User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Tick-borne disease has become a national issue
Pennsylvania had more reported cases of tick-borne disease from 2004 to 2016 than any other state, but these diseases are becoming a national threat, according to the Centers for Disease Control and Prevention.
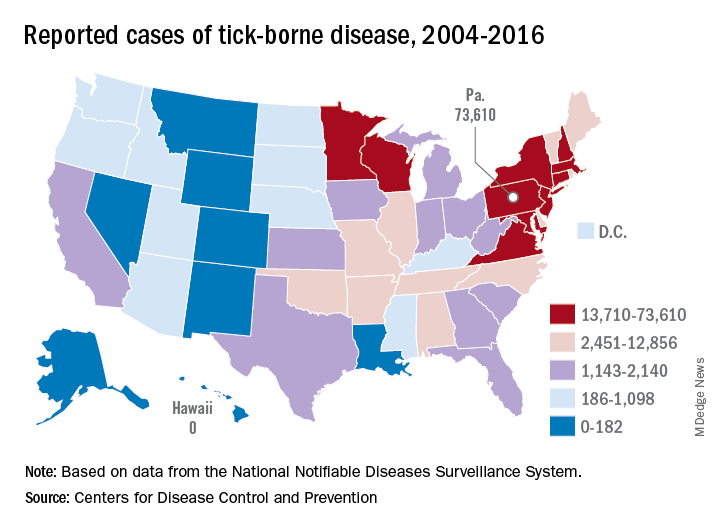
There were 73,000 cases reported in Pennsylvania over that period, and tick-borne diseases, including Lyme disease, anaplasmosis/ehrlichiosis, spotted fever rickettsiosis, babesiosis, tularemia, and Powassan virus, among others, affected almost 492,000 people nationwide, with Lyme disease representing the majority of cases, the CDC said in a Vital Signs report.
Although it’s no surprise that Pennsylvania, New York, and Connecticut were tick-borne disease hot spots, non-Northeastern states like Virginia, Wisconsin, and Minnesota also were among the top 10 in cases. States even further away from the Northeast can be found in the next 10: Arkansas had more than 7,000 cases in 13 years, and Oklahoma had over 4,600 cases, data from the National Notifiable Diseases Surveillance System show.
Nationally, the number of cases more than doubled from 23,000 in 2004 to 49,000 in 2016, and tick-borne disease hit every state except Hawaii. Over that same time, seven new tick-borne pathogens were discovered or introduced into the United States, the CDC reported.
“Local and state health departments and vector control organizations face increasing demands to respond to these threats,” the CDC said, but “more than 80% of vector control organizations report needing improvement in one or more of five core competencies, such as testing for pesticide resistance [and using] data to drive local decisions about vector control.”
Pennsylvania had more reported cases of tick-borne disease from 2004 to 2016 than any other state, but these diseases are becoming a national threat, according to the Centers for Disease Control and Prevention.
There were 73,000 cases reported in Pennsylvania over that period, and tick-borne diseases, including Lyme disease, anaplasmosis/ehrlichiosis, spotted fever rickettsiosis, babesiosis, tularemia, and Powassan virus, among others, affected almost 492,000 people nationwide, with Lyme disease representing the majority of cases, the CDC said in a Vital Signs report.
Although it’s no surprise that Pennsylvania, New York, and Connecticut were tick-borne disease hot spots, non-Northeastern states like Virginia, Wisconsin, and Minnesota also were among the top 10 in cases. States even further away from the Northeast can be found in the next 10: Arkansas had more than 7,000 cases in 13 years, and Oklahoma had over 4,600 cases, data from the National Notifiable Diseases Surveillance System show.
Nationally, the number of cases more than doubled from 23,000 in 2004 to 49,000 in 2016, and tick-borne disease hit every state except Hawaii. Over that same time, seven new tick-borne pathogens were discovered or introduced into the United States, the CDC reported.
“Local and state health departments and vector control organizations face increasing demands to respond to these threats,” the CDC said, but “more than 80% of vector control organizations report needing improvement in one or more of five core competencies, such as testing for pesticide resistance [and using] data to drive local decisions about vector control.”
Pennsylvania had more reported cases of tick-borne disease from 2004 to 2016 than any other state, but these diseases are becoming a national threat, according to the Centers for Disease Control and Prevention.
There were 73,000 cases reported in Pennsylvania over that period, and tick-borne diseases, including Lyme disease, anaplasmosis/ehrlichiosis, spotted fever rickettsiosis, babesiosis, tularemia, and Powassan virus, among others, affected almost 492,000 people nationwide, with Lyme disease representing the majority of cases, the CDC said in a Vital Signs report.
Although it’s no surprise that Pennsylvania, New York, and Connecticut were tick-borne disease hot spots, non-Northeastern states like Virginia, Wisconsin, and Minnesota also were among the top 10 in cases. States even further away from the Northeast can be found in the next 10: Arkansas had more than 7,000 cases in 13 years, and Oklahoma had over 4,600 cases, data from the National Notifiable Diseases Surveillance System show.
Nationally, the number of cases more than doubled from 23,000 in 2004 to 49,000 in 2016, and tick-borne disease hit every state except Hawaii. Over that same time, seven new tick-borne pathogens were discovered or introduced into the United States, the CDC reported.
“Local and state health departments and vector control organizations face increasing demands to respond to these threats,” the CDC said, but “more than 80% of vector control organizations report needing improvement in one or more of five core competencies, such as testing for pesticide resistance [and using] data to drive local decisions about vector control.”
A warning song to keep our children safe
Pay heed to “The House of the Rising Sun”
“There is a house in New Orleans. They call the Rising Sun. And it’s been the ruin of many a poor boy. And, God, I know I’m one.”
The 1960s rock band the Animals will tell you a tale to convince you to get vaccinated. Don’t believe me? Follow along.
The first hints of the song “House of the Rising Sun” rolled out of the hills of Appalachia.
Somewhere in the Golden Triangle, far away from New Orleans, where Virginia, Kentucky, and Tennessee rise in quiet desolation, a warning song about a tailor and a drunk emerged. Sometime around the Civil War, a hint of a tune began. Over the next century, it evolved, until it became cemented in rock culture 50 years ago by The Animals, existing as the version played most commonly today.
In the mid-19th century, medicine shows rambled through the South, stopping in places like Noetown or Daisy. The small towns would empty out for the day to see the entertainers, singers, and jugglers perform. Hundreds gathered in the hot summer day, the entertainment solely a pretext for the traveling doctors to sell their wares, the snake oil, and cure-alls, as well as various patent medicines.
These were isolated towns, with no deliveries, few visitors, and the railroad yet to arrive. Frequently, the only news from outside came from these caravans of entertainers and con men who swept into town. They were like Professor Marvel from The Wizard of Oz, or a current-day Dr. Oz, luring the crowd with false advertising, selling colored water, and then disappearing before you realized you were duped. Today, traveling doctors of the same ilk convince parents to not vaccinate their children, tell them to visit stem cell centers that claim false cures, and offer them a shiny object with one hand while taking their cash with the other.
Yet, there was a positive development in the wake of these patent medicine shows: the entertainment lingered. New songs traveled the same journeys as these medicine shows – new earworms that would then be warbled in the local bars, while doing chores around the barn, or simply during walks on the Appalachian trails.
In 1937, Alan Lomax arrived in Noetown, Ky., with a microphone and an acetate record and recorded the voice of 16-year-old Georgia Turner singing “House of the Rising Sun.” She didn’t know where she heard that song, but most likely picked it up at the medicine show.
One of those singers was Clarence Ashley, who would croon about the Rising Sun Blues. He sang with Doc Cloud and Doc Hauer, who offered tonics for whatever ailed you. Perhaps Georgia Turner heard the song in the early 1900s as well. Her 1937 version contains the lyrics most closely related to the Animals’ tune.
Lomax spent the 1940s gathering songs around the Appalachian South. He put these songs into a songbook and spread them throughout the country. He would also return to New York City and gather in a room with legendary folk singers. They would hear these new lyrics, new sounds, and make them their own.
In that room would be Lead Belly, Pete Seeger, Woody Guthrie, and Josh White, the fathers of folk music. The music Lomax pulled out of the mountains in small towns would become new again in the guitars and harmonicas of the Greenwich Village singers and musicians. Pete Seeger performed with the Weavers, named because they would weave songs from the past into new versions.
“House of the Rising Sun” was woven into the folk music landscape, evolving and growing. Josh White is credited with changing the song from a major key into the minor key we know today. Bob Dylan sang a version. And then in 1964, Eric Burdon and The Animals released their version, which became the standard. An arpeggio guitar opening, the rhythm sped up, a louder sound, and that minor key provides an emotional wallop for this warning song.
Numerous covers followed, including a beautiful version of “Amazing Grace”, sung to the tune of “House of the Rising Sun” by the Blind Boys of Alabama.
The song endures for its melody as well as for its lyrics. This was a warning song, a universal song, “not to do what I have done.” The small towns in Kentucky may have heard of the sinful ways of New Orleans and would spread the message with these songs to avoid the brothels, the drink, and the broken marriages that would reverberate with visits to the Crescent City.
“House of the Rising Sun” is one of the most covered songs, traveling wide and far, no longer with the need for a medicine show. It was a pivotal moment in rock ‘n roll, turning folk music into rock music. The Animals became huge because of this song, and their version became the standard on which all subsequent covers based their version. It made Bob Dylan’s older version seem quaint.
The song has been in my head for a while now. My wife is hoping writing about it will keep it from being played in our household any more. There are various reasons it has been resonating with me, including the following:
- It traces the origins of folk music and the importance of people like Lomax and Guthrie to collect and save Americana.
- The magic of musical evolution – a reminder of how art is built on the work of those who came before, each version with its unique personality.
- The release of “House of the Rising Sun” was a seminal, transformative moment when folk became rock music.
- The lasting power of warning songs.
- The hucksters that enabled this song to be kept alive.
That last one has really stuck with me. The medicine shows are an important part of American history. For instance, Coca-Cola started as one of those patent medicines; it was one of the many concoctions of the Atlanta pharmacist John Stith Pemberton, sold to treat all that ails us. Dr. Pepper, too, was a medicine in a sugary bottle – another that often contained alcohol or cocaine. Society wants a cure-all, and the marketing and selling done during these medicine shows offered placebos.
The hucksters exist in various forms today, selling detoxifications, magic diet cures, psychic powers of healing, or convincing parents that their kids don’t need vaccines. We need a warning song that goes viral to keep our children safe. We are blessed to be in a world without smallpox, almost rid of polio, and we have the knowledge and opportunity to rid the world of other preventable illnesses. Measles was declared eliminated in the United States in 2000; now, outbreaks emerge in every news cycle.
The CDC admits they have not been targeting misinformation well. How can we spread the science, the truth, the message faster than the lies? Better marketing? The answer may be through stories and narratives and song, with the backing of good science. “House of the Rising Sun” is a warning song. Maybe we need more. We need that deep history, that long trail to remind us of the world before vaccines, when everyone knew someone, either in their own household or next door, who succumbed to one of the childhood illnesses.
Let the “House of the Rising Sun” play on. Create a new version, and let that message reverberate, too.
Tell your children; they need to be vaccinated.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
Pay heed to “The House of the Rising Sun”
Pay heed to “The House of the Rising Sun”
“There is a house in New Orleans. They call the Rising Sun. And it’s been the ruin of many a poor boy. And, God, I know I’m one.”
The 1960s rock band the Animals will tell you a tale to convince you to get vaccinated. Don’t believe me? Follow along.
The first hints of the song “House of the Rising Sun” rolled out of the hills of Appalachia.
Somewhere in the Golden Triangle, far away from New Orleans, where Virginia, Kentucky, and Tennessee rise in quiet desolation, a warning song about a tailor and a drunk emerged. Sometime around the Civil War, a hint of a tune began. Over the next century, it evolved, until it became cemented in rock culture 50 years ago by The Animals, existing as the version played most commonly today.
In the mid-19th century, medicine shows rambled through the South, stopping in places like Noetown or Daisy. The small towns would empty out for the day to see the entertainers, singers, and jugglers perform. Hundreds gathered in the hot summer day, the entertainment solely a pretext for the traveling doctors to sell their wares, the snake oil, and cure-alls, as well as various patent medicines.
These were isolated towns, with no deliveries, few visitors, and the railroad yet to arrive. Frequently, the only news from outside came from these caravans of entertainers and con men who swept into town. They were like Professor Marvel from The Wizard of Oz, or a current-day Dr. Oz, luring the crowd with false advertising, selling colored water, and then disappearing before you realized you were duped. Today, traveling doctors of the same ilk convince parents to not vaccinate their children, tell them to visit stem cell centers that claim false cures, and offer them a shiny object with one hand while taking their cash with the other.
Yet, there was a positive development in the wake of these patent medicine shows: the entertainment lingered. New songs traveled the same journeys as these medicine shows – new earworms that would then be warbled in the local bars, while doing chores around the barn, or simply during walks on the Appalachian trails.
In 1937, Alan Lomax arrived in Noetown, Ky., with a microphone and an acetate record and recorded the voice of 16-year-old Georgia Turner singing “House of the Rising Sun.” She didn’t know where she heard that song, but most likely picked it up at the medicine show.
One of those singers was Clarence Ashley, who would croon about the Rising Sun Blues. He sang with Doc Cloud and Doc Hauer, who offered tonics for whatever ailed you. Perhaps Georgia Turner heard the song in the early 1900s as well. Her 1937 version contains the lyrics most closely related to the Animals’ tune.
Lomax spent the 1940s gathering songs around the Appalachian South. He put these songs into a songbook and spread them throughout the country. He would also return to New York City and gather in a room with legendary folk singers. They would hear these new lyrics, new sounds, and make them their own.
In that room would be Lead Belly, Pete Seeger, Woody Guthrie, and Josh White, the fathers of folk music. The music Lomax pulled out of the mountains in small towns would become new again in the guitars and harmonicas of the Greenwich Village singers and musicians. Pete Seeger performed with the Weavers, named because they would weave songs from the past into new versions.
“House of the Rising Sun” was woven into the folk music landscape, evolving and growing. Josh White is credited with changing the song from a major key into the minor key we know today. Bob Dylan sang a version. And then in 1964, Eric Burdon and The Animals released their version, which became the standard. An arpeggio guitar opening, the rhythm sped up, a louder sound, and that minor key provides an emotional wallop for this warning song.
Numerous covers followed, including a beautiful version of “Amazing Grace”, sung to the tune of “House of the Rising Sun” by the Blind Boys of Alabama.
The song endures for its melody as well as for its lyrics. This was a warning song, a universal song, “not to do what I have done.” The small towns in Kentucky may have heard of the sinful ways of New Orleans and would spread the message with these songs to avoid the brothels, the drink, and the broken marriages that would reverberate with visits to the Crescent City.
“House of the Rising Sun” is one of the most covered songs, traveling wide and far, no longer with the need for a medicine show. It was a pivotal moment in rock ‘n roll, turning folk music into rock music. The Animals became huge because of this song, and their version became the standard on which all subsequent covers based their version. It made Bob Dylan’s older version seem quaint.
The song has been in my head for a while now. My wife is hoping writing about it will keep it from being played in our household any more. There are various reasons it has been resonating with me, including the following:
- It traces the origins of folk music and the importance of people like Lomax and Guthrie to collect and save Americana.
- The magic of musical evolution – a reminder of how art is built on the work of those who came before, each version with its unique personality.
- The release of “House of the Rising Sun” was a seminal, transformative moment when folk became rock music.
- The lasting power of warning songs.
- The hucksters that enabled this song to be kept alive.
That last one has really stuck with me. The medicine shows are an important part of American history. For instance, Coca-Cola started as one of those patent medicines; it was one of the many concoctions of the Atlanta pharmacist John Stith Pemberton, sold to treat all that ails us. Dr. Pepper, too, was a medicine in a sugary bottle – another that often contained alcohol or cocaine. Society wants a cure-all, and the marketing and selling done during these medicine shows offered placebos.
The hucksters exist in various forms today, selling detoxifications, magic diet cures, psychic powers of healing, or convincing parents that their kids don’t need vaccines. We need a warning song that goes viral to keep our children safe. We are blessed to be in a world without smallpox, almost rid of polio, and we have the knowledge and opportunity to rid the world of other preventable illnesses. Measles was declared eliminated in the United States in 2000; now, outbreaks emerge in every news cycle.
The CDC admits they have not been targeting misinformation well. How can we spread the science, the truth, the message faster than the lies? Better marketing? The answer may be through stories and narratives and song, with the backing of good science. “House of the Rising Sun” is a warning song. Maybe we need more. We need that deep history, that long trail to remind us of the world before vaccines, when everyone knew someone, either in their own household or next door, who succumbed to one of the childhood illnesses.
Let the “House of the Rising Sun” play on. Create a new version, and let that message reverberate, too.
Tell your children; they need to be vaccinated.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
“There is a house in New Orleans. They call the Rising Sun. And it’s been the ruin of many a poor boy. And, God, I know I’m one.”
The 1960s rock band the Animals will tell you a tale to convince you to get vaccinated. Don’t believe me? Follow along.
The first hints of the song “House of the Rising Sun” rolled out of the hills of Appalachia.
Somewhere in the Golden Triangle, far away from New Orleans, where Virginia, Kentucky, and Tennessee rise in quiet desolation, a warning song about a tailor and a drunk emerged. Sometime around the Civil War, a hint of a tune began. Over the next century, it evolved, until it became cemented in rock culture 50 years ago by The Animals, existing as the version played most commonly today.
In the mid-19th century, medicine shows rambled through the South, stopping in places like Noetown or Daisy. The small towns would empty out for the day to see the entertainers, singers, and jugglers perform. Hundreds gathered in the hot summer day, the entertainment solely a pretext for the traveling doctors to sell their wares, the snake oil, and cure-alls, as well as various patent medicines.
These were isolated towns, with no deliveries, few visitors, and the railroad yet to arrive. Frequently, the only news from outside came from these caravans of entertainers and con men who swept into town. They were like Professor Marvel from The Wizard of Oz, or a current-day Dr. Oz, luring the crowd with false advertising, selling colored water, and then disappearing before you realized you were duped. Today, traveling doctors of the same ilk convince parents to not vaccinate their children, tell them to visit stem cell centers that claim false cures, and offer them a shiny object with one hand while taking their cash with the other.
Yet, there was a positive development in the wake of these patent medicine shows: the entertainment lingered. New songs traveled the same journeys as these medicine shows – new earworms that would then be warbled in the local bars, while doing chores around the barn, or simply during walks on the Appalachian trails.
In 1937, Alan Lomax arrived in Noetown, Ky., with a microphone and an acetate record and recorded the voice of 16-year-old Georgia Turner singing “House of the Rising Sun.” She didn’t know where she heard that song, but most likely picked it up at the medicine show.
One of those singers was Clarence Ashley, who would croon about the Rising Sun Blues. He sang with Doc Cloud and Doc Hauer, who offered tonics for whatever ailed you. Perhaps Georgia Turner heard the song in the early 1900s as well. Her 1937 version contains the lyrics most closely related to the Animals’ tune.
Lomax spent the 1940s gathering songs around the Appalachian South. He put these songs into a songbook and spread them throughout the country. He would also return to New York City and gather in a room with legendary folk singers. They would hear these new lyrics, new sounds, and make them their own.
In that room would be Lead Belly, Pete Seeger, Woody Guthrie, and Josh White, the fathers of folk music. The music Lomax pulled out of the mountains in small towns would become new again in the guitars and harmonicas of the Greenwich Village singers and musicians. Pete Seeger performed with the Weavers, named because they would weave songs from the past into new versions.
“House of the Rising Sun” was woven into the folk music landscape, evolving and growing. Josh White is credited with changing the song from a major key into the minor key we know today. Bob Dylan sang a version. And then in 1964, Eric Burdon and The Animals released their version, which became the standard. An arpeggio guitar opening, the rhythm sped up, a louder sound, and that minor key provides an emotional wallop for this warning song.
Numerous covers followed, including a beautiful version of “Amazing Grace”, sung to the tune of “House of the Rising Sun” by the Blind Boys of Alabama.
The song endures for its melody as well as for its lyrics. This was a warning song, a universal song, “not to do what I have done.” The small towns in Kentucky may have heard of the sinful ways of New Orleans and would spread the message with these songs to avoid the brothels, the drink, and the broken marriages that would reverberate with visits to the Crescent City.
“House of the Rising Sun” is one of the most covered songs, traveling wide and far, no longer with the need for a medicine show. It was a pivotal moment in rock ‘n roll, turning folk music into rock music. The Animals became huge because of this song, and their version became the standard on which all subsequent covers based their version. It made Bob Dylan’s older version seem quaint.
The song has been in my head for a while now. My wife is hoping writing about it will keep it from being played in our household any more. There are various reasons it has been resonating with me, including the following:
- It traces the origins of folk music and the importance of people like Lomax and Guthrie to collect and save Americana.
- The magic of musical evolution – a reminder of how art is built on the work of those who came before, each version with its unique personality.
- The release of “House of the Rising Sun” was a seminal, transformative moment when folk became rock music.
- The lasting power of warning songs.
- The hucksters that enabled this song to be kept alive.
That last one has really stuck with me. The medicine shows are an important part of American history. For instance, Coca-Cola started as one of those patent medicines; it was one of the many concoctions of the Atlanta pharmacist John Stith Pemberton, sold to treat all that ails us. Dr. Pepper, too, was a medicine in a sugary bottle – another that often contained alcohol or cocaine. Society wants a cure-all, and the marketing and selling done during these medicine shows offered placebos.
The hucksters exist in various forms today, selling detoxifications, magic diet cures, psychic powers of healing, or convincing parents that their kids don’t need vaccines. We need a warning song that goes viral to keep our children safe. We are blessed to be in a world without smallpox, almost rid of polio, and we have the knowledge and opportunity to rid the world of other preventable illnesses. Measles was declared eliminated in the United States in 2000; now, outbreaks emerge in every news cycle.
The CDC admits they have not been targeting misinformation well. How can we spread the science, the truth, the message faster than the lies? Better marketing? The answer may be through stories and narratives and song, with the backing of good science. “House of the Rising Sun” is a warning song. Maybe we need more. We need that deep history, that long trail to remind us of the world before vaccines, when everyone knew someone, either in their own household or next door, who succumbed to one of the childhood illnesses.
Let the “House of the Rising Sun” play on. Create a new version, and let that message reverberate, too.
Tell your children; they need to be vaccinated.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
FDA approves new treatment for hospital-acquired, ventilator-associated bacterial pneumonia
authorizing it for the treatment of both hospital-acquired and ventilator-associated bacterial pneumonia.
The new indication is for patients 18 years and older. It was based on results of a multinational, double-blind study that compared Zerbaxa with a different antibacterial drug in 726 patients hospitalized with hospital-acquired/ventilator-associated bacterial pneumonia. Mortality and cure rates were similar in the Zerbaxa and comparator groups.
The most common adverse events observed in the trial were elevated liver enzyme levels, renal impairment or failure, and diarrhea. Patients with hypersensitivity to beta-lactam drugs should not be receive Zerbaxa.
“A key global challenge we face as a public health agency is addressing the threat of antimicrobial-resistant infections. Hospital-acquired and ventilator-associated bacterial pneumonia are serious infections that can result in death in some patients. ... That’s why, among our other efforts to address antimicrobial resistance, we’re focused on facilitating the development of safe and effective new treatments to give patients more options to fight life-threatening infections,” said Amy Abernethy, MD, PhD, the FDA’s principal deputy commissioner.
Zerbaxa was initially approved in 2014 for treatment of complicated intra-abdominal and urinary tract infections.
Find the full press release on the FDA website.
authorizing it for the treatment of both hospital-acquired and ventilator-associated bacterial pneumonia.
The new indication is for patients 18 years and older. It was based on results of a multinational, double-blind study that compared Zerbaxa with a different antibacterial drug in 726 patients hospitalized with hospital-acquired/ventilator-associated bacterial pneumonia. Mortality and cure rates were similar in the Zerbaxa and comparator groups.
The most common adverse events observed in the trial were elevated liver enzyme levels, renal impairment or failure, and diarrhea. Patients with hypersensitivity to beta-lactam drugs should not be receive Zerbaxa.
“A key global challenge we face as a public health agency is addressing the threat of antimicrobial-resistant infections. Hospital-acquired and ventilator-associated bacterial pneumonia are serious infections that can result in death in some patients. ... That’s why, among our other efforts to address antimicrobial resistance, we’re focused on facilitating the development of safe and effective new treatments to give patients more options to fight life-threatening infections,” said Amy Abernethy, MD, PhD, the FDA’s principal deputy commissioner.
Zerbaxa was initially approved in 2014 for treatment of complicated intra-abdominal and urinary tract infections.
Find the full press release on the FDA website.
authorizing it for the treatment of both hospital-acquired and ventilator-associated bacterial pneumonia.
The new indication is for patients 18 years and older. It was based on results of a multinational, double-blind study that compared Zerbaxa with a different antibacterial drug in 726 patients hospitalized with hospital-acquired/ventilator-associated bacterial pneumonia. Mortality and cure rates were similar in the Zerbaxa and comparator groups.
The most common adverse events observed in the trial were elevated liver enzyme levels, renal impairment or failure, and diarrhea. Patients with hypersensitivity to beta-lactam drugs should not be receive Zerbaxa.
“A key global challenge we face as a public health agency is addressing the threat of antimicrobial-resistant infections. Hospital-acquired and ventilator-associated bacterial pneumonia are serious infections that can result in death in some patients. ... That’s why, among our other efforts to address antimicrobial resistance, we’re focused on facilitating the development of safe and effective new treatments to give patients more options to fight life-threatening infections,” said Amy Abernethy, MD, PhD, the FDA’s principal deputy commissioner.
Zerbaxa was initially approved in 2014 for treatment of complicated intra-abdominal and urinary tract infections.
Find the full press release on the FDA website.
Why you should re-credential with Medicare as a hospitalist
CMS needs a better database of hospitalist information
In April 2017, the Centers for Medicare and Medicaid Services implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it.
Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by the CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce concurrent care denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day.
And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to re-credentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist.
While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “apples to apples” comparisons
A second reason to re-credential as a hospitalist is to ensure that when the CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes.
The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than has the mix of CPT codes reported by the CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time!
The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic).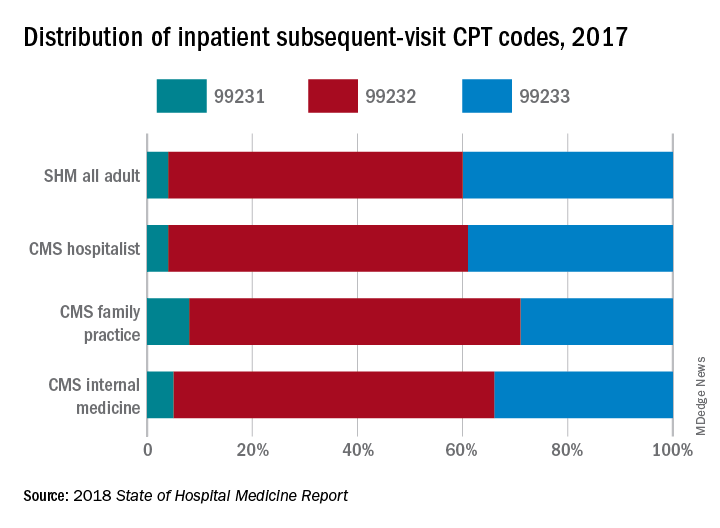
If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure the CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity.
Improve CMS data used for research purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall health care system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system.
We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for health care services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at the CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself re-credentialed in PECOS using the C6 “hospitalist” physician specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
CMS needs a better database of hospitalist information
CMS needs a better database of hospitalist information
In April 2017, the Centers for Medicare and Medicaid Services implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it.
Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by the CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce concurrent care denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day.
And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to re-credentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist.
While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “apples to apples” comparisons
A second reason to re-credential as a hospitalist is to ensure that when the CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes.
The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than has the mix of CPT codes reported by the CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time!
The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic).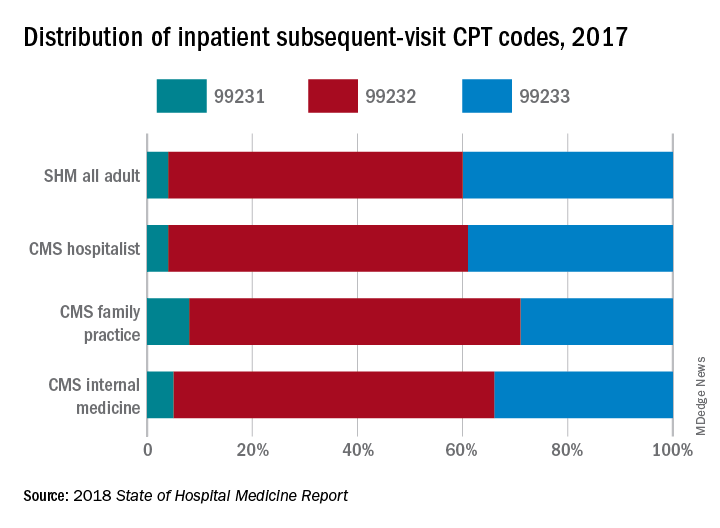
If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure the CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity.
Improve CMS data used for research purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall health care system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system.
We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for health care services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at the CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself re-credentialed in PECOS using the C6 “hospitalist” physician specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
In April 2017, the Centers for Medicare and Medicaid Services implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it.
Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by the CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce concurrent care denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day.
And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to re-credentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist.
While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “apples to apples” comparisons
A second reason to re-credential as a hospitalist is to ensure that when the CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes.
The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than has the mix of CPT codes reported by the CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time!
The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic).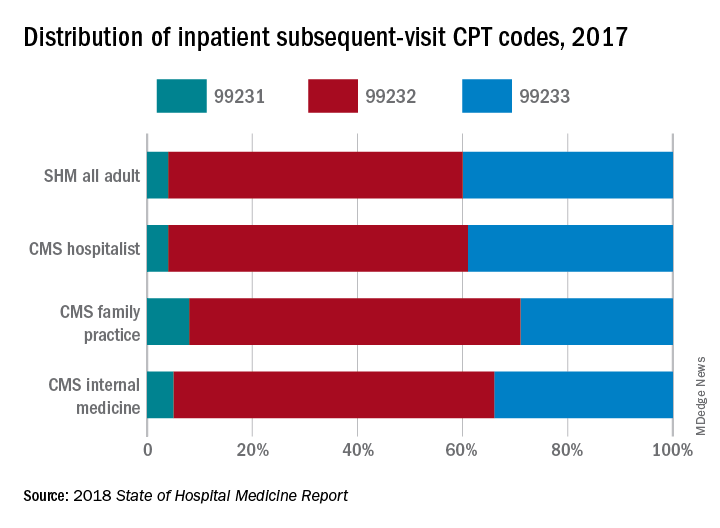
If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure the CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity.
Improve CMS data used for research purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall health care system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system.
We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for health care services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at the CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself re-credentialed in PECOS using the C6 “hospitalist” physician specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
Hospitalists can help alleviate rising drug costs
Four key actions providers can take
Because of the increasing costs of prescription drugs and medical therapies, many patients are unable to afford the treatment they need that could improve their health or even save their lives. In the United States, drug manufacturers can set their own prices – a policy that has resulted in overall medicine costs being far higher than in other places around the globe. Increasingly, insurers are passing the costs along to patients through higher deductibles, and pharmaceutical companies are making record profits.
Something needs to change in order to achieve the right balance between maintaining pharmaceutical innovation and ensuring patients have proper access to treatments they need. Waiting for legislation, regulation, or the courts is not an effective short-term solution. Instead, hospitalists can take immediate actions to help by alleviating the costs for as many patients possible.
Historical context
Many might be wondering how prescription costs became so imbalanced in the first place. Here are a few important factors that played a role in the dramatic price increase of pharmaceuticals:
Entrance of generic drugs: Around 2012 the entrance of generic drugs caused major unexpected competition in the medical industry. During this time, many insurers were promoting the generic drugs and not allowing brand names to be covered when a generic substitute was available.
“Orphan drugs” and manufacturer pricing: In 2014, 33 new brand-name drugs were launched in the United States, and only 8 had a direct price competitor at the time they were introduced. In addition, manufacturers were free to set their prices. Over the past decade, introductory prices for brand name drugs have reached unprecedented levels. Furthermore, manufacturers use the patent protections to increase their prices every year, even when no significant improvements have been made to the drug.
Expiring patents: According to research, there are 182 drugs that no longer have patent protection or any associated generics available. This creates opportunities for manufacturers to maintain patent-era pricing or even engage in price gouging.
Lack of robust competition: Several high-priced blockbuster drugs hit the market to treat serious diseases, most of which do not have generic brand substitutes, which leaves only one option for patients – and it’s usually not affordable. According to research, more than 500 drugs have only one marketed generic. In addition, manufacturer mergers and acquisitions have occurred, which has led to a more concentrated and less competitive market for pricing.
Stricter Food and Drug Administration policies: American consumers have access to the safest and most advanced pharmaceutical system in the world, which requires several trials and testing before the drug can be approved and brought to the market. Despite the benefits of these strict procedures, the downside means higher costs for the brand and manufacturer that they will want to recoup through the price of the drug on the market.
Number of new drugs allowed to enter the market: New drugs that enter the market in the United States do so more quickly than in most other countries. Research shows the U.S. pharmaceutical market contributes to 45% of the global pharmaceutical market. The $76 billion in research and development that pharmaceutical companies claim overlooks the ways that U.S. employers and taxpayers pay for at least 44% through tax subsidies and credits. What makes it worse is that research shows most corporate research and development is directed at minimally innovative new drugs, using the system to secure patents and charge monopoly prices.
Compared with other high-income countries, the United States spends the most per capita on prescription drugs. While insured U.S. patients often pay little or nothing for generic prescriptions, they can be billed tens of thousands of dollars for certain high-priced medicines. The United States has the highest rate of insured patients skipping or not filling prescriptions because of cost. For example, the price of EpiPens, a drug delivery system that is crucial for persons experiencing life-threatening allergic reactions, has increased more than $500 in just 9 years.
How to alleviate rising drug costs
The good news is that hospitalists can do something about the high costs of pharmaceuticals.
Understand and offer alternative ways for drug intake: Many patients admitted to a hospital with severe infections are initially started with intravenous medications. Although conversion from intravenous to oral therapy is inappropriate for a patient who is critically ill or has an inability to absorb oral medications, every hospital will have a certain number of patients who are eligible for a switch from intravenous to oral therapy.
The World Health Organization (WHO) reports that the irrational use of medicines is a major problem worldwide, including antibiotics. Switching from IV to oral enables one to select a cheaper or older antibiotic that is as effective as the IV antibiotic. However, this requires breaking the belief that many physicians still have that IV medications’ bioavailability is stronger and creates less susceptibility to the illness reoccurring in the patient. For many medications, essentially the same amount of drug is found in the blood when given intravenously or orally. In addition, research has shown several benefits beyond cost reduction for oral over IV, such as earlier discharge and reduced risk of infections.
Limit unnecessary antibiotic prescriptions and consider antibiotics stewardship programs: The Center for Disease Control reports that one in three (47 million) antibiotic prescriptions are unnecessary. Most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses including common colds, viral sore throats, bronchitis, and sinus and ear infections that do not respond to antibiotics. Although the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) in 2015, which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020, hospitalists can still do more by being extremely cautious with prescribing drugs to patients. Use appropriate consultants whenever necessary to suggest the right drug. For example, consider an infectious disease specialist to suggest the appropriate type and length of time for an antibiotic. In addition, hospital-based programs dedicated to improving antibiotic use, known as antibiotic stewardship programs (ASPs), have been shown to optimize the treatment of infections and reduce adverse events associated with antibiotic use.
Review labs and vitals carefully and encourage a higher level of patient care beyond the digital tools available: Studies have shown an oversight in an exam (a “miss”) can result in real consequences, including death. Our $3.4 trillion health care system is responsible for more than a quarter of a million deaths per year because of medical error. Much of that is a result of poorly coordinated care, poor communication, patients falling through the cracks, or knowledge not being transferred. “True clinical judgment is more than addressing the avalanche of blood work, imaging, and lab tests; it is about using human skills to understand where the patient is in the trajectory of a life and the disease, what the nature of the patient’s family and social circumstances is, and how much they want done,” wrote Dr. Abraham Verghese in the New York Times in 2018 (“How Tech Can Turn Doctors into Clerical Workers”). This also means understanding whether the patient is on any other type of medication and, as a result, having knowledge of possible consequences for drug interactions. Always look for safe medications or discontinue the use of any unnecessary drugs the patient is currently taking.
Allow pharmacies to automatically substitute less expensive equivalent drugs: When prescribing pharmaceuticals for patients, determine if there are any substitutes that can help alleviate costs while delivering equivalent care to the patient. This requires excellent ongoing communication with pharmacists and understanding the substitutes available, as well as any side effects or consequences.
Hospitalists can make a difference
There are many variables that play a role in rising pharmaceutical costs in the United States. One of the most significant is that there are no strategies in place to control pricing of drugs and the profits made by the pharmaceutical companies.
Although finding new drugs that can cure major life-threatening diseases or illnesses is important, so is ensuring that more patients have access to such drugs at a reasonable cost. While there are several ways that the government can and should help with enabling and supporting this balance, it most likely requires such large changes that it will take a long time. As a result, it is important for hospitalists to find effective short-term solutions that can be implemented right away to alleviate the rising costs of pharmaceuticals and provide proper patient care regardless of their economic status – all of which requires better research, analysis, and comparison before prescribing treatment to patients.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Contact him at [email protected]. Dr. Devireddy is a hospitalist based at Sri Ramachandra Medical Centre, Porur, Tamilnadu, India. Contact her at [email protected].
FURTHER READING
Olson and Sheiner (2017). “The Hutchins Center Explains: Prescription drug spending” Brooking.edu
Lo, Chris (2018). “Cost control: drug pricing policies around the world,” Pharmaceutical-Technology.com
Center for Disease Control and Prevention. (2016). 1 in 3 antibiotic prescriptions unnecessary. Retrieved Jan 31, 2019, from https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
Verghese, Abraham (2018). “How Tech Can Turn Doctors Into Clerical Workers” NYTimes.Com
Waxman, Corr, Martin et al (2017). “Getting to the Root of High Prescription Drug Prices” Commonwealthfund.org
American Council on Science and Health. (2018). Government Is The Big Reason EpiPen And Other Generics Are So Expensive. Retrieved Jan 31, 2019, from https://www.acsh.org/news/2018/06/23/government-big-reason-epipen-and-other-generics-are-so-expensive-13114
Statista. (2018). U.S. Pharmaceutical Industry – Statistics & Facts. Retrieved Jan 31, 2019, from https://www.statista.com/topics/1719/pharmaceutical-industry/
Four key actions providers can take
Four key actions providers can take
Because of the increasing costs of prescription drugs and medical therapies, many patients are unable to afford the treatment they need that could improve their health or even save their lives. In the United States, drug manufacturers can set their own prices – a policy that has resulted in overall medicine costs being far higher than in other places around the globe. Increasingly, insurers are passing the costs along to patients through higher deductibles, and pharmaceutical companies are making record profits.
Something needs to change in order to achieve the right balance between maintaining pharmaceutical innovation and ensuring patients have proper access to treatments they need. Waiting for legislation, regulation, or the courts is not an effective short-term solution. Instead, hospitalists can take immediate actions to help by alleviating the costs for as many patients possible.
Historical context
Many might be wondering how prescription costs became so imbalanced in the first place. Here are a few important factors that played a role in the dramatic price increase of pharmaceuticals:
Entrance of generic drugs: Around 2012 the entrance of generic drugs caused major unexpected competition in the medical industry. During this time, many insurers were promoting the generic drugs and not allowing brand names to be covered when a generic substitute was available.
“Orphan drugs” and manufacturer pricing: In 2014, 33 new brand-name drugs were launched in the United States, and only 8 had a direct price competitor at the time they were introduced. In addition, manufacturers were free to set their prices. Over the past decade, introductory prices for brand name drugs have reached unprecedented levels. Furthermore, manufacturers use the patent protections to increase their prices every year, even when no significant improvements have been made to the drug.
Expiring patents: According to research, there are 182 drugs that no longer have patent protection or any associated generics available. This creates opportunities for manufacturers to maintain patent-era pricing or even engage in price gouging.
Lack of robust competition: Several high-priced blockbuster drugs hit the market to treat serious diseases, most of which do not have generic brand substitutes, which leaves only one option for patients – and it’s usually not affordable. According to research, more than 500 drugs have only one marketed generic. In addition, manufacturer mergers and acquisitions have occurred, which has led to a more concentrated and less competitive market for pricing.
Stricter Food and Drug Administration policies: American consumers have access to the safest and most advanced pharmaceutical system in the world, which requires several trials and testing before the drug can be approved and brought to the market. Despite the benefits of these strict procedures, the downside means higher costs for the brand and manufacturer that they will want to recoup through the price of the drug on the market.
Number of new drugs allowed to enter the market: New drugs that enter the market in the United States do so more quickly than in most other countries. Research shows the U.S. pharmaceutical market contributes to 45% of the global pharmaceutical market. The $76 billion in research and development that pharmaceutical companies claim overlooks the ways that U.S. employers and taxpayers pay for at least 44% through tax subsidies and credits. What makes it worse is that research shows most corporate research and development is directed at minimally innovative new drugs, using the system to secure patents and charge monopoly prices.
Compared with other high-income countries, the United States spends the most per capita on prescription drugs. While insured U.S. patients often pay little or nothing for generic prescriptions, they can be billed tens of thousands of dollars for certain high-priced medicines. The United States has the highest rate of insured patients skipping or not filling prescriptions because of cost. For example, the price of EpiPens, a drug delivery system that is crucial for persons experiencing life-threatening allergic reactions, has increased more than $500 in just 9 years.
How to alleviate rising drug costs
The good news is that hospitalists can do something about the high costs of pharmaceuticals.
Understand and offer alternative ways for drug intake: Many patients admitted to a hospital with severe infections are initially started with intravenous medications. Although conversion from intravenous to oral therapy is inappropriate for a patient who is critically ill or has an inability to absorb oral medications, every hospital will have a certain number of patients who are eligible for a switch from intravenous to oral therapy.
The World Health Organization (WHO) reports that the irrational use of medicines is a major problem worldwide, including antibiotics. Switching from IV to oral enables one to select a cheaper or older antibiotic that is as effective as the IV antibiotic. However, this requires breaking the belief that many physicians still have that IV medications’ bioavailability is stronger and creates less susceptibility to the illness reoccurring in the patient. For many medications, essentially the same amount of drug is found in the blood when given intravenously or orally. In addition, research has shown several benefits beyond cost reduction for oral over IV, such as earlier discharge and reduced risk of infections.
Limit unnecessary antibiotic prescriptions and consider antibiotics stewardship programs: The Center for Disease Control reports that one in three (47 million) antibiotic prescriptions are unnecessary. Most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses including common colds, viral sore throats, bronchitis, and sinus and ear infections that do not respond to antibiotics. Although the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) in 2015, which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020, hospitalists can still do more by being extremely cautious with prescribing drugs to patients. Use appropriate consultants whenever necessary to suggest the right drug. For example, consider an infectious disease specialist to suggest the appropriate type and length of time for an antibiotic. In addition, hospital-based programs dedicated to improving antibiotic use, known as antibiotic stewardship programs (ASPs), have been shown to optimize the treatment of infections and reduce adverse events associated with antibiotic use.
Review labs and vitals carefully and encourage a higher level of patient care beyond the digital tools available: Studies have shown an oversight in an exam (a “miss”) can result in real consequences, including death. Our $3.4 trillion health care system is responsible for more than a quarter of a million deaths per year because of medical error. Much of that is a result of poorly coordinated care, poor communication, patients falling through the cracks, or knowledge not being transferred. “True clinical judgment is more than addressing the avalanche of blood work, imaging, and lab tests; it is about using human skills to understand where the patient is in the trajectory of a life and the disease, what the nature of the patient’s family and social circumstances is, and how much they want done,” wrote Dr. Abraham Verghese in the New York Times in 2018 (“How Tech Can Turn Doctors into Clerical Workers”). This also means understanding whether the patient is on any other type of medication and, as a result, having knowledge of possible consequences for drug interactions. Always look for safe medications or discontinue the use of any unnecessary drugs the patient is currently taking.
Allow pharmacies to automatically substitute less expensive equivalent drugs: When prescribing pharmaceuticals for patients, determine if there are any substitutes that can help alleviate costs while delivering equivalent care to the patient. This requires excellent ongoing communication with pharmacists and understanding the substitutes available, as well as any side effects or consequences.
Hospitalists can make a difference
There are many variables that play a role in rising pharmaceutical costs in the United States. One of the most significant is that there are no strategies in place to control pricing of drugs and the profits made by the pharmaceutical companies.
Although finding new drugs that can cure major life-threatening diseases or illnesses is important, so is ensuring that more patients have access to such drugs at a reasonable cost. While there are several ways that the government can and should help with enabling and supporting this balance, it most likely requires such large changes that it will take a long time. As a result, it is important for hospitalists to find effective short-term solutions that can be implemented right away to alleviate the rising costs of pharmaceuticals and provide proper patient care regardless of their economic status – all of which requires better research, analysis, and comparison before prescribing treatment to patients.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Contact him at [email protected]. Dr. Devireddy is a hospitalist based at Sri Ramachandra Medical Centre, Porur, Tamilnadu, India. Contact her at [email protected].
FURTHER READING
Olson and Sheiner (2017). “The Hutchins Center Explains: Prescription drug spending” Brooking.edu
Lo, Chris (2018). “Cost control: drug pricing policies around the world,” Pharmaceutical-Technology.com
Center for Disease Control and Prevention. (2016). 1 in 3 antibiotic prescriptions unnecessary. Retrieved Jan 31, 2019, from https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
Verghese, Abraham (2018). “How Tech Can Turn Doctors Into Clerical Workers” NYTimes.Com
Waxman, Corr, Martin et al (2017). “Getting to the Root of High Prescription Drug Prices” Commonwealthfund.org
American Council on Science and Health. (2018). Government Is The Big Reason EpiPen And Other Generics Are So Expensive. Retrieved Jan 31, 2019, from https://www.acsh.org/news/2018/06/23/government-big-reason-epipen-and-other-generics-are-so-expensive-13114
Statista. (2018). U.S. Pharmaceutical Industry – Statistics & Facts. Retrieved Jan 31, 2019, from https://www.statista.com/topics/1719/pharmaceutical-industry/
Because of the increasing costs of prescription drugs and medical therapies, many patients are unable to afford the treatment they need that could improve their health or even save their lives. In the United States, drug manufacturers can set their own prices – a policy that has resulted in overall medicine costs being far higher than in other places around the globe. Increasingly, insurers are passing the costs along to patients through higher deductibles, and pharmaceutical companies are making record profits.
Something needs to change in order to achieve the right balance between maintaining pharmaceutical innovation and ensuring patients have proper access to treatments they need. Waiting for legislation, regulation, or the courts is not an effective short-term solution. Instead, hospitalists can take immediate actions to help by alleviating the costs for as many patients possible.
Historical context
Many might be wondering how prescription costs became so imbalanced in the first place. Here are a few important factors that played a role in the dramatic price increase of pharmaceuticals:
Entrance of generic drugs: Around 2012 the entrance of generic drugs caused major unexpected competition in the medical industry. During this time, many insurers were promoting the generic drugs and not allowing brand names to be covered when a generic substitute was available.
“Orphan drugs” and manufacturer pricing: In 2014, 33 new brand-name drugs were launched in the United States, and only 8 had a direct price competitor at the time they were introduced. In addition, manufacturers were free to set their prices. Over the past decade, introductory prices for brand name drugs have reached unprecedented levels. Furthermore, manufacturers use the patent protections to increase their prices every year, even when no significant improvements have been made to the drug.
Expiring patents: According to research, there are 182 drugs that no longer have patent protection or any associated generics available. This creates opportunities for manufacturers to maintain patent-era pricing or even engage in price gouging.
Lack of robust competition: Several high-priced blockbuster drugs hit the market to treat serious diseases, most of which do not have generic brand substitutes, which leaves only one option for patients – and it’s usually not affordable. According to research, more than 500 drugs have only one marketed generic. In addition, manufacturer mergers and acquisitions have occurred, which has led to a more concentrated and less competitive market for pricing.
Stricter Food and Drug Administration policies: American consumers have access to the safest and most advanced pharmaceutical system in the world, which requires several trials and testing before the drug can be approved and brought to the market. Despite the benefits of these strict procedures, the downside means higher costs for the brand and manufacturer that they will want to recoup through the price of the drug on the market.
Number of new drugs allowed to enter the market: New drugs that enter the market in the United States do so more quickly than in most other countries. Research shows the U.S. pharmaceutical market contributes to 45% of the global pharmaceutical market. The $76 billion in research and development that pharmaceutical companies claim overlooks the ways that U.S. employers and taxpayers pay for at least 44% through tax subsidies and credits. What makes it worse is that research shows most corporate research and development is directed at minimally innovative new drugs, using the system to secure patents and charge monopoly prices.
Compared with other high-income countries, the United States spends the most per capita on prescription drugs. While insured U.S. patients often pay little or nothing for generic prescriptions, they can be billed tens of thousands of dollars for certain high-priced medicines. The United States has the highest rate of insured patients skipping or not filling prescriptions because of cost. For example, the price of EpiPens, a drug delivery system that is crucial for persons experiencing life-threatening allergic reactions, has increased more than $500 in just 9 years.
How to alleviate rising drug costs
The good news is that hospitalists can do something about the high costs of pharmaceuticals.
Understand and offer alternative ways for drug intake: Many patients admitted to a hospital with severe infections are initially started with intravenous medications. Although conversion from intravenous to oral therapy is inappropriate for a patient who is critically ill or has an inability to absorb oral medications, every hospital will have a certain number of patients who are eligible for a switch from intravenous to oral therapy.
The World Health Organization (WHO) reports that the irrational use of medicines is a major problem worldwide, including antibiotics. Switching from IV to oral enables one to select a cheaper or older antibiotic that is as effective as the IV antibiotic. However, this requires breaking the belief that many physicians still have that IV medications’ bioavailability is stronger and creates less susceptibility to the illness reoccurring in the patient. For many medications, essentially the same amount of drug is found in the blood when given intravenously or orally. In addition, research has shown several benefits beyond cost reduction for oral over IV, such as earlier discharge and reduced risk of infections.
Limit unnecessary antibiotic prescriptions and consider antibiotics stewardship programs: The Center for Disease Control reports that one in three (47 million) antibiotic prescriptions are unnecessary. Most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses including common colds, viral sore throats, bronchitis, and sinus and ear infections that do not respond to antibiotics. Although the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) in 2015, which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020, hospitalists can still do more by being extremely cautious with prescribing drugs to patients. Use appropriate consultants whenever necessary to suggest the right drug. For example, consider an infectious disease specialist to suggest the appropriate type and length of time for an antibiotic. In addition, hospital-based programs dedicated to improving antibiotic use, known as antibiotic stewardship programs (ASPs), have been shown to optimize the treatment of infections and reduce adverse events associated with antibiotic use.
Review labs and vitals carefully and encourage a higher level of patient care beyond the digital tools available: Studies have shown an oversight in an exam (a “miss”) can result in real consequences, including death. Our $3.4 trillion health care system is responsible for more than a quarter of a million deaths per year because of medical error. Much of that is a result of poorly coordinated care, poor communication, patients falling through the cracks, or knowledge not being transferred. “True clinical judgment is more than addressing the avalanche of blood work, imaging, and lab tests; it is about using human skills to understand where the patient is in the trajectory of a life and the disease, what the nature of the patient’s family and social circumstances is, and how much they want done,” wrote Dr. Abraham Verghese in the New York Times in 2018 (“How Tech Can Turn Doctors into Clerical Workers”). This also means understanding whether the patient is on any other type of medication and, as a result, having knowledge of possible consequences for drug interactions. Always look for safe medications or discontinue the use of any unnecessary drugs the patient is currently taking.
Allow pharmacies to automatically substitute less expensive equivalent drugs: When prescribing pharmaceuticals for patients, determine if there are any substitutes that can help alleviate costs while delivering equivalent care to the patient. This requires excellent ongoing communication with pharmacists and understanding the substitutes available, as well as any side effects or consequences.
Hospitalists can make a difference
There are many variables that play a role in rising pharmaceutical costs in the United States. One of the most significant is that there are no strategies in place to control pricing of drugs and the profits made by the pharmaceutical companies.
Although finding new drugs that can cure major life-threatening diseases or illnesses is important, so is ensuring that more patients have access to such drugs at a reasonable cost. While there are several ways that the government can and should help with enabling and supporting this balance, it most likely requires such large changes that it will take a long time. As a result, it is important for hospitalists to find effective short-term solutions that can be implemented right away to alleviate the rising costs of pharmaceuticals and provide proper patient care regardless of their economic status – all of which requires better research, analysis, and comparison before prescribing treatment to patients.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Contact him at [email protected]. Dr. Devireddy is a hospitalist based at Sri Ramachandra Medical Centre, Porur, Tamilnadu, India. Contact her at [email protected].
FURTHER READING
Olson and Sheiner (2017). “The Hutchins Center Explains: Prescription drug spending” Brooking.edu
Lo, Chris (2018). “Cost control: drug pricing policies around the world,” Pharmaceutical-Technology.com
Center for Disease Control and Prevention. (2016). 1 in 3 antibiotic prescriptions unnecessary. Retrieved Jan 31, 2019, from https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
Verghese, Abraham (2018). “How Tech Can Turn Doctors Into Clerical Workers” NYTimes.Com
Waxman, Corr, Martin et al (2017). “Getting to the Root of High Prescription Drug Prices” Commonwealthfund.org
American Council on Science and Health. (2018). Government Is The Big Reason EpiPen And Other Generics Are So Expensive. Retrieved Jan 31, 2019, from https://www.acsh.org/news/2018/06/23/government-big-reason-epipen-and-other-generics-are-so-expensive-13114
Statista. (2018). U.S. Pharmaceutical Industry – Statistics & Facts. Retrieved Jan 31, 2019, from https://www.statista.com/topics/1719/pharmaceutical-industry/
HM19: Things we do for no reason
The pediatric version
Presenters
Amit K. Pahwa, MD, FAAP; Nicola Orlov, MD, MPH, FAAP
Workshop title
Things we do for no reason (pediatrics)
Session summary
As he began by stating the Institute of Medicine definition of high-value care (HVC), Amit K. Pahwa, MD, of Johns Hopkins Medicine, Baltimore, described HVC as the best care for the patient, with the optimal result for the circumstances, at the right price. But few pediatric residency programs provide education regarding HVC, with only 11% providing a formal HVC curriculum, as found by a survey of pediatric program directors and chief residents in a study published in 2017.
Dr. Pahwa then provided examples of cases in which HVC could be optimized, including reducing rebound bilirubin levels in neonatal hyperbilirubinemia, giving nasogastric feeds instead of IV hydration in bronchiolitis, reducing unnecessary vital sign checks, and providing apple juice supplemented with liquids of choice instead of more expensive oral electrolyte solutions.
Nicola Orlov, MD, of the University of Chicago presented another illustrative case which highlighted the need to reduce vital sign frequency when appropriate. This was linked to her work at Comer Children’s Hospital on reducing nighttime sleep disruptions in hospitalized children, as part of the SIESTA (Sleep for Inpatients: Empowering Staff to Act) study. This led to a significant reduction in nurse/physician interruptions during the study period.
Key takeaways for HM
- High-value care (HVC) is a key focus of systems improvement in the field of pediatric hospital medicine.
- Educational efforts for all levels of learners is inadequate currently, and needs to be augmented.
- Quality improvement projects to promote HVC can lead not only to reduced costs, but improved quality and patient experience.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
The pediatric version
The pediatric version
Presenters
Amit K. Pahwa, MD, FAAP; Nicola Orlov, MD, MPH, FAAP
Workshop title
Things we do for no reason (pediatrics)
Session summary
As he began by stating the Institute of Medicine definition of high-value care (HVC), Amit K. Pahwa, MD, of Johns Hopkins Medicine, Baltimore, described HVC as the best care for the patient, with the optimal result for the circumstances, at the right price. But few pediatric residency programs provide education regarding HVC, with only 11% providing a formal HVC curriculum, as found by a survey of pediatric program directors and chief residents in a study published in 2017.
Dr. Pahwa then provided examples of cases in which HVC could be optimized, including reducing rebound bilirubin levels in neonatal hyperbilirubinemia, giving nasogastric feeds instead of IV hydration in bronchiolitis, reducing unnecessary vital sign checks, and providing apple juice supplemented with liquids of choice instead of more expensive oral electrolyte solutions.
Nicola Orlov, MD, of the University of Chicago presented another illustrative case which highlighted the need to reduce vital sign frequency when appropriate. This was linked to her work at Comer Children’s Hospital on reducing nighttime sleep disruptions in hospitalized children, as part of the SIESTA (Sleep for Inpatients: Empowering Staff to Act) study. This led to a significant reduction in nurse/physician interruptions during the study period.
Key takeaways for HM
- High-value care (HVC) is a key focus of systems improvement in the field of pediatric hospital medicine.
- Educational efforts for all levels of learners is inadequate currently, and needs to be augmented.
- Quality improvement projects to promote HVC can lead not only to reduced costs, but improved quality and patient experience.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
Presenters
Amit K. Pahwa, MD, FAAP; Nicola Orlov, MD, MPH, FAAP
Workshop title
Things we do for no reason (pediatrics)
Session summary
As he began by stating the Institute of Medicine definition of high-value care (HVC), Amit K. Pahwa, MD, of Johns Hopkins Medicine, Baltimore, described HVC as the best care for the patient, with the optimal result for the circumstances, at the right price. But few pediatric residency programs provide education regarding HVC, with only 11% providing a formal HVC curriculum, as found by a survey of pediatric program directors and chief residents in a study published in 2017.
Dr. Pahwa then provided examples of cases in which HVC could be optimized, including reducing rebound bilirubin levels in neonatal hyperbilirubinemia, giving nasogastric feeds instead of IV hydration in bronchiolitis, reducing unnecessary vital sign checks, and providing apple juice supplemented with liquids of choice instead of more expensive oral electrolyte solutions.
Nicola Orlov, MD, of the University of Chicago presented another illustrative case which highlighted the need to reduce vital sign frequency when appropriate. This was linked to her work at Comer Children’s Hospital on reducing nighttime sleep disruptions in hospitalized children, as part of the SIESTA (Sleep for Inpatients: Empowering Staff to Act) study. This led to a significant reduction in nurse/physician interruptions during the study period.
Key takeaways for HM
- High-value care (HVC) is a key focus of systems improvement in the field of pediatric hospital medicine.
- Educational efforts for all levels of learners is inadequate currently, and needs to be augmented.
- Quality improvement projects to promote HVC can lead not only to reduced costs, but improved quality and patient experience.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
Subsegmental PEs overtreated despite link with patient harm
Background: CT pulmonary angiography (CTPA) often detects distal, subsegmental pulmonary embolisms (SSPE) for which there is unclear clinical significance. For these isolated SSPEs, the 2016 CHEST guidelines recommend clinical surveillance in lieu of treatment. Such clinical surveillance has not been associated with an increased recurrence of venous thromboembolism (VTE) over 3 months.
Study design: Retrospective review.
Setting: Tertiary care center in Quebec.
Synopsis: A review of all CTPAs at McGill University in Montreal, from 2014-2016 yielded 222 acute pulmonary emboli (PEs), 71 of which were SSPEs without associated Doppler imaging positive for deep vein thrombosis. Of those 71, 62 (87%) were systemically anticoagulated, compared with 135/143 (94%) of the more proximal PEs. The adverse events of both groups of anticoagulated patients were common and similar. Over the following 3 months, 26 patients in the SSPE group visited the ED or were readmitted (42%; 95% confidence interval, 30%-55%), 21 had a drop in hemoglobin level of 2 g/dL or greater and/or received a blood transfusion (34%; 95% CI, 22%-47%), and 10 died from causes unrelated to VTE (16%; 95% CI, 8%-28%). Limitations of this study included the small number of participants and short time to follow-up.
Bottom line: Although SSPEs have unknown clinical significance, they are being treated with systemic anticoagulation at a similar rate to more proximal PEs and are associated with patient harm.
Citation: Raslan IA et al. Rates of overtreatment and treatment-related adverse effects among patients with subsegmental pulmonary embolism. JAMA Intern Med. 2018 Sep 1;178(9):1272-4.
Dr. Shaw is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: CT pulmonary angiography (CTPA) often detects distal, subsegmental pulmonary embolisms (SSPE) for which there is unclear clinical significance. For these isolated SSPEs, the 2016 CHEST guidelines recommend clinical surveillance in lieu of treatment. Such clinical surveillance has not been associated with an increased recurrence of venous thromboembolism (VTE) over 3 months.
Study design: Retrospective review.
Setting: Tertiary care center in Quebec.
Synopsis: A review of all CTPAs at McGill University in Montreal, from 2014-2016 yielded 222 acute pulmonary emboli (PEs), 71 of which were SSPEs without associated Doppler imaging positive for deep vein thrombosis. Of those 71, 62 (87%) were systemically anticoagulated, compared with 135/143 (94%) of the more proximal PEs. The adverse events of both groups of anticoagulated patients were common and similar. Over the following 3 months, 26 patients in the SSPE group visited the ED or were readmitted (42%; 95% confidence interval, 30%-55%), 21 had a drop in hemoglobin level of 2 g/dL or greater and/or received a blood transfusion (34%; 95% CI, 22%-47%), and 10 died from causes unrelated to VTE (16%; 95% CI, 8%-28%). Limitations of this study included the small number of participants and short time to follow-up.
Bottom line: Although SSPEs have unknown clinical significance, they are being treated with systemic anticoagulation at a similar rate to more proximal PEs and are associated with patient harm.
Citation: Raslan IA et al. Rates of overtreatment and treatment-related adverse effects among patients with subsegmental pulmonary embolism. JAMA Intern Med. 2018 Sep 1;178(9):1272-4.
Dr. Shaw is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: CT pulmonary angiography (CTPA) often detects distal, subsegmental pulmonary embolisms (SSPE) for which there is unclear clinical significance. For these isolated SSPEs, the 2016 CHEST guidelines recommend clinical surveillance in lieu of treatment. Such clinical surveillance has not been associated with an increased recurrence of venous thromboembolism (VTE) over 3 months.
Study design: Retrospective review.
Setting: Tertiary care center in Quebec.
Synopsis: A review of all CTPAs at McGill University in Montreal, from 2014-2016 yielded 222 acute pulmonary emboli (PEs), 71 of which were SSPEs without associated Doppler imaging positive for deep vein thrombosis. Of those 71, 62 (87%) were systemically anticoagulated, compared with 135/143 (94%) of the more proximal PEs. The adverse events of both groups of anticoagulated patients were common and similar. Over the following 3 months, 26 patients in the SSPE group visited the ED or were readmitted (42%; 95% confidence interval, 30%-55%), 21 had a drop in hemoglobin level of 2 g/dL or greater and/or received a blood transfusion (34%; 95% CI, 22%-47%), and 10 died from causes unrelated to VTE (16%; 95% CI, 8%-28%). Limitations of this study included the small number of participants and short time to follow-up.
Bottom line: Although SSPEs have unknown clinical significance, they are being treated with systemic anticoagulation at a similar rate to more proximal PEs and are associated with patient harm.
Citation: Raslan IA et al. Rates of overtreatment and treatment-related adverse effects among patients with subsegmental pulmonary embolism. JAMA Intern Med. 2018 Sep 1;178(9):1272-4.
Dr. Shaw is an assistant professor in the division of hospital medicine, University of New Mexico.
When is electroconvulsive therapy (ECT) indicated?
Know the general work-up and contraindications
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
Know the general work-up and contraindications
Know the general work-up and contraindications
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
By the numbers: Readmissions for skin conditions
Almost 10% of patients
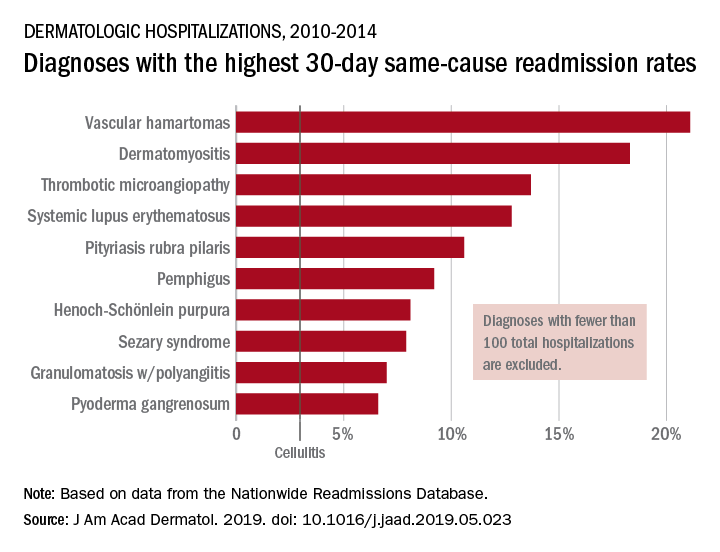
Data from the Nationwide Readmissions Database also showed that the same-cause readmission rate was 3.3% after 30 days and 7.8% within the calendar year (CY) over the 5-year study period of 2010-2014, Myron Zhang, MD, of the department of dermatology at Weill Cornell Medicine, New York, and his associates reported in the Journal of the American Academy of Dermatology.
The total cost of the CY readmissions was $2.54 billion, which works out to $508 million per year or $8,995 per visit. The most common dermatologic diagnosis – cellulitis made up 83.6% of all hospitalizations – was also the most expensive in terms of readmissions, resulting in $1.9 billion in CY costs, Dr. Zhang and associates wrote.
Overall readmission rates for cellulitis were not provided, but annual rates ranged from 9.1% to 9.3% (30-day all cause), from 7.7% to 8.1% (CY same cause), and from 3.1% to 3.3% (30-day same cause), they wrote.
The dermatologic diagnosis with the highest 30-day same-cause readmission rate was vascular hamartomas at 21.1%, followed by dermatomyositis (18.3%) and thrombotic microangiopathy (13.7%). Dermatomyositis had the highest CY same-cause readmission rate (30.8%) and mycosis fungoides had the highest 30-day all-cause rate (32.3%), according to the investigators.
“Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well studied,” Dr. Zhang and associates wrote. They noted that there have been “very few prior studies of readmissions for skin diseases.”
[email protected]
SOURCE: Zhang M et al. J Am Acad. Dermatol. 2019. doi: 10.1016/j.jaad.2019.05.023. .
Almost 10% of patients
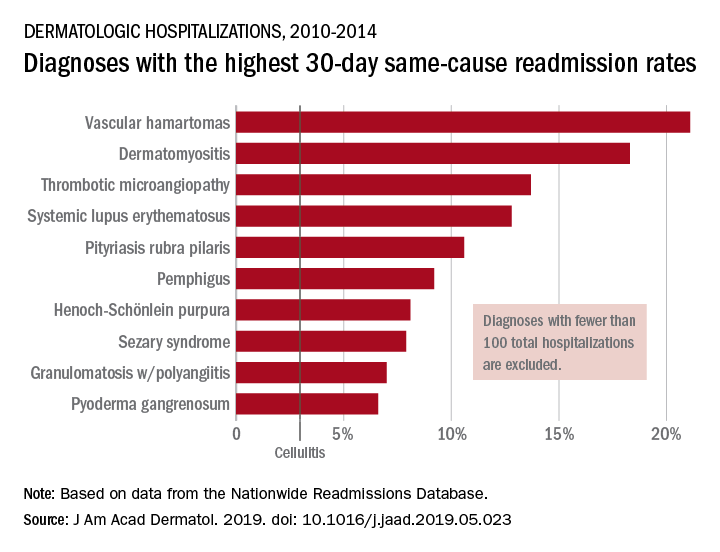
Data from the Nationwide Readmissions Database also showed that the same-cause readmission rate was 3.3% after 30 days and 7.8% within the calendar year (CY) over the 5-year study period of 2010-2014, Myron Zhang, MD, of the department of dermatology at Weill Cornell Medicine, New York, and his associates reported in the Journal of the American Academy of Dermatology.
The total cost of the CY readmissions was $2.54 billion, which works out to $508 million per year or $8,995 per visit. The most common dermatologic diagnosis – cellulitis made up 83.6% of all hospitalizations – was also the most expensive in terms of readmissions, resulting in $1.9 billion in CY costs, Dr. Zhang and associates wrote.
Overall readmission rates for cellulitis were not provided, but annual rates ranged from 9.1% to 9.3% (30-day all cause), from 7.7% to 8.1% (CY same cause), and from 3.1% to 3.3% (30-day same cause), they wrote.
The dermatologic diagnosis with the highest 30-day same-cause readmission rate was vascular hamartomas at 21.1%, followed by dermatomyositis (18.3%) and thrombotic microangiopathy (13.7%). Dermatomyositis had the highest CY same-cause readmission rate (30.8%) and mycosis fungoides had the highest 30-day all-cause rate (32.3%), according to the investigators.
“Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well studied,” Dr. Zhang and associates wrote. They noted that there have been “very few prior studies of readmissions for skin diseases.”
[email protected]
SOURCE: Zhang M et al. J Am Acad. Dermatol. 2019. doi: 10.1016/j.jaad.2019.05.023. .
Almost 10% of patients
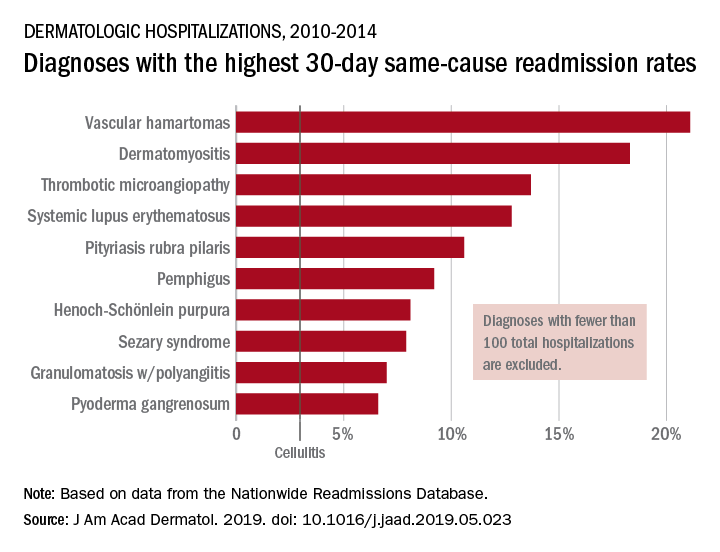
Data from the Nationwide Readmissions Database also showed that the same-cause readmission rate was 3.3% after 30 days and 7.8% within the calendar year (CY) over the 5-year study period of 2010-2014, Myron Zhang, MD, of the department of dermatology at Weill Cornell Medicine, New York, and his associates reported in the Journal of the American Academy of Dermatology.
The total cost of the CY readmissions was $2.54 billion, which works out to $508 million per year or $8,995 per visit. The most common dermatologic diagnosis – cellulitis made up 83.6% of all hospitalizations – was also the most expensive in terms of readmissions, resulting in $1.9 billion in CY costs, Dr. Zhang and associates wrote.
Overall readmission rates for cellulitis were not provided, but annual rates ranged from 9.1% to 9.3% (30-day all cause), from 7.7% to 8.1% (CY same cause), and from 3.1% to 3.3% (30-day same cause), they wrote.
The dermatologic diagnosis with the highest 30-day same-cause readmission rate was vascular hamartomas at 21.1%, followed by dermatomyositis (18.3%) and thrombotic microangiopathy (13.7%). Dermatomyositis had the highest CY same-cause readmission rate (30.8%) and mycosis fungoides had the highest 30-day all-cause rate (32.3%), according to the investigators.
“Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well studied,” Dr. Zhang and associates wrote. They noted that there have been “very few prior studies of readmissions for skin diseases.”
[email protected]
SOURCE: Zhang M et al. J Am Acad. Dermatol. 2019. doi: 10.1016/j.jaad.2019.05.023. .
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Restrictive transfusion strategy in cardiac surgery remains noninferior
Clinical question: Does using a restrictive transfusion strategy with patients undergoing cardiac surgery affect long-term outcomes?
Background: Using a restrictive transfusion strategy in patients undergoing cardiac surgery is known to use fewer units of allogeneic red cells, compared with a liberal strategy, while still having noninferior short-term clinical outcomes. At this time, little is known about such a strategy’s long-term effects.
Study design: Randomized, open-label, noninferiority trial.
Setting: 74 hospitals in 19 countries.
Synopsis: 5,243 adults undergoing nontransplant cardiac surgeries and having at least a moderate predicted risk for death were randomly divided into a liberal or restrictive transfusion strategy. Restrictive-strategy participants received a transfusion when hemoglobin was less than 7.5 g/dL, compared with either a hemoglobin of 8.5 g/dL on the floor or 9.5 g/dL in the ICU for the liberal-strategy group. During the hospitalization, the restrictive group received fewer U of red cells and had a lower mean predischarge hemoglobin. At 6 months, the groups were compared for the primary outcomes of death, MI, stroke, or renal failure requiring dialysis, finding an occurrence of such in 402/2,317 in the restrictive-strategy group and 402/2,347 in the liberal-strategy group (P = .006 for noninferiority). Limitations include the study being a noninferiority trial and the very specific patient population selected.
Bottom line: In patients undergoing cardiac surgery, a restrictive transfusion strategy is noninferior to a liberal strategy with respect to death from any cause, MI, stroke, and new renal failure requiring dialysis at 6 months postop.
Citation: Mazer CD et al. Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Eng J Med. 2018 Sep 27;379(13):1224-33.
Dr. Shaw is an assistant professor in the division of hospital medicine,University of New Mexico.
Clinical question: Does using a restrictive transfusion strategy with patients undergoing cardiac surgery affect long-term outcomes?
Background: Using a restrictive transfusion strategy in patients undergoing cardiac surgery is known to use fewer units of allogeneic red cells, compared with a liberal strategy, while still having noninferior short-term clinical outcomes. At this time, little is known about such a strategy’s long-term effects.
Study design: Randomized, open-label, noninferiority trial.
Setting: 74 hospitals in 19 countries.
Synopsis: 5,243 adults undergoing nontransplant cardiac surgeries and having at least a moderate predicted risk for death were randomly divided into a liberal or restrictive transfusion strategy. Restrictive-strategy participants received a transfusion when hemoglobin was less than 7.5 g/dL, compared with either a hemoglobin of 8.5 g/dL on the floor or 9.5 g/dL in the ICU for the liberal-strategy group. During the hospitalization, the restrictive group received fewer U of red cells and had a lower mean predischarge hemoglobin. At 6 months, the groups were compared for the primary outcomes of death, MI, stroke, or renal failure requiring dialysis, finding an occurrence of such in 402/2,317 in the restrictive-strategy group and 402/2,347 in the liberal-strategy group (P = .006 for noninferiority). Limitations include the study being a noninferiority trial and the very specific patient population selected.
Bottom line: In patients undergoing cardiac surgery, a restrictive transfusion strategy is noninferior to a liberal strategy with respect to death from any cause, MI, stroke, and new renal failure requiring dialysis at 6 months postop.
Citation: Mazer CD et al. Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Eng J Med. 2018 Sep 27;379(13):1224-33.
Dr. Shaw is an assistant professor in the division of hospital medicine,University of New Mexico.
Clinical question: Does using a restrictive transfusion strategy with patients undergoing cardiac surgery affect long-term outcomes?
Background: Using a restrictive transfusion strategy in patients undergoing cardiac surgery is known to use fewer units of allogeneic red cells, compared with a liberal strategy, while still having noninferior short-term clinical outcomes. At this time, little is known about such a strategy’s long-term effects.
Study design: Randomized, open-label, noninferiority trial.
Setting: 74 hospitals in 19 countries.
Synopsis: 5,243 adults undergoing nontransplant cardiac surgeries and having at least a moderate predicted risk for death were randomly divided into a liberal or restrictive transfusion strategy. Restrictive-strategy participants received a transfusion when hemoglobin was less than 7.5 g/dL, compared with either a hemoglobin of 8.5 g/dL on the floor or 9.5 g/dL in the ICU for the liberal-strategy group. During the hospitalization, the restrictive group received fewer U of red cells and had a lower mean predischarge hemoglobin. At 6 months, the groups were compared for the primary outcomes of death, MI, stroke, or renal failure requiring dialysis, finding an occurrence of such in 402/2,317 in the restrictive-strategy group and 402/2,347 in the liberal-strategy group (P = .006 for noninferiority). Limitations include the study being a noninferiority trial and the very specific patient population selected.
Bottom line: In patients undergoing cardiac surgery, a restrictive transfusion strategy is noninferior to a liberal strategy with respect to death from any cause, MI, stroke, and new renal failure requiring dialysis at 6 months postop.
Citation: Mazer CD et al. Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Eng J Med. 2018 Sep 27;379(13):1224-33.
Dr. Shaw is an assistant professor in the division of hospital medicine,University of New Mexico.