User login
Psoriasis Journal Scan: June 2019
Management of psoriasis as a systemic disease: What is the evidence?
Korman NJ. Br J Dermatol. 2019 Jun 21.
This narrative review explores the pathophysiological relationship between psoriasis and its common comorbidities and discusses the need for new treatment paradigms that include strategies to reduce systemic inflammation in patients with moderate-to-severe psoriasis.
Managing Psoriasis in Patients with HBV or HCV Infection: Practical Considerations.
Piaserico S, Messina F, Russo FP. Am J Clin Dermatol. 2019 Jun 20.
It has been estimated that two billion individuals are infected with HBV worldwide and approximately 240 million have chronic HBV infection. Moreover, there are approximately 71 million individuals with chronic HCV infection worldwide, with a high percentage of them unaware of being infected. As patients with HBV and HCV infections are excluded from controlled clinical trials investigating new drugs, data regarding their safety in patients with psoriasis are based almost exclusively on case reports and small retrospective cohort studies and need to be constantly updated.
Effects of Online Care on Functional and Psychological Outcomes in Patients with Psoriasis: A Randomized Controlled Trial.
Young PM, Chen AY, Ford AR, Cheng MY, Lane CJ, Armstrong AW. J Am Acad Dermatol. 2019 Jun 5.
The impact of online care on patients' functional and psychological outcomes is critical to determine yet still unknown. This 12-month randomized controlled equivalency trial evaluated how a novel online health model that facilitates physician-patient collaboration compares with in-person care for improving psoriasis patients' functional status and mental health.
Feasibility and Utility of the Psoriasis Symptom Inventory (PSI) in Clinical Care Settings: A Study from the International Psoriasis Council.
Strober B, van de Kerkhof PCM, Callis Duffin K, et al. Am J Clin Dermatol. 2019 Jun 21.
The Psoriasis Symptom Inventory (PSI) is a patient-reported outcome measure designed to assess psoriasis signs and symptoms. The aim of the study was to assess the usefulness of the PSI in enhancing patient care in the clinical setting. Eight dermatology clinics in six countries enrolled adults representing the full spectrum of psoriasis severity who regularly received care at the clinic. Key benefits of PSI discussions included the following: new information regarding symptom location and severity for physicians; prompting of quality-of-life discussions; better understanding of patient treatment priorities; change in treatment regimens to target specific symptoms or areas; and improvement of patient-physician relationship.
Socioeconomic Costs and Health Inequalities from Psoriasis: A Cohort Study.
Thomsen SF, Skov L, Dodge R, Hedegaard MS, Kjellberg J. Dermatology. 2019 Jun 25:1-8.
Incentives for health care management based on patient-related outcomes and value (IMPROVE) in psoriasis and psoriatic arthritis is a project aimed at assisting movement from activity-based to outcome-based health care management. One of the key objectives in IMPROVE is to describe the disease-associated socioeconomic burden of psoriasis. The IMPROVE study was a retrospective analysis of patients with a hospital diagnosis of psoriasis identified from the Danish National Patient Registry.
Management of psoriasis as a systemic disease: What is the evidence?
Korman NJ. Br J Dermatol. 2019 Jun 21.
This narrative review explores the pathophysiological relationship between psoriasis and its common comorbidities and discusses the need for new treatment paradigms that include strategies to reduce systemic inflammation in patients with moderate-to-severe psoriasis.
Managing Psoriasis in Patients with HBV or HCV Infection: Practical Considerations.
Piaserico S, Messina F, Russo FP. Am J Clin Dermatol. 2019 Jun 20.
It has been estimated that two billion individuals are infected with HBV worldwide and approximately 240 million have chronic HBV infection. Moreover, there are approximately 71 million individuals with chronic HCV infection worldwide, with a high percentage of them unaware of being infected. As patients with HBV and HCV infections are excluded from controlled clinical trials investigating new drugs, data regarding their safety in patients with psoriasis are based almost exclusively on case reports and small retrospective cohort studies and need to be constantly updated.
Effects of Online Care on Functional and Psychological Outcomes in Patients with Psoriasis: A Randomized Controlled Trial.
Young PM, Chen AY, Ford AR, Cheng MY, Lane CJ, Armstrong AW. J Am Acad Dermatol. 2019 Jun 5.
The impact of online care on patients' functional and psychological outcomes is critical to determine yet still unknown. This 12-month randomized controlled equivalency trial evaluated how a novel online health model that facilitates physician-patient collaboration compares with in-person care for improving psoriasis patients' functional status and mental health.
Feasibility and Utility of the Psoriasis Symptom Inventory (PSI) in Clinical Care Settings: A Study from the International Psoriasis Council.
Strober B, van de Kerkhof PCM, Callis Duffin K, et al. Am J Clin Dermatol. 2019 Jun 21.
The Psoriasis Symptom Inventory (PSI) is a patient-reported outcome measure designed to assess psoriasis signs and symptoms. The aim of the study was to assess the usefulness of the PSI in enhancing patient care in the clinical setting. Eight dermatology clinics in six countries enrolled adults representing the full spectrum of psoriasis severity who regularly received care at the clinic. Key benefits of PSI discussions included the following: new information regarding symptom location and severity for physicians; prompting of quality-of-life discussions; better understanding of patient treatment priorities; change in treatment regimens to target specific symptoms or areas; and improvement of patient-physician relationship.
Socioeconomic Costs and Health Inequalities from Psoriasis: A Cohort Study.
Thomsen SF, Skov L, Dodge R, Hedegaard MS, Kjellberg J. Dermatology. 2019 Jun 25:1-8.
Incentives for health care management based on patient-related outcomes and value (IMPROVE) in psoriasis and psoriatic arthritis is a project aimed at assisting movement from activity-based to outcome-based health care management. One of the key objectives in IMPROVE is to describe the disease-associated socioeconomic burden of psoriasis. The IMPROVE study was a retrospective analysis of patients with a hospital diagnosis of psoriasis identified from the Danish National Patient Registry.
Management of psoriasis as a systemic disease: What is the evidence?
Korman NJ. Br J Dermatol. 2019 Jun 21.
This narrative review explores the pathophysiological relationship between psoriasis and its common comorbidities and discusses the need for new treatment paradigms that include strategies to reduce systemic inflammation in patients with moderate-to-severe psoriasis.
Managing Psoriasis in Patients with HBV or HCV Infection: Practical Considerations.
Piaserico S, Messina F, Russo FP. Am J Clin Dermatol. 2019 Jun 20.
It has been estimated that two billion individuals are infected with HBV worldwide and approximately 240 million have chronic HBV infection. Moreover, there are approximately 71 million individuals with chronic HCV infection worldwide, with a high percentage of them unaware of being infected. As patients with HBV and HCV infections are excluded from controlled clinical trials investigating new drugs, data regarding their safety in patients with psoriasis are based almost exclusively on case reports and small retrospective cohort studies and need to be constantly updated.
Effects of Online Care on Functional and Psychological Outcomes in Patients with Psoriasis: A Randomized Controlled Trial.
Young PM, Chen AY, Ford AR, Cheng MY, Lane CJ, Armstrong AW. J Am Acad Dermatol. 2019 Jun 5.
The impact of online care on patients' functional and psychological outcomes is critical to determine yet still unknown. This 12-month randomized controlled equivalency trial evaluated how a novel online health model that facilitates physician-patient collaboration compares with in-person care for improving psoriasis patients' functional status and mental health.
Feasibility and Utility of the Psoriasis Symptom Inventory (PSI) in Clinical Care Settings: A Study from the International Psoriasis Council.
Strober B, van de Kerkhof PCM, Callis Duffin K, et al. Am J Clin Dermatol. 2019 Jun 21.
The Psoriasis Symptom Inventory (PSI) is a patient-reported outcome measure designed to assess psoriasis signs and symptoms. The aim of the study was to assess the usefulness of the PSI in enhancing patient care in the clinical setting. Eight dermatology clinics in six countries enrolled adults representing the full spectrum of psoriasis severity who regularly received care at the clinic. Key benefits of PSI discussions included the following: new information regarding symptom location and severity for physicians; prompting of quality-of-life discussions; better understanding of patient treatment priorities; change in treatment regimens to target specific symptoms or areas; and improvement of patient-physician relationship.
Socioeconomic Costs and Health Inequalities from Psoriasis: A Cohort Study.
Thomsen SF, Skov L, Dodge R, Hedegaard MS, Kjellberg J. Dermatology. 2019 Jun 25:1-8.
Incentives for health care management based on patient-related outcomes and value (IMPROVE) in psoriasis and psoriatic arthritis is a project aimed at assisting movement from activity-based to outcome-based health care management. One of the key objectives in IMPROVE is to describe the disease-associated socioeconomic burden of psoriasis. The IMPROVE study was a retrospective analysis of patients with a hospital diagnosis of psoriasis identified from the Danish National Patient Registry.
Systemic psoriasis treatments less often prescribed in elderly with psoriasis, despite comparable response rates
MILAN – an analysis of German and Swiss registry data shows.
There was an “imbalance” in the types of medications prescribed for older and younger patients in the registry, with biologics used more frequently in younger patients, according to investigator Matthias Augustin, MD, director of the Institute For Health Services Research in Dermatology and Nursing in Hamburg, Germany.
However, the efficacy of systemic treatments, including nonbiologic therapies, was comparable between older and younger patients, other than a few differences in response rates early in treatment that disappeared with longer follow-up, Dr. Augustin said at the World Congress of Dermatology. Coupled with evidence from the medical literature, results of this registry data analysis suggest there are “very few reasons” to avoid use of systemic drugs in elderly patients.
“I think we should create awareness and discuss possible reasons that deter dermatologists from prescribing systemic antipsoriatics in elderly patients,” he said.
Concerns about safety and drug interactions in the elderly may be one barrier to prescribing systemic therapy in this patient population: More data on this issue are needed, since the elderly are taking more medications than younger patients and have more contraindications, Dr. Augustin said. “I think this is a job for all registries for the future.”
Older individuals have typically been excluded from psoriasis clinical trials, making it difficult to extrapolate existing safety and efficacy data to those patients, he pointed out.
Accordingly, Dr. Augustin and coinvestigators evaluated prospectively collected data for patients with moderate to severe psoriasis who were included in either the German Psoriasis registry (PsoBest) or the Swiss Dermatology Network for Targeted Therapies (SDNTT). They split the cohort into a control group of those younger than 65 years (about 4,600 individuals) and those 65 years or older (about 740 individuals).
A few systemic drugs were used more frequently in the elderly, including apremilast and methotrexate, while most other drugs, including biologics, were used more frequently in younger patients, Dr. Augustin and colleagues found in their analysis. There were a few differences between the elderly and controls related to weight, smoking, and other factors, but not so pronounced that they would explain differences in the use of the systemic therapy.
Response rates to systemic therapies were generally comparable between the elderly and controls, as measured by Psoriasis Area Severity Index (PASI) 75 responses, PASI scores of 3 or less, and Dermatology Life Quality Index scores of one or less, he added.
One exception was methotrexate, which was more effective in the elderly after 3 and 6 months of treatment, but that difference was no longer apparent after 12 months of treatment, he said. Likewise, cyclosporine showed a higher response rate in younger patients at 3 months, but not at 6 or 12 months.
Based on the findings, “overall, we observed comparable responses between the controls and the elderly,” Dr. Augustin concluded.
The PsoBest registry is sponsored by CVderm, DDG, and BVDD, and “has been established and is operated in close cooperation with the involved pharmaceutical companies whose statutory pharmacovigilance requirements are taken into account,” according to a statement on the PsoBest website. The Swiss registry is supported by Janssen, AbbVie, Pfizer, Celgene, Lilly, and Novartis. The investigators did not report any disclosures.
MILAN – an analysis of German and Swiss registry data shows.
There was an “imbalance” in the types of medications prescribed for older and younger patients in the registry, with biologics used more frequently in younger patients, according to investigator Matthias Augustin, MD, director of the Institute For Health Services Research in Dermatology and Nursing in Hamburg, Germany.
However, the efficacy of systemic treatments, including nonbiologic therapies, was comparable between older and younger patients, other than a few differences in response rates early in treatment that disappeared with longer follow-up, Dr. Augustin said at the World Congress of Dermatology. Coupled with evidence from the medical literature, results of this registry data analysis suggest there are “very few reasons” to avoid use of systemic drugs in elderly patients.
“I think we should create awareness and discuss possible reasons that deter dermatologists from prescribing systemic antipsoriatics in elderly patients,” he said.
Concerns about safety and drug interactions in the elderly may be one barrier to prescribing systemic therapy in this patient population: More data on this issue are needed, since the elderly are taking more medications than younger patients and have more contraindications, Dr. Augustin said. “I think this is a job for all registries for the future.”
Older individuals have typically been excluded from psoriasis clinical trials, making it difficult to extrapolate existing safety and efficacy data to those patients, he pointed out.
Accordingly, Dr. Augustin and coinvestigators evaluated prospectively collected data for patients with moderate to severe psoriasis who were included in either the German Psoriasis registry (PsoBest) or the Swiss Dermatology Network for Targeted Therapies (SDNTT). They split the cohort into a control group of those younger than 65 years (about 4,600 individuals) and those 65 years or older (about 740 individuals).
A few systemic drugs were used more frequently in the elderly, including apremilast and methotrexate, while most other drugs, including biologics, were used more frequently in younger patients, Dr. Augustin and colleagues found in their analysis. There were a few differences between the elderly and controls related to weight, smoking, and other factors, but not so pronounced that they would explain differences in the use of the systemic therapy.
Response rates to systemic therapies were generally comparable between the elderly and controls, as measured by Psoriasis Area Severity Index (PASI) 75 responses, PASI scores of 3 or less, and Dermatology Life Quality Index scores of one or less, he added.
One exception was methotrexate, which was more effective in the elderly after 3 and 6 months of treatment, but that difference was no longer apparent after 12 months of treatment, he said. Likewise, cyclosporine showed a higher response rate in younger patients at 3 months, but not at 6 or 12 months.
Based on the findings, “overall, we observed comparable responses between the controls and the elderly,” Dr. Augustin concluded.
The PsoBest registry is sponsored by CVderm, DDG, and BVDD, and “has been established and is operated in close cooperation with the involved pharmaceutical companies whose statutory pharmacovigilance requirements are taken into account,” according to a statement on the PsoBest website. The Swiss registry is supported by Janssen, AbbVie, Pfizer, Celgene, Lilly, and Novartis. The investigators did not report any disclosures.
MILAN – an analysis of German and Swiss registry data shows.
There was an “imbalance” in the types of medications prescribed for older and younger patients in the registry, with biologics used more frequently in younger patients, according to investigator Matthias Augustin, MD, director of the Institute For Health Services Research in Dermatology and Nursing in Hamburg, Germany.
However, the efficacy of systemic treatments, including nonbiologic therapies, was comparable between older and younger patients, other than a few differences in response rates early in treatment that disappeared with longer follow-up, Dr. Augustin said at the World Congress of Dermatology. Coupled with evidence from the medical literature, results of this registry data analysis suggest there are “very few reasons” to avoid use of systemic drugs in elderly patients.
“I think we should create awareness and discuss possible reasons that deter dermatologists from prescribing systemic antipsoriatics in elderly patients,” he said.
Concerns about safety and drug interactions in the elderly may be one barrier to prescribing systemic therapy in this patient population: More data on this issue are needed, since the elderly are taking more medications than younger patients and have more contraindications, Dr. Augustin said. “I think this is a job for all registries for the future.”
Older individuals have typically been excluded from psoriasis clinical trials, making it difficult to extrapolate existing safety and efficacy data to those patients, he pointed out.
Accordingly, Dr. Augustin and coinvestigators evaluated prospectively collected data for patients with moderate to severe psoriasis who were included in either the German Psoriasis registry (PsoBest) or the Swiss Dermatology Network for Targeted Therapies (SDNTT). They split the cohort into a control group of those younger than 65 years (about 4,600 individuals) and those 65 years or older (about 740 individuals).
A few systemic drugs were used more frequently in the elderly, including apremilast and methotrexate, while most other drugs, including biologics, were used more frequently in younger patients, Dr. Augustin and colleagues found in their analysis. There were a few differences between the elderly and controls related to weight, smoking, and other factors, but not so pronounced that they would explain differences in the use of the systemic therapy.
Response rates to systemic therapies were generally comparable between the elderly and controls, as measured by Psoriasis Area Severity Index (PASI) 75 responses, PASI scores of 3 or less, and Dermatology Life Quality Index scores of one or less, he added.
One exception was methotrexate, which was more effective in the elderly after 3 and 6 months of treatment, but that difference was no longer apparent after 12 months of treatment, he said. Likewise, cyclosporine showed a higher response rate in younger patients at 3 months, but not at 6 or 12 months.
Based on the findings, “overall, we observed comparable responses between the controls and the elderly,” Dr. Augustin concluded.
The PsoBest registry is sponsored by CVderm, DDG, and BVDD, and “has been established and is operated in close cooperation with the involved pharmaceutical companies whose statutory pharmacovigilance requirements are taken into account,” according to a statement on the PsoBest website. The Swiss registry is supported by Janssen, AbbVie, Pfizer, Celgene, Lilly, and Novartis. The investigators did not report any disclosures.
REPORTING FROM WCD2019
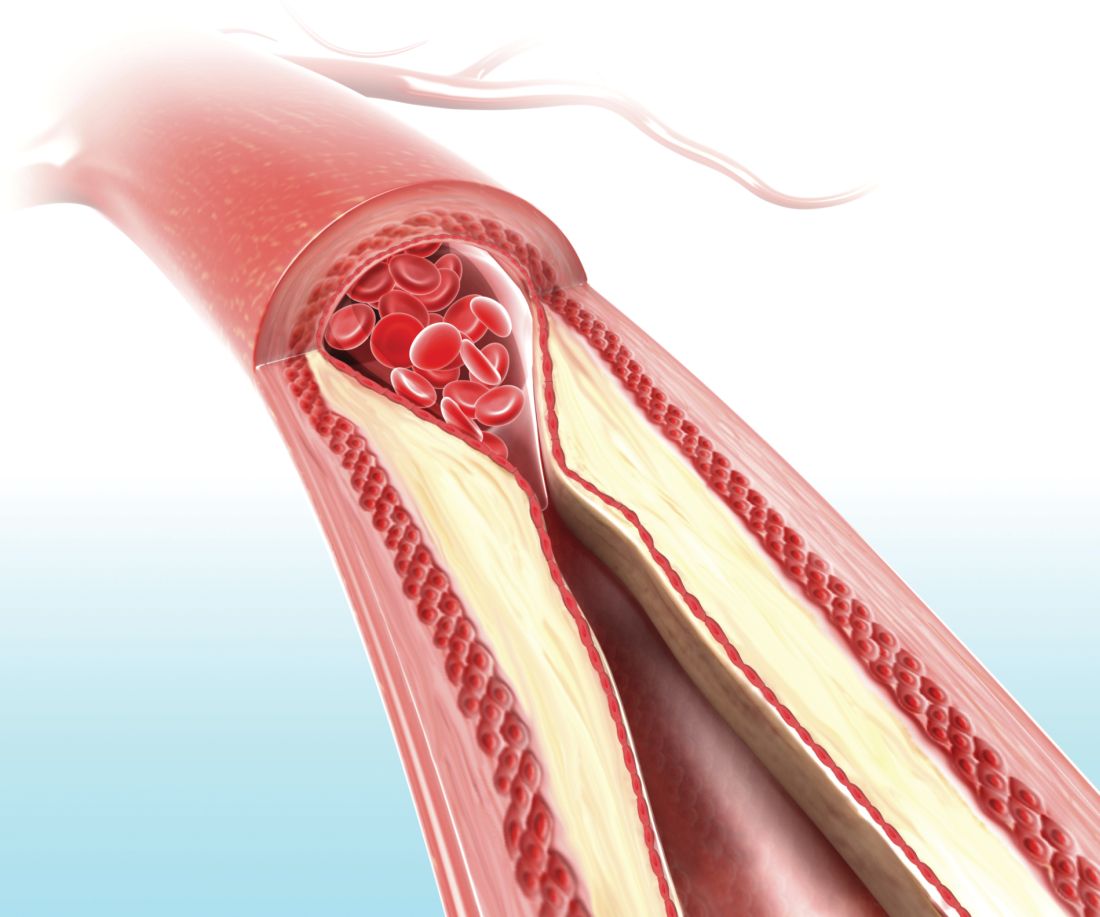
Carotid ultrasound may aid cardiovascular risk stratification of patients with psoriatic disease
according to findings from a retrospective study.
When added to the Framingham risk score, the measurement significantly improved its predictive ability, Curtis Sobchak, MD, and colleagues wrote in Arthritis & Rheumatology.
The findings indicate that carotid ultrasound could be a useful addition to cardiovascular risk stratification among these patients.
“Traditional algorithms do not consider other factors that may contribute to increased cardiovascular risk in rheumatic disease patients and tend to underestimate cardiovascular risk,” wrote Dr. Sobchak of the University of Toronto and coauthors.
“The advantage of ultrasound over other modalities for vascular imaging includes lack of radiation, low cost of the examination, and its widespread use in rheumatology for joint evaluation. Thus, this assessment could potentially be performed ‘at the bedside’ during consultation to provide immediate valuable information to complement clinical data from history, physical examination, and laboratory data,” they added.
The study retrospectively examined a prospective, observational cohort of 559 patients with psoriasis alone or psoriasis and psoriatic arthritis enrolled in the University of Toronto Psoriatic Disease Program. The investigators evaluated five ultrasound measures of atherosclerosis, including total plaque area (TPA), mean carotid intima-media thickness (cIMT), maximal cIMT, plaque category, and TPA category. Then they analyzed the risk relationship with major cardiovascular events (CVEs) classified as myocardial infarction, unstable angina, ischemic stroke, revascularization procedures, or cardiovascular-related death. Minor CVEs included stable angina, exacerbation of congestive heart failure, and transient ischemic attack over a mean follow-up close to 4 years.
The mean baseline TPA was 0.18 cm2 and mean cIMT was 639 mcm. Most patients had plaques, including 27.0% with unilateral and 31.5% with bilateral plaques.
The rate of a first CVE during the study period was 1.11 per 100 patient-years, and the rate of a first major CVE was 0.91 per 100 patient-years. The risk of each was significantly related to a higher baseline burden of atherosclerosis.
A multivariate analysis determined that increased TPA at baseline increased the risk of an event by nearly 200% (hazard ratio, 2.85). Mean cIMT was not an independent predictor in the final analysis, “suggesting that TPA is a stronger predictor for CVE than cIMT,” the authors wrote.
Finally, they examined the predictive value of atherosclerosis alone, as well as combined with the Framingham risk score. The 5-year model indicated that the bivariate model was slightly more accurate than the Framingham score alone (area under the curve, 0.84 vs. 0.81), although this was not a significant difference. The predictive value of the Framingham risk score plus maximal cIMT, mean cIMT, or TPA all significantly improved when they were calculated using only high-risk patients (those above the treatment threshold for dyslipidemia).
“To the best of our knowledge this is the first study to assess the utility of various measures of carotid atherosclerosis to predict CVE in patients with psoriasis and PsA [psoriatic arthritis]. ... Combining vascular imaging data with clinical and laboratory measures of traditional cardiovascular risk factors could improve accuracy of cardiovascular risk stratification in patients with psoriatic disease and facilitate earlier initiation of appropriate treatment to reduce CVE in this population,” the investigators wrote.
The study was supported in part by a Young Investigator Operating Grant from the Arthritis Society. Dr. Sobchak had no financial disclosures.
SOURCE: Sobchak C et al. Arthritis Rheumatol. 2019 Jun 5. doi: 10.1002/art.40925.
according to findings from a retrospective study.
When added to the Framingham risk score, the measurement significantly improved its predictive ability, Curtis Sobchak, MD, and colleagues wrote in Arthritis & Rheumatology.
The findings indicate that carotid ultrasound could be a useful addition to cardiovascular risk stratification among these patients.
“Traditional algorithms do not consider other factors that may contribute to increased cardiovascular risk in rheumatic disease patients and tend to underestimate cardiovascular risk,” wrote Dr. Sobchak of the University of Toronto and coauthors.
“The advantage of ultrasound over other modalities for vascular imaging includes lack of radiation, low cost of the examination, and its widespread use in rheumatology for joint evaluation. Thus, this assessment could potentially be performed ‘at the bedside’ during consultation to provide immediate valuable information to complement clinical data from history, physical examination, and laboratory data,” they added.
The study retrospectively examined a prospective, observational cohort of 559 patients with psoriasis alone or psoriasis and psoriatic arthritis enrolled in the University of Toronto Psoriatic Disease Program. The investigators evaluated five ultrasound measures of atherosclerosis, including total plaque area (TPA), mean carotid intima-media thickness (cIMT), maximal cIMT, plaque category, and TPA category. Then they analyzed the risk relationship with major cardiovascular events (CVEs) classified as myocardial infarction, unstable angina, ischemic stroke, revascularization procedures, or cardiovascular-related death. Minor CVEs included stable angina, exacerbation of congestive heart failure, and transient ischemic attack over a mean follow-up close to 4 years.
The mean baseline TPA was 0.18 cm2 and mean cIMT was 639 mcm. Most patients had plaques, including 27.0% with unilateral and 31.5% with bilateral plaques.
The rate of a first CVE during the study period was 1.11 per 100 patient-years, and the rate of a first major CVE was 0.91 per 100 patient-years. The risk of each was significantly related to a higher baseline burden of atherosclerosis.
A multivariate analysis determined that increased TPA at baseline increased the risk of an event by nearly 200% (hazard ratio, 2.85). Mean cIMT was not an independent predictor in the final analysis, “suggesting that TPA is a stronger predictor for CVE than cIMT,” the authors wrote.
Finally, they examined the predictive value of atherosclerosis alone, as well as combined with the Framingham risk score. The 5-year model indicated that the bivariate model was slightly more accurate than the Framingham score alone (area under the curve, 0.84 vs. 0.81), although this was not a significant difference. The predictive value of the Framingham risk score plus maximal cIMT, mean cIMT, or TPA all significantly improved when they were calculated using only high-risk patients (those above the treatment threshold for dyslipidemia).
“To the best of our knowledge this is the first study to assess the utility of various measures of carotid atherosclerosis to predict CVE in patients with psoriasis and PsA [psoriatic arthritis]. ... Combining vascular imaging data with clinical and laboratory measures of traditional cardiovascular risk factors could improve accuracy of cardiovascular risk stratification in patients with psoriatic disease and facilitate earlier initiation of appropriate treatment to reduce CVE in this population,” the investigators wrote.
The study was supported in part by a Young Investigator Operating Grant from the Arthritis Society. Dr. Sobchak had no financial disclosures.
SOURCE: Sobchak C et al. Arthritis Rheumatol. 2019 Jun 5. doi: 10.1002/art.40925.
according to findings from a retrospective study.
When added to the Framingham risk score, the measurement significantly improved its predictive ability, Curtis Sobchak, MD, and colleagues wrote in Arthritis & Rheumatology.
The findings indicate that carotid ultrasound could be a useful addition to cardiovascular risk stratification among these patients.
“Traditional algorithms do not consider other factors that may contribute to increased cardiovascular risk in rheumatic disease patients and tend to underestimate cardiovascular risk,” wrote Dr. Sobchak of the University of Toronto and coauthors.
“The advantage of ultrasound over other modalities for vascular imaging includes lack of radiation, low cost of the examination, and its widespread use in rheumatology for joint evaluation. Thus, this assessment could potentially be performed ‘at the bedside’ during consultation to provide immediate valuable information to complement clinical data from history, physical examination, and laboratory data,” they added.
The study retrospectively examined a prospective, observational cohort of 559 patients with psoriasis alone or psoriasis and psoriatic arthritis enrolled in the University of Toronto Psoriatic Disease Program. The investigators evaluated five ultrasound measures of atherosclerosis, including total plaque area (TPA), mean carotid intima-media thickness (cIMT), maximal cIMT, plaque category, and TPA category. Then they analyzed the risk relationship with major cardiovascular events (CVEs) classified as myocardial infarction, unstable angina, ischemic stroke, revascularization procedures, or cardiovascular-related death. Minor CVEs included stable angina, exacerbation of congestive heart failure, and transient ischemic attack over a mean follow-up close to 4 years.
The mean baseline TPA was 0.18 cm2 and mean cIMT was 639 mcm. Most patients had plaques, including 27.0% with unilateral and 31.5% with bilateral plaques.
The rate of a first CVE during the study period was 1.11 per 100 patient-years, and the rate of a first major CVE was 0.91 per 100 patient-years. The risk of each was significantly related to a higher baseline burden of atherosclerosis.
A multivariate analysis determined that increased TPA at baseline increased the risk of an event by nearly 200% (hazard ratio, 2.85). Mean cIMT was not an independent predictor in the final analysis, “suggesting that TPA is a stronger predictor for CVE than cIMT,” the authors wrote.
Finally, they examined the predictive value of atherosclerosis alone, as well as combined with the Framingham risk score. The 5-year model indicated that the bivariate model was slightly more accurate than the Framingham score alone (area under the curve, 0.84 vs. 0.81), although this was not a significant difference. The predictive value of the Framingham risk score plus maximal cIMT, mean cIMT, or TPA all significantly improved when they were calculated using only high-risk patients (those above the treatment threshold for dyslipidemia).
“To the best of our knowledge this is the first study to assess the utility of various measures of carotid atherosclerosis to predict CVE in patients with psoriasis and PsA [psoriatic arthritis]. ... Combining vascular imaging data with clinical and laboratory measures of traditional cardiovascular risk factors could improve accuracy of cardiovascular risk stratification in patients with psoriatic disease and facilitate earlier initiation of appropriate treatment to reduce CVE in this population,” the investigators wrote.
The study was supported in part by a Young Investigator Operating Grant from the Arthritis Society. Dr. Sobchak had no financial disclosures.
SOURCE: Sobchak C et al. Arthritis Rheumatol. 2019 Jun 5. doi: 10.1002/art.40925.
FROM ARTHRITIS & RHEUMATOLOGY
VIDEO: Did You Know? Psoriasis and mental health
The American Academy of Dermatology and the National Psoriasis Foundation recently issued a joint guideline on the management and treatment of psoriasis, with a focus on comorbidities. The guideline offers information and recommendations on mental health in patients with psoriasis.

The American Academy of Dermatology and the National Psoriasis Foundation recently issued a joint guideline on the management and treatment of psoriasis, with a focus on comorbidities. The guideline offers information and recommendations on mental health in patients with psoriasis.

The American Academy of Dermatology and the National Psoriasis Foundation recently issued a joint guideline on the management and treatment of psoriasis, with a focus on comorbidities. The guideline offers information and recommendations on mental health in patients with psoriasis.

Psoriasis Journal Scan: May 2019
The Broad-Spectrum Impact of Hidradenitis Suppurativa on Quality of Life: A Comparison with Psoriasis.
Sampogna F, Fania L, Mazzanti C, et al. Dermatology. 2019 May 23:1-7.
The aim of this study was to evaluate in detail the QoL impact of HS comparing it with other skin conditions, and in particular with psoriasis. HS had the worst QoL among several skin conditions. Compared to psoriasis the mean symptom score was 69.4 versus 53.7, and the mean psychosocial score was 56.1 versus 32.7. Overall, the scores of patients with HS were higher than those of psoriasis patients on 16 of the 17 items of the Skindex-17.
Suicidality and risk of suicidality in psoriasis: A critical appraisal of two systematic reviews and meta-analyses.
Matterne U, Baumeister SE, Apfelbacher C. Br J Dermatol. 2019 May 10.
Chi et al. and Singh et al each conducted a systematic review and meta-analysis of observational studies examining the relationship between suicidality and psoriasis. Singh et al. concluded that patients with psoriasis have a significantly higher risk of suicidal ideation, suicide attempts, and completed suicides, while Chi et al concluded that the available limited, very low-quality evidence does not support the notion of an association between psoriasis on the one hand, and suicide, suicidal ideation and attempts on the other.
Psoriasis and Inflammatory Bowel Disease.
Cottone M, Sapienza C, Macaluso FS, Cannizzaro M. Dig Dis. 2019 May 10:1-7.
Inflammatory bowel disease (IBD) and psoriasis (PS) are associated conditions. The reason for this association lies in the sharing of predisposition genes and common immunological mechanisms. This review will focus on the interplay between IBD and PS, with details on prevalence and phenotype of PS in IBD, genetics, pathogenetic pathways, and therapy.
Psoriasis in HIV infection: an update.
Alpalhão M, Borges-Costa J, Filipe P. Int J STD AIDS. 2019 May;30(6):596-604.
A review of the available literature to highlight the updated evidence on psoriasis in HIV-infected individuals, particularly in regards to its epidemiology, proposed pathophysiology, clinical presentation, currently available therapeutic options, and future perspectives.
All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis.
Dhana A, Yen H, Yen H, Cho E. J Am Acad Dermatol. 2019 May;80(5):1332-1343.
A systematic review and meta-analysis of mortality risk in psoriasis that included studies reporting all-cause or cause-specific mortality risk estimates in psoriasis patients compared with general population or subjects free of psoriasis. The pooled RRs for cardiovascular mortality were 1.15 (95% CI 1.09-1.21) in psoriasis, 1.05 (95% CI 0.92-1.20) in mild psoriasis, and 1.38 (95% CI 1.09-1.74) in severe psoriasis. For noncardiovascular causes, mortality risk from liver disease, kidney disease, and infection was significantly increased in psoriasis, regardless of disease severity.
The Broad-Spectrum Impact of Hidradenitis Suppurativa on Quality of Life: A Comparison with Psoriasis.
Sampogna F, Fania L, Mazzanti C, et al. Dermatology. 2019 May 23:1-7.
The aim of this study was to evaluate in detail the QoL impact of HS comparing it with other skin conditions, and in particular with psoriasis. HS had the worst QoL among several skin conditions. Compared to psoriasis the mean symptom score was 69.4 versus 53.7, and the mean psychosocial score was 56.1 versus 32.7. Overall, the scores of patients with HS were higher than those of psoriasis patients on 16 of the 17 items of the Skindex-17.
Suicidality and risk of suicidality in psoriasis: A critical appraisal of two systematic reviews and meta-analyses.
Matterne U, Baumeister SE, Apfelbacher C. Br J Dermatol. 2019 May 10.
Chi et al. and Singh et al each conducted a systematic review and meta-analysis of observational studies examining the relationship between suicidality and psoriasis. Singh et al. concluded that patients with psoriasis have a significantly higher risk of suicidal ideation, suicide attempts, and completed suicides, while Chi et al concluded that the available limited, very low-quality evidence does not support the notion of an association between psoriasis on the one hand, and suicide, suicidal ideation and attempts on the other.
Psoriasis and Inflammatory Bowel Disease.
Cottone M, Sapienza C, Macaluso FS, Cannizzaro M. Dig Dis. 2019 May 10:1-7.
Inflammatory bowel disease (IBD) and psoriasis (PS) are associated conditions. The reason for this association lies in the sharing of predisposition genes and common immunological mechanisms. This review will focus on the interplay between IBD and PS, with details on prevalence and phenotype of PS in IBD, genetics, pathogenetic pathways, and therapy.
Psoriasis in HIV infection: an update.
Alpalhão M, Borges-Costa J, Filipe P. Int J STD AIDS. 2019 May;30(6):596-604.
A review of the available literature to highlight the updated evidence on psoriasis in HIV-infected individuals, particularly in regards to its epidemiology, proposed pathophysiology, clinical presentation, currently available therapeutic options, and future perspectives.
All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis.
Dhana A, Yen H, Yen H, Cho E. J Am Acad Dermatol. 2019 May;80(5):1332-1343.
A systematic review and meta-analysis of mortality risk in psoriasis that included studies reporting all-cause or cause-specific mortality risk estimates in psoriasis patients compared with general population or subjects free of psoriasis. The pooled RRs for cardiovascular mortality were 1.15 (95% CI 1.09-1.21) in psoriasis, 1.05 (95% CI 0.92-1.20) in mild psoriasis, and 1.38 (95% CI 1.09-1.74) in severe psoriasis. For noncardiovascular causes, mortality risk from liver disease, kidney disease, and infection was significantly increased in psoriasis, regardless of disease severity.
The Broad-Spectrum Impact of Hidradenitis Suppurativa on Quality of Life: A Comparison with Psoriasis.
Sampogna F, Fania L, Mazzanti C, et al. Dermatology. 2019 May 23:1-7.
The aim of this study was to evaluate in detail the QoL impact of HS comparing it with other skin conditions, and in particular with psoriasis. HS had the worst QoL among several skin conditions. Compared to psoriasis the mean symptom score was 69.4 versus 53.7, and the mean psychosocial score was 56.1 versus 32.7. Overall, the scores of patients with HS were higher than those of psoriasis patients on 16 of the 17 items of the Skindex-17.
Suicidality and risk of suicidality in psoriasis: A critical appraisal of two systematic reviews and meta-analyses.
Matterne U, Baumeister SE, Apfelbacher C. Br J Dermatol. 2019 May 10.
Chi et al. and Singh et al each conducted a systematic review and meta-analysis of observational studies examining the relationship between suicidality and psoriasis. Singh et al. concluded that patients with psoriasis have a significantly higher risk of suicidal ideation, suicide attempts, and completed suicides, while Chi et al concluded that the available limited, very low-quality evidence does not support the notion of an association between psoriasis on the one hand, and suicide, suicidal ideation and attempts on the other.
Psoriasis and Inflammatory Bowel Disease.
Cottone M, Sapienza C, Macaluso FS, Cannizzaro M. Dig Dis. 2019 May 10:1-7.
Inflammatory bowel disease (IBD) and psoriasis (PS) are associated conditions. The reason for this association lies in the sharing of predisposition genes and common immunological mechanisms. This review will focus on the interplay between IBD and PS, with details on prevalence and phenotype of PS in IBD, genetics, pathogenetic pathways, and therapy.
Psoriasis in HIV infection: an update.
Alpalhão M, Borges-Costa J, Filipe P. Int J STD AIDS. 2019 May;30(6):596-604.
A review of the available literature to highlight the updated evidence on psoriasis in HIV-infected individuals, particularly in regards to its epidemiology, proposed pathophysiology, clinical presentation, currently available therapeutic options, and future perspectives.
All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis.
Dhana A, Yen H, Yen H, Cho E. J Am Acad Dermatol. 2019 May;80(5):1332-1343.
A systematic review and meta-analysis of mortality risk in psoriasis that included studies reporting all-cause or cause-specific mortality risk estimates in psoriasis patients compared with general population or subjects free of psoriasis. The pooled RRs for cardiovascular mortality were 1.15 (95% CI 1.09-1.21) in psoriasis, 1.05 (95% CI 0.92-1.20) in mild psoriasis, and 1.38 (95% CI 1.09-1.74) in severe psoriasis. For noncardiovascular causes, mortality risk from liver disease, kidney disease, and infection was significantly increased in psoriasis, regardless of disease severity.
Etanercept biosimilar SB4 a cost-effective alternative for psoriasis, PsA
The development of biosimilars such as etanercept SB4 offers a “significant opportunity to decrease medical care cost and increase treatment options,” Alessandro Giunta, MD, of the department of dermatology at the University of Rome Tor Vergata, and associates reported in a letter to the editor in the British Journal of Dermatology.
Dr. Giunta and his associates performed an observational, retrospective, single-center study to investigate etanercept biosimilar SB4 in patients being treated for plaque type psoriasis and psoriatic arthritis (PsA). They evaluated 40 patients – 21 men and 19 women – mean age 55, ranging from 19 to 79 years. The patients received the etanercept biosimilar SB4 between Oct. 21, 2016, and March 31, 2017, at University of Rome Tor Vergata’s department of dermatology. (The etanercept biosimilar SB4 was approved April 29 by the Food and Drug Administration under the brand name Eticovo [etanercept-ykro]. It is also approved in other countries under the names Benepali and Brenzys.)
Accounting for erythrocyte sedimentation rate as a variable, Dr. Giunta and colleagues calculated disease activity scores based on 28 joints; 14 patients (35%) had plaque psoriasis (mean Psoriasis Area Severity Index [PASI] of 9.61 at baseline), while 26 (65%) had psoriatic arthritis (mean PASI, 4.69). All patients reported prior treatment with systemic conventional and biologic treatments. A group of 10 patients (25%) who had been previously treated with etanercept originator underwent an intermittent treatment regimen of 24 weeks with etanercept biosimilar, which was interrupted once clinical resolution was achieved. No treatments were prescribed between etanercept originator and etanercept biosimilar. Mean exposure was 50.4 weeks, ranging from 24 to 96 weeks, with an average washout period of 12.1 weeks from originator to biosimilar (range 8-24).
A significant improvement in mean PASI score was observed in plaque type psoriasis patients as well as psoriatic arthritis patients at week 24 (P less than .0001 and P less than .001, respectively), noted Dr. Giunta and associates.
“All scores achieved a statistical significant improvement with the exception of [swollen joint count] that markedly improved but not significantly,” they added. One patient experienced injection site reaction, but no serious adverse events were observed.
Despite low sample size and limited follow-up time, the authors concluded that etanercept biosimilar achieved effectiveness as a treatment for psoriatic patients even in cases involving previous exposure to originator etanercept. Cost savings of 61.58% for 50-mg treatment and 62.55% for 25-mg treatment respectively guaranteed “the continuity of etanercept-treated patients’ care and gave us the opportunity to allocate patients in innovative but more expensive agents with marginal increase in our annual budget,” they noted.
The authors reported serving as consultants and speakers for AbbVie, Biogen, Eli Lilly, Janssen, Pfizer, and Novartis.
SOURCE: Giunta A et al. Br J Dermatol. 2019 May 3. doi: 10.1111/bjd.18090.
The development of biosimilars such as etanercept SB4 offers a “significant opportunity to decrease medical care cost and increase treatment options,” Alessandro Giunta, MD, of the department of dermatology at the University of Rome Tor Vergata, and associates reported in a letter to the editor in the British Journal of Dermatology.
Dr. Giunta and his associates performed an observational, retrospective, single-center study to investigate etanercept biosimilar SB4 in patients being treated for plaque type psoriasis and psoriatic arthritis (PsA). They evaluated 40 patients – 21 men and 19 women – mean age 55, ranging from 19 to 79 years. The patients received the etanercept biosimilar SB4 between Oct. 21, 2016, and March 31, 2017, at University of Rome Tor Vergata’s department of dermatology. (The etanercept biosimilar SB4 was approved April 29 by the Food and Drug Administration under the brand name Eticovo [etanercept-ykro]. It is also approved in other countries under the names Benepali and Brenzys.)
Accounting for erythrocyte sedimentation rate as a variable, Dr. Giunta and colleagues calculated disease activity scores based on 28 joints; 14 patients (35%) had plaque psoriasis (mean Psoriasis Area Severity Index [PASI] of 9.61 at baseline), while 26 (65%) had psoriatic arthritis (mean PASI, 4.69). All patients reported prior treatment with systemic conventional and biologic treatments. A group of 10 patients (25%) who had been previously treated with etanercept originator underwent an intermittent treatment regimen of 24 weeks with etanercept biosimilar, which was interrupted once clinical resolution was achieved. No treatments were prescribed between etanercept originator and etanercept biosimilar. Mean exposure was 50.4 weeks, ranging from 24 to 96 weeks, with an average washout period of 12.1 weeks from originator to biosimilar (range 8-24).
A significant improvement in mean PASI score was observed in plaque type psoriasis patients as well as psoriatic arthritis patients at week 24 (P less than .0001 and P less than .001, respectively), noted Dr. Giunta and associates.
“All scores achieved a statistical significant improvement with the exception of [swollen joint count] that markedly improved but not significantly,” they added. One patient experienced injection site reaction, but no serious adverse events were observed.
Despite low sample size and limited follow-up time, the authors concluded that etanercept biosimilar achieved effectiveness as a treatment for psoriatic patients even in cases involving previous exposure to originator etanercept. Cost savings of 61.58% for 50-mg treatment and 62.55% for 25-mg treatment respectively guaranteed “the continuity of etanercept-treated patients’ care and gave us the opportunity to allocate patients in innovative but more expensive agents with marginal increase in our annual budget,” they noted.
The authors reported serving as consultants and speakers for AbbVie, Biogen, Eli Lilly, Janssen, Pfizer, and Novartis.
SOURCE: Giunta A et al. Br J Dermatol. 2019 May 3. doi: 10.1111/bjd.18090.
The development of biosimilars such as etanercept SB4 offers a “significant opportunity to decrease medical care cost and increase treatment options,” Alessandro Giunta, MD, of the department of dermatology at the University of Rome Tor Vergata, and associates reported in a letter to the editor in the British Journal of Dermatology.
Dr. Giunta and his associates performed an observational, retrospective, single-center study to investigate etanercept biosimilar SB4 in patients being treated for plaque type psoriasis and psoriatic arthritis (PsA). They evaluated 40 patients – 21 men and 19 women – mean age 55, ranging from 19 to 79 years. The patients received the etanercept biosimilar SB4 between Oct. 21, 2016, and March 31, 2017, at University of Rome Tor Vergata’s department of dermatology. (The etanercept biosimilar SB4 was approved April 29 by the Food and Drug Administration under the brand name Eticovo [etanercept-ykro]. It is also approved in other countries under the names Benepali and Brenzys.)
Accounting for erythrocyte sedimentation rate as a variable, Dr. Giunta and colleagues calculated disease activity scores based on 28 joints; 14 patients (35%) had plaque psoriasis (mean Psoriasis Area Severity Index [PASI] of 9.61 at baseline), while 26 (65%) had psoriatic arthritis (mean PASI, 4.69). All patients reported prior treatment with systemic conventional and biologic treatments. A group of 10 patients (25%) who had been previously treated with etanercept originator underwent an intermittent treatment regimen of 24 weeks with etanercept biosimilar, which was interrupted once clinical resolution was achieved. No treatments were prescribed between etanercept originator and etanercept biosimilar. Mean exposure was 50.4 weeks, ranging from 24 to 96 weeks, with an average washout period of 12.1 weeks from originator to biosimilar (range 8-24).
A significant improvement in mean PASI score was observed in plaque type psoriasis patients as well as psoriatic arthritis patients at week 24 (P less than .0001 and P less than .001, respectively), noted Dr. Giunta and associates.
“All scores achieved a statistical significant improvement with the exception of [swollen joint count] that markedly improved but not significantly,” they added. One patient experienced injection site reaction, but no serious adverse events were observed.
Despite low sample size and limited follow-up time, the authors concluded that etanercept biosimilar achieved effectiveness as a treatment for psoriatic patients even in cases involving previous exposure to originator etanercept. Cost savings of 61.58% for 50-mg treatment and 62.55% for 25-mg treatment respectively guaranteed “the continuity of etanercept-treated patients’ care and gave us the opportunity to allocate patients in innovative but more expensive agents with marginal increase in our annual budget,” they noted.
The authors reported serving as consultants and speakers for AbbVie, Biogen, Eli Lilly, Janssen, Pfizer, and Novartis.
SOURCE: Giunta A et al. Br J Dermatol. 2019 May 3. doi: 10.1111/bjd.18090.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Apremilast and Phototherapy for Treatment of Psoriasis in a Patient With Human Immunodeficiency Virus
To the Editor:
A 50-year old man with Fitzpatrick skin type IV, human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected) currently treated with clobetasol spray and calcitriol ointment presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. His CD4 count was 460 and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to the current presentation. He had been undergoing phototherapy 3 times weekly for the last 5 months for treatment of psoriasis.
At the current presentation, he was started on an apremilast starter pack with the dosage titrated from 10 mg to 30 mg over the course of 1 week. He was maintained on a dose of 30 mg twice daily after 1 week and continued clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the affected BSA was 0%. He continued apremilast, and phototherapy was reduced to once weekly. Phototherapy was discontinued after 7 months of concomitant treatment with apremilast after clearance was maintained. It was reinitiated twice weekly after a mild flare (3% BSA affected). After 20 total months of treatment, the patient was no longer able to afford apremilast treatment and presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with a plan to apply for apremilast financial assistance programs.
Psoriasis treatment in the HIV population poses a challenge given the immunosuppressed state of these patients, the risk of reactivation of latent infections, and the refractory nature of psoriasis in the setting of HIV. Two of the authors (S.P.R. and J.J.W.) previously reported a case of moderate to severe psoriasis in a patient with HIV and hepatitis C who demonstrated treatment success with apremilast until it was discontinued due to financial implications.1 Currently, apremilast is not widely used to treat psoriasis in the HIV population. The National Psoriasis Foundation 2010 guidelines recommended UV light therapy for treatment of moderate to severe psoriasis in HIV-positive patients, with oral retinoids as the second-line treatment.2 There remains a need for updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population.
Apremilast, a phosphodiesterase 4 inhibitor, is an oral therapy that restores the balance of proinflammatory and anti-inflammatory cytokines by inhibiting inflammatory cytokine (eg, tumor necrosis factor α, IFN-γ, IL-2, IL-12, IL-23) secretion and stimulating anti-inflammatory cytokine (eg, IL-6, IL-10) production. In 2015, the phase 3 ESTEEM 13 and ESTEEM 24 trials demonstrated the efficacy of apremilast 30 mg twice daily for treatment of psoriasis. In both trials, the psoriasis area and severity index 75 response rate at week 16 was significantly
Use of other systemic agents such as tumor necrosis factor α inhibitors and ustekinumab has been reported in HIV-positive patients.5-7 There is no current data on IL-17 and IL-23 inhibitors. Acitretin generally is recommended as a second-line agent in HIV patients given its lack of immunosuppression2; however, methotrexate and cyclosporine should be avoided given the risk of opportunistic infections.8
Apremilast is a promising therapy with a favorable safety profile that should be considered as an adjuvant treatment to first-line agents such as phototherapy in HIV-positive patients. Apremilast has been successfully used in an HIV patient with a concomitant chronic hepatitis C infection.1 Systemic medications such as apremilast should be managed in coordination with infectious disease specialists with close monitoring of CD4 levels and viral loads as well as prophylactic agents.
- Reddy SP, Shah VV, Wu JJ. Apremilast for a psoriasis patient with HIV and hepatitis C. J Eur Acad Dermatol Venereol. 2017;31:e481-e482.
- Menon K, Van Voorhees AS, Bebo BF Jr, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation [published online July 31, 2009]. J Am Acad Dermatol. 2010;62:291-299.
- Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73:37-49.
- Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173:1387-1399.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV-positive patient. J Drugs Dermatol. 2014;13:869-871.
- Saeki H, Ito T, Hayashi M, et al. Successful treatment of ustekinumab in a severe psoriasis patient with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 2015;29:1653-1655.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatolog Treat. 2012;23:398-399.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections [published online July 11, 2018]. J Am Acad Dermatol. 2019;80:43-53.
To the Editor:
A 50-year old man with Fitzpatrick skin type IV, human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected) currently treated with clobetasol spray and calcitriol ointment presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. His CD4 count was 460 and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to the current presentation. He had been undergoing phototherapy 3 times weekly for the last 5 months for treatment of psoriasis.
At the current presentation, he was started on an apremilast starter pack with the dosage titrated from 10 mg to 30 mg over the course of 1 week. He was maintained on a dose of 30 mg twice daily after 1 week and continued clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the affected BSA was 0%. He continued apremilast, and phototherapy was reduced to once weekly. Phototherapy was discontinued after 7 months of concomitant treatment with apremilast after clearance was maintained. It was reinitiated twice weekly after a mild flare (3% BSA affected). After 20 total months of treatment, the patient was no longer able to afford apremilast treatment and presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with a plan to apply for apremilast financial assistance programs.
Psoriasis treatment in the HIV population poses a challenge given the immunosuppressed state of these patients, the risk of reactivation of latent infections, and the refractory nature of psoriasis in the setting of HIV. Two of the authors (S.P.R. and J.J.W.) previously reported a case of moderate to severe psoriasis in a patient with HIV and hepatitis C who demonstrated treatment success with apremilast until it was discontinued due to financial implications.1 Currently, apremilast is not widely used to treat psoriasis in the HIV population. The National Psoriasis Foundation 2010 guidelines recommended UV light therapy for treatment of moderate to severe psoriasis in HIV-positive patients, with oral retinoids as the second-line treatment.2 There remains a need for updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population.
Apremilast, a phosphodiesterase 4 inhibitor, is an oral therapy that restores the balance of proinflammatory and anti-inflammatory cytokines by inhibiting inflammatory cytokine (eg, tumor necrosis factor α, IFN-γ, IL-2, IL-12, IL-23) secretion and stimulating anti-inflammatory cytokine (eg, IL-6, IL-10) production. In 2015, the phase 3 ESTEEM 13 and ESTEEM 24 trials demonstrated the efficacy of apremilast 30 mg twice daily for treatment of psoriasis. In both trials, the psoriasis area and severity index 75 response rate at week 16 was significantly
Use of other systemic agents such as tumor necrosis factor α inhibitors and ustekinumab has been reported in HIV-positive patients.5-7 There is no current data on IL-17 and IL-23 inhibitors. Acitretin generally is recommended as a second-line agent in HIV patients given its lack of immunosuppression2; however, methotrexate and cyclosporine should be avoided given the risk of opportunistic infections.8
Apremilast is a promising therapy with a favorable safety profile that should be considered as an adjuvant treatment to first-line agents such as phototherapy in HIV-positive patients. Apremilast has been successfully used in an HIV patient with a concomitant chronic hepatitis C infection.1 Systemic medications such as apremilast should be managed in coordination with infectious disease specialists with close monitoring of CD4 levels and viral loads as well as prophylactic agents.
To the Editor:
A 50-year old man with Fitzpatrick skin type IV, human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected) currently treated with clobetasol spray and calcitriol ointment presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. His CD4 count was 460 and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to the current presentation. He had been undergoing phototherapy 3 times weekly for the last 5 months for treatment of psoriasis.
At the current presentation, he was started on an apremilast starter pack with the dosage titrated from 10 mg to 30 mg over the course of 1 week. He was maintained on a dose of 30 mg twice daily after 1 week and continued clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the affected BSA was 0%. He continued apremilast, and phototherapy was reduced to once weekly. Phototherapy was discontinued after 7 months of concomitant treatment with apremilast after clearance was maintained. It was reinitiated twice weekly after a mild flare (3% BSA affected). After 20 total months of treatment, the patient was no longer able to afford apremilast treatment and presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with a plan to apply for apremilast financial assistance programs.
Psoriasis treatment in the HIV population poses a challenge given the immunosuppressed state of these patients, the risk of reactivation of latent infections, and the refractory nature of psoriasis in the setting of HIV. Two of the authors (S.P.R. and J.J.W.) previously reported a case of moderate to severe psoriasis in a patient with HIV and hepatitis C who demonstrated treatment success with apremilast until it was discontinued due to financial implications.1 Currently, apremilast is not widely used to treat psoriasis in the HIV population. The National Psoriasis Foundation 2010 guidelines recommended UV light therapy for treatment of moderate to severe psoriasis in HIV-positive patients, with oral retinoids as the second-line treatment.2 There remains a need for updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population.
Apremilast, a phosphodiesterase 4 inhibitor, is an oral therapy that restores the balance of proinflammatory and anti-inflammatory cytokines by inhibiting inflammatory cytokine (eg, tumor necrosis factor α, IFN-γ, IL-2, IL-12, IL-23) secretion and stimulating anti-inflammatory cytokine (eg, IL-6, IL-10) production. In 2015, the phase 3 ESTEEM 13 and ESTEEM 24 trials demonstrated the efficacy of apremilast 30 mg twice daily for treatment of psoriasis. In both trials, the psoriasis area and severity index 75 response rate at week 16 was significantly
Use of other systemic agents such as tumor necrosis factor α inhibitors and ustekinumab has been reported in HIV-positive patients.5-7 There is no current data on IL-17 and IL-23 inhibitors. Acitretin generally is recommended as a second-line agent in HIV patients given its lack of immunosuppression2; however, methotrexate and cyclosporine should be avoided given the risk of opportunistic infections.8
Apremilast is a promising therapy with a favorable safety profile that should be considered as an adjuvant treatment to first-line agents such as phototherapy in HIV-positive patients. Apremilast has been successfully used in an HIV patient with a concomitant chronic hepatitis C infection.1 Systemic medications such as apremilast should be managed in coordination with infectious disease specialists with close monitoring of CD4 levels and viral loads as well as prophylactic agents.
- Reddy SP, Shah VV, Wu JJ. Apremilast for a psoriasis patient with HIV and hepatitis C. J Eur Acad Dermatol Venereol. 2017;31:e481-e482.
- Menon K, Van Voorhees AS, Bebo BF Jr, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation [published online July 31, 2009]. J Am Acad Dermatol. 2010;62:291-299.
- Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73:37-49.
- Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173:1387-1399.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV-positive patient. J Drugs Dermatol. 2014;13:869-871.
- Saeki H, Ito T, Hayashi M, et al. Successful treatment of ustekinumab in a severe psoriasis patient with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 2015;29:1653-1655.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatolog Treat. 2012;23:398-399.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections [published online July 11, 2018]. J Am Acad Dermatol. 2019;80:43-53.
- Reddy SP, Shah VV, Wu JJ. Apremilast for a psoriasis patient with HIV and hepatitis C. J Eur Acad Dermatol Venereol. 2017;31:e481-e482.
- Menon K, Van Voorhees AS, Bebo BF Jr, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation [published online July 31, 2009]. J Am Acad Dermatol. 2010;62:291-299.
- Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73:37-49.
- Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173:1387-1399.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV-positive patient. J Drugs Dermatol. 2014;13:869-871.
- Saeki H, Ito T, Hayashi M, et al. Successful treatment of ustekinumab in a severe psoriasis patient with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 2015;29:1653-1655.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatolog Treat. 2012;23:398-399.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections [published online July 11, 2018]. J Am Acad Dermatol. 2019;80:43-53.
Practice Point
- Apremilast may be considered as a first-line therapy in the human immunodeficiency virus population due to decreased immunosuppression.
Positive psoriatic arthritis screens occur often in psoriasis patients
One out of eight patients with psoriasis had a positive screen for possibly undiagnosed psoriatic arthritis, according to an analysis of data from a prospective registry.
The finding highlights the need for better psoriatic arthritis screening among patients with psoriasis, said Philip J. Mease, MD, of the University of Washington, Seattle, and associates. The simple, five-question Psoriasis Epidemiology Screening Tool (PEST) used in this study could be deployed in general or dermatology practices to identify psoriasis patients who might need a rheumatology referral, they wrote. The report is in the Journal of the European Academy of Dermatology and Venereology.
Up to 30% of patients with psoriasis have comorbid psoriatic arthritis, but many such cases go undiagnosed, and even a 6-month diagnostic delay can worsen peripheral joint erosion and physical disability.
This study included 1,516 patients with psoriasis seen at 114 private and academic practices in 34 states that participate in the independent, prospective Corrona Psoriasis Registry. A total of 904 patients without dermatologist-reported psoriatic arthritis responded to the validated PEST, which assesses risk of psoriatic arthritis by asking whether the test taker has been told by a doctor that he or she has arthritis and whether they have experienced swollen joints, heel pain, pronounced and unexplained swelling of a finger or toe, and pitting of the fingernails or toenails. Each “yes” response is worth 1 point, and total scores of 3 or higher indicate risk of psoriatic arthritis. A total of 112 (12.4%) had a score of 3 or higher.
The average age of patients who met this threshold was 53 years, 4 years older than those who did not (P = .02). Patients with PEST scores of 3 or more also had a significantly longer duration of psoriasis and were significantly more likely to have nail disease and a family history of psoriasis. Demographically, they were more likely to be white, female, and unemployed. They had significantly higher rates of several comorbidities, including depression and anxiety, cardiovascular disease, obesity, and serious infections. Finally, they reported having significantly more pain and fatigue and significantly worse health-related quality of life.
The study did not account for possible confounding. “Further research is needed to characterize patients by individual PEST score and to assess outcomes over time,” the researchers wrote. “The use of screening tools can be beneficial in the detection of psoriatic arthritis, and comprehensive efforts to validate them in multiple clinical settings must continue, along with collection of critical feedback from patients and clinicians.”
Corrona and Novartis designed and helped conduct the study. Novartis, the chief funder, participated in data analysis and manuscript review. Dr. Mease disclosed research funding from Novartis and several other pharmaceutical companies. He also disclosed consulting and speakers bureau fees from Novartis, Corrona, and several other companies.
SOURCE: Mease PJ et al. J Eur Acad Dermatol Venereol. 2019 Mar 5. doi: 10.1111/jdv.15443.
One out of eight patients with psoriasis had a positive screen for possibly undiagnosed psoriatic arthritis, according to an analysis of data from a prospective registry.
The finding highlights the need for better psoriatic arthritis screening among patients with psoriasis, said Philip J. Mease, MD, of the University of Washington, Seattle, and associates. The simple, five-question Psoriasis Epidemiology Screening Tool (PEST) used in this study could be deployed in general or dermatology practices to identify psoriasis patients who might need a rheumatology referral, they wrote. The report is in the Journal of the European Academy of Dermatology and Venereology.
Up to 30% of patients with psoriasis have comorbid psoriatic arthritis, but many such cases go undiagnosed, and even a 6-month diagnostic delay can worsen peripheral joint erosion and physical disability.
This study included 1,516 patients with psoriasis seen at 114 private and academic practices in 34 states that participate in the independent, prospective Corrona Psoriasis Registry. A total of 904 patients without dermatologist-reported psoriatic arthritis responded to the validated PEST, which assesses risk of psoriatic arthritis by asking whether the test taker has been told by a doctor that he or she has arthritis and whether they have experienced swollen joints, heel pain, pronounced and unexplained swelling of a finger or toe, and pitting of the fingernails or toenails. Each “yes” response is worth 1 point, and total scores of 3 or higher indicate risk of psoriatic arthritis. A total of 112 (12.4%) had a score of 3 or higher.
The average age of patients who met this threshold was 53 years, 4 years older than those who did not (P = .02). Patients with PEST scores of 3 or more also had a significantly longer duration of psoriasis and were significantly more likely to have nail disease and a family history of psoriasis. Demographically, they were more likely to be white, female, and unemployed. They had significantly higher rates of several comorbidities, including depression and anxiety, cardiovascular disease, obesity, and serious infections. Finally, they reported having significantly more pain and fatigue and significantly worse health-related quality of life.
The study did not account for possible confounding. “Further research is needed to characterize patients by individual PEST score and to assess outcomes over time,” the researchers wrote. “The use of screening tools can be beneficial in the detection of psoriatic arthritis, and comprehensive efforts to validate them in multiple clinical settings must continue, along with collection of critical feedback from patients and clinicians.”
Corrona and Novartis designed and helped conduct the study. Novartis, the chief funder, participated in data analysis and manuscript review. Dr. Mease disclosed research funding from Novartis and several other pharmaceutical companies. He also disclosed consulting and speakers bureau fees from Novartis, Corrona, and several other companies.
SOURCE: Mease PJ et al. J Eur Acad Dermatol Venereol. 2019 Mar 5. doi: 10.1111/jdv.15443.
One out of eight patients with psoriasis had a positive screen for possibly undiagnosed psoriatic arthritis, according to an analysis of data from a prospective registry.
The finding highlights the need for better psoriatic arthritis screening among patients with psoriasis, said Philip J. Mease, MD, of the University of Washington, Seattle, and associates. The simple, five-question Psoriasis Epidemiology Screening Tool (PEST) used in this study could be deployed in general or dermatology practices to identify psoriasis patients who might need a rheumatology referral, they wrote. The report is in the Journal of the European Academy of Dermatology and Venereology.
Up to 30% of patients with psoriasis have comorbid psoriatic arthritis, but many such cases go undiagnosed, and even a 6-month diagnostic delay can worsen peripheral joint erosion and physical disability.
This study included 1,516 patients with psoriasis seen at 114 private and academic practices in 34 states that participate in the independent, prospective Corrona Psoriasis Registry. A total of 904 patients without dermatologist-reported psoriatic arthritis responded to the validated PEST, which assesses risk of psoriatic arthritis by asking whether the test taker has been told by a doctor that he or she has arthritis and whether they have experienced swollen joints, heel pain, pronounced and unexplained swelling of a finger or toe, and pitting of the fingernails or toenails. Each “yes” response is worth 1 point, and total scores of 3 or higher indicate risk of psoriatic arthritis. A total of 112 (12.4%) had a score of 3 or higher.
The average age of patients who met this threshold was 53 years, 4 years older than those who did not (P = .02). Patients with PEST scores of 3 or more also had a significantly longer duration of psoriasis and were significantly more likely to have nail disease and a family history of psoriasis. Demographically, they were more likely to be white, female, and unemployed. They had significantly higher rates of several comorbidities, including depression and anxiety, cardiovascular disease, obesity, and serious infections. Finally, they reported having significantly more pain and fatigue and significantly worse health-related quality of life.
The study did not account for possible confounding. “Further research is needed to characterize patients by individual PEST score and to assess outcomes over time,” the researchers wrote. “The use of screening tools can be beneficial in the detection of psoriatic arthritis, and comprehensive efforts to validate them in multiple clinical settings must continue, along with collection of critical feedback from patients and clinicians.”
Corrona and Novartis designed and helped conduct the study. Novartis, the chief funder, participated in data analysis and manuscript review. Dr. Mease disclosed research funding from Novartis and several other pharmaceutical companies. He also disclosed consulting and speakers bureau fees from Novartis, Corrona, and several other companies.
SOURCE: Mease PJ et al. J Eur Acad Dermatol Venereol. 2019 Mar 5. doi: 10.1111/jdv.15443.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
FDA approves new etanercept biosimilar, Eticovo
The Food and Drug Administration has approved Eticovo (etanercept-ykro), a biosimilar of Enbrel (etanercept), for the treatment of several different rheumatologic and dermatologic conditions.
FDA approval was based in part on the results of a phase 3 trial in which 596 patients with moderate to severe rheumatoid arthritis uncontrolled by methotrexate received either Eticovo or Enbrel. The American College of Rheumatology 20% response rate after 24 weeks was 78.1% for Eticovo and 80.3% for Enbrel; the two drugs were statistically equivalent. Both groups had statistically equivalent rates of treatment-emergent adverse events (55.2% vs. 58.2%).
According to the label, Eticovo is a tumor necrosis factor blocker approved for the treatment of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis in patients aged 4 years or older. The most common adverse events associated with the drug include infections and injection site reactions.
Eticovo is the second etanercept biosimilar approved by the FDA. The first FDA-approved etanercept biosimilar, etanercept-szzs (Erelzi), is currently facing a legal challenge from Amgen, the manufacturer of Enbrel.
The Food and Drug Administration has approved Eticovo (etanercept-ykro), a biosimilar of Enbrel (etanercept), for the treatment of several different rheumatologic and dermatologic conditions.
FDA approval was based in part on the results of a phase 3 trial in which 596 patients with moderate to severe rheumatoid arthritis uncontrolled by methotrexate received either Eticovo or Enbrel. The American College of Rheumatology 20% response rate after 24 weeks was 78.1% for Eticovo and 80.3% for Enbrel; the two drugs were statistically equivalent. Both groups had statistically equivalent rates of treatment-emergent adverse events (55.2% vs. 58.2%).
According to the label, Eticovo is a tumor necrosis factor blocker approved for the treatment of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis in patients aged 4 years or older. The most common adverse events associated with the drug include infections and injection site reactions.
Eticovo is the second etanercept biosimilar approved by the FDA. The first FDA-approved etanercept biosimilar, etanercept-szzs (Erelzi), is currently facing a legal challenge from Amgen, the manufacturer of Enbrel.
The Food and Drug Administration has approved Eticovo (etanercept-ykro), a biosimilar of Enbrel (etanercept), for the treatment of several different rheumatologic and dermatologic conditions.
FDA approval was based in part on the results of a phase 3 trial in which 596 patients with moderate to severe rheumatoid arthritis uncontrolled by methotrexate received either Eticovo or Enbrel. The American College of Rheumatology 20% response rate after 24 weeks was 78.1% for Eticovo and 80.3% for Enbrel; the two drugs were statistically equivalent. Both groups had statistically equivalent rates of treatment-emergent adverse events (55.2% vs. 58.2%).
According to the label, Eticovo is a tumor necrosis factor blocker approved for the treatment of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis in patients aged 4 years or older. The most common adverse events associated with the drug include infections and injection site reactions.
Eticovo is the second etanercept biosimilar approved by the FDA. The first FDA-approved etanercept biosimilar, etanercept-szzs (Erelzi), is currently facing a legal challenge from Amgen, the manufacturer of Enbrel.
FDA approves corticosteroid-retinoid lotion for plaque psoriasis
The in a lotion formulation, for the treatment of plaque psoriasis in adults, the manufacturer announced on April 25.
A press release from the manufacturer, Ortho Dermatologics, summarized the results of two phase 3 studies that compared treatment with the combination product, in 418 adults with moderate to severe plaque psoriasis. At week 8, the proportion of patients who had achieved treatment success – defined as at least a two-grade improvement in Investigator Global Assessment score and a score of “clear” or “almost clear” – was 36% and 45% in the treatment groups, compared with 7% and 13% of those on vehicle, respectively (P less than .001 for both).
The release also refers to a phase 2 study of 212 patients, which found that the combination treatment was more effective in treating plaque psoriasis than was either component separately (J Drugs Dermatol. 2017 Mar 1;16[1]:197-204). By week 8, 52.5% of patients treated with the combination lotion had shown treatment success – compared with 33.3% of those treated with halobetasol, 18.6% of those treated with tazarotene, and 9.7% of those treated with vehicle (P = .033).
Common treatment-related adverse events included treatment site reactions, such as irritation, pain, itching, and folliculitis. Treatment may cause birth defects if used during pregnancy, so a negative pregnancy test should be obtained before treatment begins and effective birth control should be used during treatment.
It will be marketed under the trade name Duobrii and is priced at $825 for a 100-gram tube, according to the press release.
The in a lotion formulation, for the treatment of plaque psoriasis in adults, the manufacturer announced on April 25.
A press release from the manufacturer, Ortho Dermatologics, summarized the results of two phase 3 studies that compared treatment with the combination product, in 418 adults with moderate to severe plaque psoriasis. At week 8, the proportion of patients who had achieved treatment success – defined as at least a two-grade improvement in Investigator Global Assessment score and a score of “clear” or “almost clear” – was 36% and 45% in the treatment groups, compared with 7% and 13% of those on vehicle, respectively (P less than .001 for both).
The release also refers to a phase 2 study of 212 patients, which found that the combination treatment was more effective in treating plaque psoriasis than was either component separately (J Drugs Dermatol. 2017 Mar 1;16[1]:197-204). By week 8, 52.5% of patients treated with the combination lotion had shown treatment success – compared with 33.3% of those treated with halobetasol, 18.6% of those treated with tazarotene, and 9.7% of those treated with vehicle (P = .033).
Common treatment-related adverse events included treatment site reactions, such as irritation, pain, itching, and folliculitis. Treatment may cause birth defects if used during pregnancy, so a negative pregnancy test should be obtained before treatment begins and effective birth control should be used during treatment.
It will be marketed under the trade name Duobrii and is priced at $825 for a 100-gram tube, according to the press release.
The in a lotion formulation, for the treatment of plaque psoriasis in adults, the manufacturer announced on April 25.
A press release from the manufacturer, Ortho Dermatologics, summarized the results of two phase 3 studies that compared treatment with the combination product, in 418 adults with moderate to severe plaque psoriasis. At week 8, the proportion of patients who had achieved treatment success – defined as at least a two-grade improvement in Investigator Global Assessment score and a score of “clear” or “almost clear” – was 36% and 45% in the treatment groups, compared with 7% and 13% of those on vehicle, respectively (P less than .001 for both).
The release also refers to a phase 2 study of 212 patients, which found that the combination treatment was more effective in treating plaque psoriasis than was either component separately (J Drugs Dermatol. 2017 Mar 1;16[1]:197-204). By week 8, 52.5% of patients treated with the combination lotion had shown treatment success – compared with 33.3% of those treated with halobetasol, 18.6% of those treated with tazarotene, and 9.7% of those treated with vehicle (P = .033).
Common treatment-related adverse events included treatment site reactions, such as irritation, pain, itching, and folliculitis. Treatment may cause birth defects if used during pregnancy, so a negative pregnancy test should be obtained before treatment begins and effective birth control should be used during treatment.
It will be marketed under the trade name Duobrii and is priced at $825 for a 100-gram tube, according to the press release.