User login
EMERGENCY MEDICINE is a practical, peer-reviewed monthly publication and Web site that meets the educational needs of emergency clinicians and urgent care clinicians for their practice.
Doxycycline Kits Boost Chlamydia Treatment in ED
TOPLINE:
METHODOLOGY:
- A single-center retrospective chart review included adults with positive chlamydia tests in the ED between 2021 and 2023.
- In total, 98 received doxycycline discharge kits; 72 patients were enrolled before the implementation of discharge kits for comparison.
- There were no differences in symptoms of infection between patients who received and those who did not receive the kit.
- Main outcome was the number of patients who received treatment.
- Secondary outcomes included 90-day return visits for complaints of sexually transmitted infections and time to treatment initiation.
TAKEAWAY:
- Appropriate treatment rates rose significantly post-implementation of the discharge kit (69.1% vs 45.8%; odds ratio, 2.63; P = .002).
- Implementation of the discharge kit also reduced the time to definitive treatment from 22.7 hours to 1.3 hours (P < .001).
- No significant differences in 90-day ED return visits, time to initial treatment in the ED, and doxycycline prescription via culture callback programs between the two groups.
IN PRACTICE:
“Pharmacy-driven doxycycline discharge kits significantly increased guideline-directed treatment and decreased time to treatment for chlamydia infections in the ED population at an urban academic medical center,” the authors wrote. “Overall, this initiative overcame barriers to treatment for a significant public health issue, supporting the need for expansion to other emergency departments across the country.”
SOURCE:
The study was led by Carly Loudermilk, Department of Pharmacy, Louisville, Kentucky, and was published online on November 14, 2024, in The American Journal of Emergency Medicine.
LIMITATIONS:
Retrospective design is the main limitation and lack of insurance fill history in some patients.
DISCLOSURES:
The study received no external funding. The authors disclosed no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A single-center retrospective chart review included adults with positive chlamydia tests in the ED between 2021 and 2023.
- In total, 98 received doxycycline discharge kits; 72 patients were enrolled before the implementation of discharge kits for comparison.
- There were no differences in symptoms of infection between patients who received and those who did not receive the kit.
- Main outcome was the number of patients who received treatment.
- Secondary outcomes included 90-day return visits for complaints of sexually transmitted infections and time to treatment initiation.
TAKEAWAY:
- Appropriate treatment rates rose significantly post-implementation of the discharge kit (69.1% vs 45.8%; odds ratio, 2.63; P = .002).
- Implementation of the discharge kit also reduced the time to definitive treatment from 22.7 hours to 1.3 hours (P < .001).
- No significant differences in 90-day ED return visits, time to initial treatment in the ED, and doxycycline prescription via culture callback programs between the two groups.
IN PRACTICE:
“Pharmacy-driven doxycycline discharge kits significantly increased guideline-directed treatment and decreased time to treatment for chlamydia infections in the ED population at an urban academic medical center,” the authors wrote. “Overall, this initiative overcame barriers to treatment for a significant public health issue, supporting the need for expansion to other emergency departments across the country.”
SOURCE:
The study was led by Carly Loudermilk, Department of Pharmacy, Louisville, Kentucky, and was published online on November 14, 2024, in The American Journal of Emergency Medicine.
LIMITATIONS:
Retrospective design is the main limitation and lack of insurance fill history in some patients.
DISCLOSURES:
The study received no external funding. The authors disclosed no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A single-center retrospective chart review included adults with positive chlamydia tests in the ED between 2021 and 2023.
- In total, 98 received doxycycline discharge kits; 72 patients were enrolled before the implementation of discharge kits for comparison.
- There were no differences in symptoms of infection between patients who received and those who did not receive the kit.
- Main outcome was the number of patients who received treatment.
- Secondary outcomes included 90-day return visits for complaints of sexually transmitted infections and time to treatment initiation.
TAKEAWAY:
- Appropriate treatment rates rose significantly post-implementation of the discharge kit (69.1% vs 45.8%; odds ratio, 2.63; P = .002).
- Implementation of the discharge kit also reduced the time to definitive treatment from 22.7 hours to 1.3 hours (P < .001).
- No significant differences in 90-day ED return visits, time to initial treatment in the ED, and doxycycline prescription via culture callback programs between the two groups.
IN PRACTICE:
“Pharmacy-driven doxycycline discharge kits significantly increased guideline-directed treatment and decreased time to treatment for chlamydia infections in the ED population at an urban academic medical center,” the authors wrote. “Overall, this initiative overcame barriers to treatment for a significant public health issue, supporting the need for expansion to other emergency departments across the country.”
SOURCE:
The study was led by Carly Loudermilk, Department of Pharmacy, Louisville, Kentucky, and was published online on November 14, 2024, in The American Journal of Emergency Medicine.
LIMITATIONS:
Retrospective design is the main limitation and lack of insurance fill history in some patients.
DISCLOSURES:
The study received no external funding. The authors disclosed no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Residency to Reality: The Job Outlook for New Docs
Roshan Bransden didn’t count how many job offers she received during her recently completed training in family medicine. “It was pretty nonstop throughout all of my PGY-3 year,” she said.
Most of the job opportunities were different from the type of position she sought or where she wanted to work. Bransden graduated from residency at Montefiore Hospital in New York and accepted a position as a primary care doctor in Miami, close to where she grew up and where her family lives.
More than half (56%) of all residents in AMN Healthcare’s 2023 Survey of Final-Year Medical Residents received 100 or more job solicitations during their training, the highest figure since the survey began more than 30 years ago, the staffing agency reported.
Employers are recruiting residents earlier, offering residency stipends of $1500 to $2500 up to 18 months before they finish their training if they commit to an employment contract, said Leah Grant, president of AMN Healthcare’s Physician Permanent Solutions division, specializing in doctor recruitment. She said that the company’s clients are already eyeing residents completing their training in 2026.
“The key for residents is not about finding a position but choosing the right one out of many.” Grant added that residents typically aren’t taught negotiation skills or how to evaluate job offers. They tend to choose a position based on location, but they should also consider work–life balance issues such as call schedules and whether incentives such as signing bonuses, relocation allowances, and student loan reimbursement offset the job’s time commitment.
“If you are a physician and you are willing to go anywhere, you will have hundreds of opportunities,” said Tibor Nagy, DO, an emergency medicine fellow who recently searched for jobs. “It depends on what they want out of their careers.”
Location Is a Key Consideration
Nagy said he had fewer options because he was limited by location, staying close to where his wife is finishing her internal medicine residency. He is completing his fellowship at Atrium Health Carolinas Medical Center in Charlotte, North Carolina, and preparing to return to Prisma Health in Greenville, South Carolina, where he did his residency.
He said that the job search was easier than he anticipated considering the tight market following a job report from the American College of Emergency Physicians in 2021 that predicted an oversupply of 8000 emergency medicine physicians by 2030.
Halfway through Nagy’s residency, he sought a fellowship in emergency medical services (EMS) to be more competitive in the job market. After that, “Every door I knocked on was open to hiring. Maybe it’s a regional thing. They were happy to interview me.”
In addition to location, Nagy’s top priorities when choosing a job were stability and being able to use his EMS fellowship to become a medical director of an EMS system, agency, or fire department. He wanted to work for a hospital system with an academic focus without much employee turnover.
Salary vs Benefits
AMN Healthcare received the most physician searches for family medicine doctors, followed by OB/GYNs. The staffing agency reported that close to two thirds (63%) of its search engagements during the 2023-2024 review period were for specialists, reflecting the needs of an aging population.
The highest average starting salaries were for surgical and internal medicine subspecialties, according to AMN Healthcare’s 2024 Physician and Advanced Practitioner Recruiting Incentives. Orthopedic surgery averaged $633,000; urology, $540,000; gastroenterology, $506,000; and pulmonary medicine, $418,000. For comparison, the average starting salaries for primary care doctors were family medicine, $255,000; internal medicine, $255,000; and pediatrics, $233,000.
In addition to starting salaries, many physicians receive signing bonuses, relocation allowances, and continuing medical education (CME) allowances. According to the report, the average signing bonus for physicians was $31,473. The average relocation allowance for physicians was $11,284 and the average CME allowance was $3969.
Salary wasn’t Nagy’s top priority when choosing a job, though he admits that the ability to pay back thousands of dollars in medical school loans will be helpful. Instead of focusing on higher pay to offset student loans, Nagy said he sought nonprofit positions to help him qualify for public service loan forgiveness.
The federal program forgives loan balances after the recipient makes monthly payments for 10 years while working for a government or nonprofit organization. He also racked up 3 years of residency and his fellowship year at nonprofit hospitals toward that commitment.
He said jobs that pay more may require doctors to see more patients. “The hustle may be different. There are definitely tradeoffs,” he said.
Bransden said the position she begins in January will allow her to work part-time with full benefits, among other perks. “My employer is a membership-based practice, so I’ll be able to gift a few memberships to family and friends.”
Going Solo
Mohammad Ibrahim, DO, is among a minority of new physicians who have chosen to set up their own practice.
Only 6% of residents in AMN Healthcare’s 2024 report indicated that a solo practice was among their top two choices, while 20% listed partnering with another physician.
Ibrahim is a sports medicine fellow at the University of Michigan Health-West in Wyoming, after finishing his family medicine residency at Trinity Health Livingston Hospital in Howell, Michigan.
After his fellowship ends, he said he plans to stay in Michigan, where his family lives.
Ibrahim said he began his medical education knowing he wanted to become a solo clinician in private practice. He sees it as a way to have more control over his decisions about patient care and business practices.
Working in a hospital often requires doctors to gain approval from several levels of authority for decisions such as ordering new equipment or forgiving part of a service payment. He also wanted to set his schedule to take Friday afternoons off for Muslim prayer.
Although he realizes the challenges of starting a private practice, Ibrahim said those who go through graduate medical education can figure out how to adapt and overcome any obstacles. “I think it’s more doable than we are led to believe.”
He said that if more residents were exposed to private practice, they might pursue that path. During his training, Ibrahim did a rotation with a private practice physician. “It’s nice to see people proud of what they built, what they contributed.”
Most residents don’t choose private practice. In the AMN Healthcare survey, 68% of residents said that employment by a hospital was among their top two choices for a practice setting, 42% said employment by a single-specialty group, and 32%, employment by a multispecialty group.
Of the majority of job searches AMN Healthcare conducted, 28% were to fill positions in hospital settings, followed by 26% for medical groups, 22% for academic medical centers, 13% for urgent care centers and retail clinics, 6% for solo practices, partnerships, or concierge practice settings, and 5% for Federally Qualified Health Centers/Community Health Centers or Indian Health facilities.
Still, the report noted an increase in recruiting for independent medical practice ownership, which dwindled in recent years, with the majority of doctors today employed likely due to financial obstacles of starting a practice.
The increase in recruiting indicates possible renewed interest in these practice settings, particularly concierge medicine, which allows doctors to avoid the challenges of third-party payments, the report stated.
Grant said that despite the flexibility and financial autonomy of starting their own practice, new providers who choose this path face obstacles, such as competing with urgent care centers and retail health clinics, which have been on the rise in the past year.
Saddled with debt from medical training, most graduating residents will choose to work toward financial stability and then consider their own practice later in their career, she said.
Flexible Schedules
Work schedule/call hours or work-life balance was the biggest factor (36%) guiding residents’ choice of first post-residency positions compared with starting salary (19%), according to the Medscape Resident Salary & Debt Report 2024.
Grant said that larger practices and those closer to rural communities tend to offer more innovative work schedules, especially for certain specialists. Some solo practices that form partnerships could potentially allow flexible schedules such as 4-day work weeks or week-on-week-off arrangements, she added.
Physicians are also opting for the flexibility of temporary, locum tenens work to improve job conditions and address feelings of burnout. Dr. Kaydo, DO, as she’s known on Instagram, posts about her experiences as locum tenens. “I found that I could have more flexibility as a locum. I want to be able to take time off when I want and as long as I wanted,” said the full-time family medicine doctor who practices at an outpatient clinic in Philadelphia.
“Basically, I’m contract-working, and they pay me as much as I work, and I can also take more time off.” Her employer for the past year also allowed her to work 10 hours a day, 4 days a week instead of the more traditional 8-hour, 5-day schedule.
Dr. Kaydo said she believes many young doctors think contract employees don’t have a permanent job, are not guaranteed a certain salary, and could easily lose their jobs. “I’ve found that most places really need doctors and are willing to negotiate.”
She said primary care locum doctors are particularly in demand in rural clinics and urban underserved areas.
Nagy said he is considering being a nocturnist, an emergency medicine doctor who works nights, to have more control over his schedule, higher pay, and more flexible shifts. “I switch days and nights and that can be tiring.”
Bransden said job flexibility was her primary job criterion. “I have a young child, so I wanted to work part-time with the potential for even more flexibility down the line. I am working 3 days a week, 8-hour days with a 1-hour break. A 3-day work week came with a pay cut, but for me, it works and is what I need right now.”
A version of this article appeared on Medscape.com.
Roshan Bransden didn’t count how many job offers she received during her recently completed training in family medicine. “It was pretty nonstop throughout all of my PGY-3 year,” she said.
Most of the job opportunities were different from the type of position she sought or where she wanted to work. Bransden graduated from residency at Montefiore Hospital in New York and accepted a position as a primary care doctor in Miami, close to where she grew up and where her family lives.
More than half (56%) of all residents in AMN Healthcare’s 2023 Survey of Final-Year Medical Residents received 100 or more job solicitations during their training, the highest figure since the survey began more than 30 years ago, the staffing agency reported.
Employers are recruiting residents earlier, offering residency stipends of $1500 to $2500 up to 18 months before they finish their training if they commit to an employment contract, said Leah Grant, president of AMN Healthcare’s Physician Permanent Solutions division, specializing in doctor recruitment. She said that the company’s clients are already eyeing residents completing their training in 2026.
“The key for residents is not about finding a position but choosing the right one out of many.” Grant added that residents typically aren’t taught negotiation skills or how to evaluate job offers. They tend to choose a position based on location, but they should also consider work–life balance issues such as call schedules and whether incentives such as signing bonuses, relocation allowances, and student loan reimbursement offset the job’s time commitment.
“If you are a physician and you are willing to go anywhere, you will have hundreds of opportunities,” said Tibor Nagy, DO, an emergency medicine fellow who recently searched for jobs. “It depends on what they want out of their careers.”
Location Is a Key Consideration
Nagy said he had fewer options because he was limited by location, staying close to where his wife is finishing her internal medicine residency. He is completing his fellowship at Atrium Health Carolinas Medical Center in Charlotte, North Carolina, and preparing to return to Prisma Health in Greenville, South Carolina, where he did his residency.
He said that the job search was easier than he anticipated considering the tight market following a job report from the American College of Emergency Physicians in 2021 that predicted an oversupply of 8000 emergency medicine physicians by 2030.
Halfway through Nagy’s residency, he sought a fellowship in emergency medical services (EMS) to be more competitive in the job market. After that, “Every door I knocked on was open to hiring. Maybe it’s a regional thing. They were happy to interview me.”
In addition to location, Nagy’s top priorities when choosing a job were stability and being able to use his EMS fellowship to become a medical director of an EMS system, agency, or fire department. He wanted to work for a hospital system with an academic focus without much employee turnover.
Salary vs Benefits
AMN Healthcare received the most physician searches for family medicine doctors, followed by OB/GYNs. The staffing agency reported that close to two thirds (63%) of its search engagements during the 2023-2024 review period were for specialists, reflecting the needs of an aging population.
The highest average starting salaries were for surgical and internal medicine subspecialties, according to AMN Healthcare’s 2024 Physician and Advanced Practitioner Recruiting Incentives. Orthopedic surgery averaged $633,000; urology, $540,000; gastroenterology, $506,000; and pulmonary medicine, $418,000. For comparison, the average starting salaries for primary care doctors were family medicine, $255,000; internal medicine, $255,000; and pediatrics, $233,000.
In addition to starting salaries, many physicians receive signing bonuses, relocation allowances, and continuing medical education (CME) allowances. According to the report, the average signing bonus for physicians was $31,473. The average relocation allowance for physicians was $11,284 and the average CME allowance was $3969.
Salary wasn’t Nagy’s top priority when choosing a job, though he admits that the ability to pay back thousands of dollars in medical school loans will be helpful. Instead of focusing on higher pay to offset student loans, Nagy said he sought nonprofit positions to help him qualify for public service loan forgiveness.
The federal program forgives loan balances after the recipient makes monthly payments for 10 years while working for a government or nonprofit organization. He also racked up 3 years of residency and his fellowship year at nonprofit hospitals toward that commitment.
He said jobs that pay more may require doctors to see more patients. “The hustle may be different. There are definitely tradeoffs,” he said.
Bransden said the position she begins in January will allow her to work part-time with full benefits, among other perks. “My employer is a membership-based practice, so I’ll be able to gift a few memberships to family and friends.”
Going Solo
Mohammad Ibrahim, DO, is among a minority of new physicians who have chosen to set up their own practice.
Only 6% of residents in AMN Healthcare’s 2024 report indicated that a solo practice was among their top two choices, while 20% listed partnering with another physician.
Ibrahim is a sports medicine fellow at the University of Michigan Health-West in Wyoming, after finishing his family medicine residency at Trinity Health Livingston Hospital in Howell, Michigan.
After his fellowship ends, he said he plans to stay in Michigan, where his family lives.
Ibrahim said he began his medical education knowing he wanted to become a solo clinician in private practice. He sees it as a way to have more control over his decisions about patient care and business practices.
Working in a hospital often requires doctors to gain approval from several levels of authority for decisions such as ordering new equipment or forgiving part of a service payment. He also wanted to set his schedule to take Friday afternoons off for Muslim prayer.
Although he realizes the challenges of starting a private practice, Ibrahim said those who go through graduate medical education can figure out how to adapt and overcome any obstacles. “I think it’s more doable than we are led to believe.”
He said that if more residents were exposed to private practice, they might pursue that path. During his training, Ibrahim did a rotation with a private practice physician. “It’s nice to see people proud of what they built, what they contributed.”
Most residents don’t choose private practice. In the AMN Healthcare survey, 68% of residents said that employment by a hospital was among their top two choices for a practice setting, 42% said employment by a single-specialty group, and 32%, employment by a multispecialty group.
Of the majority of job searches AMN Healthcare conducted, 28% were to fill positions in hospital settings, followed by 26% for medical groups, 22% for academic medical centers, 13% for urgent care centers and retail clinics, 6% for solo practices, partnerships, or concierge practice settings, and 5% for Federally Qualified Health Centers/Community Health Centers or Indian Health facilities.
Still, the report noted an increase in recruiting for independent medical practice ownership, which dwindled in recent years, with the majority of doctors today employed likely due to financial obstacles of starting a practice.
The increase in recruiting indicates possible renewed interest in these practice settings, particularly concierge medicine, which allows doctors to avoid the challenges of third-party payments, the report stated.
Grant said that despite the flexibility and financial autonomy of starting their own practice, new providers who choose this path face obstacles, such as competing with urgent care centers and retail health clinics, which have been on the rise in the past year.
Saddled with debt from medical training, most graduating residents will choose to work toward financial stability and then consider their own practice later in their career, she said.
Flexible Schedules
Work schedule/call hours or work-life balance was the biggest factor (36%) guiding residents’ choice of first post-residency positions compared with starting salary (19%), according to the Medscape Resident Salary & Debt Report 2024.
Grant said that larger practices and those closer to rural communities tend to offer more innovative work schedules, especially for certain specialists. Some solo practices that form partnerships could potentially allow flexible schedules such as 4-day work weeks or week-on-week-off arrangements, she added.
Physicians are also opting for the flexibility of temporary, locum tenens work to improve job conditions and address feelings of burnout. Dr. Kaydo, DO, as she’s known on Instagram, posts about her experiences as locum tenens. “I found that I could have more flexibility as a locum. I want to be able to take time off when I want and as long as I wanted,” said the full-time family medicine doctor who practices at an outpatient clinic in Philadelphia.
“Basically, I’m contract-working, and they pay me as much as I work, and I can also take more time off.” Her employer for the past year also allowed her to work 10 hours a day, 4 days a week instead of the more traditional 8-hour, 5-day schedule.
Dr. Kaydo said she believes many young doctors think contract employees don’t have a permanent job, are not guaranteed a certain salary, and could easily lose their jobs. “I’ve found that most places really need doctors and are willing to negotiate.”
She said primary care locum doctors are particularly in demand in rural clinics and urban underserved areas.
Nagy said he is considering being a nocturnist, an emergency medicine doctor who works nights, to have more control over his schedule, higher pay, and more flexible shifts. “I switch days and nights and that can be tiring.”
Bransden said job flexibility was her primary job criterion. “I have a young child, so I wanted to work part-time with the potential for even more flexibility down the line. I am working 3 days a week, 8-hour days with a 1-hour break. A 3-day work week came with a pay cut, but for me, it works and is what I need right now.”
A version of this article appeared on Medscape.com.
Roshan Bransden didn’t count how many job offers she received during her recently completed training in family medicine. “It was pretty nonstop throughout all of my PGY-3 year,” she said.
Most of the job opportunities were different from the type of position she sought or where she wanted to work. Bransden graduated from residency at Montefiore Hospital in New York and accepted a position as a primary care doctor in Miami, close to where she grew up and where her family lives.
More than half (56%) of all residents in AMN Healthcare’s 2023 Survey of Final-Year Medical Residents received 100 or more job solicitations during their training, the highest figure since the survey began more than 30 years ago, the staffing agency reported.
Employers are recruiting residents earlier, offering residency stipends of $1500 to $2500 up to 18 months before they finish their training if they commit to an employment contract, said Leah Grant, president of AMN Healthcare’s Physician Permanent Solutions division, specializing in doctor recruitment. She said that the company’s clients are already eyeing residents completing their training in 2026.
“The key for residents is not about finding a position but choosing the right one out of many.” Grant added that residents typically aren’t taught negotiation skills or how to evaluate job offers. They tend to choose a position based on location, but they should also consider work–life balance issues such as call schedules and whether incentives such as signing bonuses, relocation allowances, and student loan reimbursement offset the job’s time commitment.
“If you are a physician and you are willing to go anywhere, you will have hundreds of opportunities,” said Tibor Nagy, DO, an emergency medicine fellow who recently searched for jobs. “It depends on what they want out of their careers.”
Location Is a Key Consideration
Nagy said he had fewer options because he was limited by location, staying close to where his wife is finishing her internal medicine residency. He is completing his fellowship at Atrium Health Carolinas Medical Center in Charlotte, North Carolina, and preparing to return to Prisma Health in Greenville, South Carolina, where he did his residency.
He said that the job search was easier than he anticipated considering the tight market following a job report from the American College of Emergency Physicians in 2021 that predicted an oversupply of 8000 emergency medicine physicians by 2030.
Halfway through Nagy’s residency, he sought a fellowship in emergency medical services (EMS) to be more competitive in the job market. After that, “Every door I knocked on was open to hiring. Maybe it’s a regional thing. They were happy to interview me.”
In addition to location, Nagy’s top priorities when choosing a job were stability and being able to use his EMS fellowship to become a medical director of an EMS system, agency, or fire department. He wanted to work for a hospital system with an academic focus without much employee turnover.
Salary vs Benefits
AMN Healthcare received the most physician searches for family medicine doctors, followed by OB/GYNs. The staffing agency reported that close to two thirds (63%) of its search engagements during the 2023-2024 review period were for specialists, reflecting the needs of an aging population.
The highest average starting salaries were for surgical and internal medicine subspecialties, according to AMN Healthcare’s 2024 Physician and Advanced Practitioner Recruiting Incentives. Orthopedic surgery averaged $633,000; urology, $540,000; gastroenterology, $506,000; and pulmonary medicine, $418,000. For comparison, the average starting salaries for primary care doctors were family medicine, $255,000; internal medicine, $255,000; and pediatrics, $233,000.
In addition to starting salaries, many physicians receive signing bonuses, relocation allowances, and continuing medical education (CME) allowances. According to the report, the average signing bonus for physicians was $31,473. The average relocation allowance for physicians was $11,284 and the average CME allowance was $3969.
Salary wasn’t Nagy’s top priority when choosing a job, though he admits that the ability to pay back thousands of dollars in medical school loans will be helpful. Instead of focusing on higher pay to offset student loans, Nagy said he sought nonprofit positions to help him qualify for public service loan forgiveness.
The federal program forgives loan balances after the recipient makes monthly payments for 10 years while working for a government or nonprofit organization. He also racked up 3 years of residency and his fellowship year at nonprofit hospitals toward that commitment.
He said jobs that pay more may require doctors to see more patients. “The hustle may be different. There are definitely tradeoffs,” he said.
Bransden said the position she begins in January will allow her to work part-time with full benefits, among other perks. “My employer is a membership-based practice, so I’ll be able to gift a few memberships to family and friends.”
Going Solo
Mohammad Ibrahim, DO, is among a minority of new physicians who have chosen to set up their own practice.
Only 6% of residents in AMN Healthcare’s 2024 report indicated that a solo practice was among their top two choices, while 20% listed partnering with another physician.
Ibrahim is a sports medicine fellow at the University of Michigan Health-West in Wyoming, after finishing his family medicine residency at Trinity Health Livingston Hospital in Howell, Michigan.
After his fellowship ends, he said he plans to stay in Michigan, where his family lives.
Ibrahim said he began his medical education knowing he wanted to become a solo clinician in private practice. He sees it as a way to have more control over his decisions about patient care and business practices.
Working in a hospital often requires doctors to gain approval from several levels of authority for decisions such as ordering new equipment or forgiving part of a service payment. He also wanted to set his schedule to take Friday afternoons off for Muslim prayer.
Although he realizes the challenges of starting a private practice, Ibrahim said those who go through graduate medical education can figure out how to adapt and overcome any obstacles. “I think it’s more doable than we are led to believe.”
He said that if more residents were exposed to private practice, they might pursue that path. During his training, Ibrahim did a rotation with a private practice physician. “It’s nice to see people proud of what they built, what they contributed.”
Most residents don’t choose private practice. In the AMN Healthcare survey, 68% of residents said that employment by a hospital was among their top two choices for a practice setting, 42% said employment by a single-specialty group, and 32%, employment by a multispecialty group.
Of the majority of job searches AMN Healthcare conducted, 28% were to fill positions in hospital settings, followed by 26% for medical groups, 22% for academic medical centers, 13% for urgent care centers and retail clinics, 6% for solo practices, partnerships, or concierge practice settings, and 5% for Federally Qualified Health Centers/Community Health Centers or Indian Health facilities.
Still, the report noted an increase in recruiting for independent medical practice ownership, which dwindled in recent years, with the majority of doctors today employed likely due to financial obstacles of starting a practice.
The increase in recruiting indicates possible renewed interest in these practice settings, particularly concierge medicine, which allows doctors to avoid the challenges of third-party payments, the report stated.
Grant said that despite the flexibility and financial autonomy of starting their own practice, new providers who choose this path face obstacles, such as competing with urgent care centers and retail health clinics, which have been on the rise in the past year.
Saddled with debt from medical training, most graduating residents will choose to work toward financial stability and then consider their own practice later in their career, she said.
Flexible Schedules
Work schedule/call hours or work-life balance was the biggest factor (36%) guiding residents’ choice of first post-residency positions compared with starting salary (19%), according to the Medscape Resident Salary & Debt Report 2024.
Grant said that larger practices and those closer to rural communities tend to offer more innovative work schedules, especially for certain specialists. Some solo practices that form partnerships could potentially allow flexible schedules such as 4-day work weeks or week-on-week-off arrangements, she added.
Physicians are also opting for the flexibility of temporary, locum tenens work to improve job conditions and address feelings of burnout. Dr. Kaydo, DO, as she’s known on Instagram, posts about her experiences as locum tenens. “I found that I could have more flexibility as a locum. I want to be able to take time off when I want and as long as I wanted,” said the full-time family medicine doctor who practices at an outpatient clinic in Philadelphia.
“Basically, I’m contract-working, and they pay me as much as I work, and I can also take more time off.” Her employer for the past year also allowed her to work 10 hours a day, 4 days a week instead of the more traditional 8-hour, 5-day schedule.
Dr. Kaydo said she believes many young doctors think contract employees don’t have a permanent job, are not guaranteed a certain salary, and could easily lose their jobs. “I’ve found that most places really need doctors and are willing to negotiate.”
She said primary care locum doctors are particularly in demand in rural clinics and urban underserved areas.
Nagy said he is considering being a nocturnist, an emergency medicine doctor who works nights, to have more control over his schedule, higher pay, and more flexible shifts. “I switch days and nights and that can be tiring.”
Bransden said job flexibility was her primary job criterion. “I have a young child, so I wanted to work part-time with the potential for even more flexibility down the line. I am working 3 days a week, 8-hour days with a 1-hour break. A 3-day work week came with a pay cut, but for me, it works and is what I need right now.”
A version of this article appeared on Medscape.com.
High-Volume Burn Resuscitation Increases Neurologic Risk
TOPLINE:
METHODOLOGY:
- Researchers conducted a single-center review of 5176 patients with burn injuries who were admitted to a verified American Burn Association center (2003-2017); 622 of them underwent head CT within 96 hours of admission, and 83 showed intracranial abnormalities.
- Of 42 patients (mean age, 49.7 years; 80.5% men) who were admitted within 24 hours of burn, 30 patients received < 200 mL/kg and 11 received > 200 mL/kg of total resuscitation fluids, with a median total body surface area (TBSA) of 20.0.
- The primary outcome assessed was the worsening of neurologic findings on imaging related to the volume of the resuscitation fluid administered; the secondary outcomes were the incidence of new or worsening intracranial abnormalities, including hemorrhage, edema, ischemia, or infarction.
TAKEAWAY:
- Neurologic findings worsened in 47.6% patients receiving < 200 mL/kg of fluid resuscitation and 85.7% of those receiving > 200 mL/kg (P =.064).
- Repeat imaging was performed in 21 (70.0%) patients receiving < 200 mL/kg and 7 (63.6%) patients receiving > 200 mL/kg of resuscitation who underwent follow-up imaging.
- The median TBSA was 16.5 in the < 200 mL/kg group and 53.2 in the > 200 mL/kg group (P <.001).
- Intracranial abnormalities were found in 31.3% patients with hemorrhage, 18.8% with worsening edema, and 43.8% with ischemia or infarction.
IN PRACTICE:
“Patients who received over 200 mL/kg of resuscitation had an increased progression of intracranial abnormalities when compared with patients receiving less volume resuscitation,” the authors wrote. “Neurologic changes prompting imaging in burn patients may be undetectable, and our study further highlights the need for routine evaluation with neurologic imaging when undergoing large-volume resuscitations.”
SOURCE:
The study was led by Connor L. Kenney, MD, Brooke Army Medical Center, San Antonio, and was published online on November 07, 2024, in the Journal of Surgical Research.
LIMITATIONS:
Study limitations included a small patient sample and unclear guidelines for obtaining head CT scans, making it difficult to distinguish between trauma-related brain changes and disease progression. Additionally, the study lacked data on hypotensive episodes and long-term neurologic outcomes.
DISCLOSURES:
This study did not receive any specific funding. The authors declared no conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a single-center review of 5176 patients with burn injuries who were admitted to a verified American Burn Association center (2003-2017); 622 of them underwent head CT within 96 hours of admission, and 83 showed intracranial abnormalities.
- Of 42 patients (mean age, 49.7 years; 80.5% men) who were admitted within 24 hours of burn, 30 patients received < 200 mL/kg and 11 received > 200 mL/kg of total resuscitation fluids, with a median total body surface area (TBSA) of 20.0.
- The primary outcome assessed was the worsening of neurologic findings on imaging related to the volume of the resuscitation fluid administered; the secondary outcomes were the incidence of new or worsening intracranial abnormalities, including hemorrhage, edema, ischemia, or infarction.
TAKEAWAY:
- Neurologic findings worsened in 47.6% patients receiving < 200 mL/kg of fluid resuscitation and 85.7% of those receiving > 200 mL/kg (P =.064).
- Repeat imaging was performed in 21 (70.0%) patients receiving < 200 mL/kg and 7 (63.6%) patients receiving > 200 mL/kg of resuscitation who underwent follow-up imaging.
- The median TBSA was 16.5 in the < 200 mL/kg group and 53.2 in the > 200 mL/kg group (P <.001).
- Intracranial abnormalities were found in 31.3% patients with hemorrhage, 18.8% with worsening edema, and 43.8% with ischemia or infarction.
IN PRACTICE:
“Patients who received over 200 mL/kg of resuscitation had an increased progression of intracranial abnormalities when compared with patients receiving less volume resuscitation,” the authors wrote. “Neurologic changes prompting imaging in burn patients may be undetectable, and our study further highlights the need for routine evaluation with neurologic imaging when undergoing large-volume resuscitations.”
SOURCE:
The study was led by Connor L. Kenney, MD, Brooke Army Medical Center, San Antonio, and was published online on November 07, 2024, in the Journal of Surgical Research.
LIMITATIONS:
Study limitations included a small patient sample and unclear guidelines for obtaining head CT scans, making it difficult to distinguish between trauma-related brain changes and disease progression. Additionally, the study lacked data on hypotensive episodes and long-term neurologic outcomes.
DISCLOSURES:
This study did not receive any specific funding. The authors declared no conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a single-center review of 5176 patients with burn injuries who were admitted to a verified American Burn Association center (2003-2017); 622 of them underwent head CT within 96 hours of admission, and 83 showed intracranial abnormalities.
- Of 42 patients (mean age, 49.7 years; 80.5% men) who were admitted within 24 hours of burn, 30 patients received < 200 mL/kg and 11 received > 200 mL/kg of total resuscitation fluids, with a median total body surface area (TBSA) of 20.0.
- The primary outcome assessed was the worsening of neurologic findings on imaging related to the volume of the resuscitation fluid administered; the secondary outcomes were the incidence of new or worsening intracranial abnormalities, including hemorrhage, edema, ischemia, or infarction.
TAKEAWAY:
- Neurologic findings worsened in 47.6% patients receiving < 200 mL/kg of fluid resuscitation and 85.7% of those receiving > 200 mL/kg (P =.064).
- Repeat imaging was performed in 21 (70.0%) patients receiving < 200 mL/kg and 7 (63.6%) patients receiving > 200 mL/kg of resuscitation who underwent follow-up imaging.
- The median TBSA was 16.5 in the < 200 mL/kg group and 53.2 in the > 200 mL/kg group (P <.001).
- Intracranial abnormalities were found in 31.3% patients with hemorrhage, 18.8% with worsening edema, and 43.8% with ischemia or infarction.
IN PRACTICE:
“Patients who received over 200 mL/kg of resuscitation had an increased progression of intracranial abnormalities when compared with patients receiving less volume resuscitation,” the authors wrote. “Neurologic changes prompting imaging in burn patients may be undetectable, and our study further highlights the need for routine evaluation with neurologic imaging when undergoing large-volume resuscitations.”
SOURCE:
The study was led by Connor L. Kenney, MD, Brooke Army Medical Center, San Antonio, and was published online on November 07, 2024, in the Journal of Surgical Research.
LIMITATIONS:
Study limitations included a small patient sample and unclear guidelines for obtaining head CT scans, making it difficult to distinguish between trauma-related brain changes and disease progression. Additionally, the study lacked data on hypotensive episodes and long-term neurologic outcomes.
DISCLOSURES:
This study did not receive any specific funding. The authors declared no conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Key Updates in Resuscitation Procedure After Drowning
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
From Pediatrics
A New, Easily Identifiable Sign of Concussion?
Spontaneous Headshake After a Kinematic Event (SHAAKE) refers to the rapid, back-and-forth head movement athletes exhibit following a blow to the head. This voluntary motion typically occurs within seconds to minutes after impact and is a familiar response in athletes.
In a recent survey, 7 out of 10 adult athletes recalled making this movement after a collision, and three out of four times they attributed this back-and-forth head movement to a concussion. The association was strongest among football players, who reported that over 90% of SHAAKE episodes were associated with a concussion.
The results were published online in Diagnostics.
Call to Action
“Everyone” — including sports and medical organizations — “should be adding this to their list of potential concussion signs and their protocol immediately,” study investigator Chris Nowinski, PhD, CEO and co-founder of the Concussion Legacy Foundation, told this news organization.
Nowinski said it’s “fascinating” that this concussion sign hasn’t been formally studied or added to formal concussion screening metrics before now, given that it’s been depicted in movies, television, and cartoons for decades.
Coaches, medical professionals, and concussion spotters should be trained to recognize when a SHAAKE happens, he said.
“The interesting thing is, I don’t think coaches or parents need much training other than to officially tie this to suspicion of a concussion,” Nowinski added.
The Case of Miami Dolphins QB Tua Tagovailoa
Nowinski said he was tipped off to SHAAKE as a concussion sign after Miami Dolphins quarterback Tua Tagovailoa’s controversial undiagnosed concussion during a National Football League (NFL) game in 2022.
After Tagovailoa’s head hit the ground, he rapidly shook his head side to side, indicating displaying SHAAKE, before stumbling and collapsing. At the time, a sideline doctor attributed his collapse to a prior back injury.
If Tagovailoa had been diagnosed with a concussion, he likely would not have been playing in a game just 4 days later, where he lost consciousness after suffering a suspected second concussion and was removed from the field on a stretcher.
For the survey, Nowinski and colleagues showed 347 current and former athletes, including 109 football players, video examples of SHAAKE and them asked about their experiences with this potential indicator of concussion.
Nearly 69% of athletes reported exhibiting a SHAAKE during their career, and 93% of those reported a SHAAKE in association with concussion at least once. Athletes reported SHAAKE a median of five times in their lives.
Of the athletes who reported SHAAKE, 85% linked this head-shaking movement to concussion symptoms such as disorientation (71%) and dizziness (54%).
Across all sports, SHAAKE showed a sensitivity of 49.6% and a positive predictive value (PPV) of 72.4% for diagnosing concussions.
Among football players, sensitivity improved to 52.3%, with an estimated specificity of 99.9%, a PPV of 91.9%, and an estimated negative predictive value of 99.5%.
The main limitation of the survey was the potential for recall bias due to survey participants self-reporting prior concussions. The researchers called for future prospective studies to validate SHAAKE as a sign of concussion.
Instant Replay for Brain Injury?
Experts echoed the need for validation. SHAAKE represents a “promising advance” in objective TBI assessment, particularly for sideline evaluation, said Shaheen Lakhan, MD, PhD, neurologist, and researcher based in Miami, Florida, who wasn’t involved in the research.
The potential value of SHAAKE is “particularly notable given the well-documented tendency for athletes to minimize or conceal symptoms to maintain play eligibility, a limitation that has historically challenged our reliance on subjective reporting and observational assessments,” Lakhan said.
“Moving forward, validation through prospective studies incorporating real-time video analysis, helmet sensor data, and clinician-confirmed TBI diagnoses will be essential. With appropriate validation, SHAAKE could emerge as a valuable component of our sideline assessment arsenal, complementing rather than replacing existing diagnostic approaches,” Lakhan said.
“SHAAKE could be the ‘instant replay’ for brain injuries that sports medicine has been waiting for — but like any new technology, we need to make sure it works for every player, not just some,” Lakhan added.
Also weighing in, Richard Figler, MD, director of the Concussion Center, Cleveland Clinic Sports Medicine Center, Cleveland, cautioned that the survey participants were recruited from a concussion registry and self-reported an average of 23 concussions — more than one third of which happened 5-10 years prior — which begs the question, “How much are they actually remembering?”
“Our goal is to make sure that the athletes are safe and that we’re not missing concussions, and we don’t have great tools to start off with. This study opens up the door for some prospective studies [of SHAAKE] moving forward. I think we need more data before this should be listed as a definitive marker,” said Figler, who also wasn’t involved in the study.
In any case, he said, when it comes to suspected concussion in sports, “when in doubt, you sit them out,” Figler said.
This research received no external funding. Nowinski has received travel reimbursement from the NFL Players Association (NFLPA), NFL, World Rugby, WWE, and All Elite Wrestling; served as an expert witness in cases related to concussion and chronic traumatic encephalopathy; and is compensated for speaking appearances and serving on the NFL Concussion Settlement Player Advocacy Committee. Daniel H. Daneshvar served as an expert witness in legal cases involving brain injury and concussion and received funding from the Football Players Health Study at Harvard University, which is funded by the NFLPA and evaluates patients for the MGH Brain and Body TRUST Center, sponsored in part by the NFLPA. Lakhan and Figler had no relevant disclosures.
A version of this article appeared on Medscape.com.
Spontaneous Headshake After a Kinematic Event (SHAAKE) refers to the rapid, back-and-forth head movement athletes exhibit following a blow to the head. This voluntary motion typically occurs within seconds to minutes after impact and is a familiar response in athletes.
In a recent survey, 7 out of 10 adult athletes recalled making this movement after a collision, and three out of four times they attributed this back-and-forth head movement to a concussion. The association was strongest among football players, who reported that over 90% of SHAAKE episodes were associated with a concussion.
The results were published online in Diagnostics.
Call to Action
“Everyone” — including sports and medical organizations — “should be adding this to their list of potential concussion signs and their protocol immediately,” study investigator Chris Nowinski, PhD, CEO and co-founder of the Concussion Legacy Foundation, told this news organization.
Nowinski said it’s “fascinating” that this concussion sign hasn’t been formally studied or added to formal concussion screening metrics before now, given that it’s been depicted in movies, television, and cartoons for decades.
Coaches, medical professionals, and concussion spotters should be trained to recognize when a SHAAKE happens, he said.
“The interesting thing is, I don’t think coaches or parents need much training other than to officially tie this to suspicion of a concussion,” Nowinski added.
The Case of Miami Dolphins QB Tua Tagovailoa
Nowinski said he was tipped off to SHAAKE as a concussion sign after Miami Dolphins quarterback Tua Tagovailoa’s controversial undiagnosed concussion during a National Football League (NFL) game in 2022.
After Tagovailoa’s head hit the ground, he rapidly shook his head side to side, indicating displaying SHAAKE, before stumbling and collapsing. At the time, a sideline doctor attributed his collapse to a prior back injury.
If Tagovailoa had been diagnosed with a concussion, he likely would not have been playing in a game just 4 days later, where he lost consciousness after suffering a suspected second concussion and was removed from the field on a stretcher.
For the survey, Nowinski and colleagues showed 347 current and former athletes, including 109 football players, video examples of SHAAKE and them asked about their experiences with this potential indicator of concussion.
Nearly 69% of athletes reported exhibiting a SHAAKE during their career, and 93% of those reported a SHAAKE in association with concussion at least once. Athletes reported SHAAKE a median of five times in their lives.
Of the athletes who reported SHAAKE, 85% linked this head-shaking movement to concussion symptoms such as disorientation (71%) and dizziness (54%).
Across all sports, SHAAKE showed a sensitivity of 49.6% and a positive predictive value (PPV) of 72.4% for diagnosing concussions.
Among football players, sensitivity improved to 52.3%, with an estimated specificity of 99.9%, a PPV of 91.9%, and an estimated negative predictive value of 99.5%.
The main limitation of the survey was the potential for recall bias due to survey participants self-reporting prior concussions. The researchers called for future prospective studies to validate SHAAKE as a sign of concussion.
Instant Replay for Brain Injury?
Experts echoed the need for validation. SHAAKE represents a “promising advance” in objective TBI assessment, particularly for sideline evaluation, said Shaheen Lakhan, MD, PhD, neurologist, and researcher based in Miami, Florida, who wasn’t involved in the research.
The potential value of SHAAKE is “particularly notable given the well-documented tendency for athletes to minimize or conceal symptoms to maintain play eligibility, a limitation that has historically challenged our reliance on subjective reporting and observational assessments,” Lakhan said.
“Moving forward, validation through prospective studies incorporating real-time video analysis, helmet sensor data, and clinician-confirmed TBI diagnoses will be essential. With appropriate validation, SHAAKE could emerge as a valuable component of our sideline assessment arsenal, complementing rather than replacing existing diagnostic approaches,” Lakhan said.
“SHAAKE could be the ‘instant replay’ for brain injuries that sports medicine has been waiting for — but like any new technology, we need to make sure it works for every player, not just some,” Lakhan added.
Also weighing in, Richard Figler, MD, director of the Concussion Center, Cleveland Clinic Sports Medicine Center, Cleveland, cautioned that the survey participants were recruited from a concussion registry and self-reported an average of 23 concussions — more than one third of which happened 5-10 years prior — which begs the question, “How much are they actually remembering?”
“Our goal is to make sure that the athletes are safe and that we’re not missing concussions, and we don’t have great tools to start off with. This study opens up the door for some prospective studies [of SHAAKE] moving forward. I think we need more data before this should be listed as a definitive marker,” said Figler, who also wasn’t involved in the study.
In any case, he said, when it comes to suspected concussion in sports, “when in doubt, you sit them out,” Figler said.
This research received no external funding. Nowinski has received travel reimbursement from the NFL Players Association (NFLPA), NFL, World Rugby, WWE, and All Elite Wrestling; served as an expert witness in cases related to concussion and chronic traumatic encephalopathy; and is compensated for speaking appearances and serving on the NFL Concussion Settlement Player Advocacy Committee. Daniel H. Daneshvar served as an expert witness in legal cases involving brain injury and concussion and received funding from the Football Players Health Study at Harvard University, which is funded by the NFLPA and evaluates patients for the MGH Brain and Body TRUST Center, sponsored in part by the NFLPA. Lakhan and Figler had no relevant disclosures.
A version of this article appeared on Medscape.com.
Spontaneous Headshake After a Kinematic Event (SHAAKE) refers to the rapid, back-and-forth head movement athletes exhibit following a blow to the head. This voluntary motion typically occurs within seconds to minutes after impact and is a familiar response in athletes.
In a recent survey, 7 out of 10 adult athletes recalled making this movement after a collision, and three out of four times they attributed this back-and-forth head movement to a concussion. The association was strongest among football players, who reported that over 90% of SHAAKE episodes were associated with a concussion.
The results were published online in Diagnostics.
Call to Action
“Everyone” — including sports and medical organizations — “should be adding this to their list of potential concussion signs and their protocol immediately,” study investigator Chris Nowinski, PhD, CEO and co-founder of the Concussion Legacy Foundation, told this news organization.
Nowinski said it’s “fascinating” that this concussion sign hasn’t been formally studied or added to formal concussion screening metrics before now, given that it’s been depicted in movies, television, and cartoons for decades.
Coaches, medical professionals, and concussion spotters should be trained to recognize when a SHAAKE happens, he said.
“The interesting thing is, I don’t think coaches or parents need much training other than to officially tie this to suspicion of a concussion,” Nowinski added.
The Case of Miami Dolphins QB Tua Tagovailoa
Nowinski said he was tipped off to SHAAKE as a concussion sign after Miami Dolphins quarterback Tua Tagovailoa’s controversial undiagnosed concussion during a National Football League (NFL) game in 2022.
After Tagovailoa’s head hit the ground, he rapidly shook his head side to side, indicating displaying SHAAKE, before stumbling and collapsing. At the time, a sideline doctor attributed his collapse to a prior back injury.
If Tagovailoa had been diagnosed with a concussion, he likely would not have been playing in a game just 4 days later, where he lost consciousness after suffering a suspected second concussion and was removed from the field on a stretcher.
For the survey, Nowinski and colleagues showed 347 current and former athletes, including 109 football players, video examples of SHAAKE and them asked about their experiences with this potential indicator of concussion.
Nearly 69% of athletes reported exhibiting a SHAAKE during their career, and 93% of those reported a SHAAKE in association with concussion at least once. Athletes reported SHAAKE a median of five times in their lives.
Of the athletes who reported SHAAKE, 85% linked this head-shaking movement to concussion symptoms such as disorientation (71%) and dizziness (54%).
Across all sports, SHAAKE showed a sensitivity of 49.6% and a positive predictive value (PPV) of 72.4% for diagnosing concussions.
Among football players, sensitivity improved to 52.3%, with an estimated specificity of 99.9%, a PPV of 91.9%, and an estimated negative predictive value of 99.5%.
The main limitation of the survey was the potential for recall bias due to survey participants self-reporting prior concussions. The researchers called for future prospective studies to validate SHAAKE as a sign of concussion.
Instant Replay for Brain Injury?
Experts echoed the need for validation. SHAAKE represents a “promising advance” in objective TBI assessment, particularly for sideline evaluation, said Shaheen Lakhan, MD, PhD, neurologist, and researcher based in Miami, Florida, who wasn’t involved in the research.
The potential value of SHAAKE is “particularly notable given the well-documented tendency for athletes to minimize or conceal symptoms to maintain play eligibility, a limitation that has historically challenged our reliance on subjective reporting and observational assessments,” Lakhan said.
“Moving forward, validation through prospective studies incorporating real-time video analysis, helmet sensor data, and clinician-confirmed TBI diagnoses will be essential. With appropriate validation, SHAAKE could emerge as a valuable component of our sideline assessment arsenal, complementing rather than replacing existing diagnostic approaches,” Lakhan said.
“SHAAKE could be the ‘instant replay’ for brain injuries that sports medicine has been waiting for — but like any new technology, we need to make sure it works for every player, not just some,” Lakhan added.
Also weighing in, Richard Figler, MD, director of the Concussion Center, Cleveland Clinic Sports Medicine Center, Cleveland, cautioned that the survey participants were recruited from a concussion registry and self-reported an average of 23 concussions — more than one third of which happened 5-10 years prior — which begs the question, “How much are they actually remembering?”
“Our goal is to make sure that the athletes are safe and that we’re not missing concussions, and we don’t have great tools to start off with. This study opens up the door for some prospective studies [of SHAAKE] moving forward. I think we need more data before this should be listed as a definitive marker,” said Figler, who also wasn’t involved in the study.
In any case, he said, when it comes to suspected concussion in sports, “when in doubt, you sit them out,” Figler said.
This research received no external funding. Nowinski has received travel reimbursement from the NFL Players Association (NFLPA), NFL, World Rugby, WWE, and All Elite Wrestling; served as an expert witness in cases related to concussion and chronic traumatic encephalopathy; and is compensated for speaking appearances and serving on the NFL Concussion Settlement Player Advocacy Committee. Daniel H. Daneshvar served as an expert witness in legal cases involving brain injury and concussion and received funding from the Football Players Health Study at Harvard University, which is funded by the NFLPA and evaluates patients for the MGH Brain and Body TRUST Center, sponsored in part by the NFLPA. Lakhan and Figler had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM DIAGNOSTICS
Heat-Related Pediatric ED Visits More Than Double
ORLANDO – according to research presented at the annual meeting of the American Academy of Pediatrics (AAP).
“Our study really highlights the adverse effects that can come from extreme heat, and how increasing heat-related illness is affecting our children,” Taylor Merritt, MD, a pediatric resident at the University of Texas Southwestern Medical Center and Children’s Health in Dallas, said during a press briefing.
Underestimating the Problem?
Lori Byron, MD, a pediatrician from Red Lodge, Montana, who heads the AAP Chapter Climate Advocates program and was not involved in this research, was not surprised by the findings. “If anything, we’re vastly underestimating it because when people come in with heat exhaustion or heat smoke, that gets coded correctly, but when people come in with heart attacks, asthma attacks, strokes, and other exacerbations of chronic disease, it very rarely gets coded as a heat-related illness.”
Record-breaking summer temperatures from the changing climate have led to increased heat-related morbidity and mortality. Past research suggests that children and teens make up nearly half of all those affected by heat-related illnesses, she noted. 2023, for example, was the hottest year on record, and 2024 is predicted to be hotter, Dr. Merritt said.
A Sharp Increase in Cases
The retrospective study examined emergency department diagnoses during May-September from 2012-2023 at two large children’s hospitals within a north Texas pediatric health care system. The researchers compared heat-specific conditions with rhabdomyolysis encounters based on ICD-10 coding.
Heat-specific conditions include heatstroke/sunstroke, exertion heatstroke, heat syncope, heat crap, heat exhaustion, heat fatigue, heat edema, and exposure to excessive natural heat. Rhabdomyolysis encounters included both exertional and nonexertional rhabdomyolysis as well as non-traumatic rhabdomyolysis and elevated creatine kinase (CK) levels.
Among 542 heat-related encounters, 77% had heat-specific diagnoses and 24% had a rhabdomyolysis diagnosis. Combined, heat-related encounters increased 170% from 2012 to 2023, from 4.3 per 10,000 to 11.6 per 10,000 (P = .1). Summer months with higher peak temperatures were also associated with higher heat-related volume in the emergency department (P < .001).
Teenage boys were most likely to have rhabdomyolysis, with 82% of the cases occurring in boys and 70% in ages 12-18 (P < .001). “Compared to the rhabdomyolysis group, the heat-specific group was more likely to be younger, Hispanic, use government-based insurance, and live in an area with a lower Child Opportunity Index,” Dr. Merritt reported. “Most heat-specific encounters resulted in an ED discharge (96%), while most rhabdomyolysis encounters resulted in hospital admission (63%)” (P < .001).
”Thankfully, pediatric heat-related illness is still relatively rare,” Dr. Merritt said. “However, given the context of increasing temperatures, this is important for us all to know, anyone who cares for children, whether that be families or parents or pediatricians.”
Prevention Is Key
Dr. Byron noted that about half of AAP chapters now have climate committees, many of which have created educational materials on heat and wildfire smoke and on talking with athletes about risk of heat-related illnesses.
“A lot of the state high school sports associations are actually now adopting guidelines on when it’s safe to practice and when it’s safe to play for heat and for smoke, so that’s definitely something that we can talk to parents about and kids about,” Dr. Byron said. “Otherwise, you still have a lot of coaches and a lot of kids out there that think you’re just supposed to be tough and barrel through it.”
Rhabdomyolysis and heat stroke are both potentially deadly illnesses, so the biggest focus needs to be on prevention, Dr. Byron said. “Not just working with individuals in your office, but working within your school or within your state high school sports association is totally within the lane of a pediatrician to get involved.”
The research had no external funding. Dr. Merritt and Dr. Byron had no disclosures.
ORLANDO – according to research presented at the annual meeting of the American Academy of Pediatrics (AAP).
“Our study really highlights the adverse effects that can come from extreme heat, and how increasing heat-related illness is affecting our children,” Taylor Merritt, MD, a pediatric resident at the University of Texas Southwestern Medical Center and Children’s Health in Dallas, said during a press briefing.
Underestimating the Problem?
Lori Byron, MD, a pediatrician from Red Lodge, Montana, who heads the AAP Chapter Climate Advocates program and was not involved in this research, was not surprised by the findings. “If anything, we’re vastly underestimating it because when people come in with heat exhaustion or heat smoke, that gets coded correctly, but when people come in with heart attacks, asthma attacks, strokes, and other exacerbations of chronic disease, it very rarely gets coded as a heat-related illness.”
Record-breaking summer temperatures from the changing climate have led to increased heat-related morbidity and mortality. Past research suggests that children and teens make up nearly half of all those affected by heat-related illnesses, she noted. 2023, for example, was the hottest year on record, and 2024 is predicted to be hotter, Dr. Merritt said.
A Sharp Increase in Cases
The retrospective study examined emergency department diagnoses during May-September from 2012-2023 at two large children’s hospitals within a north Texas pediatric health care system. The researchers compared heat-specific conditions with rhabdomyolysis encounters based on ICD-10 coding.
Heat-specific conditions include heatstroke/sunstroke, exertion heatstroke, heat syncope, heat crap, heat exhaustion, heat fatigue, heat edema, and exposure to excessive natural heat. Rhabdomyolysis encounters included both exertional and nonexertional rhabdomyolysis as well as non-traumatic rhabdomyolysis and elevated creatine kinase (CK) levels.
Among 542 heat-related encounters, 77% had heat-specific diagnoses and 24% had a rhabdomyolysis diagnosis. Combined, heat-related encounters increased 170% from 2012 to 2023, from 4.3 per 10,000 to 11.6 per 10,000 (P = .1). Summer months with higher peak temperatures were also associated with higher heat-related volume in the emergency department (P < .001).
Teenage boys were most likely to have rhabdomyolysis, with 82% of the cases occurring in boys and 70% in ages 12-18 (P < .001). “Compared to the rhabdomyolysis group, the heat-specific group was more likely to be younger, Hispanic, use government-based insurance, and live in an area with a lower Child Opportunity Index,” Dr. Merritt reported. “Most heat-specific encounters resulted in an ED discharge (96%), while most rhabdomyolysis encounters resulted in hospital admission (63%)” (P < .001).
”Thankfully, pediatric heat-related illness is still relatively rare,” Dr. Merritt said. “However, given the context of increasing temperatures, this is important for us all to know, anyone who cares for children, whether that be families or parents or pediatricians.”
Prevention Is Key
Dr. Byron noted that about half of AAP chapters now have climate committees, many of which have created educational materials on heat and wildfire smoke and on talking with athletes about risk of heat-related illnesses.
“A lot of the state high school sports associations are actually now adopting guidelines on when it’s safe to practice and when it’s safe to play for heat and for smoke, so that’s definitely something that we can talk to parents about and kids about,” Dr. Byron said. “Otherwise, you still have a lot of coaches and a lot of kids out there that think you’re just supposed to be tough and barrel through it.”
Rhabdomyolysis and heat stroke are both potentially deadly illnesses, so the biggest focus needs to be on prevention, Dr. Byron said. “Not just working with individuals in your office, but working within your school or within your state high school sports association is totally within the lane of a pediatrician to get involved.”
The research had no external funding. Dr. Merritt and Dr. Byron had no disclosures.
ORLANDO – according to research presented at the annual meeting of the American Academy of Pediatrics (AAP).
“Our study really highlights the adverse effects that can come from extreme heat, and how increasing heat-related illness is affecting our children,” Taylor Merritt, MD, a pediatric resident at the University of Texas Southwestern Medical Center and Children’s Health in Dallas, said during a press briefing.
Underestimating the Problem?
Lori Byron, MD, a pediatrician from Red Lodge, Montana, who heads the AAP Chapter Climate Advocates program and was not involved in this research, was not surprised by the findings. “If anything, we’re vastly underestimating it because when people come in with heat exhaustion or heat smoke, that gets coded correctly, but when people come in with heart attacks, asthma attacks, strokes, and other exacerbations of chronic disease, it very rarely gets coded as a heat-related illness.”
Record-breaking summer temperatures from the changing climate have led to increased heat-related morbidity and mortality. Past research suggests that children and teens make up nearly half of all those affected by heat-related illnesses, she noted. 2023, for example, was the hottest year on record, and 2024 is predicted to be hotter, Dr. Merritt said.
A Sharp Increase in Cases
The retrospective study examined emergency department diagnoses during May-September from 2012-2023 at two large children’s hospitals within a north Texas pediatric health care system. The researchers compared heat-specific conditions with rhabdomyolysis encounters based on ICD-10 coding.
Heat-specific conditions include heatstroke/sunstroke, exertion heatstroke, heat syncope, heat crap, heat exhaustion, heat fatigue, heat edema, and exposure to excessive natural heat. Rhabdomyolysis encounters included both exertional and nonexertional rhabdomyolysis as well as non-traumatic rhabdomyolysis and elevated creatine kinase (CK) levels.
Among 542 heat-related encounters, 77% had heat-specific diagnoses and 24% had a rhabdomyolysis diagnosis. Combined, heat-related encounters increased 170% from 2012 to 2023, from 4.3 per 10,000 to 11.6 per 10,000 (P = .1). Summer months with higher peak temperatures were also associated with higher heat-related volume in the emergency department (P < .001).
Teenage boys were most likely to have rhabdomyolysis, with 82% of the cases occurring in boys and 70% in ages 12-18 (P < .001). “Compared to the rhabdomyolysis group, the heat-specific group was more likely to be younger, Hispanic, use government-based insurance, and live in an area with a lower Child Opportunity Index,” Dr. Merritt reported. “Most heat-specific encounters resulted in an ED discharge (96%), while most rhabdomyolysis encounters resulted in hospital admission (63%)” (P < .001).
”Thankfully, pediatric heat-related illness is still relatively rare,” Dr. Merritt said. “However, given the context of increasing temperatures, this is important for us all to know, anyone who cares for children, whether that be families or parents or pediatricians.”
Prevention Is Key
Dr. Byron noted that about half of AAP chapters now have climate committees, many of which have created educational materials on heat and wildfire smoke and on talking with athletes about risk of heat-related illnesses.
“A lot of the state high school sports associations are actually now adopting guidelines on when it’s safe to practice and when it’s safe to play for heat and for smoke, so that’s definitely something that we can talk to parents about and kids about,” Dr. Byron said. “Otherwise, you still have a lot of coaches and a lot of kids out there that think you’re just supposed to be tough and barrel through it.”
Rhabdomyolysis and heat stroke are both potentially deadly illnesses, so the biggest focus needs to be on prevention, Dr. Byron said. “Not just working with individuals in your office, but working within your school or within your state high school sports association is totally within the lane of a pediatrician to get involved.”
The research had no external funding. Dr. Merritt and Dr. Byron had no disclosures.
FROM AAP 2024
Beyond the Title: How PAs Handle the Burden of MD-Level Responsibilities
Within the physician assistant (PA) community, many PAs have expressed the heavy weight of their job expectation and their subsequent feelings of discontent.
Mirela Bruza-Augatis, PhD, MS, PA-C, a researcher at the National Commission on Certification of Physician Assistants, said the sentiment is similar to what she’s heard from colleagues, as well as seen in her own research examining PA work-life balance.
“Unfortunately, part of this is just the culture of medicine — and other healthcare workers report similar experiences. The patient comes first, and you are secondary,” she said. “You have to make do with the resources you have, and that’s not always enough.”
Yet, despite the challenges of working as a PA in today’s healthcare industry, many are finding ways not just to survive but to thrive. Brian McCambley, DHSc, PA-C, who works as both an emergency medicine PA and a system wellness officer at Nuvance Health, has been looking at ways to improve morale (and, consequently, lower turnover rates), especially among new PA recruits.
He said that the first step is finding the right practice environment. He encourages even experienced PAs to take the time to understand the culture of any practice they consider joining — and ask a lot of questions about what kind of support is available.
“Ask the right questions from the very beginning. What does the job truly entail? What is the culture within the group that you’ll be joining? Talk to the entire team to get a real sense of what’s going on there day to day,” he said. “One benefit of being a PA is that most of us are trained as generalists. We have a lot of mobility between specialties. If the work hours, culture, or fit doesn’t work, it is possible to morph and try something different.”
See How Other PAs Are Managing
Dr. Bruza-Augatis added that finding peer support is also beneficial. She said being able to discuss your experiences with other PAs, both within your workplace and outside of it, offers more than just the benefit of knowing you are not alone.
“When you talk to other colleagues who have had similar experiences, they may have found solutions to help,” she said. “The solution that works for one person may not work for everyone. But it can at least offer some ideas and help you focus on the things you may be able to control and change.”
Raquelle Akavan, DMSc, PA-C, founder of the popular PA Moms® group, agreed on both points. She said that finding both institutional and personal support is remarkably helpful in dealing with the stressors most PAs face both at work and home. With that kind of support in place, you can start to set the appropriate boundaries to help ensure you aren’t feeling overwhelmed by all the expectations placed on you.
“This is crucial to finding good work-life integration,” she said. “You can set boundaries with both your patients and your managers. You can carve out time for your family and let your job know that you won’t be taking calls between 5:00 pm and 9:00 pm. You can go to your manager and let them know what you need to do your job well — whether it’s a scribe, continuing medical education, or help managing the workload.”
Speak Up
Advocating for yourself is key, said Hope Cook, PA-C, who works as both a PA in a dermatology practice and as a licensed life coach. She said that taking the time to be self-aware of the work stressors that negatively affect you allows you to “give yourself permission” to do something about them.
“Like any profession, you have to know your limits,” she said. “If you need more collaboration from your team, you need to figure out how to get that. You need to ask for it. If you feel like you have insufficient training to deal with the complexity of the patients who are coming to see you, you need to talk to the practice about how to fix that. It’s important to let people know what support you need. And, if they aren’t going to help provide it, understand that it may be time to go elsewhere.”
None of these things are necessarily easy, said Dr. McCambley. But replacing a PA costs a practice significant time and money. So, finding ways to promote growth and resilience early on in your career will help protect you from later burnout, and save the healthcare organization in the long run, too. He believes Nuvance has had great success in their efforts to support clinician wellness across the board by having PAs contribute to leadership discussions and decisions.
“When you can get with like-minded folks and sit with hospital administration to talk about the best ways to get PAs intermixed with the medical staff and how to support them in their roles, you can make a difference,” he told this news organization. “I’ve been at my healthcare institution for 26 years. We PAs didn’t really have a big voice at the beginning. But, little by little, by having important discussions with our leadership, we’ve been able to show our medical staff that PAs bring something really important to the table — and that it benefits everyone when we support them.”
A version of this article first appeared on Medscape.com.
Within the physician assistant (PA) community, many PAs have expressed the heavy weight of their job expectation and their subsequent feelings of discontent.
Mirela Bruza-Augatis, PhD, MS, PA-C, a researcher at the National Commission on Certification of Physician Assistants, said the sentiment is similar to what she’s heard from colleagues, as well as seen in her own research examining PA work-life balance.
“Unfortunately, part of this is just the culture of medicine — and other healthcare workers report similar experiences. The patient comes first, and you are secondary,” she said. “You have to make do with the resources you have, and that’s not always enough.”
Yet, despite the challenges of working as a PA in today’s healthcare industry, many are finding ways not just to survive but to thrive. Brian McCambley, DHSc, PA-C, who works as both an emergency medicine PA and a system wellness officer at Nuvance Health, has been looking at ways to improve morale (and, consequently, lower turnover rates), especially among new PA recruits.
He said that the first step is finding the right practice environment. He encourages even experienced PAs to take the time to understand the culture of any practice they consider joining — and ask a lot of questions about what kind of support is available.
“Ask the right questions from the very beginning. What does the job truly entail? What is the culture within the group that you’ll be joining? Talk to the entire team to get a real sense of what’s going on there day to day,” he said. “One benefit of being a PA is that most of us are trained as generalists. We have a lot of mobility between specialties. If the work hours, culture, or fit doesn’t work, it is possible to morph and try something different.”
See How Other PAs Are Managing
Dr. Bruza-Augatis added that finding peer support is also beneficial. She said being able to discuss your experiences with other PAs, both within your workplace and outside of it, offers more than just the benefit of knowing you are not alone.
“When you talk to other colleagues who have had similar experiences, they may have found solutions to help,” she said. “The solution that works for one person may not work for everyone. But it can at least offer some ideas and help you focus on the things you may be able to control and change.”
Raquelle Akavan, DMSc, PA-C, founder of the popular PA Moms® group, agreed on both points. She said that finding both institutional and personal support is remarkably helpful in dealing with the stressors most PAs face both at work and home. With that kind of support in place, you can start to set the appropriate boundaries to help ensure you aren’t feeling overwhelmed by all the expectations placed on you.
“This is crucial to finding good work-life integration,” she said. “You can set boundaries with both your patients and your managers. You can carve out time for your family and let your job know that you won’t be taking calls between 5:00 pm and 9:00 pm. You can go to your manager and let them know what you need to do your job well — whether it’s a scribe, continuing medical education, or help managing the workload.”
Speak Up
Advocating for yourself is key, said Hope Cook, PA-C, who works as both a PA in a dermatology practice and as a licensed life coach. She said that taking the time to be self-aware of the work stressors that negatively affect you allows you to “give yourself permission” to do something about them.
“Like any profession, you have to know your limits,” she said. “If you need more collaboration from your team, you need to figure out how to get that. You need to ask for it. If you feel like you have insufficient training to deal with the complexity of the patients who are coming to see you, you need to talk to the practice about how to fix that. It’s important to let people know what support you need. And, if they aren’t going to help provide it, understand that it may be time to go elsewhere.”
None of these things are necessarily easy, said Dr. McCambley. But replacing a PA costs a practice significant time and money. So, finding ways to promote growth and resilience early on in your career will help protect you from later burnout, and save the healthcare organization in the long run, too. He believes Nuvance has had great success in their efforts to support clinician wellness across the board by having PAs contribute to leadership discussions and decisions.
“When you can get with like-minded folks and sit with hospital administration to talk about the best ways to get PAs intermixed with the medical staff and how to support them in their roles, you can make a difference,” he told this news organization. “I’ve been at my healthcare institution for 26 years. We PAs didn’t really have a big voice at the beginning. But, little by little, by having important discussions with our leadership, we’ve been able to show our medical staff that PAs bring something really important to the table — and that it benefits everyone when we support them.”
A version of this article first appeared on Medscape.com.
Within the physician assistant (PA) community, many PAs have expressed the heavy weight of their job expectation and their subsequent feelings of discontent.
Mirela Bruza-Augatis, PhD, MS, PA-C, a researcher at the National Commission on Certification of Physician Assistants, said the sentiment is similar to what she’s heard from colleagues, as well as seen in her own research examining PA work-life balance.
“Unfortunately, part of this is just the culture of medicine — and other healthcare workers report similar experiences. The patient comes first, and you are secondary,” she said. “You have to make do with the resources you have, and that’s not always enough.”
Yet, despite the challenges of working as a PA in today’s healthcare industry, many are finding ways not just to survive but to thrive. Brian McCambley, DHSc, PA-C, who works as both an emergency medicine PA and a system wellness officer at Nuvance Health, has been looking at ways to improve morale (and, consequently, lower turnover rates), especially among new PA recruits.
He said that the first step is finding the right practice environment. He encourages even experienced PAs to take the time to understand the culture of any practice they consider joining — and ask a lot of questions about what kind of support is available.
“Ask the right questions from the very beginning. What does the job truly entail? What is the culture within the group that you’ll be joining? Talk to the entire team to get a real sense of what’s going on there day to day,” he said. “One benefit of being a PA is that most of us are trained as generalists. We have a lot of mobility between specialties. If the work hours, culture, or fit doesn’t work, it is possible to morph and try something different.”
See How Other PAs Are Managing
Dr. Bruza-Augatis added that finding peer support is also beneficial. She said being able to discuss your experiences with other PAs, both within your workplace and outside of it, offers more than just the benefit of knowing you are not alone.
“When you talk to other colleagues who have had similar experiences, they may have found solutions to help,” she said. “The solution that works for one person may not work for everyone. But it can at least offer some ideas and help you focus on the things you may be able to control and change.”
Raquelle Akavan, DMSc, PA-C, founder of the popular PA Moms® group, agreed on both points. She said that finding both institutional and personal support is remarkably helpful in dealing with the stressors most PAs face both at work and home. With that kind of support in place, you can start to set the appropriate boundaries to help ensure you aren’t feeling overwhelmed by all the expectations placed on you.
“This is crucial to finding good work-life integration,” she said. “You can set boundaries with both your patients and your managers. You can carve out time for your family and let your job know that you won’t be taking calls between 5:00 pm and 9:00 pm. You can go to your manager and let them know what you need to do your job well — whether it’s a scribe, continuing medical education, or help managing the workload.”
Speak Up
Advocating for yourself is key, said Hope Cook, PA-C, who works as both a PA in a dermatology practice and as a licensed life coach. She said that taking the time to be self-aware of the work stressors that negatively affect you allows you to “give yourself permission” to do something about them.
“Like any profession, you have to know your limits,” she said. “If you need more collaboration from your team, you need to figure out how to get that. You need to ask for it. If you feel like you have insufficient training to deal with the complexity of the patients who are coming to see you, you need to talk to the practice about how to fix that. It’s important to let people know what support you need. And, if they aren’t going to help provide it, understand that it may be time to go elsewhere.”
None of these things are necessarily easy, said Dr. McCambley. But replacing a PA costs a practice significant time and money. So, finding ways to promote growth and resilience early on in your career will help protect you from later burnout, and save the healthcare organization in the long run, too. He believes Nuvance has had great success in their efforts to support clinician wellness across the board by having PAs contribute to leadership discussions and decisions.
“When you can get with like-minded folks and sit with hospital administration to talk about the best ways to get PAs intermixed with the medical staff and how to support them in their roles, you can make a difference,” he told this news organization. “I’ve been at my healthcare institution for 26 years. We PAs didn’t really have a big voice at the beginning. But, little by little, by having important discussions with our leadership, we’ve been able to show our medical staff that PAs bring something really important to the table — and that it benefits everyone when we support them.”
A version of this article first appeared on Medscape.com.
When You and Your Malpractice Insurer Disagree on Your Case
You’ve been sued for medical malpractice. If you are a physician in the United States, that is not an unlikely scenario.
An analysis by the American Medical Association shows that almost half of all physicians are sued by the time they reach 54. In some specialties, such as ob.gyn., one is almost guaranteed to be sued at some point.
But that’s what medical malpractice insurance is for, right? Your medical malpractice insurer will assign an attorney to take care of you and help you through this situation. Won’t they?
Maybe so, but the attorney and the claims representative your insurer assigns to your case may have a different idea about how to proceed than you do. Though the defense attorney assigned to you represents you, he or she gets paid by the insurance carrier.
This can create a conflict when your defense counsel and your insurance claims representative aim to take your case in a direction you don’t like.
Disagreements might include:
- Choice of expert witnesses
- Tactical decisions related to trial strategy
- Public relations considerations
- Admissions of liability
- Allocation of resources
To Settle or Not?
One of the most challenging — and common — disagreements is whether to settle the case.
Sometimes a malpractice insurer wants to settle the case against the defendant doctor’s wishes. Or the doctor wants to settle but is pushed into going to trial. In the following case, one doctor had to face the consequences of a decision he didn’t even make.
The Underlying Medical Malpractice Case
Dr. D was sued by a patient who had allegedly called Dr. D’s office six times in 2 days complaining of intermittent chest pain.
Dr. D had been swamped with patients and couldn’t squeeze this patient in for an office visit, but he did call back. The patient later claimed that during the call he told the doctor he was suffering from chest pain. The doctor recalled that the patient had complained of abdominal discomfort that began after he had exercised.
The physician wrote a prescription for an ECG at the local hospital and called to ensure that the patient could just walk in. The ECG was allegedly abnormal but was not read as representing an impending or current heart attack. Later that evening, however, the patient went to the emergency department of another hospital where it was confirmed that he had suffered a heart attack. The patient underwent cardiac catheterization and stent placement to address a blockage in his left anterior descending artery.
The patient subsequently sued Dr. D and the hospital where he had the original ECG. Dr. D contacted his medical malpractice insurance company. The insurance company assigned an attorney to represent Dr. D. Discovery in the case began.
The plaintiff’s own medical expert testified in a deposition that there was no way for the heart attack to have been prevented and that the treatment would have been the same either way. But Dr. D could not find a record of the phone calls with the patient, and he had not noted his conversation the patient in their medical records.
Dr. D held a policy for $1 million, and his state had a fund that would kick in an additional $1 million. But the plaintiffs demanded $4 million to settle.
A month before trial, the plaintiff’s attorney sent a threatening letter to Dr. D’s attorney warning him that Dr. D was underinsured and suggesting that it would be in the physician’s best interests to settle.
“I want to stress to you that it is not my desire to harm your client’s reputation or to destroy his business,” wrote the plaintiff’s attorney. “However, now is the time to avoid consequences such as these by making a good faith effort to get this case resolved.”
The letter went on to note that the defense attorney should give Dr. D a copy of the letter so that everyone would be aware of the potential consequences of an award against Dr. D in excess of his limits of insurance coverage. The plaintiff’s attorney even suggested that Dr. D should retain personal counsel.
Dr. D’s defense attorney downplayed the letter and assured him that there was no reason to worry.
Meanwhile the case inched closer to trial.
The codefendant hospital settled with the plaintiff on the night before jury selection, leaving Dr. D in the uncomfortable position of being the only defendant in the case. At this point, Dr. D decided he would like to settle, and he sent his attorney an email telling him so. But the attorney instead referred him to an insurance company claims.
Just days before the trial was to start, Dr. D repeatedly told the claims representative assigned to his claim that he did not want to go to trial but rather wanted to settle. The representative told Dr. D that he had no choice in whether the action settled.
A committee at the insurance company had decided to proceed with the trial rather than settle.
The trial proved a painful debacle for Dr. D. His attorney’s idea of showing a “gotcha” video of the allegedly permanently injured plaintiff carrying a large, heavy box backfired when the jury was shown by the plaintiff that the box actually contained ice cream cones and weighed very little.
Prior to trial, the plaintiff offered to settle for $1 million. On the first day of trial, they lowered that amount to $750,000, yet the defense attorney did not settle the case, and it proceeded to a jury verdict. The jury awarded the plaintiff over $4 million — well in excess of Dr. D’s policy limits.
The Follow-up
Dr. D was horrified, but the insurance company claims representative said the insurer would promptly offer $2 million in available insurance coverage to settle the case post verdict. This did not happen. Instead, the insurer chose to appeal the verdict against Dr. D’s wishes.
Ultimately, Dr. D was forced to hire his own lawyer. He ultimately sued the insurance company for breach of contract and bad faith.
The insurance company eventually attempted to settle with the plaintiffs’ counsel, but the plaintiff refused to accept the available insurance coverage. The insurance carrier still has not posted the entire appeal bond. The case is still pending.
Protecting Yourself
The lesson from Dr. D’s experience: Understand that the insurance company is not your friend. It’s a business looking out for its own interests.
The plaintiff’s attorney was absolutely correct in suggesting that Dr. D retain his own attorney to represent his own interests. You should hire your own lawyer when:
- You disagree with your insurer on how to proceed in a case.
- You receive a demand that exceeds your available insurance coverage or for damages that may not be covered by your policy, such as punitive damages.
- Your insurance carrier attempts to deny insurance coverage for your claim or sends you a letter stating that it is “reserving its rights” not to cover or to limit coverage for your claim.
Retaining independent counsel protects your interests, not those of your insurance company.
Independent counsel can give you a second opinion on the strengths and weaknesses of your claim, help you prepare for your deposition, and attend court dates with you to ensure that you are completely protected.
Independent counsel can challenge your insurance company’s decision to deny or limit your insurance coverage and ensure that you receive all of the benefits to which you are entitled under your insurance policy. Some policies may include an independent lawyer to be paid for by your insurance carrier in case of a conflicts.
The most important takeaway? Your medical malpractice insurance carrier is not your friend, so act accordingly in times of conflict.
A version of this article first appeared on Medscape.com.
You’ve been sued for medical malpractice. If you are a physician in the United States, that is not an unlikely scenario.
An analysis by the American Medical Association shows that almost half of all physicians are sued by the time they reach 54. In some specialties, such as ob.gyn., one is almost guaranteed to be sued at some point.
But that’s what medical malpractice insurance is for, right? Your medical malpractice insurer will assign an attorney to take care of you and help you through this situation. Won’t they?
Maybe so, but the attorney and the claims representative your insurer assigns to your case may have a different idea about how to proceed than you do. Though the defense attorney assigned to you represents you, he or she gets paid by the insurance carrier.
This can create a conflict when your defense counsel and your insurance claims representative aim to take your case in a direction you don’t like.
Disagreements might include:
- Choice of expert witnesses
- Tactical decisions related to trial strategy
- Public relations considerations
- Admissions of liability
- Allocation of resources
To Settle or Not?
One of the most challenging — and common — disagreements is whether to settle the case.
Sometimes a malpractice insurer wants to settle the case against the defendant doctor’s wishes. Or the doctor wants to settle but is pushed into going to trial. In the following case, one doctor had to face the consequences of a decision he didn’t even make.
The Underlying Medical Malpractice Case
Dr. D was sued by a patient who had allegedly called Dr. D’s office six times in 2 days complaining of intermittent chest pain.
Dr. D had been swamped with patients and couldn’t squeeze this patient in for an office visit, but he did call back. The patient later claimed that during the call he told the doctor he was suffering from chest pain. The doctor recalled that the patient had complained of abdominal discomfort that began after he had exercised.
The physician wrote a prescription for an ECG at the local hospital and called to ensure that the patient could just walk in. The ECG was allegedly abnormal but was not read as representing an impending or current heart attack. Later that evening, however, the patient went to the emergency department of another hospital where it was confirmed that he had suffered a heart attack. The patient underwent cardiac catheterization and stent placement to address a blockage in his left anterior descending artery.
The patient subsequently sued Dr. D and the hospital where he had the original ECG. Dr. D contacted his medical malpractice insurance company. The insurance company assigned an attorney to represent Dr. D. Discovery in the case began.
The plaintiff’s own medical expert testified in a deposition that there was no way for the heart attack to have been prevented and that the treatment would have been the same either way. But Dr. D could not find a record of the phone calls with the patient, and he had not noted his conversation the patient in their medical records.
Dr. D held a policy for $1 million, and his state had a fund that would kick in an additional $1 million. But the plaintiffs demanded $4 million to settle.
A month before trial, the plaintiff’s attorney sent a threatening letter to Dr. D’s attorney warning him that Dr. D was underinsured and suggesting that it would be in the physician’s best interests to settle.
“I want to stress to you that it is not my desire to harm your client’s reputation or to destroy his business,” wrote the plaintiff’s attorney. “However, now is the time to avoid consequences such as these by making a good faith effort to get this case resolved.”
The letter went on to note that the defense attorney should give Dr. D a copy of the letter so that everyone would be aware of the potential consequences of an award against Dr. D in excess of his limits of insurance coverage. The plaintiff’s attorney even suggested that Dr. D should retain personal counsel.
Dr. D’s defense attorney downplayed the letter and assured him that there was no reason to worry.
Meanwhile the case inched closer to trial.
The codefendant hospital settled with the plaintiff on the night before jury selection, leaving Dr. D in the uncomfortable position of being the only defendant in the case. At this point, Dr. D decided he would like to settle, and he sent his attorney an email telling him so. But the attorney instead referred him to an insurance company claims.
Just days before the trial was to start, Dr. D repeatedly told the claims representative assigned to his claim that he did not want to go to trial but rather wanted to settle. The representative told Dr. D that he had no choice in whether the action settled.
A committee at the insurance company had decided to proceed with the trial rather than settle.
The trial proved a painful debacle for Dr. D. His attorney’s idea of showing a “gotcha” video of the allegedly permanently injured plaintiff carrying a large, heavy box backfired when the jury was shown by the plaintiff that the box actually contained ice cream cones and weighed very little.
Prior to trial, the plaintiff offered to settle for $1 million. On the first day of trial, they lowered that amount to $750,000, yet the defense attorney did not settle the case, and it proceeded to a jury verdict. The jury awarded the plaintiff over $4 million — well in excess of Dr. D’s policy limits.
The Follow-up
Dr. D was horrified, but the insurance company claims representative said the insurer would promptly offer $2 million in available insurance coverage to settle the case post verdict. This did not happen. Instead, the insurer chose to appeal the verdict against Dr. D’s wishes.
Ultimately, Dr. D was forced to hire his own lawyer. He ultimately sued the insurance company for breach of contract and bad faith.
The insurance company eventually attempted to settle with the plaintiffs’ counsel, but the plaintiff refused to accept the available insurance coverage. The insurance carrier still has not posted the entire appeal bond. The case is still pending.
Protecting Yourself
The lesson from Dr. D’s experience: Understand that the insurance company is not your friend. It’s a business looking out for its own interests.
The plaintiff’s attorney was absolutely correct in suggesting that Dr. D retain his own attorney to represent his own interests. You should hire your own lawyer when:
- You disagree with your insurer on how to proceed in a case.
- You receive a demand that exceeds your available insurance coverage or for damages that may not be covered by your policy, such as punitive damages.
- Your insurance carrier attempts to deny insurance coverage for your claim or sends you a letter stating that it is “reserving its rights” not to cover or to limit coverage for your claim.
Retaining independent counsel protects your interests, not those of your insurance company.
Independent counsel can give you a second opinion on the strengths and weaknesses of your claim, help you prepare for your deposition, and attend court dates with you to ensure that you are completely protected.
Independent counsel can challenge your insurance company’s decision to deny or limit your insurance coverage and ensure that you receive all of the benefits to which you are entitled under your insurance policy. Some policies may include an independent lawyer to be paid for by your insurance carrier in case of a conflicts.
The most important takeaway? Your medical malpractice insurance carrier is not your friend, so act accordingly in times of conflict.
A version of this article first appeared on Medscape.com.
You’ve been sued for medical malpractice. If you are a physician in the United States, that is not an unlikely scenario.
An analysis by the American Medical Association shows that almost half of all physicians are sued by the time they reach 54. In some specialties, such as ob.gyn., one is almost guaranteed to be sued at some point.
But that’s what medical malpractice insurance is for, right? Your medical malpractice insurer will assign an attorney to take care of you and help you through this situation. Won’t they?
Maybe so, but the attorney and the claims representative your insurer assigns to your case may have a different idea about how to proceed than you do. Though the defense attorney assigned to you represents you, he or she gets paid by the insurance carrier.
This can create a conflict when your defense counsel and your insurance claims representative aim to take your case in a direction you don’t like.
Disagreements might include:
- Choice of expert witnesses
- Tactical decisions related to trial strategy
- Public relations considerations
- Admissions of liability
- Allocation of resources
To Settle or Not?
One of the most challenging — and common — disagreements is whether to settle the case.
Sometimes a malpractice insurer wants to settle the case against the defendant doctor’s wishes. Or the doctor wants to settle but is pushed into going to trial. In the following case, one doctor had to face the consequences of a decision he didn’t even make.
The Underlying Medical Malpractice Case
Dr. D was sued by a patient who had allegedly called Dr. D’s office six times in 2 days complaining of intermittent chest pain.
Dr. D had been swamped with patients and couldn’t squeeze this patient in for an office visit, but he did call back. The patient later claimed that during the call he told the doctor he was suffering from chest pain. The doctor recalled that the patient had complained of abdominal discomfort that began after he had exercised.
The physician wrote a prescription for an ECG at the local hospital and called to ensure that the patient could just walk in. The ECG was allegedly abnormal but was not read as representing an impending or current heart attack. Later that evening, however, the patient went to the emergency department of another hospital where it was confirmed that he had suffered a heart attack. The patient underwent cardiac catheterization and stent placement to address a blockage in his left anterior descending artery.
The patient subsequently sued Dr. D and the hospital where he had the original ECG. Dr. D contacted his medical malpractice insurance company. The insurance company assigned an attorney to represent Dr. D. Discovery in the case began.
The plaintiff’s own medical expert testified in a deposition that there was no way for the heart attack to have been prevented and that the treatment would have been the same either way. But Dr. D could not find a record of the phone calls with the patient, and he had not noted his conversation the patient in their medical records.
Dr. D held a policy for $1 million, and his state had a fund that would kick in an additional $1 million. But the plaintiffs demanded $4 million to settle.
A month before trial, the plaintiff’s attorney sent a threatening letter to Dr. D’s attorney warning him that Dr. D was underinsured and suggesting that it would be in the physician’s best interests to settle.
“I want to stress to you that it is not my desire to harm your client’s reputation or to destroy his business,” wrote the plaintiff’s attorney. “However, now is the time to avoid consequences such as these by making a good faith effort to get this case resolved.”
The letter went on to note that the defense attorney should give Dr. D a copy of the letter so that everyone would be aware of the potential consequences of an award against Dr. D in excess of his limits of insurance coverage. The plaintiff’s attorney even suggested that Dr. D should retain personal counsel.
Dr. D’s defense attorney downplayed the letter and assured him that there was no reason to worry.
Meanwhile the case inched closer to trial.
The codefendant hospital settled with the plaintiff on the night before jury selection, leaving Dr. D in the uncomfortable position of being the only defendant in the case. At this point, Dr. D decided he would like to settle, and he sent his attorney an email telling him so. But the attorney instead referred him to an insurance company claims.
Just days before the trial was to start, Dr. D repeatedly told the claims representative assigned to his claim that he did not want to go to trial but rather wanted to settle. The representative told Dr. D that he had no choice in whether the action settled.
A committee at the insurance company had decided to proceed with the trial rather than settle.
The trial proved a painful debacle for Dr. D. His attorney’s idea of showing a “gotcha” video of the allegedly permanently injured plaintiff carrying a large, heavy box backfired when the jury was shown by the plaintiff that the box actually contained ice cream cones and weighed very little.
Prior to trial, the plaintiff offered to settle for $1 million. On the first day of trial, they lowered that amount to $750,000, yet the defense attorney did not settle the case, and it proceeded to a jury verdict. The jury awarded the plaintiff over $4 million — well in excess of Dr. D’s policy limits.
The Follow-up
Dr. D was horrified, but the insurance company claims representative said the insurer would promptly offer $2 million in available insurance coverage to settle the case post verdict. This did not happen. Instead, the insurer chose to appeal the verdict against Dr. D’s wishes.
Ultimately, Dr. D was forced to hire his own lawyer. He ultimately sued the insurance company for breach of contract and bad faith.
The insurance company eventually attempted to settle with the plaintiffs’ counsel, but the plaintiff refused to accept the available insurance coverage. The insurance carrier still has not posted the entire appeal bond. The case is still pending.
Protecting Yourself
The lesson from Dr. D’s experience: Understand that the insurance company is not your friend. It’s a business looking out for its own interests.
The plaintiff’s attorney was absolutely correct in suggesting that Dr. D retain his own attorney to represent his own interests. You should hire your own lawyer when:
- You disagree with your insurer on how to proceed in a case.
- You receive a demand that exceeds your available insurance coverage or for damages that may not be covered by your policy, such as punitive damages.
- Your insurance carrier attempts to deny insurance coverage for your claim or sends you a letter stating that it is “reserving its rights” not to cover or to limit coverage for your claim.
Retaining independent counsel protects your interests, not those of your insurance company.
Independent counsel can give you a second opinion on the strengths and weaknesses of your claim, help you prepare for your deposition, and attend court dates with you to ensure that you are completely protected.
Independent counsel can challenge your insurance company’s decision to deny or limit your insurance coverage and ensure that you receive all of the benefits to which you are entitled under your insurance policy. Some policies may include an independent lawyer to be paid for by your insurance carrier in case of a conflicts.
The most important takeaway? Your medical malpractice insurance carrier is not your friend, so act accordingly in times of conflict.
A version of this article first appeared on Medscape.com.
Coffee’s ‘Sweet Spot’: Daily Consumption and Cardiometabolic Risk
Each and every day, 1 billion people on this planet ingest a particular psychoactive substance. This chemical has fairly profound physiologic effects. It increases levels of nitric oxide in the blood, leads to vasodilation, and, of course, makes you feel more awake. The substance comes in many forms but almost always in a liquid medium. Do you have it yet? That’s right. The substance is caffeine, quite possibly the healthiest recreational drug that has ever been discovered.
This might be my New England upbringing speaking, but when it comes to lifestyle and health, one of the rules I’ve internalized is that things that are pleasurable are generally bad for you. I know, I know — some of you love to exercise. Some of you love doing crosswords. But you know what I mean. I’m talking French fries, smoked meats, drugs, smoking, alcohol, binge-watching Firefly. You’d be suspicious if a study came out suggesting that eating ice cream in bed reduces your risk for heart attack, and so would I. So I’m always on the lookout for those unicorns of lifestyle factors, those rare things that you want to do and are also good for you.
So far, the data are strong for three things: sleeping, (safe) sexual activity, and coffee. You’ll have to stay tuned for articles about the first two. Today, we’re brewing up some deeper insights about the power of java.
I was inspired to write this article because of a paper, “Habitual Coffee, Tea, and Caffeine Consumption, Circulating Metabolites, and the Risk of Cardiometabolic Multimorbidity,” appearing September 17 in The Journal of Clinical Endocrinology and Metabolism (JCEM).
This is not the first study to suggest that coffee intake may be beneficial. A 2013 meta-analysis summarized the results of 36 studies with more than a million participants and found a U-shaped relationship between coffee intake and cardiovascular risk. The sweet spot was at three to five cups a day; people drinking that much coffee had about a 15% reduced risk for cardiovascular disease compared with nondrinkers.
But here’s the thing. Coffee contains caffeine, but it is much more than that. It is a heady brew of various chemicals and compounds, phenols, and chlorogenic acids. And, of course, you can get caffeine from stuff that isn’t coffee — natural things like tea — and decidedly unnatural things like energy drinks. How do you figure out where the benefit really lies?
The JCEM study leveraged the impressive UK Biobank dataset to figure this out. The Biobank recruited more than half a million people from the UK between 2006 and 2010 and collected a wealth of data from each of them: surveys, blood samples, biometrics, medical imaging — the works. And then they followed what would happen to those people medically over time. It’s a pretty amazing resource.
But for the purposes of this study, what you need to know is that just under 200,000 of those participants met the key criteria for this study: being free from cardiovascular disease at baseline; having completed a detailed survey about their coffee, tea, and other caffeinated beverage intake; and having adequate follow-up. A subset of that number, just under 100,000, had metabolomic data — which is where this study really gets interesting.
We’ll dive into the metabolome in a moment, but first let’s just talk about the main finding, the relationship between coffee, tea, or caffeine and cardiovascular disease. But to do that, we need to acknowledge that people who drink a lot of coffee are different from people who don’t, and it might be those differences, not the coffee itself, that are beneficial.
What were those differences? People who drank more coffee tended to be a bit older, were less likely to be female, and were slightly more likely to engage in physical activity. They ate less processed meat but also fewer vegetables. Some of those factors, like being female, are generally protective against cardiovascular disease; but some, like age, are definitely not. The authors adjusted for these and multiple other factors, including alcohol intake, BMI, kidney function, and many others to try to disentangle the effect of being the type of person who drinks a lot of coffee from the drinking a lot of coffee itself.
These are the results of the fully adjusted model. Compared with nonconsumers, you can see that people in the higher range of coffee, tea, or just caffeine intake have almost a 40% reduction in cardiovascular disease in follow-up.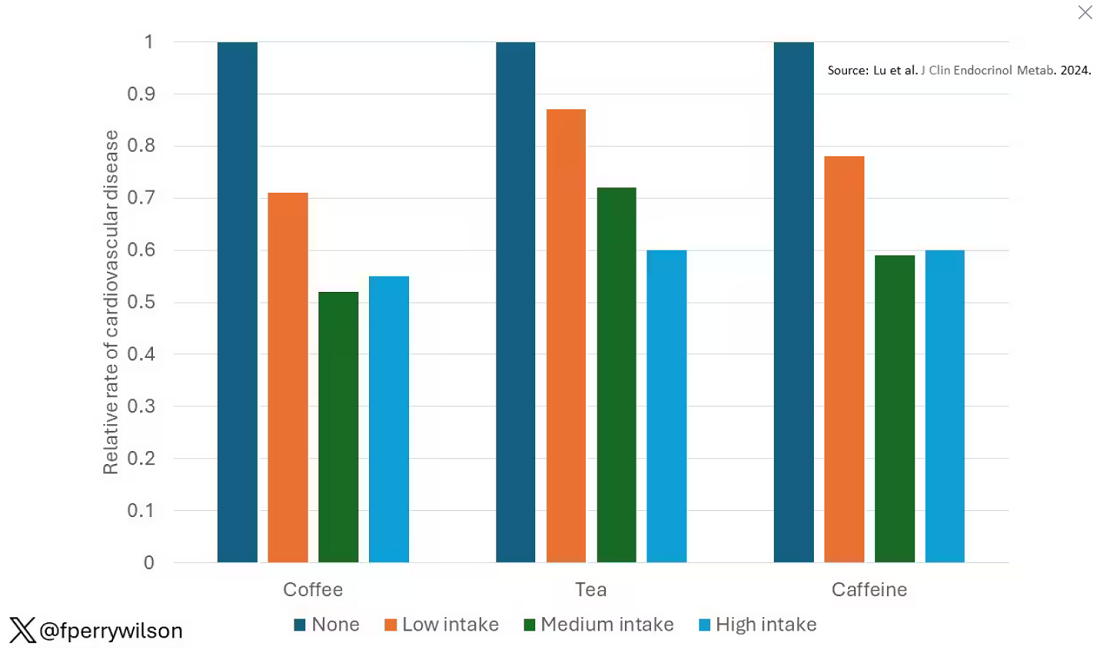
Looking at the benefit across the spectrum of intake, you again see that U-shaped curve, suggesting that a sweet spot for daily consumption can be found around 3 cups of coffee or tea (or 250 mg of caffeine). A standard energy drink contains about 120 mg of caffeine. 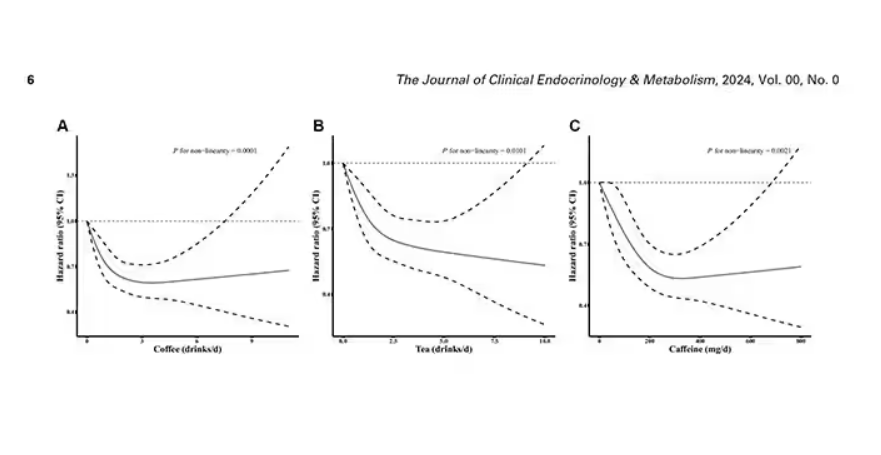
But if this is true, it would be good to know why. To figure that out, the authors turned to the metabolome. The idea here is that your body is constantly breaking stuff down, taking all these proteins and chemicals and compounds that we ingest and turning them into metabolites. Using advanced measurement techniques, researchers can measure hundreds or even thousands of metabolites from a single blood sample. They provide information, obviously, about the food you eat and the drinks you drink, but what is really intriguing is that some metabolites are associated with better health and some with worse
In this study, researchers measured 168 individual metabolites. Eighty of them, nearly half, were significantly altered in people who drank more coffee.
This figure summarizes the findings, and yes, this is way too complicated. 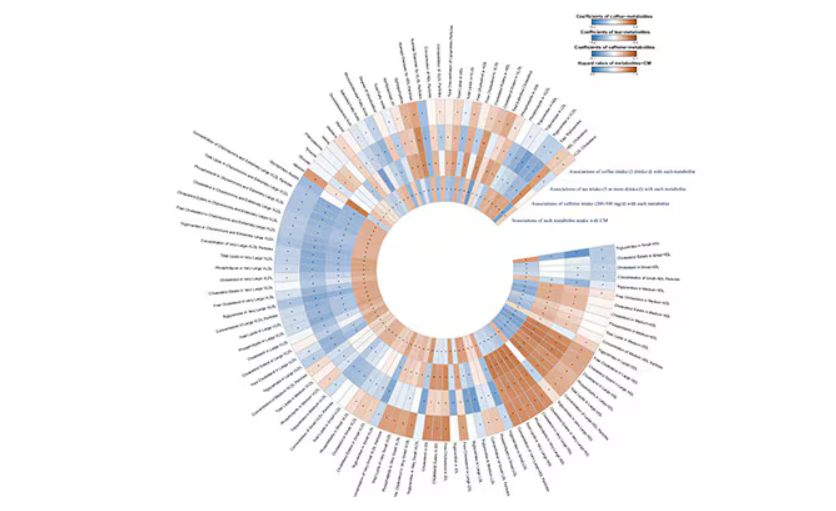
But here’s how to interpret it. The inner ring shows you how certain metabolites are associated with cardiovascular disease. The outer rings show you how those metabolites are associated with coffee, tea, or caffeine. The interesting part is that the sections of the ring (outer rings and inner rings) are very different colors.
Like here.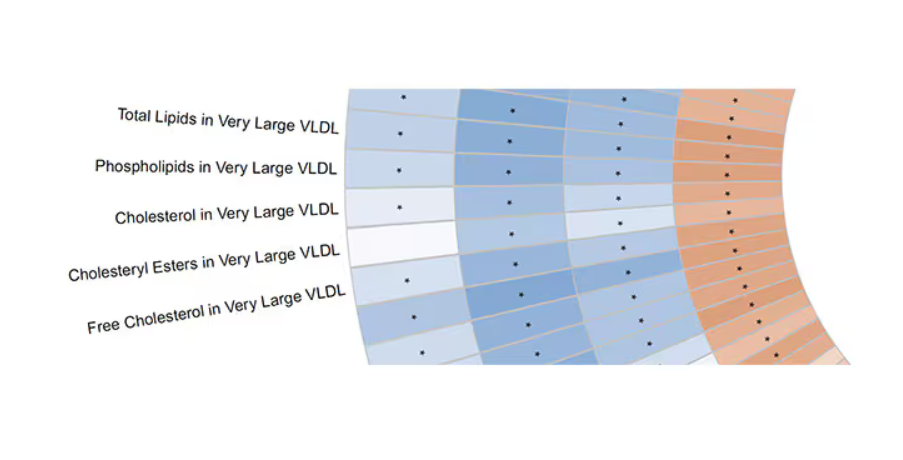
What you see here is a fairly profound effect that coffee, tea, or caffeine intake has on metabolites of VLDL — bad cholesterol. The beverages lower it, and, of course, higher levels lead to cardiovascular disease. This means that this is a potential causal pathway from coffee intake to heart protection.
And that’s not the only one.
You see a similar relationship for saturated fatty acids. Higher levels lead to cardiovascular disease, and coffee intake lowers levels. The reverse works too: Lower levels of histidine (an amino acid) increase cardiovascular risk, and coffee seems to raise those levels.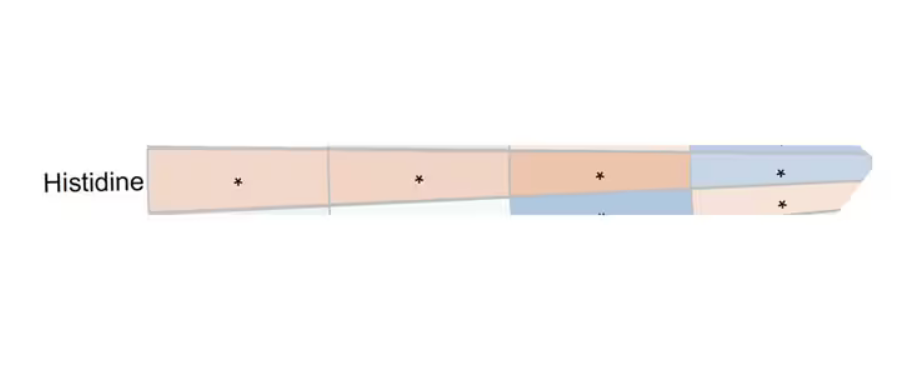
Is this all too good to be true? It’s hard to say. The data on coffee’s benefits have been remarkably consistent. Still, I wouldn’t be a good doctor if I didn’t mention that clearly there is a difference between a cup of black coffee and a venti caramel Frappuccino.
Nevertheless, coffee remains firmly in my holy trinity of enjoyable things that are, for whatever reason, still good for you. So, when you’re having that second, or third, or maybe fourth cup of the day, you can take that to heart.
Dr. Wilson, associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Each and every day, 1 billion people on this planet ingest a particular psychoactive substance. This chemical has fairly profound physiologic effects. It increases levels of nitric oxide in the blood, leads to vasodilation, and, of course, makes you feel more awake. The substance comes in many forms but almost always in a liquid medium. Do you have it yet? That’s right. The substance is caffeine, quite possibly the healthiest recreational drug that has ever been discovered.
This might be my New England upbringing speaking, but when it comes to lifestyle and health, one of the rules I’ve internalized is that things that are pleasurable are generally bad for you. I know, I know — some of you love to exercise. Some of you love doing crosswords. But you know what I mean. I’m talking French fries, smoked meats, drugs, smoking, alcohol, binge-watching Firefly. You’d be suspicious if a study came out suggesting that eating ice cream in bed reduces your risk for heart attack, and so would I. So I’m always on the lookout for those unicorns of lifestyle factors, those rare things that you want to do and are also good for you.
So far, the data are strong for three things: sleeping, (safe) sexual activity, and coffee. You’ll have to stay tuned for articles about the first two. Today, we’re brewing up some deeper insights about the power of java.
I was inspired to write this article because of a paper, “Habitual Coffee, Tea, and Caffeine Consumption, Circulating Metabolites, and the Risk of Cardiometabolic Multimorbidity,” appearing September 17 in The Journal of Clinical Endocrinology and Metabolism (JCEM).
This is not the first study to suggest that coffee intake may be beneficial. A 2013 meta-analysis summarized the results of 36 studies with more than a million participants and found a U-shaped relationship between coffee intake and cardiovascular risk. The sweet spot was at three to five cups a day; people drinking that much coffee had about a 15% reduced risk for cardiovascular disease compared with nondrinkers.
But here’s the thing. Coffee contains caffeine, but it is much more than that. It is a heady brew of various chemicals and compounds, phenols, and chlorogenic acids. And, of course, you can get caffeine from stuff that isn’t coffee — natural things like tea — and decidedly unnatural things like energy drinks. How do you figure out where the benefit really lies?
The JCEM study leveraged the impressive UK Biobank dataset to figure this out. The Biobank recruited more than half a million people from the UK between 2006 and 2010 and collected a wealth of data from each of them: surveys, blood samples, biometrics, medical imaging — the works. And then they followed what would happen to those people medically over time. It’s a pretty amazing resource.
But for the purposes of this study, what you need to know is that just under 200,000 of those participants met the key criteria for this study: being free from cardiovascular disease at baseline; having completed a detailed survey about their coffee, tea, and other caffeinated beverage intake; and having adequate follow-up. A subset of that number, just under 100,000, had metabolomic data — which is where this study really gets interesting.
We’ll dive into the metabolome in a moment, but first let’s just talk about the main finding, the relationship between coffee, tea, or caffeine and cardiovascular disease. But to do that, we need to acknowledge that people who drink a lot of coffee are different from people who don’t, and it might be those differences, not the coffee itself, that are beneficial.
What were those differences? People who drank more coffee tended to be a bit older, were less likely to be female, and were slightly more likely to engage in physical activity. They ate less processed meat but also fewer vegetables. Some of those factors, like being female, are generally protective against cardiovascular disease; but some, like age, are definitely not. The authors adjusted for these and multiple other factors, including alcohol intake, BMI, kidney function, and many others to try to disentangle the effect of being the type of person who drinks a lot of coffee from the drinking a lot of coffee itself.
These are the results of the fully adjusted model. Compared with nonconsumers, you can see that people in the higher range of coffee, tea, or just caffeine intake have almost a 40% reduction in cardiovascular disease in follow-up.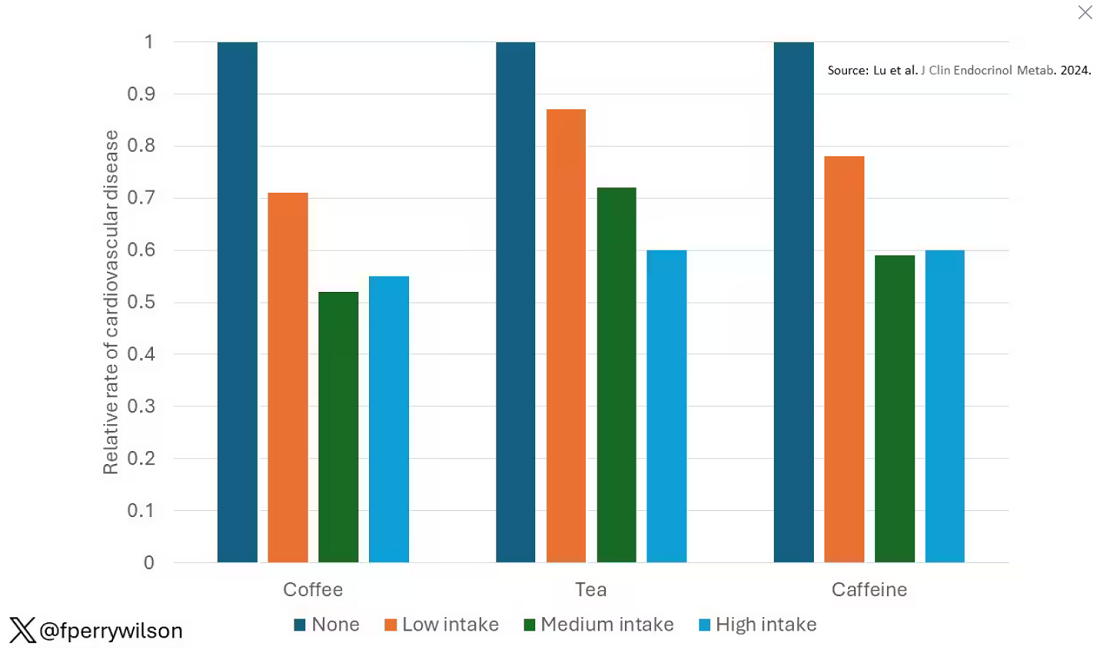
Looking at the benefit across the spectrum of intake, you again see that U-shaped curve, suggesting that a sweet spot for daily consumption can be found around 3 cups of coffee or tea (or 250 mg of caffeine). A standard energy drink contains about 120 mg of caffeine. 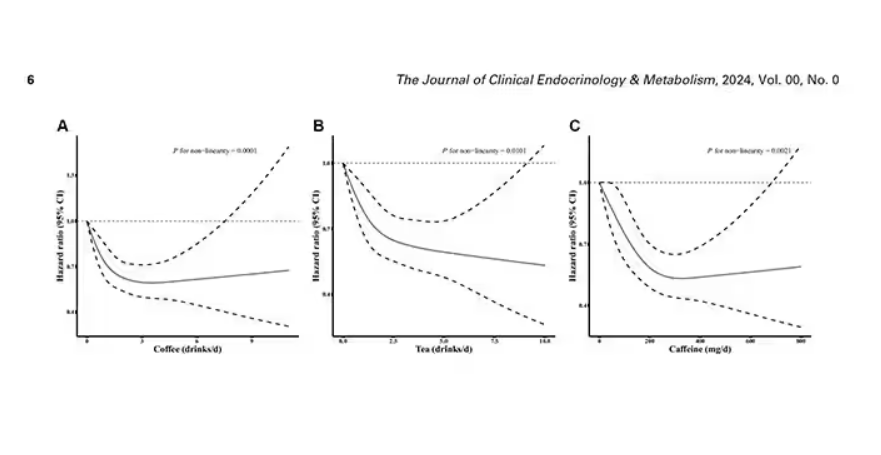
But if this is true, it would be good to know why. To figure that out, the authors turned to the metabolome. The idea here is that your body is constantly breaking stuff down, taking all these proteins and chemicals and compounds that we ingest and turning them into metabolites. Using advanced measurement techniques, researchers can measure hundreds or even thousands of metabolites from a single blood sample. They provide information, obviously, about the food you eat and the drinks you drink, but what is really intriguing is that some metabolites are associated with better health and some with worse
In this study, researchers measured 168 individual metabolites. Eighty of them, nearly half, were significantly altered in people who drank more coffee.
This figure summarizes the findings, and yes, this is way too complicated. 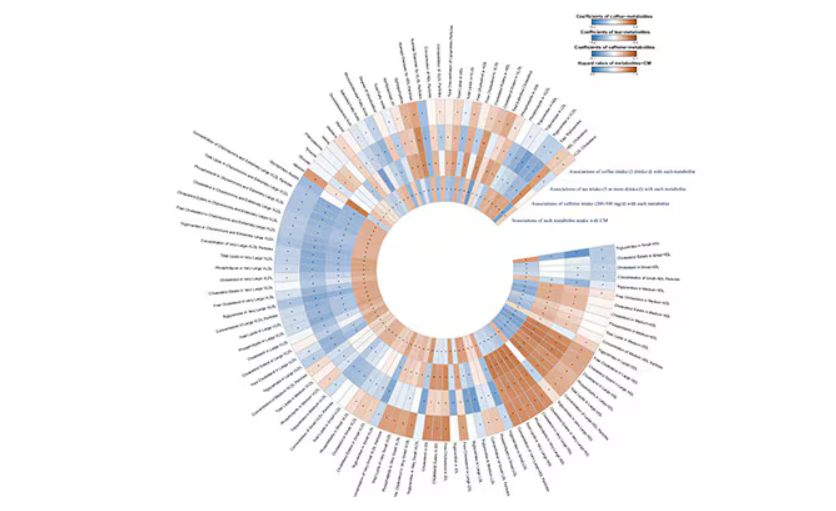
But here’s how to interpret it. The inner ring shows you how certain metabolites are associated with cardiovascular disease. The outer rings show you how those metabolites are associated with coffee, tea, or caffeine. The interesting part is that the sections of the ring (outer rings and inner rings) are very different colors.
Like here.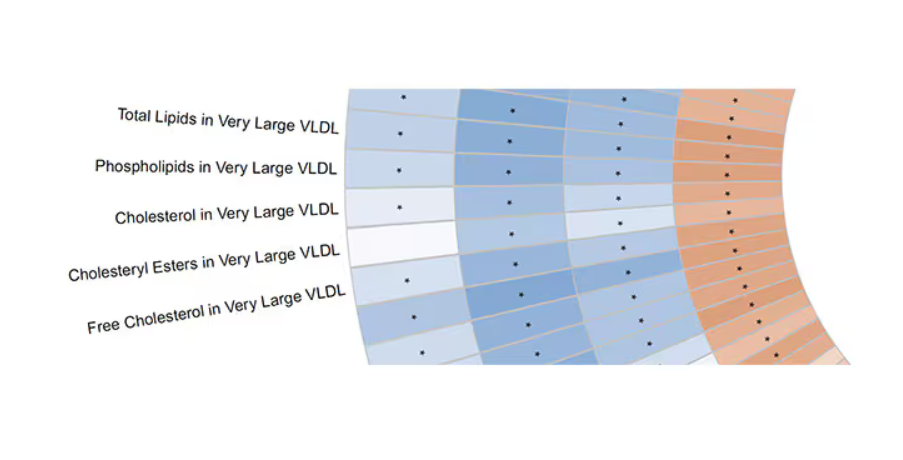
What you see here is a fairly profound effect that coffee, tea, or caffeine intake has on metabolites of VLDL — bad cholesterol. The beverages lower it, and, of course, higher levels lead to cardiovascular disease. This means that this is a potential causal pathway from coffee intake to heart protection.
And that’s not the only one.
You see a similar relationship for saturated fatty acids. Higher levels lead to cardiovascular disease, and coffee intake lowers levels. The reverse works too: Lower levels of histidine (an amino acid) increase cardiovascular risk, and coffee seems to raise those levels.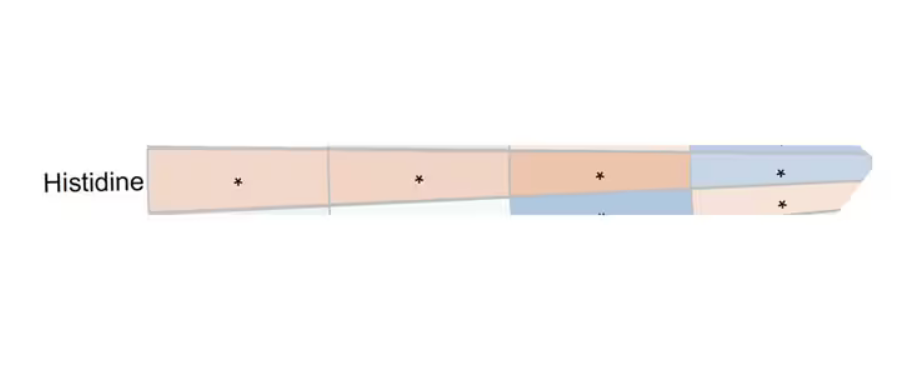
Is this all too good to be true? It’s hard to say. The data on coffee’s benefits have been remarkably consistent. Still, I wouldn’t be a good doctor if I didn’t mention that clearly there is a difference between a cup of black coffee and a venti caramel Frappuccino.
Nevertheless, coffee remains firmly in my holy trinity of enjoyable things that are, for whatever reason, still good for you. So, when you’re having that second, or third, or maybe fourth cup of the day, you can take that to heart.
Dr. Wilson, associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Each and every day, 1 billion people on this planet ingest a particular psychoactive substance. This chemical has fairly profound physiologic effects. It increases levels of nitric oxide in the blood, leads to vasodilation, and, of course, makes you feel more awake. The substance comes in many forms but almost always in a liquid medium. Do you have it yet? That’s right. The substance is caffeine, quite possibly the healthiest recreational drug that has ever been discovered.
This might be my New England upbringing speaking, but when it comes to lifestyle and health, one of the rules I’ve internalized is that things that are pleasurable are generally bad for you. I know, I know — some of you love to exercise. Some of you love doing crosswords. But you know what I mean. I’m talking French fries, smoked meats, drugs, smoking, alcohol, binge-watching Firefly. You’d be suspicious if a study came out suggesting that eating ice cream in bed reduces your risk for heart attack, and so would I. So I’m always on the lookout for those unicorns of lifestyle factors, those rare things that you want to do and are also good for you.
So far, the data are strong for three things: sleeping, (safe) sexual activity, and coffee. You’ll have to stay tuned for articles about the first two. Today, we’re brewing up some deeper insights about the power of java.
I was inspired to write this article because of a paper, “Habitual Coffee, Tea, and Caffeine Consumption, Circulating Metabolites, and the Risk of Cardiometabolic Multimorbidity,” appearing September 17 in The Journal of Clinical Endocrinology and Metabolism (JCEM).
This is not the first study to suggest that coffee intake may be beneficial. A 2013 meta-analysis summarized the results of 36 studies with more than a million participants and found a U-shaped relationship between coffee intake and cardiovascular risk. The sweet spot was at three to five cups a day; people drinking that much coffee had about a 15% reduced risk for cardiovascular disease compared with nondrinkers.
But here’s the thing. Coffee contains caffeine, but it is much more than that. It is a heady brew of various chemicals and compounds, phenols, and chlorogenic acids. And, of course, you can get caffeine from stuff that isn’t coffee — natural things like tea — and decidedly unnatural things like energy drinks. How do you figure out where the benefit really lies?
The JCEM study leveraged the impressive UK Biobank dataset to figure this out. The Biobank recruited more than half a million people from the UK between 2006 and 2010 and collected a wealth of data from each of them: surveys, blood samples, biometrics, medical imaging — the works. And then they followed what would happen to those people medically over time. It’s a pretty amazing resource.
But for the purposes of this study, what you need to know is that just under 200,000 of those participants met the key criteria for this study: being free from cardiovascular disease at baseline; having completed a detailed survey about their coffee, tea, and other caffeinated beverage intake; and having adequate follow-up. A subset of that number, just under 100,000, had metabolomic data — which is where this study really gets interesting.
We’ll dive into the metabolome in a moment, but first let’s just talk about the main finding, the relationship between coffee, tea, or caffeine and cardiovascular disease. But to do that, we need to acknowledge that people who drink a lot of coffee are different from people who don’t, and it might be those differences, not the coffee itself, that are beneficial.
What were those differences? People who drank more coffee tended to be a bit older, were less likely to be female, and were slightly more likely to engage in physical activity. They ate less processed meat but also fewer vegetables. Some of those factors, like being female, are generally protective against cardiovascular disease; but some, like age, are definitely not. The authors adjusted for these and multiple other factors, including alcohol intake, BMI, kidney function, and many others to try to disentangle the effect of being the type of person who drinks a lot of coffee from the drinking a lot of coffee itself.
These are the results of the fully adjusted model. Compared with nonconsumers, you can see that people in the higher range of coffee, tea, or just caffeine intake have almost a 40% reduction in cardiovascular disease in follow-up.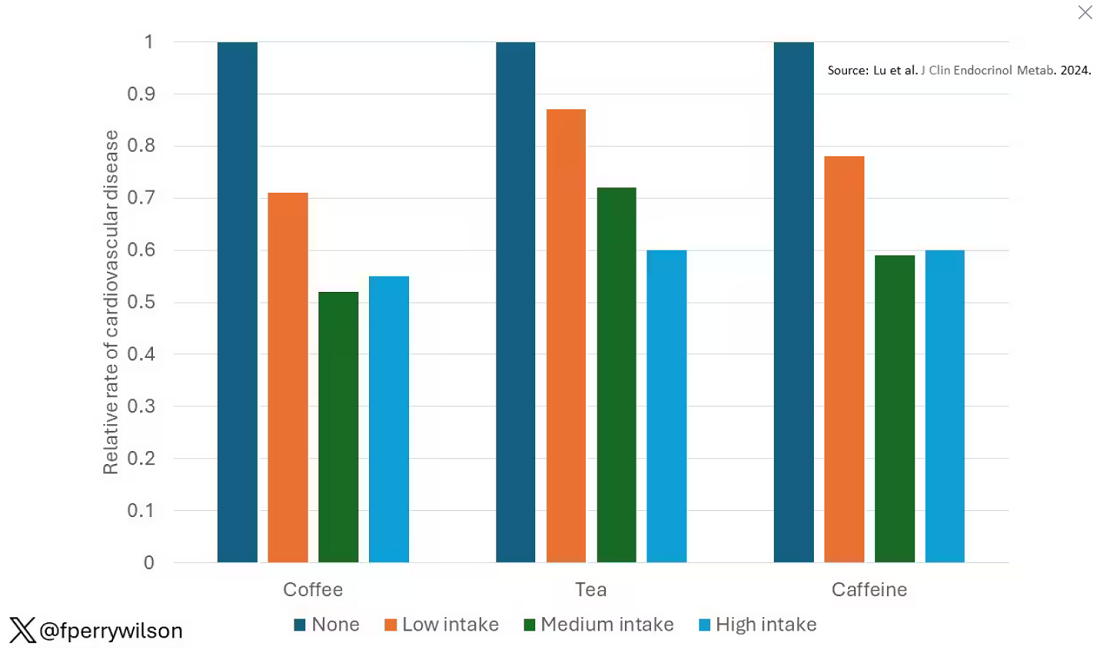
Looking at the benefit across the spectrum of intake, you again see that U-shaped curve, suggesting that a sweet spot for daily consumption can be found around 3 cups of coffee or tea (or 250 mg of caffeine). A standard energy drink contains about 120 mg of caffeine. 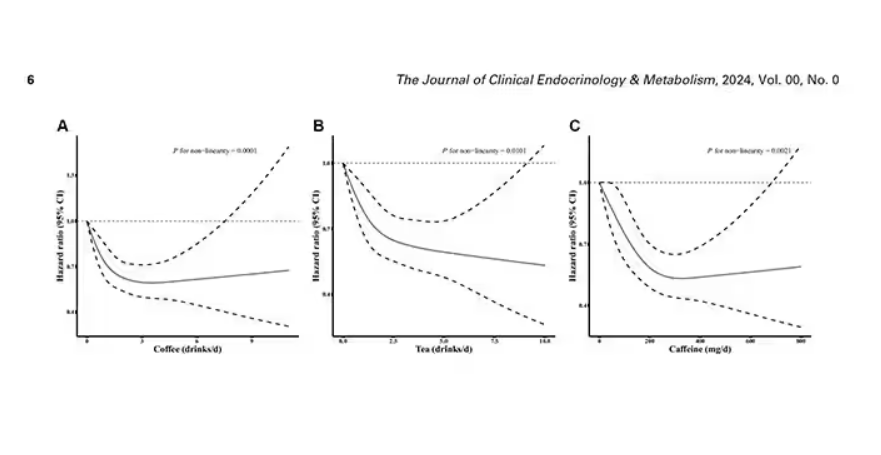
But if this is true, it would be good to know why. To figure that out, the authors turned to the metabolome. The idea here is that your body is constantly breaking stuff down, taking all these proteins and chemicals and compounds that we ingest and turning them into metabolites. Using advanced measurement techniques, researchers can measure hundreds or even thousands of metabolites from a single blood sample. They provide information, obviously, about the food you eat and the drinks you drink, but what is really intriguing is that some metabolites are associated with better health and some with worse
In this study, researchers measured 168 individual metabolites. Eighty of them, nearly half, were significantly altered in people who drank more coffee.
This figure summarizes the findings, and yes, this is way too complicated. 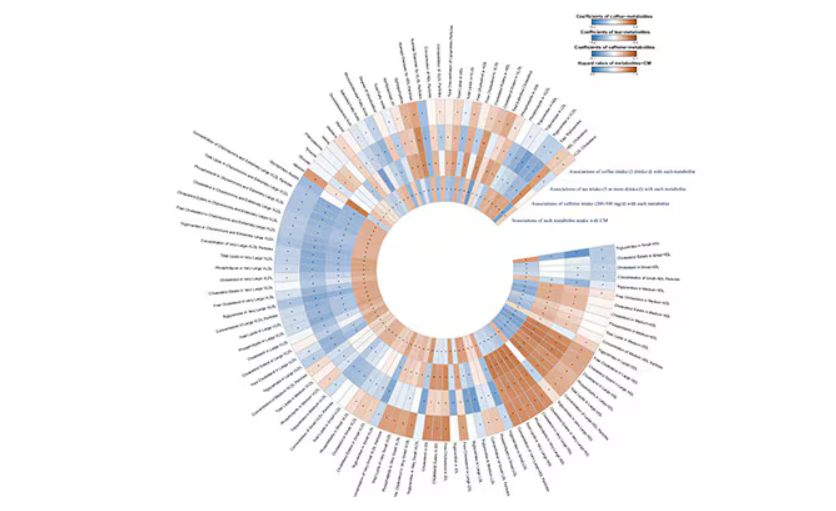
But here’s how to interpret it. The inner ring shows you how certain metabolites are associated with cardiovascular disease. The outer rings show you how those metabolites are associated with coffee, tea, or caffeine. The interesting part is that the sections of the ring (outer rings and inner rings) are very different colors.
Like here.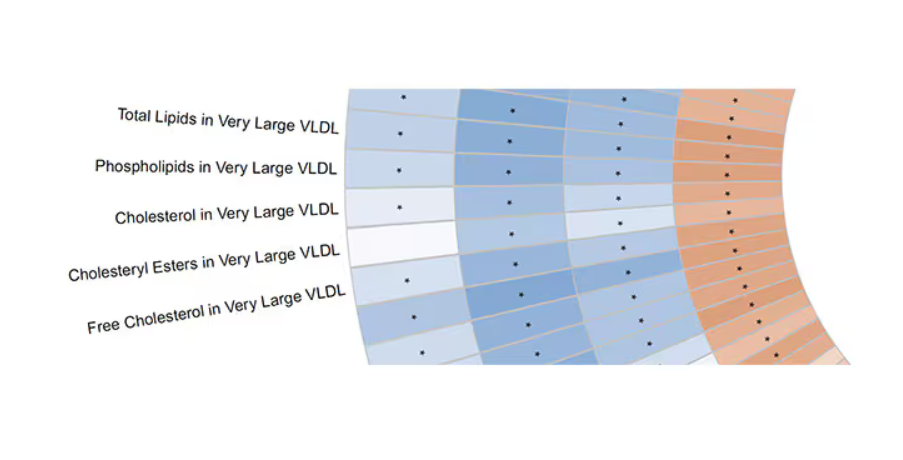
What you see here is a fairly profound effect that coffee, tea, or caffeine intake has on metabolites of VLDL — bad cholesterol. The beverages lower it, and, of course, higher levels lead to cardiovascular disease. This means that this is a potential causal pathway from coffee intake to heart protection.
And that’s not the only one.
You see a similar relationship for saturated fatty acids. Higher levels lead to cardiovascular disease, and coffee intake lowers levels. The reverse works too: Lower levels of histidine (an amino acid) increase cardiovascular risk, and coffee seems to raise those levels.
Is this all too good to be true? It’s hard to say. The data on coffee’s benefits have been remarkably consistent. Still, I wouldn’t be a good doctor if I didn’t mention that clearly there is a difference between a cup of black coffee and a venti caramel Frappuccino.
Nevertheless, coffee remains firmly in my holy trinity of enjoyable things that are, for whatever reason, still good for you. So, when you’re having that second, or third, or maybe fourth cup of the day, you can take that to heart.
Dr. Wilson, associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
How Common Is Pediatric Emergency Mistriage?
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
FROM JAMA PEDIATRICS