User login
Palliative care for patients suffering from severe persistent mental illness
While palliative care grows as an interdisciplinary specialty, more clinicians are asking how it can benefit certain patients with severe mental illness.
Palliative care, which developed with the founding of hospices in the 1960s, initially focused on patients who were dying from cancer. The specialty – which emphasizes improving patients’ quality of life rather than finding a cure, and which is different from hospice – can now be used for patients with noncancer diagnoses such as dementia and HIV/AIDS (Psychiatry. 2009 Jun;8[6]:212-15).
Some psychiatrists think that certain patients with another diagnosis would benefit from palliative care: those with severe persistent mental illness.
In fact, this approach might apply to psychiatric patients who are in long-term residential care with “severe/chronic schizophrenia and insufficient quality of life, those with therapy-refractory depressions and repeated suicide attempts, and those with severe long-standing therapy-refractory anorexia nervosa,” wrote Manuel Trachsel, MD, PhD, and his colleagues (BMC Psychiatry (2016 Jul 14:1-9).
Scott A. Irwin, MD, PhD, who coauthored that article and a letter examining these issues, said Dr. Trachsel’s theories lie on the frontiers of current thinking about incorporating palliative care and psychiatric medicine.
Meanwhile, both Dr. Irwin and Maria I. Lapid, MD, another psychiatrist with expertise in palliative care, said that in many ways, the field of psychiatry is inherently palliative in nature.
Palliative ‘approach’ in SPMI
Dr. Trachsel presented unpublished results from a survey of U.S. psychiatrists at the annual meeting of the American Psychiatric Association in May that sought to discern whether they favored supporting short-term quality of life rather than long-term disease modification in certain patients with severe and persistent mental illness (SPMI) – defined as mental illness that is chronic or recurring, requires ongoing intensive psychiatric treatment, and seriously impairs functioning.

Specifically, a palliative care approach to SPMI could include a more relaxed use of agents considered potentially addictive or problematic long term, such as benzodiazepines, Dr. Trachsel said. For patients with medical decision-making capacity, it could 1) include withdrawal of care at a patient’s insistence or periods of intermittent sedation – which is used in palliative medicine for patients with intractable pain; or 2) mean switching a patient with end-stage anorexia and multiple failed treatment attempts to hospice care rather than force feeding, Dr. Trachsel said.
Neither Dr. Trachsel’s survey respondents nor those who attended his presentation seemed comfortable with the idea of extending the term “palliative care” – which is often and incorrectly associated with well-defined end-of-life scenarios – to serious, treatment-refractory mental illness. In those illnesses, disease trajectories may be less certain and futility is harder to define. They and other clinicians, however, did voice general support for the underlying concepts of promoting quality of life and decision-making autonomy for patients with SPMI, as well as palliative care targeted at the medical illnesses often acquired by those with SPMI.
According to Dr. Irwin and Dr. Lapid, reducing symptoms, acknowledging that there is no cure for SPMI, and focusing on optimizing patients’ quality of life would be core components of palliative care.
Futility difficult to define
Dr. Irwin said in an interview that the ideas in the letter (Lancet Psychiatry. 2016 Mar;3[3]:200) in which he and a few other colleagues collaborated with Dr. Trachsel were essentially “a thought experiment and very philosophical.” In addition, the letter, which proposed palliative psychiatry “as a means to improve quality of care, person-centeredness, and autonomy” for patients with SPMI, was supported by a handful of case studies, most of them in patients with end-stage anorexia, he said. Furthermore, end-of-life interventions are only a subset of what palliative care brings to the table, said Dr. Irwin, palliative care psychiatrist at Cedars-Sinai Health System’s Samuel Oschin Comprehensive Cancer Center in Los Angeles.
With a psychiatric illness, the goals are usually around symptom management and quality of life, and for certain palliative care interventions reserved for end-of-life situations, “there’s usually not something knocking at the door that’s putting that end-of-life question into focus,” Dr. Irwin said. To create end-of-life protocols for SPMI, “you would need to know what the prognosis and trajectory are of each stage of these illnesses. And we don’t have good evidence guiding us.
“If we have a patient who is depressed and wants to commit suicide, who knows how many years they could have left if we intervene?” said Dr. Irwin, who has mentored Dr. Trachsel. “If we had the data that this person’s 90% likely to complete a suicide within the next year, it might change the conversation and treatment decisions.”
Dr. Lapid, a board-certified practitioner of palliative and hospice medicine and geriatric psychiatry at the Mayo Clinic in Rochester, Minn., agreed in an interview that for patients with an SPMI and no life-limiting comorbidity, it becomes complicated to attempt to define futility.

Moreover, while Medicare and insurance have precisely detailed guidelines for hospice, which provides palliative care for those with a prognosis of 6 months or less, “there’s no psychiatric illness currently considered a terminal disease eligible for hospice care,” Dr. Lapid said.
Obstacles to access
Patients with SPMI die 25 years earlier than do their peers without SPMI. Most of the premature mortality associated with SPMI, which cuts across age groups, is attributable to chronic diseases rather than to violence or suicide. Less overall engagement with the health care system, leading to late treatment or undertreatment of disease, is one explanation for the premature mortality found among some people in this demographic.
In addition, studies have shown that individuals with SPMI have less access to palliative and hospice care. One study, for example, found that people with schizophrenia and a terminal illness went into hospice half as often as did people without SPMI (Schizophr Res. 2012 Nov;141:241-6). In a recent editorial, a team of psychiatrists and pain specialists called such disparities “unacceptable” and demanded cross-collaboration to resolve them (Gen Hospital Psych. 2017 Jan-Feb;44:1-3).
Dr. Lapid said one reason people with SPMI – with or without a life-limiting comorbidity – end up with less access to palliative and hospice care is that “the art of what we do in hospice and palliative care, advanced planning – is not something we do well or routinely in psychiatry.”
And palliative care specialists may find that for some people with severe mental illness, “it can be hard to really palliate their symptoms,” Dr. Lapid said.
Dr. Irwin noted that patients with SPMI and a terminal illness generally are not extended the same level of agency over their treatment choices as are people without it. Cancer patients, for example, can elect not to receive a treatment even when their prognosis is good. People with serious mental illness – even when they have life-limiting medical comorbidities – may not be given the option of deciding whether to opt for treatment.
Rebecca L. Bauer, MD, a psychosomatic medicine fellow at the Medical College of Wisconsin in Milwaukee, said that psychiatrists, including those with outpatient practices, are well positioned to help patients gain greater access to palliative care and end-of-life planning.

These patients’ medical needs become so pressing at the end of life that psychiatric disease and the distress it inflicts end up a secondary concern, she said, resulting in the patient suffering.
Psychiatrists “can play an important role in removing some of these barriers,” Dr. Bauer said, especially on multidisciplinary teams. For one thing, psychiatrists are adept at prescribing medications aimed at treating concurrent psychiatric symptoms. In addition, they are more likely than are other clinicians to have experience in communicating with patients with psychosis or other thought disorders.
Another important way psychiatrists can help secure access to palliative care for their patients who need it, she said, is to engage patients during times of relative wellness by encouraging them to discuss end-of-life desires and plans, and help them create formal health care directives.
“We know that sometimes patients [with SPMI] are not as engaged in their primary and medical care, and sometimes the psychiatrist is the only provider they consistently follow up with,” Dr. Bauer said.
All the clinicians interviewed acknowledged that, regardless of the feasibility or ethical viability of any single approach, the idea of incorporating some of the pillars of palliative care for patients with SPMI merits more consideration.
The approach used by psychiatrists treating patients with SPMI is very palliative in approach, Dr. Irwin and Dr. Lapid said. Psychiatrists reduce symptoms and acknowledge that SPMIs are chronic diseases for which there is no cure. To palliate is to make comfortable, to reduce symptoms, to reduce distress and pain, and to relieve suffering and optimize quality of life.
“In cancer, we’ve been telling people for 30 years, ‘keep fighting, because tomorrow there could be a new cure.’ But there’ve been very few new cures,” Dr. Irwin said. “And while some people want to fight to the end in case that cure comes, there are many who would have rather known that there really was little chance and might have made different choices.” In psychiatry, for psychiatric illnesses, he continued, “we need to really start thinking about the course of a person’s life, their quality of life, and the likelihood that they will get better or meet their goals, and what is a tolerable symptom burden for them. Because in the end, these questions apply to all patients.”
While palliative care grows as an interdisciplinary specialty, more clinicians are asking how it can benefit certain patients with severe mental illness.
Palliative care, which developed with the founding of hospices in the 1960s, initially focused on patients who were dying from cancer. The specialty – which emphasizes improving patients’ quality of life rather than finding a cure, and which is different from hospice – can now be used for patients with noncancer diagnoses such as dementia and HIV/AIDS (Psychiatry. 2009 Jun;8[6]:212-15).
Some psychiatrists think that certain patients with another diagnosis would benefit from palliative care: those with severe persistent mental illness.
In fact, this approach might apply to psychiatric patients who are in long-term residential care with “severe/chronic schizophrenia and insufficient quality of life, those with therapy-refractory depressions and repeated suicide attempts, and those with severe long-standing therapy-refractory anorexia nervosa,” wrote Manuel Trachsel, MD, PhD, and his colleagues (BMC Psychiatry (2016 Jul 14:1-9).
Scott A. Irwin, MD, PhD, who coauthored that article and a letter examining these issues, said Dr. Trachsel’s theories lie on the frontiers of current thinking about incorporating palliative care and psychiatric medicine.
Meanwhile, both Dr. Irwin and Maria I. Lapid, MD, another psychiatrist with expertise in palliative care, said that in many ways, the field of psychiatry is inherently palliative in nature.
Palliative ‘approach’ in SPMI
Dr. Trachsel presented unpublished results from a survey of U.S. psychiatrists at the annual meeting of the American Psychiatric Association in May that sought to discern whether they favored supporting short-term quality of life rather than long-term disease modification in certain patients with severe and persistent mental illness (SPMI) – defined as mental illness that is chronic or recurring, requires ongoing intensive psychiatric treatment, and seriously impairs functioning.

Specifically, a palliative care approach to SPMI could include a more relaxed use of agents considered potentially addictive or problematic long term, such as benzodiazepines, Dr. Trachsel said. For patients with medical decision-making capacity, it could 1) include withdrawal of care at a patient’s insistence or periods of intermittent sedation – which is used in palliative medicine for patients with intractable pain; or 2) mean switching a patient with end-stage anorexia and multiple failed treatment attempts to hospice care rather than force feeding, Dr. Trachsel said.
Neither Dr. Trachsel’s survey respondents nor those who attended his presentation seemed comfortable with the idea of extending the term “palliative care” – which is often and incorrectly associated with well-defined end-of-life scenarios – to serious, treatment-refractory mental illness. In those illnesses, disease trajectories may be less certain and futility is harder to define. They and other clinicians, however, did voice general support for the underlying concepts of promoting quality of life and decision-making autonomy for patients with SPMI, as well as palliative care targeted at the medical illnesses often acquired by those with SPMI.
According to Dr. Irwin and Dr. Lapid, reducing symptoms, acknowledging that there is no cure for SPMI, and focusing on optimizing patients’ quality of life would be core components of palliative care.
Futility difficult to define
Dr. Irwin said in an interview that the ideas in the letter (Lancet Psychiatry. 2016 Mar;3[3]:200) in which he and a few other colleagues collaborated with Dr. Trachsel were essentially “a thought experiment and very philosophical.” In addition, the letter, which proposed palliative psychiatry “as a means to improve quality of care, person-centeredness, and autonomy” for patients with SPMI, was supported by a handful of case studies, most of them in patients with end-stage anorexia, he said. Furthermore, end-of-life interventions are only a subset of what palliative care brings to the table, said Dr. Irwin, palliative care psychiatrist at Cedars-Sinai Health System’s Samuel Oschin Comprehensive Cancer Center in Los Angeles.
With a psychiatric illness, the goals are usually around symptom management and quality of life, and for certain palliative care interventions reserved for end-of-life situations, “there’s usually not something knocking at the door that’s putting that end-of-life question into focus,” Dr. Irwin said. To create end-of-life protocols for SPMI, “you would need to know what the prognosis and trajectory are of each stage of these illnesses. And we don’t have good evidence guiding us.
“If we have a patient who is depressed and wants to commit suicide, who knows how many years they could have left if we intervene?” said Dr. Irwin, who has mentored Dr. Trachsel. “If we had the data that this person’s 90% likely to complete a suicide within the next year, it might change the conversation and treatment decisions.”
Dr. Lapid, a board-certified practitioner of palliative and hospice medicine and geriatric psychiatry at the Mayo Clinic in Rochester, Minn., agreed in an interview that for patients with an SPMI and no life-limiting comorbidity, it becomes complicated to attempt to define futility.

Moreover, while Medicare and insurance have precisely detailed guidelines for hospice, which provides palliative care for those with a prognosis of 6 months or less, “there’s no psychiatric illness currently considered a terminal disease eligible for hospice care,” Dr. Lapid said.
Obstacles to access
Patients with SPMI die 25 years earlier than do their peers without SPMI. Most of the premature mortality associated with SPMI, which cuts across age groups, is attributable to chronic diseases rather than to violence or suicide. Less overall engagement with the health care system, leading to late treatment or undertreatment of disease, is one explanation for the premature mortality found among some people in this demographic.
In addition, studies have shown that individuals with SPMI have less access to palliative and hospice care. One study, for example, found that people with schizophrenia and a terminal illness went into hospice half as often as did people without SPMI (Schizophr Res. 2012 Nov;141:241-6). In a recent editorial, a team of psychiatrists and pain specialists called such disparities “unacceptable” and demanded cross-collaboration to resolve them (Gen Hospital Psych. 2017 Jan-Feb;44:1-3).
Dr. Lapid said one reason people with SPMI – with or without a life-limiting comorbidity – end up with less access to palliative and hospice care is that “the art of what we do in hospice and palliative care, advanced planning – is not something we do well or routinely in psychiatry.”
And palliative care specialists may find that for some people with severe mental illness, “it can be hard to really palliate their symptoms,” Dr. Lapid said.
Dr. Irwin noted that patients with SPMI and a terminal illness generally are not extended the same level of agency over their treatment choices as are people without it. Cancer patients, for example, can elect not to receive a treatment even when their prognosis is good. People with serious mental illness – even when they have life-limiting medical comorbidities – may not be given the option of deciding whether to opt for treatment.
Rebecca L. Bauer, MD, a psychosomatic medicine fellow at the Medical College of Wisconsin in Milwaukee, said that psychiatrists, including those with outpatient practices, are well positioned to help patients gain greater access to palliative care and end-of-life planning.

These patients’ medical needs become so pressing at the end of life that psychiatric disease and the distress it inflicts end up a secondary concern, she said, resulting in the patient suffering.
Psychiatrists “can play an important role in removing some of these barriers,” Dr. Bauer said, especially on multidisciplinary teams. For one thing, psychiatrists are adept at prescribing medications aimed at treating concurrent psychiatric symptoms. In addition, they are more likely than are other clinicians to have experience in communicating with patients with psychosis or other thought disorders.
Another important way psychiatrists can help secure access to palliative care for their patients who need it, she said, is to engage patients during times of relative wellness by encouraging them to discuss end-of-life desires and plans, and help them create formal health care directives.
“We know that sometimes patients [with SPMI] are not as engaged in their primary and medical care, and sometimes the psychiatrist is the only provider they consistently follow up with,” Dr. Bauer said.
All the clinicians interviewed acknowledged that, regardless of the feasibility or ethical viability of any single approach, the idea of incorporating some of the pillars of palliative care for patients with SPMI merits more consideration.
The approach used by psychiatrists treating patients with SPMI is very palliative in approach, Dr. Irwin and Dr. Lapid said. Psychiatrists reduce symptoms and acknowledge that SPMIs are chronic diseases for which there is no cure. To palliate is to make comfortable, to reduce symptoms, to reduce distress and pain, and to relieve suffering and optimize quality of life.
“In cancer, we’ve been telling people for 30 years, ‘keep fighting, because tomorrow there could be a new cure.’ But there’ve been very few new cures,” Dr. Irwin said. “And while some people want to fight to the end in case that cure comes, there are many who would have rather known that there really was little chance and might have made different choices.” In psychiatry, for psychiatric illnesses, he continued, “we need to really start thinking about the course of a person’s life, their quality of life, and the likelihood that they will get better or meet their goals, and what is a tolerable symptom burden for them. Because in the end, these questions apply to all patients.”
While palliative care grows as an interdisciplinary specialty, more clinicians are asking how it can benefit certain patients with severe mental illness.
Palliative care, which developed with the founding of hospices in the 1960s, initially focused on patients who were dying from cancer. The specialty – which emphasizes improving patients’ quality of life rather than finding a cure, and which is different from hospice – can now be used for patients with noncancer diagnoses such as dementia and HIV/AIDS (Psychiatry. 2009 Jun;8[6]:212-15).
Some psychiatrists think that certain patients with another diagnosis would benefit from palliative care: those with severe persistent mental illness.
In fact, this approach might apply to psychiatric patients who are in long-term residential care with “severe/chronic schizophrenia and insufficient quality of life, those with therapy-refractory depressions and repeated suicide attempts, and those with severe long-standing therapy-refractory anorexia nervosa,” wrote Manuel Trachsel, MD, PhD, and his colleagues (BMC Psychiatry (2016 Jul 14:1-9).
Scott A. Irwin, MD, PhD, who coauthored that article and a letter examining these issues, said Dr. Trachsel’s theories lie on the frontiers of current thinking about incorporating palliative care and psychiatric medicine.
Meanwhile, both Dr. Irwin and Maria I. Lapid, MD, another psychiatrist with expertise in palliative care, said that in many ways, the field of psychiatry is inherently palliative in nature.
Palliative ‘approach’ in SPMI
Dr. Trachsel presented unpublished results from a survey of U.S. psychiatrists at the annual meeting of the American Psychiatric Association in May that sought to discern whether they favored supporting short-term quality of life rather than long-term disease modification in certain patients with severe and persistent mental illness (SPMI) – defined as mental illness that is chronic or recurring, requires ongoing intensive psychiatric treatment, and seriously impairs functioning.

Specifically, a palliative care approach to SPMI could include a more relaxed use of agents considered potentially addictive or problematic long term, such as benzodiazepines, Dr. Trachsel said. For patients with medical decision-making capacity, it could 1) include withdrawal of care at a patient’s insistence or periods of intermittent sedation – which is used in palliative medicine for patients with intractable pain; or 2) mean switching a patient with end-stage anorexia and multiple failed treatment attempts to hospice care rather than force feeding, Dr. Trachsel said.
Neither Dr. Trachsel’s survey respondents nor those who attended his presentation seemed comfortable with the idea of extending the term “palliative care” – which is often and incorrectly associated with well-defined end-of-life scenarios – to serious, treatment-refractory mental illness. In those illnesses, disease trajectories may be less certain and futility is harder to define. They and other clinicians, however, did voice general support for the underlying concepts of promoting quality of life and decision-making autonomy for patients with SPMI, as well as palliative care targeted at the medical illnesses often acquired by those with SPMI.
According to Dr. Irwin and Dr. Lapid, reducing symptoms, acknowledging that there is no cure for SPMI, and focusing on optimizing patients’ quality of life would be core components of palliative care.
Futility difficult to define
Dr. Irwin said in an interview that the ideas in the letter (Lancet Psychiatry. 2016 Mar;3[3]:200) in which he and a few other colleagues collaborated with Dr. Trachsel were essentially “a thought experiment and very philosophical.” In addition, the letter, which proposed palliative psychiatry “as a means to improve quality of care, person-centeredness, and autonomy” for patients with SPMI, was supported by a handful of case studies, most of them in patients with end-stage anorexia, he said. Furthermore, end-of-life interventions are only a subset of what palliative care brings to the table, said Dr. Irwin, palliative care psychiatrist at Cedars-Sinai Health System’s Samuel Oschin Comprehensive Cancer Center in Los Angeles.
With a psychiatric illness, the goals are usually around symptom management and quality of life, and for certain palliative care interventions reserved for end-of-life situations, “there’s usually not something knocking at the door that’s putting that end-of-life question into focus,” Dr. Irwin said. To create end-of-life protocols for SPMI, “you would need to know what the prognosis and trajectory are of each stage of these illnesses. And we don’t have good evidence guiding us.
“If we have a patient who is depressed and wants to commit suicide, who knows how many years they could have left if we intervene?” said Dr. Irwin, who has mentored Dr. Trachsel. “If we had the data that this person’s 90% likely to complete a suicide within the next year, it might change the conversation and treatment decisions.”
Dr. Lapid, a board-certified practitioner of palliative and hospice medicine and geriatric psychiatry at the Mayo Clinic in Rochester, Minn., agreed in an interview that for patients with an SPMI and no life-limiting comorbidity, it becomes complicated to attempt to define futility.

Moreover, while Medicare and insurance have precisely detailed guidelines for hospice, which provides palliative care for those with a prognosis of 6 months or less, “there’s no psychiatric illness currently considered a terminal disease eligible for hospice care,” Dr. Lapid said.
Obstacles to access
Patients with SPMI die 25 years earlier than do their peers without SPMI. Most of the premature mortality associated with SPMI, which cuts across age groups, is attributable to chronic diseases rather than to violence or suicide. Less overall engagement with the health care system, leading to late treatment or undertreatment of disease, is one explanation for the premature mortality found among some people in this demographic.
In addition, studies have shown that individuals with SPMI have less access to palliative and hospice care. One study, for example, found that people with schizophrenia and a terminal illness went into hospice half as often as did people without SPMI (Schizophr Res. 2012 Nov;141:241-6). In a recent editorial, a team of psychiatrists and pain specialists called such disparities “unacceptable” and demanded cross-collaboration to resolve them (Gen Hospital Psych. 2017 Jan-Feb;44:1-3).
Dr. Lapid said one reason people with SPMI – with or without a life-limiting comorbidity – end up with less access to palliative and hospice care is that “the art of what we do in hospice and palliative care, advanced planning – is not something we do well or routinely in psychiatry.”
And palliative care specialists may find that for some people with severe mental illness, “it can be hard to really palliate their symptoms,” Dr. Lapid said.
Dr. Irwin noted that patients with SPMI and a terminal illness generally are not extended the same level of agency over their treatment choices as are people without it. Cancer patients, for example, can elect not to receive a treatment even when their prognosis is good. People with serious mental illness – even when they have life-limiting medical comorbidities – may not be given the option of deciding whether to opt for treatment.
Rebecca L. Bauer, MD, a psychosomatic medicine fellow at the Medical College of Wisconsin in Milwaukee, said that psychiatrists, including those with outpatient practices, are well positioned to help patients gain greater access to palliative care and end-of-life planning.

These patients’ medical needs become so pressing at the end of life that psychiatric disease and the distress it inflicts end up a secondary concern, she said, resulting in the patient suffering.
Psychiatrists “can play an important role in removing some of these barriers,” Dr. Bauer said, especially on multidisciplinary teams. For one thing, psychiatrists are adept at prescribing medications aimed at treating concurrent psychiatric symptoms. In addition, they are more likely than are other clinicians to have experience in communicating with patients with psychosis or other thought disorders.
Another important way psychiatrists can help secure access to palliative care for their patients who need it, she said, is to engage patients during times of relative wellness by encouraging them to discuss end-of-life desires and plans, and help them create formal health care directives.
“We know that sometimes patients [with SPMI] are not as engaged in their primary and medical care, and sometimes the psychiatrist is the only provider they consistently follow up with,” Dr. Bauer said.
All the clinicians interviewed acknowledged that, regardless of the feasibility or ethical viability of any single approach, the idea of incorporating some of the pillars of palliative care for patients with SPMI merits more consideration.
The approach used by psychiatrists treating patients with SPMI is very palliative in approach, Dr. Irwin and Dr. Lapid said. Psychiatrists reduce symptoms and acknowledge that SPMIs are chronic diseases for which there is no cure. To palliate is to make comfortable, to reduce symptoms, to reduce distress and pain, and to relieve suffering and optimize quality of life.
“In cancer, we’ve been telling people for 30 years, ‘keep fighting, because tomorrow there could be a new cure.’ But there’ve been very few new cures,” Dr. Irwin said. “And while some people want to fight to the end in case that cure comes, there are many who would have rather known that there really was little chance and might have made different choices.” In psychiatry, for psychiatric illnesses, he continued, “we need to really start thinking about the course of a person’s life, their quality of life, and the likelihood that they will get better or meet their goals, and what is a tolerable symptom burden for them. Because in the end, these questions apply to all patients.”
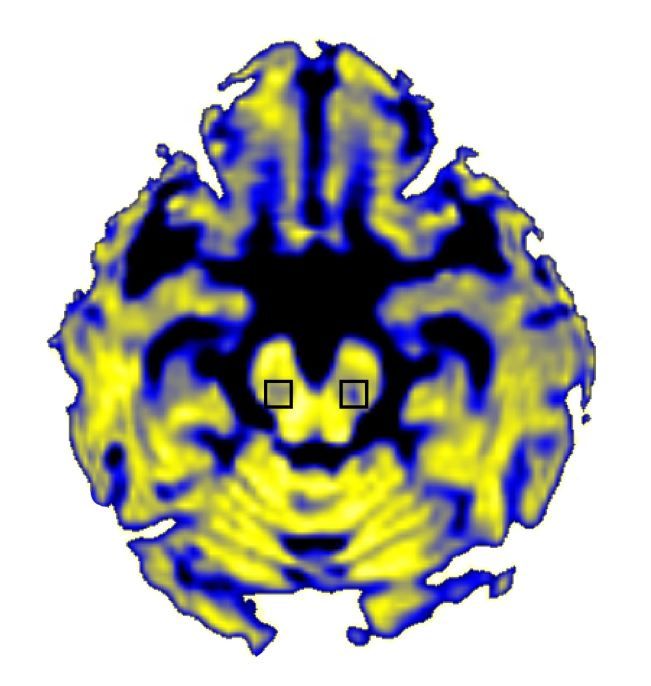
Cognitive decline not seen with lower BP treatment targets
Tighter blood pressure control is not linked to cognitive decline among older adults and may instead be associated with preservation of cognitive function, according to a new analysis.
Further, the cognitive benefits of tighter control are even more pronounced among black patients.
Dr. Hajjar and colleagues report that subjects whose systolic blood pressure (SBP) was maintained at 150 mm Hg or higher during the study period saw significantly greater cognitive decline over 10 years, compared with those treated to levels of 120 mm Hg or lower (JAMA Neurol. 2017 Aug 21; doi: 10.1001/jamaneurol.2017.1863). Furthermore, the investigators noted a differential decrease by blood pressure levels for both cognitive scoring systems, with the greatest decline seen in the group with SBP of 150 mm/Hg or higher and the lowest decrease in the group with 120 mm/Hg or lower (P less than .001 for both).
Black patients saw a greater difference, compared with white patients, between the higher and lower SBP levels in the decrease in cognition. Adjusted differences between the group with 150 mm Hg or higher and those with 120 mm Hg or lower were –0.05 in white patients and –0.08 in black patients for the 3MSE test (P = .03), and –0.07 in white patients and –0.13 in black patients for the DSST (P = .05).
“Almost all guidelines have recommended that target blood pressures be similar for black and white patients,” the investigators wrote in their analysis, adding that “future recommendations for the management of hypertension and cognitive outcomes need to take this racial disparity into consideration.”
The study was funded by the National Institutes on Health and National Institute on Aging. Dr. Hajjar and his colleagues disclosed no conflicts of interest.
Although unanswered questions remain, the data presented by Dr. Hajjar and colleagues add to the existing literature by emphasizing that tight blood pressure control does not appear to lead to poorer cognitive trajectories in older adults and may even be associated with improved cognitive trajectories. An important and unique feature of the data is the diverse population included, with nearly half of the enrollment composed of black individuals. The finding that lower systolic BP was especially protective for black individuals is important, given a noted disparity in rates of dementia among black and white persons. Adding to that the finding that hypertension is more common and more severe in black than in white persons (also supported by the data in this study), and that black persons tend to have more poorly controlled hypertension than do white persons, this outcome points to an important opportunity from a public health standpoint. BP reduction might actually reduce the rates of dementia and reduce the disparities by race with regard to dementia rates; the fact that BP control may require more medications for black than for white patients needs to be considered when monitoring blood pressure levels.
Rebecca F. Gottesman, MD, PhD, of Johns Hopkins University, Baltimore, made these comments in an accompanying editorial (JAMA Neurol. 2017 Aug. 21; doi: 10.1001/jamaneurol.2017.1869). She is an associate editor at JAMA Neurology, and reports no other conflicts of interest.
Although unanswered questions remain, the data presented by Dr. Hajjar and colleagues add to the existing literature by emphasizing that tight blood pressure control does not appear to lead to poorer cognitive trajectories in older adults and may even be associated with improved cognitive trajectories. An important and unique feature of the data is the diverse population included, with nearly half of the enrollment composed of black individuals. The finding that lower systolic BP was especially protective for black individuals is important, given a noted disparity in rates of dementia among black and white persons. Adding to that the finding that hypertension is more common and more severe in black than in white persons (also supported by the data in this study), and that black persons tend to have more poorly controlled hypertension than do white persons, this outcome points to an important opportunity from a public health standpoint. BP reduction might actually reduce the rates of dementia and reduce the disparities by race with regard to dementia rates; the fact that BP control may require more medications for black than for white patients needs to be considered when monitoring blood pressure levels.
Rebecca F. Gottesman, MD, PhD, of Johns Hopkins University, Baltimore, made these comments in an accompanying editorial (JAMA Neurol. 2017 Aug. 21; doi: 10.1001/jamaneurol.2017.1869). She is an associate editor at JAMA Neurology, and reports no other conflicts of interest.
Although unanswered questions remain, the data presented by Dr. Hajjar and colleagues add to the existing literature by emphasizing that tight blood pressure control does not appear to lead to poorer cognitive trajectories in older adults and may even be associated with improved cognitive trajectories. An important and unique feature of the data is the diverse population included, with nearly half of the enrollment composed of black individuals. The finding that lower systolic BP was especially protective for black individuals is important, given a noted disparity in rates of dementia among black and white persons. Adding to that the finding that hypertension is more common and more severe in black than in white persons (also supported by the data in this study), and that black persons tend to have more poorly controlled hypertension than do white persons, this outcome points to an important opportunity from a public health standpoint. BP reduction might actually reduce the rates of dementia and reduce the disparities by race with regard to dementia rates; the fact that BP control may require more medications for black than for white patients needs to be considered when monitoring blood pressure levels.
Rebecca F. Gottesman, MD, PhD, of Johns Hopkins University, Baltimore, made these comments in an accompanying editorial (JAMA Neurol. 2017 Aug. 21; doi: 10.1001/jamaneurol.2017.1869). She is an associate editor at JAMA Neurology, and reports no other conflicts of interest.
Tighter blood pressure control is not linked to cognitive decline among older adults and may instead be associated with preservation of cognitive function, according to a new analysis.
Further, the cognitive benefits of tighter control are even more pronounced among black patients.
Dr. Hajjar and colleagues report that subjects whose systolic blood pressure (SBP) was maintained at 150 mm Hg or higher during the study period saw significantly greater cognitive decline over 10 years, compared with those treated to levels of 120 mm Hg or lower (JAMA Neurol. 2017 Aug 21; doi: 10.1001/jamaneurol.2017.1863). Furthermore, the investigators noted a differential decrease by blood pressure levels for both cognitive scoring systems, with the greatest decline seen in the group with SBP of 150 mm/Hg or higher and the lowest decrease in the group with 120 mm/Hg or lower (P less than .001 for both).
Black patients saw a greater difference, compared with white patients, between the higher and lower SBP levels in the decrease in cognition. Adjusted differences between the group with 150 mm Hg or higher and those with 120 mm Hg or lower were –0.05 in white patients and –0.08 in black patients for the 3MSE test (P = .03), and –0.07 in white patients and –0.13 in black patients for the DSST (P = .05).
“Almost all guidelines have recommended that target blood pressures be similar for black and white patients,” the investigators wrote in their analysis, adding that “future recommendations for the management of hypertension and cognitive outcomes need to take this racial disparity into consideration.”
The study was funded by the National Institutes on Health and National Institute on Aging. Dr. Hajjar and his colleagues disclosed no conflicts of interest.
Tighter blood pressure control is not linked to cognitive decline among older adults and may instead be associated with preservation of cognitive function, according to a new analysis.
Further, the cognitive benefits of tighter control are even more pronounced among black patients.
Dr. Hajjar and colleagues report that subjects whose systolic blood pressure (SBP) was maintained at 150 mm Hg or higher during the study period saw significantly greater cognitive decline over 10 years, compared with those treated to levels of 120 mm Hg or lower (JAMA Neurol. 2017 Aug 21; doi: 10.1001/jamaneurol.2017.1863). Furthermore, the investigators noted a differential decrease by blood pressure levels for both cognitive scoring systems, with the greatest decline seen in the group with SBP of 150 mm/Hg or higher and the lowest decrease in the group with 120 mm/Hg or lower (P less than .001 for both).
Black patients saw a greater difference, compared with white patients, between the higher and lower SBP levels in the decrease in cognition. Adjusted differences between the group with 150 mm Hg or higher and those with 120 mm Hg or lower were –0.05 in white patients and –0.08 in black patients for the 3MSE test (P = .03), and –0.07 in white patients and –0.13 in black patients for the DSST (P = .05).
“Almost all guidelines have recommended that target blood pressures be similar for black and white patients,” the investigators wrote in their analysis, adding that “future recommendations for the management of hypertension and cognitive outcomes need to take this racial disparity into consideration.”
The study was funded by the National Institutes on Health and National Institute on Aging. Dr. Hajjar and his colleagues disclosed no conflicts of interest.
FROM JAMA NEUROLOGY
Key clinical point: Treating to more aggressive blood pressure targets does not promote cognitive decline and may help stem it, particularly among black patients.
Major finding: Black patients saw significantly greater decline in cognition over time associated with systolic BP control to 150 mm Hg vs. 120 mm Hg.
Data source: A cohort of 1,700 hypertension-treated patients aged 70-79, about half of them black, drawn from a 10-year observational study of 3,000 patients.
Disclosures: Both the larger cohort and this study were funded by the National Institutes of Health and the National Institute on Aging. None of the investigators declared conflicts of interest.
Air pollution seen acting on stress hormones
Increases in stress hormone levels and other adverse metabolic changes accompany higher exposure to air pollution, Chinese researchers have found, while cutting indoor pollution levels appears to mitigate these effects.
Air pollution has been linked in epidemiological studies to increased risk of cardiovascular and metabolic diseases, but the mechanisms remain poorly understood. The new findings, published online Aug. 14 in Circulation, offer compelling evidence that air pollution may impact the central nervous system, and the hypothalamus-pituitary-adrenal axis especially (Circulation 2017 Aug 14;136:618-27).
The study design required that students spend as much time in their dorms as possible with the windows closed, though they could venture out for classes and exams. Fine particle concentration in the dorms treated by purifiers was 8.6 mcg per cubic meter during the study period, compared with a mean 101.4 outdoors. The researchers determined that the time-weighted average student exposure to fine particle pollutants was reduced by more than half when the dorm air was being purified, though average student exposure was estimated at 24 mcg per cubic meter at best. The World Health Organization considers levels below 10 mcg to be safe.
Students in untreated dorms had significant increases in cortisol, cortisone, epinephrine, norepinephrine, and biomarkers of oxidative stress at 9 days compared to those in treated ones. Glucose, insulin, measures of insulin resistance, amino acids, fatty acids, and lipids differed significantly between treatment assignments, and the untreated dorm groups also saw 2.61% higher systolic blood pressure (95% confidence interval [CI], 0.39-4.79).
Glucocorticoids are known to affect blood pressure, the investigators noted. Serum cortisol and cortisone levels were 1.3 and 1.2 times higher for the students in the sham-treated dorms, with each 10-mcg increase in pollutant exposure associated with a 7.8% increase in cortisol (95% CI, 4.75-10.91) and a nearly 3.8% increase in cortisone (95% CI, 1.84-5.71). Similar exposure-dependent increases were seen for norepinephrine, melatonin, phenylalanine, tyrosine, L-tryptophan and other compounds.
“To the best of our knowledge, this is the first study that used the untargeted metabolomics approach to investigate human global metabolic changes in relation to changes in ambient [air pollution] exposures,” the investigators wrote in their analysis, adding that the findings “provide insights into the potential mechanisms of the adverse health effects that have been found to be associated with [pollution] exposure.”
Mr. Li and Dr. Cai recommended the use of indoor air purification technology as a practical way to reduce harmful exposure, noting that the benefits of long-term use, particularly relating to cardiovascular and metabolic health, remain to be established.
The study was funded with grants from national and regional government agencies in China, and none of its authors declared conflicts of interest.
Although the past decade has seen much advancement in our knowledge of how air pollutants promote cardiovascular diseases, important questions remain.
There is a need to better understand the precise nature and systemic pathways whereby ambient air pollution elicits a multitude of adverse responses in the heart and vasculature anatomically remote from the site of inhalation. Also, what can (and should) an individual do to protect oneself against the hazards of air pollution, given that substantial improvements in air quality throughout many parts of the world are likely decades away?
Li and colleagues have provided some significant insights into both of these issues. Responses to short-term exposure to high levels of pollution include increased blood pressure and insulin resistance, along with alterations in a battery of circulating markers indicative of systemic inflammation, oxidative stress, and platelet activation.
A distinguishing feature of their work is the detailed exploration of health responses using state-of-the-art metabolomic profiling. Although similar outcomes after brief exposure to ozone have been shown, this was the first usage of an untargeted metabolomic approach to evaluate the impact of ambient air pollution. The results confirm and extend the growing body of evidence that air pollution elicits systemic perturbations favoring the development of the metabolic syndrome. The findings also add to the growing body of evidence that simple interventions such as air purifier systems with high-efficiency filters can help protect against adverse health impacts of air pollution. The reduction in estimated exposure afforded by filtration favorably influenced most of the health outcomes (blood pressure, insulin resistance, oxidative stress, inflammation), curtailed pollution-induced activation of the sympathetic nervous system and hypothalamic-pituitary-adrenal axis, and helped mitigate the ensuing metabolomic perturbations.
Robert D Brook, MD, of the University of Michigan in Ann Arbor, and Sanjay Rajagopalan, MD, of Cleveland Hospitals, made these comments in an editorial (Circulation. 2017 Aug 14;136:628-31). Dr. Brook receives research support from RB, Inc. Dr. Rajagopalan had no disclosures.
Although the past decade has seen much advancement in our knowledge of how air pollutants promote cardiovascular diseases, important questions remain.
There is a need to better understand the precise nature and systemic pathways whereby ambient air pollution elicits a multitude of adverse responses in the heart and vasculature anatomically remote from the site of inhalation. Also, what can (and should) an individual do to protect oneself against the hazards of air pollution, given that substantial improvements in air quality throughout many parts of the world are likely decades away?
Li and colleagues have provided some significant insights into both of these issues. Responses to short-term exposure to high levels of pollution include increased blood pressure and insulin resistance, along with alterations in a battery of circulating markers indicative of systemic inflammation, oxidative stress, and platelet activation.
A distinguishing feature of their work is the detailed exploration of health responses using state-of-the-art metabolomic profiling. Although similar outcomes after brief exposure to ozone have been shown, this was the first usage of an untargeted metabolomic approach to evaluate the impact of ambient air pollution. The results confirm and extend the growing body of evidence that air pollution elicits systemic perturbations favoring the development of the metabolic syndrome. The findings also add to the growing body of evidence that simple interventions such as air purifier systems with high-efficiency filters can help protect against adverse health impacts of air pollution. The reduction in estimated exposure afforded by filtration favorably influenced most of the health outcomes (blood pressure, insulin resistance, oxidative stress, inflammation), curtailed pollution-induced activation of the sympathetic nervous system and hypothalamic-pituitary-adrenal axis, and helped mitigate the ensuing metabolomic perturbations.
Robert D Brook, MD, of the University of Michigan in Ann Arbor, and Sanjay Rajagopalan, MD, of Cleveland Hospitals, made these comments in an editorial (Circulation. 2017 Aug 14;136:628-31). Dr. Brook receives research support from RB, Inc. Dr. Rajagopalan had no disclosures.
Although the past decade has seen much advancement in our knowledge of how air pollutants promote cardiovascular diseases, important questions remain.
There is a need to better understand the precise nature and systemic pathways whereby ambient air pollution elicits a multitude of adverse responses in the heart and vasculature anatomically remote from the site of inhalation. Also, what can (and should) an individual do to protect oneself against the hazards of air pollution, given that substantial improvements in air quality throughout many parts of the world are likely decades away?
Li and colleagues have provided some significant insights into both of these issues. Responses to short-term exposure to high levels of pollution include increased blood pressure and insulin resistance, along with alterations in a battery of circulating markers indicative of systemic inflammation, oxidative stress, and platelet activation.
A distinguishing feature of their work is the detailed exploration of health responses using state-of-the-art metabolomic profiling. Although similar outcomes after brief exposure to ozone have been shown, this was the first usage of an untargeted metabolomic approach to evaluate the impact of ambient air pollution. The results confirm and extend the growing body of evidence that air pollution elicits systemic perturbations favoring the development of the metabolic syndrome. The findings also add to the growing body of evidence that simple interventions such as air purifier systems with high-efficiency filters can help protect against adverse health impacts of air pollution. The reduction in estimated exposure afforded by filtration favorably influenced most of the health outcomes (blood pressure, insulin resistance, oxidative stress, inflammation), curtailed pollution-induced activation of the sympathetic nervous system and hypothalamic-pituitary-adrenal axis, and helped mitigate the ensuing metabolomic perturbations.
Robert D Brook, MD, of the University of Michigan in Ann Arbor, and Sanjay Rajagopalan, MD, of Cleveland Hospitals, made these comments in an editorial (Circulation. 2017 Aug 14;136:628-31). Dr. Brook receives research support from RB, Inc. Dr. Rajagopalan had no disclosures.
Increases in stress hormone levels and other adverse metabolic changes accompany higher exposure to air pollution, Chinese researchers have found, while cutting indoor pollution levels appears to mitigate these effects.
Air pollution has been linked in epidemiological studies to increased risk of cardiovascular and metabolic diseases, but the mechanisms remain poorly understood. The new findings, published online Aug. 14 in Circulation, offer compelling evidence that air pollution may impact the central nervous system, and the hypothalamus-pituitary-adrenal axis especially (Circulation 2017 Aug 14;136:618-27).
The study design required that students spend as much time in their dorms as possible with the windows closed, though they could venture out for classes and exams. Fine particle concentration in the dorms treated by purifiers was 8.6 mcg per cubic meter during the study period, compared with a mean 101.4 outdoors. The researchers determined that the time-weighted average student exposure to fine particle pollutants was reduced by more than half when the dorm air was being purified, though average student exposure was estimated at 24 mcg per cubic meter at best. The World Health Organization considers levels below 10 mcg to be safe.
Students in untreated dorms had significant increases in cortisol, cortisone, epinephrine, norepinephrine, and biomarkers of oxidative stress at 9 days compared to those in treated ones. Glucose, insulin, measures of insulin resistance, amino acids, fatty acids, and lipids differed significantly between treatment assignments, and the untreated dorm groups also saw 2.61% higher systolic blood pressure (95% confidence interval [CI], 0.39-4.79).
Glucocorticoids are known to affect blood pressure, the investigators noted. Serum cortisol and cortisone levels were 1.3 and 1.2 times higher for the students in the sham-treated dorms, with each 10-mcg increase in pollutant exposure associated with a 7.8% increase in cortisol (95% CI, 4.75-10.91) and a nearly 3.8% increase in cortisone (95% CI, 1.84-5.71). Similar exposure-dependent increases were seen for norepinephrine, melatonin, phenylalanine, tyrosine, L-tryptophan and other compounds.
“To the best of our knowledge, this is the first study that used the untargeted metabolomics approach to investigate human global metabolic changes in relation to changes in ambient [air pollution] exposures,” the investigators wrote in their analysis, adding that the findings “provide insights into the potential mechanisms of the adverse health effects that have been found to be associated with [pollution] exposure.”
Mr. Li and Dr. Cai recommended the use of indoor air purification technology as a practical way to reduce harmful exposure, noting that the benefits of long-term use, particularly relating to cardiovascular and metabolic health, remain to be established.
The study was funded with grants from national and regional government agencies in China, and none of its authors declared conflicts of interest.
Increases in stress hormone levels and other adverse metabolic changes accompany higher exposure to air pollution, Chinese researchers have found, while cutting indoor pollution levels appears to mitigate these effects.
Air pollution has been linked in epidemiological studies to increased risk of cardiovascular and metabolic diseases, but the mechanisms remain poorly understood. The new findings, published online Aug. 14 in Circulation, offer compelling evidence that air pollution may impact the central nervous system, and the hypothalamus-pituitary-adrenal axis especially (Circulation 2017 Aug 14;136:618-27).
The study design required that students spend as much time in their dorms as possible with the windows closed, though they could venture out for classes and exams. Fine particle concentration in the dorms treated by purifiers was 8.6 mcg per cubic meter during the study period, compared with a mean 101.4 outdoors. The researchers determined that the time-weighted average student exposure to fine particle pollutants was reduced by more than half when the dorm air was being purified, though average student exposure was estimated at 24 mcg per cubic meter at best. The World Health Organization considers levels below 10 mcg to be safe.
Students in untreated dorms had significant increases in cortisol, cortisone, epinephrine, norepinephrine, and biomarkers of oxidative stress at 9 days compared to those in treated ones. Glucose, insulin, measures of insulin resistance, amino acids, fatty acids, and lipids differed significantly between treatment assignments, and the untreated dorm groups also saw 2.61% higher systolic blood pressure (95% confidence interval [CI], 0.39-4.79).
Glucocorticoids are known to affect blood pressure, the investigators noted. Serum cortisol and cortisone levels were 1.3 and 1.2 times higher for the students in the sham-treated dorms, with each 10-mcg increase in pollutant exposure associated with a 7.8% increase in cortisol (95% CI, 4.75-10.91) and a nearly 3.8% increase in cortisone (95% CI, 1.84-5.71). Similar exposure-dependent increases were seen for norepinephrine, melatonin, phenylalanine, tyrosine, L-tryptophan and other compounds.
“To the best of our knowledge, this is the first study that used the untargeted metabolomics approach to investigate human global metabolic changes in relation to changes in ambient [air pollution] exposures,” the investigators wrote in their analysis, adding that the findings “provide insights into the potential mechanisms of the adverse health effects that have been found to be associated with [pollution] exposure.”
Mr. Li and Dr. Cai recommended the use of indoor air purification technology as a practical way to reduce harmful exposure, noting that the benefits of long-term use, particularly relating to cardiovascular and metabolic health, remain to be established.
The study was funded with grants from national and regional government agencies in China, and none of its authors declared conflicts of interest.
FROM CIRCULATION
Key clinical point: Air pollution exposure is associated with increases in stress hormones and a wide array of other biochemical changes.
Major finding: Increases in pollution exposure corresponded to increases in cortisol, cortisone, epinephrine, and norepinephrine.
Data source: A randomized, double-blinded crossover trial on 55 subjects in Shanghai, China.
Disclosures: Chinese national and regional governments supported the study, whose authors declared no conflicts of interest.
APAP improves aerophagia symptoms
Switching continuous positive airway pressure–treated patients to autotitrating positive airway pressure (APAP) systems resulted in reduced severity of patient-reported aerophagia symptoms, according to results from a double-blind, randomized study.
Aerophagia, the swallowing of air leading to gastrointestinal distress, is a frequently reported adverse effect among people treated for obstructive sleep apnea with continuous positive airway pressure (CPAP).
The APAP-treated group saw significantly reduced median therapeutic pressure levels compared with the CPAP-treated patients (9.8 vs. 14.0 cm H2O, P less than .001) and slight but statistically significant reductions in self-reported symptoms of bloating, flatulence, and belching. No significant difference was seen in compliance with therapy between the two treatment groups in this study, published in the August 2017 issue of Journal of Clinical Sleep Medicine (J Clin Sleep Med. 2017;13[7]:881-8).
For their research, Teresa Shirlaw and her colleagues in the sleep clinic at Princess Alexandra Hospital in Woolloongabba, Queensland, Australia, analyzed results from 56 adult patients with sleep apnea who had been recently treated with CPAP and reported bloating, flatulence, or belching following therapy.
Patients were randomized 1:1 to in-clinic nighttime CPAP or APAP for 2 weeks and blinded to treatment assignment, while investigators recorded therapy usage hours, pressure, leak, and residual apnea-hypopnea index across the study period. Most of the subjects (n = 39) used full face masks, while others used nasal-only systems.
The researchers considered differences in PAP therapy usage of at least 30 minutes per night to be statistically significant. The APAP group used the assigned therapy a mean 7 hours per night, vs. 6.8 for the CPAP group. Daytime sleepiness outcomes were also similar for the two treatment groups.
Ms. Shirlaw and her colleagues described the compliance findings as a surprise, noting that an earlier meta-analysis had shown slight improvements in compliance associated with APAP (Syst Rev. 2012;1[1]:20). In clinical practice, patients complaining of aerophagia associated with CPAP are frequently switched to APAP based on the belief that doing so “will lead to improved therapy acceptance and … improved compliance,” they wrote.
The investigators described the self-reporting of aerophagia symptoms as one of the study’s limitations. They surmised that the lack of difference seen for compliance measures might be explained in part by the 30-minute usage increments in the study design (compared with 10-minute increments used in some other studies), and the fact that the cohort had relatively high compliance with CPAP at baseline (5.5 hours/night), suggesting a motivated patient population at entry.
The study received some funding from the government of Queensland, and the authors disclosed no conflicts of interest related to their findings.
Switching continuous positive airway pressure–treated patients to autotitrating positive airway pressure (APAP) systems resulted in reduced severity of patient-reported aerophagia symptoms, according to results from a double-blind, randomized study.
Aerophagia, the swallowing of air leading to gastrointestinal distress, is a frequently reported adverse effect among people treated for obstructive sleep apnea with continuous positive airway pressure (CPAP).
The APAP-treated group saw significantly reduced median therapeutic pressure levels compared with the CPAP-treated patients (9.8 vs. 14.0 cm H2O, P less than .001) and slight but statistically significant reductions in self-reported symptoms of bloating, flatulence, and belching. No significant difference was seen in compliance with therapy between the two treatment groups in this study, published in the August 2017 issue of Journal of Clinical Sleep Medicine (J Clin Sleep Med. 2017;13[7]:881-8).
For their research, Teresa Shirlaw and her colleagues in the sleep clinic at Princess Alexandra Hospital in Woolloongabba, Queensland, Australia, analyzed results from 56 adult patients with sleep apnea who had been recently treated with CPAP and reported bloating, flatulence, or belching following therapy.
Patients were randomized 1:1 to in-clinic nighttime CPAP or APAP for 2 weeks and blinded to treatment assignment, while investigators recorded therapy usage hours, pressure, leak, and residual apnea-hypopnea index across the study period. Most of the subjects (n = 39) used full face masks, while others used nasal-only systems.
The researchers considered differences in PAP therapy usage of at least 30 minutes per night to be statistically significant. The APAP group used the assigned therapy a mean 7 hours per night, vs. 6.8 for the CPAP group. Daytime sleepiness outcomes were also similar for the two treatment groups.
Ms. Shirlaw and her colleagues described the compliance findings as a surprise, noting that an earlier meta-analysis had shown slight improvements in compliance associated with APAP (Syst Rev. 2012;1[1]:20). In clinical practice, patients complaining of aerophagia associated with CPAP are frequently switched to APAP based on the belief that doing so “will lead to improved therapy acceptance and … improved compliance,” they wrote.
The investigators described the self-reporting of aerophagia symptoms as one of the study’s limitations. They surmised that the lack of difference seen for compliance measures might be explained in part by the 30-minute usage increments in the study design (compared with 10-minute increments used in some other studies), and the fact that the cohort had relatively high compliance with CPAP at baseline (5.5 hours/night), suggesting a motivated patient population at entry.
The study received some funding from the government of Queensland, and the authors disclosed no conflicts of interest related to their findings.
Switching continuous positive airway pressure–treated patients to autotitrating positive airway pressure (APAP) systems resulted in reduced severity of patient-reported aerophagia symptoms, according to results from a double-blind, randomized study.
Aerophagia, the swallowing of air leading to gastrointestinal distress, is a frequently reported adverse effect among people treated for obstructive sleep apnea with continuous positive airway pressure (CPAP).
The APAP-treated group saw significantly reduced median therapeutic pressure levels compared with the CPAP-treated patients (9.8 vs. 14.0 cm H2O, P less than .001) and slight but statistically significant reductions in self-reported symptoms of bloating, flatulence, and belching. No significant difference was seen in compliance with therapy between the two treatment groups in this study, published in the August 2017 issue of Journal of Clinical Sleep Medicine (J Clin Sleep Med. 2017;13[7]:881-8).
For their research, Teresa Shirlaw and her colleagues in the sleep clinic at Princess Alexandra Hospital in Woolloongabba, Queensland, Australia, analyzed results from 56 adult patients with sleep apnea who had been recently treated with CPAP and reported bloating, flatulence, or belching following therapy.
Patients were randomized 1:1 to in-clinic nighttime CPAP or APAP for 2 weeks and blinded to treatment assignment, while investigators recorded therapy usage hours, pressure, leak, and residual apnea-hypopnea index across the study period. Most of the subjects (n = 39) used full face masks, while others used nasal-only systems.
The researchers considered differences in PAP therapy usage of at least 30 minutes per night to be statistically significant. The APAP group used the assigned therapy a mean 7 hours per night, vs. 6.8 for the CPAP group. Daytime sleepiness outcomes were also similar for the two treatment groups.
Ms. Shirlaw and her colleagues described the compliance findings as a surprise, noting that an earlier meta-analysis had shown slight improvements in compliance associated with APAP (Syst Rev. 2012;1[1]:20). In clinical practice, patients complaining of aerophagia associated with CPAP are frequently switched to APAP based on the belief that doing so “will lead to improved therapy acceptance and … improved compliance,” they wrote.
The investigators described the self-reporting of aerophagia symptoms as one of the study’s limitations. They surmised that the lack of difference seen for compliance measures might be explained in part by the 30-minute usage increments in the study design (compared with 10-minute increments used in some other studies), and the fact that the cohort had relatively high compliance with CPAP at baseline (5.5 hours/night), suggesting a motivated patient population at entry.
The study received some funding from the government of Queensland, and the authors disclosed no conflicts of interest related to their findings.
FROM THE JOURNAL OF CLINICAL SLEEP MEDICINE
Key clinical point: Sleep apnea patients complaining of aerophagia associated with continuous positive airway pressure may find relief using autotitrating positive airway pressure.
Major finding: The APAP-treated group saw significantly reduced median therapeutic pressure levels compared with the CPAP-treated patients (9.8 vs. 14.0 cm H2O, P less than .001) and slight but statistically significant reductions in self-reported symptoms of bloating, flatulence, and belching.
Data source: A randomized, double-blinded trial of 56 adult sleep apnea patients, with previous CPAP and aerophagia, treated at a hospital sleep clinic in Australia.
Disclosures: The government of Queensland helped fund the study. The authors disclosed no conflicts of interest.
Eye disease affects 1 in 5 adults with severe atopic dermatitis
Results of a large cohort study in Denmark found that adults with atopic dermatitis (AD) were significantly more likely to be affected by certain ocular conditions, compared with those who did not have AD.
“Keratitis, conjunctivitis, and keratoconus as well as cataracts in patients younger than 50 years occurred more frequently in patients with AD and in a disease severity–dependent manner,” concluded the authors, who wrote that as far as they know, this is the largest study conducted to date of ocular disorders in adults with AD.
The investigators also found an elevated risk of a keratitis diagnosis among patients with mild AD (hazard ratio, 1.66; 95% confidence interval, 1.15-2.40) and those with severe AD (HR, 3.17; 95% CI, 2.31-4.35). Severe AD was associated with an elevated risk of keratoconus (HR, 10.01; 95% CI, 5.02-19.96),
Cataracts and glaucoma were not more common among those with AD overall. However, cataracts were increased among those under age 50 years with mild and severe AD, which were significant associations for both, but not among those over age 50 with AD. There were no differences for glaucoma risk associated with AD by age.
The investigators acknowledged that the study could not capture the reasons why anti-inflammatory ocular medicines were prescribed and that such medicines could have been prescribed for conditions other than the ocular conditions.
Capturing the risk of ocular diseases in AD is important, they wrote. They referred to “emerging concern” about the incidence of conjunctivitis with “near-future” biologic treatments for AD and the potential for long-term consequences. They referred to adverse event data from randomized clinical trials of dupilumab, an interleukin-4 receptor–alpha antagonist, approved by the Food and Drug Administration in March 2017 for treatment of moderate to severe AD, which included more cases of conjunctivitis among those treated with the biologic, compared with those on placebo (N Engl J Med. 2016 Dec 15;375:2335-48). A “weak trend” for more cases of conjunctivitis was also reported among treated patients with an IL-13 inhibitor, lebrikizumab, in a phase 2 study of adults with AD, they wrote.
Treatments targeting IL-4 receptor–alpha have been shown to result in increased blood eosinophil counts, and “these elevations might have clinical effects,” Dr. Thyssen and his colleagues wrote, adding: “Notably, eosinophils are pathognomonic for allergic eye disease.”
Dr. Thyssen disclosed funding from the Lundbeck Foundation and honoraria from Roche, Sanofi Genzyme, and LEO Pharma. Three other authors on the study reported research funding and/or honoraria from pharmaceutical firms.
Results of a large cohort study in Denmark found that adults with atopic dermatitis (AD) were significantly more likely to be affected by certain ocular conditions, compared with those who did not have AD.
“Keratitis, conjunctivitis, and keratoconus as well as cataracts in patients younger than 50 years occurred more frequently in patients with AD and in a disease severity–dependent manner,” concluded the authors, who wrote that as far as they know, this is the largest study conducted to date of ocular disorders in adults with AD.
The investigators also found an elevated risk of a keratitis diagnosis among patients with mild AD (hazard ratio, 1.66; 95% confidence interval, 1.15-2.40) and those with severe AD (HR, 3.17; 95% CI, 2.31-4.35). Severe AD was associated with an elevated risk of keratoconus (HR, 10.01; 95% CI, 5.02-19.96),
Cataracts and glaucoma were not more common among those with AD overall. However, cataracts were increased among those under age 50 years with mild and severe AD, which were significant associations for both, but not among those over age 50 with AD. There were no differences for glaucoma risk associated with AD by age.
The investigators acknowledged that the study could not capture the reasons why anti-inflammatory ocular medicines were prescribed and that such medicines could have been prescribed for conditions other than the ocular conditions.
Capturing the risk of ocular diseases in AD is important, they wrote. They referred to “emerging concern” about the incidence of conjunctivitis with “near-future” biologic treatments for AD and the potential for long-term consequences. They referred to adverse event data from randomized clinical trials of dupilumab, an interleukin-4 receptor–alpha antagonist, approved by the Food and Drug Administration in March 2017 for treatment of moderate to severe AD, which included more cases of conjunctivitis among those treated with the biologic, compared with those on placebo (N Engl J Med. 2016 Dec 15;375:2335-48). A “weak trend” for more cases of conjunctivitis was also reported among treated patients with an IL-13 inhibitor, lebrikizumab, in a phase 2 study of adults with AD, they wrote.
Treatments targeting IL-4 receptor–alpha have been shown to result in increased blood eosinophil counts, and “these elevations might have clinical effects,” Dr. Thyssen and his colleagues wrote, adding: “Notably, eosinophils are pathognomonic for allergic eye disease.”
Dr. Thyssen disclosed funding from the Lundbeck Foundation and honoraria from Roche, Sanofi Genzyme, and LEO Pharma. Three other authors on the study reported research funding and/or honoraria from pharmaceutical firms.
Results of a large cohort study in Denmark found that adults with atopic dermatitis (AD) were significantly more likely to be affected by certain ocular conditions, compared with those who did not have AD.
“Keratitis, conjunctivitis, and keratoconus as well as cataracts in patients younger than 50 years occurred more frequently in patients with AD and in a disease severity–dependent manner,” concluded the authors, who wrote that as far as they know, this is the largest study conducted to date of ocular disorders in adults with AD.
The investigators also found an elevated risk of a keratitis diagnosis among patients with mild AD (hazard ratio, 1.66; 95% confidence interval, 1.15-2.40) and those with severe AD (HR, 3.17; 95% CI, 2.31-4.35). Severe AD was associated with an elevated risk of keratoconus (HR, 10.01; 95% CI, 5.02-19.96),
Cataracts and glaucoma were not more common among those with AD overall. However, cataracts were increased among those under age 50 years with mild and severe AD, which were significant associations for both, but not among those over age 50 with AD. There were no differences for glaucoma risk associated with AD by age.
The investigators acknowledged that the study could not capture the reasons why anti-inflammatory ocular medicines were prescribed and that such medicines could have been prescribed for conditions other than the ocular conditions.
Capturing the risk of ocular diseases in AD is important, they wrote. They referred to “emerging concern” about the incidence of conjunctivitis with “near-future” biologic treatments for AD and the potential for long-term consequences. They referred to adverse event data from randomized clinical trials of dupilumab, an interleukin-4 receptor–alpha antagonist, approved by the Food and Drug Administration in March 2017 for treatment of moderate to severe AD, which included more cases of conjunctivitis among those treated with the biologic, compared with those on placebo (N Engl J Med. 2016 Dec 15;375:2335-48). A “weak trend” for more cases of conjunctivitis was also reported among treated patients with an IL-13 inhibitor, lebrikizumab, in a phase 2 study of adults with AD, they wrote.
Treatments targeting IL-4 receptor–alpha have been shown to result in increased blood eosinophil counts, and “these elevations might have clinical effects,” Dr. Thyssen and his colleagues wrote, adding: “Notably, eosinophils are pathognomonic for allergic eye disease.”
Dr. Thyssen disclosed funding from the Lundbeck Foundation and honoraria from Roche, Sanofi Genzyme, and LEO Pharma. Three other authors on the study reported research funding and/or honoraria from pharmaceutical firms.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point: Conjunctivitis, keratitis, and keratoconus are common in patients with atopic dermatitis, compared with the general population
Major finding: 19% of adults with severe AD received a prescription for an anti-inflammatory eye medication, compared with 4.5% of the general population.
Data source: Epidemiologic data from more than 4 million patients in Danish health care and prescription registries.
Disclosures: Four investigators disclosed outside grant funding and/or financial relationships with pharmaceutical manufacturers.
Acute otitis media: Which children to treat
Children whose ear infections involve severe bulging of the eardrum are likely to benefit from antibiotic treatment, while children with a peaked tympanogram pattern are likely to recover from the infections without the use of antibiotics, according to results from a new study.
The findings, published online Aug. 8 (Pediatrics. 2017), may help restrict pediatricians’ use of antibiotics to the patients who are most likely to benefit. For their research, Paula A. Tähtinen, MD, PhD, of Turku (Finland) University Hospital, and her colleagues, analyzed results from a previous placebo-controlled trial of 319 children in Finland with acute otitis media. Subjects were aged 6-35 months (median age 14 months; 57% boys; 99% white). The children in the cohort were evenly randomized to treatment with amoxicillin or placebo for 7 days. In the antibiotic arm, about 19% of patients failed to respond to treatment, while about 45% in the placebo arm did.
Dr. Tähtinen and her colleagues noted that in their study, severe bulging was an important prognostic factor irrespective of the number of ears affected or the severity of other common symptoms such as pain or fever. In this study, involvement of both ears and severity of other symptoms such as pain or fever were not seen affecting risk of treatment failure. Though only a minority of children in the study had a peaked tympanogram, failure rates for these were low in both treatment and placebo groups, and the number needed to treat to prevent treatment failure was 1 in 29.
“The evaluation of otoscopic signs is always subjective and prone to interobserver bias,” the researchers wrote. “Severe bulging is, however, a sign that is difficult to miss even for a less experienced otoscopist, and therefore this prognostic factor as an indication for antimicrobial treatment could be easily applied into clinical practice.”
Dr. Tähtinen and her colleagues’ research was supported by grants from the European Society for Pediatric Infectious Diseases and several other foundations. The study authors disclosed no financial conflicts of interest.
Children whose ear infections involve severe bulging of the eardrum are likely to benefit from antibiotic treatment, while children with a peaked tympanogram pattern are likely to recover from the infections without the use of antibiotics, according to results from a new study.
The findings, published online Aug. 8 (Pediatrics. 2017), may help restrict pediatricians’ use of antibiotics to the patients who are most likely to benefit. For their research, Paula A. Tähtinen, MD, PhD, of Turku (Finland) University Hospital, and her colleagues, analyzed results from a previous placebo-controlled trial of 319 children in Finland with acute otitis media. Subjects were aged 6-35 months (median age 14 months; 57% boys; 99% white). The children in the cohort were evenly randomized to treatment with amoxicillin or placebo for 7 days. In the antibiotic arm, about 19% of patients failed to respond to treatment, while about 45% in the placebo arm did.
Dr. Tähtinen and her colleagues noted that in their study, severe bulging was an important prognostic factor irrespective of the number of ears affected or the severity of other common symptoms such as pain or fever. In this study, involvement of both ears and severity of other symptoms such as pain or fever were not seen affecting risk of treatment failure. Though only a minority of children in the study had a peaked tympanogram, failure rates for these were low in both treatment and placebo groups, and the number needed to treat to prevent treatment failure was 1 in 29.
“The evaluation of otoscopic signs is always subjective and prone to interobserver bias,” the researchers wrote. “Severe bulging is, however, a sign that is difficult to miss even for a less experienced otoscopist, and therefore this prognostic factor as an indication for antimicrobial treatment could be easily applied into clinical practice.”
Dr. Tähtinen and her colleagues’ research was supported by grants from the European Society for Pediatric Infectious Diseases and several other foundations. The study authors disclosed no financial conflicts of interest.
Children whose ear infections involve severe bulging of the eardrum are likely to benefit from antibiotic treatment, while children with a peaked tympanogram pattern are likely to recover from the infections without the use of antibiotics, according to results from a new study.
The findings, published online Aug. 8 (Pediatrics. 2017), may help restrict pediatricians’ use of antibiotics to the patients who are most likely to benefit. For their research, Paula A. Tähtinen, MD, PhD, of Turku (Finland) University Hospital, and her colleagues, analyzed results from a previous placebo-controlled trial of 319 children in Finland with acute otitis media. Subjects were aged 6-35 months (median age 14 months; 57% boys; 99% white). The children in the cohort were evenly randomized to treatment with amoxicillin or placebo for 7 days. In the antibiotic arm, about 19% of patients failed to respond to treatment, while about 45% in the placebo arm did.
Dr. Tähtinen and her colleagues noted that in their study, severe bulging was an important prognostic factor irrespective of the number of ears affected or the severity of other common symptoms such as pain or fever. In this study, involvement of both ears and severity of other symptoms such as pain or fever were not seen affecting risk of treatment failure. Though only a minority of children in the study had a peaked tympanogram, failure rates for these were low in both treatment and placebo groups, and the number needed to treat to prevent treatment failure was 1 in 29.
“The evaluation of otoscopic signs is always subjective and prone to interobserver bias,” the researchers wrote. “Severe bulging is, however, a sign that is difficult to miss even for a less experienced otoscopist, and therefore this prognostic factor as an indication for antimicrobial treatment could be easily applied into clinical practice.”
Dr. Tähtinen and her colleagues’ research was supported by grants from the European Society for Pediatric Infectious Diseases and several other foundations. The study authors disclosed no financial conflicts of interest.
FROM PEDIATRICS
Key clinical point: Severe bulging of the eardrum, or a peaked tympanogram pattern, can inform the administration or withholding of antibiotic treatment in AOM.
Major finding: The number needed to treat using antibiotics among children presenting with severe eardrum bulging was 1.9.
Data source: Analysis of results from a randomized, placebo controlled trial (n = 319) of children younger than 3 with AOM conducted in Finland during 2006-2008.
Disclosures: Study authors disclosed research support from several foundations but no commercial conflicts of interest.
Studies support early use of genetic tests in early childhood disorders
Results from two new studies suggest that genetic testing early in the diagnostic pathway may allow for earlier and more precise diagnoses in early-life epilepsies and a range of other childhood-onset disorders, and potentially limit costs associated with a long diagnostic course.
Both papers, published online July 31 in JAMA Pediatrics, showed the diagnostic yield of genetic testing approaches, including whole-exome sequencing (WES), to be high.
The results also argue for the incorporation of genetic testing into the first diagnostic assessments; not limiting it to severe presentations only; and for broad testing methods to be employed in lieu of narrower ones.
Of these patients, just under half (n = 327) underwent various forms of genetic testing at the discretion of the treating physician, including karyotyping, microarrays, epilepsy gene panels, WES, mitochondrial panels, and other tests. Pathogenic variants were discovered in 132 children, or 40% of those receiving genetic testing (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1743).
Of all the genetic testing methods employed in the study, diagnostic yields were significantly greater for epilepsy gene panels (29.2%) and WES (27.8%), compared with chromosome microarray (7.9%).
The results, the investigators said, provide “added impetus to move the diagnosis of the specific cause to the point of initial presentation ... it is time to provide greater emphasis on and support for thorough genetic evaluations, particularly sequencing-based evaluations, for children with newly presenting epilepsies in the first few years of life.”
In addition to aiding management decisions, early genetic testing “ends the diagnostic odyssey during which parents and physicians spend untold amounts of time searching for an explanation for a child’s epilepsy and reduces associated costs,” Dr. Berg and her colleagues concluded.
In a separate study led by Tiong Yang Tan, MBBS, PhD, of Victorian Clinical Genetics Services in Melbourne, Australia, and his colleagues, singleton WES was used in 44 children recruited at outpatient clinics of a Melbourne hospital system (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1755).
Children in the study were aged 2-18 years (with mean age at presentation 28 months) and had a wide variety of suspected genetic disorders, including skeletal, skin, neurometabolic, and intellectual disorders. Some of these had features overlapping several conditions. The children in the cohort had not received prior genetic testing before undergoing WES.
The molecular test resulted in a diagnosis in 52% (n = 23) of the children, including unexpected diagnoses in eight of these. Clinical management was altered as result of sequencing findings in six children.
“Although phenotyping is critical, 35% of children had a diagnosis caused by a gene outside the initially prioritized gene list. This finding not only possibly reflects lack of clinical recognition but also underscores the utility of WES in achieving a diagnosis even when the a priori hypothesis is imprecise,” Dr. Tan and his associates wrote in their analysis.
Dr. Tan and his colleagues conducted a cost analysis that found WES performed at initial tertiary presentation resulted in a cost savings of U.S. $6,838 per additional diagnosis (95% confidence interval, U.S. $3,263-$11,678), compared with the standard diagnostic pathway. The figures reflect costs in an Australian care setting.
The children in the study had a mean diagnostic odyssey of 6 years, including a mean of 19 tests and four clinical genetics and four non–genetics specialist consultations. A quarter of them had undergone at least one diagnostic procedure under general anesthesia.
“The diagnostic odyssey of children suspected of having monogenic disorders is protracted and painful and may not provide a precise diagnosis,” Dr. Tan and his colleagues wrote in their analysis. “This paradigm has markedly shifted with the advent of WES.”
WES is best targeted to children “with genetically heterogeneous disorders or features overlapping several conditions,” the investigators concluded. “Our findings suggest that these children are best served by early recognition by their pediatrician and expedited referral to clinical genetics with WES applied after chromosomal microarray but before an extensive diagnostic process.”
Dr. Tan and his colleagues’ study was funded by the Melbourne Genomics Health Alliance and state and national governments in Australia. None of the authors declared conflicts of interest. Dr. Berg and her colleagues’ study was funded by the Pediatric Epilepsy Research Foundation, and none of its authors disclosed commercial conflicts of interest.
The studies by Tan et al. and Berg et al. demonstrate the dramatic effect of the diagnostic yield of different genetic testing approaches on cost-effectiveness and the potential design of testing strategies in children with suspected monogenic conditions. Both studies emphasize the effect of the results of genetic testing. Whereas Tan et al. showed that, in 26% of cases, the result enabled a specific modification of patient care, Berg et al. also demonstrated that there is no basis for identifying optimal, targeted treatments, when testing is not performed and genetic diagnoses are not made.
However, in the absence of targeted treatments, a genetic diagnosis is of high value for the patients, their families, and treating physicians. A clear diagnosis may not only be of prognostic value but also put an end to a possibly stressful and demanding diagnostic odyssey. It may enable patient care that is explicitly focused on the individual needs of the patient. A clear diagnosis usually also allows a better assessment of the risks of recurrence in the family and possibly enables prenatal testing in relatives. Finally, it enables research and a better scientific understanding of the underlying pathophysiology, which may ideally lead to the identification of novel therapeutic prospects. Seven years ago, an international consensus statement endorsed the replacement of classic cytogenetic karyotype analysis by chromosomal microarrays as a first-tier diagnostic test in individuals with developmental disabilities or congenital anomalies. The studies add to the growing evidence that this consensus may already be outdated, as high-throughput sequencing techniques may achieve even higher diagnostic yields and, thus, are capable to become the new first-tier diagnostic test in congenital and early-onset disorders.
Johannes R. Lemke, MD, is with the Institute of Human Genetics at the University of Leipzig (Germany) Hospitals and Clinics. He reports no conflicts of interest associated with his editorial, which accompanied the JAMA Pediatrics reports (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1743).
The studies by Tan et al. and Berg et al. demonstrate the dramatic effect of the diagnostic yield of different genetic testing approaches on cost-effectiveness and the potential design of testing strategies in children with suspected monogenic conditions. Both studies emphasize the effect of the results of genetic testing. Whereas Tan et al. showed that, in 26% of cases, the result enabled a specific modification of patient care, Berg et al. also demonstrated that there is no basis for identifying optimal, targeted treatments, when testing is not performed and genetic diagnoses are not made.
However, in the absence of targeted treatments, a genetic diagnosis is of high value for the patients, their families, and treating physicians. A clear diagnosis may not only be of prognostic value but also put an end to a possibly stressful and demanding diagnostic odyssey. It may enable patient care that is explicitly focused on the individual needs of the patient. A clear diagnosis usually also allows a better assessment of the risks of recurrence in the family and possibly enables prenatal testing in relatives. Finally, it enables research and a better scientific understanding of the underlying pathophysiology, which may ideally lead to the identification of novel therapeutic prospects. Seven years ago, an international consensus statement endorsed the replacement of classic cytogenetic karyotype analysis by chromosomal microarrays as a first-tier diagnostic test in individuals with developmental disabilities or congenital anomalies. The studies add to the growing evidence that this consensus may already be outdated, as high-throughput sequencing techniques may achieve even higher diagnostic yields and, thus, are capable to become the new first-tier diagnostic test in congenital and early-onset disorders.
Johannes R. Lemke, MD, is with the Institute of Human Genetics at the University of Leipzig (Germany) Hospitals and Clinics. He reports no conflicts of interest associated with his editorial, which accompanied the JAMA Pediatrics reports (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1743).
The studies by Tan et al. and Berg et al. demonstrate the dramatic effect of the diagnostic yield of different genetic testing approaches on cost-effectiveness and the potential design of testing strategies in children with suspected monogenic conditions. Both studies emphasize the effect of the results of genetic testing. Whereas Tan et al. showed that, in 26% of cases, the result enabled a specific modification of patient care, Berg et al. also demonstrated that there is no basis for identifying optimal, targeted treatments, when testing is not performed and genetic diagnoses are not made.
However, in the absence of targeted treatments, a genetic diagnosis is of high value for the patients, their families, and treating physicians. A clear diagnosis may not only be of prognostic value but also put an end to a possibly stressful and demanding diagnostic odyssey. It may enable patient care that is explicitly focused on the individual needs of the patient. A clear diagnosis usually also allows a better assessment of the risks of recurrence in the family and possibly enables prenatal testing in relatives. Finally, it enables research and a better scientific understanding of the underlying pathophysiology, which may ideally lead to the identification of novel therapeutic prospects. Seven years ago, an international consensus statement endorsed the replacement of classic cytogenetic karyotype analysis by chromosomal microarrays as a first-tier diagnostic test in individuals with developmental disabilities or congenital anomalies. The studies add to the growing evidence that this consensus may already be outdated, as high-throughput sequencing techniques may achieve even higher diagnostic yields and, thus, are capable to become the new first-tier diagnostic test in congenital and early-onset disorders.
Johannes R. Lemke, MD, is with the Institute of Human Genetics at the University of Leipzig (Germany) Hospitals and Clinics. He reports no conflicts of interest associated with his editorial, which accompanied the JAMA Pediatrics reports (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1743).
Results from two new studies suggest that genetic testing early in the diagnostic pathway may allow for earlier and more precise diagnoses in early-life epilepsies and a range of other childhood-onset disorders, and potentially limit costs associated with a long diagnostic course.
Both papers, published online July 31 in JAMA Pediatrics, showed the diagnostic yield of genetic testing approaches, including whole-exome sequencing (WES), to be high.
The results also argue for the incorporation of genetic testing into the first diagnostic assessments; not limiting it to severe presentations only; and for broad testing methods to be employed in lieu of narrower ones.
Of these patients, just under half (n = 327) underwent various forms of genetic testing at the discretion of the treating physician, including karyotyping, microarrays, epilepsy gene panels, WES, mitochondrial panels, and other tests. Pathogenic variants were discovered in 132 children, or 40% of those receiving genetic testing (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1743).
Of all the genetic testing methods employed in the study, diagnostic yields were significantly greater for epilepsy gene panels (29.2%) and WES (27.8%), compared with chromosome microarray (7.9%).
The results, the investigators said, provide “added impetus to move the diagnosis of the specific cause to the point of initial presentation ... it is time to provide greater emphasis on and support for thorough genetic evaluations, particularly sequencing-based evaluations, for children with newly presenting epilepsies in the first few years of life.”
In addition to aiding management decisions, early genetic testing “ends the diagnostic odyssey during which parents and physicians spend untold amounts of time searching for an explanation for a child’s epilepsy and reduces associated costs,” Dr. Berg and her colleagues concluded.
In a separate study led by Tiong Yang Tan, MBBS, PhD, of Victorian Clinical Genetics Services in Melbourne, Australia, and his colleagues, singleton WES was used in 44 children recruited at outpatient clinics of a Melbourne hospital system (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1755).
Children in the study were aged 2-18 years (with mean age at presentation 28 months) and had a wide variety of suspected genetic disorders, including skeletal, skin, neurometabolic, and intellectual disorders. Some of these had features overlapping several conditions. The children in the cohort had not received prior genetic testing before undergoing WES.
The molecular test resulted in a diagnosis in 52% (n = 23) of the children, including unexpected diagnoses in eight of these. Clinical management was altered as result of sequencing findings in six children.
“Although phenotyping is critical, 35% of children had a diagnosis caused by a gene outside the initially prioritized gene list. This finding not only possibly reflects lack of clinical recognition but also underscores the utility of WES in achieving a diagnosis even when the a priori hypothesis is imprecise,” Dr. Tan and his associates wrote in their analysis.
Dr. Tan and his colleagues conducted a cost analysis that found WES performed at initial tertiary presentation resulted in a cost savings of U.S. $6,838 per additional diagnosis (95% confidence interval, U.S. $3,263-$11,678), compared with the standard diagnostic pathway. The figures reflect costs in an Australian care setting.
The children in the study had a mean diagnostic odyssey of 6 years, including a mean of 19 tests and four clinical genetics and four non–genetics specialist consultations. A quarter of them had undergone at least one diagnostic procedure under general anesthesia.
“The diagnostic odyssey of children suspected of having monogenic disorders is protracted and painful and may not provide a precise diagnosis,” Dr. Tan and his colleagues wrote in their analysis. “This paradigm has markedly shifted with the advent of WES.”
WES is best targeted to children “with genetically heterogeneous disorders or features overlapping several conditions,” the investigators concluded. “Our findings suggest that these children are best served by early recognition by their pediatrician and expedited referral to clinical genetics with WES applied after chromosomal microarray but before an extensive diagnostic process.”
Dr. Tan and his colleagues’ study was funded by the Melbourne Genomics Health Alliance and state and national governments in Australia. None of the authors declared conflicts of interest. Dr. Berg and her colleagues’ study was funded by the Pediatric Epilepsy Research Foundation, and none of its authors disclosed commercial conflicts of interest.
Results from two new studies suggest that genetic testing early in the diagnostic pathway may allow for earlier and more precise diagnoses in early-life epilepsies and a range of other childhood-onset disorders, and potentially limit costs associated with a long diagnostic course.
Both papers, published online July 31 in JAMA Pediatrics, showed the diagnostic yield of genetic testing approaches, including whole-exome sequencing (WES), to be high.
The results also argue for the incorporation of genetic testing into the first diagnostic assessments; not limiting it to severe presentations only; and for broad testing methods to be employed in lieu of narrower ones.
Of these patients, just under half (n = 327) underwent various forms of genetic testing at the discretion of the treating physician, including karyotyping, microarrays, epilepsy gene panels, WES, mitochondrial panels, and other tests. Pathogenic variants were discovered in 132 children, or 40% of those receiving genetic testing (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1743).
Of all the genetic testing methods employed in the study, diagnostic yields were significantly greater for epilepsy gene panels (29.2%) and WES (27.8%), compared with chromosome microarray (7.9%).
The results, the investigators said, provide “added impetus to move the diagnosis of the specific cause to the point of initial presentation ... it is time to provide greater emphasis on and support for thorough genetic evaluations, particularly sequencing-based evaluations, for children with newly presenting epilepsies in the first few years of life.”
In addition to aiding management decisions, early genetic testing “ends the diagnostic odyssey during which parents and physicians spend untold amounts of time searching for an explanation for a child’s epilepsy and reduces associated costs,” Dr. Berg and her colleagues concluded.
In a separate study led by Tiong Yang Tan, MBBS, PhD, of Victorian Clinical Genetics Services in Melbourne, Australia, and his colleagues, singleton WES was used in 44 children recruited at outpatient clinics of a Melbourne hospital system (JAMA Pediatr. 2017 July 31. doi: 10.1001/jamapediatrics.2017.1755).
Children in the study were aged 2-18 years (with mean age at presentation 28 months) and had a wide variety of suspected genetic disorders, including skeletal, skin, neurometabolic, and intellectual disorders. Some of these had features overlapping several conditions. The children in the cohort had not received prior genetic testing before undergoing WES.
The molecular test resulted in a diagnosis in 52% (n = 23) of the children, including unexpected diagnoses in eight of these. Clinical management was altered as result of sequencing findings in six children.
“Although phenotyping is critical, 35% of children had a diagnosis caused by a gene outside the initially prioritized gene list. This finding not only possibly reflects lack of clinical recognition but also underscores the utility of WES in achieving a diagnosis even when the a priori hypothesis is imprecise,” Dr. Tan and his associates wrote in their analysis.
Dr. Tan and his colleagues conducted a cost analysis that found WES performed at initial tertiary presentation resulted in a cost savings of U.S. $6,838 per additional diagnosis (95% confidence interval, U.S. $3,263-$11,678), compared with the standard diagnostic pathway. The figures reflect costs in an Australian care setting.
The children in the study had a mean diagnostic odyssey of 6 years, including a mean of 19 tests and four clinical genetics and four non–genetics specialist consultations. A quarter of them had undergone at least one diagnostic procedure under general anesthesia.
“The diagnostic odyssey of children suspected of having monogenic disorders is protracted and painful and may not provide a precise diagnosis,” Dr. Tan and his colleagues wrote in their analysis. “This paradigm has markedly shifted with the advent of WES.”
WES is best targeted to children “with genetically heterogeneous disorders or features overlapping several conditions,” the investigators concluded. “Our findings suggest that these children are best served by early recognition by their pediatrician and expedited referral to clinical genetics with WES applied after chromosomal microarray but before an extensive diagnostic process.”
Dr. Tan and his colleagues’ study was funded by the Melbourne Genomics Health Alliance and state and national governments in Australia. None of the authors declared conflicts of interest. Dr. Berg and her colleagues’ study was funded by the Pediatric Epilepsy Research Foundation, and none of its authors disclosed commercial conflicts of interest.
FROM JAMA PEDIATRICS
Short, simple antibiotic courses effective in latent TB
Latent tuberculosis infection can be safely and effectively treated with 3- and 4-month medication regimens, including those using once-weekly dosing, according to results from a new meta-analysis.
The findings, published online July 31 in Annals of Internal Medicine, bolster evidence that shorter antibiotic regimens using rifamycins alone or in combination with other drugs are a viable alternative to the longer courses (Ann Intern Med. 2017;167:248-55).
For their research, Dominik Zenner, MD, an epidemiologist with Public Health England in London, and his colleagues updated a meta-analysis they published in 2014. The team added 8 new randomized studies to the 53 that had been included in the earlier paper (Ann Intern Med. 2014 Sep;161:419-28).
Using pairwise comparisons and a Bayesian network analysis, Dr. Zenner and his colleagues found comparable efficacy among isoniazid regimens of 6 months or more; rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-only regimens, and rifampicin-pyrazinamide regimens, compared with placebo (P less than .05 for all).
Importantly, a rifapentine-based regimen in which patients took a weekly dose for 12 weeks was as effective as the others.
“We think that you can get away with shorter regimens,” Dr. Zenner said in an interview. Although 3- to 4-month courses are already recommended in some countries, including the United Kingdom, for most patients with latent TB, “clinicians in some settings have been quite slow to adopt them,” he said.
The U.S. Centers for Disease Control and Prevention currently recommend multiple treatment strategies for latent TB, depending on patient characteristics. These include 6 or 9 months of isoniazid; 3 months of once-weekly isoniazid and rifapentine; or 4 months of daily rifampin.
In the meta-analysis, rifamycin-only regimens performed as well as did those regimens that also used isoniazid, the study showed, suggesting that, for most patients who can safely be treated with rifamycins, “there is no added gain of using isoniazid,” Dr. Zenner said.
He noted that the longer isoniazid-alone regimens are nonetheless effective and appropriate for some, including people who might have potential drug interactions, such as HIV patients taking antiretroviral medications.
About 2 billion people worldwide are estimated to have latent TB, and most will not go on to develop active TB. However, because latent TB acts as the reservoir for active TB, screening of high-risk groups and close contacts of TB patients and treating latent infections is a public health priority.
But many of these asymptomatic patients will get lost between a positive screen result and successful treatment completion, Dr. Zenner said.
“We have huge drop-offs in the cascade of treatment, and treatment completion is one of the worries,” he said. “Whether it makes a huge difference in compliance to take only 12 doses is not sufficiently studied, but it does make a lot of sense. By reducing the pill burden, as we call it, we think that we will see quite good adherence rates – but that’s a subject of further detailed study.”
The investigators noted as a limitation of their study that hepatotoxicity outcomes were not available for all studies and that some of the included trials had a potential for bias. They did not see statistically significant differences in treatment efficacy between regimens in HIV-positive and HIV-negative patients, but noted in their analysis that “efficacy may have been weaker in HIV-positive populations.”
The U.K. National Institute for Health Research provided some funding for Dr. Zenner and his colleagues’ study. One coauthor, Helen Stagg, PhD, reported nonfinancial support from Sanofi during the study, and financial support from Otsuka for unrelated work.
Latent tuberculosis infection can be safely and effectively treated with 3- and 4-month medication regimens, including those using once-weekly dosing, according to results from a new meta-analysis.
The findings, published online July 31 in Annals of Internal Medicine, bolster evidence that shorter antibiotic regimens using rifamycins alone or in combination with other drugs are a viable alternative to the longer courses (Ann Intern Med. 2017;167:248-55).
For their research, Dominik Zenner, MD, an epidemiologist with Public Health England in London, and his colleagues updated a meta-analysis they published in 2014. The team added 8 new randomized studies to the 53 that had been included in the earlier paper (Ann Intern Med. 2014 Sep;161:419-28).
Using pairwise comparisons and a Bayesian network analysis, Dr. Zenner and his colleagues found comparable efficacy among isoniazid regimens of 6 months or more; rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-only regimens, and rifampicin-pyrazinamide regimens, compared with placebo (P less than .05 for all).
Importantly, a rifapentine-based regimen in which patients took a weekly dose for 12 weeks was as effective as the others.
“We think that you can get away with shorter regimens,” Dr. Zenner said in an interview. Although 3- to 4-month courses are already recommended in some countries, including the United Kingdom, for most patients with latent TB, “clinicians in some settings have been quite slow to adopt them,” he said.
The U.S. Centers for Disease Control and Prevention currently recommend multiple treatment strategies for latent TB, depending on patient characteristics. These include 6 or 9 months of isoniazid; 3 months of once-weekly isoniazid and rifapentine; or 4 months of daily rifampin.
In the meta-analysis, rifamycin-only regimens performed as well as did those regimens that also used isoniazid, the study showed, suggesting that, for most patients who can safely be treated with rifamycins, “there is no added gain of using isoniazid,” Dr. Zenner said.
He noted that the longer isoniazid-alone regimens are nonetheless effective and appropriate for some, including people who might have potential drug interactions, such as HIV patients taking antiretroviral medications.
About 2 billion people worldwide are estimated to have latent TB, and most will not go on to develop active TB. However, because latent TB acts as the reservoir for active TB, screening of high-risk groups and close contacts of TB patients and treating latent infections is a public health priority.
But many of these asymptomatic patients will get lost between a positive screen result and successful treatment completion, Dr. Zenner said.
“We have huge drop-offs in the cascade of treatment, and treatment completion is one of the worries,” he said. “Whether it makes a huge difference in compliance to take only 12 doses is not sufficiently studied, but it does make a lot of sense. By reducing the pill burden, as we call it, we think that we will see quite good adherence rates – but that’s a subject of further detailed study.”
The investigators noted as a limitation of their study that hepatotoxicity outcomes were not available for all studies and that some of the included trials had a potential for bias. They did not see statistically significant differences in treatment efficacy between regimens in HIV-positive and HIV-negative patients, but noted in their analysis that “efficacy may have been weaker in HIV-positive populations.”
The U.K. National Institute for Health Research provided some funding for Dr. Zenner and his colleagues’ study. One coauthor, Helen Stagg, PhD, reported nonfinancial support from Sanofi during the study, and financial support from Otsuka for unrelated work.
Latent tuberculosis infection can be safely and effectively treated with 3- and 4-month medication regimens, including those using once-weekly dosing, according to results from a new meta-analysis.
The findings, published online July 31 in Annals of Internal Medicine, bolster evidence that shorter antibiotic regimens using rifamycins alone or in combination with other drugs are a viable alternative to the longer courses (Ann Intern Med. 2017;167:248-55).
For their research, Dominik Zenner, MD, an epidemiologist with Public Health England in London, and his colleagues updated a meta-analysis they published in 2014. The team added 8 new randomized studies to the 53 that had been included in the earlier paper (Ann Intern Med. 2014 Sep;161:419-28).
Using pairwise comparisons and a Bayesian network analysis, Dr. Zenner and his colleagues found comparable efficacy among isoniazid regimens of 6 months or more; rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-only regimens, and rifampicin-pyrazinamide regimens, compared with placebo (P less than .05 for all).
Importantly, a rifapentine-based regimen in which patients took a weekly dose for 12 weeks was as effective as the others.
“We think that you can get away with shorter regimens,” Dr. Zenner said in an interview. Although 3- to 4-month courses are already recommended in some countries, including the United Kingdom, for most patients with latent TB, “clinicians in some settings have been quite slow to adopt them,” he said.
The U.S. Centers for Disease Control and Prevention currently recommend multiple treatment strategies for latent TB, depending on patient characteristics. These include 6 or 9 months of isoniazid; 3 months of once-weekly isoniazid and rifapentine; or 4 months of daily rifampin.
In the meta-analysis, rifamycin-only regimens performed as well as did those regimens that also used isoniazid, the study showed, suggesting that, for most patients who can safely be treated with rifamycins, “there is no added gain of using isoniazid,” Dr. Zenner said.
He noted that the longer isoniazid-alone regimens are nonetheless effective and appropriate for some, including people who might have potential drug interactions, such as HIV patients taking antiretroviral medications.
About 2 billion people worldwide are estimated to have latent TB, and most will not go on to develop active TB. However, because latent TB acts as the reservoir for active TB, screening of high-risk groups and close contacts of TB patients and treating latent infections is a public health priority.
But many of these asymptomatic patients will get lost between a positive screen result and successful treatment completion, Dr. Zenner said.
“We have huge drop-offs in the cascade of treatment, and treatment completion is one of the worries,” he said. “Whether it makes a huge difference in compliance to take only 12 doses is not sufficiently studied, but it does make a lot of sense. By reducing the pill burden, as we call it, we think that we will see quite good adherence rates – but that’s a subject of further detailed study.”
The investigators noted as a limitation of their study that hepatotoxicity outcomes were not available for all studies and that some of the included trials had a potential for bias. They did not see statistically significant differences in treatment efficacy between regimens in HIV-positive and HIV-negative patients, but noted in their analysis that “efficacy may have been weaker in HIV-positive populations.”
The U.K. National Institute for Health Research provided some funding for Dr. Zenner and his colleagues’ study. One coauthor, Helen Stagg, PhD, reported nonfinancial support from Sanofi during the study, and financial support from Otsuka for unrelated work.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Rifamycin-only treatment of latent TB works as well as combination regimens, and shorter dosing schedules show no loss in efficacy vs. longer ones.
Major finding: Rifamycin-only regimens, rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-pyrazinamide regimens were all effective, compared with placebo and with isoniazid regimens of 6, 12 and 72 months.
Data source: A network meta-analysis of 61 randomized trials, 8 of them published in last 3 years
Disclosures: The National Institute for Health Research (UK) funded some co-authors; one co-author disclosed a financial relationship with a pharmaceutical firm.
Free water in brain marks Parkinson’s progression
Free water in the posterior substantia nigra brain region increased as clinical Parkinson’s disease progressed in a 4-year longitudinal study of participants in the Parkinson’s Progression Markers Initiative.
Free water in this brain region is measurable via diffusion MRI, and this study – the first to look at free water in Parkinson’s patients across this time frame – suggests it to be a viable biomarker of disease progression that could be used in clinical trials evaluating Parkinson’s therapies.
Dr. Burciu and her colleagues found that free water increased over the first year post diagnosis in Parkinson’s patients but not in controls (P = .043), confirming similar results from an earlier study (Neurobiol Aging. 2015a;36:1097-104; Brain. 2015b;138:2322-31).
The researchers also looked at data from 46 Parkinson’s patients in the cohort who underwent imaging at 2 and 4 years to learn whether the observed increases in free water corresponded to progression measured on the Hoehn and Yahr scale, a widely used measure of Parkinson’s symptom severity.
Free water continued to increase in the Parkinson’s patients through 4 years, and increases in the first and second years after diagnosis were significantly associated with worsening of symptoms through 4 years (P less than .05 for both). Moreover, the investigators noted, men saw greater 4-year increases in free water levels, compared with women.
“The short-term increase in free water is related to the long-term progression of motor symptoms. Moreover, sex and baseline free water levels significantly predicted the rate of change in free water in [the posterior substantia nigra] over 4 years,” the investigators wrote.
The results were consistent across study sites, they found.
Dr. Burciu and her colleagues disclosed funding from the PPMI, which is supported by the Michael J. Fox Foundation and a consortium of pharmaceutical, biotech, and financial firms. The researchers also received funding from the National Institutes of Health. None disclosed financial conflicts of interest.
Free water in the posterior substantia nigra brain region increased as clinical Parkinson’s disease progressed in a 4-year longitudinal study of participants in the Parkinson’s Progression Markers Initiative.
Free water in this brain region is measurable via diffusion MRI, and this study – the first to look at free water in Parkinson’s patients across this time frame – suggests it to be a viable biomarker of disease progression that could be used in clinical trials evaluating Parkinson’s therapies.
Dr. Burciu and her colleagues found that free water increased over the first year post diagnosis in Parkinson’s patients but not in controls (P = .043), confirming similar results from an earlier study (Neurobiol Aging. 2015a;36:1097-104; Brain. 2015b;138:2322-31).
The researchers also looked at data from 46 Parkinson’s patients in the cohort who underwent imaging at 2 and 4 years to learn whether the observed increases in free water corresponded to progression measured on the Hoehn and Yahr scale, a widely used measure of Parkinson’s symptom severity.
Free water continued to increase in the Parkinson’s patients through 4 years, and increases in the first and second years after diagnosis were significantly associated with worsening of symptoms through 4 years (P less than .05 for both). Moreover, the investigators noted, men saw greater 4-year increases in free water levels, compared with women.
“The short-term increase in free water is related to the long-term progression of motor symptoms. Moreover, sex and baseline free water levels significantly predicted the rate of change in free water in [the posterior substantia nigra] over 4 years,” the investigators wrote.
The results were consistent across study sites, they found.
Dr. Burciu and her colleagues disclosed funding from the PPMI, which is supported by the Michael J. Fox Foundation and a consortium of pharmaceutical, biotech, and financial firms. The researchers also received funding from the National Institutes of Health. None disclosed financial conflicts of interest.
Free water in the posterior substantia nigra brain region increased as clinical Parkinson’s disease progressed in a 4-year longitudinal study of participants in the Parkinson’s Progression Markers Initiative.
Free water in this brain region is measurable via diffusion MRI, and this study – the first to look at free water in Parkinson’s patients across this time frame – suggests it to be a viable biomarker of disease progression that could be used in clinical trials evaluating Parkinson’s therapies.
Dr. Burciu and her colleagues found that free water increased over the first year post diagnosis in Parkinson’s patients but not in controls (P = .043), confirming similar results from an earlier study (Neurobiol Aging. 2015a;36:1097-104; Brain. 2015b;138:2322-31).
The researchers also looked at data from 46 Parkinson’s patients in the cohort who underwent imaging at 2 and 4 years to learn whether the observed increases in free water corresponded to progression measured on the Hoehn and Yahr scale, a widely used measure of Parkinson’s symptom severity.
Free water continued to increase in the Parkinson’s patients through 4 years, and increases in the first and second years after diagnosis were significantly associated with worsening of symptoms through 4 years (P less than .05 for both). Moreover, the investigators noted, men saw greater 4-year increases in free water levels, compared with women.
“The short-term increase in free water is related to the long-term progression of motor symptoms. Moreover, sex and baseline free water levels significantly predicted the rate of change in free water in [the posterior substantia nigra] over 4 years,” the investigators wrote.
The results were consistent across study sites, they found.
Dr. Burciu and her colleagues disclosed funding from the PPMI, which is supported by the Michael J. Fox Foundation and a consortium of pharmaceutical, biotech, and financial firms. The researchers also received funding from the National Institutes of Health. None disclosed financial conflicts of interest.
FROM BRAIN
Key clinical point:
Major finding: Increases measured in years 1 or 2 after diagnosis were associated with worsening of symptoms through year 4 (P less than .05)
Data source: Analysis of 103 patients and 49 controls from a large, multisite, international, observational, longitudinal study seeking Parkinson’s biomarkers.
Disclosures: The National Institutes of Health and the Parkinson’s Progression Markers Initiative (PPMI) funded this analysis. The PPMI receives broad funding from industry and foundations. None of the researchers disclosed financial conflicts of interest.
CDC refocuses Zika testing recommendations in pregnancy
, including those who may have been exposed before pregnancy through travel or sexual contact.
In updated guidance released July 24, the Centers for Disease Control and Prevention cited a combination of factors behind the change in recommendations, including the declining prevalence of Zika virus across the Americas and a high likelihood of false positives associated with the use of a common serologic assay (MMWR Morb Mortal Wkly Rep. ePub 2017 Jul 24. doi: 10.15585/mmwr.mm6629e1).
Positive IgM results can also occur after previous exposure to other flaviviruses besides Zika, Dr. Oduyebo and her colleagues noted.
The CDC now recommends that pregnant women with likely continuing – not previous – exposure to the Zika virus and those with symptoms suggestive of Zika virus disease be tested. Those higher-risk groups should receive nucleic acid testing (NAT).
The new guidance presents two updated testing algorithms, one for each group.
Any pregnant woman with symptoms suggestive of Zika should be tested “as soon as possible through 12 weeks after symptom onset,” the CDC said, with both NAT (serum and urine) and IgM serology testing.
Women with likely ongoing exposure to Zika – such as those living in or traveling to an area of mosquito-borne Zika transmission or those whose partners are living in or traveling to such an area – should be tested up to three times during the pregnancy using NAT serum and urine tests. IgM testing is not recommended for that group.
All pregnant women should be asked about their potential Zika exposures before and during the current pregnancy, the CDC said. That discussion, which covers potential travel and partner exposures along with questions about symptoms, should be repeated at every prenatal visit.
While routine testing of asymptomatic women without ongoing exposure is not recommended, patient preferences, clinical judgment, and a “balanced assessment of risks and expected outcomes” should guide decisions about testing, according to the CDC.
, including those who may have been exposed before pregnancy through travel or sexual contact.
In updated guidance released July 24, the Centers for Disease Control and Prevention cited a combination of factors behind the change in recommendations, including the declining prevalence of Zika virus across the Americas and a high likelihood of false positives associated with the use of a common serologic assay (MMWR Morb Mortal Wkly Rep. ePub 2017 Jul 24. doi: 10.15585/mmwr.mm6629e1).
Positive IgM results can also occur after previous exposure to other flaviviruses besides Zika, Dr. Oduyebo and her colleagues noted.
The CDC now recommends that pregnant women with likely continuing – not previous – exposure to the Zika virus and those with symptoms suggestive of Zika virus disease be tested. Those higher-risk groups should receive nucleic acid testing (NAT).
The new guidance presents two updated testing algorithms, one for each group.
Any pregnant woman with symptoms suggestive of Zika should be tested “as soon as possible through 12 weeks after symptom onset,” the CDC said, with both NAT (serum and urine) and IgM serology testing.
Women with likely ongoing exposure to Zika – such as those living in or traveling to an area of mosquito-borne Zika transmission or those whose partners are living in or traveling to such an area – should be tested up to three times during the pregnancy using NAT serum and urine tests. IgM testing is not recommended for that group.
All pregnant women should be asked about their potential Zika exposures before and during the current pregnancy, the CDC said. That discussion, which covers potential travel and partner exposures along with questions about symptoms, should be repeated at every prenatal visit.
While routine testing of asymptomatic women without ongoing exposure is not recommended, patient preferences, clinical judgment, and a “balanced assessment of risks and expected outcomes” should guide decisions about testing, according to the CDC.
, including those who may have been exposed before pregnancy through travel or sexual contact.
In updated guidance released July 24, the Centers for Disease Control and Prevention cited a combination of factors behind the change in recommendations, including the declining prevalence of Zika virus across the Americas and a high likelihood of false positives associated with the use of a common serologic assay (MMWR Morb Mortal Wkly Rep. ePub 2017 Jul 24. doi: 10.15585/mmwr.mm6629e1).
Positive IgM results can also occur after previous exposure to other flaviviruses besides Zika, Dr. Oduyebo and her colleagues noted.
The CDC now recommends that pregnant women with likely continuing – not previous – exposure to the Zika virus and those with symptoms suggestive of Zika virus disease be tested. Those higher-risk groups should receive nucleic acid testing (NAT).
The new guidance presents two updated testing algorithms, one for each group.
Any pregnant woman with symptoms suggestive of Zika should be tested “as soon as possible through 12 weeks after symptom onset,” the CDC said, with both NAT (serum and urine) and IgM serology testing.
Women with likely ongoing exposure to Zika – such as those living in or traveling to an area of mosquito-borne Zika transmission or those whose partners are living in or traveling to such an area – should be tested up to three times during the pregnancy using NAT serum and urine tests. IgM testing is not recommended for that group.
All pregnant women should be asked about their potential Zika exposures before and during the current pregnancy, the CDC said. That discussion, which covers potential travel and partner exposures along with questions about symptoms, should be repeated at every prenatal visit.
While routine testing of asymptomatic women without ongoing exposure is not recommended, patient preferences, clinical judgment, and a “balanced assessment of risks and expected outcomes” should guide decisions about testing, according to the CDC.
FROM MMWR