User login
News and Views that Matter to Physicians
Employer-provided insurance stable after ACA implementation
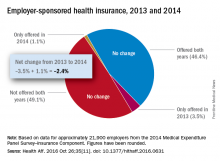
Concerns that Affordable Care Act (ACA) provisions implemented in 2014 would lead large numbers of employers to drop health insurance coverage appear to have been unfounded, according to a study published in the journal Health Affairs.
More than 95% of employers did not change their insurance coverage policy between 2013 and 2014: 46.4% offered coverage in 2013 and continued it in 2014 and 49.1% did not offer coverage either year. Of the 21,900 private-sector employers included in the analysis, 3.5% provided coverage in 2013 but not in 2014 and 1.1% did not offer it in 2013 but did in 2014, reported Jean Abraham, PhD, of the University of Minnesota, Minneapolis, and her associates (Health Aff. 2016 Oct 26;35[11]. doi: 10.1377/hlthaff.2016.0631).
The analysis of data from the 2014 Medical Expenditure Panel Survey–Insurance Component, however, did show associations between coverage changes and several workforce and employer characteristics. “Small firms were more likely to drop coverage compared to large ones, as were those with more low-wage workers compared to those with fewer such workers, newer establishments compared to older ones, and those in the service sector compared to those in blue- and white-collar industries,” Dr. Abraham and her associates wrote.
The Robert Wood Johnson Foundation’s State Health Access Reform Evaluation program supported the study. No other financial disclosures were provided.
Concerns that Affordable Care Act (ACA) provisions implemented in 2014 would lead large numbers of employers to drop health insurance coverage appear to have been unfounded, according to a study published in the journal Health Affairs.
More than 95% of employers did not change their insurance coverage policy between 2013 and 2014: 46.4% offered coverage in 2013 and continued it in 2014 and 49.1% did not offer coverage either year. Of the 21,900 private-sector employers included in the analysis, 3.5% provided coverage in 2013 but not in 2014 and 1.1% did not offer it in 2013 but did in 2014, reported Jean Abraham, PhD, of the University of Minnesota, Minneapolis, and her associates (Health Aff. 2016 Oct 26;35[11]. doi: 10.1377/hlthaff.2016.0631).
The analysis of data from the 2014 Medical Expenditure Panel Survey–Insurance Component, however, did show associations between coverage changes and several workforce and employer characteristics. “Small firms were more likely to drop coverage compared to large ones, as were those with more low-wage workers compared to those with fewer such workers, newer establishments compared to older ones, and those in the service sector compared to those in blue- and white-collar industries,” Dr. Abraham and her associates wrote.
The Robert Wood Johnson Foundation’s State Health Access Reform Evaluation program supported the study. No other financial disclosures were provided.
Concerns that Affordable Care Act (ACA) provisions implemented in 2014 would lead large numbers of employers to drop health insurance coverage appear to have been unfounded, according to a study published in the journal Health Affairs.
More than 95% of employers did not change their insurance coverage policy between 2013 and 2014: 46.4% offered coverage in 2013 and continued it in 2014 and 49.1% did not offer coverage either year. Of the 21,900 private-sector employers included in the analysis, 3.5% provided coverage in 2013 but not in 2014 and 1.1% did not offer it in 2013 but did in 2014, reported Jean Abraham, PhD, of the University of Minnesota, Minneapolis, and her associates (Health Aff. 2016 Oct 26;35[11]. doi: 10.1377/hlthaff.2016.0631).
The analysis of data from the 2014 Medical Expenditure Panel Survey–Insurance Component, however, did show associations between coverage changes and several workforce and employer characteristics. “Small firms were more likely to drop coverage compared to large ones, as were those with more low-wage workers compared to those with fewer such workers, newer establishments compared to older ones, and those in the service sector compared to those in blue- and white-collar industries,” Dr. Abraham and her associates wrote.
The Robert Wood Johnson Foundation’s State Health Access Reform Evaluation program supported the study. No other financial disclosures were provided.
Number of Medicare part D drug plans continues to decline
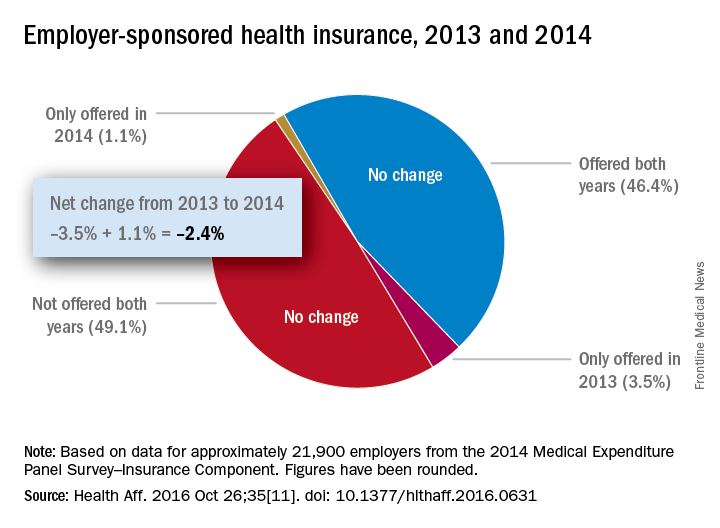
There will be 16% fewer Medicare part D prescription drug plans available in 2017, compared with 2016, according to an analysis by the Kaiser Family Foundation.
In 2017, there will be 746 stand-alone prescription drug plans available to Medicare beneficiaries in the 50 states and the District of Columbia, which is 140 (16%) less than were available in 2016 and 1,129 (60%) less than the peak in 2007, Kaiser reported.
Of the nearly 41 million people enrolled in Medicare part D plans in 2016, about 12 million receive the low-income subsidy. The Congressional Budget Office estimates that spending on part D benefits will be $94 billion in 2017, which is 15.6% of overall Medicare costs. Medicare actuaries have projected that the cost per enrollee will increase by 5.8% annually from 2015 to 2025, Kaiser reported.
There will be 16% fewer Medicare part D prescription drug plans available in 2017, compared with 2016, according to an analysis by the Kaiser Family Foundation.
In 2017, there will be 746 stand-alone prescription drug plans available to Medicare beneficiaries in the 50 states and the District of Columbia, which is 140 (16%) less than were available in 2016 and 1,129 (60%) less than the peak in 2007, Kaiser reported.
Of the nearly 41 million people enrolled in Medicare part D plans in 2016, about 12 million receive the low-income subsidy. The Congressional Budget Office estimates that spending on part D benefits will be $94 billion in 2017, which is 15.6% of overall Medicare costs. Medicare actuaries have projected that the cost per enrollee will increase by 5.8% annually from 2015 to 2025, Kaiser reported.
There will be 16% fewer Medicare part D prescription drug plans available in 2017, compared with 2016, according to an analysis by the Kaiser Family Foundation.
In 2017, there will be 746 stand-alone prescription drug plans available to Medicare beneficiaries in the 50 states and the District of Columbia, which is 140 (16%) less than were available in 2016 and 1,129 (60%) less than the peak in 2007, Kaiser reported.
Of the nearly 41 million people enrolled in Medicare part D plans in 2016, about 12 million receive the low-income subsidy. The Congressional Budget Office estimates that spending on part D benefits will be $94 billion in 2017, which is 15.6% of overall Medicare costs. Medicare actuaries have projected that the cost per enrollee will increase by 5.8% annually from 2015 to 2025, Kaiser reported.
7 tips for successful value-based care contracts
During a recent webinar presented by the American Bar Association, legal experts provided guidance on how doctors can successfully draft pay-for-performance contracts and prevent disputes with payers.
1. Clearly define terms
Contract terms and definitions should be clearly outlined and understood by both parties before value-based agreements are signed, said Melissa J. Hulke, a director in the Berkeley Research Group, LLC health analytics practice.
“Contract terms become central to resolving differences, so it’s important the contract is well defined, especially when moving away from fee for service,” she said. “These are more complex arrangements.”
Another area that needs thorough definition surrounds referral volume. Contracts can include the phrases, “predominately refer” or “primarily refer,” without defining the meaning of “predominately” or “primarily,” Ms. Hulke said.
“If that’s not defined in the contract, it’s hard to establish a benchmark to not only project the provider’s performance under the arrangement and how much revenue they can expect to receive, but it’s hard to know if you’re meeting that benchmark, as well,” she said. “I strongly encourage that if [a term states] “primarily, predominately, [or] mostly refer,” that you have a specific percentage benchmark included. That will help to avoid any disagreement later on.”
2. Review payment calculations
Ensure that payment formulas are examined and agreed upon.
“I think that should be baked into the contracts of today because they are so complex and there is so much money at stake,” she said. “Walk through that compensation exhibit, walk through the examples of what’s supposed to happen.
If not in agreement with calculations, talk to the payer’s financial personnel about how the numbers were reached and try to resolve any differences.
3. Monitor results
Actively monitor projected-to-actual financial performance under the contract. If performance is not being monitored and results are not being tested, it’s impossible to tell whether the contract is succeeding or failing, Ms. Hulke said.
It’s a good idea to monitor projected-to-actual financial performance monthly or at least quarterly, she advised.
“Tracking budget to actual performance and investigating successes and failures are important if the contracts are material to the provider’s business,” Ms. Hulke said.
4. Institute time frames for government methodologies
Be specific about when contracts are linked to Medicare reimbursement methodologies.
If commercial payers are tying payment rates to government programs, which often occurs, contracts should include whether the reimbursement is based on Medicare rates and methodologies as of a particular date and time, according to Ms. Hulke. For instance, the contract could specify that rates are tied to Medicare methodologies at the time the contract was executed. Alternatively, contracts could allow the physician payment rate to fluctuate depending on changes the government makes to Medicare rates and methodologies during the span of the contract.
“If this is not defined, when Medicare makes a change, the parties may have differing opinions on the appropriate rate of reimbursement that’s being paid,” she said.
5. Structure around state and federal laws
Conduct a regulatory analysis before inking any value based payment arrangement/transaction, and structure and document around potential legal constraints, Ms. Hanna said.
Know the laws in your state, she advised. Some states have requirements for provider incentive programs, while others may have rules for provider organizations or intermediaries that assume certain financial risk. When working with federal health care payers, review the Stark Law and Anti-Kickback regulations and ensure that if triggered by the arrangement, the venture falls within an exception of the statutes. Other legal considerations when drafting contracts include:
• HIPAA and state privacy laws.
• Antitrust laws.
• Telemedicine and telehealth laws.
• Medicare Advantage benefit guidelines for programs designed for specific Medicare Advantage populations.
• Scope of practice laws applicable to mid-level medical providers.
6. Design a dispute-resolution strategy
Include a thorough dispute-resolution strategy within the contract. The strategies help facilitate an orderly process for resolving disputes cost effectively, Ms. Hanna said. She suggested that policies start with an informal dispute-resolution process that sends unresolved matters to senior executives at each organization.
“This allows business leaders – and not the lawyers – to find a business solution to a thorny and potentially costly problem before each party gets entrenched in its own position and own sense of having been wronged,” she said in an interview. “The business solution may or may not rely on contract language but may be tailored to keep the relationship moving forward. However, if the informal process proves unsuccessful, then the process gets punted to the legal system – whether in a court proceeding or arbitration.”
7. Have an exit strategy
Include an exit strategy that ensures an end to the arrangement goes as smoothly and fairly as possible. The strategy will depend on the nature and structure of the payer-provider alignment and the value-based payment arrangement, Ms. Hanna said in an interview.
For example, in a true, corporate joint venture, the exit strategy may include buyout rights of the newly formed entity. In this case, it’s important to consider and negotiate the price of the buyout and what circumstances that will trigger the buyout. Termination rights should also be included in an exit strategy, Ms. Hanna said. One option is to allow termination “without case,” by either party.
“Clients often do not like this approach because the intention of the parties going in is to build a strong, long-term relationship where provider and payer benefit,” she said. “A ‘without cause’ termination rights gives the parties a safety valve if circumstances change or the relationship is just not successful.”
An alternative is to allow the relationship time to mature and grow before either party can exercise a without cause termination. A related approach is to develop triggering events that would give one or both parties the right to terminate the agreement, without the other party “having committed a bad act,” Ms. Hanna said in the interview.
“For instance, if the relationship does not meet certain financial or other benchmarks within an agreed-upon time frame, this may be a sufficient reason to terminate the relationship, abandon, or renegotiate the value-based purchasing payment formula or, perhaps, end an exclusive or other preferential relationship,” she said.
[email protected]
On Twitter @legal_med
During a recent webinar presented by the American Bar Association, legal experts provided guidance on how doctors can successfully draft pay-for-performance contracts and prevent disputes with payers.
1. Clearly define terms
Contract terms and definitions should be clearly outlined and understood by both parties before value-based agreements are signed, said Melissa J. Hulke, a director in the Berkeley Research Group, LLC health analytics practice.
“Contract terms become central to resolving differences, so it’s important the contract is well defined, especially when moving away from fee for service,” she said. “These are more complex arrangements.”
Another area that needs thorough definition surrounds referral volume. Contracts can include the phrases, “predominately refer” or “primarily refer,” without defining the meaning of “predominately” or “primarily,” Ms. Hulke said.
“If that’s not defined in the contract, it’s hard to establish a benchmark to not only project the provider’s performance under the arrangement and how much revenue they can expect to receive, but it’s hard to know if you’re meeting that benchmark, as well,” she said. “I strongly encourage that if [a term states] “primarily, predominately, [or] mostly refer,” that you have a specific percentage benchmark included. That will help to avoid any disagreement later on.”
2. Review payment calculations
Ensure that payment formulas are examined and agreed upon.
“I think that should be baked into the contracts of today because they are so complex and there is so much money at stake,” she said. “Walk through that compensation exhibit, walk through the examples of what’s supposed to happen.
If not in agreement with calculations, talk to the payer’s financial personnel about how the numbers were reached and try to resolve any differences.
3. Monitor results
Actively monitor projected-to-actual financial performance under the contract. If performance is not being monitored and results are not being tested, it’s impossible to tell whether the contract is succeeding or failing, Ms. Hulke said.
It’s a good idea to monitor projected-to-actual financial performance monthly or at least quarterly, she advised.
“Tracking budget to actual performance and investigating successes and failures are important if the contracts are material to the provider’s business,” Ms. Hulke said.
4. Institute time frames for government methodologies
Be specific about when contracts are linked to Medicare reimbursement methodologies.
If commercial payers are tying payment rates to government programs, which often occurs, contracts should include whether the reimbursement is based on Medicare rates and methodologies as of a particular date and time, according to Ms. Hulke. For instance, the contract could specify that rates are tied to Medicare methodologies at the time the contract was executed. Alternatively, contracts could allow the physician payment rate to fluctuate depending on changes the government makes to Medicare rates and methodologies during the span of the contract.
“If this is not defined, when Medicare makes a change, the parties may have differing opinions on the appropriate rate of reimbursement that’s being paid,” she said.
5. Structure around state and federal laws
Conduct a regulatory analysis before inking any value based payment arrangement/transaction, and structure and document around potential legal constraints, Ms. Hanna said.
Know the laws in your state, she advised. Some states have requirements for provider incentive programs, while others may have rules for provider organizations or intermediaries that assume certain financial risk. When working with federal health care payers, review the Stark Law and Anti-Kickback regulations and ensure that if triggered by the arrangement, the venture falls within an exception of the statutes. Other legal considerations when drafting contracts include:
• HIPAA and state privacy laws.
• Antitrust laws.
• Telemedicine and telehealth laws.
• Medicare Advantage benefit guidelines for programs designed for specific Medicare Advantage populations.
• Scope of practice laws applicable to mid-level medical providers.
6. Design a dispute-resolution strategy
Include a thorough dispute-resolution strategy within the contract. The strategies help facilitate an orderly process for resolving disputes cost effectively, Ms. Hanna said. She suggested that policies start with an informal dispute-resolution process that sends unresolved matters to senior executives at each organization.
“This allows business leaders – and not the lawyers – to find a business solution to a thorny and potentially costly problem before each party gets entrenched in its own position and own sense of having been wronged,” she said in an interview. “The business solution may or may not rely on contract language but may be tailored to keep the relationship moving forward. However, if the informal process proves unsuccessful, then the process gets punted to the legal system – whether in a court proceeding or arbitration.”
7. Have an exit strategy
Include an exit strategy that ensures an end to the arrangement goes as smoothly and fairly as possible. The strategy will depend on the nature and structure of the payer-provider alignment and the value-based payment arrangement, Ms. Hanna said in an interview.
For example, in a true, corporate joint venture, the exit strategy may include buyout rights of the newly formed entity. In this case, it’s important to consider and negotiate the price of the buyout and what circumstances that will trigger the buyout. Termination rights should also be included in an exit strategy, Ms. Hanna said. One option is to allow termination “without case,” by either party.
“Clients often do not like this approach because the intention of the parties going in is to build a strong, long-term relationship where provider and payer benefit,” she said. “A ‘without cause’ termination rights gives the parties a safety valve if circumstances change or the relationship is just not successful.”
An alternative is to allow the relationship time to mature and grow before either party can exercise a without cause termination. A related approach is to develop triggering events that would give one or both parties the right to terminate the agreement, without the other party “having committed a bad act,” Ms. Hanna said in the interview.
“For instance, if the relationship does not meet certain financial or other benchmarks within an agreed-upon time frame, this may be a sufficient reason to terminate the relationship, abandon, or renegotiate the value-based purchasing payment formula or, perhaps, end an exclusive or other preferential relationship,” she said.
[email protected]
On Twitter @legal_med
During a recent webinar presented by the American Bar Association, legal experts provided guidance on how doctors can successfully draft pay-for-performance contracts and prevent disputes with payers.
1. Clearly define terms
Contract terms and definitions should be clearly outlined and understood by both parties before value-based agreements are signed, said Melissa J. Hulke, a director in the Berkeley Research Group, LLC health analytics practice.
“Contract terms become central to resolving differences, so it’s important the contract is well defined, especially when moving away from fee for service,” she said. “These are more complex arrangements.”
Another area that needs thorough definition surrounds referral volume. Contracts can include the phrases, “predominately refer” or “primarily refer,” without defining the meaning of “predominately” or “primarily,” Ms. Hulke said.
“If that’s not defined in the contract, it’s hard to establish a benchmark to not only project the provider’s performance under the arrangement and how much revenue they can expect to receive, but it’s hard to know if you’re meeting that benchmark, as well,” she said. “I strongly encourage that if [a term states] “primarily, predominately, [or] mostly refer,” that you have a specific percentage benchmark included. That will help to avoid any disagreement later on.”
2. Review payment calculations
Ensure that payment formulas are examined and agreed upon.
“I think that should be baked into the contracts of today because they are so complex and there is so much money at stake,” she said. “Walk through that compensation exhibit, walk through the examples of what’s supposed to happen.
If not in agreement with calculations, talk to the payer’s financial personnel about how the numbers were reached and try to resolve any differences.
3. Monitor results
Actively monitor projected-to-actual financial performance under the contract. If performance is not being monitored and results are not being tested, it’s impossible to tell whether the contract is succeeding or failing, Ms. Hulke said.
It’s a good idea to monitor projected-to-actual financial performance monthly or at least quarterly, she advised.
“Tracking budget to actual performance and investigating successes and failures are important if the contracts are material to the provider’s business,” Ms. Hulke said.
4. Institute time frames for government methodologies
Be specific about when contracts are linked to Medicare reimbursement methodologies.
If commercial payers are tying payment rates to government programs, which often occurs, contracts should include whether the reimbursement is based on Medicare rates and methodologies as of a particular date and time, according to Ms. Hulke. For instance, the contract could specify that rates are tied to Medicare methodologies at the time the contract was executed. Alternatively, contracts could allow the physician payment rate to fluctuate depending on changes the government makes to Medicare rates and methodologies during the span of the contract.
“If this is not defined, when Medicare makes a change, the parties may have differing opinions on the appropriate rate of reimbursement that’s being paid,” she said.
5. Structure around state and federal laws
Conduct a regulatory analysis before inking any value based payment arrangement/transaction, and structure and document around potential legal constraints, Ms. Hanna said.
Know the laws in your state, she advised. Some states have requirements for provider incentive programs, while others may have rules for provider organizations or intermediaries that assume certain financial risk. When working with federal health care payers, review the Stark Law and Anti-Kickback regulations and ensure that if triggered by the arrangement, the venture falls within an exception of the statutes. Other legal considerations when drafting contracts include:
• HIPAA and state privacy laws.
• Antitrust laws.
• Telemedicine and telehealth laws.
• Medicare Advantage benefit guidelines for programs designed for specific Medicare Advantage populations.
• Scope of practice laws applicable to mid-level medical providers.
6. Design a dispute-resolution strategy
Include a thorough dispute-resolution strategy within the contract. The strategies help facilitate an orderly process for resolving disputes cost effectively, Ms. Hanna said. She suggested that policies start with an informal dispute-resolution process that sends unresolved matters to senior executives at each organization.
“This allows business leaders – and not the lawyers – to find a business solution to a thorny and potentially costly problem before each party gets entrenched in its own position and own sense of having been wronged,” she said in an interview. “The business solution may or may not rely on contract language but may be tailored to keep the relationship moving forward. However, if the informal process proves unsuccessful, then the process gets punted to the legal system – whether in a court proceeding or arbitration.”
7. Have an exit strategy
Include an exit strategy that ensures an end to the arrangement goes as smoothly and fairly as possible. The strategy will depend on the nature and structure of the payer-provider alignment and the value-based payment arrangement, Ms. Hanna said in an interview.
For example, in a true, corporate joint venture, the exit strategy may include buyout rights of the newly formed entity. In this case, it’s important to consider and negotiate the price of the buyout and what circumstances that will trigger the buyout. Termination rights should also be included in an exit strategy, Ms. Hanna said. One option is to allow termination “without case,” by either party.
“Clients often do not like this approach because the intention of the parties going in is to build a strong, long-term relationship where provider and payer benefit,” she said. “A ‘without cause’ termination rights gives the parties a safety valve if circumstances change or the relationship is just not successful.”
An alternative is to allow the relationship time to mature and grow before either party can exercise a without cause termination. A related approach is to develop triggering events that would give one or both parties the right to terminate the agreement, without the other party “having committed a bad act,” Ms. Hanna said in the interview.
“For instance, if the relationship does not meet certain financial or other benchmarks within an agreed-upon time frame, this may be a sufficient reason to terminate the relationship, abandon, or renegotiate the value-based purchasing payment formula or, perhaps, end an exclusive or other preferential relationship,” she said.
[email protected]
On Twitter @legal_med
Fatal measles complication occurs more often than realized
NEW ORLEANS – A fatal complication of measles known as subacute sclerosing panencephalitis (SSPE) can develop years after measles infection and appears to occur much more often than published reports suggest, according to a review of cases in California from 1998 to 2015.
The findings underscore the vital importance of herd immunity by vaccination, Kristen Wendorf, MD, reported at an annual scientific meeting on infectious diseases.
The incidence of postmeasles SSPE was previously thought be about 1 in 100,000, according to an IDWeek press release.
“There is no cure for SSPE, and the only way to prevent it is to vaccinate everyone against measles,” the release stated.
The cases in the current study were among children with a clinically compatible illness, and either measles IgG antibody detected in cerebrospinal fluid, a characteristic pattern on electroencephalography, typical histologic findings on brain biopsy, or medical record documentation of SSPE-related complications. They were identified based on death certificates, reports from the Centers for Diseases Control and Prevention, or through investigations for undiagnosed neurologic disease. Twelve of the 17 affected children had a clinical history of a febrile rash illness compatible with measles, and all 12 of those experienced illness before age 15 months and before measles vaccination.
Most (67%) were living in the United States when they had measles, Dr. Wendorf said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The median age at diagnosis of SSPE was 12 years, although the range was 3-35 years, and the mean latency period was 9.5 years. In many cases, long-standing cognitive or motor problems were experienced prior to diagnosis, she noted.
The findings suggest that SSPE is more common than previously recognized in unvaccinated children with measles during infancy, Dr. Wendorf said.
Protection of infants younger than 12-15 months of age – before the time when measles vaccine is routinely administered – and in those who can’t be vaccinated because of immune system disorders requires avoidance of travel to endemic areas. Parents also may consider early vaccination prior to such travel.
Further, clinicians should be aware of the risk of SSPE in patients with symptoms suggestive of the disease. This is true even among older patients in whom no specific history of measles infection is known, she said.
In the press release, coauthor James D. Cherry, MD, professor of pediatrics at the University of California, Los Angeles, further stressed the importance of protecting unvaccinated infants.
“Parents of infants who have not yet been vaccinated should avoid putting their children at risk. For example, they should postpone trips overseas – including to Europe – where measles is endemic and epidemic until after their baby has been vaccinated with two doses,” he said. “It’s just not worth the risk.”
The authors reported having no disclosures.
NEW ORLEANS – A fatal complication of measles known as subacute sclerosing panencephalitis (SSPE) can develop years after measles infection and appears to occur much more often than published reports suggest, according to a review of cases in California from 1998 to 2015.
The findings underscore the vital importance of herd immunity by vaccination, Kristen Wendorf, MD, reported at an annual scientific meeting on infectious diseases.
The incidence of postmeasles SSPE was previously thought be about 1 in 100,000, according to an IDWeek press release.
“There is no cure for SSPE, and the only way to prevent it is to vaccinate everyone against measles,” the release stated.
The cases in the current study were among children with a clinically compatible illness, and either measles IgG antibody detected in cerebrospinal fluid, a characteristic pattern on electroencephalography, typical histologic findings on brain biopsy, or medical record documentation of SSPE-related complications. They were identified based on death certificates, reports from the Centers for Diseases Control and Prevention, or through investigations for undiagnosed neurologic disease. Twelve of the 17 affected children had a clinical history of a febrile rash illness compatible with measles, and all 12 of those experienced illness before age 15 months and before measles vaccination.
Most (67%) were living in the United States when they had measles, Dr. Wendorf said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The median age at diagnosis of SSPE was 12 years, although the range was 3-35 years, and the mean latency period was 9.5 years. In many cases, long-standing cognitive or motor problems were experienced prior to diagnosis, she noted.
The findings suggest that SSPE is more common than previously recognized in unvaccinated children with measles during infancy, Dr. Wendorf said.
Protection of infants younger than 12-15 months of age – before the time when measles vaccine is routinely administered – and in those who can’t be vaccinated because of immune system disorders requires avoidance of travel to endemic areas. Parents also may consider early vaccination prior to such travel.
Further, clinicians should be aware of the risk of SSPE in patients with symptoms suggestive of the disease. This is true even among older patients in whom no specific history of measles infection is known, she said.
In the press release, coauthor James D. Cherry, MD, professor of pediatrics at the University of California, Los Angeles, further stressed the importance of protecting unvaccinated infants.
“Parents of infants who have not yet been vaccinated should avoid putting their children at risk. For example, they should postpone trips overseas – including to Europe – where measles is endemic and epidemic until after their baby has been vaccinated with two doses,” he said. “It’s just not worth the risk.”
The authors reported having no disclosures.
NEW ORLEANS – A fatal complication of measles known as subacute sclerosing panencephalitis (SSPE) can develop years after measles infection and appears to occur much more often than published reports suggest, according to a review of cases in California from 1998 to 2015.
The findings underscore the vital importance of herd immunity by vaccination, Kristen Wendorf, MD, reported at an annual scientific meeting on infectious diseases.
The incidence of postmeasles SSPE was previously thought be about 1 in 100,000, according to an IDWeek press release.
“There is no cure for SSPE, and the only way to prevent it is to vaccinate everyone against measles,” the release stated.
The cases in the current study were among children with a clinically compatible illness, and either measles IgG antibody detected in cerebrospinal fluid, a characteristic pattern on electroencephalography, typical histologic findings on brain biopsy, or medical record documentation of SSPE-related complications. They were identified based on death certificates, reports from the Centers for Diseases Control and Prevention, or through investigations for undiagnosed neurologic disease. Twelve of the 17 affected children had a clinical history of a febrile rash illness compatible with measles, and all 12 of those experienced illness before age 15 months and before measles vaccination.
Most (67%) were living in the United States when they had measles, Dr. Wendorf said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The median age at diagnosis of SSPE was 12 years, although the range was 3-35 years, and the mean latency period was 9.5 years. In many cases, long-standing cognitive or motor problems were experienced prior to diagnosis, she noted.
The findings suggest that SSPE is more common than previously recognized in unvaccinated children with measles during infancy, Dr. Wendorf said.
Protection of infants younger than 12-15 months of age – before the time when measles vaccine is routinely administered – and in those who can’t be vaccinated because of immune system disorders requires avoidance of travel to endemic areas. Parents also may consider early vaccination prior to such travel.
Further, clinicians should be aware of the risk of SSPE in patients with symptoms suggestive of the disease. This is true even among older patients in whom no specific history of measles infection is known, she said.
In the press release, coauthor James D. Cherry, MD, professor of pediatrics at the University of California, Los Angeles, further stressed the importance of protecting unvaccinated infants.
“Parents of infants who have not yet been vaccinated should avoid putting their children at risk. For example, they should postpone trips overseas – including to Europe – where measles is endemic and epidemic until after their baby has been vaccinated with two doses,” he said. “It’s just not worth the risk.”
The authors reported having no disclosures.
AT IDWEEK 2016
Key clinical point:
Major finding: The incidence of SSPE among measles cases was 1 in 1,367 children under age 5 years and 1 in 609 children under age 12 months at the time of measles disease.
Data source: A review of records and 17 cases of SSPE.
Disclosures: The authors reported having no disclosures.
Staple line reinforcement linked to increased leak risk in bariatric surgery
Laparoscopic sleeve gastrectomy is safe and effective overall, but staple line reinforcement appears to increase the rate of postsurgical leaks – which were associated with readmissions and, in some cases, reoperations.
A large review of quality improvement data found that staple line reinforcement – an extremely common technique – was associated with a 60% increased risk of leak, compared with closures without staple line reinforcement, Elizabeth R. Berger, MD, and her colleagues reported in the October issue of the Annals of Surgery (2016;264:464-73).
“This study also demonstrates that leaks were significantly more morbid than bleeding with higher readmission and reoperation rates in patients with a leak vs. a bleed,” wrote Dr. Berger of Loyola University, Chicago, and her coauthors. “Therefore, a surgeon should consider the benefits, risks, and costs of each surgical technique in performing a laparoscopic sleeve gastrectomy and selectively utilize those that, in their hands, minimize morbidity while maximizing clinical effectiveness.”
The team examined outcomes in 189,477 laparoscopic sleeve gastrectomies performed by 1,634 surgeons at 720 centers from 2012 to 2014. All of the data were extracted from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, created in 2012 by the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery.
They examined the impact of staple line reinforcement, oversewing the staple line, bougie size, and distance of the staple line from the pylorus on 30-day outcomes, and their effect on weight loss and weight-related comorbidities at 1 year. Outcomes included morbidity, leak rates, and bleeding, which were examined at both the patient and surgeon levels.
Most patients (126,904; 67%) patients had some type of staple line reinforcement (SLR); the rest had only oversewn staple lines (OSL) or no reinforcement. Leaks occurred in 1,703 patients and bleeds in 1,436 patients. Leaks were more serious than bleeds: Patients with a leak were almost 28% more likely to readmitted and 11% more likely to need a reoperation than were patients who had only a bleed.
At the patient level, those with SLR with or without OSL were 20%-46% more likely to experience a leak than were those who had neither. Bleeding rates were about 70% lower in the SLR groups.
Most surgeons in the analysis (80%) used some type of SLR; almost 20% routinely used only OSL, and 30% routinely used only SLR. At the surgeon level, SLR was associated with a 60% increased risk of a postoperative leak, compared with no reinforcement. There was no association between SLR and bleeding risk, however.
Oversewing had an effect on 1-year weight loss. Patients with oversewn staple lines lost an additional 1.3 points on the body mass index (BMI) scale, compared with patients with no type of reinforcement.
“The reason for increased leaks from SLR is relatively unclear,” the authors wrote. “The two layers of material that are placed within the staple line could increase ischemia or decrease the relative staple heights. At the notches, where one staple firing ends and the next one begins, there is sandwiching of the two layers of staples and a combined four layers of SLR. This bulk may predispose to leaks.”
Larger bougie sizes (BS) seemed more beneficial than did smaller ones, in both the surgeon- and patient-level analyses. A BS of at least 38 French was associated with a 28% decreased risk of a leak (odds ratio 0.72) at the patient level and a 10% decreased risk at the surgeon level (OR 0.90). There were no associations with bleeding.
“Our findings support literature that describes narrower BSs leads to increased ischemia secondary to increased intraluminal pressure, causing more leaks,” the authors wrote.
A BS of at least 40 French had a significant impact on weight loss. At 1 year, patients with the larger BS had lost 2.45 points more on the BMI scale than did those with smaller sizes.
This finding is in accord with other studies, including one that found the best weight-loss outcomes associated with a BS of more than 60 French. “Perhaps the sleeve works because of more rapid emptying, which is favored by a relatively larger BS, rather than because of restriction,” they said.
The distance to the pylorus (DP) from the staple line initiation point was divided into four sections: less than 4 cm; 4-5 cm; 5-6 cm; and 6 cm or more.
On a patient level, there was no association between DP and leak rates. There was, however, an association with bleeding. A DP of 4-4.99 cm had the highest rate, 90%, while a DP of 5-5.99 cm had the lowest (71%). DP was also associated with weight loss on this level, with a distance of more than 6 cm being associated with the biggest BMI decrease (3.7 points).
“Our data show significantly increased excess weight loss in a stepwise fashion as the DP increases,” the authors said. “Our data suggest that as DP increased, there was an increased excess weight loss, possibly explained by preserving the ‘antral mill.’ Stapling further from the pylorus perhaps keeps the antrum’s functional component intact and allows food to enter the distal gut more quickly, leading to earlier satiety and increased weight loss.”
Only 114 surgeons (8%) used a DP of less than 4 cm. There were no significant associations with any 30-day outcomes and DP after adjustment.
The authors had no financial disclosures.
Before drawing overarching conclusions and implementing recommendations based on this study, there are several limitations that must be borne in mind when considering data-mining exercises such as this one:
• It should be taken into account that there was significant intraoperative variation in technique and experience among the surgeons that was not captured through the data acquisition.
• Similarly, the true distance between the stapler and the selected bougie is also variable, adding an inherent lack of accuracy of the true real diameter of the completed gastric tube.
• There is a lack of granular information, including the type of SLR or staplers used, thereby also limiting any reliable conclusions that could be drawn.
• There are additional techniques, such as omental buttressing, and the use of clips, sutures, or hemostatic agents that are not reported, yet may have an impact on leak and bleeding rates.
• The reported follow-up rate of 39.4% at 1 year is typically considered to be suboptimal.
• SLR techniques may also include oversewing, and these are also subject to wide variation, including the type of suture material used, and the actual suturing technique that was implemented.
• Only those patients whose bleeding was severe enough to warrant transfusions were included, such that lower level bleeding would have not been represented in this report.
• There were also deficiencies in correlating leaks or bleeding rates with staple height selection, or the experience and learning curve of the surgeon.
Samer Mattar, MD, is a bariatric surgeon and professor of surgery at Oregon Health and Science University, Portland. Dr. Mattar has no disclosures.
Before drawing overarching conclusions and implementing recommendations based on this study, there are several limitations that must be borne in mind when considering data-mining exercises such as this one:
• It should be taken into account that there was significant intraoperative variation in technique and experience among the surgeons that was not captured through the data acquisition.
• Similarly, the true distance between the stapler and the selected bougie is also variable, adding an inherent lack of accuracy of the true real diameter of the completed gastric tube.
• There is a lack of granular information, including the type of SLR or staplers used, thereby also limiting any reliable conclusions that could be drawn.
• There are additional techniques, such as omental buttressing, and the use of clips, sutures, or hemostatic agents that are not reported, yet may have an impact on leak and bleeding rates.
• The reported follow-up rate of 39.4% at 1 year is typically considered to be suboptimal.
• SLR techniques may also include oversewing, and these are also subject to wide variation, including the type of suture material used, and the actual suturing technique that was implemented.
• Only those patients whose bleeding was severe enough to warrant transfusions were included, such that lower level bleeding would have not been represented in this report.
• There were also deficiencies in correlating leaks or bleeding rates with staple height selection, or the experience and learning curve of the surgeon.
Samer Mattar, MD, is a bariatric surgeon and professor of surgery at Oregon Health and Science University, Portland. Dr. Mattar has no disclosures.
Before drawing overarching conclusions and implementing recommendations based on this study, there are several limitations that must be borne in mind when considering data-mining exercises such as this one:
• It should be taken into account that there was significant intraoperative variation in technique and experience among the surgeons that was not captured through the data acquisition.
• Similarly, the true distance between the stapler and the selected bougie is also variable, adding an inherent lack of accuracy of the true real diameter of the completed gastric tube.
• There is a lack of granular information, including the type of SLR or staplers used, thereby also limiting any reliable conclusions that could be drawn.
• There are additional techniques, such as omental buttressing, and the use of clips, sutures, or hemostatic agents that are not reported, yet may have an impact on leak and bleeding rates.
• The reported follow-up rate of 39.4% at 1 year is typically considered to be suboptimal.
• SLR techniques may also include oversewing, and these are also subject to wide variation, including the type of suture material used, and the actual suturing technique that was implemented.
• Only those patients whose bleeding was severe enough to warrant transfusions were included, such that lower level bleeding would have not been represented in this report.
• There were also deficiencies in correlating leaks or bleeding rates with staple height selection, or the experience and learning curve of the surgeon.
Samer Mattar, MD, is a bariatric surgeon and professor of surgery at Oregon Health and Science University, Portland. Dr. Mattar has no disclosures.
Laparoscopic sleeve gastrectomy is safe and effective overall, but staple line reinforcement appears to increase the rate of postsurgical leaks – which were associated with readmissions and, in some cases, reoperations.
A large review of quality improvement data found that staple line reinforcement – an extremely common technique – was associated with a 60% increased risk of leak, compared with closures without staple line reinforcement, Elizabeth R. Berger, MD, and her colleagues reported in the October issue of the Annals of Surgery (2016;264:464-73).
“This study also demonstrates that leaks were significantly more morbid than bleeding with higher readmission and reoperation rates in patients with a leak vs. a bleed,” wrote Dr. Berger of Loyola University, Chicago, and her coauthors. “Therefore, a surgeon should consider the benefits, risks, and costs of each surgical technique in performing a laparoscopic sleeve gastrectomy and selectively utilize those that, in their hands, minimize morbidity while maximizing clinical effectiveness.”
The team examined outcomes in 189,477 laparoscopic sleeve gastrectomies performed by 1,634 surgeons at 720 centers from 2012 to 2014. All of the data were extracted from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, created in 2012 by the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery.
They examined the impact of staple line reinforcement, oversewing the staple line, bougie size, and distance of the staple line from the pylorus on 30-day outcomes, and their effect on weight loss and weight-related comorbidities at 1 year. Outcomes included morbidity, leak rates, and bleeding, which were examined at both the patient and surgeon levels.
Most patients (126,904; 67%) patients had some type of staple line reinforcement (SLR); the rest had only oversewn staple lines (OSL) or no reinforcement. Leaks occurred in 1,703 patients and bleeds in 1,436 patients. Leaks were more serious than bleeds: Patients with a leak were almost 28% more likely to readmitted and 11% more likely to need a reoperation than were patients who had only a bleed.
At the patient level, those with SLR with or without OSL were 20%-46% more likely to experience a leak than were those who had neither. Bleeding rates were about 70% lower in the SLR groups.
Most surgeons in the analysis (80%) used some type of SLR; almost 20% routinely used only OSL, and 30% routinely used only SLR. At the surgeon level, SLR was associated with a 60% increased risk of a postoperative leak, compared with no reinforcement. There was no association between SLR and bleeding risk, however.
Oversewing had an effect on 1-year weight loss. Patients with oversewn staple lines lost an additional 1.3 points on the body mass index (BMI) scale, compared with patients with no type of reinforcement.
“The reason for increased leaks from SLR is relatively unclear,” the authors wrote. “The two layers of material that are placed within the staple line could increase ischemia or decrease the relative staple heights. At the notches, where one staple firing ends and the next one begins, there is sandwiching of the two layers of staples and a combined four layers of SLR. This bulk may predispose to leaks.”
Larger bougie sizes (BS) seemed more beneficial than did smaller ones, in both the surgeon- and patient-level analyses. A BS of at least 38 French was associated with a 28% decreased risk of a leak (odds ratio 0.72) at the patient level and a 10% decreased risk at the surgeon level (OR 0.90). There were no associations with bleeding.
“Our findings support literature that describes narrower BSs leads to increased ischemia secondary to increased intraluminal pressure, causing more leaks,” the authors wrote.
A BS of at least 40 French had a significant impact on weight loss. At 1 year, patients with the larger BS had lost 2.45 points more on the BMI scale than did those with smaller sizes.
This finding is in accord with other studies, including one that found the best weight-loss outcomes associated with a BS of more than 60 French. “Perhaps the sleeve works because of more rapid emptying, which is favored by a relatively larger BS, rather than because of restriction,” they said.
The distance to the pylorus (DP) from the staple line initiation point was divided into four sections: less than 4 cm; 4-5 cm; 5-6 cm; and 6 cm or more.
On a patient level, there was no association between DP and leak rates. There was, however, an association with bleeding. A DP of 4-4.99 cm had the highest rate, 90%, while a DP of 5-5.99 cm had the lowest (71%). DP was also associated with weight loss on this level, with a distance of more than 6 cm being associated with the biggest BMI decrease (3.7 points).
“Our data show significantly increased excess weight loss in a stepwise fashion as the DP increases,” the authors said. “Our data suggest that as DP increased, there was an increased excess weight loss, possibly explained by preserving the ‘antral mill.’ Stapling further from the pylorus perhaps keeps the antrum’s functional component intact and allows food to enter the distal gut more quickly, leading to earlier satiety and increased weight loss.”
Only 114 surgeons (8%) used a DP of less than 4 cm. There were no significant associations with any 30-day outcomes and DP after adjustment.
The authors had no financial disclosures.
Laparoscopic sleeve gastrectomy is safe and effective overall, but staple line reinforcement appears to increase the rate of postsurgical leaks – which were associated with readmissions and, in some cases, reoperations.
A large review of quality improvement data found that staple line reinforcement – an extremely common technique – was associated with a 60% increased risk of leak, compared with closures without staple line reinforcement, Elizabeth R. Berger, MD, and her colleagues reported in the October issue of the Annals of Surgery (2016;264:464-73).
“This study also demonstrates that leaks were significantly more morbid than bleeding with higher readmission and reoperation rates in patients with a leak vs. a bleed,” wrote Dr. Berger of Loyola University, Chicago, and her coauthors. “Therefore, a surgeon should consider the benefits, risks, and costs of each surgical technique in performing a laparoscopic sleeve gastrectomy and selectively utilize those that, in their hands, minimize morbidity while maximizing clinical effectiveness.”
The team examined outcomes in 189,477 laparoscopic sleeve gastrectomies performed by 1,634 surgeons at 720 centers from 2012 to 2014. All of the data were extracted from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, created in 2012 by the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery.
They examined the impact of staple line reinforcement, oversewing the staple line, bougie size, and distance of the staple line from the pylorus on 30-day outcomes, and their effect on weight loss and weight-related comorbidities at 1 year. Outcomes included morbidity, leak rates, and bleeding, which were examined at both the patient and surgeon levels.
Most patients (126,904; 67%) patients had some type of staple line reinforcement (SLR); the rest had only oversewn staple lines (OSL) or no reinforcement. Leaks occurred in 1,703 patients and bleeds in 1,436 patients. Leaks were more serious than bleeds: Patients with a leak were almost 28% more likely to readmitted and 11% more likely to need a reoperation than were patients who had only a bleed.
At the patient level, those with SLR with or without OSL were 20%-46% more likely to experience a leak than were those who had neither. Bleeding rates were about 70% lower in the SLR groups.
Most surgeons in the analysis (80%) used some type of SLR; almost 20% routinely used only OSL, and 30% routinely used only SLR. At the surgeon level, SLR was associated with a 60% increased risk of a postoperative leak, compared with no reinforcement. There was no association between SLR and bleeding risk, however.
Oversewing had an effect on 1-year weight loss. Patients with oversewn staple lines lost an additional 1.3 points on the body mass index (BMI) scale, compared with patients with no type of reinforcement.
“The reason for increased leaks from SLR is relatively unclear,” the authors wrote. “The two layers of material that are placed within the staple line could increase ischemia or decrease the relative staple heights. At the notches, where one staple firing ends and the next one begins, there is sandwiching of the two layers of staples and a combined four layers of SLR. This bulk may predispose to leaks.”
Larger bougie sizes (BS) seemed more beneficial than did smaller ones, in both the surgeon- and patient-level analyses. A BS of at least 38 French was associated with a 28% decreased risk of a leak (odds ratio 0.72) at the patient level and a 10% decreased risk at the surgeon level (OR 0.90). There were no associations with bleeding.
“Our findings support literature that describes narrower BSs leads to increased ischemia secondary to increased intraluminal pressure, causing more leaks,” the authors wrote.
A BS of at least 40 French had a significant impact on weight loss. At 1 year, patients with the larger BS had lost 2.45 points more on the BMI scale than did those with smaller sizes.
This finding is in accord with other studies, including one that found the best weight-loss outcomes associated with a BS of more than 60 French. “Perhaps the sleeve works because of more rapid emptying, which is favored by a relatively larger BS, rather than because of restriction,” they said.
The distance to the pylorus (DP) from the staple line initiation point was divided into four sections: less than 4 cm; 4-5 cm; 5-6 cm; and 6 cm or more.
On a patient level, there was no association between DP and leak rates. There was, however, an association with bleeding. A DP of 4-4.99 cm had the highest rate, 90%, while a DP of 5-5.99 cm had the lowest (71%). DP was also associated with weight loss on this level, with a distance of more than 6 cm being associated with the biggest BMI decrease (3.7 points).
“Our data show significantly increased excess weight loss in a stepwise fashion as the DP increases,” the authors said. “Our data suggest that as DP increased, there was an increased excess weight loss, possibly explained by preserving the ‘antral mill.’ Stapling further from the pylorus perhaps keeps the antrum’s functional component intact and allows food to enter the distal gut more quickly, leading to earlier satiety and increased weight loss.”
Only 114 surgeons (8%) used a DP of less than 4 cm. There were no significant associations with any 30-day outcomes and DP after adjustment.
The authors had no financial disclosures.
FROM THE ANNALS OF SURGERY
Key clinical point:
Major finding: Compared to not reinforcing the staple line, doing sow as associated with up to a 60% increase in the risk of a postsurgical leak.
Data source: The database review contained outcomes on 189,477 laparoscopic sleeve gastrectomies.
Disclosures: None of the study authors had any financial disclosures.
Heart failure targets African Americans
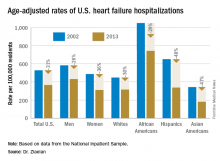
ORLANDO – The disparity in U.S. heart failure incidence continued undiminished during 2002-2013, with African Americans maintaining a steady 2.3-fold increased rate of heart failure, compared with whites, based on national levels of heart failure hospitalizations, a reasonable surrogate for incidence rates, Boback Ziaeian, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
The same period also showed a substantial relative improvement in the heart failure hospitalization rates among U.S. Hispanics, compared with whites, so that, by 2013, the ethnic disparity seen in 2002 between Hispanics and whites largely disappeared, reported Dr. Ziaeian, a cardiologist at the University of California, Los Angeles. The data he analyzed also showed that Asian Americans had the lowest heart failure hospitalization rates of any racial or ethnic group throughout the 11-year period, and that the incidence of heart failure fell more sharply in women than in men during the period, based on the hospitalization numbers.
Age-adjusted heart failure hospitalizations among whites dropped by 30%, and among African Americans by a nearly identical 29%. But this maintained a greater than twofold disparity in rates between the two groups. Among whites, the rate per 100,000 fell from 448 to 315; among African Americans, it dropped from 1,048 to 741. In 2013, the rate of heart failure hospitalizations was 2.4-fold higher in African Americans, compared with whites.
Heart failure hospitalizations fell among Hispanics from 650 per 100,000 to 337 per 100,000 in 2013, a 48% drop that brought the rate among Hispanics to nearly the same as among whites. Asian Americans remained the group with the least heart failure throughout the period, falling from 343 hospitalizations per 100,000 in 2002 to 181 per 100,000 in 2013, a 47% drop.
Among women, the age-adjusted rate per 100,000 fell from 486 to 311, a 36% drop, compared with a decrease from 582 to 431 per 100,000 in men, a 26% reduction. Lower incidence in women may reflect better risk factor control during the study period, compared with men, such as a higher rate of quiting smoking and better treatment compliance, Dr. Ziaeian suggested.
[email protected]
On Twitter @mitchelzoler
ORLANDO – The disparity in U.S. heart failure incidence continued undiminished during 2002-2013, with African Americans maintaining a steady 2.3-fold increased rate of heart failure, compared with whites, based on national levels of heart failure hospitalizations, a reasonable surrogate for incidence rates, Boback Ziaeian, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
The same period also showed a substantial relative improvement in the heart failure hospitalization rates among U.S. Hispanics, compared with whites, so that, by 2013, the ethnic disparity seen in 2002 between Hispanics and whites largely disappeared, reported Dr. Ziaeian, a cardiologist at the University of California, Los Angeles. The data he analyzed also showed that Asian Americans had the lowest heart failure hospitalization rates of any racial or ethnic group throughout the 11-year period, and that the incidence of heart failure fell more sharply in women than in men during the period, based on the hospitalization numbers.
Age-adjusted heart failure hospitalizations among whites dropped by 30%, and among African Americans by a nearly identical 29%. But this maintained a greater than twofold disparity in rates between the two groups. Among whites, the rate per 100,000 fell from 448 to 315; among African Americans, it dropped from 1,048 to 741. In 2013, the rate of heart failure hospitalizations was 2.4-fold higher in African Americans, compared with whites.
Heart failure hospitalizations fell among Hispanics from 650 per 100,000 to 337 per 100,000 in 2013, a 48% drop that brought the rate among Hispanics to nearly the same as among whites. Asian Americans remained the group with the least heart failure throughout the period, falling from 343 hospitalizations per 100,000 in 2002 to 181 per 100,000 in 2013, a 47% drop.
Among women, the age-adjusted rate per 100,000 fell from 486 to 311, a 36% drop, compared with a decrease from 582 to 431 per 100,000 in men, a 26% reduction. Lower incidence in women may reflect better risk factor control during the study period, compared with men, such as a higher rate of quiting smoking and better treatment compliance, Dr. Ziaeian suggested.
[email protected]
On Twitter @mitchelzoler
ORLANDO – The disparity in U.S. heart failure incidence continued undiminished during 2002-2013, with African Americans maintaining a steady 2.3-fold increased rate of heart failure, compared with whites, based on national levels of heart failure hospitalizations, a reasonable surrogate for incidence rates, Boback Ziaeian, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
The same period also showed a substantial relative improvement in the heart failure hospitalization rates among U.S. Hispanics, compared with whites, so that, by 2013, the ethnic disparity seen in 2002 between Hispanics and whites largely disappeared, reported Dr. Ziaeian, a cardiologist at the University of California, Los Angeles. The data he analyzed also showed that Asian Americans had the lowest heart failure hospitalization rates of any racial or ethnic group throughout the 11-year period, and that the incidence of heart failure fell more sharply in women than in men during the period, based on the hospitalization numbers.
Age-adjusted heart failure hospitalizations among whites dropped by 30%, and among African Americans by a nearly identical 29%. But this maintained a greater than twofold disparity in rates between the two groups. Among whites, the rate per 100,000 fell from 448 to 315; among African Americans, it dropped from 1,048 to 741. In 2013, the rate of heart failure hospitalizations was 2.4-fold higher in African Americans, compared with whites.
Heart failure hospitalizations fell among Hispanics from 650 per 100,000 to 337 per 100,000 in 2013, a 48% drop that brought the rate among Hispanics to nearly the same as among whites. Asian Americans remained the group with the least heart failure throughout the period, falling from 343 hospitalizations per 100,000 in 2002 to 181 per 100,000 in 2013, a 47% drop.
Among women, the age-adjusted rate per 100,000 fell from 486 to 311, a 36% drop, compared with a decrease from 582 to 431 per 100,000 in men, a 26% reduction. Lower incidence in women may reflect better risk factor control during the study period, compared with men, such as a higher rate of quiting smoking and better treatment compliance, Dr. Ziaeian suggested.
[email protected]
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: In 2013, age-adjusted heart failure hospitalization was 741/100,000 in African Americans and 315/100,000 in whites.
Data source: The National Inpatient Sample and U.S. Census data.
Disclosures: Dr. Ziaeian had no disclosures.
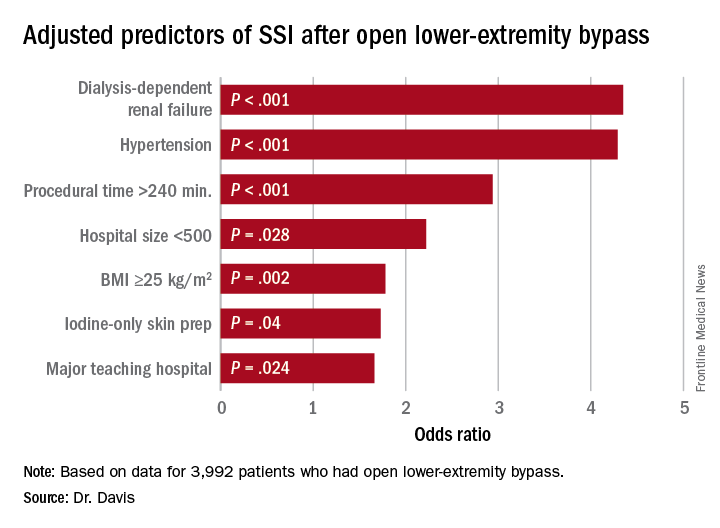
Study identifies SSI risk factors after open LEB
COLUMBUS, OHIO – A study of vascular procedures at 35 Michigan hospitals has identified three risk factors for surgical site infection after lower-extremity bypass that hospitals and vascular surgery teams may be able to modify.
“Patients who had iodine-only skin antiseptic preparation, a high-peak intraoperative glucose, or long operative times were more likely to have substantially increased risk for surgical site infection (SSI),” Frank Davis, MD, of the University of Michigan said in reporting the study results at the annual meeting of the Midwestern Vascular Surgical Society. Those risk factors are modifiable, Dr. Davis said.
“Specific attention needs to be served moving forward in attempts to decrease the risk of SSI for lower-extremity bypass,” Dr. Davis said. “The incidence of SSI in our cohort across the state of Michigan was approximately 9.2%, and for those who did develop a SSI, there was a substantial increase in 30-day morbidity.”
Patients who had an SSI were more than three times more likely to have a major amputation (9% vs. 2.3%) than those without, and more than five times more likely to have a reoperation (3.9% vs. 0.7%), Dr. Davis said.
“With regard to preoperative symptomatology, those with lower peripheral artery questionnaire scores, resting pain, or acute ischemia were more likely to develop SSI postoperatively,” Dr. Davis said. “Patients who underwent an interim coronal bypass had a significant increase of SSI in comparison to all other bypass configurations.”
He also noted that major teaching hospitals or hospitals with 500 or fewer beds had higher rates of SSI.
“Targeted improvements in preoperative care may decrease complications and improve vascular patient outcomes,” Dr. Davis said.
Dr. Davis had no relationships to disclose.
COLUMBUS, OHIO – A study of vascular procedures at 35 Michigan hospitals has identified three risk factors for surgical site infection after lower-extremity bypass that hospitals and vascular surgery teams may be able to modify.
“Patients who had iodine-only skin antiseptic preparation, a high-peak intraoperative glucose, or long operative times were more likely to have substantially increased risk for surgical site infection (SSI),” Frank Davis, MD, of the University of Michigan said in reporting the study results at the annual meeting of the Midwestern Vascular Surgical Society. Those risk factors are modifiable, Dr. Davis said.
“Specific attention needs to be served moving forward in attempts to decrease the risk of SSI for lower-extremity bypass,” Dr. Davis said. “The incidence of SSI in our cohort across the state of Michigan was approximately 9.2%, and for those who did develop a SSI, there was a substantial increase in 30-day morbidity.”
Patients who had an SSI were more than three times more likely to have a major amputation (9% vs. 2.3%) than those without, and more than five times more likely to have a reoperation (3.9% vs. 0.7%), Dr. Davis said.
“With regard to preoperative symptomatology, those with lower peripheral artery questionnaire scores, resting pain, or acute ischemia were more likely to develop SSI postoperatively,” Dr. Davis said. “Patients who underwent an interim coronal bypass had a significant increase of SSI in comparison to all other bypass configurations.”
He also noted that major teaching hospitals or hospitals with 500 or fewer beds had higher rates of SSI.
“Targeted improvements in preoperative care may decrease complications and improve vascular patient outcomes,” Dr. Davis said.
Dr. Davis had no relationships to disclose.
COLUMBUS, OHIO – A study of vascular procedures at 35 Michigan hospitals has identified three risk factors for surgical site infection after lower-extremity bypass that hospitals and vascular surgery teams may be able to modify.
“Patients who had iodine-only skin antiseptic preparation, a high-peak intraoperative glucose, or long operative times were more likely to have substantially increased risk for surgical site infection (SSI),” Frank Davis, MD, of the University of Michigan said in reporting the study results at the annual meeting of the Midwestern Vascular Surgical Society. Those risk factors are modifiable, Dr. Davis said.
“Specific attention needs to be served moving forward in attempts to decrease the risk of SSI for lower-extremity bypass,” Dr. Davis said. “The incidence of SSI in our cohort across the state of Michigan was approximately 9.2%, and for those who did develop a SSI, there was a substantial increase in 30-day morbidity.”
Patients who had an SSI were more than three times more likely to have a major amputation (9% vs. 2.3%) than those without, and more than five times more likely to have a reoperation (3.9% vs. 0.7%), Dr. Davis said.
“With regard to preoperative symptomatology, those with lower peripheral artery questionnaire scores, resting pain, or acute ischemia were more likely to develop SSI postoperatively,” Dr. Davis said. “Patients who underwent an interim coronal bypass had a significant increase of SSI in comparison to all other bypass configurations.”
He also noted that major teaching hospitals or hospitals with 500 or fewer beds had higher rates of SSI.
“Targeted improvements in preoperative care may decrease complications and improve vascular patient outcomes,” Dr. Davis said.
Dr. Davis had no relationships to disclose.
AT MIDWESTERN VASCULAR 2016
Key clinical point: Study identified three key modifiable risk factors in surgical site infection (SSI) open after lower-extremity bypass (LEB).
Major finding: Incidence of SSI was 9.2% in the study cohort.
Data source: Blue Cross Blue Shield Michigan Vascular Intervention Collaborative database of 3,992 open LEB operations at 35 centers from January 2012 to June 2015.
Disclosures: Dr. Davis reported having no financial disclosures.
Syphilis testing before and after stillbirth is suboptimal
ATLANTA – Physicians are falling short on syphilis testing in both the prenatal period and at the time of delivery, suggest the findings of a study examining insurance claims from nearly 10,000 women who experienced stillbirths.
Overall, less than 10% of women in the study were tested for syphilis following a stillbirth delivery, while less than two-thirds of women who experienced a stillbirth had received prenatal syphilis testing.
Dr. Patel and his coinvestigators examined data from the Truven Health MarketScan Medicaid and commercial claims database to evaluate the proportion of women who had syphilis testing within at least 1 week before and 1 week after a stillbirth delivery.
The investigators identified women aged 15-44 years who had a stillbirth delivery in 2013. Stillbirths were identified via ICD-9 codes and these codes were also used to track prenatal syphilis testing, as well as syphilis testing, placental examination and complete blood count (CBC) performed at the time of delivery.
In total, there were 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who experienced stillbirths and were included in the study. Of these women, 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-insured women and 9.3% of commercially-insured women received syphilis testing.
Most women in the study were receiving prenatal care. In all, 73.2% of Medicaid-covered women and 76.5% of commercially-insured women received it. Placental examination at the time of delivery occurred for 61.5% of Medicaid-covered women and 58.0% of commercially-insured women, while CBC was performed in 31.2% and 35.8% of women, respectively.
“Overall, prenatal syphilis testing was significantly higher than syphilis testing at the time of delivery,” Dr. Patel said. “Women with prenatal syphilis testing were more likely to be tested for syphilis at delivery than those not tested, regardless of [their] insurance.”
Dr. Patel did not report information on financial disclosures.
ATLANTA – Physicians are falling short on syphilis testing in both the prenatal period and at the time of delivery, suggest the findings of a study examining insurance claims from nearly 10,000 women who experienced stillbirths.
Overall, less than 10% of women in the study were tested for syphilis following a stillbirth delivery, while less than two-thirds of women who experienced a stillbirth had received prenatal syphilis testing.
Dr. Patel and his coinvestigators examined data from the Truven Health MarketScan Medicaid and commercial claims database to evaluate the proportion of women who had syphilis testing within at least 1 week before and 1 week after a stillbirth delivery.
The investigators identified women aged 15-44 years who had a stillbirth delivery in 2013. Stillbirths were identified via ICD-9 codes and these codes were also used to track prenatal syphilis testing, as well as syphilis testing, placental examination and complete blood count (CBC) performed at the time of delivery.
In total, there were 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who experienced stillbirths and were included in the study. Of these women, 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-insured women and 9.3% of commercially-insured women received syphilis testing.
Most women in the study were receiving prenatal care. In all, 73.2% of Medicaid-covered women and 76.5% of commercially-insured women received it. Placental examination at the time of delivery occurred for 61.5% of Medicaid-covered women and 58.0% of commercially-insured women, while CBC was performed in 31.2% and 35.8% of women, respectively.
“Overall, prenatal syphilis testing was significantly higher than syphilis testing at the time of delivery,” Dr. Patel said. “Women with prenatal syphilis testing were more likely to be tested for syphilis at delivery than those not tested, regardless of [their] insurance.”
Dr. Patel did not report information on financial disclosures.
ATLANTA – Physicians are falling short on syphilis testing in both the prenatal period and at the time of delivery, suggest the findings of a study examining insurance claims from nearly 10,000 women who experienced stillbirths.
Overall, less than 10% of women in the study were tested for syphilis following a stillbirth delivery, while less than two-thirds of women who experienced a stillbirth had received prenatal syphilis testing.
Dr. Patel and his coinvestigators examined data from the Truven Health MarketScan Medicaid and commercial claims database to evaluate the proportion of women who had syphilis testing within at least 1 week before and 1 week after a stillbirth delivery.
The investigators identified women aged 15-44 years who had a stillbirth delivery in 2013. Stillbirths were identified via ICD-9 codes and these codes were also used to track prenatal syphilis testing, as well as syphilis testing, placental examination and complete blood count (CBC) performed at the time of delivery.
In total, there were 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who experienced stillbirths and were included in the study. Of these women, 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-insured women and 9.3% of commercially-insured women received syphilis testing.
Most women in the study were receiving prenatal care. In all, 73.2% of Medicaid-covered women and 76.5% of commercially-insured women received it. Placental examination at the time of delivery occurred for 61.5% of Medicaid-covered women and 58.0% of commercially-insured women, while CBC was performed in 31.2% and 35.8% of women, respectively.
“Overall, prenatal syphilis testing was significantly higher than syphilis testing at the time of delivery,” Dr. Patel said. “Women with prenatal syphilis testing were more likely to be tested for syphilis at delivery than those not tested, regardless of [their] insurance.”
Dr. Patel did not report information on financial disclosures.
AT THE 2016 STD PREVENTION CONFERENCE
Key clinical point:
Major finding: A total of 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-covered women and 9.3% of commercially-insured women received syphilis testing.
Data source: Review of claims data from 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who had stillbirth deliveries in 2013.
Disclosures: Dr. Patel did not report information on financial disclosures.
VIDEO: Two PCI vs. CABG trials produce conflicting results
WASHINGTON – Results from two large, multicenter comparisons of coronary stenting and coronary bypass surgery for treating patients with unprotected left main coronary disease may have superficially shown sharp differences, but the bottom line will likely be greater empowerment of percutaneous coronary intervention as an option for selected patients with less complex coronary disease.
Prior to the results from the EXCEL and NOBLE trials, reported at the Transcatheter Cardiovascular Therapeutics annual meeting, “guidelines put PCI [percutaneous coronary intervention] into a class 1, 2 or 3 status for treating left main coronary disease depending on disease complexity, but in the United States, PCI for patients eligible for CABG [coronary artery bypass grafting] has not been frequently done. I think these results, in a very circumscribed subset of patients and using a state-of-the-art stent, will affect the guidelines,” predicted Gregg W. Stone, MD, lead investigator for EXCEL and professor of medicine at Columbia University in New York.
“What the guidelines have not addressed are the patients with low- or intermediate-complexity disease who have an acceptable risk for undergoing either PCI or CABG. I think the trial results answer this question,” said David Kandzari, MD, director of interventional cardiology and chief scientific officer at the Piedmont Heart Institute in Atlanta and an EXCEL investigator.
While the EXCEL and NOBLE results don’t provide a simple answer on the relative merits of PCI and CABG, many of their outcome differences seem explicable, several experts said at the meeting.
The Nordic-Baltic-British Left Main Revascularisation (NOBLE) trial randomized 1,201 patients who had unprotected left main coronary disease and were judged by a heart team to be reasonable candidates for both PCI or CABG at 36 centers in nine European countries during 2008-2015. The primary endpoint was death from any cause, nonprocedural MIs, stroke, or repeat revascularization.
The researchers followed patients for a median of just over 3 years, but they calculated the primary endpoint based on a Kaplan-Meier estimate for 5-year outcomes, which showed the primary endpoint in 29% of the PCI patients and in 19% of the CABG patients, a statistically significant benefit in favor of CABG, Evald H. Christiansen, MD, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation. Concurrently with his report, the results were published online (Lancet. 2016 Oct. 31. doi: 10.1016/S0140-6736[16]32052-9).
This difference between PCI and CABG was largely driven by an excess of postprocedural MIs and repeat revascularizations among the PCI patients, said Dr. Christiansen, an interventional cardiologist at Aarhus University Hospital in Denmark. Another notable finding was that the superior outcomes with CABG primarily occurred among patients with a SYNTAX score – a measure of coronary disease complexity – of 22 or less, which identifies patients with low complexity disease. The outcomes of patients with SYNTAX scores of 23-32, which identifies intermediate complexity disease, and of patients with scores of 33 or higher, with very complex disease, were similar in the PCI and CABG arms, he reported. This finding was “very surprising,” Dr. Christiansen said, because it reversed the finding originally made in the SYNTAX trial that PCI performed best compared with CABG in patients with the lowest scores and least-complex coronary disease.
The superiority of CABG over PCI seen in the NOBLE results, especially in patients with lower SYNTAX scores, seemed at odds with the EXCEL results, reported at the meeting by Dr. Stone and simultaneously online (N Engl J Med. 2016 Oct. 31. doi: 10.1056/NEJMoa1610227). In EXCEL, which enrolled only patients with a SYNTAX score of 32 or less (low- or intermediate-complexity coronary disease), patients had a 3-year incidence of death, stroke or MI of 15% in both the PCI and CABG arms.
But the EXCEL and NOBLE trials had several important differences, and it seemed like cumulatively these differences account for their differing results.
“One of the biggest differences” was the exclusion of procedural MIs in the NOBLE tally of adverse events, noted Dr. Stone. These were diagnosed in EXCEL using the MI definition published in 2013 by a panel of the Society for Cardiovascular Angiography and Interventions (SCAI). NOBLE disregarded procedural MIs because many of its participating hospitals did not have the laboratory resources to make these diagnoses and because the trial’s design predated the SCAI definition by several years, Dr. Christiansen explained.
Other important differences included the shorter follow-up in EXCEL, the inclusion of revascularization as an endpoint component in NOBLE but not in EXCEL, and differences in the stents used. In EXCEL, all patients undergoing PCI received Xience everolimus-eluting stents. In NOBLE, the first 11% of the enrolled patients received first-generation, sirolimus-eluting Cypher stents; the next 89% of enrollees received a biolimus-eluting Biomatrix Flex stent. Dr. Christiansen acknowledged the confounding caused by having many patients in the NOBLE PCI arm who received outmoded Cypher stents, especially because their relatively longer follow-up made them overrepresented in the primary outcome results. Plus, the Biomatrix Flex stent was disparaged by Martin B. Leon, MD, an EXCEL investigator and professor of medicine at Columbia University, who called the device “not currently widely used for PCI and more of historic interest.”
Dr. Leon added that the EXCEL and NOBLE patients also had substantially different prevalence rates of diabetes and acute coronary syndrome.
“The huge difference [between EXCEL and NOBLE] is the endpoint,” declared Marc Ruel, MD, another EXCEL investigator and head of cardiac surgery at the Ottawa Heart Institute. “The EXCEL endpoint was driven by the high rate of periprocedural MIs in the CABG arm. Once you get past 30 days, the noninferiority is not met by PCI.”
Another big endpoint difference was leaving revascularizations out of the EXCEL composite. “Once you take revascularization out of the primary endpoint, the outcome [of EXCEL] was more or less preordained,” noted Craig R. Smith, MD, chairman of surgery at Columbia University and an EXCEL investigator. “It’s the slope of events [in the PCI arm] after 3 months that’s the story. I think the CABG and PCI slopes in EXCEL will continue to diverge with time” beyond the current 3-year follow-up, Dr. Smith said.
“I agree that after 30 days surgery was the more durable procedure,” said Dr. Stone. “There is a big upfront hit for patients to take with surgery compared with PCI. If patients get through that, then they have a more durable procedure. That’s the trade-off.”
Dr. Stone hinted that future reports of EXCEL data will highlight other hits that patients must endure upfront if they choose CABG over PCI. “The early difference was quite profound not only for the primary endpoint but also for renal failure, infections, arrhythmias, and blood transfusions,” he said. Choosing between PCI and CABG for patients with left main disease and a lower SYNTAX score “is a decision that should be made by the heart team and patients. Some patients will prefer surgery, and some will prefer PCI.”
The NOBLE trial received partial funding from Biosensors, the company that markets the Biomatrix Flex stent used in the trial. The EXCEL trial was sponsored by Abbott Vascular, the company that markets the Xience stent used in the trial. Dr. Stone, Dr. Kandzari, Dr. Christiansen, Dr. Ruel, and Dr. Smith had no disclosures. Dr. Leon has been a consultant to and received research support from Abbott Vascular and Boston Scientific and has also received research support from Edwards, Medtronic and St. Jude.
[email protected]
On Twitter @mitchelzoler
The results from EXCEL and NOBLE were not that different, but what was different was how the two trials were designed and how their endpoints were defined. The biggest difference between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) seemed to be in the rate of late MIs, with a little higher rate following PCI, and more repeat revascularizations with PCI, but with similar mortality rates with both treatments. There was a lot of similarity in the results despite the differences in the trials.
The evidence in both studies gives more support to the concept that, for patients with simpler left main lesions, PCI is a competitive alternative to CABG. Until now, in U.S. practice patients with left main coronary disease have been preferentially referred for CABG. These results will open us up to giving selected patients a more balanced view of the two options. After we explain differences in recovery and late events patients can decide which treatment to receive.
Despite these new findings, PCI is still not for every patient. A substantial fraction of patients with left main coronary disease were excluded from these studies because they had more complex coronary anatomy, and for patients like that, CABG remains the clear standard of care.
David J. Cohen, MD, is director of cardiovascular research and an interventional cardiologist at Saint Luke’s Health System in Kansas City, Mo. He made these comments in a video interview. He had received research support from Abbott Vascular, and is an investigator in the EXCEL trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The results from EXCEL and NOBLE were not that different, but what was different was how the two trials were designed and how their endpoints were defined. The biggest difference between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) seemed to be in the rate of late MIs, with a little higher rate following PCI, and more repeat revascularizations with PCI, but with similar mortality rates with both treatments. There was a lot of similarity in the results despite the differences in the trials.
The evidence in both studies gives more support to the concept that, for patients with simpler left main lesions, PCI is a competitive alternative to CABG. Until now, in U.S. practice patients with left main coronary disease have been preferentially referred for CABG. These results will open us up to giving selected patients a more balanced view of the two options. After we explain differences in recovery and late events patients can decide which treatment to receive.
Despite these new findings, PCI is still not for every patient. A substantial fraction of patients with left main coronary disease were excluded from these studies because they had more complex coronary anatomy, and for patients like that, CABG remains the clear standard of care.
David J. Cohen, MD, is director of cardiovascular research and an interventional cardiologist at Saint Luke’s Health System in Kansas City, Mo. He made these comments in a video interview. He had received research support from Abbott Vascular, and is an investigator in the EXCEL trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The results from EXCEL and NOBLE were not that different, but what was different was how the two trials were designed and how their endpoints were defined. The biggest difference between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) seemed to be in the rate of late MIs, with a little higher rate following PCI, and more repeat revascularizations with PCI, but with similar mortality rates with both treatments. There was a lot of similarity in the results despite the differences in the trials.
The evidence in both studies gives more support to the concept that, for patients with simpler left main lesions, PCI is a competitive alternative to CABG. Until now, in U.S. practice patients with left main coronary disease have been preferentially referred for CABG. These results will open us up to giving selected patients a more balanced view of the two options. After we explain differences in recovery and late events patients can decide which treatment to receive.
Despite these new findings, PCI is still not for every patient. A substantial fraction of patients with left main coronary disease were excluded from these studies because they had more complex coronary anatomy, and for patients like that, CABG remains the clear standard of care.
David J. Cohen, MD, is director of cardiovascular research and an interventional cardiologist at Saint Luke’s Health System in Kansas City, Mo. He made these comments in a video interview. He had received research support from Abbott Vascular, and is an investigator in the EXCEL trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – Results from two large, multicenter comparisons of coronary stenting and coronary bypass surgery for treating patients with unprotected left main coronary disease may have superficially shown sharp differences, but the bottom line will likely be greater empowerment of percutaneous coronary intervention as an option for selected patients with less complex coronary disease.
Prior to the results from the EXCEL and NOBLE trials, reported at the Transcatheter Cardiovascular Therapeutics annual meeting, “guidelines put PCI [percutaneous coronary intervention] into a class 1, 2 or 3 status for treating left main coronary disease depending on disease complexity, but in the United States, PCI for patients eligible for CABG [coronary artery bypass grafting] has not been frequently done. I think these results, in a very circumscribed subset of patients and using a state-of-the-art stent, will affect the guidelines,” predicted Gregg W. Stone, MD, lead investigator for EXCEL and professor of medicine at Columbia University in New York.
“What the guidelines have not addressed are the patients with low- or intermediate-complexity disease who have an acceptable risk for undergoing either PCI or CABG. I think the trial results answer this question,” said David Kandzari, MD, director of interventional cardiology and chief scientific officer at the Piedmont Heart Institute in Atlanta and an EXCEL investigator.
While the EXCEL and NOBLE results don’t provide a simple answer on the relative merits of PCI and CABG, many of their outcome differences seem explicable, several experts said at the meeting.
The Nordic-Baltic-British Left Main Revascularisation (NOBLE) trial randomized 1,201 patients who had unprotected left main coronary disease and were judged by a heart team to be reasonable candidates for both PCI or CABG at 36 centers in nine European countries during 2008-2015. The primary endpoint was death from any cause, nonprocedural MIs, stroke, or repeat revascularization.
The researchers followed patients for a median of just over 3 years, but they calculated the primary endpoint based on a Kaplan-Meier estimate for 5-year outcomes, which showed the primary endpoint in 29% of the PCI patients and in 19% of the CABG patients, a statistically significant benefit in favor of CABG, Evald H. Christiansen, MD, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation. Concurrently with his report, the results were published online (Lancet. 2016 Oct. 31. doi: 10.1016/S0140-6736[16]32052-9).
This difference between PCI and CABG was largely driven by an excess of postprocedural MIs and repeat revascularizations among the PCI patients, said Dr. Christiansen, an interventional cardiologist at Aarhus University Hospital in Denmark. Another notable finding was that the superior outcomes with CABG primarily occurred among patients with a SYNTAX score – a measure of coronary disease complexity – of 22 or less, which identifies patients with low complexity disease. The outcomes of patients with SYNTAX scores of 23-32, which identifies intermediate complexity disease, and of patients with scores of 33 or higher, with very complex disease, were similar in the PCI and CABG arms, he reported. This finding was “very surprising,” Dr. Christiansen said, because it reversed the finding originally made in the SYNTAX trial that PCI performed best compared with CABG in patients with the lowest scores and least-complex coronary disease.
The superiority of CABG over PCI seen in the NOBLE results, especially in patients with lower SYNTAX scores, seemed at odds with the EXCEL results, reported at the meeting by Dr. Stone and simultaneously online (N Engl J Med. 2016 Oct. 31. doi: 10.1056/NEJMoa1610227). In EXCEL, which enrolled only patients with a SYNTAX score of 32 or less (low- or intermediate-complexity coronary disease), patients had a 3-year incidence of death, stroke or MI of 15% in both the PCI and CABG arms.
But the EXCEL and NOBLE trials had several important differences, and it seemed like cumulatively these differences account for their differing results.
“One of the biggest differences” was the exclusion of procedural MIs in the NOBLE tally of adverse events, noted Dr. Stone. These were diagnosed in EXCEL using the MI definition published in 2013 by a panel of the Society for Cardiovascular Angiography and Interventions (SCAI). NOBLE disregarded procedural MIs because many of its participating hospitals did not have the laboratory resources to make these diagnoses and because the trial’s design predated the SCAI definition by several years, Dr. Christiansen explained.
Other important differences included the shorter follow-up in EXCEL, the inclusion of revascularization as an endpoint component in NOBLE but not in EXCEL, and differences in the stents used. In EXCEL, all patients undergoing PCI received Xience everolimus-eluting stents. In NOBLE, the first 11% of the enrolled patients received first-generation, sirolimus-eluting Cypher stents; the next 89% of enrollees received a biolimus-eluting Biomatrix Flex stent. Dr. Christiansen acknowledged the confounding caused by having many patients in the NOBLE PCI arm who received outmoded Cypher stents, especially because their relatively longer follow-up made them overrepresented in the primary outcome results. Plus, the Biomatrix Flex stent was disparaged by Martin B. Leon, MD, an EXCEL investigator and professor of medicine at Columbia University, who called the device “not currently widely used for PCI and more of historic interest.”
Dr. Leon added that the EXCEL and NOBLE patients also had substantially different prevalence rates of diabetes and acute coronary syndrome.
“The huge difference [between EXCEL and NOBLE] is the endpoint,” declared Marc Ruel, MD, another EXCEL investigator and head of cardiac surgery at the Ottawa Heart Institute. “The EXCEL endpoint was driven by the high rate of periprocedural MIs in the CABG arm. Once you get past 30 days, the noninferiority is not met by PCI.”
Another big endpoint difference was leaving revascularizations out of the EXCEL composite. “Once you take revascularization out of the primary endpoint, the outcome [of EXCEL] was more or less preordained,” noted Craig R. Smith, MD, chairman of surgery at Columbia University and an EXCEL investigator. “It’s the slope of events [in the PCI arm] after 3 months that’s the story. I think the CABG and PCI slopes in EXCEL will continue to diverge with time” beyond the current 3-year follow-up, Dr. Smith said.
“I agree that after 30 days surgery was the more durable procedure,” said Dr. Stone. “There is a big upfront hit for patients to take with surgery compared with PCI. If patients get through that, then they have a more durable procedure. That’s the trade-off.”
Dr. Stone hinted that future reports of EXCEL data will highlight other hits that patients must endure upfront if they choose CABG over PCI. “The early difference was quite profound not only for the primary endpoint but also for renal failure, infections, arrhythmias, and blood transfusions,” he said. Choosing between PCI and CABG for patients with left main disease and a lower SYNTAX score “is a decision that should be made by the heart team and patients. Some patients will prefer surgery, and some will prefer PCI.”
The NOBLE trial received partial funding from Biosensors, the company that markets the Biomatrix Flex stent used in the trial. The EXCEL trial was sponsored by Abbott Vascular, the company that markets the Xience stent used in the trial. Dr. Stone, Dr. Kandzari, Dr. Christiansen, Dr. Ruel, and Dr. Smith had no disclosures. Dr. Leon has been a consultant to and received research support from Abbott Vascular and Boston Scientific and has also received research support from Edwards, Medtronic and St. Jude.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – Results from two large, multicenter comparisons of coronary stenting and coronary bypass surgery for treating patients with unprotected left main coronary disease may have superficially shown sharp differences, but the bottom line will likely be greater empowerment of percutaneous coronary intervention as an option for selected patients with less complex coronary disease.
Prior to the results from the EXCEL and NOBLE trials, reported at the Transcatheter Cardiovascular Therapeutics annual meeting, “guidelines put PCI [percutaneous coronary intervention] into a class 1, 2 or 3 status for treating left main coronary disease depending on disease complexity, but in the United States, PCI for patients eligible for CABG [coronary artery bypass grafting] has not been frequently done. I think these results, in a very circumscribed subset of patients and using a state-of-the-art stent, will affect the guidelines,” predicted Gregg W. Stone, MD, lead investigator for EXCEL and professor of medicine at Columbia University in New York.
“What the guidelines have not addressed are the patients with low- or intermediate-complexity disease who have an acceptable risk for undergoing either PCI or CABG. I think the trial results answer this question,” said David Kandzari, MD, director of interventional cardiology and chief scientific officer at the Piedmont Heart Institute in Atlanta and an EXCEL investigator.
While the EXCEL and NOBLE results don’t provide a simple answer on the relative merits of PCI and CABG, many of their outcome differences seem explicable, several experts said at the meeting.
The Nordic-Baltic-British Left Main Revascularisation (NOBLE) trial randomized 1,201 patients who had unprotected left main coronary disease and were judged by a heart team to be reasonable candidates for both PCI or CABG at 36 centers in nine European countries during 2008-2015. The primary endpoint was death from any cause, nonprocedural MIs, stroke, or repeat revascularization.
The researchers followed patients for a median of just over 3 years, but they calculated the primary endpoint based on a Kaplan-Meier estimate for 5-year outcomes, which showed the primary endpoint in 29% of the PCI patients and in 19% of the CABG patients, a statistically significant benefit in favor of CABG, Evald H. Christiansen, MD, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation. Concurrently with his report, the results were published online (Lancet. 2016 Oct. 31. doi: 10.1016/S0140-6736[16]32052-9).
This difference between PCI and CABG was largely driven by an excess of postprocedural MIs and repeat revascularizations among the PCI patients, said Dr. Christiansen, an interventional cardiologist at Aarhus University Hospital in Denmark. Another notable finding was that the superior outcomes with CABG primarily occurred among patients with a SYNTAX score – a measure of coronary disease complexity – of 22 or less, which identifies patients with low complexity disease. The outcomes of patients with SYNTAX scores of 23-32, which identifies intermediate complexity disease, and of patients with scores of 33 or higher, with very complex disease, were similar in the PCI and CABG arms, he reported. This finding was “very surprising,” Dr. Christiansen said, because it reversed the finding originally made in the SYNTAX trial that PCI performed best compared with CABG in patients with the lowest scores and least-complex coronary disease.
The superiority of CABG over PCI seen in the NOBLE results, especially in patients with lower SYNTAX scores, seemed at odds with the EXCEL results, reported at the meeting by Dr. Stone and simultaneously online (N Engl J Med. 2016 Oct. 31. doi: 10.1056/NEJMoa1610227). In EXCEL, which enrolled only patients with a SYNTAX score of 32 or less (low- or intermediate-complexity coronary disease), patients had a 3-year incidence of death, stroke or MI of 15% in both the PCI and CABG arms.
But the EXCEL and NOBLE trials had several important differences, and it seemed like cumulatively these differences account for their differing results.
“One of the biggest differences” was the exclusion of procedural MIs in the NOBLE tally of adverse events, noted Dr. Stone. These were diagnosed in EXCEL using the MI definition published in 2013 by a panel of the Society for Cardiovascular Angiography and Interventions (SCAI). NOBLE disregarded procedural MIs because many of its participating hospitals did not have the laboratory resources to make these diagnoses and because the trial’s design predated the SCAI definition by several years, Dr. Christiansen explained.
Other important differences included the shorter follow-up in EXCEL, the inclusion of revascularization as an endpoint component in NOBLE but not in EXCEL, and differences in the stents used. In EXCEL, all patients undergoing PCI received Xience everolimus-eluting stents. In NOBLE, the first 11% of the enrolled patients received first-generation, sirolimus-eluting Cypher stents; the next 89% of enrollees received a biolimus-eluting Biomatrix Flex stent. Dr. Christiansen acknowledged the confounding caused by having many patients in the NOBLE PCI arm who received outmoded Cypher stents, especially because their relatively longer follow-up made them overrepresented in the primary outcome results. Plus, the Biomatrix Flex stent was disparaged by Martin B. Leon, MD, an EXCEL investigator and professor of medicine at Columbia University, who called the device “not currently widely used for PCI and more of historic interest.”
Dr. Leon added that the EXCEL and NOBLE patients also had substantially different prevalence rates of diabetes and acute coronary syndrome.
“The huge difference [between EXCEL and NOBLE] is the endpoint,” declared Marc Ruel, MD, another EXCEL investigator and head of cardiac surgery at the Ottawa Heart Institute. “The EXCEL endpoint was driven by the high rate of periprocedural MIs in the CABG arm. Once you get past 30 days, the noninferiority is not met by PCI.”
Another big endpoint difference was leaving revascularizations out of the EXCEL composite. “Once you take revascularization out of the primary endpoint, the outcome [of EXCEL] was more or less preordained,” noted Craig R. Smith, MD, chairman of surgery at Columbia University and an EXCEL investigator. “It’s the slope of events [in the PCI arm] after 3 months that’s the story. I think the CABG and PCI slopes in EXCEL will continue to diverge with time” beyond the current 3-year follow-up, Dr. Smith said.
“I agree that after 30 days surgery was the more durable procedure,” said Dr. Stone. “There is a big upfront hit for patients to take with surgery compared with PCI. If patients get through that, then they have a more durable procedure. That’s the trade-off.”
Dr. Stone hinted that future reports of EXCEL data will highlight other hits that patients must endure upfront if they choose CABG over PCI. “The early difference was quite profound not only for the primary endpoint but also for renal failure, infections, arrhythmias, and blood transfusions,” he said. Choosing between PCI and CABG for patients with left main disease and a lower SYNTAX score “is a decision that should be made by the heart team and patients. Some patients will prefer surgery, and some will prefer PCI.”
The NOBLE trial received partial funding from Biosensors, the company that markets the Biomatrix Flex stent used in the trial. The EXCEL trial was sponsored by Abbott Vascular, the company that markets the Xience stent used in the trial. Dr. Stone, Dr. Kandzari, Dr. Christiansen, Dr. Ruel, and Dr. Smith had no disclosures. Dr. Leon has been a consultant to and received research support from Abbott Vascular and Boston Scientific and has also received research support from Edwards, Medtronic and St. Jude.
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM TCT 2016
ReACT: No benefit from routine coronary angiography after PCI
Routine follow-up coronary angiography after percutaneous coronary intervention leads to increased rates of coronary revascularization but without any significant benefits for outcomes, according to a study presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously on Nov. 1 in the Journal of the American College of Cardiology: Cardiovascular Interventions.
Hiroki Shiomi, MD, from Kyoto University, and his coauthors reported on ReACT, a prospective, open-label randomized controlled trial of routine follow-up coronary angiography in 700 patients who underwent successful percutaneous coronary intervention (PCI).
Among the 349 patients randomized to follow-up coronary angiography (FUCAG), 12.8% underwent any coronary revascularization within the first year after PCI, compared with 3.8% of the 351 patients randomized to standard clinical follow-up. The routine angiography group also had a higher incidence of target lesion revascularization in the first year after the index PCI (7.0% vs. 1.7%).
In both these cases, the cumulative 5-year incidence of coronary or target lesion revascularization was not significantly different between the routine angiography and control groups. However researchers saw no significant benefit from routine FUCAG in terms of the cumulative 5-year incidence of all-cause death, myocardial infarction, stroke, or emergency hospitalizations for acute coronary syndrome or heart failure, compared with clinical follow-up (22.4% vs. 24.7%; P = 0.70).
Nor were there any significant differences between the two groups in these individual components, or in the cumulative 5-year incidence of major bleeding (JACC Cardiovasc Interv. 2016 Nov 1.)
The authors commented that several previous studies have shown that routine FUCAG does not improve clinical outcomes, although it is still commonly performed in Japan after PCI.
“However, previous studies in the drug-eluting stents (DES) era were conducted in the context of pivotal randomized trials of DES and there have been no randomized clinical trials evaluating long-term clinical impact of routine FUCAG after PCI in the real world clinical practice including high-risk patients for cardiovascular events risk such as complex coronary artery disease and acute myocardial infarction (AMI) presentation,” the authors wrote.
Overall, 85.4% of patients in the routine angiography group and 12% of those in the clinical care group underwent coronary angiography in the first year, including for clinical reasons.
In the clinical follow-up group, coronary angiography was performed because of acute coronary syndrome (14%), recurrence of angina (60%), other clinical reasons (14%), or no clinical reason (12%). The control group also had more noninvasive physiological stress testing such as treadmill exercise test and stress nuclear study.
“Considering the invasive nature of coronary angiography and increased medical expenses, routine FUCAG after PCI would not be allowed as the usual clinical practice, unless patients have recurrent symptoms or objective evidence of ischemia,” the authors wrote.
“On the other hand, there was no excess of adverse clinical events with routine angiographic follow-up strategy except for the increased rate of 1-year repeat coronary revascularization.”
Given this, they suggested that scheduled angiographic follow-up might still be considered acceptable for early in vivo or significant coronary device trials.
While the authors said the trial ended up being underpowered because of a reduced final sample size and lower-than-anticipated event rate, it did warrant further larger-scale studies. In particular, they highlighted the question of what impact routine follow-up angiography might have in higher-risk patients, such as those with left main or multivessel coronary artery disease.
“Finally, because patient demographics, practice patterns including the indication of coronary revascularization, and clinical outcomes in Japan may be different from those outside Japan, generalizing the present study results to populations outside Japan should be done with caution.”
This study was supported by an educational grant from the Research Institute for Production Development (Kyoto). One author declared honoraria for education consulting from Boston Scientific Corporation.
Routine follow-up coronary angiography after percutaneous coronary intervention leads to increased rates of coronary revascularization but without any significant benefits for outcomes, according to a study presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously on Nov. 1 in the Journal of the American College of Cardiology: Cardiovascular Interventions.
Hiroki Shiomi, MD, from Kyoto University, and his coauthors reported on ReACT, a prospective, open-label randomized controlled trial of routine follow-up coronary angiography in 700 patients who underwent successful percutaneous coronary intervention (PCI).
Among the 349 patients randomized to follow-up coronary angiography (FUCAG), 12.8% underwent any coronary revascularization within the first year after PCI, compared with 3.8% of the 351 patients randomized to standard clinical follow-up. The routine angiography group also had a higher incidence of target lesion revascularization in the first year after the index PCI (7.0% vs. 1.7%).
In both these cases, the cumulative 5-year incidence of coronary or target lesion revascularization was not significantly different between the routine angiography and control groups. However researchers saw no significant benefit from routine FUCAG in terms of the cumulative 5-year incidence of all-cause death, myocardial infarction, stroke, or emergency hospitalizations for acute coronary syndrome or heart failure, compared with clinical follow-up (22.4% vs. 24.7%; P = 0.70).
Nor were there any significant differences between the two groups in these individual components, or in the cumulative 5-year incidence of major bleeding (JACC Cardiovasc Interv. 2016 Nov 1.)
The authors commented that several previous studies have shown that routine FUCAG does not improve clinical outcomes, although it is still commonly performed in Japan after PCI.
“However, previous studies in the drug-eluting stents (DES) era were conducted in the context of pivotal randomized trials of DES and there have been no randomized clinical trials evaluating long-term clinical impact of routine FUCAG after PCI in the real world clinical practice including high-risk patients for cardiovascular events risk such as complex coronary artery disease and acute myocardial infarction (AMI) presentation,” the authors wrote.
Overall, 85.4% of patients in the routine angiography group and 12% of those in the clinical care group underwent coronary angiography in the first year, including for clinical reasons.
In the clinical follow-up group, coronary angiography was performed because of acute coronary syndrome (14%), recurrence of angina (60%), other clinical reasons (14%), or no clinical reason (12%). The control group also had more noninvasive physiological stress testing such as treadmill exercise test and stress nuclear study.
“Considering the invasive nature of coronary angiography and increased medical expenses, routine FUCAG after PCI would not be allowed as the usual clinical practice, unless patients have recurrent symptoms or objective evidence of ischemia,” the authors wrote.
“On the other hand, there was no excess of adverse clinical events with routine angiographic follow-up strategy except for the increased rate of 1-year repeat coronary revascularization.”
Given this, they suggested that scheduled angiographic follow-up might still be considered acceptable for early in vivo or significant coronary device trials.
While the authors said the trial ended up being underpowered because of a reduced final sample size and lower-than-anticipated event rate, it did warrant further larger-scale studies. In particular, they highlighted the question of what impact routine follow-up angiography might have in higher-risk patients, such as those with left main or multivessel coronary artery disease.
“Finally, because patient demographics, practice patterns including the indication of coronary revascularization, and clinical outcomes in Japan may be different from those outside Japan, generalizing the present study results to populations outside Japan should be done with caution.”
This study was supported by an educational grant from the Research Institute for Production Development (Kyoto). One author declared honoraria for education consulting from Boston Scientific Corporation.
Routine follow-up coronary angiography after percutaneous coronary intervention leads to increased rates of coronary revascularization but without any significant benefits for outcomes, according to a study presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously on Nov. 1 in the Journal of the American College of Cardiology: Cardiovascular Interventions.
Hiroki Shiomi, MD, from Kyoto University, and his coauthors reported on ReACT, a prospective, open-label randomized controlled trial of routine follow-up coronary angiography in 700 patients who underwent successful percutaneous coronary intervention (PCI).
Among the 349 patients randomized to follow-up coronary angiography (FUCAG), 12.8% underwent any coronary revascularization within the first year after PCI, compared with 3.8% of the 351 patients randomized to standard clinical follow-up. The routine angiography group also had a higher incidence of target lesion revascularization in the first year after the index PCI (7.0% vs. 1.7%).
In both these cases, the cumulative 5-year incidence of coronary or target lesion revascularization was not significantly different between the routine angiography and control groups. However researchers saw no significant benefit from routine FUCAG in terms of the cumulative 5-year incidence of all-cause death, myocardial infarction, stroke, or emergency hospitalizations for acute coronary syndrome or heart failure, compared with clinical follow-up (22.4% vs. 24.7%; P = 0.70).
Nor were there any significant differences between the two groups in these individual components, or in the cumulative 5-year incidence of major bleeding (JACC Cardiovasc Interv. 2016 Nov 1.)
The authors commented that several previous studies have shown that routine FUCAG does not improve clinical outcomes, although it is still commonly performed in Japan after PCI.
“However, previous studies in the drug-eluting stents (DES) era were conducted in the context of pivotal randomized trials of DES and there have been no randomized clinical trials evaluating long-term clinical impact of routine FUCAG after PCI in the real world clinical practice including high-risk patients for cardiovascular events risk such as complex coronary artery disease and acute myocardial infarction (AMI) presentation,” the authors wrote.
Overall, 85.4% of patients in the routine angiography group and 12% of those in the clinical care group underwent coronary angiography in the first year, including for clinical reasons.
In the clinical follow-up group, coronary angiography was performed because of acute coronary syndrome (14%), recurrence of angina (60%), other clinical reasons (14%), or no clinical reason (12%). The control group also had more noninvasive physiological stress testing such as treadmill exercise test and stress nuclear study.
“Considering the invasive nature of coronary angiography and increased medical expenses, routine FUCAG after PCI would not be allowed as the usual clinical practice, unless patients have recurrent symptoms or objective evidence of ischemia,” the authors wrote.
“On the other hand, there was no excess of adverse clinical events with routine angiographic follow-up strategy except for the increased rate of 1-year repeat coronary revascularization.”
Given this, they suggested that scheduled angiographic follow-up might still be considered acceptable for early in vivo or significant coronary device trials.
While the authors said the trial ended up being underpowered because of a reduced final sample size and lower-than-anticipated event rate, it did warrant further larger-scale studies. In particular, they highlighted the question of what impact routine follow-up angiography might have in higher-risk patients, such as those with left main or multivessel coronary artery disease.
“Finally, because patient demographics, practice patterns including the indication of coronary revascularization, and clinical outcomes in Japan may be different from those outside Japan, generalizing the present study results to populations outside Japan should be done with caution.”
This study was supported by an educational grant from the Research Institute for Production Development (Kyoto). One author declared honoraria for education consulting from Boston Scientific Corporation.
Key clinical point: Routine follow-up coronary angiography after percutaneous coronary intervention increases rates of coronary revascularization but does not improve outcomes.
Major finding: Patients who underwent routine angiographic follow-up had a similar cumulative 5-year incidence of all-cause death, myocardial infarction, stroke, or emergency hospitalizations for acute coronary syndrome or heart failure as those who had standard clinical follow-up.
Data source: ReACT: a prospective, open-label randomized controlled trial in 700 patients after percutaneous coronary intervention.
Disclosures: This study was supported by an educational grant from the Research Institute for Production Development (Kyoto). One author declared honoraria for education consulting from Boston Scientific Corporation.