User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Top reads from the CHEST journal portfolio
Understanding RA with COPD, lung cancer prediction models, and chronic cardiac dysfunction
Journal CHEST®
Does Rheumatoid Arthritis Increase the Risk of COPD?
By: Chiwook Chung, MD, and colleagues
Notably, individuals with seropositive RA exhibit a greater risk of COPD onset than those with seronegative RA. Although smoking history didn’t affect the relationship between RA and COPD, monitoring respiratory symptoms and pulmonary function in patients with RA, especially patients who are seropositive, is crucial. These findings underscore the importance of interdisciplinary collaboration between rheumatologists and pulmonologists to enhance early detection and management strategies for pulmonary complications in patients with RA.
– Commentary by Corinne Young, MSN, FNP-C, FCCP, Member of the CHEST Physician® Editorial Board
CHEST Pulmonary®
The Lung Cancer Prediction Model “Stress Test”
By: Brent E. Heideman, MD, and colleagues
Current lung cancer prediction models have limited utility in high-risk patients referred for diagnostic biopsy. In a study of 322 indeterminate pulmonary nodules, the Brock, Mayo Clinic, Herder, and Veterans Affairs models showed modest discrimination between benign and malignant nodules (AUCs 0.67-0.77). The models performed poorly for low-risk patients (negative predictive values 63%-71%) and suboptimally for high-risk patients (positive predictive values 73%-87%), suggesting referring physicians use additional clinical information not captured in these models to identify high-risk patients needing biopsy. New prediction models and biomarkers specifically developed and calibrated for high-risk populations are needed to better inform clinical decision-making. Incorporating interval imaging to assess changes in nodule characteristics could potentially improve model performance. Tailored risk assessment tools are crucial for optimizing management and reducing unnecessary invasive procedures in this challenging patient population.
– Commentary by Russell Miller, MD, Member of the CHEST Physician Editorial Board
CHEST Critical Care ®
Characterizing Cardiac Function in ICU Survivors of Sepsis
By: Kevin Garrity, MBChB, and colleagues
While chronic cardiac dysfunction is one of the proposed mechanisms of long-term impairment post critical illness, its prevalence, mechanisms, and associations with disability following admission for sepsis are not well understood. Garrity and colleagues describe the Characterization of Cardiovascular Function in ICU Survivors of Sepsis (CONDUCT-ICU) protocol, a prospective study including two ICUs in Scotland aimed to better define cardiovascular dysfunction in survivors of sepsis. Designed to enroll 69 patients, demographics, cardiac and inflammatory biomarkers, and echocardiograms will be obtained on ICU discharge with additional laboratory data, cardiac magnetic resonance imaging, and patient-reported outcome measures to be obtained at 6 to 10 weeks. This novel multimodal approach will provide understanding into the role of cardiovascular dysfunction following critical illness as well as offer mechanistic insights. The investigators hope to obtain operational and pilot data for larger future studies.
– Commentary by Eugene Yuriditsky, MD, FCCP, Member of the CHEST Physician Editorial Board
Understanding RA with COPD, lung cancer prediction models, and chronic cardiac dysfunction
Understanding RA with COPD, lung cancer prediction models, and chronic cardiac dysfunction
Journal CHEST®
Does Rheumatoid Arthritis Increase the Risk of COPD?
By: Chiwook Chung, MD, and colleagues
Notably, individuals with seropositive RA exhibit a greater risk of COPD onset than those with seronegative RA. Although smoking history didn’t affect the relationship between RA and COPD, monitoring respiratory symptoms and pulmonary function in patients with RA, especially patients who are seropositive, is crucial. These findings underscore the importance of interdisciplinary collaboration between rheumatologists and pulmonologists to enhance early detection and management strategies for pulmonary complications in patients with RA.
– Commentary by Corinne Young, MSN, FNP-C, FCCP, Member of the CHEST Physician® Editorial Board
CHEST Pulmonary®
The Lung Cancer Prediction Model “Stress Test”
By: Brent E. Heideman, MD, and colleagues
Current lung cancer prediction models have limited utility in high-risk patients referred for diagnostic biopsy. In a study of 322 indeterminate pulmonary nodules, the Brock, Mayo Clinic, Herder, and Veterans Affairs models showed modest discrimination between benign and malignant nodules (AUCs 0.67-0.77). The models performed poorly for low-risk patients (negative predictive values 63%-71%) and suboptimally for high-risk patients (positive predictive values 73%-87%), suggesting referring physicians use additional clinical information not captured in these models to identify high-risk patients needing biopsy. New prediction models and biomarkers specifically developed and calibrated for high-risk populations are needed to better inform clinical decision-making. Incorporating interval imaging to assess changes in nodule characteristics could potentially improve model performance. Tailored risk assessment tools are crucial for optimizing management and reducing unnecessary invasive procedures in this challenging patient population.
– Commentary by Russell Miller, MD, Member of the CHEST Physician Editorial Board
CHEST Critical Care ®
Characterizing Cardiac Function in ICU Survivors of Sepsis
By: Kevin Garrity, MBChB, and colleagues
While chronic cardiac dysfunction is one of the proposed mechanisms of long-term impairment post critical illness, its prevalence, mechanisms, and associations with disability following admission for sepsis are not well understood. Garrity and colleagues describe the Characterization of Cardiovascular Function in ICU Survivors of Sepsis (CONDUCT-ICU) protocol, a prospective study including two ICUs in Scotland aimed to better define cardiovascular dysfunction in survivors of sepsis. Designed to enroll 69 patients, demographics, cardiac and inflammatory biomarkers, and echocardiograms will be obtained on ICU discharge with additional laboratory data, cardiac magnetic resonance imaging, and patient-reported outcome measures to be obtained at 6 to 10 weeks. This novel multimodal approach will provide understanding into the role of cardiovascular dysfunction following critical illness as well as offer mechanistic insights. The investigators hope to obtain operational and pilot data for larger future studies.
– Commentary by Eugene Yuriditsky, MD, FCCP, Member of the CHEST Physician Editorial Board
Journal CHEST®
Does Rheumatoid Arthritis Increase the Risk of COPD?
By: Chiwook Chung, MD, and colleagues
Notably, individuals with seropositive RA exhibit a greater risk of COPD onset than those with seronegative RA. Although smoking history didn’t affect the relationship between RA and COPD, monitoring respiratory symptoms and pulmonary function in patients with RA, especially patients who are seropositive, is crucial. These findings underscore the importance of interdisciplinary collaboration between rheumatologists and pulmonologists to enhance early detection and management strategies for pulmonary complications in patients with RA.
– Commentary by Corinne Young, MSN, FNP-C, FCCP, Member of the CHEST Physician® Editorial Board
CHEST Pulmonary®
The Lung Cancer Prediction Model “Stress Test”
By: Brent E. Heideman, MD, and colleagues
Current lung cancer prediction models have limited utility in high-risk patients referred for diagnostic biopsy. In a study of 322 indeterminate pulmonary nodules, the Brock, Mayo Clinic, Herder, and Veterans Affairs models showed modest discrimination between benign and malignant nodules (AUCs 0.67-0.77). The models performed poorly for low-risk patients (negative predictive values 63%-71%) and suboptimally for high-risk patients (positive predictive values 73%-87%), suggesting referring physicians use additional clinical information not captured in these models to identify high-risk patients needing biopsy. New prediction models and biomarkers specifically developed and calibrated for high-risk populations are needed to better inform clinical decision-making. Incorporating interval imaging to assess changes in nodule characteristics could potentially improve model performance. Tailored risk assessment tools are crucial for optimizing management and reducing unnecessary invasive procedures in this challenging patient population.
– Commentary by Russell Miller, MD, Member of the CHEST Physician Editorial Board
CHEST Critical Care ®
Characterizing Cardiac Function in ICU Survivors of Sepsis
By: Kevin Garrity, MBChB, and colleagues
While chronic cardiac dysfunction is one of the proposed mechanisms of long-term impairment post critical illness, its prevalence, mechanisms, and associations with disability following admission for sepsis are not well understood. Garrity and colleagues describe the Characterization of Cardiovascular Function in ICU Survivors of Sepsis (CONDUCT-ICU) protocol, a prospective study including two ICUs in Scotland aimed to better define cardiovascular dysfunction in survivors of sepsis. Designed to enroll 69 patients, demographics, cardiac and inflammatory biomarkers, and echocardiograms will be obtained on ICU discharge with additional laboratory data, cardiac magnetic resonance imaging, and patient-reported outcome measures to be obtained at 6 to 10 weeks. This novel multimodal approach will provide understanding into the role of cardiovascular dysfunction following critical illness as well as offer mechanistic insights. The investigators hope to obtain operational and pilot data for larger future studies.
– Commentary by Eugene Yuriditsky, MD, FCCP, Member of the CHEST Physician Editorial Board
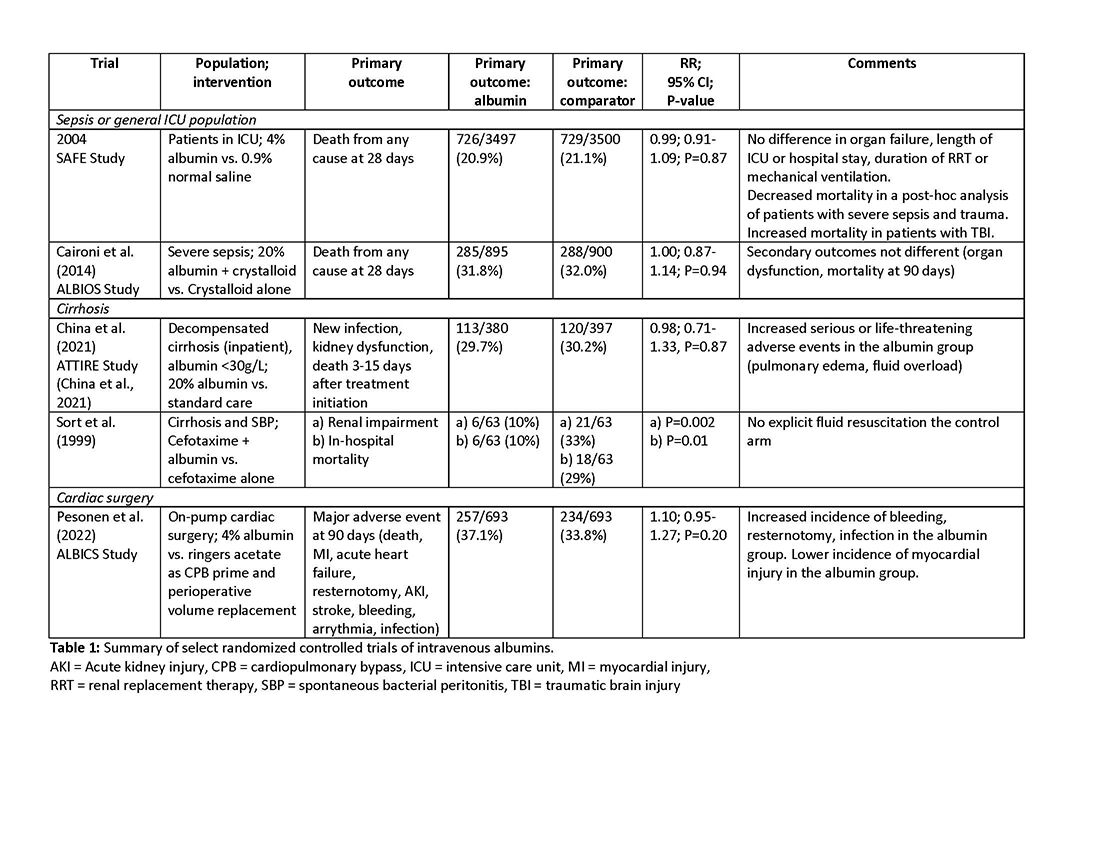
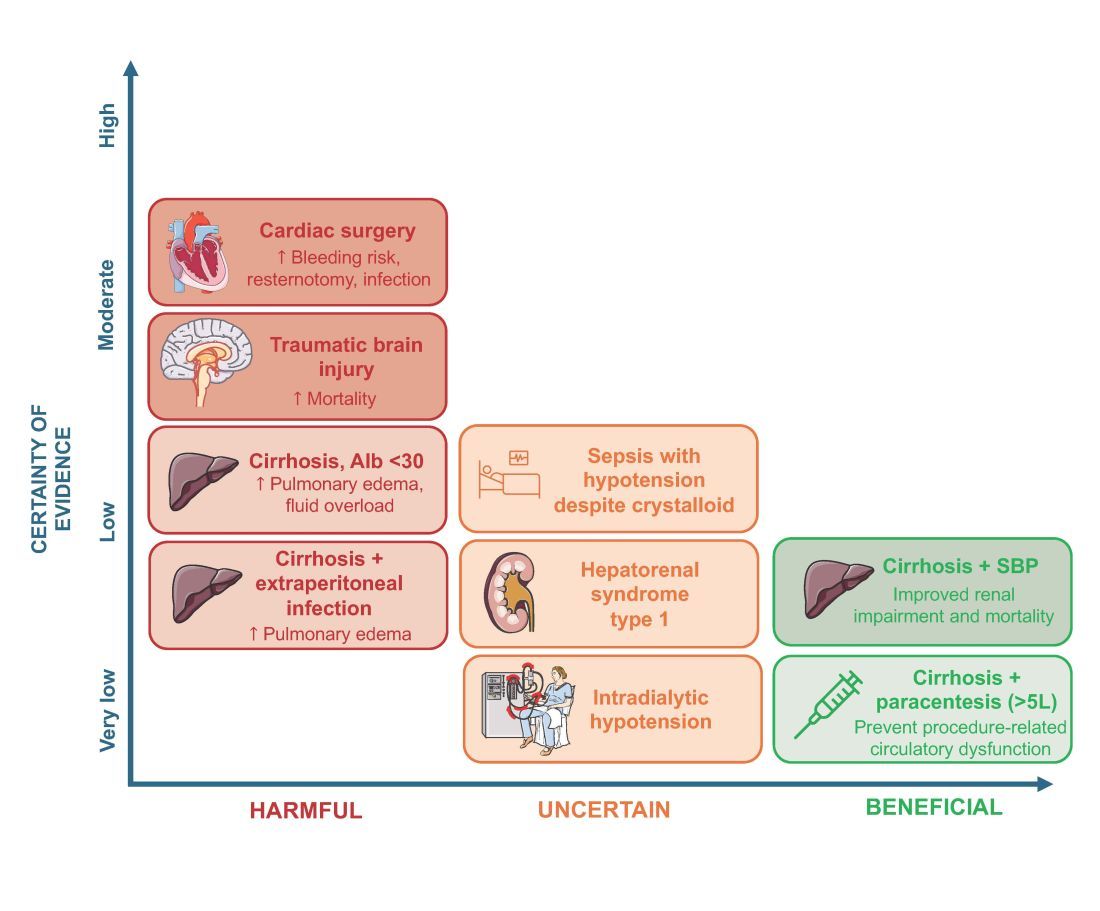
Use of albumin in critically ill patients
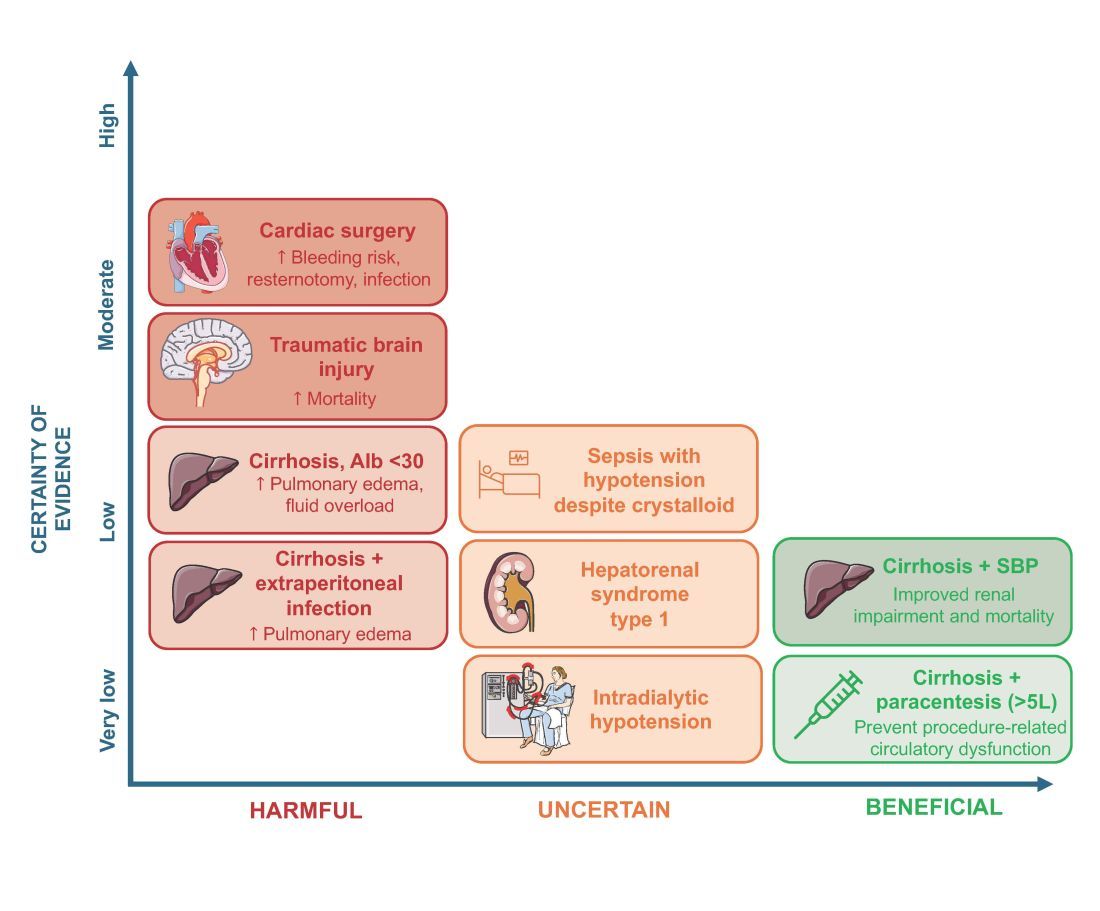
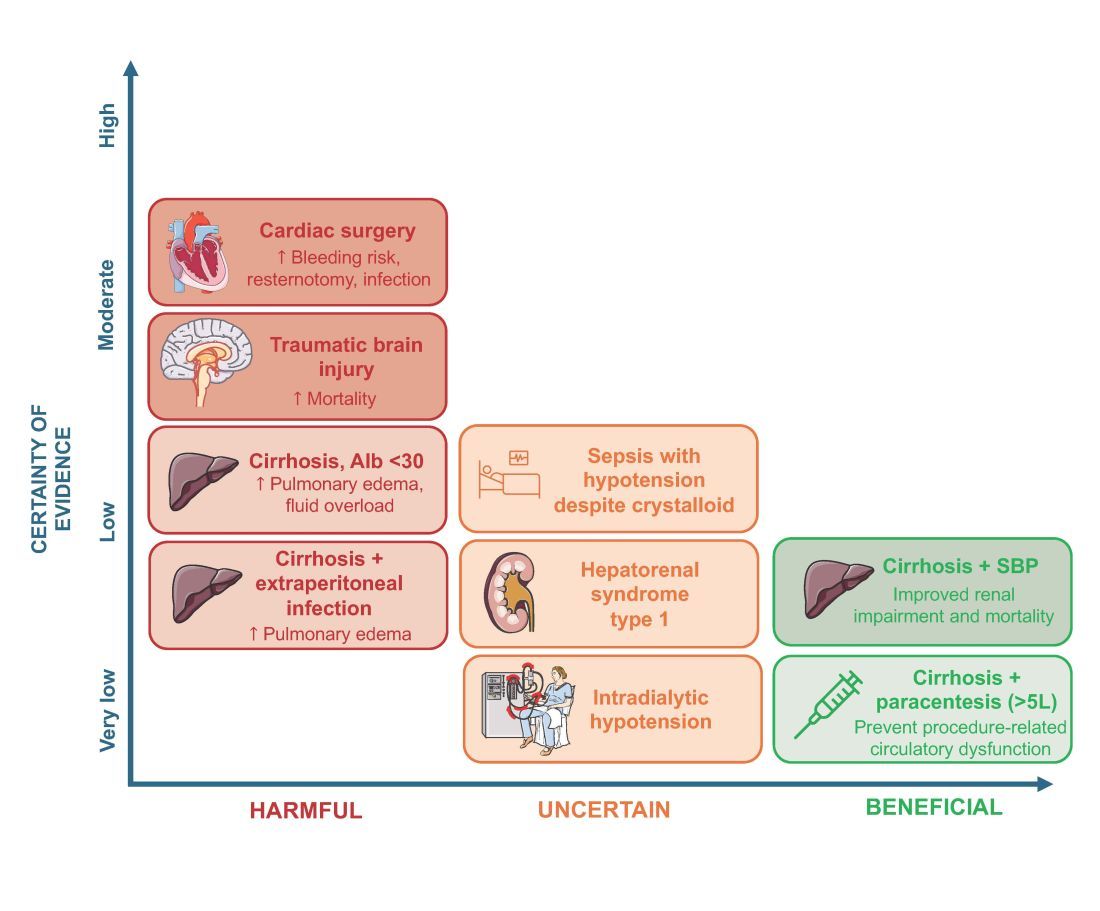
Intravenous albumin is a human-derived blood product studied widely in a variety of patient populations. Despite its frequent use in critical care, few high-quality studies have demonstrated improvements in patient-important outcomes. Compared with crystalloids, albumin increases the risk of fluid overload and bleeding and infections in patients undergoing cardiac surgery.1,2 In addition, albumin is costly, and its production is fraught with donor supply chain ethical concerns (the majority of albumin is derived from paid plasma donors).
Albumin use is highly variable between countries, hospitals, and even clinicians within the same specialty due to several factors, including the perception of minimal risk with albumin, concerns regarding insufficient short-term hemodynamic response to crystalloid, and lack of high-quality evidence to inform clinical practice. We will discuss when intensivists should consider albumin use (with prescription personalized to patient context) and when it should be avoided due to the concerns for patient harm.
An intensivist might consider albumin as a reasonable treatment option in patients with cirrhosis undergoing large volume paracentesis to prevent paracentesis-induced circulatory dysfunction, and in patients with cirrhosis and spontaneous bacterial peritonitis (SBP), as data suggests use in this setting leads to a reduction in mortality.3 Clinicians should be aware that even for these widely accepted albumin indications, which are supported by published guidelines, the certainty of evidence is low, recommendations are weak (conditional), and, therefore, albumin should always be personalized to the patient based on volume of paracentesis fluid removed, prior history of hypotension after procedures, and degree of renal dysfunction.4
There are also several conditions for which an intensivist might consider albumin and for which albumin is commonly administered but lacks high-quality studies to support its use either as a frontline or rescue fluid therapy. One such condition is type 1 hepatorenal syndrome (HRS), for which albumin is widely used; however, there are no randomized controlled trials that have compared albumin with placebo.
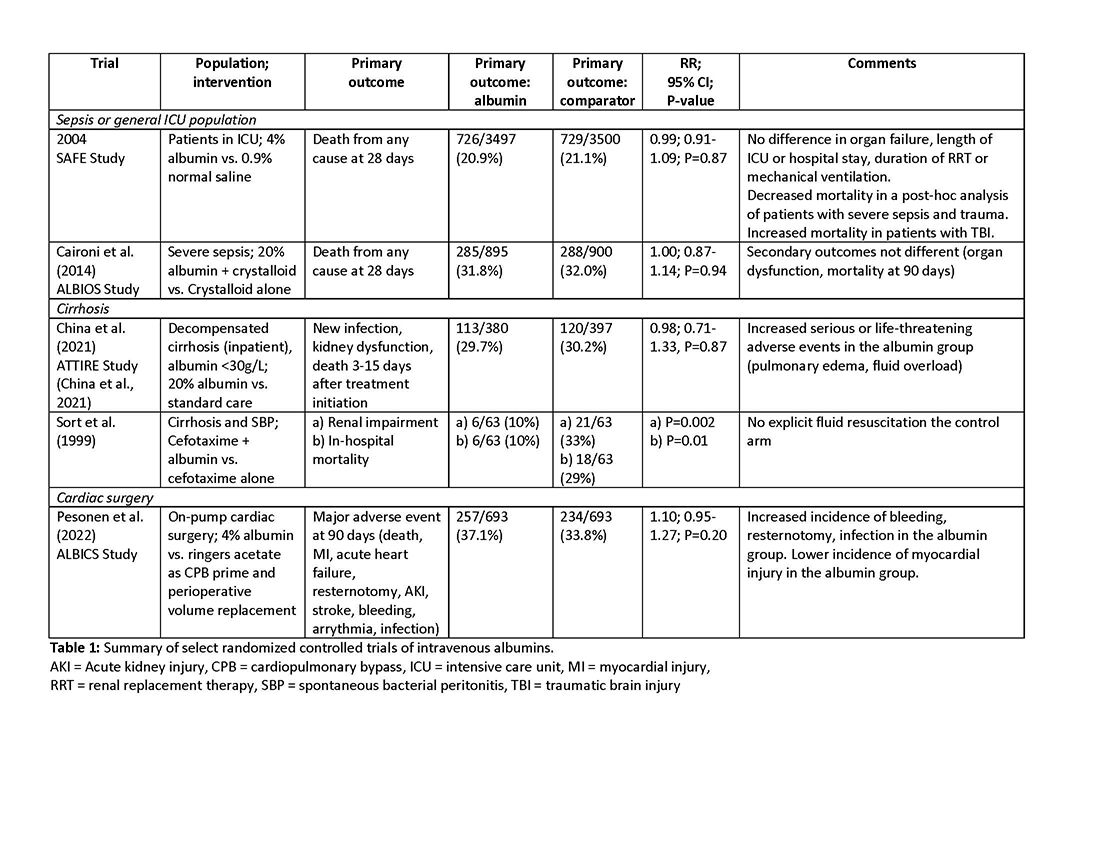
As with any intervention, the use of albumin is associated with risks. In patients undergoing on-pump cardiac surgery, the ALBICS study showed that albumin did not reduce the risk of major adverse events and, instead, increased risk of bleeding, resternotomy, and infection.2 The ATTIRE trial showed that in patients hospitalized with decompensated cirrhosis and serum albumin <30 g/L, albumin failed to reduce infection, renal impairment, or mortality while increasing life-threatening adverse events, including pulmonary edema and fluid overload.1 Similarly, in patients with cirrhosis and extraperitoneal infections, albumin showed no benefit in reducing renal impairment or mortality, and its use was associated with higher rates of pulmonary edema.6 Lastly, critically ill patients with traumatic brain injury (TBI) who received fluid resuscitation with albumin have been shown to experience higher mortality compared with saline.7 Thus, based on current evidence, intravenous albumin is not recommended for patients undergoing cardiac surgery (priming of the bypass circuit or volume replacement), patients hospitalized with decompensated cirrhosis and hypoalbuminemia, patients hospitalized with cirrhosis and extraperitoneal infections, and critically ill patients with TBI.4
Overall, intravenous albumin prescription in critical care patients requires a personalized approach informed by current best evidence and is not without potential harm.
High-quality evidence is currently lacking in many clinical settings, and large randomized controlled trials are underway to provide further insights into the utility of albumin. These trials will address albumin use in the following: acute kidney injury requiring renal replacement therapy (ALTER-AKI, NCT04705896), inpatients with community-acquired pneumonia (NCT04071041), high-risk cardiac surgery (ACTRN1261900135516703), and septic shock (NCT03869385).
Financial/nonfinancial disclosures
Nicole Relke: None. Mark Hewitt: None. Bram Rochwerg: None. Jeannie Callum: Research support from Canadian Blood Services and Octapharma.
References
1. China L, Freemantle N, Forrest E, et al. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384(9):808-817. doi:10.1056/NEJMoa2022166
2. Pesonen E, Vlasov H, Suojaranta R, et al. Effect of 4% albumin solution vs ringer acetate on major adverse events in patients undergoing cardiac surgery with cardiopulmonary bypass: a randomized clinical trial. JAMA. 2022;328(3):251-258. doi:10.1001/jama.2022.10461
3. Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. NEJM. 1999;341:403-409.
4. Callum J, Skubas NJ, Bathla A, et al. Use of intravenous albumin: a guideline from the international collaboration for transfusion medicine guidelines. Chest. 2024:S0012-3692(24)00285-X. doi:10.1016/j.chest.2024.02.049
5. Torp N. High doses of albumin increases mortality and complications in terlipressin treated patients with cirrhosis: insights from the ATTIRE trial. Paper presented at the AASLD; 2023; San Diego, CA. https://www.aasld.org/the-liver-meeting/high-doses-albumin-increases-mortality-and-complications-terlipressin-treated
6. Wong YJ, Qiu TY, Tam YC, Mohan BP, Gallegos-Orozco JF, Adler DG. Efficacy and safety of IV albumin for non-spontaneous bacterial peritonitis infection among patients with cirrhosis: a systematic review and meta-analysis. Dig Liver Dis. 2020;52(10):1137-1142. doi:10.1016/j.dld.2020.05.047
7. Myburgh J, Cooper JD, Finfer S, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357(9):874-884.
Intravenous albumin is a human-derived blood product studied widely in a variety of patient populations. Despite its frequent use in critical care, few high-quality studies have demonstrated improvements in patient-important outcomes. Compared with crystalloids, albumin increases the risk of fluid overload and bleeding and infections in patients undergoing cardiac surgery.1,2 In addition, albumin is costly, and its production is fraught with donor supply chain ethical concerns (the majority of albumin is derived from paid plasma donors).
Albumin use is highly variable between countries, hospitals, and even clinicians within the same specialty due to several factors, including the perception of minimal risk with albumin, concerns regarding insufficient short-term hemodynamic response to crystalloid, and lack of high-quality evidence to inform clinical practice. We will discuss when intensivists should consider albumin use (with prescription personalized to patient context) and when it should be avoided due to the concerns for patient harm.
An intensivist might consider albumin as a reasonable treatment option in patients with cirrhosis undergoing large volume paracentesis to prevent paracentesis-induced circulatory dysfunction, and in patients with cirrhosis and spontaneous bacterial peritonitis (SBP), as data suggests use in this setting leads to a reduction in mortality.3 Clinicians should be aware that even for these widely accepted albumin indications, which are supported by published guidelines, the certainty of evidence is low, recommendations are weak (conditional), and, therefore, albumin should always be personalized to the patient based on volume of paracentesis fluid removed, prior history of hypotension after procedures, and degree of renal dysfunction.4
There are also several conditions for which an intensivist might consider albumin and for which albumin is commonly administered but lacks high-quality studies to support its use either as a frontline or rescue fluid therapy. One such condition is type 1 hepatorenal syndrome (HRS), for which albumin is widely used; however, there are no randomized controlled trials that have compared albumin with placebo.
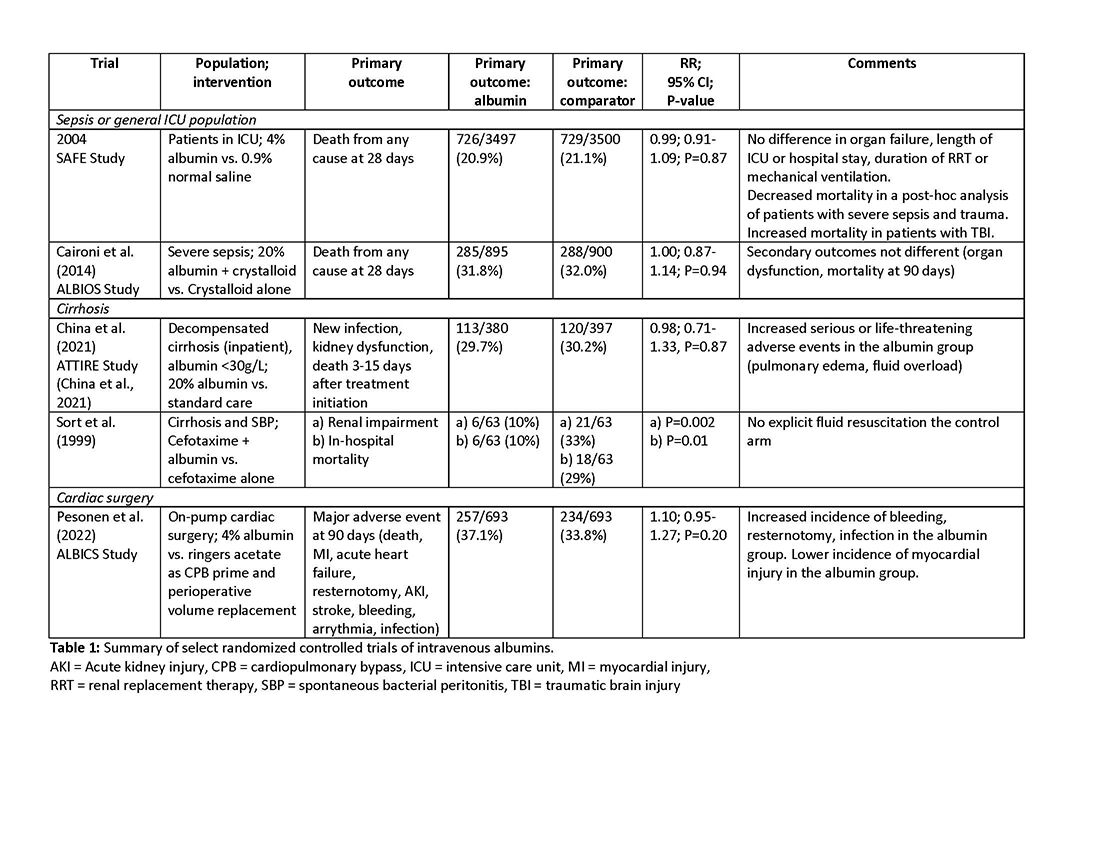
As with any intervention, the use of albumin is associated with risks. In patients undergoing on-pump cardiac surgery, the ALBICS study showed that albumin did not reduce the risk of major adverse events and, instead, increased risk of bleeding, resternotomy, and infection.2 The ATTIRE trial showed that in patients hospitalized with decompensated cirrhosis and serum albumin <30 g/L, albumin failed to reduce infection, renal impairment, or mortality while increasing life-threatening adverse events, including pulmonary edema and fluid overload.1 Similarly, in patients with cirrhosis and extraperitoneal infections, albumin showed no benefit in reducing renal impairment or mortality, and its use was associated with higher rates of pulmonary edema.6 Lastly, critically ill patients with traumatic brain injury (TBI) who received fluid resuscitation with albumin have been shown to experience higher mortality compared with saline.7 Thus, based on current evidence, intravenous albumin is not recommended for patients undergoing cardiac surgery (priming of the bypass circuit or volume replacement), patients hospitalized with decompensated cirrhosis and hypoalbuminemia, patients hospitalized with cirrhosis and extraperitoneal infections, and critically ill patients with TBI.4
Overall, intravenous albumin prescription in critical care patients requires a personalized approach informed by current best evidence and is not without potential harm.
High-quality evidence is currently lacking in many clinical settings, and large randomized controlled trials are underway to provide further insights into the utility of albumin. These trials will address albumin use in the following: acute kidney injury requiring renal replacement therapy (ALTER-AKI, NCT04705896), inpatients with community-acquired pneumonia (NCT04071041), high-risk cardiac surgery (ACTRN1261900135516703), and septic shock (NCT03869385).
Financial/nonfinancial disclosures
Nicole Relke: None. Mark Hewitt: None. Bram Rochwerg: None. Jeannie Callum: Research support from Canadian Blood Services and Octapharma.
References
1. China L, Freemantle N, Forrest E, et al. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384(9):808-817. doi:10.1056/NEJMoa2022166
2. Pesonen E, Vlasov H, Suojaranta R, et al. Effect of 4% albumin solution vs ringer acetate on major adverse events in patients undergoing cardiac surgery with cardiopulmonary bypass: a randomized clinical trial. JAMA. 2022;328(3):251-258. doi:10.1001/jama.2022.10461
3. Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. NEJM. 1999;341:403-409.
4. Callum J, Skubas NJ, Bathla A, et al. Use of intravenous albumin: a guideline from the international collaboration for transfusion medicine guidelines. Chest. 2024:S0012-3692(24)00285-X. doi:10.1016/j.chest.2024.02.049
5. Torp N. High doses of albumin increases mortality and complications in terlipressin treated patients with cirrhosis: insights from the ATTIRE trial. Paper presented at the AASLD; 2023; San Diego, CA. https://www.aasld.org/the-liver-meeting/high-doses-albumin-increases-mortality-and-complications-terlipressin-treated
6. Wong YJ, Qiu TY, Tam YC, Mohan BP, Gallegos-Orozco JF, Adler DG. Efficacy and safety of IV albumin for non-spontaneous bacterial peritonitis infection among patients with cirrhosis: a systematic review and meta-analysis. Dig Liver Dis. 2020;52(10):1137-1142. doi:10.1016/j.dld.2020.05.047
7. Myburgh J, Cooper JD, Finfer S, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357(9):874-884.
Intravenous albumin is a human-derived blood product studied widely in a variety of patient populations. Despite its frequent use in critical care, few high-quality studies have demonstrated improvements in patient-important outcomes. Compared with crystalloids, albumin increases the risk of fluid overload and bleeding and infections in patients undergoing cardiac surgery.1,2 In addition, albumin is costly, and its production is fraught with donor supply chain ethical concerns (the majority of albumin is derived from paid plasma donors).
Albumin use is highly variable between countries, hospitals, and even clinicians within the same specialty due to several factors, including the perception of minimal risk with albumin, concerns regarding insufficient short-term hemodynamic response to crystalloid, and lack of high-quality evidence to inform clinical practice. We will discuss when intensivists should consider albumin use (with prescription personalized to patient context) and when it should be avoided due to the concerns for patient harm.
An intensivist might consider albumin as a reasonable treatment option in patients with cirrhosis undergoing large volume paracentesis to prevent paracentesis-induced circulatory dysfunction, and in patients with cirrhosis and spontaneous bacterial peritonitis (SBP), as data suggests use in this setting leads to a reduction in mortality.3 Clinicians should be aware that even for these widely accepted albumin indications, which are supported by published guidelines, the certainty of evidence is low, recommendations are weak (conditional), and, therefore, albumin should always be personalized to the patient based on volume of paracentesis fluid removed, prior history of hypotension after procedures, and degree of renal dysfunction.4
There are also several conditions for which an intensivist might consider albumin and for which albumin is commonly administered but lacks high-quality studies to support its use either as a frontline or rescue fluid therapy. One such condition is type 1 hepatorenal syndrome (HRS), for which albumin is widely used; however, there are no randomized controlled trials that have compared albumin with placebo.
As with any intervention, the use of albumin is associated with risks. In patients undergoing on-pump cardiac surgery, the ALBICS study showed that albumin did not reduce the risk of major adverse events and, instead, increased risk of bleeding, resternotomy, and infection.2 The ATTIRE trial showed that in patients hospitalized with decompensated cirrhosis and serum albumin <30 g/L, albumin failed to reduce infection, renal impairment, or mortality while increasing life-threatening adverse events, including pulmonary edema and fluid overload.1 Similarly, in patients with cirrhosis and extraperitoneal infections, albumin showed no benefit in reducing renal impairment or mortality, and its use was associated with higher rates of pulmonary edema.6 Lastly, critically ill patients with traumatic brain injury (TBI) who received fluid resuscitation with albumin have been shown to experience higher mortality compared with saline.7 Thus, based on current evidence, intravenous albumin is not recommended for patients undergoing cardiac surgery (priming of the bypass circuit or volume replacement), patients hospitalized with decompensated cirrhosis and hypoalbuminemia, patients hospitalized with cirrhosis and extraperitoneal infections, and critically ill patients with TBI.4
Overall, intravenous albumin prescription in critical care patients requires a personalized approach informed by current best evidence and is not without potential harm.
High-quality evidence is currently lacking in many clinical settings, and large randomized controlled trials are underway to provide further insights into the utility of albumin. These trials will address albumin use in the following: acute kidney injury requiring renal replacement therapy (ALTER-AKI, NCT04705896), inpatients with community-acquired pneumonia (NCT04071041), high-risk cardiac surgery (ACTRN1261900135516703), and septic shock (NCT03869385).
Financial/nonfinancial disclosures
Nicole Relke: None. Mark Hewitt: None. Bram Rochwerg: None. Jeannie Callum: Research support from Canadian Blood Services and Octapharma.
References
1. China L, Freemantle N, Forrest E, et al. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384(9):808-817. doi:10.1056/NEJMoa2022166
2. Pesonen E, Vlasov H, Suojaranta R, et al. Effect of 4% albumin solution vs ringer acetate on major adverse events in patients undergoing cardiac surgery with cardiopulmonary bypass: a randomized clinical trial. JAMA. 2022;328(3):251-258. doi:10.1001/jama.2022.10461
3. Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. NEJM. 1999;341:403-409.
4. Callum J, Skubas NJ, Bathla A, et al. Use of intravenous albumin: a guideline from the international collaboration for transfusion medicine guidelines. Chest. 2024:S0012-3692(24)00285-X. doi:10.1016/j.chest.2024.02.049
5. Torp N. High doses of albumin increases mortality and complications in terlipressin treated patients with cirrhosis: insights from the ATTIRE trial. Paper presented at the AASLD; 2023; San Diego, CA. https://www.aasld.org/the-liver-meeting/high-doses-albumin-increases-mortality-and-complications-terlipressin-treated
6. Wong YJ, Qiu TY, Tam YC, Mohan BP, Gallegos-Orozco JF, Adler DG. Efficacy and safety of IV albumin for non-spontaneous bacterial peritonitis infection among patients with cirrhosis: a systematic review and meta-analysis. Dig Liver Dis. 2020;52(10):1137-1142. doi:10.1016/j.dld.2020.05.047
7. Myburgh J, Cooper JD, Finfer S, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357(9):874-884.
Primary Care: Try These Steps to Boost Lung Cancer Screens
A few years ago, Kim Lori Sandler, MD, realized many patients newly diagnosed with lung cancer had never been screened for the disease — they received CT scans only because they were symptomatic.
But Dr. Sandler, a radiologist at Vanderbilt University Medical Center in Nashville, Tennessee, could see in medical charts that most of these patients had been eligible for a screening before becoming symptomatic. And for women, most had received decades worth of mammograms. She saw an opportunity and launched a study to find out if an intervention would work.
Low-dose CT and mammography services often are available in the same imaging facility, so women who qualified for a lung cancer screening were offered the scan during their mammography visit. Over a 3-year period, monthly rates of lung scans in women rose by 50% at one facility and 36% at the other.
“What we found is that women are really receptive, if you talk to them about it,” Dr. Sandler said. “I don’t think that lung cancer is thought of as a disease in women.”
Although lung cancer is the leading cause of cancer deaths in the United States, a recent study in JAMA Internal Medicine found only 18% of eligible patients were screened in 2022, a far cry from the rates of 72% for colon cancer — which itself falls short of goals from US medical groups like the American Cancer Society (ACS). Among those eligible, rates of lung screenings were lowest among younger people without comorbid conditions, who did not have health insurance or a usual source of care, and those living in southern states and states that did not expand Medicaid as part of the Affordable Care Act.
Getting patients screened is lifesaving: 27% of people with lung cancer survive 5 years after diagnosis. But the survival rate rises to 63% when cases are diagnosed at an early stage.
Increasing Uptake
The formal recommendation to use low-dose chest CT to screen for lung cancer is only a decade old. The approach was first endorsed by the United States Preventive Services Task Force (USPSTF) on the basis of an influential trial that found such testing was linked to a 20% reduction in mortality from the disease. Updated 2021 USPSTF guidelines call for annual screening of people aged 50-80 years who have a 20 pack-year history of smoking and currently smoke or have quit within the past 15 years.
But implementing the recommendation is not always simple. Unlike a colorectal or breast cancer screening, which is recommended primarily on patient age, eligibility for a lung cancer screening requires calculating pack-years of smoking, and, for past smokers, knowledge of when they quit.
The structured fields in most electronic medical records (EMRs) inquire about current or past use of cigarettes and the number of daily packs smoked. But few EMRs can calculate when a patient starts smoking two cigarettes a day but then increases to a pack a day and cuts down again. EMRs also do not track when a patient has stopped smoking permanently. Individual clinicians or health systems must identify patients who are eligible for screening, but the lack of automated calculations makes that job more difficult.
Dr. Sandler and colleagues turned to the informatics team at Vanderbilt to develop a natural language processing approach that extracts smoking data directly from clinician notes instead of using standard variables in their EMR.
The number of patients identified as needing a screening using the algorithm nearly doubled from baseline, from 5887 to 10,231 over a 3-year period, according to results from another study that Dr. Sandler published.
Although the algorithm may occasionally flag someone who does not need screening as eligible, “you can always have a conversation with the patient to determine if they actually meet eligibility criteria,” Dr. Sandler said.
Patient Navigators to the Rescue?
About a decade ago, Travis Baggett, MD, MPH, an associate professor of internal medicine at Harvard Medical School, Boston, Massachusetts, received pilot funding from the ACS to study cancer epidemiology among patients at Boston Health Care for the Homeless Program (BHCHP), which serves nearly 10,000 patients at a variety of Boston-area clinics each year.
“We found that both the incidence and mortality rates for lung cancer were more than twofold higher than in the general population,” Dr. Baggett, who is also the director of research at BHCHP, said.
He also discovered that BHCHP patients were diagnosed at significantly later stages than people in the general population for malignancies like breast and colorectal cancer.
Screening for lung cancer was a new recommendation at the time. With additional funding from the ACS, he launched a clinical trial in 2020 that randomized patients who were eligible for lung cancer screening to either work with a patient navigator or receive usual care.
The navigators eased the burden on primary care clinicians: They facilitated shared decision-making visits, helped participants make and attend appointments for low-dose CT, assisted with transportation, and arranged follow-up as needed.
The 3-year study found 43% of patients who received navigation services underwent screening for lung cancer, compared with 9% in the usual-care arm. Participants said the navigators played a critical role in educating them about the importance of screening, coordinating care, and providing emotional support.
“At the root of it all, it was quite clear that one thing that made the navigator successful was their interpersonal qualities and having someone that the patient could trust to help guide them through the process,” Dr. Baggett said.
The navigator program, however, stopped when the funding for the study ended.
But another health system has implemented navigators in a sustainable way through a quality improvement project. Michael Gieske, MD, director of lung cancer screening at St. Elizabeth Healthcare in Edgewood, Kentucky, starts his Friday morning meeting with a multidisciplinary group, including a thoracic surgeon, radiologist, pulmonologist, and several screening nurse navigators. They review the week’s chest CTs, with approximately one-third from patients who underwent lung cancer screening.
Nurse navigators at St. Elizabeth Healthcare follow up with any patient whose scan is suspicious for lung cancer and guide them through the process of seeing specialists and obtaining additional testing.
“They essentially hold the patient’s hand through this scary time in their life and make sure that everything flows smoothly and efficiently,” said Dr. Gieske, a family medicine physician.
St. Elizabeth’s program also draws on several evidence-based strategies used for other cancer screening programs, such as patient and provider education and quarterly feedback to their 194 primary care clinicians on rates of lung cancer screening among their eligible patients.
Several requirements for reimbursement for a lung cancer screening from the US Centers for Medicare & Medicaid Services can also serve as barriers to getting patients screened: Clinicians must identify who is eligible, provide tobacco cessation counseling, and document the shared decision-making process.
To streamline the steps, St. Elizabeth’s clinicians use an EMR smart set that reminds clinicians to verify smoking history and helps them document the required counseling.
Last year, 47% of eligible patients received their recommended screening, and Dr. Gieske said he expects even more improvement.
“We’re on track this year to complete 60% uptake if things continue,” he said, adding that 76% of the new cases of lung cancer are now diagnosed in stage I, with only 5% diagnosed in stage IV.
Dr. Gieske has shared his experience with many clinics in Appalachia, home to some of the highest rates of mortality from lung cancer in the country. A major part of his role with the Appalachian Community Cancer Alliance is helping educate primary care clinicians in the region about the importance of early detection of lung cancer.
“I think one of the most important things is just to convey a message of hope,” he said. “We’re trying to get the good word out there that if you screen individuals, you’re going to catch it early, when you have an extremely high chance of curing the lung cancer.”
Dr. Baggett reported support from grants from the ACS and the Massachusetts General Hospital Research Scholars Program. Dr. Sandler and Dr. Gieske reported no financial conflicts.
A version of this article first appeared on Medscape.com.
A few years ago, Kim Lori Sandler, MD, realized many patients newly diagnosed with lung cancer had never been screened for the disease — they received CT scans only because they were symptomatic.
But Dr. Sandler, a radiologist at Vanderbilt University Medical Center in Nashville, Tennessee, could see in medical charts that most of these patients had been eligible for a screening before becoming symptomatic. And for women, most had received decades worth of mammograms. She saw an opportunity and launched a study to find out if an intervention would work.
Low-dose CT and mammography services often are available in the same imaging facility, so women who qualified for a lung cancer screening were offered the scan during their mammography visit. Over a 3-year period, monthly rates of lung scans in women rose by 50% at one facility and 36% at the other.
“What we found is that women are really receptive, if you talk to them about it,” Dr. Sandler said. “I don’t think that lung cancer is thought of as a disease in women.”
Although lung cancer is the leading cause of cancer deaths in the United States, a recent study in JAMA Internal Medicine found only 18% of eligible patients were screened in 2022, a far cry from the rates of 72% for colon cancer — which itself falls short of goals from US medical groups like the American Cancer Society (ACS). Among those eligible, rates of lung screenings were lowest among younger people without comorbid conditions, who did not have health insurance or a usual source of care, and those living in southern states and states that did not expand Medicaid as part of the Affordable Care Act.
Getting patients screened is lifesaving: 27% of people with lung cancer survive 5 years after diagnosis. But the survival rate rises to 63% when cases are diagnosed at an early stage.
Increasing Uptake
The formal recommendation to use low-dose chest CT to screen for lung cancer is only a decade old. The approach was first endorsed by the United States Preventive Services Task Force (USPSTF) on the basis of an influential trial that found such testing was linked to a 20% reduction in mortality from the disease. Updated 2021 USPSTF guidelines call for annual screening of people aged 50-80 years who have a 20 pack-year history of smoking and currently smoke or have quit within the past 15 years.
But implementing the recommendation is not always simple. Unlike a colorectal or breast cancer screening, which is recommended primarily on patient age, eligibility for a lung cancer screening requires calculating pack-years of smoking, and, for past smokers, knowledge of when they quit.
The structured fields in most electronic medical records (EMRs) inquire about current or past use of cigarettes and the number of daily packs smoked. But few EMRs can calculate when a patient starts smoking two cigarettes a day but then increases to a pack a day and cuts down again. EMRs also do not track when a patient has stopped smoking permanently. Individual clinicians or health systems must identify patients who are eligible for screening, but the lack of automated calculations makes that job more difficult.
Dr. Sandler and colleagues turned to the informatics team at Vanderbilt to develop a natural language processing approach that extracts smoking data directly from clinician notes instead of using standard variables in their EMR.
The number of patients identified as needing a screening using the algorithm nearly doubled from baseline, from 5887 to 10,231 over a 3-year period, according to results from another study that Dr. Sandler published.
Although the algorithm may occasionally flag someone who does not need screening as eligible, “you can always have a conversation with the patient to determine if they actually meet eligibility criteria,” Dr. Sandler said.
Patient Navigators to the Rescue?
About a decade ago, Travis Baggett, MD, MPH, an associate professor of internal medicine at Harvard Medical School, Boston, Massachusetts, received pilot funding from the ACS to study cancer epidemiology among patients at Boston Health Care for the Homeless Program (BHCHP), which serves nearly 10,000 patients at a variety of Boston-area clinics each year.
“We found that both the incidence and mortality rates for lung cancer were more than twofold higher than in the general population,” Dr. Baggett, who is also the director of research at BHCHP, said.
He also discovered that BHCHP patients were diagnosed at significantly later stages than people in the general population for malignancies like breast and colorectal cancer.
Screening for lung cancer was a new recommendation at the time. With additional funding from the ACS, he launched a clinical trial in 2020 that randomized patients who were eligible for lung cancer screening to either work with a patient navigator or receive usual care.
The navigators eased the burden on primary care clinicians: They facilitated shared decision-making visits, helped participants make and attend appointments for low-dose CT, assisted with transportation, and arranged follow-up as needed.
The 3-year study found 43% of patients who received navigation services underwent screening for lung cancer, compared with 9% in the usual-care arm. Participants said the navigators played a critical role in educating them about the importance of screening, coordinating care, and providing emotional support.
“At the root of it all, it was quite clear that one thing that made the navigator successful was their interpersonal qualities and having someone that the patient could trust to help guide them through the process,” Dr. Baggett said.
The navigator program, however, stopped when the funding for the study ended.
But another health system has implemented navigators in a sustainable way through a quality improvement project. Michael Gieske, MD, director of lung cancer screening at St. Elizabeth Healthcare in Edgewood, Kentucky, starts his Friday morning meeting with a multidisciplinary group, including a thoracic surgeon, radiologist, pulmonologist, and several screening nurse navigators. They review the week’s chest CTs, with approximately one-third from patients who underwent lung cancer screening.
Nurse navigators at St. Elizabeth Healthcare follow up with any patient whose scan is suspicious for lung cancer and guide them through the process of seeing specialists and obtaining additional testing.
“They essentially hold the patient’s hand through this scary time in their life and make sure that everything flows smoothly and efficiently,” said Dr. Gieske, a family medicine physician.
St. Elizabeth’s program also draws on several evidence-based strategies used for other cancer screening programs, such as patient and provider education and quarterly feedback to their 194 primary care clinicians on rates of lung cancer screening among their eligible patients.
Several requirements for reimbursement for a lung cancer screening from the US Centers for Medicare & Medicaid Services can also serve as barriers to getting patients screened: Clinicians must identify who is eligible, provide tobacco cessation counseling, and document the shared decision-making process.
To streamline the steps, St. Elizabeth’s clinicians use an EMR smart set that reminds clinicians to verify smoking history and helps them document the required counseling.
Last year, 47% of eligible patients received their recommended screening, and Dr. Gieske said he expects even more improvement.
“We’re on track this year to complete 60% uptake if things continue,” he said, adding that 76% of the new cases of lung cancer are now diagnosed in stage I, with only 5% diagnosed in stage IV.
Dr. Gieske has shared his experience with many clinics in Appalachia, home to some of the highest rates of mortality from lung cancer in the country. A major part of his role with the Appalachian Community Cancer Alliance is helping educate primary care clinicians in the region about the importance of early detection of lung cancer.
“I think one of the most important things is just to convey a message of hope,” he said. “We’re trying to get the good word out there that if you screen individuals, you’re going to catch it early, when you have an extremely high chance of curing the lung cancer.”
Dr. Baggett reported support from grants from the ACS and the Massachusetts General Hospital Research Scholars Program. Dr. Sandler and Dr. Gieske reported no financial conflicts.
A version of this article first appeared on Medscape.com.
A few years ago, Kim Lori Sandler, MD, realized many patients newly diagnosed with lung cancer had never been screened for the disease — they received CT scans only because they were symptomatic.
But Dr. Sandler, a radiologist at Vanderbilt University Medical Center in Nashville, Tennessee, could see in medical charts that most of these patients had been eligible for a screening before becoming symptomatic. And for women, most had received decades worth of mammograms. She saw an opportunity and launched a study to find out if an intervention would work.
Low-dose CT and mammography services often are available in the same imaging facility, so women who qualified for a lung cancer screening were offered the scan during their mammography visit. Over a 3-year period, monthly rates of lung scans in women rose by 50% at one facility and 36% at the other.
“What we found is that women are really receptive, if you talk to them about it,” Dr. Sandler said. “I don’t think that lung cancer is thought of as a disease in women.”
Although lung cancer is the leading cause of cancer deaths in the United States, a recent study in JAMA Internal Medicine found only 18% of eligible patients were screened in 2022, a far cry from the rates of 72% for colon cancer — which itself falls short of goals from US medical groups like the American Cancer Society (ACS). Among those eligible, rates of lung screenings were lowest among younger people without comorbid conditions, who did not have health insurance or a usual source of care, and those living in southern states and states that did not expand Medicaid as part of the Affordable Care Act.
Getting patients screened is lifesaving: 27% of people with lung cancer survive 5 years after diagnosis. But the survival rate rises to 63% when cases are diagnosed at an early stage.
Increasing Uptake
The formal recommendation to use low-dose chest CT to screen for lung cancer is only a decade old. The approach was first endorsed by the United States Preventive Services Task Force (USPSTF) on the basis of an influential trial that found such testing was linked to a 20% reduction in mortality from the disease. Updated 2021 USPSTF guidelines call for annual screening of people aged 50-80 years who have a 20 pack-year history of smoking and currently smoke or have quit within the past 15 years.
But implementing the recommendation is not always simple. Unlike a colorectal or breast cancer screening, which is recommended primarily on patient age, eligibility for a lung cancer screening requires calculating pack-years of smoking, and, for past smokers, knowledge of when they quit.
The structured fields in most electronic medical records (EMRs) inquire about current or past use of cigarettes and the number of daily packs smoked. But few EMRs can calculate when a patient starts smoking two cigarettes a day but then increases to a pack a day and cuts down again. EMRs also do not track when a patient has stopped smoking permanently. Individual clinicians or health systems must identify patients who are eligible for screening, but the lack of automated calculations makes that job more difficult.
Dr. Sandler and colleagues turned to the informatics team at Vanderbilt to develop a natural language processing approach that extracts smoking data directly from clinician notes instead of using standard variables in their EMR.
The number of patients identified as needing a screening using the algorithm nearly doubled from baseline, from 5887 to 10,231 over a 3-year period, according to results from another study that Dr. Sandler published.
Although the algorithm may occasionally flag someone who does not need screening as eligible, “you can always have a conversation with the patient to determine if they actually meet eligibility criteria,” Dr. Sandler said.
Patient Navigators to the Rescue?
About a decade ago, Travis Baggett, MD, MPH, an associate professor of internal medicine at Harvard Medical School, Boston, Massachusetts, received pilot funding from the ACS to study cancer epidemiology among patients at Boston Health Care for the Homeless Program (BHCHP), which serves nearly 10,000 patients at a variety of Boston-area clinics each year.
“We found that both the incidence and mortality rates for lung cancer were more than twofold higher than in the general population,” Dr. Baggett, who is also the director of research at BHCHP, said.
He also discovered that BHCHP patients were diagnosed at significantly later stages than people in the general population for malignancies like breast and colorectal cancer.
Screening for lung cancer was a new recommendation at the time. With additional funding from the ACS, he launched a clinical trial in 2020 that randomized patients who were eligible for lung cancer screening to either work with a patient navigator or receive usual care.
The navigators eased the burden on primary care clinicians: They facilitated shared decision-making visits, helped participants make and attend appointments for low-dose CT, assisted with transportation, and arranged follow-up as needed.
The 3-year study found 43% of patients who received navigation services underwent screening for lung cancer, compared with 9% in the usual-care arm. Participants said the navigators played a critical role in educating them about the importance of screening, coordinating care, and providing emotional support.
“At the root of it all, it was quite clear that one thing that made the navigator successful was their interpersonal qualities and having someone that the patient could trust to help guide them through the process,” Dr. Baggett said.
The navigator program, however, stopped when the funding for the study ended.
But another health system has implemented navigators in a sustainable way through a quality improvement project. Michael Gieske, MD, director of lung cancer screening at St. Elizabeth Healthcare in Edgewood, Kentucky, starts his Friday morning meeting with a multidisciplinary group, including a thoracic surgeon, radiologist, pulmonologist, and several screening nurse navigators. They review the week’s chest CTs, with approximately one-third from patients who underwent lung cancer screening.
Nurse navigators at St. Elizabeth Healthcare follow up with any patient whose scan is suspicious for lung cancer and guide them through the process of seeing specialists and obtaining additional testing.
“They essentially hold the patient’s hand through this scary time in their life and make sure that everything flows smoothly and efficiently,” said Dr. Gieske, a family medicine physician.
St. Elizabeth’s program also draws on several evidence-based strategies used for other cancer screening programs, such as patient and provider education and quarterly feedback to their 194 primary care clinicians on rates of lung cancer screening among their eligible patients.
Several requirements for reimbursement for a lung cancer screening from the US Centers for Medicare & Medicaid Services can also serve as barriers to getting patients screened: Clinicians must identify who is eligible, provide tobacco cessation counseling, and document the shared decision-making process.
To streamline the steps, St. Elizabeth’s clinicians use an EMR smart set that reminds clinicians to verify smoking history and helps them document the required counseling.
Last year, 47% of eligible patients received their recommended screening, and Dr. Gieske said he expects even more improvement.
“We’re on track this year to complete 60% uptake if things continue,” he said, adding that 76% of the new cases of lung cancer are now diagnosed in stage I, with only 5% diagnosed in stage IV.
Dr. Gieske has shared his experience with many clinics in Appalachia, home to some of the highest rates of mortality from lung cancer in the country. A major part of his role with the Appalachian Community Cancer Alliance is helping educate primary care clinicians in the region about the importance of early detection of lung cancer.
“I think one of the most important things is just to convey a message of hope,” he said. “We’re trying to get the good word out there that if you screen individuals, you’re going to catch it early, when you have an extremely high chance of curing the lung cancer.”
Dr. Baggett reported support from grants from the ACS and the Massachusetts General Hospital Research Scholars Program. Dr. Sandler and Dr. Gieske reported no financial conflicts.
A version of this article first appeared on Medscape.com.
More Evidence PTSD Tied to Obstructive Sleep Apnea Risk
Posttraumatic stress disorder (PTSD) may enhance the risk for obstructive sleep apnea (OSA) in older male veterans, the results of a cross-sectional twin study suggested. However, additional high-quality research is needed and may yield important mechanistic insights into both conditions and improve treatment, experts said.
“The strength of the association was a bit surprising,” said study investigator Amit J. Shah, MD, MSCR, Emory University, Atlanta, Georgia. “Many physicians and scientists may otherwise assume that the relationship between PTSD and sleep apnea would be primarily mediated by obesity, but we did not find that obesity explained our findings.”
The study was published online in JAMA Network Open.
A More Rigorous Evaluation
“Prior studies have shown an association between PTSD and sleep apnea, but the size of the association was not as strong,” Dr. Shah said, possibly because many were based on symptomatic patients referred for clinical evaluation of OSA and some relied on self-report of a sleep apnea diagnosis.
The current study involved 181 male twins, aged 61-71 years, including 66 pairs discordant for PTSD symptoms and 15 pairs discordant for PTSD diagnosis, who were recruited from the Vietnam Era Twin Registry and underwent a formal psychiatric and polysomnography evaluation as follow-up of the Emory Twin Study.
PTSD symptom severity was assessed using the self-administered Posttraumatic Stress Disorder Checklist (PCL). OSA was mild in 74% of participants, moderate to severe in 40%, and severe in 18%.
The mean apnea-hypopnea index (AHI) was 17.7 events per hour, and the mean proportion of the night with SaO2 less than 90% was 8.9%.
In fully adjusted models, each 15-point within-pair difference in PCL score was associated with a 4.6 events-per-hour higher AHI, a 6.4 events-per-hour higher oxygen desaturation index, and a 4.8% greater sleep duration with SaO2 less than 90%.
A current PTSD diagnosis is associated with an approximate 10-unit higher adjusted AHI in separate models involving potential cardiovascular mediators (10.5-unit; 95% CI, 5.7-15.3) and sociodemographic and psychiatric confounders (10.7-unit; 95% CI, 4.0-17.4).
The investigators called for more research into the underlying mechanisms but speculated that pharyngeal collapsibility and exaggerated loop gain, among others, may play a role.
“Our findings broaden the concept of OSA as one that may involve stress pathways in addition to the traditional mechanisms involving airway collapse and obesity,” Dr. Shah said. “We should be more suspicious of OSA as an important comorbidity in PTSD, given the high OSA prevalence that we found in PTSD veterans.”
Questions Remain
In an accompanying editorial, Steven H. Woodward, PhD, and Ruth M. Benca, MD, PhD, VA Palo Alto Health Care Systems, Palo Alto, California, noted the study affirmatively answers the decades-old question of whether rates of OSA are elevated in PTSD and “eliminates many potential confounders that might cast doubt on the PTSD-OSA association.”
However, they noted, it’s difficult to ascertain the directionality of this association and point out that, in terms of potential mechanisms, the oft-cited 1994 study linking sleep fragmentation with upper airway collapsibility has never been replicated and that a recent study found no difference in airway collapsibility or evidence of differential loop gain in combat veterans with and without PTSD.
Dr. Woodward and Dr. Benca also highlighted the large body of evidence that psychiatric disorders such as bipolar disorder, schizophrenia, and, in particular, major depressive disorder, are strongly associated with higher rates of OSA.
“In sum, we do not believe that a fair reading of the current literature supports a conclusion that PTSD bears an association with OSA that does not overlap with those manifested by other psychiatric disorders,” they wrote.
“This commentary is not intended to discourage any specific line of inquiry. Rather, we seek to keep the door open as wide as possible to hypotheses and research designs aimed at elucidating the relationships between OSA and psychiatric disorders,” Dr. Woodward and Dr. Benca concluded.
In response, Dr. Shah said the editorialists’ “point about psychiatric conditions other than PTSD also being important in OSA is well taken. In our own cohort, we did not see such an association, but that does not mean that this does not exist.
“Autonomic physiology, which we plan to study next, may underlie not only the PTSD-OSA relationship but also the relationship between other psychiatric factors and OSA,” he added.
The study was funded by grants from the National Institutes of Health (NIH). One study author reported receiving personal fees from Idorsia, and another reported receiving personal fees from Clinilabs, Eisai, Ferring Pharmaceuticals, Huxley, Idorsia, and Merck Sharp & Dohme. Dr. Benca reported receiving grants from the NIH and Eisai and personal fees from Eisai, Idorsia, Haleon, and Sage Therapeutics. Dr. Woodward reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Posttraumatic stress disorder (PTSD) may enhance the risk for obstructive sleep apnea (OSA) in older male veterans, the results of a cross-sectional twin study suggested. However, additional high-quality research is needed and may yield important mechanistic insights into both conditions and improve treatment, experts said.
“The strength of the association was a bit surprising,” said study investigator Amit J. Shah, MD, MSCR, Emory University, Atlanta, Georgia. “Many physicians and scientists may otherwise assume that the relationship between PTSD and sleep apnea would be primarily mediated by obesity, but we did not find that obesity explained our findings.”
The study was published online in JAMA Network Open.
A More Rigorous Evaluation
“Prior studies have shown an association between PTSD and sleep apnea, but the size of the association was not as strong,” Dr. Shah said, possibly because many were based on symptomatic patients referred for clinical evaluation of OSA and some relied on self-report of a sleep apnea diagnosis.
The current study involved 181 male twins, aged 61-71 years, including 66 pairs discordant for PTSD symptoms and 15 pairs discordant for PTSD diagnosis, who were recruited from the Vietnam Era Twin Registry and underwent a formal psychiatric and polysomnography evaluation as follow-up of the Emory Twin Study.
PTSD symptom severity was assessed using the self-administered Posttraumatic Stress Disorder Checklist (PCL). OSA was mild in 74% of participants, moderate to severe in 40%, and severe in 18%.
The mean apnea-hypopnea index (AHI) was 17.7 events per hour, and the mean proportion of the night with SaO2 less than 90% was 8.9%.
In fully adjusted models, each 15-point within-pair difference in PCL score was associated with a 4.6 events-per-hour higher AHI, a 6.4 events-per-hour higher oxygen desaturation index, and a 4.8% greater sleep duration with SaO2 less than 90%.
A current PTSD diagnosis is associated with an approximate 10-unit higher adjusted AHI in separate models involving potential cardiovascular mediators (10.5-unit; 95% CI, 5.7-15.3) and sociodemographic and psychiatric confounders (10.7-unit; 95% CI, 4.0-17.4).
The investigators called for more research into the underlying mechanisms but speculated that pharyngeal collapsibility and exaggerated loop gain, among others, may play a role.
“Our findings broaden the concept of OSA as one that may involve stress pathways in addition to the traditional mechanisms involving airway collapse and obesity,” Dr. Shah said. “We should be more suspicious of OSA as an important comorbidity in PTSD, given the high OSA prevalence that we found in PTSD veterans.”
Questions Remain
In an accompanying editorial, Steven H. Woodward, PhD, and Ruth M. Benca, MD, PhD, VA Palo Alto Health Care Systems, Palo Alto, California, noted the study affirmatively answers the decades-old question of whether rates of OSA are elevated in PTSD and “eliminates many potential confounders that might cast doubt on the PTSD-OSA association.”
However, they noted, it’s difficult to ascertain the directionality of this association and point out that, in terms of potential mechanisms, the oft-cited 1994 study linking sleep fragmentation with upper airway collapsibility has never been replicated and that a recent study found no difference in airway collapsibility or evidence of differential loop gain in combat veterans with and without PTSD.
Dr. Woodward and Dr. Benca also highlighted the large body of evidence that psychiatric disorders such as bipolar disorder, schizophrenia, and, in particular, major depressive disorder, are strongly associated with higher rates of OSA.
“In sum, we do not believe that a fair reading of the current literature supports a conclusion that PTSD bears an association with OSA that does not overlap with those manifested by other psychiatric disorders,” they wrote.
“This commentary is not intended to discourage any specific line of inquiry. Rather, we seek to keep the door open as wide as possible to hypotheses and research designs aimed at elucidating the relationships between OSA and psychiatric disorders,” Dr. Woodward and Dr. Benca concluded.
In response, Dr. Shah said the editorialists’ “point about psychiatric conditions other than PTSD also being important in OSA is well taken. In our own cohort, we did not see such an association, but that does not mean that this does not exist.
“Autonomic physiology, which we plan to study next, may underlie not only the PTSD-OSA relationship but also the relationship between other psychiatric factors and OSA,” he added.
The study was funded by grants from the National Institutes of Health (NIH). One study author reported receiving personal fees from Idorsia, and another reported receiving personal fees from Clinilabs, Eisai, Ferring Pharmaceuticals, Huxley, Idorsia, and Merck Sharp & Dohme. Dr. Benca reported receiving grants from the NIH and Eisai and personal fees from Eisai, Idorsia, Haleon, and Sage Therapeutics. Dr. Woodward reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Posttraumatic stress disorder (PTSD) may enhance the risk for obstructive sleep apnea (OSA) in older male veterans, the results of a cross-sectional twin study suggested. However, additional high-quality research is needed and may yield important mechanistic insights into both conditions and improve treatment, experts said.
“The strength of the association was a bit surprising,” said study investigator Amit J. Shah, MD, MSCR, Emory University, Atlanta, Georgia. “Many physicians and scientists may otherwise assume that the relationship between PTSD and sleep apnea would be primarily mediated by obesity, but we did not find that obesity explained our findings.”
The study was published online in JAMA Network Open.
A More Rigorous Evaluation
“Prior studies have shown an association between PTSD and sleep apnea, but the size of the association was not as strong,” Dr. Shah said, possibly because many were based on symptomatic patients referred for clinical evaluation of OSA and some relied on self-report of a sleep apnea diagnosis.
The current study involved 181 male twins, aged 61-71 years, including 66 pairs discordant for PTSD symptoms and 15 pairs discordant for PTSD diagnosis, who were recruited from the Vietnam Era Twin Registry and underwent a formal psychiatric and polysomnography evaluation as follow-up of the Emory Twin Study.
PTSD symptom severity was assessed using the self-administered Posttraumatic Stress Disorder Checklist (PCL). OSA was mild in 74% of participants, moderate to severe in 40%, and severe in 18%.
The mean apnea-hypopnea index (AHI) was 17.7 events per hour, and the mean proportion of the night with SaO2 less than 90% was 8.9%.
In fully adjusted models, each 15-point within-pair difference in PCL score was associated with a 4.6 events-per-hour higher AHI, a 6.4 events-per-hour higher oxygen desaturation index, and a 4.8% greater sleep duration with SaO2 less than 90%.
A current PTSD diagnosis is associated with an approximate 10-unit higher adjusted AHI in separate models involving potential cardiovascular mediators (10.5-unit; 95% CI, 5.7-15.3) and sociodemographic and psychiatric confounders (10.7-unit; 95% CI, 4.0-17.4).
The investigators called for more research into the underlying mechanisms but speculated that pharyngeal collapsibility and exaggerated loop gain, among others, may play a role.
“Our findings broaden the concept of OSA as one that may involve stress pathways in addition to the traditional mechanisms involving airway collapse and obesity,” Dr. Shah said. “We should be more suspicious of OSA as an important comorbidity in PTSD, given the high OSA prevalence that we found in PTSD veterans.”
Questions Remain
In an accompanying editorial, Steven H. Woodward, PhD, and Ruth M. Benca, MD, PhD, VA Palo Alto Health Care Systems, Palo Alto, California, noted the study affirmatively answers the decades-old question of whether rates of OSA are elevated in PTSD and “eliminates many potential confounders that might cast doubt on the PTSD-OSA association.”
However, they noted, it’s difficult to ascertain the directionality of this association and point out that, in terms of potential mechanisms, the oft-cited 1994 study linking sleep fragmentation with upper airway collapsibility has never been replicated and that a recent study found no difference in airway collapsibility or evidence of differential loop gain in combat veterans with and without PTSD.
Dr. Woodward and Dr. Benca also highlighted the large body of evidence that psychiatric disorders such as bipolar disorder, schizophrenia, and, in particular, major depressive disorder, are strongly associated with higher rates of OSA.
“In sum, we do not believe that a fair reading of the current literature supports a conclusion that PTSD bears an association with OSA that does not overlap with those manifested by other psychiatric disorders,” they wrote.
“This commentary is not intended to discourage any specific line of inquiry. Rather, we seek to keep the door open as wide as possible to hypotheses and research designs aimed at elucidating the relationships between OSA and psychiatric disorders,” Dr. Woodward and Dr. Benca concluded.
In response, Dr. Shah said the editorialists’ “point about psychiatric conditions other than PTSD also being important in OSA is well taken. In our own cohort, we did not see such an association, but that does not mean that this does not exist.
“Autonomic physiology, which we plan to study next, may underlie not only the PTSD-OSA relationship but also the relationship between other psychiatric factors and OSA,” he added.
The study was funded by grants from the National Institutes of Health (NIH). One study author reported receiving personal fees from Idorsia, and another reported receiving personal fees from Clinilabs, Eisai, Ferring Pharmaceuticals, Huxley, Idorsia, and Merck Sharp & Dohme. Dr. Benca reported receiving grants from the NIH and Eisai and personal fees from Eisai, Idorsia, Haleon, and Sage Therapeutics. Dr. Woodward reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
MUC-1 vaccine associated with notable overall survival rates in breast cancer
“This is the first successful study of a breast cancer vaccine to date,” Christian F. Singer, MD, said during an interview. Dr. Singer, the lead author of the new study, presented the results during a poster session at the 2024 annual meeting of the American Society of Clinical Oncology (ASCO).
Previously known as both liposomal BLP25 and Stimuvax, tecemotide is an antigen-specific immunotherapy that targets the cancer therapy–resistant MUC-1 glycoprotein, which is overexpressed in over 90% of breast cancers. Tecemotide also has been shown to moderately improve overall survival rates in non–small cell lung cancer.
“We are not at all surprised by the results of this study in breast cancer,” Gregory T. Wurz, PhD, senior researcher at RCU Labs in Lincoln, California, said in an interview.
Dr. Wurz is coauthor of several studies on peptide vaccines, including a mouse model study of human MUC-1–expressing mammary tumors showing that tecemotide combined with letrozole had additive antitumor activity. Another paper he coauthored showed that ospemifene enhanced the immune response to tecemotide in both tumor-bearing and non–tumor-bearing mice. These findings, combined with other research, led to the creation of a patented method of combining therapies to enhance the efficacy of immunotherapy in the treatment of cancer and infectious diseases. Dr. Wurz was not involved in the new research that Dr. Singer presented at ASCO.
Study Methods and Results
Dr. Singer, head of obstetrics and gynecology at the Medical University of Vienna, Vienna, Austria, and coauthors randomized 400 patients with HER2-negative early breast cancer in a prospective, multicenter, two-arm, phase 2 ABCSG 34 trial to receive preoperative standard of care (SOC) neoadjuvant treatment with or without tecemotide.
Postmenopausal women with luminal A tumors were given 6 months of letrozole as SOC. Postmenopausal patients with triple-negative breast cancer, luminal B tumors, in whom chemotherapy was SOC, as well as all premenopausal study participants, were given four cycles of both epirubicin cyclophosphamide and docetaxel every 3 weeks.
The study’s primary endpoint was the residual cancer burden at the time of surgery.
Long-term outcomes were measured as part of a translational project, while distant relapse-free survival (DRFS) and overall survival (OS) were analyzed with Cox regression models. Long-term outcome data were available for 291 women, of whom 236 had received chemotherapy as SOC.
While tecemotide plus neoadjuvant SOC was not associated with a significant increase in residual cancer burden (RCB) at the time of surgery (36.4% vs 31.5%; P = .42; 40.5% vs 34.8%; P = .37 for the chemotherapy-only cohort), follow-up at 7 years showed 80.8% of patients who had received SOC plus tecemotide were still alive and free from metastasis.
In patients who had received SOC alone, the OS rate at 7 years with no metastasis was 64.7% (hazard ratio [HR] for DRFS, 0.53; 95% CI, 0.34-0.83; P = .005). The OS rate for the study group was 83.0% vs 68.2% in the non-tecemotide cohort (HR for OS, 0.53; 95% CI, 0.33-0.85; P = .008).
The lack of RCB signal at the endpoints, “tells us that pathologic complete response and residual cancer burden simply are not adequate endpoints for cancer vaccination studies and we need to find other predictive/prognostic markers, said Dr. Singer. “We are currently looking into this in exploratory studies.”
The chemotherapy plus tecemotide cohort had a notable outcome with a DRFS of 81.9% vs 65.0% in the SOC group (HR, 0.50; 95% CI, 0.31-0.83; P = .007), and an OS rate of 83.6% vs 67.8% (HR, 0.51; 95% CI, 0.30-0.88; P = .016).
Dr. Singer characterized the HRs as intriguing, saying that they “pave the way for new trials.”
Ideas for Further Study of Tecemotide
“What we would like to see next for tecemotide are clinical studies that explore whether immunomodulatory agents can further enhance the response to tecemotide in lung, breast, and potentially other MUC-1–expressing cancers,” Dr. Wurz said.
Future phase 3 studies of MUC-1 cancer vaccines, possibly those using mRNA technology, are yet to come, according to Dr. Singer. “We also need to find out why the vaccine works sometimes and sometimes not.”
Dr. Singer disclosed financial ties to AstraZeneca/MedImmune, Daiichi Sankyo Europe, Novartis, Gilead Sciences, Sanofi/Aventis, Amgen, Myriad Genetics, and Roche. Dr. Wurz had no disclosures, but his research partner and founder of RCU Labs, Michael De Gregorio, is the sole inventor of the patent referenced in the story. That patent has been assigned to the Regents of the University of California.
“This is the first successful study of a breast cancer vaccine to date,” Christian F. Singer, MD, said during an interview. Dr. Singer, the lead author of the new study, presented the results during a poster session at the 2024 annual meeting of the American Society of Clinical Oncology (ASCO).
Previously known as both liposomal BLP25 and Stimuvax, tecemotide is an antigen-specific immunotherapy that targets the cancer therapy–resistant MUC-1 glycoprotein, which is overexpressed in over 90% of breast cancers. Tecemotide also has been shown to moderately improve overall survival rates in non–small cell lung cancer.
“We are not at all surprised by the results of this study in breast cancer,” Gregory T. Wurz, PhD, senior researcher at RCU Labs in Lincoln, California, said in an interview.
Dr. Wurz is coauthor of several studies on peptide vaccines, including a mouse model study of human MUC-1–expressing mammary tumors showing that tecemotide combined with letrozole had additive antitumor activity. Another paper he coauthored showed that ospemifene enhanced the immune response to tecemotide in both tumor-bearing and non–tumor-bearing mice. These findings, combined with other research, led to the creation of a patented method of combining therapies to enhance the efficacy of immunotherapy in the treatment of cancer and infectious diseases. Dr. Wurz was not involved in the new research that Dr. Singer presented at ASCO.
Study Methods and Results
Dr. Singer, head of obstetrics and gynecology at the Medical University of Vienna, Vienna, Austria, and coauthors randomized 400 patients with HER2-negative early breast cancer in a prospective, multicenter, two-arm, phase 2 ABCSG 34 trial to receive preoperative standard of care (SOC) neoadjuvant treatment with or without tecemotide.
Postmenopausal women with luminal A tumors were given 6 months of letrozole as SOC. Postmenopausal patients with triple-negative breast cancer, luminal B tumors, in whom chemotherapy was SOC, as well as all premenopausal study participants, were given four cycles of both epirubicin cyclophosphamide and docetaxel every 3 weeks.
The study’s primary endpoint was the residual cancer burden at the time of surgery.
Long-term outcomes were measured as part of a translational project, while distant relapse-free survival (DRFS) and overall survival (OS) were analyzed with Cox regression models. Long-term outcome data were available for 291 women, of whom 236 had received chemotherapy as SOC.
While tecemotide plus neoadjuvant SOC was not associated with a significant increase in residual cancer burden (RCB) at the time of surgery (36.4% vs 31.5%; P = .42; 40.5% vs 34.8%; P = .37 for the chemotherapy-only cohort), follow-up at 7 years showed 80.8% of patients who had received SOC plus tecemotide were still alive and free from metastasis.
In patients who had received SOC alone, the OS rate at 7 years with no metastasis was 64.7% (hazard ratio [HR] for DRFS, 0.53; 95% CI, 0.34-0.83; P = .005). The OS rate for the study group was 83.0% vs 68.2% in the non-tecemotide cohort (HR for OS, 0.53; 95% CI, 0.33-0.85; P = .008).
The lack of RCB signal at the endpoints, “tells us that pathologic complete response and residual cancer burden simply are not adequate endpoints for cancer vaccination studies and we need to find other predictive/prognostic markers, said Dr. Singer. “We are currently looking into this in exploratory studies.”
The chemotherapy plus tecemotide cohort had a notable outcome with a DRFS of 81.9% vs 65.0% in the SOC group (HR, 0.50; 95% CI, 0.31-0.83; P = .007), and an OS rate of 83.6% vs 67.8% (HR, 0.51; 95% CI, 0.30-0.88; P = .016).
Dr. Singer characterized the HRs as intriguing, saying that they “pave the way for new trials.”
Ideas for Further Study of Tecemotide
“What we would like to see next for tecemotide are clinical studies that explore whether immunomodulatory agents can further enhance the response to tecemotide in lung, breast, and potentially other MUC-1–expressing cancers,” Dr. Wurz said.
Future phase 3 studies of MUC-1 cancer vaccines, possibly those using mRNA technology, are yet to come, according to Dr. Singer. “We also need to find out why the vaccine works sometimes and sometimes not.”
Dr. Singer disclosed financial ties to AstraZeneca/MedImmune, Daiichi Sankyo Europe, Novartis, Gilead Sciences, Sanofi/Aventis, Amgen, Myriad Genetics, and Roche. Dr. Wurz had no disclosures, but his research partner and founder of RCU Labs, Michael De Gregorio, is the sole inventor of the patent referenced in the story. That patent has been assigned to the Regents of the University of California.
“This is the first successful study of a breast cancer vaccine to date,” Christian F. Singer, MD, said during an interview. Dr. Singer, the lead author of the new study, presented the results during a poster session at the 2024 annual meeting of the American Society of Clinical Oncology (ASCO).
Previously known as both liposomal BLP25 and Stimuvax, tecemotide is an antigen-specific immunotherapy that targets the cancer therapy–resistant MUC-1 glycoprotein, which is overexpressed in over 90% of breast cancers. Tecemotide also has been shown to moderately improve overall survival rates in non–small cell lung cancer.
“We are not at all surprised by the results of this study in breast cancer,” Gregory T. Wurz, PhD, senior researcher at RCU Labs in Lincoln, California, said in an interview.
Dr. Wurz is coauthor of several studies on peptide vaccines, including a mouse model study of human MUC-1–expressing mammary tumors showing that tecemotide combined with letrozole had additive antitumor activity. Another paper he coauthored showed that ospemifene enhanced the immune response to tecemotide in both tumor-bearing and non–tumor-bearing mice. These findings, combined with other research, led to the creation of a patented method of combining therapies to enhance the efficacy of immunotherapy in the treatment of cancer and infectious diseases. Dr. Wurz was not involved in the new research that Dr. Singer presented at ASCO.
Study Methods and Results
Dr. Singer, head of obstetrics and gynecology at the Medical University of Vienna, Vienna, Austria, and coauthors randomized 400 patients with HER2-negative early breast cancer in a prospective, multicenter, two-arm, phase 2 ABCSG 34 trial to receive preoperative standard of care (SOC) neoadjuvant treatment with or without tecemotide.
Postmenopausal women with luminal A tumors were given 6 months of letrozole as SOC. Postmenopausal patients with triple-negative breast cancer, luminal B tumors, in whom chemotherapy was SOC, as well as all premenopausal study participants, were given four cycles of both epirubicin cyclophosphamide and docetaxel every 3 weeks.
The study’s primary endpoint was the residual cancer burden at the time of surgery.
Long-term outcomes were measured as part of a translational project, while distant relapse-free survival (DRFS) and overall survival (OS) were analyzed with Cox regression models. Long-term outcome data were available for 291 women, of whom 236 had received chemotherapy as SOC.
While tecemotide plus neoadjuvant SOC was not associated with a significant increase in residual cancer burden (RCB) at the time of surgery (36.4% vs 31.5%; P = .42; 40.5% vs 34.8%; P = .37 for the chemotherapy-only cohort), follow-up at 7 years showed 80.8% of patients who had received SOC plus tecemotide were still alive and free from metastasis.
In patients who had received SOC alone, the OS rate at 7 years with no metastasis was 64.7% (hazard ratio [HR] for DRFS, 0.53; 95% CI, 0.34-0.83; P = .005). The OS rate for the study group was 83.0% vs 68.2% in the non-tecemotide cohort (HR for OS, 0.53; 95% CI, 0.33-0.85; P = .008).
The lack of RCB signal at the endpoints, “tells us that pathologic complete response and residual cancer burden simply are not adequate endpoints for cancer vaccination studies and we need to find other predictive/prognostic markers, said Dr. Singer. “We are currently looking into this in exploratory studies.”
The chemotherapy plus tecemotide cohort had a notable outcome with a DRFS of 81.9% vs 65.0% in the SOC group (HR, 0.50; 95% CI, 0.31-0.83; P = .007), and an OS rate of 83.6% vs 67.8% (HR, 0.51; 95% CI, 0.30-0.88; P = .016).
Dr. Singer characterized the HRs as intriguing, saying that they “pave the way for new trials.”
Ideas for Further Study of Tecemotide
“What we would like to see next for tecemotide are clinical studies that explore whether immunomodulatory agents can further enhance the response to tecemotide in lung, breast, and potentially other MUC-1–expressing cancers,” Dr. Wurz said.
Future phase 3 studies of MUC-1 cancer vaccines, possibly those using mRNA technology, are yet to come, according to Dr. Singer. “We also need to find out why the vaccine works sometimes and sometimes not.”
Dr. Singer disclosed financial ties to AstraZeneca/MedImmune, Daiichi Sankyo Europe, Novartis, Gilead Sciences, Sanofi/Aventis, Amgen, Myriad Genetics, and Roche. Dr. Wurz had no disclosures, but his research partner and founder of RCU Labs, Michael De Gregorio, is the sole inventor of the patent referenced in the story. That patent has been assigned to the Regents of the University of California.
FROM ASCO 2024
Neurofilament Light Chain Detects Early Chemotherapy-Related Neurotoxicity
Investigators found Nfl levels increased in cancer patients following a first infusion of the medication paclitaxel and corresponded to neuropathy severity 6-12 months post-treatment, suggesting the blood protein may provide an early CIPN biomarker.
“Nfl after a single cycle could detect axonal degeneration,” said lead investigator Masarra Joda, a researcher and PhD candidate at the University of Sydney in Australia. She added that “quantification of Nfl may provide a clinically useful marker of emerging neurotoxicity in patients vulnerable to CIPN.”
The findings were presented at the Peripheral Nerve Society (PNS) 2024 annual meeting.
Common, Burdensome Side Effect
A common side effect of chemotherapy, CIPN manifests as sensory neuropathy and causes degeneration of the peripheral axons. A protein biomarker of axonal degeneration, Nfl has previously been investigated as a way of identifying patients at risk of CIPN.
The goal of the current study was to identify the potential link between Nfl with neurophysiological markers of axon degeneration in patients receiving the neurotoxin chemotherapy paclitaxel.
The study included 93 cancer patients. All were assessed at the beginning, middle, and end of treatment. CIPN was assessed using blood samples of Nfl and the Total Neuropathy Score (TNS), the Common Terminology Criteria for Adverse Events (CTCAE) neuropathy scale, and patient-reported measures using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire–Chemotherapy-Induced Peripheral Neuropathy Module (EORTC-CIPN20).
Axonal degeneration was measured with neurophysiological tests including sural nerve compound sensory action potential (CSAP) for the lower limbs, and sensory median nerve CSAP, as well as stimulus threshold testing, for the upper limbs.
Almost all of study participants (97%) were female. The majority (66%) had breast cancer and 30% had gynecological cancer. Most (73%) were receiving a weekly regimen of paclitaxel, and the remainder were treated with taxanes plus platinum once every 3 weeks. By the end of treatment, 82% of the patients had developed CIPN, which was mild in 44% and moderate/severe in 38%.
Nfl levels increased significantly from baseline to after the first dose of chemotherapy (P < .001), “highlighting that nerve damage occurs from the very beginning of treatment,” senior investigator Susanna Park, PhD, told this news organization.
In addition, “patients with higher Nfl levels after a single paclitaxel treatment had greater neuropathy at the end of treatment (higher EORTC scores [P ≤ .026], and higher TNS scores [P ≤ .00]),” added Dr. Park, who is associate professor at the University of Sydney.
“Importantly, we also looked at long-term outcomes beyond the end of chemotherapy, because chronic neuropathy produces a significant burden in cancer survivors,” said Dr. Park.
“Among a total of 44 patients who completed the 6- to 12-month post-treatment follow-up, NfL levels after a single treatment were linked to severity of nerve damage quantified with neurophysiological tests, and greater Nfl levels at mid-treatment were correlated with worse patient and neurologically graded neuropathy at 6-12 months.”
Dr. Park said the results suggest that NfL may provide a biomarker of long-term axon damage and that Nfl assays “may enable clinicians to evaluate the risk of long-term toxicity early during paclitaxel treatment to hopefully provide clinically significant information to guide better treatment titration.”
Currently, she said, CIPN is a prominent cause of dose reduction and early chemotherapy cessation.
“For example, in early breast cancer around 25% of patients experience a dose reduction due to the severity of neuropathy symptoms.” But, she said, “there is no standardized way of identifying which patients are at risk of long-term neuropathy and therefore, may benefit more from dose reduction. In this setting, a biomarker such as Nfl could provide oncologists with more information about the risk of long-term toxicity and take that into account in dose decision-making.”
For some cancers, she added, there are multiple potential therapy options.
“A biomarker such as NfL could assist in determining risk-benefit profile in terms of switching to alternate therapies. However, further studies will be needed to fully define the utility of NfL as a biomarker of paclitaxel neuropathy.”
Promising Research
Commenting on the research for this news organization, Maryam Lustberg, MD, associate professor, director of the Center for Breast Cancer at Smilow Cancer Hospital and Yale Cancer Center, and chief of Breast Medical Oncology at Yale Cancer Center, in New Haven, Connecticut, said the study “builds on a body of work previously reported by others showing that neurofilament light chains as detected in the blood can be associated with early signs of neurotoxic injury.”
She added that the research “is promising, since existing clinical and patient-reported measures tend to under-detect chemotherapy-induced neuropathy until more permanent injury might have occurred.”
Dr. Lustberg, who is immediate past president of the Multinational Association of Supportive Care in Cancer, said future studies are needed before Nfl testing can be implemented in routine practice, but that “early detection will allow earlier initiation of supportive care strategies such as physical therapy and exercise, as well as dose modifications, which may be helpful for preventing permanent damage and improving quality of life.”
The investigators and Dr. Lustberg report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Investigators found Nfl levels increased in cancer patients following a first infusion of the medication paclitaxel and corresponded to neuropathy severity 6-12 months post-treatment, suggesting the blood protein may provide an early CIPN biomarker.
“Nfl after a single cycle could detect axonal degeneration,” said lead investigator Masarra Joda, a researcher and PhD candidate at the University of Sydney in Australia. She added that “quantification of Nfl may provide a clinically useful marker of emerging neurotoxicity in patients vulnerable to CIPN.”
The findings were presented at the Peripheral Nerve Society (PNS) 2024 annual meeting.
Common, Burdensome Side Effect
A common side effect of chemotherapy, CIPN manifests as sensory neuropathy and causes degeneration of the peripheral axons. A protein biomarker of axonal degeneration, Nfl has previously been investigated as a way of identifying patients at risk of CIPN.
The goal of the current study was to identify the potential link between Nfl with neurophysiological markers of axon degeneration in patients receiving the neurotoxin chemotherapy paclitaxel.
The study included 93 cancer patients. All were assessed at the beginning, middle, and end of treatment. CIPN was assessed using blood samples of Nfl and the Total Neuropathy Score (TNS), the Common Terminology Criteria for Adverse Events (CTCAE) neuropathy scale, and patient-reported measures using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire–Chemotherapy-Induced Peripheral Neuropathy Module (EORTC-CIPN20).
Axonal degeneration was measured with neurophysiological tests including sural nerve compound sensory action potential (CSAP) for the lower limbs, and sensory median nerve CSAP, as well as stimulus threshold testing, for the upper limbs.
Almost all of study participants (97%) were female. The majority (66%) had breast cancer and 30% had gynecological cancer. Most (73%) were receiving a weekly regimen of paclitaxel, and the remainder were treated with taxanes plus platinum once every 3 weeks. By the end of treatment, 82% of the patients had developed CIPN, which was mild in 44% and moderate/severe in 38%.
Nfl levels increased significantly from baseline to after the first dose of chemotherapy (P < .001), “highlighting that nerve damage occurs from the very beginning of treatment,” senior investigator Susanna Park, PhD, told this news organization.
In addition, “patients with higher Nfl levels after a single paclitaxel treatment had greater neuropathy at the end of treatment (higher EORTC scores [P ≤ .026], and higher TNS scores [P ≤ .00]),” added Dr. Park, who is associate professor at the University of Sydney.
“Importantly, we also looked at long-term outcomes beyond the end of chemotherapy, because chronic neuropathy produces a significant burden in cancer survivors,” said Dr. Park.
“Among a total of 44 patients who completed the 6- to 12-month post-treatment follow-up, NfL levels after a single treatment were linked to severity of nerve damage quantified with neurophysiological tests, and greater Nfl levels at mid-treatment were correlated with worse patient and neurologically graded neuropathy at 6-12 months.”
Dr. Park said the results suggest that NfL may provide a biomarker of long-term axon damage and that Nfl assays “may enable clinicians to evaluate the risk of long-term toxicity early during paclitaxel treatment to hopefully provide clinically significant information to guide better treatment titration.”
Currently, she said, CIPN is a prominent cause of dose reduction and early chemotherapy cessation.
“For example, in early breast cancer around 25% of patients experience a dose reduction due to the severity of neuropathy symptoms.” But, she said, “there is no standardized way of identifying which patients are at risk of long-term neuropathy and therefore, may benefit more from dose reduction. In this setting, a biomarker such as Nfl could provide oncologists with more information about the risk of long-term toxicity and take that into account in dose decision-making.”
For some cancers, she added, there are multiple potential therapy options.
“A biomarker such as NfL could assist in determining risk-benefit profile in terms of switching to alternate therapies. However, further studies will be needed to fully define the utility of NfL as a biomarker of paclitaxel neuropathy.”
Promising Research
Commenting on the research for this news organization, Maryam Lustberg, MD, associate professor, director of the Center for Breast Cancer at Smilow Cancer Hospital and Yale Cancer Center, and chief of Breast Medical Oncology at Yale Cancer Center, in New Haven, Connecticut, said the study “builds on a body of work previously reported by others showing that neurofilament light chains as detected in the blood can be associated with early signs of neurotoxic injury.”
She added that the research “is promising, since existing clinical and patient-reported measures tend to under-detect chemotherapy-induced neuropathy until more permanent injury might have occurred.”
Dr. Lustberg, who is immediate past president of the Multinational Association of Supportive Care in Cancer, said future studies are needed before Nfl testing can be implemented in routine practice, but that “early detection will allow earlier initiation of supportive care strategies such as physical therapy and exercise, as well as dose modifications, which may be helpful for preventing permanent damage and improving quality of life.”
The investigators and Dr. Lustberg report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Investigators found Nfl levels increased in cancer patients following a first infusion of the medication paclitaxel and corresponded to neuropathy severity 6-12 months post-treatment, suggesting the blood protein may provide an early CIPN biomarker.
“Nfl after a single cycle could detect axonal degeneration,” said lead investigator Masarra Joda, a researcher and PhD candidate at the University of Sydney in Australia. She added that “quantification of Nfl may provide a clinically useful marker of emerging neurotoxicity in patients vulnerable to CIPN.”
The findings were presented at the Peripheral Nerve Society (PNS) 2024 annual meeting.
Common, Burdensome Side Effect
A common side effect of chemotherapy, CIPN manifests as sensory neuropathy and causes degeneration of the peripheral axons. A protein biomarker of axonal degeneration, Nfl has previously been investigated as a way of identifying patients at risk of CIPN.
The goal of the current study was to identify the potential link between Nfl with neurophysiological markers of axon degeneration in patients receiving the neurotoxin chemotherapy paclitaxel.
The study included 93 cancer patients. All were assessed at the beginning, middle, and end of treatment. CIPN was assessed using blood samples of Nfl and the Total Neuropathy Score (TNS), the Common Terminology Criteria for Adverse Events (CTCAE) neuropathy scale, and patient-reported measures using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire–Chemotherapy-Induced Peripheral Neuropathy Module (EORTC-CIPN20).
Axonal degeneration was measured with neurophysiological tests including sural nerve compound sensory action potential (CSAP) for the lower limbs, and sensory median nerve CSAP, as well as stimulus threshold testing, for the upper limbs.
Almost all of study participants (97%) were female. The majority (66%) had breast cancer and 30% had gynecological cancer. Most (73%) were receiving a weekly regimen of paclitaxel, and the remainder were treated with taxanes plus platinum once every 3 weeks. By the end of treatment, 82% of the patients had developed CIPN, which was mild in 44% and moderate/severe in 38%.
Nfl levels increased significantly from baseline to after the first dose of chemotherapy (P < .001), “highlighting that nerve damage occurs from the very beginning of treatment,” senior investigator Susanna Park, PhD, told this news organization.
In addition, “patients with higher Nfl levels after a single paclitaxel treatment had greater neuropathy at the end of treatment (higher EORTC scores [P ≤ .026], and higher TNS scores [P ≤ .00]),” added Dr. Park, who is associate professor at the University of Sydney.
“Importantly, we also looked at long-term outcomes beyond the end of chemotherapy, because chronic neuropathy produces a significant burden in cancer survivors,” said Dr. Park.
“Among a total of 44 patients who completed the 6- to 12-month post-treatment follow-up, NfL levels after a single treatment were linked to severity of nerve damage quantified with neurophysiological tests, and greater Nfl levels at mid-treatment were correlated with worse patient and neurologically graded neuropathy at 6-12 months.”
Dr. Park said the results suggest that NfL may provide a biomarker of long-term axon damage and that Nfl assays “may enable clinicians to evaluate the risk of long-term toxicity early during paclitaxel treatment to hopefully provide clinically significant information to guide better treatment titration.”
Currently, she said, CIPN is a prominent cause of dose reduction and early chemotherapy cessation.
“For example, in early breast cancer around 25% of patients experience a dose reduction due to the severity of neuropathy symptoms.” But, she said, “there is no standardized way of identifying which patients are at risk of long-term neuropathy and therefore, may benefit more from dose reduction. In this setting, a biomarker such as Nfl could provide oncologists with more information about the risk of long-term toxicity and take that into account in dose decision-making.”
For some cancers, she added, there are multiple potential therapy options.
“A biomarker such as NfL could assist in determining risk-benefit profile in terms of switching to alternate therapies. However, further studies will be needed to fully define the utility of NfL as a biomarker of paclitaxel neuropathy.”
Promising Research
Commenting on the research for this news organization, Maryam Lustberg, MD, associate professor, director of the Center for Breast Cancer at Smilow Cancer Hospital and Yale Cancer Center, and chief of Breast Medical Oncology at Yale Cancer Center, in New Haven, Connecticut, said the study “builds on a body of work previously reported by others showing that neurofilament light chains as detected in the blood can be associated with early signs of neurotoxic injury.”
She added that the research “is promising, since existing clinical and patient-reported measures tend to under-detect chemotherapy-induced neuropathy until more permanent injury might have occurred.”
Dr. Lustberg, who is immediate past president of the Multinational Association of Supportive Care in Cancer, said future studies are needed before Nfl testing can be implemented in routine practice, but that “early detection will allow earlier initiation of supportive care strategies such as physical therapy and exercise, as well as dose modifications, which may be helpful for preventing permanent damage and improving quality of life.”
The investigators and Dr. Lustberg report no relevant financial relationships.
A version of this article appeared on Medscape.com.
AT PNS 2024
New Trials in Lung Cancer: Could Your Patients Benefit?
Resected stage II, IIIA, or IIIB with nodal involvement non–small cell lung cancer (NSCLC). Adult patients with this type of cancer can join a randomized, controlled, phase 3 study assessing whether an investigational drug called V940 added to pembrolizumab (Keytruda) delays cancer recurrence better than pembrolizumab alone.
V940 is an individualized neoantigen therapy designed to generate T-cell antitumor responses targeted to a patient’s specific mutation profile.
V940 plus pembrolizumab showed a trend toward longer recurrence-free survival vs pembrolizumab alone in a recent phase 2 study in melanoma (hazard ratio, 0.561; P = .053).
In the current trial, one group of participants will receive intramuscular injections of V940 every 3 weeks plus intravenous (IV) pembrolizumab every 6 weeks for up to approximately 1 year or until disease recurrence or unacceptable toxicity, whichever happens first. The other people in the trial will be on the same schedule, with a placebo replacing V940.
Centers in Florida, Georgia, Kentucky, Montana, New Jersey, New York, North Dakota, and six other countries started recruiting for the trial’s 868 participants in December 2023. Disease-free survival is the primary endpoint. Overall survival over approximately 12 years and quality of life (QoL) are secondary endpoints. More details at clinicaltrials.gov.
Metastatic NSCLC with a programmed cell death ligand 1 (PD-L1)–tumor proportion score of > 50%. Adults in this clinical situation are eligible for a randomized, open-label, phase 3 trial to determine whether an experimental antibody-drug conjugate called MK-2870 added to standard pembrolizumab prolongs survival.
MK-2870 delivers a cytotoxin to cancer cells by binding to trophoblast cell-surface antigen 2, known to promote tumor cell growth and metastasis. For up to 2 years, half of participants will receive MK-2870 by IV every 2 weeks plus IV pembrolizumab every 6 weeks. The other group will receive only pembrolizumab.
In December 2023, study sites in Georgia, Minnesota, Mississippi, Nevada, Oregon, Australia, Denmark, Taiwan, and Turkey started seeking the trial’s 614 participants. Overall survival over approximately 4 years is the primary endpoint; QoL is a secondary endpoint. More details at clinicaltrials.gov.
Untreated locally advanced or metastatic NSCLC with KRAS G12C mutations. Individuals with this type of lung cancer may be interested in a randomized, controlled, phase 3 study examining whether an experimental oral KRAS G12C inhibitor called LY3537982 boosts the effectiveness of standard treatment and patients can tolerate the combination. Currently approved KRAS G12C inhibitors sotorasib (Lumakras, Lumykras) and adagrasib (Krazati) are indicated for second-line treatment; this trial may lead to a first-line approval for newcomer LY3537982.
The trial has three parts: dose optimization, safety, and efficacy. During dose optimization, each participant will take one of two oral doses of LY3537982 and receive IV pembrolizumab every 3 weeks. In the safety phase, all participants will receive oral LY3537982 at the chosen dose plus standard therapy of 3-times-weekly IV pembrolizumab, pemetrexed, and a platinum therapy (cisplatin or carboplatin). In the experimental phase, for up to about 1 year, participants will receive one of these four options: Pembrolizumab plus LY3537982, pembrolizumab plus a placebo, standard therapy plus LY3537982, or standard therapy plus a placebo.
The study, which is planning to recruit 1016 participants, opened across 16 US states and 12 countries worldwide in December 2023. Sites in 11 more US states, the District of Columbia, Brazil, Canada, China, India, and 11 more European countries are gearing up. Adverse events and progression-free survival are the primary endpoints. Overall survival over approximately 3 years and QoL are secondary endpoints. More details at clinicaltrials.gov.
Unresectable, untreated locally advanced or metastatic non-squamous NSCLC with human epidermal growth factor receptor 2 (HER2) mutations. People with this diagnosis who have HER2 mutations instead of KRAS G12C mutations can participate in a phase 3 study comparing an investigational oral first-line treatment with standard IV therapy. The drug in this study, zongertinib, is a HER2 tyrosine kinase inhibitor.
For up to approximately 4 years, one group of participants will take oral zongertinib only, and the other individuals will receive IV pembrolizumab, pemetrexed, and a platinum agent (cisplatin or carboplatin). Study sites in California, Missouri, South Carolina, Australia, China, Japan, South Korea, and Singapore opened in January ready to welcome 270 participants. Progression-free survival is the primary outcome. Overall survival over 53 months and QoL are secondary endpoints. More details at clinicaltrials.gov.
Completely resected stage IIB, IIIA, or select IIIB, PD-L1–positive NSCLC. Adults with this type of lung cancer who have received adjuvant platinum-based chemotherapy may be eligible for a randomized, controlled, phase 3 study to assess whether two immune checkpoint inhibitors are better than one at delaying cancer recurrence. In this trial, tiragolumab will be added to the approved PD-L1 inhibitor atezolizumab (Tecentriq).
A recent study, however, found that tiragolumab did not confer an additional benefit when added to atezolizumab, carboplatin, and etoposide in untreated extensive-stage small cell lung cancer.
In the current trial, one group of participants will receive IV atezolizumab and tiragolumab, while the other people will receive a placebo instead of tiragolumab. Centers in California, Georgia, Illinois, New Mexico, Australia, China, South Korea, and Taiwan started recruiting for the trial’s 1150 participants in March 2024. Disease-free survival is the primary endpoint. Overall survival over approximately 15 years and QoL are secondary outcomes. More details at clinicaltrials.gov.
Previously treated metastatic or non-operable non-squamous NSCLC. Adults in this position who have received no more than one platinum-based chemotherapy and one anti–PD-L1 drug are sought for a randomized, open-label, phase 3 trial comparing second-line standard docetaxel with experimental antibody-drug conjugate sigvotatug vedotin. Patients who have tumors with certain treatable genomic alterations must have received at least one drug targeted to that alteration, as well as a platinum-based agent.
Approximately half the participants will receive sigvotatug vedotin by IV every 2 weeks, and the other half will receive IV docetaxel every 3 weeks. The study opened in March across 13 US states, France, Hungary, Poland, and Spain seeking 600 people eligible to participate. The primary outcomes are overall survival over approximately 5 years and objective response rate. QoL is a secondary outcome. More details at clinicaltrials.gov.All trial information is from the National Institutes of Health US National Library of Medicine (online at clinicaltrials.gov).
A version of this article appeared on Medscape.com .
Resected stage II, IIIA, or IIIB with nodal involvement non–small cell lung cancer (NSCLC). Adult patients with this type of cancer can join a randomized, controlled, phase 3 study assessing whether an investigational drug called V940 added to pembrolizumab (Keytruda) delays cancer recurrence better than pembrolizumab alone.
V940 is an individualized neoantigen therapy designed to generate T-cell antitumor responses targeted to a patient’s specific mutation profile.
V940 plus pembrolizumab showed a trend toward longer recurrence-free survival vs pembrolizumab alone in a recent phase 2 study in melanoma (hazard ratio, 0.561; P = .053).
In the current trial, one group of participants will receive intramuscular injections of V940 every 3 weeks plus intravenous (IV) pembrolizumab every 6 weeks for up to approximately 1 year or until disease recurrence or unacceptable toxicity, whichever happens first. The other people in the trial will be on the same schedule, with a placebo replacing V940.
Centers in Florida, Georgia, Kentucky, Montana, New Jersey, New York, North Dakota, and six other countries started recruiting for the trial’s 868 participants in December 2023. Disease-free survival is the primary endpoint. Overall survival over approximately 12 years and quality of life (QoL) are secondary endpoints. More details at clinicaltrials.gov.
Metastatic NSCLC with a programmed cell death ligand 1 (PD-L1)–tumor proportion score of > 50%. Adults in this clinical situation are eligible for a randomized, open-label, phase 3 trial to determine whether an experimental antibody-drug conjugate called MK-2870 added to standard pembrolizumab prolongs survival.
MK-2870 delivers a cytotoxin to cancer cells by binding to trophoblast cell-surface antigen 2, known to promote tumor cell growth and metastasis. For up to 2 years, half of participants will receive MK-2870 by IV every 2 weeks plus IV pembrolizumab every 6 weeks. The other group will receive only pembrolizumab.
In December 2023, study sites in Georgia, Minnesota, Mississippi, Nevada, Oregon, Australia, Denmark, Taiwan, and Turkey started seeking the trial’s 614 participants. Overall survival over approximately 4 years is the primary endpoint; QoL is a secondary endpoint. More details at clinicaltrials.gov.
Untreated locally advanced or metastatic NSCLC with KRAS G12C mutations. Individuals with this type of lung cancer may be interested in a randomized, controlled, phase 3 study examining whether an experimental oral KRAS G12C inhibitor called LY3537982 boosts the effectiveness of standard treatment and patients can tolerate the combination. Currently approved KRAS G12C inhibitors sotorasib (Lumakras, Lumykras) and adagrasib (Krazati) are indicated for second-line treatment; this trial may lead to a first-line approval for newcomer LY3537982.
The trial has three parts: dose optimization, safety, and efficacy. During dose optimization, each participant will take one of two oral doses of LY3537982 and receive IV pembrolizumab every 3 weeks. In the safety phase, all participants will receive oral LY3537982 at the chosen dose plus standard therapy of 3-times-weekly IV pembrolizumab, pemetrexed, and a platinum therapy (cisplatin or carboplatin). In the experimental phase, for up to about 1 year, participants will receive one of these four options: Pembrolizumab plus LY3537982, pembrolizumab plus a placebo, standard therapy plus LY3537982, or standard therapy plus a placebo.
The study, which is planning to recruit 1016 participants, opened across 16 US states and 12 countries worldwide in December 2023. Sites in 11 more US states, the District of Columbia, Brazil, Canada, China, India, and 11 more European countries are gearing up. Adverse events and progression-free survival are the primary endpoints. Overall survival over approximately 3 years and QoL are secondary endpoints. More details at clinicaltrials.gov.
Unresectable, untreated locally advanced or metastatic non-squamous NSCLC with human epidermal growth factor receptor 2 (HER2) mutations. People with this diagnosis who have HER2 mutations instead of KRAS G12C mutations can participate in a phase 3 study comparing an investigational oral first-line treatment with standard IV therapy. The drug in this study, zongertinib, is a HER2 tyrosine kinase inhibitor.
For up to approximately 4 years, one group of participants will take oral zongertinib only, and the other individuals will receive IV pembrolizumab, pemetrexed, and a platinum agent (cisplatin or carboplatin). Study sites in California, Missouri, South Carolina, Australia, China, Japan, South Korea, and Singapore opened in January ready to welcome 270 participants. Progression-free survival is the primary outcome. Overall survival over 53 months and QoL are secondary endpoints. More details at clinicaltrials.gov.
Completely resected stage IIB, IIIA, or select IIIB, PD-L1–positive NSCLC. Adults with this type of lung cancer who have received adjuvant platinum-based chemotherapy may be eligible for a randomized, controlled, phase 3 study to assess whether two immune checkpoint inhibitors are better than one at delaying cancer recurrence. In this trial, tiragolumab will be added to the approved PD-L1 inhibitor atezolizumab (Tecentriq).
A recent study, however, found that tiragolumab did not confer an additional benefit when added to atezolizumab, carboplatin, and etoposide in untreated extensive-stage small cell lung cancer.
In the current trial, one group of participants will receive IV atezolizumab and tiragolumab, while the other people will receive a placebo instead of tiragolumab. Centers in California, Georgia, Illinois, New Mexico, Australia, China, South Korea, and Taiwan started recruiting for the trial’s 1150 participants in March 2024. Disease-free survival is the primary endpoint. Overall survival over approximately 15 years and QoL are secondary outcomes. More details at clinicaltrials.gov.
Previously treated metastatic or non-operable non-squamous NSCLC. Adults in this position who have received no more than one platinum-based chemotherapy and one anti–PD-L1 drug are sought for a randomized, open-label, phase 3 trial comparing second-line standard docetaxel with experimental antibody-drug conjugate sigvotatug vedotin. Patients who have tumors with certain treatable genomic alterations must have received at least one drug targeted to that alteration, as well as a platinum-based agent.
Approximately half the participants will receive sigvotatug vedotin by IV every 2 weeks, and the other half will receive IV docetaxel every 3 weeks. The study opened in March across 13 US states, France, Hungary, Poland, and Spain seeking 600 people eligible to participate. The primary outcomes are overall survival over approximately 5 years and objective response rate. QoL is a secondary outcome. More details at clinicaltrials.gov.All trial information is from the National Institutes of Health US National Library of Medicine (online at clinicaltrials.gov).
A version of this article appeared on Medscape.com .
Resected stage II, IIIA, or IIIB with nodal involvement non–small cell lung cancer (NSCLC). Adult patients with this type of cancer can join a randomized, controlled, phase 3 study assessing whether an investigational drug called V940 added to pembrolizumab (Keytruda) delays cancer recurrence better than pembrolizumab alone.
V940 is an individualized neoantigen therapy designed to generate T-cell antitumor responses targeted to a patient’s specific mutation profile.
V940 plus pembrolizumab showed a trend toward longer recurrence-free survival vs pembrolizumab alone in a recent phase 2 study in melanoma (hazard ratio, 0.561; P = .053).
In the current trial, one group of participants will receive intramuscular injections of V940 every 3 weeks plus intravenous (IV) pembrolizumab every 6 weeks for up to approximately 1 year or until disease recurrence or unacceptable toxicity, whichever happens first. The other people in the trial will be on the same schedule, with a placebo replacing V940.
Centers in Florida, Georgia, Kentucky, Montana, New Jersey, New York, North Dakota, and six other countries started recruiting for the trial’s 868 participants in December 2023. Disease-free survival is the primary endpoint. Overall survival over approximately 12 years and quality of life (QoL) are secondary endpoints. More details at clinicaltrials.gov.
Metastatic NSCLC with a programmed cell death ligand 1 (PD-L1)–tumor proportion score of > 50%. Adults in this clinical situation are eligible for a randomized, open-label, phase 3 trial to determine whether an experimental antibody-drug conjugate called MK-2870 added to standard pembrolizumab prolongs survival.
MK-2870 delivers a cytotoxin to cancer cells by binding to trophoblast cell-surface antigen 2, known to promote tumor cell growth and metastasis. For up to 2 years, half of participants will receive MK-2870 by IV every 2 weeks plus IV pembrolizumab every 6 weeks. The other group will receive only pembrolizumab.
In December 2023, study sites in Georgia, Minnesota, Mississippi, Nevada, Oregon, Australia, Denmark, Taiwan, and Turkey started seeking the trial’s 614 participants. Overall survival over approximately 4 years is the primary endpoint; QoL is a secondary endpoint. More details at clinicaltrials.gov.
Untreated locally advanced or metastatic NSCLC with KRAS G12C mutations. Individuals with this type of lung cancer may be interested in a randomized, controlled, phase 3 study examining whether an experimental oral KRAS G12C inhibitor called LY3537982 boosts the effectiveness of standard treatment and patients can tolerate the combination. Currently approved KRAS G12C inhibitors sotorasib (Lumakras, Lumykras) and adagrasib (Krazati) are indicated for second-line treatment; this trial may lead to a first-line approval for newcomer LY3537982.
The trial has three parts: dose optimization, safety, and efficacy. During dose optimization, each participant will take one of two oral doses of LY3537982 and receive IV pembrolizumab every 3 weeks. In the safety phase, all participants will receive oral LY3537982 at the chosen dose plus standard therapy of 3-times-weekly IV pembrolizumab, pemetrexed, and a platinum therapy (cisplatin or carboplatin). In the experimental phase, for up to about 1 year, participants will receive one of these four options: Pembrolizumab plus LY3537982, pembrolizumab plus a placebo, standard therapy plus LY3537982, or standard therapy plus a placebo.
The study, which is planning to recruit 1016 participants, opened across 16 US states and 12 countries worldwide in December 2023. Sites in 11 more US states, the District of Columbia, Brazil, Canada, China, India, and 11 more European countries are gearing up. Adverse events and progression-free survival are the primary endpoints. Overall survival over approximately 3 years and QoL are secondary endpoints. More details at clinicaltrials.gov.
Unresectable, untreated locally advanced or metastatic non-squamous NSCLC with human epidermal growth factor receptor 2 (HER2) mutations. People with this diagnosis who have HER2 mutations instead of KRAS G12C mutations can participate in a phase 3 study comparing an investigational oral first-line treatment with standard IV therapy. The drug in this study, zongertinib, is a HER2 tyrosine kinase inhibitor.
For up to approximately 4 years, one group of participants will take oral zongertinib only, and the other individuals will receive IV pembrolizumab, pemetrexed, and a platinum agent (cisplatin or carboplatin). Study sites in California, Missouri, South Carolina, Australia, China, Japan, South Korea, and Singapore opened in January ready to welcome 270 participants. Progression-free survival is the primary outcome. Overall survival over 53 months and QoL are secondary endpoints. More details at clinicaltrials.gov.
Completely resected stage IIB, IIIA, or select IIIB, PD-L1–positive NSCLC. Adults with this type of lung cancer who have received adjuvant platinum-based chemotherapy may be eligible for a randomized, controlled, phase 3 study to assess whether two immune checkpoint inhibitors are better than one at delaying cancer recurrence. In this trial, tiragolumab will be added to the approved PD-L1 inhibitor atezolizumab (Tecentriq).
A recent study, however, found that tiragolumab did not confer an additional benefit when added to atezolizumab, carboplatin, and etoposide in untreated extensive-stage small cell lung cancer.
In the current trial, one group of participants will receive IV atezolizumab and tiragolumab, while the other people will receive a placebo instead of tiragolumab. Centers in California, Georgia, Illinois, New Mexico, Australia, China, South Korea, and Taiwan started recruiting for the trial’s 1150 participants in March 2024. Disease-free survival is the primary endpoint. Overall survival over approximately 15 years and QoL are secondary outcomes. More details at clinicaltrials.gov.
Previously treated metastatic or non-operable non-squamous NSCLC. Adults in this position who have received no more than one platinum-based chemotherapy and one anti–PD-L1 drug are sought for a randomized, open-label, phase 3 trial comparing second-line standard docetaxel with experimental antibody-drug conjugate sigvotatug vedotin. Patients who have tumors with certain treatable genomic alterations must have received at least one drug targeted to that alteration, as well as a platinum-based agent.
Approximately half the participants will receive sigvotatug vedotin by IV every 2 weeks, and the other half will receive IV docetaxel every 3 weeks. The study opened in March across 13 US states, France, Hungary, Poland, and Spain seeking 600 people eligible to participate. The primary outcomes are overall survival over approximately 5 years and objective response rate. QoL is a secondary outcome. More details at clinicaltrials.gov.All trial information is from the National Institutes of Health US National Library of Medicine (online at clinicaltrials.gov).
A version of this article appeared on Medscape.com .
CMS Announces End to Cyberattack Relief Program
The Centers for Medicare & Medicaid Services (CMS) has announced the conclusion of a program that provided billions in early Medicare payments to those affected by the Change Healthcare/UnitedHealth Group cyberattack last winter.
CMS reported that the program advanced more than $2.55 billion in Medicare payments to > 4200 Part A providers, including hospitals, and more than $717.18 million in payments to Part B suppliers such as physicians, nonphysician practitioners, and durable medical equipment suppliers.
According to CMS, the Medicare billing system is now functioning properly, and 96% of the early payments have been recovered. The advances were to represent ≤ 30 days of typical claims payments in a 3-month period of 2023, with full repayment expected within 90 days through “automatic recoupment from Medicare claims” — no extensions allowed.
The agency took a victory lap regarding its response. “In the face of one of the most widespread cyberattacks on the US health care industry, CMS promptly took action to get providers and suppliers access to the funds they needed to continue providing patients with vital care,” CMS Administrator Chiquita Brooks-LaSure said in a statement. “Our efforts helped minimize the disruptive fallout from this incident, and we will remain vigilant to be ready to address future events.”
Ongoing Concerns from Health Care Organizations
Ben Teicher, an American Hospital Association spokesman, said that the organization hopes that CMS will be responsive if there’s more need for action after the advance payment program expires. The organization represents about 5000 hospitals, health care systems, and other providers.
“Our members report that the aftereffects of this event will likely be felt throughout the remainder of the year,” he said. According to Teicher, hospitals remain concerned about their ability to process claims and appeal denials, the safety of reconnecting to cyber services, and access to information needed to bill patients and reconcile payments.
In addition, hospitals are concerned about “financial support to mitigate the considerable costs incurred as a result of the cyberattack,” he said.
Charlene MacDonald, executive vice-president of public affairs at the Federation of American Hospitals, which represents more than 1000 for-profit hospitals, sent a statement to this news organization that said some providers “are still feeling the effects of care denials and delays caused by insurer inaction.
“We appreciate that the Administration acted within its authority to support providers during this unprecedented crisis and blunt these devastating impacts, especially because a vast majority of managed care companies failed to step up to the plate,” she said. “It is now time to shift our focus to holding plans accountable for using tactics to delay and deny needed patient care.”
Cyberattack Impact and Response
The ransom-based cyberattack against Change Healthcare/UnitedHealth Group targeted an electronic data interchange clearing house processing payer reimbursement systems, disrupting cash flows at hospitals and medical practices, and affecting patient access to prescriptions and life-saving therapy.
Change Healthcare — part of the UnitedHealth Group subsidiary Optum — processes half of all medical claims, according to a Department of Justice lawsuit. The American Hospital Association described the cyberattack as “the most significant and consequential incident of its kind” in US history.
By late March, UnitedHealth Group said nearly all medical and pharmacy claims were processing properly, while a deputy secretary of the US Department of Health & Human Services told clinicians that officials were focusing on the last group of clinicians who were facing cash-flow problems.
Still, a senior advisor with CMS told providers at that time that “we have heard from so many providers over the last several weeks who are really struggling to make ends meet right now or who are worried that they will not be able to make payroll in the weeks to come.”
Randy Dotinga is a freelance health/medical reporter and board member of the Association of Health Care Journalists.
A version of this article appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) has announced the conclusion of a program that provided billions in early Medicare payments to those affected by the Change Healthcare/UnitedHealth Group cyberattack last winter.
CMS reported that the program advanced more than $2.55 billion in Medicare payments to > 4200 Part A providers, including hospitals, and more than $717.18 million in payments to Part B suppliers such as physicians, nonphysician practitioners, and durable medical equipment suppliers.
According to CMS, the Medicare billing system is now functioning properly, and 96% of the early payments have been recovered. The advances were to represent ≤ 30 days of typical claims payments in a 3-month period of 2023, with full repayment expected within 90 days through “automatic recoupment from Medicare claims” — no extensions allowed.
The agency took a victory lap regarding its response. “In the face of one of the most widespread cyberattacks on the US health care industry, CMS promptly took action to get providers and suppliers access to the funds they needed to continue providing patients with vital care,” CMS Administrator Chiquita Brooks-LaSure said in a statement. “Our efforts helped minimize the disruptive fallout from this incident, and we will remain vigilant to be ready to address future events.”
Ongoing Concerns from Health Care Organizations
Ben Teicher, an American Hospital Association spokesman, said that the organization hopes that CMS will be responsive if there’s more need for action after the advance payment program expires. The organization represents about 5000 hospitals, health care systems, and other providers.
“Our members report that the aftereffects of this event will likely be felt throughout the remainder of the year,” he said. According to Teicher, hospitals remain concerned about their ability to process claims and appeal denials, the safety of reconnecting to cyber services, and access to information needed to bill patients and reconcile payments.
In addition, hospitals are concerned about “financial support to mitigate the considerable costs incurred as a result of the cyberattack,” he said.
Charlene MacDonald, executive vice-president of public affairs at the Federation of American Hospitals, which represents more than 1000 for-profit hospitals, sent a statement to this news organization that said some providers “are still feeling the effects of care denials and delays caused by insurer inaction.
“We appreciate that the Administration acted within its authority to support providers during this unprecedented crisis and blunt these devastating impacts, especially because a vast majority of managed care companies failed to step up to the plate,” she said. “It is now time to shift our focus to holding plans accountable for using tactics to delay and deny needed patient care.”
Cyberattack Impact and Response
The ransom-based cyberattack against Change Healthcare/UnitedHealth Group targeted an electronic data interchange clearing house processing payer reimbursement systems, disrupting cash flows at hospitals and medical practices, and affecting patient access to prescriptions and life-saving therapy.
Change Healthcare — part of the UnitedHealth Group subsidiary Optum — processes half of all medical claims, according to a Department of Justice lawsuit. The American Hospital Association described the cyberattack as “the most significant and consequential incident of its kind” in US history.
By late March, UnitedHealth Group said nearly all medical and pharmacy claims were processing properly, while a deputy secretary of the US Department of Health & Human Services told clinicians that officials were focusing on the last group of clinicians who were facing cash-flow problems.
Still, a senior advisor with CMS told providers at that time that “we have heard from so many providers over the last several weeks who are really struggling to make ends meet right now or who are worried that they will not be able to make payroll in the weeks to come.”
Randy Dotinga is a freelance health/medical reporter and board member of the Association of Health Care Journalists.
A version of this article appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) has announced the conclusion of a program that provided billions in early Medicare payments to those affected by the Change Healthcare/UnitedHealth Group cyberattack last winter.
CMS reported that the program advanced more than $2.55 billion in Medicare payments to > 4200 Part A providers, including hospitals, and more than $717.18 million in payments to Part B suppliers such as physicians, nonphysician practitioners, and durable medical equipment suppliers.
According to CMS, the Medicare billing system is now functioning properly, and 96% of the early payments have been recovered. The advances were to represent ≤ 30 days of typical claims payments in a 3-month period of 2023, with full repayment expected within 90 days through “automatic recoupment from Medicare claims” — no extensions allowed.
The agency took a victory lap regarding its response. “In the face of one of the most widespread cyberattacks on the US health care industry, CMS promptly took action to get providers and suppliers access to the funds they needed to continue providing patients with vital care,” CMS Administrator Chiquita Brooks-LaSure said in a statement. “Our efforts helped minimize the disruptive fallout from this incident, and we will remain vigilant to be ready to address future events.”
Ongoing Concerns from Health Care Organizations
Ben Teicher, an American Hospital Association spokesman, said that the organization hopes that CMS will be responsive if there’s more need for action after the advance payment program expires. The organization represents about 5000 hospitals, health care systems, and other providers.
“Our members report that the aftereffects of this event will likely be felt throughout the remainder of the year,” he said. According to Teicher, hospitals remain concerned about their ability to process claims and appeal denials, the safety of reconnecting to cyber services, and access to information needed to bill patients and reconcile payments.
In addition, hospitals are concerned about “financial support to mitigate the considerable costs incurred as a result of the cyberattack,” he said.
Charlene MacDonald, executive vice-president of public affairs at the Federation of American Hospitals, which represents more than 1000 for-profit hospitals, sent a statement to this news organization that said some providers “are still feeling the effects of care denials and delays caused by insurer inaction.
“We appreciate that the Administration acted within its authority to support providers during this unprecedented crisis and blunt these devastating impacts, especially because a vast majority of managed care companies failed to step up to the plate,” she said. “It is now time to shift our focus to holding plans accountable for using tactics to delay and deny needed patient care.”
Cyberattack Impact and Response
The ransom-based cyberattack against Change Healthcare/UnitedHealth Group targeted an electronic data interchange clearing house processing payer reimbursement systems, disrupting cash flows at hospitals and medical practices, and affecting patient access to prescriptions and life-saving therapy.
Change Healthcare — part of the UnitedHealth Group subsidiary Optum — processes half of all medical claims, according to a Department of Justice lawsuit. The American Hospital Association described the cyberattack as “the most significant and consequential incident of its kind” in US history.
By late March, UnitedHealth Group said nearly all medical and pharmacy claims were processing properly, while a deputy secretary of the US Department of Health & Human Services told clinicians that officials were focusing on the last group of clinicians who were facing cash-flow problems.
Still, a senior advisor with CMS told providers at that time that “we have heard from so many providers over the last several weeks who are really struggling to make ends meet right now or who are worried that they will not be able to make payroll in the weeks to come.”
Randy Dotinga is a freelance health/medical reporter and board member of the Association of Health Care Journalists.
A version of this article appeared on Medscape.com.
Is This Journal Legit? Predatory Publishers
This transcript has been edited for clarity.
Andrew N. Wilner, MD: My guest today is Dr. Jose Merino, editor in chief of the Neurology family of journals and professor of neurology and co-vice chair of education at Georgetown University in Washington, DC.
Our program today is a follow-up of Dr. Merino’s presentation at the recent American Academy of Neurology meeting in Denver, Colorado. Along with two other panelists, Dr. Merino discussed the role of open-access publication and the dangers of predatory journals.
Jose G. Merino, MD, MPhil: Thank you for having me here. It’s a pleasure.
Open Access Defined
Dr. Wilner: I remember when publication in neurology was pretty straightforward. It was either the green journal or the blue journal, but things have certainly changed. I think one topic that is not clear to everyone is this concept of open access. Could you define that for us?
Dr. Merino: Sure. Open access is a mode of publication that fosters more open or accessible science. The idea of open access is that it combines two main elements. One is that the papers that are published become immediately available to anybody with an internet connection anywhere in the world without any restrictions.
The second important element from open access, which makes it different from other models we can talk about, is the fact that the authors retain the copyright of their work, but they give the journal and readers a license to use, reproduce, and modify the content.
This is different, for example, from instances where we have funder mandates. For example, NIH papers have to become available 6 months after publication, so they’re available to everybody but not immediately.
Dr. Wilner: I remember that when a journal article was published, say, in Neurology, if you didn’t have a subscription to Neurology, you went to the library that hopefully had a subscription.
If they didn’t have it, you would write to the author and say, “Hey, I heard you have this great paper because the abstract was out there. Could you send me a reprint?” Has that whole universe evaporated?
Dr. Merino: It depends on how the paper is published. For example, in Neurology, some of the research we publish is open access. Basically, if you have an internet connection, you can access the paper.
That’s the case for papers published in our wholly open-access journals in the Neurology family like Neurology Neuroimmunology & Neuroinflammation, Neurology Genetics, or Neurology Education.
For other papers that are published in Neurology, not under open access, there is a paywall. For some of them, the paywall comes down after a few months based on funder mandates and so on. As I was mentioning, the NIH-funded papers are available 6 months later.
In the first 6 months, you may have to go to your library, and if your library has a subscription, you can download it directly. [This is also true for] those that always stay behind the paywall, where you have to have a subscription or your library has to have a subscription.
Is Pay to Publish a Red Flag?
Dr. Wilner: I’m a professional writer. With any luck, when I write something, I get paid to write it. There’s been a long tradition in academic medicine that when you submit an article to, say, Neurology, you don’t get paid as an author for the publication. Your reward is the honor of it being published.
Neurology supports itself in various ways, including advertising and so on. That’s been the contract: free publication for work that merits it, and the journal survives on its own.
With open access, one of the things that’s happened is that — and I’ve published open access myself — is that I get a notification that I need to pay to have my article that I’ve slaved over published. Explain that, please.
Dr. Merino: This is the issue with open access. As I mentioned, the paper gets published. You’re giving the journal a license to publish it. You’re retaining the copyright of your work. That means that the journal cannot make money or support itself by just publishing open access because they belong to you.
Typically, open-access journals are not in print and don’t have much in terms of advertising. The contract is you’re giving me a license to publish it, but it’s your journal, so you’re paying a fee for the journal expenses to basically produce your paper. That’s what’s happening with open access.
That’s been recognized with many funders, for example, with NIH funding or many of the European funders, they’re including open-access fees as part of their funding for research. Now, of course, this doesn’t help if you’re not a funded researcher or if you’re a fellow who’s doing work and so on.
Typically, most journals will have waived fees or lower fees for these situations. The reason for the open-access fee is the fact that you’re retaining the copyright. You’re not giving it to the journal who can then use it to generate its revenue for supporting itself, the editorial staff, and so on.
Dr. Wilner: This idea of charging for publication has created a satellite business of what are called predatory journals. How does one know if the open-access journal that I’m submitting to is really just in the business of wanting my $300 or my $900 to get published? How do I know if that’s a reasonable place to publish?
Predatory Journals
Dr. Merino: That’s a big challenge that has come with this whole idea of open access and the fact that now, many journals are online only, so you’re no longer seeing a physical copy. That has given rise to the predatory journals.
The predatory journal, by definition, is a journal that claims to be open access. They’ll take your paper and publish it, but they don’t provide all the other services that you would typically expect from the fact that you’re paying an open-access fee. This includes getting appropriate peer review, production of the manuscript, and long-term curation and storage of the manuscript.
Many predatory journals will take your open-access fee, accept any paper that you submit, regardless of the quality, because they’re charging the fees for that. They don’t send it to real peer review, and then in a few months, the journal disappears so there’s no way for anybody to actually find your paper anymore.
There are certain checklists. Dr. David Moher at the University of Toronto has produced some work trying to help us identify predatory journals.
One thing I typically suggest to people who ask me this question is: Have you ever heard of this journal before? Does the journal have a track record? How far back does the story of the journal go? Is it supported by a publisher that you know? Do you know anybody who has published there? Is it something you can easily access?
If in doubt, always ask your friendly medical librarian. There used to be lists that were kept in terms of predatory journals that were being constantly updated, but those had to be shut down. As far as I understand, there were legal issues in terms of how things got on that list.
I think that overall, if you’ve heard of it, if it’s relevant, if it’s known in your field, and if your librarian knows it, it’s probably a good legitimate open-access journal. There are many very good legitimate open-access journals.
I mentioned the two that we have in our family, but all the other major journals have their own open-access journal within their family. There are some, like BMC or PLOS, that are completely open-access and legitimate journals.
Impact Factor
Dr. Wilner: What about impact factor? Many journals boast about their impact factor. I’m not sure how to interpret that number.
Dr. Merino: Impact factor is very interesting. The impact factor was developed by medical librarians to try to identify the journals they should be subscribing to. It’s a measure of the average citations to an average paper in the journal.
It doesn’t tell you about specific papers. It tells you, on average, how many of the papers in this journal get cited so many times. It’s calculated by the number of articles that were cited divided by the number of articles that were published. Journals that publish many papers, like Neurology, have a hard time bringing up their impact factor beyond a certain level.
Similarly, very small journals with one or two very highly cited papers have a very high impact factor. It’s being used as a measure, perhaps inappropriately, of how good or how reputable a journal is. We all say we don’t care about journal impact factors, but we all know our journal impact factor and we used to know it to three decimals. Now, they changed the system, and there’s only one decimal point, which makes more sense.
This is more important, for example, for authors when deciding where to submit papers. I know that in some countries, particularly in Europe, the impact factor of the journal where you publish has an impact on your promotion decisions.
I would say what’s even more important than the impact factor, is to say, “Well, is this the journal that fits the scope of my paper? Is this the journal that reaches the audience that I want to reach when I write my paper?”
There are some papers, for example, that are very influential. The impact factor just captures citations. There are some papers that are very influential that may not get cited very often. There may be papers that change clinical practice.
If you read a paper that tells you that you should be changing how you treat your patients with myasthenia based on this paper, that may not get cited. It’s a very clinically focused paper, but it’s probably more impactful than one that gets cited very much in some respect, or they make it to public policy decisions, and so on.
I think it’s important to look more at the audience and the journal scope when you submit your papers.
Dr. Wilner: One other technical question. The journals also say they’re indexed in PubMed or Google Scholar. If I want to publish my paper and I want it indexed where the right people are going to find it, where does it need to be indexed?
Dr. Merino: I grew up using Index Medicus, MedlinePlus, and the Library of Science. I still do. If I need to find something, I go to PubMed. Ideally, papers are listed in MedlinePlus or can be found in PubMed. They’re not the same thing, but you can find them through them.
That would be an important thing. Nowadays, a lot more people are using Google Scholar or Google just to identify papers. It may be a little bit less relevant, but it’s still a measure of the quality of the journal before they get indexed in some of these. For example, if you get listed in MedlinePlus, it has gone through certain quality checks by the index itself to see whether they would accept the journal or not. That’s something you want to check.
Typically, most of the large journals or the journals you and I know about are listed in more than one place, right? They’re listed in Scopus and Web of Science. They’re listed in MedlinePlus and so on. Again, if you’re submitting your paper, go somewhere where you know the journal and you’ve heard about it.
Dr. Wilner: I’m not going to ask you about artificial intelligence. We can do that another time. I want to ask something closer to me, which is this question of publish or perish.
There seems to be, in academics, more emphasis on the number of papers that one has published rather than their quality. How does a younger academician or one who really needs to publish cope with that?
Dr. Merino: Many people are writing up research that may not be relevant or that may not be high quality just because you need to have a long list of papers to get promoted, for example, if you’re an academician.
Doug Altman, who was a very influential person in the field quality of not only medical statistics but also medical publishing, had the idea that we need less research, but we need better research.
We often receive papers where you say, well, what’s the rationale behind the question in this paper? It’s like they had a large amount of data and were trying to squeeze as much as they could out of that. I think, as a young academician, the important thing to think about is whether it is an important question that matters to you and to the field, from whatever perspective, whether it’s going to advance research, advance clinical care, or have public policy implications.
Is this one where the answer will be important no matter what the answer is? If you’re thinking of that, your work will be well recognized, people will know you, and you’ll get invited to collaborate. I think that’s the most important thing rather than just churning out a large number of papers.
The productivity will come from the fact that you start by saying, let me ask something that’s really meaningful to me and to the field, with a good question and using strong research methodology.
Dr. Wilner: Thanks for that, Dr. Merino. I think that’s very valuable for all of us. This has been a great discussion. Do you have any final comments before we wrap up?
Dr. Merino: I want to encourage people to continue reading medical journals all the time and submitting to us, again, good research and important questions with robust methodology. That’s what we’re looking for in Neurology and most serious medical journals.
Dr. Wilner is an associate professor of neurology at the University of Tennessee Health Science Center, Memphis. Dr. Merino is a professor in the department of neurology at Georgetown University Medical Center, Washington, DC. Dr. Wilner reported conflicts of interest with Accordant Health Services and Lulu Publishing. Dr. Merino reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Andrew N. Wilner, MD: My guest today is Dr. Jose Merino, editor in chief of the Neurology family of journals and professor of neurology and co-vice chair of education at Georgetown University in Washington, DC.
Our program today is a follow-up of Dr. Merino’s presentation at the recent American Academy of Neurology meeting in Denver, Colorado. Along with two other panelists, Dr. Merino discussed the role of open-access publication and the dangers of predatory journals.
Jose G. Merino, MD, MPhil: Thank you for having me here. It’s a pleasure.
Open Access Defined
Dr. Wilner: I remember when publication in neurology was pretty straightforward. It was either the green journal or the blue journal, but things have certainly changed. I think one topic that is not clear to everyone is this concept of open access. Could you define that for us?
Dr. Merino: Sure. Open access is a mode of publication that fosters more open or accessible science. The idea of open access is that it combines two main elements. One is that the papers that are published become immediately available to anybody with an internet connection anywhere in the world without any restrictions.
The second important element from open access, which makes it different from other models we can talk about, is the fact that the authors retain the copyright of their work, but they give the journal and readers a license to use, reproduce, and modify the content.
This is different, for example, from instances where we have funder mandates. For example, NIH papers have to become available 6 months after publication, so they’re available to everybody but not immediately.
Dr. Wilner: I remember that when a journal article was published, say, in Neurology, if you didn’t have a subscription to Neurology, you went to the library that hopefully had a subscription.
If they didn’t have it, you would write to the author and say, “Hey, I heard you have this great paper because the abstract was out there. Could you send me a reprint?” Has that whole universe evaporated?
Dr. Merino: It depends on how the paper is published. For example, in Neurology, some of the research we publish is open access. Basically, if you have an internet connection, you can access the paper.
That’s the case for papers published in our wholly open-access journals in the Neurology family like Neurology Neuroimmunology & Neuroinflammation, Neurology Genetics, or Neurology Education.
For other papers that are published in Neurology, not under open access, there is a paywall. For some of them, the paywall comes down after a few months based on funder mandates and so on. As I was mentioning, the NIH-funded papers are available 6 months later.
In the first 6 months, you may have to go to your library, and if your library has a subscription, you can download it directly. [This is also true for] those that always stay behind the paywall, where you have to have a subscription or your library has to have a subscription.
Is Pay to Publish a Red Flag?
Dr. Wilner: I’m a professional writer. With any luck, when I write something, I get paid to write it. There’s been a long tradition in academic medicine that when you submit an article to, say, Neurology, you don’t get paid as an author for the publication. Your reward is the honor of it being published.
Neurology supports itself in various ways, including advertising and so on. That’s been the contract: free publication for work that merits it, and the journal survives on its own.
With open access, one of the things that’s happened is that — and I’ve published open access myself — is that I get a notification that I need to pay to have my article that I’ve slaved over published. Explain that, please.
Dr. Merino: This is the issue with open access. As I mentioned, the paper gets published. You’re giving the journal a license to publish it. You’re retaining the copyright of your work. That means that the journal cannot make money or support itself by just publishing open access because they belong to you.
Typically, open-access journals are not in print and don’t have much in terms of advertising. The contract is you’re giving me a license to publish it, but it’s your journal, so you’re paying a fee for the journal expenses to basically produce your paper. That’s what’s happening with open access.
That’s been recognized with many funders, for example, with NIH funding or many of the European funders, they’re including open-access fees as part of their funding for research. Now, of course, this doesn’t help if you’re not a funded researcher or if you’re a fellow who’s doing work and so on.
Typically, most journals will have waived fees or lower fees for these situations. The reason for the open-access fee is the fact that you’re retaining the copyright. You’re not giving it to the journal who can then use it to generate its revenue for supporting itself, the editorial staff, and so on.
Dr. Wilner: This idea of charging for publication has created a satellite business of what are called predatory journals. How does one know if the open-access journal that I’m submitting to is really just in the business of wanting my $300 or my $900 to get published? How do I know if that’s a reasonable place to publish?
Predatory Journals
Dr. Merino: That’s a big challenge that has come with this whole idea of open access and the fact that now, many journals are online only, so you’re no longer seeing a physical copy. That has given rise to the predatory journals.
The predatory journal, by definition, is a journal that claims to be open access. They’ll take your paper and publish it, but they don’t provide all the other services that you would typically expect from the fact that you’re paying an open-access fee. This includes getting appropriate peer review, production of the manuscript, and long-term curation and storage of the manuscript.
Many predatory journals will take your open-access fee, accept any paper that you submit, regardless of the quality, because they’re charging the fees for that. They don’t send it to real peer review, and then in a few months, the journal disappears so there’s no way for anybody to actually find your paper anymore.
There are certain checklists. Dr. David Moher at the University of Toronto has produced some work trying to help us identify predatory journals.
One thing I typically suggest to people who ask me this question is: Have you ever heard of this journal before? Does the journal have a track record? How far back does the story of the journal go? Is it supported by a publisher that you know? Do you know anybody who has published there? Is it something you can easily access?
If in doubt, always ask your friendly medical librarian. There used to be lists that were kept in terms of predatory journals that were being constantly updated, but those had to be shut down. As far as I understand, there were legal issues in terms of how things got on that list.
I think that overall, if you’ve heard of it, if it’s relevant, if it’s known in your field, and if your librarian knows it, it’s probably a good legitimate open-access journal. There are many very good legitimate open-access journals.
I mentioned the two that we have in our family, but all the other major journals have their own open-access journal within their family. There are some, like BMC or PLOS, that are completely open-access and legitimate journals.
Impact Factor
Dr. Wilner: What about impact factor? Many journals boast about their impact factor. I’m not sure how to interpret that number.
Dr. Merino: Impact factor is very interesting. The impact factor was developed by medical librarians to try to identify the journals they should be subscribing to. It’s a measure of the average citations to an average paper in the journal.
It doesn’t tell you about specific papers. It tells you, on average, how many of the papers in this journal get cited so many times. It’s calculated by the number of articles that were cited divided by the number of articles that were published. Journals that publish many papers, like Neurology, have a hard time bringing up their impact factor beyond a certain level.
Similarly, very small journals with one or two very highly cited papers have a very high impact factor. It’s being used as a measure, perhaps inappropriately, of how good or how reputable a journal is. We all say we don’t care about journal impact factors, but we all know our journal impact factor and we used to know it to three decimals. Now, they changed the system, and there’s only one decimal point, which makes more sense.
This is more important, for example, for authors when deciding where to submit papers. I know that in some countries, particularly in Europe, the impact factor of the journal where you publish has an impact on your promotion decisions.
I would say what’s even more important than the impact factor, is to say, “Well, is this the journal that fits the scope of my paper? Is this the journal that reaches the audience that I want to reach when I write my paper?”
There are some papers, for example, that are very influential. The impact factor just captures citations. There are some papers that are very influential that may not get cited very often. There may be papers that change clinical practice.
If you read a paper that tells you that you should be changing how you treat your patients with myasthenia based on this paper, that may not get cited. It’s a very clinically focused paper, but it’s probably more impactful than one that gets cited very much in some respect, or they make it to public policy decisions, and so on.
I think it’s important to look more at the audience and the journal scope when you submit your papers.
Dr. Wilner: One other technical question. The journals also say they’re indexed in PubMed or Google Scholar. If I want to publish my paper and I want it indexed where the right people are going to find it, where does it need to be indexed?
Dr. Merino: I grew up using Index Medicus, MedlinePlus, and the Library of Science. I still do. If I need to find something, I go to PubMed. Ideally, papers are listed in MedlinePlus or can be found in PubMed. They’re not the same thing, but you can find them through them.
That would be an important thing. Nowadays, a lot more people are using Google Scholar or Google just to identify papers. It may be a little bit less relevant, but it’s still a measure of the quality of the journal before they get indexed in some of these. For example, if you get listed in MedlinePlus, it has gone through certain quality checks by the index itself to see whether they would accept the journal or not. That’s something you want to check.
Typically, most of the large journals or the journals you and I know about are listed in more than one place, right? They’re listed in Scopus and Web of Science. They’re listed in MedlinePlus and so on. Again, if you’re submitting your paper, go somewhere where you know the journal and you’ve heard about it.
Dr. Wilner: I’m not going to ask you about artificial intelligence. We can do that another time. I want to ask something closer to me, which is this question of publish or perish.
There seems to be, in academics, more emphasis on the number of papers that one has published rather than their quality. How does a younger academician or one who really needs to publish cope with that?
Dr. Merino: Many people are writing up research that may not be relevant or that may not be high quality just because you need to have a long list of papers to get promoted, for example, if you’re an academician.
Doug Altman, who was a very influential person in the field quality of not only medical statistics but also medical publishing, had the idea that we need less research, but we need better research.
We often receive papers where you say, well, what’s the rationale behind the question in this paper? It’s like they had a large amount of data and were trying to squeeze as much as they could out of that. I think, as a young academician, the important thing to think about is whether it is an important question that matters to you and to the field, from whatever perspective, whether it’s going to advance research, advance clinical care, or have public policy implications.
Is this one where the answer will be important no matter what the answer is? If you’re thinking of that, your work will be well recognized, people will know you, and you’ll get invited to collaborate. I think that’s the most important thing rather than just churning out a large number of papers.
The productivity will come from the fact that you start by saying, let me ask something that’s really meaningful to me and to the field, with a good question and using strong research methodology.
Dr. Wilner: Thanks for that, Dr. Merino. I think that’s very valuable for all of us. This has been a great discussion. Do you have any final comments before we wrap up?
Dr. Merino: I want to encourage people to continue reading medical journals all the time and submitting to us, again, good research and important questions with robust methodology. That’s what we’re looking for in Neurology and most serious medical journals.
Dr. Wilner is an associate professor of neurology at the University of Tennessee Health Science Center, Memphis. Dr. Merino is a professor in the department of neurology at Georgetown University Medical Center, Washington, DC. Dr. Wilner reported conflicts of interest with Accordant Health Services and Lulu Publishing. Dr. Merino reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Andrew N. Wilner, MD: My guest today is Dr. Jose Merino, editor in chief of the Neurology family of journals and professor of neurology and co-vice chair of education at Georgetown University in Washington, DC.
Our program today is a follow-up of Dr. Merino’s presentation at the recent American Academy of Neurology meeting in Denver, Colorado. Along with two other panelists, Dr. Merino discussed the role of open-access publication and the dangers of predatory journals.
Jose G. Merino, MD, MPhil: Thank you for having me here. It’s a pleasure.
Open Access Defined
Dr. Wilner: I remember when publication in neurology was pretty straightforward. It was either the green journal or the blue journal, but things have certainly changed. I think one topic that is not clear to everyone is this concept of open access. Could you define that for us?
Dr. Merino: Sure. Open access is a mode of publication that fosters more open or accessible science. The idea of open access is that it combines two main elements. One is that the papers that are published become immediately available to anybody with an internet connection anywhere in the world without any restrictions.
The second important element from open access, which makes it different from other models we can talk about, is the fact that the authors retain the copyright of their work, but they give the journal and readers a license to use, reproduce, and modify the content.
This is different, for example, from instances where we have funder mandates. For example, NIH papers have to become available 6 months after publication, so they’re available to everybody but not immediately.
Dr. Wilner: I remember that when a journal article was published, say, in Neurology, if you didn’t have a subscription to Neurology, you went to the library that hopefully had a subscription.
If they didn’t have it, you would write to the author and say, “Hey, I heard you have this great paper because the abstract was out there. Could you send me a reprint?” Has that whole universe evaporated?
Dr. Merino: It depends on how the paper is published. For example, in Neurology, some of the research we publish is open access. Basically, if you have an internet connection, you can access the paper.
That’s the case for papers published in our wholly open-access journals in the Neurology family like Neurology Neuroimmunology & Neuroinflammation, Neurology Genetics, or Neurology Education.
For other papers that are published in Neurology, not under open access, there is a paywall. For some of them, the paywall comes down after a few months based on funder mandates and so on. As I was mentioning, the NIH-funded papers are available 6 months later.
In the first 6 months, you may have to go to your library, and if your library has a subscription, you can download it directly. [This is also true for] those that always stay behind the paywall, where you have to have a subscription or your library has to have a subscription.
Is Pay to Publish a Red Flag?
Dr. Wilner: I’m a professional writer. With any luck, when I write something, I get paid to write it. There’s been a long tradition in academic medicine that when you submit an article to, say, Neurology, you don’t get paid as an author for the publication. Your reward is the honor of it being published.
Neurology supports itself in various ways, including advertising and so on. That’s been the contract: free publication for work that merits it, and the journal survives on its own.
With open access, one of the things that’s happened is that — and I’ve published open access myself — is that I get a notification that I need to pay to have my article that I’ve slaved over published. Explain that, please.
Dr. Merino: This is the issue with open access. As I mentioned, the paper gets published. You’re giving the journal a license to publish it. You’re retaining the copyright of your work. That means that the journal cannot make money or support itself by just publishing open access because they belong to you.
Typically, open-access journals are not in print and don’t have much in terms of advertising. The contract is you’re giving me a license to publish it, but it’s your journal, so you’re paying a fee for the journal expenses to basically produce your paper. That’s what’s happening with open access.
That’s been recognized with many funders, for example, with NIH funding or many of the European funders, they’re including open-access fees as part of their funding for research. Now, of course, this doesn’t help if you’re not a funded researcher or if you’re a fellow who’s doing work and so on.
Typically, most journals will have waived fees or lower fees for these situations. The reason for the open-access fee is the fact that you’re retaining the copyright. You’re not giving it to the journal who can then use it to generate its revenue for supporting itself, the editorial staff, and so on.
Dr. Wilner: This idea of charging for publication has created a satellite business of what are called predatory journals. How does one know if the open-access journal that I’m submitting to is really just in the business of wanting my $300 or my $900 to get published? How do I know if that’s a reasonable place to publish?
Predatory Journals
Dr. Merino: That’s a big challenge that has come with this whole idea of open access and the fact that now, many journals are online only, so you’re no longer seeing a physical copy. That has given rise to the predatory journals.
The predatory journal, by definition, is a journal that claims to be open access. They’ll take your paper and publish it, but they don’t provide all the other services that you would typically expect from the fact that you’re paying an open-access fee. This includes getting appropriate peer review, production of the manuscript, and long-term curation and storage of the manuscript.
Many predatory journals will take your open-access fee, accept any paper that you submit, regardless of the quality, because they’re charging the fees for that. They don’t send it to real peer review, and then in a few months, the journal disappears so there’s no way for anybody to actually find your paper anymore.
There are certain checklists. Dr. David Moher at the University of Toronto has produced some work trying to help us identify predatory journals.
One thing I typically suggest to people who ask me this question is: Have you ever heard of this journal before? Does the journal have a track record? How far back does the story of the journal go? Is it supported by a publisher that you know? Do you know anybody who has published there? Is it something you can easily access?
If in doubt, always ask your friendly medical librarian. There used to be lists that were kept in terms of predatory journals that were being constantly updated, but those had to be shut down. As far as I understand, there were legal issues in terms of how things got on that list.
I think that overall, if you’ve heard of it, if it’s relevant, if it’s known in your field, and if your librarian knows it, it’s probably a good legitimate open-access journal. There are many very good legitimate open-access journals.
I mentioned the two that we have in our family, but all the other major journals have their own open-access journal within their family. There are some, like BMC or PLOS, that are completely open-access and legitimate journals.
Impact Factor
Dr. Wilner: What about impact factor? Many journals boast about their impact factor. I’m not sure how to interpret that number.
Dr. Merino: Impact factor is very interesting. The impact factor was developed by medical librarians to try to identify the journals they should be subscribing to. It’s a measure of the average citations to an average paper in the journal.
It doesn’t tell you about specific papers. It tells you, on average, how many of the papers in this journal get cited so many times. It’s calculated by the number of articles that were cited divided by the number of articles that were published. Journals that publish many papers, like Neurology, have a hard time bringing up their impact factor beyond a certain level.
Similarly, very small journals with one or two very highly cited papers have a very high impact factor. It’s being used as a measure, perhaps inappropriately, of how good or how reputable a journal is. We all say we don’t care about journal impact factors, but we all know our journal impact factor and we used to know it to three decimals. Now, they changed the system, and there’s only one decimal point, which makes more sense.
This is more important, for example, for authors when deciding where to submit papers. I know that in some countries, particularly in Europe, the impact factor of the journal where you publish has an impact on your promotion decisions.
I would say what’s even more important than the impact factor, is to say, “Well, is this the journal that fits the scope of my paper? Is this the journal that reaches the audience that I want to reach when I write my paper?”
There are some papers, for example, that are very influential. The impact factor just captures citations. There are some papers that are very influential that may not get cited very often. There may be papers that change clinical practice.
If you read a paper that tells you that you should be changing how you treat your patients with myasthenia based on this paper, that may not get cited. It’s a very clinically focused paper, but it’s probably more impactful than one that gets cited very much in some respect, or they make it to public policy decisions, and so on.
I think it’s important to look more at the audience and the journal scope when you submit your papers.
Dr. Wilner: One other technical question. The journals also say they’re indexed in PubMed or Google Scholar. If I want to publish my paper and I want it indexed where the right people are going to find it, where does it need to be indexed?
Dr. Merino: I grew up using Index Medicus, MedlinePlus, and the Library of Science. I still do. If I need to find something, I go to PubMed. Ideally, papers are listed in MedlinePlus or can be found in PubMed. They’re not the same thing, but you can find them through them.
That would be an important thing. Nowadays, a lot more people are using Google Scholar or Google just to identify papers. It may be a little bit less relevant, but it’s still a measure of the quality of the journal before they get indexed in some of these. For example, if you get listed in MedlinePlus, it has gone through certain quality checks by the index itself to see whether they would accept the journal or not. That’s something you want to check.
Typically, most of the large journals or the journals you and I know about are listed in more than one place, right? They’re listed in Scopus and Web of Science. They’re listed in MedlinePlus and so on. Again, if you’re submitting your paper, go somewhere where you know the journal and you’ve heard about it.
Dr. Wilner: I’m not going to ask you about artificial intelligence. We can do that another time. I want to ask something closer to me, which is this question of publish or perish.
There seems to be, in academics, more emphasis on the number of papers that one has published rather than their quality. How does a younger academician or one who really needs to publish cope with that?
Dr. Merino: Many people are writing up research that may not be relevant or that may not be high quality just because you need to have a long list of papers to get promoted, for example, if you’re an academician.
Doug Altman, who was a very influential person in the field quality of not only medical statistics but also medical publishing, had the idea that we need less research, but we need better research.
We often receive papers where you say, well, what’s the rationale behind the question in this paper? It’s like they had a large amount of data and were trying to squeeze as much as they could out of that. I think, as a young academician, the important thing to think about is whether it is an important question that matters to you and to the field, from whatever perspective, whether it’s going to advance research, advance clinical care, or have public policy implications.
Is this one where the answer will be important no matter what the answer is? If you’re thinking of that, your work will be well recognized, people will know you, and you’ll get invited to collaborate. I think that’s the most important thing rather than just churning out a large number of papers.
The productivity will come from the fact that you start by saying, let me ask something that’s really meaningful to me and to the field, with a good question and using strong research methodology.
Dr. Wilner: Thanks for that, Dr. Merino. I think that’s very valuable for all of us. This has been a great discussion. Do you have any final comments before we wrap up?
Dr. Merino: I want to encourage people to continue reading medical journals all the time and submitting to us, again, good research and important questions with robust methodology. That’s what we’re looking for in Neurology and most serious medical journals.
Dr. Wilner is an associate professor of neurology at the University of Tennessee Health Science Center, Memphis. Dr. Merino is a professor in the department of neurology at Georgetown University Medical Center, Washington, DC. Dr. Wilner reported conflicts of interest with Accordant Health Services and Lulu Publishing. Dr. Merino reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Oncology Mergers Are on the Rise. How Can Independent Practices Survive?
When he completed his fellowship at Fox Chase Cancer Center in Philadelphia, Moshe Chasky, MD, joined a small five-person practice that rented space from the city’s Jefferson Hospital in Philadelphia. The arrangement seemed to work well for the hospital and the small practice, which remained independent.
Within 10 years, the hospital sought to buy the practice, Alliance Cancer Specialists.
But the oncologists at Alliance did not want to join Jefferson.
The hospital eventually entered into an exclusive agreement with its own medical group to provide inpatient oncology/hematology services at three Jefferson Health–Northeast hospitals and stripped Dr. Chasky and his colleagues of their privileges at those facilities, Medscape Medical News reported last year.
said Jeff Patton, MD, CEO of OneOncology, a management services organization.
A 2020 report from the Community Oncology Alliance (COA), for instance, tracked mergers, acquisitions, and closures in the community oncology setting and found the number of practices acquired by hospitals, known as vertical integration, nearly tripled from 2010 to 2020.
“Some hospitals are pretty predatory in their approach,” Dr. Patton said. If hospitals have their own oncology program, “they’ll employ the referring doctors and then discourage them or prevent them from referring patients to our independent practices that are not owned by the hospital.”
Still, in the face of growing pressure to join hospitals, some community oncology practices are finding ways to survive and maintain their independence.
A Growing Trend
The latest data continue to show a clear trend: Consolidation in oncology is on the rise.
A 2024 study revealed that the pace of consolidation seems to be increasing.
The analysis found that, between 2015 and 2022, the number of medical oncologists increased by 14% and the number of medical oncologists per practice increased by 40%, while the number of practices decreased by 18%.
While about 44% of practices remain independent, the percentage of medical oncologists working in practices with more than 25 clinicians has increased from 34% in 2015 to 44% in 2022. By 2022, the largest 102 practices in the United States employed more than 40% of all medical oncologists.
“The rate of consolidation seems to be rapid,” study coauthor Parsa Erfani, MD, an internal medicine resident at Brigham & Women’s Hospital, Boston, explained.
Consolidation appears to breed more consolidation. The researchers found, for instance, that markets with greater hospital consolidation and more hospital beds per capita were more likely to undergo consolidation in oncology.
Consolidation may be higher in these markets “because hospitals or health systems are buying up oncology practices or conversely because oncology practices are merging to compete more effectively with larger hospitals in the area,” Dr. Erfani told this news organization.
Mergers among independent practices, known as horizontal integration, have also been on the rise, according to the 2020 COA report. These mergers can help counter pressures from hospitals seeking to acquire community practices as well as prevent practices and their clinics from closing.
Although Dr. Erfani’s research wasn’t designed to determine the factors behind consolidation, he and his colleagues point to the Affordable Care Act (ACA) and the federal 340B Drug Pricing Program as potential drivers of this trend.
The ACA encouraged consolidation as a way to improve efficiency and created the need for ever-larger information systems to collect and report quality data. But these data collection and reporting requirements have become increasingly difficult for smaller practices to take on.
The 340B Program, however, may be a bigger contributing factor to consolidation. Created in 1992, the 340B Program allows qualifying hospitals and clinics that treat low-income and uninsured patients to buy outpatient prescription drugs at a 25%-50% discount.
Hospitals seeking to capitalize on the margins possible under the 340B Program will “buy all the referring physicians in a market so that the medical oncology group is left with little choice but to sell to the hospital,” said Dr. Patton.
“Those 340B dollars are worth a lot to hospitals,” said David A. Eagle, MD, a hematologist/oncologist with New York Cancer & Blood Specialists and past president of COA. The program “creates an appetite for nonprofit hospitals to want to grow their medical oncology programs,” he told this news organization.
Declining Medicare reimbursement has also hit independent practices hard.
Over the past 15 years, compared with inflation, physicians have gotten “a pay rate decrease from Medicare,” said Dr. Patton. Payers have followed that lead and tried to cut pay for clinicians, especially those who do not have market share, he said. Paying them less is “disingenuous knowing that our costs of providing care are going up,” he said.
Less Access, Higher Costs, Worse Care?
Many studies have demonstrated that, when hospitals become behemoths in a given market, healthcare costs go up.
“There are robust data showing that consolidation increases healthcare costs by reducing competition, including in oncology,” wrote Dr. Erfani and colleagues.
Oncology practices that are owned by hospitals bill facility fees for outpatient chemotherapy treatment, adding another layer of cost, the researchers explained, citing a 2019 Health Economics study.
Another analysis, published in 2020, found that hospital prices for the top 37 infused cancer drugs averaged 86% more per unit than the price charged by physician offices. Hospital outpatient departments charged even more, on average, for drugs — 128% more for nivolumab and 428% more for fluorouracil, for instance.
In their 2024 analysis, Dr. Erfani and colleagues also found that increased hospital market concentration was associated with worse quality of care, across all assessed patient satisfaction measures, and may result in worse access to care as well.
Overall, these consolidation “trends have important implications for cancer care cost, quality, and access,” the authors concluded.
Navigating the Consolidation Trend
In the face of mounting pressure to join hospitals, community oncology practices have typically relied on horizontal mergers to maintain their independence. An increasing number of practices, however, are now turning to another strategy: Management services organizations.
According to some oncologists, a core benefit of joining a management services organization is their community practices can maintain autonomy, hold on to referrals, and benefit from access to a wider network of peers and recently approved treatments such as chimeric antigen receptor T-cell therapies.
In these arrangements, the management company also provides business assistance to practices, including help with billing and collection, payer negotiations, supply chain issues, and credentialing, as well as recruiting, hiring, and marketing.
These management organizations, which include American Oncology Network, Integrated Oncology Network, OneOncology, and Verdi Oncology, are, however, backed by private equity. According to a 2022 report, private equity–backed management organizations have ramped up arrangements with community oncology practices over the past few years — a trend that has concerned some experts.
The authors of a recent analysis in JAMA Internal Medicine explained that, although private equity involvement in physician practices may enable operational efficiencies, “critics point to potential conflicts of interest” and highlight concerns that patients “may face additional barriers to both accessibility and affordability of care.”
The difference, according to some oncologists, is their practices are not owned by the management services organization; instead, the practices enter contracts that outline the boundaries of the relationship and stipulate fees to the management organizations.
In 2020, Dr. Chasky’s practice, Alliance Cancer Specialists, joined The US Oncology Network, a management services organization wholly owned by McKesson. The organization provides the practice with capital and other resources, as well as access to the Sarah Cannon Research Institute, so patients can participate in clinical trials.
“We totally function as an independent practice,” said Dr. Chasky. “We make our own management decisions,” he said. For instance, if Alliance wants to hire a new clinician, US Oncology helps with the recruitment. “But at the end of the day, it’s our practice,” he said.
Davey Daniel, MD — whose community practice joined the management services organization OneOncology — has seen the benefits of being part of a larger network. For instance, bispecific therapies for leukemias, lymphomas, and multiple myeloma are typically administered at academic centers because of the risk for cytokine release syndrome.
However, physician leaders in the OneOncology network “came up with a playbook on how to do it safely” in the community setting, said Dr. Daniel. “It meant that we were adopting FDA newly approved therapies in a very short course.”
Being able to draw from a wider pool of expertise has had other advantages. Dr. Daniel can lean on pathologists and research scientists in the network for advice on targeted therapy use. “We’re actually bringing precision medicine expertise to the community,” Dr. Daniel said.
Dr. Chasky and Dr. Eagle, whose practice is also part of OneOncology, said that continuing to work in the community setting has allowed them greater flexibility.
Dr. Eagle explained that New York Cancer & Blood Specialists tries to offer patients an appointment within 2 days of a referral, and it allows walk-in visits.
Dr. Chasky leans into the flexibility by having staff stay late, when needed, to ensure that all patients are seen. “We’re there for our patients at all hours,” Dr. Chasky said, adding that often “you don’t have that flexibility when you work for a big hospital system.”
The bottom line is community oncology can still thrive, said Nick Ferreyros, managing director of COA, “as long as we have a healthy competitive ecosystem where [we] are valued and seen as an important part of our cancer care system.”
A version of this article first appeared on Medscape.com.
When he completed his fellowship at Fox Chase Cancer Center in Philadelphia, Moshe Chasky, MD, joined a small five-person practice that rented space from the city’s Jefferson Hospital in Philadelphia. The arrangement seemed to work well for the hospital and the small practice, which remained independent.
Within 10 years, the hospital sought to buy the practice, Alliance Cancer Specialists.
But the oncologists at Alliance did not want to join Jefferson.
The hospital eventually entered into an exclusive agreement with its own medical group to provide inpatient oncology/hematology services at three Jefferson Health–Northeast hospitals and stripped Dr. Chasky and his colleagues of their privileges at those facilities, Medscape Medical News reported last year.
said Jeff Patton, MD, CEO of OneOncology, a management services organization.
A 2020 report from the Community Oncology Alliance (COA), for instance, tracked mergers, acquisitions, and closures in the community oncology setting and found the number of practices acquired by hospitals, known as vertical integration, nearly tripled from 2010 to 2020.
“Some hospitals are pretty predatory in their approach,” Dr. Patton said. If hospitals have their own oncology program, “they’ll employ the referring doctors and then discourage them or prevent them from referring patients to our independent practices that are not owned by the hospital.”
Still, in the face of growing pressure to join hospitals, some community oncology practices are finding ways to survive and maintain their independence.
A Growing Trend
The latest data continue to show a clear trend: Consolidation in oncology is on the rise.
A 2024 study revealed that the pace of consolidation seems to be increasing.
The analysis found that, between 2015 and 2022, the number of medical oncologists increased by 14% and the number of medical oncologists per practice increased by 40%, while the number of practices decreased by 18%.
While about 44% of practices remain independent, the percentage of medical oncologists working in practices with more than 25 clinicians has increased from 34% in 2015 to 44% in 2022. By 2022, the largest 102 practices in the United States employed more than 40% of all medical oncologists.
“The rate of consolidation seems to be rapid,” study coauthor Parsa Erfani, MD, an internal medicine resident at Brigham & Women’s Hospital, Boston, explained.
Consolidation appears to breed more consolidation. The researchers found, for instance, that markets with greater hospital consolidation and more hospital beds per capita were more likely to undergo consolidation in oncology.
Consolidation may be higher in these markets “because hospitals or health systems are buying up oncology practices or conversely because oncology practices are merging to compete more effectively with larger hospitals in the area,” Dr. Erfani told this news organization.
Mergers among independent practices, known as horizontal integration, have also been on the rise, according to the 2020 COA report. These mergers can help counter pressures from hospitals seeking to acquire community practices as well as prevent practices and their clinics from closing.
Although Dr. Erfani’s research wasn’t designed to determine the factors behind consolidation, he and his colleagues point to the Affordable Care Act (ACA) and the federal 340B Drug Pricing Program as potential drivers of this trend.
The ACA encouraged consolidation as a way to improve efficiency and created the need for ever-larger information systems to collect and report quality data. But these data collection and reporting requirements have become increasingly difficult for smaller practices to take on.
The 340B Program, however, may be a bigger contributing factor to consolidation. Created in 1992, the 340B Program allows qualifying hospitals and clinics that treat low-income and uninsured patients to buy outpatient prescription drugs at a 25%-50% discount.
Hospitals seeking to capitalize on the margins possible under the 340B Program will “buy all the referring physicians in a market so that the medical oncology group is left with little choice but to sell to the hospital,” said Dr. Patton.
“Those 340B dollars are worth a lot to hospitals,” said David A. Eagle, MD, a hematologist/oncologist with New York Cancer & Blood Specialists and past president of COA. The program “creates an appetite for nonprofit hospitals to want to grow their medical oncology programs,” he told this news organization.
Declining Medicare reimbursement has also hit independent practices hard.
Over the past 15 years, compared with inflation, physicians have gotten “a pay rate decrease from Medicare,” said Dr. Patton. Payers have followed that lead and tried to cut pay for clinicians, especially those who do not have market share, he said. Paying them less is “disingenuous knowing that our costs of providing care are going up,” he said.
Less Access, Higher Costs, Worse Care?
Many studies have demonstrated that, when hospitals become behemoths in a given market, healthcare costs go up.
“There are robust data showing that consolidation increases healthcare costs by reducing competition, including in oncology,” wrote Dr. Erfani and colleagues.
Oncology practices that are owned by hospitals bill facility fees for outpatient chemotherapy treatment, adding another layer of cost, the researchers explained, citing a 2019 Health Economics study.
Another analysis, published in 2020, found that hospital prices for the top 37 infused cancer drugs averaged 86% more per unit than the price charged by physician offices. Hospital outpatient departments charged even more, on average, for drugs — 128% more for nivolumab and 428% more for fluorouracil, for instance.
In their 2024 analysis, Dr. Erfani and colleagues also found that increased hospital market concentration was associated with worse quality of care, across all assessed patient satisfaction measures, and may result in worse access to care as well.
Overall, these consolidation “trends have important implications for cancer care cost, quality, and access,” the authors concluded.
Navigating the Consolidation Trend
In the face of mounting pressure to join hospitals, community oncology practices have typically relied on horizontal mergers to maintain their independence. An increasing number of practices, however, are now turning to another strategy: Management services organizations.
According to some oncologists, a core benefit of joining a management services organization is their community practices can maintain autonomy, hold on to referrals, and benefit from access to a wider network of peers and recently approved treatments such as chimeric antigen receptor T-cell therapies.
In these arrangements, the management company also provides business assistance to practices, including help with billing and collection, payer negotiations, supply chain issues, and credentialing, as well as recruiting, hiring, and marketing.
These management organizations, which include American Oncology Network, Integrated Oncology Network, OneOncology, and Verdi Oncology, are, however, backed by private equity. According to a 2022 report, private equity–backed management organizations have ramped up arrangements with community oncology practices over the past few years — a trend that has concerned some experts.
The authors of a recent analysis in JAMA Internal Medicine explained that, although private equity involvement in physician practices may enable operational efficiencies, “critics point to potential conflicts of interest” and highlight concerns that patients “may face additional barriers to both accessibility and affordability of care.”
The difference, according to some oncologists, is their practices are not owned by the management services organization; instead, the practices enter contracts that outline the boundaries of the relationship and stipulate fees to the management organizations.
In 2020, Dr. Chasky’s practice, Alliance Cancer Specialists, joined The US Oncology Network, a management services organization wholly owned by McKesson. The organization provides the practice with capital and other resources, as well as access to the Sarah Cannon Research Institute, so patients can participate in clinical trials.
“We totally function as an independent practice,” said Dr. Chasky. “We make our own management decisions,” he said. For instance, if Alliance wants to hire a new clinician, US Oncology helps with the recruitment. “But at the end of the day, it’s our practice,” he said.
Davey Daniel, MD — whose community practice joined the management services organization OneOncology — has seen the benefits of being part of a larger network. For instance, bispecific therapies for leukemias, lymphomas, and multiple myeloma are typically administered at academic centers because of the risk for cytokine release syndrome.
However, physician leaders in the OneOncology network “came up with a playbook on how to do it safely” in the community setting, said Dr. Daniel. “It meant that we were adopting FDA newly approved therapies in a very short course.”
Being able to draw from a wider pool of expertise has had other advantages. Dr. Daniel can lean on pathologists and research scientists in the network for advice on targeted therapy use. “We’re actually bringing precision medicine expertise to the community,” Dr. Daniel said.
Dr. Chasky and Dr. Eagle, whose practice is also part of OneOncology, said that continuing to work in the community setting has allowed them greater flexibility.
Dr. Eagle explained that New York Cancer & Blood Specialists tries to offer patients an appointment within 2 days of a referral, and it allows walk-in visits.
Dr. Chasky leans into the flexibility by having staff stay late, when needed, to ensure that all patients are seen. “We’re there for our patients at all hours,” Dr. Chasky said, adding that often “you don’t have that flexibility when you work for a big hospital system.”
The bottom line is community oncology can still thrive, said Nick Ferreyros, managing director of COA, “as long as we have a healthy competitive ecosystem where [we] are valued and seen as an important part of our cancer care system.”
A version of this article first appeared on Medscape.com.
When he completed his fellowship at Fox Chase Cancer Center in Philadelphia, Moshe Chasky, MD, joined a small five-person practice that rented space from the city’s Jefferson Hospital in Philadelphia. The arrangement seemed to work well for the hospital and the small practice, which remained independent.
Within 10 years, the hospital sought to buy the practice, Alliance Cancer Specialists.
But the oncologists at Alliance did not want to join Jefferson.
The hospital eventually entered into an exclusive agreement with its own medical group to provide inpatient oncology/hematology services at three Jefferson Health–Northeast hospitals and stripped Dr. Chasky and his colleagues of their privileges at those facilities, Medscape Medical News reported last year.
said Jeff Patton, MD, CEO of OneOncology, a management services organization.
A 2020 report from the Community Oncology Alliance (COA), for instance, tracked mergers, acquisitions, and closures in the community oncology setting and found the number of practices acquired by hospitals, known as vertical integration, nearly tripled from 2010 to 2020.
“Some hospitals are pretty predatory in their approach,” Dr. Patton said. If hospitals have their own oncology program, “they’ll employ the referring doctors and then discourage them or prevent them from referring patients to our independent practices that are not owned by the hospital.”
Still, in the face of growing pressure to join hospitals, some community oncology practices are finding ways to survive and maintain their independence.
A Growing Trend
The latest data continue to show a clear trend: Consolidation in oncology is on the rise.
A 2024 study revealed that the pace of consolidation seems to be increasing.
The analysis found that, between 2015 and 2022, the number of medical oncologists increased by 14% and the number of medical oncologists per practice increased by 40%, while the number of practices decreased by 18%.
While about 44% of practices remain independent, the percentage of medical oncologists working in practices with more than 25 clinicians has increased from 34% in 2015 to 44% in 2022. By 2022, the largest 102 practices in the United States employed more than 40% of all medical oncologists.
“The rate of consolidation seems to be rapid,” study coauthor Parsa Erfani, MD, an internal medicine resident at Brigham & Women’s Hospital, Boston, explained.
Consolidation appears to breed more consolidation. The researchers found, for instance, that markets with greater hospital consolidation and more hospital beds per capita were more likely to undergo consolidation in oncology.
Consolidation may be higher in these markets “because hospitals or health systems are buying up oncology practices or conversely because oncology practices are merging to compete more effectively with larger hospitals in the area,” Dr. Erfani told this news organization.
Mergers among independent practices, known as horizontal integration, have also been on the rise, according to the 2020 COA report. These mergers can help counter pressures from hospitals seeking to acquire community practices as well as prevent practices and their clinics from closing.
Although Dr. Erfani’s research wasn’t designed to determine the factors behind consolidation, he and his colleagues point to the Affordable Care Act (ACA) and the federal 340B Drug Pricing Program as potential drivers of this trend.
The ACA encouraged consolidation as a way to improve efficiency and created the need for ever-larger information systems to collect and report quality data. But these data collection and reporting requirements have become increasingly difficult for smaller practices to take on.
The 340B Program, however, may be a bigger contributing factor to consolidation. Created in 1992, the 340B Program allows qualifying hospitals and clinics that treat low-income and uninsured patients to buy outpatient prescription drugs at a 25%-50% discount.
Hospitals seeking to capitalize on the margins possible under the 340B Program will “buy all the referring physicians in a market so that the medical oncology group is left with little choice but to sell to the hospital,” said Dr. Patton.
“Those 340B dollars are worth a lot to hospitals,” said David A. Eagle, MD, a hematologist/oncologist with New York Cancer & Blood Specialists and past president of COA. The program “creates an appetite for nonprofit hospitals to want to grow their medical oncology programs,” he told this news organization.
Declining Medicare reimbursement has also hit independent practices hard.
Over the past 15 years, compared with inflation, physicians have gotten “a pay rate decrease from Medicare,” said Dr. Patton. Payers have followed that lead and tried to cut pay for clinicians, especially those who do not have market share, he said. Paying them less is “disingenuous knowing that our costs of providing care are going up,” he said.
Less Access, Higher Costs, Worse Care?
Many studies have demonstrated that, when hospitals become behemoths in a given market, healthcare costs go up.
“There are robust data showing that consolidation increases healthcare costs by reducing competition, including in oncology,” wrote Dr. Erfani and colleagues.
Oncology practices that are owned by hospitals bill facility fees for outpatient chemotherapy treatment, adding another layer of cost, the researchers explained, citing a 2019 Health Economics study.
Another analysis, published in 2020, found that hospital prices for the top 37 infused cancer drugs averaged 86% more per unit than the price charged by physician offices. Hospital outpatient departments charged even more, on average, for drugs — 128% more for nivolumab and 428% more for fluorouracil, for instance.
In their 2024 analysis, Dr. Erfani and colleagues also found that increased hospital market concentration was associated with worse quality of care, across all assessed patient satisfaction measures, and may result in worse access to care as well.
Overall, these consolidation “trends have important implications for cancer care cost, quality, and access,” the authors concluded.
Navigating the Consolidation Trend
In the face of mounting pressure to join hospitals, community oncology practices have typically relied on horizontal mergers to maintain their independence. An increasing number of practices, however, are now turning to another strategy: Management services organizations.
According to some oncologists, a core benefit of joining a management services organization is their community practices can maintain autonomy, hold on to referrals, and benefit from access to a wider network of peers and recently approved treatments such as chimeric antigen receptor T-cell therapies.
In these arrangements, the management company also provides business assistance to practices, including help with billing and collection, payer negotiations, supply chain issues, and credentialing, as well as recruiting, hiring, and marketing.
These management organizations, which include American Oncology Network, Integrated Oncology Network, OneOncology, and Verdi Oncology, are, however, backed by private equity. According to a 2022 report, private equity–backed management organizations have ramped up arrangements with community oncology practices over the past few years — a trend that has concerned some experts.
The authors of a recent analysis in JAMA Internal Medicine explained that, although private equity involvement in physician practices may enable operational efficiencies, “critics point to potential conflicts of interest” and highlight concerns that patients “may face additional barriers to both accessibility and affordability of care.”
The difference, according to some oncologists, is their practices are not owned by the management services organization; instead, the practices enter contracts that outline the boundaries of the relationship and stipulate fees to the management organizations.
In 2020, Dr. Chasky’s practice, Alliance Cancer Specialists, joined The US Oncology Network, a management services organization wholly owned by McKesson. The organization provides the practice with capital and other resources, as well as access to the Sarah Cannon Research Institute, so patients can participate in clinical trials.
“We totally function as an independent practice,” said Dr. Chasky. “We make our own management decisions,” he said. For instance, if Alliance wants to hire a new clinician, US Oncology helps with the recruitment. “But at the end of the day, it’s our practice,” he said.
Davey Daniel, MD — whose community practice joined the management services organization OneOncology — has seen the benefits of being part of a larger network. For instance, bispecific therapies for leukemias, lymphomas, and multiple myeloma are typically administered at academic centers because of the risk for cytokine release syndrome.
However, physician leaders in the OneOncology network “came up with a playbook on how to do it safely” in the community setting, said Dr. Daniel. “It meant that we were adopting FDA newly approved therapies in a very short course.”
Being able to draw from a wider pool of expertise has had other advantages. Dr. Daniel can lean on pathologists and research scientists in the network for advice on targeted therapy use. “We’re actually bringing precision medicine expertise to the community,” Dr. Daniel said.
Dr. Chasky and Dr. Eagle, whose practice is also part of OneOncology, said that continuing to work in the community setting has allowed them greater flexibility.
Dr. Eagle explained that New York Cancer & Blood Specialists tries to offer patients an appointment within 2 days of a referral, and it allows walk-in visits.
Dr. Chasky leans into the flexibility by having staff stay late, when needed, to ensure that all patients are seen. “We’re there for our patients at all hours,” Dr. Chasky said, adding that often “you don’t have that flexibility when you work for a big hospital system.”
The bottom line is community oncology can still thrive, said Nick Ferreyros, managing director of COA, “as long as we have a healthy competitive ecosystem where [we] are valued and seen as an important part of our cancer care system.”
A version of this article first appeared on Medscape.com.








