User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Recognizing Burnout: Why Physicians Often Miss the Signs in Themselves
Summary and Key Highlights
Summary: This section explores why physicians often struggle to recognize burnout within themselves, partly due to stigma and a tendency to focus on productivity over well-being. Dr. Tyra Fainstad shares personal experiences of burnout symptoms, emphasizing the importance of awareness and self-reflection. Recognizing and addressing burnout early can help physicians find healthier coping strategies, avoid productivity traps, and seek support.
Key Takeaways:
- Many physicians struggle to identify burnout due to stigma and self-blame.
- Awareness of burnout symptoms is essential for early intervention and healthy coping.
- Seeking support can prevent burnout from worsening and improve quality of life.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: This section explores why physicians often struggle to recognize burnout within themselves, partly due to stigma and a tendency to focus on productivity over well-being. Dr. Tyra Fainstad shares personal experiences of burnout symptoms, emphasizing the importance of awareness and self-reflection. Recognizing and addressing burnout early can help physicians find healthier coping strategies, avoid productivity traps, and seek support.
Key Takeaways:
- Many physicians struggle to identify burnout due to stigma and self-blame.
- Awareness of burnout symptoms is essential for early intervention and healthy coping.
- Seeking support can prevent burnout from worsening and improve quality of life.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: This section explores why physicians often struggle to recognize burnout within themselves, partly due to stigma and a tendency to focus on productivity over well-being. Dr. Tyra Fainstad shares personal experiences of burnout symptoms, emphasizing the importance of awareness and self-reflection. Recognizing and addressing burnout early can help physicians find healthier coping strategies, avoid productivity traps, and seek support.
Key Takeaways:
- Many physicians struggle to identify burnout due to stigma and self-blame.
- Awareness of burnout symptoms is essential for early intervention and healthy coping.
- Seeking support can prevent burnout from worsening and improve quality of life.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Breaking the Cycle: Why Self-Compassion Is Essential for Today’s Physicians
Summary and Key Highlights
Summary: Dr Tyra Fainstad explores the ingrained culture in medicine that encourages self-criticism, with many physicians feeling that they must be hard on themselves to succeed. Dr Fainstad challenges this belief, advocating for self-compassion as a healthier alternative. The evolving medical field now includes physicians who prioritize well-being without sacrificing quality of care, underscoring the importance of self-kindness for sustainable practice.
Key Takeaways:
- Many physicians believe that self-criticism is necessary for success, a mindset rooted in medical culture.
- Practicing self-compassion can improve long-term resilience and prevent burnout.
- The changing landscape of healthcare supports a more balanced approach to physician well-being.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad explores the ingrained culture in medicine that encourages self-criticism, with many physicians feeling that they must be hard on themselves to succeed. Dr Fainstad challenges this belief, advocating for self-compassion as a healthier alternative. The evolving medical field now includes physicians who prioritize well-being without sacrificing quality of care, underscoring the importance of self-kindness for sustainable practice.
Key Takeaways:
- Many physicians believe that self-criticism is necessary for success, a mindset rooted in medical culture.
- Practicing self-compassion can improve long-term resilience and prevent burnout.
- The changing landscape of healthcare supports a more balanced approach to physician well-being.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad explores the ingrained culture in medicine that encourages self-criticism, with many physicians feeling that they must be hard on themselves to succeed. Dr Fainstad challenges this belief, advocating for self-compassion as a healthier alternative. The evolving medical field now includes physicians who prioritize well-being without sacrificing quality of care, underscoring the importance of self-kindness for sustainable practice.
Key Takeaways:
- Many physicians believe that self-criticism is necessary for success, a mindset rooted in medical culture.
- Practicing self-compassion can improve long-term resilience and prevent burnout.
- The changing landscape of healthcare supports a more balanced approach to physician well-being.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Finding Fulfillment Beyond Metrics: A Physician’s Path to Lasting Well-Being
Summary and Key Highlights
Summary: Dr Tyra Fainstad shares her personal experience with burnout and the journey to recovery through coaching and self-compassion. She describes the pressures of seeking validation through external achievements, which ultimately led to a crisis in self-worth after medical training. Through coaching, she learned to cultivate a sense of internal fulfillment, reconnecting with her passion for medicine and achieving a healthier balance.
Key Takeaways:
- Relying solely on external validation can deepen burnout and affect well-being.
- Coaching empowers physicians to develop self-compassion and sustainable coping strategies.
- Shifting from external to internal validation strengthens long-term fulfillment and job satisfaction.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad shares her personal experience with burnout and the journey to recovery through coaching and self-compassion. She describes the pressures of seeking validation through external achievements, which ultimately led to a crisis in self-worth after medical training. Through coaching, she learned to cultivate a sense of internal fulfillment, reconnecting with her passion for medicine and achieving a healthier balance.
Key Takeaways:
- Relying solely on external validation can deepen burnout and affect well-being.
- Coaching empowers physicians to develop self-compassion and sustainable coping strategies.
- Shifting from external to internal validation strengthens long-term fulfillment and job satisfaction.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad shares her personal experience with burnout and the journey to recovery through coaching and self-compassion. She describes the pressures of seeking validation through external achievements, which ultimately led to a crisis in self-worth after medical training. Through coaching, she learned to cultivate a sense of internal fulfillment, reconnecting with her passion for medicine and achieving a healthier balance.
Key Takeaways:
- Relying solely on external validation can deepen burnout and affect well-being.
- Coaching empowers physicians to develop self-compassion and sustainable coping strategies.
- Shifting from external to internal validation strengthens long-term fulfillment and job satisfaction.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
A version of this article first appeared on Medscape.com.
Levonorgestrel IUDs Linked to Higher Skin Side Effects
TOPLINE:
, with some differences between the available levonorgestrel IUDs.
METHODOLOGY:
- Researchers reviewed the US Food and Drug Administration (FDA) Adverse Events Reporting System (FAERS) through December 2023 for adverse events associated with levonorgestrel IUDs where IUDs were the only suspected cause, focusing on acne, alopecia, and hirsutism.
- They included 139,348 reports for the levonorgestrel IUDs (Mirena, Liletta, Kyleena, Skyla) and 50,450 reports for the copper IUD (Paragard).
TAKEAWAY:
- Levonorgestrel IUD users showed higher odds of reporting acne (odds ratio [OR], 3.21), alopecia (OR, 5.96), and hirsutism (OR, 15.48; all P < .0001) than copper IUD users.
- The Kyleena 19.5 mg levonorgestrel IUD was associated with the highest odds of acne reports (OR, 3.42), followed by the Mirena 52 mg (OR, 3.40) and Skyla 13.5 mg (OR, 2.30) levonorgestrel IUDs (all P < .0001).
- The Mirena IUD was associated with the highest odds of alopecia and hirsutism reports (OR, 6.62 and 17.43, respectively), followed by the Kyleena (ORs, 2.90 and 8.17, respectively) and Skyla (ORs, 2.69 and 1.48, respectively) IUDs (all P < .0001).
- Reports of acne, alopecia, and hirsutism were not significantly different between the Liletta 52 mg levonorgestrel IUD and the copper IUD.
IN PRACTICE:
“Overall, we identified significant associations between levonorgestrel IUDs and androgenic cutaneous adverse events,” the authors wrote. “Counseling prior to initiation of levonorgestrel IUDs should include information on possible cutaneous AEs including acne, alopecia, and hirsutism to guide contraceptive shared decision making,” they added.
SOURCE:
The study was led by Lydia Cassard, Cleveland Clinic Lerner College of Medicine, Cleveland, Ohio, and was published online November 3 in Journal of the American Academy of Dermatology.
LIMITATIONS:
FAERS database reports could not be verified, and differences in FDA approval dates for IUDs could have influenced reporting rates. Moreover, a lack of data on prior medication use limits the ability to determine if these AEs are a result of changes in androgenic or antiandrogenic medication use. Cutaneous adverse events associated with copper IUDs may have been underreported because of assumptions that a nonhormonal device would not cause these adverse events.
DISCLOSURES:
The authors did not report any funding source or conflict of interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, with some differences between the available levonorgestrel IUDs.
METHODOLOGY:
- Researchers reviewed the US Food and Drug Administration (FDA) Adverse Events Reporting System (FAERS) through December 2023 for adverse events associated with levonorgestrel IUDs where IUDs were the only suspected cause, focusing on acne, alopecia, and hirsutism.
- They included 139,348 reports for the levonorgestrel IUDs (Mirena, Liletta, Kyleena, Skyla) and 50,450 reports for the copper IUD (Paragard).
TAKEAWAY:
- Levonorgestrel IUD users showed higher odds of reporting acne (odds ratio [OR], 3.21), alopecia (OR, 5.96), and hirsutism (OR, 15.48; all P < .0001) than copper IUD users.
- The Kyleena 19.5 mg levonorgestrel IUD was associated with the highest odds of acne reports (OR, 3.42), followed by the Mirena 52 mg (OR, 3.40) and Skyla 13.5 mg (OR, 2.30) levonorgestrel IUDs (all P < .0001).
- The Mirena IUD was associated with the highest odds of alopecia and hirsutism reports (OR, 6.62 and 17.43, respectively), followed by the Kyleena (ORs, 2.90 and 8.17, respectively) and Skyla (ORs, 2.69 and 1.48, respectively) IUDs (all P < .0001).
- Reports of acne, alopecia, and hirsutism were not significantly different between the Liletta 52 mg levonorgestrel IUD and the copper IUD.
IN PRACTICE:
“Overall, we identified significant associations between levonorgestrel IUDs and androgenic cutaneous adverse events,” the authors wrote. “Counseling prior to initiation of levonorgestrel IUDs should include information on possible cutaneous AEs including acne, alopecia, and hirsutism to guide contraceptive shared decision making,” they added.
SOURCE:
The study was led by Lydia Cassard, Cleveland Clinic Lerner College of Medicine, Cleveland, Ohio, and was published online November 3 in Journal of the American Academy of Dermatology.
LIMITATIONS:
FAERS database reports could not be verified, and differences in FDA approval dates for IUDs could have influenced reporting rates. Moreover, a lack of data on prior medication use limits the ability to determine if these AEs are a result of changes in androgenic or antiandrogenic medication use. Cutaneous adverse events associated with copper IUDs may have been underreported because of assumptions that a nonhormonal device would not cause these adverse events.
DISCLOSURES:
The authors did not report any funding source or conflict of interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, with some differences between the available levonorgestrel IUDs.
METHODOLOGY:
- Researchers reviewed the US Food and Drug Administration (FDA) Adverse Events Reporting System (FAERS) through December 2023 for adverse events associated with levonorgestrel IUDs where IUDs were the only suspected cause, focusing on acne, alopecia, and hirsutism.
- They included 139,348 reports for the levonorgestrel IUDs (Mirena, Liletta, Kyleena, Skyla) and 50,450 reports for the copper IUD (Paragard).
TAKEAWAY:
- Levonorgestrel IUD users showed higher odds of reporting acne (odds ratio [OR], 3.21), alopecia (OR, 5.96), and hirsutism (OR, 15.48; all P < .0001) than copper IUD users.
- The Kyleena 19.5 mg levonorgestrel IUD was associated with the highest odds of acne reports (OR, 3.42), followed by the Mirena 52 mg (OR, 3.40) and Skyla 13.5 mg (OR, 2.30) levonorgestrel IUDs (all P < .0001).
- The Mirena IUD was associated with the highest odds of alopecia and hirsutism reports (OR, 6.62 and 17.43, respectively), followed by the Kyleena (ORs, 2.90 and 8.17, respectively) and Skyla (ORs, 2.69 and 1.48, respectively) IUDs (all P < .0001).
- Reports of acne, alopecia, and hirsutism were not significantly different between the Liletta 52 mg levonorgestrel IUD and the copper IUD.
IN PRACTICE:
“Overall, we identified significant associations between levonorgestrel IUDs and androgenic cutaneous adverse events,” the authors wrote. “Counseling prior to initiation of levonorgestrel IUDs should include information on possible cutaneous AEs including acne, alopecia, and hirsutism to guide contraceptive shared decision making,” they added.
SOURCE:
The study was led by Lydia Cassard, Cleveland Clinic Lerner College of Medicine, Cleveland, Ohio, and was published online November 3 in Journal of the American Academy of Dermatology.
LIMITATIONS:
FAERS database reports could not be verified, and differences in FDA approval dates for IUDs could have influenced reporting rates. Moreover, a lack of data on prior medication use limits the ability to determine if these AEs are a result of changes in androgenic or antiandrogenic medication use. Cutaneous adverse events associated with copper IUDs may have been underreported because of assumptions that a nonhormonal device would not cause these adverse events.
DISCLOSURES:
The authors did not report any funding source or conflict of interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
FDA Approves Bimekizumab For Treating Hidradenitis Suppurativa
.
Approval was based on results from two phase 3 studies, BE HEARD I and BE HEARD II, which found that bimekizumab improved the signs and symptoms of disease compared with placebo at week 16 and were sustained to week 48, according to a press release from UCB, the drug’s manufacturer. In both trials, a higher proportion of patients treated with bimekizumab achieved Hidradenitis Suppurativa Clinical Response (HiSCR) scores of 50 and 75 compared with those who received placebo.
The company noted that bimekizumab (Bimzelx) is the first and only approved medicine designed to selectively inhibit IL-17F in addition to IL-17A. According to the prescribing information, the recommended dosing for patients with HS is 320 mg administered by subcutaneous injection at week 0, 2, 4, 6, 8, 10, 12, 14, and 16, then every 4 weeks thereafter.
“The approval of bimekizumab for moderate-to-severe HS is tremendous news for people living with HS” and the clinicians who care for them, Jennifer L. Hsiao, MD, director of the HS clinic at the University of Southern California, Los Angeles, told this news organization.
“It is exciting that we already have two-year trial data for bimekizumab in HS and can see that bimekizumab raises the bar in terms of depth and durability of response that we can expect to see in our patients,” she added. “Given the limited treatment options for HS at this time, the addition of bimekizumab to our treatment armamentarium is a huge step forward for the HS community.”
This development marks the fifth approved indication for bimekizumab since it was first approved in October 2023 for the treatment of moderate to severe plaque psoriasis, followed by approvals for active psoriatic arthritis, nonradiographic axial spondyloarthritis, and active ankylosing spondylitis in September 2024.
According to the prescribing information, certain adverse reactions have been observed with bimekizumab, including suicidal ideation and behavior, infections, liver biochemical abnormalities, and inflammatory bowel disease. A pregnancy exposure registry has been established that monitors pregnancy outcomes in women exposed to bimekizumab. For information, clinicians or patients can contact the Organization of Teratology Information Specialists (OTIS) Autoimmune Diseases Study at 1-877-311- 8972 or visit MotherToBaby Pregnancy Studies.
Hsiao disclosed that she is a member of the board of directors for the HS Foundation and has served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, Sanofi, and UCB; a speaker for AbbVie, Galderma, Novartis, Sanofi Regeneron, and UCB; and an investigator for Amgen, Boehringer Ingelheim, and Incyte.
A version of this article first appeared on Medscape.com.
.
Approval was based on results from two phase 3 studies, BE HEARD I and BE HEARD II, which found that bimekizumab improved the signs and symptoms of disease compared with placebo at week 16 and were sustained to week 48, according to a press release from UCB, the drug’s manufacturer. In both trials, a higher proportion of patients treated with bimekizumab achieved Hidradenitis Suppurativa Clinical Response (HiSCR) scores of 50 and 75 compared with those who received placebo.
The company noted that bimekizumab (Bimzelx) is the first and only approved medicine designed to selectively inhibit IL-17F in addition to IL-17A. According to the prescribing information, the recommended dosing for patients with HS is 320 mg administered by subcutaneous injection at week 0, 2, 4, 6, 8, 10, 12, 14, and 16, then every 4 weeks thereafter.
“The approval of bimekizumab for moderate-to-severe HS is tremendous news for people living with HS” and the clinicians who care for them, Jennifer L. Hsiao, MD, director of the HS clinic at the University of Southern California, Los Angeles, told this news organization.
“It is exciting that we already have two-year trial data for bimekizumab in HS and can see that bimekizumab raises the bar in terms of depth and durability of response that we can expect to see in our patients,” she added. “Given the limited treatment options for HS at this time, the addition of bimekizumab to our treatment armamentarium is a huge step forward for the HS community.”
This development marks the fifth approved indication for bimekizumab since it was first approved in October 2023 for the treatment of moderate to severe plaque psoriasis, followed by approvals for active psoriatic arthritis, nonradiographic axial spondyloarthritis, and active ankylosing spondylitis in September 2024.
According to the prescribing information, certain adverse reactions have been observed with bimekizumab, including suicidal ideation and behavior, infections, liver biochemical abnormalities, and inflammatory bowel disease. A pregnancy exposure registry has been established that monitors pregnancy outcomes in women exposed to bimekizumab. For information, clinicians or patients can contact the Organization of Teratology Information Specialists (OTIS) Autoimmune Diseases Study at 1-877-311- 8972 or visit MotherToBaby Pregnancy Studies.
Hsiao disclosed that she is a member of the board of directors for the HS Foundation and has served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, Sanofi, and UCB; a speaker for AbbVie, Galderma, Novartis, Sanofi Regeneron, and UCB; and an investigator for Amgen, Boehringer Ingelheim, and Incyte.
A version of this article first appeared on Medscape.com.
.
Approval was based on results from two phase 3 studies, BE HEARD I and BE HEARD II, which found that bimekizumab improved the signs and symptoms of disease compared with placebo at week 16 and were sustained to week 48, according to a press release from UCB, the drug’s manufacturer. In both trials, a higher proportion of patients treated with bimekizumab achieved Hidradenitis Suppurativa Clinical Response (HiSCR) scores of 50 and 75 compared with those who received placebo.
The company noted that bimekizumab (Bimzelx) is the first and only approved medicine designed to selectively inhibit IL-17F in addition to IL-17A. According to the prescribing information, the recommended dosing for patients with HS is 320 mg administered by subcutaneous injection at week 0, 2, 4, 6, 8, 10, 12, 14, and 16, then every 4 weeks thereafter.
“The approval of bimekizumab for moderate-to-severe HS is tremendous news for people living with HS” and the clinicians who care for them, Jennifer L. Hsiao, MD, director of the HS clinic at the University of Southern California, Los Angeles, told this news organization.
“It is exciting that we already have two-year trial data for bimekizumab in HS and can see that bimekizumab raises the bar in terms of depth and durability of response that we can expect to see in our patients,” she added. “Given the limited treatment options for HS at this time, the addition of bimekizumab to our treatment armamentarium is a huge step forward for the HS community.”
This development marks the fifth approved indication for bimekizumab since it was first approved in October 2023 for the treatment of moderate to severe plaque psoriasis, followed by approvals for active psoriatic arthritis, nonradiographic axial spondyloarthritis, and active ankylosing spondylitis in September 2024.
According to the prescribing information, certain adverse reactions have been observed with bimekizumab, including suicidal ideation and behavior, infections, liver biochemical abnormalities, and inflammatory bowel disease. A pregnancy exposure registry has been established that monitors pregnancy outcomes in women exposed to bimekizumab. For information, clinicians or patients can contact the Organization of Teratology Information Specialists (OTIS) Autoimmune Diseases Study at 1-877-311- 8972 or visit MotherToBaby Pregnancy Studies.
Hsiao disclosed that she is a member of the board of directors for the HS Foundation and has served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, Sanofi, and UCB; a speaker for AbbVie, Galderma, Novartis, Sanofi Regeneron, and UCB; and an investigator for Amgen, Boehringer Ingelheim, and Incyte.
A version of this article first appeared on Medscape.com.
Cancer Mortality Not Higher for Patients With Autoimmune Disease on Checkpoint Inhibitors
WASHINGTON — Immune checkpoint inhibitor (ICI) therapy does not increase mortality in people with preexisting autoimmune diseases, new research has found.
Results from a large database analysis of patients with and without autoimmune diseases suggest it is safe to treat them with ICI if they develop a cancer for which it is indicated, Greg Challener, MD, a postdoctoral fellow at the Rheumatology and Allergy Clinical Epidemiology Research Center, Massachusetts General Hospital, Boston, said at the American College of Rheumatology 2024 Annual Meeting.
“One message is that, when rheumatologists are asked by oncologists about patients with rheumatoid arthritis or vasculitis or other autoimmune diseases and whether it’s safe to treat them with immune checkpoint inhibitors, this result provides some evidence that it probably is safe…. Checkpoint inhibitors are really incredible drugs, and they’ve improved mortality for a lot of cancers, particularly melanoma, and so I think there should be a pretty high threshold for us to say a patient shouldn’t receive them because of an autoimmune condition,” he told this news organization.
Another implication, Challener said, is that people with autoimmune diseases shouldn’t routinely be excluded from clinical trials of ICIs. Currently they are excluded because of concerns about exacerbation of underlying autoimmunity, possible interference between the ICI and the immunosuppressive drugs used to treat the autoimmune condition, and a theoretical risk for serious adverse events.
“Clinical trials are continuing to exclude these patients, and they paint with a very broad brush anyone with underlying autoimmunity ... I’m hoping that that changes. I don’t think there’s a great evidence base to support that practice, and it’s unfortunate that patients with underlying autoimmune diseases are excluded from important studies,” Challener said.
Asked to comment, session moderator Matlock Jeffries, MD, director of the Arthritis Research Unit at the Oklahoma Medical Research Foundation, Oklahoma City, told this news organization that he agrees the data are generally reassuring. “If one of our patients gets cancer and their oncologist wants to use a checkpoint inhibitor, we’d obviously still monitor them for complications, but we wouldn’t automatically assume the combination of a checkpoint inhibitor and autoimmune disease would increase their mortality.”
No Difference in Mortality for Those With and Without Autoimmune Disease
Challener and colleagues used administrative health data from the TriNetX Diamond network of 92 US healthcare sites with 212 million patients. All patients included in the study were receiving anti-programmed death protein 1/programmed death ligand 1 to treat malignancies involving the skin, lung/bronchus, digestive organs, or urinary tract. The study population also had at least one rheumatologic, gastrointestinal, neurologic, dermatologic, or endocrine autoimmune disease.
Propensity score matching between those with and without autoimmune disease was performed for about 100 covariates. Prior to the matching, the autoimmune disease group had significantly higher rates of cardiovascular and other comorbidities. The matching yielded 23,714 individuals with autoimmune disease and the same number without who had similar demographics and comorbidity rates, as well as malignancy type, alcohol/tobacco use, and medication use.
At a median follow-up of 250 days, the risk for mortality prior to propensity matching was 40.0% in the autoimmune disease group and 38.1% for those without, a significant difference with hazard ratio 1.07 (95% CI, 1.05-1.10). But after the matching, the difference was no longer significant: 39.8% vs 40.2%, respectively (0.97, 0.94-1.00).
The Kaplan-Meier curves for survival probability for those with or without autoimmune disease were nearly superimposed, showing no difference up to 1600 days. An analysis of just the patients with rheumatic diseases yielded similar results, Challener said.
Some Caveats About the Data
Jeffries, who is also an associate professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, and the Oklahoma VA, said he would like to see additional data on outcomes, both for the autoimmune conditions and the cancers. Challener said there are plans to look at other hard endpoints such as myocardial infarction and end-stage renal disease, but that the database is limited.
Both Challener and Jeffries also cautioned that the reassurance may not apply to patients with active disease.
“One thing this research doesn’t address is whether active autoimmune disease might have a different outcome compared to more kind of quiet disease…. If you have a patient who has extremely active rheumatoid arthritis or extremely active giant cell arthritis, for instance, I think that could be more challenging. I would be frightened to put a patient with really active GCA on pembrolizumab or say that it’s safe without their disease being controlled. But for someone who has well-controlled disease or minimally active disease, this is very reassuring,” Challener told this news organization.
“I think this may also be important in that it’s a good argument to tell the drug companies to include autoimmune patients in these trials so we can get better data,” Jeffries said.
Challener and Jeffries had no relevant disclosures.
A version of this article appeared on Medscape.com.
WASHINGTON — Immune checkpoint inhibitor (ICI) therapy does not increase mortality in people with preexisting autoimmune diseases, new research has found.
Results from a large database analysis of patients with and without autoimmune diseases suggest it is safe to treat them with ICI if they develop a cancer for which it is indicated, Greg Challener, MD, a postdoctoral fellow at the Rheumatology and Allergy Clinical Epidemiology Research Center, Massachusetts General Hospital, Boston, said at the American College of Rheumatology 2024 Annual Meeting.
“One message is that, when rheumatologists are asked by oncologists about patients with rheumatoid arthritis or vasculitis or other autoimmune diseases and whether it’s safe to treat them with immune checkpoint inhibitors, this result provides some evidence that it probably is safe…. Checkpoint inhibitors are really incredible drugs, and they’ve improved mortality for a lot of cancers, particularly melanoma, and so I think there should be a pretty high threshold for us to say a patient shouldn’t receive them because of an autoimmune condition,” he told this news organization.
Another implication, Challener said, is that people with autoimmune diseases shouldn’t routinely be excluded from clinical trials of ICIs. Currently they are excluded because of concerns about exacerbation of underlying autoimmunity, possible interference between the ICI and the immunosuppressive drugs used to treat the autoimmune condition, and a theoretical risk for serious adverse events.
“Clinical trials are continuing to exclude these patients, and they paint with a very broad brush anyone with underlying autoimmunity ... I’m hoping that that changes. I don’t think there’s a great evidence base to support that practice, and it’s unfortunate that patients with underlying autoimmune diseases are excluded from important studies,” Challener said.
Asked to comment, session moderator Matlock Jeffries, MD, director of the Arthritis Research Unit at the Oklahoma Medical Research Foundation, Oklahoma City, told this news organization that he agrees the data are generally reassuring. “If one of our patients gets cancer and their oncologist wants to use a checkpoint inhibitor, we’d obviously still monitor them for complications, but we wouldn’t automatically assume the combination of a checkpoint inhibitor and autoimmune disease would increase their mortality.”
No Difference in Mortality for Those With and Without Autoimmune Disease
Challener and colleagues used administrative health data from the TriNetX Diamond network of 92 US healthcare sites with 212 million patients. All patients included in the study were receiving anti-programmed death protein 1/programmed death ligand 1 to treat malignancies involving the skin, lung/bronchus, digestive organs, or urinary tract. The study population also had at least one rheumatologic, gastrointestinal, neurologic, dermatologic, or endocrine autoimmune disease.
Propensity score matching between those with and without autoimmune disease was performed for about 100 covariates. Prior to the matching, the autoimmune disease group had significantly higher rates of cardiovascular and other comorbidities. The matching yielded 23,714 individuals with autoimmune disease and the same number without who had similar demographics and comorbidity rates, as well as malignancy type, alcohol/tobacco use, and medication use.
At a median follow-up of 250 days, the risk for mortality prior to propensity matching was 40.0% in the autoimmune disease group and 38.1% for those without, a significant difference with hazard ratio 1.07 (95% CI, 1.05-1.10). But after the matching, the difference was no longer significant: 39.8% vs 40.2%, respectively (0.97, 0.94-1.00).
The Kaplan-Meier curves for survival probability for those with or without autoimmune disease were nearly superimposed, showing no difference up to 1600 days. An analysis of just the patients with rheumatic diseases yielded similar results, Challener said.
Some Caveats About the Data
Jeffries, who is also an associate professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, and the Oklahoma VA, said he would like to see additional data on outcomes, both for the autoimmune conditions and the cancers. Challener said there are plans to look at other hard endpoints such as myocardial infarction and end-stage renal disease, but that the database is limited.
Both Challener and Jeffries also cautioned that the reassurance may not apply to patients with active disease.
“One thing this research doesn’t address is whether active autoimmune disease might have a different outcome compared to more kind of quiet disease…. If you have a patient who has extremely active rheumatoid arthritis or extremely active giant cell arthritis, for instance, I think that could be more challenging. I would be frightened to put a patient with really active GCA on pembrolizumab or say that it’s safe without their disease being controlled. But for someone who has well-controlled disease or minimally active disease, this is very reassuring,” Challener told this news organization.
“I think this may also be important in that it’s a good argument to tell the drug companies to include autoimmune patients in these trials so we can get better data,” Jeffries said.
Challener and Jeffries had no relevant disclosures.
A version of this article appeared on Medscape.com.
WASHINGTON — Immune checkpoint inhibitor (ICI) therapy does not increase mortality in people with preexisting autoimmune diseases, new research has found.
Results from a large database analysis of patients with and without autoimmune diseases suggest it is safe to treat them with ICI if they develop a cancer for which it is indicated, Greg Challener, MD, a postdoctoral fellow at the Rheumatology and Allergy Clinical Epidemiology Research Center, Massachusetts General Hospital, Boston, said at the American College of Rheumatology 2024 Annual Meeting.
“One message is that, when rheumatologists are asked by oncologists about patients with rheumatoid arthritis or vasculitis or other autoimmune diseases and whether it’s safe to treat them with immune checkpoint inhibitors, this result provides some evidence that it probably is safe…. Checkpoint inhibitors are really incredible drugs, and they’ve improved mortality for a lot of cancers, particularly melanoma, and so I think there should be a pretty high threshold for us to say a patient shouldn’t receive them because of an autoimmune condition,” he told this news organization.
Another implication, Challener said, is that people with autoimmune diseases shouldn’t routinely be excluded from clinical trials of ICIs. Currently they are excluded because of concerns about exacerbation of underlying autoimmunity, possible interference between the ICI and the immunosuppressive drugs used to treat the autoimmune condition, and a theoretical risk for serious adverse events.
“Clinical trials are continuing to exclude these patients, and they paint with a very broad brush anyone with underlying autoimmunity ... I’m hoping that that changes. I don’t think there’s a great evidence base to support that practice, and it’s unfortunate that patients with underlying autoimmune diseases are excluded from important studies,” Challener said.
Asked to comment, session moderator Matlock Jeffries, MD, director of the Arthritis Research Unit at the Oklahoma Medical Research Foundation, Oklahoma City, told this news organization that he agrees the data are generally reassuring. “If one of our patients gets cancer and their oncologist wants to use a checkpoint inhibitor, we’d obviously still monitor them for complications, but we wouldn’t automatically assume the combination of a checkpoint inhibitor and autoimmune disease would increase their mortality.”
No Difference in Mortality for Those With and Without Autoimmune Disease
Challener and colleagues used administrative health data from the TriNetX Diamond network of 92 US healthcare sites with 212 million patients. All patients included in the study were receiving anti-programmed death protein 1/programmed death ligand 1 to treat malignancies involving the skin, lung/bronchus, digestive organs, or urinary tract. The study population also had at least one rheumatologic, gastrointestinal, neurologic, dermatologic, or endocrine autoimmune disease.
Propensity score matching between those with and without autoimmune disease was performed for about 100 covariates. Prior to the matching, the autoimmune disease group had significantly higher rates of cardiovascular and other comorbidities. The matching yielded 23,714 individuals with autoimmune disease and the same number without who had similar demographics and comorbidity rates, as well as malignancy type, alcohol/tobacco use, and medication use.
At a median follow-up of 250 days, the risk for mortality prior to propensity matching was 40.0% in the autoimmune disease group and 38.1% for those without, a significant difference with hazard ratio 1.07 (95% CI, 1.05-1.10). But after the matching, the difference was no longer significant: 39.8% vs 40.2%, respectively (0.97, 0.94-1.00).
The Kaplan-Meier curves for survival probability for those with or without autoimmune disease were nearly superimposed, showing no difference up to 1600 days. An analysis of just the patients with rheumatic diseases yielded similar results, Challener said.
Some Caveats About the Data
Jeffries, who is also an associate professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, and the Oklahoma VA, said he would like to see additional data on outcomes, both for the autoimmune conditions and the cancers. Challener said there are plans to look at other hard endpoints such as myocardial infarction and end-stage renal disease, but that the database is limited.
Both Challener and Jeffries also cautioned that the reassurance may not apply to patients with active disease.
“One thing this research doesn’t address is whether active autoimmune disease might have a different outcome compared to more kind of quiet disease…. If you have a patient who has extremely active rheumatoid arthritis or extremely active giant cell arthritis, for instance, I think that could be more challenging. I would be frightened to put a patient with really active GCA on pembrolizumab or say that it’s safe without their disease being controlled. But for someone who has well-controlled disease or minimally active disease, this is very reassuring,” Challener told this news organization.
“I think this may also be important in that it’s a good argument to tell the drug companies to include autoimmune patients in these trials so we can get better data,” Jeffries said.
Challener and Jeffries had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM ACR 2024
Case Series Highlight Necrotic Wounds Associated with Xylazine-Tainted Fentanyl
TOPLINE:
including 9% that involved exposed deep structures such as bone or tendon.
METHODOLOGY:
- The alpha-2 agonist xylazine, a veterinary sedative, is increasingly detected in fentanyl used illicitly in the United States and may be causing necrotizing wounds in drug users.
- To characterize specific clinical features of xylazine-associated wounds, researchers conducted a case series at three academic medical hospitals in Philadelphia from April 2022 to February 2023.
- They included 29 patients with confirmed xylazine exposure and a chief complaint that was wound-related, seen as inpatients or in the emergency department.
TAKEAWAY:
- The 29 patients (mean age, 39.4 years; 52% men) had a total of 59 wounds, 90% were located on the arms and legs, and 69% were on the posterior upper or anterior lower extremities. Five wounds (9%) involved exposed deep structures such as the bone or tendon.
- Of the 57 wounds with available photographs, 60% had wound beds with predominantly devitalized tissue (eschar or slough), 11% were blisters, 9% had granulation tissue, and 21% had mixed tissue or other types of wound beds. Devitalized tissue was more commonly observed in medium or large wounds (odds ratio [OR], 5.2; P = .02) than in small wounds.
- As reported by patients, 48% were acute wounds, 20% were subacute, and 29% were chronic (present for 3 months or longer). Subacute and chronic wounds were often medium or large compared with acute wounds (OR, 48.5; P < .001) and contained devitalized tissue (OR, 9.5; P < .001).
- Of the 39 wounds with patient-reported etiology, 34 (87%) occurred at drug injection sites.
IN PRACTICE:
To the best of their knowledge, this is “the largest study of wounds among patients with confirmed exposure to xylazine and the first to systematically describe wound characteristics,” the authors wrote. The results, they concluded, “may help identify xylazine exposure and can guide research on the etiology and management of these wounds.”
SOURCE:
This study was conducted by Lydia Lutz, MD, Johns Hopkins University School of Medicine, Baltimore, Maryland, and coinvestigators and was published online in JAMA Dermatology.
LIMITATIONS:
This single-city, retrospective study limited generalizability, and the selection of the largest wounds may bias results. Additionally, chronicity data relied on patient recall, potentially introducing recall bias.
DISCLOSURES:
Two authors received support from the National Institute on Drug Abuse for the study. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
including 9% that involved exposed deep structures such as bone or tendon.
METHODOLOGY:
- The alpha-2 agonist xylazine, a veterinary sedative, is increasingly detected in fentanyl used illicitly in the United States and may be causing necrotizing wounds in drug users.
- To characterize specific clinical features of xylazine-associated wounds, researchers conducted a case series at three academic medical hospitals in Philadelphia from April 2022 to February 2023.
- They included 29 patients with confirmed xylazine exposure and a chief complaint that was wound-related, seen as inpatients or in the emergency department.
TAKEAWAY:
- The 29 patients (mean age, 39.4 years; 52% men) had a total of 59 wounds, 90% were located on the arms and legs, and 69% were on the posterior upper or anterior lower extremities. Five wounds (9%) involved exposed deep structures such as the bone or tendon.
- Of the 57 wounds with available photographs, 60% had wound beds with predominantly devitalized tissue (eschar or slough), 11% were blisters, 9% had granulation tissue, and 21% had mixed tissue or other types of wound beds. Devitalized tissue was more commonly observed in medium or large wounds (odds ratio [OR], 5.2; P = .02) than in small wounds.
- As reported by patients, 48% were acute wounds, 20% were subacute, and 29% were chronic (present for 3 months or longer). Subacute and chronic wounds were often medium or large compared with acute wounds (OR, 48.5; P < .001) and contained devitalized tissue (OR, 9.5; P < .001).
- Of the 39 wounds with patient-reported etiology, 34 (87%) occurred at drug injection sites.
IN PRACTICE:
To the best of their knowledge, this is “the largest study of wounds among patients with confirmed exposure to xylazine and the first to systematically describe wound characteristics,” the authors wrote. The results, they concluded, “may help identify xylazine exposure and can guide research on the etiology and management of these wounds.”
SOURCE:
This study was conducted by Lydia Lutz, MD, Johns Hopkins University School of Medicine, Baltimore, Maryland, and coinvestigators and was published online in JAMA Dermatology.
LIMITATIONS:
This single-city, retrospective study limited generalizability, and the selection of the largest wounds may bias results. Additionally, chronicity data relied on patient recall, potentially introducing recall bias.
DISCLOSURES:
Two authors received support from the National Institute on Drug Abuse for the study. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
including 9% that involved exposed deep structures such as bone or tendon.
METHODOLOGY:
- The alpha-2 agonist xylazine, a veterinary sedative, is increasingly detected in fentanyl used illicitly in the United States and may be causing necrotizing wounds in drug users.
- To characterize specific clinical features of xylazine-associated wounds, researchers conducted a case series at three academic medical hospitals in Philadelphia from April 2022 to February 2023.
- They included 29 patients with confirmed xylazine exposure and a chief complaint that was wound-related, seen as inpatients or in the emergency department.
TAKEAWAY:
- The 29 patients (mean age, 39.4 years; 52% men) had a total of 59 wounds, 90% were located on the arms and legs, and 69% were on the posterior upper or anterior lower extremities. Five wounds (9%) involved exposed deep structures such as the bone or tendon.
- Of the 57 wounds with available photographs, 60% had wound beds with predominantly devitalized tissue (eschar or slough), 11% were blisters, 9% had granulation tissue, and 21% had mixed tissue or other types of wound beds. Devitalized tissue was more commonly observed in medium or large wounds (odds ratio [OR], 5.2; P = .02) than in small wounds.
- As reported by patients, 48% were acute wounds, 20% were subacute, and 29% were chronic (present for 3 months or longer). Subacute and chronic wounds were often medium or large compared with acute wounds (OR, 48.5; P < .001) and contained devitalized tissue (OR, 9.5; P < .001).
- Of the 39 wounds with patient-reported etiology, 34 (87%) occurred at drug injection sites.
IN PRACTICE:
To the best of their knowledge, this is “the largest study of wounds among patients with confirmed exposure to xylazine and the first to systematically describe wound characteristics,” the authors wrote. The results, they concluded, “may help identify xylazine exposure and can guide research on the etiology and management of these wounds.”
SOURCE:
This study was conducted by Lydia Lutz, MD, Johns Hopkins University School of Medicine, Baltimore, Maryland, and coinvestigators and was published online in JAMA Dermatology.
LIMITATIONS:
This single-city, retrospective study limited generalizability, and the selection of the largest wounds may bias results. Additionally, chronicity data relied on patient recall, potentially introducing recall bias.
DISCLOSURES:
Two authors received support from the National Institute on Drug Abuse for the study. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
A Portrait of the Patient
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
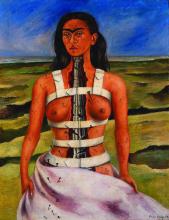
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
Post COVID-19, Long-term Risk for Autoimmune, Autoinflammatory Skin Disorders Increased, Study Finds
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Dupilumab Beneficial When Antihistamines Fall Short for Chronic Spontaneous Urticaria
based on data from 151 individuals.
“Approximately 50% of patients with chronic spontaneous urticaria do not respond to antihistamines,” said Thomas B. Casale, MD, professor of internal medicine at the University of South Florida, Tampa, in an interview. Omalizumab, the only biologic approved for this condition, is not effective in all patients, and additional treatment options are needed, added Casale, the lead author who presented the new data, at the American College of Allergy, Asthma & Immunology (ACAAI) 2024 Annual Scientific Meeting.
Dupilumab (Dupixent), a fully human monoclonal antibody that targets the interleukin (IL)–4 and IL-13 pathways, is currently approved in the United States for the treatment of several allergy and dermatology indications, including atopic dermatitis, severe asthma exacerbations, chronic rhinosinusitis with nasal polyps, and prurigo nodularis.
In the study, known as LIBERTY-CSU CUPID Study C, researchers randomized 74 patients with CSU aged 6 years or older to add-on dupilumab subcutaneously every 2 weeks and 77 to placebo. (Patients were omalizumab-naive and had symptomatic CSU, despite treatment with up to four times the approved dose of standard-of-care H1-antihistamines.) Dupilumab doses were 300 mg for adults and adolescents weighing ≥ 60 kg or 200 mg for adolescents weighing < 60 kg and children weighing ≥ 30 kg.
The primary outcomes were Itch Severity Score over 7 days (ISS7; range, 0-21) and Urticaria Activity Score over 7 days (UAS7; range, 0-42).
Over the 24-week study period, patients in the dupilumab group showed significantly greater change from baseline than those in the placebo group on both measures, with least squares mean changes of 8.6 vs 6.1 for ISS7 and 15.9 vs 11.2 for UAS7 (P = .02 for both).
In addition, at 24 weeks, significantly more patients in the dupilumab group than in the placebo group achieved well-controlled disease based on a UAS of 6 or lower (41% vs 23%; P = .005). Significantly more dupilumab-treated patients also achieved a complete response (defined as a UAS of 0), compared with placebo-treated patients (30% vs 18%; P = .02).
Overall rates of treatment-emergent adverse events were 53% for both groups, and safety data were mainly consistent with dupilumab’s known safety profile, the researchers wrote.
The findings were not surprising, as a previous related study, LIBERTY-CSU CUPID Study A, showed that dupilumab was effective for CSU, Casale told this news organization. “This replicate study confirms the previous study and provides evidence for regulatory approval.”
If approved by the Food and Drug Administration (FDA), “dupilumab will provide another therapeutic option for patients with chronic urticaria unresponsive to antihistamines,” Casale commented.
No new safety signals occurred, and the ability to self-administer the medication at home provides an advantage for patients, he added. As for additional research, “analysis of patient characteristics and potential biomarkers that would predict responsiveness is needed.”
More Research Needed to Fine-Tune Management
An unmet need persists for patients with CSU whose disease is not adequately controlled by higher-dose H1-antihistamines, Robert G. Micheletti, MD, associate professor of dermatology and medicine at the University of Pennsylvania, Philadelphia, said in an interview. “It is important not only to identify effective add-on therapies for these patients but also to generate data to support insurance coverage and drug access,” said Micheletti, who was not involved in the study.
Also referring to the similar findings reported in the LIBERTY-CSU CUPID Study A, Micheletti said, “as in the earlier study, the results demonstrate significantly reduced itch and urticaria in treated patients compared to placebo.”
“While many providers currently prescribe dupilumab off-label for refractory CSU, FDA approval would improve access to the drug for patients who need it and provide an alternative for patients who may not be good candidates for omalizumab,” he added. However, more research is needed to define optimal management of patients with CSU with inadequate response to omalizumab.
“The LIBERTY-CSU CUPID Study B showed a small improvement in itch severity and urticaria activity among such patients receiving dupilumab,” he noted. “Future work should aim to identify biomarkers and other features predictive of response to various therapies.”
Study B involved patients with CSU who were uncontrolled on standard-of-care antihistamines and refractory or intolerant to omalizumab, according to Regeneron.
On November 15, after the ACAAI meeting had ended, the company announced that the FDA had accepted the resubmission of an application for approval of dupilumab for the treatment of CSU in adults and pediatric patients aged 12 years or older not adequately controlled with H1-antihistamines.
The study was supported and sponsored by Sanofi and Regeneron Pharmaceuticals. Casale disclosed serving as a consultant for ALK, ARS Pharma, AstraZeneca, Bryn Pharma, Celgene, Eli Lilly, Genentech, GSK, Jasper, Novartis, Regeneron, and Sanofi and as a speaker for Genentech and Regeneron. Micheletti had no relevant financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
based on data from 151 individuals.
“Approximately 50% of patients with chronic spontaneous urticaria do not respond to antihistamines,” said Thomas B. Casale, MD, professor of internal medicine at the University of South Florida, Tampa, in an interview. Omalizumab, the only biologic approved for this condition, is not effective in all patients, and additional treatment options are needed, added Casale, the lead author who presented the new data, at the American College of Allergy, Asthma & Immunology (ACAAI) 2024 Annual Scientific Meeting.
Dupilumab (Dupixent), a fully human monoclonal antibody that targets the interleukin (IL)–4 and IL-13 pathways, is currently approved in the United States for the treatment of several allergy and dermatology indications, including atopic dermatitis, severe asthma exacerbations, chronic rhinosinusitis with nasal polyps, and prurigo nodularis.
In the study, known as LIBERTY-CSU CUPID Study C, researchers randomized 74 patients with CSU aged 6 years or older to add-on dupilumab subcutaneously every 2 weeks and 77 to placebo. (Patients were omalizumab-naive and had symptomatic CSU, despite treatment with up to four times the approved dose of standard-of-care H1-antihistamines.) Dupilumab doses were 300 mg for adults and adolescents weighing ≥ 60 kg or 200 mg for adolescents weighing < 60 kg and children weighing ≥ 30 kg.
The primary outcomes were Itch Severity Score over 7 days (ISS7; range, 0-21) and Urticaria Activity Score over 7 days (UAS7; range, 0-42).
Over the 24-week study period, patients in the dupilumab group showed significantly greater change from baseline than those in the placebo group on both measures, with least squares mean changes of 8.6 vs 6.1 for ISS7 and 15.9 vs 11.2 for UAS7 (P = .02 for both).
In addition, at 24 weeks, significantly more patients in the dupilumab group than in the placebo group achieved well-controlled disease based on a UAS of 6 or lower (41% vs 23%; P = .005). Significantly more dupilumab-treated patients also achieved a complete response (defined as a UAS of 0), compared with placebo-treated patients (30% vs 18%; P = .02).
Overall rates of treatment-emergent adverse events were 53% for both groups, and safety data were mainly consistent with dupilumab’s known safety profile, the researchers wrote.
The findings were not surprising, as a previous related study, LIBERTY-CSU CUPID Study A, showed that dupilumab was effective for CSU, Casale told this news organization. “This replicate study confirms the previous study and provides evidence for regulatory approval.”
If approved by the Food and Drug Administration (FDA), “dupilumab will provide another therapeutic option for patients with chronic urticaria unresponsive to antihistamines,” Casale commented.
No new safety signals occurred, and the ability to self-administer the medication at home provides an advantage for patients, he added. As for additional research, “analysis of patient characteristics and potential biomarkers that would predict responsiveness is needed.”
More Research Needed to Fine-Tune Management
An unmet need persists for patients with CSU whose disease is not adequately controlled by higher-dose H1-antihistamines, Robert G. Micheletti, MD, associate professor of dermatology and medicine at the University of Pennsylvania, Philadelphia, said in an interview. “It is important not only to identify effective add-on therapies for these patients but also to generate data to support insurance coverage and drug access,” said Micheletti, who was not involved in the study.
Also referring to the similar findings reported in the LIBERTY-CSU CUPID Study A, Micheletti said, “as in the earlier study, the results demonstrate significantly reduced itch and urticaria in treated patients compared to placebo.”
“While many providers currently prescribe dupilumab off-label for refractory CSU, FDA approval would improve access to the drug for patients who need it and provide an alternative for patients who may not be good candidates for omalizumab,” he added. However, more research is needed to define optimal management of patients with CSU with inadequate response to omalizumab.
“The LIBERTY-CSU CUPID Study B showed a small improvement in itch severity and urticaria activity among such patients receiving dupilumab,” he noted. “Future work should aim to identify biomarkers and other features predictive of response to various therapies.”
Study B involved patients with CSU who were uncontrolled on standard-of-care antihistamines and refractory or intolerant to omalizumab, according to Regeneron.
On November 15, after the ACAAI meeting had ended, the company announced that the FDA had accepted the resubmission of an application for approval of dupilumab for the treatment of CSU in adults and pediatric patients aged 12 years or older not adequately controlled with H1-antihistamines.
The study was supported and sponsored by Sanofi and Regeneron Pharmaceuticals. Casale disclosed serving as a consultant for ALK, ARS Pharma, AstraZeneca, Bryn Pharma, Celgene, Eli Lilly, Genentech, GSK, Jasper, Novartis, Regeneron, and Sanofi and as a speaker for Genentech and Regeneron. Micheletti had no relevant financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
based on data from 151 individuals.
“Approximately 50% of patients with chronic spontaneous urticaria do not respond to antihistamines,” said Thomas B. Casale, MD, professor of internal medicine at the University of South Florida, Tampa, in an interview. Omalizumab, the only biologic approved for this condition, is not effective in all patients, and additional treatment options are needed, added Casale, the lead author who presented the new data, at the American College of Allergy, Asthma & Immunology (ACAAI) 2024 Annual Scientific Meeting.
Dupilumab (Dupixent), a fully human monoclonal antibody that targets the interleukin (IL)–4 and IL-13 pathways, is currently approved in the United States for the treatment of several allergy and dermatology indications, including atopic dermatitis, severe asthma exacerbations, chronic rhinosinusitis with nasal polyps, and prurigo nodularis.
In the study, known as LIBERTY-CSU CUPID Study C, researchers randomized 74 patients with CSU aged 6 years or older to add-on dupilumab subcutaneously every 2 weeks and 77 to placebo. (Patients were omalizumab-naive and had symptomatic CSU, despite treatment with up to four times the approved dose of standard-of-care H1-antihistamines.) Dupilumab doses were 300 mg for adults and adolescents weighing ≥ 60 kg or 200 mg for adolescents weighing < 60 kg and children weighing ≥ 30 kg.
The primary outcomes were Itch Severity Score over 7 days (ISS7; range, 0-21) and Urticaria Activity Score over 7 days (UAS7; range, 0-42).
Over the 24-week study period, patients in the dupilumab group showed significantly greater change from baseline than those in the placebo group on both measures, with least squares mean changes of 8.6 vs 6.1 for ISS7 and 15.9 vs 11.2 for UAS7 (P = .02 for both).
In addition, at 24 weeks, significantly more patients in the dupilumab group than in the placebo group achieved well-controlled disease based on a UAS of 6 or lower (41% vs 23%; P = .005). Significantly more dupilumab-treated patients also achieved a complete response (defined as a UAS of 0), compared with placebo-treated patients (30% vs 18%; P = .02).
Overall rates of treatment-emergent adverse events were 53% for both groups, and safety data were mainly consistent with dupilumab’s known safety profile, the researchers wrote.
The findings were not surprising, as a previous related study, LIBERTY-CSU CUPID Study A, showed that dupilumab was effective for CSU, Casale told this news organization. “This replicate study confirms the previous study and provides evidence for regulatory approval.”
If approved by the Food and Drug Administration (FDA), “dupilumab will provide another therapeutic option for patients with chronic urticaria unresponsive to antihistamines,” Casale commented.
No new safety signals occurred, and the ability to self-administer the medication at home provides an advantage for patients, he added. As for additional research, “analysis of patient characteristics and potential biomarkers that would predict responsiveness is needed.”
More Research Needed to Fine-Tune Management
An unmet need persists for patients with CSU whose disease is not adequately controlled by higher-dose H1-antihistamines, Robert G. Micheletti, MD, associate professor of dermatology and medicine at the University of Pennsylvania, Philadelphia, said in an interview. “It is important not only to identify effective add-on therapies for these patients but also to generate data to support insurance coverage and drug access,” said Micheletti, who was not involved in the study.
Also referring to the similar findings reported in the LIBERTY-CSU CUPID Study A, Micheletti said, “as in the earlier study, the results demonstrate significantly reduced itch and urticaria in treated patients compared to placebo.”
“While many providers currently prescribe dupilumab off-label for refractory CSU, FDA approval would improve access to the drug for patients who need it and provide an alternative for patients who may not be good candidates for omalizumab,” he added. However, more research is needed to define optimal management of patients with CSU with inadequate response to omalizumab.
“The LIBERTY-CSU CUPID Study B showed a small improvement in itch severity and urticaria activity among such patients receiving dupilumab,” he noted. “Future work should aim to identify biomarkers and other features predictive of response to various therapies.”
Study B involved patients with CSU who were uncontrolled on standard-of-care antihistamines and refractory or intolerant to omalizumab, according to Regeneron.
On November 15, after the ACAAI meeting had ended, the company announced that the FDA had accepted the resubmission of an application for approval of dupilumab for the treatment of CSU in adults and pediatric patients aged 12 years or older not adequately controlled with H1-antihistamines.
The study was supported and sponsored by Sanofi and Regeneron Pharmaceuticals. Casale disclosed serving as a consultant for ALK, ARS Pharma, AstraZeneca, Bryn Pharma, Celgene, Eli Lilly, Genentech, GSK, Jasper, Novartis, Regeneron, and Sanofi and as a speaker for Genentech and Regeneron. Micheletti had no relevant financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
FROM ACAAI 2024