User login
News and Views that Matter to Physicians
Infection, readmission linked after open lower-extremity procedures
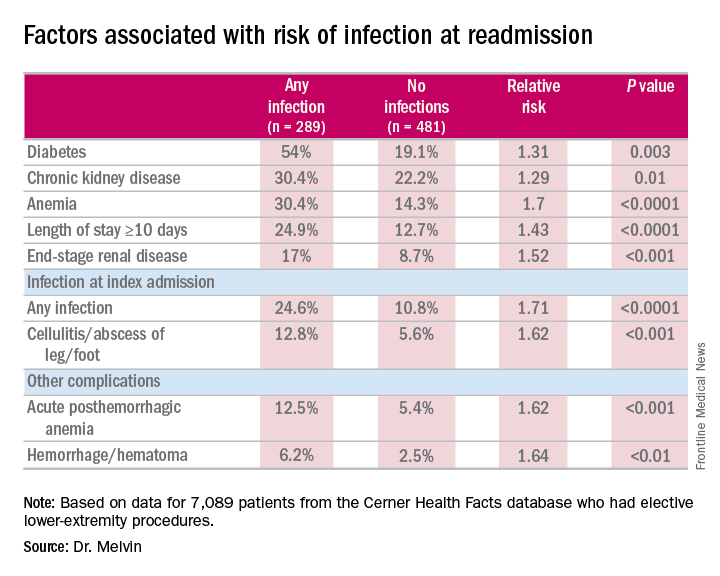
COLUMBUS, OHIO – Infections account for more than one-third of readmissions after endovascular lower-extremity procedures, but an analysis of these procedures over a 6-year period has identified a handful of factors, including an extended hospital stay, that may help vascular surgeons identify patients at greatest risk and reduce infection-related readmissions.
“Of a little over 7,000 patients that we evaluated with peripheral artery disease who underwent an elective lower-extremity procedure, we found an overall readmission rate of 10.9%; about 9.5% for those who underwent an open procedure and just over 12% for those who underwent an endovascular procedure,” Joseph C. Melvin, MD, of the University of Missouri Hospitals & Clinics in Columbia said at the annual meeting of the Midwestern Vascular Surgery Society.
While the readmission rate for open operations was lower, the infection rate at readmission was higher for open procedures: 45.5% (157 of 345 readmissions) vs. 31.1% (132 of 425 readmissions), Dr. Melvin said.
“The risk factors for diagnosis of infection at readmission we found to be significant were anemia, chronic kidney disease, and end-stage renal disease, any infection at the time of the index admission, specifically cellulitis or abscess of the lower extremity given the patient’s peripheral artery disease status, diabetes, and then complications including posthemorrhagic anemia,” Dr. Melvin said. Laboratory testing values at the time of index admissions confirmed the risk factors.
The investigators also used multivariable logistic regression models in the analysis and found that factors most predictive of an infection-related readmission were length of stay, having the procedure at a teaching facility, anemia, and infection at the index admission, Dr. Melvin said.
The surgical site was the most common source of the infection, and Staphylococcus “not surprisingly” accounted for 25% of pathogens, Dr. Melvin said. “But what we did find to be interesting was that just over 40% of patients were found to have a gram-negative bacteria isolated, which would come into play with our decision with regards to antibiotic treatment,” he said.
The data suggest that further evaluation of ways to decrease postoperative infections and use of broad-spectrum antibiotics during readmissions may improve outcomes after open lower-extremity procedures, Dr. Melvin said.
Dr. Melvin had no financial relationships to disclose.
COLUMBUS, OHIO – Infections account for more than one-third of readmissions after endovascular lower-extremity procedures, but an analysis of these procedures over a 6-year period has identified a handful of factors, including an extended hospital stay, that may help vascular surgeons identify patients at greatest risk and reduce infection-related readmissions.
“Of a little over 7,000 patients that we evaluated with peripheral artery disease who underwent an elective lower-extremity procedure, we found an overall readmission rate of 10.9%; about 9.5% for those who underwent an open procedure and just over 12% for those who underwent an endovascular procedure,” Joseph C. Melvin, MD, of the University of Missouri Hospitals & Clinics in Columbia said at the annual meeting of the Midwestern Vascular Surgery Society.
While the readmission rate for open operations was lower, the infection rate at readmission was higher for open procedures: 45.5% (157 of 345 readmissions) vs. 31.1% (132 of 425 readmissions), Dr. Melvin said.
“The risk factors for diagnosis of infection at readmission we found to be significant were anemia, chronic kidney disease, and end-stage renal disease, any infection at the time of the index admission, specifically cellulitis or abscess of the lower extremity given the patient’s peripheral artery disease status, diabetes, and then complications including posthemorrhagic anemia,” Dr. Melvin said. Laboratory testing values at the time of index admissions confirmed the risk factors.
The investigators also used multivariable logistic regression models in the analysis and found that factors most predictive of an infection-related readmission were length of stay, having the procedure at a teaching facility, anemia, and infection at the index admission, Dr. Melvin said.
The surgical site was the most common source of the infection, and Staphylococcus “not surprisingly” accounted for 25% of pathogens, Dr. Melvin said. “But what we did find to be interesting was that just over 40% of patients were found to have a gram-negative bacteria isolated, which would come into play with our decision with regards to antibiotic treatment,” he said.
The data suggest that further evaluation of ways to decrease postoperative infections and use of broad-spectrum antibiotics during readmissions may improve outcomes after open lower-extremity procedures, Dr. Melvin said.
Dr. Melvin had no financial relationships to disclose.
COLUMBUS, OHIO – Infections account for more than one-third of readmissions after endovascular lower-extremity procedures, but an analysis of these procedures over a 6-year period has identified a handful of factors, including an extended hospital stay, that may help vascular surgeons identify patients at greatest risk and reduce infection-related readmissions.
“Of a little over 7,000 patients that we evaluated with peripheral artery disease who underwent an elective lower-extremity procedure, we found an overall readmission rate of 10.9%; about 9.5% for those who underwent an open procedure and just over 12% for those who underwent an endovascular procedure,” Joseph C. Melvin, MD, of the University of Missouri Hospitals & Clinics in Columbia said at the annual meeting of the Midwestern Vascular Surgery Society.
While the readmission rate for open operations was lower, the infection rate at readmission was higher for open procedures: 45.5% (157 of 345 readmissions) vs. 31.1% (132 of 425 readmissions), Dr. Melvin said.
“The risk factors for diagnosis of infection at readmission we found to be significant were anemia, chronic kidney disease, and end-stage renal disease, any infection at the time of the index admission, specifically cellulitis or abscess of the lower extremity given the patient’s peripheral artery disease status, diabetes, and then complications including posthemorrhagic anemia,” Dr. Melvin said. Laboratory testing values at the time of index admissions confirmed the risk factors.
The investigators also used multivariable logistic regression models in the analysis and found that factors most predictive of an infection-related readmission were length of stay, having the procedure at a teaching facility, anemia, and infection at the index admission, Dr. Melvin said.
The surgical site was the most common source of the infection, and Staphylococcus “not surprisingly” accounted for 25% of pathogens, Dr. Melvin said. “But what we did find to be interesting was that just over 40% of patients were found to have a gram-negative bacteria isolated, which would come into play with our decision with regards to antibiotic treatment,” he said.
The data suggest that further evaluation of ways to decrease postoperative infections and use of broad-spectrum antibiotics during readmissions may improve outcomes after open lower-extremity procedures, Dr. Melvin said.
Dr. Melvin had no financial relationships to disclose.
AT MIDWESTERN VASCULAR 2016
Key clinical point: Extended hospital stay and other factors can help identify patients at greatest risk for readmission due to infection.
Major finding: More than one-third of readmissions from lower-extremity procedures are the result of infections.
Data source: 7,089 elective lower extremity procedures selected from the Cerner Health Facts database.
Disclosures: Dr. Melvin reported having no financial disclosures.
Meaningful use: CMS extends 90-day reporting period to 2016, 2017
Physicians who already participate in the EHR incentive program for meaningful use will have to demonstrate they are meaningful users for only 90 days in 2016 and 2017.
The Centers for Medicare & Medicaid Services finalized the 90-day reporting period in its annual update to the hospital outpatient prospective payment system, scheduled for publication in the Federal Register on Nov. 14.
The CMS was preparing to require a full year of reporting in 2017 to be eligible for bonuses under the EHR Incentive Program; but instead extended the 90-day reporting requirement to address concerns about technical functionalities and to help ease the transition to the Merit-based Incentive Payment System (MIPS) created by the 2015 MACRA law, according to an agency fact sheet.
The Outpatient Prospective Payment System (OPPS) final rule also eliminated clinical decision support and computerized order entry objectives and measures for eligible hospitals and critical access hospitals.
Instead of requiring that eligible professionals and hospitals new to the EHR Incentive Program in 2017 to meet Stage 3 requirements, the CMS has provided modified Stage 2 requirements.
Physicians who are new to the EHR Incentive Program in 2017 but are transitioning their practice to MIPS next year can apply for a significant hardship exemption to avoid any penalties to their 2018 Medicare payments.
Physicians who already participate in the EHR incentive program for meaningful use will have to demonstrate they are meaningful users for only 90 days in 2016 and 2017.
The Centers for Medicare & Medicaid Services finalized the 90-day reporting period in its annual update to the hospital outpatient prospective payment system, scheduled for publication in the Federal Register on Nov. 14.
The CMS was preparing to require a full year of reporting in 2017 to be eligible for bonuses under the EHR Incentive Program; but instead extended the 90-day reporting requirement to address concerns about technical functionalities and to help ease the transition to the Merit-based Incentive Payment System (MIPS) created by the 2015 MACRA law, according to an agency fact sheet.
The Outpatient Prospective Payment System (OPPS) final rule also eliminated clinical decision support and computerized order entry objectives and measures for eligible hospitals and critical access hospitals.
Instead of requiring that eligible professionals and hospitals new to the EHR Incentive Program in 2017 to meet Stage 3 requirements, the CMS has provided modified Stage 2 requirements.
Physicians who are new to the EHR Incentive Program in 2017 but are transitioning their practice to MIPS next year can apply for a significant hardship exemption to avoid any penalties to their 2018 Medicare payments.
Physicians who already participate in the EHR incentive program for meaningful use will have to demonstrate they are meaningful users for only 90 days in 2016 and 2017.
The Centers for Medicare & Medicaid Services finalized the 90-day reporting period in its annual update to the hospital outpatient prospective payment system, scheduled for publication in the Federal Register on Nov. 14.
The CMS was preparing to require a full year of reporting in 2017 to be eligible for bonuses under the EHR Incentive Program; but instead extended the 90-day reporting requirement to address concerns about technical functionalities and to help ease the transition to the Merit-based Incentive Payment System (MIPS) created by the 2015 MACRA law, according to an agency fact sheet.
The Outpatient Prospective Payment System (OPPS) final rule also eliminated clinical decision support and computerized order entry objectives and measures for eligible hospitals and critical access hospitals.
Instead of requiring that eligible professionals and hospitals new to the EHR Incentive Program in 2017 to meet Stage 3 requirements, the CMS has provided modified Stage 2 requirements.
Physicians who are new to the EHR Incentive Program in 2017 but are transitioning their practice to MIPS next year can apply for a significant hardship exemption to avoid any penalties to their 2018 Medicare payments.
How to reduce early readmissions after bariatric surgery
NEW ORLEANS – A couple of home nursing visits early after bariatric surgery halved emergency department visits and hospital readmissions within the first 30 days in a case-control study, Linden A. Karas, MD, reported at Obesity Week 2016.
“Home nursing visits during the month following surgery, between doctor’s office visits, are a simple and inexpensive intervention that drastically decreases hospital revisits,” she declared at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
These early revisits to the hospital following bariatric surgery are not only common, they carry a substantial cost. An ED visit for hydration runs about $3,000 and a 2-day inpatient admission about $18,000. In contrast, the price tag for two home nursing visits in this study was $300, noted Dr. Karas, a surgeon at Mercy Catholic Medical Center in Philadelphia.
The triad of dehydration, nausea, and vomiting in addition to abdominal pain account for up to 40% of early readmissions following bariatric surgery. Because most hospital revisits for these reasons entail very little intervention other than IV fluids, Dr. Karas and her coinvestigators decided to investigate whether preemptive structured home visits by nurses prepared to administer IV fluids on the spot would cut down on hospital revisits. They found that indeed this strategy was successful.
Mercy Catholic Medical Center serves a largely low-income Medicare/Medicaid population. Part of the local culture is for many patients to obtain their primary care in the ED, so bariatric surgery patients are generally not reluctant to show up there if they don’t feel well in the first few weeks post surgery. That’s why in the year prior to the study the 30-day readmission rate was 23.6%, she explained.
The study included 193 consecutive prospectively followed adult participants in the home nursing program who underwent Roux-en-Y gastric bypass, laparoscopic adjustable banding, or revision surgery in 2014 and a control group of 267 matched bariatric surgery patients who underwent the same procedures in 2013, before introduction of the home nursing visits.
The first home visit occurred roughly 3 days after hospital discharge. The second one bridged the period between the first scheduled postoperative office visit at 2 weeks and the next office visit at 4 weeks. At discharge, patients were given a checklist concerning the signs and symptoms of dehydration, dietary recommendations, and lifestyle choices. Patients were encouraged to use the checklist to self-evaluate for dehydration and hand it over to the visiting nurses. The same checklist was provided to the home nurses. If the nurses found that patients met three or more criteria on the dehydration checklist, which included dry mucus membranes, heart rate greater than 90 beats/minute, headache, going more than 8 hours without urination, weakness, abdominal pain, and roughly a dozen other well-known criteria, they were instructed to initiate home hydration therapy with a banana bag and 2 L of normal saline.
If 1-2 days of home hydration failed to resolve the symptoms, the home care nurse was supposed to refer the patient to the ED. If the patient improved in response to home hydration therapy, the home nurse informed the surgeon’s office, which then set up a follow-up office visit to take place within the next 24 hours. Also, if the patient’s responses on the nutrition and behavioral health questionnaire raised any red flags regarding inadequate food and fluid intake, nonadherence to the recommended daily minimum of 30 minutes of physical activity, or depressive symptoms, the nurse was supposed to notify the surgeon to schedule a behavioral or nutrition appointment at the patient’s next scheduled visit.
The 30-day rate of all-cause hospital revisits in the home nursing care group was 11.9%, compared with 23.6% in controls. The rate of hospital revisits specifically for dehydration was 6.2% in the home visit group vs. 8.6% in controls, a 28% relative risk reduction in the home treatment group, which didn’t achieve statistical significance. However, in hindsight, it was evident that some of the visiting nurses didn’t fully understand the treatment protocol; they sent patients straight to the ED without first providing home hydration therapy. The visiting nurses were subcontracted out and weren’t part of the hospital’s bariatric surgery program.
Among those patients who did receive the therapy, however, it prevented readmission in 77% of cases. The 23% of patients who didn’t improve were referred to the hospital for further workup and treatment.
Patients with early hospital readmission had an average of 4.38 comorbid conditions, significantly more than the average 3.46 comorbidities in patients who weren’t readmitted. Several specific comorbid conditions were independently associated with significantly increased risk of hospital readmission: asthma, chronic obstructive pulmonary disease, anxiety, heart failure, and gastroesophageal reflux disease.
“Patients with those comorbidities are the ones to watch aggressively in the postop period,” according to Dr. Karas.
Insurers have paid for the home nursing visits without hesitation.
Her presentation met with an enthusiastic audience reception.
“I think it’s important that you’ve shown a return on investment for this initiative,” one surgeon commented.
Session cochair John J. Kelly, MD, chief of general and minimally invasive surgery at the University of Massachusetts in Worcester, declared, “I think this is a very-important paper. We’re obviously all faced with this dilemma in terms of readmission rates. If you can prevent them, it’s to be commended.”
Dr. Karas reported having no financial conflicts of interest regarding her study.
NEW ORLEANS – A couple of home nursing visits early after bariatric surgery halved emergency department visits and hospital readmissions within the first 30 days in a case-control study, Linden A. Karas, MD, reported at Obesity Week 2016.
“Home nursing visits during the month following surgery, between doctor’s office visits, are a simple and inexpensive intervention that drastically decreases hospital revisits,” she declared at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
These early revisits to the hospital following bariatric surgery are not only common, they carry a substantial cost. An ED visit for hydration runs about $3,000 and a 2-day inpatient admission about $18,000. In contrast, the price tag for two home nursing visits in this study was $300, noted Dr. Karas, a surgeon at Mercy Catholic Medical Center in Philadelphia.
The triad of dehydration, nausea, and vomiting in addition to abdominal pain account for up to 40% of early readmissions following bariatric surgery. Because most hospital revisits for these reasons entail very little intervention other than IV fluids, Dr. Karas and her coinvestigators decided to investigate whether preemptive structured home visits by nurses prepared to administer IV fluids on the spot would cut down on hospital revisits. They found that indeed this strategy was successful.
Mercy Catholic Medical Center serves a largely low-income Medicare/Medicaid population. Part of the local culture is for many patients to obtain their primary care in the ED, so bariatric surgery patients are generally not reluctant to show up there if they don’t feel well in the first few weeks post surgery. That’s why in the year prior to the study the 30-day readmission rate was 23.6%, she explained.
The study included 193 consecutive prospectively followed adult participants in the home nursing program who underwent Roux-en-Y gastric bypass, laparoscopic adjustable banding, or revision surgery in 2014 and a control group of 267 matched bariatric surgery patients who underwent the same procedures in 2013, before introduction of the home nursing visits.
The first home visit occurred roughly 3 days after hospital discharge. The second one bridged the period between the first scheduled postoperative office visit at 2 weeks and the next office visit at 4 weeks. At discharge, patients were given a checklist concerning the signs and symptoms of dehydration, dietary recommendations, and lifestyle choices. Patients were encouraged to use the checklist to self-evaluate for dehydration and hand it over to the visiting nurses. The same checklist was provided to the home nurses. If the nurses found that patients met three or more criteria on the dehydration checklist, which included dry mucus membranes, heart rate greater than 90 beats/minute, headache, going more than 8 hours without urination, weakness, abdominal pain, and roughly a dozen other well-known criteria, they were instructed to initiate home hydration therapy with a banana bag and 2 L of normal saline.
If 1-2 days of home hydration failed to resolve the symptoms, the home care nurse was supposed to refer the patient to the ED. If the patient improved in response to home hydration therapy, the home nurse informed the surgeon’s office, which then set up a follow-up office visit to take place within the next 24 hours. Also, if the patient’s responses on the nutrition and behavioral health questionnaire raised any red flags regarding inadequate food and fluid intake, nonadherence to the recommended daily minimum of 30 minutes of physical activity, or depressive symptoms, the nurse was supposed to notify the surgeon to schedule a behavioral or nutrition appointment at the patient’s next scheduled visit.
The 30-day rate of all-cause hospital revisits in the home nursing care group was 11.9%, compared with 23.6% in controls. The rate of hospital revisits specifically for dehydration was 6.2% in the home visit group vs. 8.6% in controls, a 28% relative risk reduction in the home treatment group, which didn’t achieve statistical significance. However, in hindsight, it was evident that some of the visiting nurses didn’t fully understand the treatment protocol; they sent patients straight to the ED without first providing home hydration therapy. The visiting nurses were subcontracted out and weren’t part of the hospital’s bariatric surgery program.
Among those patients who did receive the therapy, however, it prevented readmission in 77% of cases. The 23% of patients who didn’t improve were referred to the hospital for further workup and treatment.
Patients with early hospital readmission had an average of 4.38 comorbid conditions, significantly more than the average 3.46 comorbidities in patients who weren’t readmitted. Several specific comorbid conditions were independently associated with significantly increased risk of hospital readmission: asthma, chronic obstructive pulmonary disease, anxiety, heart failure, and gastroesophageal reflux disease.
“Patients with those comorbidities are the ones to watch aggressively in the postop period,” according to Dr. Karas.
Insurers have paid for the home nursing visits without hesitation.
Her presentation met with an enthusiastic audience reception.
“I think it’s important that you’ve shown a return on investment for this initiative,” one surgeon commented.
Session cochair John J. Kelly, MD, chief of general and minimally invasive surgery at the University of Massachusetts in Worcester, declared, “I think this is a very-important paper. We’re obviously all faced with this dilemma in terms of readmission rates. If you can prevent them, it’s to be commended.”
Dr. Karas reported having no financial conflicts of interest regarding her study.
NEW ORLEANS – A couple of home nursing visits early after bariatric surgery halved emergency department visits and hospital readmissions within the first 30 days in a case-control study, Linden A. Karas, MD, reported at Obesity Week 2016.
“Home nursing visits during the month following surgery, between doctor’s office visits, are a simple and inexpensive intervention that drastically decreases hospital revisits,” she declared at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
These early revisits to the hospital following bariatric surgery are not only common, they carry a substantial cost. An ED visit for hydration runs about $3,000 and a 2-day inpatient admission about $18,000. In contrast, the price tag for two home nursing visits in this study was $300, noted Dr. Karas, a surgeon at Mercy Catholic Medical Center in Philadelphia.
The triad of dehydration, nausea, and vomiting in addition to abdominal pain account for up to 40% of early readmissions following bariatric surgery. Because most hospital revisits for these reasons entail very little intervention other than IV fluids, Dr. Karas and her coinvestigators decided to investigate whether preemptive structured home visits by nurses prepared to administer IV fluids on the spot would cut down on hospital revisits. They found that indeed this strategy was successful.
Mercy Catholic Medical Center serves a largely low-income Medicare/Medicaid population. Part of the local culture is for many patients to obtain their primary care in the ED, so bariatric surgery patients are generally not reluctant to show up there if they don’t feel well in the first few weeks post surgery. That’s why in the year prior to the study the 30-day readmission rate was 23.6%, she explained.
The study included 193 consecutive prospectively followed adult participants in the home nursing program who underwent Roux-en-Y gastric bypass, laparoscopic adjustable banding, or revision surgery in 2014 and a control group of 267 matched bariatric surgery patients who underwent the same procedures in 2013, before introduction of the home nursing visits.
The first home visit occurred roughly 3 days after hospital discharge. The second one bridged the period between the first scheduled postoperative office visit at 2 weeks and the next office visit at 4 weeks. At discharge, patients were given a checklist concerning the signs and symptoms of dehydration, dietary recommendations, and lifestyle choices. Patients were encouraged to use the checklist to self-evaluate for dehydration and hand it over to the visiting nurses. The same checklist was provided to the home nurses. If the nurses found that patients met three or more criteria on the dehydration checklist, which included dry mucus membranes, heart rate greater than 90 beats/minute, headache, going more than 8 hours without urination, weakness, abdominal pain, and roughly a dozen other well-known criteria, they were instructed to initiate home hydration therapy with a banana bag and 2 L of normal saline.
If 1-2 days of home hydration failed to resolve the symptoms, the home care nurse was supposed to refer the patient to the ED. If the patient improved in response to home hydration therapy, the home nurse informed the surgeon’s office, which then set up a follow-up office visit to take place within the next 24 hours. Also, if the patient’s responses on the nutrition and behavioral health questionnaire raised any red flags regarding inadequate food and fluid intake, nonadherence to the recommended daily minimum of 30 minutes of physical activity, or depressive symptoms, the nurse was supposed to notify the surgeon to schedule a behavioral or nutrition appointment at the patient’s next scheduled visit.
The 30-day rate of all-cause hospital revisits in the home nursing care group was 11.9%, compared with 23.6% in controls. The rate of hospital revisits specifically for dehydration was 6.2% in the home visit group vs. 8.6% in controls, a 28% relative risk reduction in the home treatment group, which didn’t achieve statistical significance. However, in hindsight, it was evident that some of the visiting nurses didn’t fully understand the treatment protocol; they sent patients straight to the ED without first providing home hydration therapy. The visiting nurses were subcontracted out and weren’t part of the hospital’s bariatric surgery program.
Among those patients who did receive the therapy, however, it prevented readmission in 77% of cases. The 23% of patients who didn’t improve were referred to the hospital for further workup and treatment.
Patients with early hospital readmission had an average of 4.38 comorbid conditions, significantly more than the average 3.46 comorbidities in patients who weren’t readmitted. Several specific comorbid conditions were independently associated with significantly increased risk of hospital readmission: asthma, chronic obstructive pulmonary disease, anxiety, heart failure, and gastroesophageal reflux disease.
“Patients with those comorbidities are the ones to watch aggressively in the postop period,” according to Dr. Karas.
Insurers have paid for the home nursing visits without hesitation.
Her presentation met with an enthusiastic audience reception.
“I think it’s important that you’ve shown a return on investment for this initiative,” one surgeon commented.
Session cochair John J. Kelly, MD, chief of general and minimally invasive surgery at the University of Massachusetts in Worcester, declared, “I think this is a very-important paper. We’re obviously all faced with this dilemma in terms of readmission rates. If you can prevent them, it’s to be commended.”
Dr. Karas reported having no financial conflicts of interest regarding her study.
AT OBESITY WEEK 2016
Key clinical point:
Major finding: The combined rate of ED visits and hospital readmissions within 30 days post–bariatric surgery was 11.9% in a group of patients who received two home nursing visits that included home hydration therapy as indicated, compared with 23.6% in bariatric surgery patients who weren’t involved in the home visit program.
Data source: This study compared 30-day hospital readmission rates in 193 consecutive prospectively followed bariatric surgery patients who received two structured home nursing visits in the first 4 postoperative weeks to readmissions in 267 matched controls whose surgery occurred prior to implementation of the home nursing program.
Disclosures: The presenter reported having no financial conflicts of interest regarding the study.
Optimal MPE management requires early pulmonology referral
LOS ANGELES – About half of patients with symptomatic malignant pleural effusions at McGill University Health Centre in Montreal had unnecessary procedures and hospital admissions before definitive treatment with chemical pleurodesis or indwelling pleural catheters, according to researchers.
Instead of chest taps to relieve symptoms followed by referrals for definitive treatment, some patients got chest tubes – without pleurodesis – after presenting to the emergency department and being referred to radiology; they were then admitted to the hospital for a few days while the tubes were in place. In short, cancer patients were wasting what time they had left on medical care they didn’t need, and incurring unnecessary costs, said lead investigator Benjamin Shieh, MD, formerly at McGill but now an interventional pulmonology fellow at the University of Calgary.
McGill is a tertiary care center able to perform both definitive procedures, so “we should be a center of excellence. I imagine there are similar situations” at other hospitals, especially those without the resources of McGill, Dr. Shieh said at the annual meeting of the American College of Chest Physicians.
McGill has taken several steps to address the problem, including early ED referral to the pulmonology service and discouraging radiology from placing chest tubes for malignant pleural effusions (MPE). “I think we can avoid a big proportion of hospitalizations for MPE, and certainly a proportion of repeat [ED] visits,” said senior author Anne Gonzalez, MD, an attending pulmonologist at McGill.
The investigators looked into the issue after noting that a lot of their MPE cases had been hospitalized with chest tubes. They reviewed 72 symptomatic MPE cases in 69 patients treated in 2014 and 2015. Management was ideal in 36 cases (50%), meaning that, prior to definitive treatment, patients had no more than two pleural taps for symptom relief, no more than one ED visit, no chest tubes without pleurodesis, and no hospitalizations. “We thought this would be reasonable to try to achieve for MPE,” since there’s no definition of ideal management, Dr. Shieh said.
Nonideal patients had a mean of 2.5 pleural procedures – almost twice the number in the ideal group – before definitive palliation, with no respiratory consult beforehand. Chest tubes were placed in 27 cases (38%) for an average of 3.7 days; 28 cases (39%) were hospitalized. Nonideal patients were far more likely to present first to the ED, and ED presentations were more likely to get chest tubes and be admitted. All the cases were eventually treated definitively, 68 with indwelling pleural catheters and 4 by thoracoscopic talc insufflation. Time from initial presentation to definitive palliation was about 1 month in both groups. The investigators didn’t consider rate of effusion recurrence, which might help explain why the ideal group wasn’t treated sooner; they might not have needed it. The higher number of ED visits in the nonideal group suggests that they may have had quicker recurrences, and should have been treated sooner, Dr. Gonzalez said.
The patients were 70 years old, on average, and about 60% were women. Lung and breast were the most common cancers.
There was no industry funding for the work, and the investigators had no disclosures.
LOS ANGELES – About half of patients with symptomatic malignant pleural effusions at McGill University Health Centre in Montreal had unnecessary procedures and hospital admissions before definitive treatment with chemical pleurodesis or indwelling pleural catheters, according to researchers.
Instead of chest taps to relieve symptoms followed by referrals for definitive treatment, some patients got chest tubes – without pleurodesis – after presenting to the emergency department and being referred to radiology; they were then admitted to the hospital for a few days while the tubes were in place. In short, cancer patients were wasting what time they had left on medical care they didn’t need, and incurring unnecessary costs, said lead investigator Benjamin Shieh, MD, formerly at McGill but now an interventional pulmonology fellow at the University of Calgary.
McGill is a tertiary care center able to perform both definitive procedures, so “we should be a center of excellence. I imagine there are similar situations” at other hospitals, especially those without the resources of McGill, Dr. Shieh said at the annual meeting of the American College of Chest Physicians.
McGill has taken several steps to address the problem, including early ED referral to the pulmonology service and discouraging radiology from placing chest tubes for malignant pleural effusions (MPE). “I think we can avoid a big proportion of hospitalizations for MPE, and certainly a proportion of repeat [ED] visits,” said senior author Anne Gonzalez, MD, an attending pulmonologist at McGill.
The investigators looked into the issue after noting that a lot of their MPE cases had been hospitalized with chest tubes. They reviewed 72 symptomatic MPE cases in 69 patients treated in 2014 and 2015. Management was ideal in 36 cases (50%), meaning that, prior to definitive treatment, patients had no more than two pleural taps for symptom relief, no more than one ED visit, no chest tubes without pleurodesis, and no hospitalizations. “We thought this would be reasonable to try to achieve for MPE,” since there’s no definition of ideal management, Dr. Shieh said.
Nonideal patients had a mean of 2.5 pleural procedures – almost twice the number in the ideal group – before definitive palliation, with no respiratory consult beforehand. Chest tubes were placed in 27 cases (38%) for an average of 3.7 days; 28 cases (39%) were hospitalized. Nonideal patients were far more likely to present first to the ED, and ED presentations were more likely to get chest tubes and be admitted. All the cases were eventually treated definitively, 68 with indwelling pleural catheters and 4 by thoracoscopic talc insufflation. Time from initial presentation to definitive palliation was about 1 month in both groups. The investigators didn’t consider rate of effusion recurrence, which might help explain why the ideal group wasn’t treated sooner; they might not have needed it. The higher number of ED visits in the nonideal group suggests that they may have had quicker recurrences, and should have been treated sooner, Dr. Gonzalez said.
The patients were 70 years old, on average, and about 60% were women. Lung and breast were the most common cancers.
There was no industry funding for the work, and the investigators had no disclosures.
LOS ANGELES – About half of patients with symptomatic malignant pleural effusions at McGill University Health Centre in Montreal had unnecessary procedures and hospital admissions before definitive treatment with chemical pleurodesis or indwelling pleural catheters, according to researchers.
Instead of chest taps to relieve symptoms followed by referrals for definitive treatment, some patients got chest tubes – without pleurodesis – after presenting to the emergency department and being referred to radiology; they were then admitted to the hospital for a few days while the tubes were in place. In short, cancer patients were wasting what time they had left on medical care they didn’t need, and incurring unnecessary costs, said lead investigator Benjamin Shieh, MD, formerly at McGill but now an interventional pulmonology fellow at the University of Calgary.
McGill is a tertiary care center able to perform both definitive procedures, so “we should be a center of excellence. I imagine there are similar situations” at other hospitals, especially those without the resources of McGill, Dr. Shieh said at the annual meeting of the American College of Chest Physicians.
McGill has taken several steps to address the problem, including early ED referral to the pulmonology service and discouraging radiology from placing chest tubes for malignant pleural effusions (MPE). “I think we can avoid a big proportion of hospitalizations for MPE, and certainly a proportion of repeat [ED] visits,” said senior author Anne Gonzalez, MD, an attending pulmonologist at McGill.
The investigators looked into the issue after noting that a lot of their MPE cases had been hospitalized with chest tubes. They reviewed 72 symptomatic MPE cases in 69 patients treated in 2014 and 2015. Management was ideal in 36 cases (50%), meaning that, prior to definitive treatment, patients had no more than two pleural taps for symptom relief, no more than one ED visit, no chest tubes without pleurodesis, and no hospitalizations. “We thought this would be reasonable to try to achieve for MPE,” since there’s no definition of ideal management, Dr. Shieh said.
Nonideal patients had a mean of 2.5 pleural procedures – almost twice the number in the ideal group – before definitive palliation, with no respiratory consult beforehand. Chest tubes were placed in 27 cases (38%) for an average of 3.7 days; 28 cases (39%) were hospitalized. Nonideal patients were far more likely to present first to the ED, and ED presentations were more likely to get chest tubes and be admitted. All the cases were eventually treated definitively, 68 with indwelling pleural catheters and 4 by thoracoscopic talc insufflation. Time from initial presentation to definitive palliation was about 1 month in both groups. The investigators didn’t consider rate of effusion recurrence, which might help explain why the ideal group wasn’t treated sooner; they might not have needed it. The higher number of ED visits in the nonideal group suggests that they may have had quicker recurrences, and should have been treated sooner, Dr. Gonzalez said.
The patients were 70 years old, on average, and about 60% were women. Lung and breast were the most common cancers.
There was no industry funding for the work, and the investigators had no disclosures.
AT CHEST 2016
Key clinical point:
Major finding: Those patients had a mean of 2.5 pleural procedures before definitive palliation, with no respiratory consult beforehand. Chest tubes were placed for an average of 3.7 days.
Data source: Review of 72 MPE cases in 69 patients.
Disclosures: There was no industry funding for the work, and the investigators had no disclosures.
Mitral valve disease often missed in pulmonary hypertension
LOS ANGELES – Dyspnea in pulmonary hypertension is caused by mitral valve disease until proven otherwise, according to Paul Forfia, MD, director of pulmonary hypertension, right heart failure, and pulmonary thromboendarterectomy at Temple University, Philadelphia.
Although mitral valve disease is a well-recognized cause of pulmonary hypertension, its significance is often underestimated in practice.
“Whether the valve is regurgitant or stenotic makes absolutely no difference. When you delay” repair or replacement, “the patient keeps getting sicker,” he said. In time, “everyone is standing around wringing their hands going, ‘Oh my god, what are we going to do? Are you serious? Fix the valve.’ We see this type of patient a couple times a month,” Dr. Forfia said at the American College of Chest Physicians annual meeting.
“I have seen lifesaving mitral valve surgery put off for many years in patients with pulmonary hypertension, when all they needed was to have their valve fixed,” he said.
Whatever the case, pulmonologists who want the valve fixed often end up playing patient ping pong with cardiologists who want the hypertension controlled beforehand, but “if I treat the pulmonary circulation first, all I am going to do is unmask the left heart failure. There will be no functional improvement whatsoever,” Dr. Forfia said.
Surgery is the best solution as long as patients are well enough to recover. “With pulmonary hypertension in the setting of severe mitral valve regurgitation or stenosis, whether the pulmonary hypertension is related to passive left heart congestion or associated with pulmonary arteriopathy, the only sensible option is to correct the underlying valvular abnormality,” he said. The surgery should be done at an institution capable of managing postop pulmonary arteriopathy, if present.
The ping pong solution is to send patients to an expert pulmonology center; the mitral valve problem will be spotted right away.
“There is no pulmonary pressure cutoff that should prohibit surgery” in patients able to recover. “There is no such thing as a pulmonary artery pressure too high to be explained by mitral valve disease. The pulmonary pressure can be as high as it wants to be. You will get nowhere by thinking the pressure is too high to address the valve,” Dr. Forfia said.
Often “you hear, ‘I’m afraid the person is going to die on the table.’ I always say ‘if the patient is not going to die on the table, they are going to die in their living room of progressive heart failure because you [didn’t] fix their valve. I have never had a patient with pulmonary hypertension not separate from cardiopulmonary bypass. It’s a myth,” he said.
When there’s a “question if the dyspnea is coming from the mitral valve, we routinely use exercise right heart catheterization to probe the situation. We have a recumbent bike in the cath lab. You’ll often provoke significant left heart congestion with a low workload. It’s very revealing to the significance of mitral valve disease,” he said.
Aortic valve disease is also missed in pulmonary hypertension. “It’s not [a] similar” problem; “it’s the same” problem, Dr. Forfia said.
Dr. Forfia is a consultant for Bayer, Actelion, and United Therapeutics.
LOS ANGELES – Dyspnea in pulmonary hypertension is caused by mitral valve disease until proven otherwise, according to Paul Forfia, MD, director of pulmonary hypertension, right heart failure, and pulmonary thromboendarterectomy at Temple University, Philadelphia.
Although mitral valve disease is a well-recognized cause of pulmonary hypertension, its significance is often underestimated in practice.
“Whether the valve is regurgitant or stenotic makes absolutely no difference. When you delay” repair or replacement, “the patient keeps getting sicker,” he said. In time, “everyone is standing around wringing their hands going, ‘Oh my god, what are we going to do? Are you serious? Fix the valve.’ We see this type of patient a couple times a month,” Dr. Forfia said at the American College of Chest Physicians annual meeting.
“I have seen lifesaving mitral valve surgery put off for many years in patients with pulmonary hypertension, when all they needed was to have their valve fixed,” he said.
Whatever the case, pulmonologists who want the valve fixed often end up playing patient ping pong with cardiologists who want the hypertension controlled beforehand, but “if I treat the pulmonary circulation first, all I am going to do is unmask the left heart failure. There will be no functional improvement whatsoever,” Dr. Forfia said.
Surgery is the best solution as long as patients are well enough to recover. “With pulmonary hypertension in the setting of severe mitral valve regurgitation or stenosis, whether the pulmonary hypertension is related to passive left heart congestion or associated with pulmonary arteriopathy, the only sensible option is to correct the underlying valvular abnormality,” he said. The surgery should be done at an institution capable of managing postop pulmonary arteriopathy, if present.
The ping pong solution is to send patients to an expert pulmonology center; the mitral valve problem will be spotted right away.
“There is no pulmonary pressure cutoff that should prohibit surgery” in patients able to recover. “There is no such thing as a pulmonary artery pressure too high to be explained by mitral valve disease. The pulmonary pressure can be as high as it wants to be. You will get nowhere by thinking the pressure is too high to address the valve,” Dr. Forfia said.
Often “you hear, ‘I’m afraid the person is going to die on the table.’ I always say ‘if the patient is not going to die on the table, they are going to die in their living room of progressive heart failure because you [didn’t] fix their valve. I have never had a patient with pulmonary hypertension not separate from cardiopulmonary bypass. It’s a myth,” he said.
When there’s a “question if the dyspnea is coming from the mitral valve, we routinely use exercise right heart catheterization to probe the situation. We have a recumbent bike in the cath lab. You’ll often provoke significant left heart congestion with a low workload. It’s very revealing to the significance of mitral valve disease,” he said.
Aortic valve disease is also missed in pulmonary hypertension. “It’s not [a] similar” problem; “it’s the same” problem, Dr. Forfia said.
Dr. Forfia is a consultant for Bayer, Actelion, and United Therapeutics.
LOS ANGELES – Dyspnea in pulmonary hypertension is caused by mitral valve disease until proven otherwise, according to Paul Forfia, MD, director of pulmonary hypertension, right heart failure, and pulmonary thromboendarterectomy at Temple University, Philadelphia.
Although mitral valve disease is a well-recognized cause of pulmonary hypertension, its significance is often underestimated in practice.
“Whether the valve is regurgitant or stenotic makes absolutely no difference. When you delay” repair or replacement, “the patient keeps getting sicker,” he said. In time, “everyone is standing around wringing their hands going, ‘Oh my god, what are we going to do? Are you serious? Fix the valve.’ We see this type of patient a couple times a month,” Dr. Forfia said at the American College of Chest Physicians annual meeting.
“I have seen lifesaving mitral valve surgery put off for many years in patients with pulmonary hypertension, when all they needed was to have their valve fixed,” he said.
Whatever the case, pulmonologists who want the valve fixed often end up playing patient ping pong with cardiologists who want the hypertension controlled beforehand, but “if I treat the pulmonary circulation first, all I am going to do is unmask the left heart failure. There will be no functional improvement whatsoever,” Dr. Forfia said.
Surgery is the best solution as long as patients are well enough to recover. “With pulmonary hypertension in the setting of severe mitral valve regurgitation or stenosis, whether the pulmonary hypertension is related to passive left heart congestion or associated with pulmonary arteriopathy, the only sensible option is to correct the underlying valvular abnormality,” he said. The surgery should be done at an institution capable of managing postop pulmonary arteriopathy, if present.
The ping pong solution is to send patients to an expert pulmonology center; the mitral valve problem will be spotted right away.
“There is no pulmonary pressure cutoff that should prohibit surgery” in patients able to recover. “There is no such thing as a pulmonary artery pressure too high to be explained by mitral valve disease. The pulmonary pressure can be as high as it wants to be. You will get nowhere by thinking the pressure is too high to address the valve,” Dr. Forfia said.
Often “you hear, ‘I’m afraid the person is going to die on the table.’ I always say ‘if the patient is not going to die on the table, they are going to die in their living room of progressive heart failure because you [didn’t] fix their valve. I have never had a patient with pulmonary hypertension not separate from cardiopulmonary bypass. It’s a myth,” he said.
When there’s a “question if the dyspnea is coming from the mitral valve, we routinely use exercise right heart catheterization to probe the situation. We have a recumbent bike in the cath lab. You’ll often provoke significant left heart congestion with a low workload. It’s very revealing to the significance of mitral valve disease,” he said.
Aortic valve disease is also missed in pulmonary hypertension. “It’s not [a] similar” problem; “it’s the same” problem, Dr. Forfia said.
Dr. Forfia is a consultant for Bayer, Actelion, and United Therapeutics.
EXPERT ANALYSIS FROM CHEST 2016
Bezlotoxumab reduces CDI recurrence across antibiotic subgroups
NEW ORLEANS – The monoclonal antibody bezlotoxumab significantly reduces the risk of Clostridium difficile infection (CDI) recurrence in adults receiving standard of care antibiotic treatment, regardless of whether that treatment is with metronidazole, vancomycin, or fidaxomicin, according to an analysis of data from the MODIFY I and II trials.
The global, randomized, double-blind, placebo-controlled trials demonstrated that bezlotoxumab was safe and effective for preventing CDI recurrence, and the current prespecified analysis further showed that choice of standard of care antibiotic therapy did not affect the outcomes, Erik R. Dubberke, MD, of Washington University in St. Louis, reported at IDWeek, an annual scientific meeting on infectious diseases.
Consistent with the overall study results, clinical cure rates were similar with bezlotoxumab and placebo, regardless of the standard of care antibiotic received (80% vs. 80.3%, respectively, overall; 81% vs. 81.3% in the metronidazole group; 78.5% vs. 79.6% in the vancomycin group; and 86.7% vs. 76.9% in the fidaxomicin group), he said.
However, CDI recurrence rates were lower among those who received bezlotoxumab, compared with those who received placebo in all three standard of care subgroups, with 10%, 15%, and 12% fewer bezlotoxumab vs. placebo patients experiencing recurrence in the metronidazole, vancomycin, and fidaxomicin groups, respectively, and 12% fewer experiencing recurrence overall.
The primary endpoint of CDI recurrence was defined in the studies as a new episode of diarrhea (at least three unformed stools in 24 hours) and a positive stool test for toxigenic C. difficile after clinical cure of the baseline CDI episode. Clinical cure was defined as standard of care antibiotics given for 14 days or less and no diarrhea for 2 consecutive days after completing standard of care treatment.
Of note, the patients in the vancomycin group were older and sicker, and had more risk factors for CDI, he said, noting, for example, that 57% of vancomycin patients were aged at least 65 years and 33% were aged at least 75 years, vs. 46% and 26% for metronidazole, respectively, and 46% and 18% for fidaxomicin; 72% of vancomycin patients were inpatients, compared with 65% and 50% of metronidazole and fidaxomicin patients.
Further, 19% of vancomycin patients, vs. 13% and 14% of metronidazole and fidaxomicin patients met criteria for severe CDI.
The findings of the current analysis are important, because the incidence of CDI recurrence is about 25%, and the risk increases with each subsequent recurrence, Dr. Dubberke said, concluding that this novel, nonantibiotic approach to prevention of CDI recurrence using bezlotoxumab, which recently received Food and Drug Administration approval for this indication, is of benefit for reducing that risk, regardless of the antibiotic used as part of standard of care therapy for CDI.
Dr. Dubberke reported serving as an investigator, adviser and/or consultant for Merck, Rebiotix, Sanofi Pasteur, and Summit, and receiving consultant fees and/or grant/research support from these companies.
NEW ORLEANS – The monoclonal antibody bezlotoxumab significantly reduces the risk of Clostridium difficile infection (CDI) recurrence in adults receiving standard of care antibiotic treatment, regardless of whether that treatment is with metronidazole, vancomycin, or fidaxomicin, according to an analysis of data from the MODIFY I and II trials.
The global, randomized, double-blind, placebo-controlled trials demonstrated that bezlotoxumab was safe and effective for preventing CDI recurrence, and the current prespecified analysis further showed that choice of standard of care antibiotic therapy did not affect the outcomes, Erik R. Dubberke, MD, of Washington University in St. Louis, reported at IDWeek, an annual scientific meeting on infectious diseases.
Consistent with the overall study results, clinical cure rates were similar with bezlotoxumab and placebo, regardless of the standard of care antibiotic received (80% vs. 80.3%, respectively, overall; 81% vs. 81.3% in the metronidazole group; 78.5% vs. 79.6% in the vancomycin group; and 86.7% vs. 76.9% in the fidaxomicin group), he said.
However, CDI recurrence rates were lower among those who received bezlotoxumab, compared with those who received placebo in all three standard of care subgroups, with 10%, 15%, and 12% fewer bezlotoxumab vs. placebo patients experiencing recurrence in the metronidazole, vancomycin, and fidaxomicin groups, respectively, and 12% fewer experiencing recurrence overall.
The primary endpoint of CDI recurrence was defined in the studies as a new episode of diarrhea (at least three unformed stools in 24 hours) and a positive stool test for toxigenic C. difficile after clinical cure of the baseline CDI episode. Clinical cure was defined as standard of care antibiotics given for 14 days or less and no diarrhea for 2 consecutive days after completing standard of care treatment.
Of note, the patients in the vancomycin group were older and sicker, and had more risk factors for CDI, he said, noting, for example, that 57% of vancomycin patients were aged at least 65 years and 33% were aged at least 75 years, vs. 46% and 26% for metronidazole, respectively, and 46% and 18% for fidaxomicin; 72% of vancomycin patients were inpatients, compared with 65% and 50% of metronidazole and fidaxomicin patients.
Further, 19% of vancomycin patients, vs. 13% and 14% of metronidazole and fidaxomicin patients met criteria for severe CDI.
The findings of the current analysis are important, because the incidence of CDI recurrence is about 25%, and the risk increases with each subsequent recurrence, Dr. Dubberke said, concluding that this novel, nonantibiotic approach to prevention of CDI recurrence using bezlotoxumab, which recently received Food and Drug Administration approval for this indication, is of benefit for reducing that risk, regardless of the antibiotic used as part of standard of care therapy for CDI.
Dr. Dubberke reported serving as an investigator, adviser and/or consultant for Merck, Rebiotix, Sanofi Pasteur, and Summit, and receiving consultant fees and/or grant/research support from these companies.
NEW ORLEANS – The monoclonal antibody bezlotoxumab significantly reduces the risk of Clostridium difficile infection (CDI) recurrence in adults receiving standard of care antibiotic treatment, regardless of whether that treatment is with metronidazole, vancomycin, or fidaxomicin, according to an analysis of data from the MODIFY I and II trials.
The global, randomized, double-blind, placebo-controlled trials demonstrated that bezlotoxumab was safe and effective for preventing CDI recurrence, and the current prespecified analysis further showed that choice of standard of care antibiotic therapy did not affect the outcomes, Erik R. Dubberke, MD, of Washington University in St. Louis, reported at IDWeek, an annual scientific meeting on infectious diseases.
Consistent with the overall study results, clinical cure rates were similar with bezlotoxumab and placebo, regardless of the standard of care antibiotic received (80% vs. 80.3%, respectively, overall; 81% vs. 81.3% in the metronidazole group; 78.5% vs. 79.6% in the vancomycin group; and 86.7% vs. 76.9% in the fidaxomicin group), he said.
However, CDI recurrence rates were lower among those who received bezlotoxumab, compared with those who received placebo in all three standard of care subgroups, with 10%, 15%, and 12% fewer bezlotoxumab vs. placebo patients experiencing recurrence in the metronidazole, vancomycin, and fidaxomicin groups, respectively, and 12% fewer experiencing recurrence overall.
The primary endpoint of CDI recurrence was defined in the studies as a new episode of diarrhea (at least three unformed stools in 24 hours) and a positive stool test for toxigenic C. difficile after clinical cure of the baseline CDI episode. Clinical cure was defined as standard of care antibiotics given for 14 days or less and no diarrhea for 2 consecutive days after completing standard of care treatment.
Of note, the patients in the vancomycin group were older and sicker, and had more risk factors for CDI, he said, noting, for example, that 57% of vancomycin patients were aged at least 65 years and 33% were aged at least 75 years, vs. 46% and 26% for metronidazole, respectively, and 46% and 18% for fidaxomicin; 72% of vancomycin patients were inpatients, compared with 65% and 50% of metronidazole and fidaxomicin patients.
Further, 19% of vancomycin patients, vs. 13% and 14% of metronidazole and fidaxomicin patients met criteria for severe CDI.
The findings of the current analysis are important, because the incidence of CDI recurrence is about 25%, and the risk increases with each subsequent recurrence, Dr. Dubberke said, concluding that this novel, nonantibiotic approach to prevention of CDI recurrence using bezlotoxumab, which recently received Food and Drug Administration approval for this indication, is of benefit for reducing that risk, regardless of the antibiotic used as part of standard of care therapy for CDI.
Dr. Dubberke reported serving as an investigator, adviser and/or consultant for Merck, Rebiotix, Sanofi Pasteur, and Summit, and receiving consultant fees and/or grant/research support from these companies.
AT IDWEEK 2016
Key clinical point:
Major finding: 12% fewer bezlotoxumab vs. placebo patients experienced CDI recurrence.
Data source: A prespecified analysis of data from 1,554 subjects from the MODIFY I and II trials.
Disclosures: Dr. Dubberke reported serving as an investigator, adviser, and/or consultant for Merck, Rebiotix, Sanofi Pasteur, and Summit, and receiving consultant fees and/or grant/research support from these companies.
Can carotid interventions affect cognitive function?
COLUMBUS, OHIO – The primary goal of carotid artery revascularization is to prevent stroke, heart attack or death, but carotid artery stenting and carotid endarterectomy may also cause changes in cognitive skills, according Raghu Motaganahalli, MD, of the Indiana University, Indianapolis.
“What about cognitive dysfunction as a result of carotid artery stenting (CAS) or carotid endarterectomy (CEA)?” Dr. Motaganahalli asked at the annual meeting of the Midwestern Vascular Surgical Society. “I think this is real, that there’s some truth to the matter. The question is how much and what domains of cognitive functions are affected?”
“Cerebrovascular hemodynamics status plays a role in cognitive function, but we need a better understanding of cerebrovascular hemodynamic failure and either improvement or decline of cognitive function after CAS or CEA,” he said.
A review of published trials shows that 10%-20% of patients who have either CAS or CEA have some degree of cognitive dysfunction as early as a day after the procedure. “It’s not a small number, compared to stoke, risk of myocardial infarction and death,” he said.
Some series have reported up to 40% of patients showed some cognitive dysfunction, and post–carotid endarterectomy cognitive dysfunction has been associated with early death, Dr. Motaganahalli said.
Cognitive dysfunction manifests in various forms, ranging from level of consciousness and memory to mood and ability to make calculations. Although the Mini-Mental State Examination Global Cognitive Assessment tool provides a method for evaluating cognitive function, “There is no uniformly accepted neurocognition test,” Dr. Motaganahalli said. That explains the wide variability of findings among published studies.
Vascular surgeons take a somewhat casual approach to their patients’ cognitive abilities after carotid revascularization, Dr. Motaganahalli said. “We don’t evaluate their memory and their cognitive functions on post-op day one; we just look to see whether they have neurologic dysfunction up front and that they’re capable of going home after that.”
But predicting in advance which patients are predisposed to cognitive decline after the procedures is difficult, he said. He cited a systematic review of 32 studies published between 1990-2007 that showed variable results (Stroke. 2008;39:3116-27): 11 studies during 1990-2005 suggested cognition actually improved after CEA; 9 studies during 1994-2006 suggested the opposite; 4 trials during 1992-2005 suggested no change in cognition after CEA; 5 studies during 2003-2007 showed improvement in cognition after CAS; and 3 trials comparing CAS and CEA and cognition found no differences in how the two procedures affect cognition.
Dr. Motaganahalli also cited a systematic review of 37 studies, 18 of which examined CEA, 12 CAS and seven compared CEA and CAS, found that either cognitive improvement or impairment for CEA and CAS separately were 10–15% of patients (Cerebrovasc Dis Extra. 2014;4:132-48).
“We have 69 papers that looked at cognitive function alone, but unfortunately, we don’t know whether cognitive function really improved based on this data set,” he said. “None of them are making the argument so clearly that there is cognitive improvement after revascularization.”
The variability in study findings can be due to differences in methodologies, the types of psychometric tests used, statistical analyses and the timing of cognitive assessments, Dr. Motaganahalli said.
Cognitive impairment after stroke caused by carotid disease is better understood than is cognitive impairment in the absence of a major stroke, Dr. Motaganahalli said.
“The mechanisms of how carotid disease can cause the cognitive impairment are threefold: It could be microembolism and hypoperfusion, which together can cause white matter disease and thereby some cognitive dysfunction in the long term,” he said (Neuroimaging Clin N Am. 2007 Aug;17:313-24).
Functional neurons may be a biomarker of cognitive outcome, he said. Hypoperfusion of functional neurons may lead to hypofunctional neurons, which can increase cerebral blood flow and cerebral metabolic rate for oxygen (CMRO2), and thus improve cognition. However, when additional variables are introduced to the hypofunctional neurons – such as microembolism, white matter disease, and prolonged hypoperfusion – that can lead to neuronal infarction that, while increasing cerebral blood flow, causes no change in CMRO2 and, thus, no cognitive improvement. The interval between hypofunctional neurons and neuronal infarction “is the time to do the revascularization, as long as you can demonstrate that there may be some truth to matter that it influences cognition,” Dr. Motaganahalli said.
While vascular surgeons may not be able to predict who will have cognitive decline after carotid interventions, “There are some pointers for possibly picking those patients who may benefit,” Dr. Motaganahalli said.
That choice of patients revolves around recognizing that chronic ischemia induces and increases the severity of cognitive dysfunction. Therefore, incorporating the pathophysiology of chronic ischemia into the algorithm for carotid artery disease may provide an opportunity to extend the goals of carotid artery revascularization to include preventing or reversing cognitive decline, he said.
Dr. Motaganahalli disclosed he is a consultant to Silk Road Medical.
COLUMBUS, OHIO – The primary goal of carotid artery revascularization is to prevent stroke, heart attack or death, but carotid artery stenting and carotid endarterectomy may also cause changes in cognitive skills, according Raghu Motaganahalli, MD, of the Indiana University, Indianapolis.
“What about cognitive dysfunction as a result of carotid artery stenting (CAS) or carotid endarterectomy (CEA)?” Dr. Motaganahalli asked at the annual meeting of the Midwestern Vascular Surgical Society. “I think this is real, that there’s some truth to the matter. The question is how much and what domains of cognitive functions are affected?”
“Cerebrovascular hemodynamics status plays a role in cognitive function, but we need a better understanding of cerebrovascular hemodynamic failure and either improvement or decline of cognitive function after CAS or CEA,” he said.
A review of published trials shows that 10%-20% of patients who have either CAS or CEA have some degree of cognitive dysfunction as early as a day after the procedure. “It’s not a small number, compared to stoke, risk of myocardial infarction and death,” he said.
Some series have reported up to 40% of patients showed some cognitive dysfunction, and post–carotid endarterectomy cognitive dysfunction has been associated with early death, Dr. Motaganahalli said.
Cognitive dysfunction manifests in various forms, ranging from level of consciousness and memory to mood and ability to make calculations. Although the Mini-Mental State Examination Global Cognitive Assessment tool provides a method for evaluating cognitive function, “There is no uniformly accepted neurocognition test,” Dr. Motaganahalli said. That explains the wide variability of findings among published studies.
Vascular surgeons take a somewhat casual approach to their patients’ cognitive abilities after carotid revascularization, Dr. Motaganahalli said. “We don’t evaluate their memory and their cognitive functions on post-op day one; we just look to see whether they have neurologic dysfunction up front and that they’re capable of going home after that.”
But predicting in advance which patients are predisposed to cognitive decline after the procedures is difficult, he said. He cited a systematic review of 32 studies published between 1990-2007 that showed variable results (Stroke. 2008;39:3116-27): 11 studies during 1990-2005 suggested cognition actually improved after CEA; 9 studies during 1994-2006 suggested the opposite; 4 trials during 1992-2005 suggested no change in cognition after CEA; 5 studies during 2003-2007 showed improvement in cognition after CAS; and 3 trials comparing CAS and CEA and cognition found no differences in how the two procedures affect cognition.
Dr. Motaganahalli also cited a systematic review of 37 studies, 18 of which examined CEA, 12 CAS and seven compared CEA and CAS, found that either cognitive improvement or impairment for CEA and CAS separately were 10–15% of patients (Cerebrovasc Dis Extra. 2014;4:132-48).
“We have 69 papers that looked at cognitive function alone, but unfortunately, we don’t know whether cognitive function really improved based on this data set,” he said. “None of them are making the argument so clearly that there is cognitive improvement after revascularization.”
The variability in study findings can be due to differences in methodologies, the types of psychometric tests used, statistical analyses and the timing of cognitive assessments, Dr. Motaganahalli said.
Cognitive impairment after stroke caused by carotid disease is better understood than is cognitive impairment in the absence of a major stroke, Dr. Motaganahalli said.
“The mechanisms of how carotid disease can cause the cognitive impairment are threefold: It could be microembolism and hypoperfusion, which together can cause white matter disease and thereby some cognitive dysfunction in the long term,” he said (Neuroimaging Clin N Am. 2007 Aug;17:313-24).
Functional neurons may be a biomarker of cognitive outcome, he said. Hypoperfusion of functional neurons may lead to hypofunctional neurons, which can increase cerebral blood flow and cerebral metabolic rate for oxygen (CMRO2), and thus improve cognition. However, when additional variables are introduced to the hypofunctional neurons – such as microembolism, white matter disease, and prolonged hypoperfusion – that can lead to neuronal infarction that, while increasing cerebral blood flow, causes no change in CMRO2 and, thus, no cognitive improvement. The interval between hypofunctional neurons and neuronal infarction “is the time to do the revascularization, as long as you can demonstrate that there may be some truth to matter that it influences cognition,” Dr. Motaganahalli said.
While vascular surgeons may not be able to predict who will have cognitive decline after carotid interventions, “There are some pointers for possibly picking those patients who may benefit,” Dr. Motaganahalli said.
That choice of patients revolves around recognizing that chronic ischemia induces and increases the severity of cognitive dysfunction. Therefore, incorporating the pathophysiology of chronic ischemia into the algorithm for carotid artery disease may provide an opportunity to extend the goals of carotid artery revascularization to include preventing or reversing cognitive decline, he said.
Dr. Motaganahalli disclosed he is a consultant to Silk Road Medical.
COLUMBUS, OHIO – The primary goal of carotid artery revascularization is to prevent stroke, heart attack or death, but carotid artery stenting and carotid endarterectomy may also cause changes in cognitive skills, according Raghu Motaganahalli, MD, of the Indiana University, Indianapolis.
“What about cognitive dysfunction as a result of carotid artery stenting (CAS) or carotid endarterectomy (CEA)?” Dr. Motaganahalli asked at the annual meeting of the Midwestern Vascular Surgical Society. “I think this is real, that there’s some truth to the matter. The question is how much and what domains of cognitive functions are affected?”
“Cerebrovascular hemodynamics status plays a role in cognitive function, but we need a better understanding of cerebrovascular hemodynamic failure and either improvement or decline of cognitive function after CAS or CEA,” he said.
A review of published trials shows that 10%-20% of patients who have either CAS or CEA have some degree of cognitive dysfunction as early as a day after the procedure. “It’s not a small number, compared to stoke, risk of myocardial infarction and death,” he said.
Some series have reported up to 40% of patients showed some cognitive dysfunction, and post–carotid endarterectomy cognitive dysfunction has been associated with early death, Dr. Motaganahalli said.
Cognitive dysfunction manifests in various forms, ranging from level of consciousness and memory to mood and ability to make calculations. Although the Mini-Mental State Examination Global Cognitive Assessment tool provides a method for evaluating cognitive function, “There is no uniformly accepted neurocognition test,” Dr. Motaganahalli said. That explains the wide variability of findings among published studies.
Vascular surgeons take a somewhat casual approach to their patients’ cognitive abilities after carotid revascularization, Dr. Motaganahalli said. “We don’t evaluate their memory and their cognitive functions on post-op day one; we just look to see whether they have neurologic dysfunction up front and that they’re capable of going home after that.”
But predicting in advance which patients are predisposed to cognitive decline after the procedures is difficult, he said. He cited a systematic review of 32 studies published between 1990-2007 that showed variable results (Stroke. 2008;39:3116-27): 11 studies during 1990-2005 suggested cognition actually improved after CEA; 9 studies during 1994-2006 suggested the opposite; 4 trials during 1992-2005 suggested no change in cognition after CEA; 5 studies during 2003-2007 showed improvement in cognition after CAS; and 3 trials comparing CAS and CEA and cognition found no differences in how the two procedures affect cognition.
Dr. Motaganahalli also cited a systematic review of 37 studies, 18 of which examined CEA, 12 CAS and seven compared CEA and CAS, found that either cognitive improvement or impairment for CEA and CAS separately were 10–15% of patients (Cerebrovasc Dis Extra. 2014;4:132-48).
“We have 69 papers that looked at cognitive function alone, but unfortunately, we don’t know whether cognitive function really improved based on this data set,” he said. “None of them are making the argument so clearly that there is cognitive improvement after revascularization.”
The variability in study findings can be due to differences in methodologies, the types of psychometric tests used, statistical analyses and the timing of cognitive assessments, Dr. Motaganahalli said.
Cognitive impairment after stroke caused by carotid disease is better understood than is cognitive impairment in the absence of a major stroke, Dr. Motaganahalli said.
“The mechanisms of how carotid disease can cause the cognitive impairment are threefold: It could be microembolism and hypoperfusion, which together can cause white matter disease and thereby some cognitive dysfunction in the long term,” he said (Neuroimaging Clin N Am. 2007 Aug;17:313-24).
Functional neurons may be a biomarker of cognitive outcome, he said. Hypoperfusion of functional neurons may lead to hypofunctional neurons, which can increase cerebral blood flow and cerebral metabolic rate for oxygen (CMRO2), and thus improve cognition. However, when additional variables are introduced to the hypofunctional neurons – such as microembolism, white matter disease, and prolonged hypoperfusion – that can lead to neuronal infarction that, while increasing cerebral blood flow, causes no change in CMRO2 and, thus, no cognitive improvement. The interval between hypofunctional neurons and neuronal infarction “is the time to do the revascularization, as long as you can demonstrate that there may be some truth to matter that it influences cognition,” Dr. Motaganahalli said.
While vascular surgeons may not be able to predict who will have cognitive decline after carotid interventions, “There are some pointers for possibly picking those patients who may benefit,” Dr. Motaganahalli said.
That choice of patients revolves around recognizing that chronic ischemia induces and increases the severity of cognitive dysfunction. Therefore, incorporating the pathophysiology of chronic ischemia into the algorithm for carotid artery disease may provide an opportunity to extend the goals of carotid artery revascularization to include preventing or reversing cognitive decline, he said.
Dr. Motaganahalli disclosed he is a consultant to Silk Road Medical.
AT THE ANNUAL MEETING OF THE MIDWESTERN VASCULAR SURGERY SOCIETY
Key clinical point: Incorporating the pathophysiology of chronic ischemia into the algorithm for carotid artery disease could expand the goals of revascularization to encompass cognitive decline.
Major finding: Cerebrovascular hemodynamic status plays a role in cognitive function after carotid artery interventions, but the mechanisms of either improvement or decline need better understanding.
Data source: Systematic review of 32 papers on neurocognition after carotid interventions published between 1990-2007 and analysis of 37 studies of CAS or CEA or both published since 2007.
Disclosures: Dr. Motaganahalli disclosed he is a consultant to Silk Road Medical Inc.
Prognostic scores helpful in subset of COPD patients
LOS ANGELES – The Sequential Organ Failure Assessment (SOFA) score and the Glasgow Coma Scale (GCS) are simple, accurate tools for risk stratification of hospitalized patients with acute exacerbation of COPD, results from a single-center study showed.
“Acute exacerbations of chronic obstructive pulmonary disease often require hospitalization, may necessitate mechanical ventilation, and can be fatal,” Mohamed Metwally, MD, FCCP, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “There are currently no validated disease-specific scores that measure the severity of acute exacerbation. Prognostic tools are needed to assess acute exacerbations of chronic obstructive pulmonary disease.”
For the 2-year study, Dr. Metwally and his associates prospectively evaluated 250 critically ill ICU AECOPD patients, mean age 65 years, at Assiut University Hospital between December 2012 and December 2014. The primary outcome was in-hospital mortality while the secondary endpoint was need for intubation and mechanical ventilation. The researchers excluded patients who died less than 24 hours after admission, those with underlying COPD who were admitted with another primary diagnosis such as an accident or a stroke, or for elective hospitalizations such as elective surgery or diagnostic procedures.
Dr. Metwally and his associates collected sociodemographic data, vital signs, and other clinical variables, and collected scores from five tools used to measure mortality prediction: the Acute Physiology and Chronic Health Evaluation (APACHE II), the SOFA score, the Early Warning Score (EWS), the GCS, and the Charlson Comorbidity Index (CCI). To assess performance of the scores, they used area under the receiver operating characteristic curve (AUC) analysis and the Hosmer-Lemeshow goodness-of-fit test for logistic regression.
Of the 250 patients, 43 (17%) died during their hospital stay and 54% required mechanical ventilation. All recorded scores were significantly higher in nonsurvivors, compared with survivors, and the risk of clinical deterioration increased with increasing scores. The discriminatory power of each score varied as measured by AUC analysis. The AUC of APACHE II, SOFA, EWS, GCS, and CCI were 0.79, 0.81, 0.76, 0.69, and 0.68, respectively “and all these models had good calibration in mortality prediction,” Dr. Metwally said. The SOFA score was the best in predicting mortality (its predicted mortality was 16%, compared with the actual mortality of 17%), while the APACHE II score overestimated mortality by at least twofold (46% vs. 17%). In addition, the EWS outperformed the GCS in predicting mortality. “This may be due to EWS containing all vital signs plus level of consciousness,” he said in an interview.
The GCS was found to be the most useful in predicting need for mechanical ventilation, with an AUC of 0.81. The AUCs of APACHE II, SOFA, EWS, and CCI were 0.79, 0.80, 0.73, and 0.61, respectively. All of the scores had good calibration in mortality prediction, Dr. Metwally said, with the exception of SOFA.
As for the APACHE II, Dr. Metwally said that instrument “can be used as a tool to predict both mortality and intubation in a specific group of patients, but with low discriminatory power.” He acknowledged certain limitations of the study, including the fact that it was limited to patients with AECOPD. “Future studies should include any critically ill respiratory patients,” he said.
He reported having no financial disclosures.
LOS ANGELES – The Sequential Organ Failure Assessment (SOFA) score and the Glasgow Coma Scale (GCS) are simple, accurate tools for risk stratification of hospitalized patients with acute exacerbation of COPD, results from a single-center study showed.
“Acute exacerbations of chronic obstructive pulmonary disease often require hospitalization, may necessitate mechanical ventilation, and can be fatal,” Mohamed Metwally, MD, FCCP, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “There are currently no validated disease-specific scores that measure the severity of acute exacerbation. Prognostic tools are needed to assess acute exacerbations of chronic obstructive pulmonary disease.”
For the 2-year study, Dr. Metwally and his associates prospectively evaluated 250 critically ill ICU AECOPD patients, mean age 65 years, at Assiut University Hospital between December 2012 and December 2014. The primary outcome was in-hospital mortality while the secondary endpoint was need for intubation and mechanical ventilation. The researchers excluded patients who died less than 24 hours after admission, those with underlying COPD who were admitted with another primary diagnosis such as an accident or a stroke, or for elective hospitalizations such as elective surgery or diagnostic procedures.
Dr. Metwally and his associates collected sociodemographic data, vital signs, and other clinical variables, and collected scores from five tools used to measure mortality prediction: the Acute Physiology and Chronic Health Evaluation (APACHE II), the SOFA score, the Early Warning Score (EWS), the GCS, and the Charlson Comorbidity Index (CCI). To assess performance of the scores, they used area under the receiver operating characteristic curve (AUC) analysis and the Hosmer-Lemeshow goodness-of-fit test for logistic regression.
Of the 250 patients, 43 (17%) died during their hospital stay and 54% required mechanical ventilation. All recorded scores were significantly higher in nonsurvivors, compared with survivors, and the risk of clinical deterioration increased with increasing scores. The discriminatory power of each score varied as measured by AUC analysis. The AUC of APACHE II, SOFA, EWS, GCS, and CCI were 0.79, 0.81, 0.76, 0.69, and 0.68, respectively “and all these models had good calibration in mortality prediction,” Dr. Metwally said. The SOFA score was the best in predicting mortality (its predicted mortality was 16%, compared with the actual mortality of 17%), while the APACHE II score overestimated mortality by at least twofold (46% vs. 17%). In addition, the EWS outperformed the GCS in predicting mortality. “This may be due to EWS containing all vital signs plus level of consciousness,” he said in an interview.
The GCS was found to be the most useful in predicting need for mechanical ventilation, with an AUC of 0.81. The AUCs of APACHE II, SOFA, EWS, and CCI were 0.79, 0.80, 0.73, and 0.61, respectively. All of the scores had good calibration in mortality prediction, Dr. Metwally said, with the exception of SOFA.
As for the APACHE II, Dr. Metwally said that instrument “can be used as a tool to predict both mortality and intubation in a specific group of patients, but with low discriminatory power.” He acknowledged certain limitations of the study, including the fact that it was limited to patients with AECOPD. “Future studies should include any critically ill respiratory patients,” he said.
He reported having no financial disclosures.
LOS ANGELES – The Sequential Organ Failure Assessment (SOFA) score and the Glasgow Coma Scale (GCS) are simple, accurate tools for risk stratification of hospitalized patients with acute exacerbation of COPD, results from a single-center study showed.
“Acute exacerbations of chronic obstructive pulmonary disease often require hospitalization, may necessitate mechanical ventilation, and can be fatal,” Mohamed Metwally, MD, FCCP, said in an interview in advance of the annual meeting of the American College of Chest Physicians. “There are currently no validated disease-specific scores that measure the severity of acute exacerbation. Prognostic tools are needed to assess acute exacerbations of chronic obstructive pulmonary disease.”
For the 2-year study, Dr. Metwally and his associates prospectively evaluated 250 critically ill ICU AECOPD patients, mean age 65 years, at Assiut University Hospital between December 2012 and December 2014. The primary outcome was in-hospital mortality while the secondary endpoint was need for intubation and mechanical ventilation. The researchers excluded patients who died less than 24 hours after admission, those with underlying COPD who were admitted with another primary diagnosis such as an accident or a stroke, or for elective hospitalizations such as elective surgery or diagnostic procedures.
Dr. Metwally and his associates collected sociodemographic data, vital signs, and other clinical variables, and collected scores from five tools used to measure mortality prediction: the Acute Physiology and Chronic Health Evaluation (APACHE II), the SOFA score, the Early Warning Score (EWS), the GCS, and the Charlson Comorbidity Index (CCI). To assess performance of the scores, they used area under the receiver operating characteristic curve (AUC) analysis and the Hosmer-Lemeshow goodness-of-fit test for logistic regression.
Of the 250 patients, 43 (17%) died during their hospital stay and 54% required mechanical ventilation. All recorded scores were significantly higher in nonsurvivors, compared with survivors, and the risk of clinical deterioration increased with increasing scores. The discriminatory power of each score varied as measured by AUC analysis. The AUC of APACHE II, SOFA, EWS, GCS, and CCI were 0.79, 0.81, 0.76, 0.69, and 0.68, respectively “and all these models had good calibration in mortality prediction,” Dr. Metwally said. The SOFA score was the best in predicting mortality (its predicted mortality was 16%, compared with the actual mortality of 17%), while the APACHE II score overestimated mortality by at least twofold (46% vs. 17%). In addition, the EWS outperformed the GCS in predicting mortality. “This may be due to EWS containing all vital signs plus level of consciousness,” he said in an interview.
The GCS was found to be the most useful in predicting need for mechanical ventilation, with an AUC of 0.81. The AUCs of APACHE II, SOFA, EWS, and CCI were 0.79, 0.80, 0.73, and 0.61, respectively. All of the scores had good calibration in mortality prediction, Dr. Metwally said, with the exception of SOFA.
As for the APACHE II, Dr. Metwally said that instrument “can be used as a tool to predict both mortality and intubation in a specific group of patients, but with low discriminatory power.” He acknowledged certain limitations of the study, including the fact that it was limited to patients with AECOPD. “Future studies should include any critically ill respiratory patients,” he said.
He reported having no financial disclosures.
AT CHEST 2016
Key clinical point:
Major finding: The Sequential Organ Failure Assessment score was the best in predicting mortality of patients with acute exacerbation of COPD (its predicted mortality was 16%, compared with the actual mortality of 17%).
Data source: A prospective evaluation of 250 critically ill ICU patients hospitalized with acute exacerbation of COPD.
Disclosures: Dr. Metwally reported having no financial disclosures.
He/O2 does not reduce NIV failure in severe COPD exacerbations
Inhaling He/O2 did not result in a lower NIV failure rate than inhaling Air/O2 in COPD patients requiring noninvasive ventilation, in a randomized, controlled study.
In the study, known as the E.C.H.O.ICU trial, patients either received He/02 (a 78%/22% mixture blended with 100% O2) or a conventional Air/O2 mixture for up to 72 hours, during both noninvasive ventilation (NIV) and spontaneous breathing.
Previous research had demonstrated that during hypercapnic COPD exacerbations, the He/O2 mixture reduces airway resistance, partial pressure of carbon dioxide in arterial blood (PaCO2), intrinsic positive end-expiratory pressure, and work of breathing during both spontaneous breathing and NIV, compared with Air/O2, said Philippe Jolliet, MD, and his colleagues.
The two treatment groups in the E.C.H.O.ICU trial had similar NIV failure rates – defined as endotracheal intubation or death without intubation. The rates were 14.7% for the patients who received He/O2 and 14.5% for the patients who received Air/O2. The NIV failures for 31 the patients in the He/O2 group resulted in intubation; the remaining two patients who were classified as having NIV failure died. All 32 of the patients in the Air/O2 group who had NIV failures were intubated.
The length of ICU stay was also comparable between the two groups. In the subgroups of patients with severe acidosis (having a pH of less than 7.30) from both the He/O2 and Air/O2 groups, the NIV failure rates were again nearly identical (AJRCCM. 2016 Oct 13; doi: 10.1164/rccm.201601-0083OC).
The average times to NIV failure were 93 hours in the He/O2 group (N = 33) and 52 hours in the Air/O2 group (N = 32, P = .12). The He/O2 group achieved a significantly quicker improvement in respiratory acidosis, encephalopathy score, and respiratory rate.
Patients intubated following an NIV failure who had received He/O2 had a shorter ventilation duration and a shorter ICU stay than did the intubated patients who had received Air/O2 (7.4 days, vs. 13.6 days, P = .02, and 15.8 vs. 26.7 days, P = .01).
No significant differences appeared in the safety profile of the two groups, nor were significant differences seen in ICU, hospital, or 6-month mortality rates; or in 6-month hospital readmission rates.
“[The] study was stopped prematurely after a futility analysis due the low event rate identified by [an independent adjudication committee],” said Dr. Jolliet of the intensive care and burn unit at Le Centre Hospitalier Universitaire Vaudois (CHUV), in Lausanne, Switzerland, and his fellow researchers.
The study included 445 patients from ICUs or intermediate care units in six countries. The inclusion criteria were presenting with current COPD exacerbation with hypercapnic acute respiratory failure, a PaCO2 of at least 45 mm Hg, an arterial pH of less than or equal to 7.35, and at least one of the following: respiration rate of at least 25 breaths per minute, a PaO2 less than or equal to 50 mm Hg, and an arterial oxygen saturation of less than or equal to 90%.
Half of the patients in each group were already receiving NIV prior to enrollment in the study. Males constituted two thirds of all enrolled patients.
HeO2 administration was limited to 72 hours for each patient and about a third of NIV failures occurred after the end of the HeO2 administration, the researchers said.
“The main reason for the absence of observed benefit on outcome in the He/O2 probably lies in the very low NIV failure rate now observed in both groups. One possible mechanism explaining the low intubation rate could be that some patients had received uncontrolled oxygen therapy prior to ICU admission, thereby worsening initial hypercapnia and acidosis, a problem that can easily be corrected by adequate titration,” the researchers said. “The 14.5% failure rate in the Air/O2 group was much lower than the 25% rate used in designing the study,” which was based on previous research.
The trial’s sponsor, Air Liquide Healthcare, provided input into the design and conduct of the study; oversaw the collection, management, and statistical analysis of data; and contributed to the manuscript’s preparation and review.
Inhaling He/O2 did not result in a lower NIV failure rate than inhaling Air/O2 in COPD patients requiring noninvasive ventilation, in a randomized, controlled study.
In the study, known as the E.C.H.O.ICU trial, patients either received He/02 (a 78%/22% mixture blended with 100% O2) or a conventional Air/O2 mixture for up to 72 hours, during both noninvasive ventilation (NIV) and spontaneous breathing.
Previous research had demonstrated that during hypercapnic COPD exacerbations, the He/O2 mixture reduces airway resistance, partial pressure of carbon dioxide in arterial blood (PaCO2), intrinsic positive end-expiratory pressure, and work of breathing during both spontaneous breathing and NIV, compared with Air/O2, said Philippe Jolliet, MD, and his colleagues.
The two treatment groups in the E.C.H.O.ICU trial had similar NIV failure rates – defined as endotracheal intubation or death without intubation. The rates were 14.7% for the patients who received He/O2 and 14.5% for the patients who received Air/O2. The NIV failures for 31 the patients in the He/O2 group resulted in intubation; the remaining two patients who were classified as having NIV failure died. All 32 of the patients in the Air/O2 group who had NIV failures were intubated.
The length of ICU stay was also comparable between the two groups. In the subgroups of patients with severe acidosis (having a pH of less than 7.30) from both the He/O2 and Air/O2 groups, the NIV failure rates were again nearly identical (AJRCCM. 2016 Oct 13; doi: 10.1164/rccm.201601-0083OC).
The average times to NIV failure were 93 hours in the He/O2 group (N = 33) and 52 hours in the Air/O2 group (N = 32, P = .12). The He/O2 group achieved a significantly quicker improvement in respiratory acidosis, encephalopathy score, and respiratory rate.
Patients intubated following an NIV failure who had received He/O2 had a shorter ventilation duration and a shorter ICU stay than did the intubated patients who had received Air/O2 (7.4 days, vs. 13.6 days, P = .02, and 15.8 vs. 26.7 days, P = .01).
No significant differences appeared in the safety profile of the two groups, nor were significant differences seen in ICU, hospital, or 6-month mortality rates; or in 6-month hospital readmission rates.
“[The] study was stopped prematurely after a futility analysis due the low event rate identified by [an independent adjudication committee],” said Dr. Jolliet of the intensive care and burn unit at Le Centre Hospitalier Universitaire Vaudois (CHUV), in Lausanne, Switzerland, and his fellow researchers.
The study included 445 patients from ICUs or intermediate care units in six countries. The inclusion criteria were presenting with current COPD exacerbation with hypercapnic acute respiratory failure, a PaCO2 of at least 45 mm Hg, an arterial pH of less than or equal to 7.35, and at least one of the following: respiration rate of at least 25 breaths per minute, a PaO2 less than or equal to 50 mm Hg, and an arterial oxygen saturation of less than or equal to 90%.
Half of the patients in each group were already receiving NIV prior to enrollment in the study. Males constituted two thirds of all enrolled patients.
HeO2 administration was limited to 72 hours for each patient and about a third of NIV failures occurred after the end of the HeO2 administration, the researchers said.
“The main reason for the absence of observed benefit on outcome in the He/O2 probably lies in the very low NIV failure rate now observed in both groups. One possible mechanism explaining the low intubation rate could be that some patients had received uncontrolled oxygen therapy prior to ICU admission, thereby worsening initial hypercapnia and acidosis, a problem that can easily be corrected by adequate titration,” the researchers said. “The 14.5% failure rate in the Air/O2 group was much lower than the 25% rate used in designing the study,” which was based on previous research.
The trial’s sponsor, Air Liquide Healthcare, provided input into the design and conduct of the study; oversaw the collection, management, and statistical analysis of data; and contributed to the manuscript’s preparation and review.
Inhaling He/O2 did not result in a lower NIV failure rate than inhaling Air/O2 in COPD patients requiring noninvasive ventilation, in a randomized, controlled study.
In the study, known as the E.C.H.O.ICU trial, patients either received He/02 (a 78%/22% mixture blended with 100% O2) or a conventional Air/O2 mixture for up to 72 hours, during both noninvasive ventilation (NIV) and spontaneous breathing.
Previous research had demonstrated that during hypercapnic COPD exacerbations, the He/O2 mixture reduces airway resistance, partial pressure of carbon dioxide in arterial blood (PaCO2), intrinsic positive end-expiratory pressure, and work of breathing during both spontaneous breathing and NIV, compared with Air/O2, said Philippe Jolliet, MD, and his colleagues.
The two treatment groups in the E.C.H.O.ICU trial had similar NIV failure rates – defined as endotracheal intubation or death without intubation. The rates were 14.7% for the patients who received He/O2 and 14.5% for the patients who received Air/O2. The NIV failures for 31 the patients in the He/O2 group resulted in intubation; the remaining two patients who were classified as having NIV failure died. All 32 of the patients in the Air/O2 group who had NIV failures were intubated.
The length of ICU stay was also comparable between the two groups. In the subgroups of patients with severe acidosis (having a pH of less than 7.30) from both the He/O2 and Air/O2 groups, the NIV failure rates were again nearly identical (AJRCCM. 2016 Oct 13; doi: 10.1164/rccm.201601-0083OC).
The average times to NIV failure were 93 hours in the He/O2 group (N = 33) and 52 hours in the Air/O2 group (N = 32, P = .12). The He/O2 group achieved a significantly quicker improvement in respiratory acidosis, encephalopathy score, and respiratory rate.
Patients intubated following an NIV failure who had received He/O2 had a shorter ventilation duration and a shorter ICU stay than did the intubated patients who had received Air/O2 (7.4 days, vs. 13.6 days, P = .02, and 15.8 vs. 26.7 days, P = .01).
No significant differences appeared in the safety profile of the two groups, nor were significant differences seen in ICU, hospital, or 6-month mortality rates; or in 6-month hospital readmission rates.
“[The] study was stopped prematurely after a futility analysis due the low event rate identified by [an independent adjudication committee],” said Dr. Jolliet of the intensive care and burn unit at Le Centre Hospitalier Universitaire Vaudois (CHUV), in Lausanne, Switzerland, and his fellow researchers.
The study included 445 patients from ICUs or intermediate care units in six countries. The inclusion criteria were presenting with current COPD exacerbation with hypercapnic acute respiratory failure, a PaCO2 of at least 45 mm Hg, an arterial pH of less than or equal to 7.35, and at least one of the following: respiration rate of at least 25 breaths per minute, a PaO2 less than or equal to 50 mm Hg, and an arterial oxygen saturation of less than or equal to 90%.
Half of the patients in each group were already receiving NIV prior to enrollment in the study. Males constituted two thirds of all enrolled patients.
HeO2 administration was limited to 72 hours for each patient and about a third of NIV failures occurred after the end of the HeO2 administration, the researchers said.
“The main reason for the absence of observed benefit on outcome in the He/O2 probably lies in the very low NIV failure rate now observed in both groups. One possible mechanism explaining the low intubation rate could be that some patients had received uncontrolled oxygen therapy prior to ICU admission, thereby worsening initial hypercapnia and acidosis, a problem that can easily be corrected by adequate titration,” the researchers said. “The 14.5% failure rate in the Air/O2 group was much lower than the 25% rate used in designing the study,” which was based on previous research.
The trial’s sponsor, Air Liquide Healthcare, provided input into the design and conduct of the study; oversaw the collection, management, and statistical analysis of data; and contributed to the manuscript’s preparation and review.
FROM AJRCCM
Key clinical point: .
Major finding: The trial was stopped prematurely due to a low event rate. The NIV failure rates for patients who received Air/O2 and He/O2 were 14.5% (N = 32) and 14.7% ( N = 33, P = .97), respectively.
Data source: A prospective, open-label, randomized, controlled trial of 445 patients.
Disclosures: Air Liquide Healthcare sponsored and contributed to the study.
Comorbidities common in COPD patients
LOS ANGELES – Comorbidities are common in patients with chronic obstructive pulmonary disease, especially cardiovascular disease, diabetes, anemia, and osteoporosis, results from a single-center analysis showed.
“These affect the course and outcome of COPD, so identification and treatment of these comorbidities is very important,” Hamdy Mohammadien, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians.
In an effort to estimate the presence of comorbidities in patients with COPD and to assess the relationship of comorbid diseases with age, sex, C-reactive protein, and COPD severity, Dr. Mohammadien and his associates at Sohag (Egypt) University, retrospectively evaluated 400 COPD patients who were at least 40 years of age. Those who presented with bronchial asthma or other lung diseases were excluded from the analysis. The mean age of patients was 62 years, 69% were male, and 36% were current smokers. Their mean FEV1/FVC ratio (forced expiratory volume in 1 second/forced vital capacity) was 48%, and 57% had two or more exacerbations in the previous year.
Dr. Mohammadien reported that all patients had at least one comorbidity. The most common comorbidities were cardiovascular diseases (85%), diabetes (35%), dyslipidemia (23%), osteopenia (11%), anemia (10%), muscle wasting (9%), pneumonia (7%), osteoporosis (6%), GERD (2%), and lung cancer (2%). He also noted that the association between cardiovascular events, dyslipidemia, diabetes, osteoporosis, muscle wasting, and anemia was highly significant in COPD patients aged 60 years and older, in men, and in patients with stage III and IV COPD. In addition, a significant relationship was observed between a positive CRP level and each comorbidity, with the exception of gastroesophageal reflux disease and lung cancer. The three comorbidities with the greatest significance were ischemic heart disease (P = .0001), dyslipidemia (P = .0001), and pneumonia (P = .0003). Finally, frequent exacerbators were significantly more likely to have two or more comorbidities (odds ratio 2; P = .04) and to have more hospitalizations in the past year (P less than .01).
“Comorbidities are common in patients with COPD, and have a significant impact on health status and prognosis, thus justifying the need for a comprehensive and integrating therapeutic approach,” Dr. Mohammadien said at the meeting. “In the management of COPD all these conditions need to be carefully evaluated and treated.”
He acknowledged certain limitations of the study, including its relatively small sample size and the fact that bone density was measured by sonar and not by dual-energy x-ray absorptiometry. Dr. Mohammadien reported having no financial disclosures.
LOS ANGELES – Comorbidities are common in patients with chronic obstructive pulmonary disease, especially cardiovascular disease, diabetes, anemia, and osteoporosis, results from a single-center analysis showed.
“These affect the course and outcome of COPD, so identification and treatment of these comorbidities is very important,” Hamdy Mohammadien, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians.
In an effort to estimate the presence of comorbidities in patients with COPD and to assess the relationship of comorbid diseases with age, sex, C-reactive protein, and COPD severity, Dr. Mohammadien and his associates at Sohag (Egypt) University, retrospectively evaluated 400 COPD patients who were at least 40 years of age. Those who presented with bronchial asthma or other lung diseases were excluded from the analysis. The mean age of patients was 62 years, 69% were male, and 36% were current smokers. Their mean FEV1/FVC ratio (forced expiratory volume in 1 second/forced vital capacity) was 48%, and 57% had two or more exacerbations in the previous year.
Dr. Mohammadien reported that all patients had at least one comorbidity. The most common comorbidities were cardiovascular diseases (85%), diabetes (35%), dyslipidemia (23%), osteopenia (11%), anemia (10%), muscle wasting (9%), pneumonia (7%), osteoporosis (6%), GERD (2%), and lung cancer (2%). He also noted that the association between cardiovascular events, dyslipidemia, diabetes, osteoporosis, muscle wasting, and anemia was highly significant in COPD patients aged 60 years and older, in men, and in patients with stage III and IV COPD. In addition, a significant relationship was observed between a positive CRP level and each comorbidity, with the exception of gastroesophageal reflux disease and lung cancer. The three comorbidities with the greatest significance were ischemic heart disease (P = .0001), dyslipidemia (P = .0001), and pneumonia (P = .0003). Finally, frequent exacerbators were significantly more likely to have two or more comorbidities (odds ratio 2; P = .04) and to have more hospitalizations in the past year (P less than .01).
“Comorbidities are common in patients with COPD, and have a significant impact on health status and prognosis, thus justifying the need for a comprehensive and integrating therapeutic approach,” Dr. Mohammadien said at the meeting. “In the management of COPD all these conditions need to be carefully evaluated and treated.”
He acknowledged certain limitations of the study, including its relatively small sample size and the fact that bone density was measured by sonar and not by dual-energy x-ray absorptiometry. Dr. Mohammadien reported having no financial disclosures.
LOS ANGELES – Comorbidities are common in patients with chronic obstructive pulmonary disease, especially cardiovascular disease, diabetes, anemia, and osteoporosis, results from a single-center analysis showed.
“These affect the course and outcome of COPD, so identification and treatment of these comorbidities is very important,” Hamdy Mohammadien, MD, said in an interview in advance of the annual meeting of the American College of Chest Physicians.
In an effort to estimate the presence of comorbidities in patients with COPD and to assess the relationship of comorbid diseases with age, sex, C-reactive protein, and COPD severity, Dr. Mohammadien and his associates at Sohag (Egypt) University, retrospectively evaluated 400 COPD patients who were at least 40 years of age. Those who presented with bronchial asthma or other lung diseases were excluded from the analysis. The mean age of patients was 62 years, 69% were male, and 36% were current smokers. Their mean FEV1/FVC ratio (forced expiratory volume in 1 second/forced vital capacity) was 48%, and 57% had two or more exacerbations in the previous year.
Dr. Mohammadien reported that all patients had at least one comorbidity. The most common comorbidities were cardiovascular diseases (85%), diabetes (35%), dyslipidemia (23%), osteopenia (11%), anemia (10%), muscle wasting (9%), pneumonia (7%), osteoporosis (6%), GERD (2%), and lung cancer (2%). He also noted that the association between cardiovascular events, dyslipidemia, diabetes, osteoporosis, muscle wasting, and anemia was highly significant in COPD patients aged 60 years and older, in men, and in patients with stage III and IV COPD. In addition, a significant relationship was observed between a positive CRP level and each comorbidity, with the exception of gastroesophageal reflux disease and lung cancer. The three comorbidities with the greatest significance were ischemic heart disease (P = .0001), dyslipidemia (P = .0001), and pneumonia (P = .0003). Finally, frequent exacerbators were significantly more likely to have two or more comorbidities (odds ratio 2; P = .04) and to have more hospitalizations in the past year (P less than .01).
“Comorbidities are common in patients with COPD, and have a significant impact on health status and prognosis, thus justifying the need for a comprehensive and integrating therapeutic approach,” Dr. Mohammadien said at the meeting. “In the management of COPD all these conditions need to be carefully evaluated and treated.”
He acknowledged certain limitations of the study, including its relatively small sample size and the fact that bone density was measured by sonar and not by dual-energy x-ray absorptiometry. Dr. Mohammadien reported having no financial disclosures.
AT CHEST 2016
Key clinical point:
Major finding: The three most common comorbidities in COPD patients were cardiovascular diseases (85%), diabetes (35%), and dyslipidemia (23%).
Data source: A retrospective study of 400 patients with COPD.
Disclosures: Dr. Mohammadien reported having no financial disclosures.