User login
Therese Borden is the editor of CHEST Physician. After 20 years of research, writing, and editing in the field of international development and economics, she began working in the field of medical editing and has held a variety of editorial positions with the company. She holds a PhD in International Economics from American University, Washington, and a BA in history from the University of Washington, Seattle.
VIDEO: Hybrid thoracoscopic and transcatheter ablation of persistent AF
SEATTLE – The presentation of the late-breaking HISTORIC-AF Trial by Dr. Claudio Muneretto and his colleagues “is a very interesting one, which brings to the table a very different approach of hybrid procedures to treat stand-alone atrial fibrillation,” said Dr. Niv Ad of Inova Heart and Vascular Institute, Falls Church, Va.
Dr. Ad gave his comments in a video interview at the annual meeting of the American Association for Thoracic Surgery.
In his assessment, Dr. Ad noted that such studies are useful and can stimulate discussion, even if he would prefer a prospective, comparative study of all procedures. “I hope someday we can create an algorithm where everything has a place: catheter ablation, hybrid procedures where you do catheter ablation and surgical procedure together or in stage, and the stand-alone Maze procedure on pump,” Dr. Ad said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – The presentation of the late-breaking HISTORIC-AF Trial by Dr. Claudio Muneretto and his colleagues “is a very interesting one, which brings to the table a very different approach of hybrid procedures to treat stand-alone atrial fibrillation,” said Dr. Niv Ad of Inova Heart and Vascular Institute, Falls Church, Va.
Dr. Ad gave his comments in a video interview at the annual meeting of the American Association for Thoracic Surgery.
In his assessment, Dr. Ad noted that such studies are useful and can stimulate discussion, even if he would prefer a prospective, comparative study of all procedures. “I hope someday we can create an algorithm where everything has a place: catheter ablation, hybrid procedures where you do catheter ablation and surgical procedure together or in stage, and the stand-alone Maze procedure on pump,” Dr. Ad said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – The presentation of the late-breaking HISTORIC-AF Trial by Dr. Claudio Muneretto and his colleagues “is a very interesting one, which brings to the table a very different approach of hybrid procedures to treat stand-alone atrial fibrillation,” said Dr. Niv Ad of Inova Heart and Vascular Institute, Falls Church, Va.
Dr. Ad gave his comments in a video interview at the annual meeting of the American Association for Thoracic Surgery.
In his assessment, Dr. Ad noted that such studies are useful and can stimulate discussion, even if he would prefer a prospective, comparative study of all procedures. “I hope someday we can create an algorithm where everything has a place: catheter ablation, hybrid procedures where you do catheter ablation and surgical procedure together or in stage, and the stand-alone Maze procedure on pump,” Dr. Ad said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING
ACS offers information on its Ebola virus transmission resource page
The American College of Surgeons has posted a recommended surgical protocol for possible or confirmed Ebola cases on the Ebola virus transmission resource page. The protocol was developed by Dr. Sherry M. Wren, F.A.C.S., and Dr. Adam L. Kushner, M.P.H., F.A.C.S.
“Elective surgical procedures should not be performed in cases of suspected or confirmed Ebola. In cases where an emergency operation must be performed this protocol should be implemented to minimize risk to hospital personnel. The choice of operative approach (open or [minimally invasive surgery]) should take into consideration minimizing potential hazards to all members of the OR team,” according to the protocol.
The document continues, “Although protocols for personal protective equipment (PPE) are in place to protect health care workers, there is no guideline for operating room personnel and surgical providers who might need to perform an operation on a patient with confirmed or suspected Ebola infection, therefore we have adapted relevant Centers for Disease Control recommendations and apply them specifically to the OR environment.”
Dr. David B. Hoyt, F.A.C.S., executive director of ACS, explains that, “the College, like other societies and various governmental entities, wants to do its part to share resources that may be helpful to the medical community and patients in the face of an emerging presence of Ebola, including this surgical protocol. It is important to emphasize, though, that what we learn about transmission, treatment, and protection will continue to evolve. Ultimately, I think all of us who are disseminating this and various other resources recognize that evidence-based guidelines will ultimately emerge. Until then we must be proactive in sharing even early recommendations from credible sources.”
The resource page provides news, health care organization links, and other helpful information about Ebola. In addition, some guidance on surgical protocols is listed, including an overview of patient transport or transfer to the OR, a surgical checklist, protective equipment and draping, and special instrument requirements. A brief directive on how to handle cases of possible exposure of medical staff also is provided.
The ACS resource page will be updated as new information becomes available.
The American College of Surgeons has posted a recommended surgical protocol for possible or confirmed Ebola cases on the Ebola virus transmission resource page. The protocol was developed by Dr. Sherry M. Wren, F.A.C.S., and Dr. Adam L. Kushner, M.P.H., F.A.C.S.
“Elective surgical procedures should not be performed in cases of suspected or confirmed Ebola. In cases where an emergency operation must be performed this protocol should be implemented to minimize risk to hospital personnel. The choice of operative approach (open or [minimally invasive surgery]) should take into consideration minimizing potential hazards to all members of the OR team,” according to the protocol.
The document continues, “Although protocols for personal protective equipment (PPE) are in place to protect health care workers, there is no guideline for operating room personnel and surgical providers who might need to perform an operation on a patient with confirmed or suspected Ebola infection, therefore we have adapted relevant Centers for Disease Control recommendations and apply them specifically to the OR environment.”
Dr. David B. Hoyt, F.A.C.S., executive director of ACS, explains that, “the College, like other societies and various governmental entities, wants to do its part to share resources that may be helpful to the medical community and patients in the face of an emerging presence of Ebola, including this surgical protocol. It is important to emphasize, though, that what we learn about transmission, treatment, and protection will continue to evolve. Ultimately, I think all of us who are disseminating this and various other resources recognize that evidence-based guidelines will ultimately emerge. Until then we must be proactive in sharing even early recommendations from credible sources.”
The resource page provides news, health care organization links, and other helpful information about Ebola. In addition, some guidance on surgical protocols is listed, including an overview of patient transport or transfer to the OR, a surgical checklist, protective equipment and draping, and special instrument requirements. A brief directive on how to handle cases of possible exposure of medical staff also is provided.
The ACS resource page will be updated as new information becomes available.
The American College of Surgeons has posted a recommended surgical protocol for possible or confirmed Ebola cases on the Ebola virus transmission resource page. The protocol was developed by Dr. Sherry M. Wren, F.A.C.S., and Dr. Adam L. Kushner, M.P.H., F.A.C.S.
“Elective surgical procedures should not be performed in cases of suspected or confirmed Ebola. In cases where an emergency operation must be performed this protocol should be implemented to minimize risk to hospital personnel. The choice of operative approach (open or [minimally invasive surgery]) should take into consideration minimizing potential hazards to all members of the OR team,” according to the protocol.
The document continues, “Although protocols for personal protective equipment (PPE) are in place to protect health care workers, there is no guideline for operating room personnel and surgical providers who might need to perform an operation on a patient with confirmed or suspected Ebola infection, therefore we have adapted relevant Centers for Disease Control recommendations and apply them specifically to the OR environment.”
Dr. David B. Hoyt, F.A.C.S., executive director of ACS, explains that, “the College, like other societies and various governmental entities, wants to do its part to share resources that may be helpful to the medical community and patients in the face of an emerging presence of Ebola, including this surgical protocol. It is important to emphasize, though, that what we learn about transmission, treatment, and protection will continue to evolve. Ultimately, I think all of us who are disseminating this and various other resources recognize that evidence-based guidelines will ultimately emerge. Until then we must be proactive in sharing even early recommendations from credible sources.”
The resource page provides news, health care organization links, and other helpful information about Ebola. In addition, some guidance on surgical protocols is listed, including an overview of patient transport or transfer to the OR, a surgical checklist, protective equipment and draping, and special instrument requirements. A brief directive on how to handle cases of possible exposure of medical staff also is provided.
The ACS resource page will be updated as new information becomes available.
A century of evolution in trauma resuscitation: The Scudder Oration 2013
WASHINGTON – The medical understanding of shock and trauma resuscitation has evolved over many decades. But cutting-edge research is revolutionizing the understanding of the mechanisms of trauma and will eventually have a profound impact on treatment models, according to Dr. Ronald V. Maier.
Dr. Maier, an ACS Fellow and the Jane and Donald D. Trunkey Professor and vice-chair of the department of surgery at the University of Washington, Seattle, delivered the Scudder Oration on Trauma during the American College of Surgeons Clinical Congress. He discussed the development of treatment models for trauma resuscitation in the 20th century, beginning with Cannon’s toxins theory of shock (Cannon WB. Traumatic Shock. New York: D. Appleton & Co; 1923), and continuing into the 1930s with Blalock’s pioneering work in developing the homeostasis theory of trauma treatment (Arch. Surg.1934;29:837-57) .
Many advancements in the theory of trauma came out of experiences on the battlefields of World War I, World War II, the Korean War, and the Vietnam War, he said.
The progression of ideas about treatment also evolved, beginning with a minimalist approach developed during World War I to the more interventionist models involving blood transfusion developed during the Korean War era, leading to a focus on crystalloid resuscitation and oxygen deficit that became prominent during the Vietnam War.
Dr. Maier traced the progression of interventionist strategies, each supplanted by new models based on improved understanding of the mechanism of trauma and a growing realization that many of the earlier approaches amounted to overtreatment with limited improvement in survival rates.
The recent paradigm is summed up as hypotensive resuscitation, meaning damage control and supporting blood pressure without reaching normotension, taking account of the natural coagulation process that occurs in the body in response to trauma.
"The goal is to recognize that if we try to chase interventions until they’ve completely corrected the system they impact, we will end up overtreating and having all the harmful effects of the treatment," Dr. Maier said.
Dr. Maier discussed the emerging "genomic storm" model of the mechanisms of trauma that zeros in on patterns of genetic expression. "In the overall genomic response of injured patients, there is a major change in the genomic activity. After a major injury, [the expression of] 80% of the genes change significantly." Damage to the immune system is evident, especially as reflected in down regulation of T-cell pathways and responses.
Dr. Maier’s research efforts have yielded new insight into the nature of that genomic shift. "What we were able to show is that in the patients who develop major complications vs. those who do not develop complications after severe injury, there is a limited number of genes that have a marked difference in reactivity." Sixty-four genes have been identified as having a bearing on the risk of complications.
The path to recovery involves a return of those patterns to a pre-trauma state. And the pursuit of a treatment model from this new understanding of the trauma mechanism means finding a way of predicting which patients will achieve that pre-trauma pattern and which will need intervention to prevent complicated outcomes.
The next step in this line of research will involve close scrutiny of individual responses to interventions, with a focus on timing and amounts. The details of the human body’s natural response to trauma are largely unknown, so this research will be expensive and time consuming, but according to Dr. Maier, necessary if progress is to be made in treatment models.
Dr. Maier described the emerging paradigm of trauma resuscitation in terms of chaos theory. Chaos theory in the context of trauma means that for the highly complex biological system that is the human body, small early perturbations can create significant changes in outcome. An example would be a small blood transfusion early in the treatment process of a trauma patient could have a profoundly positive impact on outcomes.
Dr. Maier argued that future treatment models will involve giving patients the correct treatment at the correct time and in the correct amounts based on the particular characteristics of the patient and the injury as determined by an understanding of their genetic response pattern and timing. "We have just been funded to develop a bedside test where, with a half cc of blood, we can test the 64 genes, and hopefully, by trending the responses ... we can predict patients who are going to have numerous, severe complications vs. those patients who will not," he said.
Despite the advances that have been made, Dr. Maier acknowledged the remaining challenges in transforming trauma resuscitation. "The holy grail is to be able to identify what patient needs what therapy. That is what we are still aspiring to find, and we have not achieved it yet."
Dr. Maier stated that he had no disclosures.
WASHINGTON – The medical understanding of shock and trauma resuscitation has evolved over many decades. But cutting-edge research is revolutionizing the understanding of the mechanisms of trauma and will eventually have a profound impact on treatment models, according to Dr. Ronald V. Maier.
Dr. Maier, an ACS Fellow and the Jane and Donald D. Trunkey Professor and vice-chair of the department of surgery at the University of Washington, Seattle, delivered the Scudder Oration on Trauma during the American College of Surgeons Clinical Congress. He discussed the development of treatment models for trauma resuscitation in the 20th century, beginning with Cannon’s toxins theory of shock (Cannon WB. Traumatic Shock. New York: D. Appleton & Co; 1923), and continuing into the 1930s with Blalock’s pioneering work in developing the homeostasis theory of trauma treatment (Arch. Surg.1934;29:837-57) .
Many advancements in the theory of trauma came out of experiences on the battlefields of World War I, World War II, the Korean War, and the Vietnam War, he said.
The progression of ideas about treatment also evolved, beginning with a minimalist approach developed during World War I to the more interventionist models involving blood transfusion developed during the Korean War era, leading to a focus on crystalloid resuscitation and oxygen deficit that became prominent during the Vietnam War.
Dr. Maier traced the progression of interventionist strategies, each supplanted by new models based on improved understanding of the mechanism of trauma and a growing realization that many of the earlier approaches amounted to overtreatment with limited improvement in survival rates.
The recent paradigm is summed up as hypotensive resuscitation, meaning damage control and supporting blood pressure without reaching normotension, taking account of the natural coagulation process that occurs in the body in response to trauma.
"The goal is to recognize that if we try to chase interventions until they’ve completely corrected the system they impact, we will end up overtreating and having all the harmful effects of the treatment," Dr. Maier said.
Dr. Maier discussed the emerging "genomic storm" model of the mechanisms of trauma that zeros in on patterns of genetic expression. "In the overall genomic response of injured patients, there is a major change in the genomic activity. After a major injury, [the expression of] 80% of the genes change significantly." Damage to the immune system is evident, especially as reflected in down regulation of T-cell pathways and responses.
Dr. Maier’s research efforts have yielded new insight into the nature of that genomic shift. "What we were able to show is that in the patients who develop major complications vs. those who do not develop complications after severe injury, there is a limited number of genes that have a marked difference in reactivity." Sixty-four genes have been identified as having a bearing on the risk of complications.
The path to recovery involves a return of those patterns to a pre-trauma state. And the pursuit of a treatment model from this new understanding of the trauma mechanism means finding a way of predicting which patients will achieve that pre-trauma pattern and which will need intervention to prevent complicated outcomes.
The next step in this line of research will involve close scrutiny of individual responses to interventions, with a focus on timing and amounts. The details of the human body’s natural response to trauma are largely unknown, so this research will be expensive and time consuming, but according to Dr. Maier, necessary if progress is to be made in treatment models.
Dr. Maier described the emerging paradigm of trauma resuscitation in terms of chaos theory. Chaos theory in the context of trauma means that for the highly complex biological system that is the human body, small early perturbations can create significant changes in outcome. An example would be a small blood transfusion early in the treatment process of a trauma patient could have a profoundly positive impact on outcomes.
Dr. Maier argued that future treatment models will involve giving patients the correct treatment at the correct time and in the correct amounts based on the particular characteristics of the patient and the injury as determined by an understanding of their genetic response pattern and timing. "We have just been funded to develop a bedside test where, with a half cc of blood, we can test the 64 genes, and hopefully, by trending the responses ... we can predict patients who are going to have numerous, severe complications vs. those patients who will not," he said.
Despite the advances that have been made, Dr. Maier acknowledged the remaining challenges in transforming trauma resuscitation. "The holy grail is to be able to identify what patient needs what therapy. That is what we are still aspiring to find, and we have not achieved it yet."
Dr. Maier stated that he had no disclosures.
WASHINGTON – The medical understanding of shock and trauma resuscitation has evolved over many decades. But cutting-edge research is revolutionizing the understanding of the mechanisms of trauma and will eventually have a profound impact on treatment models, according to Dr. Ronald V. Maier.
Dr. Maier, an ACS Fellow and the Jane and Donald D. Trunkey Professor and vice-chair of the department of surgery at the University of Washington, Seattle, delivered the Scudder Oration on Trauma during the American College of Surgeons Clinical Congress. He discussed the development of treatment models for trauma resuscitation in the 20th century, beginning with Cannon’s toxins theory of shock (Cannon WB. Traumatic Shock. New York: D. Appleton & Co; 1923), and continuing into the 1930s with Blalock’s pioneering work in developing the homeostasis theory of trauma treatment (Arch. Surg.1934;29:837-57) .
Many advancements in the theory of trauma came out of experiences on the battlefields of World War I, World War II, the Korean War, and the Vietnam War, he said.
The progression of ideas about treatment also evolved, beginning with a minimalist approach developed during World War I to the more interventionist models involving blood transfusion developed during the Korean War era, leading to a focus on crystalloid resuscitation and oxygen deficit that became prominent during the Vietnam War.
Dr. Maier traced the progression of interventionist strategies, each supplanted by new models based on improved understanding of the mechanism of trauma and a growing realization that many of the earlier approaches amounted to overtreatment with limited improvement in survival rates.
The recent paradigm is summed up as hypotensive resuscitation, meaning damage control and supporting blood pressure without reaching normotension, taking account of the natural coagulation process that occurs in the body in response to trauma.
"The goal is to recognize that if we try to chase interventions until they’ve completely corrected the system they impact, we will end up overtreating and having all the harmful effects of the treatment," Dr. Maier said.
Dr. Maier discussed the emerging "genomic storm" model of the mechanisms of trauma that zeros in on patterns of genetic expression. "In the overall genomic response of injured patients, there is a major change in the genomic activity. After a major injury, [the expression of] 80% of the genes change significantly." Damage to the immune system is evident, especially as reflected in down regulation of T-cell pathways and responses.
Dr. Maier’s research efforts have yielded new insight into the nature of that genomic shift. "What we were able to show is that in the patients who develop major complications vs. those who do not develop complications after severe injury, there is a limited number of genes that have a marked difference in reactivity." Sixty-four genes have been identified as having a bearing on the risk of complications.
The path to recovery involves a return of those patterns to a pre-trauma state. And the pursuit of a treatment model from this new understanding of the trauma mechanism means finding a way of predicting which patients will achieve that pre-trauma pattern and which will need intervention to prevent complicated outcomes.
The next step in this line of research will involve close scrutiny of individual responses to interventions, with a focus on timing and amounts. The details of the human body’s natural response to trauma are largely unknown, so this research will be expensive and time consuming, but according to Dr. Maier, necessary if progress is to be made in treatment models.
Dr. Maier described the emerging paradigm of trauma resuscitation in terms of chaos theory. Chaos theory in the context of trauma means that for the highly complex biological system that is the human body, small early perturbations can create significant changes in outcome. An example would be a small blood transfusion early in the treatment process of a trauma patient could have a profoundly positive impact on outcomes.
Dr. Maier argued that future treatment models will involve giving patients the correct treatment at the correct time and in the correct amounts based on the particular characteristics of the patient and the injury as determined by an understanding of their genetic response pattern and timing. "We have just been funded to develop a bedside test where, with a half cc of blood, we can test the 64 genes, and hopefully, by trending the responses ... we can predict patients who are going to have numerous, severe complications vs. those patients who will not," he said.
Despite the advances that have been made, Dr. Maier acknowledged the remaining challenges in transforming trauma resuscitation. "The holy grail is to be able to identify what patient needs what therapy. That is what we are still aspiring to find, and we have not achieved it yet."
Dr. Maier stated that he had no disclosures.
A surgeon in troubled times
WASHINGTON – The political violence that plagued Northern Ireland for nearly 40 years has subsided, and the memories of those dark days in Belfast have begun to fade. But for Roy A. J. Spence, OBE, J.D., M.D., LL.D., FRCS, those years of treating trauma patients in the emergency room of the Royal Victoria Hospital in that city served as an important opportunity for learning and service.
Dr. Spence worked with a team of surgeons and other staff to treat thousands of victims of bombings, shootings, torture, kneecapping, and assault that happened in the context of clashes between two sides of a sectarian conflict and the British Army. Dr. Spence, who delivered the I.S. Ravdin Lecture in the Basic and Surgical Sciences during the annual clinical congress of the American College of Surgeons, discussed his experiences and lessons learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
During the worst period of The Troubles, as the conflict is called, emergency room surgeons were treating what were essentially combat injuries in an urban hospital setting. The great majority of the injuries in Belfast occurred within 1 mile of the Royal Victoria Hospital and the Belfast City Hospital, "some at the door of the hospital, some within the hospital, and we even had one patient shot in a bed in the hospital," he said. One victim was killed in the presence of Dr. Spence in the ER.
Dr. Spence, now professor and head of the department of surgery, imaging, and perioperative medicine at Queen’s University of Belfast, stated that despite the at times overwhelming numbers of injured that flooded into the ER, 90% of patients were delivered to the ER within 30 minutes and 50% within 15 minutes. The staff developed systems to speed patients through the ER to treatment and surgery if needed. In 1972 alone, 20,000 individuals were injured in various ways, and most of these injuries occurred in Belfast.
In addition to a streamlined admission process, the surgeons developed their protocol based on lessons learned over the years.
"We had disaster plans, but, in truth, we almost never had a rehearsal. The rehearsals were for real. The rehearsals were occurring day by day."
It became clear in the early years of the conflict that, in most cases, patients were best served if the doctors stayed at the hospital to receive patients instead of rushing to the scene of a bombing or shooting. "We were almost a nuisance if we went to the scene, because there was often continuing gunfire, there were secondary explosions, and sometimes the bodies themselves were booby-trapped."
In addition, the system of handling large numbers of injured patients worked best if there was a senior surgeon and senior nurse at the door to triage patients. Those with minor injuries were taken to a separate room for treatment.
It was also important that one senior surgeon took charge of the situation and led the team. Surgeons discovered that in these crisis situations, x-raying patients could turn into a bottleneck in the treatment process, leading to dangerous delays, so at times surgery proceeded without imaging to save a patient’s life.
Dr. Spence said that the Royal Victoria distinguished itself in treating patients in the midst of a civil war by upholding the highest standards of care, documenting cases thoroughly, and treating all patients with the same level of care. Although the duty surgeons lived in the community, knew many of the victims, were aware of which group had carried out an attack, and even had family members killed in the conflict, Dr. Spence asserted that they maintained their professional standards and did not allow politics to deter them from their duties as physicians.
In the peak years of violence, the early 1970s to the early 1980s, two types of injuries – gunshot wounds to the head and kneecapping trauma – led to innovative treatment plans. The hospital established the standard of care for gunshot wounds to the head in that era, and also pioneered the use of vascular shunts to treat blast-injured limbs. The vascular shunt in particular was considered invaluable by Dr. Spence. This procedure reduced the number of amputations in cases of limb trauma from one-third to less than 10% and "allowed a very unhurried fracture reduction and external fixation."
Dr. Spence noted that general surgeons were valued in the ER because of their capacity to deal with a wide variety of injuries and because of the potentially fatal delays caused by waiting for a specialist. Although specialists were definitely needed and utilized in complex cases, most patients were treated by general surgeons. "I come from a generation that could do chest and abdominal surgery and amputations," said Dr. Spence.
Staff doctors were on call every other night and worked very long hours, a situation no longer allowed in U.K. hospitals. Surgeons worked "until the work was done" to care for all the injured and to maintain continuity of care. "There could be 100 injured people in the ER. You couldn’t just walk out at half past five."
In conclusion, Dr. Spence noted that the extended crisis of violence and trauma resulted in a close-knit "band of brothers, and occasionally, sisters" who worked in trying circumstances as colleagues. Many of those colleagues have left surgery or have died relatively young, and Dr. Spence intended his lecture to be a tribute to their service, dedication, and sacrifice in troubled times.
WASHINGTON – The political violence that plagued Northern Ireland for nearly 40 years has subsided, and the memories of those dark days in Belfast have begun to fade. But for Roy A. J. Spence, OBE, J.D., M.D., LL.D., FRCS, those years of treating trauma patients in the emergency room of the Royal Victoria Hospital in that city served as an important opportunity for learning and service.
Dr. Spence worked with a team of surgeons and other staff to treat thousands of victims of bombings, shootings, torture, kneecapping, and assault that happened in the context of clashes between two sides of a sectarian conflict and the British Army. Dr. Spence, who delivered the I.S. Ravdin Lecture in the Basic and Surgical Sciences during the annual clinical congress of the American College of Surgeons, discussed his experiences and lessons learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
During the worst period of The Troubles, as the conflict is called, emergency room surgeons were treating what were essentially combat injuries in an urban hospital setting. The great majority of the injuries in Belfast occurred within 1 mile of the Royal Victoria Hospital and the Belfast City Hospital, "some at the door of the hospital, some within the hospital, and we even had one patient shot in a bed in the hospital," he said. One victim was killed in the presence of Dr. Spence in the ER.
Dr. Spence, now professor and head of the department of surgery, imaging, and perioperative medicine at Queen’s University of Belfast, stated that despite the at times overwhelming numbers of injured that flooded into the ER, 90% of patients were delivered to the ER within 30 minutes and 50% within 15 minutes. The staff developed systems to speed patients through the ER to treatment and surgery if needed. In 1972 alone, 20,000 individuals were injured in various ways, and most of these injuries occurred in Belfast.
In addition to a streamlined admission process, the surgeons developed their protocol based on lessons learned over the years.
"We had disaster plans, but, in truth, we almost never had a rehearsal. The rehearsals were for real. The rehearsals were occurring day by day."
It became clear in the early years of the conflict that, in most cases, patients were best served if the doctors stayed at the hospital to receive patients instead of rushing to the scene of a bombing or shooting. "We were almost a nuisance if we went to the scene, because there was often continuing gunfire, there were secondary explosions, and sometimes the bodies themselves were booby-trapped."
In addition, the system of handling large numbers of injured patients worked best if there was a senior surgeon and senior nurse at the door to triage patients. Those with minor injuries were taken to a separate room for treatment.
It was also important that one senior surgeon took charge of the situation and led the team. Surgeons discovered that in these crisis situations, x-raying patients could turn into a bottleneck in the treatment process, leading to dangerous delays, so at times surgery proceeded without imaging to save a patient’s life.
Dr. Spence said that the Royal Victoria distinguished itself in treating patients in the midst of a civil war by upholding the highest standards of care, documenting cases thoroughly, and treating all patients with the same level of care. Although the duty surgeons lived in the community, knew many of the victims, were aware of which group had carried out an attack, and even had family members killed in the conflict, Dr. Spence asserted that they maintained their professional standards and did not allow politics to deter them from their duties as physicians.
In the peak years of violence, the early 1970s to the early 1980s, two types of injuries – gunshot wounds to the head and kneecapping trauma – led to innovative treatment plans. The hospital established the standard of care for gunshot wounds to the head in that era, and also pioneered the use of vascular shunts to treat blast-injured limbs. The vascular shunt in particular was considered invaluable by Dr. Spence. This procedure reduced the number of amputations in cases of limb trauma from one-third to less than 10% and "allowed a very unhurried fracture reduction and external fixation."
Dr. Spence noted that general surgeons were valued in the ER because of their capacity to deal with a wide variety of injuries and because of the potentially fatal delays caused by waiting for a specialist. Although specialists were definitely needed and utilized in complex cases, most patients were treated by general surgeons. "I come from a generation that could do chest and abdominal surgery and amputations," said Dr. Spence.
Staff doctors were on call every other night and worked very long hours, a situation no longer allowed in U.K. hospitals. Surgeons worked "until the work was done" to care for all the injured and to maintain continuity of care. "There could be 100 injured people in the ER. You couldn’t just walk out at half past five."
In conclusion, Dr. Spence noted that the extended crisis of violence and trauma resulted in a close-knit "band of brothers, and occasionally, sisters" who worked in trying circumstances as colleagues. Many of those colleagues have left surgery or have died relatively young, and Dr. Spence intended his lecture to be a tribute to their service, dedication, and sacrifice in troubled times.
WASHINGTON – The political violence that plagued Northern Ireland for nearly 40 years has subsided, and the memories of those dark days in Belfast have begun to fade. But for Roy A. J. Spence, OBE, J.D., M.D., LL.D., FRCS, those years of treating trauma patients in the emergency room of the Royal Victoria Hospital in that city served as an important opportunity for learning and service.
Dr. Spence worked with a team of surgeons and other staff to treat thousands of victims of bombings, shootings, torture, kneecapping, and assault that happened in the context of clashes between two sides of a sectarian conflict and the British Army. Dr. Spence, who delivered the I.S. Ravdin Lecture in the Basic and Surgical Sciences during the annual clinical congress of the American College of Surgeons, discussed his experiences and lessons learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
During the worst period of The Troubles, as the conflict is called, emergency room surgeons were treating what were essentially combat injuries in an urban hospital setting. The great majority of the injuries in Belfast occurred within 1 mile of the Royal Victoria Hospital and the Belfast City Hospital, "some at the door of the hospital, some within the hospital, and we even had one patient shot in a bed in the hospital," he said. One victim was killed in the presence of Dr. Spence in the ER.
Dr. Spence, now professor and head of the department of surgery, imaging, and perioperative medicine at Queen’s University of Belfast, stated that despite the at times overwhelming numbers of injured that flooded into the ER, 90% of patients were delivered to the ER within 30 minutes and 50% within 15 minutes. The staff developed systems to speed patients through the ER to treatment and surgery if needed. In 1972 alone, 20,000 individuals were injured in various ways, and most of these injuries occurred in Belfast.
In addition to a streamlined admission process, the surgeons developed their protocol based on lessons learned over the years.
"We had disaster plans, but, in truth, we almost never had a rehearsal. The rehearsals were for real. The rehearsals were occurring day by day."
It became clear in the early years of the conflict that, in most cases, patients were best served if the doctors stayed at the hospital to receive patients instead of rushing to the scene of a bombing or shooting. "We were almost a nuisance if we went to the scene, because there was often continuing gunfire, there were secondary explosions, and sometimes the bodies themselves were booby-trapped."
In addition, the system of handling large numbers of injured patients worked best if there was a senior surgeon and senior nurse at the door to triage patients. Those with minor injuries were taken to a separate room for treatment.
It was also important that one senior surgeon took charge of the situation and led the team. Surgeons discovered that in these crisis situations, x-raying patients could turn into a bottleneck in the treatment process, leading to dangerous delays, so at times surgery proceeded without imaging to save a patient’s life.
Dr. Spence said that the Royal Victoria distinguished itself in treating patients in the midst of a civil war by upholding the highest standards of care, documenting cases thoroughly, and treating all patients with the same level of care. Although the duty surgeons lived in the community, knew many of the victims, were aware of which group had carried out an attack, and even had family members killed in the conflict, Dr. Spence asserted that they maintained their professional standards and did not allow politics to deter them from their duties as physicians.
In the peak years of violence, the early 1970s to the early 1980s, two types of injuries – gunshot wounds to the head and kneecapping trauma – led to innovative treatment plans. The hospital established the standard of care for gunshot wounds to the head in that era, and also pioneered the use of vascular shunts to treat blast-injured limbs. The vascular shunt in particular was considered invaluable by Dr. Spence. This procedure reduced the number of amputations in cases of limb trauma from one-third to less than 10% and "allowed a very unhurried fracture reduction and external fixation."
Dr. Spence noted that general surgeons were valued in the ER because of their capacity to deal with a wide variety of injuries and because of the potentially fatal delays caused by waiting for a specialist. Although specialists were definitely needed and utilized in complex cases, most patients were treated by general surgeons. "I come from a generation that could do chest and abdominal surgery and amputations," said Dr. Spence.
Staff doctors were on call every other night and worked very long hours, a situation no longer allowed in U.K. hospitals. Surgeons worked "until the work was done" to care for all the injured and to maintain continuity of care. "There could be 100 injured people in the ER. You couldn’t just walk out at half past five."
In conclusion, Dr. Spence noted that the extended crisis of violence and trauma resulted in a close-knit "band of brothers, and occasionally, sisters" who worked in trying circumstances as colleagues. Many of those colleagues have left surgery or have died relatively young, and Dr. Spence intended his lecture to be a tribute to their service, dedication, and sacrifice in troubled times.
AT THE ACS CLINICAL CONGRESS
Reengineering of care: Surgical leadership
WASHINGTON – Years of research have taught us that when it comes to heath care delivery, there is no relationship between cost and quality, according to Dr. Glenn D. Steele, the president and CEO of Geisinger Health System. Dr. Steele delivered the 2013 Commission on Cancer Oncology Lecture at the annual clinical congress of the American College of Surgeons.
Geisinger Health System, based in Danville, Pa., is a renowned leader in transforming health care delivery through innovative multi-institution collaboration and an emphasis on consistent use of best practices and evidence-based medicine, he said. The goal over the past decade has been to reengineer complex medical care to improve quality and reduce costs. Dr. Steele asserted that these two goals are not mutually exclusive.
"We now believe that if you look at a patient cohort – whether it is hospital based or whether it’s ambulatory care – for folks with three, four, or five chronic diseases, you find that the population with the highest costs has also the least-quality health care ... more often than not, high cost equals a less-than-optimal outcome," he said.
At the heart of the reengineering concept is the recognition that many patients in conventional treatment situations end up with what Dr. Steele referred to as "unjustified variation" in the execution of the treatment. A noted study by Little et al. showed that only half of patients treated for lung cancer, for example, receive the recommended care (Ann. Thorac. Surg. 2005;80:2051-6). The Geisinger Health System tackled the problem of unwarranted variation in treatment and "road tested" a wide range of innovations involving standardization of treatment, electronic data gathering and tracking, and institutional culture change.
The ProvenCare model was developed to incorporate all the initiatives that had been researched and tested at Geisinger, and the model was first applied in 2005 to coronary artery bypass grafting (CABG). This application of ProvenCare showed that "an improvement model that embeds evidence-based medicine into the workflow, applies the principles of reliability science (standardization, error proofing, and failure mode redesign) to the care redesign process, employs effective data feedback strategies, and engages patients in their care results in the right care delivered 100% of the time with better patient outcomes" (CA: A Cancer Journal for Clinicians 2011;61:382-96). The model has since been applied to hip replacement surgery, percutaneous coronary intervention, and cataract surgery.
Dr. Steele gave an update on a recent ProvenCare project, a model for treatment of resectable non–small cell lung cancer. The project is a collaboration between Geisinger and the American College of Surgeons Commission on Cancer. The initial survey of lung cancer care revealed substantial room for improvement. The ProvenCare goals initially were to standardize care; build in redundancy to make sure all tasks are done; bundle related tasks; build teams, feedback protocols, and training models; move toward a multi-institutional collaboration; and achieve widespread change in institutional practices, protocol, and culture of care. The project involved an 18-month period of training and testing in the participating institutions.
Engagement of patients and a "very well-articulated set of expectations" were a critical part of the ProvenCare model. The challenge involved achieving 100% compliance across the many institutions
Geisinger has created an insurance company that has some role in controlling costs. Dr. Steele estimated that many resources spent in health care are wasted. "If we could figure out how to extract much of that 25%-30% of needless cost, we can redistribute it. ... Some of that redistribution would go to our bottom line and allow us to grow programs and make our balance sheet comfortable. ... Some of that value would go back to our insurance company and to the middle-size and small businesses that are buying our insurance premiums." This is where cost savings are reducing the cost of premiums and "giving some of that value back to consumers."
Dr. Steele said, "In most industries where you have reengineered whatever it is you are doing, you’ve got better outcomes on both the quality side and the cost side, and you are in heavy-duty competition in the consolidating market. What do you do? You lower your price. And you maintain your contribution margin. And you run your competition out of business. We don’t think that way in health care. But my bet is, in 5 years, we will think that way."
Ultimately, the drive to lower costs goes hand in hand with improving quality of care, he said. "If you believe that, and you are a professional driven to help your patients, you are much more enthusiastic about reengineering than simply working to keep costs down."
WASHINGTON – Years of research have taught us that when it comes to heath care delivery, there is no relationship between cost and quality, according to Dr. Glenn D. Steele, the president and CEO of Geisinger Health System. Dr. Steele delivered the 2013 Commission on Cancer Oncology Lecture at the annual clinical congress of the American College of Surgeons.
Geisinger Health System, based in Danville, Pa., is a renowned leader in transforming health care delivery through innovative multi-institution collaboration and an emphasis on consistent use of best practices and evidence-based medicine, he said. The goal over the past decade has been to reengineer complex medical care to improve quality and reduce costs. Dr. Steele asserted that these two goals are not mutually exclusive.
"We now believe that if you look at a patient cohort – whether it is hospital based or whether it’s ambulatory care – for folks with three, four, or five chronic diseases, you find that the population with the highest costs has also the least-quality health care ... more often than not, high cost equals a less-than-optimal outcome," he said.
At the heart of the reengineering concept is the recognition that many patients in conventional treatment situations end up with what Dr. Steele referred to as "unjustified variation" in the execution of the treatment. A noted study by Little et al. showed that only half of patients treated for lung cancer, for example, receive the recommended care (Ann. Thorac. Surg. 2005;80:2051-6). The Geisinger Health System tackled the problem of unwarranted variation in treatment and "road tested" a wide range of innovations involving standardization of treatment, electronic data gathering and tracking, and institutional culture change.
The ProvenCare model was developed to incorporate all the initiatives that had been researched and tested at Geisinger, and the model was first applied in 2005 to coronary artery bypass grafting (CABG). This application of ProvenCare showed that "an improvement model that embeds evidence-based medicine into the workflow, applies the principles of reliability science (standardization, error proofing, and failure mode redesign) to the care redesign process, employs effective data feedback strategies, and engages patients in their care results in the right care delivered 100% of the time with better patient outcomes" (CA: A Cancer Journal for Clinicians 2011;61:382-96). The model has since been applied to hip replacement surgery, percutaneous coronary intervention, and cataract surgery.
Dr. Steele gave an update on a recent ProvenCare project, a model for treatment of resectable non–small cell lung cancer. The project is a collaboration between Geisinger and the American College of Surgeons Commission on Cancer. The initial survey of lung cancer care revealed substantial room for improvement. The ProvenCare goals initially were to standardize care; build in redundancy to make sure all tasks are done; bundle related tasks; build teams, feedback protocols, and training models; move toward a multi-institutional collaboration; and achieve widespread change in institutional practices, protocol, and culture of care. The project involved an 18-month period of training and testing in the participating institutions.
Engagement of patients and a "very well-articulated set of expectations" were a critical part of the ProvenCare model. The challenge involved achieving 100% compliance across the many institutions
Geisinger has created an insurance company that has some role in controlling costs. Dr. Steele estimated that many resources spent in health care are wasted. "If we could figure out how to extract much of that 25%-30% of needless cost, we can redistribute it. ... Some of that redistribution would go to our bottom line and allow us to grow programs and make our balance sheet comfortable. ... Some of that value would go back to our insurance company and to the middle-size and small businesses that are buying our insurance premiums." This is where cost savings are reducing the cost of premiums and "giving some of that value back to consumers."
Dr. Steele said, "In most industries where you have reengineered whatever it is you are doing, you’ve got better outcomes on both the quality side and the cost side, and you are in heavy-duty competition in the consolidating market. What do you do? You lower your price. And you maintain your contribution margin. And you run your competition out of business. We don’t think that way in health care. But my bet is, in 5 years, we will think that way."
Ultimately, the drive to lower costs goes hand in hand with improving quality of care, he said. "If you believe that, and you are a professional driven to help your patients, you are much more enthusiastic about reengineering than simply working to keep costs down."
WASHINGTON – Years of research have taught us that when it comes to heath care delivery, there is no relationship between cost and quality, according to Dr. Glenn D. Steele, the president and CEO of Geisinger Health System. Dr. Steele delivered the 2013 Commission on Cancer Oncology Lecture at the annual clinical congress of the American College of Surgeons.
Geisinger Health System, based in Danville, Pa., is a renowned leader in transforming health care delivery through innovative multi-institution collaboration and an emphasis on consistent use of best practices and evidence-based medicine, he said. The goal over the past decade has been to reengineer complex medical care to improve quality and reduce costs. Dr. Steele asserted that these two goals are not mutually exclusive.
"We now believe that if you look at a patient cohort – whether it is hospital based or whether it’s ambulatory care – for folks with three, four, or five chronic diseases, you find that the population with the highest costs has also the least-quality health care ... more often than not, high cost equals a less-than-optimal outcome," he said.
At the heart of the reengineering concept is the recognition that many patients in conventional treatment situations end up with what Dr. Steele referred to as "unjustified variation" in the execution of the treatment. A noted study by Little et al. showed that only half of patients treated for lung cancer, for example, receive the recommended care (Ann. Thorac. Surg. 2005;80:2051-6). The Geisinger Health System tackled the problem of unwarranted variation in treatment and "road tested" a wide range of innovations involving standardization of treatment, electronic data gathering and tracking, and institutional culture change.
The ProvenCare model was developed to incorporate all the initiatives that had been researched and tested at Geisinger, and the model was first applied in 2005 to coronary artery bypass grafting (CABG). This application of ProvenCare showed that "an improvement model that embeds evidence-based medicine into the workflow, applies the principles of reliability science (standardization, error proofing, and failure mode redesign) to the care redesign process, employs effective data feedback strategies, and engages patients in their care results in the right care delivered 100% of the time with better patient outcomes" (CA: A Cancer Journal for Clinicians 2011;61:382-96). The model has since been applied to hip replacement surgery, percutaneous coronary intervention, and cataract surgery.
Dr. Steele gave an update on a recent ProvenCare project, a model for treatment of resectable non–small cell lung cancer. The project is a collaboration between Geisinger and the American College of Surgeons Commission on Cancer. The initial survey of lung cancer care revealed substantial room for improvement. The ProvenCare goals initially were to standardize care; build in redundancy to make sure all tasks are done; bundle related tasks; build teams, feedback protocols, and training models; move toward a multi-institutional collaboration; and achieve widespread change in institutional practices, protocol, and culture of care. The project involved an 18-month period of training and testing in the participating institutions.
Engagement of patients and a "very well-articulated set of expectations" were a critical part of the ProvenCare model. The challenge involved achieving 100% compliance across the many institutions
Geisinger has created an insurance company that has some role in controlling costs. Dr. Steele estimated that many resources spent in health care are wasted. "If we could figure out how to extract much of that 25%-30% of needless cost, we can redistribute it. ... Some of that redistribution would go to our bottom line and allow us to grow programs and make our balance sheet comfortable. ... Some of that value would go back to our insurance company and to the middle-size and small businesses that are buying our insurance premiums." This is where cost savings are reducing the cost of premiums and "giving some of that value back to consumers."
Dr. Steele said, "In most industries where you have reengineered whatever it is you are doing, you’ve got better outcomes on both the quality side and the cost side, and you are in heavy-duty competition in the consolidating market. What do you do? You lower your price. And you maintain your contribution margin. And you run your competition out of business. We don’t think that way in health care. But my bet is, in 5 years, we will think that way."
Ultimately, the drive to lower costs goes hand in hand with improving quality of care, he said. "If you believe that, and you are a professional driven to help your patients, you are much more enthusiastic about reengineering than simply working to keep costs down."
Surgery and technology: A complicated partnership
WASHINGTON – Technological innovation is transforming surgery at a rapid pace. The question, according to Dr. Mark Talamini, is how can surgeons prepare for and participate in that transformation.
Dr. Talamini delivered the Excelsior Surgical Society/Edward D. Churchill Lecture at the annual clinical congress of the American College of Surgeons. He discussed his own early interest in medical technology, the trends in technological change, and the complex issues that face surgeons in maintaining currency in training and working to develop new devices.
The most profound change in surgery in recent decades has been the insertion of high-tech devices between the surgeon and the patient. There is now most commonly a physical distance between the patient’s body and the surgeon’s hands, and "the majority of surgical procedures involve the surgeon looking at a screen." Surgical tasks of dissecting, controlling bleeding, and suturing in particular have been all but transformed by devices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The drive to introduce new surgical devices has come up against the stringent approval process of the Food and Drug Administration and has led to public criticism of that process. Dr. Talamini, who chairs the surgery department at the State University of New York at Stony Brook, and who has worked with the FDA for more than 10 years in various capacities, argued that there must be a correct balance between innovation and regulation. "We’ve got to have both. We cannot just have instruments released to the public without understanding what the issues are regarding safety and effectiveness. For the FDA, that is the mantra: safety and effectiveness." He added, "They have a tough task to figure out the balance between getting new things to the market to benefit patients and yet maintaining overall public safety."
Dr. Talamini asserted that the growing number and complexity of surgical instruments mean that surgeons may be falling behind in their skills without realizing it. He illustrated his point by posing specific questions about the use of some recently introduced instruments and polling the audience on correct use. In response to the many wrong answers, he asserted that "we don’t know as much as we think we do about surgical technology."
To address this problem of maintaining currency and training on innovative devices, Dr. Talamini mentioned the Fundamental Use of Surgical Energy (FUSE) program created by the Society of American Gastrointestinal and Endoscopic Surgeons. FUSE is a web-based educational and testing program for all operating room participants, including surgeons.
Dr. Talamini is particularly proud of the Center for the Future of Surgery located at the University of California, San Diego, which he was instrumental in developing. This center has a research suite for doctors and scientists to collaborate on innovative devices; training suites for the latest in surgical, robotic, laparoscopic, and microscopic techniques; and simulated operating rooms and emergency departments.
Dr. Talamini reflected on the complex relationship between innovative surgeons and device development and manufacturing companies. He cautioned the audience to consider some principles when engaging in technology development with industry. First, there would be no technological innovation without collaboration between the medical device industry and surgeons. But development and training cannot be simply a means of selling equipment. Education and sales must be clearly differentiated. In addition, disclosure and transparency are fundamental to maintaining public trust.
Finally, Dr. Talamini argued that conflict of interest in this area cannot be eliminated, but it must be managed to foster innovation.
Dr. Talamini had no disclosures.
WASHINGTON – Technological innovation is transforming surgery at a rapid pace. The question, according to Dr. Mark Talamini, is how can surgeons prepare for and participate in that transformation.
Dr. Talamini delivered the Excelsior Surgical Society/Edward D. Churchill Lecture at the annual clinical congress of the American College of Surgeons. He discussed his own early interest in medical technology, the trends in technological change, and the complex issues that face surgeons in maintaining currency in training and working to develop new devices.
The most profound change in surgery in recent decades has been the insertion of high-tech devices between the surgeon and the patient. There is now most commonly a physical distance between the patient’s body and the surgeon’s hands, and "the majority of surgical procedures involve the surgeon looking at a screen." Surgical tasks of dissecting, controlling bleeding, and suturing in particular have been all but transformed by devices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The drive to introduce new surgical devices has come up against the stringent approval process of the Food and Drug Administration and has led to public criticism of that process. Dr. Talamini, who chairs the surgery department at the State University of New York at Stony Brook, and who has worked with the FDA for more than 10 years in various capacities, argued that there must be a correct balance between innovation and regulation. "We’ve got to have both. We cannot just have instruments released to the public without understanding what the issues are regarding safety and effectiveness. For the FDA, that is the mantra: safety and effectiveness." He added, "They have a tough task to figure out the balance between getting new things to the market to benefit patients and yet maintaining overall public safety."
Dr. Talamini asserted that the growing number and complexity of surgical instruments mean that surgeons may be falling behind in their skills without realizing it. He illustrated his point by posing specific questions about the use of some recently introduced instruments and polling the audience on correct use. In response to the many wrong answers, he asserted that "we don’t know as much as we think we do about surgical technology."
To address this problem of maintaining currency and training on innovative devices, Dr. Talamini mentioned the Fundamental Use of Surgical Energy (FUSE) program created by the Society of American Gastrointestinal and Endoscopic Surgeons. FUSE is a web-based educational and testing program for all operating room participants, including surgeons.
Dr. Talamini is particularly proud of the Center for the Future of Surgery located at the University of California, San Diego, which he was instrumental in developing. This center has a research suite for doctors and scientists to collaborate on innovative devices; training suites for the latest in surgical, robotic, laparoscopic, and microscopic techniques; and simulated operating rooms and emergency departments.
Dr. Talamini reflected on the complex relationship between innovative surgeons and device development and manufacturing companies. He cautioned the audience to consider some principles when engaging in technology development with industry. First, there would be no technological innovation without collaboration between the medical device industry and surgeons. But development and training cannot be simply a means of selling equipment. Education and sales must be clearly differentiated. In addition, disclosure and transparency are fundamental to maintaining public trust.
Finally, Dr. Talamini argued that conflict of interest in this area cannot be eliminated, but it must be managed to foster innovation.
Dr. Talamini had no disclosures.
WASHINGTON – Technological innovation is transforming surgery at a rapid pace. The question, according to Dr. Mark Talamini, is how can surgeons prepare for and participate in that transformation.
Dr. Talamini delivered the Excelsior Surgical Society/Edward D. Churchill Lecture at the annual clinical congress of the American College of Surgeons. He discussed his own early interest in medical technology, the trends in technological change, and the complex issues that face surgeons in maintaining currency in training and working to develop new devices.
The most profound change in surgery in recent decades has been the insertion of high-tech devices between the surgeon and the patient. There is now most commonly a physical distance between the patient’s body and the surgeon’s hands, and "the majority of surgical procedures involve the surgeon looking at a screen." Surgical tasks of dissecting, controlling bleeding, and suturing in particular have been all but transformed by devices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The drive to introduce new surgical devices has come up against the stringent approval process of the Food and Drug Administration and has led to public criticism of that process. Dr. Talamini, who chairs the surgery department at the State University of New York at Stony Brook, and who has worked with the FDA for more than 10 years in various capacities, argued that there must be a correct balance between innovation and regulation. "We’ve got to have both. We cannot just have instruments released to the public without understanding what the issues are regarding safety and effectiveness. For the FDA, that is the mantra: safety and effectiveness." He added, "They have a tough task to figure out the balance between getting new things to the market to benefit patients and yet maintaining overall public safety."
Dr. Talamini asserted that the growing number and complexity of surgical instruments mean that surgeons may be falling behind in their skills without realizing it. He illustrated his point by posing specific questions about the use of some recently introduced instruments and polling the audience on correct use. In response to the many wrong answers, he asserted that "we don’t know as much as we think we do about surgical technology."
To address this problem of maintaining currency and training on innovative devices, Dr. Talamini mentioned the Fundamental Use of Surgical Energy (FUSE) program created by the Society of American Gastrointestinal and Endoscopic Surgeons. FUSE is a web-based educational and testing program for all operating room participants, including surgeons.
Dr. Talamini is particularly proud of the Center for the Future of Surgery located at the University of California, San Diego, which he was instrumental in developing. This center has a research suite for doctors and scientists to collaborate on innovative devices; training suites for the latest in surgical, robotic, laparoscopic, and microscopic techniques; and simulated operating rooms and emergency departments.
Dr. Talamini reflected on the complex relationship between innovative surgeons and device development and manufacturing companies. He cautioned the audience to consider some principles when engaging in technology development with industry. First, there would be no technological innovation without collaboration between the medical device industry and surgeons. But development and training cannot be simply a means of selling equipment. Education and sales must be clearly differentiated. In addition, disclosure and transparency are fundamental to maintaining public trust.
Finally, Dr. Talamini argued that conflict of interest in this area cannot be eliminated, but it must be managed to foster innovation.
Dr. Talamini had no disclosures.
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
MULTIMEDIA: Vemurafenib -- Melanoma Drug Cuts Death Risk
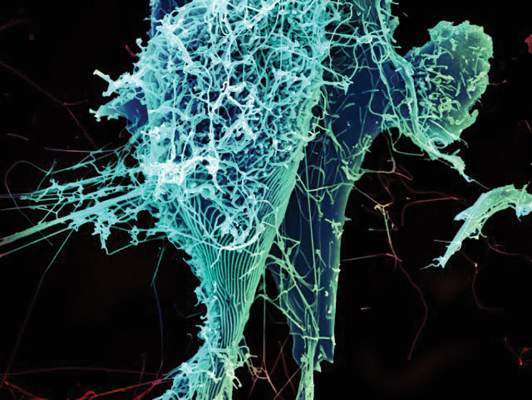
This drug works by attacking a specific genetic mutation, BRAF V600E, that accelerates tumor growth.
This drug works by attacking a specific genetic mutation, BRAF V600E, that accelerates tumor growth.
This drug works by attacking a specific genetic mutation, BRAF V600E, that accelerates tumor growth.
Rhinoplasty Seekers Should Be Screened for Mental Disorder
More than a third of patients seeking cosmetic nose surgery have symptoms of body dysmorphic disorder, according to a preoperative study of 226 patients at a Belgian university hospital.
"This study shows that the prevalence of body dysmorphic disorder symptoms in a cosmetic rhinoplasty population is high and that the severity of symptoms has a clearly negative effect on daily functioning," wrote Dr. Valerie A. Picavet of University Hospitals Leuven (Belgium), and her associates.
The link between body dysmorphic disorder (BDD) and cosmetic surgery seekers is well documented (Body Image 2004;1:99-111; Br. J. Plast. Surg. 2003;56:546-51), but Dr. Picavet and her team focused on its prevalence among rhinoplasty seekers.
In collaboration with the psychiatric department of University Hospitals, the team conducted preoperative interviews with patients at a referral center for nasal disease. These patients were over age 16 years and seeking rhinoplasty for aesthetic and/or functional reasons. The same interviews were conducted in a 65-person control group not seeking rhinoplasty (Plast. Reconstr. Surg. 2011;128:509-17).
The researchers used the DSM-IV definition of BDD by which individuals have a preoccupation with an imagined or slight physical defect.
Individuals with this disorder devote a significant amount of time each day focused on their perceived defect, have daily distress about this concern, and suffer social impairment as a result of their preoccupation.
For this study, patients were given questionnaires to establish a clinical profile and evidence of BDD symptoms. They were asked to evaluate their nasal shape on a visual analog scale. In addition, they were given the Yale-Brown Obsessive Compulsive scale modified for BDD to rate BDD-related thoughts and behaviors. Social impairment was assessed with the Sheehan Disability Scale and the Derriford Appearance Scale.
The researchers accounted for the possibility that not every nasal shape defect is imaginary by developing a scoring system in which patients' noses were evaluated by two independent observers.
Each patient's nose was rated on a scale from severely deformed to zero deformity. But patients' evaluations of their own noses did not match these evaluations by the observers. No correlation was found between subjective and objective assessments of nasal deformity.
In all, 74 patients (33%) had at least moderate symptoms of BDD. These individuals scored 16 or higher on the Yale-Brown scale. There were no patients with the most extreme BDD symptoms. Among the control group, only one patient (2%) had moderate or higher BDD symptoms.
The reason patients gave for seeking rhinoplasty had a bearing on their likelihood of their having BDD symptoms. Among those seeking surgery for functional reasons, only 9 (12%) had moderate or higher symptoms of BDD. Among those seeking rhinoplasty for aesthetic reasons, 65 (43%) had moderate or higher symptoms of BDD. The correlation between Yale-Brown score and reason for seeking surgery was statistically significant (P < .001).
The correlation between having a previous rhinoplasty and BDD symptom severity also was statistically significant (P = .003). For surgeons screening rhinoplasty patients, a primarily aesthetic motivation or a history of previous rhinoplasty may be a red flag indicating that the patient should be carefully assessed for symptoms of BDD.
The study also found a statistically significant relationship between number of BDD symptoms and degree of social impairment and distress in these rhinoplasty-seeking patients. There was also a positive correlation between patients' Yale-Brown score, and psychiatric history and comorbidities.
The researchers conclude, "Thorough preoperative evaluation, including informing about psychiatric history, especially depression, should therefore be included in the preoperative assessment of cosmetic surgery patients, as it might be an indicator for latent body dysmorphic disorder."
Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
In a commentary accompanying this study, David B. Sarwer, Ph.D., wrote that few individuals are completely content with their own body image, and a degree of body dissatisfaction is often the motivating force behind weight loss, physical activity, and cosmetic surgery. His own research indicates that body image dissatisfaction falls on a continuum.
Dr. Sarwer wrote that while the work of Dr. Picavet and colleagues advances the literature on the extreme end of the continuum – BDD – "of equal importance will be the article that reports on the psychological outcomes of rhinoplasty patients with BDD symptoms. Studies in the literature to date suggest that the great majority of persons with the disorder who undergo appearance-enhancing procedures report either no change or worsening of their disorder symptoms after these treatments." More conclusive evidence of these outcomes would lend support to recommendations that "BDD be considered a psychiatric contraindication to cosmetic surgery."
Dr. Sarwer is a clinical psychologist at the University of Pennsylvania Center for Human Appearance in Philadelphia. He reported that he has grant support from the National Institutes of Health, several medical societies, and Ethicon Endo-Surgery. He also has consulting relationships with Allergan, Enteromedics, and Ethicon Endo-Surgery (Plast. Reconstr. Surg. 2011;128:518-9).
In a commentary accompanying this study, David B. Sarwer, Ph.D., wrote that few individuals are completely content with their own body image, and a degree of body dissatisfaction is often the motivating force behind weight loss, physical activity, and cosmetic surgery. His own research indicates that body image dissatisfaction falls on a continuum.
Dr. Sarwer wrote that while the work of Dr. Picavet and colleagues advances the literature on the extreme end of the continuum – BDD – "of equal importance will be the article that reports on the psychological outcomes of rhinoplasty patients with BDD symptoms. Studies in the literature to date suggest that the great majority of persons with the disorder who undergo appearance-enhancing procedures report either no change or worsening of their disorder symptoms after these treatments." More conclusive evidence of these outcomes would lend support to recommendations that "BDD be considered a psychiatric contraindication to cosmetic surgery."
Dr. Sarwer is a clinical psychologist at the University of Pennsylvania Center for Human Appearance in Philadelphia. He reported that he has grant support from the National Institutes of Health, several medical societies, and Ethicon Endo-Surgery. He also has consulting relationships with Allergan, Enteromedics, and Ethicon Endo-Surgery (Plast. Reconstr. Surg. 2011;128:518-9).
In a commentary accompanying this study, David B. Sarwer, Ph.D., wrote that few individuals are completely content with their own body image, and a degree of body dissatisfaction is often the motivating force behind weight loss, physical activity, and cosmetic surgery. His own research indicates that body image dissatisfaction falls on a continuum.
Dr. Sarwer wrote that while the work of Dr. Picavet and colleagues advances the literature on the extreme end of the continuum – BDD – "of equal importance will be the article that reports on the psychological outcomes of rhinoplasty patients with BDD symptoms. Studies in the literature to date suggest that the great majority of persons with the disorder who undergo appearance-enhancing procedures report either no change or worsening of their disorder symptoms after these treatments." More conclusive evidence of these outcomes would lend support to recommendations that "BDD be considered a psychiatric contraindication to cosmetic surgery."
Dr. Sarwer is a clinical psychologist at the University of Pennsylvania Center for Human Appearance in Philadelphia. He reported that he has grant support from the National Institutes of Health, several medical societies, and Ethicon Endo-Surgery. He also has consulting relationships with Allergan, Enteromedics, and Ethicon Endo-Surgery (Plast. Reconstr. Surg. 2011;128:518-9).
More than a third of patients seeking cosmetic nose surgery have symptoms of body dysmorphic disorder, according to a preoperative study of 226 patients at a Belgian university hospital.
"This study shows that the prevalence of body dysmorphic disorder symptoms in a cosmetic rhinoplasty population is high and that the severity of symptoms has a clearly negative effect on daily functioning," wrote Dr. Valerie A. Picavet of University Hospitals Leuven (Belgium), and her associates.
The link between body dysmorphic disorder (BDD) and cosmetic surgery seekers is well documented (Body Image 2004;1:99-111; Br. J. Plast. Surg. 2003;56:546-51), but Dr. Picavet and her team focused on its prevalence among rhinoplasty seekers.
In collaboration with the psychiatric department of University Hospitals, the team conducted preoperative interviews with patients at a referral center for nasal disease. These patients were over age 16 years and seeking rhinoplasty for aesthetic and/or functional reasons. The same interviews were conducted in a 65-person control group not seeking rhinoplasty (Plast. Reconstr. Surg. 2011;128:509-17).
The researchers used the DSM-IV definition of BDD by which individuals have a preoccupation with an imagined or slight physical defect.
Individuals with this disorder devote a significant amount of time each day focused on their perceived defect, have daily distress about this concern, and suffer social impairment as a result of their preoccupation.
For this study, patients were given questionnaires to establish a clinical profile and evidence of BDD symptoms. They were asked to evaluate their nasal shape on a visual analog scale. In addition, they were given the Yale-Brown Obsessive Compulsive scale modified for BDD to rate BDD-related thoughts and behaviors. Social impairment was assessed with the Sheehan Disability Scale and the Derriford Appearance Scale.
The researchers accounted for the possibility that not every nasal shape defect is imaginary by developing a scoring system in which patients' noses were evaluated by two independent observers.
Each patient's nose was rated on a scale from severely deformed to zero deformity. But patients' evaluations of their own noses did not match these evaluations by the observers. No correlation was found between subjective and objective assessments of nasal deformity.
In all, 74 patients (33%) had at least moderate symptoms of BDD. These individuals scored 16 or higher on the Yale-Brown scale. There were no patients with the most extreme BDD symptoms. Among the control group, only one patient (2%) had moderate or higher BDD symptoms.
The reason patients gave for seeking rhinoplasty had a bearing on their likelihood of their having BDD symptoms. Among those seeking surgery for functional reasons, only 9 (12%) had moderate or higher symptoms of BDD. Among those seeking rhinoplasty for aesthetic reasons, 65 (43%) had moderate or higher symptoms of BDD. The correlation between Yale-Brown score and reason for seeking surgery was statistically significant (P < .001).
The correlation between having a previous rhinoplasty and BDD symptom severity also was statistically significant (P = .003). For surgeons screening rhinoplasty patients, a primarily aesthetic motivation or a history of previous rhinoplasty may be a red flag indicating that the patient should be carefully assessed for symptoms of BDD.
The study also found a statistically significant relationship between number of BDD symptoms and degree of social impairment and distress in these rhinoplasty-seeking patients. There was also a positive correlation between patients' Yale-Brown score, and psychiatric history and comorbidities.
The researchers conclude, "Thorough preoperative evaluation, including informing about psychiatric history, especially depression, should therefore be included in the preoperative assessment of cosmetic surgery patients, as it might be an indicator for latent body dysmorphic disorder."
Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
More than a third of patients seeking cosmetic nose surgery have symptoms of body dysmorphic disorder, according to a preoperative study of 226 patients at a Belgian university hospital.
"This study shows that the prevalence of body dysmorphic disorder symptoms in a cosmetic rhinoplasty population is high and that the severity of symptoms has a clearly negative effect on daily functioning," wrote Dr. Valerie A. Picavet of University Hospitals Leuven (Belgium), and her associates.
The link between body dysmorphic disorder (BDD) and cosmetic surgery seekers is well documented (Body Image 2004;1:99-111; Br. J. Plast. Surg. 2003;56:546-51), but Dr. Picavet and her team focused on its prevalence among rhinoplasty seekers.
In collaboration with the psychiatric department of University Hospitals, the team conducted preoperative interviews with patients at a referral center for nasal disease. These patients were over age 16 years and seeking rhinoplasty for aesthetic and/or functional reasons. The same interviews were conducted in a 65-person control group not seeking rhinoplasty (Plast. Reconstr. Surg. 2011;128:509-17).
The researchers used the DSM-IV definition of BDD by which individuals have a preoccupation with an imagined or slight physical defect.
Individuals with this disorder devote a significant amount of time each day focused on their perceived defect, have daily distress about this concern, and suffer social impairment as a result of their preoccupation.
For this study, patients were given questionnaires to establish a clinical profile and evidence of BDD symptoms. They were asked to evaluate their nasal shape on a visual analog scale. In addition, they were given the Yale-Brown Obsessive Compulsive scale modified for BDD to rate BDD-related thoughts and behaviors. Social impairment was assessed with the Sheehan Disability Scale and the Derriford Appearance Scale.
The researchers accounted for the possibility that not every nasal shape defect is imaginary by developing a scoring system in which patients' noses were evaluated by two independent observers.
Each patient's nose was rated on a scale from severely deformed to zero deformity. But patients' evaluations of their own noses did not match these evaluations by the observers. No correlation was found between subjective and objective assessments of nasal deformity.
In all, 74 patients (33%) had at least moderate symptoms of BDD. These individuals scored 16 or higher on the Yale-Brown scale. There were no patients with the most extreme BDD symptoms. Among the control group, only one patient (2%) had moderate or higher BDD symptoms.
The reason patients gave for seeking rhinoplasty had a bearing on their likelihood of their having BDD symptoms. Among those seeking surgery for functional reasons, only 9 (12%) had moderate or higher symptoms of BDD. Among those seeking rhinoplasty for aesthetic reasons, 65 (43%) had moderate or higher symptoms of BDD. The correlation between Yale-Brown score and reason for seeking surgery was statistically significant (P < .001).
The correlation between having a previous rhinoplasty and BDD symptom severity also was statistically significant (P = .003). For surgeons screening rhinoplasty patients, a primarily aesthetic motivation or a history of previous rhinoplasty may be a red flag indicating that the patient should be carefully assessed for symptoms of BDD.
The study also found a statistically significant relationship between number of BDD symptoms and degree of social impairment and distress in these rhinoplasty-seeking patients. There was also a positive correlation between patients' Yale-Brown score, and psychiatric history and comorbidities.
The researchers conclude, "Thorough preoperative evaluation, including informing about psychiatric history, especially depression, should therefore be included in the preoperative assessment of cosmetic surgery patients, as it might be an indicator for latent body dysmorphic disorder."
Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
FROM PLASTIC AND RECONSTRUCTIVE SURGERY
Rhinoplasty Seekers Should Be Screened for Mental Disorder
More than a third of patients seeking cosmetic nose surgery have symptoms of body dysmorphic disorder, according to a preoperative study of 226 patients at a Belgian university hospital.
"This study shows that the prevalence of body dysmorphic disorder symptoms in a cosmetic rhinoplasty population is high and that the severity of symptoms has a clearly negative effect on daily functioning," wrote Dr. Valerie A. Picavet of University Hospitals Leuven (Belgium), and her associates.
The link between body dysmorphic disorder (BDD) and cosmetic surgery seekers is well documented (Body Image 2004;1:99-111; Br. J. Plast. Surg. 2003;56:546-51), but Dr. Picavet and her team focused on its prevalence among rhinoplasty seekers. In collaboration with the psychiatric department of University Hospitals, the team conducted preoperative interviews with patients at a referral center for nasal disease. These patients were over age 16 years and seeking rhinoplasty for aesthetic and/or functional reasons. The same interviews were conducted in a 65-person control group not seeking rhinoplasty (Plast. Reconstr. Surg. 2011;128:509-17).
The researchers used the DSM-IV definition of BDD by which individuals have a preoccupation with an imagined or slight physical defect. Individuals with this disorder devote a significant amount of time each day focused on their perceived defect, have daily distress about this concern, and suffer social impairment as a result of their preoccupation.
For this study, patients were given questionnaires to establish a clinical profile and evidence of BDD symptoms. They were asked to evaluate their nasal shape on a visual analog scale. In addition, they were given the Yale-Brown Obsessive Compulsive scale modified for BDD to rate BDD-related thoughts and behaviors. Social impairment was assessed with the Sheehan Disability Scale and the Derriford Appearance Scale.
The researchers accounted for the possibility that not every nasal shape defect is imaginary by developing a scoring system in which patients’ noses were evaluated by two independent observers. Each patient’s nose was rated on a scale from severely deformed to zero deformity. But patients’ evaluations of their own noses did not match these evaluations by the observers. No correlation was found between subjective and objective assessments of nasal deformity.
In all, 74 patients (33%) had at least moderate symptoms of BDD. These individuals scored 16 or higher on the Yale-Brown scale. There were no patients with the most extreme BDD symptoms. Among the control group, only one patient (2%) had moderate or higher BDD symptoms.
The reason patients gave for seeking rhinoplasty had a bearing on their likelihood of their having BDD symptoms. Among those seeking surgery for functional reasons, only 9 (12%) had moderate or higher symptoms of BDD. Among those seeking rhinoplasty for aesthetic reasons, 65 (43%) had moderate or higher symptoms of BDD. The correlation between Yale-Brown score and reason for seeking surgery was statistically significant (P < .001).
The correlation between having a previous rhinoplasty and BDD symptom severity also was statistically significant (P = .003). For surgeons screening rhinoplasty patients, a primarily aesthetic motivation or a history of previous rhinoplasty may be a red flag indicating that the patient should be carefully assessed for symptoms of BDD.
The study also found a statistically significant relationship between number of BDD symptoms and degree of social impairment and distress in these rhinoplasty-seeking patients. There was also a positive correlation between patients’ Yale-Brown score, and psychiatric history and comorbidities.
The researchers conclude, "Thorough preoperative evaluation, including informing about psychiatric history, especially depression, should therefore be included in the preoperative assessment of cosmetic surgery patients, as it might be an indicator for latent body dysmorphic disorder."
Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
In a commentary accompanying this study, David B. Sarwer, Ph.D., wrote that few individuals are completely content with their own body image, and a degree of body dissatisfaction is often the motivating force behind weight loss, physical activity, and cosmetic surgery. His own research indicates that body image dissatisfaction falls on a continuum.
Dr. Sarwer wrote that while the work of Dr. Picavet and colleagues advances the literature on the extreme end of the continuum – BDD – "of equal importance will be the article that reports on the psychological outcomes of rhinoplasty patients with BDD symptoms. Studies in the literature to date suggest that the great majority of persons with the disorder who undergo appearance-enhancing procedures report either no change or worsening of their disorder symptoms after these treatments." More conclusive evidence of these outcomes would lend support to recommendations that "BDD be considered a psychiatric contraindication to cosmetic surgery."
Dr. Sarwer is a clinical psychologist at the University of Pennsylvania Center for Human Appearance in Philadelphia. He reported that he has grant support from the National Institutes of Health, several medical societies, and Ethicon Endo-Surgery. He also has consulting relationships with Allergan, Enteromedics, and Ethicon Endo-Surgery (Plast. Reconstr. Surg. 2011;128:518-9).
In a commentary accompanying this study, David B. Sarwer, Ph.D., wrote that few individuals are completely content with their own body image, and a degree of body dissatisfaction is often the motivating force behind weight loss, physical activity, and cosmetic surgery. His own research indicates that body image dissatisfaction falls on a continuum.
Dr. Sarwer wrote that while the work of Dr. Picavet and colleagues advances the literature on the extreme end of the continuum – BDD – "of equal importance will be the article that reports on the psychological outcomes of rhinoplasty patients with BDD symptoms. Studies in the literature to date suggest that the great majority of persons with the disorder who undergo appearance-enhancing procedures report either no change or worsening of their disorder symptoms after these treatments." More conclusive evidence of these outcomes would lend support to recommendations that "BDD be considered a psychiatric contraindication to cosmetic surgery."
Dr. Sarwer is a clinical psychologist at the University of Pennsylvania Center for Human Appearance in Philadelphia. He reported that he has grant support from the National Institutes of Health, several medical societies, and Ethicon Endo-Surgery. He also has consulting relationships with Allergan, Enteromedics, and Ethicon Endo-Surgery (Plast. Reconstr. Surg. 2011;128:518-9).
In a commentary accompanying this study, David B. Sarwer, Ph.D., wrote that few individuals are completely content with their own body image, and a degree of body dissatisfaction is often the motivating force behind weight loss, physical activity, and cosmetic surgery. His own research indicates that body image dissatisfaction falls on a continuum.
Dr. Sarwer wrote that while the work of Dr. Picavet and colleagues advances the literature on the extreme end of the continuum – BDD – "of equal importance will be the article that reports on the psychological outcomes of rhinoplasty patients with BDD symptoms. Studies in the literature to date suggest that the great majority of persons with the disorder who undergo appearance-enhancing procedures report either no change or worsening of their disorder symptoms after these treatments." More conclusive evidence of these outcomes would lend support to recommendations that "BDD be considered a psychiatric contraindication to cosmetic surgery."
Dr. Sarwer is a clinical psychologist at the University of Pennsylvania Center for Human Appearance in Philadelphia. He reported that he has grant support from the National Institutes of Health, several medical societies, and Ethicon Endo-Surgery. He also has consulting relationships with Allergan, Enteromedics, and Ethicon Endo-Surgery (Plast. Reconstr. Surg. 2011;128:518-9).
More than a third of patients seeking cosmetic nose surgery have symptoms of body dysmorphic disorder, according to a preoperative study of 226 patients at a Belgian university hospital.
"This study shows that the prevalence of body dysmorphic disorder symptoms in a cosmetic rhinoplasty population is high and that the severity of symptoms has a clearly negative effect on daily functioning," wrote Dr. Valerie A. Picavet of University Hospitals Leuven (Belgium), and her associates.
The link between body dysmorphic disorder (BDD) and cosmetic surgery seekers is well documented (Body Image 2004;1:99-111; Br. J. Plast. Surg. 2003;56:546-51), but Dr. Picavet and her team focused on its prevalence among rhinoplasty seekers. In collaboration with the psychiatric department of University Hospitals, the team conducted preoperative interviews with patients at a referral center for nasal disease. These patients were over age 16 years and seeking rhinoplasty for aesthetic and/or functional reasons. The same interviews were conducted in a 65-person control group not seeking rhinoplasty (Plast. Reconstr. Surg. 2011;128:509-17).
The researchers used the DSM-IV definition of BDD by which individuals have a preoccupation with an imagined or slight physical defect. Individuals with this disorder devote a significant amount of time each day focused on their perceived defect, have daily distress about this concern, and suffer social impairment as a result of their preoccupation.
For this study, patients were given questionnaires to establish a clinical profile and evidence of BDD symptoms. They were asked to evaluate their nasal shape on a visual analog scale. In addition, they were given the Yale-Brown Obsessive Compulsive scale modified for BDD to rate BDD-related thoughts and behaviors. Social impairment was assessed with the Sheehan Disability Scale and the Derriford Appearance Scale.
The researchers accounted for the possibility that not every nasal shape defect is imaginary by developing a scoring system in which patients’ noses were evaluated by two independent observers. Each patient’s nose was rated on a scale from severely deformed to zero deformity. But patients’ evaluations of their own noses did not match these evaluations by the observers. No correlation was found between subjective and objective assessments of nasal deformity.
In all, 74 patients (33%) had at least moderate symptoms of BDD. These individuals scored 16 or higher on the Yale-Brown scale. There were no patients with the most extreme BDD symptoms. Among the control group, only one patient (2%) had moderate or higher BDD symptoms.
The reason patients gave for seeking rhinoplasty had a bearing on their likelihood of their having BDD symptoms. Among those seeking surgery for functional reasons, only 9 (12%) had moderate or higher symptoms of BDD. Among those seeking rhinoplasty for aesthetic reasons, 65 (43%) had moderate or higher symptoms of BDD. The correlation between Yale-Brown score and reason for seeking surgery was statistically significant (P < .001).
The correlation between having a previous rhinoplasty and BDD symptom severity also was statistically significant (P = .003). For surgeons screening rhinoplasty patients, a primarily aesthetic motivation or a history of previous rhinoplasty may be a red flag indicating that the patient should be carefully assessed for symptoms of BDD.
The study also found a statistically significant relationship between number of BDD symptoms and degree of social impairment and distress in these rhinoplasty-seeking patients. There was also a positive correlation between patients’ Yale-Brown score, and psychiatric history and comorbidities.
The researchers conclude, "Thorough preoperative evaluation, including informing about psychiatric history, especially depression, should therefore be included in the preoperative assessment of cosmetic surgery patients, as it might be an indicator for latent body dysmorphic disorder."
Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
More than a third of patients seeking cosmetic nose surgery have symptoms of body dysmorphic disorder, according to a preoperative study of 226 patients at a Belgian university hospital.
"This study shows that the prevalence of body dysmorphic disorder symptoms in a cosmetic rhinoplasty population is high and that the severity of symptoms has a clearly negative effect on daily functioning," wrote Dr. Valerie A. Picavet of University Hospitals Leuven (Belgium), and her associates.
The link between body dysmorphic disorder (BDD) and cosmetic surgery seekers is well documented (Body Image 2004;1:99-111; Br. J. Plast. Surg. 2003;56:546-51), but Dr. Picavet and her team focused on its prevalence among rhinoplasty seekers. In collaboration with the psychiatric department of University Hospitals, the team conducted preoperative interviews with patients at a referral center for nasal disease. These patients were over age 16 years and seeking rhinoplasty for aesthetic and/or functional reasons. The same interviews were conducted in a 65-person control group not seeking rhinoplasty (Plast. Reconstr. Surg. 2011;128:509-17).
The researchers used the DSM-IV definition of BDD by which individuals have a preoccupation with an imagined or slight physical defect. Individuals with this disorder devote a significant amount of time each day focused on their perceived defect, have daily distress about this concern, and suffer social impairment as a result of their preoccupation.
For this study, patients were given questionnaires to establish a clinical profile and evidence of BDD symptoms. They were asked to evaluate their nasal shape on a visual analog scale. In addition, they were given the Yale-Brown Obsessive Compulsive scale modified for BDD to rate BDD-related thoughts and behaviors. Social impairment was assessed with the Sheehan Disability Scale and the Derriford Appearance Scale.
The researchers accounted for the possibility that not every nasal shape defect is imaginary by developing a scoring system in which patients’ noses were evaluated by two independent observers. Each patient’s nose was rated on a scale from severely deformed to zero deformity. But patients’ evaluations of their own noses did not match these evaluations by the observers. No correlation was found between subjective and objective assessments of nasal deformity.
In all, 74 patients (33%) had at least moderate symptoms of BDD. These individuals scored 16 or higher on the Yale-Brown scale. There were no patients with the most extreme BDD symptoms. Among the control group, only one patient (2%) had moderate or higher BDD symptoms.
The reason patients gave for seeking rhinoplasty had a bearing on their likelihood of their having BDD symptoms. Among those seeking surgery for functional reasons, only 9 (12%) had moderate or higher symptoms of BDD. Among those seeking rhinoplasty for aesthetic reasons, 65 (43%) had moderate or higher symptoms of BDD. The correlation between Yale-Brown score and reason for seeking surgery was statistically significant (P < .001).
The correlation between having a previous rhinoplasty and BDD symptom severity also was statistically significant (P = .003). For surgeons screening rhinoplasty patients, a primarily aesthetic motivation or a history of previous rhinoplasty may be a red flag indicating that the patient should be carefully assessed for symptoms of BDD.
The study also found a statistically significant relationship between number of BDD symptoms and degree of social impairment and distress in these rhinoplasty-seeking patients. There was also a positive correlation between patients’ Yale-Brown score, and psychiatric history and comorbidities.
The researchers conclude, "Thorough preoperative evaluation, including informing about psychiatric history, especially depression, should therefore be included in the preoperative assessment of cosmetic surgery patients, as it might be an indicator for latent body dysmorphic disorder."
Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
FROM PLASTIC AND RECONSTRUCTIVE SURGERY
Major findings: A total of 74 prospective rhinoplasty patients (33%) had at least moderate symptoms of body dismorphic disorder.
Data source: A preoperative study of 226 patients at a Belgian university hospital who were seeking rhinoplasty.
Disclosures: Dr. Picavet and her team reported no financial interest in relation to this study and no outside funding was received.
FDA Releases New Sunscreen Label Regulations
The Food and Drug Administration has issued new rules on sunscreen labeling to help consumers select products that prevent sunburn and reduce the risk of skin cancer and early skin aging.
The new labeling will differentiate sunscreen products according to their protective properties. Those products that meet FDA requirements of protection from ultraviolet A (UVA) and ultraviolet B (UVB) will be labeled "Broad Spectrum."
UVA and UVB radiation are known to contribute to sunburn, skin cancer, and premature skin aging. Under the new rules, only products that qualify as broad spectrum and have SPF values of 15 (or higher) can include labeling that the product helps prevent skin cancer and reduces the risk of early skin aging. Other products with SPF values between 2 and 14 may be labeled broad spectrum if they meet FDA tests for UVA and UVB protection, but will be required to have a warning stating that the product has not been shown to prevent skin cancer or early skin aging.
"FDA has evaluated the data and developed testing and labeling requirements for sunscreen products, so that manufacturers can modernize their product information and consumers can be well-informed on which products offer the greatest benefit," said Dr. Janet Woodcock, director of the FDA's Center for Drug Evaluation and Research. "These changes to sunscreen labels are an important part of helping consumers have the information they need so they can choose the right sun protection for themselves and their families."
The new regulations will go into effective in 1 year for most manufacturers. Other sunscreen makers with annual sales of less than $25,000 will have 2 years to comply with the new rules.
For physician perspectives on the announcement, see the story and related video interview "FDA's Sunscreen Regs Should Ease Skin Protection."
The Food and Drug Administration has issued new rules on sunscreen labeling to help consumers select products that prevent sunburn and reduce the risk of skin cancer and early skin aging.
The new labeling will differentiate sunscreen products according to their protective properties. Those products that meet FDA requirements of protection from ultraviolet A (UVA) and ultraviolet B (UVB) will be labeled "Broad Spectrum."
UVA and UVB radiation are known to contribute to sunburn, skin cancer, and premature skin aging. Under the new rules, only products that qualify as broad spectrum and have SPF values of 15 (or higher) can include labeling that the product helps prevent skin cancer and reduces the risk of early skin aging. Other products with SPF values between 2 and 14 may be labeled broad spectrum if they meet FDA tests for UVA and UVB protection, but will be required to have a warning stating that the product has not been shown to prevent skin cancer or early skin aging.
"FDA has evaluated the data and developed testing and labeling requirements for sunscreen products, so that manufacturers can modernize their product information and consumers can be well-informed on which products offer the greatest benefit," said Dr. Janet Woodcock, director of the FDA's Center for Drug Evaluation and Research. "These changes to sunscreen labels are an important part of helping consumers have the information they need so they can choose the right sun protection for themselves and their families."
The new regulations will go into effective in 1 year for most manufacturers. Other sunscreen makers with annual sales of less than $25,000 will have 2 years to comply with the new rules.
For physician perspectives on the announcement, see the story and related video interview "FDA's Sunscreen Regs Should Ease Skin Protection."
The Food and Drug Administration has issued new rules on sunscreen labeling to help consumers select products that prevent sunburn and reduce the risk of skin cancer and early skin aging.
The new labeling will differentiate sunscreen products according to their protective properties. Those products that meet FDA requirements of protection from ultraviolet A (UVA) and ultraviolet B (UVB) will be labeled "Broad Spectrum."
UVA and UVB radiation are known to contribute to sunburn, skin cancer, and premature skin aging. Under the new rules, only products that qualify as broad spectrum and have SPF values of 15 (or higher) can include labeling that the product helps prevent skin cancer and reduces the risk of early skin aging. Other products with SPF values between 2 and 14 may be labeled broad spectrum if they meet FDA tests for UVA and UVB protection, but will be required to have a warning stating that the product has not been shown to prevent skin cancer or early skin aging.
"FDA has evaluated the data and developed testing and labeling requirements for sunscreen products, so that manufacturers can modernize their product information and consumers can be well-informed on which products offer the greatest benefit," said Dr. Janet Woodcock, director of the FDA's Center for Drug Evaluation and Research. "These changes to sunscreen labels are an important part of helping consumers have the information they need so they can choose the right sun protection for themselves and their families."
The new regulations will go into effective in 1 year for most manufacturers. Other sunscreen makers with annual sales of less than $25,000 will have 2 years to comply with the new rules.
For physician perspectives on the announcement, see the story and related video interview "FDA's Sunscreen Regs Should Ease Skin Protection."