User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
More fatalities in heart transplant patients with COVID-19
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.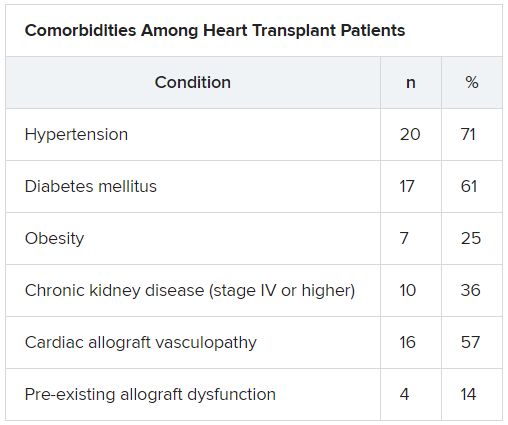
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.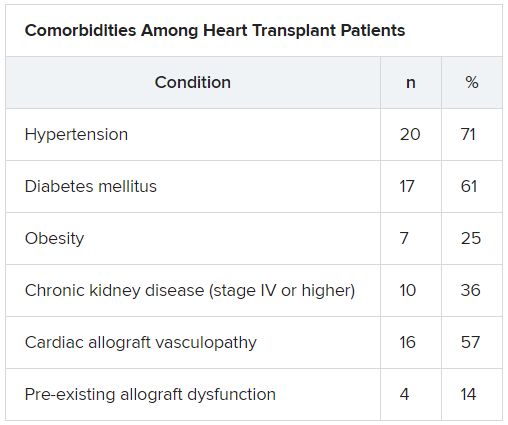
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.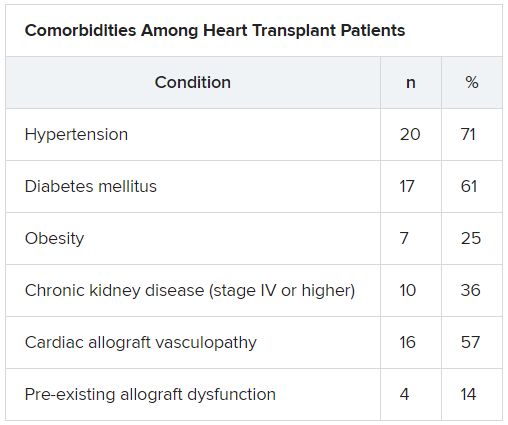
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Today’s top news highlights: COVID-19 could worsen gambling problems, food allergies less common than thought
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
The grocery store hug
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Today’s top news highlights: Addressing racism in maternity care, group forms to protect health professionals from retaliation
Here are the stories our MDedge editors across specialties think you need to know about today:
Addressing racism in the maternal mortality crisis
The emerging racial disparities in COVID-19 incidence and outcomes in the United States are on a collision course with long-standing racial disparities in U.S. maternal care and mortality. “The saying is that ‘the virus doesn’t discriminate,’ but it understands our biases, right? So, the virus takes advantage of the weaknesses in our system,” said Joia A. Crear-Perry, MD, an ob.gyn. and founder and president of the National Birth Equity Collaborative, a New Orleans–based research, training, and advocacy organization working to optimize black maternal and infant health. This article is part of an ongoing feature series on the crisis in maternal mortality in the United States. Here we explore potential solutions for addressing the inequities as proposed by thought leaders and key stakeholders. Read more.
A ‘Beacon’ for physicians, nurses facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy. Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality. The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment supply and other matters of public concern related to coronavirus. “There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.” Read more.
COVID-19 ravages the Navajo Nation
The Navajo Nation has the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths. These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average rates of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%. “We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language), is a monster confronting the Navajo today. It has had significant impact on our nation and people,” Mary Hasbah Roessel, MD, a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., wrote in a commentary on MDedge. Read more.
Heart pump system authorized for COVID-19 patients
The Food and Drug Administration issued an emergency use authorization (EUA) for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation. The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including pulmonary embolism. Read more.
Deprescribing hypertension meds looks safe for older adults
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure control, researchers concluded based on findings from a randomized multicenter trial. The study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” said James P. Sheppard, PhD, of University of Oxford (England). The report was published in JAMA. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Addressing racism in the maternal mortality crisis
The emerging racial disparities in COVID-19 incidence and outcomes in the United States are on a collision course with long-standing racial disparities in U.S. maternal care and mortality. “The saying is that ‘the virus doesn’t discriminate,’ but it understands our biases, right? So, the virus takes advantage of the weaknesses in our system,” said Joia A. Crear-Perry, MD, an ob.gyn. and founder and president of the National Birth Equity Collaborative, a New Orleans–based research, training, and advocacy organization working to optimize black maternal and infant health. This article is part of an ongoing feature series on the crisis in maternal mortality in the United States. Here we explore potential solutions for addressing the inequities as proposed by thought leaders and key stakeholders. Read more.
A ‘Beacon’ for physicians, nurses facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy. Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality. The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment supply and other matters of public concern related to coronavirus. “There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.” Read more.
COVID-19 ravages the Navajo Nation
The Navajo Nation has the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths. These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average rates of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%. “We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language), is a monster confronting the Navajo today. It has had significant impact on our nation and people,” Mary Hasbah Roessel, MD, a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., wrote in a commentary on MDedge. Read more.
Heart pump system authorized for COVID-19 patients
The Food and Drug Administration issued an emergency use authorization (EUA) for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation. The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including pulmonary embolism. Read more.
Deprescribing hypertension meds looks safe for older adults
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure control, researchers concluded based on findings from a randomized multicenter trial. The study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” said James P. Sheppard, PhD, of University of Oxford (England). The report was published in JAMA. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Addressing racism in the maternal mortality crisis
The emerging racial disparities in COVID-19 incidence and outcomes in the United States are on a collision course with long-standing racial disparities in U.S. maternal care and mortality. “The saying is that ‘the virus doesn’t discriminate,’ but it understands our biases, right? So, the virus takes advantage of the weaknesses in our system,” said Joia A. Crear-Perry, MD, an ob.gyn. and founder and president of the National Birth Equity Collaborative, a New Orleans–based research, training, and advocacy organization working to optimize black maternal and infant health. This article is part of an ongoing feature series on the crisis in maternal mortality in the United States. Here we explore potential solutions for addressing the inequities as proposed by thought leaders and key stakeholders. Read more.
A ‘Beacon’ for physicians, nurses facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy. Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality. The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment supply and other matters of public concern related to coronavirus. “There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.” Read more.
COVID-19 ravages the Navajo Nation
The Navajo Nation has the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths. These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average rates of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%. “We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language), is a monster confronting the Navajo today. It has had significant impact on our nation and people,” Mary Hasbah Roessel, MD, a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., wrote in a commentary on MDedge. Read more.
Heart pump system authorized for COVID-19 patients
The Food and Drug Administration issued an emergency use authorization (EUA) for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation. The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including pulmonary embolism. Read more.
Deprescribing hypertension meds looks safe for older adults
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure control, researchers concluded based on findings from a randomized multicenter trial. The study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” said James P. Sheppard, PhD, of University of Oxford (England). The report was published in JAMA. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
COVID-19: New group stands up for health professionals facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
FDA okays emergency use for Impella RP in COVID-19 right heart failure
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
Distancing works, N95 respirators work better
A study that claims to be the first review of all the available evidence of the effectiveness of physical distancing, face masks, and eye protection to prevent spread of COVID-19 and other respiratory diseases has quantified the effectiveness of these protective measures. The study found that greater physical distancing from an exposed person significantly reduces risk of transmission and that N95 masks, particularly for health care workers, are more effective than other face coverings.
The meta-analysis, published online in The Lancet (2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9) also marks the first evaluation of these protective measures in both community and health care settings for COVID-19, the study authors stated.
“The risk for infection is highly dependent on distance to the individual infected and the type of face mask and eye protection worn,” wrote Derek K. Chu, MD, PhD, of McMaster University in Hamilton, Ont., and colleagues, reporting on behalf of the COVID-19 Systematic Urgent Review Group Effort, or SURGE.
The study reported that physical distancing of at least 1 meter, or about a yard, “seems to be strongly associated with a large protective effect,” but that distancing of 2 meters or about 6 feet could be more effective.
The study involved a systematic review of 172 observational studies across six continents that evaluated distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, other severe acute respiratory syndrome (SARS) disease, and Middle East respiratory syndrome (MERS), and their family members, caregivers and health care workers up to May 3, 2020. The meta-analysis involved pooled estimates from 44 comparative studies with 25,697 participants, including seven studies of COVID-19 with 6,674 participants. None of the studies included in the meta-analysis were randomized clinical trials.
A subanalysis of 29 unadjusted and 9 adjusted studies found that the absolute risk of infection in proximity to an exposed individual was 12.8% at 1 m and 2.6% at 2 m. The risk remained constant even when the six COVID-19 studies in this subanalysis were isolated and regardless of being in a health care or non–health-care setting. Each meter of increased distance resulted in a doubling in the change in relative risk (P = .041).
The study also identified what Dr. Chu and colleagues characterized as a “large reduction” in infection risk with the use of both N95 or similar respirators or face masks, with an adjusted risk of infection of 3.1% with a face covering vs. a 17.4% without. The researchers also found a stronger association in health care settings vs. non–health care settings, with a relative risk of 0.3 vs. 0.56, respectively (P = .049). The protective effect of N95 or similar respirators was greater than other masks, with adjusted odds ratios of 0.04 vs. 0.33 (P = .09).
Eye protection was found to reduce the risk of infection to 5.5% vs. 16% without eye protection.
The study also identified potential barriers to social distancing and use of masks and eye protection: discomfort, resource use “linked with potentially decreased equity,” less clear communication, and a perceived lack of empathy on the part of providers toward patients.
Dr. Chu and colleagues wrote that more “high-quality” research, including randomized trials of the optimal physical distance and evaluation of different mask types in non–health care settings “is urgently needed.” They added, “Policymakers at all levels should, therefore, strive to address equity implications for groups with currently limited access to face masks and eye protection.”
The goal of this study was to “inform WHO guidance documents,” the study noted. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk,” said study co-leader Holger Schünemann, MD, MSc, PhD, of McMaster University.
Prof. Raina MacIntyre, MBBS, PhD, head of the biosecurity research program at the Kirby Institute at the University of New South Wales in Sydney, who authored the comment that accompanied the article, said that this study provides evidence for stronger PPE guidelines.
“The Centers for Disease Control and Prevention initially recommended N95s for health workers treating COVID-19 patients, but later downgraded this to surgical masks and even cloth masks and bandannas when there was a supply shortage,” she said. “This study shows that N95s are superior masks and should prompt a review of guidelines that recommend anything less for health workers.”
Recommending anything less than N95 masks for health workers is like sending troops into battle “unarmed or with bows and arrows against a fully armed enemy,” she said. “We are not talking about a device that costs hundreds or thousands of dollars; a N95 costs less than a dollar to produce. All that is needed to address the supply shortage is political will.”
While the study has some shortcomings – namely that it didn’t provide a breakdown of positive tests among COVID-19 participants – it does provide important insight for physicians, Sachin Gupta, MD, a pulmonary and critical care specialist in San Francisco, said in an interview. “The strength of a meta-analysis is that you’re able to get a composite idea; that’s one up side to this,” he said. “They’re confirming what we knew: that distance matters; that more protective masks reduce risk of infection; and that eye protection has an important role.”
Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The World Health Organization provided partial funding for the study.
SOURCE: Chu DK et al. Lancet. 2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9 .
A study that claims to be the first review of all the available evidence of the effectiveness of physical distancing, face masks, and eye protection to prevent spread of COVID-19 and other respiratory diseases has quantified the effectiveness of these protective measures. The study found that greater physical distancing from an exposed person significantly reduces risk of transmission and that N95 masks, particularly for health care workers, are more effective than other face coverings.
The meta-analysis, published online in The Lancet (2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9) also marks the first evaluation of these protective measures in both community and health care settings for COVID-19, the study authors stated.
“The risk for infection is highly dependent on distance to the individual infected and the type of face mask and eye protection worn,” wrote Derek K. Chu, MD, PhD, of McMaster University in Hamilton, Ont., and colleagues, reporting on behalf of the COVID-19 Systematic Urgent Review Group Effort, or SURGE.
The study reported that physical distancing of at least 1 meter, or about a yard, “seems to be strongly associated with a large protective effect,” but that distancing of 2 meters or about 6 feet could be more effective.
The study involved a systematic review of 172 observational studies across six continents that evaluated distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, other severe acute respiratory syndrome (SARS) disease, and Middle East respiratory syndrome (MERS), and their family members, caregivers and health care workers up to May 3, 2020. The meta-analysis involved pooled estimates from 44 comparative studies with 25,697 participants, including seven studies of COVID-19 with 6,674 participants. None of the studies included in the meta-analysis were randomized clinical trials.
A subanalysis of 29 unadjusted and 9 adjusted studies found that the absolute risk of infection in proximity to an exposed individual was 12.8% at 1 m and 2.6% at 2 m. The risk remained constant even when the six COVID-19 studies in this subanalysis were isolated and regardless of being in a health care or non–health-care setting. Each meter of increased distance resulted in a doubling in the change in relative risk (P = .041).
The study also identified what Dr. Chu and colleagues characterized as a “large reduction” in infection risk with the use of both N95 or similar respirators or face masks, with an adjusted risk of infection of 3.1% with a face covering vs. a 17.4% without. The researchers also found a stronger association in health care settings vs. non–health care settings, with a relative risk of 0.3 vs. 0.56, respectively (P = .049). The protective effect of N95 or similar respirators was greater than other masks, with adjusted odds ratios of 0.04 vs. 0.33 (P = .09).
Eye protection was found to reduce the risk of infection to 5.5% vs. 16% without eye protection.
The study also identified potential barriers to social distancing and use of masks and eye protection: discomfort, resource use “linked with potentially decreased equity,” less clear communication, and a perceived lack of empathy on the part of providers toward patients.
Dr. Chu and colleagues wrote that more “high-quality” research, including randomized trials of the optimal physical distance and evaluation of different mask types in non–health care settings “is urgently needed.” They added, “Policymakers at all levels should, therefore, strive to address equity implications for groups with currently limited access to face masks and eye protection.”
The goal of this study was to “inform WHO guidance documents,” the study noted. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk,” said study co-leader Holger Schünemann, MD, MSc, PhD, of McMaster University.
Prof. Raina MacIntyre, MBBS, PhD, head of the biosecurity research program at the Kirby Institute at the University of New South Wales in Sydney, who authored the comment that accompanied the article, said that this study provides evidence for stronger PPE guidelines.
“The Centers for Disease Control and Prevention initially recommended N95s for health workers treating COVID-19 patients, but later downgraded this to surgical masks and even cloth masks and bandannas when there was a supply shortage,” she said. “This study shows that N95s are superior masks and should prompt a review of guidelines that recommend anything less for health workers.”
Recommending anything less than N95 masks for health workers is like sending troops into battle “unarmed or with bows and arrows against a fully armed enemy,” she said. “We are not talking about a device that costs hundreds or thousands of dollars; a N95 costs less than a dollar to produce. All that is needed to address the supply shortage is political will.”
While the study has some shortcomings – namely that it didn’t provide a breakdown of positive tests among COVID-19 participants – it does provide important insight for physicians, Sachin Gupta, MD, a pulmonary and critical care specialist in San Francisco, said in an interview. “The strength of a meta-analysis is that you’re able to get a composite idea; that’s one up side to this,” he said. “They’re confirming what we knew: that distance matters; that more protective masks reduce risk of infection; and that eye protection has an important role.”
Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The World Health Organization provided partial funding for the study.
SOURCE: Chu DK et al. Lancet. 2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9 .
A study that claims to be the first review of all the available evidence of the effectiveness of physical distancing, face masks, and eye protection to prevent spread of COVID-19 and other respiratory diseases has quantified the effectiveness of these protective measures. The study found that greater physical distancing from an exposed person significantly reduces risk of transmission and that N95 masks, particularly for health care workers, are more effective than other face coverings.
The meta-analysis, published online in The Lancet (2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9) also marks the first evaluation of these protective measures in both community and health care settings for COVID-19, the study authors stated.
“The risk for infection is highly dependent on distance to the individual infected and the type of face mask and eye protection worn,” wrote Derek K. Chu, MD, PhD, of McMaster University in Hamilton, Ont., and colleagues, reporting on behalf of the COVID-19 Systematic Urgent Review Group Effort, or SURGE.
The study reported that physical distancing of at least 1 meter, or about a yard, “seems to be strongly associated with a large protective effect,” but that distancing of 2 meters or about 6 feet could be more effective.
The study involved a systematic review of 172 observational studies across six continents that evaluated distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, other severe acute respiratory syndrome (SARS) disease, and Middle East respiratory syndrome (MERS), and their family members, caregivers and health care workers up to May 3, 2020. The meta-analysis involved pooled estimates from 44 comparative studies with 25,697 participants, including seven studies of COVID-19 with 6,674 participants. None of the studies included in the meta-analysis were randomized clinical trials.
A subanalysis of 29 unadjusted and 9 adjusted studies found that the absolute risk of infection in proximity to an exposed individual was 12.8% at 1 m and 2.6% at 2 m. The risk remained constant even when the six COVID-19 studies in this subanalysis were isolated and regardless of being in a health care or non–health-care setting. Each meter of increased distance resulted in a doubling in the change in relative risk (P = .041).
The study also identified what Dr. Chu and colleagues characterized as a “large reduction” in infection risk with the use of both N95 or similar respirators or face masks, with an adjusted risk of infection of 3.1% with a face covering vs. a 17.4% without. The researchers also found a stronger association in health care settings vs. non–health care settings, with a relative risk of 0.3 vs. 0.56, respectively (P = .049). The protective effect of N95 or similar respirators was greater than other masks, with adjusted odds ratios of 0.04 vs. 0.33 (P = .09).
Eye protection was found to reduce the risk of infection to 5.5% vs. 16% without eye protection.
The study also identified potential barriers to social distancing and use of masks and eye protection: discomfort, resource use “linked with potentially decreased equity,” less clear communication, and a perceived lack of empathy on the part of providers toward patients.
Dr. Chu and colleagues wrote that more “high-quality” research, including randomized trials of the optimal physical distance and evaluation of different mask types in non–health care settings “is urgently needed.” They added, “Policymakers at all levels should, therefore, strive to address equity implications for groups with currently limited access to face masks and eye protection.”
The goal of this study was to “inform WHO guidance documents,” the study noted. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk,” said study co-leader Holger Schünemann, MD, MSc, PhD, of McMaster University.
Prof. Raina MacIntyre, MBBS, PhD, head of the biosecurity research program at the Kirby Institute at the University of New South Wales in Sydney, who authored the comment that accompanied the article, said that this study provides evidence for stronger PPE guidelines.
“The Centers for Disease Control and Prevention initially recommended N95s for health workers treating COVID-19 patients, but later downgraded this to surgical masks and even cloth masks and bandannas when there was a supply shortage,” she said. “This study shows that N95s are superior masks and should prompt a review of guidelines that recommend anything less for health workers.”
Recommending anything less than N95 masks for health workers is like sending troops into battle “unarmed or with bows and arrows against a fully armed enemy,” she said. “We are not talking about a device that costs hundreds or thousands of dollars; a N95 costs less than a dollar to produce. All that is needed to address the supply shortage is political will.”
While the study has some shortcomings – namely that it didn’t provide a breakdown of positive tests among COVID-19 participants – it does provide important insight for physicians, Sachin Gupta, MD, a pulmonary and critical care specialist in San Francisco, said in an interview. “The strength of a meta-analysis is that you’re able to get a composite idea; that’s one up side to this,” he said. “They’re confirming what we knew: that distance matters; that more protective masks reduce risk of infection; and that eye protection has an important role.”
Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The World Health Organization provided partial funding for the study.
SOURCE: Chu DK et al. Lancet. 2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9 .
FROM THE LANCET
Key clinical point: Meta-analysis confirms protective measures reduce risk of spread of COVID-19.
Major finding: Adjusted risk of infection was 3.1% with a face covering vs. 17.4% without.
Study details: Systematic review and meta-analysis of 172 observational studies with 25,697 participants assessing measures to prevent spread of respiratory disease up to May 3, 2020.
Disclosures: Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The study was in part funded by the World Health Organization.
Source: Chu DK et al. Lancet. 2020 Jun 1. doi. org/10.1016/ S0140-6736(20)31142-9.
Sleep burden index predicts recurrent stroke
A sleep burden index that considers multiple sleep-wake disturbances (SWDs) predicts subsequent cardiocerebrovascular events during the 2 years after a stroke, preliminary results on an ongoing study suggest.
The index, which combines sleep duration, sleep disordered breathing, restless leg syndrome (RLS), insomnia, and sleep duration, is a better predictor of new events than a single sleep disorder alone.
With further evidence of its usefulness, “the sleep burden index could be integrated into clinical routine,” Simone B. Duss, PhD, of the department of neurology at Bern (Switzerland) University Hospital, told a press briefing.
The findings were presented online at the Congress of the European Academy of Neurology 2020, which transitioned to a virtual meeting because of the COVID-19 pandemic.
Sleep-wake disorders are very common in stroke patients and may preexist or appear de novo as a consequence of brain damage, said Dr. Duss. “They may also be a result of medical, psychological, or environmental challenges these patients face after a stroke.”
Clear Evidence
There’s “clear evidence” that sleep disordered breathing is a risk factor for stroke, and negatively affects stroke outcome if left untreated, said Dr. Duss.
But for other SWDs, such as insomnia, RLS, and long and short sleep duration, “the evidence is less compelling,” she said. “However, some studies still suggest they influence stroke risk and outcome.”
Experts believe that sleep disturbances after a stroke lead to sleep fragmentation, as well as decreased slow wave sleep and REM sleep.
“This negatively affects inflammatory neuroprotective and synaptic plasticity processes during the recovery process of a stroke,” said Dr. Duss. “In the end, this results in worse outcomes with regard to recurrent events but also in activities of daily living and mood.”
The new analysis aimed to assess the impact of sleep-wake disturbances on recurrent events and outcomes following a stroke or transient ischemic attack (TIA). It included 438 patients with acute stroke (85%) or TIA (15%). The mean age of the study population was 65 years, and 64% were male.
Researchers used the National Institutes of Health Stroke Scale (NIHSS) to assess stroke severity. At admission, the mean NIHSS score was 4. Most strokes (77.2%) were supratentorial.
About one-fifth of stroke patients and one-third of TIA patients had experienced a previous event.
Researchers used functional outcome scores to assess the clinical course of the stroke or TIA. In addition, they regularly asked patients about recurrence of cardiocerebrovascular events.
Investigators assessed sleep disordered breathing during the acute phase of stroke, so within the first few days, using respirography. They collected information on the presence of other sleep-wake disturbances from questionnaires and clinical interviews at 1 month, 3 months, 1 year, and 2 years after the event.
About 26% of subjects showed severe sleep disordered breathing, “meaning that they had more than 20 apnea-hypopnea events per hour,” said Dr. Duss.
More than a quarter of patients reported subclinical symptoms of insomnia (measured using the Insomnia Severity Index), and up to 10% reported severe insomnia symptoms corresponding to the clinical diagnosis of insomnia, she said.
About 9% of patients in the acute phase of stroke, and 6% in the more chronic phase, fulfilled the diagnostic criteria of RLS.
More ‘skewed’
The results for sleep duration were relatively “skewed,” said Dr. Duss. More patients reported longer sleep duration (more than 9 hours) at 1 month than at month 3, and more reported shorter sleep duration (4.0 hours or less) at month 3 than at month 1.
The researchers built a sleep burden index for the combined impact of the various sleep-wake disturbances.
They used this index as a predictor of subsequent cardiocerebrovascular events within 3 months after an event. They used a composite outcome that included recurrent stroke or TIA, MI, heart failure, and urgent revascularization, as well as new cardiocerebrovascular events, from 3 to 24 months.
The analysis showed that the mean sleep burden index was higher for stroke patients with a recurrent event, compared with stroke or TIA patients without a recurrent event (P = .0002).
A multiple logistical regression model with the presence or absence of a recurrent event as an outcome showed that the sleep burden index is a significant predictor of recurrent events (odds ratio, 2.10; P = .001). This was true even after controlling for age, gender, and baseline stroke severity.
The baseline apnea/hypopnea index and sleep duration were also significant predictors of new events. Importantly, though, the sleep burden index remained a significant predictor of recurrent events even after excluding the apnea/hypopnea index component, said Dr. Duss. “So the predictive power of the sleep burden index is not only driven by the apnea-hypopnea index at the beginning of a stroke.”
Sleep-wake disturbances “should be more carefully assessed and considered in comprehensive treatment approaches,” not only in stroke patients, but in neurologic patients in general, said Dr. Duss
She noted that these are preliminary observations from an ongoing study. The results need to be confirmed and should be when the study is finalized, she said.
Researchers are also analyzing MRI data to assess whether certain brain lesions are associated with sleep disturbances.
Jesse Dawson, MD, professor of stroke medicine at the University of Glasgow, said the clinical scoring system the study included “will be a big help in design and conduct of clinical trials.”
Although he and other stroke experts are aware of the high prevalence of sleep disorders after stroke, “we don’t routinely look for them as we’re uncertain whether intervention is of benefit,” said Dr. Dawson.
This new study “suggests there is an association with adverse outcome,” he said.
The research was supported by grants from the Swiss National Science Foundation and the Swiss Heart Foundation. Dr. Duss and Dr. Dawson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A sleep burden index that considers multiple sleep-wake disturbances (SWDs) predicts subsequent cardiocerebrovascular events during the 2 years after a stroke, preliminary results on an ongoing study suggest.
The index, which combines sleep duration, sleep disordered breathing, restless leg syndrome (RLS), insomnia, and sleep duration, is a better predictor of new events than a single sleep disorder alone.
With further evidence of its usefulness, “the sleep burden index could be integrated into clinical routine,” Simone B. Duss, PhD, of the department of neurology at Bern (Switzerland) University Hospital, told a press briefing.
The findings were presented online at the Congress of the European Academy of Neurology 2020, which transitioned to a virtual meeting because of the COVID-19 pandemic.
Sleep-wake disorders are very common in stroke patients and may preexist or appear de novo as a consequence of brain damage, said Dr. Duss. “They may also be a result of medical, psychological, or environmental challenges these patients face after a stroke.”
Clear Evidence
There’s “clear evidence” that sleep disordered breathing is a risk factor for stroke, and negatively affects stroke outcome if left untreated, said Dr. Duss.
But for other SWDs, such as insomnia, RLS, and long and short sleep duration, “the evidence is less compelling,” she said. “However, some studies still suggest they influence stroke risk and outcome.”
Experts believe that sleep disturbances after a stroke lead to sleep fragmentation, as well as decreased slow wave sleep and REM sleep.
“This negatively affects inflammatory neuroprotective and synaptic plasticity processes during the recovery process of a stroke,” said Dr. Duss. “In the end, this results in worse outcomes with regard to recurrent events but also in activities of daily living and mood.”
The new analysis aimed to assess the impact of sleep-wake disturbances on recurrent events and outcomes following a stroke or transient ischemic attack (TIA). It included 438 patients with acute stroke (85%) or TIA (15%). The mean age of the study population was 65 years, and 64% were male.
Researchers used the National Institutes of Health Stroke Scale (NIHSS) to assess stroke severity. At admission, the mean NIHSS score was 4. Most strokes (77.2%) were supratentorial.
About one-fifth of stroke patients and one-third of TIA patients had experienced a previous event.
Researchers used functional outcome scores to assess the clinical course of the stroke or TIA. In addition, they regularly asked patients about recurrence of cardiocerebrovascular events.
Investigators assessed sleep disordered breathing during the acute phase of stroke, so within the first few days, using respirography. They collected information on the presence of other sleep-wake disturbances from questionnaires and clinical interviews at 1 month, 3 months, 1 year, and 2 years after the event.
About 26% of subjects showed severe sleep disordered breathing, “meaning that they had more than 20 apnea-hypopnea events per hour,” said Dr. Duss.
More than a quarter of patients reported subclinical symptoms of insomnia (measured using the Insomnia Severity Index), and up to 10% reported severe insomnia symptoms corresponding to the clinical diagnosis of insomnia, she said.
About 9% of patients in the acute phase of stroke, and 6% in the more chronic phase, fulfilled the diagnostic criteria of RLS.
More ‘skewed’
The results for sleep duration were relatively “skewed,” said Dr. Duss. More patients reported longer sleep duration (more than 9 hours) at 1 month than at month 3, and more reported shorter sleep duration (4.0 hours or less) at month 3 than at month 1.
The researchers built a sleep burden index for the combined impact of the various sleep-wake disturbances.
They used this index as a predictor of subsequent cardiocerebrovascular events within 3 months after an event. They used a composite outcome that included recurrent stroke or TIA, MI, heart failure, and urgent revascularization, as well as new cardiocerebrovascular events, from 3 to 24 months.
The analysis showed that the mean sleep burden index was higher for stroke patients with a recurrent event, compared with stroke or TIA patients without a recurrent event (P = .0002).
A multiple logistical regression model with the presence or absence of a recurrent event as an outcome showed that the sleep burden index is a significant predictor of recurrent events (odds ratio, 2.10; P = .001). This was true even after controlling for age, gender, and baseline stroke severity.
The baseline apnea/hypopnea index and sleep duration were also significant predictors of new events. Importantly, though, the sleep burden index remained a significant predictor of recurrent events even after excluding the apnea/hypopnea index component, said Dr. Duss. “So the predictive power of the sleep burden index is not only driven by the apnea-hypopnea index at the beginning of a stroke.”
Sleep-wake disturbances “should be more carefully assessed and considered in comprehensive treatment approaches,” not only in stroke patients, but in neurologic patients in general, said Dr. Duss
She noted that these are preliminary observations from an ongoing study. The results need to be confirmed and should be when the study is finalized, she said.
Researchers are also analyzing MRI data to assess whether certain brain lesions are associated with sleep disturbances.
Jesse Dawson, MD, professor of stroke medicine at the University of Glasgow, said the clinical scoring system the study included “will be a big help in design and conduct of clinical trials.”
Although he and other stroke experts are aware of the high prevalence of sleep disorders after stroke, “we don’t routinely look for them as we’re uncertain whether intervention is of benefit,” said Dr. Dawson.
This new study “suggests there is an association with adverse outcome,” he said.
The research was supported by grants from the Swiss National Science Foundation and the Swiss Heart Foundation. Dr. Duss and Dr. Dawson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A sleep burden index that considers multiple sleep-wake disturbances (SWDs) predicts subsequent cardiocerebrovascular events during the 2 years after a stroke, preliminary results on an ongoing study suggest.
The index, which combines sleep duration, sleep disordered breathing, restless leg syndrome (RLS), insomnia, and sleep duration, is a better predictor of new events than a single sleep disorder alone.
With further evidence of its usefulness, “the sleep burden index could be integrated into clinical routine,” Simone B. Duss, PhD, of the department of neurology at Bern (Switzerland) University Hospital, told a press briefing.
The findings were presented online at the Congress of the European Academy of Neurology 2020, which transitioned to a virtual meeting because of the COVID-19 pandemic.
Sleep-wake disorders are very common in stroke patients and may preexist or appear de novo as a consequence of brain damage, said Dr. Duss. “They may also be a result of medical, psychological, or environmental challenges these patients face after a stroke.”
Clear Evidence
There’s “clear evidence” that sleep disordered breathing is a risk factor for stroke, and negatively affects stroke outcome if left untreated, said Dr. Duss.
But for other SWDs, such as insomnia, RLS, and long and short sleep duration, “the evidence is less compelling,” she said. “However, some studies still suggest they influence stroke risk and outcome.”
Experts believe that sleep disturbances after a stroke lead to sleep fragmentation, as well as decreased slow wave sleep and REM sleep.
“This negatively affects inflammatory neuroprotective and synaptic plasticity processes during the recovery process of a stroke,” said Dr. Duss. “In the end, this results in worse outcomes with regard to recurrent events but also in activities of daily living and mood.”
The new analysis aimed to assess the impact of sleep-wake disturbances on recurrent events and outcomes following a stroke or transient ischemic attack (TIA). It included 438 patients with acute stroke (85%) or TIA (15%). The mean age of the study population was 65 years, and 64% were male.
Researchers used the National Institutes of Health Stroke Scale (NIHSS) to assess stroke severity. At admission, the mean NIHSS score was 4. Most strokes (77.2%) were supratentorial.
About one-fifth of stroke patients and one-third of TIA patients had experienced a previous event.
Researchers used functional outcome scores to assess the clinical course of the stroke or TIA. In addition, they regularly asked patients about recurrence of cardiocerebrovascular events.
Investigators assessed sleep disordered breathing during the acute phase of stroke, so within the first few days, using respirography. They collected information on the presence of other sleep-wake disturbances from questionnaires and clinical interviews at 1 month, 3 months, 1 year, and 2 years after the event.
About 26% of subjects showed severe sleep disordered breathing, “meaning that they had more than 20 apnea-hypopnea events per hour,” said Dr. Duss.
More than a quarter of patients reported subclinical symptoms of insomnia (measured using the Insomnia Severity Index), and up to 10% reported severe insomnia symptoms corresponding to the clinical diagnosis of insomnia, she said.
About 9% of patients in the acute phase of stroke, and 6% in the more chronic phase, fulfilled the diagnostic criteria of RLS.
More ‘skewed’
The results for sleep duration were relatively “skewed,” said Dr. Duss. More patients reported longer sleep duration (more than 9 hours) at 1 month than at month 3, and more reported shorter sleep duration (4.0 hours or less) at month 3 than at month 1.
The researchers built a sleep burden index for the combined impact of the various sleep-wake disturbances.
They used this index as a predictor of subsequent cardiocerebrovascular events within 3 months after an event. They used a composite outcome that included recurrent stroke or TIA, MI, heart failure, and urgent revascularization, as well as new cardiocerebrovascular events, from 3 to 24 months.
The analysis showed that the mean sleep burden index was higher for stroke patients with a recurrent event, compared with stroke or TIA patients without a recurrent event (P = .0002).
A multiple logistical regression model with the presence or absence of a recurrent event as an outcome showed that the sleep burden index is a significant predictor of recurrent events (odds ratio, 2.10; P = .001). This was true even after controlling for age, gender, and baseline stroke severity.
The baseline apnea/hypopnea index and sleep duration were also significant predictors of new events. Importantly, though, the sleep burden index remained a significant predictor of recurrent events even after excluding the apnea/hypopnea index component, said Dr. Duss. “So the predictive power of the sleep burden index is not only driven by the apnea-hypopnea index at the beginning of a stroke.”
Sleep-wake disturbances “should be more carefully assessed and considered in comprehensive treatment approaches,” not only in stroke patients, but in neurologic patients in general, said Dr. Duss
She noted that these are preliminary observations from an ongoing study. The results need to be confirmed and should be when the study is finalized, she said.
Researchers are also analyzing MRI data to assess whether certain brain lesions are associated with sleep disturbances.
Jesse Dawson, MD, professor of stroke medicine at the University of Glasgow, said the clinical scoring system the study included “will be a big help in design and conduct of clinical trials.”
Although he and other stroke experts are aware of the high prevalence of sleep disorders after stroke, “we don’t routinely look for them as we’re uncertain whether intervention is of benefit,” said Dr. Dawson.
This new study “suggests there is an association with adverse outcome,” he said.
The research was supported by grants from the Swiss National Science Foundation and the Swiss Heart Foundation. Dr. Duss and Dr. Dawson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Despite guidelines, controversy remains over corticosteroids in COVID-19
Three main reasons have been put forth for using corticosteroids in critically ill patients with COVID-19, but only one – the hope of preventing lung fibrosis in patients with unresolved acute respiratory distress syndrome – is reasonable to employ now outside of formal randomized trials, Peter Pickkers, MD, PhD, asserted at a webinar on COVID-19 sponsored by the European Society of Intensive Care Medicine.
The most commonly invoked rationale for giving steroids in patients with severe COVID-19 is to modulate the destructive inflammatory immune response that occurs with advancing disease. Another justification cited for giving steroids is to treat suspected adrenal insufficiency in those with refractory shock. Of note, both practices are endorsed in the recent Surviving Sepsis Campaign guidelines on management of critically ill patients with COVID-19 (Intensive Care Med. 2020 May;46[5]:854-87).
But those recommendations – numbers 22 and 42 out of a total of 50 recommendations included in the guidelines – should never have been made, according to Dr. Pickkers, professor of experimental intensive care medicine at Radboud University Medical Center in Nijmegen, the Netherlands.
Dueling guidelines
The Surviving Sepsis Campaign guidelines, which were developed by a panel comprising 36 experts in 12 countries, are quite frank in conceding that the guidance in favor of corticosteroids are weak recommendations based on low-quality evidence.
The guidelines recommend against using corticosteroids to try to modulate the immune system in mechanically ventilated COVID-19 patients without acute respiratory distress syndrome (ARDS), but do recommend steroids in those with COVID-19 and ARDS. However, the guidelines also note that, because of the very low quality of the evidence, some experts on the panel preferred not to issue a pro-steroids recommendation at all until higher-quality evidence becomes available. Dr. Pickkers said he believes that the minority view should have prevailed. Moreover, current COVID-19 guidance from the World Health Organization is at odds with the Surviving Sepsis Campaign recommendations; the WHO advises against corticosteroids unless the treatment is indicated for a reason other than immunomodulation, he noted.
The evidence in favor of steroids in an effort to blunt the immune response in COVID patients with ARDS is based largely upon a single small, retrospective, non–peer-reviewed report that 5-7 days of treatment with 1-2 mg/kg per day of methylprednisolone was associated with shortened fever duration and need for supplemental oxygen.
The evidence against steroids for immunomodulation comes mainly from earlier studies of the SARS and MERS novel coronaviruses. For example, in a multicenter study of 309 patients with the MERS (Middle East respiratory syndrome) virus, those who received corticosteroids received no benefit and experienced delayed viral clearance (Am J Respir Crit Care Med. 2018 Mar 15;197[6]:757-67).
“The thing is, virtually all COVID-19 patients in the ICU fulfill the criteria for ARDS, so following the Surviving Sepsis Campaign guidelines would have far-reaching consequences,” Dr. Pickkers said.
Those consequences include a theoretic potential for serious harm arising from dampening the immune response at a point in the course of COVID-19 when the virus is still present, which could result in slowed viral clearance and prolonged viral shedding. Moreover so far no one has been able to identify a sweet spot in the disease course where the viral load has waned and the immune response is sufficiently early that intervention with corticosteroids might have an optimal benefit/risk ratio, he continued.
“My opinion is that at this moment there is no benefit at all for corticosteroids for immunomodulation in patients with COVID-19,” Dr. Pickkers said. “My personal recommendation, in contrast to the Surviving Sepsis Campaign recommendation, is not to use this therapy outside of a study.”
He added that randomized, controlled trials of corticosteroid therapy in critically ill patients with COVID-19 are ongoing in Europe and the United States, including the large RECOVERY study of dexamethasone in the United Kingdom.
As for the Surviving Sepsis Campaign recommendation to use corticosteroids to treat refractory shock in COVID-19, Dr. Pickkers dismissed this guidance as largely irrelevant. That’s because few patients with COVID-19 who need mechanical ventilation have refractory shock as evidenced by the need for a high infusion rate of norepinephrine. Anyway, he noted, that Surviving Sepsis recommendation is based upon extrapolation from evidence of benefit in bacterial septic shock patients, which he deemed to be of questionable relevance to the COVID-19 pandemic.
Attacking the fibroproliferative phase of ARDS
First off, Dr. Pickkers conceded, there is no evidence that treatment with corticosteroids to prevent lung fibrosis in COVID-19 patients with nonresolving ARDS is an effective strategy; the pandemic is simply too new at this point for the appropriate studies to have been done. But this much is known: Postmortem pathologic studies show fibroplastic proliferation is present in the lungs of COVID-19 patients, as in those who die of ARDS of other causes. Also, COVID-19 patients typically aren’t admitted to the ICU until day 11 or 12 after developing their first symptoms, so by the time they display indications that their ARDS is not resolving, the virus has typically left the scene; thus, there is little risk at that point that corticosteroids will promote viral proliferation. Additionally, studies in critically ill patients with nonresolving ARDS of other causes show clinically meaningful benefits for corticosteroid therapy.
Dr. Pickkers cited as “must reading” an analysis of five randomized trials of corticosteroid therapy in a total of 518 patients with acute lung injury ARDS of non–COVID-19 origin. The analysis by investigators at the University of Tennessee, Memphis, concluded that treatment resulted in clinically meaningful reductions in duration of mechanical ventilation and ICU length of stay. Moreover, in the 400 patients whose steroid therapy commenced before day 14 of ARDS, there was a statistically significant 22% reduction in risk of death, compared with patients in whom corticosteroids were started later (Intensive Care Med. 2008 Jan;34[1]:61-9).
Session cochair Jan De Waele, MD, PhD, struck a cautious note, remarking, “It’s my perception that we’re using the evidence that we’ve gathered in other conditions and are now trying to apply it in COVID-19. But quality data on patients with COVID-19 itself is pretty scare, and it’s really hard to say whether this disease behaves similarly to bacterial septic shock or to other viral infections.”
“We need more information about the use of corticosteroids in COVID-19, although I think a lot of people are using it at this moment,” added Dr. De Waele, a surgical intensivist at Ghent (Belgium) University.
That being said, he asked Dr. Pickkers when he considers using corticosteroids to prevent pulmonary fibrosis.
Dr. Pickkers said that when he notices that a COVID-19 patient’s lung compliance is worsening, that stiff lung is a clue that fibrosis is occurring and is having clinical consequences. “We also measure blood procollagen, a not very sensitive but moderately specific marker of fibroproliferation. If we see an increase in this biomarker and the lung mechanics are changing, then we do treat these patients with corticosteroids,” Dr. Pickkers replied.
He and his colleagues try to start steroids before day 14 of ARDS, and they continue treatment for longer than 7 days in order to prevent a rebound inflammatory response upon treatment discontinuation. They also avoid using neuromuscular agents and engage in meticulous infection surveillance in order to minimize potential complications of corticosteroid therapy in the ICU.
Dr. Pickkers reported having no financial conflicts regarding his presentation.
Three main reasons have been put forth for using corticosteroids in critically ill patients with COVID-19, but only one – the hope of preventing lung fibrosis in patients with unresolved acute respiratory distress syndrome – is reasonable to employ now outside of formal randomized trials, Peter Pickkers, MD, PhD, asserted at a webinar on COVID-19 sponsored by the European Society of Intensive Care Medicine.
The most commonly invoked rationale for giving steroids in patients with severe COVID-19 is to modulate the destructive inflammatory immune response that occurs with advancing disease. Another justification cited for giving steroids is to treat suspected adrenal insufficiency in those with refractory shock. Of note, both practices are endorsed in the recent Surviving Sepsis Campaign guidelines on management of critically ill patients with COVID-19 (Intensive Care Med. 2020 May;46[5]:854-87).
But those recommendations – numbers 22 and 42 out of a total of 50 recommendations included in the guidelines – should never have been made, according to Dr. Pickkers, professor of experimental intensive care medicine at Radboud University Medical Center in Nijmegen, the Netherlands.
Dueling guidelines
The Surviving Sepsis Campaign guidelines, which were developed by a panel comprising 36 experts in 12 countries, are quite frank in conceding that the guidance in favor of corticosteroids are weak recommendations based on low-quality evidence.
The guidelines recommend against using corticosteroids to try to modulate the immune system in mechanically ventilated COVID-19 patients without acute respiratory distress syndrome (ARDS), but do recommend steroids in those with COVID-19 and ARDS. However, the guidelines also note that, because of the very low quality of the evidence, some experts on the panel preferred not to issue a pro-steroids recommendation at all until higher-quality evidence becomes available. Dr. Pickkers said he believes that the minority view should have prevailed. Moreover, current COVID-19 guidance from the World Health Organization is at odds with the Surviving Sepsis Campaign recommendations; the WHO advises against corticosteroids unless the treatment is indicated for a reason other than immunomodulation, he noted.
The evidence in favor of steroids in an effort to blunt the immune response in COVID patients with ARDS is based largely upon a single small, retrospective, non–peer-reviewed report that 5-7 days of treatment with 1-2 mg/kg per day of methylprednisolone was associated with shortened fever duration and need for supplemental oxygen.
The evidence against steroids for immunomodulation comes mainly from earlier studies of the SARS and MERS novel coronaviruses. For example, in a multicenter study of 309 patients with the MERS (Middle East respiratory syndrome) virus, those who received corticosteroids received no benefit and experienced delayed viral clearance (Am J Respir Crit Care Med. 2018 Mar 15;197[6]:757-67).
“The thing is, virtually all COVID-19 patients in the ICU fulfill the criteria for ARDS, so following the Surviving Sepsis Campaign guidelines would have far-reaching consequences,” Dr. Pickkers said.
Those consequences include a theoretic potential for serious harm arising from dampening the immune response at a point in the course of COVID-19 when the virus is still present, which could result in slowed viral clearance and prolonged viral shedding. Moreover so far no one has been able to identify a sweet spot in the disease course where the viral load has waned and the immune response is sufficiently early that intervention with corticosteroids might have an optimal benefit/risk ratio, he continued.
“My opinion is that at this moment there is no benefit at all for corticosteroids for immunomodulation in patients with COVID-19,” Dr. Pickkers said. “My personal recommendation, in contrast to the Surviving Sepsis Campaign recommendation, is not to use this therapy outside of a study.”
He added that randomized, controlled trials of corticosteroid therapy in critically ill patients with COVID-19 are ongoing in Europe and the United States, including the large RECOVERY study of dexamethasone in the United Kingdom.
As for the Surviving Sepsis Campaign recommendation to use corticosteroids to treat refractory shock in COVID-19, Dr. Pickkers dismissed this guidance as largely irrelevant. That’s because few patients with COVID-19 who need mechanical ventilation have refractory shock as evidenced by the need for a high infusion rate of norepinephrine. Anyway, he noted, that Surviving Sepsis recommendation is based upon extrapolation from evidence of benefit in bacterial septic shock patients, which he deemed to be of questionable relevance to the COVID-19 pandemic.
Attacking the fibroproliferative phase of ARDS
First off, Dr. Pickkers conceded, there is no evidence that treatment with corticosteroids to prevent lung fibrosis in COVID-19 patients with nonresolving ARDS is an effective strategy; the pandemic is simply too new at this point for the appropriate studies to have been done. But this much is known: Postmortem pathologic studies show fibroplastic proliferation is present in the lungs of COVID-19 patients, as in those who die of ARDS of other causes. Also, COVID-19 patients typically aren’t admitted to the ICU until day 11 or 12 after developing their first symptoms, so by the time they display indications that their ARDS is not resolving, the virus has typically left the scene; thus, there is little risk at that point that corticosteroids will promote viral proliferation. Additionally, studies in critically ill patients with nonresolving ARDS of other causes show clinically meaningful benefits for corticosteroid therapy.
Dr. Pickkers cited as “must reading” an analysis of five randomized trials of corticosteroid therapy in a total of 518 patients with acute lung injury ARDS of non–COVID-19 origin. The analysis by investigators at the University of Tennessee, Memphis, concluded that treatment resulted in clinically meaningful reductions in duration of mechanical ventilation and ICU length of stay. Moreover, in the 400 patients whose steroid therapy commenced before day 14 of ARDS, there was a statistically significant 22% reduction in risk of death, compared with patients in whom corticosteroids were started later (Intensive Care Med. 2008 Jan;34[1]:61-9).
Session cochair Jan De Waele, MD, PhD, struck a cautious note, remarking, “It’s my perception that we’re using the evidence that we’ve gathered in other conditions and are now trying to apply it in COVID-19. But quality data on patients with COVID-19 itself is pretty scare, and it’s really hard to say whether this disease behaves similarly to bacterial septic shock or to other viral infections.”
“We need more information about the use of corticosteroids in COVID-19, although I think a lot of people are using it at this moment,” added Dr. De Waele, a surgical intensivist at Ghent (Belgium) University.
That being said, he asked Dr. Pickkers when he considers using corticosteroids to prevent pulmonary fibrosis.
Dr. Pickkers said that when he notices that a COVID-19 patient’s lung compliance is worsening, that stiff lung is a clue that fibrosis is occurring and is having clinical consequences. “We also measure blood procollagen, a not very sensitive but moderately specific marker of fibroproliferation. If we see an increase in this biomarker and the lung mechanics are changing, then we do treat these patients with corticosteroids,” Dr. Pickkers replied.
He and his colleagues try to start steroids before day 14 of ARDS, and they continue treatment for longer than 7 days in order to prevent a rebound inflammatory response upon treatment discontinuation. They also avoid using neuromuscular agents and engage in meticulous infection surveillance in order to minimize potential complications of corticosteroid therapy in the ICU.
Dr. Pickkers reported having no financial conflicts regarding his presentation.
Three main reasons have been put forth for using corticosteroids in critically ill patients with COVID-19, but only one – the hope of preventing lung fibrosis in patients with unresolved acute respiratory distress syndrome – is reasonable to employ now outside of formal randomized trials, Peter Pickkers, MD, PhD, asserted at a webinar on COVID-19 sponsored by the European Society of Intensive Care Medicine.
The most commonly invoked rationale for giving steroids in patients with severe COVID-19 is to modulate the destructive inflammatory immune response that occurs with advancing disease. Another justification cited for giving steroids is to treat suspected adrenal insufficiency in those with refractory shock. Of note, both practices are endorsed in the recent Surviving Sepsis Campaign guidelines on management of critically ill patients with COVID-19 (Intensive Care Med. 2020 May;46[5]:854-87).
But those recommendations – numbers 22 and 42 out of a total of 50 recommendations included in the guidelines – should never have been made, according to Dr. Pickkers, professor of experimental intensive care medicine at Radboud University Medical Center in Nijmegen, the Netherlands.
Dueling guidelines
The Surviving Sepsis Campaign guidelines, which were developed by a panel comprising 36 experts in 12 countries, are quite frank in conceding that the guidance in favor of corticosteroids are weak recommendations based on low-quality evidence.
The guidelines recommend against using corticosteroids to try to modulate the immune system in mechanically ventilated COVID-19 patients without acute respiratory distress syndrome (ARDS), but do recommend steroids in those with COVID-19 and ARDS. However, the guidelines also note that, because of the very low quality of the evidence, some experts on the panel preferred not to issue a pro-steroids recommendation at all until higher-quality evidence becomes available. Dr. Pickkers said he believes that the minority view should have prevailed. Moreover, current COVID-19 guidance from the World Health Organization is at odds with the Surviving Sepsis Campaign recommendations; the WHO advises against corticosteroids unless the treatment is indicated for a reason other than immunomodulation, he noted.
The evidence in favor of steroids in an effort to blunt the immune response in COVID patients with ARDS is based largely upon a single small, retrospective, non–peer-reviewed report that 5-7 days of treatment with 1-2 mg/kg per day of methylprednisolone was associated with shortened fever duration and need for supplemental oxygen.
The evidence against steroids for immunomodulation comes mainly from earlier studies of the SARS and MERS novel coronaviruses. For example, in a multicenter study of 309 patients with the MERS (Middle East respiratory syndrome) virus, those who received corticosteroids received no benefit and experienced delayed viral clearance (Am J Respir Crit Care Med. 2018 Mar 15;197[6]:757-67).
“The thing is, virtually all COVID-19 patients in the ICU fulfill the criteria for ARDS, so following the Surviving Sepsis Campaign guidelines would have far-reaching consequences,” Dr. Pickkers said.
Those consequences include a theoretic potential for serious harm arising from dampening the immune response at a point in the course of COVID-19 when the virus is still present, which could result in slowed viral clearance and prolonged viral shedding. Moreover so far no one has been able to identify a sweet spot in the disease course where the viral load has waned and the immune response is sufficiently early that intervention with corticosteroids might have an optimal benefit/risk ratio, he continued.
“My opinion is that at this moment there is no benefit at all for corticosteroids for immunomodulation in patients with COVID-19,” Dr. Pickkers said. “My personal recommendation, in contrast to the Surviving Sepsis Campaign recommendation, is not to use this therapy outside of a study.”
He added that randomized, controlled trials of corticosteroid therapy in critically ill patients with COVID-19 are ongoing in Europe and the United States, including the large RECOVERY study of dexamethasone in the United Kingdom.
As for the Surviving Sepsis Campaign recommendation to use corticosteroids to treat refractory shock in COVID-19, Dr. Pickkers dismissed this guidance as largely irrelevant. That’s because few patients with COVID-19 who need mechanical ventilation have refractory shock as evidenced by the need for a high infusion rate of norepinephrine. Anyway, he noted, that Surviving Sepsis recommendation is based upon extrapolation from evidence of benefit in bacterial septic shock patients, which he deemed to be of questionable relevance to the COVID-19 pandemic.
Attacking the fibroproliferative phase of ARDS
First off, Dr. Pickkers conceded, there is no evidence that treatment with corticosteroids to prevent lung fibrosis in COVID-19 patients with nonresolving ARDS is an effective strategy; the pandemic is simply too new at this point for the appropriate studies to have been done. But this much is known: Postmortem pathologic studies show fibroplastic proliferation is present in the lungs of COVID-19 patients, as in those who die of ARDS of other causes. Also, COVID-19 patients typically aren’t admitted to the ICU until day 11 or 12 after developing their first symptoms, so by the time they display indications that their ARDS is not resolving, the virus has typically left the scene; thus, there is little risk at that point that corticosteroids will promote viral proliferation. Additionally, studies in critically ill patients with nonresolving ARDS of other causes show clinically meaningful benefits for corticosteroid therapy.
Dr. Pickkers cited as “must reading” an analysis of five randomized trials of corticosteroid therapy in a total of 518 patients with acute lung injury ARDS of non–COVID-19 origin. The analysis by investigators at the University of Tennessee, Memphis, concluded that treatment resulted in clinically meaningful reductions in duration of mechanical ventilation and ICU length of stay. Moreover, in the 400 patients whose steroid therapy commenced before day 14 of ARDS, there was a statistically significant 22% reduction in risk of death, compared with patients in whom corticosteroids were started later (Intensive Care Med. 2008 Jan;34[1]:61-9).
Session cochair Jan De Waele, MD, PhD, struck a cautious note, remarking, “It’s my perception that we’re using the evidence that we’ve gathered in other conditions and are now trying to apply it in COVID-19. But quality data on patients with COVID-19 itself is pretty scare, and it’s really hard to say whether this disease behaves similarly to bacterial septic shock or to other viral infections.”
“We need more information about the use of corticosteroids in COVID-19, although I think a lot of people are using it at this moment,” added Dr. De Waele, a surgical intensivist at Ghent (Belgium) University.
That being said, he asked Dr. Pickkers when he considers using corticosteroids to prevent pulmonary fibrosis.
Dr. Pickkers said that when he notices that a COVID-19 patient’s lung compliance is worsening, that stiff lung is a clue that fibrosis is occurring and is having clinical consequences. “We also measure blood procollagen, a not very sensitive but moderately specific marker of fibroproliferation. If we see an increase in this biomarker and the lung mechanics are changing, then we do treat these patients with corticosteroids,” Dr. Pickkers replied.
He and his colleagues try to start steroids before day 14 of ARDS, and they continue treatment for longer than 7 days in order to prevent a rebound inflammatory response upon treatment discontinuation. They also avoid using neuromuscular agents and engage in meticulous infection surveillance in order to minimize potential complications of corticosteroid therapy in the ICU.
Dr. Pickkers reported having no financial conflicts regarding his presentation.
Today’s top news highlights: Cancer makes COVID-19 more dangerous, treatment for heavy menstrual bleeding, and more
Here are the stories our MDedge editors across specialties think you need to know about today:
Active cancer ups death risk for patients with COVID-19
New data show that patients with COVID-19 and progressing cancer had a significantly higher risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer. Interestingly, one of the independent risk factor for death in patients with COVID-19 and cancer was treatment with hydroxychloroquine plus azithromycin. This finding, however, was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville. Read more.
Two new studies indicate that social distancing successfully flattened the curve on COVID-19 hospitalizations. One study, published in JAMA, showed significantly lower numbers of observed cases versus worst-case projections in four states: Colorado, Minnesota, Ohio, and Virginia. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In a separate study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention. Read more.
FDA approves treatment for heavy menstrual bleeding
The Food and Drug Administration has approved a medication for the management of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. The medication, marketed as Oriahnn, is an estrogen and progestin combination product that consists of elagolix, estradiol, and norethindrone acetate capsules packaged together for oral use. The most common side effects of the drug included hot flushes, headache, fatigue, and irregular vaginal bleeding. The drug’s label includes a boxed warning about a risk of strokes and blood clots, especially in women at increased risk for these events. Read more.
Lessons from a drive-through COVID testing center
Chris Notte, MD, and Neil Skolnik, MD, were part of a team of clinicians charged with launching a drive-through COVID-19 testing center. Their task was to get the operation up and running in 2 days. It took them 3 days. While the launch was a success, the experience taught them some lessons about the limits of medical technology and the importance of personal protective equipment. “Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site,” they wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Active cancer ups death risk for patients with COVID-19
New data show that patients with COVID-19 and progressing cancer had a significantly higher risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer. Interestingly, one of the independent risk factor for death in patients with COVID-19 and cancer was treatment with hydroxychloroquine plus azithromycin. This finding, however, was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville. Read more.
Two new studies indicate that social distancing successfully flattened the curve on COVID-19 hospitalizations. One study, published in JAMA, showed significantly lower numbers of observed cases versus worst-case projections in four states: Colorado, Minnesota, Ohio, and Virginia. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In a separate study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention. Read more.
FDA approves treatment for heavy menstrual bleeding
The Food and Drug Administration has approved a medication for the management of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. The medication, marketed as Oriahnn, is an estrogen and progestin combination product that consists of elagolix, estradiol, and norethindrone acetate capsules packaged together for oral use. The most common side effects of the drug included hot flushes, headache, fatigue, and irregular vaginal bleeding. The drug’s label includes a boxed warning about a risk of strokes and blood clots, especially in women at increased risk for these events. Read more.
Lessons from a drive-through COVID testing center
Chris Notte, MD, and Neil Skolnik, MD, were part of a team of clinicians charged with launching a drive-through COVID-19 testing center. Their task was to get the operation up and running in 2 days. It took them 3 days. While the launch was a success, the experience taught them some lessons about the limits of medical technology and the importance of personal protective equipment. “Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site,” they wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Active cancer ups death risk for patients with COVID-19
New data show that patients with COVID-19 and progressing cancer had a significantly higher risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer. Interestingly, one of the independent risk factor for death in patients with COVID-19 and cancer was treatment with hydroxychloroquine plus azithromycin. This finding, however, was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville. Read more.
Two new studies indicate that social distancing successfully flattened the curve on COVID-19 hospitalizations. One study, published in JAMA, showed significantly lower numbers of observed cases versus worst-case projections in four states: Colorado, Minnesota, Ohio, and Virginia. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In a separate study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention. Read more.
FDA approves treatment for heavy menstrual bleeding
The Food and Drug Administration has approved a medication for the management of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. The medication, marketed as Oriahnn, is an estrogen and progestin combination product that consists of elagolix, estradiol, and norethindrone acetate capsules packaged together for oral use. The most common side effects of the drug included hot flushes, headache, fatigue, and irregular vaginal bleeding. The drug’s label includes a boxed warning about a risk of strokes and blood clots, especially in women at increased risk for these events. Read more.
Lessons from a drive-through COVID testing center
Chris Notte, MD, and Neil Skolnik, MD, were part of a team of clinicians charged with launching a drive-through COVID-19 testing center. Their task was to get the operation up and running in 2 days. It took them 3 days. While the launch was a success, the experience taught them some lessons about the limits of medical technology and the importance of personal protective equipment. “Prior to the coronavirus pandemic, I had never considered surgical masks, face shields, and nasal swabs to be critical components of medical technology. My opinion quickly changed after opening our drive-through COVID-19 site,” they wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.






