User login
FDA approves sublingual immunotherapy for dust mite allergies
Odactra (Merck, Sharp & Dohme) had been approved in adults aged 18-65 years, with allergic rhinitis with or without conjunctivitis. The tablets offer an alternative to subcutaneous injections, the FDA said in a statement issued March 1.
The sublingual tablets are intended to be taken daily, year-round, and the first dose must be taken under physician supervision to monitor for adverse reactions, according to the FDA. As with other sublingual immunotherapies, patients using the tablets should be simultaneously prescribed autoinjectable epinephrine.
The approval was based on results from randomized trials enrolling about 2,500 patients in Europe and the United States, according to the FDA. Patients taking the tablets saw a 16%-18% reduction in symptoms across studies, compared with placebo. Clinical benefit may be delayed by 8-14 weeks after starting the therapy, the agency said. Common adverse reactions reported in the studies included nausea, itching of the ears and mouth, and swelling of the lips and tongue.
Odactra is the fourth sublingual immunotherapy to be approved in the United States since 2014. Other approved therapies target grass and ragweed allergies.
Odactra (Merck, Sharp & Dohme) had been approved in adults aged 18-65 years, with allergic rhinitis with or without conjunctivitis. The tablets offer an alternative to subcutaneous injections, the FDA said in a statement issued March 1.
The sublingual tablets are intended to be taken daily, year-round, and the first dose must be taken under physician supervision to monitor for adverse reactions, according to the FDA. As with other sublingual immunotherapies, patients using the tablets should be simultaneously prescribed autoinjectable epinephrine.
The approval was based on results from randomized trials enrolling about 2,500 patients in Europe and the United States, according to the FDA. Patients taking the tablets saw a 16%-18% reduction in symptoms across studies, compared with placebo. Clinical benefit may be delayed by 8-14 weeks after starting the therapy, the agency said. Common adverse reactions reported in the studies included nausea, itching of the ears and mouth, and swelling of the lips and tongue.
Odactra is the fourth sublingual immunotherapy to be approved in the United States since 2014. Other approved therapies target grass and ragweed allergies.
Odactra (Merck, Sharp & Dohme) had been approved in adults aged 18-65 years, with allergic rhinitis with or without conjunctivitis. The tablets offer an alternative to subcutaneous injections, the FDA said in a statement issued March 1.
The sublingual tablets are intended to be taken daily, year-round, and the first dose must be taken under physician supervision to monitor for adverse reactions, according to the FDA. As with other sublingual immunotherapies, patients using the tablets should be simultaneously prescribed autoinjectable epinephrine.
The approval was based on results from randomized trials enrolling about 2,500 patients in Europe and the United States, according to the FDA. Patients taking the tablets saw a 16%-18% reduction in symptoms across studies, compared with placebo. Clinical benefit may be delayed by 8-14 weeks after starting the therapy, the agency said. Common adverse reactions reported in the studies included nausea, itching of the ears and mouth, and swelling of the lips and tongue.
Odactra is the fourth sublingual immunotherapy to be approved in the United States since 2014. Other approved therapies target grass and ragweed allergies.
Use of IHC stains on rise in melanoma diagnosis
While there is little consensus on the ideal role of immunohistochemical (IHC) stains in the diagnosis of melanoma, their use increased dramatically over a 15-year period, according to results from a study.
Randie H. Kim, MD, PhD, and Shane A. Meehan, MD, of New York University, reviewed nearly 6,300 pathology reports from patients with melanomas, all referred (along with tissue samples) to their center from other institutions during 2001-2015. One or more IHC stains were used diagnostically in 871 cases during the study period, with use increasing from 5% of patients in 2001 to 25% in 2015 (P less than .0001). Usage increased gradually over time, although the number of stains used per case did not increase significantly (J Cutan Pathol. 2017 Mar;44[3]:221-7).
IHC stain use was associated with melanomas occurring on the head or neck (odds ratio = 1.6; 95% confidence interval, 1.4-1.9), acral melanomas (OR = 1.5; 95% CI 1.1-2.0) and melanomas thicker than 4 mm (OR = 2.5; 95% CI 1.7-3.6). The most common stain used in the study was Melan-A/MART-1 (melanoma antigen recognized by T cells), the most specific of the IHC markers available and the one “largely responsible for the increased incidence in overall immunostain use in our study,” the researchers wrote. “The perception that melanocytic markers, such as Melan-A, can more accurately stage melanomas, is a potential explanation for its increased usage over the duration of the study period.”
The higher use of immunostains in thicker melanomas may be because these “exhibit greater morphological heterogeneity, such as nodular, spindled and desmoplastic subtypes, that lead to additional confirmational testing,” Dr. Kim and Dr. Meehan noted. However, they cautioned that extrinsic factors, including reimbursement fees and concerns about malpractice claims, could also influence the use of IHC stains in the diagnosis of melanomas.
“While Melan-A/MART-1 is a useful adjunct for determining melanocytic density or the presence of invasion in difficult cases, its routine use on melanomas has not been validated,” the researchers wrote in their analysis. “A consensus conference delineating the appropriate use of IHC in the diagnosis of melanoma may be of value in this regard.”
Dr. Kim and Dr. Meehan also noted that while a greater proportion of the melanomas seen in the study were thick (greater than 4 mm) compared with most population-based studies, this may reflect patient management practices in which thinner melanomas are treated in outpatient centers while thicker ones get referred to tertiary care centers such as theirs.
The researchers disclosed no outside funding or conflicts of interest.
While there is little consensus on the ideal role of immunohistochemical (IHC) stains in the diagnosis of melanoma, their use increased dramatically over a 15-year period, according to results from a study.
Randie H. Kim, MD, PhD, and Shane A. Meehan, MD, of New York University, reviewed nearly 6,300 pathology reports from patients with melanomas, all referred (along with tissue samples) to their center from other institutions during 2001-2015. One or more IHC stains were used diagnostically in 871 cases during the study period, with use increasing from 5% of patients in 2001 to 25% in 2015 (P less than .0001). Usage increased gradually over time, although the number of stains used per case did not increase significantly (J Cutan Pathol. 2017 Mar;44[3]:221-7).
IHC stain use was associated with melanomas occurring on the head or neck (odds ratio = 1.6; 95% confidence interval, 1.4-1.9), acral melanomas (OR = 1.5; 95% CI 1.1-2.0) and melanomas thicker than 4 mm (OR = 2.5; 95% CI 1.7-3.6). The most common stain used in the study was Melan-A/MART-1 (melanoma antigen recognized by T cells), the most specific of the IHC markers available and the one “largely responsible for the increased incidence in overall immunostain use in our study,” the researchers wrote. “The perception that melanocytic markers, such as Melan-A, can more accurately stage melanomas, is a potential explanation for its increased usage over the duration of the study period.”
The higher use of immunostains in thicker melanomas may be because these “exhibit greater morphological heterogeneity, such as nodular, spindled and desmoplastic subtypes, that lead to additional confirmational testing,” Dr. Kim and Dr. Meehan noted. However, they cautioned that extrinsic factors, including reimbursement fees and concerns about malpractice claims, could also influence the use of IHC stains in the diagnosis of melanomas.
“While Melan-A/MART-1 is a useful adjunct for determining melanocytic density or the presence of invasion in difficult cases, its routine use on melanomas has not been validated,” the researchers wrote in their analysis. “A consensus conference delineating the appropriate use of IHC in the diagnosis of melanoma may be of value in this regard.”
Dr. Kim and Dr. Meehan also noted that while a greater proportion of the melanomas seen in the study were thick (greater than 4 mm) compared with most population-based studies, this may reflect patient management practices in which thinner melanomas are treated in outpatient centers while thicker ones get referred to tertiary care centers such as theirs.
The researchers disclosed no outside funding or conflicts of interest.
While there is little consensus on the ideal role of immunohistochemical (IHC) stains in the diagnosis of melanoma, their use increased dramatically over a 15-year period, according to results from a study.
Randie H. Kim, MD, PhD, and Shane A. Meehan, MD, of New York University, reviewed nearly 6,300 pathology reports from patients with melanomas, all referred (along with tissue samples) to their center from other institutions during 2001-2015. One or more IHC stains were used diagnostically in 871 cases during the study period, with use increasing from 5% of patients in 2001 to 25% in 2015 (P less than .0001). Usage increased gradually over time, although the number of stains used per case did not increase significantly (J Cutan Pathol. 2017 Mar;44[3]:221-7).
IHC stain use was associated with melanomas occurring on the head or neck (odds ratio = 1.6; 95% confidence interval, 1.4-1.9), acral melanomas (OR = 1.5; 95% CI 1.1-2.0) and melanomas thicker than 4 mm (OR = 2.5; 95% CI 1.7-3.6). The most common stain used in the study was Melan-A/MART-1 (melanoma antigen recognized by T cells), the most specific of the IHC markers available and the one “largely responsible for the increased incidence in overall immunostain use in our study,” the researchers wrote. “The perception that melanocytic markers, such as Melan-A, can more accurately stage melanomas, is a potential explanation for its increased usage over the duration of the study period.”
The higher use of immunostains in thicker melanomas may be because these “exhibit greater morphological heterogeneity, such as nodular, spindled and desmoplastic subtypes, that lead to additional confirmational testing,” Dr. Kim and Dr. Meehan noted. However, they cautioned that extrinsic factors, including reimbursement fees and concerns about malpractice claims, could also influence the use of IHC stains in the diagnosis of melanomas.
“While Melan-A/MART-1 is a useful adjunct for determining melanocytic density or the presence of invasion in difficult cases, its routine use on melanomas has not been validated,” the researchers wrote in their analysis. “A consensus conference delineating the appropriate use of IHC in the diagnosis of melanoma may be of value in this regard.”
Dr. Kim and Dr. Meehan also noted that while a greater proportion of the melanomas seen in the study were thick (greater than 4 mm) compared with most population-based studies, this may reflect patient management practices in which thinner melanomas are treated in outpatient centers while thicker ones get referred to tertiary care centers such as theirs.
The researchers disclosed no outside funding or conflicts of interest.
FROM THE JOURNAL OF CUTANEOUS PATHOLOGY
Key clinical point:
Major finding: One or more stains was used diagnostically in 5% of melanoma cases in 2001, compared with 25% in 2015 (P less than .0001).
Data source: A retrospective review of more than 6,000 case records referred after diagnosis to a tertiary care center during 2001-2015.
Disclosures: The researchers disclosed no outside funding or conflicts of interest.
Stable response in sickle cell disease patient treated with gene therapy
A teenage boy with sickle cell disease has been successfully treated with a therapy that uses a viral vector to insert functional genes into blood-producing stem cells.
The patient’s positive response to the intervention was first reported in 2015, and his clinical remission was reported in late 2016 at the American Society of Hematology’s annual meeting.
The new report, published online March 1 in the New England Journal of Medicine, contains the first detailed description of the case (2017;376:848-55).
Treatment consisted of LentiGlobin BB305, an engineered lentiviral vector–mediated addition of an antisickling human beta-globin gene (HbAT87Q ) into the patient’s hematopoietic stem cells. The technology was developed by bluebird bio, which partially funded the study and helped design its protocol.
The investigators, led by Marina Cavazzana, MD, PhD, of Necker Children’s Hospital, Assistance Publique–Hôpitaux de Paris, collected blood-producing stem cells from the patient’s bone marrow. The cells were transduced ex vivo using LentiGlobin BB305.
After the patient underwent 4 days of myeloablation and a 2-day washout period, the transduced stem cells were infused at 5.6x106 CD34+ cells per kilogram. The patient continued receiving red blood cell transfusions until at least 30% healthy hemoglobin with the signature of the introduced gene could be detected.
Neutrophil engraftment occurred at 38 days after transplantation, and platelet engraftment, at 3 months. Red cell transfusions were discontinued at 3 months.
The patient saw vector-bearing healthy cells in the blood increase during the first 3 months after transplantation, the investigators reported, and the cells continue to be produced at stable levels through month 15, which suggests “engraftment of transduced stem cells that were capable of long-term repopulation,” the investigators wrote.
Also at 15 months after transplantation, the patient had 48% HbAT87Q, while 30% healthy hemoglobin is considered sufficient to see clinical improvement in SCD patients.
The patient has not experienced sickle cell disease–related clinical events or hospitalization since transplantation, Dr. Cavazzana and her colleagues reported, noting all his medications, including pain medication, have been stopped.
Most adverse events seen in the study were associated with busulfan, the drug used in myeloablation, and no adverse events were associated with the gene therapy itself.
These results, the investigators concluded, provide proof of concept for lentiviral vectors in delivering this gene therapy for SCD. This approach, they said, “may help to guide the design of future clinical trials of gene therapy for sickle cell disease.” One important advantage for lentiviral vectors over retroviral vectors is that the former appear less likely to generate cancer-causing mutations; the engineered vector used in this study is self-inactivating.
Two more SCD patients have since been enrolled in the same study.
In a press statement accompanying the March 1 publication, the makers of the gene therapy said these results had prompted them to modify protocols in an ongoing U.S-based study of the same therapy in SCD, in the hope of achieving outcomes similar to those seen in France.
The study was funded by bluebird bio and grants from Assistance Publique–Hôpitaux de Paris and INSERM. Of the 27 authors, 9 disclosed being stockholders of bluebird, receiving fees, holding patents on technologies used in the study, or being employees. One reported financial relationships with other firms, and 17, including the corresponding author, reported no commercial conflicts of interest.
A teenage boy with sickle cell disease has been successfully treated with a therapy that uses a viral vector to insert functional genes into blood-producing stem cells.
The patient’s positive response to the intervention was first reported in 2015, and his clinical remission was reported in late 2016 at the American Society of Hematology’s annual meeting.
The new report, published online March 1 in the New England Journal of Medicine, contains the first detailed description of the case (2017;376:848-55).
Treatment consisted of LentiGlobin BB305, an engineered lentiviral vector–mediated addition of an antisickling human beta-globin gene (HbAT87Q ) into the patient’s hematopoietic stem cells. The technology was developed by bluebird bio, which partially funded the study and helped design its protocol.
The investigators, led by Marina Cavazzana, MD, PhD, of Necker Children’s Hospital, Assistance Publique–Hôpitaux de Paris, collected blood-producing stem cells from the patient’s bone marrow. The cells were transduced ex vivo using LentiGlobin BB305.
After the patient underwent 4 days of myeloablation and a 2-day washout period, the transduced stem cells were infused at 5.6x106 CD34+ cells per kilogram. The patient continued receiving red blood cell transfusions until at least 30% healthy hemoglobin with the signature of the introduced gene could be detected.
Neutrophil engraftment occurred at 38 days after transplantation, and platelet engraftment, at 3 months. Red cell transfusions were discontinued at 3 months.
The patient saw vector-bearing healthy cells in the blood increase during the first 3 months after transplantation, the investigators reported, and the cells continue to be produced at stable levels through month 15, which suggests “engraftment of transduced stem cells that were capable of long-term repopulation,” the investigators wrote.
Also at 15 months after transplantation, the patient had 48% HbAT87Q, while 30% healthy hemoglobin is considered sufficient to see clinical improvement in SCD patients.
The patient has not experienced sickle cell disease–related clinical events or hospitalization since transplantation, Dr. Cavazzana and her colleagues reported, noting all his medications, including pain medication, have been stopped.
Most adverse events seen in the study were associated with busulfan, the drug used in myeloablation, and no adverse events were associated with the gene therapy itself.
These results, the investigators concluded, provide proof of concept for lentiviral vectors in delivering this gene therapy for SCD. This approach, they said, “may help to guide the design of future clinical trials of gene therapy for sickle cell disease.” One important advantage for lentiviral vectors over retroviral vectors is that the former appear less likely to generate cancer-causing mutations; the engineered vector used in this study is self-inactivating.
Two more SCD patients have since been enrolled in the same study.
In a press statement accompanying the March 1 publication, the makers of the gene therapy said these results had prompted them to modify protocols in an ongoing U.S-based study of the same therapy in SCD, in the hope of achieving outcomes similar to those seen in France.
The study was funded by bluebird bio and grants from Assistance Publique–Hôpitaux de Paris and INSERM. Of the 27 authors, 9 disclosed being stockholders of bluebird, receiving fees, holding patents on technologies used in the study, or being employees. One reported financial relationships with other firms, and 17, including the corresponding author, reported no commercial conflicts of interest.
A teenage boy with sickle cell disease has been successfully treated with a therapy that uses a viral vector to insert functional genes into blood-producing stem cells.
The patient’s positive response to the intervention was first reported in 2015, and his clinical remission was reported in late 2016 at the American Society of Hematology’s annual meeting.
The new report, published online March 1 in the New England Journal of Medicine, contains the first detailed description of the case (2017;376:848-55).
Treatment consisted of LentiGlobin BB305, an engineered lentiviral vector–mediated addition of an antisickling human beta-globin gene (HbAT87Q ) into the patient’s hematopoietic stem cells. The technology was developed by bluebird bio, which partially funded the study and helped design its protocol.
The investigators, led by Marina Cavazzana, MD, PhD, of Necker Children’s Hospital, Assistance Publique–Hôpitaux de Paris, collected blood-producing stem cells from the patient’s bone marrow. The cells were transduced ex vivo using LentiGlobin BB305.
After the patient underwent 4 days of myeloablation and a 2-day washout period, the transduced stem cells were infused at 5.6x106 CD34+ cells per kilogram. The patient continued receiving red blood cell transfusions until at least 30% healthy hemoglobin with the signature of the introduced gene could be detected.
Neutrophil engraftment occurred at 38 days after transplantation, and platelet engraftment, at 3 months. Red cell transfusions were discontinued at 3 months.
The patient saw vector-bearing healthy cells in the blood increase during the first 3 months after transplantation, the investigators reported, and the cells continue to be produced at stable levels through month 15, which suggests “engraftment of transduced stem cells that were capable of long-term repopulation,” the investigators wrote.
Also at 15 months after transplantation, the patient had 48% HbAT87Q, while 30% healthy hemoglobin is considered sufficient to see clinical improvement in SCD patients.
The patient has not experienced sickle cell disease–related clinical events or hospitalization since transplantation, Dr. Cavazzana and her colleagues reported, noting all his medications, including pain medication, have been stopped.
Most adverse events seen in the study were associated with busulfan, the drug used in myeloablation, and no adverse events were associated with the gene therapy itself.
These results, the investigators concluded, provide proof of concept for lentiviral vectors in delivering this gene therapy for SCD. This approach, they said, “may help to guide the design of future clinical trials of gene therapy for sickle cell disease.” One important advantage for lentiviral vectors over retroviral vectors is that the former appear less likely to generate cancer-causing mutations; the engineered vector used in this study is self-inactivating.
Two more SCD patients have since been enrolled in the same study.
In a press statement accompanying the March 1 publication, the makers of the gene therapy said these results had prompted them to modify protocols in an ongoing U.S-based study of the same therapy in SCD, in the hope of achieving outcomes similar to those seen in France.
The study was funded by bluebird bio and grants from Assistance Publique–Hôpitaux de Paris and INSERM. Of the 27 authors, 9 disclosed being stockholders of bluebird, receiving fees, holding patents on technologies used in the study, or being employees. One reported financial relationships with other firms, and 17, including the corresponding author, reported no commercial conflicts of interest.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Using gene therapy in blood-producing stem cells led to clinical remission and durable healthy hemoglobin production in a teenage boy with sickle cell disease.
Major finding: At 15 months post treatment, the patient’s level of therapeutic antisickling beta-globin was 50%, suggesting engraftment and ongoing healthy cell production.
Data source: The first case report from a phase I/II open label trial in France, enrolling three patients with sickle cell disease.
Disclosures: The study was funded by bluebird bio, maker of the technology, and grants from Assistance Publique–Hôpitaux de Paris and INSERM. One-third of coauthors disclosed financial relationships with the sponsor.
Oral contraceptive use confers long-term cancer protection
New findings from a cohort study with more than 4 decades of follow-up show that, while women who have ever used combined oral contraceptives see an increased risk of breast and cervical cancer, the risk disappears within about 5 years after stopping, but a protective effect against colorectal, endometrial, and ovarian cancer persists for more than 30 years.
The findings provide an update to the General Practitioners’ Oral Contraception Study of a United Kingdom cohort recruited in the late 1960s.
The mean age was 70.2 years, most were white, and the mean follow-up was 40.7 years. Women who had used the pill did so a mean 3.66 years and used older, higher-estrogen formulations.
Compared with never users, users of oral contraception had a nonsignificant 4% reduced risk of any cancer. The incidence rate ratio for breast cancer was similar between ever users and nonusers (IRR 1.04; 99% CI, 0.91-1.17). Women who had used OCs saw significant reductions in colorectal (IRR, 0.81; 99% CI, 0.66-0.99), endometrial (IRR, 0.66; 99% CI, 0.48-0.89), ovarian (IRR, 0.67; 99% CI, 0.50-0.89), and lymphatic and hematopoietic cancers (IRR, 0.74; 0.58-0.94), compared with never users.
Lung cancer incidence was increased among ever users of OCs, but only in women who smoked at the time of recruitment.
“There was no evidence of new cancer risks appearing later in life among women who had used oral contraceptives,” the researchers wrote. “Thus, the overall balance of cancer risk among past users of oral contraceptives was neutral with the increased risks counterbalanced by the endometrial, ovarian, and colorectal cancer benefits that persist at least 30 years.”
The results, the researchers wrote, “provide strong evidence that most women do not expose themselves to long-term cancer harm if they choose to use oral contraception, indeed many are likely to be protected.”
The study was funded by the Royal College of General Practitioners, Medical Research Council, Imperial Cancer Research Fund, British Heart Foundation, Schering AG, Schering Health Care, Wyeth Ayerst International, Ortho Cilag, and Searle. The researchers reported having no conflicts of interest.
New findings from a cohort study with more than 4 decades of follow-up show that, while women who have ever used combined oral contraceptives see an increased risk of breast and cervical cancer, the risk disappears within about 5 years after stopping, but a protective effect against colorectal, endometrial, and ovarian cancer persists for more than 30 years.
The findings provide an update to the General Practitioners’ Oral Contraception Study of a United Kingdom cohort recruited in the late 1960s.
The mean age was 70.2 years, most were white, and the mean follow-up was 40.7 years. Women who had used the pill did so a mean 3.66 years and used older, higher-estrogen formulations.
Compared with never users, users of oral contraception had a nonsignificant 4% reduced risk of any cancer. The incidence rate ratio for breast cancer was similar between ever users and nonusers (IRR 1.04; 99% CI, 0.91-1.17). Women who had used OCs saw significant reductions in colorectal (IRR, 0.81; 99% CI, 0.66-0.99), endometrial (IRR, 0.66; 99% CI, 0.48-0.89), ovarian (IRR, 0.67; 99% CI, 0.50-0.89), and lymphatic and hematopoietic cancers (IRR, 0.74; 0.58-0.94), compared with never users.
Lung cancer incidence was increased among ever users of OCs, but only in women who smoked at the time of recruitment.
“There was no evidence of new cancer risks appearing later in life among women who had used oral contraceptives,” the researchers wrote. “Thus, the overall balance of cancer risk among past users of oral contraceptives was neutral with the increased risks counterbalanced by the endometrial, ovarian, and colorectal cancer benefits that persist at least 30 years.”
The results, the researchers wrote, “provide strong evidence that most women do not expose themselves to long-term cancer harm if they choose to use oral contraception, indeed many are likely to be protected.”
The study was funded by the Royal College of General Practitioners, Medical Research Council, Imperial Cancer Research Fund, British Heart Foundation, Schering AG, Schering Health Care, Wyeth Ayerst International, Ortho Cilag, and Searle. The researchers reported having no conflicts of interest.
New findings from a cohort study with more than 4 decades of follow-up show that, while women who have ever used combined oral contraceptives see an increased risk of breast and cervical cancer, the risk disappears within about 5 years after stopping, but a protective effect against colorectal, endometrial, and ovarian cancer persists for more than 30 years.
The findings provide an update to the General Practitioners’ Oral Contraception Study of a United Kingdom cohort recruited in the late 1960s.
The mean age was 70.2 years, most were white, and the mean follow-up was 40.7 years. Women who had used the pill did so a mean 3.66 years and used older, higher-estrogen formulations.
Compared with never users, users of oral contraception had a nonsignificant 4% reduced risk of any cancer. The incidence rate ratio for breast cancer was similar between ever users and nonusers (IRR 1.04; 99% CI, 0.91-1.17). Women who had used OCs saw significant reductions in colorectal (IRR, 0.81; 99% CI, 0.66-0.99), endometrial (IRR, 0.66; 99% CI, 0.48-0.89), ovarian (IRR, 0.67; 99% CI, 0.50-0.89), and lymphatic and hematopoietic cancers (IRR, 0.74; 0.58-0.94), compared with never users.
Lung cancer incidence was increased among ever users of OCs, but only in women who smoked at the time of recruitment.
“There was no evidence of new cancer risks appearing later in life among women who had used oral contraceptives,” the researchers wrote. “Thus, the overall balance of cancer risk among past users of oral contraceptives was neutral with the increased risks counterbalanced by the endometrial, ovarian, and colorectal cancer benefits that persist at least 30 years.”
The results, the researchers wrote, “provide strong evidence that most women do not expose themselves to long-term cancer harm if they choose to use oral contraception, indeed many are likely to be protected.”
The study was funded by the Royal College of General Practitioners, Medical Research Council, Imperial Cancer Research Fund, British Heart Foundation, Schering AG, Schering Health Care, Wyeth Ayerst International, Ortho Cilag, and Searle. The researchers reported having no conflicts of interest.
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Key clinical point:
Major finding: At about 40 years of follow-up, women who had ever used combined OCs saw reduced incidence of colorectal (IRR, 0.81), endometrial (IRR, 0.66), ovarian (IRR, 0.67), and lymphatic and hematopoietic cancer (IRR, 0.74), compared with never users.
Data source: A prospective cohort study originally enrolling 46,000 women who were followed for up to 44 years.
Disclosures: The study was funded by the Royal College of General Practitioners, Medical Research Council, Imperial Cancer Research Fund, British Heart Foundation, Schering AG, Schering Health Care, Wyeth Ayerst International, Ortho Cilag, and Searle. The researchers reported having no conflicts of interest.
Overweight, obesity linked to pelvic organ prolapse risk
Older age and parity are established risk factors for pelvic organ prolapse, but the role of obesity has not been precisely determined. Results from a new meta-analysis show that overweight and obese women are significantly more likely to experience pelvic organ prolapse, compared with women of normal weight.
Researchers identified 22 published observational studies of varying design that evaluated pelvic organ prolapse (POP) and obesity. The studies enrolled 96,875 participants and logged 17,249 POP cases, of which 3,043 were considered clinically significant, and 2,359 cases that were classified as self-reported/symptomatic POP (Am J Obstet Gynecol. 2017 Feb 7. doi: 10.1016/j.ajog.2017.01.039)
Ayush Giri, PhD, of Vanderbilt University in Nashville, and his colleagues, found that overweight women (BMI of 25-30 kg/m2) had a risk ratio ranging from 1.36 to 1.40, compared with normal-weight women. For obese women (BMI of 30 kg/m2 or greater) there was a risk ratio ranging from 1.47 to 1.61, compared with normal-weight women. The association between overweight and obesity and POP was stronger when the POP was clinically significant rather than self-reported and symptomatic.
The researchers called for more studies to prospectively evaluate the the association between obesity and POP.
In the meantime, they wrote, more can be done to educate women. “From a policy perspective, educating parous women about the association between obesity and POP, a common, yet less often talked about condition with debilitating effects on quality of life, may not only help reduce future burden of POP but may also help reduce obesity and related comorbidities in the population.”
The researchers reported having no conflicts of interest.
Older age and parity are established risk factors for pelvic organ prolapse, but the role of obesity has not been precisely determined. Results from a new meta-analysis show that overweight and obese women are significantly more likely to experience pelvic organ prolapse, compared with women of normal weight.
Researchers identified 22 published observational studies of varying design that evaluated pelvic organ prolapse (POP) and obesity. The studies enrolled 96,875 participants and logged 17,249 POP cases, of which 3,043 were considered clinically significant, and 2,359 cases that were classified as self-reported/symptomatic POP (Am J Obstet Gynecol. 2017 Feb 7. doi: 10.1016/j.ajog.2017.01.039)
Ayush Giri, PhD, of Vanderbilt University in Nashville, and his colleagues, found that overweight women (BMI of 25-30 kg/m2) had a risk ratio ranging from 1.36 to 1.40, compared with normal-weight women. For obese women (BMI of 30 kg/m2 or greater) there was a risk ratio ranging from 1.47 to 1.61, compared with normal-weight women. The association between overweight and obesity and POP was stronger when the POP was clinically significant rather than self-reported and symptomatic.
The researchers called for more studies to prospectively evaluate the the association between obesity and POP.
In the meantime, they wrote, more can be done to educate women. “From a policy perspective, educating parous women about the association between obesity and POP, a common, yet less often talked about condition with debilitating effects on quality of life, may not only help reduce future burden of POP but may also help reduce obesity and related comorbidities in the population.”
The researchers reported having no conflicts of interest.
Older age and parity are established risk factors for pelvic organ prolapse, but the role of obesity has not been precisely determined. Results from a new meta-analysis show that overweight and obese women are significantly more likely to experience pelvic organ prolapse, compared with women of normal weight.
Researchers identified 22 published observational studies of varying design that evaluated pelvic organ prolapse (POP) and obesity. The studies enrolled 96,875 participants and logged 17,249 POP cases, of which 3,043 were considered clinically significant, and 2,359 cases that were classified as self-reported/symptomatic POP (Am J Obstet Gynecol. 2017 Feb 7. doi: 10.1016/j.ajog.2017.01.039)
Ayush Giri, PhD, of Vanderbilt University in Nashville, and his colleagues, found that overweight women (BMI of 25-30 kg/m2) had a risk ratio ranging from 1.36 to 1.40, compared with normal-weight women. For obese women (BMI of 30 kg/m2 or greater) there was a risk ratio ranging from 1.47 to 1.61, compared with normal-weight women. The association between overweight and obesity and POP was stronger when the POP was clinically significant rather than self-reported and symptomatic.
The researchers called for more studies to prospectively evaluate the the association between obesity and POP.
In the meantime, they wrote, more can be done to educate women. “From a policy perspective, educating parous women about the association between obesity and POP, a common, yet less often talked about condition with debilitating effects on quality of life, may not only help reduce future burden of POP but may also help reduce obesity and related comorbidities in the population.”
The researchers reported having no conflicts of interest.
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Key clinical point:
Major finding: Compared with women of normal weight, overweight women had a risk ratio of 1.36-1.40 for pelvic organ prolapse, while obese women had a risk ratio of 1.47-1.61.
Data source: A meta-analysis of 22 observational studies, enrolling nearly 100,000 women, including about 17,000 POP cases, 3,000 of which were considered clinically significant.
Disclosures: The researchers reported having no conflicts of interest.
Thigh muscle weakness predicts knee osteoarthritis in women only
Weakness in the lower thigh muscles is a stronger risk factor for knee osteoarthritis in women than in men, possibly because of the greater influence that high body mass index has on thigh muscle strength in women, according to new case-control study findings.
The findings, published online Feb. 8 in Arthritis Care & Research (doi: 10.1002/acr.23182), come from a study enrolling 161 patients with radiographic knee osteoarthritis and 186 controls without arthritis at baseline who were observed over a 4-year period in the ongoing multicenter Osteoarthritis Initiative cohort study. About 60% of patients and controls were women.
They found that lower muscle-specific strength in these areas significantly increased the risk of incident knee osteoarthritis in women, with odds ratios of 1.47 (95% confidence interval, 1.10-1.96) for knee flexors and 1.41 (95% CI, 1.06-1.89) for extensors. This relationship was not significant in men, and in women, the relationship lost statistical significance after adjustment for high body mass index (BMI). Lower specific strength was associated with higher BMI in women (r = –0.29, P less than .001), but not in men.
“The lower muscle-specific strength in the presence of higher BMI in women (possibly driven by greater intramuscular adiposity), but not in men, may provide a possible explanation” for the differences in knee osteoarthritis incidence in men and women with muscle strength deficits, Dr. Culvenor and colleagues wrote in their analysis.
“The response of thigh muscle to variations in BMI differed between men and women, with apparently more contractile tissue (and strength) being present in men with greater BMI, and apparently more noncontractile (adipose) tissue in women with greater BMI,” the researchers concluded.
The Osteoarthritis Initiative is cofunded by the National Institutes of Health and a consortium of pharmacological manufacturers. The work for this analysis also received funding from Paracelsus Medical University and the European Union Seventh Framework Programme. Three of the study’s seven coauthors disclosed extensive financial relationships, including employment, with Chondrometrics GmbH, a company that provides MRI analysis services, among other firms, while four disclosed no commercial conflicts.
Weakness in the lower thigh muscles is a stronger risk factor for knee osteoarthritis in women than in men, possibly because of the greater influence that high body mass index has on thigh muscle strength in women, according to new case-control study findings.
The findings, published online Feb. 8 in Arthritis Care & Research (doi: 10.1002/acr.23182), come from a study enrolling 161 patients with radiographic knee osteoarthritis and 186 controls without arthritis at baseline who were observed over a 4-year period in the ongoing multicenter Osteoarthritis Initiative cohort study. About 60% of patients and controls were women.
They found that lower muscle-specific strength in these areas significantly increased the risk of incident knee osteoarthritis in women, with odds ratios of 1.47 (95% confidence interval, 1.10-1.96) for knee flexors and 1.41 (95% CI, 1.06-1.89) for extensors. This relationship was not significant in men, and in women, the relationship lost statistical significance after adjustment for high body mass index (BMI). Lower specific strength was associated with higher BMI in women (r = –0.29, P less than .001), but not in men.
“The lower muscle-specific strength in the presence of higher BMI in women (possibly driven by greater intramuscular adiposity), but not in men, may provide a possible explanation” for the differences in knee osteoarthritis incidence in men and women with muscle strength deficits, Dr. Culvenor and colleagues wrote in their analysis.
“The response of thigh muscle to variations in BMI differed between men and women, with apparently more contractile tissue (and strength) being present in men with greater BMI, and apparently more noncontractile (adipose) tissue in women with greater BMI,” the researchers concluded.
The Osteoarthritis Initiative is cofunded by the National Institutes of Health and a consortium of pharmacological manufacturers. The work for this analysis also received funding from Paracelsus Medical University and the European Union Seventh Framework Programme. Three of the study’s seven coauthors disclosed extensive financial relationships, including employment, with Chondrometrics GmbH, a company that provides MRI analysis services, among other firms, while four disclosed no commercial conflicts.
Weakness in the lower thigh muscles is a stronger risk factor for knee osteoarthritis in women than in men, possibly because of the greater influence that high body mass index has on thigh muscle strength in women, according to new case-control study findings.
The findings, published online Feb. 8 in Arthritis Care & Research (doi: 10.1002/acr.23182), come from a study enrolling 161 patients with radiographic knee osteoarthritis and 186 controls without arthritis at baseline who were observed over a 4-year period in the ongoing multicenter Osteoarthritis Initiative cohort study. About 60% of patients and controls were women.
They found that lower muscle-specific strength in these areas significantly increased the risk of incident knee osteoarthritis in women, with odds ratios of 1.47 (95% confidence interval, 1.10-1.96) for knee flexors and 1.41 (95% CI, 1.06-1.89) for extensors. This relationship was not significant in men, and in women, the relationship lost statistical significance after adjustment for high body mass index (BMI). Lower specific strength was associated with higher BMI in women (r = –0.29, P less than .001), but not in men.
“The lower muscle-specific strength in the presence of higher BMI in women (possibly driven by greater intramuscular adiposity), but not in men, may provide a possible explanation” for the differences in knee osteoarthritis incidence in men and women with muscle strength deficits, Dr. Culvenor and colleagues wrote in their analysis.
“The response of thigh muscle to variations in BMI differed between men and women, with apparently more contractile tissue (and strength) being present in men with greater BMI, and apparently more noncontractile (adipose) tissue in women with greater BMI,” the researchers concluded.
The Osteoarthritis Initiative is cofunded by the National Institutes of Health and a consortium of pharmacological manufacturers. The work for this analysis also received funding from Paracelsus Medical University and the European Union Seventh Framework Programme. Three of the study’s seven coauthors disclosed extensive financial relationships, including employment, with Chondrometrics GmbH, a company that provides MRI analysis services, among other firms, while four disclosed no commercial conflicts.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: Weaker thigh muscle significantly increased the risk of incident knee osteoarthritis in women, but after adjusting for BMI the relationship lost significance.
Data source: Men and women (n = 161) with knee osteoarthritis and matched controls (n = 186) without osteoarthritis at baseline who were recruited from a multisite longitudinal cohort.
Disclosures: The Osteoarthritis Initiative is cofunded by the National Institutes of Health and a consortium of pharmacological manufacturers. The work for this analysis also received funding from Paracelsus Medical University and the European Union Seventh Framework Programme. Three of the study’s seven coauthors disclosed extensive financial relationships, including employment, with Chondrometrics GmbH, a company that provides MRI analysis services, among other firms, while four disclosed no commercial conflicts.
Subcutaneous high-dose methotrexate controls psoriasis
Subcutaneous high-dose methotrexate can be safely initiated in people with moderate to severe psoriasis, and produces a rapid and sustained response, researchers found.
Although methotrexate is a first-line agent in moderate to severe psoriasis, and is considerably cheaper than biological agents, much remains unknown about its ideal dosage and route of administration.
Authors of a 2016 systematic review noted that, despite the fact that methotrexate has been used for more than 50 years in psoriasis, high-quality trial evidence remains wanting (PLoS One 2016 May 11. doi: 10.1371/journal.pone.0153740). Recent, well-designed trials have compared methotrexate to biological drugs used in psoriasis rather than placebo. These studies also have used oral formulations of methotrexate, in a range of starting doses as low as 5 mg, rather than subcutaneous formulations.
In their 52-week, multicenter trial conducted across 13 study sites in Europe, Dr. Warren and his colleagues randomized 120 patients to subcutaneous methotrexate at a dose of 17.5 mg/week (n = 91) or sham injections (n = 29) for 16 weeks. Patients in the intervention arm who did not achieve at least 50% improvement on the baseline Psoriasis Area and Severity Index (PASI) score at 8 weeks were increased to 22.5 mg methotrexate per week; 31% received this dose increase.
The study’s primary endpoint was reduction of the PASI score by 75% or more at 16 weeks, which 41% of the intervention arm achieved, compared with 10% of patients in the placebo arm (relative risk 3.93, P = .0026). After 16 weeks, all patients in the cohort were converted to open-label methotrexate for the remainder of the trial, following the same dosing schedule of between 17.5 and 22.5 mg, depending on response at 8 weeks after initiation.
At week 52, PASI 75 response rates were 45% in the methotrexate-methotrexate group and 34% in the placebo-methotrexate group. This compared favorably, the researchers wrote, with a previous study in which the PASI 75 response rate at week 52 was 24% with oral methotrexate at doses of up to 25 mg per week.
No serious adverse events were associated with methotrexate, although gastrointestinal problems (mostly nausea) and elevated liver enzymes were more common in patients receiving the treatment.
“Our findings encourage the use of subcutaneous methotrexate for treatment of psoriasis, and suggest long-term clinical outcomes better than previously reported for oral administration, although final confirmation will be needed in a direct head-to-head trial of subcutaneous versus oral dosing. Our findings might also help to guide future recommendations for the optimum dosing of methotrexate,” the investigators wrote.
Medac Pharma funded the study. Dr. Warren and six of his coauthors disclosed financial relationships with multiple pharmaceutical firms, including the study sponsor, while three coauthors declared no financial conflicts of interest.
The results from this study compare favorably with those of a previous 52-week study of oral methotrexate in this population, suggesting that subcutaneous administration is superior to oral administration in the management of psoriasis. However, response rates for methotrexate are still lower than those reported with biological therapy, especially with infliximab, adalimumab, ustekinumab, and, more recently, the anti-interleukin-17 drugs secukinumab and ixekizumab.
The question that remains is whether methotrexate should remain the first-line systemic therapy for moderate to severe psoriasis. Because we now know that psoriasis is not just skin deep, and that many of the comorbidities – including psoriatic arthritis, metabolic syndrome, and cardiovascular events, in addition to premature death – are related to the extent of skin involvement, perhaps drugs that effectively control inflammation should be used initially. This approach could be addressed only via long-term observations of prospective studies of patients treated with methotrexate, compared with those treated with biological therapy, with collection of information not only about clinical improvement of skin disease, but also about comorbidities.
Dafna D. Gladman, MD, is director of the psoriatic arthritis program at the Centre for Prognosis Studies in The Rheumatic Diseases at Toronto Western Hospital. This comment was excerpted and modified from an editorial (Lancet. 2017;389[10068]:482-3). that accompanied the study by Warren et al. Dr. Gladman disclosed financial relationships, mostly grants and fees related to clinical trials, with several pharmaceutical manufacturers.
The results from this study compare favorably with those of a previous 52-week study of oral methotrexate in this population, suggesting that subcutaneous administration is superior to oral administration in the management of psoriasis. However, response rates for methotrexate are still lower than those reported with biological therapy, especially with infliximab, adalimumab, ustekinumab, and, more recently, the anti-interleukin-17 drugs secukinumab and ixekizumab.
The question that remains is whether methotrexate should remain the first-line systemic therapy for moderate to severe psoriasis. Because we now know that psoriasis is not just skin deep, and that many of the comorbidities – including psoriatic arthritis, metabolic syndrome, and cardiovascular events, in addition to premature death – are related to the extent of skin involvement, perhaps drugs that effectively control inflammation should be used initially. This approach could be addressed only via long-term observations of prospective studies of patients treated with methotrexate, compared with those treated with biological therapy, with collection of information not only about clinical improvement of skin disease, but also about comorbidities.
Dafna D. Gladman, MD, is director of the psoriatic arthritis program at the Centre for Prognosis Studies in The Rheumatic Diseases at Toronto Western Hospital. This comment was excerpted and modified from an editorial (Lancet. 2017;389[10068]:482-3). that accompanied the study by Warren et al. Dr. Gladman disclosed financial relationships, mostly grants and fees related to clinical trials, with several pharmaceutical manufacturers.
The results from this study compare favorably with those of a previous 52-week study of oral methotrexate in this population, suggesting that subcutaneous administration is superior to oral administration in the management of psoriasis. However, response rates for methotrexate are still lower than those reported with biological therapy, especially with infliximab, adalimumab, ustekinumab, and, more recently, the anti-interleukin-17 drugs secukinumab and ixekizumab.
The question that remains is whether methotrexate should remain the first-line systemic therapy for moderate to severe psoriasis. Because we now know that psoriasis is not just skin deep, and that many of the comorbidities – including psoriatic arthritis, metabolic syndrome, and cardiovascular events, in addition to premature death – are related to the extent of skin involvement, perhaps drugs that effectively control inflammation should be used initially. This approach could be addressed only via long-term observations of prospective studies of patients treated with methotrexate, compared with those treated with biological therapy, with collection of information not only about clinical improvement of skin disease, but also about comorbidities.
Dafna D. Gladman, MD, is director of the psoriatic arthritis program at the Centre for Prognosis Studies in The Rheumatic Diseases at Toronto Western Hospital. This comment was excerpted and modified from an editorial (Lancet. 2017;389[10068]:482-3). that accompanied the study by Warren et al. Dr. Gladman disclosed financial relationships, mostly grants and fees related to clinical trials, with several pharmaceutical manufacturers.
Subcutaneous high-dose methotrexate can be safely initiated in people with moderate to severe psoriasis, and produces a rapid and sustained response, researchers found.
Although methotrexate is a first-line agent in moderate to severe psoriasis, and is considerably cheaper than biological agents, much remains unknown about its ideal dosage and route of administration.
Authors of a 2016 systematic review noted that, despite the fact that methotrexate has been used for more than 50 years in psoriasis, high-quality trial evidence remains wanting (PLoS One 2016 May 11. doi: 10.1371/journal.pone.0153740). Recent, well-designed trials have compared methotrexate to biological drugs used in psoriasis rather than placebo. These studies also have used oral formulations of methotrexate, in a range of starting doses as low as 5 mg, rather than subcutaneous formulations.
In their 52-week, multicenter trial conducted across 13 study sites in Europe, Dr. Warren and his colleagues randomized 120 patients to subcutaneous methotrexate at a dose of 17.5 mg/week (n = 91) or sham injections (n = 29) for 16 weeks. Patients in the intervention arm who did not achieve at least 50% improvement on the baseline Psoriasis Area and Severity Index (PASI) score at 8 weeks were increased to 22.5 mg methotrexate per week; 31% received this dose increase.
The study’s primary endpoint was reduction of the PASI score by 75% or more at 16 weeks, which 41% of the intervention arm achieved, compared with 10% of patients in the placebo arm (relative risk 3.93, P = .0026). After 16 weeks, all patients in the cohort were converted to open-label methotrexate for the remainder of the trial, following the same dosing schedule of between 17.5 and 22.5 mg, depending on response at 8 weeks after initiation.
At week 52, PASI 75 response rates were 45% in the methotrexate-methotrexate group and 34% in the placebo-methotrexate group. This compared favorably, the researchers wrote, with a previous study in which the PASI 75 response rate at week 52 was 24% with oral methotrexate at doses of up to 25 mg per week.
No serious adverse events were associated with methotrexate, although gastrointestinal problems (mostly nausea) and elevated liver enzymes were more common in patients receiving the treatment.
“Our findings encourage the use of subcutaneous methotrexate for treatment of psoriasis, and suggest long-term clinical outcomes better than previously reported for oral administration, although final confirmation will be needed in a direct head-to-head trial of subcutaneous versus oral dosing. Our findings might also help to guide future recommendations for the optimum dosing of methotrexate,” the investigators wrote.
Medac Pharma funded the study. Dr. Warren and six of his coauthors disclosed financial relationships with multiple pharmaceutical firms, including the study sponsor, while three coauthors declared no financial conflicts of interest.
Subcutaneous high-dose methotrexate can be safely initiated in people with moderate to severe psoriasis, and produces a rapid and sustained response, researchers found.
Although methotrexate is a first-line agent in moderate to severe psoriasis, and is considerably cheaper than biological agents, much remains unknown about its ideal dosage and route of administration.
Authors of a 2016 systematic review noted that, despite the fact that methotrexate has been used for more than 50 years in psoriasis, high-quality trial evidence remains wanting (PLoS One 2016 May 11. doi: 10.1371/journal.pone.0153740). Recent, well-designed trials have compared methotrexate to biological drugs used in psoriasis rather than placebo. These studies also have used oral formulations of methotrexate, in a range of starting doses as low as 5 mg, rather than subcutaneous formulations.
In their 52-week, multicenter trial conducted across 13 study sites in Europe, Dr. Warren and his colleagues randomized 120 patients to subcutaneous methotrexate at a dose of 17.5 mg/week (n = 91) or sham injections (n = 29) for 16 weeks. Patients in the intervention arm who did not achieve at least 50% improvement on the baseline Psoriasis Area and Severity Index (PASI) score at 8 weeks were increased to 22.5 mg methotrexate per week; 31% received this dose increase.
The study’s primary endpoint was reduction of the PASI score by 75% or more at 16 weeks, which 41% of the intervention arm achieved, compared with 10% of patients in the placebo arm (relative risk 3.93, P = .0026). After 16 weeks, all patients in the cohort were converted to open-label methotrexate for the remainder of the trial, following the same dosing schedule of between 17.5 and 22.5 mg, depending on response at 8 weeks after initiation.
At week 52, PASI 75 response rates were 45% in the methotrexate-methotrexate group and 34% in the placebo-methotrexate group. This compared favorably, the researchers wrote, with a previous study in which the PASI 75 response rate at week 52 was 24% with oral methotrexate at doses of up to 25 mg per week.
No serious adverse events were associated with methotrexate, although gastrointestinal problems (mostly nausea) and elevated liver enzymes were more common in patients receiving the treatment.
“Our findings encourage the use of subcutaneous methotrexate for treatment of psoriasis, and suggest long-term clinical outcomes better than previously reported for oral administration, although final confirmation will be needed in a direct head-to-head trial of subcutaneous versus oral dosing. Our findings might also help to guide future recommendations for the optimum dosing of methotrexate,” the investigators wrote.
Medac Pharma funded the study. Dr. Warren and six of his coauthors disclosed financial relationships with multiple pharmaceutical firms, including the study sponsor, while three coauthors declared no financial conflicts of interest.
FROM THE LANCET
Key clinical point:
Major finding: At 16 weeks, 41% of patients started on methotrexate achieved a 75% reduction in psoriasis severity scores, compared with 10% of patients in the placebo arm. At 1 year of treatment, 45% of patients saw this level of response.
Data source: A multisite, placebo-controlled trial randomizing 120 patients to subcutaneous methotrexate or placebo for 16 weeks, then converting all patients to open-label subcutaneous methotrexate through week 52.
Disclosures: Medac Pharma funded the study. Dr. Warren and six of his coauthors disclosed financial relationships with multiple pharmaceutical firms, including the study sponsor, while three coauthors declared no financial conflicts of interest.
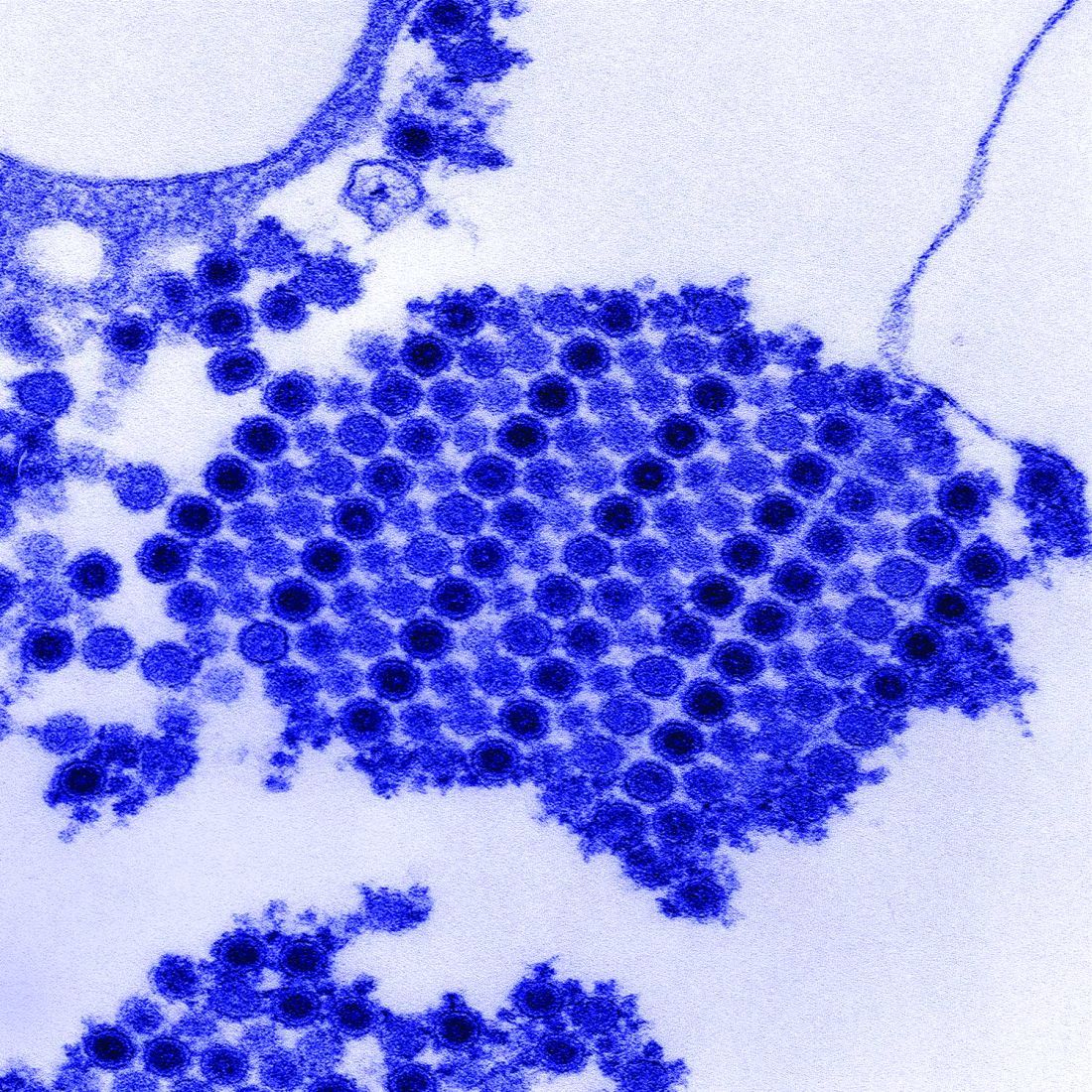
Chikungunya arthritis symptoms reduced with immunomodulatory drugs
Several different currently approved immunomodulatory therapies ameliorated arthritis symptoms in chikungunya-infected mice in two studies that separate teams of researchers published online Feb. 1 in Science Translational Medicine.
The first team, led by Jonathan J. Miner, MD, PhD, of Washington University in St. Louis tested six different approved oral and biologic antirheumatic agents (along with control agents) in chikungunya virus-infected mice with acute arthritis and foot swelling (Sci Transl Med. 2017;9:eaah3438).
When the researchers paired abatacept with an antiviral therapy (monoclonal anti-CHIKV human antibody) the combination “was highly effective at reducing joint inflammation, periarticular swelling, migration of inflammatory leukocytes, and infection, even when administered several days after virus inoculation,” Dr. Miner and his colleagues wrote.
The researchers concluded that a combination of anti-inflammatory and antibody-based antiviral therapy “may serve as a model for treating humans with arthritis caused by CHIKV or other related viruses.”
In the second study, researchers led by Teck-Hui Teo, PhD, of the Agency for Science, Technology and Research (A*STAR) in Singapore, further elucidated the mechanisms by which CHIKV proteins act on T cells (Sci Transl Med. 2017;9:eaal1333). They also found that CHIKV-infected mice treated with fingolimod (Gilenya), a drug that blocks T-cell migration from the lymph nodes to the joints and is approved for the treatment of multiple sclerosis, saw reduced arthritis symptoms even without reduction of viral replication.
Infection with the chikungunya virus can produce arthritis that mimics symptoms of rheumatoid arthritis and may in some cases lead to joint damage. Though the mechanisms driving chikungunya-related arthritis are not well understood, preliminary studies have suggested a T-cell–mediated adverse response.
The Singapore team received funding from its own agency, A*STAR, while the Washington University researchers received grants from the National Institutes of Health and the Rheumatology Research Foundation. Two coauthors on the U.S. study reported extensive commercial conflicts, including consulting and advisory relationships with pharmaceutical and vaccine manufacturers, and one patent.
The studies by Dr. Miner and his colleagues and Dr. Teo and his associates demonstrate the potential value of combination therapies for ameliorating heightened T-cell responses and their pathogenic role in joint inflammation. They explored how T-cell responses could be blunted during ongoing viral replication to control overt inflammation, an approach that also may be valuable for treating immune-mediated tissue damage associated with other infectious agents.
Selective T-cell immunomodulatory therapies that offset damaging immune responses offer an attractive option for future pharmacologic interventions for treating chikungunya virus–induced inflammatory disease. The small market size and the rapid sporadic nature of outbreaks could be major obstacles to the development and deployment of virus-specific interventions such as therapeutic antiviral neutralizing monoclonal antibodies or even vaccines. Targeted drug and immunotherapy treatments are likely to offer practical and beneficial options for most patients with chikungunya.
Preliminary reports in humans have suggested that methotrexate may be effective for treating chikungunya virus–induced arthritis. In Dr. Miner and colleagues’ study, a low dose of methotrexate (0.3 mg/kg) was ineffective at treating acute joint swelling in mice. It remains to be addressed whether a higher dose of methotrexate for a longer time period could be of benefit in the setting of chronic chikungunya virus–induced arthritis.
Philippe Gasque, MD, PhD, is with the Université de La Réunion, Saint-Denis, Réunion, and Marie Christine Jaffar-Bandjee, MD, PhD, is with the Centre Hospitalier Universitaire Félix Guyon, Saint-Denis, Réunion. They made these remarks in an editorial (Sci Transl Med. 2017;9:eaam6567).
The studies by Dr. Miner and his colleagues and Dr. Teo and his associates demonstrate the potential value of combination therapies for ameliorating heightened T-cell responses and their pathogenic role in joint inflammation. They explored how T-cell responses could be blunted during ongoing viral replication to control overt inflammation, an approach that also may be valuable for treating immune-mediated tissue damage associated with other infectious agents.
Selective T-cell immunomodulatory therapies that offset damaging immune responses offer an attractive option for future pharmacologic interventions for treating chikungunya virus–induced inflammatory disease. The small market size and the rapid sporadic nature of outbreaks could be major obstacles to the development and deployment of virus-specific interventions such as therapeutic antiviral neutralizing monoclonal antibodies or even vaccines. Targeted drug and immunotherapy treatments are likely to offer practical and beneficial options for most patients with chikungunya.
Preliminary reports in humans have suggested that methotrexate may be effective for treating chikungunya virus–induced arthritis. In Dr. Miner and colleagues’ study, a low dose of methotrexate (0.3 mg/kg) was ineffective at treating acute joint swelling in mice. It remains to be addressed whether a higher dose of methotrexate for a longer time period could be of benefit in the setting of chronic chikungunya virus–induced arthritis.
Philippe Gasque, MD, PhD, is with the Université de La Réunion, Saint-Denis, Réunion, and Marie Christine Jaffar-Bandjee, MD, PhD, is with the Centre Hospitalier Universitaire Félix Guyon, Saint-Denis, Réunion. They made these remarks in an editorial (Sci Transl Med. 2017;9:eaam6567).
The studies by Dr. Miner and his colleagues and Dr. Teo and his associates demonstrate the potential value of combination therapies for ameliorating heightened T-cell responses and their pathogenic role in joint inflammation. They explored how T-cell responses could be blunted during ongoing viral replication to control overt inflammation, an approach that also may be valuable for treating immune-mediated tissue damage associated with other infectious agents.
Selective T-cell immunomodulatory therapies that offset damaging immune responses offer an attractive option for future pharmacologic interventions for treating chikungunya virus–induced inflammatory disease. The small market size and the rapid sporadic nature of outbreaks could be major obstacles to the development and deployment of virus-specific interventions such as therapeutic antiviral neutralizing monoclonal antibodies or even vaccines. Targeted drug and immunotherapy treatments are likely to offer practical and beneficial options for most patients with chikungunya.
Preliminary reports in humans have suggested that methotrexate may be effective for treating chikungunya virus–induced arthritis. In Dr. Miner and colleagues’ study, a low dose of methotrexate (0.3 mg/kg) was ineffective at treating acute joint swelling in mice. It remains to be addressed whether a higher dose of methotrexate for a longer time period could be of benefit in the setting of chronic chikungunya virus–induced arthritis.
Philippe Gasque, MD, PhD, is with the Université de La Réunion, Saint-Denis, Réunion, and Marie Christine Jaffar-Bandjee, MD, PhD, is with the Centre Hospitalier Universitaire Félix Guyon, Saint-Denis, Réunion. They made these remarks in an editorial (Sci Transl Med. 2017;9:eaam6567).
Several different currently approved immunomodulatory therapies ameliorated arthritis symptoms in chikungunya-infected mice in two studies that separate teams of researchers published online Feb. 1 in Science Translational Medicine.
The first team, led by Jonathan J. Miner, MD, PhD, of Washington University in St. Louis tested six different approved oral and biologic antirheumatic agents (along with control agents) in chikungunya virus-infected mice with acute arthritis and foot swelling (Sci Transl Med. 2017;9:eaah3438).
When the researchers paired abatacept with an antiviral therapy (monoclonal anti-CHIKV human antibody) the combination “was highly effective at reducing joint inflammation, periarticular swelling, migration of inflammatory leukocytes, and infection, even when administered several days after virus inoculation,” Dr. Miner and his colleagues wrote.
The researchers concluded that a combination of anti-inflammatory and antibody-based antiviral therapy “may serve as a model for treating humans with arthritis caused by CHIKV or other related viruses.”
In the second study, researchers led by Teck-Hui Teo, PhD, of the Agency for Science, Technology and Research (A*STAR) in Singapore, further elucidated the mechanisms by which CHIKV proteins act on T cells (Sci Transl Med. 2017;9:eaal1333). They also found that CHIKV-infected mice treated with fingolimod (Gilenya), a drug that blocks T-cell migration from the lymph nodes to the joints and is approved for the treatment of multiple sclerosis, saw reduced arthritis symptoms even without reduction of viral replication.
Infection with the chikungunya virus can produce arthritis that mimics symptoms of rheumatoid arthritis and may in some cases lead to joint damage. Though the mechanisms driving chikungunya-related arthritis are not well understood, preliminary studies have suggested a T-cell–mediated adverse response.
The Singapore team received funding from its own agency, A*STAR, while the Washington University researchers received grants from the National Institutes of Health and the Rheumatology Research Foundation. Two coauthors on the U.S. study reported extensive commercial conflicts, including consulting and advisory relationships with pharmaceutical and vaccine manufacturers, and one patent.
Several different currently approved immunomodulatory therapies ameliorated arthritis symptoms in chikungunya-infected mice in two studies that separate teams of researchers published online Feb. 1 in Science Translational Medicine.
The first team, led by Jonathan J. Miner, MD, PhD, of Washington University in St. Louis tested six different approved oral and biologic antirheumatic agents (along with control agents) in chikungunya virus-infected mice with acute arthritis and foot swelling (Sci Transl Med. 2017;9:eaah3438).
When the researchers paired abatacept with an antiviral therapy (monoclonal anti-CHIKV human antibody) the combination “was highly effective at reducing joint inflammation, periarticular swelling, migration of inflammatory leukocytes, and infection, even when administered several days after virus inoculation,” Dr. Miner and his colleagues wrote.
The researchers concluded that a combination of anti-inflammatory and antibody-based antiviral therapy “may serve as a model for treating humans with arthritis caused by CHIKV or other related viruses.”
In the second study, researchers led by Teck-Hui Teo, PhD, of the Agency for Science, Technology and Research (A*STAR) in Singapore, further elucidated the mechanisms by which CHIKV proteins act on T cells (Sci Transl Med. 2017;9:eaal1333). They also found that CHIKV-infected mice treated with fingolimod (Gilenya), a drug that blocks T-cell migration from the lymph nodes to the joints and is approved for the treatment of multiple sclerosis, saw reduced arthritis symptoms even without reduction of viral replication.
Infection with the chikungunya virus can produce arthritis that mimics symptoms of rheumatoid arthritis and may in some cases lead to joint damage. Though the mechanisms driving chikungunya-related arthritis are not well understood, preliminary studies have suggested a T-cell–mediated adverse response.
The Singapore team received funding from its own agency, A*STAR, while the Washington University researchers received grants from the National Institutes of Health and the Rheumatology Research Foundation. Two coauthors on the U.S. study reported extensive commercial conflicts, including consulting and advisory relationships with pharmaceutical and vaccine manufacturers, and one patent.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Abatacept, tofacitinib, and fingolimod all reduced arthritis symptoms, compared with controls.
Data source: Two studies testing multiple immunomodulatory or antirheumatic agents in chikungunya virus–infected mice.
Disclosures: The Agency for Science, Technology and Research (A*STAR) funded the Singapore researchers, while grants from the NIH and the Rheumatology Research Foundation funded the U.S. team. Two coauthors on the U.S. study disclosed extensive financial relationships with multiple pharmaceutical and vaccine manufacturers.
Lung cancer screening a challenge to implement
A comprehensive lung cancer screening program carried out at Veterans Health Administration hospitals was taxing to implement and revealed a large number of patients with results requiring follow-up, though only 1.5% had cancers.
Investigators at eight VHA hospitals, led by Linda S. Kinsinger, MD, of the VHA’s National Center for Health Promotion and Disease Prevention in Durham, N.C., looked at records from about 93,000 primary care patients and identified 4,246 eligible for screening, based on age, medical history, and smoking history (JAMA Intern Med. 2017 Jan 30. doi: 10.1001/jamainternmed.2016.9022).
Approximately 58% of the eligible patients consented, and 2,106 underwent screening with low-dose computed tomography (LDCT). The mean age of patients was 65 years, and 96% of patients were male.
Nearly 60% of patients screened (1,257) had nodules, 1,184 patients (56.2%) required tracking, and 31 patients (1.5%) had lung cancer.
The pilot study was developed in response to a 2013 recommendation from the U.S. Preventive Services Task Force favoring annual screening with LDCT in current or former heavy smokers between 55 and 80 years old.
The recommendation sparked concerns about the practicability of implementing large-scale lung cancer screening, which Dr. Kinsinger and her colleagues’ study seemed to underscore. For example, “creating electronic tools to capture the necessary clinical data in real time … proved to be difficult, even with the VHA’s highly regarded electronic medical record,” the investigators wrote. A key measure used in the screening program – cigarette pack-years – was “not fully captured” in the system’s EMR.
The investigators also noted that if the eligibility criteria used in the pilot program were applied to the VHA nationwide, about 900,000 patients would be eligible for LDCT screening, and that fewer than 60% of patients in this study had consented. That meant that “accurately identifying these patients and discussing with them the benefits and harms of [screening] will take significant effort for primary care teams,” the researchers noted.
In addition, the required follow-up “may stress the capacity” of radiology and pulmonology services, the study authors cautioned.
Finally, “primary care will need to be involved in deciding which incidental findings need further evaluation,” they wrote. “These clinical efforts will require coordination and communication among clinical services and between patients and staff, and dedicated coordinators will need to be hired.”
The investigators noted that their findings might not be generalizable to non-VHA health care systems. The experience of the VHA, “owing to its central organizational structure, may represent a best-case scenario,” they wrote.
The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
A comprehensive lung cancer screening program carried out at Veterans Health Administration hospitals was taxing to implement and revealed a large number of patients with results requiring follow-up, though only 1.5% had cancers.
Investigators at eight VHA hospitals, led by Linda S. Kinsinger, MD, of the VHA’s National Center for Health Promotion and Disease Prevention in Durham, N.C., looked at records from about 93,000 primary care patients and identified 4,246 eligible for screening, based on age, medical history, and smoking history (JAMA Intern Med. 2017 Jan 30. doi: 10.1001/jamainternmed.2016.9022).
Approximately 58% of the eligible patients consented, and 2,106 underwent screening with low-dose computed tomography (LDCT). The mean age of patients was 65 years, and 96% of patients were male.
Nearly 60% of patients screened (1,257) had nodules, 1,184 patients (56.2%) required tracking, and 31 patients (1.5%) had lung cancer.
The pilot study was developed in response to a 2013 recommendation from the U.S. Preventive Services Task Force favoring annual screening with LDCT in current or former heavy smokers between 55 and 80 years old.
The recommendation sparked concerns about the practicability of implementing large-scale lung cancer screening, which Dr. Kinsinger and her colleagues’ study seemed to underscore. For example, “creating electronic tools to capture the necessary clinical data in real time … proved to be difficult, even with the VHA’s highly regarded electronic medical record,” the investigators wrote. A key measure used in the screening program – cigarette pack-years – was “not fully captured” in the system’s EMR.
The investigators also noted that if the eligibility criteria used in the pilot program were applied to the VHA nationwide, about 900,000 patients would be eligible for LDCT screening, and that fewer than 60% of patients in this study had consented. That meant that “accurately identifying these patients and discussing with them the benefits and harms of [screening] will take significant effort for primary care teams,” the researchers noted.
In addition, the required follow-up “may stress the capacity” of radiology and pulmonology services, the study authors cautioned.
Finally, “primary care will need to be involved in deciding which incidental findings need further evaluation,” they wrote. “These clinical efforts will require coordination and communication among clinical services and between patients and staff, and dedicated coordinators will need to be hired.”
The investigators noted that their findings might not be generalizable to non-VHA health care systems. The experience of the VHA, “owing to its central organizational structure, may represent a best-case scenario,” they wrote.
The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
A comprehensive lung cancer screening program carried out at Veterans Health Administration hospitals was taxing to implement and revealed a large number of patients with results requiring follow-up, though only 1.5% had cancers.
Investigators at eight VHA hospitals, led by Linda S. Kinsinger, MD, of the VHA’s National Center for Health Promotion and Disease Prevention in Durham, N.C., looked at records from about 93,000 primary care patients and identified 4,246 eligible for screening, based on age, medical history, and smoking history (JAMA Intern Med. 2017 Jan 30. doi: 10.1001/jamainternmed.2016.9022).
Approximately 58% of the eligible patients consented, and 2,106 underwent screening with low-dose computed tomography (LDCT). The mean age of patients was 65 years, and 96% of patients were male.
Nearly 60% of patients screened (1,257) had nodules, 1,184 patients (56.2%) required tracking, and 31 patients (1.5%) had lung cancer.
The pilot study was developed in response to a 2013 recommendation from the U.S. Preventive Services Task Force favoring annual screening with LDCT in current or former heavy smokers between 55 and 80 years old.
The recommendation sparked concerns about the practicability of implementing large-scale lung cancer screening, which Dr. Kinsinger and her colleagues’ study seemed to underscore. For example, “creating electronic tools to capture the necessary clinical data in real time … proved to be difficult, even with the VHA’s highly regarded electronic medical record,” the investigators wrote. A key measure used in the screening program – cigarette pack-years – was “not fully captured” in the system’s EMR.
The investigators also noted that if the eligibility criteria used in the pilot program were applied to the VHA nationwide, about 900,000 patients would be eligible for LDCT screening, and that fewer than 60% of patients in this study had consented. That meant that “accurately identifying these patients and discussing with them the benefits and harms of [screening] will take significant effort for primary care teams,” the researchers noted.
In addition, the required follow-up “may stress the capacity” of radiology and pulmonology services, the study authors cautioned.
Finally, “primary care will need to be involved in deciding which incidental findings need further evaluation,” they wrote. “These clinical efforts will require coordination and communication among clinical services and between patients and staff, and dedicated coordinators will need to be hired.”
The investigators noted that their findings might not be generalizable to non-VHA health care systems. The experience of the VHA, “owing to its central organizational structure, may represent a best-case scenario,” they wrote.
The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Comprehensive lung cancer screening is complex to implement in hospital primary care settings and may trigger resource-intensive follow-up.
Major finding: Of more than 2,000 patients screened, nearly 60% were positive for nodules, though only 1.5% had cancer.
Data source: A pilot study in 4,246 eligible primary care patients at eight Veterans Health Administration hospitals; 2,106 were screened using low-dose computed tomography.
Disclosures: The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
Hypothermia confers no benefits in children with cardiac arrest
Comatose children who survived cardiac arrest in the hospital do not benefit more from treatment with therapeutic hypothermia than from keeping their body temperatures normal, according to results from a randomized trial conducted in 37 hospitals in three countries.
The findings were presented in Honolulu at the Critical Care Congress, sponsored by the Society for Critical Care Medicine, and published online Jan. 24 in the New England Journal of Medicine (2017 Jan 24. doi: 10.1056/NEJMoa1610493). They add to a growing consensus from adult studies that the use of induced hypothermia to prevent fevers and neurologic injury after cardiac arrest does not confer additional survival or functional benefit over normothermia. Less was known about children, particularly those whose cardiac arrest occurred in a hospital setting.
Frank W. Moler, MD, of the University of Michigan, Ann Arbor, led the study, which randomized 329 comatose children, from newborns to age 18 years, to either 120 hours of normothermia (target temperature, 36.8° C) or 48 hours of hypothermia (33°) followed by normal temperature maintenance to 120 days following an in-hospital cardiac arrest.
Fever prevention in both groups was achieved through active intervention, with hypothermia-treated patients also having been pharmacologically paralyzed and sedated. The investigators used the Vineland Adaptive Behavioral Scales to measure neurobehavioral function, with a score of 70 or higher deemed indicative of good function.
The study’s primary outcome was survival at 12 months after cardiac arrest and a favorable neurobehavioral outcome. In the 257 children with scores of 70 or higher before cardiac arrest, no significant differences were seen between the two different groups, with 36% of the hypothermia-treated patients (48/133) and 39% of normothermia-treated patients (48/124) surviving with a favorable neurobehavioral outcome (relative risk, 0.92; 95% confidence interval, 0.67-1.27; P = .63). In 317 children who could be evaluated for changes in neurobehavioral function, the changes from baseline between groups did not reach statistical significance (P = .70), and 1-year survival also did not differ significantly (49% for hypothermia-treated vs. 46% for normothermia; RR, 1.07; 95% CI, 0.85-1.34, P = .56). Adverse events did not differ significantly between groups.
The trial was stopped early for futility, leaving fewer than the hoped-for number of patients available for analysis, and wider confidence intervals. However, the investigators said their hypothesized 15 percentage point benefit for hypothermia treatment could be ruled out. Dr. Moler and his colleagues wrote in their analysis that unanswered questions remain regarding the role of body temperature interventions in this population, noting that different duration of treatment, different temperatures, and combination of temperature management with neuroprotective agents are worth considering for future studies. Dr. Moler and his colleagues’ study was funded by the National Heart, Lung, and Blood Institute. Four of its 49 coauthors disclosed commercial conflicts of interest.
Comatose children who survived cardiac arrest in the hospital do not benefit more from treatment with therapeutic hypothermia than from keeping their body temperatures normal, according to results from a randomized trial conducted in 37 hospitals in three countries.
The findings were presented in Honolulu at the Critical Care Congress, sponsored by the Society for Critical Care Medicine, and published online Jan. 24 in the New England Journal of Medicine (2017 Jan 24. doi: 10.1056/NEJMoa1610493). They add to a growing consensus from adult studies that the use of induced hypothermia to prevent fevers and neurologic injury after cardiac arrest does not confer additional survival or functional benefit over normothermia. Less was known about children, particularly those whose cardiac arrest occurred in a hospital setting.
Frank W. Moler, MD, of the University of Michigan, Ann Arbor, led the study, which randomized 329 comatose children, from newborns to age 18 years, to either 120 hours of normothermia (target temperature, 36.8° C) or 48 hours of hypothermia (33°) followed by normal temperature maintenance to 120 days following an in-hospital cardiac arrest.
Fever prevention in both groups was achieved through active intervention, with hypothermia-treated patients also having been pharmacologically paralyzed and sedated. The investigators used the Vineland Adaptive Behavioral Scales to measure neurobehavioral function, with a score of 70 or higher deemed indicative of good function.
The study’s primary outcome was survival at 12 months after cardiac arrest and a favorable neurobehavioral outcome. In the 257 children with scores of 70 or higher before cardiac arrest, no significant differences were seen between the two different groups, with 36% of the hypothermia-treated patients (48/133) and 39% of normothermia-treated patients (48/124) surviving with a favorable neurobehavioral outcome (relative risk, 0.92; 95% confidence interval, 0.67-1.27; P = .63). In 317 children who could be evaluated for changes in neurobehavioral function, the changes from baseline between groups did not reach statistical significance (P = .70), and 1-year survival also did not differ significantly (49% for hypothermia-treated vs. 46% for normothermia; RR, 1.07; 95% CI, 0.85-1.34, P = .56). Adverse events did not differ significantly between groups.
The trial was stopped early for futility, leaving fewer than the hoped-for number of patients available for analysis, and wider confidence intervals. However, the investigators said their hypothesized 15 percentage point benefit for hypothermia treatment could be ruled out. Dr. Moler and his colleagues wrote in their analysis that unanswered questions remain regarding the role of body temperature interventions in this population, noting that different duration of treatment, different temperatures, and combination of temperature management with neuroprotective agents are worth considering for future studies. Dr. Moler and his colleagues’ study was funded by the National Heart, Lung, and Blood Institute. Four of its 49 coauthors disclosed commercial conflicts of interest.
Comatose children who survived cardiac arrest in the hospital do not benefit more from treatment with therapeutic hypothermia than from keeping their body temperatures normal, according to results from a randomized trial conducted in 37 hospitals in three countries.
The findings were presented in Honolulu at the Critical Care Congress, sponsored by the Society for Critical Care Medicine, and published online Jan. 24 in the New England Journal of Medicine (2017 Jan 24. doi: 10.1056/NEJMoa1610493). They add to a growing consensus from adult studies that the use of induced hypothermia to prevent fevers and neurologic injury after cardiac arrest does not confer additional survival or functional benefit over normothermia. Less was known about children, particularly those whose cardiac arrest occurred in a hospital setting.
Frank W. Moler, MD, of the University of Michigan, Ann Arbor, led the study, which randomized 329 comatose children, from newborns to age 18 years, to either 120 hours of normothermia (target temperature, 36.8° C) or 48 hours of hypothermia (33°) followed by normal temperature maintenance to 120 days following an in-hospital cardiac arrest.
Fever prevention in both groups was achieved through active intervention, with hypothermia-treated patients also having been pharmacologically paralyzed and sedated. The investigators used the Vineland Adaptive Behavioral Scales to measure neurobehavioral function, with a score of 70 or higher deemed indicative of good function.
The study’s primary outcome was survival at 12 months after cardiac arrest and a favorable neurobehavioral outcome. In the 257 children with scores of 70 or higher before cardiac arrest, no significant differences were seen between the two different groups, with 36% of the hypothermia-treated patients (48/133) and 39% of normothermia-treated patients (48/124) surviving with a favorable neurobehavioral outcome (relative risk, 0.92; 95% confidence interval, 0.67-1.27; P = .63). In 317 children who could be evaluated for changes in neurobehavioral function, the changes from baseline between groups did not reach statistical significance (P = .70), and 1-year survival also did not differ significantly (49% for hypothermia-treated vs. 46% for normothermia; RR, 1.07; 95% CI, 0.85-1.34, P = .56). Adverse events did not differ significantly between groups.
The trial was stopped early for futility, leaving fewer than the hoped-for number of patients available for analysis, and wider confidence intervals. However, the investigators said their hypothesized 15 percentage point benefit for hypothermia treatment could be ruled out. Dr. Moler and his colleagues wrote in their analysis that unanswered questions remain regarding the role of body temperature interventions in this population, noting that different duration of treatment, different temperatures, and combination of temperature management with neuroprotective agents are worth considering for future studies. Dr. Moler and his colleagues’ study was funded by the National Heart, Lung, and Blood Institute. Four of its 49 coauthors disclosed commercial conflicts of interest.
FROM THE CRITICAL CARE CONGRESS
Key clinical point: Treating comatose children with hypothermia following cardiac arrest did not produce better neurobehavioral or survival outcomes at 1 year, compared with children whose body temperatures were held to normal.
Major finding: 36% of hypothermia-treated patients and 39% of normothermia-treated patients survived with a favorable neurobehavioral outcome (RR, 0.92; 95% CI, 0.67-1.27; P = .63).
Data source: A multisite, international trial randomizing 329 infants and children comatose after cardiac arrest while in hospital to hypothermia or normothermia.
Disclosures: The National Heart, Lung, and Blood Institute sponsored the study. Several investigators disclosed National Institutes of Health or university funding while four disclosed commercial conflicts.