User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
New saliva-based COVID-19 test provides rapid results
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
Bone density loss in lean male runners parallels similar issue in women
Similar to a phenomenon already well documented in women, inadequate nutrition appears to be linked to hormonal abnormalities and potentially preventable tibial cortical bone density loss in athletic men, according to results of a small, prospective study.
Based on these findings, “we suspect that a subset of male runners might not be fueling their bodies with enough nutrition and calories for their physical activity,” reported Melanie S. Haines, MD, at the annual meeting of the Endocrine Society.
This is not the first study to suggest male athletes are at risk of a condition equivalent to what has been commonly referred to as the female athlete triad, but it enlarges the objective data that the phenomenon is real, and it makes insufficient availability of energy the likely cause.
In women, the triad is described as a lack of adequate stored energy, irregular menses, and bone density loss. In men, menstrual cycles are not relevant, of course, but this study like others suggests a link between the failure to maintain adequate stores of energy, disturbances in hormone function, and decreased bone density in both men and women, Dr. Haines explained.
RED-S vs. male or female athlete triad
“There is now a move away from the term female athlete triad or male athlete triad,” Dr. Haines reported. Rather the factors of failing to maintain adequate energy for metabolic demands, hormonal disturbances, and bone density loss appear to be relevant to both sexes, according to Dr. Haines, an endocrinologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston. She said several groups, including the International Olympic Committee (IOC), have transitioned to the term RED-S to apply to both sexes.
“RED-S is an acronym for relative energy deficiency in sport, and it appears to be gaining traction,” Dr. Haines said in an interview.
According to her study and others, excessive lean body mass from failure to supply sufficient energy for physiological needs “negatively affects hormones and bone,” Dr. Haines explained. In men and women, endocrine disturbances are triggered when insufficient calories lead to inadequate macro- and micronutrients.
In this study, 31 men aged 16-30 years were evaluated. Fifteen were in the athlete group, defined by running at least 30 miles per week for at least the previous 6 months. There were 16 control subjects; all exercised less than 2 hours per week and did not participate in team sports, but they were not permitted in the study if their body mass index exceeded 27.5 kg/m2.
Athletes vs. otherwise healthy controls
Conditions that affect bone health were exclusion criteria in both groups, and neither group was permitted to take medications affecting bone health other than dietary calcium or vitamin D supplements for 2 months prior to the study.
Tibial cortical porosity was significantly greater – signaling deterioration in microarchitecture – in athletes, compared with control subjects (P = .003), according to quantitative computed tomography measurements. There was also significantly lower tibial cortical bone mineral density (P = .008) among athletes relative to controls.
Conversely, tibial trabecular measures of bone density and architecture were better among athletes than controls, but this was expected and did not contradict the hypothesis of the study.
“Trabecular bone refers to the inner part of the bone, which increases with weight-bearing exercise, but cortical bone is the outer shell, and the source of stress fractures,” Dr. Haines explained.
The median age of both the athletes and the controls was 24 years. Baseline measurements were similar. Body mass index, fat mass, estradiol, and leptin were all numerically lower in the athletes than controls, but none were significant, although there was a trend for the difference in leptin (P = .085).
Hormones correlated with tibial failure load
When these characteristics were evaluated in the context of mean tibial failure load, a metric related to strength, there was a strongly significant positive association with lean body mass (R = 0.85; P < 0.001) and estradiol level (R = 0.66; P = .007). The relationship with leptin also reached significance (R = 0.59; P = .046).
Unexpectedly, there was no relationship between testosterone and tibial failure load. The reason is unclear, but Dr. Haines’s interpretation is that the relationship between specific hormonal disturbances and bone density loss “might not be as simple” as once hypothesized.
The next step is a longitudinal evaluation of the same group of athletes to follow changes in the relationship between these variables over time, according to Dr. Haines.
Eventually, with evidence that there is a causal relationship between nutrition, hormonal changes, and bone loss, the research in this area will focus on better detection of risk and prophylactic strategies.
“Intervention trials to show that we can prevent stress factors will be difficult to perform,” Dr. Haines acknowledged, but she said that preventing adverse changes in bone at relatively young ages could have implications for long-term bone health, including protection from osteoporosis later in life.
The research presented by Dr. Haines is consistent with an area of research that is several decades old, at least in females, according to Siobhan M. Statuta, MD, a sports medicine primary care specialist at the University of Virginia, Charlottesville. The evidence that the same phenomenon occurs in men is more recent, but she said that it is now well accepted the there is a parallel hormonal issue in men and women.
“It is not a question of not eating enough. Often, athletes continue to consume the same diet, but their activity increases,” Dr. Statuta explained. “The problem is that they are not supplying enough of the calories they need to sustain the energy they are expending. You might say they are not fueling their engines appropriately.”
In 2014, the International Olympic Committee published a consensus statement on RED-S. They described this as a condition in which a state of energy deficiency leads to numerous complications in athletes, not just osteoporosis. Rather, a host of physiological systems, ranging from gastrointestinal complaints to cardiovascular events, were described.
RED-S addresses health beyond bones
“The RED-S theory is better described as a spoke-and-wheel concept rather than a triad. While inadequate energy availability is important to both, RED-S places this at the center of the wheel with spokes leading to all the possible complications rather than as a first event in a limited triad,” Dr. Statuta said in an interview.
However, she noted that the term RED-S is not yet appropriate to replace that of the male and female athlete triad.
“More research is required to hash out the relationship of a body in a state of energy deficiency and how it affects the entire body, which is the principle of RED-S,” Dr. Statuta said. “There likely are scientific effects, and we are currently investigating these relationships more.”
“These are really quite similar entities but have different foci,” she added. Based on data collected over several decades, “the triad narrows in on two body systems affected by low energy – the reproductive system and bones. RED-S incorporates these same systems yet adds on many more organ systems.
The original group of researchers have remained loyal to the concept of the triad that involves inadequate availability of energy followed by hormonal irregularities and osteoporosis. This group, the Female and Male Athlete Triad Coalition, has issued publications on this topic several times. Consensus statements were updated last year.
“The premise is that the triad leading to bone loss is shared by both men and women, even if the clinical manifestations differ,” said Dr. Statuta. The most notable difference is that men do not experience menstrual irregularities, but Dr. Statuta suggested that the clinical consequences are not necessarily any less.
“Males do not have menstrual cycles as an outward marker of an endocrine disturbance, so it is harder to recognize clinically, but I think there is agreement that not having enough energy available is the trigger of endocrine changes and then bone loss is relevant to both sexes,” she said. She said this is supported by a growing body of evidence, including the data presented by Dr. Haines at the Endocrine Society meeting.
Dr. Haines and Dr. Statuta report no potential conflicts of interest.
Similar to a phenomenon already well documented in women, inadequate nutrition appears to be linked to hormonal abnormalities and potentially preventable tibial cortical bone density loss in athletic men, according to results of a small, prospective study.
Based on these findings, “we suspect that a subset of male runners might not be fueling their bodies with enough nutrition and calories for their physical activity,” reported Melanie S. Haines, MD, at the annual meeting of the Endocrine Society.
This is not the first study to suggest male athletes are at risk of a condition equivalent to what has been commonly referred to as the female athlete triad, but it enlarges the objective data that the phenomenon is real, and it makes insufficient availability of energy the likely cause.
In women, the triad is described as a lack of adequate stored energy, irregular menses, and bone density loss. In men, menstrual cycles are not relevant, of course, but this study like others suggests a link between the failure to maintain adequate stores of energy, disturbances in hormone function, and decreased bone density in both men and women, Dr. Haines explained.
RED-S vs. male or female athlete triad
“There is now a move away from the term female athlete triad or male athlete triad,” Dr. Haines reported. Rather the factors of failing to maintain adequate energy for metabolic demands, hormonal disturbances, and bone density loss appear to be relevant to both sexes, according to Dr. Haines, an endocrinologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston. She said several groups, including the International Olympic Committee (IOC), have transitioned to the term RED-S to apply to both sexes.
“RED-S is an acronym for relative energy deficiency in sport, and it appears to be gaining traction,” Dr. Haines said in an interview.
According to her study and others, excessive lean body mass from failure to supply sufficient energy for physiological needs “negatively affects hormones and bone,” Dr. Haines explained. In men and women, endocrine disturbances are triggered when insufficient calories lead to inadequate macro- and micronutrients.
In this study, 31 men aged 16-30 years were evaluated. Fifteen were in the athlete group, defined by running at least 30 miles per week for at least the previous 6 months. There were 16 control subjects; all exercised less than 2 hours per week and did not participate in team sports, but they were not permitted in the study if their body mass index exceeded 27.5 kg/m2.
Athletes vs. otherwise healthy controls
Conditions that affect bone health were exclusion criteria in both groups, and neither group was permitted to take medications affecting bone health other than dietary calcium or vitamin D supplements for 2 months prior to the study.
Tibial cortical porosity was significantly greater – signaling deterioration in microarchitecture – in athletes, compared with control subjects (P = .003), according to quantitative computed tomography measurements. There was also significantly lower tibial cortical bone mineral density (P = .008) among athletes relative to controls.
Conversely, tibial trabecular measures of bone density and architecture were better among athletes than controls, but this was expected and did not contradict the hypothesis of the study.
“Trabecular bone refers to the inner part of the bone, which increases with weight-bearing exercise, but cortical bone is the outer shell, and the source of stress fractures,” Dr. Haines explained.
The median age of both the athletes and the controls was 24 years. Baseline measurements were similar. Body mass index, fat mass, estradiol, and leptin were all numerically lower in the athletes than controls, but none were significant, although there was a trend for the difference in leptin (P = .085).
Hormones correlated with tibial failure load
When these characteristics were evaluated in the context of mean tibial failure load, a metric related to strength, there was a strongly significant positive association with lean body mass (R = 0.85; P < 0.001) and estradiol level (R = 0.66; P = .007). The relationship with leptin also reached significance (R = 0.59; P = .046).
Unexpectedly, there was no relationship between testosterone and tibial failure load. The reason is unclear, but Dr. Haines’s interpretation is that the relationship between specific hormonal disturbances and bone density loss “might not be as simple” as once hypothesized.
The next step is a longitudinal evaluation of the same group of athletes to follow changes in the relationship between these variables over time, according to Dr. Haines.
Eventually, with evidence that there is a causal relationship between nutrition, hormonal changes, and bone loss, the research in this area will focus on better detection of risk and prophylactic strategies.
“Intervention trials to show that we can prevent stress factors will be difficult to perform,” Dr. Haines acknowledged, but she said that preventing adverse changes in bone at relatively young ages could have implications for long-term bone health, including protection from osteoporosis later in life.
The research presented by Dr. Haines is consistent with an area of research that is several decades old, at least in females, according to Siobhan M. Statuta, MD, a sports medicine primary care specialist at the University of Virginia, Charlottesville. The evidence that the same phenomenon occurs in men is more recent, but she said that it is now well accepted the there is a parallel hormonal issue in men and women.
“It is not a question of not eating enough. Often, athletes continue to consume the same diet, but their activity increases,” Dr. Statuta explained. “The problem is that they are not supplying enough of the calories they need to sustain the energy they are expending. You might say they are not fueling their engines appropriately.”
In 2014, the International Olympic Committee published a consensus statement on RED-S. They described this as a condition in which a state of energy deficiency leads to numerous complications in athletes, not just osteoporosis. Rather, a host of physiological systems, ranging from gastrointestinal complaints to cardiovascular events, were described.
RED-S addresses health beyond bones
“The RED-S theory is better described as a spoke-and-wheel concept rather than a triad. While inadequate energy availability is important to both, RED-S places this at the center of the wheel with spokes leading to all the possible complications rather than as a first event in a limited triad,” Dr. Statuta said in an interview.
However, she noted that the term RED-S is not yet appropriate to replace that of the male and female athlete triad.
“More research is required to hash out the relationship of a body in a state of energy deficiency and how it affects the entire body, which is the principle of RED-S,” Dr. Statuta said. “There likely are scientific effects, and we are currently investigating these relationships more.”
“These are really quite similar entities but have different foci,” she added. Based on data collected over several decades, “the triad narrows in on two body systems affected by low energy – the reproductive system and bones. RED-S incorporates these same systems yet adds on many more organ systems.
The original group of researchers have remained loyal to the concept of the triad that involves inadequate availability of energy followed by hormonal irregularities and osteoporosis. This group, the Female and Male Athlete Triad Coalition, has issued publications on this topic several times. Consensus statements were updated last year.
“The premise is that the triad leading to bone loss is shared by both men and women, even if the clinical manifestations differ,” said Dr. Statuta. The most notable difference is that men do not experience menstrual irregularities, but Dr. Statuta suggested that the clinical consequences are not necessarily any less.
“Males do not have menstrual cycles as an outward marker of an endocrine disturbance, so it is harder to recognize clinically, but I think there is agreement that not having enough energy available is the trigger of endocrine changes and then bone loss is relevant to both sexes,” she said. She said this is supported by a growing body of evidence, including the data presented by Dr. Haines at the Endocrine Society meeting.
Dr. Haines and Dr. Statuta report no potential conflicts of interest.
Similar to a phenomenon already well documented in women, inadequate nutrition appears to be linked to hormonal abnormalities and potentially preventable tibial cortical bone density loss in athletic men, according to results of a small, prospective study.
Based on these findings, “we suspect that a subset of male runners might not be fueling their bodies with enough nutrition and calories for their physical activity,” reported Melanie S. Haines, MD, at the annual meeting of the Endocrine Society.
This is not the first study to suggest male athletes are at risk of a condition equivalent to what has been commonly referred to as the female athlete triad, but it enlarges the objective data that the phenomenon is real, and it makes insufficient availability of energy the likely cause.
In women, the triad is described as a lack of adequate stored energy, irregular menses, and bone density loss. In men, menstrual cycles are not relevant, of course, but this study like others suggests a link between the failure to maintain adequate stores of energy, disturbances in hormone function, and decreased bone density in both men and women, Dr. Haines explained.
RED-S vs. male or female athlete triad
“There is now a move away from the term female athlete triad or male athlete triad,” Dr. Haines reported. Rather the factors of failing to maintain adequate energy for metabolic demands, hormonal disturbances, and bone density loss appear to be relevant to both sexes, according to Dr. Haines, an endocrinologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston. She said several groups, including the International Olympic Committee (IOC), have transitioned to the term RED-S to apply to both sexes.
“RED-S is an acronym for relative energy deficiency in sport, and it appears to be gaining traction,” Dr. Haines said in an interview.
According to her study and others, excessive lean body mass from failure to supply sufficient energy for physiological needs “negatively affects hormones and bone,” Dr. Haines explained. In men and women, endocrine disturbances are triggered when insufficient calories lead to inadequate macro- and micronutrients.
In this study, 31 men aged 16-30 years were evaluated. Fifteen were in the athlete group, defined by running at least 30 miles per week for at least the previous 6 months. There were 16 control subjects; all exercised less than 2 hours per week and did not participate in team sports, but they were not permitted in the study if their body mass index exceeded 27.5 kg/m2.
Athletes vs. otherwise healthy controls
Conditions that affect bone health were exclusion criteria in both groups, and neither group was permitted to take medications affecting bone health other than dietary calcium or vitamin D supplements for 2 months prior to the study.
Tibial cortical porosity was significantly greater – signaling deterioration in microarchitecture – in athletes, compared with control subjects (P = .003), according to quantitative computed tomography measurements. There was also significantly lower tibial cortical bone mineral density (P = .008) among athletes relative to controls.
Conversely, tibial trabecular measures of bone density and architecture were better among athletes than controls, but this was expected and did not contradict the hypothesis of the study.
“Trabecular bone refers to the inner part of the bone, which increases with weight-bearing exercise, but cortical bone is the outer shell, and the source of stress fractures,” Dr. Haines explained.
The median age of both the athletes and the controls was 24 years. Baseline measurements were similar. Body mass index, fat mass, estradiol, and leptin were all numerically lower in the athletes than controls, but none were significant, although there was a trend for the difference in leptin (P = .085).
Hormones correlated with tibial failure load
When these characteristics were evaluated in the context of mean tibial failure load, a metric related to strength, there was a strongly significant positive association with lean body mass (R = 0.85; P < 0.001) and estradiol level (R = 0.66; P = .007). The relationship with leptin also reached significance (R = 0.59; P = .046).
Unexpectedly, there was no relationship between testosterone and tibial failure load. The reason is unclear, but Dr. Haines’s interpretation is that the relationship between specific hormonal disturbances and bone density loss “might not be as simple” as once hypothesized.
The next step is a longitudinal evaluation of the same group of athletes to follow changes in the relationship between these variables over time, according to Dr. Haines.
Eventually, with evidence that there is a causal relationship between nutrition, hormonal changes, and bone loss, the research in this area will focus on better detection of risk and prophylactic strategies.
“Intervention trials to show that we can prevent stress factors will be difficult to perform,” Dr. Haines acknowledged, but she said that preventing adverse changes in bone at relatively young ages could have implications for long-term bone health, including protection from osteoporosis later in life.
The research presented by Dr. Haines is consistent with an area of research that is several decades old, at least in females, according to Siobhan M. Statuta, MD, a sports medicine primary care specialist at the University of Virginia, Charlottesville. The evidence that the same phenomenon occurs in men is more recent, but she said that it is now well accepted the there is a parallel hormonal issue in men and women.
“It is not a question of not eating enough. Often, athletes continue to consume the same diet, but their activity increases,” Dr. Statuta explained. “The problem is that they are not supplying enough of the calories they need to sustain the energy they are expending. You might say they are not fueling their engines appropriately.”
In 2014, the International Olympic Committee published a consensus statement on RED-S. They described this as a condition in which a state of energy deficiency leads to numerous complications in athletes, not just osteoporosis. Rather, a host of physiological systems, ranging from gastrointestinal complaints to cardiovascular events, were described.
RED-S addresses health beyond bones
“The RED-S theory is better described as a spoke-and-wheel concept rather than a triad. While inadequate energy availability is important to both, RED-S places this at the center of the wheel with spokes leading to all the possible complications rather than as a first event in a limited triad,” Dr. Statuta said in an interview.
However, she noted that the term RED-S is not yet appropriate to replace that of the male and female athlete triad.
“More research is required to hash out the relationship of a body in a state of energy deficiency and how it affects the entire body, which is the principle of RED-S,” Dr. Statuta said. “There likely are scientific effects, and we are currently investigating these relationships more.”
“These are really quite similar entities but have different foci,” she added. Based on data collected over several decades, “the triad narrows in on two body systems affected by low energy – the reproductive system and bones. RED-S incorporates these same systems yet adds on many more organ systems.
The original group of researchers have remained loyal to the concept of the triad that involves inadequate availability of energy followed by hormonal irregularities and osteoporosis. This group, the Female and Male Athlete Triad Coalition, has issued publications on this topic several times. Consensus statements were updated last year.
“The premise is that the triad leading to bone loss is shared by both men and women, even if the clinical manifestations differ,” said Dr. Statuta. The most notable difference is that men do not experience menstrual irregularities, but Dr. Statuta suggested that the clinical consequences are not necessarily any less.
“Males do not have menstrual cycles as an outward marker of an endocrine disturbance, so it is harder to recognize clinically, but I think there is agreement that not having enough energy available is the trigger of endocrine changes and then bone loss is relevant to both sexes,” she said. She said this is supported by a growing body of evidence, including the data presented by Dr. Haines at the Endocrine Society meeting.
Dr. Haines and Dr. Statuta report no potential conflicts of interest.
FROM ENDO 2022
Biden moves to limit nicotine levels in cigarettes
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
COVID-19 Pandemic stress affected ovulation, not menstruation
ATLANTA – Disturbances in ovulation that didn’t produce any actual changes in the menstrual cycle of women were extremely common during the first year of the COVID-19 pandemic and were linked to emotional stress, according to the findings of an “experiment of nature” that allowed for comparison with women a decade earlier.
Findings from two studies of reproductive-age women, one conducted in 2006-2008 and the other in 2020-2021, were presented by Jerilynn C. Prior, MD, at the annual meeting of the Endocrine Society.
The comparison of the two time periods yielded several novel findings. “I was taught in medical school that when women don’t eat enough they lose their period. But what we now understand is there’s a graded response to various stressors, acting through the hypothalamus in a common pathway. There is a gradation of disturbances, some of which are subclinical or not obvious,” said Dr. Prior, professor of endocrinology and metabolism at the University of British Columbia, Vancouver.
Moreover, women’s menstrual cycle lengths didn’t differ across the two time periods, despite a dramatic 63% decrement in normal ovulatory function related to increased depression, anxiety, and outside stresses that the women reported in diaries.
“Assuming that regular cycles need normal ovulation is something we should just get out of our minds. It changes our concept about what’s normal if we only know about the cycle length,” she observed.
It will be critical going forward to see whether the ovulatory disturbances have resolved as the pandemic has shifted “because there’s strong evidence that ovulatory disturbances, even with normal cycle length, are related to bone loss and some evidence it’s related to early heart attacks, breast and endometrial cancers,” Dr. Prior said during a press conference.
Asked to comment, session moderator Genevieve Neal-Perry, MD, PhD, told this news organization: “I think what we can take away is that stress itself is a modifier of the way the brain and the gonads communicate with each other, and that then has an impact on ovulatory function.”
Dr. Neal-Perry noted that the association of stress and ovulatory disruption has been reported in various ways previously, but “clearly it doesn’t affect everyone. What we don’t know is who is most susceptible. There have been some studies showing a genetic predisposition and a genetic anomaly that actually makes them more susceptible to the impact of stress on the reproductive system.”
But the lack of data on weight change in the study cohorts is a limitation. “To me one of the more important questions was what was going on with weight. Just looking at a static number doesn’t tell you whether there were changes. We know that weight gain or weight loss can stress the reproductive axis,” noted Dr. Neal-Parry of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
‘Experiment of nature’ revealed invisible effect of pandemic stress
The women in both cohorts of the Menstruation Ovulation Study (MOS) were healthy volunteers aged 19-35 years recruited from the metropolitan Vancouver region. All were menstruating monthly and none were taking hormonal birth control. Recruitment for the second cohort had begun just prior to the March 2020 COVID-19 pandemic lockdown.
Interviewer-administered questionnaires (CaMos) covering demographics, socioeconomic status, and reproductive history, and daily diaries kept by the women (menstrual cycle diary) were identical for both cohorts.
Assessments of ovulation differed for the two studies but were cross-validated. For the earlier time period, ovulation was assessed by a threefold increase in follicular-to-luteal urinary progesterone (PdG). For the pandemic-era study, the validated quantitative basal temperature (QBT) method was used.
There were 301 women in the earlier cohort and 125 during the pandemic. Both were an average age of about 29 years and had a body mass index of about 24.3 kg/m2 (within the normal range). The pandemic cohort was more racially/ethnically diverse than the earlier one and more in-line with recent census data.
More of the women were nulliparous during the pandemic than earlier (92.7% vs. 80.4%; P = .002).
The distribution of menstrual cycle lengths didn’t differ, with both cohorts averaging about 30 days (P = .893). However, while 90% of the women in the earlier cohort ovulated normally, only 37% did during the pandemic, a highly significant difference (P < .0001).
Thus, during the pandemic, 63% of women had “silent ovulatory disturbances,” either with short luteal phases after ovulation or no ovulation, compared with just 10% in the earlier cohort, “which is remarkable, unbelievable actually,” Dr. Prior remarked.
The difference wasn’t explained by any of the demographic information collected either, including socioeconomic status, lifestyle, or reproductive history variables.
And it wasn’t because of COVID-19 vaccination, as the vaccine wasn’t available when most of the women were recruited, and of the 79 who were recruited during vaccine availability, only two received a COVID-19 vaccine during the study (and both had normal ovulation).
Employment changes, caring responsibilities, and worry likely causes
The information from the diaries was more revealing. Several diary components were far more common during the pandemic, including negative mood (feeling depressed or anxious, sleep problems, and outside stresses), self-worth, interest in sex, energy level, and appetite. All were significantly different between the two cohorts (P < .001) and between those with and without ovulatory disturbances.
“So menstrual cycle lengths and long cycles didn’t differ, but there was a much higher prevalence of silent or subclinical ovulatory disturbances, and these were related to the increased stresses that women recorded in their diaries. This means that the estrogen levels were pretty close to normal but the progesterone levels were remarkably decreased,” Dr. Prior said.
Interestingly, reported menstrual cramps were also significantly more common during the pandemic and associated with ovulatory disruption.
“That is a new observation because previously we’ve always thought that you needed to ovulate in order to even have cramps,” she commented.
Asked whether COVID-19 itself might have played a role, Dr. Prior said no woman in the study tested positive for the virus or had long COVID.
“As far as I’m aware, it was the changes in employment … and caring for elders and worry about illness in somebody you loved that was related,” she said.
Asked what she thinks the result would be if the study were conducted now, she said: “I don’t know. We’re still in a stressful time with inflation and not complete recovery, so probably the issue is still very present.”
Dr. Prior and Dr. Neal-Perry have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA – Disturbances in ovulation that didn’t produce any actual changes in the menstrual cycle of women were extremely common during the first year of the COVID-19 pandemic and were linked to emotional stress, according to the findings of an “experiment of nature” that allowed for comparison with women a decade earlier.
Findings from two studies of reproductive-age women, one conducted in 2006-2008 and the other in 2020-2021, were presented by Jerilynn C. Prior, MD, at the annual meeting of the Endocrine Society.
The comparison of the two time periods yielded several novel findings. “I was taught in medical school that when women don’t eat enough they lose their period. But what we now understand is there’s a graded response to various stressors, acting through the hypothalamus in a common pathway. There is a gradation of disturbances, some of which are subclinical or not obvious,” said Dr. Prior, professor of endocrinology and metabolism at the University of British Columbia, Vancouver.
Moreover, women’s menstrual cycle lengths didn’t differ across the two time periods, despite a dramatic 63% decrement in normal ovulatory function related to increased depression, anxiety, and outside stresses that the women reported in diaries.
“Assuming that regular cycles need normal ovulation is something we should just get out of our minds. It changes our concept about what’s normal if we only know about the cycle length,” she observed.
It will be critical going forward to see whether the ovulatory disturbances have resolved as the pandemic has shifted “because there’s strong evidence that ovulatory disturbances, even with normal cycle length, are related to bone loss and some evidence it’s related to early heart attacks, breast and endometrial cancers,” Dr. Prior said during a press conference.
Asked to comment, session moderator Genevieve Neal-Perry, MD, PhD, told this news organization: “I think what we can take away is that stress itself is a modifier of the way the brain and the gonads communicate with each other, and that then has an impact on ovulatory function.”
Dr. Neal-Perry noted that the association of stress and ovulatory disruption has been reported in various ways previously, but “clearly it doesn’t affect everyone. What we don’t know is who is most susceptible. There have been some studies showing a genetic predisposition and a genetic anomaly that actually makes them more susceptible to the impact of stress on the reproductive system.”
But the lack of data on weight change in the study cohorts is a limitation. “To me one of the more important questions was what was going on with weight. Just looking at a static number doesn’t tell you whether there were changes. We know that weight gain or weight loss can stress the reproductive axis,” noted Dr. Neal-Parry of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
‘Experiment of nature’ revealed invisible effect of pandemic stress
The women in both cohorts of the Menstruation Ovulation Study (MOS) were healthy volunteers aged 19-35 years recruited from the metropolitan Vancouver region. All were menstruating monthly and none were taking hormonal birth control. Recruitment for the second cohort had begun just prior to the March 2020 COVID-19 pandemic lockdown.
Interviewer-administered questionnaires (CaMos) covering demographics, socioeconomic status, and reproductive history, and daily diaries kept by the women (menstrual cycle diary) were identical for both cohorts.
Assessments of ovulation differed for the two studies but were cross-validated. For the earlier time period, ovulation was assessed by a threefold increase in follicular-to-luteal urinary progesterone (PdG). For the pandemic-era study, the validated quantitative basal temperature (QBT) method was used.
There were 301 women in the earlier cohort and 125 during the pandemic. Both were an average age of about 29 years and had a body mass index of about 24.3 kg/m2 (within the normal range). The pandemic cohort was more racially/ethnically diverse than the earlier one and more in-line with recent census data.
More of the women were nulliparous during the pandemic than earlier (92.7% vs. 80.4%; P = .002).
The distribution of menstrual cycle lengths didn’t differ, with both cohorts averaging about 30 days (P = .893). However, while 90% of the women in the earlier cohort ovulated normally, only 37% did during the pandemic, a highly significant difference (P < .0001).
Thus, during the pandemic, 63% of women had “silent ovulatory disturbances,” either with short luteal phases after ovulation or no ovulation, compared with just 10% in the earlier cohort, “which is remarkable, unbelievable actually,” Dr. Prior remarked.
The difference wasn’t explained by any of the demographic information collected either, including socioeconomic status, lifestyle, or reproductive history variables.
And it wasn’t because of COVID-19 vaccination, as the vaccine wasn’t available when most of the women were recruited, and of the 79 who were recruited during vaccine availability, only two received a COVID-19 vaccine during the study (and both had normal ovulation).
Employment changes, caring responsibilities, and worry likely causes
The information from the diaries was more revealing. Several diary components were far more common during the pandemic, including negative mood (feeling depressed or anxious, sleep problems, and outside stresses), self-worth, interest in sex, energy level, and appetite. All were significantly different between the two cohorts (P < .001) and between those with and without ovulatory disturbances.
“So menstrual cycle lengths and long cycles didn’t differ, but there was a much higher prevalence of silent or subclinical ovulatory disturbances, and these were related to the increased stresses that women recorded in their diaries. This means that the estrogen levels were pretty close to normal but the progesterone levels were remarkably decreased,” Dr. Prior said.
Interestingly, reported menstrual cramps were also significantly more common during the pandemic and associated with ovulatory disruption.
“That is a new observation because previously we’ve always thought that you needed to ovulate in order to even have cramps,” she commented.
Asked whether COVID-19 itself might have played a role, Dr. Prior said no woman in the study tested positive for the virus or had long COVID.
“As far as I’m aware, it was the changes in employment … and caring for elders and worry about illness in somebody you loved that was related,” she said.
Asked what she thinks the result would be if the study were conducted now, she said: “I don’t know. We’re still in a stressful time with inflation and not complete recovery, so probably the issue is still very present.”
Dr. Prior and Dr. Neal-Perry have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA – Disturbances in ovulation that didn’t produce any actual changes in the menstrual cycle of women were extremely common during the first year of the COVID-19 pandemic and were linked to emotional stress, according to the findings of an “experiment of nature” that allowed for comparison with women a decade earlier.
Findings from two studies of reproductive-age women, one conducted in 2006-2008 and the other in 2020-2021, were presented by Jerilynn C. Prior, MD, at the annual meeting of the Endocrine Society.
The comparison of the two time periods yielded several novel findings. “I was taught in medical school that when women don’t eat enough they lose their period. But what we now understand is there’s a graded response to various stressors, acting through the hypothalamus in a common pathway. There is a gradation of disturbances, some of which are subclinical or not obvious,” said Dr. Prior, professor of endocrinology and metabolism at the University of British Columbia, Vancouver.
Moreover, women’s menstrual cycle lengths didn’t differ across the two time periods, despite a dramatic 63% decrement in normal ovulatory function related to increased depression, anxiety, and outside stresses that the women reported in diaries.
“Assuming that regular cycles need normal ovulation is something we should just get out of our minds. It changes our concept about what’s normal if we only know about the cycle length,” she observed.
It will be critical going forward to see whether the ovulatory disturbances have resolved as the pandemic has shifted “because there’s strong evidence that ovulatory disturbances, even with normal cycle length, are related to bone loss and some evidence it’s related to early heart attacks, breast and endometrial cancers,” Dr. Prior said during a press conference.
Asked to comment, session moderator Genevieve Neal-Perry, MD, PhD, told this news organization: “I think what we can take away is that stress itself is a modifier of the way the brain and the gonads communicate with each other, and that then has an impact on ovulatory function.”
Dr. Neal-Perry noted that the association of stress and ovulatory disruption has been reported in various ways previously, but “clearly it doesn’t affect everyone. What we don’t know is who is most susceptible. There have been some studies showing a genetic predisposition and a genetic anomaly that actually makes them more susceptible to the impact of stress on the reproductive system.”
But the lack of data on weight change in the study cohorts is a limitation. “To me one of the more important questions was what was going on with weight. Just looking at a static number doesn’t tell you whether there were changes. We know that weight gain or weight loss can stress the reproductive axis,” noted Dr. Neal-Parry of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
‘Experiment of nature’ revealed invisible effect of pandemic stress
The women in both cohorts of the Menstruation Ovulation Study (MOS) were healthy volunteers aged 19-35 years recruited from the metropolitan Vancouver region. All were menstruating monthly and none were taking hormonal birth control. Recruitment for the second cohort had begun just prior to the March 2020 COVID-19 pandemic lockdown.
Interviewer-administered questionnaires (CaMos) covering demographics, socioeconomic status, and reproductive history, and daily diaries kept by the women (menstrual cycle diary) were identical for both cohorts.
Assessments of ovulation differed for the two studies but were cross-validated. For the earlier time period, ovulation was assessed by a threefold increase in follicular-to-luteal urinary progesterone (PdG). For the pandemic-era study, the validated quantitative basal temperature (QBT) method was used.
There were 301 women in the earlier cohort and 125 during the pandemic. Both were an average age of about 29 years and had a body mass index of about 24.3 kg/m2 (within the normal range). The pandemic cohort was more racially/ethnically diverse than the earlier one and more in-line with recent census data.
More of the women were nulliparous during the pandemic than earlier (92.7% vs. 80.4%; P = .002).
The distribution of menstrual cycle lengths didn’t differ, with both cohorts averaging about 30 days (P = .893). However, while 90% of the women in the earlier cohort ovulated normally, only 37% did during the pandemic, a highly significant difference (P < .0001).
Thus, during the pandemic, 63% of women had “silent ovulatory disturbances,” either with short luteal phases after ovulation or no ovulation, compared with just 10% in the earlier cohort, “which is remarkable, unbelievable actually,” Dr. Prior remarked.
The difference wasn’t explained by any of the demographic information collected either, including socioeconomic status, lifestyle, or reproductive history variables.
And it wasn’t because of COVID-19 vaccination, as the vaccine wasn’t available when most of the women were recruited, and of the 79 who were recruited during vaccine availability, only two received a COVID-19 vaccine during the study (and both had normal ovulation).
Employment changes, caring responsibilities, and worry likely causes
The information from the diaries was more revealing. Several diary components were far more common during the pandemic, including negative mood (feeling depressed or anxious, sleep problems, and outside stresses), self-worth, interest in sex, energy level, and appetite. All were significantly different between the two cohorts (P < .001) and between those with and without ovulatory disturbances.
“So menstrual cycle lengths and long cycles didn’t differ, but there was a much higher prevalence of silent or subclinical ovulatory disturbances, and these were related to the increased stresses that women recorded in their diaries. This means that the estrogen levels were pretty close to normal but the progesterone levels were remarkably decreased,” Dr. Prior said.
Interestingly, reported menstrual cramps were also significantly more common during the pandemic and associated with ovulatory disruption.
“That is a new observation because previously we’ve always thought that you needed to ovulate in order to even have cramps,” she commented.
Asked whether COVID-19 itself might have played a role, Dr. Prior said no woman in the study tested positive for the virus or had long COVID.
“As far as I’m aware, it was the changes in employment … and caring for elders and worry about illness in somebody you loved that was related,” she said.
Asked what she thinks the result would be if the study were conducted now, she said: “I don’t know. We’re still in a stressful time with inflation and not complete recovery, so probably the issue is still very present.”
Dr. Prior and Dr. Neal-Perry have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ENDO 2022
Pandemic public health measures may have mitigated Kawasaki disease
The social behavior associated with the COVID-19 pandemic may have reduced the incidence of Kawasaki disease, according to results of a cohort study of nearly 4,000 children.
The incidence of Kawasaki disease in the United States declined by 28.2% between 2018 and 2020, possibly as a result of factors including school closures, mask mandates, and reduced ambient pollution that might reduce exposure to Kawasaki disease (KD) in the environment, but a potential association has not been explored, wrote Jennifer A. Burney, PhD, of the University of California, San Diego, and colleagues.
KD received greater attention in the public and medical communities because of the emergence of multisystem inflammatory syndrome in children (MIS-C), which is similar to, but distinct from, KD, and because of the noticeable drop in KD cases during the pandemic, the researchers said.
In a multicenter cohort study published in JAMA Network Open , the researchers reviewed data from 2,461 consecutive patients with KD who were diagnosed between Jan. 1, 2018, and Dec. 31, 2020. They conducted a detailed analysis of analysis of 1,461 children with KD who were diagnosed between Jan. 1, 2002, and Nov. 15, 2021, at Rady Children’s Hospital San Diego (RCHSD), using data from before, during, and after the height of the pandemic. The median age of the children in the RCHSD analysis was 2.8 years, 62% were male, and 35% were Hispanic.
Overall, the prevalence of KD declined from 894 in 2018 to 646 in 2020, across the United States, but the decline was uneven, the researchers noted.
In the RCHSD cohort in San Diego, KD cases in children aged 1-5 years decreased significantly from 2020 to 2021 compared to the mean number of cases in previous years (22 vs. 44.9, P = .02). KD cases also decreased significantly among males and Asian children.
Notably, the occurrence of the KD clinical features of strawberry tongue, enlarged cervical lymph node, and subacute periungual desquamation decreased during 2020 compared with the baseline period, although only strawberry tongue reached statistical significance (39% vs. 63%, P = .04). The prevalence of patients with an enlarged lymph node was 21% in 2020 vs. 32% prior to the pandemic (P = .09); the prevalence of periungual desquamation during these periods was 47% vs. 58%, P = .16).
The researchers also used data from Census Block Groups (CBGs) to assess the impact of mobility metrics and environmental exposures on KD during the pandemic for the San Diego patient cohort. They found that KD cases during the pandemic were more likely to occur in neighborhoods of higher socioeconomic status, and that neighborhoods with lower levels of nitrous oxides had fewer KD cases.
Overall, “The reduction in KD case numbers coincided with masking, school closures, reduced circulation of respiratory viruses, and reduced air pollution,” the researchers wrote in their discussion of the findings. “A rebound in KD case numbers to prepandemic levels coincided with the lifting of mask mandates and, subsequently, the return to in-person schooling,” they wrote.
The study findings were limited by several factors including the small sample sizes, which also limit the interpretation of mobility and pollution data, the researchers noted. Other limitations include the high interannual variability of KD and the inclusion of 2021 rebound data from the San Diego region only.
“Although our original hypothesis was that shelter-in-place measures would track with reduced KD cases, this was not borne out by the San Diego region data. Instead, the San Diego case occurrence data suggest that exposures that triggered KD were more likely to occur in the home, with a shift toward households with higher SES during the pandemic,” the researchers noted. However, “The results presented here are consistent with a respiratory portal of entry for the trigger(s) of KD,” they said.
Study fails to validate its conclusions
“This study attempts to test the hypothesis that various social restrictions were associated with a decrease in rate of diagnosed Kawasaki disease cases during portions of the SARS-CoV-2 pandemic,” Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, said in an interview.
“However, it appears that it fails to achieve this conclusion and I disagree with the findings,” said Dr. Gorelik, who was not involved in the study but served as first author on an updated Kawasaki disease treatment guideline published earlier this spring in Arthritis & Rheumatology.
“The study does not find statistically significant associations either with shelter in place orders or with cell phone mobility data, as stated in the conclusion, directly contradicting its own claim,” Dr. Gorelik said. “Secondly, the study makes an assumption that various methods, especially the wearing of masks by children and school closures, had a significant effect on the spread of respiratory viruses. There are no prospective, population based, controlled real world studies that validate this claim, and two prospective controlled real-world studies that dispute this,” he emphasized. “Cloth masks and surgical masks, which were the types of masks worn by school students, are also known to have a nonsignificant and paltry – in the latter, certainly less than 50%, and perhaps as little as 10% – effect on the reduction of respiratory viral spread,” he added.
“Mechanistic studies on mask wearing may suggest some mask efficacy, but these studies are as valid as mechanistic studies showing the effect of various antifungal pharmaceuticals on the replication of SARS-CoV-2 virus in culture, meaning only valid as hypothesis generating, and ultimately the latter hypothesis failed to bear out,” Dr. Gorelik explained. “We do not know the reason why other respiratory viruses and non-SARS-CoV-2 coronaviruses declined during the pandemic, but we do know that despite this, the SARS-CoV-2 coronavirus itself did not appear to suffer the same fate. Thus, it is very possible that another factor was at work, and we know that during other viral pandemics, typically circulating viruses decline, potentially due to induction of interferon responses in hosts, in a general effect known as ‘viral interference,’ ” he said.
“Overall, we must have robust evidence to support benefits of hypotheses that have demonstrated clear damage to children during this pandemic (such as school closures), and this study fails to live up to that requirement,” Dr. Gorelik said.
The study was supported by the Gordon and Marilyn Macklin Foundation and the Patient-Centered Outcomes Research Institute. Dr. Burney and Dr. Gorelik had no financial conflicts to disclose.
The social behavior associated with the COVID-19 pandemic may have reduced the incidence of Kawasaki disease, according to results of a cohort study of nearly 4,000 children.
The incidence of Kawasaki disease in the United States declined by 28.2% between 2018 and 2020, possibly as a result of factors including school closures, mask mandates, and reduced ambient pollution that might reduce exposure to Kawasaki disease (KD) in the environment, but a potential association has not been explored, wrote Jennifer A. Burney, PhD, of the University of California, San Diego, and colleagues.
KD received greater attention in the public and medical communities because of the emergence of multisystem inflammatory syndrome in children (MIS-C), which is similar to, but distinct from, KD, and because of the noticeable drop in KD cases during the pandemic, the researchers said.
In a multicenter cohort study published in JAMA Network Open , the researchers reviewed data from 2,461 consecutive patients with KD who were diagnosed between Jan. 1, 2018, and Dec. 31, 2020. They conducted a detailed analysis of analysis of 1,461 children with KD who were diagnosed between Jan. 1, 2002, and Nov. 15, 2021, at Rady Children’s Hospital San Diego (RCHSD), using data from before, during, and after the height of the pandemic. The median age of the children in the RCHSD analysis was 2.8 years, 62% were male, and 35% were Hispanic.
Overall, the prevalence of KD declined from 894 in 2018 to 646 in 2020, across the United States, but the decline was uneven, the researchers noted.
In the RCHSD cohort in San Diego, KD cases in children aged 1-5 years decreased significantly from 2020 to 2021 compared to the mean number of cases in previous years (22 vs. 44.9, P = .02). KD cases also decreased significantly among males and Asian children.
Notably, the occurrence of the KD clinical features of strawberry tongue, enlarged cervical lymph node, and subacute periungual desquamation decreased during 2020 compared with the baseline period, although only strawberry tongue reached statistical significance (39% vs. 63%, P = .04). The prevalence of patients with an enlarged lymph node was 21% in 2020 vs. 32% prior to the pandemic (P = .09); the prevalence of periungual desquamation during these periods was 47% vs. 58%, P = .16).
The researchers also used data from Census Block Groups (CBGs) to assess the impact of mobility metrics and environmental exposures on KD during the pandemic for the San Diego patient cohort. They found that KD cases during the pandemic were more likely to occur in neighborhoods of higher socioeconomic status, and that neighborhoods with lower levels of nitrous oxides had fewer KD cases.
Overall, “The reduction in KD case numbers coincided with masking, school closures, reduced circulation of respiratory viruses, and reduced air pollution,” the researchers wrote in their discussion of the findings. “A rebound in KD case numbers to prepandemic levels coincided with the lifting of mask mandates and, subsequently, the return to in-person schooling,” they wrote.
The study findings were limited by several factors including the small sample sizes, which also limit the interpretation of mobility and pollution data, the researchers noted. Other limitations include the high interannual variability of KD and the inclusion of 2021 rebound data from the San Diego region only.
“Although our original hypothesis was that shelter-in-place measures would track with reduced KD cases, this was not borne out by the San Diego region data. Instead, the San Diego case occurrence data suggest that exposures that triggered KD were more likely to occur in the home, with a shift toward households with higher SES during the pandemic,” the researchers noted. However, “The results presented here are consistent with a respiratory portal of entry for the trigger(s) of KD,” they said.
Study fails to validate its conclusions
“This study attempts to test the hypothesis that various social restrictions were associated with a decrease in rate of diagnosed Kawasaki disease cases during portions of the SARS-CoV-2 pandemic,” Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, said in an interview.
“However, it appears that it fails to achieve this conclusion and I disagree with the findings,” said Dr. Gorelik, who was not involved in the study but served as first author on an updated Kawasaki disease treatment guideline published earlier this spring in Arthritis & Rheumatology.
“The study does not find statistically significant associations either with shelter in place orders or with cell phone mobility data, as stated in the conclusion, directly contradicting its own claim,” Dr. Gorelik said. “Secondly, the study makes an assumption that various methods, especially the wearing of masks by children and school closures, had a significant effect on the spread of respiratory viruses. There are no prospective, population based, controlled real world studies that validate this claim, and two prospective controlled real-world studies that dispute this,” he emphasized. “Cloth masks and surgical masks, which were the types of masks worn by school students, are also known to have a nonsignificant and paltry – in the latter, certainly less than 50%, and perhaps as little as 10% – effect on the reduction of respiratory viral spread,” he added.
“Mechanistic studies on mask wearing may suggest some mask efficacy, but these studies are as valid as mechanistic studies showing the effect of various antifungal pharmaceuticals on the replication of SARS-CoV-2 virus in culture, meaning only valid as hypothesis generating, and ultimately the latter hypothesis failed to bear out,” Dr. Gorelik explained. “We do not know the reason why other respiratory viruses and non-SARS-CoV-2 coronaviruses declined during the pandemic, but we do know that despite this, the SARS-CoV-2 coronavirus itself did not appear to suffer the same fate. Thus, it is very possible that another factor was at work, and we know that during other viral pandemics, typically circulating viruses decline, potentially due to induction of interferon responses in hosts, in a general effect known as ‘viral interference,’ ” he said.
“Overall, we must have robust evidence to support benefits of hypotheses that have demonstrated clear damage to children during this pandemic (such as school closures), and this study fails to live up to that requirement,” Dr. Gorelik said.
The study was supported by the Gordon and Marilyn Macklin Foundation and the Patient-Centered Outcomes Research Institute. Dr. Burney and Dr. Gorelik had no financial conflicts to disclose.
The social behavior associated with the COVID-19 pandemic may have reduced the incidence of Kawasaki disease, according to results of a cohort study of nearly 4,000 children.
The incidence of Kawasaki disease in the United States declined by 28.2% between 2018 and 2020, possibly as a result of factors including school closures, mask mandates, and reduced ambient pollution that might reduce exposure to Kawasaki disease (KD) in the environment, but a potential association has not been explored, wrote Jennifer A. Burney, PhD, of the University of California, San Diego, and colleagues.
KD received greater attention in the public and medical communities because of the emergence of multisystem inflammatory syndrome in children (MIS-C), which is similar to, but distinct from, KD, and because of the noticeable drop in KD cases during the pandemic, the researchers said.
In a multicenter cohort study published in JAMA Network Open , the researchers reviewed data from 2,461 consecutive patients with KD who were diagnosed between Jan. 1, 2018, and Dec. 31, 2020. They conducted a detailed analysis of analysis of 1,461 children with KD who were diagnosed between Jan. 1, 2002, and Nov. 15, 2021, at Rady Children’s Hospital San Diego (RCHSD), using data from before, during, and after the height of the pandemic. The median age of the children in the RCHSD analysis was 2.8 years, 62% were male, and 35% were Hispanic.
Overall, the prevalence of KD declined from 894 in 2018 to 646 in 2020, across the United States, but the decline was uneven, the researchers noted.
In the RCHSD cohort in San Diego, KD cases in children aged 1-5 years decreased significantly from 2020 to 2021 compared to the mean number of cases in previous years (22 vs. 44.9, P = .02). KD cases also decreased significantly among males and Asian children.
Notably, the occurrence of the KD clinical features of strawberry tongue, enlarged cervical lymph node, and subacute periungual desquamation decreased during 2020 compared with the baseline period, although only strawberry tongue reached statistical significance (39% vs. 63%, P = .04). The prevalence of patients with an enlarged lymph node was 21% in 2020 vs. 32% prior to the pandemic (P = .09); the prevalence of periungual desquamation during these periods was 47% vs. 58%, P = .16).
The researchers also used data from Census Block Groups (CBGs) to assess the impact of mobility metrics and environmental exposures on KD during the pandemic for the San Diego patient cohort. They found that KD cases during the pandemic were more likely to occur in neighborhoods of higher socioeconomic status, and that neighborhoods with lower levels of nitrous oxides had fewer KD cases.
Overall, “The reduction in KD case numbers coincided with masking, school closures, reduced circulation of respiratory viruses, and reduced air pollution,” the researchers wrote in their discussion of the findings. “A rebound in KD case numbers to prepandemic levels coincided with the lifting of mask mandates and, subsequently, the return to in-person schooling,” they wrote.
The study findings were limited by several factors including the small sample sizes, which also limit the interpretation of mobility and pollution data, the researchers noted. Other limitations include the high interannual variability of KD and the inclusion of 2021 rebound data from the San Diego region only.
“Although our original hypothesis was that shelter-in-place measures would track with reduced KD cases, this was not borne out by the San Diego region data. Instead, the San Diego case occurrence data suggest that exposures that triggered KD were more likely to occur in the home, with a shift toward households with higher SES during the pandemic,” the researchers noted. However, “The results presented here are consistent with a respiratory portal of entry for the trigger(s) of KD,” they said.
Study fails to validate its conclusions
“This study attempts to test the hypothesis that various social restrictions were associated with a decrease in rate of diagnosed Kawasaki disease cases during portions of the SARS-CoV-2 pandemic,” Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, said in an interview.
“However, it appears that it fails to achieve this conclusion and I disagree with the findings,” said Dr. Gorelik, who was not involved in the study but served as first author on an updated Kawasaki disease treatment guideline published earlier this spring in Arthritis & Rheumatology.
“The study does not find statistically significant associations either with shelter in place orders or with cell phone mobility data, as stated in the conclusion, directly contradicting its own claim,” Dr. Gorelik said. “Secondly, the study makes an assumption that various methods, especially the wearing of masks by children and school closures, had a significant effect on the spread of respiratory viruses. There are no prospective, population based, controlled real world studies that validate this claim, and two prospective controlled real-world studies that dispute this,” he emphasized. “Cloth masks and surgical masks, which were the types of masks worn by school students, are also known to have a nonsignificant and paltry – in the latter, certainly less than 50%, and perhaps as little as 10% – effect on the reduction of respiratory viral spread,” he added.
“Mechanistic studies on mask wearing may suggest some mask efficacy, but these studies are as valid as mechanistic studies showing the effect of various antifungal pharmaceuticals on the replication of SARS-CoV-2 virus in culture, meaning only valid as hypothesis generating, and ultimately the latter hypothesis failed to bear out,” Dr. Gorelik explained. “We do not know the reason why other respiratory viruses and non-SARS-CoV-2 coronaviruses declined during the pandemic, but we do know that despite this, the SARS-CoV-2 coronavirus itself did not appear to suffer the same fate. Thus, it is very possible that another factor was at work, and we know that during other viral pandemics, typically circulating viruses decline, potentially due to induction of interferon responses in hosts, in a general effect known as ‘viral interference,’ ” he said.
“Overall, we must have robust evidence to support benefits of hypotheses that have demonstrated clear damage to children during this pandemic (such as school closures), and this study fails to live up to that requirement,” Dr. Gorelik said.
The study was supported by the Gordon and Marilyn Macklin Foundation and the Patient-Centered Outcomes Research Institute. Dr. Burney and Dr. Gorelik had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Remnant cholesterol improves CV risk prediction
, a new study suggests.
The study, which followed almost 42,000 Danish individuals without a history of ischemic cardiovascular disease, diabetes, or statin use for more than 10 years, found that elevated remnant cholesterol appropriately reclassified up to 40% of those who later experienced myocardial infarction and ischemic heart disease.
“The clinical implications of our study include that doctors and patients should be aware of remnant cholesterol levels to prevent future risk of MI and ischemic heart disease,” the authors conclude.
They suggest that the development of a cardiovascular risk algorithm, including remnant cholesterol together with LDL cholesterol, would help to better identify high-risk individuals who could be candidates for statins in a primary prevention setting.
They note that physicians are encouraged to evaluate non-HDL cholesterol and/or apolipoprotein B rather than LDL cholesterol and certainly not yet remnant cholesterol, possibly because of the limited availability of remnant cholesterol values in some parts of the world.
However, they point out that remnant cholesterol can be calculated with a standard lipid profile without additional cost, which is currently already the standard procedure in the greater Copenhagen area.
“This means that the use of remnant cholesterol is easy to introduce into daily clinical practice,” they say.
The study was published online in the Journal of the American College of Cardiology.
The authors, Takahito Doi, MD, Anne Langsted, MD, and Børge Nordestgaard, from Copenhagen University Hospital, Denmark, explain that remnant cholesterol is total cholesterol minus LDL-cholesterol minus HDL-cholesterol and includes the cholesterol content of the triglyceride-rich very-low-density lipoproteins, intermediate-density lipoproteins, and chylomicron remnants in the nonfasting state.
“When these particles enter the arterial wall, they are taken up by macrophages to produce foam cells, and therefore elevated remnant cholesterol likely enhance accumulation of cholesterol in the arterial wall, leading to progression of atherosclerosis and in consequence ischemic heart disease,” they note.
They point out that most guidelines for assessment of the 10-year risk of ischemic heart and atherosclerotic cardiovascular disease include levels of total and HDL cholesterol, but remnant cholesterol levels are not included.
They conducted the current study to investigate whether elevated remnant cholesterol would lead to appropriate reclassification of individuals who later experienced MI or ischemic heart disease.
The researchers analyzed data from the Copenhagen General Population Study, which recruited individuals from the White Danish general population from 2003-2015 and followed them until 2018. Information on lifestyle, health, and medication, including statin therapy, was obtained through a questionnaire, and participants underwent physical examinations and had nonfasting blood samples drawn for biochemical measurements.
For the current study, they included 41,928 individuals aged 40-100 years enrolled before 2009 without a history of ischemic cardiovascular disease, diabetes, and statin use at baseline. The median follow-up time was 12 years. Information on diagnoses of MI and ischemic heart disease was collected from the national Danish Causes of Death Registry and all hospital admissions and diagnoses entered in the national Danish Patient Registry.
During the first 10 years of follow-up there were 1,063 MIs and 1,460 ischemic heart disease events (death of ischemic heart disease, nonfatal MI, and coronary revascularization).
Results showed that in models based on conventional risk factors estimating risk of heart disease of above or below 5% in 10 years, adding remnant cholesterol at levels above the 95th percentile, appropriately reclassified 23% of individuals who had an MI and 21% of individuals who had an ischemic heart disease event.
Using remnant cholesterol levels above the 75th percentile appropriately reclassified 10% of those who had an MI and 8% of those who had an ischemic heart disease event. No events were reclassified incorrectly.
Using measurements of remnant cholesterol also improved reclassification of individuals with heart disease risk above or below 7.5% or 10% in 10 years.
When reclassifications were combined from below to above 5%, 7.5%, and 10% risk of events, 42% of individuals with MI and 41% with ischemic heart disease events were reclassified appropriately.
In an editorial accompanying publication of the study in JACC, Peter Wilson, MD, Emory University School of Medicine, Atlanta, and Alan Remaley, MD, National Heart, Lung, and Blood Institute, say these findings rekindle interest in atherogenic nonfasting lipid measurements and emphasize an important role for elevated nonfasting remnant cholesterol as a value-added predictor of ischemic events.
The editorialists note that both fasting and nonfasting lipid values provide useful information for atherosclerotic cardiovascular disease (ASCVD) risk estimation, and elevated nonfasting remnant cholesterol appears to help identify persons at greater risk for an initial cardiovascular ischemic event.
They add that very elevated levels (above the 75th percentile) of nonfasting remnant cholesterol deserve further evaluation as a potentially valuable “modifier of ASCVD risk,” and replication of the results could move these findings forward to potentially improve prognostication and care for patients at risk for ischemic heart disease events.
An indirect measure of triglycerides
Dr. Wilson explained that remnant cholesterol is an indirect measure of triglycerides beyond LDL levels, and it is thus including a new lipid measurement in risk prediction.
“We are completely focused on LDL cholesterol,” he said. “This opens it up a bit by adding in another measure that takes into account triglycerides as well as LDL.”
He also pointed out that use of a nonfasting sample is another advantage of measuring remnant cholesterol.
“An accurate measure of LDL needs a fasting sample, which is a nuisance, whereas remnant cholesterol can be measured in a nonfasting blood sample, so it is more convenient,” Dr. Wilson said.
While this study shows this measure is helpful for risk prediction in the primary prevention population, Dr. Wilson believes remnant cholesterol could be most useful in helping to guide further medication choice in patients who are already taking statins.
“Statins mainly target LDL, but if we can also measure nonfasting triglycerides this will be helpful. It may help us select some patients who may need a different type of drug to use in addition to statins that lowers triglycerides,” he said.
This work was supported by the Global Excellence Programme, the Research Fund for the Capital Region of Denmark, the Japanese College of Cardiology Overseas Research Fellowship, and the Scandinavia Japan Sasakawa Foundation. Mr. Nordestgaard has reported consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Amarin, Kowa, Denka, Novartis, Novo Nordisk, Esperion, and Silence Therapeutics. Dr. Doi has reported talks sponsored by MSD.
A version of this article first appeared on Medscape.com.
, a new study suggests.
The study, which followed almost 42,000 Danish individuals without a history of ischemic cardiovascular disease, diabetes, or statin use for more than 10 years, found that elevated remnant cholesterol appropriately reclassified up to 40% of those who later experienced myocardial infarction and ischemic heart disease.
“The clinical implications of our study include that doctors and patients should be aware of remnant cholesterol levels to prevent future risk of MI and ischemic heart disease,” the authors conclude.
They suggest that the development of a cardiovascular risk algorithm, including remnant cholesterol together with LDL cholesterol, would help to better identify high-risk individuals who could be candidates for statins in a primary prevention setting.
They note that physicians are encouraged to evaluate non-HDL cholesterol and/or apolipoprotein B rather than LDL cholesterol and certainly not yet remnant cholesterol, possibly because of the limited availability of remnant cholesterol values in some parts of the world.
However, they point out that remnant cholesterol can be calculated with a standard lipid profile without additional cost, which is currently already the standard procedure in the greater Copenhagen area.
“This means that the use of remnant cholesterol is easy to introduce into daily clinical practice,” they say.
The study was published online in the Journal of the American College of Cardiology.
The authors, Takahito Doi, MD, Anne Langsted, MD, and Børge Nordestgaard, from Copenhagen University Hospital, Denmark, explain that remnant cholesterol is total cholesterol minus LDL-cholesterol minus HDL-cholesterol and includes the cholesterol content of the triglyceride-rich very-low-density lipoproteins, intermediate-density lipoproteins, and chylomicron remnants in the nonfasting state.
“When these particles enter the arterial wall, they are taken up by macrophages to produce foam cells, and therefore elevated remnant cholesterol likely enhance accumulation of cholesterol in the arterial wall, leading to progression of atherosclerosis and in consequence ischemic heart disease,” they note.
They point out that most guidelines for assessment of the 10-year risk of ischemic heart and atherosclerotic cardiovascular disease include levels of total and HDL cholesterol, but remnant cholesterol levels are not included.
They conducted the current study to investigate whether elevated remnant cholesterol would lead to appropriate reclassification of individuals who later experienced MI or ischemic heart disease.
The researchers analyzed data from the Copenhagen General Population Study, which recruited individuals from the White Danish general population from 2003-2015 and followed them until 2018. Information on lifestyle, health, and medication, including statin therapy, was obtained through a questionnaire, and participants underwent physical examinations and had nonfasting blood samples drawn for biochemical measurements.
For the current study, they included 41,928 individuals aged 40-100 years enrolled before 2009 without a history of ischemic cardiovascular disease, diabetes, and statin use at baseline. The median follow-up time was 12 years. Information on diagnoses of MI and ischemic heart disease was collected from the national Danish Causes of Death Registry and all hospital admissions and diagnoses entered in the national Danish Patient Registry.
During the first 10 years of follow-up there were 1,063 MIs and 1,460 ischemic heart disease events (death of ischemic heart disease, nonfatal MI, and coronary revascularization).
Results showed that in models based on conventional risk factors estimating risk of heart disease of above or below 5% in 10 years, adding remnant cholesterol at levels above the 95th percentile, appropriately reclassified 23% of individuals who had an MI and 21% of individuals who had an ischemic heart disease event.
Using remnant cholesterol levels above the 75th percentile appropriately reclassified 10% of those who had an MI and 8% of those who had an ischemic heart disease event. No events were reclassified incorrectly.
Using measurements of remnant cholesterol also improved reclassification of individuals with heart disease risk above or below 7.5% or 10% in 10 years.
When reclassifications were combined from below to above 5%, 7.5%, and 10% risk of events, 42% of individuals with MI and 41% with ischemic heart disease events were reclassified appropriately.
In an editorial accompanying publication of the study in JACC, Peter Wilson, MD, Emory University School of Medicine, Atlanta, and Alan Remaley, MD, National Heart, Lung, and Blood Institute, say these findings rekindle interest in atherogenic nonfasting lipid measurements and emphasize an important role for elevated nonfasting remnant cholesterol as a value-added predictor of ischemic events.
The editorialists note that both fasting and nonfasting lipid values provide useful information for atherosclerotic cardiovascular disease (ASCVD) risk estimation, and elevated nonfasting remnant cholesterol appears to help identify persons at greater risk for an initial cardiovascular ischemic event.
They add that very elevated levels (above the 75th percentile) of nonfasting remnant cholesterol deserve further evaluation as a potentially valuable “modifier of ASCVD risk,” and replication of the results could move these findings forward to potentially improve prognostication and care for patients at risk for ischemic heart disease events.
An indirect measure of triglycerides
Dr. Wilson explained that remnant cholesterol is an indirect measure of triglycerides beyond LDL levels, and it is thus including a new lipid measurement in risk prediction.
“We are completely focused on LDL cholesterol,” he said. “This opens it up a bit by adding in another measure that takes into account triglycerides as well as LDL.”
He also pointed out that use of a nonfasting sample is another advantage of measuring remnant cholesterol.
“An accurate measure of LDL needs a fasting sample, which is a nuisance, whereas remnant cholesterol can be measured in a nonfasting blood sample, so it is more convenient,” Dr. Wilson said.
While this study shows this measure is helpful for risk prediction in the primary prevention population, Dr. Wilson believes remnant cholesterol could be most useful in helping to guide further medication choice in patients who are already taking statins.
“Statins mainly target LDL, but if we can also measure nonfasting triglycerides this will be helpful. It may help us select some patients who may need a different type of drug to use in addition to statins that lowers triglycerides,” he said.
This work was supported by the Global Excellence Programme, the Research Fund for the Capital Region of Denmark, the Japanese College of Cardiology Overseas Research Fellowship, and the Scandinavia Japan Sasakawa Foundation. Mr. Nordestgaard has reported consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Amarin, Kowa, Denka, Novartis, Novo Nordisk, Esperion, and Silence Therapeutics. Dr. Doi has reported talks sponsored by MSD.
A version of this article first appeared on Medscape.com.
, a new study suggests.
The study, which followed almost 42,000 Danish individuals without a history of ischemic cardiovascular disease, diabetes, or statin use for more than 10 years, found that elevated remnant cholesterol appropriately reclassified up to 40% of those who later experienced myocardial infarction and ischemic heart disease.
“The clinical implications of our study include that doctors and patients should be aware of remnant cholesterol levels to prevent future risk of MI and ischemic heart disease,” the authors conclude.
They suggest that the development of a cardiovascular risk algorithm, including remnant cholesterol together with LDL cholesterol, would help to better identify high-risk individuals who could be candidates for statins in a primary prevention setting.
They note that physicians are encouraged to evaluate non-HDL cholesterol and/or apolipoprotein B rather than LDL cholesterol and certainly not yet remnant cholesterol, possibly because of the limited availability of remnant cholesterol values in some parts of the world.
However, they point out that remnant cholesterol can be calculated with a standard lipid profile without additional cost, which is currently already the standard procedure in the greater Copenhagen area.
“This means that the use of remnant cholesterol is easy to introduce into daily clinical practice,” they say.
The study was published online in the Journal of the American College of Cardiology.
The authors, Takahito Doi, MD, Anne Langsted, MD, and Børge Nordestgaard, from Copenhagen University Hospital, Denmark, explain that remnant cholesterol is total cholesterol minus LDL-cholesterol minus HDL-cholesterol and includes the cholesterol content of the triglyceride-rich very-low-density lipoproteins, intermediate-density lipoproteins, and chylomicron remnants in the nonfasting state.
“When these particles enter the arterial wall, they are taken up by macrophages to produce foam cells, and therefore elevated remnant cholesterol likely enhance accumulation of cholesterol in the arterial wall, leading to progression of atherosclerosis and in consequence ischemic heart disease,” they note.
They point out that most guidelines for assessment of the 10-year risk of ischemic heart and atherosclerotic cardiovascular disease include levels of total and HDL cholesterol, but remnant cholesterol levels are not included.
They conducted the current study to investigate whether elevated remnant cholesterol would lead to appropriate reclassification of individuals who later experienced MI or ischemic heart disease.
The researchers analyzed data from the Copenhagen General Population Study, which recruited individuals from the White Danish general population from 2003-2015 and followed them until 2018. Information on lifestyle, health, and medication, including statin therapy, was obtained through a questionnaire, and participants underwent physical examinations and had nonfasting blood samples drawn for biochemical measurements.
For the current study, they included 41,928 individuals aged 40-100 years enrolled before 2009 without a history of ischemic cardiovascular disease, diabetes, and statin use at baseline. The median follow-up time was 12 years. Information on diagnoses of MI and ischemic heart disease was collected from the national Danish Causes of Death Registry and all hospital admissions and diagnoses entered in the national Danish Patient Registry.
During the first 10 years of follow-up there were 1,063 MIs and 1,460 ischemic heart disease events (death of ischemic heart disease, nonfatal MI, and coronary revascularization).
Results showed that in models based on conventional risk factors estimating risk of heart disease of above or below 5% in 10 years, adding remnant cholesterol at levels above the 95th percentile, appropriately reclassified 23% of individuals who had an MI and 21% of individuals who had an ischemic heart disease event.
Using remnant cholesterol levels above the 75th percentile appropriately reclassified 10% of those who had an MI and 8% of those who had an ischemic heart disease event. No events were reclassified incorrectly.
Using measurements of remnant cholesterol also improved reclassification of individuals with heart disease risk above or below 7.5% or 10% in 10 years.
When reclassifications were combined from below to above 5%, 7.5%, and 10% risk of events, 42% of individuals with MI and 41% with ischemic heart disease events were reclassified appropriately.
In an editorial accompanying publication of the study in JACC, Peter Wilson, MD, Emory University School of Medicine, Atlanta, and Alan Remaley, MD, National Heart, Lung, and Blood Institute, say these findings rekindle interest in atherogenic nonfasting lipid measurements and emphasize an important role for elevated nonfasting remnant cholesterol as a value-added predictor of ischemic events.
The editorialists note that both fasting and nonfasting lipid values provide useful information for atherosclerotic cardiovascular disease (ASCVD) risk estimation, and elevated nonfasting remnant cholesterol appears to help identify persons at greater risk for an initial cardiovascular ischemic event.
They add that very elevated levels (above the 75th percentile) of nonfasting remnant cholesterol deserve further evaluation as a potentially valuable “modifier of ASCVD risk,” and replication of the results could move these findings forward to potentially improve prognostication and care for patients at risk for ischemic heart disease events.
An indirect measure of triglycerides
Dr. Wilson explained that remnant cholesterol is an indirect measure of triglycerides beyond LDL levels, and it is thus including a new lipid measurement in risk prediction.
“We are completely focused on LDL cholesterol,” he said. “This opens it up a bit by adding in another measure that takes into account triglycerides as well as LDL.”
He also pointed out that use of a nonfasting sample is another advantage of measuring remnant cholesterol.
“An accurate measure of LDL needs a fasting sample, which is a nuisance, whereas remnant cholesterol can be measured in a nonfasting blood sample, so it is more convenient,” Dr. Wilson said.
While this study shows this measure is helpful for risk prediction in the primary prevention population, Dr. Wilson believes remnant cholesterol could be most useful in helping to guide further medication choice in patients who are already taking statins.
“Statins mainly target LDL, but if we can also measure nonfasting triglycerides this will be helpful. It may help us select some patients who may need a different type of drug to use in addition to statins that lowers triglycerides,” he said.
This work was supported by the Global Excellence Programme, the Research Fund for the Capital Region of Denmark, the Japanese College of Cardiology Overseas Research Fellowship, and the Scandinavia Japan Sasakawa Foundation. Mr. Nordestgaard has reported consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amgen, Amarin, Kowa, Denka, Novartis, Novo Nordisk, Esperion, and Silence Therapeutics. Dr. Doi has reported talks sponsored by MSD.
A version of this article first appeared on Medscape.com.
FDA approves setmelanotide for obesity in Bardet-Biedl syndrome
The Food and Drug Administration has approved a supplemental indication for setmelanotide (Imcivree, Rhythm Pharmaceuticals) injection for chronic weight management in adults and pediatric patients age 6 and older with obesity due to Bardet-Biedl Syndrome (BBS).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for BBS, a rare genetic disorder that impairs a hunger signal along the melanocortin-4 receptor (MC4R) pathway.
BBS affects an estimated 1,500-2,500 people in the United States.
Individuals with BBS typically have obesity that starts at age 1 along with insatiable hunger (hyperphagia). Available weight management options are generally unsuccessful.
Other symptoms may include retinal degeneration, reduced kidney function, or extra digits of the hands or feet.
Setmelanotide received priority review, orphan drug designation, and breakthrough designation for this new indication.
As previously reported, in November 2020, the FDA approved setmelanotide for weight management in adults and children as young as 6 years with obesity due to proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing – who also have impaired hunger signaling from the brain.
These individuals have a normal weight at birth but develop persistent, severe obesity within months due to hyperphagia.
The FDA approval of Imcivree for BBS “represents a significant milestone for Rhythm [Pharmaceuticals], validating our strategy of developing Imcivree for people with hyperphagia and severe obesity caused by rare MC4R-pathway diseases and allowing us to provide our precision therapy to an established community of patients living with BBS and their families who are eagerly awaiting a new treatment option,” said David Meeker, MD, chair, president and CEO of Rhythm, in a press release.
Safety, effectiveness in 66-week trial in 44 patients
The safety and effectiveness of setmelanotidewas evaluated in a 66-week phase 3 clinical trial that enrolled 44 patients age 6 and older who had a diagnosis of BBS and obesity – defined as a body mass index greater than or equal to 30 kg/m2 or greater than or equal to 97th percentile for pediatric patients.
After an initial 14-week, randomized, double-blind, placebo-controlled treatment period, patients entered a 52-week, open-label period.
The trial met its primary endpoint and all key secondary endpoints, with statistically significant reductions in weight and hunger at 52 weeks on therapy.
- After 52 weeks of treatment, patients taking setmelanotide lost, on average, 7.9% of their initial BMI.
- 61% of patients lost 5% or more of their initial BMI, and 39% lost 10% or more of their initial BMI.
- In the 14-week, placebo-controlled treatment, on average, BMI dropped by 4.6% in the 22 patients treated with the study drug and dropped 0.1% in the 22 patients treated with placebo.
- At 52 weeks, the 14 patients aged 12 and older who were able to self-report their hunger had a significant –2.1 mean change in hunger score.
Setmelanotide is associated with the following warnings and precautions:
- Spontaneous penile erections in males and sexual adverse reactions in females. Instruct males with erection lasting longer than 4 hours to seek emergency medical attention.
- Depression and suicidal ideation. Monitor patients for new onset or worsening depression or suicidal thoughts or behaviors. Consider discontinuing the drug if patients have suicidal thoughts or behaviors or clinically significant or persistent depression symptoms.
- Skin pigmentation and darkening of preexisting nevi (moles). Examine skin before and during treatment.
- Setmelanotide is not approved for use in neonates or infants. Serious and fatal adverse reactions including “gasping syndrome” can occur in neonates and low-birth-weight infants treated with benzyl alcohol-preserved drugs.
The most common adverse reactions (with an incidence greater than or equal to 20%) included skin hyperpigmentation, injection site reactions, nausea, headache, diarrhea, abdominal pain, vomiting, depression, and spontaneous penile erection.
The FDA did not approve the company’s supplemental new drug application for setmelanotide in Alström syndrome.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a supplemental indication for setmelanotide (Imcivree, Rhythm Pharmaceuticals) injection for chronic weight management in adults and pediatric patients age 6 and older with obesity due to Bardet-Biedl Syndrome (BBS).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for BBS, a rare genetic disorder that impairs a hunger signal along the melanocortin-4 receptor (MC4R) pathway.
BBS affects an estimated 1,500-2,500 people in the United States.
Individuals with BBS typically have obesity that starts at age 1 along with insatiable hunger (hyperphagia). Available weight management options are generally unsuccessful.
Other symptoms may include retinal degeneration, reduced kidney function, or extra digits of the hands or feet.
Setmelanotide received priority review, orphan drug designation, and breakthrough designation for this new indication.
As previously reported, in November 2020, the FDA approved setmelanotide for weight management in adults and children as young as 6 years with obesity due to proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing – who also have impaired hunger signaling from the brain.
These individuals have a normal weight at birth but develop persistent, severe obesity within months due to hyperphagia.
The FDA approval of Imcivree for BBS “represents a significant milestone for Rhythm [Pharmaceuticals], validating our strategy of developing Imcivree for people with hyperphagia and severe obesity caused by rare MC4R-pathway diseases and allowing us to provide our precision therapy to an established community of patients living with BBS and their families who are eagerly awaiting a new treatment option,” said David Meeker, MD, chair, president and CEO of Rhythm, in a press release.
Safety, effectiveness in 66-week trial in 44 patients
The safety and effectiveness of setmelanotidewas evaluated in a 66-week phase 3 clinical trial that enrolled 44 patients age 6 and older who had a diagnosis of BBS and obesity – defined as a body mass index greater than or equal to 30 kg/m2 or greater than or equal to 97th percentile for pediatric patients.
After an initial 14-week, randomized, double-blind, placebo-controlled treatment period, patients entered a 52-week, open-label period.
The trial met its primary endpoint and all key secondary endpoints, with statistically significant reductions in weight and hunger at 52 weeks on therapy.
- After 52 weeks of treatment, patients taking setmelanotide lost, on average, 7.9% of their initial BMI.
- 61% of patients lost 5% or more of their initial BMI, and 39% lost 10% or more of their initial BMI.
- In the 14-week, placebo-controlled treatment, on average, BMI dropped by 4.6% in the 22 patients treated with the study drug and dropped 0.1% in the 22 patients treated with placebo.
- At 52 weeks, the 14 patients aged 12 and older who were able to self-report their hunger had a significant –2.1 mean change in hunger score.
Setmelanotide is associated with the following warnings and precautions:
- Spontaneous penile erections in males and sexual adverse reactions in females. Instruct males with erection lasting longer than 4 hours to seek emergency medical attention.
- Depression and suicidal ideation. Monitor patients for new onset or worsening depression or suicidal thoughts or behaviors. Consider discontinuing the drug if patients have suicidal thoughts or behaviors or clinically significant or persistent depression symptoms.
- Skin pigmentation and darkening of preexisting nevi (moles). Examine skin before and during treatment.
- Setmelanotide is not approved for use in neonates or infants. Serious and fatal adverse reactions including “gasping syndrome” can occur in neonates and low-birth-weight infants treated with benzyl alcohol-preserved drugs.
The most common adverse reactions (with an incidence greater than or equal to 20%) included skin hyperpigmentation, injection site reactions, nausea, headache, diarrhea, abdominal pain, vomiting, depression, and spontaneous penile erection.
The FDA did not approve the company’s supplemental new drug application for setmelanotide in Alström syndrome.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a supplemental indication for setmelanotide (Imcivree, Rhythm Pharmaceuticals) injection for chronic weight management in adults and pediatric patients age 6 and older with obesity due to Bardet-Biedl Syndrome (BBS).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for BBS, a rare genetic disorder that impairs a hunger signal along the melanocortin-4 receptor (MC4R) pathway.
BBS affects an estimated 1,500-2,500 people in the United States.
Individuals with BBS typically have obesity that starts at age 1 along with insatiable hunger (hyperphagia). Available weight management options are generally unsuccessful.
Other symptoms may include retinal degeneration, reduced kidney function, or extra digits of the hands or feet.
Setmelanotide received priority review, orphan drug designation, and breakthrough designation for this new indication.
As previously reported, in November 2020, the FDA approved setmelanotide for weight management in adults and children as young as 6 years with obesity due to proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing – who also have impaired hunger signaling from the brain.
These individuals have a normal weight at birth but develop persistent, severe obesity within months due to hyperphagia.
The FDA approval of Imcivree for BBS “represents a significant milestone for Rhythm [Pharmaceuticals], validating our strategy of developing Imcivree for people with hyperphagia and severe obesity caused by rare MC4R-pathway diseases and allowing us to provide our precision therapy to an established community of patients living with BBS and their families who are eagerly awaiting a new treatment option,” said David Meeker, MD, chair, president and CEO of Rhythm, in a press release.
Safety, effectiveness in 66-week trial in 44 patients
The safety and effectiveness of setmelanotidewas evaluated in a 66-week phase 3 clinical trial that enrolled 44 patients age 6 and older who had a diagnosis of BBS and obesity – defined as a body mass index greater than or equal to 30 kg/m2 or greater than or equal to 97th percentile for pediatric patients.
After an initial 14-week, randomized, double-blind, placebo-controlled treatment period, patients entered a 52-week, open-label period.
The trial met its primary endpoint and all key secondary endpoints, with statistically significant reductions in weight and hunger at 52 weeks on therapy.
- After 52 weeks of treatment, patients taking setmelanotide lost, on average, 7.9% of their initial BMI.
- 61% of patients lost 5% or more of their initial BMI, and 39% lost 10% or more of their initial BMI.
- In the 14-week, placebo-controlled treatment, on average, BMI dropped by 4.6% in the 22 patients treated with the study drug and dropped 0.1% in the 22 patients treated with placebo.
- At 52 weeks, the 14 patients aged 12 and older who were able to self-report their hunger had a significant –2.1 mean change in hunger score.
Setmelanotide is associated with the following warnings and precautions:
- Spontaneous penile erections in males and sexual adverse reactions in females. Instruct males with erection lasting longer than 4 hours to seek emergency medical attention.
- Depression and suicidal ideation. Monitor patients for new onset or worsening depression or suicidal thoughts or behaviors. Consider discontinuing the drug if patients have suicidal thoughts or behaviors or clinically significant or persistent depression symptoms.
- Skin pigmentation and darkening of preexisting nevi (moles). Examine skin before and during treatment.
- Setmelanotide is not approved for use in neonates or infants. Serious and fatal adverse reactions including “gasping syndrome” can occur in neonates and low-birth-weight infants treated with benzyl alcohol-preserved drugs.
The most common adverse reactions (with an incidence greater than or equal to 20%) included skin hyperpigmentation, injection site reactions, nausea, headache, diarrhea, abdominal pain, vomiting, depression, and spontaneous penile erection.
The FDA did not approve the company’s supplemental new drug application for setmelanotide in Alström syndrome.
A version of this article first appeared on Medscape.com.
Meta-analysis points to safety of acetylcholine coronary testing
Provocation testing with intracoronary acetylcholine is safe, particularly among Western patients, suggests a large systematic review that underscores the importance of functional coronary angiography to diagnose epicardial or microvascular spasm.
The results, derived from more than 12,000 patients in 16 studies, showed a 0.5% risk of major complications, defined as death, ventricular tachycardia/ventricular fibrillation, myocardial infarction, and shock requiring resuscitation.
Ventricular tachycardia/fibrillation were the most common events and mainly reported from two Japanese studies. There were no deaths.
Exploratory subgroup analyses revealed significantly fewer major complications in Western populations (0.0%; P for heterogeneity = .938), compared with Asian populations (2.3%; P for heterogeneity < .001).
The pooled positive vasospasm rate was also lower in Western versus Asian studies (37.9% vs. 50.7%; P for between-group heterogeneity = .010), as reported by the Microvascular Network in the Journal of the American College of Cardiology.
“If you look at the data between Asian studies versus others, mainly European or U.S. studies, primarily in Caucasian populations, it’s like zero percent history of major complications. So, it sounds extremely safe to do this testing in Caucasian populations,” Yuhei Kobayashi, MD, NewYork-Presbyterian Brooklyn Methodist Hospital, Weill Cornell Medicine, said.
Safety will need to be assessed in African Americans and other racial/ethnic groups, but “it makes us think we should end up testing more in the United States,” he told this news organization.
Intracoronary acetylcholine testing is daily practice in Japan but is limited in the United States and Europe to a few specialized centers due to safety concerns. Three deaths were reported in 1980 with intravenous ergonovine testing, whereas the safety of acetylcholine protocols has been studied largely in single-center retrospective studies, typically in Asian populations.
Growing recognition of myocardial infarction with nonobstructive coronary arteries (MINOCA) and ischemia with no obstructive coronary arteries (INOCA), however, is changing the landscape. In recent U.S. and European guidelines, intracoronary acetylcholine testing is indicated as a class 2a recommendation in MINOCA/INOCA.
“More and more institutions in Europe and the United States are starting to do acetylcholine testing, because now we know that chest pain isn’t necessarily coming from the blocked arteries,” Dr. Kobayashi said. “There are functional abnormalities, including coronary spasm, and if we diagnose it, we have appropriate medical regimens for this kind of disease.”
First safety meta-analysis
The present review and meta-analysis included 12,585 participants in 16 studies through November 2021. Of these, 63% were conducted in Western countries, and most were prospective studies published over the past decade in patients with MINOCA or INOCA.
Ten studies used the contemporary diagnostic criteria for epicardial spasm of at least 90% reduction in coronary diameter. Acetylcholine was administered into the left coronary artery at up to 100 mcg and 200 mcg in seven and six studies, respectively, and was used in the other three studies to assess endothelial function with a slower infusion of up to 36.4 mcg.
Major complications were significantly higher in studies following the contemporary diagnostic cutoff than in those using a lower cutoff of at least 75% diameter reduction (1.0% vs. 0.0%; P for between-group heterogeneity < .001).
The incidence of major complications was 0.2% with the slower infusion of up to 36.4 mcg, 0.8% with a maximum dose of 100 mcg, and 0.3% with a maximum dose of 200 mcg. The positive vasospasm rate was similar with the latter two protocols, at 46.3% and 41.4%, respectively.
Minor complications occurred in 3.3% of patients but were not detailed. They can include paroxysmal atrial fibrillation, ventricular ectopic beats, transient hypotension, and bradycardia requiring intervention.
As with major complications, minor complications were lower in studies using noncontemporary versus contemporary diagnostic cutoffs for epicardial spasm (1.8% vs. 4.7%) and in Western versus Asian populations (2.6% vs. 9.4%). Minor complications were similar between protocols with maximum doses of 100 mcg and 200 mcg (3.6% vs. 3.8%).
Dr. Kobayashi suggested that several factors may explain the racial differences, including previously reported smooth muscle hyperresponsiveness to provocation stimuli in Japanese patients and the inclusion of a wide range of patients in Japanese studies, such as those with obstructive coronary disease.
Japanese studies also used sequential acetylcholine injection into both the right and left coronaries, a faster injection speed of 20 seconds, and upfront placement of a temporary pacing catheter in case of acetylcholine-induced bradycardia, particularly with right coronary injection.
Although the protocol is largely settled in Japan, he said, provocation protocols need to be standardized because “depending on the country and depending on the institution, people are doing totally different things.”
A big step forward
Commenting on the study, C. Noel Bairey Merz, MD, from Cedars Sinai, Los Angeles, said it has “widespread relevance” because half of all coronary angiograms done invasively in the United States for suspected ischemia find no obstructive coronary disease. Left untreated, however, MINOCA has a 2.5% annual event rate, and a quarter of that is death.
“This is a big step forward with likely equal opportunity to improve women and men’s ischemic heart disease,” she said.
On the other hand, all studies were conducted at centers of excellence, so safety will need to be carefully watched as testing rolls out to more community care, Dr. Merz said. “And it always needs to be underscored that this is done by an interventional cardiologist because they’re familiar with wires that can dissect arteries, and they’re familiar with minor complications that could turn into major, if someone didn’t act appropriately.”
Dr. Merz also called for unifying protocols and the need to raise awareness within the general cardiology community to ask interventionalists for acetylcholine spasm testing. Randomized controlled data from within the WISE study and the CorMica study showed that diagnostic certainty leads to greater therapeutic certainty. “You do a much better job about who and how to treat,” she said.
There are also three ongoing randomized controlled trials – WARRIOR, MINOCA-BAT, and iCorMica – in the INOCA and MINOCA populations testing different treatment strategies for hard clinical outcomes like death and myocardial infarction.
“So in addition to this publication being guideline-forming for diagnosis, we anticipate in the next several years to have clinical trial evidence about therapeutics, again, for formulation of class 1 guidelines,” Dr. Merz said.
John Beltrame, BMBS, PhD, University of Adelaide, Australia, said the meta-analysis shows that intracoronary acetylcholine spasm testing is safe and should prompt greater adoption of invasive functional angiography.
Interventionalists are quite happy to do fractional flow reserve using intravenous adenosine to assess coronary microvascular dysfunction, he said, and “what we think is that functional angiography should test both – both the spasm as well as the microvasculature – and that will give us a clear direction because the treatments are slightly different when you’re treating the large arteries as compared to the microscopic arteries. It’s an important thing.”
Dr. Beltrame and colleagues further detail the benefits of comprehensive invasive functional angiography over structural angiography in a related editorial.
He also noted that the Coronary Vasomotion Disorders International Study Group published international diagnostic criteria for microvascular angina and that several protocols for acetylcholine spasm testing are in the works, including one from Australia. Australian investigators are also organizing an accreditation program for those performing the test.
“The protocol itself is relatively straightforward, but it’s not merely picking up a manual and following the instructions,” Dr. Beltrame said. “Just the same as when you train someone in angioplasty, you don’t just go out and do it. You need to develop some experience in it and so should be proctored.”
Dr. Kobayashi reported consulting agreements with Abbott Vascular. Coauthor disclosures are listed in the paper. Dr. Beltrame and colleagues have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Provocation testing with intracoronary acetylcholine is safe, particularly among Western patients, suggests a large systematic review that underscores the importance of functional coronary angiography to diagnose epicardial or microvascular spasm.
The results, derived from more than 12,000 patients in 16 studies, showed a 0.5% risk of major complications, defined as death, ventricular tachycardia/ventricular fibrillation, myocardial infarction, and shock requiring resuscitation.
Ventricular tachycardia/fibrillation were the most common events and mainly reported from two Japanese studies. There were no deaths.
Exploratory subgroup analyses revealed significantly fewer major complications in Western populations (0.0%; P for heterogeneity = .938), compared with Asian populations (2.3%; P for heterogeneity < .001).
The pooled positive vasospasm rate was also lower in Western versus Asian studies (37.9% vs. 50.7%; P for between-group heterogeneity = .010), as reported by the Microvascular Network in the Journal of the American College of Cardiology.
“If you look at the data between Asian studies versus others, mainly European or U.S. studies, primarily in Caucasian populations, it’s like zero percent history of major complications. So, it sounds extremely safe to do this testing in Caucasian populations,” Yuhei Kobayashi, MD, NewYork-Presbyterian Brooklyn Methodist Hospital, Weill Cornell Medicine, said.
Safety will need to be assessed in African Americans and other racial/ethnic groups, but “it makes us think we should end up testing more in the United States,” he told this news organization.
Intracoronary acetylcholine testing is daily practice in Japan but is limited in the United States and Europe to a few specialized centers due to safety concerns. Three deaths were reported in 1980 with intravenous ergonovine testing, whereas the safety of acetylcholine protocols has been studied largely in single-center retrospective studies, typically in Asian populations.
Growing recognition of myocardial infarction with nonobstructive coronary arteries (MINOCA) and ischemia with no obstructive coronary arteries (INOCA), however, is changing the landscape. In recent U.S. and European guidelines, intracoronary acetylcholine testing is indicated as a class 2a recommendation in MINOCA/INOCA.
“More and more institutions in Europe and the United States are starting to do acetylcholine testing, because now we know that chest pain isn’t necessarily coming from the blocked arteries,” Dr. Kobayashi said. “There are functional abnormalities, including coronary spasm, and if we diagnose it, we have appropriate medical regimens for this kind of disease.”
First safety meta-analysis
The present review and meta-analysis included 12,585 participants in 16 studies through November 2021. Of these, 63% were conducted in Western countries, and most were prospective studies published over the past decade in patients with MINOCA or INOCA.
Ten studies used the contemporary diagnostic criteria for epicardial spasm of at least 90% reduction in coronary diameter. Acetylcholine was administered into the left coronary artery at up to 100 mcg and 200 mcg in seven and six studies, respectively, and was used in the other three studies to assess endothelial function with a slower infusion of up to 36.4 mcg.
Major complications were significantly higher in studies following the contemporary diagnostic cutoff than in those using a lower cutoff of at least 75% diameter reduction (1.0% vs. 0.0%; P for between-group heterogeneity < .001).
The incidence of major complications was 0.2% with the slower infusion of up to 36.4 mcg, 0.8% with a maximum dose of 100 mcg, and 0.3% with a maximum dose of 200 mcg. The positive vasospasm rate was similar with the latter two protocols, at 46.3% and 41.4%, respectively.
Minor complications occurred in 3.3% of patients but were not detailed. They can include paroxysmal atrial fibrillation, ventricular ectopic beats, transient hypotension, and bradycardia requiring intervention.
As with major complications, minor complications were lower in studies using noncontemporary versus contemporary diagnostic cutoffs for epicardial spasm (1.8% vs. 4.7%) and in Western versus Asian populations (2.6% vs. 9.4%). Minor complications were similar between protocols with maximum doses of 100 mcg and 200 mcg (3.6% vs. 3.8%).
Dr. Kobayashi suggested that several factors may explain the racial differences, including previously reported smooth muscle hyperresponsiveness to provocation stimuli in Japanese patients and the inclusion of a wide range of patients in Japanese studies, such as those with obstructive coronary disease.
Japanese studies also used sequential acetylcholine injection into both the right and left coronaries, a faster injection speed of 20 seconds, and upfront placement of a temporary pacing catheter in case of acetylcholine-induced bradycardia, particularly with right coronary injection.
Although the protocol is largely settled in Japan, he said, provocation protocols need to be standardized because “depending on the country and depending on the institution, people are doing totally different things.”
A big step forward
Commenting on the study, C. Noel Bairey Merz, MD, from Cedars Sinai, Los Angeles, said it has “widespread relevance” because half of all coronary angiograms done invasively in the United States for suspected ischemia find no obstructive coronary disease. Left untreated, however, MINOCA has a 2.5% annual event rate, and a quarter of that is death.
“This is a big step forward with likely equal opportunity to improve women and men’s ischemic heart disease,” she said.
On the other hand, all studies were conducted at centers of excellence, so safety will need to be carefully watched as testing rolls out to more community care, Dr. Merz said. “And it always needs to be underscored that this is done by an interventional cardiologist because they’re familiar with wires that can dissect arteries, and they’re familiar with minor complications that could turn into major, if someone didn’t act appropriately.”
Dr. Merz also called for unifying protocols and the need to raise awareness within the general cardiology community to ask interventionalists for acetylcholine spasm testing. Randomized controlled data from within the WISE study and the CorMica study showed that diagnostic certainty leads to greater therapeutic certainty. “You do a much better job about who and how to treat,” she said.
There are also three ongoing randomized controlled trials – WARRIOR, MINOCA-BAT, and iCorMica – in the INOCA and MINOCA populations testing different treatment strategies for hard clinical outcomes like death and myocardial infarction.
“So in addition to this publication being guideline-forming for diagnosis, we anticipate in the next several years to have clinical trial evidence about therapeutics, again, for formulation of class 1 guidelines,” Dr. Merz said.
John Beltrame, BMBS, PhD, University of Adelaide, Australia, said the meta-analysis shows that intracoronary acetylcholine spasm testing is safe and should prompt greater adoption of invasive functional angiography.
Interventionalists are quite happy to do fractional flow reserve using intravenous adenosine to assess coronary microvascular dysfunction, he said, and “what we think is that functional angiography should test both – both the spasm as well as the microvasculature – and that will give us a clear direction because the treatments are slightly different when you’re treating the large arteries as compared to the microscopic arteries. It’s an important thing.”
Dr. Beltrame and colleagues further detail the benefits of comprehensive invasive functional angiography over structural angiography in a related editorial.
He also noted that the Coronary Vasomotion Disorders International Study Group published international diagnostic criteria for microvascular angina and that several protocols for acetylcholine spasm testing are in the works, including one from Australia. Australian investigators are also organizing an accreditation program for those performing the test.
“The protocol itself is relatively straightforward, but it’s not merely picking up a manual and following the instructions,” Dr. Beltrame said. “Just the same as when you train someone in angioplasty, you don’t just go out and do it. You need to develop some experience in it and so should be proctored.”
Dr. Kobayashi reported consulting agreements with Abbott Vascular. Coauthor disclosures are listed in the paper. Dr. Beltrame and colleagues have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Provocation testing with intracoronary acetylcholine is safe, particularly among Western patients, suggests a large systematic review that underscores the importance of functional coronary angiography to diagnose epicardial or microvascular spasm.
The results, derived from more than 12,000 patients in 16 studies, showed a 0.5% risk of major complications, defined as death, ventricular tachycardia/ventricular fibrillation, myocardial infarction, and shock requiring resuscitation.
Ventricular tachycardia/fibrillation were the most common events and mainly reported from two Japanese studies. There were no deaths.
Exploratory subgroup analyses revealed significantly fewer major complications in Western populations (0.0%; P for heterogeneity = .938), compared with Asian populations (2.3%; P for heterogeneity < .001).
The pooled positive vasospasm rate was also lower in Western versus Asian studies (37.9% vs. 50.7%; P for between-group heterogeneity = .010), as reported by the Microvascular Network in the Journal of the American College of Cardiology.
“If you look at the data between Asian studies versus others, mainly European or U.S. studies, primarily in Caucasian populations, it’s like zero percent history of major complications. So, it sounds extremely safe to do this testing in Caucasian populations,” Yuhei Kobayashi, MD, NewYork-Presbyterian Brooklyn Methodist Hospital, Weill Cornell Medicine, said.
Safety will need to be assessed in African Americans and other racial/ethnic groups, but “it makes us think we should end up testing more in the United States,” he told this news organization.
Intracoronary acetylcholine testing is daily practice in Japan but is limited in the United States and Europe to a few specialized centers due to safety concerns. Three deaths were reported in 1980 with intravenous ergonovine testing, whereas the safety of acetylcholine protocols has been studied largely in single-center retrospective studies, typically in Asian populations.
Growing recognition of myocardial infarction with nonobstructive coronary arteries (MINOCA) and ischemia with no obstructive coronary arteries (INOCA), however, is changing the landscape. In recent U.S. and European guidelines, intracoronary acetylcholine testing is indicated as a class 2a recommendation in MINOCA/INOCA.
“More and more institutions in Europe and the United States are starting to do acetylcholine testing, because now we know that chest pain isn’t necessarily coming from the blocked arteries,” Dr. Kobayashi said. “There are functional abnormalities, including coronary spasm, and if we diagnose it, we have appropriate medical regimens for this kind of disease.”
First safety meta-analysis
The present review and meta-analysis included 12,585 participants in 16 studies through November 2021. Of these, 63% were conducted in Western countries, and most were prospective studies published over the past decade in patients with MINOCA or INOCA.
Ten studies used the contemporary diagnostic criteria for epicardial spasm of at least 90% reduction in coronary diameter. Acetylcholine was administered into the left coronary artery at up to 100 mcg and 200 mcg in seven and six studies, respectively, and was used in the other three studies to assess endothelial function with a slower infusion of up to 36.4 mcg.
Major complications were significantly higher in studies following the contemporary diagnostic cutoff than in those using a lower cutoff of at least 75% diameter reduction (1.0% vs. 0.0%; P for between-group heterogeneity < .001).
The incidence of major complications was 0.2% with the slower infusion of up to 36.4 mcg, 0.8% with a maximum dose of 100 mcg, and 0.3% with a maximum dose of 200 mcg. The positive vasospasm rate was similar with the latter two protocols, at 46.3% and 41.4%, respectively.
Minor complications occurred in 3.3% of patients but were not detailed. They can include paroxysmal atrial fibrillation, ventricular ectopic beats, transient hypotension, and bradycardia requiring intervention.
As with major complications, minor complications were lower in studies using noncontemporary versus contemporary diagnostic cutoffs for epicardial spasm (1.8% vs. 4.7%) and in Western versus Asian populations (2.6% vs. 9.4%). Minor complications were similar between protocols with maximum doses of 100 mcg and 200 mcg (3.6% vs. 3.8%).
Dr. Kobayashi suggested that several factors may explain the racial differences, including previously reported smooth muscle hyperresponsiveness to provocation stimuli in Japanese patients and the inclusion of a wide range of patients in Japanese studies, such as those with obstructive coronary disease.
Japanese studies also used sequential acetylcholine injection into both the right and left coronaries, a faster injection speed of 20 seconds, and upfront placement of a temporary pacing catheter in case of acetylcholine-induced bradycardia, particularly with right coronary injection.
Although the protocol is largely settled in Japan, he said, provocation protocols need to be standardized because “depending on the country and depending on the institution, people are doing totally different things.”
A big step forward
Commenting on the study, C. Noel Bairey Merz, MD, from Cedars Sinai, Los Angeles, said it has “widespread relevance” because half of all coronary angiograms done invasively in the United States for suspected ischemia find no obstructive coronary disease. Left untreated, however, MINOCA has a 2.5% annual event rate, and a quarter of that is death.
“This is a big step forward with likely equal opportunity to improve women and men’s ischemic heart disease,” she said.
On the other hand, all studies were conducted at centers of excellence, so safety will need to be carefully watched as testing rolls out to more community care, Dr. Merz said. “And it always needs to be underscored that this is done by an interventional cardiologist because they’re familiar with wires that can dissect arteries, and they’re familiar with minor complications that could turn into major, if someone didn’t act appropriately.”
Dr. Merz also called for unifying protocols and the need to raise awareness within the general cardiology community to ask interventionalists for acetylcholine spasm testing. Randomized controlled data from within the WISE study and the CorMica study showed that diagnostic certainty leads to greater therapeutic certainty. “You do a much better job about who and how to treat,” she said.
There are also three ongoing randomized controlled trials – WARRIOR, MINOCA-BAT, and iCorMica – in the INOCA and MINOCA populations testing different treatment strategies for hard clinical outcomes like death and myocardial infarction.
“So in addition to this publication being guideline-forming for diagnosis, we anticipate in the next several years to have clinical trial evidence about therapeutics, again, for formulation of class 1 guidelines,” Dr. Merz said.
John Beltrame, BMBS, PhD, University of Adelaide, Australia, said the meta-analysis shows that intracoronary acetylcholine spasm testing is safe and should prompt greater adoption of invasive functional angiography.
Interventionalists are quite happy to do fractional flow reserve using intravenous adenosine to assess coronary microvascular dysfunction, he said, and “what we think is that functional angiography should test both – both the spasm as well as the microvasculature – and that will give us a clear direction because the treatments are slightly different when you’re treating the large arteries as compared to the microscopic arteries. It’s an important thing.”
Dr. Beltrame and colleagues further detail the benefits of comprehensive invasive functional angiography over structural angiography in a related editorial.
He also noted that the Coronary Vasomotion Disorders International Study Group published international diagnostic criteria for microvascular angina and that several protocols for acetylcholine spasm testing are in the works, including one from Australia. Australian investigators are also organizing an accreditation program for those performing the test.
“The protocol itself is relatively straightforward, but it’s not merely picking up a manual and following the instructions,” Dr. Beltrame said. “Just the same as when you train someone in angioplasty, you don’t just go out and do it. You need to develop some experience in it and so should be proctored.”
Dr. Kobayashi reported consulting agreements with Abbott Vascular. Coauthor disclosures are listed in the paper. Dr. Beltrame and colleagues have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“How long, how long to sing this song?”
“My soul is in deep anguish. How long, Lord, how long?” – Psalm 6
. A once-common word in the 1800s, it fell steeply in popularity in the 20th century. Lately, I see it everywhere. It’s a beautiful word, capturing not only sorrow, but also weariness. It is also audacious, facing injustice and acknowledging that it ought not be this way, and communal, bearing witness to the shared hardship of being human. The Hebrew scriptures captured the experience of lament in the form of psalms, from the Greek, psalmoi or “words to accompany the music.” A few thousand years later, the words still resonate, especially in times of grief. “I am weary with my groaning; all the night make I my bed to swim; I water my couch with my tears.”
“Hair loss” is not the chief complaint you want to see when running behind in clinic – it’s never a 15-minute visit. A woman in her late 30s with wavy, light-brown hair that grew to her waistline was seated on the exam chair. When I sat across from her, I couldn’t see her scalp. No erythema or scale. No frontal band of hair loss. Just a bit thin everywhere. Perhaps another post-COVID telogen? This might be easy. I blew right by her mother, who was sitting in the corner of the room. Her black and white horizontal striped shirt seemed to match her gray and white hair. She looked worried.
Having perused my patient’s labs and done an exam, I announced that the diagnosis was telogen effluvium. “There are many possible causes, stress is a common one. Have you been under a lot of stress lately?” (The answer is always yes, thus providing a good foothold to climb out of a hair-loss visit). “Yes. My 1-year-old daughter died last year. She had choked on a cashew from a granola bar given by her sister.” I gasped and turned from her green eyes to her mom’s. Without saying a word, mom pleaded with me to help. “I don’t know what to say,” I said, “I’m so sorry.” Neither replied.
On the commute home that day I listened to a live recording of the U2 song, “40.” I had recently read about it in a touching essay about lament by Enuma Okoro of the Financial Times. I thought about my patient’s suffering and the brutal injustice of fate. It feels like it’s everywhere lately. Reporting from the events in Ukraine, Buffalo, Uvalde, Tulsa has put agonized faces like hers in the public square for us all to gape at and quietly mourn.
Even from a secular lens, it can be seen that a beauty of psalms is how they move from despair to hope. Prayers will be answered. Things will get better. Turn up the volume and feel the urgency and pathos Bono injects into your soul as he sings the refrain; “How long, how long? How long to sing this song?” In the live version we the audience take over for him. The words accompanying the music swell over the crowd. How much longer? How much more suffering? My patient’s hair will grow back. It will take years. All we can do is lament with her.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“My soul is in deep anguish. How long, Lord, how long?” – Psalm 6
. A once-common word in the 1800s, it fell steeply in popularity in the 20th century. Lately, I see it everywhere. It’s a beautiful word, capturing not only sorrow, but also weariness. It is also audacious, facing injustice and acknowledging that it ought not be this way, and communal, bearing witness to the shared hardship of being human. The Hebrew scriptures captured the experience of lament in the form of psalms, from the Greek, psalmoi or “words to accompany the music.” A few thousand years later, the words still resonate, especially in times of grief. “I am weary with my groaning; all the night make I my bed to swim; I water my couch with my tears.”
“Hair loss” is not the chief complaint you want to see when running behind in clinic – it’s never a 15-minute visit. A woman in her late 30s with wavy, light-brown hair that grew to her waistline was seated on the exam chair. When I sat across from her, I couldn’t see her scalp. No erythema or scale. No frontal band of hair loss. Just a bit thin everywhere. Perhaps another post-COVID telogen? This might be easy. I blew right by her mother, who was sitting in the corner of the room. Her black and white horizontal striped shirt seemed to match her gray and white hair. She looked worried.
Having perused my patient’s labs and done an exam, I announced that the diagnosis was telogen effluvium. “There are many possible causes, stress is a common one. Have you been under a lot of stress lately?” (The answer is always yes, thus providing a good foothold to climb out of a hair-loss visit). “Yes. My 1-year-old daughter died last year. She had choked on a cashew from a granola bar given by her sister.” I gasped and turned from her green eyes to her mom’s. Without saying a word, mom pleaded with me to help. “I don’t know what to say,” I said, “I’m so sorry.” Neither replied.
On the commute home that day I listened to a live recording of the U2 song, “40.” I had recently read about it in a touching essay about lament by Enuma Okoro of the Financial Times. I thought about my patient’s suffering and the brutal injustice of fate. It feels like it’s everywhere lately. Reporting from the events in Ukraine, Buffalo, Uvalde, Tulsa has put agonized faces like hers in the public square for us all to gape at and quietly mourn.
Even from a secular lens, it can be seen that a beauty of psalms is how they move from despair to hope. Prayers will be answered. Things will get better. Turn up the volume and feel the urgency and pathos Bono injects into your soul as he sings the refrain; “How long, how long? How long to sing this song?” In the live version we the audience take over for him. The words accompanying the music swell over the crowd. How much longer? How much more suffering? My patient’s hair will grow back. It will take years. All we can do is lament with her.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“My soul is in deep anguish. How long, Lord, how long?” – Psalm 6
. A once-common word in the 1800s, it fell steeply in popularity in the 20th century. Lately, I see it everywhere. It’s a beautiful word, capturing not only sorrow, but also weariness. It is also audacious, facing injustice and acknowledging that it ought not be this way, and communal, bearing witness to the shared hardship of being human. The Hebrew scriptures captured the experience of lament in the form of psalms, from the Greek, psalmoi or “words to accompany the music.” A few thousand years later, the words still resonate, especially in times of grief. “I am weary with my groaning; all the night make I my bed to swim; I water my couch with my tears.”
“Hair loss” is not the chief complaint you want to see when running behind in clinic – it’s never a 15-minute visit. A woman in her late 30s with wavy, light-brown hair that grew to her waistline was seated on the exam chair. When I sat across from her, I couldn’t see her scalp. No erythema or scale. No frontal band of hair loss. Just a bit thin everywhere. Perhaps another post-COVID telogen? This might be easy. I blew right by her mother, who was sitting in the corner of the room. Her black and white horizontal striped shirt seemed to match her gray and white hair. She looked worried.
Having perused my patient’s labs and done an exam, I announced that the diagnosis was telogen effluvium. “There are many possible causes, stress is a common one. Have you been under a lot of stress lately?” (The answer is always yes, thus providing a good foothold to climb out of a hair-loss visit). “Yes. My 1-year-old daughter died last year. She had choked on a cashew from a granola bar given by her sister.” I gasped and turned from her green eyes to her mom’s. Without saying a word, mom pleaded with me to help. “I don’t know what to say,” I said, “I’m so sorry.” Neither replied.
On the commute home that day I listened to a live recording of the U2 song, “40.” I had recently read about it in a touching essay about lament by Enuma Okoro of the Financial Times. I thought about my patient’s suffering and the brutal injustice of fate. It feels like it’s everywhere lately. Reporting from the events in Ukraine, Buffalo, Uvalde, Tulsa has put agonized faces like hers in the public square for us all to gape at and quietly mourn.
Even from a secular lens, it can be seen that a beauty of psalms is how they move from despair to hope. Prayers will be answered. Things will get better. Turn up the volume and feel the urgency and pathos Bono injects into your soul as he sings the refrain; “How long, how long? How long to sing this song?” In the live version we the audience take over for him. The words accompanying the music swell over the crowd. How much longer? How much more suffering? My patient’s hair will grow back. It will take years. All we can do is lament with her.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Heart failure: Medicare cost sharing may put quadruple therapy out of reach
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.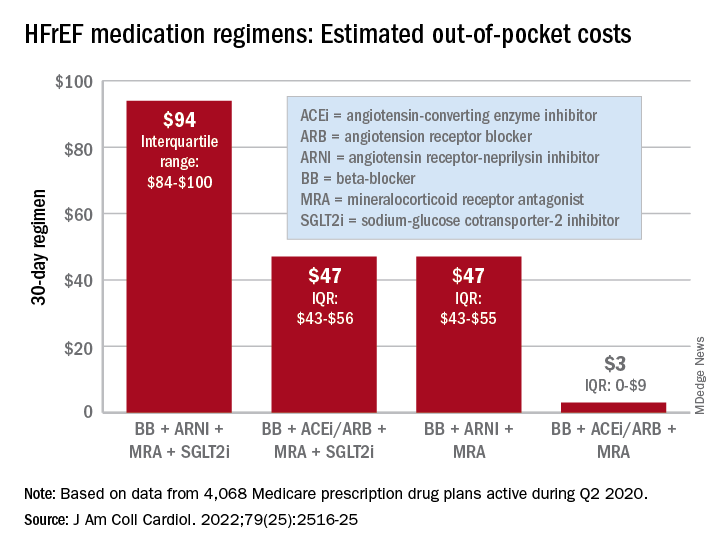
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.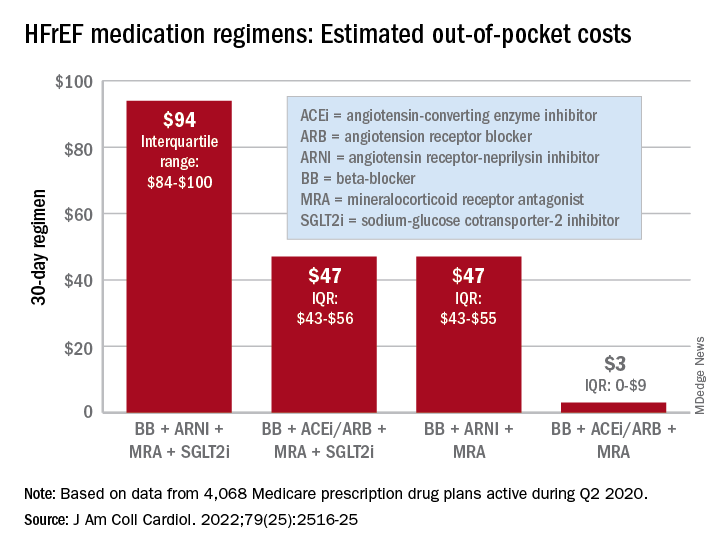
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.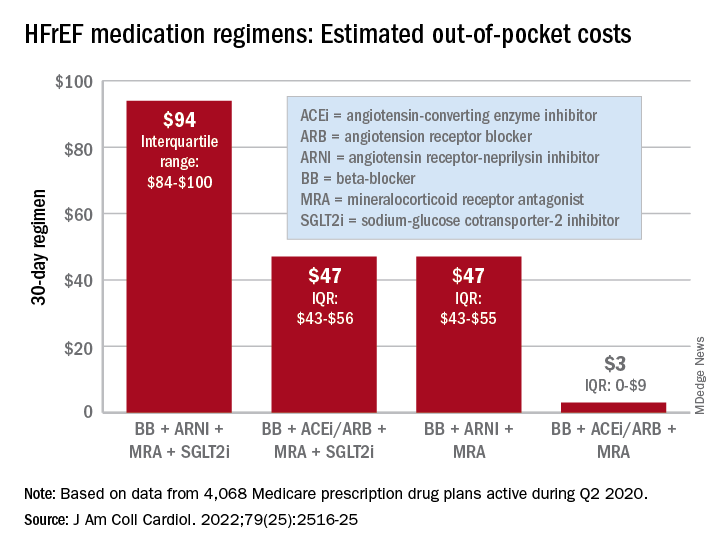
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
FROM THE JOURNAL Of the AMERICAN COLLEGE OF CARDIOLOGY
















