater than that of placebo (50 mg: 38.6%, P = .0023; 100 mg: 37.7%, P = .0023; placebo: 27.8%).
Adverse events in the ubrogepant groups were similar to those of placebo, the most reported to be nausea, somnolence, and dry mouth.
Several authors are employees of Allergan, which sponsored the study.
SOURCE: Trugman J et al. AAN 2018 emerging science abstract 008.
REPORTING FROM AAN 2018
Cannabis users at highest psychosis risk may elect to quit
Cannabis users who experience symptoms suggestive of psychosis are more likely to stop using the drug – or report wanting to stop – than are those who report more pleasurable experiences.
This finding, published March 23 in Psychological Medicine, might help explain an epidemiological conundrum related to cannabis use.
Yet, despite evidence of increasing cannabis potency and cannabis use over the last 15 years, levels of psychotic disorders, such as schizophrenia, “are stable and have remained stable over time,” said Musa Basseer Sami, MD, the study’s lead author, in an interview. “This is a big stumbling block for anyone who says pot is associated with psychosis.”
Dr. Sami’s findings suggest that people who report psychosis-like experiences with cannabis might be those most likely to stop consuming it, in turn reducing their risk. “If people are discontinuing after bad experiences, and if such experiences are a risk factor for developing a psychotic disorder, they may be deselecting themselves” out of the cannabis-using population, said Dr. Sami of King’s College London.
For their research, the investigators conducted a cross-sectional online survey study of more than 1,200 current or previous cannabis users, about three-quarters of whom reported current use. To do this, they modified a validated survey tool called the Cannabis Experiences Questionnaire, which measures the euphoric and paranoid-dysphoric effects of cannabis. They also collected qualitative data from respondents explaining how their experiences shaped their attitudes on whether to continue using.
Current users who said they intended to quit cannabis reported greater psychosis-like experiences (OR, 1.131; 95% CI, 1.044-1.225; P less than 0.003). People who expressed a desire to continue, meanwhile, reported increased pleasurable experiences (OR, 0.892; 95% CI, 0.814-0.978; P less than 0.015).
The differences remained statistically significant across groups when age, sex, frequency of use, age of first use, and other drug use were accounted for.
Dr. Sami said. “And even if you continue using, you’re more likely to say you’re going to stop using in the future.”
Dr. Sami noted that nearly 40% of survey respondents reported having been treated for, or sought treatment for, a mental health complaint but cautioned against assuming these were attributable to cannabis use. “It’s very difficult to tease out whether they were using cannabis to self-medicate,” he said.
The new findings could help guide clinicians whose patients express a desire to quit and report psychosis-like experiences associated with cannabis. Helping patients elucidate those experiences could help inform conversations about risk and plans to quit, he said.
Currently, “we don’t really treat people who have these kind of experiences. If you came to me, as a psychiatrist, and asked me why I’m getting paranoid when I use cannabis, I’d tell you to stop using cannabis,” he said.
“But people who continue to use cannabis have a higher risk of psychotic disorder. And we’re now finding out that people who have psychotic-like experiences when they use cannabis tend to be more likely to develop psychotic disorders. So if I smoke weed and I start hearing voices and become suspicious, it might be a marker for me to develop schizophrenia.”
Dr. Sami and his colleagues are continuing to examine, by way of an online survey, why people might have very different experiences with the same drug. The survey is open to all adults whether they use cannabis or not at thecannabissurvey.com.
The research group declared support from the U.K. National Institute for Health Research, King’s College London, the Medical Research Council, and the U.K. Society for the Study of Addiction. The researchers reported no financial conflicts of interest.
SOURCE: Sami MB et al. Psychol Med. 2018 Mar 23. doi: 10.1017/S0033291718000569.
Cannabis users who experience symptoms suggestive of psychosis are more likely to stop using the drug – or report wanting to stop – than are those who report more pleasurable experiences.
This finding, published March 23 in Psychological Medicine, might help explain an epidemiological conundrum related to cannabis use.
Yet, despite evidence of increasing cannabis potency and cannabis use over the last 15 years, levels of psychotic disorders, such as schizophrenia, “are stable and have remained stable over time,” said Musa Basseer Sami, MD, the study’s lead author, in an interview. “This is a big stumbling block for anyone who says pot is associated with psychosis.”
Dr. Sami’s findings suggest that people who report psychosis-like experiences with cannabis might be those most likely to stop consuming it, in turn reducing their risk. “If people are discontinuing after bad experiences, and if such experiences are a risk factor for developing a psychotic disorder, they may be deselecting themselves” out of the cannabis-using population, said Dr. Sami of King’s College London.
For their research, the investigators conducted a cross-sectional online survey study of more than 1,200 current or previous cannabis users, about three-quarters of whom reported current use. To do this, they modified a validated survey tool called the Cannabis Experiences Questionnaire, which measures the euphoric and paranoid-dysphoric effects of cannabis. They also collected qualitative data from respondents explaining how their experiences shaped their attitudes on whether to continue using.
Current users who said they intended to quit cannabis reported greater psychosis-like experiences (OR, 1.131; 95% CI, 1.044-1.225; P less than 0.003). People who expressed a desire to continue, meanwhile, reported increased pleasurable experiences (OR, 0.892; 95% CI, 0.814-0.978; P less than 0.015).
The differences remained statistically significant across groups when age, sex, frequency of use, age of first use, and other drug use were accounted for.
Dr. Sami said. “And even if you continue using, you’re more likely to say you’re going to stop using in the future.”
Dr. Sami noted that nearly 40% of survey respondents reported having been treated for, or sought treatment for, a mental health complaint but cautioned against assuming these were attributable to cannabis use. “It’s very difficult to tease out whether they were using cannabis to self-medicate,” he said.
The new findings could help guide clinicians whose patients express a desire to quit and report psychosis-like experiences associated with cannabis. Helping patients elucidate those experiences could help inform conversations about risk and plans to quit, he said.
Currently, “we don’t really treat people who have these kind of experiences. If you came to me, as a psychiatrist, and asked me why I’m getting paranoid when I use cannabis, I’d tell you to stop using cannabis,” he said.
“But people who continue to use cannabis have a higher risk of psychotic disorder. And we’re now finding out that people who have psychotic-like experiences when they use cannabis tend to be more likely to develop psychotic disorders. So if I smoke weed and I start hearing voices and become suspicious, it might be a marker for me to develop schizophrenia.”
Dr. Sami and his colleagues are continuing to examine, by way of an online survey, why people might have very different experiences with the same drug. The survey is open to all adults whether they use cannabis or not at thecannabissurvey.com.
The research group declared support from the U.K. National Institute for Health Research, King’s College London, the Medical Research Council, and the U.K. Society for the Study of Addiction. The researchers reported no financial conflicts of interest.
SOURCE: Sami MB et al. Psychol Med. 2018 Mar 23. doi: 10.1017/S0033291718000569.
Cannabis users who experience symptoms suggestive of psychosis are more likely to stop using the drug – or report wanting to stop – than are those who report more pleasurable experiences.
This finding, published March 23 in Psychological Medicine, might help explain an epidemiological conundrum related to cannabis use.
Yet, despite evidence of increasing cannabis potency and cannabis use over the last 15 years, levels of psychotic disorders, such as schizophrenia, “are stable and have remained stable over time,” said Musa Basseer Sami, MD, the study’s lead author, in an interview. “This is a big stumbling block for anyone who says pot is associated with psychosis.”
Dr. Sami’s findings suggest that people who report psychosis-like experiences with cannabis might be those most likely to stop consuming it, in turn reducing their risk. “If people are discontinuing after bad experiences, and if such experiences are a risk factor for developing a psychotic disorder, they may be deselecting themselves” out of the cannabis-using population, said Dr. Sami of King’s College London.
For their research, the investigators conducted a cross-sectional online survey study of more than 1,200 current or previous cannabis users, about three-quarters of whom reported current use. To do this, they modified a validated survey tool called the Cannabis Experiences Questionnaire, which measures the euphoric and paranoid-dysphoric effects of cannabis. They also collected qualitative data from respondents explaining how their experiences shaped their attitudes on whether to continue using.
Current users who said they intended to quit cannabis reported greater psychosis-like experiences (OR, 1.131; 95% CI, 1.044-1.225; P less than 0.003). People who expressed a desire to continue, meanwhile, reported increased pleasurable experiences (OR, 0.892; 95% CI, 0.814-0.978; P less than 0.015).
The differences remained statistically significant across groups when age, sex, frequency of use, age of first use, and other drug use were accounted for.
Dr. Sami said. “And even if you continue using, you’re more likely to say you’re going to stop using in the future.”
Dr. Sami noted that nearly 40% of survey respondents reported having been treated for, or sought treatment for, a mental health complaint but cautioned against assuming these were attributable to cannabis use. “It’s very difficult to tease out whether they were using cannabis to self-medicate,” he said.
The new findings could help guide clinicians whose patients express a desire to quit and report psychosis-like experiences associated with cannabis. Helping patients elucidate those experiences could help inform conversations about risk and plans to quit, he said.
Currently, “we don’t really treat people who have these kind of experiences. If you came to me, as a psychiatrist, and asked me why I’m getting paranoid when I use cannabis, I’d tell you to stop using cannabis,” he said.
“But people who continue to use cannabis have a higher risk of psychotic disorder. And we’re now finding out that people who have psychotic-like experiences when they use cannabis tend to be more likely to develop psychotic disorders. So if I smoke weed and I start hearing voices and become suspicious, it might be a marker for me to develop schizophrenia.”
Dr. Sami and his colleagues are continuing to examine, by way of an online survey, why people might have very different experiences with the same drug. The survey is open to all adults whether they use cannabis or not at thecannabissurvey.com.
The research group declared support from the U.K. National Institute for Health Research, King’s College London, the Medical Research Council, and the U.K. Society for the Study of Addiction. The researchers reported no financial conflicts of interest.
SOURCE: Sami MB et al. Psychol Med. 2018 Mar 23. doi: 10.1017/S0033291718000569.
FROM PSYCHOLOGICAL MEDICINE
Key clinical point: Psychosis-like experiences with cannabis use predict cannabis cessation and the desire to quit.
Major finding: Cessation of cannabis use was associated with having greater self-reported psychosis-like experiences (odds ratio, 1.262; 95% confidence interval, 1.179-1.351; P less than 0.001).
Study details: An online survey of 1,231 cannabis users (69% male; n = 926 current users) measuring the effects of psychosis-like and pleasurable experiences on quitting or intending to quit.
Disclosures: The research group declared support from the U.K. National Institute for Health Research, King’s College London, the Medical Research Council, and the U.K. Society for the Study of Addiction. The researchers reported no financial conflicts of interest.
Source: Sami MB et al. Psychol Med. 2018 Mar 23. doi: 10.1017/S0033291718000569.
Tear proteins seen as Parkinson’s biomarker
The tears of people with established Parkinson’s disease have protein signatures distinct from those of healthy controls, researchers have learned.
Mark Lew, MD, and his colleagues at the University of Southern California, Los Angeles, used a noninvasive method to collect the tears and readily available assays to detect the proteins, paving the way for future studies of these proteins as biomarkers in early Parkinson’s disease (PD).
The researchers will report on their study at the annual meeting of the American Academy of Neurology in Los Angeles on April 22.
This research from Dr. Lew and his colleagues joins a host of ongoing efforts to find biomarkers for PD that can be used in the early stages of the disease, before motor dysfunction occurs. Other research groups are working on biomarkers in saliva and salivary glands, skin, blood, and cerebrospinal fluid. “Right now, a diagnosis of Parkinson’s disease is based on clinical history and then examination and then, potentially, on response to medication,” said Dr. Lew, professor of neurology, the vice chair of the department of neurology, and the director of the division of movement disorders at USC. “The difficulty is really being able to definitively be able to diagnose patients with early disease.”
Dr. Lew and his coinvestigators measured the levels of the protein alpha-synuclein in the tears of 55 people with PD and compared them with levels in the tears of 27 age- and sex-matched controls. They also measured oligomeric alpha-synuclein, an abnormal form of the protein whose aggregates are implicated in nerve damage in PD.
The test administered is based on a Schirmer’s test, which is used in ophthalmology to measure tear production. A strip of paper is placed in the lower eyelid pouch to collect tears, which the researchers then can analyze using commercially available assays.
Dr. Lew and his colleagues found levels of the oligomeric form of alpha-synuclein to be significantly greater in PD patients than they were in controls: an average of 1.45 ng/mg of tear protein, compared with 0.27 ng/mg in controls (P = .0007).
Total alpha-synuclein was decreased significantly in PD patients relative to healthy controls.
While the team looked at the levels of two additional proteins, CC chemokine ligand 2 and DJ-1 (Parkinson’s disease protein 7), neither of them varied significantly between PD patients and non-PD controls.
“We’re cautiously optimistic, and I don’t want to overstate the results because it’s still a relatively small group of subjects – we need to more than double the control population to make sure our results are maintained,” Dr. Lew said in an interview in advance of the meeting. “But it’s very exciting.”
At AAN, Dr. Lew’s research group will present findings from a larger cohort of both patients and controls. “Our expectation is that things will look similar and we will continue to see a significant difference in the oligomeric form of alpha-synuclein,” the tear protein associated with PD.
The idea of using tear proteins as biomarkers for PD came as a result of a collaboration with scientists working in USC’s ophthalmology lab, who had previously worked on tear biomarkers in other disorders, including Sjogren’s syndrome, Dr. Lew said.
Dr. Lew said that, if the initial results bear out in a larger cohort, the next step is to test the tears of people with genetic or atypical forms of PD and compare the results with those for idiopathic forms. “These atypical forms, like progressive supranuclear palsy [PSP] and multiple system atrophy [MSA], can be very difficult to tell apart clinically in the early stages. If we had a simple test to do that, it would be very helpful.”
A reliable biomarker, if it can be shown to be sensitive early in disease, also would have implications for the timing of disease-modifying interventions, such as the monoclonal antibodies or gene therapies that are currently being investigated.
“We don’t have those therapies now, but in a few years we very well could,” Dr. Lew said. “If we could identify patients early and if we had a therapy that we could give them that was disease-modifying, or neuroprotective, you’d want to start much earlier than we currently do.”
This study from Dr. Lew and his colleagues was supported by the Michael J. Fox Foundation and the Plotkin Foundation. Dr. Lew has received personal compensation for consulting for, serving on a scientific advisory board for, speaking for, or other activities with Teva Pharmaceutical Industries, US WorldMeds, AbbVie, Lundbeck, Acadia Pharmaceuticals, UCB, Revance Therapeutics, and Adamas Pharmaceuticals. Dr. Lew has received research support from Acorda Therapeutics, Biotie Therapies, NeuroDerm, and Lilly. None of the other authors had anything to disclose.
SOURCE: Feigenbaum D et al. Abstract 4209.
The tears of people with established Parkinson’s disease have protein signatures distinct from those of healthy controls, researchers have learned.
Mark Lew, MD, and his colleagues at the University of Southern California, Los Angeles, used a noninvasive method to collect the tears and readily available assays to detect the proteins, paving the way for future studies of these proteins as biomarkers in early Parkinson’s disease (PD).
The researchers will report on their study at the annual meeting of the American Academy of Neurology in Los Angeles on April 22.
This research from Dr. Lew and his colleagues joins a host of ongoing efforts to find biomarkers for PD that can be used in the early stages of the disease, before motor dysfunction occurs. Other research groups are working on biomarkers in saliva and salivary glands, skin, blood, and cerebrospinal fluid. “Right now, a diagnosis of Parkinson’s disease is based on clinical history and then examination and then, potentially, on response to medication,” said Dr. Lew, professor of neurology, the vice chair of the department of neurology, and the director of the division of movement disorders at USC. “The difficulty is really being able to definitively be able to diagnose patients with early disease.”
Dr. Lew and his coinvestigators measured the levels of the protein alpha-synuclein in the tears of 55 people with PD and compared them with levels in the tears of 27 age- and sex-matched controls. They also measured oligomeric alpha-synuclein, an abnormal form of the protein whose aggregates are implicated in nerve damage in PD.
The test administered is based on a Schirmer’s test, which is used in ophthalmology to measure tear production. A strip of paper is placed in the lower eyelid pouch to collect tears, which the researchers then can analyze using commercially available assays.
Dr. Lew and his colleagues found levels of the oligomeric form of alpha-synuclein to be significantly greater in PD patients than they were in controls: an average of 1.45 ng/mg of tear protein, compared with 0.27 ng/mg in controls (P = .0007).
Total alpha-synuclein was decreased significantly in PD patients relative to healthy controls.
While the team looked at the levels of two additional proteins, CC chemokine ligand 2 and DJ-1 (Parkinson’s disease protein 7), neither of them varied significantly between PD patients and non-PD controls.
“We’re cautiously optimistic, and I don’t want to overstate the results because it’s still a relatively small group of subjects – we need to more than double the control population to make sure our results are maintained,” Dr. Lew said in an interview in advance of the meeting. “But it’s very exciting.”
At AAN, Dr. Lew’s research group will present findings from a larger cohort of both patients and controls. “Our expectation is that things will look similar and we will continue to see a significant difference in the oligomeric form of alpha-synuclein,” the tear protein associated with PD.
The idea of using tear proteins as biomarkers for PD came as a result of a collaboration with scientists working in USC’s ophthalmology lab, who had previously worked on tear biomarkers in other disorders, including Sjogren’s syndrome, Dr. Lew said.
Dr. Lew said that, if the initial results bear out in a larger cohort, the next step is to test the tears of people with genetic or atypical forms of PD and compare the results with those for idiopathic forms. “These atypical forms, like progressive supranuclear palsy [PSP] and multiple system atrophy [MSA], can be very difficult to tell apart clinically in the early stages. If we had a simple test to do that, it would be very helpful.”
A reliable biomarker, if it can be shown to be sensitive early in disease, also would have implications for the timing of disease-modifying interventions, such as the monoclonal antibodies or gene therapies that are currently being investigated.
“We don’t have those therapies now, but in a few years we very well could,” Dr. Lew said. “If we could identify patients early and if we had a therapy that we could give them that was disease-modifying, or neuroprotective, you’d want to start much earlier than we currently do.”
This study from Dr. Lew and his colleagues was supported by the Michael J. Fox Foundation and the Plotkin Foundation. Dr. Lew has received personal compensation for consulting for, serving on a scientific advisory board for, speaking for, or other activities with Teva Pharmaceutical Industries, US WorldMeds, AbbVie, Lundbeck, Acadia Pharmaceuticals, UCB, Revance Therapeutics, and Adamas Pharmaceuticals. Dr. Lew has received research support from Acorda Therapeutics, Biotie Therapies, NeuroDerm, and Lilly. None of the other authors had anything to disclose.
SOURCE: Feigenbaum D et al. Abstract 4209.
The tears of people with established Parkinson’s disease have protein signatures distinct from those of healthy controls, researchers have learned.
Mark Lew, MD, and his colleagues at the University of Southern California, Los Angeles, used a noninvasive method to collect the tears and readily available assays to detect the proteins, paving the way for future studies of these proteins as biomarkers in early Parkinson’s disease (PD).
The researchers will report on their study at the annual meeting of the American Academy of Neurology in Los Angeles on April 22.
This research from Dr. Lew and his colleagues joins a host of ongoing efforts to find biomarkers for PD that can be used in the early stages of the disease, before motor dysfunction occurs. Other research groups are working on biomarkers in saliva and salivary glands, skin, blood, and cerebrospinal fluid. “Right now, a diagnosis of Parkinson’s disease is based on clinical history and then examination and then, potentially, on response to medication,” said Dr. Lew, professor of neurology, the vice chair of the department of neurology, and the director of the division of movement disorders at USC. “The difficulty is really being able to definitively be able to diagnose patients with early disease.”
Dr. Lew and his coinvestigators measured the levels of the protein alpha-synuclein in the tears of 55 people with PD and compared them with levels in the tears of 27 age- and sex-matched controls. They also measured oligomeric alpha-synuclein, an abnormal form of the protein whose aggregates are implicated in nerve damage in PD.
The test administered is based on a Schirmer’s test, which is used in ophthalmology to measure tear production. A strip of paper is placed in the lower eyelid pouch to collect tears, which the researchers then can analyze using commercially available assays.
Dr. Lew and his colleagues found levels of the oligomeric form of alpha-synuclein to be significantly greater in PD patients than they were in controls: an average of 1.45 ng/mg of tear protein, compared with 0.27 ng/mg in controls (P = .0007).
Total alpha-synuclein was decreased significantly in PD patients relative to healthy controls.
While the team looked at the levels of two additional proteins, CC chemokine ligand 2 and DJ-1 (Parkinson’s disease protein 7), neither of them varied significantly between PD patients and non-PD controls.
“We’re cautiously optimistic, and I don’t want to overstate the results because it’s still a relatively small group of subjects – we need to more than double the control population to make sure our results are maintained,” Dr. Lew said in an interview in advance of the meeting. “But it’s very exciting.”
At AAN, Dr. Lew’s research group will present findings from a larger cohort of both patients and controls. “Our expectation is that things will look similar and we will continue to see a significant difference in the oligomeric form of alpha-synuclein,” the tear protein associated with PD.
The idea of using tear proteins as biomarkers for PD came as a result of a collaboration with scientists working in USC’s ophthalmology lab, who had previously worked on tear biomarkers in other disorders, including Sjogren’s syndrome, Dr. Lew said.
Dr. Lew said that, if the initial results bear out in a larger cohort, the next step is to test the tears of people with genetic or atypical forms of PD and compare the results with those for idiopathic forms. “These atypical forms, like progressive supranuclear palsy [PSP] and multiple system atrophy [MSA], can be very difficult to tell apart clinically in the early stages. If we had a simple test to do that, it would be very helpful.”
A reliable biomarker, if it can be shown to be sensitive early in disease, also would have implications for the timing of disease-modifying interventions, such as the monoclonal antibodies or gene therapies that are currently being investigated.
“We don’t have those therapies now, but in a few years we very well could,” Dr. Lew said. “If we could identify patients early and if we had a therapy that we could give them that was disease-modifying, or neuroprotective, you’d want to start much earlier than we currently do.”
This study from Dr. Lew and his colleagues was supported by the Michael J. Fox Foundation and the Plotkin Foundation. Dr. Lew has received personal compensation for consulting for, serving on a scientific advisory board for, speaking for, or other activities with Teva Pharmaceutical Industries, US WorldMeds, AbbVie, Lundbeck, Acadia Pharmaceuticals, UCB, Revance Therapeutics, and Adamas Pharmaceuticals. Dr. Lew has received research support from Acorda Therapeutics, Biotie Therapies, NeuroDerm, and Lilly. None of the other authors had anything to disclose.
SOURCE: Feigenbaum D et al. Abstract 4209.
FROM AAN 2018
Key clinical point: Elevated oligomeric alpha-synuclein in tears shows promise as an early biomarker for Parkinson’s disease.
Major finding: Levels of the oligomeric form of alpha-synuclein were significantly greater in PD patients, compared with controls: an average of 1.45 ng/mg of tear protein, compared with 0.27 ng/mg in controls (P = .0007).
Study details: An ongoing study that has so far measured tear proteins in 55 people with PD and 27 age- and sex-matched controls.
Disclosures: Dr. Lew and his colleagues’ study was supported by the Michael J. Fox Foundation and the Plotkin Foundation. Dr. Lew has received personal compensation for consulting for, serving on a scientific advisory board for, speaking for, or other activities with Teva Pharmaceutical Industries, US WorldMeds, AbbVie, Lundbeck, Acadia Pharmaceuticals, UCB, Revance Therapeutics, and Adamas Pharmaceuticals. Dr. Lew has received research support from Acorda Therapeutics, Biotie Therapies, NeuroDerm, and Lilly. None of the other authors had anything to disclose.
Source: Feigenbaum D et al. AAN 2018, Abstract 4209